Abstract
Prescription stimulant misuse (PSM) is common in young adult college students, at over 10% in the past year, and it is associated with other substance use and risk behaviors. Research focused on the real-time drivers of PSM is absent, impeding prevention and intervention. This research aimed to fill that gap by examining the relationships between affect, global stress, or academic stress and PSM via ecological momentary assessment (EMA); we also investigated baseline predictors of PSM frequency during the 21-day EMA period. Forty-one full-time college students (mean age: 20.5, 66% female) who endorsed current PSM (≥ 6 past-year episodes) participated. Participants were asked to complete EMA questions in response to three daily investigator-initiated prompts and after every PSM episode. Assessments were selected based on affect regulation (e.g., positive affect [PA], negative affect [NA]) and drug instrumentalization (e.g., academic stress and/or demands) theories of substance use. Mixed effects linear models examined EMA data, and negative binomial regression analyses examined baseline predictors of PSM episode frequency. PA was higher on PSM days and increased post-PSM, whereas NA was unrelated to PSM. Although global and academic stress were largely unrelated to PSM, when the motive endorsed for PSM was “to study”, pre-PSM ratings of academic demand and stress were significantly higher. Finally, a history of recreational motives (e.g., to get high) or higher levels of ADHD symptoms predicted a greater number of PSM episodes over the EMA period. The results offered mixed support for both affect regulation and instrumentalization as applied to PSM.
Keywords: prescription stimulant, prescription misuse, college student, affect, stress
Prescription stimulant misuse (PSM), or misuse of medications commonly prescribed for symptoms of Attention Deficit Hyperactivity Disorder (Clemow & Walker, 2014), is most common in young adults, 18–25 years (Ford & Pomykacz, 2016; McCabe, West, Teter, & Boyd, 2014). Full-time college students and recent college graduates evidence the highest past-year PSM prevalence rates: 10.3% and 11.2%, respectively; these are significantly higher than the 5.6% and 4.4% among high school graduates and those who dropped out, respectively (Schepis, Teter, & McCabe, 2018).
PSM is commonly defined as use without a prescription or use of one’s own stimulant medication in ways not intended by the prescriber (e.g., greater doses, non-oral administration), and it is associated with concerning correlates, such as poorer academic performance (Arria & DuPont, 2010) and problematic other substance use (Schepis, Acheson, Zapp, & Swartzwelder, 2019; Weyandt et al., 2013). PSM in college students is mainly motivated by perceived academic enhancement, such as to promote focus, concentration or studying, and/or to improve one’s GPA (DeSantis, Webb, & Noar, 2008; Norman & Ford, 2018). Despite this, the evidence suggests no academic benefit from PSM (e.g., Garnier-Dykstra, Caldeira, Vincent, O’Grady, & Arria, 2012; McCabe, Knight, Teter, & Wechsler, 2005).
Little work has examined proximal influences on college student PSM. Research evaluating real-time PSM risk factors via ecological momentary assessment (EMA) could provide a better understanding of proximal causal relationships between PSM and theoretically important variables, such as affect and stress. Affect regulation models posit that substance use is prompted to reduce negative affect (NA), increase positive affect (PA), and/or improve emotional control (Cheetham, Allen, Yucel, & Lubman, 2010), though many models emphasize NA reduction, especially for physiological dependence (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Zorrilla & Koob, 2019). Drug instrumentalization (Muller & Schumann, 2011) suggests that substance use is an instrument to achieve an outcome, like affective changes or perceived academic enhancement for PSM. In college students, limited research suggests that expectation of stimulant receipt is associated with increases in PA and NA (Looby & Earleywine, 2011), and PSM is associated with higher global stress levels (Dussault & Weyandt, 2013). Also, as key motives for college student PSM relate to academic enhancement, PSM may be driven by academic stress.
Aims and Hypotheses
This study used EMA techniques, with two aims: 1) evaluate the relationships between affect or stress and PSM over a 21-day EMA period, and 2) investigate baseline predictors of PSM frequency in the 21-day EMA period. For the first aim, we hypothesized that PSM would be linked to prospective increases in PA and decreases in NA; we also expected episodes of PSM when pre-PSM episode PA is lower, NA is higher, and with elevated stress levels, especially academic stress. For the second aim, we hypothesized that more frequent PSM will be predicted by greater levels of trait impulsivity, delay discounting, ADHD symptoms, and by a history of recreational motives, which is associated with greater concurrent risk behavior among those engaged in PSM (McCabe, Boyd, & Teter, 2009).
METHODS
Participants
Forty-five full-time college students signed informed consent; 41 completed the baseline session and EMA period. Eligibility criteria: 18–25 years; able to read/write in English; enrolled in ≥9 hours (i.e., full-time student); engaged in ≥6 past-year PSM episodes; and owned an iOS (Apple) or Android smartphone. The criterion of 6 or more PSM episodes is more stringent than other survey- (Holt & Looby, 2018; Smith, Martel, & DeSantis, 2017) and lab-based (Looby & Earleywine, 2011; Wilens et al., 2017) assessments of PSM, necessitated by a need to maximize likelihood of episodes in the EMA period; other criteria were consistent with past PSM research. The final sample of 41 participants were 66% female (n=27), primarily Caucasian, non-Latinx (56%, n=23) or Latinx (29%, n=12), with a mean age of 20.5 (SD=1.57). Participants came from 26 undergraduate majors, though the modal major was Psychology (n=13). Fifteen (36.6%) had a current stimulant medication prescription.
