Abstract
BACKGROUND/OBJECTIVES:
The majority of end-of-life (EOL) caregiving is provided by unpaid family members. An increasing number of older adults are kinless (without close family/partnerships) and may have insufficient caregiver support to remain at home at the EOL. We therefore determined what proportion of older adults are kinless at the EOL and assessed the association of kinlessness with EOL care.
DESIGN:
Retrospective analysis of Health and Retirement Study decedents, 2002-2015.
SETTING:
US population-based sample.
PARTICIPANTS:
Decedents age 51+ who died within 1 year of interview (n=3,844) and subset who are community-dwelling at last interview.
MEASUREMENTS:
Kinlessness was defined as lacking a spouse/partner and children. Primary outcome measure was location of death. Secondary outcome measures included contextual EOL measures such as: symptom burden and caregiver support.
RESULTS:
7.4% of decedents were kinless at the EOL. Kinless decedents were more likely to be female, non-white, enrolled in Medicaid, living alone, or living in a nursing home prior to death. Although community-dwelling kinless decedents received fewer hours of caregiving per week at the EOL (34.7 vs 56.2, p<0.05) and were more likely to die in nursing homes (18.1% vs 10.3%, p<0.05) than those with kin, they did not have higher EOL symptom burden or treatment intensity (e.g., ICU use). In multinomial logistic analysis controlling for demographic and illness characteristics, kinless decedents living in the community before death had a two-fold increased risk of dying in the nursing home (OR=2.02[95% CI=1.09-3.72]) and a trend toward increased risk of hospital death (OR=1.60[95% CI=0.96-2.69]) vs. home setting.
CONCLUSIONS:
Kinless individuals are more likely to die in nursing homes, even if they are living in the community in their last year of life. Expanded long-term care services and policies are needed to enable all older adults regardless of their family support systems to receive high-quality EOL care.
Keywords: end of life, kinlessness, caregiving, location of death, families
Introduction
As Americans increasingly die at home, the vast majority are supported by unpaid family and friend caregivers, typically spouses or daughters.1,2 On average, end-of-life (EOL) caregivers provide 40-60 hours of care per week, with as many as 84.4% providing daily assistance.1–3 Caregivers at the EOL report helping with a range of tasks, from tending to patient personal care needs to navigating health system logistics and coordinating medical care.1
There is a growing population of older adults who are kinless, or lacking traditional family relationships such as a spouse and/or a child.4–7 Margolis and Verdery have estimated rates of kinlessness to be as high as 7% among US adults 55+ and 11% in Canada, Ireland, the Netherlands, and Switzerland.8,9 These rates are projected to increase in accordance with changing family structures, including modern shifts in preferences about family formation (e.g., families and individuals without children) and partnership (e.g., unmarried families and individuals) that are reflected in declining rates of marriage and fertility and increasing divorce among older adults.10 Although the divorce rate for the US population has been declining since 1980, the divorce rate for those aged 50 and older nearly doubled from 1990 and 202010,11 while rates of childlessness for the US population also doubled from 1980 to 2000.10 By 2060, there are expected to be approximately 21.1 million adults in the US who do not have a spouse or child.12 These numbers reflect marked changes in family structure over the last 20-30 years that will shape EOL support options for current and future generations of older adults.
While the EOL experience of kinless older adults has not been directly studied, prior work has shown that availability of family caregivers can meaningfully affect EOL care. For instance, individuals without a partner have increased risk of admission to long-term care facilities, and patients with terminal cancer who receive 40+ hours of unpaid care per week are twice as likely to receive hospice care at the EOL compared to patients receiving <6 hours of unpaid care.3,13 While some kinless older adults may compensate for having less close family support with paid assistance, this is not common. Only 20% of older adults at the EOL utilize paid care, indicating that informal sources (other family or perhaps friends) or no supplemental caregiving sources are more common in this group.1,3
Kinlessness may be of critical importance relative to EOL treatment intensity and overall quality of care. Repeat hospitalizations in the last months of life and hospital death are commonly used surrogate measures for high intensity EOL care.14,15 Patients who die in hospitals report worse quality of life characterized by more physical, emotional, and psychological distress compared to individuals who die at home with or without hospice.16,17 These outcomes are reflected in more Americans preferring to die at home and increasing rates of hospice deaths.16,18 However, many Americans still die in institutional settings, with about 30% occurring in inpatient hospital settings.19,20
Despite mounting evidence of disparities in the quality of care at the EOL, including glaring racial and socioeconomic inequity,21 there is surprisingly little research on how being kinless impacts treatment intensity at the EOL. We hypothesize that without the availability of kin to support and advocate for them, older adults without kin will experience worse quality of care at the EOL. Therefore, we aim to characterize the population of kinless decedents and compare EOL experiences among those with and without kin at the EOL. We hypothesize that kinless older adults will experience higher intensity treatment at the EOL, especially higher rates of in-hospital death compared to those with kin.
