Abstract
Background:
Offloading interventions are commonly used in clinical practice to heal foot ulcers. The aim of this updated systematic review is to investigate the effectiveness of offloading interventions to heal diabetic foot ulcers.
Methods:
We updated our previous systematic review search of PubMed, EMBASE, and Cochrane databases to also include original studies published between July 29, 2014 and August 13, 2018 relating to four offloading intervention categories in populations with diabetic foot ulcers: (a) offloading devices, (b) footwear, (c) other offloading techniques, and (d) surgical offloading techniques. Outcomes included ulcer healing, plantar pressure, ambulatory activity, adherence, adverse events, patient-reported measures, and cost-effectiveness. Included controlled studies were assessed for methodological quality and had key data extracted into evidence and risk of bias tables. Included non-controlled studies were summarised on a narrative basis.
Results:
We identified 41 studies from our updated search for a total of 165 included studies. Six included studies were meta-analyses, 26 randomised controlled trials (RCTs), 13 other controlled studies, and 120 non-controlled studies. Five meta-analyses and 12 RCTs provided high-quality evidence for non-removable knee-high offloading devices being more effective than removable offloading devices and therapeutic footwear for healing plantar forefoot and midfoot ulcers. Total contact casts (TCCs) and non-removable knee-high walkers were shown to be equally effective. Moderate-quality evidence exists for removable knee-high and ankle-high offloading devices being equally effective in healing, but knee-high devices have a larger effect on reducing plantar pressure and ambulatory activity. Low-quality evidence exists for the use of felted foam and surgical offloading to promote healing of plantar forefoot and midfoot ulcers. Very limited evidence exists for the efficacy of any offloading intervention for healing plantar heel ulcers, non-plantar ulcers, and neuropathic ulcers with infection or ischemia.
Conclusion:
Strong evidence supports the use of non-removable knee-high offloading devices (either TCC or non-removable walker) as the first-choice offloading intervention for healing plantar neuropathic forefoot and midfoot ulcers. Removable offloading devices, either knee-high or ankle-high, are preferred as second choice over other offloading interventions. The evidence bases to support any other offloading intervention is still weak and more high-quality controlled studies are needed in these areas.
Keywords: diabetes mellitus, diabetic foot, foot ulcer, footwear, offloading, off-loading, offloading device, pressure, surgery, systematic review
1 |. INTRODUCTION
Diabetic foot ulcers (DFUs) are a leading global cause of amputation, hospitalisation, and disability.1–5 Around 26 million people worldwide annually have a DFU with another 130 million at risk with diabetic peripheral neuropathy.4,5
The most common pathway to a DFU is via excessive mechanical stress on an insensate foot.5–9 Mechanical stress is an accumulation of the effects of plantar pressure, shear stress, and ambulatory activity over time.5–9 If excessive, mechanical stress results in inflammation, DFU development, and prolonged DFU healing, which in turn increases the risk of infection, hospitalisation, and amputation.5–9 Reducing excessive mechanical stress using offloading interventions is considered the cornerstone of treatment for neuropathic DFU.1,5–10 Offloading interventions typically include offloading devices, footwear, surgical procedures, and other techniques such as felted foam.8,9,11
In 2016, we published a systematic review into the effectiveness of these offloading interventions to heal DFUs.11 Since then, a number of meta-analyses12–15 and well-designed controlled trials16–19 have been published that add to the evidence base. Thus, the aim of this systematic review is to update our previous systematic review investigating the effectiveness of offloading interventions to heal foot ulcers in people with diabetes.11 The findings will also be used to support the International Working Group on the Diabetic Foot (IWGDF) guideline on offloading interventions to heal foot ulcers in persons with diabetes.20
2 |. METHODS
This systematic review was performed in accordance with the preferred reporting item for systematic reviews and meta-analyses (PRISMA) guidelines21,22 and was prospectively registered in the PROSPERO database for systematic reviews (CRD42018105681). The population (P), interventions (I), controls (C), and outcomes (O) of interest were initially defined and pertinent clinical questions (PICOs) formulated by the authors. These definitions and clinical questions were subsequently reviewed and approved by the IWGDF Editorial Board and 10 external experts from diverse global geographic regions. All clinical questions can be found within this paper and all definitions can be found in accompanying IWGDF publications.20,23,24
2.1 |. Eligibility criteria
To be included, studies had to include an eligible population, intervention, outcome, and design.
2.1.1 |. Population
The population of interest for this review were people with a DFU, defined as any full thickness lesion below the malleoli associated with peripheral neuropathy and/or peripheral artery disease in people with diabetes.20,23,24 People at-risk of DFU were also eligible if they were specifically being used as a “surrogate DFU population” to test offloading interventions for potential offloading effectiveness in a future DFU population. Those at-risk were defined as people with diabetes and previous DFU, peripheral neuropathy, or peripheral arterial disease.20,23,24
2.1.2 |. Interventions
Offloading interventions were defined as any intervention undertaken with the intention of relieving mechanical stress from a specific region of the foot.20,23,24 They were grouped into four categories typically used in clinical practice as follows:
Offloading devices. Any offloading intervention that was a custom-made or prefabricated device, excluding footwear.20 Offloading devices were further subcategorised into non-removable or removable and knee-high or ankle-high devices.20
Footwear. Any offloading intervention that was shoe-gear, including insoles and socks.20 Footwear was further subcategorised into conventional and therapeutic footwear.20
Other offloading techniques. Any other non-surgical offloading intervention that was not an offloading device or footwear.20
Surgical offloading techniques. Any offloading intervention that was a surgical procedure or technique.20
2.1.3 |. Outcomes
Primary, surrogate, and secondary outcomes of interest were included in this review. In brief, the primary outcome was a healed DFU, typically defined by studies as complete epithelialization.20,23,24
Surrogate outcomes were changes in plantar pressure, ulcer area, ambulatory activity, and adherence.20,23,24 Plantar pressure was typically defined by studies as peak plantar pressure or peak pressure time integral.20,23,24 Ulcer area was typically defined as ulcer surface area.20,24 Ambulatory activity was typically defined as average number of daily steps.20,24 Adherence was typically defined as the proportion of total time or total steps during which the offloading intervention was used.20,24
Secondary outcomes included adverse events, patient-reported outcome measures (PROMs), and cost-effectiveness.20,24 Adverse events were typically defined as complications related to the intervention.20,24 PROMs were typically defined through validated patient self-reporting tools, including quality of life, satisfaction, or preference.20,24 Cost-effectiveness was typically defined as the degree to which the intervention was effective in relation to cost.20,24
2.1.4 |. Designs
Eligible study designs included systematic reviews and meta-analyses, randomised controlled trials (RCTs), nonrandomised controlled trials (NRCTs), cohort studies, case-control studies, within-subject repeated measures studies, interrupted time series, non-controlled prospective or retrospective studies, cross-sectional studies, and case series. Case studies, commentaries, and published conference abstracts were not eligible. Any systematic review that included the exact same papers as identified by our systematic search was excluded, unless they under-took a meta-analysis.
2.2 |. Search strategy
2.2.1 |. Validation set
A validation set of 30 publications was created,8,12,13,15–19,25–46 including key studies known to the authors published since our previous search (July 29, 2014).11 Using this set, the search strings used were validated; ie, each publication had to be identified before the search strings were used in this systematic review.
2.2.2 |. Search
The search was performed on August 13, 2018 and included studies in any language that were published since July 29, 2014. The following databases were searched: PubMed, EMBASE and the Cochrane Library Databases for Cochrane Reviews, Cochrane Protocols and Trials. We did not use CINAHL this time as it did not identify any additional relevant papers in our last review.11 For each search string, the population was added to each of the four offloading intervention categories and produced results for the four categories for each database. The search strings for each database are shown in Appendices 1 to 3.
2.2.3 |. Eligibility assessment
Two authors independently screened records by title and abstract for eligibility based on the four defined criteria: population, intervention, outcome, and design. Cohen’s kappa was calculated for agreement between authors. Any disagreements were then discussed between authors until consensus was reached. If this was not possible, a third author decided. All records deemed eligible were included for full text assessment.
Two authors then independently assessed all included full text records for inclusion based on the same four criteria. Any papers not in the English language were translated to English via Onlinedoctranslator.47 Any disagreements on inclusion were discussed until consensus was reached. If this was not possible, a third author decided. If an author was a co-author of the full text, another author replaced that author for assessment. All full text records remaining eligible were included in this review. We used the online application Rayyan to assist with these eligibility assessment processes.48
2.3 |. Qualitative assessments
All included studies were assessed for study design, methodological quality, level of evidence, and key data were extracted.
2.3.1 |. Study design assessment
Two authors jointly classified the study design of all included studies using the SIGN algorithm for classifying study design (http://www.sign.ac.uk/pdf/studydesign.pdf). Studies classified as being a meta-analysis or of controlled study design (RCT, controlled cohort, case-control studies) were assessed for methodological quality and had key data extracted. Studies classified as being a non-controlled design were narratively described if no controlled studies were identified that addressed the clinical question or if the non-controlled studies added relevant evidence.
2.3.2 |. Methodological quality assessment
Two authors independently assessed each included study deemed to be a meta-analysis or controlled study design for methodological quality (ie, risk of bias). For meta-analyses, this was performed using the 12-item SIGN methodology checklist for systematic reviews and meta-analyses tool (https://www.sign.ac.uk/checklists-and-notes.html). For controlled studies, this was performed using one of two Dutch Cochrane Centre quality assessment tools: a 10-item tool for RCTs or a 10-item tool for cohort studies (www.cochrane.nl). Additionally, for all controlled studies, the 21-item IWGDF quality assessment tool on reporting standards for diabetic foot studies was used.24 Any disagreements were discussed until consensus was reached. If this was not possible, a third author decided. If an author was a co-author of the included study, another author replaced that author for assessment.
2.3.3 |. Level of evidence assessment
For each controlled study, two authors jointly used the study design and methodological quality assessments to determine its level of evidence. Level 1 evidence referred to meta-analyses, systematic reviews, or RCTs. Level 2 evidence referred to NRCTs, cohort, case-control, or interrupted time series studies. Risk of bias was then scored using the total methodological quality assessment score obtained from the respective SIGN or Dutch Cochrane Centre tools as follows: ++ (very low risk of bias) for any meta-analyses scoring greater than or equal to 10/12, or any controlled study scoring greater than or equal to 8/10; + (low risk of bias) for any meta-analyses scoring a 7 to 9/12, or any controlled study scoring 6 to 7/10; and − (high risk of bias) for any meta-analyses scoring less than or equal to 6/12, or any controlled study scoring less than or equal to 5/10. Equal weighting was applied to each item in the SIGN or Dutch Cochrane Centre tools. All non-controlled studies were automatically deemed as Level 3 evidence and not assessed for risk of bias.
2.3.4 |. Data extraction assessment
Key data were extracted for each meta-analysis and controlled study and summarised in evidence tables. One author extracted all data, and a second author checked the accuracy of data entry. Data extracted included intervention category, outcomes reported, study design, setting, population, intervention and control characteristics, follow-up period, and key findings. The risk of bias and level of evidence scores were also entered into the evidence tables. All authors discussed the evidence tables until consensus was reached on accuracy.
2.4 |. Previously included studies
Our previous systematic review included some eligibility criteria not used in this updated review, including populations at risk of DFU, if offloading interventions were tested to prevent DFU, and outcomes of DFU incidence.11 Thus, all previously included studies were reassessed by one author and checked by another to ensure eligibility. Any studies deemed not eligible for this review were excluded.
All previously included studies that remained eligible had their methodological quality and data extraction item assessments from our previous review used for this updated review and entered into the evidence tables. Any additional items not included in the previous review were assessed for as per methods described above.
2.5 |. Evidence statements
Finally, for each clinical question, two or more authors jointly drafted a summary of the evidence. The summary of the evidence was primarily based on the strength of all available meta-analyses and controlled study evidence from the completed evidence tables for the clinical question concerned. Evidence from non-controlled studies was only used if it added relevant evidence.
Two authors then formulated a concluding evidence statement(s) to address each clinical question according to the GRADE system.49 However, if there was no controlled study or relevant non-controlled study evidence to address the question, then no evidence statement was formulated.
The authors rated the quality of the evidence (QoE) for each formulated evidence statement as “high,” “moderate,” or “low.”50,51 A high QoE rating was defined as “further research was unlikely to change our confidence in our evidence statement.”50,51 A moderate QoE rating was defined as “further research was likely to have an impact on our confidence in our evidence statement.”50,51 A low QoE rating was defined as “further research was very likely to have an impact on our confidence in our evidence statement.”50,51 Evidence statements supported by Level 1 evidence automatically started as a high QoE rating, but this could be reduced if studies had high risk of bias, inconsistent results across studies, or publication bias was present.50,51 Conversely, evidence statements supported by Level 2 evidence started as a low QoE rating, but this could be increased if studies had a large effect size or clear evidence of a dose-response relationship.50,51 All members of the working group discussed these evidence statements and QoE ratings until consensus was reached.
3 |. RESULTS
Figure 1 displays the PRISMA flowchart. Our updated search since July 29, 2014 identified a total of 3715 records. After screening, 152 records remained for full-text assessment. Screening agreement between authors was low to very high (Cohen’s kappa: 0.16 to 0.80). After full-text assessment, 41 studies published since July 29, 2014 were included. Additionally, after full text re-assessment of the 176 included studies from our previous review, 124 studies published before July 29, 2014 remained included. Thus, a total of 165 studies were included for this review, including six meta-analyses, 26 RCTs, 13 other controlled studies, and 120 non-controlled studies.
FIGURE 1.
