Abstract
Introduction
The fatigue-sleep disturbance-depression symptom cluster (FSDSC) is one of the most common and debilitating side effects in patients with breast cancer (BC) throughout their treatment trajectory. Tai chi has been supported as a promising non-pharmacological intervention for the individual symptom relief of cancer-related fatigue, sleep disturbance and depression. However, relevant evidence of using tai chi for FSDSC management in patients with BC has been lacking.
Methods
This study will be a two-arm, single-blinded pilot randomised controlled trial involving an 8-week intervention and a 4-week follow-up. Seventy-two patients with BC experiencing the FSDSC will be recruited from two tertiary medical centres in China. The participants will be randomised to either a tai chi group (n=36) or a control group (n=36). The participants in the tai chi group will receive an 8-week tai chi intervention in addition to standard care, while the participants in the control group will receive standard care only consisting of a booklet on the self-management of cancer symptoms. The primary outcomes will include a series of feasibility assessments of the study protocol in relation to the study’s methodological procedures, including subject recruitment and follow-up process, completion of study questionnaires and the feasibility, acceptability and safety of the intervention. The secondary outcomes will be the clinical outcomes regarding the effects of tai chi on the FSDSC and quality of life, which will be evaluated by the Brief Fatigue Inventory, the Pittsburgh Sleep Quality Index, the Hospital Anxiety and Depression Scale and the Functional Assessment of Cancer Therapy-Breast questionnaires.
Ethics and dissemination
Ethics approval was obtained from relevant sites (H19094, KY2019133, 201932). The findings of the study will be published in peer-reviewed scientific journals and at conferences.
Trail registration number
Keywords: breast tumours, complementary medicine, clinical trials
Strengths and limitations of this study.
This will be the first clinical study to explore the feasibility and preliminary effects of tai chi on the fatigue-sleep disturbance-depression symptom cluster (FSDSC) in patients with breast cancer.
This study will use an evidence-based tai chi protocol in the intervention group which was comprehensively developed based on best available research evidence, guidelines, theories and practice standards.
The design of the pilot study will be guided by the Medical Research Council Framework for Developing and Evaluating Complex Interventions.
This study will use comprehensive outcome measurements, including a series of feasibility outcomes, which will support the refinement of a clinically feasible tai chi protocol for a future full-scale randomised controlled trial.
The sample size of this trial is relatively small and is not power based, which will contribute to only a preliminary analysis of the effects of tai chi on the FSDSC.
Introduction
Breast cancer (BC) is regarded as the most common cancer among women worldwide.1 Although the number of BC survivors is increasing with improved cancer treatment, the substantial negative effects associated with cancer and cancer treatments remain a significant problem for survivors. Following the treatment of surgery, radiation therapy, antihormonal therapy and/or chemotherapy, patients with BC can experience significant side effects, including fatigue, sleep disturbance and depression.2 These frequently reported, troublesome symptoms usually occur concurrently in patients with BC as a symptom cluster.3 4 According to Dodd et al,5 a symptom cluster consists of ‘three or more symptoms that are related to each other’ (p. 468). The fatigue-sleep disturbance-depression symptom cluster (FSDSC) is one of the most frequent symptom clusters among patients with BC, which can negatively impact patients’ physical and psychosocial functioning status and quality of life (QoL), including more severe cancer-related symptoms, lower treatment compliance, poorer emotional conditions, worse financial hardship and even shorter survival time.6–8
To date, no specific medications are available for the management of cancer symptom clusters. Reviewing the previous evidence, various non-pharmacological approaches have been used as a combination treatment with medication for the comprehensive management of cancer-related symptoms.9 10 However, most of the widely employed non-pharmacological approaches, such as acupuncture,11 hypnotherapy,12 guided imagery,13 massage14 and electrical stimulation,15 require intensive professional skills training, supervised practise and specific equipment, all of which can be significantly time-consuming and energy-consuming and can considerably increase the consumption of healthcare resources and costs. Moreover, due to fatigue intolerance, patients with cancer are usually reluctant to participate in energy-consuming non-pharmacological interventions such as intensive exercise.16 Thus, an energy-saving and cost-effective non-pharmacological approach would be more appropriate for FSDSC management in patients.