Methods
Data Sources
The study sample is from the Health and Retirement Study (HRS), a nationally representative longitudinal panel study of U.S. adults aged 50 and over.22 HRS conducts biennial core interviews regarding participant health, health service utilization, employment history, economic status, family structure, and decision making. Initial interviews are administered to community-dwelling (i.e., not living in a nursing home) individuals only, though respondents are retained in the HRS study if they move into nursing homes after their baseline interview. Re-interview rates are between 80-90%. Each survey year HRS identifies participants who have died since their last core interview and collects information pertaining to respondents’ health and experiences between their last core interview and death through posthumous “exit” interviews. Exit interviews are completed by a proxy who is knowledgeable about the deceased participant, usually next-of-kin. To identify decedents, survey data were linked to the National Death Index. Participants’ kin were ascertained from the RAND family data file. Finally, for eligible participants, linked Medicare claims data were used to assess hospice utilization. These participants provided informed consent upon enrollment in HRS and linkage to Medicare claims.
Sample
Eligible HRS participants were aged 51 years and older who died between 2002 and 2015 (n= 9307). We restricted the sample to individuals at the EOL (defined as participants who expired within one year of their last core HRS interview as previously described2) with sample weights >0 (n=3844). Analyses examining EOL outcomes were further restricted to participants who had a posthumous exit interview completed by a proxy (n= 3,722). Core interview data came from the last core interview preceding death, which occurred on average 6.5 months prior to death. Because individuals without close family live in nursing homes at greater rates than those with kin,13 comparisons of EOL characteristics were conducted on the full sample as well as those who were living in the community at the interview before death (n=2,889).
Measures
a) Kinlessness
Because the vast majority of unpaid caregiving at the EOL is provided by spouses and children,1 we defined kinlessness as not having a spouse (herein defined as married or partnered) or any children (biological, step-children, and in-laws’ children). Survey respondents’ kin status was extrapolated from RAND family and HRS core interview files from the year preceding participants’ death. Additionally, we included HRS respondents whose proxies self-identified as spouses and children on exit interviews regardless of respondent report.
b) Primary Outcome
Our primary outcome was location of death, a commonly used surrogate for high-intensity EOL treatment.23,24 We used survey respondents’ location of death reported by proxies in exit interviews to categorize location of death as in-hospital, nursing home or home. Home death included assisted living or retirement facilities, designated hospice facilities, outside, relatives’ homes, and other. Deaths that occurred in nursing homes were categorized as nursing home deaths regardless of whether hospice was involved.
c) Other Measures
The majority of measures were derived from the last HRS core interview completed by the respondent prior to death. These included: age, sex, race, educational attainment, net worth, Medicaid enrollment, living arrangements, religiosity, self-rated health, activities of daily living (ADLs), comorbidities, dementia (as determined by self-report and cognitive testing), and social visits. Net worth income quartiles were derived from adjusting the net worth variable to 2012 dollars using the Consumer Price Index for medical services across all years. Comorbidities were reported as a count, corresponding to the following categorization: none (0), mild (1-3), and moderate/severe (≥4). Measures of caregiving (utilization of paid help, total helpers, and hours of help) were also drawn from the core interview prior to death.
Measures describing EOL symptoms and care were derived from the HRS exit interview completed by a proxy after the respondent’s death. Proxies were asked about symptoms the respondent experienced in the last year of life, including: diminished appetite, depression, confusion, and vomiting. Additional EOL measures included treatments received (intensive care unit admission, life support such as using a respirator), length of terminal illness (> 1 year), and advance care planning (health care proxy, discussion of end of life preferences, advance directive). Finally, hospice use was defined as >=1 day and was extracted from individual Medicare claims data for respondents enrolled in Medicare and exit interviews for those who were not.
