Abstract
Background
VRC01, a potent, broadly neutralizing monoclonal antibody, inhibits simian-HIV infection in animal models. The HVTN 104 study assessed the safety and pharmacokinetics of VRC01 in humans. We extend the clinical evaluation to determine intravenously infused VRC01 distribution and protective function at mucosal sites of HIV-1 entry.
Methods
Healthy, HIV-1–uninfected men (n = 7) and women (n = 5) receiving VRC01 every 2 months provided mucosal and serum samples once, 4–13 days after infusion. Eleven male and 8 female HIV-seronegative volunteers provided untreated control samples. VRC01 levels were measured in serum, secretions, and tissue, and HIV-1 inhibition was determined in tissue explants.
Results
Median VRC01 levels were quantifiable in serum (96.2 μg/mL or 1.3 pg/ng protein), rectal tissue (0.11 pg/ng protein), rectal secretions (0.13 pg/ng protein), vaginal tissue (0.1 pg/ng protein), and cervical secretions (0.44 pg/ng protein) from all recipients. VRC01/IgG ratios in male serum correlated with those in paired rectal tissue (r = 0.893, P = 0.012) and rectal secretions (r = 0.9643, P = 0.003). Ex vivo HIV-1Bal26 challenge infected 4 of 21 rectal explants from VRC01 recipients versus 20 of 22 from controls (P = 0.005); HIV-1Du422.1 infected 20 of 21 rectal explants from VRC01 recipients and 12 of 12 from controls (P = 0.639). HIV-1Bal26 infected 0 of 14 vaginal explants of VRC01 recipients compared with 23 of 28 control explants (P = 0.003).
Conclusion
Intravenous VRC01 distributes into the female genital and male rectal mucosa and retains anti–HIV-1 functionality, inhibiting a highly neutralization-sensitive but not a highly resistant HIV-1 strain in mucosal tissue. These findings lend insight into VRC01 mucosal infiltration and provide perspective on in vivo protective efficacy.
Funding
National Institute of Allergy and Infectious Diseases and Bill & Melinda Gates Foundation.
Keywords: AIDS/HIV
Keywords: AIDS vaccine, Drug therapy
Introduction
In 2019, 1.7 million people were newly infected with HIV-1 (1), in nearly all regions of the world, even in countries with access to the latest prevention toolkit. Clearly, additional prevention modalities are required to further reduce global HIV-1 incidence. Since HIV-1 is predominantly sexually transmitted across genital and/or colorectal mucosal surfaces, development of biomedical interventions that block HIV-1 entry or provide early control at these sites is a high priority (2–9).
Broadly neutralizing antibodies (bnAbs), which target conserved sites of vulnerability on the HIV-1 envelope trimer and block infection by diverse strains, have been reported to protect against mucosal viral challenge in preclinical animal models for 20 years (6, 10–15), as well as in ex vivo human explant models (16–18). More recently, numerous monoclonal bnAbs (bn-mAbs) of exceptional potency and breadth have been cloned from B cells of HIV-1–infected donors (19, 20). Availability of these bn-mAbs has renewed enthusiasm for passive immunization strategies to prevent HIV-1 infection.
VRC01, a human IgG1 anti–HIV-1 bn-mAb, is the first prototype used to test the concept that passively transferred bn-mAbs can provide antibody-mediated protection against HIV-1 in at-risk populations (21). VRC01 neutralizes HIV-1 by binding to the conserved CD4-binding site on HIV-1 Env (22), thus preventing viral entry into target cells (23). Against a global panel of 190 viral reference strains, VRC01 neutralizes approximately 90% of these viruses in vitro, with a geometric mean 50% inhibitory concentration (IC50) of 0.33 μg/mL and IC80 of 1.0 μg/mL (22, 24). Passively administered VRC01 protects against rectal and vaginal challenge in several animal models of HIV transmission (25–31). In nonhuman primate challenge studies, the infused bn-mAb was detected in mucosal secretions and tissues (26). Notably, tissue rather than serum or secretion levels of VRC01 were associated with protection, and these decayed more rapidly in rectal compared with vaginal tissue (26).
In phase I human trials (VRC 601, VRC 602, and HVTN 104), VRC01 infusions proved safe and well tolerated, and demonstrated expected pharmacokinetic (PK) properties for a human IgG1 in both adults without HIV-1 (32, 33) and adults living with HIV-1 (34, 35). Moreover, a single infusion of the bn-mAb in people living with HIV-1 demonstrated a modest clinical antiviral effect (34–36). VRC01 PK and functionality following subcutaneous and/or i.v. administrations were evaluated in a multisite, phase Ib study in healthy adults (HVTN 104; ClinicalTrials.gov NCT02165267; ref. 32). Two groups in HVTN 104 received 3 i.v. infusions of VRC01 at 10 mg/kg (T4) or 30 mg/kg (T5) administered at 2-month intervals. Over a 24-week period, functional bn-mAb was maintained in the participant sera at concentrations predicted to neutralize a majority of circulating HIV strains in vitro (IC50 > 5 μg/mL) (32). Thus, these VRC01 infusion regimens were tested in parallel phase IIb efficacy trials of antibody-mediated prevention (AMP) in the Americas (HVTN 704/HPTN 085; NCT02716675) and in sub-Saharan Africa (HVTN 703/HPTN 081; NCT02568215) for prevention of HIV infection in populations at high risk of sexual exposure to HIV-1 (37).
Both the level and the function of bnAbs in gastrointestinal and genital tract secretions and tissues are potentially key to the success of passive immunoprophylaxis approaches that aim to prevent HIV-1 transmission through sexual exposure (26, 38). To address these features in humans for the first time to our knowledge, we designed and implemented a nested observational study among HVTN 104 participants in the 2 treatment groups, T4 and T5, to provide serum and mucosal samples. We assessed both the levels of VRC01 after infusion in rectal and cervicovaginal tissues and secretions, and its protective capacity in rectal and vaginal tissues using ex vivo HIV-1 challenge assays. The clinical and laboratory procedures established here set the stage for a standalone VRC01 mucosal PK phase I trial (HVTN 116; NCT02797171), conducted in parallel with the VRC01 efficacy trials, since invasive mucosal sampling is not feasible in the framework of efficacy trials.
Results
Study conduct.
From August to September 2015, we recruited participants from HVTN 104 groups T4 and T5 (32) into a nested study designed to assess mucosal VRC01 levels and antiviral function in rectal and cervicovaginal compartments after i.v. infusion of the bn-mAb. Enrollment criteria in HVTN 104 (32) included healthy participants of both female and male sex assigned at birth, aged 18 to 50 years, weighing between 53 and 115 kg, HIV-1 seronegative, and amenable to HIV risk reduction counseling. Female participants were not pregnant and agreed to consistent use of contraception or abstinence during the conduct of the study.
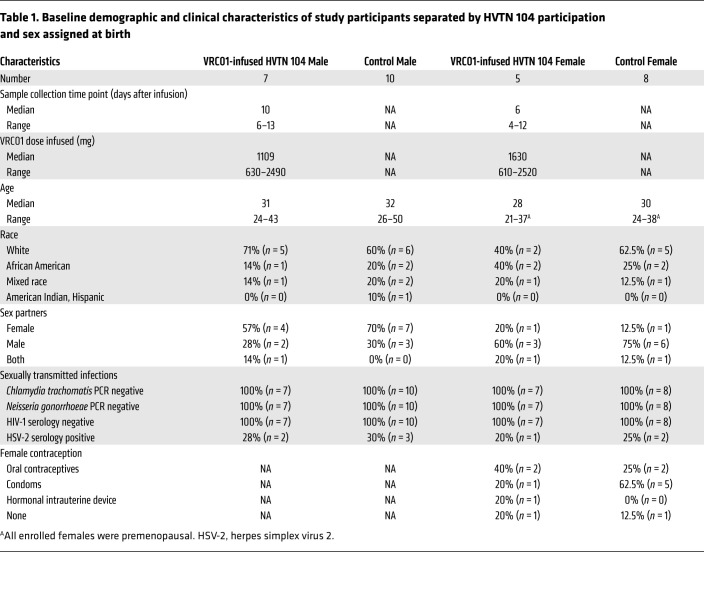
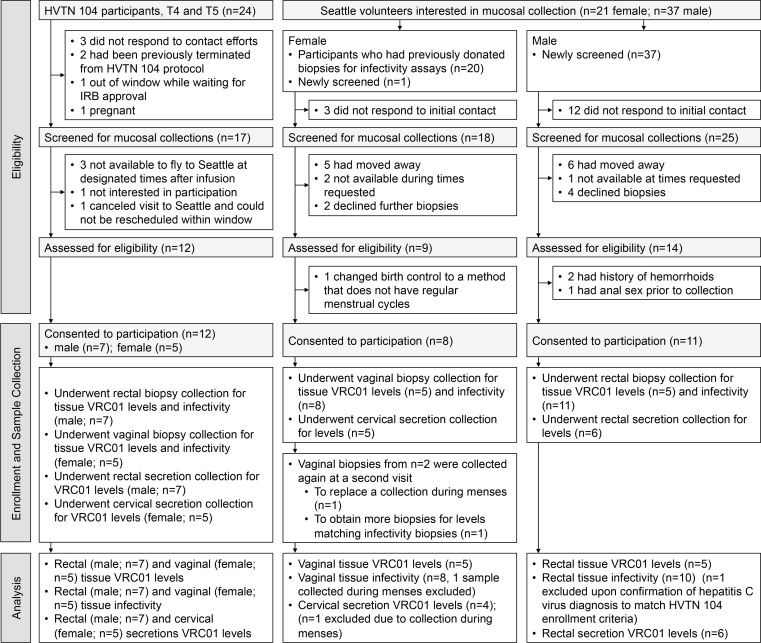
Seven male and five female eligible and consenting HVTN 104 participants (VRC01-infused group) underwent peripheral blood, mucosal secretion, and biopsy collections in a single visit at the Seattle site (Seattle Vaccine Trials Unit, Fred Hutchinson Cancer Research Center) (Table 1 and Figure 1, left). Male participants donated serum, rectal biopsies, and secretions at a median postinfusion interval of 10 days (range 6–13 days); female participants donated serum, vaginal biopsies, and cervical secretions outside of menses at a median postinfusion interval of 6 days (range 4–12 days). Most participants (9/12) completed all three HVTN 104–scheduled infusions (1 infusion every 2 months) prior to their nested mucosal visit. One male participant (PTID4) and 2 female participants (PTID8 and PTID12) completed only 2 infusions, either the first and second with sample collection conducted after the second infusion (PTID8), or the first and third infusions with sample collection conducted after the third infusion (PTID4 and PTID12).
Table 1. Baseline demographic and clinical characteristics of study participants separated by HVTN 104 participation and sex assigned at birth.
Figure 1. CONSORT diagram of participant screening, enrollment, and participation.
Left: VRC01-infused participants from HVTN 104. Middle and right: Uninfused control participants separated by sex assigned at birth.