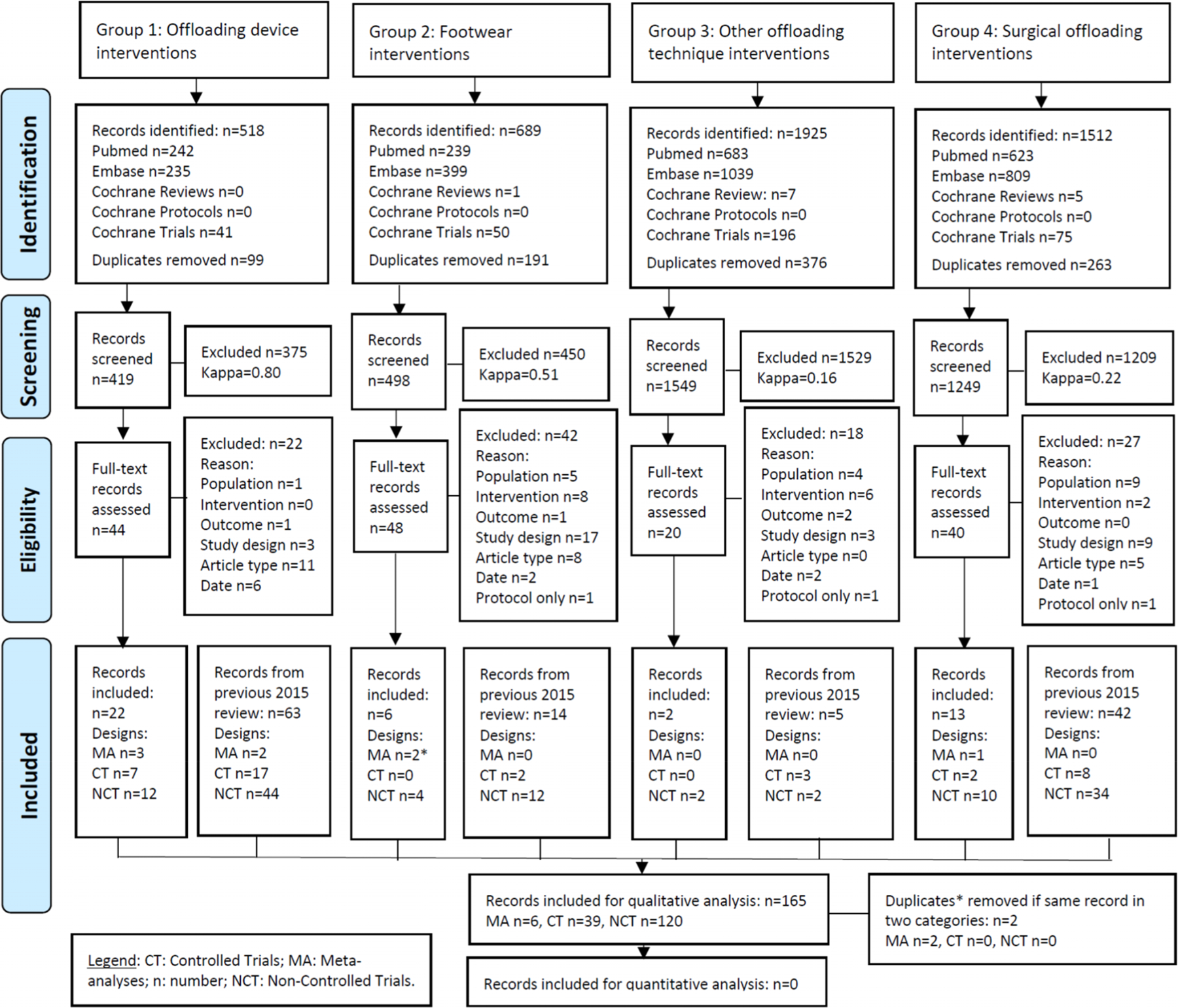
Preferred reporting items for systematic reviews and meta-analyses flow diagram
Tables 1–3 display the risk of bias tables for all included meta-analyses, RCTs, and other controlled studies by each offloading intervention category, respectively. Appendices 4 to 6 display the evidence tables for all included meta-analyses, RCTs, and other controlled studies by each offloading intervention category, respectively. Summaries of the evidence, evidence statements and quality of evidence for each clinical question addressing the primary outcome of DFU healing and the surrogate outcome of plantar pressure can be found below. Summaries of the evidence, evidence statements and quality of evidence for each clinical question addressing all other surrogate or secondary outcomes can be found in Appendices 7 and 8. Table 4 summarises all evidence statements with accompanying quality of evidence rating for each predefined clinical question.
TABLE 1.
Risk of bias tables for all meta-analyses
| Reference (in reverse chronological order) | Clearly Defined Research Question | Comprehensive Literature Search | >1 Person Selected Studies | >1 Person Extracted Data | Status of Publication Not Used as Inclusion Criteria | Excluded Studies Listed | Included Studies Characteristics Provided | Included Studies Scientific Quality Assessed + Reported | Scientific Quality Assessed Appropriately | Appropriate Methods Used to Combine Study Results | Publication Bias Assessed | Conflicts Declared | Total Score | Total Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Offloading devices | ||||||||||||||
| Health Quality Ontario 201712 | + | + | − | ? | + | − | + | + | + | + | + | − | 8/12 | + |
| Elraiyah et al 201613 | + | + | + | + | − | − | + | + | + | + | ? | − | 8/12 | + |
| Martins de Oliveira and Moore 201515 | + | + | ? | ? | − | + | − | + | + | + | + | + | 8/12 | + |
| Lewis and Lipp 201352 | + | + | + | + | + | + | + | + | + | + | − | − | 10/12 | ++ |
| Morona et al 201353 | + | + | ? | + | + | − | + | + | + | + | − | + | 9/12 | + |
| Surgical offloading techniques | ||||||||||||||
| Dallimore and Kaminski 201514 | + | + | + | + | + | + | + | + | + | + | ? | + | 11/12 | ++ |
Note. +, yes criterion is met; −, no criterion is not met; ?, not reported or not clear. Total risk of bias: ++, very low risk of bias; +, low risk of bias; −, high risk of bias.
TABLE 3.
Risk of bias tables for all other controlled studies
| Reference (in reverse chronological order) | Study Groups Clearly Defined | Selection Bias Avoided/Excluded | Intervention Clearly Defined | Outcome Clearly Defined | Outcome Assessed Blind for Exposure | Withdrawal/Drop-out Rate Acceptable (<20%) | Selective Lost-to-Follow-up Excluded | Major Confounders/Prognostic Factors Identified and Controlled | Selective Reporting of Outcomes Ruled Out | Free from Commercial Influence | Total Score | Total Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Offloading devices | ||||||||||||
| Strakhova et al 201473 | + | + | + | ? | − | ? | ? | ? | ? | + | 4/10 | − |
| Agas et al 200674 | + | ? | + | + | − | ? | ? | ? | ? | − | 3/10 | − |
| Udovichenko et al 200675 | + | − | + | + | − | + | − | − | + | ? | 5/10 | − |
| Ha Van et al 200376 | + | − | + | + | − | + | + | − | + | − | 6/10 | + |
| Birke et al 200277* | + | − | + | ? | − | + | ? | + | + | ? | 5/10 | − |
| Black et al 199078 | ? | ? | + | − | − | + | + | ? | ? | ? | 3/10 | − |
| Footwear | ||||||||||||
| Viswanathan et al 200479 | ? | − | + | − | − | ? | ? | − | + | ? | 2/10 | − |
| Surgical offloading techniques | ||||||||||||
| Kalantar Motamedi et al 201780 | − | − | + | + | − | ? | − | − | − | + | 3/10 | − |
| Vanlerberghe et al 201481 | − | ? | + | − | − | + | + | ? | ? | + | 4/10 | − |
| Armstrong et al 201282 | + | ? | + | + | − | + | + | + | ? | ? | 6/10 | + |
| Armstrong et al 200583 | + | − | + | + | ? | ? | ? | − | ? | ? | 3/10 | − |
| Armstrong et al 200384 | + | − | − | + | ? | − | ? | − | ? | ? | 2/10 | − |
| Lin et al 200085 | + | − | + | + | ? | ? | − | − | ? | ? | 3/10 | − |
Note. +, yes criterion is met; −, no criterion is not met; ?, not reported or not clear. Total risk of bias: ++ very low risk of bias; +, low risk of bias; −, high risk of bias.
: This paper was included in both Offloading devices and Other offloading techniques categories.
TABLE 4.
Evidence statements from systematic review for offloading interventions to heal neuropathic plantar forefoot or midfoot ulcers in patients with diabetes, unless otherwise stateda
| Outcome | Evidence Statement | Qualityb | References |
|---|---|---|---|
| PRIMARY: Healing | |||
| Nonremovable offloading device | Nonremovable knee-high offloading devices are more effective than removable offloading devices to heal the DFU. | High | Health Quality Ontario 2017,12 Elraiyah et al 2016,13 Martins de Oliveira and Moore 2015,15 Morona et al 2013,53 and Lewis and Lipp 201352 |
| TCCs and non-removable knee-high walkers are equally effective to heal the DFU. | Moderate | Health Quality Ontario 2017,12 Morona et al 2013,53 and Miyan et al 201436 | |
| Removable offloading device | Removable knee-high offloading devices and removable ankle-high offloading devices are equally effective to heal the DFU. | Moderate | Health Quality Ontario 201712 and Bus et al 201816 |
| Footwear | Therapeutic footwear is less effective than non-removable knee-high offloading devices to heal the DFU. | Moderate | Health Quality Ontario 2017,12 Elraiyah et al 2016,13 Morona et al 2013,53 and Miyan et al 201436 |
| Other offloading technique | Felted foam (with an aperture cut to the DFU location) attached to either the foot or the insole in a removable ankle-high offloading device seems to be more effective to heal the DFU than only wearing a removable ankle-high offloading device. | Low | Zimny et al 200368 and Birke et al 200277 |
| Surgical offloading technique | Achilles tendon lengthening in addition to a non-removable offloading device seems equally effective to heal the DFU as a non-removable offloading device alone | Low | Dallimore and Kaminski 201514 |
| Metatarsal head resection(s) in combination with a removable offloading device seems more effective to heal a neuropathic plantar metatarsal head DFU than using a removable offloading device alonea | Low | Kalantar Motamedi et al 2017,80 Armstrong et al 2012,82 Armstrong et al 2005,61 and Piaggesi et al 199872 | |
| Medial column arthrodesis in combination with a non-removable offloading device is not superior in healing a neuropathic plantar midfoot DFU associated with a Charcot deformity than using a non-removable offloading device alonea | Low | Wang et al 201569 | |
| First metatarsal-phalangeal joint arthroplasty in combination with non-removable offloading device may lead to shorter time-to-healing a neuropathic plantar hallux DFU than using a non-removable offloading device alonea | Low | Armstrong et al 200384 and Lin et al 200085 | |
| Osteotomy seems more effective to heal a metatarsal head DFU than conservative treatment (with or without offloading) alone | Low | Vanlerberghe et al 201481 | |
| Digital flexor tenotomy seems effective to heal a neuropathic plantar lesser digit apical DFU, but evidence from controlled studies is needed to confirm thisa | Low | Engels et al 2016,86 Tamir et al 2014,87 Rasmussen et al 2013,88 van Netten et al 2013,89 Kearney et al 2010,90 Schepers et al 2010,91 Tamir et al 2008,92 and Laborde et al 200793 | |
| Other DFU types | Nonremovable knee-high offloading devices seem effective to heal a neuropathic plantar forefoot DFU complicated by either mild infection or mild ischaemiaa | Low | Ha Van et al 201576 and Nabuurs-Franssen et al 200594 |
| Low | Ganguly et al 200857 | ||
| TCCs seem more effective than therapeutic footwear to heal a neuropathic plantar heel DFUa | |||
| SURROGATE | |||
| Plantar pressure | TCCs and removable knee-high offloading devices are equally effective in reducing peak pressure at the DFU location and forefoot and rearfoot areas. | Moderate | Gutekunst et al 2011,55 Gotz et al 2017,95 Armstrong et al 1999,96 Fleischli et al 1997,97 and Lavery et al 199698 |
| Removable knee-high offloading devices are more effective in reducing peak pressure at the DFU location and forefoot area than removable ankle-high offloading devices | Moderate | Bus et al 2018,16 Crews et al 2018,27 Westra et al 2018,46 Gotz et al 2017,95 Crews et al 2012,99 Nagel and Rosenbaum 2009,100 and Fleischli et al 199797 | |
| Removable ankle-high offloading devices seem more effective than conventional or standard therapeutic footwear in reducing plantar pressure at the DFU location and forefoot areas | Low | Crews et al 2018,27 Gotz et al 2017,95 Bus et al 2017,101 Crews et al 2012,99 Raspovic et al 2012,102 Bus et al 2009103 Bus et al 2009,104 Nagel and Rosenbaum 2009,100 and Fleischli et al 199797 | |
| Therapeutic footwear seems more effective than conventional footwear in reducing peak pressure at forefoot areas | Low | Viswanathan et al 2004,79 Nouman et al 2017,105 Lin et al 2013,106 Kavros et al 2011,107 Guldemond et al 2007,108 Praet et al 2003,109 Raspovic et al 2000,110 Lavery et al 1997,111 Lavery et al 1997,112 Lavery et al 1996,98 and Kato et al 1996113 | |
| Botulinum toxin injections are not superior to saline placebo injections for reducing plantar pressure at forefoot areas | Moderate | Hastings et al 201266 | |
| Felted foam applied to the forefoot with a cut out to the ulcer area seems more effective at reducing plantar pressure over 1 week compared with no felted foam | Low | Pabon-Carrasco et al 2016114 and Raspovic et al 201637 | |
| Achilles tendon lengthening in addition to a TCC seems more effective at reducing peak pressures at the forefoot in the short term than a TCC alone, but not in the long term, and at the expense of increases in rearfoot peak pressure. | Low | Maluf et al 200470 | |
| Ulcer area | TCCs and non-removable knee-high walkers are equally effective to reduce DFU area | Moderate | Piaggesi et al 201619 |
| Nonremovable knee-high offloading devices and removable knee-high offloading devices seem equally effective to reduce DFU area | Low | Najafi et al 2017,18 Piaggesi et al 2016,19 and Caravaggi et al 200759 | |
| Nonremovable knee-high offloading devices and removable ankle-high offloading devices seem equally effective to reduce DFU area | Low | Chakraborty et al 2015,54 Strakhova et al 2014,73 Faglia et al 2010,56 Van de Weg et al 2008,58 Agas et al 2006,74 and Udovichenko et al 200675 | |
| Removable knee-high offloading devices and removable ankle-high offloading devices are equally effective to reduce DFU area | Moderate | Bus et al 201816 and Johnson et al 201833 | |
| Felted foam attached to the foot (changed every 3 days) and worn in a removable ankle-high offloading device seems more effective to reduce DFU area than a removable ankle-high offloading device only | Low | Zimny et al 200368 | |
| Felted foam attached to the foot and worn in a removable ankle-high offloading device seems equally effective to reduce DFU area as attaching the felted foam to the insole of the removable ankle-high offloading device | Low | Nube et al 200667 | |
| Ambulatory activity | Nonremovable knee-high offloading devices and removable knee-high offloading devices seem to be associated with similar reductions in ambulatory activity | Low | Najafi et al 2017,18 Lavery et al 2015,34 and Armstrong et al 200163 |
| Nonremovable knee-high offloading devices are associated with a greater reduction in ambulatory activity than removable ankle-high offloading devices | Moderate | Lavery et al 201534 and Armstrong et al 200163 | |
| Removable knee-high offloading devices seem to be associated with greater reductions in ambulatory activity than removable ankle-high offloading devices | Low | Bus et al 2018,16 Lavery et al 2015,34 and Armstrong et al 200163 | |
| Adherence | Nonremovable knee-high offloading devices are associated with higher adherence than removable offloading devices. | Low | Lavery et al 201534 and Ha Van et al 200376 |
| Removable knee-high offloading devices and removable ankle-high devices seem to be associated with similar levels of adherence. | Low | Bus et al 201816 and Johnson et al 201833 | |
| SECONDARY | |||
| Adverse events | Nonremovable offloading devices and removable offloading devices seem to be associated with similar proportions of adverse events. | Low | Health Quality Ontario 2017,12 Lewis and Lipp 2013,52 Najafi et al 2017,18 Piaggesi et al 2016,19 Lavery et al 2015,34 Faglia et al 2010,56 Van de Weg et al 2008,58 Caravaggi et al 2007,59 Piaggesi et al 2007,60 Armstrong et al 2005,61 Katz et al 2005,62 and Armstrong et al 200163 |
| TCCs and non-removable knee-high walkers seem to be associated with similar proportions of adverse events | Low | Health Quality Ontario 2017,12 Piaggesi et al 2016,19 Piaggesi et al 2007,60 and Katz et al 200562 | |
| Removable knee-high and removable ankle-high offloading devices seem to be associated with similar proportions of adverse events. | Low | Health Quality Ontario 2017,12 Bus et al 2018,16 Lavery et al 2015,34 and Armstrong et al 200163 | |
| Nonremovable knee-high offloading devices and therapeutic footwear seem to be associated with similar proportions of adverse events. | Low | Health Quality Ontario 2017,12 Miyan et al 2014,36 Ganguly et al 2008,57 Caravaggi et al 2000,64 and Mueller et al 198965 | |
| Felted foam (with an aperture cut to the DFU location) attached to either the foot or the insole in a removable ankle-high offloading device (and changed every few days) seems to be associated with similar proportions of adverse events as only wearing a removable ankle-high offloading device | Low | Nube et al 200667 and Zimny et al 200368 | |
| Custom-made light-weight fibreglass heel cast in addition to usual care seems to be associated with similar proportions of adverse events as using usual care alone in patients with neuropathic rearfoot DFUa | Low | Jeffcoate et al 201717 | |
| Botulinum toxin injections and saline placebo injections seem to be associated with similar proportions of adverse events | Low | Hastings et al 201266 | |
| Achilles tendon lengthening in addition to a TCC seems to be associated with more adverse events (particularly new heel ulcers) than using a TCCs alone. | Low | Mueller et al 200371 | |
| Metatarsal head resection(s) in addition to non-surgical offloading interventions seems to be associated with fewer adverse events (particularly new infections) than non-surgical offloading alone in patients with neuropathic plantar metatarsal DFUa | Low | Kalantar Motamedi et al 2017,80 Armstrong et al 2012,82 Armstrong et al 2005,61 and Piaggesi et al 199872 | |
| Patient-reported outcomes | Nonremovable knee-high offloading devices, removable knee-high offloading devices, removable ankle-high offloading devices and therapeutic footwear seem to be associated with similar patient-reported outcomes. | Low | Piaggesi et al 2016,19 Lavery et al 2015,34 Piaggesi et al 2007,60 and Caravaggi et al 200064 |
| Custom-made light-weight fibreglass heel cast in addition to usual care seems to be associated with similar patient-reported outcomes as using usual care alone in patients with a neuropathic rearfoot DFUa | Low | Jeffcoate et al 201717 | |
| Metatarsal head resection(s) in addition to non-surgical offloading interventions seems to be associated with better patient-reported outcomes than non-surgical offloading alone in patients with neuropathic plantar metatarsal DFUa | Low | Piaggesi et al 199872 | |
| Cost-effectiveness | Nonremovable knee-high offloading devices seems to be more cost-effective than removable offloading devices in healing the DFU | Low | Health Quality Ontario 2017,12 Piaggesi et al 2016,19 and Faglia et al 201056 |
| Nonremovable knee-high walkers are more cost-effective than TCCs in healing the DFU | Moderate | Health Quality Ontario 2017,12 Piaggesi et al 201619 Piaggesi et al 2007,60 and Katz et al 200562 | |
| Removable knee-high walkers seem to be more cost-effective than therapeutic footwear in healing the DFU | Low | Health Quality Ontario 201712 | |
| Custom-made light-weight fibreglass heel cast in addition to usual care seems to be equally cost-effective as using usual care alone in patients with a neuropathic rearfoot DFUa | Low | Jeffcoate et al 201717 |
Abbreviations: DFU, diabetes-related foot ulcer; TCC, total contact cast.