Analysis
We first estimated the proportion of decedents that had no spouse, no children, and no children or spouse (kinlessness) by sex and determined corresponding population estimates. We then used χ2 and t-tests in bivariate comparisons to characterize the socioeconomic and clinical factors associated with kinlessness and to compare the EOL experiences of the kinless to those who have kin. Due to potential differences in caregiving dynamics among those in nursing homes, bivariate comparisons of EOL outcomes by kin status are shown for the full sample (community- and nursing-home dwelling combined) and also the subset of community-dwelling respondents alone. We used a multinomial logistic regression model to predict the odds of dying in the hospital vs. home and in the nursing home vs. home while adjusting for the demographic and health status variables considered in our study. These analyses were conducted for both the entire sample and the subset who were community-dwelling before death after adjusting for participant socioeconomic and clinical characteristics. We excluded caregiving variables from the model as they were hypothesized to be part of the causal pathway by which kinlessness could affect location of death—a complex social relationship process that is beyond the focus of the present paper. All analyses were weighted using HRS survey weights to account for survey design, sampling approach, and differential non-response rates. Stata 15 was used for all statistical analyses (StataCorp LP, College Station TX). The study was approved by the Icahn School of Medicine at Mount Sinai’s Institutional Review Board (IRB), the HRS Data Confidentiality Committee, and the Centers for Medicare & Medicaid Services Privacy Board.
Results
Kinlessness at End of Life:
Among decedents, 7.4% (weighted proportion) were kinless at the EOL, without spouse or children, representing 999,093 older Americans (Table 1). Women tended to experience kinlessness at higher rates than men (8.3% vs 6.4%). The majority (74.4%) of women did not have a spouse at EOL, compared to only 41.9% of men (p<0.001, Figure 1).
Table 1:
Demographic and clinical characteristics of decedents by kin status
| Kinless (N=247) | Has Kin (N=3,597) | P-value | |
|---|---|---|---|
| Population estimate | 999,093 | 12,551,949 | |
| Demographic characteristics, % | |||
| Age (mean (SD)) | 78.23 (12.24) | 78.65(11.09) | 0.68 |
| Female | 58.7% | 51.5% | 0.16 |
| White, non-Hispanic | 72.8% | 81.8% | <0.001 |
| Married | 0 | 44.6% | <0.001 |
| Less than high school education | 32.0% | 31.4% | 0.86 |
| Lowest quartile of net worth | 55.2% | 35.8% | <0.001 |
| Enrolled in Medicaid | 30.5% | 21.5% | 0.01 |
| Lives alone | 32.5% | 16.8% | <0.001 |
| Residing in a nursing home | 30.1% | 18.6% | <0.001 |
| Religion rated as not important | 16.7% | 14.2% | 0.38 |
| <1 social visit/week | 42.0% | 55.5% | <0.001 |
| Health and function characteristics, % | |||
| Excellent/very good/good self-reported health | 37.7% | 32.8% | 0.16 |
| Number of ADL impairments: | |||
| 0 | 61.0% | 54.7% | 0.09 |
| 1-2 | 12.1% | 17.2% | |
| 3+ | 27.0% | 28.1% | |
| Number of comorbidities (mean (SD)) | 2.44 (1.49) | 2.81 (1.57) | 0.01 |
| 1+ IADL impairment | 57.0% | 54.9% | 0. 60 |
| Probable dementia | 41.7% | 38.3% | 0.43 |
Data source: Health and Retirement Study, 2002-2015. Estimates adjusted for survey design, sampling approach, and non-response. Kin is defined as having a spouse/partner or child of any type. Abbreviations: HS, high school; NH, nursing home; SR, self-rated; ADL, activities of daily living (includes: eating, dressing, bathing, toileting, walking, transferring); IADL, independent activity of daily living (includes: help with meal preparation, grocery shopping, making phone calls, medications, and money). Measures derived from the last HRS core interview prior to death.
Figure 1.
