Abstract
Objectives
This study was to conduct a meta‐analysis of studies that used actigraphs to compare the influence of day and night shifts on the sleep quality of workers as well as examine the moderating effect of age.
Methods
Databases including PubMed, CINAHL, the Cochrane Library, MEDLINE, and EBSCOhost were searched for relevant studies published in English between January 1st, 2000 and April 30st, 2021. Our main targets were studies that used actigraphs to assess the sleep quality of night shift workers. This meta‐analysis included 12 papers and was performed using Comprehensive Meta‐Analysis (CMA) Version 3.0. Effect sizes were displayed in a forest plot using standardized mean difference (SMD) and 95% confidence intervals (CI).
Results
Among the sleep quality indices of the day and night shift workers, no significant difference existed in terms of sleep efficiency (SE) (SMD = 0.27, 95% CI: −0.03‐0.57), whereas night shift workers presented longer sleep‐onset latency (SOL) (SMD = 0.62, 95% CI: 0.15‐1.08), greater wake after sleep onset (WASO) (SMD = 0.41, 95% CI: 0.12‐0.70), and longer total sleep time (TST) (SMD = 0.85, 95% CI: 0.32‐1.39) than did day shift workers. The differences between the day and night shift workers in SOL, WASO, and TST did not vary with age.
Conclusions
Among the sleep quality indices, night shift workers presented longer SOL and greater WASO than did day shift workers. However, night shift workers could regulate their rest time and had adequate TST; thus, their SE was not different from that of day shift workers.
Keywords: actigraph, day shift, meta‐analysis, night shift, sleep quality, worker
1. INTRODUCTION
Sleep quality is an extremely complex health issue that involves an individual's genetics, physiological characteristics, physical health, psychological factors, such as emotions and cognition, as well as family, social, and environmental factors.1 Sleep quality is a crucial condition in an individual's satisfaction with their own healthiness.2 Not only does poor sleep quality affect job performance, but high sleep debt also causes chronic fatigue.3 Long‐term fatigue and inadequate rest lower one's alertness and therefore increase the chance of accidents.4 Research on the impact of sleep on health has found that unfulfilled sleep needs can cause headaches, tiredness, inattention, memory loss, poor performance, and psychological disorders.5, 6 Sleep issues may even increase the risk of cancers such as head and neck cancer, bladder cancer, thyroid cancer, non‐Hodgkin lymphoma, and myeloma in men as well as breast cancer, ovarian cancer, and non‐Hodgkin lymphoma in women.7 Furthermore, sleep disorders have been found to strongly correlate with inflammatory diseases and autoimmune diseases.8, 9 Thus, the importance of sleep quality should not be underestimated.
The primary factor affecting sleep is changes in one's circadian rhythms. For those who work during the night, the inconsistencies between their internal circadian rhythms and the required routines of the external environment can lead to disturbances in their sleep‐wake cycles and light‐dark cycles that then result in circadian rhythm disorders.1 Night shift workers must alter their biological clock and are often sleep‐deprived, remaining awake at night and working rather than sleeping during the night. Moreover, not only is their sleep during the day often disrupted, which consequently affects deep sleep, but it often takes them longer to fall asleep, all of which easily lead to inadequate sleep.10 Night shift workers sleep during the day during which their circadian rhythm is not in the optimal state for sleep, affecting the quality of their sleep and causing fatigue. At night when they work, their circadian rhythm makes them drowsy and less alert, which could impact work safety and productivity.11, 12 The study conducted by Vitale et al further indicates that after working a night shift, night shift workers often have difficulty maintaining good sleep quality and difficulty falling asleep in the evening before a shift change to the day shift. This is because their sleep is often disrupted, for example by street noise, family activities, or phones or doorbells ringing.13 In addition, the quality of sleep may change, and as the sleep cycle changes, there is less rapid‐eye‐movement sleep.14
It has been shown that sleep quality is highly associated with age. The occurrence of spontaneous sleep disruptions increases with age, which also causes changes in sleep and affects sleep quality.15 The pineal gland behind the third cerebral ventricle in the back of the brain secretes melatonin, a hormone that plays a crucial role in the control of the sleep‐wake cycle and begins to rise at around three months after birth. Associated with the biological clock, the levels of melatonin decrease during the day and rise during the night. Melatonin levels in the blood after one falls asleep at night are generally 10 times higher than levels during the day.16 Secretions of melatonin during the night are highest in infants, gradually decrease with age, and then drop significantly after the age of 45. In old age, circadian rhythms begin to lapse and may even disappear.17
Furthermore, the evaluation of sleep quality can be subjective or objective. Self‐reported questionnaires can provide participant data regarding individualized problems as well as subjective sleep data; however, researchers often have difficulty removing bias from their observations, which can lead to incomplete records and observations.18 Actigraphy involves the wearing of a measurement device on the wrist with sensory abilities, quantitative processing, and storage functions. This instrument can store days, weeks, or even months of data and is therefore more suitable for long‐term sleep quality monitoring than is polysomnography (PSG), which measures brain waves.19 The aims of this study were to conduct a meta‐analysis of studies comparing the influence of day and night shift work on sleep quality using actigraphs and to examine the moderating effects of age.
2. METHODS AND MEASURES
2.1. Literature search and screening
We collected and examined literature involving differences in sleep quality between individuals working day and night shifts. This study was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta‐Analysis (PRISMA).20 Figure 1 displays the screening process. The databases used included PubMed, CINAHL, Cochrane Library, MEDLINE, and EBSCOhost, and the keywords that were searched for included “night shift”, “night duty”, “day shift”, “actigraph”, “actiwatch”, “sleep quality”, and “sleep deprivation”. The inclusion criteria for the papers compiled and evaluated in this study were as follows: (1) the participants included workers working night shift, which was defined as a shift beginning between 22:00 and 2:00 at night and ending between 5:00 and 8:00 the next morning in a three‐shift system or a shift beginning between 16:00 to 17:00 in the evening and ending between 6:00 to 7:00 the next morning in a two‐shift system21, 22; (2) the paper used sleep quality as the performance index, and the tools used to assess sleep quality must have included an actigraph; and (3) the study was published in English. The exclusion criteria were the following: (1) the paper was a literature review or case report or (2) the complete results or full‐text of the paper could not be obtained.