Ulcer type that is not specifically a neuropathic plantar forefoot or midfoot ulcers in patients with diabetes.
Quality: Quality of the evidence.
3.1 |. Primary outcome: DFU healing
3.1.1 |. Non-removable offloading devices
PICO a
In people with a plantar DFU, are non-removable offloading devices compared with removable offloading devices effective to heal the DFU?
Summary of the evidence.
We identified five meta-analyses (one with very low risk of bias52 and the other four with low risk of bias12,13,15,53) and one additional controlled study (NRCT with high risk of bias73) not included in those meta-analyses. All studies primarily reported on patients with a neuropathic plantar forefoot or midfoot DFU. As each of the five meta-analyses included a different combination of studies out of a total 14 controlled studies (12 RCTs and two other controlled studies, with seven we assessed as having [very] low risk19,55,56,58,60,61,76 and seven with high risk of bias18,34,59,63–65,74), we will discuss each meta-analysis separately. We did not separately discuss the NRCT as it did not add to the evidence obtained from the meta-analyses and does not change our evidence statement.73
The most recent meta-analysis by Health Quality Ontario reported two analyses for healing rates.12 First, they included six RCTs (three [very] low risk,19,55,56 three high risk of bias34,59,63) with a cumulative total of 274 patients and found a significant risk difference (RD) to achieve healing at 3 months of 0.17 (95% confidence interval [CI], 0.00–0.33; P = .05) in favour of non-removable offloading using the total contact cast (TCC) compared with a removable knee-high walker.12 Second, they included three RCTs (two low risk,19,61 one high risk of bias18) with a cumulative total of 141 patients, and found a significant risk difference to achieve healing at 3 months of 0.21 (95% CI, 0.01–0.40; P = .04) in favour of using a non-removable knee-high walker compared with a removable knee-high walker.12
The second meta-analysis by Elraiyah et al included four RCTs (three at low risk,56,58,60 one at high risk of bias63) with a cumulative total of 162 patients and reported healing rate and time-to-healing.13 For healing rate, they included three of those RCTs56,58,63 with a cumulative total of 122 patients and reported a non-significant relative risk (RR) to achieve healing of 1.15 (95% CI 0.92–0.1.45; P = 0.217) in favour of non-removable offloading (TCC) compared with removable offloading devices (knee-high walker or custom-made temporary footwear).13 For time-to-healing they included all four RCTs and reported a significant mean difference in healing time of −12.36 days (95% CI, −22.63 to −2.09; P = .018) in favour of non-removable compared with removable offloading devices using the same definitions.13
The third meta-analysis by Martins de Oliveira and Moore included seven RCTs (four at low risk,56,58,60,61 three at high risk of bias63–65) with a cumulative total of 350 patients and reported healing rate and time-to-healing.15 For healing rate, they reported a significant odds ratio (OR) to achieve healing of 0.31 (95% CI, 0.19–0.52; P < .001) in favour of non-removable offloading (TCC or non-removable knee-high walker) compared with removable offloading (knee-high walker, forefoot offloading shoe, felted foam, or therapeutic footwear).15 For time-to-healing, they included six of those RCTs56,58,60,61,63,65 with a cumulative total of 300 patients and reported a significant mean difference in healing time of −8.14 days (95% CI, −9.51 to −6.77; P < .001) also in favour of non-removable offloading compared with removable offloading device using the same definitions.15
The fourth meta-analysis by Morona et al included eight RCTs55,56,58,59,61,63–65 and two other controlled studies74,76 (five at [very] low risk,55,56,58,61,76 five at high risk of bias59,63–65,74) with a cumulative total of 524 patients and reported healing rates.53 They found a significant RR to achieve healing of 1.43 (95% CI, 1.11–1.84; P = 0.001) in favour of non-removable offloading (TCC or non-removable walkers) compared with removable offloading (removable walker or therapeutic footwear).53 When comparing non-removable offloading (TCC or non-removable walker) with removable offloading (walker only) in five RCTs (three at [very] low risk,55,56,61 two at high risk of bias59,63), with a cumulative total of 220 patients, they found a non-significant RR to achieve healing of 1.23 again in favour of non-removable offloading (95% CI, 0.96–1.58; P = .085).53
The oldest meta-analysis with very low risk of bias by Lewis and Lipp included five RCTs (three at low risk,56,60,61 two at high risk of bias59,63) with a cumulative total of 230 patients and reported healing rate.52 They found a significant RR to achieve healing of 1.17 (95% CI, 1.01–1.36; P = .04) in favour of non-removable offloading (TCC or non-removable walker) compared with removable offloading (walker or therapeutic footwear).52
Evidence statement.
Nonremovable knee-high offloading devices are more effective than removable offloading devices to heal a neuropathic plantar forefoot or midfoot DFU.
Quality of evidence (QoE).
High: Based on five meta-analyses (all low or very low risk of bias)—that included 14 controlled studies (7 at [very] low risk of bias, 7 at high risk of bias)—all with consistent results.
References.
Health Quality Ontario 2017,12 Elraiyah et al 2016,13 Martins de Oliveira and Moore 2015,15 Morona et al 2013,53 and Lewis and Lipp 2013.52
PICO b
In people with a plantar DFU, are TCCs compared with other non-removable knee-high offloading devices effective to heal the DFU?
Summary of the evidence.
We identified two meta-analyses12,53 and four RCTs.19,36,60,62 All studies primarily reported on patients with a neuropathic plantar forefoot or midfoot DFU. As the more recent meta-analysis12 included three of those four RCTs,19,60,62 and two of those RCTs60,62 were included in the older meta-analysis,53 we only report the more recent meta-analysis12 and the RCT36 not included in either meta-analysis.
The meta-analysis by Health Quality Ontario, with low risk of bias, included three RCTs (all low risk of bias19,60,62) with a cumulative total of 126 patients.12 They found a non-significant risk difference to achieve healing between TCCs and non-removable knee-high walkers of 0.02 (95% CI, −0.11 to 0.14; P = .82).12 The additional RCT with high risk of bias allocated 70 patients into three groups: TCC, non-removable walker, and modified footwear.36 They found no difference between TCC and non-removable walker for healing rates (95.0% vs 94.7%; P = .99) and time-to-healing (45.0 vs 46.0 days; P = .767)36.
Evidence statement.
TCCs and non-removable knee-high walkers are equally effective to heal a neuropathic plantar forefoot or midfoot DFU.
QoE.
Moderate: Based on two meta-analysis with low risk of bias—that included three RCTs with low risk of bias—and another RCT with high risk of bias, all with consistent results. However, as none of the RCTs was powered for equivalence, we downgraded to moderate.
References.
Health Quality Ontario 2017,12; Morona et al 2013,53 and Miyan et al 2014.36
3.1.2 |. Removable offloading devices
PICO
In people with a plantar DFU, are removable knee-high offloading devices compared with other removable offloading devices effective to heal the DFU?
Summary of the evidence.
We identified one meta-analysis12 and three RCTs.16,34,63 All studies primarily reported on patients with a neuropathic plantar forefoot or midfoot DFU.
The meta-analysis by Health Quality Ontario, with low risk of bias, included two RCTs with high risk of bias34,63 with a cumulative total of 100 patients.12 It found a non-significant risk difference to achieve healing between removable knee-high walker and removable ankle-high devices (post-operative healing sandal or half-shoe) of −0.13 (95% CI, −0.31 to 0.06; P = .19).12
The RCT not included in the meta-analysis, with very low risk of bias, randomised 60 patients into a removable bivalved TCC, a removable cast shoe, and a removable forefoot offloading shoe.16 The authors found no significant differences between the three groups for healing rate at 12 weeks (58% vs 60% vs 70%, respectively; P = .703) or 20 weeks (63% vs 83% vs 80%, respectively; P = .305). However, participants with the bivalved TCC had more deep ulcers (University of Texas Grade 2A) at baseline (50% vs 30% vs 15%, respectively), which was significantly different compared with the forefoot offloading shoe (P = .043),16 and had more dropouts at 12 weeks (35% vs 0% vs 15%, respectively), which was significantly different compared with the cast shoe (P = .011).
Evidence statement.
Removable knee-high offloading devices and removable ankle-high offloading devices are equally effective to heal a neuropathic plantar forefoot or midfoot DFU.
QoE.
Moderate: Based on one meta-analysis with low risk of bias—that included two RCTs with high risk of bias—and another RCT with very low risk of bias, all with consistent results. However, as no study was powered for equivalence, we downgraded to moderate.
References.
3.1.3 |. Footwear
PICO
In people with a plantar DFU, are conventional or standard therapeutic footwear compared with other (non-surgical) offloading interventions effective to heal the DFU?
Summary of the evidence.
We identified three meta-analyses with low risk of bias12,13,53 and one RCT with high risk of bias36 not included in those meta-analyses. All meta-analyses compared “therapeutic footwear” with a non-removable offloading device (a TCC or non-removable walkers). All studies primarily reported on patients with a neuropathic plantar forefoot or midfoot DFU. However, studies defined “therapeutic footwear” as being either custom-made or customised footwear with or without insoles and/or ankle-high removable offloading devices (forefoot offloading shoes, post-operative healing shoes). Whereas we define therapeutic footwear as only being custom-made or customised footwear with or without insoles. Thus, we only report the meta-analyses where the majority of included RCTs defined therapeutic footwear according to our definition. We identified no controlled studies comparing conventional or therapeutic footwear with removable offloading devices.
The most recent meta-analysis by Health Quality Ontario included five RCTs (four at high risk,34,63–65 one at low risk of bias58) with a cumulative total of 229 patients.12 They found a significant risk difference to achieve healing of 0.25 (95% CI, 0.04–0.46; P = .02) in favour of non-removable offloading (TCCs) compared with therapeutic footwear.12 The second meta-analysis by Elraiyah et al included two RCTs (both at high risk of bias57,65) with a cumulative total of 98 patients13 and found a non-significant RR to achieve healing of 1.76 (95% CI, 0.77–4.02, P = .184) in favour of non-removable offloading (TCC) compared with “conventional dressings” (dressings, plus, extra-depth footwear with plastazote insole65 or custom-made footwear57).13 The third meta-analysis by Morona et al included six controlled studies (three RCTs at high risk of bias,63–65 one RCT at low risk,58 one cohort at low risk,76 one cohort at high risk of bias74) with a cumulative total of 318 patients.53 They found a significant RR to achieve healing of 1.68 (95% CI, 1.09–2.58, P = .004) in favour of non-removable offloading devices (either TCC or walkers rendered non-removable) compared with therapeutic footwear.53
The additional RCT with high risk of bias randomised 70 patients into three groups: TCC, non-removable walker, or modified footwear36 and found no difference for healing rates (95.0% vs 94.7% vs 95.7%; P = .99) and time-to-healing (45.0 vs 46.0 vs 34.0 days; P = .767) between interventions.36
Evidence statement.
Therapeutic footwear is less effective than non-removable knee-high offloading devices to heal a neuropathic plantar forefoot or midfoot DFU.
QoE.
Moderate: Based on three meta-analyses all with low risk of bias—that included nine controlled studies (seven at high risk, two at low risk of bias)—all with consistent results, except for the smallest meta-analysis which was non-significant but potentially underpowered. One additional RCT with high risk of bias also showed no differences. Thus, with some minor inconsistencies, we downgraded to moderate.
References.
Health Quality Ontario 2017,12 Elraiyah et al 2016,13 Morona et al 2013,53 and Miyan et al 2014.36
3.1.4 |. Other offloading techniques
PICO
In people with a plantar DFU, are other (non-surgical) offloading techniques that are not device- or footwear-related, effective to heal a DFU?
Summary of the evidence.
We identified two controlled studies (one RCT at high risk of bias,68 one cohort study at high risk of bias77) with both reporting on the use of felted foam. No controlled studies were identified that reported on bed rest, crutches, walking sticks/canes, wheelchairs, offloading dressings, callus debridement, or foot-related exercises to heal DFUs.