Traditional Chinese exercise (TCE) could be an appropriate and effective option for FSDSC relief in patients with BC given its low cost and mild-to-moderate intensity. Tai chi, a very popular TCE, consists of several slow, simple and repetitive body movements along with deep breathing, and it is easy to master.17 There has been increasing evidence of its positive effects in targeting the management of individual symptoms such as fatigue, sleep disturbance and depression.18–20 However, no clinical research has ever been performed using tai chi exercise for symptom cluster management, especially the FSDSC in patients with BC. The current study, therefore, proposes to assess the feasibility and the preliminary effects of using an evidence-based tai chi protocol for alleviating the FSDSC in patients with BC through a pilot randomised controlled trial (RCT).
Methods and materials
Study design
The study’s design will be a two-parallel-arm, single-blinded (assessor) pilot RCT. The participants will be randomly allocated into two groups: a tai chi intervention group and a control group, with an allocation ratio of 1:1. The study period will be 12 weeks, which will involve an 8-week tai chi intervention and a 4-week follow-up for the intervention group. A Consolidated Standards of Reporting Trials flow chart of the study is presented in figure 1. The schedule of trial enrolment, intervention data collection and assessments are presented in table 1. This protocol was reported in accordance with the Standard Protocol Items: Recommendations for Interventional Trials Checklist.
Figure 1.
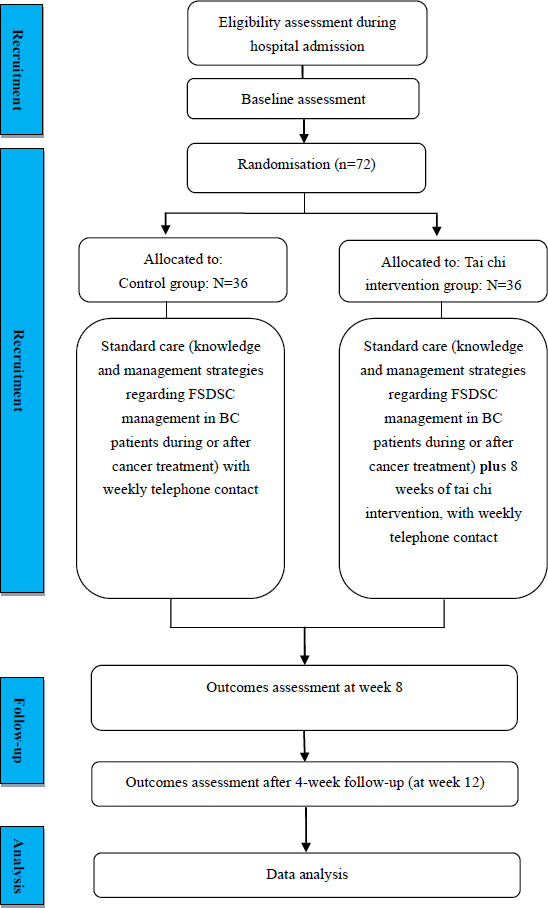
CONSORT flow chart of the study. BC, breast cancer; CONSORT, Consolidated Standards of Reporting Trials; FSDSC, fatigue-sleep disturbance-depression symptom cluster.
Table 1.
The schedule of trial enrolment, interventions and assessments
| Study period | |||||
| Upon enrolment (week 0) |
Intervention period (week 1–8) |
End of intervention (week 8 week) |
Follow-up period (week 9–12) |
End of follow-up (week 12) |
|
| Inclusion/exclusion criteria | ╳ | ||||
| Informed consent | ╳ | ||||
| Demographic characteristics | ╳ | ||||
| Randomisation and allocation | ╳ | ||||
| Feasibility of recruitment and follow-up process | ╳ | ╳ | ╳ | ╳ | |
| Feasibility assessment of the outcome measures | ╳ | ╳ | ╳ | ||
| Feasibility and acceptability of the intervention | ╳ | ||||
| BFI | ╳ | ╳ | ╳ | ||
| HADS | ╳ | ╳ | ╳ | ||
| PSQI | ╳ | ╳ | ╳ | ||
| FACT-B | ╳ | ╳ | ╳ | ||
| Safety measurement | ╳ | ||||
BFI, Brief Fatigue Inventory; FACT-B, Functional Assessment of Cancer Therapy-Breast; HADS, Hospital Anxiety and Depression Scale; PSQI, Pittsburgh Sleep Quality Index.