FIGURE 1.
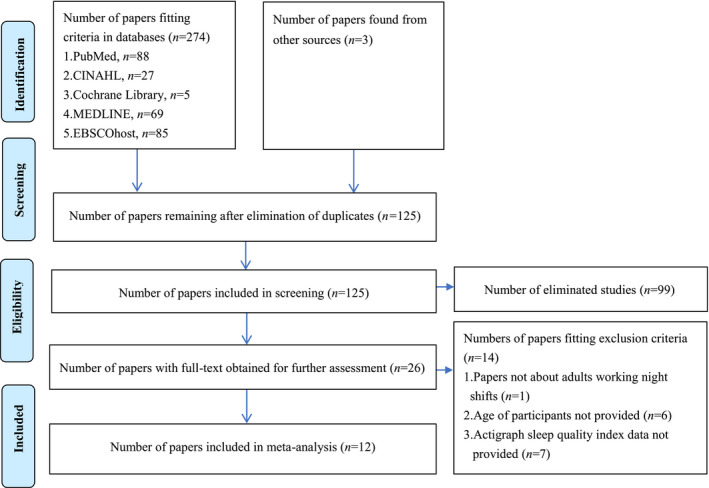
PRISMA data search process
2.2. Data extraction, quality appraisal, and recommendation level determination
After reading the abstracts, we eliminated the papers that did not fit the criteria of our study and obtained 26 papers. Subsequent reading and assessment of the full‐text version of those papers resulted in 12 eligible papers for our analysis. Figure 1 displays the screening process. The quality of the obtained papers was assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross Sectional Studies, which included eight items: (1) whether the criteria for inclusion in the sample were clearly defined, (2) whether the study subjects and the settings were described in detail, (3) whether the participant measurement methods were described in detail, (4) whether objective and standard criteria were used for measurements of the condition, (5) whether confounding factors were identified, (6) whether strategies to deal with confounding factors were stated, (7) whether the outcomes were measured in a valid and reliable way, and (8) whether appropriate statistical analysis was used. The appraisals were independently made by two reviewers, and the responses were “0”, “1”, or “2”, which respectively indicated “Yes”, “No”, or “Unclear”. Only the “1” responses were given 1 point each; the other responses were given no points.23 Only papers with a total score of 4 points or higher were included in our analysis. For interrater reliability, the English version of SPSS 22.0 was employed to calculate the Kappa coefficient, which was 0.924. The research designs, data, and appraisal scores of the 12 papers included in our meta‐analysis are presented in Table 1.
TABLE 1.
Experiment methods and results of papers in meta‐analysis
| First author (Year) | Country | Design | No. of participants | Occupation | Gender |
Age Mean (SD) |
Scheduling rules |
Duration of actigraph data (days) |
Results of actigraph sleep indices |
Empirical level |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Dayshift | Nightshift | ||||||||||
|
Baek (2020)24 |
Korea | Prospective | 94 | Nurses | Female | 28.09 (4.28) |
Night shift for 2‐3 consecutive days at least once per month, and each individual could have rapidly changed to different shifts over a period of 5 days Day shift: 7:00‐15:30 Evening shift: 15:00‐23:30 Night shift: 22:30‐23:00‐7:30 of next day |
14 | SE (%) | 78.01 (13.35) | 77.14 (12.90) | 6/8 |
| SOL (min) | 33.03 (37.98) | 34.39 (36.71) | ||||||||||
| WASO (min) | 30.34 (23.18) | 42.58 (30.94) | ||||||||||
| TST (hour) | 5.31 (1.71) | 7.12 (2.64) | ||||||||||
| Chang (2019)25 | Taiwan | Cross‐sectional |
Day:58 Night:43 |
Nurses | Female | 26.62 (5.00) |
Slow shift change once per month Day shift: 8:00‐16:00 Evening shift: 16:00‐24:00 Night shift: 0:00‐8:00 |
7 | WASO (min) | 30.14 (34.99) | 36.67 (24.23) | 5/8 |
| Choi (2016)26 | Korea | Cross‐sectional | 12 | Nurses | Female | 26.40 (4.01) | Each individual rotated through day, evening, and night shifts over a period of two weeks | 14 | SE (%) | 86.24 (8.73) | 84.67 (7.72) | 6/8 |
| SOL (min) | 7.19 (14.96) | 5.22 (8.24) | ||||||||||
| WASO (min) | 37.40 (28.79) | 31.48 (15.57) | ||||||||||
| TST (hour) | 5.55 (1.45) | 5.20 (2.01) | ||||||||||
| Flynn‐Evans (2018)27 | USA | Cross‐sectional | 41 | Pilots |
Male Female |
30.80 (7.10) | Day shift for 5 days, rest for 3 days, evening shift for 5 days, rest for 3 days, night shift for 5 days, and then rest for 4 days | 5 | SE (%) | 81.00 (7.00) | 81.00 (9.00) | 5/8 |
| SOL (min) | 21.00 (17.00) | 24.00 (28.00) | ||||||||||
| WASO (min) | 45.00 (30.00) | 55.00 (40.00) | ||||||||||
| TST (hour) | 5.70 (0.73) | 6.69 (0.93) | ||||||||||
| Ganesan (2019)28 | Australia | Cross‐sectional | 44 |
Nurses Doctors |
Male Female |
33.80 (9.70) |
Nurses rotated to different shifts irregularly Day shift: 7:00‐15:30 Evening shift: 13:00‐21:30 Night shift: 21:00‐7:30 of next day Doctors worked days shifts 8:00‐21:00 for 7 days, rested for 7 days, worked night shifts 20:00‐9:00 for 7 days, and then rested for 7 days |
28 | WASO (min) | 151.80 (78.60) | 315.00 (127.20) | 5/8 |
| TST (hour) | 5.74 (1.17) | 6.36 (1.18) | ||||||||||
| Kang (2014)29 | Taiwan | Cross‐sectional |
Day:16 Night:13 |
Nurses | Female | 25.90 (3.19) | Slow shift change once per month Day shift: 8:00‐16:00 Evening shift: 16:00‐24:00 Night shift: 0:00‐8:00 | 7 | SE (%) | 96.53 (1.69) | 95.24 (3.08) | 6/8 |
| SOL (min) | 13.87 (7.15) | 9.08 (3.06) | ||||||||||
| WASO (min) | 15.91 (8.86) | 19.63 (10.37) | ||||||||||
| TST (hour) | 6.45 (1.05) | 6.62 (1.35) | ||||||||||
| Lamond (2005)30 | Australia | Cross‐sectional | 14 |
Train drivers |
Male | 46.60 (4.90) |
Rapid shift changes over a period of 3 days Day shift: 4:00‐12:00 Evening shift: 12:00‐20:00 Night shift: 20:00‐04:00 of next day |
3 | SE (%) | 77.80 (15.60) | 79.30 (15.40) | 6/8 |
| SOL (min) | 37.70 (45.70) | 28.40 (33.40) | ||||||||||
| TST (hour) | 3.60 (1.00) | 4.60 (1.10) | ||||||||||
| Martin (2015)31 | Canada | Cross‐sectional | 39 | Police officers |
Male Female |
28.90 (3.20) |
Rapid shift changes over a period of 3 days Day shift: 7:00‐15:00 Evening shift: 15:00‐23:00 Night shift: 00:00‐7:00 |
4 | SE (%) | 85.00 (4.80) | 85.10 (4.30) | 6/8 |
| SOL (min) | 9.00 (8.00) | 7.00 (6.00) | ||||||||||
| WASO (min) | 42.00 (14.00) | 39.00 (14.00) | ||||||||||
| TST (hour) | 6.02 (0.78) | 5.30 (0.87) | ||||||||||