The RCT with high risk of bias randomised 54 patients into two groups: one received felted foam with an aperture cut to the exact location of the DFU attached to the foot (changed every third day) and worn in an ankle-high post-operative shoe, and the other an ankle-high pressure relief half shoe.68 They found a significantly shorter time-to-healing in the felted foam group (75 vs 85 days; P = .02) but did not report healing rates.68 The cohort study with high risk of bias retrospectively investigated 120 patients in four groups: TCC, non-removable walking splint, felt pad with cut-out to ulcer attached to the forefoot worn in a wedged-soled ankle-high post-operative shoe, and felt pad with cut-out to ulcer attached to the wedged-soled post-operative shoe.77 They reported similar ulcer healing rates after 12 weeks (92% vs 83% vs 93% vs 81%, respectively; P > .05) and time-to-healing (47.4 vs 50.5 vs 36.1 vs 41.4 days; P value not reported).77 Also, after adjusting for ulcer depth and width, they found time-to-healing was not significantly different between groups (31.7 vs 38.2, 20.9, and 32.7 days; P > .05).77
Evidence statement.
Felted foam (with an aperture cut to the DFU location) attached to either the foot or the insole in a removable ankle-high offloading device seems to be more effective to heal the DFU than only wearing a removable ankle-high offloading device.
QoE.
Low: Based on one RCT with high risk of bias and small effect size, and one retrospective cohort study with high risk of bias, we downgraded to low.
References.
3.1.5 |. Surgical offloading techniques
PICO
In people with a plantar DFU, are surgical offloading techniques compared with non-surgical offloading interventions effective to heal the DFU?
The evidence for this category will be discussed according to the specific surgical intervention.
Achilles tendon lengthening
Summary of the evidence.
We identified one meta-analysis with very low risk of bias14 and four additional non-controlled studies.115–118 The meta-analysis by Dallimore and Kaminski included two RCTs (one at low risk of bias on Achilles tendon lengthening71 and one at high risk of bias on Gastrocnemius recession as identified and quality assessed by the meta-analysis)119) with a cumulative total of 92 patients.14 They compared surgical offloading interventions (Achilles tendon lengthening or Gastrocnemius recession in combination with TCCs) with non-removable offloading devices (TCC only) and found a non-significant difference in risk ratio to achieve healing of 1.06 (95% CI, 0.94–1.20; P = .34) and non-significant mean difference in time-to-healing of 8.22 days (95% CI, −18.99 to 34.43 days; P = .55) between interventions.14 Four non-controlled retrospective studies investigated Achilles tendon lengthening, after unsuccessful healing with an offloading device (TCC or removable walker), in patients with reduced ankle dorsiflexion range of motion.115–118 They found 91% to 93% of plantar forefoot ulcers healed with Achilles tendon lengthening in a mean of 6 to 12 weeks.115–118
Evidence statement.
Achilles tendon lengthening in addition to a non-removable offloading device seems equally effective to heal a neuropathic plantar forefoot or midfoot DFU as a non-removable offloading device alone.
QoE.
Low: Based on one meta-analysis with very low risk of bias—that included two RCTs (one at low risk, one at high risk of bias)—all showing non-significant differences. However, as the meta-analysis may be underpowered to detect a statistical difference and none of the RCTs was powered for equivalence, we downgraded to low.
References.
Dallimore and Kaminski 2015.14
Metatarsal head resection
Summary of the evidence.
We identified four controlled studies (one RCT with low risk of bias,72 one cohort with low risk of bias,82 and two other cohort studies with high risk of bias80,83).
The RCT with low risk of bias randomised 41 patients with plantar forefoot ulcers to metatarsal head resection (a combination of surgical techniques [excision, debridement, removal of bone segments underlying the lesion and surgical closure] in combination with conservative offloading [therapeutic footwear with insoles]) or conservative offloading alone (therapeutic footwear with insoles).72 They showed significantly higher healing rates (95% vs 79%; P < .05) and shorter time-to-healing (47 vs 130 days; P < .05) in the surgical offloading group.72
The cohort study with low risk of bias retrospectively evaluated 92 patients with metatarsal head ulcers and found those treated with metatarsal head resections in combination with conservative offloading (removable walker or healing sandal) had significantly faster time-to-healing than those treated with conservative offloading alone (removable walker or healing sandal) (60.1 vs 84.2 days; P = .003).82 A cohort study with high risk of bias retrospectively evaluated 40 participants with plantar metatarsal head ulcers and found those treated with metatarsal head resection had significantly improved healing rates (100% vs 60%; P = .001) and time-to-healing (37 vs 384 days; P < .001) compared with those treated with conservative offloading (“non-weight-bearing, and, sometimes, specialized footwear”).80 The final cohort study with high risk of bias retrospectively evaluated 50 patients with plantar fifth metatarsal head ulcers and found that fifth metatarsal head resection in combination with conservative offloading (removable walker) had significantly better time-to-healing than conservative offloading alone (removable walker) (5.8 vs 8.7 weeks; P = .02).83
Evidence statement.
Metatarsal head resection(s) in combination with a removable offloading device seems more effective to heal a neuropathic plantar metatarsal head DFU than using a removable offloading device alone.
QoE.
Low: Based primarily on three cohort studies (two with high risk and one low risk of bias) and one RCT with low risk, all with consistent results.
References.
Kalantar Motamedi et al 2017,80 Armstrong et al 2012,82 Armstrong et al 2005,83 and Piaggesi et al 1998.72
Joint arthrodesis
Summary of the evidence.
We identified one RCT with high risk of bias randomising 21 patients with midfoot plantar ulcers associated with Charcot deformity to extended medial column arthrodesis in combination with TCC or to TCC alone and found similar time-to-healing (24 vs 26 days; P > .05).69
Evidence statement.
Medial column arthrodesis in combination with a non-removable offloading device is not superior in healing a neuropathic plantar midfoot DFU associated with a Charcot deformity than using a non-removable offloading device alone.
QoE.
Low: Based on one small RCT with high risk of bias and not powered for equivalence, we downgraded to low.
References.
Wang et al 2015.69
Joint arthroplasty
Summary of the evidence.
We identified two retrospective cohort studies with high risk of bias.84,85 The first retrospectively evaluated 41 patients and found a significant improvement in time-to-healing in the surgical group (first metatarsal phalangeal joint arthroplasty in combination with non-removable walker) compared with non-removable walker alone (24 vs 67 days; P = .0001).84 The second retrospectively evaluated 29 patients and found no difference in healing rate (100% vs 100%), but quicker time-to-healing (23 vs 47 days; P value not reported) in the surgical group (arthroplasty of the first proximal phalanx combined with TCC) compared with TCC alone, but did not report on statistical signficance.85
Evidence statement.
First metatarsal-phalangeal joint arthroplasty in combination with a non-removable offloading device may lead to shorter time-to-healing a neuropathic plantar hallux DFU than using a non-removable offloading device alone.
QoE.
Low: Based on two retrospective cohort studies with high risk of bias and inconsistent results.
References.
Osteotomy
Summary of the evidence.
We identified one retrospective cohort study with high risk of bias.81 The study retrospectively evaluated 22 patients treated with subtraction osteotomy for a metatarsal head ulcer to redress bone axis and arthrodesis with staples compared with 54 patients receiving conservative treatment (offloading not defined) and found significantly shorter time-to-healing in the surgical group (51 vs 159 days; P = .004).81
Evidence statement.
Osteotomy seems more effective to heal a metatarsal head DFU than conservative treatment (with or without offloading) alone.
Quality of evidence.
Low: Based on one retrospective cohort study with high risk of bias that did not define the control offloading treatment.
References.
Vanlerberghe et al 2014.81
Digital flexor tenotomy
Summary of the evidence.
We identified eight retrospective non-controlled case series with a cumulative total of 369 patients, treated with percutaneous digital flexor tenotomy to heal apical toe ulcers, reporting a 92% to 100% healing rate with a mean time-to-healing of 13 to 40 days.86–93
Evidence statement.
Digital flexor tenotomy seems effective to heal a neuropathic plantar lesser digit apical DFU, but evidence from controlled studies is needed to confirm this.
QoE.
Low: Based on eight retrospective case series all reporting consistent results.
References.
Engels et al 2016,86 Tamir et al 2014,87 Rasmussen et al 2013,88 van Netten et al 2013,89 Kearney et al 2010,90 Schepers et al 2010,91 Tamir et al 2008,92 and Laborde et al 2007.93
Other surgical offloading procedures
Summary of the evidence.
We identified multiple other non-controlled studies reporting on other surgical offloading procedures. Four non-controlled studies found relatively high percentages (74%−100%) of healing after exostectomy in patients with rigid, prominent deformities secondary to Charcot’s neuro-osteoarthropathy.120–123 Otherwise, other selected surgical procedures reported in non-controlled case series, and typically performed in patients with complex plantar soft tissue defects (with or without infection), may have value in promoting ulcer healing in selected cases. These surgical offloading techniques included using free flaps,124,125 Achilles tenotomy,126 flexor hallucis tendon transfer,127,128 plantar fascia release,129 calcanectomy,130–132 and surgical reconstruction133 or external fixation134–136 of Charcot deformity, or a combination of these procedures (resection, tendon transfer, and reconstruction).137,138
Evidence statement.
None.
3.1.6 |. Other DFU types
PICO a
In people with a plantar DFU complicated by infection or ischaemia, which offloading intervention is effective to heal the DFU?
Summary of the evidence.
We identified nine controlled studies17,33,58,65,67,75,76,80,81 and two large prospective non-controlled studies31,94 on offloading interventions that either did not exclude or specifically included participants with DFUs that were complicated by infection and/or ischaemia at baseline. None of the controlled studies specifically reported on the healing rates of subgroups of patients with DFUs complicated by infection or ischaemia at baseline, but the two non-controlled studies did.
The most recent non-controlled study prospectively compared the healing rates of a cohort of 177 patients with different subgroups of DFU that were treated with a non-removable offloading device (windowed TCC).31 They found no difference in healing after a mean of 96 days between those with uncomplicated (no infection or ischaemia) neuropathic DFU at baseline and those complicated with moderate ischaemia or those immediately post-surgery to resolve osteomyelitis with/without clinical signs of infection (“operated osteomyelitis”) (84% vs 81% vs 71%, respectively; P > .1).31
The second non-controlled study prospectively compared the healing rates of a cohort of 98 patients with different subgroups of DFUs that were treated with three different offloading devices and all instructed to not remove their cast between wound care visits: 50 with a TCC, 22 with a bivalved TCC, and 26 with a non-removable cast shoe.94 They found no differences between the healing rates of the three different offloading devices; however, the rates and P values were not reported.94 They found no difference in collective healing rates between uncomplicated DFU and mildly infected neuropathic DFU (90% vs 87%; P > .05).94 However, they did find a difference between uncomplicated DFU, DFU complicated with moderate ischaemia, and DFU with both moderate ischaemia and mild infection (90% vs 69% vs 36%, respectively; P < .01).94
Evidence statement.
Nonremovable knee-high offloading devices seem effective to heal a neuropathic plantar forefoot DFU complicated by either mild infection or mild ischaemia.
QoE.
Low: Based on two large prospective non-controlled studies, one reporting only on outcomes of non-removable knee-high offloading devices and the other predominantly.
References.
PICO b
In people with a plantar rearfoot DFU, which offloading intervention is effective to heal the DFU?
Summary of the evidence.
We identified two RCTs (one at very low risk,17 one at high risk of bias57) that included participants with DFUs on the plantar rearfoot. However, only one of these RCTs specifically reported on the healing rates of subgroups of patients with plantar rearfoot DFUs.57 This RCT with high risk of bias randomised 58 patients with DFU to either a TCC or therapeutic footwear and found shorter time-to-healing in the TCC group within the subgroup of 16 patients with plantar rearfoot DFU (69 vs 107 days; p = not reported).57
Evidence statement.
TCCs seem more effective than therapeutic footwear to heal a neuropathic plantar heel DFU.
QoE.
Low: Based on one RCT with high risk of bias that found clinical difference but did not report statistical difference, we downgraded to low.
References.
Ganguly et al 2008.57
PICO c
In people with a non-plantar DFU, which offloading intervention is effective to heal the DFU?
Summary of the evidence.
We identified one large RCT with very low risk of bias.17 This RCT randomised 509 patients, most (72%) with a non-plantar rearfoot DFU, to receive either a custom-made, light-weight, fibreglass heel cast with usual care or usual care alone.17 They found no differences between the two groups for healing rate after 24 weeks (44% vs 37%; P = .088); however, although most ulcers were non-plantar, they did not perform subgroup analyses of the outcomes for specific non-plantar heel ulcer locations.17 No studies were identified on other non-plantar DFU locations.
Evidence statement.
None. Although there was one large RCT, we were unable to provide an evidence statement as the RCT did not specifically report on non-plantar DFU outcomes.
3.2 |. Surrogate outcome: Plantar pressure
Outcomes for plantar pressure, mostly peak pressure, were obtained during walking barefoot or in a device or shoe, unless otherwise reported.
PICO
In people with a plantar DFU, which offloading intervention reduces plantar pressure most effectively?
We identified five controlled trials,16,55,66,70,79 and 29 non-controlled studies,26,27,37,46,95–114,139–143 addressing this clinical question for non-removable offloading devices, removable offloading devices, footwear, other offloading techniques, and surgical offloading.
3.2.1 |. Non-removable offloading devices
Summary of the evidence.
We identified one RCT55 and multiple cross-sectionals studies.95–98 The RCT with very low risk of bias randomised 23 patients to a non-removable knee-high device (TCC) or removable knee-high offloading device (walker).55 They found compared with baseline barefoot plantar pressures, a significantly greater reduction in plantar pressures in the removable knee-high walker compared with the TCC at the ulcer area (91% vs 80%; P = .024), forefoot (92% vs 84%; P = .011), and midfoot (77% vs 63%; P = 0.036), but no difference at the rearfoot (40% vs 54%; P = .108) or for the total foot (77% vs 73%; P = .297).55
Four cross-sectional studies found TCCs and different removable knee-high walkers (DH pressure relief walkers, aircast walkers, 3D walkers, CAM walkers, and Vaco diaped walkers) produced similar mean peak pressures reductions from conventional footwear pressure baselines at different regions of the forefoot (ulcer site, hallux, medial metatarsal heads, lateral metatarsal head).95–98 Findings in the rearfoot, however, were mixed with one study showing TCCs had greater peak pressure reduction96 and another showing removable knee-high walkers had greater peak pressure reduction.95
Three other cross-sectional studies investigated the effect of modified TCCs.26,46,139 One found a modified TCC (bivalved TCC) reduced significantly less peak pressure than a standard TCC at the hallux (108 vs 57 kPa; P < .05) and midfoot (104 vs 77 kPa; P < .05) but had similar peak pressures in other regions of the forefoot and rearfoot (all, P > .05).46 Another study found a modified TCC (with 12-mm Poron insole) reduced significantly more peak pressure at the ulcer area than the standard TCC using canvas shoe baseline values (70% vs 44%; P < .01).139 The last study found that a modified TCC (ankle-high) reduced significantly less peak pressure than a standard knee-high TCC at the forefoot (13% difference) and midfoot (8%) (P < .05), but the same for the rearfoot (2%) (P > .05).26
Evidence statement.