Study setting
This study will be implemented in two tertiary medical centres in Mainland China, including the Affiliated Hospital of Putian University (Fujian) and the Affiliated Hospital of Southwest Medical University (Sichuan).
Sample size calculation
Thirty or more participants per group are usually recommended as sufficient for a pilot study to examine intervention feasibility21 and to estimate a between-group effect for a subsequent power analysis that can be used in the main study’s sample size estimation.22 Given that the primary purpose of this study will be exploring the feasibility and acceptability of the study’s methodological procedures, intervention protocol and questionnaires, 30 participants per group were, therefore, determined to be an appropriate sample size. Taking into account a conservative anticipation of a 20% drop-out rate, the final sample size will therefore be 36 in each group, with a total of 72 participants.23
Inclusion and exclusion criteria
Eligible participants will be recruited using the following inclusion criteria:
Adult female patients aged over 18 years.
Diagnosed with stage I, II or IIIa BC (non-metastatic BC).
Have experienced at least a moderate level of fatigue, sleep disturbance and depression, with a score of greater than 3 (which means a score of ‘4’ and above) on a 10-point scale, from ‘0 (no symptom)’ to ‘10 (worst symptom)’ for each symptom in the past 1 month.
Have completed BC surgery for over 1 month.
Have recently (within the past 2 months) commenced adjuvant chemotherapy.
Able to speak and understand Mandarin Chinese.
Willing and able to give written informed consent for study participation.
Potential participants will be excluded using the following exclusion criteria:
Presently taking medications for the treatment of fatigue, sleep disturbance or depression, such as antidepressant medications, psychostimulants or hypnotics.
Extremely weak (unable to do physical activities due to advanced stages of chronic illnesses) or have cognitive impairment and/or severe mental illness.
Have participated in a tai chi programme during the previous 6 months.
Have practised other TCE for over 30 min, three times per week, during the previous 3 months.
Have scheduled other elective surgery within the trial period.
Recruitment
A research team will be formed before the commencement of the trial. Three investigators, including the doctoral investigator and two clinical nurses, will be primarily responsible for the subject recruitment and tai chi training. The investigators will receive intensive training from a qualified tai chi instructor to ensure a standardised tai chi practice. Prior to the tai chi intervention, the tai chi instructor will examine the accuracy of the movements among the three researchers, and the accuracy rate should be 100%. Two research assistants will conduct data collection and telephone follow-ups. To ensure the quality of data collection, the two research assistants will be trained on questionnaire data collection skills, including understanding the questionnaire items and standardising their conversations with the participants. The academic supervisors of the doctoral investigator will monitor the entire study procedure on an ongoing basis through regular monthly meetings.
Among the hospitalised patients in the BC unit, potential participants will be recruited directly by the doctoral investigator and the two clinical nurses. Some potential participants who attend a BC clinic for regular follow-ups will be referred by physicians and clinic nurses to the doctoral investigator and the two clinical nurses. A participant information sheet, including the research aim, the procedures and the contact details of the study investigators, will be given to potential participants and will be explained by the doctoral investigator and the two clinical nurses. Potential participants who express interest in participating in the study will be screened for eligibility with reference to the inclusion and exclusion criteria by the doctoral investigator and the two clinical nurses. After their agreement to participate, the participants will be required to provide their written informed consent. The participants will be informed that they can withdraw from the study at any moment without any consequences.
Randomisation and allocation concealment
The pilot trial will be randomised and controlled in a 1:1 allocation ratio. One set of randomisation sequences will be generated via an online randomiser (https://www.randomizer.org/) based on the estimated sample size. To ensure allocation concealment, the randomisation sequences will be generated by a statistician who will not be involved in any other parts of this study. Specifically, the statistician will use the online randomiser to generate the randomisation sequences, which will include 36 even and 36 odd numbers. The randomisation sequences will be accessed by the statistician only. Once an eligible participant consents to participate in the study and completes the baseline assessment, the two clinical nurses will telephone the statistician to determine which group the patient should be assigned to according to the predefined random numbers. The participants will be randomly assigned to either the tai chi intervention group or the control group.