| Niu (2013)32 | Taiwan | Prospective |
Day:30 Night:32 |
Nurses | Female | 27.76 (4.31) |
Day shift for 5 days, rest for 5 days, night shift for 5 days, and then rest for 5 days Day shift: 7:30‐15:30 Evening shift: 15:30‐23:30 Night shift: 23:30‐7:30 of next day |
9 | SE (%) | 79.48 (2.64) | 82.37 (1.92) | 5/8 |
| SOL (min) | 5.48 (1.75) | 11.50 (2.80) | ||||||||||
| WASO (min) | 87.07 (10.83) | 88.77 (12.45) | ||||||||||
| TST (hour) | 5.67 (0.25) | 7.16 (0.44) | ||||||||||
| Sadeghniiat‐ Haghighi (2020)33 | Iran | Cross‐sectional |
Day:4 Night:10 |
Oil rig workers | Male | 35.90 (7.90) |
Day shift for 2 weeks, rest for 2 weeks, night shift for 2 weeks, and then rest for 2 weeks Day shift: 12 hours Night shift: 12 hours |
14 | TST (hour) | 5.97 (0.87) | 6.17 (0.98) | 6/8 |
| Saksvik (2011)34 | Norway | Cross‐sectional |
Day:4 Night:10 |
Oil rig workers | Male | 44.00 (8.57) |
Day shift for 2 weeks, rest for 2 weeks, night shift for 2 weeks, and then rest for 2 weeks Day shift: 7:00‐19:00 Night shift: 19:00‐7:00 of next day |
14 | SE (%) | 84.00 (6.35) | 83.00 (6.47) | 6/8 |
| Tremaine (2011)35 | Australia | Cross‐sectional | 17 | Midwives | Male Female | 46.80 (10.30) |
Rapid rotation through day, evening, and night shifts Start time day shift: 6:00‐9:00 Start time evening shift: 11:00‐17:00 Start time night shift: 20:00‐22:00 |
28 | SOL (min) | 12.38 (15.82) | 9.29 (14.51) | 7/8 |
| WASO (min) | 42.85 (20.59) | 44.67 (23.69) | ||||||||||
| TST (hour) | 5.97 (1.04) | 6.11 (1.80) | ||||||||||
Abbreviation: SE, Sleep efficiency; SOL, Sleep‐onset latency; TST, Total sleep time; WASO, Wake after sleep onset.
We employed the Grading of Recommendation Assessment, Development, and Evaluation (GRADE) methodology developed by the GRADE Working Group to assess the quality of evidence and make clear comprehensive recommendations regarding the differences between the various sleep quality indices of day shift and night shift workers. For randomized control trials, the quality of evidence began at “High”, and the final rating was then determined based on various upgrading and downgrading factors. For observational studies, the quality of evidence began at “Low”, and the final rating was then determined based on the various upgrading and downgrading factors.36, 37
2.3. Actigraphs and sleep quality indices
Actigraphs have a built‐in accelerometer to record a subject's activities during the entire day and night, and noninvasive acceleration sensors are used to detect changes in the subject's motions, which are then recorded and analyzed using software. The activity records can then be used to determine the subject's sleep parameters. An increasing number of sleep‐related studies are using actigraphy to gauge the sleep quality of their participants.38 Some researchers believe that the objective sleep quality measurements derived using actigraphy are more suitable than are sleep‐related questionnaires.39 The sleep quality indices that actigraphy often uses in measurements include the following: sleep efficiency (SE), which equals the ratio of total sleep time (TST) to time in bed (TIB); sleep‐onset latency (SOL), which is the duration of time between getting in bed to falling asleep; wake after sleep onset (WASO), which is the total amount of time of wakefulness after sleep onset during the night; and total sleep time (TST), which is the actual amount of time spent asleep during the night and equals TIB minus other wake time durations. At present, most sleep tests mainly use brain wave signals to assess sleep quality. Although PSG is considered the gold standard and offers high accuracy, it is costly and requires professionally trained technicians to operate and interpret results. The test location must also be a designated sleep laboratory or center. For these reasons, actigraphy is more suitable than is PSG for monitoring long‐term sleep quality. Actigraphy is also currently the simplest objective method of measuring sleep quality, and it has been employed in many studies.40, 41 McCall and McCall used two‐tailed t‐tests to compare the sleep quality parameters derived using actigraphy and PSG and discovered no significant differences in SOL (24.2 ± 28.0 vs 28.4 ± 36.9), SE (82.7 ± 9.8 vs 80.7 ± 13.4), WASO (61.2 ± 40.2 vs 80.7 ± 13.4), or TST (400.4 ± 41.9 vs 387.5 ± 64.5).19
2.4. Data processing and statistical analysis methods
Our meta‐analysis was performed using Comprehensive Meta‐Analysis (CMA) Version 3.0. Homogeneity or heterogeneity was examined using Cochran's Q test. A Q value presenting significant differences (P < .05) indicated that heterogeneity existed among the samples. Inconsistency was determined based on I2 in the range from 0% to 100%. An I2 value less than 50% indicated homogeneity, whereby the fixed effects model was then used to calculate the weighted average. An I2 value greater than 50% indicated heterogeneity, whereby the random effects model was then used to calculate the weighted average. Effect sizes were displayed in forest plots using standardized mean difference (SMD) and a 95% confidence interval (CI). Sensitivity analysis was conducted to determine whether the elimination of any paper would influence the overall conclusion. Egger's regression was applied to examine whether publication bias existed. Finally, meta‐regression analysis was performed to compare the sleep quality indices of day and night shift workers after controlling age as a factor.
