Abstract
Introduction
Pulmonary rehabilitation (PR) is a low cost, high impact intervention that ameliorates the disability associated with chronic respiratory diseases (CRD). PR is becoming increasingly recognized in low resource settings where the burden of CRD is rapidly increasing. To aid the implementation of PR in Uganda, we conducted a study to assess the attitudes and opinions towards PR among patients with CRD in Uganda and explore barriers faced by health care workers (HCWs) in referring to PR.
Methods
A cross-sectional study comprising two survey populations: people living with CRD and HCWs regarded as potential PR referrers and PR deliverers. This exploratory study sought initial opinions and thoughts regarding PR, as well as baseline knowledge and potential barriers faced in the referral process.
Results
Overall, 30 HCWs (53% female, 43% doctors) and 51 adults with CRD (63% female) participated in the survey. Among those with CRD, the majority reported breathlessness as a major problem (86%) and breathlessness affected their ability to do paid and unpaid work (70%). Interest in PR was high amongst adults with CRD (92%) with preference for a hospital-based programme (67%) as opposed to community-based (16%) or home-based (17%). All HCWs considered PR important in lung disease management, but 77% do not refer patients due to a lack of information about PR. HCWs’ free-text responses identified the need for training in PR, patient education and streamlining the referral process as key elements to develop successful PR referral services.
Conclusion
To successfully set up a PR service for people with CRD in Uganda, there is a great need for appropriately tailored training and education of prospective referrers about CRD and PR programs. Educating patients about the benefits of PR as well as streamlining the referral process is critical in expanding PR services across Uganda to fulfill this unmet need.
Keywords: respiratory rehabilitation, chronic chest symptoms, medical workers, enthusiasm, knowledge, training
Introduction
The burden of chronic respiratory disease (CRD) is increasing globally1 and remains the leading cause of death and disability worldwide.2 The risk factors for CRD such as indoor air pollution, respiratory infections like pulmonary tuberculosis (PTB)3 are rife in sub-Saharan Africa (SSA), but the prevalence of CRD in the region is surprisingly low.1 Management of CRD in SSA remains a major challenge with largely unavailable and unaffordable diagnostics and treatments.4
Pulmonary rehabilitation (PR) is an evidence-based,5–7 low-cost, non-pharmacological intervention that ameliorates the disability associated with CRD,7 and is frequently used in high-income countries. PR consists of supervised, individually prescribed exercise training and health education delivered to patients by a multidisciplinary team of health professionals, and has several benefits including improved mental state,7–9 functional exercise capacity, breathlessness and health-related quality of life (HRQoL).9–11 Despite well-known benefits of PR, its availability and practice in the African region is very low.12 Policy statements from the American Thoracic Society (ATS)/European Respiratory Society (ERS) recommend increasing the implementation and provision of PR worldwide through increasing health care worker (HCW) and patient knowledge and awareness of PR, increasing patient access to PR, HCW training and education, incorporating PR into the mainstream of medical practice and making it affordable for CRD patients.13–15 Uganda is one of the few African countries with a PR program; however, the service is largely unavailable across the country with no effective PR referral system. PR training for HCWs is not mandatory in Uganda , and exposure to PR for physiotherapists is limited. As a consequence, suitable patients are not referred for PR. Currently, there is increasing interest for PR in low- and middle-income countries (LMIC)16,17 and the treatment has shown some effectiveness in people with CRD, including post-TB lung disease (PTLD).12 However, referral rates of adults with CRD to PR programs remain low among HCWs in African settings,18 and PR uptake is low and largely underprovided.10 Information on factors affecting availability or uptake of PR services in resource-poor countries is lacking. With an increasing burden of CRDs, there is a need to implement PR that is appealing to patients, effective, deliverable and sustainable in resource poor countries.10
To develop and sustain a PR programme in existing health service delivery structures in Uganda and SSA at large, an exploration of PR service needs and requirements is crucial. Accordingly, this survey study aimed at assessing opinions and attitudes towards PR by people with CRD and exploring barriers HCWs face in the referral process, to inform setting up PR services in Uganda and regionally across Africa.