Blinding
Due to the visible nature of the tai chi intervention, blinding of the study investigators and the participants will be impossible. Thus, blinding will only be applied to the outcome assessors (ie, the two research assistants) in this pilot RCT to avoid potential detection bias during data collection. The two research assistants will be responsible for data collection and telephone follow-ups, and they will not be involved in the subject recruitment process.
Tai chi intervention group
In addition to the standard care provided to both the intervention group and the control group, the participants in the intervention group will additionally receive instruction on easy eight form tai chi movements. The development and validation of the evidence-based tai chi protocol are detailed in a methodological paper.24 The intervention regimen will last 60 min per session, two sessions per week, for 8 weeks, which is based on current research evidence, practice standards/guidelines, theories and experts’ consensus.24 To ensure that the participants have fully mastered the tai chi skills, before the commencement of the intervention, they will receive at least three 60 min training sessions until they can perform the movements correctly and smoothly, along with a home learning package in an audiovisual format (ie, a recorded video). The training will be conducted and led by either the doctoral investigator or the two clinical nurses, and attendance will be recorded. All the participants will be asked to perform the tai chi movements in front of the trainers (ie, return demonstration) to make sure that they are correctly performing each movement of the tai chi exercise. In addition, the participants will be tested by the trainers during the last training session to ensure that they have correctly performed the tai chi movements (via return demonstration).
Each tai chi session will be 60 min and will be comprised of the following components: a 10 min warm-up, 25–30 min of easy 8 form tai chi practising, and a 10 min cool-down. During each session, the participants will also have a 10 min break to rest. The tai chi intervention protocol was adapted in clinical practice to develop a personalised intervention that will be tailored to the participants’ convenience and preference regarding the time and venue of the intervention. Details of the tai chi protocol are presented in a methodological paper.24 A specially designed exercise log will be provided to the participants to record information related to their tai chi practice immediately after tai chi practising each time, such as duration and frequency of practising tai chi, as well as any potential adverse reactions related to tai chi, such as dizziness, knee pain, musculoskeletal aches and pains, etc. The exercise logs will be returned to the research assistants on the date of the participants’ treatment or follow-up appointment at the hospital. To enhance the participants’ adherence to the tai chi intervention, the research assistants will conduct telephone follow-ups every week to remind them to practise their tai chi and to collect information on any potential adverse reactions related to the tai chi intervention.
Control group
The participants allocated to the control group will receive a standard care package, which will be a booklet on the self-management of cancer symptoms. This booklet will offer basic knowledge and management strategies regarding FSDSC management in patients with BC during or after chemotherapy treatment. All the information listed in this booklet will be comprehensively adapted from relevant national guidelines developed by professional associations in cancer care and government health department websites, including the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology (the NCCN Guidelines)25 and the Department of Health-Government of Western Australia.26 Research evidence in published peer-reviewed articles will also be cited as supporting information for the booklet’s development.2 27–29 Additionally, the participants will be asked to refrain from practising any exercises related to TCE during the study, with reminders at all assessment time points. On completion of the pilot RCT, the participants in the control group will have an opportunity to receive the tai chi training from the study team.
Outcome measurements and follow-up
The outcome measurements for this pilot RCT will include three categories, namely, baseline assessments, feasibility and acceptability outcomes, and clinical outcomes. The feasibility and acceptability outcomes will be the primary outcomes, while the clinical outcomes will be the secondary outcomes. All the outcomes and follow-ups will be conducted by the two research assistants.
Demographic and clinical characteristics of the participants
A self-designed demographic and clinical data form will be employed to collect the participants’ sociodemographic data (eg, age, education background, employment status, marital status and household income) and medical history (eg, date of diagnosis, the current stage of BC and date and type of treatment) at baseline (T1).