3. RESULTS
3.1. Literature characteristics and quality
According to the inclusion and exclusion criteria above, we obtained a total of 12 papers: 8 for SE meta‐analysis,24, 26, 27, 29, 30, 31, 32, 34 8 for SOL meta‐analysis,24, 26, 27, 29, 30, 31, 32, 35 9 for WASO meta‐analysis,24, 25, 26, 27, 28, 29, 31, 32, 35 and 10 for TST meta‐analysis.24, 26, 27, 28, 29, 30, 31, 32, 33, 35 Table 1 presents the basic characteristics and quality ratings of the included studies, and Table 2 shows a summary of the analysis results and the determined quality of the evidence in the studies.
TABLE 2.
Summary of meta‐analysis results and GRADE evidence profile
| Quality assessment | Summary of findings | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
No. of studies |
Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Day shift | Night shift | Effect size | Quality of evidence | ||
| No. of participants | Mean (SD) | No. of participants | Mean (SD) | SMD (95% CI) | ||||||||
| SE (%) | ||||||||||||
| 8 | 7 observational studies, 1 randomized trial | Seriousa | Seriousb | No serious | No serious | Undetected | 250 | 83.51 (7.52) | 255 | 83.48 (7.60) | 0.27 (−0.03, 0.57) |
⊕⊕○○ low because of lack of blinding and heterogeneity |
| SOL (min) | ||||||||||||
| 8 | 7 observational studies, 1 randomized trial | Seriousa | Seriousb | No serious | No serious | Undetected | 263 | 17.46 (18.55) | 262 | 16.11 (16.59) | 0.62 ( 0.15, 1.08) |
⊕⊕○○ low because of lack of blinding and heterogeneity |
| WASO (min) | ||||||||||||
| 9 | 8 observational studies, 1 randomized trial | Seriousa | Seriousb | No serious | No serious | Undetected | 351 | 53.61 (27.76) | 335 | 74.76 (33.16) | 0.41 ( 0.12, 0.70) |
⊕⊕○○ low because of lack of blinding and heterogeneity |
| TST (hour) | ||||||||||||
| 10 | 9 observational studies, 1 randomized trial | Seriousa | Seriousb | No serious | No serious | Undetected | 311 | 5.60 (1.01) | 316 | 6.13 (1.33) | 0.85 ( 0.32, 1.39) |
⊕⊕⊕○ moderate because of lack of blinding, heterogeneity and large effect (upgrading quality) |
Abbreviation: 95% CI, 95% Confidence interval; SD, Standard deviation; SDM, Standard deviation of the mean; SE, Sleep efficiency; SOL, Sleep‐onset latency; TST, Total sleep time; WASO, Wake after sleep onset.n
Lack of blinding.
Tests of heterogeneity.
3.2. Comparison of SE of day and night shift workers
The heterogeneity test presented statistically significant differences (P = .014), and I2 equaled 60.24%, thereby indicating heterogeneity among the eight papers. We therefore employed the random effects model. The forest plot presented an SMD of 0.27 and a 95% CI of −0.03‐0.57, which indicated no significant differences between the SE of the day shift workers and that of the night shift workers (P = .076). The relative weight of Baek et al was 18.60% and greater than those of the other papers (Figure 2).24 Furthermore, our sensitivity analysis revealed no significant changes in the SMD following the removal of any individual paper (95% CI = −0.03‐0.57). In the linear regression (Egger's) test, P = .402, which indicated no publication bias among the included papers. The meta‐regression analysis showed that after the age was controlled, there was still no significant difference between the SE of the day shift workers and that of the night shift workers (P =.481) (Table 3).
FIGURE 2.