All HVTN 104 placebo recipients were already outside of our study window at the time of nested study enrollment. Thus, we recruited and screened uninfused control participants in Seattle. Ten male and 8 female control participants donated similar specimens from June 2015 to June 2016 and shared demographic and clinical characteristics similar to those of participants enrolled from HVTN 104 (Table 1 and Figure 1, middle and right). No procedure-related complications were reported.
VRC01 levels in systemic, rectal, and cervicovaginal compartments following i.v. infusion.
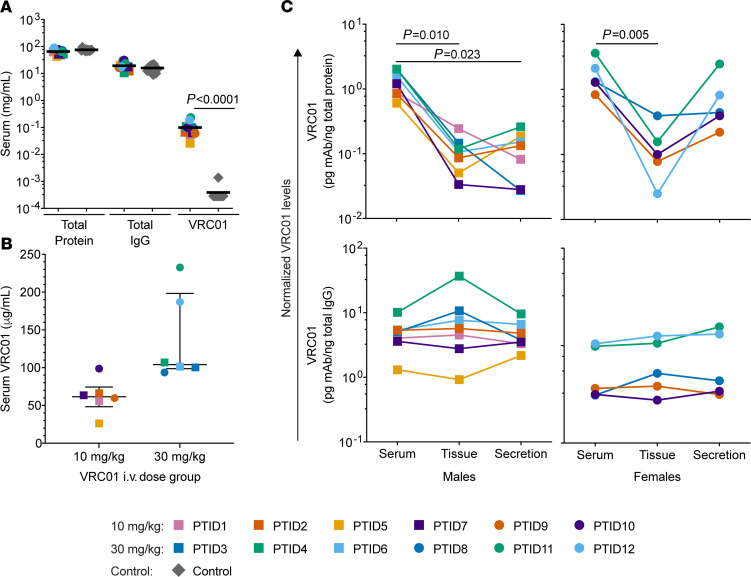
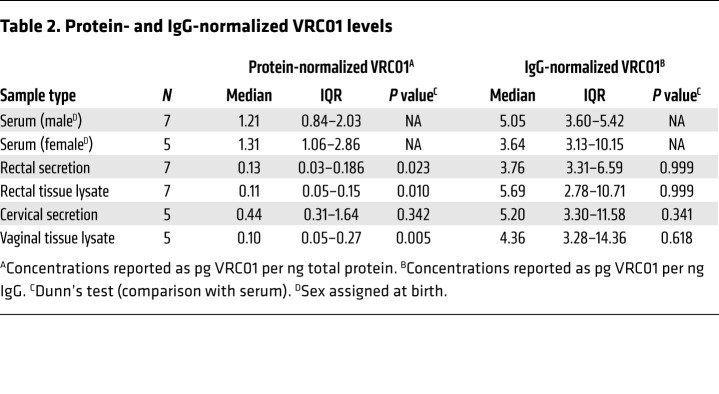
We determined total protein, total IgG, and VRC01 levels in blinded serum and mucosal samples collected from VRC01-infused and uninfused control participants. Because of the anticipated low concentrations of VRC01 in mucosal samples, we used an anti-idiotype mAb, 5C9, in a highly sensitive, custom Erenna Single Molecule Counting (SMC) immunoassay (Singulex/EMD Millipore) to measure VRC01 levels in all samples (39). Serum VRC01 levels were uniformly higher in the infused (median 96.2 μg/mL, IQR 60.7–105.5) compared with the control group (median and IQR below the lower limit of quantitation [LLOQ]; Mann-Whitney P < 0.0001; Figure 2A and Supplemental Table 1; supplemental material available online with this article; https://doi.org/10.1172/JCI146975DS1). Serum total protein and IgG levels were comparable among all participants (Mann-Whitney P = 0.051 and P = 0.211, respectively; Figure 2A). Infusion dose–normalized VRC01 serum concentrations in female participants (median 1.23/L, IQR 1.23–1.26) tended to be higher than but not significantly different from those in male participants (median 1.12/L, IQR 1.09–1.16; P = 0.090) after accounting for differences in the collection times (Table 1). The 10 mg/kg VRC01 dose group (T4) had lower serum bn-mAb concentrations (median 61.6 μg/mL, IQR 48.3–74.3) than the 30 mg/kg group (T5) (median 104.2 μg/mL, IQR 98.6–198.3; P = 0.004; Figure 2B).
Figure 2. Detection of i.v.-infused VRC01 in systemic and mucosal compartments of male and female participants.
(A) Comparison of total protein, IgG, and VRC01 levels in serum from VRC01-infused male (squares, n = 7) and female (circles, n = 5) participants and control participants (n = 11). (B) Absolute serum VRC01 levels in men and women infused with 10 mg/kg (yellow, orange, and purple) or 30 mg/kg VRC01 (green and blue) (n = 12). (C) Normalized VRC01 levels in sera, secretions, and mucosal tissue homogenates from male (left) and female (right) VRC01-infused participants (n = 12). Levels were normalized to total protein (top) and total IgG (bottom). Friedman’s tests were first used to compare normalized levels within paired sera, secretions, and tissues, and then statistical significance was assessed between 2 specific compartments using Dunn’s tests. Correlation was determined by Spearman’s rank coefficients.
All serum VRC01 concentrations measured by the Erenna assay in infused participants were within the range of values predicted by statistical modeling of participant-specific, serum VRC01 pharmacokinetics, as estimated by ELISA using the 5C9 anti-idiotype mAb in HVTN 104 (Supplemental Figure 1 and refs. 32, 40). Yet, the sensitivity of the Erenna immunoassay (median assay LLOQ 68.8 pg/mL, IQR 64.3–105.4) compared with the ELISA used for serological assays in HVTN 104 enabled the reliable detection of the lower levels of VRC01 present in cervical and colorectal secretions and tissue homogenates from VRC01-infused participants (Figure 2C, Table 2, and Supplemental Table 1). These results demonstrate that VRC01 is detectable within these mucosal compartments 4 to 13 days after infusion. By contrast, samples from control participants were all below the LLOQ, except for 2 samples (Supplemental Table 1). We also measured VRC01 levels in matched serum and mucosal sample aliquots using a binding antibody multiplex assay (41) that used 2 different gp120 probes to detect the bn-mAb. VRC01 levels measured in the 2 assays were highly correlated (Supplemental Figure 2). We focus our discussion on the results from the Erenna, as this assay uses a probe specific to VRC01.
Table 2. Protein- and IgG-normalized VRC01 levels.
Unlike serum, processing of mucosal secretions and tissues for solution-based assays results in indeterminable dilution effects, associated with the differential viscosity of the secretions and absorption in the sponges, as well as the presence of insoluble particles, such as epithelial cells and fecal matter. Thus, we normalized VRC01 levels to the total protein or IgG concentration in each serum, and in the soluble fraction of each secretion eluate and tissue homogenate, to compare across participant-matched samples in the VRC01-infused group. Overall, processed mucosal samples were orders of magnitude more dilute than serum (Supplemental Figure 3). Additionally, we measured the hemoglobin content of all secretions to determine whether blood contamination skewed bn-mAb levels found in these samples. Rectal and cervical secretions contained median hemoglobin concentrations of 0.64 μg/mL and 0.03 μg/mL, respectively, less than 1% of free hemoglobin in serum.
Protein-normalized, serum VRC01 levels in male donors were approximately 10-fold higher compared with those in matched rectal secretions and rectal tissues (Figure 2C and Table 2). Thus, despite the extensive vascularization of the rectal mucosa (42), only a fraction of the i.v.-infused mAb is transported from the serum into the tissue and secretions. Interestingly, PTID4, who had missed the second infusion, had VRC01 levels comparable to those in the male participants receiving 3 infusions. Together, these rectal levels suggest that antibody-mediated neutralization may be less efficient blocking relatively resistant HIV viruses at the intestinal mucosa than in the vasculature.
In female participants, VRC01 levels were also highest in serum but were not significantly different from those in matched cervical secretions (Figure 2C and Table 2). Vaginal tissues had approximately 13-fold lower VRC01 levels than sera. These findings suggest that distinct VRC01 levels are achieved within the cervical and vaginal compartments within 2 weeks of i.v. administration. As with PTID4, serum and mucosal VRC01 levels in the 2 donors who had received only 2 infusions (PTID8 and PTID12) were not lower than those of the other participants who had not missed a scheduled infusion (Figure 2C), suggesting that the last infusion received by the participants largely determined the antibody levels at the study collection time point. This is consistent with the previously reported approximately 15-day half-life of serum VRC01 (32), and it allows us to combine participants receiving 2 and 3 infusions in our comparisons.
We also compared VRC01 levels relative to total IgG across matched samples (Table 2 and Figure 2C). In male participants, IgG-normalized VRC01 levels in serum were not significantly different from the levels in rectal secretions or rectal tissues. Similarly, no differences were identified between IgG-normalized VRC01 levels in sera, cervical secretions, and vaginal tissues from female participants. The similar ratios of VRC01 to total IgG found across participant-matched sample types indicate that VRC01 transport into tissues is proportional to other IgGs in circulation. The differences between protein-normalized and IgG-normalized comparisons reflect that IgG is a less dominant protein in mucosal samples than serum and that the proportion of IgG in total protein varies across participant-matched sample types.
Protection of rectal and vaginal biopsies from VRC01-infused participants against ex vivo HIV-1 challenge.
To assess the antiviral functionality of VRC01 in rectal tissue explants from infused (n = 7) and control (n = 10) male participants, we used an ex vivo HIV challenge assay employing 2 recombinant strains, one sensitive (HIV-1Bal26; Figure 3) and one resistant (HIV-1Du422.1; Figure 4) to VRC01 in vitro neutralization. Sections of rectal biopsies were challenged with replication-competent, secreted nanoluciferase (sNLuc) reporter viruses expressing the Env ectodomain of either HIV-1Bal26 or HIV-1Du422.1 (in vitro neutralization IC50 = 0.04 μg/mL, IC80 = 0.15 μg/mL, and IC50 > 50 μg/mL, respectively, from CATNAP database; ref. 43) within an isogenic virus background. Neutralization sensitivities were verified for the sNLuc viruses (Supplemental Table 2). For simplicity, these reporter viruses are hereafter referred to as Bal26 and Du422.1. Since sNLuc is generated during viral stock preparation, productive infection was defined as sNLuc activity in relative light units (RLU) that is above the level corresponding to residual input sNLuc that dilutes out at each change of medium (black dashed lines in Figure 3A and Figure 4A). Total replication was summarized using area under the curve (AUC) for statistical comparisons (Figure 3B and Figure 4B).