Primary outcomes: feasibility and acceptability
The feasibility assessment of subject recruitment and the follow-up process will include: (1) the time that was taken to recruit the planned sample size of participants; (2) referral rate—the number of referrals made by clinicians in different departments and hospitals divided by all referrals; (3) recruitment rate—the number of subjects who enrolled in the study divided by all subjects eligible for enrolment; (4) retention rate—the number of subjects who completed the study divided by all subjects who enrolled in the study; (5) drop-out rate—the number of subjects who dropped out after randomisation divided by all subjects who enrolled in the study and (6) feedback from the drop-out subjects to identify their reasons for dropping out. The feasibility of recruitment and follow-up process outcomes will be collected from baseline (T1) to the completion of the intervention (T2).
The feasibility assessment of the outcome measures will include the percentage of missing values for each item of the scales used—the Brief Fatigue Inventory (BFI), the Pittsburgh Sleep Quality Index (PSQI), the Hospital Anxiety and Depression Scale (HADS) and the Functional Assessment of Cancer Therapy-Breast (FACT-B)—at baseline (T1), immediately after the intervention (T2) and 4 weeks after completion of the intervention (T3).
The feasibility and acceptability of the intervention will include: (1) adherence rates—the number of tai chi sessions practised divided by the total number of sessions required; (2) the participants’ feedback on and satisfaction with the intervention using a self-designed feedback form; (3) records of adverse events associated with tai chi, which will be obtained from the exercise logs and (4) the number of participants who completed the exercise log. The feasibility and acceptability of the intervention will be assessed immediately after the intervention (T2).
Secondary outcomes: fatigue, sleep disturbance, depression and QOL
The fatigue, sleep disturbance, depression and QoL of the patients with BC as the secondary outcomes will be measured at T1, T2 and T3 using the BFI, the PSQI, the HADS and the FACT-B.
Fatigue: The participants’ severity of fatigue and cancer-related fatigue in daily functioning will be measured using the BFI. The BFI has nine items, with higher scores corresponding to more severe fatigue.30 31 The Chinese version of the BFI has excellent internal consistency reliability (Cronbach’s alpha from 0.90 to 0.92), as well as construct validity and convergent validity.32
Sleep disturbance: The participants’ sleep quality and disturbance will be assessed using the PSQI. This questionnaire has seven domains: sleep latency, habitual sleep efficiency, subjective sleep quality, sleep duration, use of sleeping medication, sleep disturbance and daytime dysfunction.33 A total score will be calculated from the sum of the seven domains’ scores. A higher total score indicates poorer sleep quality. The Chinese version of the PSQI has been demonstrated to be a reliable and valid scale, and it has been widely used among patients with cancer.34
Depression: The HADS will be used to assess the participants’ depression. The cut-off scores have been classified and labelled as 0–7 for ‘normal’, 8–10 for ‘mild’, 11–15 for ‘moderate’ and ≥16 for ‘severe’.35 As a reliable and valid tool for measuring depression, the HADS has been widely used among Chinese patients with cancer, with well-documented psychometric properties.36
QoL: The FACT-B will be adopted to assess the participants’ QoL. A higher score demonstrates better QoL. The FACT-B is available in a simplified Chinese version, with adequate psychometric properties reported among patients with BC.37
Data management
The doctoral investigator and one of the research assistants will enter all the collected data into a computer with a double data entry approach. To ensure that there are no discrepancies or coding errors after running descriptive and inferential statistics, data cleaning will be conducted before data analysis.38 First, the datasets will be checked against the paper recordings of raw data to ensure that the data coding is correct. Then, double-checking will be undertaken by the other research assistant to ensure accuracy. All electronic data will be retained in a compressed folder using password-protected access systems, and all hard copies of the materials will be retained in a cabinet at the study sites. Storage and disposal of research data hard copies will strictly follow the regulations and policies of the lead investigator’s institution and the study sites, including the Charles Darwin University Research Data Management Guide.
Data analysis
Statistical analyses will be conducted using IBM SPSS Statistics for Windows, V.24.0 (IBM). The intention-to-treat principle will be used for the management of missing data. Effect sizes of between-group comparisons will be estimated using Cohen’s d.39 The χ2 test or Fisher’s exact test will be used to examine the comparisons between the control and intervention groups for categorical variables (eg, education background, referral rate, retention rate, etc). An independent t-test or the Mann-Whitney U test will be used for the continuous variables (eg, age). The generalised estimating equation model will be performed for repeated multivariate analysis between the two study groups for the total scores and domain scores of the BFI, the PSQI, the HADS and the FACT-B. The significance level to identify statistical differences will be p<0.05.