Procedures
Participants were recruited via campus flyers, TV signboard announcements, and emails by professors to classes. The emails were primarily from Psychology professors, but professors in Biology, Chemistry, and Engineering also sent emails. Interested students were phone screened using a structured questionnaire assessing the eligibility criteria, and those meeting criteria were scheduled for a baseline appointment. After obtaining informed consent, participants’ past-year PSM frequency was assessed to confirm eligibility. Participants then completed baseline assessments via computer. Next, study staff helped the participant download and understand the EMA app’s functions; the EMA platform was from LifeData, Inc.
Following the baseline appointment, participants completed the 21-day EMA phase. The 21-day duration was based on past research in alcohol and tobacco use (e.g., Berkman, Dickenson, Falk, & Lieberman, 2011; O’Donnell et al., 2019). Participants completed two types of assessments. First, signal-contingent assessments were completed upon receipt of a prompt. Participants were signaled at three semi-random times daily, within three blocks (9AM–2PM; 2–7PM; and 7PM–12AM). Per participant self-report of their typical daily sleep-wake cycle, time blocks were altered by up to two hours in either direction to ensure prompts were sent when participants were typically awake. After a prompt was sent, the participant had 90 minutes to complete the survey to prevent participants from answering multiple surveys retrospectively (Shiffman, Stone, & Hufford, 2008). Second, event-contingent assessments were completed as soon as possible when participants engaged in PSM. The same questions were used in both types of survey. Participants were paid $20 for completing the screening, $1 for each completed EMA survey, and a $20 bonus for completing ≥80% of the signal-contingent surveys. All procedures were approved by the Texas State University IRB.
Measures
More detail on measures is in Supplemental Table A, with means and ranges of the baseline measures in Supplemental Table B.
EMA Measures
First, participants were asked about PSM episodes: “Have you misused a stimulant since the last survey? That is, have you used your own stimulant medication in a way your doctor did not intend or have you used another person’s stimulant medication?” This definition is consistent with those of the National Survey on Drug Use and Health (NSDUH) and the National Epidemiologic Survey on Alcohol and Related Conditions-III (Center for Behavioral Health Statistics and Quality, 2018; Grant et al., 2014). Participants were instructed that “in a way your doctor did not intend” included increasing the dose, taking more often than prescribed, and non-oral administration.
In those endorsing PSM, a follow-up question assessed PSM motives, based on McCabe and Cranford (2012); PSM sources were assessed using items from McCabe and colleagues (2019). The International Positive and Negative Affect Scale, Short Form (I-PANAS-SF; Thompson, 2007) captured current affective state, and the 4-item Perceived Stress Scale (PSS-4; Cohen, Kamarck, & Mermelstein, 1983; Lee, 2012) assessed current perceived global stress. The PSS-4 was modified to fit the EMA aims by focusing on time since last survey.
Four constructs were measured via 100-point visual analogue scales (VAS): emotional control, academic stress, academic demands, and academic self-efficacy. No significant differences were found between VAS and Likert scale ratings across many measures (Cook, Heath, Thompson, & Thompson, 2001; Couper, Tourangeau, Conrad, & Singer, 2006), suggesting utility when fewer items are required.
Baseline Measures
Sociodemographics included: age, sex (male/female/transgender), race/ethnicity (Latinx/Caucasian/African-American/Asian-American/American Indian-Native American), and grade point average.
The Adult ADHD Self-Report Scale (ASRS) screener assessed ADHD symptoms over the past 6 months (Kessler et al., 2005; van de Glind et al., 2013). The Short UPPS-P Impulsive Behavior scale (SUPPS-P) captured trait impulsivity, with five subscales: negative urgency, positive urgency, lack of premeditation, lack of perseverance, and sensation seeking (Cyders, Littlefield, Coffey, & Karyadi, 2014). Delay discounting was measured through the 27-item Monetary Choice Questionnaire from Kirby and colleagues (1999), scored via spreadsheet from Kaplan and colleagues (2016).
The Stimulant Survey Questionnaire (SSQ; Weyandt et al., 2009) provided single-item questions for lifetime co-ingestion with alcohol and non-oral PSM (e.g., snorting, smoking, and/or injection). A single-item assessment of lifetime PSM motives was used, with motives classified as any recreational motives and self-treatment only motives; a single-item assessment of lifetime PSM sources was used, with single versus multiple source use captured. Co-ingestion and non-oral PSM, recreational motives, and multiple source use are associated with poorer outcomes (McCabe et al., 2019; McCabe, West, Schepis, & Teter, 2015; Messina et al., 2016).