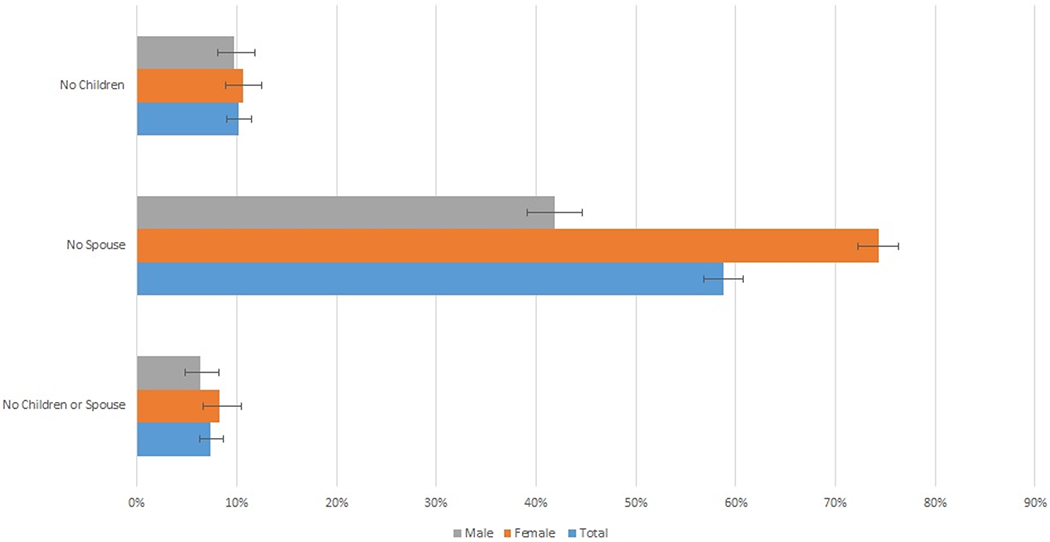
Proportion of adults age 51 and over who lack a spouse and/or children at the end of life Data source: Health and Retirement Study, 2002-2015. Estimates adjusted for survey design, sampling approach, and non-response
Demographics and Health:
Kinless decedents were more likely to be from a racial and ethnic minority group (27.2% vs. 18.2%, p=0.01), from the lowest net-worth quartile (55.2% vs 35.8%, p<0.001), and enrolled in Medicaid (30.5 vs. 21.5%, p=0.01). Almost twice as many kinless individuals lived alone (32.5% vs. 16.8%, p<0.001) and 1.6 times as many resided in a nursing home at their last HRS interview before death (30.1% vs. 18.6%, p<0.001). Individuals without kin harbored fewer comorbidities (index score of 2.4 vs. 2.8, p=0.01) and were less likely to report <1 social visit/week (40.0% vs. 55.5%, p<0.001). There were no differences in kinless status by age, education, self-rated health, number of ADLs, or dementia status.
End of Life Care Characteristics:
In bivariate analyses comparing location of death by kin status we did not observe that individuals who are kinless at EOL were more likely to die in the hospital (Table 2, 36.5% vs. 36.8%, p=0.96). However, more kinless decedents who had been living in the community prior to death ultimately died in a nursing home (18.1% vs. 10.3%, p=0.01). Among the full sample, kinless decedents were similarly more likely to die in nursing homes (Table 2, 31.9% vs. 20.3%, p<0.01). Kinless decedents were less likely to die in their homes or hospice facilities than decedents with kin (Table 2, 35.3% vs. 45.6%, p=0.02). This trend persisted in our analysis of the community-dwelling, although it did not achieve statistical significance (53.0% vs. 45.4%, p=0.18). There were no major differences in hospice use or treatment intensity, including ICU admissions or receipt of life support during the end of life. Discussions of EOL preferences were less common among individuals without kin (50.0% vs. 58.3%, p=0.04; Table 2), but other measures of advance care planning did not differ. There were minimal reported differences in symptomatology or duration of final illness.