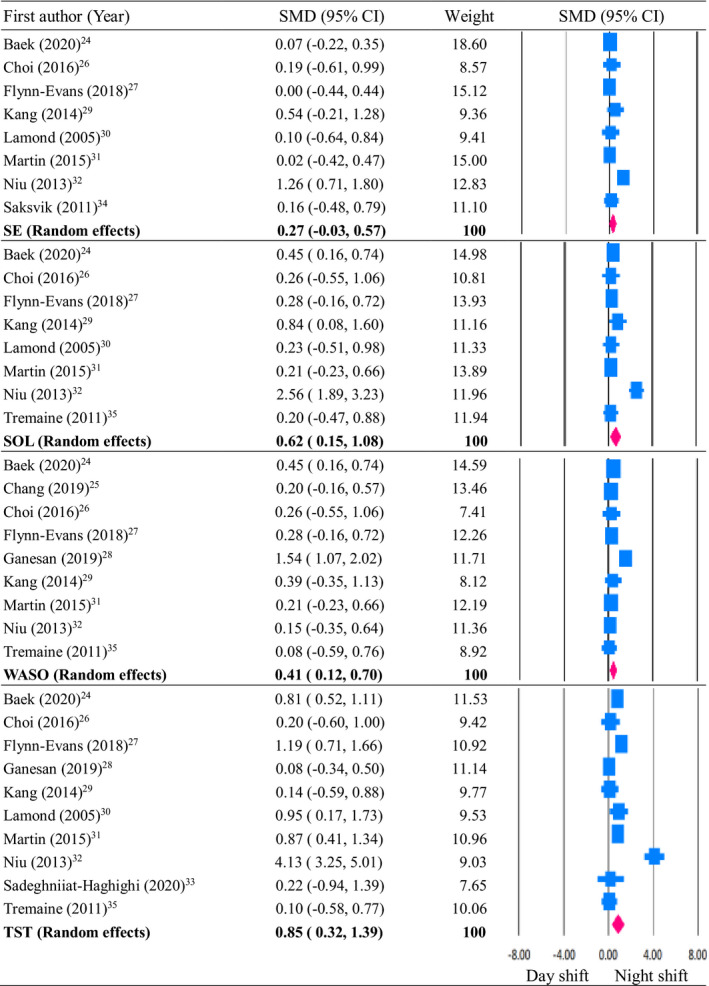
Sleep quality differences between day and night shift workers
 Result of single study;
Result of single study;  CI;
CI;  Combined effect
Combined effect
Abbrevation: Sleep efficiency, SE; Sleep‐onset latency, SOL; Wake after sleep onset, WASO; Total sleep time, TST; Standard deviation of the mean, SDM; 95% Confidence interval, 95% CI.
TABLE 3.
Meta‐regression analysis of influence of age on sleep parameters of day and night shift workers
| Sleep parameter | Model | β | SE2 | 95% CI | Z‐value | p |
|---|---|---|---|---|---|---|
| SE1 | Intercept | 0.73 | 0.68 | −0.59‐2.06 | 1.08 | 0.279 |
| Age | −0.02 | 0.02 | −0.06‐0.03 | −0.70 | 0.481 | |
| SOL | Intercept | 1.62 | 1.03 | −0.39‐3.62 | 1.58 | 0.115 |
| Age | −0.03 | 0.03 | −0.09‐0.03 | −1.00 | 0.315 | |
| WASO | Intercept | 0.19 | 0.79 | −1.36‐1.73 | 0.24 | 0.813 |
| Age | 0.01 | 0.03 | −0.04‐0.06 | 0.29 | 0.774 | |
| TST | Intercept | 2.01 | 1.54 | −1.02‐5.03 | 1.30 | 0.194 |
| Age | −0.04 | 0.05 | −0.12‐0.06 | −0.76 | 0.446 |
Abbreviations: β, Standardized beta; 95%CI, 95% Confidence interval; SE1, Sleep efficiency; SE2, Standard erroe; SOL, Sleep‐onset latency; TST, Total sleep time; WASO, Wake after sleep onset.
3.3. Comparison of SOL of day and night shift workers
The heterogeneity test presented statistically significant differences (P < .001), and I2 equaled 82.97%, thereby indicating heterogeneity among the eight papers. We therefore employed the random effects model. The forest plot presented an SMD of 0.62 and a 95% CI of 0.15‐1.08, which indicated that the SOL of the night shift workers was longer than that of the day shift workers (P = .010). The relative weight of Baek et al was 14.98% and greater than those of the other papers (Figure 2).24 Furthermore, our sensitivity analysis revealed no significant changes in the SMD following the elimination of any individual paper (95% CI = 0.15‐1.08). In the linear regression (Egger's) test, P = .526, indicating no publication bias among the included papers. The meta‐regression analysis showed that after age was controlled, the SOL of the night shift workers remained longer than that of the day shift workers (P = .315) (Table 3).
3.4. Comparison of WASO of day and night shift workers
The heterogeneity test presented statistically significant differences (P = .001), and I2 equaled 69.54%, thereby indicating heterogeneity among the nine papers. We therefore employed the random effects model. The forest plot presented an SMD of 0.41 and a 95% CI of 0.12‐0.70, which indicated that the WASO of the night shift workers was greater than that of the day shift workers (P = .006). The relative weight of Baek et al was 14.59% and greater than those of the other papers (Figure 2).24 Furthermore, our sensitivity analysis revealed no significant changes in the SMD following the removal of any individual paper (95% CI = 0.12‐0.70). In the linear regression (Egger's) test, P = .911, indicating no publication bias among the included papers. The meta‐regression analysis showed that after age was controlled, the WASO of the night shift workers was still greater than that of the day shift workers (P = .774) (Table 3).
3.5. Comparison of TST of day and night shift workers
The heterogeneity test presented statistically significant differences (P = .001), and I2 equaled 88.64%, thereby indicating heterogeneity among the 10 papers. We therefore employed the random effects model. The forest plot presented an SMD of 0.85 and a 95% CI of 0.32‐1.39, indicating that the TST of the night shift workers was longer than that of the day shift workers (P = .002). The relative weight of Baek et al was 11.53% and greater than those of the other papers (Figure 2).24 Furthermore, our sensitivity analysis revealed no significant changes in the SMD following the elimination of any individual paper (95% CI = 0.32‐1.39). In the linear regression (Egger's) test, P = .678, indicating no publication bias among the included papers. The meta‐regression analysis showed that after age was controlled, the TST of the night shift workers remained longer than that of the day shift workers (P = .446) (Table 3).
4. DISCUSSION
Our meta‐analysis revealed longer SOL and greater WASO among night shift workers than among day shift workers when these were measured using actigraphs. Although the night shift workers had longer TST than did the day shift workers, the two groups of workers showed no differences in SE. Furthermore, the differences between the day and night shift workers in SOL, WASO, and TST did not vary with age.