Data Analyses
EMA
Analyses occurred in PASW version 23.0. All models included a random effect for subject and fixed effects for other predictors. Pseudo R-squared values were calculated using error terms from the unrestricted and restricted models, per Kreft and de Leeuw (1998). The cross-sectional and prospective relationships affect to PSM were evaluated in four separate ways. First at the daily level, mixed effects linear models compared mean affect levels on PSM versus non-PSM days. Data were aggregated by participant and day, creating an average daily affect ratings by participant. Days were dummy coded (0=non-PSM, 1=PSM). At the concurrent momentary level, GLMs evaluated whether momentary levels of predictor variables were related to PSM at that time point. Next, the temporal pattern of affect and PSM was evaluated using mixed effects linear models. Specifically, pre- and post-PSM affect was modeled using linear, quadratic and cubic effects centered around the first daily PSM episode. These models included a random effect for subjects, and fixed effects for minutes, minutes2, and minutes3 (all prior to/after PSM), as well as interactions between these time components and pre/post-PSM status.
Participants completed a mean of 83.4% (SD=19.0%; range=24–100%) of signal-contingent prompts. Participants evinced comparable completion rates on PSM (85.5%) and non-PSM days (85.4%). These rates are higher than those in other EMA studies of substance use in non-treatment samples (e.g., Buckner et al., 2015; Hopper et al., 2006). Although GLM allows for missing data, we excluded days where ≥50% of the ratings were missing (Crosby et al., 2009); thus, 321 observations (11.8%) were excluded. Participants completed 2,290 signal-contingent and 101 event-contingent assessments.
PSM Episode Number
These analyses were conducted in STATA 16.0, using a log-linear approach. As variance greatly exceeded the mean of PSM episodes, a negative binomial model was used (Agresti, 2014). Fit statistics from analyses supported negative binomial model use. Only one of 41 participants had zero PSM episodes, meaning a zero-inflated model was unnecessary. Initial negative binomial regressions were univariable, with predictors retained when p≤0.25 for a second, multivariable model (Hosmer & Lemeshow, 2000). Predictors were sociodemographics, trait impulsivity, delay discounting, ADHD symptom level, lifetime co-ingestion with alcohol, lifetime recreational motives, and lifetime non-oral PSM.
RESULTS
EMA Outcomes
Participants recorded 258 prescription stimulant misuse (PSM) episodes in the 21-day EMA period (M=6.61, SD= 4.92), for an average of 0.38 (SD= 0.7) PSM episodes per day during the 21-day EMA period. When PSM occurred, 88.8% of days had one PSM episode, 10.8% two, and 0.4% three. The most common sources were using one’s own medication (36.0%), buying from a friend (27.8%), free from friend/roommate (18.8%), or buying from a stranger/dealer (12.5%). The most common medication used for PSM was Adderall (65.1% of episodes), followed by Vyvanse (23.0%), and generic methylphenidate (3.6%); other medications were used in 8.3% of episodes.
At the daily level, mean level of positive affect (PA) was greater on PSM days (Table 1). We next examined whether PSM use days were associated with specific types of PA by examining whether use day differed on individual PANAS-PA items. On PSM days, participants were more alert (p<.001), determined (p=.044), and attentive (p<.001). Both overall negative affect (NA) and PANAS-NA items were unrelated to PSM, as were Perceived Stress Scale (PSS-4) total score and items, and visual analogue scale (VAS) measures. At the concurrent momentary level (i.e., relations among PSM use and affect at each individual assessment period), PA was related to PSM, suggesting increased PA after PSM. Regarding specific PANAS-PA items, participants reported feeling significantly more alert (p<.001), inspired (p=.004), determined (p<.001), attentive (p<.001), and active (p=.005) after PSM. Neither total NA nor individual PANAS-NA items were related to PSM. PSS-4 total was significantly related to PSM (Table 1), with decreases in global stress around the PSM episode (p=.042).
Table 1:
Relations of Affect with Prescription Stimulant Misuse (PSM) when assessed by (1) Whether PSM occurred that Day, and (2) Momentary Relations between Predictors and PSM
| PSM | No PSM | |||||
|---|---|---|---|---|---|---|
| Predictor | M (SD) | M (SD) | β | SE | p | 95% CI |
| PSM Day Status | ||||||
| Negative affect | 8.57 (3.76) | 8.50 (3.68) | .01 | .03 | .865 | .057, .068 |
| Positive affect | 15.24 (4.85) | 13.55 (4.48) | .08 | .03 | .004 | .025, .135 |
| Perceived Stress (PSS-4) | 7.53 (1.91) | 7.43 (1.81) | .03 | .05 | .539 | −.064, .123 |
| Momentary PSM | ||||||
| Negative affect | 8.67 (3.54) | 8.50 (3.72) | .01 | .03 | .694 | −.050, .075 |
| Positive affect | 17.04 (4.86) | 13.64 (4.46) | .17 | .04 | <.001 | .087, .251 |
| Perceived Stress (PSS-4) | 7.73 (1.76) | 7.43 (1.84) | .09 | .04 | .042 | .003, .177 |
Temporal patterns between PSM and affect were examined by determining pre-/post-PSM affect patterns affect. Although PA did not significantly change prior to PSM, (p=.115), it increased significantly post-PSM, B=−1.86, SE=.81, p=.023 (Figure 1). NA did not significantly change before (p=.683) or after PSM (p= .805). No VAS or PSS-4 item (nor PSS-4 total score) were prospectively related to PSM.