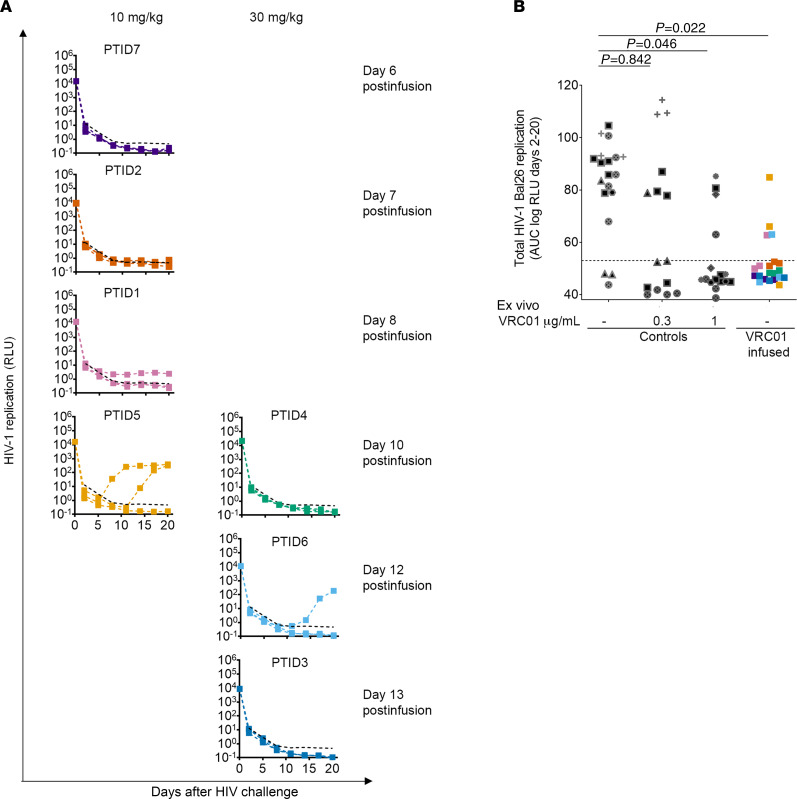
Figure 3. Resistance of rectal biopsies from VRC01-infused male participants to ex vivo HIV-1Bal26 challenge.
(A) HIV-1 infection kinetics for rectal explants from VRC01-infused participants challenged with VRC01 neutralization–sensitive HIV-1Bal26. Graphs are arranged by infusion dose (left, 10 mg/kg; right, 30 mg/kg) and collection time postinfusion (n = 7). Each curve corresponds to the infection readout of a single tissue explant section challenged with virus. Dashed black lines represent the threshold for detecting infection, defined by the average log RLU plus 2 standard deviations of explants challenged with Bal26 in the presence of bn-mAbs or antiretrovirals (n = 32). (B) Total HIV-1Bal26 replication for individual explants from VRC01-infused (color-coded squares, n = 7) or uninfused control (black/gray symbols, n = 5) participants, summarized by scaled log RLU AUC. Control explants were challenged in the absence or presence of VRC01 added ex vivo, at the indicated concentrations, demonstrating the relative sensitivity of this virus to VRC01 in an explant culture assay. Unique symbols are used to denote explants from different donors. Statistical significance was assessed by Dunn’s tests.
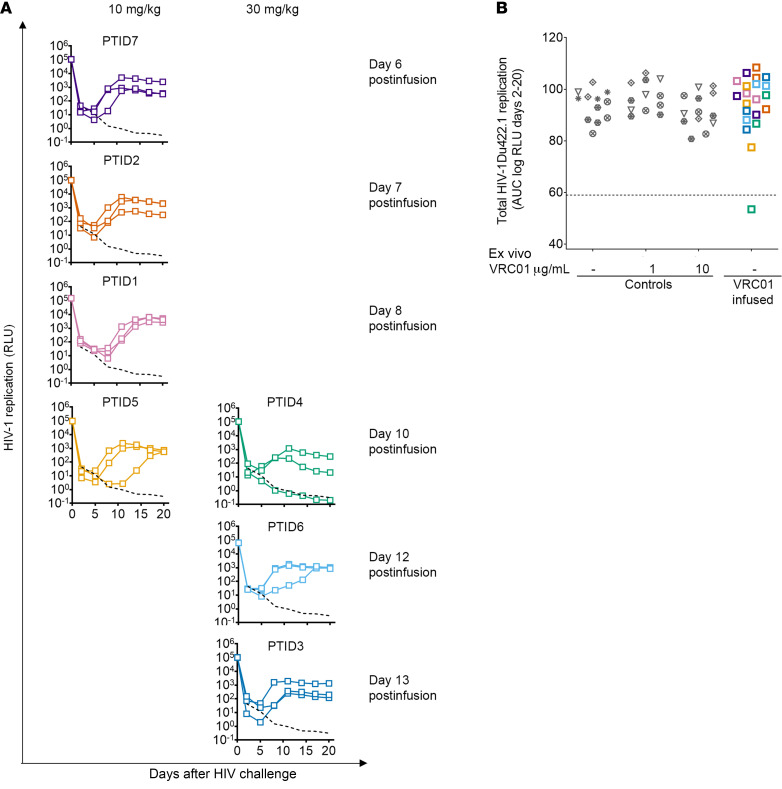
Figure 4. Susceptibility of rectal biopsies from VRC01-infused male participants to ex vivo HIV-1Du422.1 challenge.
(A) HIV-1 infection kinetics for rectal explants from VRC01-infused participants challenged with VRC01 neutralization–resistant HIV-1Du422.1. Graphs are arranged by infusion dose (left, 10 mg/kg; right, 30 mg/kg) and collection time postinfusion (n = 7). Each curve corresponds to the infection readout of a single tissue explant section challenged with virus. Dashed black lines represent the threshold for detecting infection, defined by the average log RLU plus 2 standard deviations of explants challenged with Du422.1 in the presence of bn-mAbs or antiretrovirals (n = 6). (B) Total HIV-1Du422.1 replication for individual explants from VRC01-infused (color-coded squares, n = 7) or uninfused control (gray symbols, n = 6) participants is summarized by scaled log RLU AUC. HIV-1Du422.1 challenges of control explants were done in the absence or presence of VRC01 added ex vivo, at the indicated concentrations, demonstrating the relative resistance of the virus to VRC01 in an explant culture assay. Unique symbols are used to denote explants from different donors. Statistical significance was assessed by Dunn’s tests.
As expected, ex vivo rectal challenge with either virus resulted in productive infection of explants from the male controls, thus verifying the infectivity of both HIV-1 reporter viruses (Figure 3B and Figure 4B). Addition of exogenous VRC01 24 hours before challenge of rectal explants from control donors demonstrated that Bal26 explant infection could be blocked by exogenous VRC01 in a concentration-dependent manner (Figure 3B), unlike Du422.1 infection (Figure 4B). Whereas 1 μg/mL of VRC01 significantly inhibited Bal26 infection (Dunn’s P = 0.046), the same or even a 10-fold higher concentration did not affect Du422.1 infection (Dunn’s P = 0.999 and P = 0.819, respectively). The addition of seminal proteins during the Bal26 viral challenge did not alter rectal tissue infectivity or VRC01-mediated protection (Supplemental Figure 4), so all challenges in the study were performed in the absence of semen.
From VRC01-infused male participants (n = 7), only 4 of 21 rectal explants were infected by Bal26 challenge compared with 20 of 21 explants infected by Du422.1 challenge (Figure 3A and Figure 4A). The significant difference in total replication of Bal26 compared with Du422.1 (Wilcoxon’s P = 0.016, n = 7) indicates that i.v.-infused VRC01 reaches and retains neutralization functionality in the rectal mucosa. Additionally, explants from the VRC01-infused group (n = 7) were significantly resistant to Bal26 infection compared with those from the controls (n = 5) (Dunn’s P = 0.022; Figure 3B). By contrast, rectal explants from both VRC01-infused (n = 7) and control groups (n = 6) were susceptible to Du422.1 infection, resulting in comparable levels of viral replication (Dunn’s P = 0.999; Figure 4B). Within the VRC01-infused group, the high rate and magnitude of productive ex vivo Du422.1 infection also demonstrated that these participants’ rectal tissue was not intrinsically resistant to HIV-1 (Figure 4, A and B). Together, these results show that i.v.-infused VRC01 provides significant but incomplete protection against ex vivo HIV-1 challenge of rectal tissues collected 6–13 days after infusion, consistent with its neutralization activities.
Furthermore, we investigated whether genetic resistance against VRC01 binding had developed ex vivo, which can occur early (34, 44), causing the breakthrough viral replication observed in 4 Bal26-challenged explants from VRC01-infused donors (Figure 3, A and B). We sequenced a 3036 bp fragment (corresponding to HXB2 5969–9015) of HIV-1Bal26 env in the culture supernatants (pooled from day 15–18) of the 4 explants in question (Figure 3A, PTIDs 1, 5, and 6), 3 untreated control explants, and the original Bal26 viral challenge stock. For all but 1 sample (PTID5, no virus cDNA from 1 of 2 explant cultures), we obtained a minimum of 230× coverage across all the bases, using Illumina Nextera XT indexing and sequencing on the MiSeq NGS platform (Supplemental Methods). All viral sequences were identical within and between samples except for a single G to A substitution at position 2539 identified in 1 untreated control explant culture. Thus, we found no evidence that genetic resistance to VRC01 binding developed during the 20-day explant culture of VRC01-infused biopsies. Rather, these results suggest that the breakthrough infections in the VRC01-infused group were the result of neutralization-sensitive Bal26 virions that were able to establish infection in the face of subprotective levels of VRC01 in these explants.
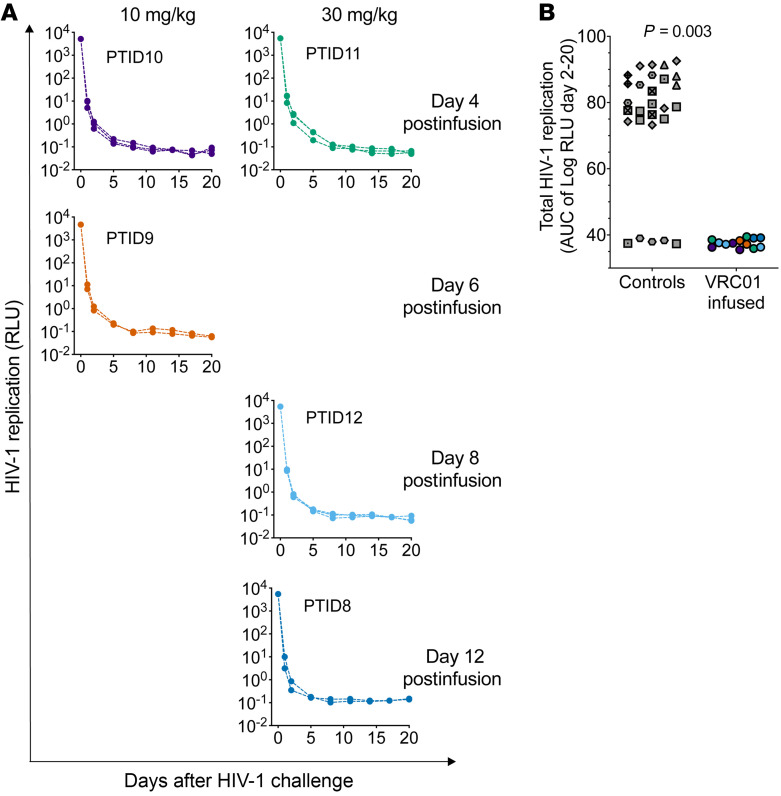
To assess the anti–HIV-1 functionality of i.v.-infused VRC01 in the female genital tract, we likewise compared the ability of Bal26 to establish infection in vaginal biopsies collected from VRC01-infused (n = 5) and uninfused control (n = 8) female participants in an ex vivo challenge assay. Vaginal biopsies are less amenable than rectal biopsies to dissection for ex vivo challenge because of the lower density of HIV-1 target cells (45–51) and the uneven distribution of the target cells within the epithelium and stroma (52, 53). Thus, whole vaginal biopsies were challenged ex vivo with Bal26 and maintained in a manner comparable to the rectal assay (see Methods), but optimized for vaginal tissues (17) to achieve consistent infection in untreated controls. Notably, none of the 13 explants from the 5 VRC01-infused female participants were infected by Bal26 challenge (Figure 5, A and B), whereas 23 of 28 vaginal explants from the 8 control female participants were infected using the same viral challenge conditions (Mann-Whitney P = 0.003; Figure 5B). Protocol restrictions in the number of vaginal biopsies that could be collected at a single visit prevented us from conducting parallel ex vivo challenges with Du422.1. Nonetheless, these results suggest that i.v.-infused VRC01 also infiltrates human vaginal tissue and retains antiviral activity 4–12 days after infusion.