TCCs and removable knee-high offloading devices are equally effective in reducing peak pressure at the DFU location and forefoot and rearfoot areas.
QoE.
Moderate: Based on one small RCT with very low risk of bias showing small effects in favour of removable knee-high walkers, plus four cross-sectional studies showing no differences but using different types of devices, we downgraded to moderate.
References.
Gutekunst et al 2011,55 Gotz et al 2017,95 Armstrong et al 1999,96 Fleischli et al 1997,97 and Lavery et al 1996.98
3.2.2 |. Removable offloading devices
Summary of the evidence.
We identified one RCT16 and multiple cross-sectional studies.27,46,95,97,99–104 The RCT with very low risk of bias tested plantar pressure reductions after 2 weeks in a subsample of 34 patients randomised to different removable offloading devices.16 Compared with the patient’s own footwear, a bivalved TCC reduced peak pressure at the ulcer area more effectively than a cast shoe and forefoot offloading shoe (67% vs 26% and 47%, respectively; P = .029).16
Six cross-sectional studies found different types of removable knee-high devices (DH pressure relief walkers, aircast walkers, 3D walkers, CAM walkers, Vaco diaped walkers, and bivalved TCCs) to be significantly more effective in reducing forefoot peak pressure than removable ankle-high devices (walkers, cast shoes, half-shoes, postoperative shoes),27,46,95,97,99,100 with two studies also reporting significantly lower rearfoot peak pressures in the knee-high devices.95,100
Nine cross-sectional studies also found different types of removable ankle-high offloading devices (walkers, cast shoes, half-shoes, postoperative shoes, forefoot offloading shoes, pressure relief shoe) to be significantly more effective in reducing forefoot peak pressure compared with different footwear types (extra-depth footwear, canvas shoes, sneaker, off-the-shelf footwear, athletic shoe, standard shoe),27,95,97,99–104 with four studies also finding significantly lower rearfoot plantar pressures in the ankle-high devices.100,101,103,104
Evidence statement a.
Removable knee-high offloading devices are more effective in reducing peak pressure at the DFU and forefoot area than removable ankle-high offloading devices.
QoE.
Moderate: Based on one RCT with very low risk of bias and six cross-sectional studies all with consistent results, but all using different types of devices, we have downgraded to moderate.
References.
Bus et al 2018,16 Crews et al 2018,27 Westra et al 2018,46 Gotz et al 2017,95 Crews et al 2012,99 Nagel et al 2009,100 Fleischli et al 1997.97
Evidence statement b.
Removable ankle-high offloading devices seem more effective than conventional or standard therapeutic footwear in reducing peak pressure at the DFU location and forefoot areas.
QoE.
Low: Based on nine cross-sectional studies, all with consistent results.
References.
Crews et al 2018,27 Gotz et al 2017,95 Bus et al 2017,101 Crews et al 2012,99 Raspovic et al 2012,102 Bus et al 2009,103 Bus et al 2009,104 Nagel et al 2009,100 and Fleischli et al 1997.97
3.2.3 |. Footwear
Summary of the evidence.
We identified one prospective cohort study79 and multiple cross-sectional studies.98,105–113 The prospective cohort study with high risk of bias allocated 241 patients with DFU history (previous or current) to four different footwear types. They found after 9 months follow-up that three different therapeutic footwear groups (two groups with different customised sandals and one group customised footwear) had significant reductions in in-shoe peak pressures at their metatarsal heads (57.4% vs 62.0% vs 58.0%, respectively) compared with baseline, but another group wearing their own conventional sandals had significant increases in peak pressures (+39.4%) (all, P < .01).79
Nine cross-sectional studies found different types of therapeutic footwear (custom-made, extra-depth shoes, rocker-bottom shoes, custom-made insoles/orthoses) reduce forefoot peak pressure more effectively than conventional footwear (canvas shoes, walking shoes, athletic shoes).98,105–113
Evidence statement.
Therapeutic footwear seems more effective than conventional footwear in reducing peak pressure at forefoot areas in people with diabetes.
QoE.
Low: Based on one controlled study with high risk bias and 10 cross-sectional studies all with consistent results.
References.
Viswanathan et al 2004,79 Nouman et al 2017,105 Lin et al 2013,106 Kavros et al 2011,107 Guldemond et al 2007,108 Praet et al 2003,109 Raspovic et al 2000,110 Lavery et al 1997,111 Lavery et al 1997,112 Lavery et al 1996,98 and Kato et al 1996.113
3.2.4 |. Other offloading techniques
Summary of the evidence.
We identified one RCT on botulinum toxin66 and five non-controlled studies on additional other offloading techniques, including felted foam,37,114 offloading dressing,140 and biofeedback gait retraining sessions.141,142 The RCT with very low risk of bias randomised 17 patients with a neuropathic plantar forefoot ulcer to receive injections of either botulinum toxin (200- or 300-unit doses) or saline into the medial and lateral gastrocnemius and soleus muscle bellies of the limb with the ulcer. The authors found no differences between groups on plantar pressure reductions at baseline or after 2 weeks.66
Two cross-sectional studies investigated felted foam.37,114 The first found felted foam of different densities applied to the foot significantly reduced forefoot peak pressure during barefoot walking, both immediately after application (57%−72%, P < .05) and after 72 hours (48%−72%, P < .05).114 The second found deflective felted foam applied to the barefoot and worn in a post-operative shoe reduced peak pressure at the ulcer site significantly more effectively than a post-operative shoe alone, both immediately after application (49%) and after 7 days wear (32%) (P < .05).37
One cross-sectional study found a 38% reduction in peak pressure at the ulcer site immediately after the application of an adhesive polyurethane foam wound dressing compared with no foam dressing (P < .01).140
Two non-controlled prospective studies investigated the effect of biofeedback gait retraining.141,142 This involved measuring patient’s in-shoe plantar pressure at baseline and then encouraging patients to practice changing their gait until they were able to demonstrate a 40% to 80% reduction in peak plantar pressure at their ulcer area.141,142 Both studies retested patients after 10 days and found significant decreases in peak pressure at the ulcer site compared with baseline (P < .05): 20% in the first study142 and 31% in the second.141
Evidence statement a.
Botulinum toxin injections are not superior to saline placebo injections for reducing plantar pressure at forefoot areas in persons with neuropathic plantar forefoot ulcers.
QoE.
Moderate: Based on one small RCT with very low risk of bias not powered for equivalence, we downgraded to moderate.
References.
Hastings et al 2012.66
Evidence statement b.
Felted foam applied to the forefoot with a cut out to the ulcer area seems more effective at reducing plantar pressure over 1 week at the DFU site compared with using no felted foam.
QoE.
Low: Based on two cross-sectional studies with consistent findings.
References.
Evidence statement c.
No evidence statements for wound dressings or biofeedback gait retraining were justified due to limited evidence.
3.2.5 |. Surgical offloading techniques
Summary of the evidence.
We identified one RCT70 and one non-controlled study.143 The RCT with low risk of bias70 tested plantar pressure reductions in a subsample of a larger RCT on Achilles tendon lengthening.71 They randomised 28 participants to have Achilles tendon lengthening in addition to a TCC (surgical group) or TCC alone (control group) and measured peak pressures at baseline immediately prior to treatment, and 3 weeks and 8 months post-treatment.70 They found no differences between groups at baseline (P > .05), but significantly lower forefoot peak pressures and higher rearfoot peak pressures in the surgical group at 3 weeks, of which the differences in rearfoot peak pressure remained at 8 months (P < .005).70 The non-controlled study of people with neuropathic plantar forefoot ulcers found peak plantar pressure reductions at the metatarsal heads following metatarsal head resections.143
Evidence statement.
Achilles tendon lengthening in addition to a TCC seems more effective at reducing peak pressures at the forefoot in the short term than a TCC alone, but not in the long term, and at the expense of increases in rearfoot peak pressure.
QoE.
Low: Based on one small RCT with low risk of bias, but because it was a subsample of a larger RCT and not powered for this outcome, we downgraded to low.
References.
Maluf et al 2004.70
4 |. DISCUSSION
In this updated systematic review on offloading interventions to heal DFUs, we identified six meta-analyses, 26 RCTs, 13 other controlled studies, and 120 non-controlled studies. New studies included since our previous review 4 years ago were four of those meta-analyses, seven RCTs, two other controlled studies, and 28 non-controlled studies. The methodological quality of the studies varied, with six meta-analyses, 13 RCTs, and two other controlled studies being high quality ([very] low risk of bias), and the rest of lower quality. Most studies investigated the effects of offloading devices, including five meta-analyses, 19 RCTs, and six other controlled studies. Therefore, for offloading devices, we were able to formulate relatively strong evidence statements where the quality of supporting evidence was typically moderate to high. However, studies investigating other interventions were limited in both number and quality, such as for footwear, surgical offloading, and other offloading techniques. Therefore, for these offloading intervention categories, we were either unable to formulate any evidence statements or were only able to formulate weaker evidence statements based on limited supporting evidence. Otherwise, virtually no evidence existed in several other important areas, including offloading interventions to heal DFU that were non-plantar, on the plantar rearfoot or complicated by infection or ischaemia.
4.1 |. Non-removable offloading devices
There is strong evidence, supported by five high-quality meta-analyses,12,13,15,52,53 that non-removable knee-high offloading devices heal plantar forefoot and midfoot ulcers more effectively and at faster rates than all other offloading interventions. Further strong evidence demonstrates that (non-removable and removable) knee-high offloading devices more effectively reduce plantar pressure at the ulcer site16,27,46,95 and non-removable knee-high offloading devices give significantly higher adherence levels34,76,144 than other removable offloading devices and therapeutic footwear. We found some evidence that they may also result in similar or reduced ambulatory activity levels to removable knee-high devices18,34,63 and removable ankle-high devices.34,63 These findings support the superiority of non-removable knee-high offloading devices in healing DFUs.
Although evidence clearly shows the healing benefits, non-removable knee-high offloading devices have also been believed to result in more adverse events than other offloading interventions. However, the available evidence, although not substantial, does not seem to support these beliefs. There is some evidence that non-removable knee-high offloading devices result in similar adverse events12,52 and patient-reported satisfaction levels to that of removable offloading devices or therapeutic footwear.19,34,60,64 There is also some evidence that non-removable offloading devices are more cost-effective than removable offloading devices and therapeutic footwear.12,19,56
From the different non-removable knee-high offloading devices available, we again identified11 that TCCs and non-removable walkers are equally effective.12,36,53 They are equally effective to heal DFU12,36,53 and reduce plantar pressure.55,95–98 We also found some evidence they produced similar levels of adverse events12 and patient satisfaction.19,34,60 However, we did find that non-removable walkers were more cost-effective than TCCs.12,19,60,62 Therefore, the available evidence base clearly demonstrates that patients with neuropathic plantar forefoot or midfoot ulcers should be provided with either a TCC or non-removable knee-high walker as their first choice of offloading treatment.
4.2 |. Removable offloading devices
We found relatively strong evidence that removable knee-high and ankle-high offloading devices are equally effective to heal plantar forefoot or midfoot ulcers and reduce ulcer surface area.12,16 However, we also found relatively strong evidence that removable knee-high offloading devices are more effective at reducing plantar pressure at the forefoot16,27,46,95,97,99,100 and some evidence they also reduce ambulatory activity to a larger extent16,34,63 than removable ankle-high offloading devices and therapeutic footwear. On the other hand, evidence suggests patients may be less adherent to wearing removable knee-high than ankle-high offloading devices.16,34 These findings on surrogate outcomes may counteract each other to explain why these devices result in similar healing outcomes, as identified in one high-quality RCT.16 Therefore, more effective healing in removable knee-high offloading devices may be achievable if improved patient adherence levels can be assured.28
Nonremovable knee-high offloading devices are sometimes contraindicated and may not be preferred by clinicians and patients.145–147 From our findings, removable offloading devices are the next best evidence-based option for DFU offloading. However, it should be noted that many different types of removable knee-high and ankle-high offloading devices have been tested, and no single type of removable device seems superior to another which further complicates the decision on which removable offloading device to use in clinical practice. Therefore, we recommend that future RCTs compare the effectiveness of more homogenous types of removable devices, such as custom-made vs prefabricated or knee-high vs above ankle-high vs below ankle-high, against gold standard non-removable knee-high offloading devices and each other. This would better inform clinicians and patients on the removable offloading devices that are most (cost-)effective for healing, preferred by patients, limit adverse events, and encourage adherence.
4.3 |. Footwear
We found strong evidence that conventional and therapeutic footwear is much less effective to heal a plantar forefoot or midfoot DFU,12,13,36,53 reduce plantar pressure at the ulcer site,27,95,97,99–104 and much less cost-effective than (non)removable knee-high offloading devices.12 Furthermore, we found some evidence that they produced similar levels of adverse events12 and patient satisfaction64 to (non)removable offloading devices. In addition, therapeutic footwear is less effective at reducing plantar pressure than removable ankle-high offloading devices27,95,97,99–104 but more effective than conventional footwear.79,98,105–113 As a result of these findings, conventional or therapeutic footwear should not be used to heal a plantar forefoot or midfoot DFU as there are more effective offloading device interventions available.
4.4 |. Other non-surgical offloading techniques
While other non-surgical offloading techniques are commonly used in clinical practice for offloading plantar DFU,145–147 such as the use of crutches and bed rest, the current evidence is virtually non-existent for these practices. We only identified studies on the effects of felted foam, offloading wound dressings, biofeedback gait retraining, and botulinum toxin injections. We found some evidence that felted foam can be more effective in healing a plantar DFU68,77 than not using felted foam, either by attaching it to the foot or to the insole of a removable ankle-high device.67,77 The basis for this seems be a more effective reduction of plantar pressure with using felted foam than without.37,114 Similar effects on pressure were also shown for a foam wound dressing,140 and for biofeedback gait retraining sessions,141,142 but all only show effects over the following days and long-term effects are unknown. Limited evidence also showed there is no benefit for botulinum toxin injections over placebo saline injections to reduce plantar pressures.66 Clearly, more high-quality controlled studies are needed to increase the evidence bases for these other non-surgical offloading interventions.
4.5 |. Surgical offloading techniques
The current evidence base for surgical offloading for healing plantar DFU is still limited, with very few controlled studies published69,80 since our previous review 4 years ago.11 Achilles tendon lengthening seems to have limited value in addition to a TCC alone in healing plantar forefoot ulcers.14 However, there is some evidence it reduces forefoot plantar pressure in the short term, but at the expense of increased rearfoot plantar pressure resulting in more new heel ulcer adverse events than when using a TCC alone.70 The evidence also indicates that most other surgical procedures do not improve the proportion of healed ulcers, only the time-to-healing. This includes metatarsal head resections72,80,82,83 and joint arthroplasty.84,85 We found some promising effects for digital flexor tenotomy to heal plantar lesser digit DFU in multiple case series,86–93 but there are no controlled studies to confirm this as yet. It should be noted that all these surgical offloading studies either included patients that had failed to heal using offloading devices, tested procedures that were used in combination with offloading devices, and/or showed effects compared with a comparator that was not considered a gold standard non-surgical offloading treatment. As we identified 4 years ago, high-quality controlled studies, preferably multi-centred RCTs,30 are still needed to further define the role of surgical offloading interventions compared with non-surgical offloading treatments.