For adults with CRD (including chronic obstructive pulmonary disease (COPD) and PTLD) in Uganda, specific aims were to assess (i) the interest in participating in PR and (ii) the preferred mode of PR. For Ugandan HCWs in regular contact with adults with CRD, specific aims were (i) to assess the PR knowledge and (ii) to explore barriers faced in referring patients to PR.
Methods
Study Design
This was a cross-sectional survey study for HCWs who are potential PR referrers, and for adults with CRD, including COPD and PTLD in Uganda.
Study Setting and Participants
The study was conducted at the Makerere University Lung Institute (MLI) clinic, a specialist outpatient lung health clinic in Kampala, Uganda. Between 24th January 2020 and 10th August 2020, patients with CRD referred from various health facilities across the country for routine care at the MLI clinic were invited to participate in the survey. Adults (aged ≥18 years) with PTLD or spirometry confirmed COPD were included in the survey. All who did not return questionnaires were excluded. Spirometry testing was performed according to the ATS/ERS guidelines19 using a Pneumotrac® spirometer with Spirotrac® V software (Vitalograph Ltd., Buckingham, United Kingdom). Patients with PTLD had successfully completed treatment for microbiologically confirmed PTB but continued to experience chronic respiratory symptoms with radiological evidence of lung parenchymal damage.
During the same enrollment period, HCWs from different disciplines were invited to participate in the survey. All HCWs who reported being in regular contact with adults with CRD (regarded as potential PR referrers) and those who would potentially deliver PR (eg, doctors and physiotherapists) were included in the survey. Some of the HCWs were either PR providers or worked in health facilities that provide PR.
Study Procedure and Data Collection
People with CRD
Survey questionnaires (Appendix 1) were distributed to a sample of people with CRD, presenting to the MLI clinic for clinical evaluation as part of routine care. Study participants were consecutively approached to participate in the survey and all who responded were included. The surveys took approximately 5–10 minutes to complete and were anonymized. No patient identifiable information or clinical data were collected. Paper surveys were locked away in a secure cabinet before and after data entry. Participants could either complete the survey whilst attending their clinic appointment or the completed questionnaires would be returned a few days later in person or in a sealed envelope.
The survey questionnaires asked participants about their breathlessness in regard to their work, activity levels, visiting their friends or family, and if they would be interested in participating in a treatment that would help them become more physically active and experience less breathlessness. Furthermore, they were asked to express their opinions as to how and where they would prefer to have this treatment, and how long they would be willing to spend participating in PR.
HCWs
Survey questionnaires (Appendix 2) were distributed to HCWs working in hospitals, private health facilities and in the community around central Uganda where PR services are offered. A range of HCWs were targeted, including specialist physicians, general practitioners, nurses, and physiotherapists. No personal data were collected, except for their professional background and years of experience in managing people with CRD. Data were collected from HCWs in regards to their knowledge about PR, patient-based factors that influence their decision to recommend PR, and their experience with the PR referral process. HCWs were also asked if the Medical Research Council (MRC) dyspnea scale influenced their decision to refer patients for PR. The MRC dyspnea scale is a short and easy to use self-administered questionnaire based on the sensation of breathing difficulty experienced by the patient during daily life activities. It has grades ranging from 1 (none) to 5 (almost complete incapacity), with high grades indicating high perceived respiratory disability.20
After checking for completeness of the surveys, data were entered into Microsoft Excel Worksheet, then exported to Stata 15 statistical software (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC) for analysis.
Data Collection During the Corona Virus Disease 2019 (COVID-19) Pandemic
Due to the ongoing worldwide pandemic of COVID-19, lockdown measures were introduced by the government of Uganda on 18th March 2020 to curb the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The lockdowns markedly restricted movement of patients to health facilities. Although 80% of the survey data had been collected before the COVID-19 related lockdown in our country, fewer survey questionnaires were returned after the lockdown was enforced. When access to health facilities became easier as the lockdown was eased, CRD patients resumed hospital visits, and we were able to complete data collection.