Figure 5. Resistance of vaginal biopsies from VRC01-infused participants to ex vivo HIV-1Bal26 challenge.
(A) HIV-1 infection kinetics for vaginal explants from VRC01-infused participants challenged with HIV-1Bal26. Each curve corresponds to the infection readout of a single biopsy throughout its 3-week culture (n = 5). Graphs are arranged by infusion dose (left, 10 mg/kg; right, 30 mg/kg) and collection time postinfusion. (B) Total HIV-1 replication in individual explants challenged with HIV-1Bal26 from VRC01-infused (n = 5) and uninfused control (n = 8) participants summarized by scaled log RLU AUC. Unique symbols are used to denote explants from different donors. Statistical significance was assessed by Mann-Whitney tests.
Collectively, the rectal and vaginal ex vivo challenge findings provide further evidence that i.v.-infused VRC01 may provide partial or full protection at these sites of HIV-1 transmission against a virus strain highly sensitive to its neutralization activity.
Correlations between i.v.-infused VRC01 levels in sera and mucosal compartments.
To investigate the relationship of VRC01 levels in the sera and mucosa following i.v. infusion, we compared IgG-normalized VRC01 levels among matched peripheral blood, intestinal, and genital locations using Spearman’s correlations (Figure 6). A poor correlation would suggest that the relative concentration of VRC01 in the local IgG pool (secretion or tissues) is significantly affected by local IgG production and not just serum IgG transudation.
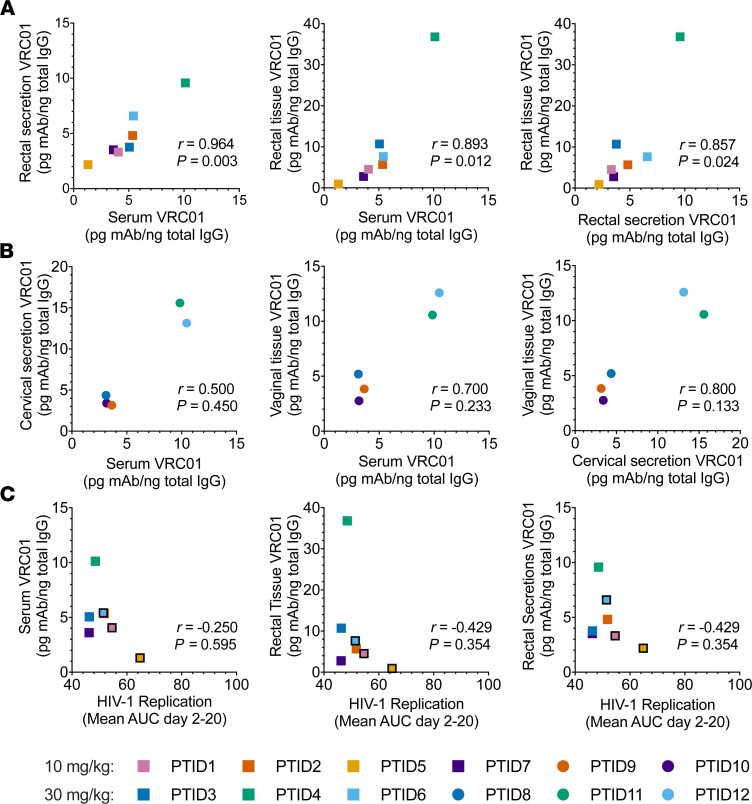
Figure 6. Correlation analysis of systemic and mucosal levels of VRC01 between compartments and in relation to ex vivo HIV-1 infection of rectal explants.
(A and B) Relationships between IgG-normalized concentrations in sera, tissue homogenates, and secretions from male (n = 7) (A) and female (n = 5) (B) participants. (C) Relationships between total ex vivo HIV-1Bal26 replication and IgG-normalized VRC01 levels in male participants (n = 7). Black-bordered symbols indicate participants in whose rectal biopsies ex vivo HIV-1 replication was detected. Correlations were determined by Spearman’s rank coefficients.
In male participants (Figure 6A), VRC01 levels in sera strongly correlated with those in rectal secretions (r = 0.964, P = 0.003) and in rectal tissues (r = 0.893, P = 0.012). Similarly, VRC01 levels in rectal tissues and secretions correlated with one another (r = 0.857, P = 0.02). Correlation analyses for VRC01 levels in female participants were not significant, and were limited by a sample above the upper limit of quantitation and small sample size (Figure 6B). Together, these results suggest a strong, positive relationship between serum VRC01 levels and those in the rectal compartment of male participants at a given time after infusion. However, the relationships in terms of the biodistribution of VRC01 between the female genital compartments and serum remain ambiguous.
Lastly, we examined whether ex vivo Bal26 infectivity in rectal tissues from VRC01-infused male participants was related to VRC01 levels in matched sera, rectal secretions, or rectal tissues. No significant correlation between total Bal26 replication and IgG-normalized (Figure 6C) or total protein–normalized (data not shown) VRC01 levels was observed for any compartment. These results suggest that in the time interval tested, the number of Bal26-infected rectal explants was too small to properly assess potential relationships between VRC01 levels and susceptibility to HIV-1 infection, as only 4 of 21 rectal explants tested showed any detectable viral replication.
Discussion
Advancement of human monoclonal antibodies to prevent and control infectious diseases has become an attractive, alternative approach to vaccines for HIV and other viral pathogens (7, 54–56). Very recent findings from the 2 large international antibody-mediated prevention (AMP) trials demonstrated that infused VRC01 has 75% efficacy in preventing HIV-1 infections from strains with sensitive neutralization profiles (IC80 < 1 μg/mL), but not in reducing infections from more resistant HIV-1 strains (37). We established ex vivo HIV-1 challenge assays that evaluated the antiviral function of infused VRC01 in human rectal and vaginal tissue biopsies, demonstrating that i.v.-infused VRC01 retains antiviral activity within the rectal and vaginal mucosa and can block most ex vivo challenges with an HIV-1Bal26 sNLuc reporter virus, which is highly sensitive to VRC01 neutralization. Our findings parallel the AMP results in regard to the importance of neutralization potency against invading strains, as we demonstrated that HIV-1Du422.1 could establish mucosal infection in the presence of VRC01. Du422.1 represents a subset of circulating HIV-1 strains, particularly of clade C, that are not neutralized (or neutralized only weakly) by this bn-mAb (24, 57). Therefore, antibody combinations may be required to achieve the breadth and potency for effective prophylaxis against global circulating HIV-1 strains (58), such as 2- and 3-antibody combinations (NCT04173819, NCT04212091, NCT03928821) as well as bi- and trispecific alternatives (NCT03875209, NCT03705169) now in clinical development.
The efficacy of VRC01 and other bn-mAbs is likely influenced by their potency, distribution, concentration, and anti-HIV activities at mucosal sites of transmission (26). However, the relationship between serum antibody levels (routinely measured) and mucosal antibody levels has been poorly defined, owing in part to practical and technical challenges in mucosal sampling and analyses within a clinical trial (59, 60). In this mucosal substudy of i.v.-administered VRC01, we successfully piloted processes to obtain genital and rectal samples, both secretions and tissues, and developed sensitive assays to specifically measure and compare VRC01 levels in the mucosal samples and peripheral blood. By taking advantage of the high sensitivity and low background characteristics of a VRC01-specific Erenna Single Molecule Counting (SMC) immunoassay, we have shown that VRC01 can be detected in serum, rectal, and cervicovaginal secretions and tissue compartments of healthy human volunteers between 4 and 13 days after they received an i.v. infusion of either 10 mg/kg or 30 mg/kg VRC01. Based on the success of this pilot study, we initiated a follow-up study, HVTN 116, in parallel with the AMP efficacy trials, which will elucidate compartment-specific bn-mAb decay rates and provide insight into mucosal antibody levels associated with ex vivo and in vivo protection. This larger and longitudinal mucosal study, with sampling from 1 day after infusion to 6 months after infusion, will address the primary limitations of the pilot study (i.e., cross-sectional, nonrandomized trial design and sample size; male-only rectal sampling; and lack of earlier and later time points) and will enable more in-depth investigations that were outside the scope of the pilot study.
Our study suggests that the i.v.-infused VRC01 circulates in the body and penetrates into rectal and cervicovaginal compartments similarly to in vivo-derived human IgG, since bn-mAb levels were largely proportional to total IgG across participant-matched sample types. Our methodology is well designed to investigate in the future whether Fc-modified monoclonals with enhanced FcRn binding (26) preferentially transport into tissues, continue to have activity against mucosal HIV exposures, and/or undergo any accumulation in mucosal compartments.
Our findings also indicate that protein-normalized VRC01 levels in rectal secretions, rectal tissues, and vaginal tissues were up to 10-fold lower than those in serum, 4–13 days after infusion. Since 70% of recently circulating strains in the Americas and South Africa have neutralization IC80 greater than 1μg/mL (37), our findings support prioritizing development of long-lasting, highly potent antibodies for immunoprophylaxis to maximize blockade of HIV-1 at the mucosa. Intravenous delivery, which has been well tolerated in all VRC01 infusion studies (32, 37), may be necessary to achieve those protective concentrations at mucosal surfaces. Importantly, our ex vivo data and those of others (26) suggest that antibodies both within tissues and in secretions may play a role in viral inhibition.
Interestingly, protein-normalized VRC01 levels in cervical secretions were not lower than those in serum; whether this reflects differences in bn-mAb transfer from serum into cervicovaginal secretions versus tissues, or into the cervix versus the vagina, warrants future investigation. It is also possible that infused bn-mAbs preferentially bind mucins in cervical mucus to achieve this increased mAb/protein ratio (61), potentially enhancing virion trapping and neutralization. Regardless of the mechanism for accumulation, our findings illustrate differences in the amount of bn-mAb that can be suffused into particular mucosal compartments through i.v. administration, which could define the degree and duration of protection afforded by a dosing regimen. The vaginal mucosal challenges do not yet address the potential role of antibodies in cervical secretions and how they may contribute to HIV inhibition, but we plan to address this contribution in future work that extends our assessments to ectocervical tissue challenges in the context of cervical secretions.