Figure 1:
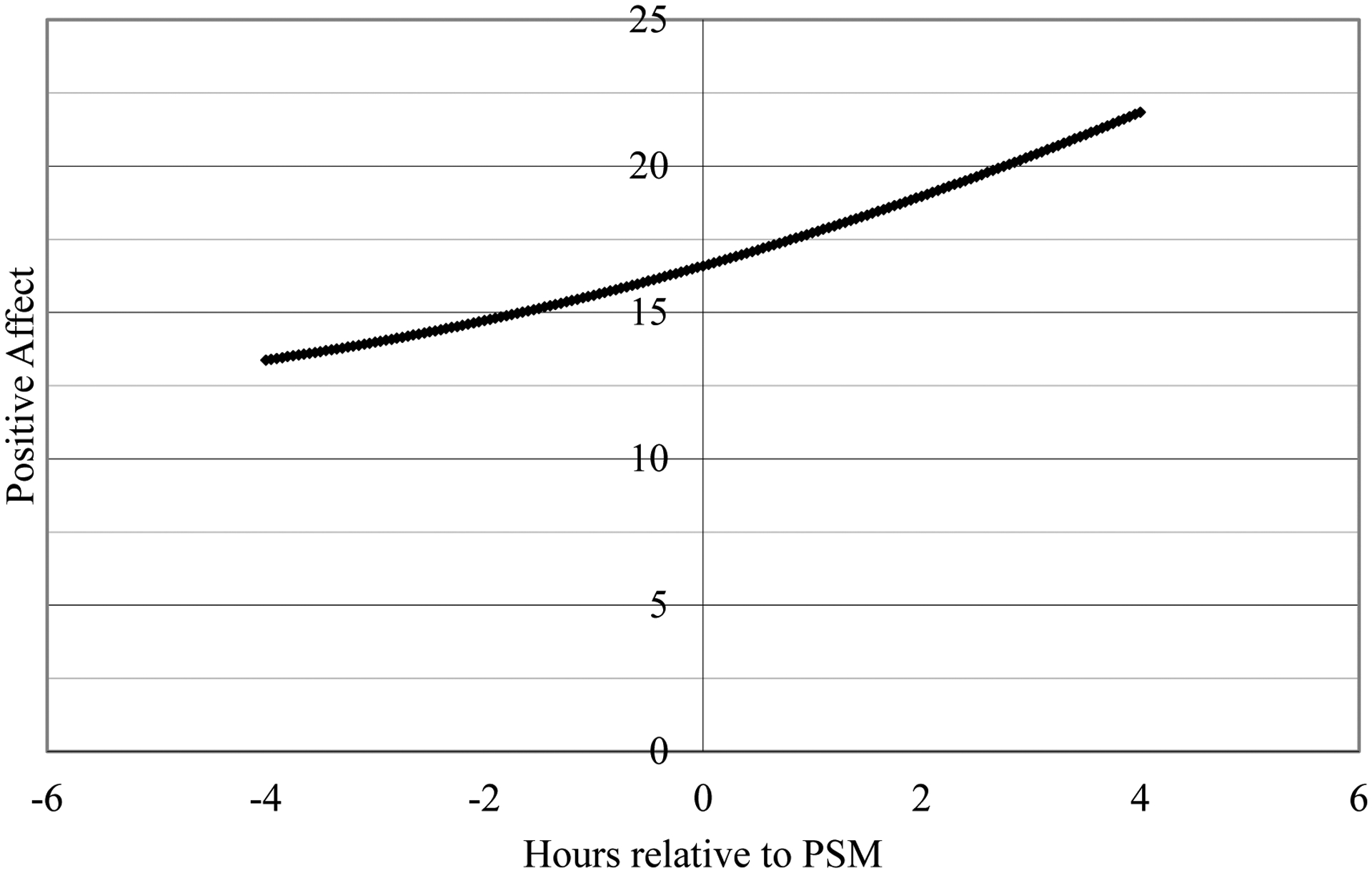
Temporal Relationship between Positive Affect and PSM Episodes
Positive affect (PA) did not increase or decrease at a significant rate prior to PSM (B= 1.06, SE= .67, p = .115), but it increased at a significant rate following PSM (B= −1.86, SE= .81, p= .023).
PA was summed scores for current ratings of “alert”, “inspired”, “determined”, “attentive”, “active” on a 5-point Likert scale (1: “not at all” to 5: “always”).