Table 2:
End-of-life characteristics of older decedents by kin status
| Community-dwelling | Full sample | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Kinless N=140 |
Has Kin N=2,749 |
P-value | Kinless N=233 |
Has Kin N=3,489 |
P-value | |
| Place of Death: | ||||||
| Hospital | 36.5 | 36.8 | 0.96 | 32.8 | 34.1 | 0.74 |
| Nursing Home | 18.1 | 10.3 | 0.01 | 31.9 | 20.30 | <0.001 |
| Home3 | 45.4 | 53.0 | 0.18 | 35.3 | 45.59 | 0.02 |
| Intensive care unit admission | 30.7 | 37.6 | 0.25 | 28.6 | 34.82 | 0.14 |
| Life support | 20.8 | 24.2 | 0.44 | 17.4 | 22.19 | 0.17 |
| Hospice enrollment2 | 29.2 | 38.7 | 0.15 | 34.5 | 40.55 | 0.23 |
| Engagement in advance care planning: | ||||||
| Discussion of care preferences1 | 45.8 | 59.6 | 0.02 | 50.0 | 58.34 | 0.04 |
| Advance directive | 65.3 | 65.3 | 0.99 | 68.8 | 67.68 | 0.75 |
| Health care proxy | 59.2 | 57.7 | 0.75 | 62.4 | 60.51 | 0.60 |
| Symptoms in the last year of life: | ||||||
| Very little appetite | 59.9 | 63.4 | 0.53 | 62.8 | 64.72 | 0.66 |
| Frequent vomiting | 10.2 | 11.0 | 0.84 | 8.5 | 10.30 | 0.55 |
| Periodic confusion | 34.1 | 41.7 | 0.11 | 45.5 | 48.37 | 0.44 |
| Depression | 41.3 | 49.8 | 0.09 | 42.7 | 51.20 | 0.01 |
| Duration of final illness: >1 year | 18.3 | 22.9 | 0.42 | 21.6 | 23.11 | 0.68 |
| Any paid helpers | 13.4 | 9.2 | 0.15 | 10.5 | 8.12 | 0.29 |
| Total number of helpers: 1 | ||||||
| 0 | 59.0 | 49.2 | 0.06 | 43.0 | 41.00 | 0.29 |
| 1 | 13.6 | 23.1 | 17.3 | 22.6 | ||
| ≥2 | 27.4 | 27.8 | 39.7 | 36.4 | ||
| Total hours/week of help, mean (SD) | 34.7 (58.5) | 56.2 (74.9) | 0.02 | 18.7 (44.5) | 42.1 (67.6) | <0.001 |
Data source: Health and Retirement Study, 2002-2015. Estimates adjusted for survey design, sampling approach, and non-response. Data are given as percentage unless otherwise indicated. Estimates adjusted for survey weights. Kin is defined as having a spouse/partner or child of any type. SD= standard deviation. Paid helpers excludes institutional employees. Total hours of help per week includes paid and unpaid help. All variables derived from exit interview unless otherwise indicated.
Helper data are ascertained from last HRS interview prior todeath.
Hospice variable derived from a combination of Medicare claims (if present) or exit interview if no claims data were present.
Includes assisted living, retirement community, and residential hospice.
A small percentage of individuals utilized paid help at the EOL, and kinless decedents were not more likely to use paid help than those with kin (13.4% vs. 9.2%, p=0.15). While there were no differences in the total number of helpers (paid or unpaid) assisting at EOL, community-dwelling decedents with kin received 1.6 times as many hours of care per week (56.2 hours vs. 34.7 hours, p=0.02). This discrepancy was more pronounced among the full sample with decedents who had kin receiving 2.2 times as many hours of care per week (Table 2, 42.1 hours vs. 18.7 hours, p<0.001).
In multinomial logistic analysis controlling for demographic and illness characteristics, kinless decedents living in the community before death had a two-fold increased risk of dying in the nursing home vs home setting (OR=2.02 [95% CI=1.09-3.72]) and tended to have an increased, but not statistically significant risk of hospital vs home death (OR=1.60 [95% CI=0.96-2.69]). Similarly, among the full sample, the kinless tended to have a greater risk of hospital death (OR=1.62 [95% CI=1.00-2.63]) and were twice as likely to die in nursing homes than the home setting (OR=2.23 [95% CI=1.29-3.85]) (Table 3).