Sample Size and Statistical Methods
Formal sample size calculation was not required, as this was an exploratory study designed to obtain baseline knowledge, initial opinions and thoughts regarding PR, as well as potential barriers faced in the referral process.
Quantitative Methods
The characteristics of the study population were summarized using descriptive statistics of frequency (%), mean and standard deviation (SD), or median and inter-quartile ranges (IQR) as appropriate.
Qualitative Methods
The qualitative data collected using the open-ended questionnaire were analyzed using autonomous qualitative counting.21 Particular words or phrases were grouped together into different categories, and then the number of times they were used in relation to a specific question were counted.
Ethics and Dissemination
The study received ethical approvals from the Mulago Hospital Research and Ethics Committee (MHREC1478), Kampala, Uganda as well as the Uganda National Council for Science and Technology (SS5105). Additional ethical approval was obtained from the University of Leicester research ethics committee (United Kingdom) (Ref No. 22349). The study was conducted in accordance with the International Council for Harmonization: Good Clinical Practice guidelines and the declaration of Helsinki. All participants provided written informed consent before taking part in the study.
Results
People with CRD
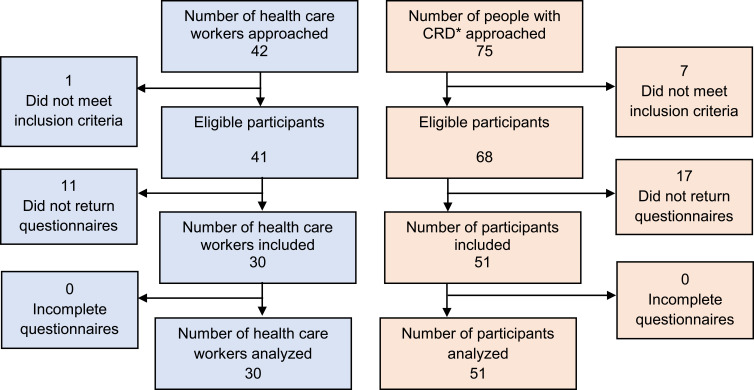
A total of 75 individuals with CRD (COPD and PTLD) were approached to participate in the survey and 51 were recruited. Of the 24 participants who did not participate, 7 presented with symptoms of an acute respiratory tract infection without underlying CRD, and 17 did not return questionnaires. A total of 51 patients with CRD were recruited (Figure 1).
Figure 1.
Diagram showing study recruitment.
Abbreviation: CRD, chronic respiratory disease.
HCWs
A total of 42 HCWs were approached to participate in the survey, and 30 were recruited. Of the 12 who did not participate, one was excluded (not in regular contact with patients) and 11 did not return questionnaires (Figure 1).
Participant Characteristics
HCWs
Overall, 53% (n=16) were females. The most common professional job category was hospital doctor (n=13, 43%), followed by physiotherapist (8, 27%), nurse (4, 13%), and then “other” which included pharmacists and patient counselors (5, 17%). HCW responsibilities included diagnosing (20, 66.7%), on-going management (18, 60%), prescribing (15, 50%), outpatient clinics (15, 50%), inpatient treatment (10, 33%), non-urgent care (8, 27%), urgent assessments (8, 27%), admission prevention (7, 23%), oxygen therapy (7, 23%), medication checks (7, 23%), primary care (6, 20%), and other (dispensing and referring patients (5, 17%)).
People with CRD
Overall, 63% were female, the majority (77%) were >40 years of age and 57% were unemployed (Table 1).
Table 1.