The most common non-mutually exclusive PSM motives were to concentrate (72.1%), study better (66.3%), and stay awake (57.0%). Less common motives were to feel better/get high (17.4%) and lose weight (9.3%). Participants reported that their most important PSM motive was to study better (36.8%), concentrate (28.3%), stay awake (23.3%), or feel better/get high (7.0%). During PSM, at the concurrent level, using to study was significantly related to academic stress, B=.02, SE=.01, p=.007, academic demand, B=.02, SE=.01, p=.007, and the PSS-4 item about difficulties piling up, B=.38, SE=.12, p=.002,.
PSM Episode Number
Demographics, all short UPPS-P Impulsive Behavior (SUPPS-P) subscales, delay discounting, and lifetime multiple source use were excluded from multivariable analyses (i.e., p>0.25). In the multivariable regression, ADHD symptom level (coefficient=0.03, SE=0.01, p=0.011) and a history of recreational motives (coefficient=0.49, SE=0.25, p=0.046) significantly predicted number of PSM episodes. Those with a history of recreational motives had a mean of 9.06 PSM episodes (SD=6.75), while those with self-treatment only motives had 5.40 (SD=4.09).
DISCUSSION
Our hypotheses were: (1) PSM would be linked to prospective increases in PA and decreased NA; (2) episodes of PSM would occur when pre-PSM episode PA is lower, NA is higher, and with elevated stress levels, especially academic stress; (3) more frequent PSM will be predicted by greater levels of trait impulsivity, delay discounting, ADHD symptoms, and by a history of recreational motives.
In all, PA enhancement was a key momentary factor in PSM. PA was higher on PSM days and increased in the hours following PSM episodes, while NA was unrelated to PSM. This is not consistent with affect regulation models that emphasize NA (e.g., Baker et al., 2004) or EMA findings evaluating NA-cannabis relationships (Buckner et al., 2015), suggesting that affect regulation may vary by type of substance use. Alternatively, Cheetham and colleagues (2010) proposed that PA enhancement is more important in early substance use. PSM initiation increases notably in late adolescence and early adulthood, so many participants may be recent initiators and in an earlier phase of PSM where PA enhancement is key.
Notably, PSM appeared to increase alertness, attentiveness and activity, which are components of PA and states that can enhance academic work. Thus, college students may engage in PSM for both PA enhancement and perceived academic benefit, consistent with the most common college student PSM motives (McCabe et al., 2009). College students at-risk for PSM or engaged in PSM could benefit from increased exposure to non-drug reinforcers, including greater one-on-one attention from peer counselors or more on-campus programming, that increase PA and reduce PSM likelihood (Carroll, 1996). Greater availability of on-campus treatments fostering positive coping and non-drug PA should be considered (e.g., cognitive-behavioral and mindfulness-based therapies), though research on the PA-specific effects of substance use treatment is limited (Boden, Heinz, & Kashdan, 2016; Kang, Fairbairn, & Ariss, 2019).
The EMA results for global and academic stress were less clear. Higher global stress potentially prompted PSM in the moment, but global stress did not decrease post-PSM. Thus, PSM may not successfully decrease overall stress. PSM episodes motivated by studying were associated with higher levels of self-reported academic stress and demands, despite perceived academic stress or demands not decreasing post-PSM. This is consistent with a drug instrumentalization model (Muller & Schumann, 2011), with PSM intended to improve academic outcomes. It is also consistent with the cross-sectional and longitudinal evidence on college student PSM, where PSM is more likely in those who perceive academic benefits (Arria et al., 2018), despite a lack of tangible benefits (Arria et al., 2013). Taken together, it may be useful to provide psychoeducation on the lack of impact of PSM on global and academic stress in college student treatment and prevention efforts.
Finally, number of PSM episodes over the EMA period was predicted by a history of recreational motives and higher levels of ADHD symptoms. All participants with past recreational motives also endorsed past self-treatment motives, and it is not surprising that individuals with a greater variety of motives would more frequently engage in PSM. Also, individuals engaged in PSM have a greater likelihood of an ADHD diagnosis or elevated ADHD symptoms (Wilens et al., 2016). Although this and past findings may reflect that students with ADHD have greater stimulant medication access, facilitating PSM, research is needed to clarify the complex and unclear causal relationships between ADHD symptoms and PSM.
Limitations
First, the study is limited by the smaller sample, and future studies should examine these theories in larger samples. Also, the college student sample does not generalize to non-college young adults (Schepis et al., 2018), and our sample was more female and Caucasian than young adults overall. Also, some measures had poorer psychometrics than longer versions or were created for this study, prompted by the need for brief measures to maximize EMA data completeness (Short et al., 2018). We also did not assess correlates such depression, anxiety, or substance use disorder symptoms and diagnosis, and factors like age of PSM initiation and self-report of perceived academic enhancement after PSM episodes or after completion of the EMA period; future studies should assess these. Finally, these data have the inherent limitations of self-report data.