Table 3:
Multinomial logistic model examining kinlessness and location of death
| Community-dwelling sample (N=2,444) | Full sample (N=3,148) | |||
|---|---|---|---|---|
| Hospital vs Home OR [95% CI] |
Nursing Home vs. Home OR [95% CI] |
Hospital vs Home OR [95% CI] |
Nursing Home vs. Home OR [95% CI] |
|
| Kinless | 1.60[0.96-2.69] | 2.02 [1.09-3.72]* | 1.62 [1.00-2.63] | 2.23 [1.29-3.85]** |
| Age | 0.99 [0.98-1.00] | 1.03[1.01-1.04]** | 0.99 [0.98-1.00] | 1.02 [1.01-1.04]** |
| Female | 0.87 [0.73-1.04] | 0.96 [0.71-1.30] | 0.91 [0.76-1.10] | 1.03 [0.82-1.29] |
| White, non-Hispanic | 0.91 [0.75-1.11] | 1.52 [1.09-2.13]* | 0.99 [0.81-1.20] | 2.30 [1.76-3.00]** |
| Less than HS Education | 1.01 [0.83-1.23] | 0.93 [0.65-1.34] | 1.01 [0.84-1.22] | 0.85 [0.65-1.11] |
| Lowest quartile of net worth | 1.03 [0.81-1.30] | 1.71 [1.24-2.35]** | 1.15 [0.92-1.45] | 1.78 [1.36-2.38]** |
| Enrolled in Medicaid | 1.25 [0.90-1.74] | 1.56 [1.00-2.45] | 1.54 [1.13-2.09]** | 2.42 [1.75-3.34]** |
| Number of ADL impairments: | ||||
| 0 | Reference | Reference | Reference | Reference |
| 1-2 | 0.87 [0.67-1.14] | 0.99 [0.66-1.50] | 0.88 [0.69-1.14] | 1.13 [0.83-1.55] |
| 3+ | 0.57 [0.43-0.76]** | 0.75 [0.48-1.16] | 0.70 [0.55-0.90]** | 2.50 [1.78-3.52]** |
| Probable dementia | 0.81 [0.63-1.04] | 1.38 [0.92-2.06] | 0.91 [0.72-1.15] | 1.92 [1.43-2.59]** |
| Number of comorbidities | 1.05 [0.98-1.13] | 0.98 [0.89-1.09] | 1.04 [0.97-1.12] | 0.98 [0.90-1.07] |
p<0.05
p<0.01
Home is the referent category; OR=Odds Ratio; HS= high school; ADL=Activities of Daily Living
Discussion
In a nationally representative sample of decedents, we found that 7.4% of older adults are kinless, or without a spouse or children, at the EOL. Unsurprisingly, kinless decedents differed from those with kin with respect to gender, race, net-worth, Medicaid utilization, and living arrangements at the EOL. The kinless were twice as likely to die in nursing homes as those with kin, even among those who were community-dwelling within one year of their death. While there was a tendency for the kinless to have an increased hospital death in adjusted models, these associations were not statistically significant among those living in the community. We also did not see any evidence of differences in hospice enrollment, symptom management or treatment intensity at the EOL. We do find that the kinless are receiving fewer total hours of care per week (paid and unpaid) at the EOL. Taken together, these findings underscore important differences in EOL experience for kinless decedents and have implications for better supporting our aging population and their caregivers.
Our work contrasts with prior literature that concludes kinless older adults were more likely to be in fair/poor health with more functional disability. Despite growing concern for the kinless as a vulnerable population, in this nationally representative sample, kinless decedents harbored fewer comorbidities than their counterparts with kin. Moreover, fewer kinless individuals report not receiving social visits. These findings portray a higher quality of life and potentially greater social engagement for kinless older adults than is invoked by literature on “elder orphans”, and lend credence to the importance of non-kin based social networks for older adults’ wellbeing.4,25,26 Yet our findings may be due, in part, to a survivor bias if a higher degree of health or an expanded social network is required for kinless older adults to remain in the community at EOL.