Based on the quality of evidence standards in GRADE,36, 37 there were no significant differences between SE (the ratio of TST to TIB) of the night shift workers and that of the day shift workers. In actigraphy, sleep logs are required to derive the time in bed because there may be discrepancies when participants recall their bedtime and wake‐up time; further long‐term research is therefore needed to reconcile these discrepancies. We therefore believe that the quality of the evidence is low. As for our recommendation regarding SOL, the observational studies that we collected indicated that the SOL measured using actigraphy was longer in night shift workers than in day shift workers. We therefore recommend that night shift workers not only block out all light but also wear sleep masks when sleeping during the day to increase melatonin secretion and shorten their SOL.42 We therefore believe that the quality of the evidence is low. Regarding our recommendation involving WASO, the observational studies that we collected similarly indicated that the WASO measured using actigraphy was longer in night shift workers than in day shift workers. We therefore recommend that night shift workers maintain quiet sleeping environments at a comfortable temperature with lighting that simulates nighttime (such as using thicker curtains). We also recommend that night shift workers restrict friends and family from calling when sleeping during the day. These actions could prevent their sleep from being disrupting as much as possible and thereby reduce their WASO.43 We therefore believe that the quality of the evidence is low. We also believe that the quality of the evidence regarding TST is moderate. The observational studies showed that the TST measured using actigraphy was longer in night shift workers than in day shift workers. Although night shift workers suffer from poor sleep quality when sleeping during the day, this can be partially remedied by increasing their duration of sleep.44 Moreover, investigations on the influence of night shift work on TST cannot consider TST alone; thus, other sleep quality indices should also be taken into account to determine overall sleep quality.
Data regarding the sleep quality of individuals who must work the night shift have generally been collected using questionnaire surveys.45, 46 Furthermore, rotating between day and night shifts can lead to irregular schedules; therefore, objective actigraphy can provide an understanding of actual sleep conditions.47 One study simultaneously used actigraphs and the Pittsburgh Sleep Quality Index (PSQI) when comparing the sleep quality of workers working rotating shifts in the manufacturing industry. The results revealed many differences between the sleep indices derived using the subjective PSQI and those derived using objective actigraphy. For the day shift workers, the PSQI‐based SOL and TST were longer than those obtained using actigraphs, whereas for the night shift workers, the PSQI‐based TST was also longer than that obtained using actigraphs.48
SOL represents the time for which it takes a person to fall asleep after getting into bed. Ideally, falling asleep should be shortly after the lights are turned off.49 The light during the day can indeed make it difficult to fall asleep for night shift workers.42 Moreover, their sleep during the day is often disrupted; consequently, night shift workers have difficulty achieving deep sleep, and their SOL is longer.50
The sleep issues of night shift workers are associated not only with work itself but also with their lifestyle.51 Rotenberg et al discovered that night shift workers have different patterns for their day sleep and social life that are easily affected by the environment, such as light, noise, uncomfortable temperatures, and phone rings. As a result, their sleep is easily disrupted, which causes night shift workers to have greater WASO during the day than do day shift workers during the night.43 This offers an explanation for the results of our meta‐analysis: working the night shift makes it more difficult to fall asleep and maintain sleep, compared with working the day shift; thus, night shift workers have longer SOL and greater WASO than do day shift workers.
Most existing studies indicate that night shift workers have poorer TST and SE.32, 52, 53 However, the TST measured using actigraphy by Vanttola et al revealed no significant differences between day and night shift workers, even though the night shift workers felt that they had significantly shorter TST, according to the subjective questionnaire given to the same participants.54 Our meta‐analysis found that night shift workers had longer TST than did the day shift workers, though the two groups of workers showed no significant differences in SE, due perhaps to the fact that the night shift workers in fact slept for longer durations despite having difficulty sleeping, sleeping lightly, or sleeping sporadically. We speculate that their TIB was also longer, which is why their SE was not significantly different from that of day shift workers.
Mizuno et al used actigraphs to collect 7 to 8 days of sleep data from seven flight control personnel working the night shift, with the data encompassing three to four consecutive night shifts. The authors observed that the participants would nap for a while during the day before their first night shift and that their TIB and TST increased significantly on the day prior to their first night shift. Significantly increased TIB and TST were also observed on the day after the first night shift. In other words, increases in TIB and TST were observed on the days before and after the night shifts. These observations confirmed that the workers may have adjusted their sleep time to adjust to night shift work.44 Dumont et al also found a positive correlation between the sleep quality of night shift workers and their sleep experience when working night shifts.55 Taken together, it suggests that SE would not be affected if night shift workers have an in‐depth understanding of their sleep conditions and could moderate their schedules to obtain adequate sleep time.
Some researchers believe that declining sleep quality is generally associated with age, noting that the ability of older individuals working night shifts to make circadian adjustments declines and that advancing age may affect one's ability to adapt to night shift work.56 Other researchers, however, have argued to the contrary. Costa declared that work experience increases with age, which instead helps workers to better adjust their sleep habits so that night shift work is better dealt with.57 Pires et al also pointed out that older workers who maintain good sleep habits can maintain TST and SE similar to those of younger workers. In addition, the impact of circadian rhythm disorders on sleep quality is greater than the impact of age on sleep quality. The occurrence of poor sleep quality among night shift workers sleeping during the day after work is higher than that among day shift workers regardless of age because the sleep of night shift workers during the day is often disrupted; consequently, night shift workers not only have difficulty sleeping deeply, but it also takes them longer to fall asleep.53 Niedhammer et al investigated the influence of different shifts on sleep among 469 nurses and found that the nurses often compensated for lost sleep during shift changes. For instance, their daily TST increased on the two days before and after night shifts, becoming longer than seven hours on average.58 These findings were consistent with those of our meta‐analysis.
5. STUDY LIMITATIONS
This meta‐analysis excluded research papers in which data for age were not available and only included studies in English. Therefore, the interpretations of the overall conclusion may be more reserved. None of the compiled papers were randomized controlled trials; thus, the influence of night shifts on sleep quality may require more research data with greater rigor for evidence. Although studies have indicated that night shift work may influence the sleep quality of nurses, these issues may also be associated with other factors, such as the number of children that the nurses had, exercise habits, and obesity. However, the data compiled in this meta‐analysis indicated that most studies did not control these confounding factors; therefore, more research will be needed in the future.
6. CONCLUSION
The results of this meta‐analysis demonstrate that according to actigraphs, night shifts may affect the sleep quality of workers. Among the sleep quality indices, night shift workers presented longer SOL and greater WASO than did day shift workers. Furthermore, the impact of working night shifts on sleep quality is greater than that of age; that is, the differences between the day and night shift workers in terms of SOL, WASO, and TST did not vary with age.