Conclusions
This EMA study provided evidence for both affective regulation, especially PA enhancement, and drug instrumentalization theories, as applied to college student PSM. While the EMA data did not support a relationship between NA and PSM, most participants are likely to be recent PSM initiators and unlikely to experience PSM-related NA (e.g., withdrawal). Notably, many individual PA items are potentially academic enhancement motives (e.g., alertness, attentiveness, and activity). Thus, PSM may be an instrument to both enhance PA and academic performance, even if the evidence supports no such benefit (Arria et al., 2017).
Supplementary Material
PUBLIC SIGNIFICANCE STATEMENT.
This study suggests that prescription stimulant misuse (PSM) in college students is likely motivated both by a desire to increase pleasurable feelings (i.e., positive affect) and increase states that facilitate studying, like alertness. Prevention and intervention programs that promote non-drug pleasurable activities, organizational and study skills, and provide psychoeducation on the lack of academic benefit from PSM could help limit college student PSM.
DISCLOSURES AND ACKNOWLEDGEMENTS
This work was funded by R03 DA041584 from the National Institute on Drug Abuse (NIDA). The content is the authors’ responsibility and does not necessarily represent the views of NIDA, and NIDA had no role in the design of the study, the analyses, interpretation of results or the decision to submit the manuscript for publication.
There are no further acknowledgements.
Footnotes
These data were presented in a symposium at the 2018 Association of Behavioral and Cognitive Therapists Annual Convention and in a poster session at the 2018 Collaborative Perspectives on Addiction Annual Meeting.
The authors have no conflicts of interest.
Finally, this manuscript has not been posted to a preprint server or archive.
Contributor Information
Ty S. Schepis, Department of Psychology, Texas State University, San Marcos, Texas, USA
Julia D. Buckner, Department of Psychology, Louisiana State University, Baton Rouge, Louisiana, USA
Dalton L. Klare, Department of Psychology, Texas State University, San Marcos, Texas, USA
Lauren R. Wade, Department of Psychology, Texas State University, San Marcos, Texas, USA
Natalie Benedetto, Wellness 360 Therapy, Dallas, Texas, USA
REFERENCES
- Agresti A (2014). Categorical Data Analysis (3rd ed.). Hoboken, NJ: Wiley. [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, O’Grady KE, Cimini MD, Geisner IM, … Larimer ME (2017). Do college students improve their grades by using prescription stimulants nonmedically? Addict Behav, 65, 245–249. doi: 10.1016/j.addbeh.2016.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, & DuPont RL (2010). Nonmedical prescription stimulant use among college students: why we need to do something and what we need to do. J Addict Dis, 29(4), 417–426. doi: 10.1080/10550887.2010.509273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Geisner IM, Cimini MD, Kilmer JR, Caldeira KM, Barrall AL, … Larimer ME (2018). Perceived academic benefit is associated with nonmedical prescription stimulant use among college students. Addict Behav, 76, 27–33. doi: 10.1016/j.addbeh.2017.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Wilcox HC, Caldeira KM, Vincent KB, Garnier-Dykstra LM, & O’Grady KE (2013). Dispelling the myth of “smart drugs”: cannabis and alcohol use problems predict nonmedical use of prescription stimulants for studying. Addict Behav, 38(3), 1643–1650. doi: 10.1016/j.addbeh.2012.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev, 111(1), 33–51. doi: 10.1037/0033-295X.111.1.33 [DOI] [PubMed] [Google Scholar]
- Berkman ET, Dickenson J, Falk EB, & Lieberman MD (2011). Using SMS text messaging to assess moderators of smoking reduction: Validating a new tool for ecological measurement of health behaviors. Health Psychol, 30(2), 186–194. doi: 10.1037/a0022201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden MT, Heinz AJ, & Kashdan TB (2016). Pleasure as an Overlooked Target of Substance Use Disorder Research and Treatment. Curr Drug Abuse Rev, 9(2), 113–125. doi: 10.2174/1874473710666170308163310 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Crosby RD, Wonderlich SA, Ecker AH, & Richter AA (2015). Antecedents and consequences of cannabis use among racially diverse cannabis users: an analysis from ecological momentary assessment. Drug and Alcohol Dependence, 147, 20–25. doi: 10.1016/j.drugalcdep.2014.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll ME (1996). Reducing drug abuse by enriching the environment with alternative nondrug reinforcers. In Green L & Kagel JH (Eds.), Advances in behavioral economics, Vol. 3: Substance use and abuse (pp. 37–68). Westport, CT: Ablex Publishing. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2018). 2017 National Survey on Drug Use and Health Public Use File Codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration [Google Scholar]