Characteristics of Study Participants with Chronic Respiratory Disease in Uganda. Data Presented as n (%) Except Where Stated
| Participant Characteristics | Frequency |
|---|---|
| Sex (female) | 32 (63.0%) |
| Age group | |
| <40 years | 12 (23.5%) |
| 40–50 years | 10 (19.6%) |
| 50–60 years | 9 (17.7%) |
| 60–70 years | 12 (23.5%) |
| 70–80 years | 3 (5.9%) |
| >80 years | 5 (9.8%) |
| Age when left full-time education (median years, IQR) | 22 (19–25) |
| Employment status | |
| Employed | 19 (37%) |
| Unemployed | 29 (57%) |
| Retired | 3 (6%) |
Abbreviation: IQR, Inter-Quartile Range.
Overall, 86% (n=44) of people with CRD reported breathlessness as a major problem. A breathing problem affected 71% (n=36) of participants’ ability to carry out paid work and 77% (n=39) of participants’ ability to carry out unpaid work. A total of 69% (n=35) had missed a day of work due to breathing problems. When asked about their ability to keep up with peers when walking, 69% (n=35) said they were unable to and breathing problems prevented 82% (n=42) from being as active as they would like. Furthermore, 63% (n=32) of participants reported breathing problems prevented them from visiting friends or family as often as they would have liked.
Interest in PR
Interest in PR was also assessed and 92% (n=47) of participants stated they would be interested in participating in a treatment that reduces breathlessness and increases activity. The preferred mode of PR was also assessed and 67% (n=34) preferred a group, supervised, hospital-based PR programme that lasts between 30 minutes to 1 hour per day (39%, n=20) (Table 2).
Table 2.
Patient Preference in Regard to the Mode of a Pulmonary Rehabilitation (PR) Programme
| Characteristic | Frequency (%) |
|---|---|
| Preferred mode of PR | |
| Group, supervised, hospital-based | 34 (66.7) |
| Group, supervised, local hospital or community based | 8 (15.7) |
| Exercise and educational manual at home | 9 (17.6) |
| Web-based | 0 (0) |
| Time willing to spend in PR | |
| <30 minutes /day | 13 (25.5) |
| 30 minutes to 1 hour /day | 20 (39.2) |
| 1 to 2 hours /day | 15 (29.4) |
| >2 hours /day | 3 (5.9) |
HCW Survey Results
In terms of PR being “worthwhile”, 97% (n=29) answered “Yes, very much”, and 3% (n=1) answered “Yes, a little”.
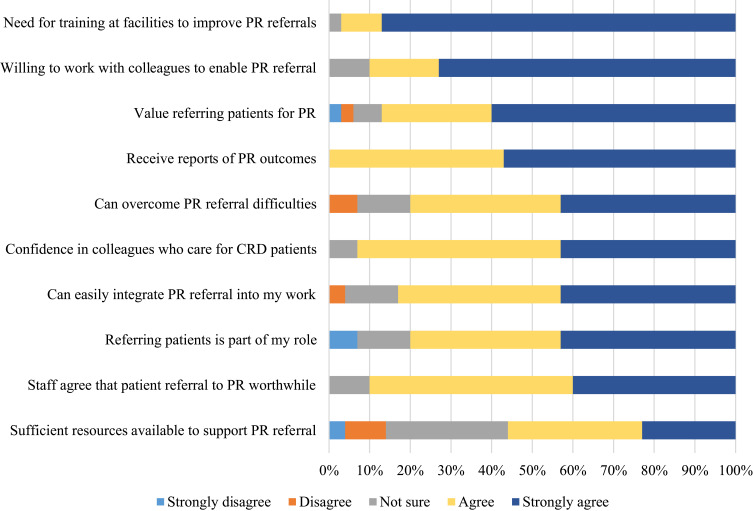
PR Referrals by HCWs (Figure 2)
Figure 2.
Health care worker opinions on referring to Pulmonary Rehabilitation (PR). Data presented as a percentage of those that strongly disagree, disagree, not sure, agree and strongly agreed.
Abbreviation: CRD, chronic respiratory disease.