Patient and public involvement
No patient was involved in the study design or any other part of this protocol.
Ethics and dissemination
The study has been approved by the Human Research Ethics Committee at Charles Darwin University (H19094), the Clinical Trial Ethics Committee at the Affiliated Hospital of Southwest Medical University (KY2019133) and the Clinical Trial Ethics Committee at the Affiliated Hospital of Putian University (201932). The abstract of this study has been submitted to Sigma’s 32nd International Nursing Research Congress for presentation in 2021. The results of the trial will be published in peer-reviewed scientific journals.
Discussion
As one of the most common symptom clusters in patients with BC, the FSDSC can significantly deteriorate patients’ QoL and daily functioning.40 41 An increasing number of studies have demonstrated that tai chi has beneficial effects on symptom management in patients with cancer; however, almost all the studies focused on individual symptoms only, such as fatigue, sleep disturbance or depression.42–44 No study has ever been performed to investigate the role of tai chi in managing symptom clusters in the BC population. This highlights a great need to explore the effects of tai chi on the FSDSC in patients with BC. Given that the patients will have already experienced fatigue on enrolment in this pilot RCT, lengthy and complicated tai chi movements will be avoided. Easy 8 form tai chi, a traditional Chinese mind-body exercise with only eight simple movements, is an appropriate intervention for FSDSC management as it is easy to learn, is less energy-consuming, and requires no specific equipment.45 46
This study has some strengths. According to the Medical Research Council Framework for Developing and Evaluating Complex Interventions, the feasibility and acceptability of a proposed intervention and research methodological procedures should be fully examined prior to performing the full-scale study.47 In this current pilot RCT, the feasibility and acceptability of an easy 8 form tai chi intervention programme will be assessed comprehensively using a series of feasibility outcomes, including subject recruitment, intervention delivery and outcome assessments. A comprehensive assessment will promote the refinement of the intervention protocol for the future main study. Furthermore, different from some current non-pharmacological studies, the tai chi intervention protocol used in the current pilot RCT will be evidence-based and rigorously developed based on systematic review evidence and recommendations48–56; TCE principles, theories,57 58 and practice standards46 59; the characteristics of cancer-related symptoms; and the consensus of an expert panel. In addition, an FSDSC self-management education booklet will be designed and provided to the participants in both the intervention and control groups. The information listed in this booklet will be comprehensively adapted from relevant national guidelines, professional bodies, and research evidence in published peer-reviewed articles. The self-management education booklet will be used as an enhanced care component to improve the patients’ knowledge and relevant coping strategies for FSDSC management. Finally, a safety assessment of the tai chi protocol for patients with cancer will be set as one of the feasibility outcomes, which has rarely been measured in existing tai chi interventional studies. Although tai chi is a non-invasive intervention that is generally regarded as a relatively safe approach, the exercise programme might still contribute to some minor adverse events such as a lumbar sprain, musculoskeletal aches and pains, dizziness, knee pain, etc.60 Therefore, any potential adverse events related to practising tai chi will be monitored and reported in the exercise log.
This study also has some limitations. Given the limited study sites, the study sample in this study may not offer a completely representative sample of patients with BC who are experiencing the FSDSC. Due to the visible nature of the tai chi intervention, the blinding of the participants and the tai chi instructor cannot be performed in this study, which might increase the risk of detection bias during the study’s implementation, although the outcome assessors will be blinded to the intervention allocation. The lack of long-term follow-up to assess the ongoing effects of tai chi might be another limitation, but this can be considered in the future full-scale RCT as one of the main study outcomes.
This study will use a rigorously designed RCT to assess the feasibility and preliminary effects of an evidence-based tai chi programme for alleviating the FSDSC in patients with BC. The convenience of the tai chi for the self-management of the FSDSC may provide patients with BC, healthcare professionals and policy-makers with further guidance in FSDSC management in the long run. Furthermore, the results of this trial will contribute to a future multicentre large-scale main RCT to further conclude the research evidence on the effects and safety of tai chi for FSDSC management in patients.