We also observed that IgG-normalized VRC01 serum levels correlated strongly with those in both rectal secretions and tissues of infused male participants. This observation could be explained by the high degree of vascularization of intestinal tissues (42) and the expected proportional transport of VRC01, as well as other IgG1 antibodies, by FcRn as it recycles IgG molecules (62). Because this cross-sectional relationship may not apply to other time points after infusion, extended longitudinal PK data in matched serum and rectal samples are needed for characterization of the biodistribution properties of VRC01 in and between serum and rectal tissues in order to determine the predictive utility of serum bn-mAb levels for estimating rectal levels over time.
The lack of significant correlations between IgG-normalized VRC01 levels in vaginal tissues, cervical secretions, and sera from infused females is difficult to interpret given the small sample size. Whereas the vaginal walls are also highly vascularized (63, 64) with IgG transport facilitated by FcRn (65), female sex hormones have been shown to regulate immunoglobulin levels (66–69) and other mediators of immunity (70) in the female genital tract. Interestingly, Nardelli-Haefliger and colleagues showed that human papilloma virus–specific, vaccine-induced IgG levels in serum and cervical secretions were strongly correlated for women on hormonal contraception but not for women who were naturally cycling (69). Thus, future studies should address the impact of female sex hormones on both antibody levels and HIV-1 susceptibility in order to better evaluate and predict the efficacy of antibody-based passive and active immunization strategies for HIV-1 prevention in women.
The ex vivo challenge assay provided strong evidence that most biopsies from VRC01-infused participants contained functional, neutralizing mAb. All vaginal explants from infusion recipients, regardless of dosage, remained uninfected after a high-dose ex vivo Bal26 challenge. All rectal explants tested from 4 male volunteers were likewise completely protected from ex vivo Bal26 challenge, whereas at least 1 of 3 rectal explants tested from each of the remaining 3 volunteers became infected (Figure 3, A and B). Postinfusion safety monitoring in the main study prevented biopsy collections within the first 3 days of infusion. As a result, we cannot ascertain how early protective VRC01 levels are achieved in vaginal and rectal tissues. Breakthrough infections occurred at days 8–12 after infusion, likely reflecting the decay of functional VRC01 over time to subprotective levels (Figure 3A). Follow-up studies under way will further address the relationship between ex vivo HIV-1 infectivity and compartment-specific VRC01 levels throughout multiple half-lives.
The complete ex vivo protection of vaginal but not rectal explants is intriguing. Follow-up studies to compare paired rectal and vaginal tissues from the same participant and visit are in progress. Several potential mechanisms could support the hypothesis that rectal tissues are more difficult to protect than vaginal tissues. There is a greater density of HIV-1 target cells (71, 72) and potentially faster antibody turnover or degradation rate (26, 73) in the intestinal mucosa. Thus, it will be important to ascertain whether a higher bn-mAb concentration will be necessary to prevent rectal transmission. Although the addition of seminal proteins did not impact VRC01 neutralization against cell-free Bal26 in the rectal explant challenge, further work will extend previous reports to address the role of seminal proteins in the neutralization of other viruses at mucosal sites (18), as well as the role of other antibodies in the prevention of infection from cell-associated viruses in semen (74, 75).
Ex vivo HIV-1 challenge assays using human tissues to model 2 compartments primarily associated with sexual transmission of HIV-1 have been used in small-molecule pre-exposure prophylaxis drug development for years, typically employing HIV-1Bal (76–78). Here, we adapted this concept to evaluate infused bn-mAbs taking into account their Env-specific targeting and extracellular activities. Our ex vivo assays employ Env-chimeric HIV-1 reporter viruses, selected for their specific neutralization sensitivities, at high virus challenge doses, compared with the estimates reported from semen exposure (79), followed by phytohemagglutinin (PHA) activation. This strategy produces consistent and reproducible infection readouts after a single challenge of untreated control tissues to facilitate the interpretation of bn-mAb doses that provide protection. Additionally, the explants were challenged quickly upon arrival with minimal manipulation to avoid bn-mAb leakage from tissues. The resulting stringency of the rectal and vaginal ex vivo challenge assays may provide conservative estimates of the overall protective efficacy of bn-mAbs. The nonpolarized virus challenge bypasses the natural barriers of intact mucosal surfaces. Also, bn-mAbs may leverage Fc-mediated effector functions from immune infiltrates in vivo and mediate systemic clearance of small, distal foci of infection (14, 80). Moving forward, ex vivo mucosal challenge assays using small, customized virus panels (including both neutralization-resistant viruses as controls and genetically diverse strains of intermediate neutralization sensitivities) are being designed to evaluate candidate bn-mAb combinations that provide better coverage than VRC01.
In summary, we have established clinical and laboratory procedures to investigate specific bn-mAb levels and function in rectal and cervicovaginal mucosae, and, importantly, our results demonstrate that VRC01 reaches mucosal tissues and secretions and exhibits functional antiviral activity in these compartments as early as 4–13 days after infusion. Currently, the development of potent bn-mAb combinations or multispecific mAbs, long-lasting Fc variants, and more efficient delivery routes is prioritized to optimize the breadth and durability of HIV-1 protection achievable by bn-mAb immunoprophylaxis (6). The mucosal assays developed here can be adapted to evaluate these parameters, and select the most promising approaches to protect sites of HIV-1 exposure, which may also be applicable to other sexually transmitted infections. Thus, integrating mucosal tissue and secretion assessments into mAb clinical development will help delineate requirements for successful passive immunization strategies, which, in turn, can provide a framework to develop vaccines that elicit the most effective antibody responses.
Methods
Study participants.
VRC01-treated participants had received 2–3 bimonthly i.v. infusions of either 10 mg/kg (group T4) or 30 mg/kg (T5), administered by clinical staff at multiple clinical sites within the HVTN 104 trial (32). They were recruited for a single mucosal sampling visit at the Seattle Vaccine Trials Unit, within 3–14 days of their second or third VRC01 infusion. We chose this schedule to enhance the likelihood of measuring functional levels of VRC01 in the mucosa and to ensure that nested study collections, which required a flight to Seattle, did not interfere with HVTN 104 protocol in-study visits. Staff at sites conducting HVTN 104 referred interested study participants directly to the nested study, or participants self-referred after reading the study flyer.
The Seattle site investigators screened interested HVTN 104 participants for additional eligibility criteria related to the mucosal sample collection. All eligible and interested participants agreed to share their HVTN 104 study medical records and were assessed for HIV risk, history of sexually transmitted infection and antithrombotic usage, willingness to undergo vaginal (female) or rectal (male) biopsy and secretion collections, and willingness to abstain from sexual intercourse for 2 days before and 5 (male) or 7 (female) days after the biopsy procedure. Females were also assessed for pregnancy, tolerability of past vaginal exams, and vaginal health, including infection and pap smear history. Males were evaluated for rectal health, including bleeding and hemorrhoids. Uninfused control participants from Seattle were screened in person using enrollment criteria similar to those of both HVTN 104 and the mucosal study (Figure 1). Many female participants had previously donated biopsy samples in our clinic, and 2 female participants were asked to provide a second set of biopsy samples (Figure 1).
During the study visit, all participants consented and were reevaluated for HIV risk, medical history, and antithrombotic usage. All participants were tested for herpes simplex virus 2 serology and Neisseria gonorrhoeae and Chlamydia trachomatis infection by PCR (Aptima, Hologic); HIV-1 testing was done through their reference HVTN 104 study site. Before sample collection each participant underwent either a rectal or a vaginal exam to confirm eligibility for sample collection to proceed. During a single visit, male participants had 1 rectal sponge and 5 rectal pinch biopsies collected via anoscopy, 8–10 cm from the anal margin, using the Radial Jaw 4 instrument (Boston Scientific). Female participants had 1 cervical sponge and 5 vaginal biopsies collected from the fornices per visit, using Baby Tischler Biopsy Forceps (Wallach Surgical). Participants remained in Seattle for 24-hour observation. HVTN 104 participants received compensation for their time, as well as paid hotel and travel expenses during their stay in Seattle. Control participants were only reimbursed for their time, since they resided nearby.
Serum collection and processing.
For each participant, peripheral blood was drawn into a single 8.5 mL BD Vacutainer serum separator tube. Serum was harvested by centrifugation at 2060g for 10 minutes at room temperature with low brake, and stored in aliquots at –80°C.
Mucosal secretion collection and extraction.
Mucosal secretions were collected by placement of a pre-wetted Weck-Cel sponge (Medtronic) into a fold of the rectal mucosa for men (5 minutes), or of a dry Merocel sponge (Medtronic) into the cervical os for women (1 minute), both of which were stored immediately after collection at –80°C. To determine mAb levels present in rectal and cervical secretions, samples were thawed on ice for 10–15 minutes and processed on ice as previously described, including the addition of 600 μL of extraction buffer (PBS [Gibco] with Protease Inhibitor Cocktail I [Calbiochem]) (81). The resulting supernatants were diluted 1:3 and 1:100 with PBS and tested for free hemoglobin using a Human Hemoglobin ELISA (Immunology Consultant Laboratories) according to manufacturer instructions.
Preparation of tissue homogenates.
Biopsies collected for tissue mAb quantitation were immediately frozen and stored at –80°C. One frozen vaginal biopsy and 2 independent rectal biopsy sections were thawed on ice and transferred into a 2 mL conical tube containing 200 μL of ice-cold extraction buffer. The tissue was homogenized with a Bio-Gen PRO200 Homogenizer and multi-Gen 7XL generator probe (Pro Scientific) using 30-second bursts and cooling on ice. Residual material was recovered from the probe by rinsing with 100 μL of ice-cold extraction buffer. Tissue homogenates were subsequently centrifuged and supernatant clarified using a Spin-X tube with 0.22 μm sterile filter (Sigma-Aldrich) at 4°C.
Protein and total IgG quantitation.
Total protein concentrations for serum, secretion, and tissue homogenate samples were quantified by bicinchoninic acid (BCA) assay (Pierce) in triplicate. Secretion samples were run undiluted; biopsy homogenates were run at 1:5; serum samples were run at 1:100 and 1:1000.
Total IgG concentrations for the same samples were also quantified by ELISA, as previously described (39), using a SpectraMax i3X ELISA plate reader (Molecular Devices). All the test samples were diluted in 1× PBS plus 10% FBS plus 0.05% Tween-20 (assay diluent) at 1:1000 for mucosal samples and 1:1,280,000 for serum samples.
VRC01 quantification.