The majority of HCWs strongly agreed that PR training at health facilities would improve PR referrals (97%, n=29) and that they were willing to work with colleagues to enable PR referrals (90%, n=27). A significant number agreed that they could easily integrate PR referral into their work (83%, n=25) and that referring patients to PR is worthwhile (90%, n=29).
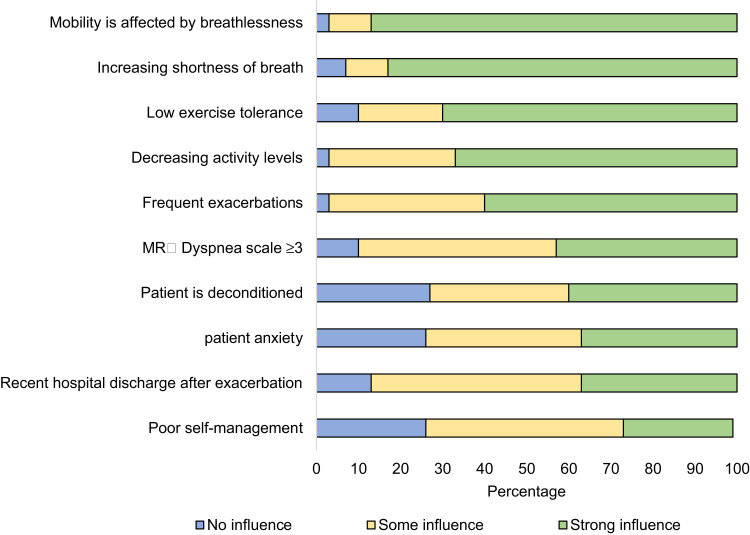
Patients Factors That Influence PR Referrals by HCWs (Figure 3)
Figure 3.
Patient-based factors influencing decision to refer to Pulmonary Rehabilitation, with influence graded as no, some or strong influence. Data presented as a percentage.
Abbreviation: MRC, Medical Research Council.
The patient-based factors that strongly influence HCW to refer to PR included breathlessness affecting movement (87%, n=26), increasing shortness of breath (83%, n=25), low exercise tolerance (70%, n=21) and decreasing activity levels (67%, n=20).
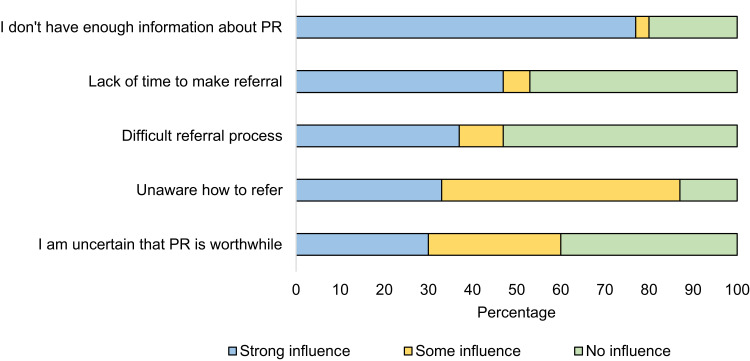
PR Referral Barriers (Figure 4)
Figure 4.
Referrer and referral process-based factors influencing decision not to refer patients to pulmonary rehabilitation (PR), with influence graded as no, some or strong influence. Data presented as a percentage.
Regarding barriers to PR referral, the referral process-based factors that strongly influence HCWs decision not to refer included: 77% (n=23) not having enough information about PR, 47% (n=14) lack time to complete the referral process, while 87% (n=26) reported that being unaware of how to refer to PR had some influence in not recommending or referring patients for the service.
Barriers to PR Referral
Two categories emerged following the question “how to improve referral and uptake of PR”, including the need for training and making the referral process easier. In terms of “need for training”, the following responses were mentioned: continuing medical education of PR and its benefits to patients, education, having adequate information about PR, knowledge on CRD and indications for PR, and adequate knowledge about PR and the referral process. Common responses related to “making the referral process easier” included referral form or tool, guidelines and criteria to guide referral of patients for PR, streamlining the referral process for HCWs, guidance on referral and clear referral criteria.