- Cheetham A, Allen NB, Yucel M, & Lubman DI (2010). The role of affective dysregulation in drug addiction. Clin Psychol Rev, 30(6), 621–634. doi: 10.1016/j.cpr.2010.04.005 [DOI] [PubMed] [Google Scholar]
- Clemow DB, & Walker DJ (2014). The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med, 126(5), 64–81. doi: 10.3810/pgm.2014.09.2801 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. J Health Soc Behav, 24(4), 385–396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cook C, Heath F, Thompson RL, & Thompson B (2001). Score reliability in Web- or Internet-based surveys: Unnumbered graphic rating scales versus likert-type scales. Educational and Psychological Measurement, 61(4), 697–706. doi:Doi 10.1177/00131640121971356 [DOI] [Google Scholar]
- Couper MP, Tourangeau R, Conrad FG, & Singer E (2006). Evaluating the effectiveness of visual analog scales - A web experiment. Social Science Computer Review, 24(2), 227–245. doi:Doi 10.1177/0894439305281503 [DOI] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, & Mitchell JE (2009). Daily mood patterns and bulimic behaviors in the natural environment. Behav Res Ther, 47(3), 181–188. doi: 10.1016/j.brat.2008.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, & Karyadi KA (2014). Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addict Behav, 39(9), 1372–1376. doi: 10.1016/j.addbeh.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis AD, Webb EM, & Noar SM (2008). Illicit use of prescription ADHD medications on a college campus: a multimethodological approach. J Am Coll Health, 57(3), 315–324. doi: 10.3200/JACH.57.3.315-324 [DOI] [PubMed] [Google Scholar]
- Dussault CL, & Weyandt LL (2013). An examination of prescription stimulant misuse and psychological variables among sorority and fraternity college populations. J Atten Disord, 17(2), 87–97. doi: 10.1177/1087054711428740 [DOI] [PubMed] [Google Scholar]
- Ford JA, & Pomykacz C (2016). Non-medical use of prescription stimulants: A comparison of college students and their same-age peers who do not attend college. J Psychoactive Drugs, 48(4), 253–260. doi: 10.1080/02791072.2016.1213471 [DOI] [PubMed] [Google Scholar]
- Garnier-Dykstra LM, Caldeira KM, Vincent KB, O’Grady KE, & Arria AM (2012). Nonmedical use of prescription stimulants during college: four-year trends in exposure opportunity, use, motives, and sources. J Am Coll Health, 60(3), 226–234. doi: 10.1080/07448481.2011.589876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, … Goldstein R (2014). Source and accuracy statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism [Google Scholar]
- Holt LJ, & Looby A (2018). Factors that Differentiate Prescription Stimulant Misusers from those At-Risk for Misuse: Expectancies, Perceived Safety, and Diversion. Subst Use Misuse, 53(7), 1068–1075. doi: 10.1080/10826084.2017.1392984 [DOI] [PubMed] [Google Scholar]
- Hopper JW, Su Z, Looby AR, Ryan ET, Penetar DM, Palmer CM, & Lukas SE (2006). Incidence and patterns of polydrug use and craving for ecstasy in regular ecstasy users: an ecological momentary assessment study. Drug and Alcohol Dependence, 85(3), 221–235. doi: 10.1016/j.drugalcdep.2006.04.012 [DOI] [PubMed] [Google Scholar]
- Hosmer DW, & Lemeshow S (2000). Applied logistic regression (2nd ed.). New York: Wiley. [Google Scholar]
- Kang D, Fairbairn CE, & Ariss TA (2019). A meta-analysis of the effect of substance use interventions on emotion outcomes. J Consult Clin Psychol, 87(12), 1106–1123. doi: 10.1037/ccp0000450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan BA, Amlung M, Reed DD, Jarmolowicz DP, McKerchar TL, & Lemley SM (2016). Automating Scoring of Delay Discounting for the 21- and 27-Item Monetary Choice Questionnaires. The Behavior Analyst, 39(2), 293–304. doi: 10.1007/s40614-016-0070-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, … Walters EE (2005). The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med, 35(2), 245–256. doi: 10.1017/s0033291704002892 [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, & Bickel WK (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen, 128(1), 78–87. doi: 10.1037//0096-3445.128.1.78 [DOI] [PubMed] [Google Scholar]
- Kreft I, & de Leeuw J (1998). Introducing multivlevel modeling. Thousand Oaks, CA US: Sage Publications, Inc. [Google Scholar]
- Lee E-H (2012). Review of the Psychometric Evidence of the Perceived Stress Scale. Asian Nursing Research, 6(4), 121–127. doi: 10.1016/j.anr.2012.08.004 [DOI] [PubMed] [Google Scholar]