While the kinless are more likely to live and die in nursing homes, we do not find strong evidence surrounding the heightened vulnerability of the kinless to higher intensity EOL care and increased symptom burden at the EOL. This is promising given that the provision of care in the home is a priority of current and future long-term and EOL care systems. Not only do the majority of Americans prefer to die in their homes, but care at home is associated with reduced healthcare expenditures relative to hospital settings.27,28 Still, as kinless rates increase, our healthcare system’s reliance on unpaid caregivers at EOL may become unsustainable. Consistent with other research,1 we found very low rates of paid care use at the EOL, and high reliance on family caregivers for support. Expanded long-term care services and policies are needed to enable older adults who do not have traditional kin or available caregivers to receive high-quality EOL care in their homes, if that is consistent with their preferences. The traditionally kinless are composed of more vulnerable sociodemographic subpopulations and we must ensure our systems of care can serve them. Improved access to EOL services for those without family ties will require several policy initiatives including bolstering state Medicaid funding of professional home-health aids and expansion of public long-term community- and home-based medical services while continuing to reduce caregiver burden through expanded protections and paid caregiver leave programs.27–30
There are several limitations to note. It is possible that some of our findings were influenced by measurement bias in that the proxy respondents of kinless decedents were more remote friends and family than that of decedents with kin. In addition, our sample size limited detailed analysis of subpopulations such as those from different racial and ethnic groups. While one strength of our study is that we collect proxy-reported data on information such as symptoms at the EOL, we may not be capturing other elements of quality EOL care that were not surveyed by HRS. For this reason, we focus on location of death, although we notably do not know respondents’ care preferences. Many patients and families may have wanted and indeed benefitted from in-hospital deaths. Finally, while we focus on a traditional measure of kinlessness (no spouse or children), there are likely many non-traditional kin including friends, distant relatives who are also involved in supporting individuals at the EOL. HRS data limit our ability to systematically examine non-traditional kin networks.
In conclusion, we characterized the population who are kinless at the EOL and found that kinless adults are far more likely to experience nursing home deaths than those with more traditional kin, although there is limited evidence of other differences in treatment intensity at the EOL. Expanded long-term care services and policies are needed to better support caregivers and enable all older adults regardless of their family support systems to receive high-quality EOL care.
Key points:
More than seven percent of older adults are kinless (no spouse or children) at the end of life
Kinless older adults living in the community receive less caregiving support and are more likely to die in nursing homes than those with kin
Acknowledgements
Funding:
HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and the Social Security Administration and is conducted by the University of Michigan. The study investigators were supported by the NIA R01AG060967 to Dr. Ornstein, NIA K76AG064437 to Dr. Ankuda, and NIA P30AG028741. Natalie Plick was funded by the Patricia S. Levinson Summer Research Award. Funding sources had no role in the design, conduct, and analysis of this study or in the decision to submit the manuscript for publication. The authors declare no conflicts of interest.
Footnotes
Why does this paper matter? Individuals without family support systems at the end of life may have less access to end of life care.
No conflicts of interest to report
References
- 1.Ornstein KA, Kelley AS, Bollens-Lund E, Wolff JL. A National Profile Of End-Of-Life Caregiving In The United States. Health Aff (Millwood) .2017;36(7):1184–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolff JL, Dy SM, Frick KD, Kasper JD. End-of-life care: findings from a national survey of informal caregivers. Archives of internal medicine .2007;167(1):40–46. [DOI] [PubMed] [Google Scholar]
- 3.Kumar V, Ankuda CK, Aldridge MD, Husain M, Ornstein KA. Family Caregiving at the End of Life and Hospice Use: A National Study of Medicare Beneficiaries. J Am Geriatr Soc .2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carney MT, Fujiwara J, Emmert BE Jr., Liberman TA, Paris B. Elder Orphans Hiding in Plain Sight: A Growing Vulnerable Population. Curr Gerontol Geriatr Res .2016;2016:4723250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cumbler E, Carter J, Kutner J. Failure at the transition of care: challenges in the discharge of the vulnerable elderly patient. Journal of hospital medicine .2008;3(4):349–352. [DOI] [PubMed] [Google Scholar]