VRC01 levels in serum and mucosal samples were assessed by a custom immunoassay using the Singulex Erenna platform (Singulex/EMD Millipore) as previously described (39). Based on previous experience with serum and mucosal secretions collected with ophthalmic sponges, these serum and mucosal samples were diluted at 1:10,000 or 1:100, respectively, using Singulex Discovery Standard Diluent (Singulex/EMD Millipore) and filtered through 96-well Filter Plates (Pall). A VRC01 standard curve, comprising 2-fold and 3-fold serial dilutions of an internal standard ranging from 142,666 pg/mL to 61.9 pg/mL, was likewise prepared with Singulex Discovery Standard Diluent. VRC01 was captured using freshly prepared 50 μg/mL 5C9 IgG2a paramagnetic microparticle beads and detected with labeled mouse anti-human IgG1 Fc secondary detection antibody (500 ng/mL in Discovery Assay Buffer, Singulex/EMD Millipore). Bound immune complexes were eluted, transferred to a 384-well plate, and then read on the Singulex Erenna instrument according to manufacturer instructions. VRC01 and 5C9 were gifts from John Mascola, NIH VRC Vaccine Production Program.
Curve fitting and extrapolation for Singulex data were done in the nCal R package (82) using the event photon (EP) raw data. The Erenna detects single molecules of VRC01 as photons over a read time. Each measurement of photons above a threshold is considered a detected event, and the sum of all photons from these events over the read time (i.e., signal intensity) is called the EP measurement for the sample or standard. The EP values of the VRC01 standards were fitted to a 5-parameter logistic curve and used to calibrate the specific mAb concentrations in mucosal and serum samples using the geometric mean of the standard triplicates. The percent coefficient of variation (CV) of technical replicates was ≤20 for 41 of 46 quantifiable samples. The lower and upper limits of quantitation (LLOQ and ULOQ) were defined by nCal, using the standards, as the estimated concentrations at which the percentage CV equals 20. All samples were below the ULOQ, except for 1 cervical secretion (PTID11) for which the CV of the estimated VRC01 concentration was greater than 20% but less than 25%. Samples above the LLOQ were confirmed to have geometric mean signal/noise ratio of at least 1.5. The percentage recovery for standards within the limits of quantitation was between 120% and 80% except for a single standard on 1 of the 7 assay plates. VRC01 concentrations, both absolute (serum) and normalized VRC01 levels (serum and mucosal), served as secondary outcome measures. ANCOVA was used to compare the mean of log-transformed dose-normalized concentrations between male and female participants accounting for differences in collection times.
Viruses.
For explant HIV-1 challenges, we titered and used secreted nanoluciferase–expressing (sNLuc-expressing), replication-competent HIV-1 proviruses (designated pNL-sNLuc.T2A) in which the ectodomain of gp160/Env is encoded by different heterologous strain env sequences Bal26 and Du422.1, which were derived from a chronic clade B isolate (83) and an early/acute clade C isolate (84), respectively (17).
Ex vivo HIV-1 challenge of rectal and vaginal explants.
Infectivity assays were conducted unblinded to group categorization (VRC01-infused vs. controls); however, details regarding infusion timing and dosage were unknown to laboratory staff. Up to 3 biopsies designated for ex vivo HIV challenge were placed immediately into a 2 mL tube containing premeasured transport medium on wet ice. Whole rectal biopsies were transported in 1 mL of medium consisting of RPMI 1640 (Gibco) supplemented with l-glutamine (Gibco), antimicrobials (100 U/mL penicillin, 100 μg/mL streptomycin, 0.25 μg/mL amphotericin B [all from Gibco], and 0.5 μg/mL Zosyn [Pfizer]), and 10% human AB serum (GemCell, Gemini Bio). The biopsies were cut into 2 mm explants (about 2–3 per biopsy), which were evenly distributed along with the transport medium into infection tubes (with 3 explants per tube per challenge virus). To test the viral neutralization with known concentrations of VRC01, some rectal pieces from control volunteers were preincubated for 24 hours with 0.3–10 μg/mL VRC01 (NIH AIDS Reagent Program) before viral challenge. Within 60–90 minutes of biopsy collection, rectal pieces were challenged for 2 hours at 37°C with 1 million or 3 million infectious particles of BaL26 or Du422.1, respectively. The virus inoculum for each strain was determined empirically by the dose of virus leading to infection in 90% of healthy rectal tissue, not incubated with bn-mAbs. A portion of the viral inoculum was saved for downstream analyses before washing of the explants 10 times using 500 μL exchanges of PBS in the infection tubes. The explants were then weighed by difference from the empty tube, transferred to individual Transwell inserts (Corning) containing Surgifoam supports (Ethicon), placed in a 24-well plate (Corning) containing 1.1 mL of growth medium (rectal transport medium with 50 IU/mL IL-2 [PeproTech]), and activated for 48 hours with 0.5 μg/mL pretitrated PHA (Remel, Thermo Fisher Scientific). Thereafter, medium was collected and replenished every 3 days for the duration of the 20-day culture.
Ex vivo vaginal challenges were performed similarly to the rectal challenges with the following modifications: Bal26 challenge virus was added directly to the original transport tubes containing whole vaginal biopsies (2–3 per tube) and transport medium, which also included 500 U/mL of IL-2, 25 ng/mL of IL-7, and 5 ng/mL of IL-15 (all from PeproTech), bringing the final volume up to 500 μL. After 2 hours at 37°C, each biopsy was weighed by difference and transferred to individual Transwell inserts (EMD Millipore) for washing and subsequent culture in a 24-well plate. After a portion of the viral inoculum was collected, the migrated cells were collected and distributed evenly among all Transwell inserts that contained individual biopsies. For 2 participants, a small vaginal biopsy disintegrated, leaving only 2 intact biopsies for explant culture. To wash the explants, PBS was added to the top of the inserts and to the bottom chambers, the Transwell plates were centrifuged, and the inserts were transferred to new wells. After 10 washes, the explants were activated for 24 hours with 0.2 or 0.6 μg/mL pretitrated PHA in transport medium (660 μL). Medium was collected and replenished again on day 2 after challenge, then every 3 days thereafter, to coincide with the collection schedule for rectal explant cultures.
To monitor HIV-1 infection, the sNLuc activity in 20 μL of conditioned explant culture medium was measured using the Nano-Glo Luciferase Assay System (Promega). The relative light unit (RLU) values were scaled by culture volume (RLU × culture volume [mL]/Nano-Glo assay volume [mL]) and plotted for each collection time point to visualize HIV-1 production over time. To quantify overall virus replication, log area under the curve (AUC) from days 2 to 20 after infection was calculated in Prism software version 8 (GraphPad), which served as the primary outcome measure for this mucosal study. The volume-scaled RLUs were multiplied by 1000 before log transformation such that all values were greater than 1, and these values were used to calculate AUC using a baseline equal to 0. Adjustment for tissue mass differences was not performed, as we found no correlation between explant mass and AUC (data not shown).
Statistics.
The study was designed based on preliminary experiments of rectal infectivity assays indicating that n = 4 provided 80% power to detect differences between tissues cultured with 1 μg/mL VRC01 and no mAb when challenged with Bal26.
Statistical comparisons were done with Prism software version 8 (GraphPad), and all tests were 2-sided. A P value less than 0.05 was considered significant. For ex vivo challenges, Dunn’s test was used to account for multiple comparisons of infectivity between controls and VRC01-infused samples, or between controls and exogenous VRC01-treated samples. Total HIV-1 replication levels are not directly comparable between rectal and vaginal assays because of differences in culture conditions (see above) that reflect the unique anatomical and immunological characteristics of each tissue type. Normalization of measured VRC01 concentrations by total IgG and total protein concentrations served as 2 methods to account for the different dilution factors between samples before the performing of statistical comparisons. Normalized VRC01 levels were compared within paired serum, secretions, and tissues using Friedman’s test, and comparisons between 2 specific locations were then analyzed using Dunn’s tests. Correlations were evaluated using Spearman’s rank correlation coefficients. For consistency, IgG-normalized VRC01 measurements were used for all correlation analyses, especially since total IgG levels are known to fluctuate in the cervicovaginal tract during the menstrual cycle (85).
Study approval.
All study protocols and study materials were approved by the appropriate institutional review board(s), including participating HVTN 104 sites (New York Blood Center Clinical Research Site, New York, New York; Brigham and Women’s Hospital Infectious Disease Clinical Trials Center, Boston, Massachusetts; Cleveland AIDS Clinical Trials Unit at Case Western Reserve University, Cleveland, Ohio; Columbia University HIV Vaccine Unit, New York, New York; University of Pennsylvania HIV Vaccine Trials Unit, Philadelphia, Pennsylvania) and the Seattle Vaccine Trials Unit at Fred Hutchinson Cancer Research Center. All participants provided written informed consent prior to participation, which included information about the risks of mucosal sample collections. All participant samples were deidentified at collection and handled in the laboratory with no access to any participant’s identifier information. All data presented were recoded with new participant IDs for publication purposes.
Author contributions
RDA and MPL contributed equally to this work and are co–first authors; they are listed alphabetically. RDA and MPL designed the study, performed experiments, provided data, analyzed the data, and wrote the initial draft manuscript and further edited the manuscript. SN, MP, KW, and LBF helped design and perform experiments, provided data, and edited the manuscript. KES, YH, LZ, and GT provided data and analyzed the data. YL analyzed data. JC designed the study, enrolled subjects, provided data, and wrote portions of the manuscript. MG, JL, and JH helped with the conduct of the substudy and edited the manuscript. CO and ABM contributed new reagents/assays and edited the manuscript. HVT, LB, SH, IF, NG, and KM were responsible for conduct of HVTN 104 and contributed to the nested study recruitment. MJM conceived, designed, and led the study, obtained funding for the study, contributed to data analysis and interpretation, and edited the manuscript.
Supplementary Material
Acknowledgments
We thank all our study participants enrolled from HVTN 104 and the Seattle Mucosal Study. We gratefully acknowledge the participation and support of many colleagues and staff on the HVTN 104 Protocol Team and at the Seattle Vaccine Trials Unit. We thank the late Benigno Rodriguez, PI of the Cleveland clinical trials site when this study was conducted. For their help coordinating the mucosal Seattle visits for HVTN 104 participants, we thank Rebecca Putnam and Weston Lawler. We thank Stephen Voght for critical reading of the manuscript and Laura Spuhler for help preparing display items. We thank Aaron Deal, Judith Lucas, Michael Archibald, Caroline Brackett, and Jack Heptinstall for their technical laboratory expertise. We also thank Greg Mize for preparation of the viruses for infectivity assays. This study was supported by the National Institute of Allergy and Infectious Diseases (UM1AI069481-S1, UM1AI068618-S2, P30AI064518-S1, UM1AI068618) and by the Bill & Melinda Gates Foundation (OPP1099507).
Version 1. 06/24/2021
In-Press Preview
Version 2. 08/16/2021
Electronic publication
Footnotes
Role of funding source: The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest: ABM, JL, MP, and SN are employed by the National Institute of Allergy and Infectious Diseases (NIAID), the HVTN 104 study sponsor and originator of the VRC01 antibody used in the study. All other authors are recipients of NIAID funding paid to their institutions, and this publication is a result of activities funded by the NIAID. ABM, JL, MP, and SN are not involved in the process of funding these awards nor in the administration of the scientific aspects of the awards, and, in accordance with NIAID policies, are deferred from decisions regarding funding of coauthors for a requisite period.