Discussion
In this survey study, breathlessness affected people’s ability to perform both paid and unpaid work, and a high number (92%) of people with CRD expressed interest in participating in PR. In addition, a high number (77%) of HCWs lacked enough information about PR to recommend or refer patients for this treatment; demonstrating the need for national training and education in PR to develop effective and sustainable PR referral systems in Uganda.
Breathlessness and activity limitation are common in CRD, and are the most troublesome symptoms reported by individuals with CRD.22 This may explain why people with CRD were highly interested in attending PR in our study. In contrast, Xie et al23 found that people with CRD in China were less enthusiastic about participating in PR despite knowledge of benefits of PR. This was mostly attributed to patients’ lack of enough information about PR.23 Although our survey did not seek to find out patients’ awareness of PR, educating patients about PR and its benefits was suggested by HCWs as one of the ways of encouraging patients to take up PR in our settings. This is congruent with the ATS/ERS policy statement that recommends increasing patient knowledge and awareness of PR as key aspects of increasing implementation of PR worldwide.13,15
This survey adds to existing knowledge of patients’ opinions on PR in Uganda. In a previous qualitative study with a similar group of PTLD patients in Uganda, improvements in respiratory symptoms, functional impairment and psychological well-being were reported by patients after PR.24 This survey provides opinions of CRD patients without prior exposure to PR and shows their willingness and readiness to participate this treatment.
The gap between patients’ enthusiasm for PR and the lack of awareness by HCWs of how to refer patients for this treatment in our study highlights a training need. Although the reasons for not recommending or referring people with CRD for PR may be multifactorial, increasing HCWs knowledge and awareness about the benefits of PR and its indications are key in setting up a successful PR programme. Clinical knowledge and skills are a critical factor in establishing and sustaining quality services, but many other factors in the work environment can directly or indirectly affect the quality of services and influence the ability of providers to apply their knowledge and skills in the services they offer.25 The lack of knowledge regarding content and benefits of PR remains a major barrier in setting up PR programs.26
Although PR in Uganda is delivered by physiotherapists, in-country formal education and training in PR is unavailable. Equipping physiotherapists across the country with PR skills is key in setting up a national PR service and potentially a training hub for the African region. Further training on how to incorporate low-cost PR within the existing physiotherapy work spaces at the health facilities would have a greater impact on PR service delivery. The incorporation of PR within existing facilities, infrastructure and staffing set-up will likely reduce the cost of the start-up and sustenance of the PR service.27 This approach would potentially be cost effective in improving uptake of PR in low resource settings, where health systems are not well adapted to manage CRD. A development study of PR in Uganda showed that it was feasible to run a low-cost PR programme within existing physiotherapy facilities within the health facility set-up.28 Participants with PTLD in Uganda reported clinically important improvements in exercise capacity and quality of life.28 Countrywide and regional training on how to set up and run low-cost PR programs has the potential to improve the quality of life of people with CRD in Uganda and is crucial in achieving sustainable development goal 3 (ensuring healthy lives and promoting well-being at all ages).16
Limitations
This was an exploratory study with a convenience sample and a small sample size, which provides a potential selection bias. In addition, recruited participants had presented to hospital, were more likely to have good health-seeking behavior, and therefore more motivated to participate in a hospital-based PR program. Furthermore, the study would have benefited from more in-depth, qualitative exploration, but the free-text responses available highlighted important training needs and educational barriers to be addressed and further investigated. However, this survey was an exploratory study designed to obtain baseline knowledge, initial opinions and thoughts in regard to PR and therefore these limitations have little effect on the study outcomes.