DISCLOSURE
Approval of the research protocol: N/A. Informed Consent: N/A. Registry and the Registration No. of the study/Trial: N/A. Animal Studies: N/A. Conflict of Interest: The authors declare that they have no competing interests.
AUTHOR CONTRIBUTIONS
WP Chang and YX Peng performed the literature search and helped write the manuscript; WP Chang conceived and revised the article; and WP Chang and YX Peng approved the final version of the manuscript.
ACKNOWLEDGMENT
This research received no specific grant from any funding agency in the commercial, or not‐for‐profit sectors.
Chang W‐P, Peng Y‐X. Meta‐analysis of differences in sleep quality based on actigraphs between day and night shift workers and the moderating effect of age. J Occup Health. 2021;63:e12262. 10.1002/1348-9585.12262
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1.James SM, Honn KA, Gaddameedhi S, Van Dongen HPA. Shift work: disrupted circadian rhythms and sleep‐implications for health and well‐being. Curr Sleep Med Rep. 2017;3:104‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shao MF, Chou YC, Yeh MY, Tzeng WC. Sleep quality and quality of life in female shift‐working nurses. J Adv Nurs. 2010;66:1565‐1572. [DOI] [PubMed] [Google Scholar]
- 3.Techera U, Hallowell M, Stambaugh N, Littlejohn R. Causes and consequences of occupational fatigue: meta‐analysis and systems model. J Occup Environ Med. 2016;58:961‐973. [DOI] [PubMed] [Google Scholar]
- 4.Ferri P, Guadi M, Marcheselli L, Balduzzi S, Magnani D, Di Lorenzo R. The impact of shift work on the psychological and physical health of nurses in a general hospital: a comparison between rotating night shifts and day shifts. Risk Manag Healthc Policy. 2016;9:203‐211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin YK, Lin GY, Lee JT, et al. Associations between sleep quality and migraine frequency: a cross‐sectional case‐control study. Medicine (Baltimore). 2016;95:e3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie W, Berry A, Lustig C, Deldin P, Zhang W. Poor sleep quality and compromised visual working memory capacity. J Int Neuropsychol Soc. 2019;25:583‐594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gu F, Xiao Q, Chu LW, et al. Sleep duration and cancer in the NIH‐AARP diet and health study cohort. PLoS ONE. 2016;11:e0161561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta‐analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80:40‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zielinski MR, Systrom DM, Rose NR. Fatigue, sleep, and autoimmune and related disorders. Front Immunol. 2019;10:1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caruso CC, Baldwin CM, Berger A, et al. Position statement: reducing fatigue associated with sleep deficiency and work hours in nurses. Nurs Outlook. 2017;65:766‐768. [DOI] [PubMed] [Google Scholar]
- 11.Izadpanah F, Nikfar S, Bakhshi Imcheh F, Amini M, Zargaran M. Assessment of frequency and causes of medication errors in pediatrics and emergency wards of Teaching Hospitals affiliated to Tehran University of Medical Sciences (24 hospitals). J Med Life. 2018;11:299‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anzan M, Alwhaibi M, Almetwazi M, Alhawassi TM. Prescribing errors and associated factors in discharge prescriptions in the emergency department: a prospective cross‐sectional study. PLoS ONE. 2021;16:e0245321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vitale S, Varrone‐Ganesh J, Vu M. Nurses working the night shift: impact on home, family and social life. J Nurs Educ Pract. 2015;5:70‐78. [Google Scholar]
- 14.Boudreau P, Dumont GA, Boivin DB. Circadian adaptation to night shift work influences sleep, performance, mood and the autonomic modulation of the heart. PLoS ONE. 2013;8:e70813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim AS, Yu L, Costa MD, et al. Quantification of the fragmentation of rest‐activity patterns in elderly individuals using a state transition analysis. Sleep. 2011;34:1569‐1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masters A, Pandi‐Perumal SR, Seixas A, Girardin JL, McFarlane SI. Melatonin, the hormone of darkness: from sleep promotion to Ebola treatment. Brain Disord Ther. 2014;4:1000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okatani Y, Morioka N, Wakatsuki A. Changes in nocturnal melatonin secretion in perimenopausal women: correlation with endogenous estrogen concentrations. J Pineal Res. 2000;28:111‐118. [DOI] [PubMed] [Google Scholar]
- 18.Kreitchmann RS, Abad FJ, Ponsoda V, Nieto MD, Morillo D. Controlling for response biases in self‐report scales: forced‐choice vs. psychometric modeling of Likert items. Front Psychol. 2019;10:2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCall C, McCall WV. Comparison of actigraphy with polysomnography and sleep logs in depressed insomniacs. J Sleep Res. 2012;21:122‐127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosa R, Colligan M. Plain Language About Shiftwork. U.S. Dept. of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Biomedical and Behavioral Science, Education and Information Division; 1997. [Google Scholar]
- 22.Borges FNS, Fischer FM, Rotenberg L, et al. Effects of naps at work on the sleepiness of 12‐hour night shift nursing personnel. Sleep Sci. 2009;2:24‐29. [Google Scholar]
- 23.Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z (Editors). Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute, 2017. Available from https://reviewersmanual.joannabriggs.org/ [Google Scholar]
- 24.Baek J, Han K, Choi‐Kwon S. Sleep diary‐ and actigraphy‐derived sleep parameters of 8‐hour fast‐rotating shift work nurses: a prospective descriptive study. Int J Nurs Stud. 2020;112:103719. [DOI] [PubMed] [Google Scholar]
- 25.Chang WP, Li HB. Differences in workday sleep fragmentation, rest‐activity cycle, sleep quality, and activity level among nurses working different shifts. Chronobiol Int. 2019;36:1761‐1771. [DOI] [PubMed] [Google Scholar]
- 26.Choi SJ, Joo EY. Light exposure and sleep‐wake pattern in rapidly rotating shift nurses. J Sleep Med. 2016;13:8‐14. [Google Scholar]