Copyright: © 2021, American Society for Clinical Investigation.
Reference information: J Clin Invest. 2021;131(16):e146975.https://doi.org/10.1172/JCI146975.
Contributor Information
Rena D. Astronomo, Email: rastrono@fredhutch.org.
Maria P. Lemos, Email: mlemos@fredhutch.org.
Sandeep R. Narpala, Email: sandeep.narpala@nih.gov.
Julie Czartoski, Email: jczartos@fredhutch.org.
Lamar Ballweber Fleming, Email: lballweb@fredhutch.org.
Kelly E. Seaton, Email: kelly.seaton@duke.edu.
Madhu Prabhakaran, Email: madhu.prabhakaran@nih.gov.
Yunda Huang, Email: yunda@scharp.org.
Yiwen Lu, Email: ylu2@scharp.org.
Katharine Westerberg, Email: kgw624@gmail.com.
Lily Zhang, Email: yzhang2@scharp.org.
Mary K. Gross, Email: mgross@fredhutch.org.
John Hural, Email: jhural@fhcrc.org.
Hong-Van Tieu, Email: htieu@nybloodcenter.org.
Lindsey R. Baden, Email: lbaden@partners.org.
Scott Hammer, Email: smh48@columbia.edu.
Ian Frank, Email: franki@mail.med.upenn.edu.
Christina Ochsenbauer, Email: christinaochsenbauer@uabmc.edu.
Nicole Grunenberg, Email: ngrunenb@fredhutch.org.
Julie E. Ledgerwood, Email: ledgerwood@mail.nih.gov.
Kenneth Mayer, Email: kmayer@fenwayhealth.org.
Georgia Tomaras, Email: georgia.tomaras@duke.edu.
Adrian B. McDermott, Email: adrian.mcdermott@nih.gov.
M. Juliana McElrath, Email: jmcelrat@fhcrc.org.
References
- 1. UNAIDS. UNAIDS Data 2019. https://www.unaids.org/en/resources/documents/2019/2019-UNAIDS-data Updated December 4, 2019. Accessed June 24, 2021.
- 2.Eakle R, et al. Pre-exposure prophylaxis (PrEP) in an era of stalled HIV prevention: can it change the game? Retrovirology. 2018;15(1):29. doi: 10.1186/s12977-018-0408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdool Karim SS, Baxter C. Microbicides for prevention of HIV infection: clinical efficacy trials. Curr Top Microbiol Immunol. 2014;383:97–115. doi: 10.1007/82_2013_330. [DOI] [PubMed] [Google Scholar]
- 4.Barouch DH, et al. Evaluation of a mosaic HIV-1 vaccine in a multicentre, randomised, double-blind, placebo-controlled, phase 1/2a clinical trial (APPROACH) and in rhesus monkeys (NHP 13-19) Lancet. 2018;392(10143):232–243. doi: 10.1016/S0140-6736(18)31364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansen SG, et al. A live-attenuated RhCMV/SIV vaccine shows long-term efficacy against heterologous SIV challenge. Sci Transl Med. 2019;11(501):eaaw2607. doi: 10.1126/scitranslmed.aaw2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Julg B, Barouch DH. Neutralizing antibodies for HIV-1 prevention. Curr Opin HIV AIDS. 2019;14(4):318–324. doi: 10.1097/COH.0000000000000556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haynes BF, et al. Multiple roles for HIV broadly neutralizing antibodies. Sci Transl Med. 2019;11(516):eaaz2686. doi: 10.1126/scitranslmed.aaz2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen SG, et al. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature. 2011;473(7348):523–527. doi: 10.1038/nature10003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stephenson KE, et al. Vaccines and broadly neutralizing antibodies for HIV-1 prevention. Annu Rev Immunol. 2020;38:673–703. doi: 10.1146/annurev-immunol-080219-023629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pegu A, et al. Use of broadly neutralizing antibodies for HIV-1 prevention. Immunol Rev. 2017;275(1):296–312. doi: 10.1111/imr.12511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baba TW, et al. Human neutralizing monoclonal antibodies of the IgG1 subtype protect against mucosal simian-human immunodeficiency virus infection. Nat Med. 2000;6(2):200–206. doi: 10.1038/72309. [DOI] [PubMed] [Google Scholar]
- 12.Mascola JR, et al. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat Med. 2000;6(2):207–210. doi: 10.1038/72318. [DOI] [PubMed] [Google Scholar]
- 13.Parren PW, et al. Antibody protects macaques against vaginal challenge with a pathogenic R5 simian/human immunodeficiency virus at serum levels giving complete neutralization in vitro. J Virol. 2001;75(17):8340–8347. doi: 10.1128/JVI.75.17.8340-8347.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hessell AJ, et al. Early short-term treatment with neutralizing human monoclonal antibodies halts SHIV infection in infant macaques. Nat Med. 2016;22(4):362–368. doi: 10.1038/nm.4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrantelli F, et al. Complete protection of neonatal rhesus macaques against oral exposure to pathogenic simian-human immunodeficiency virus by human anti-HIV monoclonal antibodies. J Infect Dis. 2004;189(12):2167–2173. doi: 10.1086/420833. [DOI] [PubMed] [Google Scholar]
- 16.Cheeseman HM, et al. Broadly neutralizing antibodies display potential for prevention of HIV-1 infection of mucosal tissue superior to that of nonneutralizing antibodies. J Virol. 2017;91(1):e01762-16. doi: 10.1128/JVI.01762-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Astronomo RD, et al. Neutralization takes precedence over IgG or IgA Isotype-related functions in mucosal HIV-1 antibody-mediated protection. EBioMedicine. 2016;14:97–111. doi: 10.1016/j.ebiom.2016.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott YM, et al. Broadly neutralizing anti-HIV antibodies prevent HIV Infection of mucosal tissue ex vivo. Antimicrob Agents Chemother. 2016;60(2):904–912. doi: 10.1128/AAC.02097-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sok D, Burton DR. Recent progress in broadly neutralizing antibodies to HIV. Nat Immunol. 2018;19(11):1179–1188. doi: 10.1038/s41590-018-0235-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCoy LE, Burton DR. Identification and specificity of broadly neutralizing antibodies against HIV. Immunol Rev. 2017;275(1):11–20. doi: 10.1111/imr.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gilbert PB, et al. Basis and statistical design of the passive HIV-1 antibody mediated prevention (AMP) test-of-concept efficacy trials. Stat Commun Infect Dis. 2017;9(1):20160001. doi: 10.1515/scid-2016-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou T, et al. Structural basis for broad and potent neutralization of HIV-1 by antibody VRC01. Science. 2010;329(5993):811–817. doi: 10.1126/science.1192819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Y, et al. Mechanism of neutralization by the broadly neutralizing HIV-1 monoclonal antibody VRC01. J Virol. 2011;85(17):8954–8967. doi: 10.1128/JVI.00754-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu X, et al. Rational design of envelope identifies broadly neutralizing human monoclonal antibodies to HIV-1. Science. 2010;329(5993):856–861. doi: 10.1126/science.1187659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gautam R, et al. A single injection of anti-HIV-1 antibodies protects against repeated SHIV challenges. Nature. 2016;533(7601):105–109. doi: 10.1038/nature17677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ko SY, et al. Enhanced neonatal Fc receptor function improves protection against primate SHIV infection. Nature. 2014;514(7524):642–645. doi: 10.1038/nature13612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pegu A, et al. Neutralizing antibodies to HIV-1 envelope protect more effectively in vivo than those to the CD4 receptor. Sci Transl Med. 2014;6(243):243ra88. doi: 10.1126/scitranslmed.3008992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun M, et al. VRC01 antibody protects against vaginal and rectal transmission of human immunodeficiency virus 1 in hu-BLT mice. Arch Virol. 2016;161(9):2449–2455. doi: 10.1007/s00705-016-2942-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Veselinovic M, et al. Topical gel formulation of broadly neutralizing anti-HIV-1 monoclonal antibody VRC01 confers protection against HIV-1 vaginal challenge in a humanized mouse model. Virology. 2012;432(2):505–510. doi: 10.1016/j.virol.2012.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saunders KO, et al. Sustained delivery of a broadly neutralizing antibody in nonhuman primates confers long-term protection against simian/human immunodeficiency virus infection. J Virol. 2015;89(11):5895–5903. doi: 10.1128/JVI.00210-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rudicell RS, et al. Enhanced potency of a broadly neutralizing HIV-1 antibody in vitro improves protection against lentiviral infection in vivo. J Virol. 2014;88(21):12669–12682. doi: 10.1128/JVI.02213-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mayer KH, et al. Safety, pharmacokinetics, and immunological activities of multiple intravenous or subcutaneous doses of an anti-HIV monoclonal antibody, VRC01, administered to HIV-uninfected adults: Results of a phase 1 randomized trial. PLoS Med. 2017;14(11):e1002435. doi: 10.1371/journal.pmed.1002435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ledgerwood JE, et al. Safety, pharmacokinetics and neutralization of the broadly neutralizing HIV-1 human monoclonal antibody VRC01 in healthy adults. Clin Exp Immunol. 2015;182(3):289–301. doi: 10.1111/cei.12692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bar KJ, et al. Effect of HIV antibody VRC01 on viral rebound after treatment interruption. N Engl J Med. 2016;375(21):2037–2050. doi: 10.1056/NEJMoa1608243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lynch RM, et al. Virologic effects of broadly neutralizing antibody VRC01 administration during chronic HIV-1 infection. Sci Transl Med. 2015;7(319):319ra206. doi: 10.1126/scitranslmed.aad5752. [DOI] [PubMed] [Google Scholar]
- 36.Riddler SA, et al. Randomized clinical trial to assess the impact of the broadly neutralizing HIV-1 monoclonal antibody VRC01 on HIV-1 persistence in individuals on effective ART. Open Forum Infect Dis. 2018;5(10):ofy242. doi: 10.1093/ofid/ofy242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corey L, et al. Two randomized trials of neutralizing antibodies to prevent HIV-1 acquisition. N Engl J Med. 2021;384(11):1003–1014. doi: 10.1056/NEJMoa2031738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klein K, et al. Neutralizing IgG at the portal of infection mediates protection against vaginal simian/human immunodeficiency virus challenge. J Virol. 2013;87(21):11604–11616. doi: 10.1128/JVI.01361-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prabhakaran M, et al. A sensitive method to quantify HIV-1 antibodies in mucosal samples. J Immunol Methods. 2021;491:112995. doi: 10.1016/j.jim.2021.112995. [DOI] [PubMed] [Google Scholar]
- 40.Huang Y, et al. Population pharmacokinetics analysis of VRC01, an HIV-1 broadly neutralizing monoclonal antibody, in healthy adults. MAbs. 2017;9(5):792–800. doi: 10.1080/19420862.2017.1311435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Archary D, et al. Distinct genital tract HIV-specific antibody profiles associated with tenofovir gel. Mucosal Immunol. 2016;9(3):821–833. doi: 10.1038/mi.2015.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eidelman S, Lagunoff D. The morphology of the normal human rectal biopsy. Hum Pathol. 1972;3(3):389–401. doi: 10.1016/S0046-8177(72)80039-X. [DOI] [PubMed] [Google Scholar]