4.6 |. Other DFU types
Nearly all evidence found in this systematic review was on the efficacy of offloading interventions to heal neuropathic plantar forefoot and midfoot DFU without infection and ischaemia. We found some evidence for the use of non-removable knee-high offloading devices to heal plantar forefoot DFU complicated by mild infection or mild ischaemia.31,94 Similarly, we found some evidence for the use of non-removable knee-high offloading devices to heal plantar rearfoot DFU.57 However, no specific evidence was found for the use of offloading interventions to heal non-plantar DFU, although these ulcers also require offloading to heal. As neuropathic foot ulcers that are complicated by infection or ischaemia or are located on the non-plantar surface currently represent a large proportion of DFU seen in clinical practice,148 we repeat our conclusion from 4 years ago that the evidence-base for the use of offloading to heal these other types of DFU types requires urgent expansion through high-quality controlled studies to inform the community on effective treatment for these DFU.
4.7 |. Key considerations
There are several key considerations that come out of this updated systematic review.
First, new evidence from this review is making it increasingly clear that patient adherence levels to wearing offloading devices heavily influences the effectiveness of ulcer healing. Even the best offloading device will not be effective if not worn. Conversely, removable devices seem to be as effective as non-removable devices when worn. While non-removable devices may be one solution to increasing adherence, these devices are sometimes contraindicated or not preferred by clinicians. Therefore, ways to encourage patients to adhere should receive immediate attention by clinicians and researchers. Offering more attractive personalised offloading treatments and improving the motivation of patients to the benefits on healing of wearing their devices may help in this regard.
Second, the available evidence identified from this review almost exclusively focuses on noncomplicated neuropathic plantar forefoot and midfoot ulcers. Little evidence exists on the efficacy to heal non-plantar ulcers, rearfoot plantar ulcers, and ulcers complicated by infection or ischaemia, even though such ulcers are very common, particularly in the case of peripheral artery disease. High-quality RCTs on foot ulcers other than neuropathic plantar forefoot and midfoot ulcers are urgently needed to better inform clinicians about effective offloading treatments for such ulcers.
Third, we acknowledge the challenges inherent in the design of RCTs involving surgical offloading procedures, including regional variations in equipment, technique, and practice, and that surgical intervention is often a last resort intervention employed after failed healing with non-surgical offloading interventions. For these reasons, we accept that other study designs investigating foot ulcer healing by surgical offloading may be suitable as well. However, we do note with interest that a protocol for a high-quality RCT on surgical offloading has recently been published.30
Fourth, in this updated review, we specifically assessed for a range of surrogate and secondary outcomes. This has illustrated that compared with the primary outcome of healing little evidence exists for the effect of offloading interventions on ambulatory activity, adherence, adverse events, patient-reported, and cost outcomes. We recommend that future controlled trials report these outcomes in alignment with international definition standards.24 This should provide more details on how these surrogate outcomes influence healing, which may enable the development of new offloading interventions that are better tailored to improve these outcomes and with that, healing. Additionally, as RCTs often do not adequately power for secondary outcomes, this would facilitate future meta-analyses on these outcomes, particularly for adverse events, such as pre-ulcerative lesions, new ulcers, and falls24.
Fifth, we note there are no known objective thresholds for surrogate outcomes that indicate improved chances of DFU healing.6 Whereas, in the field of DFU prevention, there are certain thresholds for peak plantar pressures that have been shown to reduce risk of reulceration,149,150 no such thresholds yet exist for DFU healing. We recommend that trials interrogate their surrogate outcome data to explore if such thresholds for plantar pressure, ambulatory activity, adherence, or a combination exist to better inform the field on how much offloading is needed to improve healing.44
Sixth, although this review has identified broad categories of removable offloading devices that positively affect healing, removable offloading devices are made up of a large variety of custom-made and prefabricated devices, different foot device interfaces, heights, and other features, such as rocker bottoms. Future trials should determine which specific devices or designs are most effective for offloading and improving healing.
Last, most studies in this review come from economically developed countries with relatively mild temperate climates. There is a need for more studies on optimal approaches to ulcer healing in less economically developed countries and those where climate may be a factor in adherence to, or efficacy of, treatment. This may involve the development of offloading devices that are lighter in weight, provide a cooler environment, and are less expensive than some of the devices currently on the market, without losing the key mechanical features that optimise offloading and healing.
5 |. CONCLUSIONS
Our updated systematic review shows that the evidence base to support the use of offloading interventions to heal DFU has improved substantially in several areas over the last few years but is still small or non-existent in other areas. By far, the best available evidence is for the use of non-removable knee-high offloading devices, either TCC or walkers rendered non-removable, for the healing of neuropathic plantar forefoot and midfoot ulcers. Additionally, high-quality recent evidence supports the use of different removable offloading devices to heal plantar forefoot and midfoot ulcers when patients adhere to wearing them and it does not support the use of conventional or therapeutic footwear. The evidence bases to support the use of other non-surgical offloading interventions and the use of surgical offloading is still weak. Likewise, the evidence bases to support the use of any offloading interventions to heal non-plantar foot ulcers, plantar rearfoot ulcers, and ischaemic or infected neuropathic ulcers is practically non-existent. High-quality RCTs of non-surgical and surgical offloading interventions that include measures for changes in plantar pressure, ambulatory activity, and treatment adherence (where appropriate), as well as reporting of adverse events, patient satisfaction, and costs, are needed to better inform clinicians and patients about effective offloading treatment in these areas.
Supplementary Material
TABLE 2.
Risk of bias tables for all RCTs
| Reference (in reverse chronological order) | Randomization | Independent Assignment | Patient or Care Provider Blinded | Outcome Assessor Blinded | Groups Similar at Baseline | Withdrawal/Drop-out Rates Acceptable (<20%) | Intention-to-Treat Analysis Performed | Patients Treated Equally Except for Intervention | Selective Reporting of Outcomes Ruled Out | Free from Commercial Influence | Total Score | Total Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Offloading devices | ||||||||||||
| Bus et al 201816 | + | + | − | + | − | + | + | + | + | + | 8/10 | ++ |
| Johnson et al 201833 | + | ? | − | ? | + | + | − | + | − | + | 5/10 | − |
| Najafi et al 201718 | + | ? | − | + | − | + | − | − | + | + | 5/10 | − |
| Piaggesi et al 201619 | + | + | − | + | + | + | − | + | ? | + | 7/10 | + |
| Chakraborty et al 201554 | ? | ? | + | ? | + | ? | ? | + | ? | + | 4/10 | − |
| Lavery et al 201534 | + | ? | ? | − | + | − | + | + | + | − | 5/10 | − |
| Miyan et al 201436* | + | ? | − | − | + | ? | − | + | + | ? | 4/10 | − |
| Gutekunst et al 201155 | + | + | − | − | + | + | + | + | + | + | 8/10 | ++ |
| Faglia et al 201056 | + | ? | ? | − | + | + | + | + | + | ? | 6/10 | + |
| Ganguly et al 200857 | + | ? | ? | − | ? | + | ? | − | + | ? | 3/10 | − |
| Van de Weg et al 200858 | + | + | − | + | − | + | ? | + | + | + | 7/10 | + |
| Caravaggi et al 200759 | + | ? | ? | − | ? | + | + | + | + | ? | 5/10 | − |
| Piaggesi et al 200760 | + | ? | ? | − | + | + | + | + | + | − | 6/10 | + |
| Armstrong et al 200561 | + | + | − | − | + | + | + | + | + | − | 7/10 | + |
| Katz et al 200562 | + | ? | − | − | + | + | + | + | + | − | 6/10 | + |
| Armstrong et al 200163 | + | ? | − | − | + | + | − | + | + | − | 5/10 | − |
| Caravaggi et al 200064 | + | ? | − | − | + | + | ? | + | + | ? | 5/10 | − |
| Mueller et al 198965 | + | ? | − | − | + | − | + | + | + | ? | 5/10 | − |
| Other offloading techniques | ||||||||||||
| Jeffcoate et al 201717 | + | + | − | + | + | + | + | − | + | + | 8/10 | ++ |
| Hastings et al 201266 | + | + | + | + | + | + | + | + | ? | ? | 8/10 | ++ |
| Nube et al 200667 | + | + | − | + | ? | − | + | + | ? | ? | 5/10 | − |
| Zimny et al 200368 | + | − | − | − | + | − | ? | + | ? | ? | 3/10 | − |
| Surgical offloading techniques | ||||||||||||
| Wang et al 201569 | + | ? | ? | ? | + | ? | + | + | − | + | 5/10 | − |
| Maluf et al 200470 | + | + | − | − | + | ? | − | + | + | + | 6/10 | + |
| Mueller et al 200371 | + | + | − | ? | + | + | − | + | + | + | 7/10 | + |
| Piaggesi et al 199872 | + | ? | − | − | + | + | + | + | + | ? | 6/10 | + |
Note. +, yes criterion is met; −, no criterion is not met; ?, not reported or not clear. Total risk of bias: ++ very low risk of bias; +, low risk of bias; −, high risk of bias.
: This paper was included in both Offloading devices and Footwear categories.
ACKNOWLEDGEMENTS
The authors and IWGDF Editorial Board wish to acknowledge the kind expert review of the clinical questions and definitions by the following international experts: Zufiqarali Abbas, Tanzania; Abdul Basit, Pakistan; Heidi Corcoran, Hong Kong; Ryan Crews, United States of America; Yamile Jubiz, Colombia; Klaus Kirketerp-Moller, Denmark; Grace Spencer, Caribbean / St Maarten; Gulupar Srisawasdi, Thailand; Bashir Tarazi, Palestina; and Ioan Veresiu, Romania. We would also like to acknowledge peer review of this manuscript by Jaap van Netten (on behalf of the IWGDF Editorial Board) and Ryan Crews (independent external expert).
Abbreviations:
- DFU
diabetic foot ulcer
- IWGDF
International Working Group on the Diabetic Foot
- PICOs
population, intervention, control, outcomes
- PRISMA
preferred reporting items for systematic reviews and meta-analyses
- RCT
randomised controlled trial
- SIGN
Scottish Intercollegiate Grouping Network
Footnotes
CONFLICT OF INTERESTS
Production of the 2019 IWGDF Guidelines was supported by unrestricted grants from Molnlycke Healthcare, Acelity, ConvaTec, Urgo Medical, Edixomed, Klaveness, Reapplix, Podartis, Aurealis, SoftOx, Woundcare Circle, and Essity. These sponsors did not have any communication related to the systematic reviews of the literature or related to the guidelines with working group members during the writing of the guidelines and have not seen any guideline or guideline-related document before publication. All individual conflict of interest statement of authors of this guideline can be found at https://iwgdfguidelines.org/about-iwgdf-guidelines/biographies/
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boulton AJM. Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care 2018;41(4): 645–652. [DOI] [PubMed] [Google Scholar]
- 2.Lazzarini PA, Hurn SE, Kuys SS, et al. The silent overall burden of foot disease in a representative hospitalised population. Int Wound J 2017;14(4):716–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366(9498): 1719–1724. [DOI] [PubMed] [Google Scholar]
- 4.Lazzarini PA, Pacella RE, Armstrong DG, Van Netten JJ. Diabetes-related lower-extremity complications are a leading cause of the global burden of disability. Diabet Med 2018;35:1297–1299. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. New England Journal of Medicine 2017;376(24):2367–2375. [DOI] [PubMed] [Google Scholar]
- 6.Lazzarini PA, Crews RT, Van Netten JJ, et al. Measuring plantar tissue stress in people with diabetic peripheral neuropathy: a critical concept in diabetic foot management. Journal of Diabetes Science and Technology 2019;13(5):869–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernando ME, Crowther RG, Pappas E, et al. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: a meta-analysis of observational studies. Plos One 2014;9(6):e99050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bus SA. The role of pressure offloading on diabetic foot ulcer healing and prevention of recurrence. Plast Reconstr Surg 2016;138(3 Suppl):179S–187S. [DOI] [PubMed] [Google Scholar]
- 9.Bus SA, Armstrong DG, van Deursen RW, et al. IWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetes. Diabetes Metab Res Rev 2016;32: 25–36. [DOI] [PubMed] [Google Scholar]
- 10.Schaper NC, Van Netten JJ, Apelqvist J, Lipsky BA, Bakker K, on behalf of the International Working Group on the Diabetic F. Prevention and management of foot problems in diabetes: a summary guidance for daily practice 2015, based on the IWGDF guidance documents. Diabetes Metab Res Rev 2016; 32: 7–15. [DOI] [PubMed] [Google Scholar]
- 11.Bus SA, van Deursen RW, Armstrong DG, et al. Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review. Diabetes Metab Res Rev 2016;32:99–118. [DOI] [PubMed] [Google Scholar]
- 12.Health Quality Ontario. Fibreglass total contact casting, removable cast walkers, and irremovable cast walkers to treat diabetic neuropathic foot ulcers: a health technology assessment. Ont Health Technol Assess Ser 2017;17(12):1–124. [PMC free article] [PubMed] [Google Scholar]
- 13.Elraiyah T, Prutsky G, Domecq JP, et al. A systematic review and meta-analysis of off-loading methods for diabetic foot ulcers. J Vasc Surg 2016;63(2):59S–68Se1–2. [DOI] [PubMed] [Google Scholar]
- 14.Dallimore SM, Kaminski MR. Tendon lengthening and fascia release for healing and preventing diabetic foot ulcers: a systematic review and meta-analysis. J Foot Ankle Res 2015;8:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martins de Oliveira AL, Moore Z. Treatment of the diabetic foot by offloading: a systematic review. J Wound Care 2015; 24(12): 560, 562–570. [DOI] [PubMed] [Google Scholar]