- Looby A, & Earleywine M (2011). Expectation to receive methylphenidate enhances subjective arousal but not cognitive performance. Exp Clin Psychopharmacol, 19(6), 433–444. doi: 10.1037/a0025252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, & Teter CJ (2009). Subtypes of nonmedical prescription drug misuse. Drug Alcohol Depend, 102(1–3), 63–70. doi: 10.1016/j.drugalcdep.2009.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Knight JR, Teter CJ, & Wechsler H (2005). Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction, 100(1), 96–106. doi: 10.1111/j.1360-0443.2005.00944.x [DOI] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, Wilens TE, West BT, Schepis TS, Ford JA, … Boyd CJ (2019). Sources of Nonmedical Prescription Drug Misuse Among US High School Seniors: Differences in Motives and Substance Use Behaviors. J Am Acad Child Adolesc Psychiatry, 58(7), 681–691. doi: 10.1016/j.jaac.2018.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Schepis TS, & Teter CJ (2015). Simultaneous co-ingestion of prescription stimulants, alcohol and other drugs: a multi-cohort national study of US adolescents. Hum Psychopharmacol, 30(1), 42–51. doi: 10.1002/hup.2449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, & Boyd CJ (2014). Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addict Behav, 39(7), 1176–1182. doi: 10.1016/j.addbeh.2014.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina BG, Dutta NM, Silvestri MM, Diulio AR, Garza KB, Murphy JG, & Correia CJ (2016). Modeling motivations for non-medical use of prescription drugs. Addict Behav, 52, 46–51. doi: 10.1016/j.addbeh.2015.07.024 [DOI] [PubMed] [Google Scholar]
- Muller CP, & Schumann G (2011). Drugs as instruments: a new framework for non-addictive psychoactive drug use. Behav Brain Sci, 34(6), 293–310. doi: 10.1017/S0140525X11000057 [DOI] [PubMed] [Google Scholar]
- Norman L, & Ford J (2018). Undergraduate Prescription Stimulant Misuse: The Impact of Academic Strain. Subst Use Misuse, 53(9), 1482–1491. doi: 10.1080/10826084.2017.1413393 [DOI] [PubMed] [Google Scholar]
- O’Donnell R, Richardson B, Fuller-Tyszkiewicz M, Liknaitzky P, Arulkadacham L, Dvorak R, & Staiger PK (2019). Ecological momentary assessment of drinking in young adults: An investigation into social context, affect and motives. Addict Behav, 98, 106019. doi: 10.1016/j.addbeh.2019.06.008 [DOI] [PubMed] [Google Scholar]
- Schepis TS, Acheson S, Zapp D, & Swartzwelder HS (2019). Alcohol use and consequences in matriculating US college students by prescription stimulant/opioid nonmedical misuse status. Addictive Behaviors. doi: 10.1016/j.addbeh.2019.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Teter CJ, & McCabe SE (2018). Prescription drug use, misuse and related substance use disorder symptoms vary by school enrollment status in U.S. adolescents and young adults. Drug Alcohol Depend, 189, 172–177. doi: 10.1016/j.drugalcdep.2018.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annu Rev Clin Psychol, 4, 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Short CE, DeSmet A, Woods C, Williams SL, Maher C, Middelweerd A, … Crutzen R (2018). Measuring Engagement in eHealth and mHealth Behavior Change Interventions: Viewpoint of Methodologies. J Med Internet Res, 20(11), e292. doi: 10.2196/jmir.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TE, Martel MM, & DeSantis AD (2017). Subjective Report of Side Effects of Prescribed and Nonprescribed Psychostimulant Use in Young Adults. Substance Use & Misuse, 52(4), 548–552. doi: 10.1080/10826084.2016.1240694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson ER (2007). Development and validation of an internationally reliable short-form of the positive and negative affect schedule (Panas). Journal of Cross-Cultural Psychology, 38(2), 227–242. doi: 10.1177/0022022106297301 [DOI] [Google Scholar]
- van de Glind G, van den Brink W, Koeter MWJ, Carpentier P-J, van Emmerik-van Oortmerssen K, Kaye S, … Levin FR (2013). Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug and Alcohol Dependence, 132(3), 587–596. doi: 10.1016/j.drugalcdep.2013.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weyandt LL, Janusis G, Wilson KG, Verdi G, Paquin G, Lopes J, … Dussault C (2009). Nonmedical prescription stimulant use among a sample of college students: relationship with psychological variables. J Atten Disord, 13(3), 284–296. doi: 10.1177/1087054709342212 [DOI] [PubMed] [Google Scholar]
- Weyandt LL, Marraccini ME, Gudmundsdottir BG, Zavras BM, Turcotte KD, Munro BA, & Amoroso AJ (2013). Misuse of prescription stimulants among college students: a review of the literature and implications for morphological and cognitive effects on brain functioning. Exp Clin Psychopharmacol, 21(5), 385–407. doi: 10.1037/a0034013 [DOI] [PubMed] [Google Scholar]
- Wilens TE, Carrellas NW, Martelon M, Yule AM, Fried R, Anselmo R, & McCabe SE (2017). Neuropsychological functioning in college students who misuse prescription stimulants. Am J Addict, 26(4), 379–387. doi: 10.1111/ajad.12551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilens TE, Zulauf C, Martelon M, Morrison NR, Simon A, Carrellas NW, … Anselmo R (2016). Nonmedical Stimulant Use in College Students: Association With Attention-Deficit/Hyperactivity Disorder and Other Disorders. J Clin Psychiatry, 77(7), 940–947. doi: 10.4088/JCP.14m09559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorrilla EP, & Koob GF (2019). Impulsivity Derived From the Dark Side: Neurocircuits That Contribute to Negative Urgency. Front Behav Neurosci, 13, 136. doi: 10.3389/fnbeh.2019.00136 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