- 27.Flynn‐Evans EE, Arsintescu L, Gregory K, Mulligan J, Nowinski J, Feary M. Sleep and neurobehavioral performance vary by work start time during non‐traditional day shifts. Sleep Health. 2018;4:476‐484. [DOI] [PubMed] [Google Scholar]
- 28.Ganesan S, Magee M, Stone JE, et al. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci Rep. 2019;9:4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang JH, Miao NF, Tseng IJ, Sithole T, Chung MH. Circadian activity rhythms and sleep in nurses working fixed 8‐hr shifts. Biol Res Nurs. 2015;17:348‐355. [DOI] [PubMed] [Google Scholar]
- 30.Lamond N, Darwent D, Dawson D. How well do train driver's sleep in relay vans? Ind Health. 2005;43:98‐104. [DOI] [PubMed] [Google Scholar]
- 31.Martin JS, Laberge L, Sasseville A, et al. Day and night shift schedules are associated with lower sleep quality in evening‐types. Chronobiol Int. 2015;32:627‐636. [DOI] [PubMed] [Google Scholar]
- 32.Niu SF, Chu H, Chung MH, Lin CC, Chang YS, Chou KR. Sleep quality in nurses: a randomized clinical trial of day and night shift workers. Biol Res Nurs. 2013;15:273‐279. [DOI] [PubMed] [Google Scholar]
- 33.Sadeghniiat‐Haghighi K, Zahabi A, Najafi A, Rahimi‐Golkhandan A, Aminian O. Evaluating the quality and duration of sleep using actigraphy in petroleum industry shift workers. Sleep Health. 2020;6:407‐410. [DOI] [PubMed] [Google Scholar]
- 34.Saksvik IB, Bjorvatn B, Harvey AG, Waage S, Harris A, Pallesen S. Adaptation and readaptation to different shift work schedules measured with sleep diary and actigraphy. J Occup Health Psychol. 2011;16:331‐344. [DOI] [PubMed] [Google Scholar]
- 35.Tremaine R, Dorrian J, Paterson J, et al. Actigraph estimates of the sleep of Australian midwives: the impact of shift work. Biol Res Nurs. 2013;15:191‐199. [DOI] [PubMed] [Google Scholar]
- 36.Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380‐382. [DOI] [PubMed] [Google Scholar]
- 37.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924‐926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139:1514‐1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Girschik J, Fritschi L, Heyworth J, Waters F. Validation of self‐reported sleep against actigraphy. J Epidemiol. 2012;22:462‐468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meltzer LJ, Hiruma LS, Avis K, Montgomery‐Downs H, Valentin J. Comparison of a commercial accelerometer with polysomnography and actigraphy in children and adolescents. Sleep. 2015;38:1323‐1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marino M, Li Y, Rueschman MN, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36:1747‐1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jensen HI, Markvart J, Holst R, et al. Shift work and quality of sleep: effect of working in designed dynamic light. Int Arch Occup Environ Health. 2016;89:49‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rotenberg L, Moreno C, Benedito‐Silva AA, Menna‐Barreto L, Luiz M‐B. Sleep/wake cycle parameters and sleep/fatigue complaints in female night workers. Biol Rhythm Res. 1998;29:585‐590. [Google Scholar]
- 44.Mizuno K, Matsumoto A, Aiba T, et al. Sleep patterns among shift‐working flight controllers of the International Space Station: an observational study on the JAXA Flight Control Team. J Physiol Anthropol. 2016;35:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ko SB. Night shift work, sleep quality, and obesity. J Lifestyle Med. 2013;3:110‐116. [PMC free article] [PubMed] [Google Scholar]
- 46.Lajoie P, Aronson KJ, Day A, et al. A cross‐sectional study of shift work, sleep quality and cardiometabolic risk in female hospital employees. BMJ Open. 2015;5:e007327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng PC, Walch OJ, Cuamatzi‐Castelan A, Drake C. Predicting circadian phase in night shift workers using actigraphy. Sleep Sci. 2019;12:29‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen CP, Huang SW, Chang CL. Sleep quality of shift workers through actigraphy sleep analysis from SOMNOwatch™. Int J Simul: Syst, Sci Technol. 2016;17:4.1‐4.7. [Google Scholar]
- 49.Shrivastava D, Jung S, Saadat M, Sirohi R, Crewson K. How to interpret the results of a sleep study. J Community Hosp Intern Med Perspect. 2014;4:24983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Labyak S, Lava S, Turek F, Zee P. Effects of shiftwork on sleep and menstrual function in nurses. Health Care Women Int. 2002;23:703‐714. [DOI] [PubMed] [Google Scholar]
- 51.Ohida T, Takemura S, Nozaki N, Kawahara K, Sugie T, Uehata T. The influence of lifestyle and night‐shift work on sleep problems among female hospital nurses in Japan. Nihon Koshu Eisei Zasshi. 2001;48:595‐603. [PubMed] [Google Scholar]
- 52.Gumenyuk V, Howard R, Roth T, Korzyukov O, Drake CL. Sleep loss, circadian mismatch, and abnormalities in reorienting of attention in night workers with shift work disorder. Sleep. 2014;37:545‐556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pires MLN, Teixeira CW, Esteves AM, et al. Sleep, ageing and night work. Braz J Med Biol Res. 2009;42:839‐843. [DOI] [PubMed] [Google Scholar]
- 54.Vanttola P, Härmä M, Viitasalo K, et al. Sleep and alertness in shift work disorder: findings of a field study. Int Arch Occup Environ Health. 2019;92:523‐533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dumont M, Montplaisir J, Infante‐Rivard C. Sleep quality of former night‐shift workers. Int J Occup Environ Health. 1997;3:S10‐S14. [PubMed] [Google Scholar]
- 56.Gommans FG, Jansen NW, Stynen D, De Grip A, Kant I. Need for recovery across work careers: the impact of work, health and personal characteristics. Int Arch Occup Environ Health. 2015;88:281‐295. [DOI] [PubMed] [Google Scholar]
- 57.Costa G. Some considerations about aging, shift work and work ability. Int Congr Ser. 2005;1280:67‐72. [Google Scholar]
- 58.Niedhammer I, Lert F, Marne MJ. Effects of shift work on sleep among French nurses. J Occup Med. 1994;36:667‐674. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