- 16.Bus SA, JJv N, Kottink AIR, et al. The efficacy of removable devices to offload and heal neuropathic plantar forefoot ulcers in people with diabetes: a single-blinded multicentre randomised controlled trial. Int Wound J 2018;15(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeffcoate W, Game F, Turtle-Savage V, et al. Evaluation of the effectiveness and cost-effectiveness of lightweight fibreglass heel casts in the management of ulcers of the heel in diabetes: a randomised controlled trial. Health Technol Assess 2017;21(34): 1–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Najafi B, Grewal GS, Bharara M, Menzies R, Talal TK, Armstrong DG. Can’t stand the pressure: the association between unprotected standing, walking, and wound healing in people with diabetes. J Diabetes Sci Technol 2017;11(4):657–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piaggesi A, Goretti C, Iacopi E, et al. Comparison of removable and irremovable walking boot to total contact casting in offloading the neuropathic diabetic foot ulceration. Foot Ankle Int 2016;37(8): 855–861. [DOI] [PubMed] [Google Scholar]
- 20.Bus SA, Armstrong DG, Gooday C, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev 2020;36(S1):e3274. [DOI] [PubMed] [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Plos Medicine 2009; 6(7): e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Medicine 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Netten JJ, Bus SA, Apelqvist J, et al. Definitions and criteria for diabetic foot disease. Diabetes Metab Res Rev 2020;36(S1):e3268. [DOI] [PubMed] [Google Scholar]
- 24.Jeffcoate WJ, Bus SA, Game FL, Hinchliffe RJ, Price PE, Schaper NC. Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: required details and markers of good quality. The Lancet Diabetes & Endocrinology 2016;4(9): 781–788. [DOI] [PubMed] [Google Scholar]
- 25.Arnold JF, Marmolejo V. Outcomes achieved with use of a prefabricated roll-on Total contact cast. Foot Ankle Int 2017;38(10): 1126–1131. [DOI] [PubMed] [Google Scholar]
- 26.Begg L, McLaughlin P, Vicaretti M, Fletcher J, Burns J. Total contact cast wall load in patients with a plantar forefoot ulcer and diabetes. J Foot Ankle Res 2016;9:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crews RT, Candela J. Decreasing an offloading device’s size and off-setting its imposed limb-length discrepancy lead to improved comfort and gait. Diabetes Care 2018;41(7):1400–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crews RT, Shen B-J, Campbell L, et al. Role and determinants of adherence to off-loading in diabetic foot ulcer healing: a prospective investigation. Diabetes Care 2016;39(8):1371–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernando ME, Crowther RG, Lazzarini PA, et al. Plantar pressures are elevated in people with longstanding diabetes-related foot ulcers during follow-up. PLOS One 2017;12(8):e0181916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finestone AS, Tamir E, Ron G, Wiser I, Agar G. Surgical offloading procedures for diabetic foot ulcers compared to best non-surgical treatment: a study protocol for a randomized controlled trial. J Foot Ankle Res 2018;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ha Van G, Michaux C, Parquet H, Bourron O, Pradat-Diehl P, Hartemann A. Treatment of chronic plantar ulcer of the diabetic foot using an irremovable windowed fibreglass cast boot: prospective study of 177 patients. Diabetes Metab Res Rev 2015;31(7): 691–698. [DOI] [PubMed] [Google Scholar]
- 32.Jarl G, Tranberg R. An innovative sealed shoe to off-load and heal diabetic forefoot ulcers—a feasibility study. Diabet Foot Ankle 2017; 8(1):1348178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson DJ, Saar BJ, Shevitz AJ, et al. A Total offloading foot brace for treatment of diabetic foot ulcers: results from a halted randomized controlled trial. Wounds 2018;30(7):182–185. [PubMed] [Google Scholar]
- 34.Lavery LA, Higgins KR, La Fontaine J, Zamorano RG, Constantinides GP, Kim PJ. Randomised clinical trial to compare total contact casts, healing sandals and a shear-reducing removable boot to heal diabetic foot ulcers. Int Wound J 2015;12(6):710–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lew E, Nicolosi N, McKee P. Evaluation of hallux interphalangeal joint arthroplasty compared with nonoperative treatment of recalcitrant hallux ulceration. J Foot Ankle Surg 2015;54(4):541–548. [DOI] [PubMed] [Google Scholar]
- 36.Miyan Z, Ahmed J, Zaidi SI, Ahmedani MY, Fawwad A, Basit A. Use of locally made off-loading techniques for diabetic plantar foot ulcer in Karachi, Pakistan. Int Wound J 2014;11(6):691–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raspovic A, Waller K, Wong WM. The effectiveness of felt padding for offloading diabetes-related foot ulcers, at baseline and after one week of wear. Diabetes Res Clin Pract 2016;121:166–172. [DOI] [PubMed] [Google Scholar]
- 38.Roser MC, Canavan PK, Najafi B, Watchman MC, Vaishnav K, Armstrong DG. Novel in-shoe exoskeleton for offloading of forefoot pressure for individuals with diabetic foot pathology. J Diabetes Sci Technol 2017;11(5):874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saikia P, Hariharan R, Shankar N, Gaur AK, Jose NM. Effective and economic offloading of diabetic foot ulcers in India with the Bohler iron plaster cast. Indian J Surg 2016;78(2):105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheahan H, Canning K, Refausse N, et al. Differences in the daily activity of patients with diabetic foot ulcers compared to controls in their free-living environments. Int Wound J 2017;14(6):1175–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tamir E, Tamir J, Beer Y, Kosashvili Y, Finestone AS. Resection arthroplasty for resistant ulcers underlying the hallux in insensate diabetics. Foot Ankle Int 2015;36(8):969–975. [DOI] [PubMed] [Google Scholar]
- 42.Tamir E, Finestone AS, Avisar E, Agar G. Mini-invasive floating metatarsal osteotomy for resistant or recurrent neuropathic plantar metatarsal head ulcers. J Orthop Surg Res 2016;11(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tickner A, Klinghard C, Arnold JF, Marmolejo V. Total contact cast use in patients with peripheral arterial disease: a case series and systematic review. Wounds 2018;30(2):49–56. [PubMed] [Google Scholar]
- 44.van Netten JJ, van Baal JG, Bril A, Wissink M, Bus SA. An exploratory study on differences in cumulative plantar tissue stress between healing and non-healing plantar neuropathic diabetic foot ulcers. Clin Biomech (Bristol, Avon) 2018;53:86–92. [DOI] [PubMed] [Google Scholar]
- 45.van Netten JJ, Lazzarini PA, Armstrong DG, et al. Diabetic foot Australia guideline on footwear for people with diabetes. Journal of Foot and Ankle Research 2018;11(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Westra M, JJv N, Manning HA, JGv B, Bus SA. Effect of different casting design characteristics on offloading the diabetic foot. Gait Posture 2018;64:90–94. [DOI] [PubMed] [Google Scholar]
- 47.DocTranslator. Online Document Translator 2019. https://www.onlinedoctranslator.com/(accessed 25th April 2019).
- 48.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016;5 (1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ 2001;323(7308):334–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alonso-Coello P, Oxman AD, Moberg J, et al. GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ 2016;353:i2089. [DOI] [PubMed] [Google Scholar]
- 51.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lewis J, Lipp A. Pressure-relieving interventions for treating diabetic foot ulcers. Cochrane Database Syst Rev 2013;1:CD002302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morona JK, Buckley ES, Jones S, Reddin EA, Merlin TL. Comparison of the clinical effectiveness of different off-loading devices for the treatment of neuropathic foot ulcers in patients with diabetes: a systematic review and meta-analysis. Diabetes Metab Res Rev 2013;29 (3):183–193. [DOI] [PubMed] [Google Scholar]
- 54.Chakraborty PP, Ray S, Biswas D, et al. A comparative study between total contact cast and pressure-relieving ankle foot orthosis in diabetic neuropathic foot ulcers. J Diabetes Sci Technol 2015;9(2): 302–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gutekunst DJ, Hastings MK, Bohnert KL, Strube MJ, Sinacore DR. Removable cast walker boots yield greater forefoot off-loading than total contact casts. Clin Biomech (Bristol, Avon) 2011;26(6): 649–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Faglia E, Caravaggi C, Clerici G, et al. Effectiveness of removable walker cast versus non-removable fiberglass off-bearing cast in the healing of diabetic plantar foot ulcer a randomized controlled trial. Diabetes Care 2010;33(7):1419–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ganguly S, Chakraborty K, Mandal PK, et al. A comparative study between total contact casting and conventional dressings in the non-surgical management of diabetic plantar foot ulcers. J Indian Med Assoc 2008; 106(4): 237–239, 244. [PubMed] [Google Scholar]
- 58.Van De Weg FB, Van Der Windt DA, Vahl AC. Wound healing: total contact cast vs. custom-made temporary footwear for patients with diabetic foot ulceration. Prosthet Orthot Int 2008;32(1):3–11. [DOI] [PubMed] [Google Scholar]
- 59.Caravaggi C, Sganzaroli A, Fabbi M, et al. Nonwindowed non-removable fiberglass offm-loading cast versus removable pneumatic cast (AircastXP diabetic walker) in the treatment of neuropathic noninfected plantar ulcers. Diabetes Care 2007;30(10): 2577–2578. [DOI] [PubMed] [Google Scholar]
- 60.Piaggesi A, Macchiarini S, Rizzo L, et al. An off-the-shelf instant contact casting device for the management of diabetic foot ulcers—a randomized prospective trial versus traditional fiberglass cast. Diabetes Care 2007;30(3):586–590. [DOI] [PubMed] [Google Scholar]
- 61.Armstrong DG, Lavery LA, Wu S, Boulton AJM. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds—a randomized controlled trial. Diabetes Care 2005;28(3): 551–554. [DOI] [PubMed] [Google Scholar]
- 62.Katz IA, Harlan A, Miranda-Palma B, et al. A randomized trial of two irremovable off-loading devices in the management of plantar neuropathic diabetic foot ulcers. Diabetes Care 2005;28(3): 555–559. [DOI] [PubMed] [Google Scholar]
- 63.Armstrong DG, van Schie CHM, Nguyen HC, Boulton AJM, Lavery LA, Harkless LB. Off-loading the diabetic foot wound—a randomized clinical trial. Diabetes Care 2001;24(6):1019–1022. [DOI] [PubMed] [Google Scholar]
- 64.Caravaggi C, Faglia E, De Giglio R, et al. Effectiveness and safety of a non-removable fiberglass off-bearing cast versus a therapeutic shoe in the treatment of neuropathic foot ulcers: a randomized study. Diabetes Care 2000;23(12):1746–1751. [DOI] [PubMed] [Google Scholar]
- 65.Mueller MJ, Diamond JE, Sinacore DR, et al. Total contact casting in treatment of diabetic plantar ulcers. Controlled clinical trial. Diabetes Care 1989;12(6):384–388. [DOI] [PubMed] [Google Scholar]
- 66.Hastings MK, Mueller MJ, Sinacore DR, et al. Botulinum toxin effects on gasatrocnemius strength and plantar pressure in diabetics with peripheral neuropathy and forefoot ulceration. Foot Ankle Int 2012;33(5):363–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nubé VL, Molyneaux L, Bolton T, Clingan T, Palmer E, Yue DK. The use of felt deflective padding in the management of plantar hallux and forefoot ulcers in patients with diabetes. The Foot 2006;16(1): 38–43. [Google Scholar]
- 68.Zimny S, Schatz H, Pfohl U. The effects of applied felted foam on wound healing and healing times in the therapy of neuropathic diabetic foot ulcers. Diabet Med 2003;20(8):622–625. [DOI] [PubMed] [Google Scholar]
- 69.Wang Y, Zhou J, Yan F, et al. Comparison of arthrodesis with total contact casting for midfoot ulcerations associated with charcot neuroarthropathy. Med Sci Monit 2015;21:2141–2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Maluf KS, Mueller MJ, Strube MJ, Engsberg JR, Johnson JE. Tendon Achilles lengthening for the treatment of neuropathic ulcers causes a temporary reduction in forefoot pressure associated with changes in plantar flexor power rather than ankle motion during gait. J Biomech 2004;37(6):897–906. [DOI] [PubMed] [Google Scholar]
- 71.Mueller MJ, Sinacore DR, Hastings MK, Strube MJ, Johnson JE. Effect of Achilles tendon lengthening on neuropathic plantar ulcers: a randomized clinical trial. J Bone Joint Surg Am 2003;85-A(8):1436–1445. [PubMed] [Google Scholar]
- 72.Piaggesi A, Schipani E, Campi F, et al. Conservative surgical approach versus non-surgical management for diabetic neuropathic foot ulcers: a randomized trial. Diabet Med 1998;15(5):412–417. [DOI] [PubMed] [Google Scholar]
- 73.Strakhova GY, Gorokhov SV, Ulyanova IN, Galstyan GR. Clinical efficacy and safety of a new method for pressure off-load for patients with diabetic foot syndrome: ankle-foot pneumoorthosis with TM Orlett. Diabetes Mellitus 2014;17(4):66–71. [Google Scholar]
- 74.Agas CM, Bui TD, Driver VR, Gordon IL. Effect of window casts on healing rates of diabetic foot ulcers. J Wound Care 2006;15(2): 80–83. [DOI] [PubMed] [Google Scholar]
- 75.Udovichenko O, Galstyan G. Efficacy of removable casts in difficult to off-load diabetic foot ulcers: a comparative study. Diabetic Foot Journal 2006;9(4):204–208. [Google Scholar]
- 76.Ha Van G, Siney H, Hartmann-Heurtier A, Jacqueminet S, Greau F, Grimaldi A. Nonremovable, windowed, fiberglass cast boot in the treatment of diabetic plantar ulcers: efficacy, safety, and compliance. Diabetes Care 2003;26(10):2848–2852. [DOI] [PubMed] [Google Scholar]
- 77.Birke JA, Pavich MA, Patout CA Jr, Horswell R. Comparison of forefoot ulcer healing using alternative off-loading methods in patients with diabetes mellitus. Adv Skin Wound Care 2002;15(5):210–215. [DOI] [PubMed] [Google Scholar]
- 78.Black JR. Management of diabetic plantar ulcers with a walking brace. A clinical trial. J Am Podiatr Med Assoc 1990;80(3):156–157. [DOI] [PubMed] [Google Scholar]
- 79.Viswanathan V, Madhavan S, Gnanasundaram S, et al. Effectiveness of different types of footwear insoles for the diabetic neuropathic foot: a follow-up study. Diabetes Care 2004;27(2):474–477. [DOI] [PubMed] [Google Scholar]
- 80.Kalantar Motamedi A, Ansari M. Comparison of metatarsal head resection versus conservative care in treatment of neuropathic diabetic foot ulcers. J Foot Ankle Surg 2017;56(3):428–433. [DOI] [PubMed] [Google Scholar]
- 81.Vanlerberghe B, Devemy F, Duhamel A, Guerreschi P, Torabi D. Conservative surgical treatment for diabetic foot ulcers under the metatarsal heads. A retrospective case-control study. Ann Chir Plast Esthet 2014;59(3):161–169. [DOI] [PubMed] [Google Scholar]