- 6.Montayre J, Thaggard S, Carney M. Views on the use of the term ‘elder orphans’: A qualitative study. Health Soc Care Community .2020;28(2):341–346. [DOI] [PubMed] [Google Scholar]
- 7.Montayre J MJ, & Thaggard S. The Elder Orphan in Healthcare Settings: an Integrative Review. Population Ageing . 2018. [Google Scholar]
- 8.Verdery AM, Margolis R, Zhou Z, Chai X, Rittirong J. Kinlessness Around the World. J Gerontol B Psychol Sci Soc Sci .2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Margolis R, Verdery AM. Older Adults Without Close Kin in the United States. J Gerontol B Psychol Sci Soc Sci .2017;72(4):688–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seltzer JA. Family Change and Changing Family Demography. Demography .2019;56(2):405–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allred C Age variation in the divorce rate, 1990 & 2017. Family Profiles .2019(13). [Google Scholar]
- 12.Verdery AM, Margolis R. Projections of white and black older adults without living kin in the United States, 2015 to 2060. Proceedings of the National Academy of Sciences of the United States of America .2017;114(42):11109–11114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomeer MB, Mudrazija S, Angel JL. Relationship Status and Long-Term Care Facility Use in Later Life. The Journals of Gerontology :Series B .2015;71(4):711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang B, Nilsson ME, Prigerson HG. Factors Important to Patients’ Quality of Life at the End of LifeFactors Important to QOL at the End of Life. JAMA Internal Medicine .2012;172(15):1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curtis JR, Patrick DL, Engelberg RA, Norris K, Asp C, Byock I. A measure of the quality of dying and death. Initial validation using after-death interviews with family members. J Pain Symptom Manage .2002;24(1):17–31. [DOI] [PubMed] [Google Scholar]
- 16.Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol .2010;28(29):4457–4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA .2004;291(1):88–93. [DOI] [PubMed] [Google Scholar]
- 18.Luta X, Maessen M, Egger M, Stuck AE, Goodman D, Clough-Gorr KM. Measuring intensity of end of life care: a systematic review. PLoS One .2015;10(4):e0123764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Center for Health S. Health, United States. Health, United States, 2017: With Special Feature on Mortality. Hyattsville (MD): National Center for Health Statistics (US); 2017. [PubMed] [Google Scholar]
- 20.Cross SH, Warraich HJ. Changes in the Place of Death in the United States. New England Journal of Medicine .2019;381(24):2369–2370. [DOI] [PubMed] [Google Scholar]
- 21.Ornstein KA, Roth DL, Huang J, et al. Evaluation of Racial Disparities in Hospice Use and End-of-Life Treatment Intensity in the REGARDS Cohort. JAMA network open .2020;3(8):e2014639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neff DF, Mahama N, Mohar DR, Kinion E. Nursing care delivered at academic community-based nurse-managed center. OutcomesManag .2003;7(2):84–89. [PubMed] [Google Scholar]
- 23.Ornstein KA, Garrido MM, Siu AL, Bollens-Lund E, Langa KM, Kelley AS. Impact of In-Hospital Death on Spending for Bereaved Spouses. Health Serv Res .2018;53Suppl 1:2696–2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ornstein KA, Aldridge MD, Mair CA, Gorges R, Siu AL, Kelley AS. Spousal Characteristics and Older Adults’ Hospice Use: Understanding Disparities in End-of-Life Care. J Palliat Med .2016;19(5):509–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Djundeva M, Dykstra PA, Fokkema T. Is living alone “aging alone”? Solitary living, network types and well-being. J Gerontol B Psychol Sci Soc Sci .2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mair CA. Alternatives to Aging Alone?: “Kinlessness” and the Importance of Friends Across European Contexts. The journals of gerontology Series B, Psychological sciences and social sciences .2019;74(8):1416–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ankuda CK, Leff B, Ritchie CS, et al. Implications of 2020 Skilled Home Healthcare Payment Reform for Persons with Dementia. J Am Geriatr Soc .2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ankuda CK, Meier DE. Predictors of reliably high-value end-of-life care. Curr Opin Support Palliat Care .2018;12(4):460–465. [DOI] [PubMed] [Google Scholar]
- 29.Committee on Family Caregiving for Older A, Board on Health Care S, Health, Medicine D, National Academies of Sciences E, Medicine. In: Schulz R, Eden J, eds. Families Caring for an Aging America. Washington (DC): National Academies Press (US) [PubMed] [Google Scholar]
- 30.Aldridge MD, Ornstein KA, McKendrick K, Moreno J, Reckrey JM, Li L. Trends In Residential Setting And Hospice Use At The End Of Life For Medicare Decedents. Health Aff (Millwood) .2020;39(6):1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]