Generalizability
Data were collected in a national referral hospital where adults with CRD are referred to from across Uganda. Although this provides heterogeneity of the study population, it was a convenient sample and may be subject to selection bias. Therefore, the findings may not be generalized to the target population. However, the opinions gathered during this survey provided insights into the requirements of establishing a successful PR program and referral system. A larger survey would be needed to determine if these results are generalizable to the larger population.
Conclusion
To successfully set up PR services for people with CRD in low resource settings, there is a great need for appropriately tailored training and education of prospective referrers about CRD and PR programs. This survey identified an unmet need and desire for PR among people with CRD, yet knowledge and training of health care providers is low. There is a major need for training and education of HCWs about CRD and PR. Educating patients about the benefits of PR as well as streamlining the referral process is critical in setting up a successful PR program in Uganda.
Acknowledgments
We would like to acknowledge Dr. Jonathan Fuld Addenbrookes who allowed us to modify his original survey questionnaire and who was part of the team that designed the HCW survey questionnaire for this study. In addition, we would like to appreciate the HCWs and the people with CRD who participated in this study.
Study Registration
This study has been prospectively registered with the ISRCTN (ISRCTN44754061).
Disclosure
The authors report no conflicts of interest in this work.
This research was funded by the National Institute for Health Research (NIHR) (17/63/20) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK Department of Health and Social Care.
References
- 1.Labaki WW, Han MK. Chronic respiratory diseases: a global view. Lancet Respir Med. 2020;8(6):531–533. doi: 10.1016/S2213-2600(20)30157-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soriano JB, Kendrick PJ, Paulson KR, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. 2020;8(6):585–596. doi: 10.1016/S2213-2600(20)30105-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kiadaliri AA. GBD, Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kibirige D, Sanya RE, Nantanda R, et al. Availability and affordability of medicines and diagnostic tests recommended for management of asthma and chronic obstructive pulmonary disease in sub-Saharan Africa: a systematic review. Allergy Asthma Clin Immunol. 2019;15(1):14. doi: 10.1186/s13223-019-0329-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacasse Y, Wong E, Guyatt GH, et al. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane sys rev Eur medicophysica. 2007;43(4):475–485. [PubMed] [Google Scholar]
- 6.McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Sys Rev. 2015;1(2):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nici L, ZuWallack R, Wouters E, et al. On pulmonary rehabilitation and the flight of the bumblebee: the ATS/ERS Statement on Pulmonary Rehabilitation. Eur Respir J. 2006;28(3):461. doi: 10.1183/09031936.06.00075106 [DOI] [PubMed] [Google Scholar]
- 8.Coventry PA, Hind D. Comprehensive pulmonary rehabilitation for anxiety and depression in adults with chronic obstructive pulmonary disease: systematic review and meta-analysis. J Psychosom Res. 2007;63(5):551–565. doi: 10.1016/j.jpsychores.2007.08.002 [DOI] [PubMed] [Google Scholar]
- 9.Wouters EF, Posthuma R, Koopman M, et al. An update on pulmonary rehabilitation techniques for patients with chronic obstructive pulmonary disease. Expert Rev Respir Med. 2020;14(2):149–161. doi: 10.1080/17476348.2020.1700796 [DOI] [PubMed] [Google Scholar]
- 10.Habib GMM, Rabinovich R, Divgi K, et al. Systematic review of clinical effectiveness, components, and delivery of pulmonary rehabilitation in low-resource settings. Npj Primary Care Respir Med. 2020;30(1):52. doi: 10.1038/s41533-020-00210-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi: 10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 12.Bickton FM, Fombe C, Chisati E, et al. Evidence for pulmonary rehabilitation in chronic respiratory diseases in sub-Saharan Africa: a systematic review. Int J Tuberculosis Lung Dis. 2020;24(10):991–999. doi: 10.5588/ijtld.19.0526 [DOI] [PubMed] [Google Scholar]