- 82.Armstrong DG, Fiorito JL, Leykum BJ, Mills JL. Clinical efficacy of the pan metatarsal head resection as a curative procedure in patients with diabetes mellitus and neuropathic forefoot wounds. Foot Ankle Spec 2012;5(4):235–240. [DOI] [PubMed] [Google Scholar]
- 83.Armstrong DG, Rosales MA, Gashi A. Efficacy of fifth metatarsal head resection for treatment of chronic diabetic foot ulceration. J Am Podiatr Med Assoc 2005;95(4):353–356. [DOI] [PubMed] [Google Scholar]
- 84.Armstrong DG, Lavery LA, Vazquez JR, et al. Clinical efficacy of the first metatarsophalangeal joint arthroplasty as a curative procedure for hallux interphalangeal joint wounds in patients with diabetes. Diabetes Care 2003;26(12):3284–3287. [DOI] [PubMed] [Google Scholar]
- 85.Lin SS, Bono CM, Lee TH. Total contact casting and Keller arthoplasty for diabetic great toe ulceration under the interphalangeal joint. Foot Ankle Int 2000;21(7):588–593. [DOI] [PubMed] [Google Scholar]
- 86.Engels G, Stinus H, Hochlenert D, Klein A. Concept of plantarization for toe correction in diabetic foot syndrome. Operative Orthopadie Und Traumatologie 2016;28(5):323–334. [DOI] [PubMed] [Google Scholar]
- 87.Tamir E, Vigler M, Avisar E, Finestone AS. Percutaneous tenotomy for the treatment of diabetic toe ulcers. Foot Ankle Int 2014;35(1): 38–43. [DOI] [PubMed] [Google Scholar]
- 88.Rasmussen A, Bjerre-Christensen U, Almdal TP, Holstein P. Percutaneous flexor tenotomy for preventing and treating toe ulcers in people with diabetes mellitus. J Tissue Viability 2013;22(3):68–73. [DOI] [PubMed] [Google Scholar]
- 89.van Netten JJ, Bril A, van Baal JG. The effect of flexor tenotomy on healing and prevention of neuropathic diabetic foot ulcers on the distal end of the toe. J Foot Ankle Res 2013;6(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kearney TP, Hunt NA, Lavery LA. Safety and effectiveness of flexor tenotomies to heal toe ulcers in persons with diabetes. Diabetes Res Clin Pract 2010;89(3):224–226. [DOI] [PubMed] [Google Scholar]
- 91.Schepers T, Berendsen HA, Oei IH, Koning J. Functional outcome and patient satisfaction after flexor tenotomy for plantar ulcers of the toes. J Foot Ankle Surg 2010;49(2):119–122. [DOI] [PubMed] [Google Scholar]
- 92.Tamir E, McLaren AM, Gadgil A, Daniels TR. Outpatient percutaneous flexor tenotomies for management of diabetic claw toe deformities with ulcers: a preliminary report. Can J Surg 2008;51(1): 41–44. [PMC free article] [PubMed] [Google Scholar]
- 93.Laborde JM. Neuropathic toe ulcers treated with toe flexor tenotomies. Foot Ankle Int 2007;28(11):1160–1164. [DOI] [PubMed] [Google Scholar]
- 94.Nabuurs-Franssen MH, Sleegers R, Huijberts MS, et al. Total contact casting of the diabetic foot in daily practice: a prospective follow-up study. Diabetes Care 2005;28(2):243–247. [DOI] [PubMed] [Google Scholar]
- 95.Götz J, Lange M, Dullien S, et al. Off-loading strategies in diabetic foot syndrome–evaluation of different devices. Int Orthop 2017;41 (2):239–246. [DOI] [PubMed] [Google Scholar]
- 96.Armstrong DG, Stacpoole-Shea S. Total contact casts and removable cast walkers. Mitigation of plantar heel pressure. J Am Podiatr Med Assoc 1999;89(1):50–53. [DOI] [PubMed] [Google Scholar]
- 97.Fleischli JG, Lavery LA, Vela SA, Ashry H, Lavery DC. 1997William J. Stickel bronze award. Comparison of strategies for reducing pressure at the site of neuropathic ulcers. J Am Podiatr Med Assoc 1997; 87(10):466–472. [DOI] [PubMed] [Google Scholar]
- 98.Lavery LA, Vela SA, Lavery DC, Quebedeaux TL. Reducing dynamic foot pressures in high-risk diabetic subjects with foot ulcerations: a comparison of treatments. Diabetes Care 1996;19(8):818–821. [DOI] [PubMed] [Google Scholar]
- 99.Crews RT, Sayeed F, Najafi B. Impact of strut height on offloading capacity of removable cast walkers. Clin Biomech (Bristol, Avon) 2012;27(7):725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nagel A, Rosenbaum D. Vacuum cushioned removable cast walkers reduce foot loading in patients with diabetes mellitus. Gait Posture 2009;30(1):11–15. [DOI] [PubMed] [Google Scholar]
- 101.Bus SA, Maas JC, Otterman NM. Lower-extremity dynamics of walking in neuropathic diabetic patients who wear a forefoot-offloading shoe. Clin Biomech (Bristol, Avon) 2017;50:21–26. [DOI] [PubMed] [Google Scholar]
- 102.Raspovic A, Landorf KB, Gazarek J, Stark M. Reduction of peak plantar pressure in people with diabetes-related peripheral neuropathy: an evaluation of the DH pressure relief shoe. J Foot Ankle Res 2012; 5(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bus SA, van Deursen RWM, Kanade RV, et al. Plantar pressure relief in the diabetic foot using forefoot offloading shoes. Gait Posture 2009;29(4):618–622. [DOI] [PubMed] [Google Scholar]
- 104.Bus SA, Waaijman R, Arts M, Manning H. The efficacy of a removable vacuum-cushioned cast replacement system in reducing plantar forefoot pressures in diabetic patients. Clin Biomech (Bristol, Avon) 2009;24(5):459–464. [DOI] [PubMed] [Google Scholar]
- 105.Nouman M, Leelasamran W, Chatpun S. Effectiveness of total contact orthosis for plantar pressure redistribution in neuropathic diabetic patients during different walking activities. Foot Ankle Int 2017;38(8):901–908. [DOI] [PubMed] [Google Scholar]
- 106.Lin TL, Sheen HM, Chung CT, et al. The effect of removing plugs and adding arch support to foam based insoles on plantar pressures in people with diabetic peripheral neuropathy. J Foot Ankle Res 2013;6(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kavros SJ, Van Straaten MG, Coleman Wood KA, Kaufman KR. Forefoot plantar pressure reduction of off-the-shelf rocker bottom provisional footwear. Clin Biomech (Bristol, Avon) 2011;26(7): 778–782. [DOI] [PubMed] [Google Scholar]
- 108.Guldemond NA, Leffers P, Schaper NC, et al. The effects of insole configurations on forefoot plantar pressure and walking convenience in diabetic patients with neuropathic feet. Clin Biomech (Bristol, Avon) 2007;22(1):81–87. [DOI] [PubMed] [Google Scholar]
- 109.Praet SF, Louwerens JW. The influence of shoe design on plantar pressures in neuropathic feet. Diabetes Care 2003;26(2):441–445. [DOI] [PubMed] [Google Scholar]
- 110.Raspovic A, Newcombe L, Lloyd J, Dalton E. Effect of customized insoles on vertical plantar pressures in sites of previous neuropathic ulceration in the diabetic foot. The Foot 2000;10(3):133–138. [Google Scholar]
- 111.Lavery LA, Vela SA, Fleischli JG, Armstrong DG, Lavery DC. Reducing plantar pressure in the neuropathic foot: a comparison of footwear. Diabetes Care 1997;20(11):1706–1710. [DOI] [PubMed] [Google Scholar]
- 112.Lavery LA, Vela SA, Lavery DC, Quebedeaux TL. Total contact casts: pressure reduction at ulcer sites and the effect on the contralateral foot. Arch Phys Med Rehabil 1997;78(11):1268–1271. [DOI] [PubMed] [Google Scholar]
- 113.Kato H, Takada T, Kawamura T, Hotta N, Torii S. The reduction and redistribution of plantar pressures using foot orthoses in diabetic patients. Diabetes Res Clin Pract 1996;31(1–3):115–118. [DOI] [PubMed] [Google Scholar]
- 114.Pabón-Carrasco M, Juárez-Jiménez JM, Reina-Bueno M, Coheña-Jiménez M. Behavior of provisional pressure-reducing materials in diabetic foot. J Tissue Viability 2016;25(2):143–149. [DOI] [PubMed] [Google Scholar]
- 115.Holstein P, Lohmann M, Bitsch M, Jorgensen B. Achilles tendon lengthening, the panacea for plantar forefoot ulceration? Diabetes Metab Res Rev 2004;20(Suppl 1):S37–S40. [DOI] [PubMed] [Google Scholar]
- 116.Laborde JM. Neuropathic plantar forefoot ulcers treated with tendon lengthenings. Foot Ankle Int 2008;29(4):378–384. [DOI] [PubMed] [Google Scholar]
- 117.Laborde JM. Midfoot ulcers treated with gastrocnemius-soleus recession. Foot Ankle Int 2009;30(9):842–846. [DOI] [PubMed] [Google Scholar]
- 118.Lee TH, Lin SS, Wapner KL. Tendo-achilles lengthening and total contact casting for plantar forefoot ulceration in diabetic patients with equinus deformity of the ankle. Operative Techniques in Orthopaedics 1996;6(4):222–225. [DOI] [PubMed] [Google Scholar]
- 119.Allam AM. Impact of Achilles tendon lengthening (ATL) on the diabetic plantar forefoot ulceration. Egypt J Plast Reconstr Surg 2006; 30:43–48. [Google Scholar]
- 120.Brodsky JW, Rouse AM. Exostectomy for symptomatic bony prominences in diabetic charcot feet. Clin Orthop Relat Res 1993;296: 21–26. [PubMed] [Google Scholar]
- 121.Catanzariti AR, Mendicino R, Haverstock B. Ostectomy for diabetic neuroarthropathy involving the midfoot. J Foot Ankle Surg 2000;39 (5):291–300. [DOI] [PubMed] [Google Scholar]
- 122.Laurinaviciene R, Kirketerp-Moeller K, Holstein PE. Exostectomy for chronic midfoot plantar ulcer in charcot deformity. J Wound Care 2008;17(2):53–55. 7–8. [DOI] [PubMed] [Google Scholar]
- 123.Rosenblum BI, Giurini JM, Miller LB, Chrzan JS, Habershaw GM. Neuropathic ulcerations plantar to the lateral column in patients with charcot foot deformity: a flexible approach to limb salvage. J Foot Ankle Surg 1997;36(5):360–363. [DOI] [PubMed] [Google Scholar]
- 124.Caravaggi CMF, Sganzaroli AB, Bona F, et al. Square, random fasci-ocutaneous plantar flaps for treating noninfected diabetic plantar ulcers: a patient series. Journal of Foot and Ankle Surgery 2016;55(5): 1100–1105. [DOI] [PubMed] [Google Scholar]
- 125.Sato T, Yana Y, Ichioka S. Free flap reconstruction for diabetic foot limb salvage. J Plast Surg Hand Surg 2017;51(6):399–404. [DOI] [PubMed] [Google Scholar]
- 126.Caputo WJ, Fahoury G, Johnson ES. Resurrection of the Achilles tenotomy. Surg Technol Int 2012;22:66–69. [PubMed] [Google Scholar]
- 127.Dayer R, Assal M. Chronic diabetic ulcers under the first metatarsal head treated by staged tendon balancing: a prospective cohort study. J Bone Joint Surg Br 2009;91(4):487–493. [DOI] [PubMed] [Google Scholar]
- 128.Kim JY, Lee I, Seo K, Jung W, Kim B. FHL tendon transfer in diabetics for treatment of non-healing plantar heel ulcers. Foot Ankle Int 2010;31(6):480–485. [DOI] [PubMed] [Google Scholar]
- 129.Kim JY, Hwang S, Lee Y. Selective plantar fascia release for non-healing diabetic plantar ulcerations. J Bone Joint Surg Am 2012;94 (14):1297–1302. [DOI] [PubMed] [Google Scholar]
- 130.Perez ML, Wagner SS, Yun J. Subtotal calcanectomy for chronic heel ulceration. J Foot Ankle Surg 1994;33(6):572–579. [PubMed] [Google Scholar]
- 131.Smith WJ, Jacobs RL, Fuchs MD. Salvage of the diabetic foot with exposed os calcis. Clin Orthop Relat Res. 1993;296:71–77. [PubMed] [Google Scholar]
- 132.Akkurt MO, Demirkale I, Oznur A. Partial calcanectomy and Ilizarov external fixation may reduce amputation need in severe diabetic calcaneal ulcers. Diabet Foot Ankle 2017;8(1):1264699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Early JS, Hansen ST. Surgical reconstruction of the diabetic foot: a salvage approach for midfoot collapse. Foot Ankle Int 1996;17(6): 325–330. [DOI] [PubMed] [Google Scholar]
- 134.Cooper PS. Application of external fixators for management of charcot deformities of the foot and ankle. Semin Vasc Surg 2003;16(1): 67–78. [DOI] [PubMed] [Google Scholar]
- 135.Farber DC, Juliano PJ, Cavanagh PR, Ulbrecht J, Caputo G. Single stage correction with external fixation of the ulcerated foot in individuals with charcot neuroarthropathy. Foot Ankle Int 2002;23(2): 130–134. [DOI] [PubMed] [Google Scholar]
- 136.Illgner U, Budny T, Frohne I, Osada N, Siewe J, Wetz HH. Clinical benefit and improvement of activity level after reconstruction surgery of charcot feet using external fixation: 24-months results of 292 feet. BMC Musculoskelet Disord 2014;15:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hamilton GA, Ford LA, Perez H, Rush SM. Salvage of the neuropathic foot by using bone resection and tendon balancing: a retrospective review of 10 patients. J Foot Ankle Surg 2005;44(1): 37–43. [DOI] [PubMed] [Google Scholar]
- 138.Boffeli TJ, Smith SR, Abben KW. Complete fifth Ray amputation with peroneal tendon transfer to the cuboid: a review of consecutive cases involving lateral column neuropathic foot ulceration and osteomyelitis. J Foot Ankle Surg 2016;55(6): 1148–1157. [DOI] [PubMed] [Google Scholar]
- 139.Burns J, Begg L. Optimizing the offloading properties of the total contact cast for plantar foot ulceration. Diabet Med 2011;28(2): 179–185. [DOI] [PubMed] [Google Scholar]
- 140.Piaggesi A, Romanelli M, Fallani E, Baccetti F, Navalesi R. Polyurethane foam sheets for relieving pressure from diabetic neuropathic plantar ulcers: a pilot study. Journal of Dermatological Treatment 2000;11(1):39–42. [Google Scholar]
- 141.De Leon Rodriguez D, Allet L, Golay A, et al. Biofeedback can reduce foot pressure to a safe level and without causing new at-risk zones in patients with diabetes and peripheral neuropathy. Diabetes Metab Res Rev 2013;29(2):139–144. [DOI] [PubMed] [Google Scholar]
- 142.Pataky Z, de Leon Rodriguez D, Allet L, et al. Biofeedback for foot offloading in diabetic patients with peripheral neuropathy. Diabet Med 2010;27(1):61–64. [DOI] [PubMed] [Google Scholar]
- 143.Patel VG, Wieman TJ. Effect of metatarsal head resection for diabetic foot ulcers on the dynamic plantar pressure distribution. Am J Surg 1994;167(3):297–301. [DOI] [PubMed] [Google Scholar]
- 144.Armstrong DG, Lavery LA, Kimbriel HR, Nixon BP, Boulton AJM. Activity patterns of patients with diabetic foot ulceration: patients with active ulceration may not adhere to a standard pressure off-loading regimen. Diabetes Care 2003;26(9):2595–2597. [DOI] [PubMed] [Google Scholar]
- 145.Wu SC, Jensen JL, Weber AK, Robinson DE, Armstrong DG. Use of pressure offloading devices in diabetic foot ulcers: do we practice what we preach? Diabetes Care 2008;31(11):2118–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Raspovic A, Landorf K. A survey of offloading practices for diabetes-related plantar neuropathic foot ulcers. Journal of Foot and Ankle Research 2014;7(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Quinton T, Lazzarini P, Boyle F, Russell A, Armstrong D. How do Australian podiatrists manage patients with diabetes? The Australian diabetic foot management survey. Journal of Foot and Ankle Research 2015;8(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Prompers L, Huijberts M, Apelqvist J, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007;50(1):18–25. [DOI] [PubMed] [Google Scholar]
- 149.Bus SA, Waaijman R, Arts M, et al. Effect of custom-made footwear on foot ulcer recurrence in diabetes: a multicenter randomized controlled trial. Diabetes Care 2013;36(12):4109–4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR. Prevention of recurrent foot ulcers with plantar pressure–based in-shoe Orthoses: the CareFUL prevention multicenter randomized controlled trial. Diabetes Care 2014;37(7):1982–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