- 43.Yoon H, et al. CATNAP: a tool to compile, analyze and tally neutralizing antibody panels. Nucleic Acids Res. 2015;43(W1):W213–W219. doi: 10.1093/nar/gkv404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Otsuka Y, et al. Diverse pathways of escape from all well-characterized VRC01-class broadly neutralizing HIV-1 antibodies. PLoS Pathog. 2018;14(8):e1007238. doi: 10.1371/journal.ppat.1007238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mowat AM, Viney JL. The anatomical basis of intestinal immunity. Immunol Rev. 1997;156:145–166. doi: 10.1111/j.1600-065X.1997.tb00966.x. [DOI] [PubMed] [Google Scholar]
- 46.Poles MA, et al. A preponderance of CCR5(+) CXCR4(+) mononuclear cells enhances gastrointestinal mucosal susceptibility to human immunodeficiency virus type 1 infection. J Virol. 2001;75(18):8390–8399. doi: 10.1128/JVI.75.18.8390-8399.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McElrath MJ, et al. Comprehensive assessment of HIV target cells in the distal human gut suggests increasing HIV susceptibility toward the anus. J Acquir Immune Defic Syndr. 2013;63(3):263–271. doi: 10.1097/QAI.0b013e3182898392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Patyka M, et al. Periluminal distribution of HIV-binding target cells and Gp340 in the oral, cervical and sigmoid/rectal mucosae: a mapping study. PLoS One. 2015;10(7):e0132942. doi: 10.1371/journal.pone.0132942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller CJ, Shattock RJ. Target cells in vaginal HIV transmission. Microbes Infect. 2003;5(1):59–67. doi: 10.1016/S1286-4579(02)00056-4. [DOI] [PubMed] [Google Scholar]
- 50.Shen R, et al. Interactions between HIV-1 and mucosal cells in the female reproductive tract. Am J Reprod Immunol. 2014;71(6):608–617. doi: 10.1111/aji.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shen R, et al. Macrophages in vaginal but not intestinal mucosa are monocyte-like and permissive to human immunodeficiency virus type 1 infection. J Virol. 2009;83(7):3258–3267. doi: 10.1128/JVI.01796-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pudney J, et al. Immunological microenvironments in the human vagina and cervix: mediators of cellular immunity are concentrated in the cervical transformation zone. Biol Reprod. 2005;73(6):1253–1263. doi: 10.1095/biolreprod.105.043133. [DOI] [PubMed] [Google Scholar]
- 53.Hladik F, et al. Initial events in establishing vaginal entry and infection by human immunodeficiency virus type-1. Immunity. 2007;26(2):257–270. doi: 10.1016/j.immuni.2007.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marovich M, et al. Monoclonal antibodies for prevention and treatment of COVID-19. JAMA. 2020;324(2):131–132. doi: 10.1001/jama.2020.10245. [DOI] [PubMed] [Google Scholar]
- 55.Marston HD, et al. Monoclonal antibodies for emerging infectious diseases — borrowing from history. N Engl J Med. 2018;378(16):1469–1472. doi: 10.1056/NEJMp1802256. [DOI] [PubMed] [Google Scholar]
- 56. Slifka MK, Amanna IJ. Passive immunization. In: Plotkin SA, et al., eds. Plotkin’s Vaccines. 7th ed. Elsevier; 2018:84–95.e10. [Google Scholar]
- 57.Bouvin-Pley M, et al. Evidence for a continuous drift of the HIV-1 species towards higher resistance to neutralizing antibodies over the course of the epidemic. PLoS Pathog. 2013;9(7):e1003477. doi: 10.1371/journal.ppat.1003477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wagh K, et al. Potential of conventional & bispecific broadly neutralizing antibodies for prevention of HIV-1 subtype A, C, & D infections. PLoS Pathog. 2018;14(3):e1006860. doi: 10.1371/journal.ppat.1006860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wright PF, et al. Mucosal immunity: the forgotten arm of the immune system. J Pediatric Infect Dis Soc. 2019;8(1):53–54. doi: 10.1093/jpids/pix102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Gross M, et al. Capturing Participant Data for Mucosal Interpretation: A Guide for HIV Investigators. https://www.niaid.nih.gov/sites/default/files/DAIDSMucosalGuide.pdf Updated April 2016. Accessed May 2021.
- 61.Fahrbach KM, et al. Differential binding of IgG and IgA to mucus of the female reproductive tract. PLoS One. 2013;8(10):e76176. doi: 10.1371/journal.pone.0076176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roopenian DC, et al. The MHC class I-like IgG receptor controls perinatal IgG transport, IgG homeostasis, and fate of IgG-Fc-coupled drugs. J Immunol. 2003;170(7):3528–3533. doi: 10.4049/jimmunol.170.7.3528. [DOI] [PubMed] [Google Scholar]
- 63.Iqbal Z, Dilnawaz F. Nanocarriers for vaginal drug delivery. Recent Pat Drug Deliv Formul. 2019;13(1):3–15. doi: 10.2174/1872211313666190215141507. [DOI] [PubMed] [Google Scholar]
- 64.Weber MA, et al. Vaginal microcirculation: non-invasive anatomical examination of the micro-vessel architecture, tortuosity and capillary density. Neurourol Urodyn. 2015;34(8):723–729. doi: 10.1002/nau.22662. [DOI] [PubMed] [Google Scholar]
- 65.Kumamoto Y, Iwasaki A. Unique features of antiviral immune system of the vaginal mucosa. Curr Opin Immunol. 2012;24(4):411–416. doi: 10.1016/j.coi.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Franklin RD, Kutteh WH. Characterization of immunoglobulins and cytokines in human cervical mucus: influence of exogenous and endogenous hormones. J Reprod Immunol. 1999;42(2):93–106. doi: 10.1016/S0165-0378(98)00086-2. [DOI] [PubMed] [Google Scholar]
- 67.Kutteh WH, et al. Variations in immunoglobulins and IgA subclasses of human uterine cervical secretions around the time of ovulation. Clin Exp Immunol. 1996;104(3):538–542. doi: 10.1046/j.1365-2249.1996.36742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kutteh WH, et al. Mucosal immunity in the female reproductive tract: correlation of immunoglobulins, cytokines, and reproductive hormones in human cervical mucus around the time of ovulation. AIDS Res Hum Retroviruses. 1998;14(suppl 1):S51–S55. [PubMed] [Google Scholar]
- 69.Nardelli-Haefliger D, et al. Specific antibody levels at the cervix during the menstrual cycle of women vaccinated with human papillomavirus 16 virus-like particles. J Natl Cancer Inst. 2003;95(15):1128–1137. doi: 10.1093/jnci/djg018. [DOI] [PubMed] [Google Scholar]
- 70.Wessels JM, et al. The relationship between sex hormones, the vaginal microbiome and immunity in HIV-1 susceptibility in women. Dis Model Mech. 2018;11(9):dmm035147. doi: 10.1242/dmm.035147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Grivel JC, et al. HIV-1 pathogenesis differs in rectosigmoid and tonsillar tissues infected ex vivo with CCR5- and CXCR4-tropic HIV-1. AIDS. 2007;21(10):1263–1272. doi: 10.1097/QAD.0b013e3281864667. [DOI] [PubMed] [Google Scholar]
- 72.King DF, et al. Mucosal tissue tropism and dissemination of HIV-1 subtype B acute envelope-expressing chimeric virus. J Virol. 2013;87(2):890–899. doi: 10.1128/JVI.02216-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Biancheri P, et al. Proteolytic cleavage and loss of function of biologic agents that neutralize tumor necrosis factor in the mucosa of patients with inflammatory bowel disease. Gastroenterology. 2015;149(6):1564–1574. doi: 10.1053/j.gastro.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 74.Suphaphiphat K, et al. Broadly neutralizing antibodies potently inhibit cell-to-cell transmission of semen leukocyte-derived SHIV162P3. EBioMedicine. 2020;57:102842. doi: 10.1016/j.ebiom.2020.102842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ducloy C, et al. HIV transmission from infected CD4+ T cells to allogenic T and dendritic cells is inhibited by broadly neutralizing antibodies. AIDS. 2018;32(10):1239–1245. doi: 10.1097/QAD.0000000000001834. [DOI] [PubMed] [Google Scholar]
- 76.McGowan I, et al. Long-acting rilpivirine as potential pre-exposure prophylaxis for HIV-1 prevention (the MWRI-01 study): an open-label, phase 1, compartmental, pharmacokinetic and pharmacodynamic assessment. Lancet HIV. 2016;3(12):e569–e578. doi: 10.1016/S2352-3018(16)30113-8. [DOI] [PubMed] [Google Scholar]
- 77.Dezzutti CS, et al. HIV-1 infection of female genital tract tissue for use in prevention studies. J Acquir Immune Defic Syndr. 2013;63(5):548–554. doi: 10.1097/QAI.0b013e318291f331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anton PA, et al. RMP-02/MTN-006: a phase 1 rectal safety, acceptability, pharmacokinetic, and pharmacodynamic study of tenofovir 1% gel compared with oral tenofovir disoproxil fumarate. AIDS Res Hum Retroviruses. 2012;28(11):1412–1421. doi: 10.1089/aid.2012.0262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gupta P, et al. High viral load in semen of human immunodeficiency virus type 1-infected men at all stages of disease and its reduction by therapy with protease and nonnucleoside reverse transcriptase inhibitors. J Virol. 1997;71(8):6271–6275. doi: 10.1128/jvi.71.8.6271-6275.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Liu J, et al. Antibody-mediated protection against SHIV challenge includes systemic clearance of distal virus. Science. 2016;353(6303):1045–1049. doi: 10.1126/science.aag0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Seaton KE, et al. HIV-1 specific IgA detected in vaginal secretions of HIV uninfected women participating in a microbicide trial in Southern Africa are primarily directed toward gp120 and gp140 specificities. PLoS One. 2014;9(7):e101863. doi: 10.1371/journal.pone.0101863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fong Y, et al. nCal: an R package for non-linear calibration. Bioinformatics. 2013;29(20):2653–2654. doi: 10.1093/bioinformatics/btt456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li Y, et al. Characterization of antibody responses elicited by human immunodeficiency virus type 1 primary isolate trimeric and monomeric envelope glycoproteins in selected adjuvants. J Virol. 2006;80(3):1414–1426. doi: 10.1128/JVI.80.3.1414-1426.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li M, et al. Genetic and neutralization properties of subtype C human immunodeficiency virus type 1 molecular env clones from acute and early heterosexually acquired infections in Southern Africa. J Virol. 2006;80(23):11776–11790. doi: 10.1128/JVI.01730-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Safaeian M, et al. Factors associated with fluctuations in IgA and IgG levels at the cervix during the menstrual cycle. J Infect Dis. 2009;199(3):455–463. doi: 10.1086/596060. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.