- 13.Rochester CL, Vogiatzis I, Holland AE, et al. An official American Thoracic Society/European Respiratory Society Policy Statement: enhancing Implementation, Use, and Delivery of Pulmonary Rehabilitation. Am J Respir Crit Care Med. 2015;192(11):1373–1386. doi: 10.1164/rccm.201510-1966ST [DOI] [PubMed] [Google Scholar]
- 14.Nici L, Donner C, Wouters E, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173(12):1390–1413. doi: 10.1164/rccm.200508-1211ST [DOI] [PubMed] [Google Scholar]
- 15.Vogiatzis I, Rochester CL, Spruit MA, et al. Increasing implementation and delivery of pulmonary rehabilitation: key messages from the new ATS/ERS policy statement. Eur Respir J. 2016;47(5):1336. doi: 10.1183/13993003.02151-2015 [DOI] [PubMed] [Google Scholar]
- 16.Singh SJ, Halpin DMG, Salvi S, et al. Exercise and pulmonary rehabilitation for people with chronic lung disease in LMICs: challenges and opportunities. Lancet Respir Med. 2019;7(12):1002–1004. doi: 10.1016/S2213-2600(19)30364-9 [DOI] [PubMed] [Google Scholar]
- 17.Allwood BW, Byrne A, Meghji J. et al. Post-tuberculosis lung disease: clinical review of an under-recognised global challenge. Respiration;2021. 1–13. doi: 10.1159/000512531 [DOI] [PubMed] [Google Scholar]
- 18.Desalu OO, Onyedum CC, Adeoti AO, et al. Guideline-based COPD management in a resource-limited setting — physicians’ understanding, adherence and barriers: a cross-sectional survey of internal and family medicine hospital-based physicians in Nigeria. Primary Care Respir J. 2013;22(1):79–85. doi: 10.4104/pcrj.2013.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham BL, Steenbruggen I, Miller MR, et al. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88. doi: 10.1164/rccm.201908-1590ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stenton C. The MRC breathlessness scale. Occup Med (Chic Ill). 2008;58(3):226–227. doi: 10.1093/occmed/kqm162 [DOI] [PubMed] [Google Scholar]
- 21.Hannah DR, Lautsch BA. Counting in qualitative research: why to conduct it, when to avoid it, and when to closet it. J Management Inquiry. 2011;20(1):14–22. doi: 10.1177/1056492610375988 [DOI] [Google Scholar]
- 22.O’Donnell DE. Advances in the evaluation of respiratory pathophysiology during exercise in chronic lung diseases. Front Physiol. 2017;8:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xie L, Liu Z, Hao S, et al. Assessment of knowledge, attitude, and practice towards pulmonary rehabilitation among COPD patients: a multicenter and cross-sectional survey in China. Respir Med. 2020;174:106198. doi: 10.1016/j.rmed.2020.106198 [DOI] [PubMed] [Google Scholar]
- 24.Jones R, Muyinda H, Nyakoojo G, et al. Does pulmonary rehabilitation alter patients’ experiences of living with chronic respiratory disease? A qualitative study. Int J Chron Obstruct Pulmon Dis. 2018;13:2375–2385. doi: 10.2147/COPD.S165623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelson D, Dufour W. Transfer of learning: A guide for strengthening the performance of health care workers. Education Resources Information Center; 2002. [Google Scholar]
- 26.Alsubaiei ME, Cafarella P, Frith P, et al. Barriers for setting up a pulmonary rehabilitation program in the Eastern Province of Saudi Arabia. Ann Thorac Med. 2016;11(2):121. doi: 10.4103/1817-1737.180028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cox NS, Oliveira CC, Lahham A, et al. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: a systematic review using the theoretical domains framework. J Physiother. 2017;63(2):84–93. doi: 10.1016/j.jphys.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 28.Jones R, Kirenga BJ, Katagira W, et al. A pre–post intervention study of pulmonary rehabilitation for adults with post-tuberculosis lung disease in Uganda. Int J Chron Obstruct Pulmon Dis. 2017;12:3533. doi: 10.2147/COPD.S146659 [DOI] [PMC free article] [PubMed] [Google Scholar]