Supplementary Material
Footnotes
Contributors: L-QY study conception and design, trial organisation, administration and coordination, quality assurance and manuscript drafting and revision; J-YBT: study conception and design, study procedure supervision, and manuscript revision; CT: study conception and design, study procedure supervision, and manuscript revision; TW: study design, study procedure supervision and manuscript revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Malvezzi M, Carioli G, Bertuccio P, et al. European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann Oncol 2019;30:781–7. 10.1093/annonc/mdz051 [DOI] [PubMed] [Google Scholar]
- 2.Jain S, Boyd C, Fiorentino L, et al. Are there efficacious treatments for treating the fatigue-sleep disturbance-depression symptom cluster in breast cancer patients? a rapid evidence assessment of the literature (REAL(©)). Breast Cancer 2015;7:267–91. 10.2147/BCTT.S25014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsu H-T, Lin K-C, Wu L-M, et al. Symptom cluster trajectories during chemotherapy in breast cancer outpatients. J Pain Symptom Manage 2017;53:1017–25. 10.1016/j.jpainsymman.2016.12.354 [DOI] [PubMed] [Google Scholar]
- 4.Liu L, Rissling M, Natarajan L, et al. The longitudinal relationship between fatigue and sleep in breast cancer patients undergoing chemotherapy. Sleep 2012;35:237–45. 10.5665/sleep.1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum 2001;28:465–70. [PubMed] [Google Scholar]
- 6.Aktas A, Kirkova J, Walsh D, et al. The psychometric properties of cancer multi-symptom assessment instruments: a comprehensive review. J Pain Symptom Manage 2012;43:334–5. 10.1016/j.jpainsymman.2011.12.038 [DOI] [Google Scholar]
- 7.Ho S-Y, Rohan KJ, Parent J, et al. A longitudinal study of depression, fatigue, and sleep disturbances as a symptom cluster in women with breast cancer. J Pain Symptom Manage 2015;49:707–15. 10.1016/j.jpainsymman.2014.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H-J, Barsevick AM, Beck SL, et al. Clinical subgroups of a psychoneurologic symptom cluster in women receiving treatment for breast cancer: a secondary analysis. Oncol Nurs Forum 2012;39:E20–30. 10.1188/12.ONF.E20-E30 [DOI] [PubMed] [Google Scholar]
- 9.Hökkä M, Kaakinen P, Pölkki T. A systematic review: non-pharmacological interventions in treating pain in patients with advanced cancer. J Adv Nurs 2014;70:1954–69. 10.1111/jan.12424 [DOI] [PubMed] [Google Scholar]
- 10.Larkin D, Lopez V, Aromataris E. Managing cancer-related fatigue in men with prostate cancer: a systematic review of non-pharmacological interventions. Int J Nurs Pract 2014;20:549–60. 10.1111/ijn.12211 [DOI] [PubMed] [Google Scholar]
- 11.Yin C, Buchheit TE, Park JJ. Acupuncture for chronic pain: an update and critical overview. Curr Opin Anaesthesiol 2017;30:583–92. 10.1097/ACO.0000000000000501 [DOI] [PubMed] [Google Scholar]
- 12.McKernan LC, Finn MTM, Patterson DR, et al. Clinical hypnosis for chronic pain in outpatient integrative medicine: an implementation and training model. J Altern Complement Med 2020;26:107–12. 10.1089/acm.2019.0259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charalambous A, Giannakopoulou M, Bozas E, et al. Guided imagery and progressive muscle relaxation as a cluster of symptoms management intervention in patients receiving chemotherapy: a randomized control trial. PLoS One 2016;11:e0156911. 10.1371/journal.pone.0156911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lopez G, Liu W, Milbury K, et al. The effects of oncology massage on symptom self-report for cancer patients and their caregivers. Support Care Cancer 2017;25:3645–50. 10.1007/s00520-017-3784-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen LT, Yates P, Annoussamy LC, et al. The effectiveness of non-pharmacological interventions in the management of symptom clusters in adult cancer patients: a systematic review protocol. JBI Database System Rev Implement Rep 2016;14:49–59. 10.11124/JBISRIR-2016-2476 [DOI] [PubMed] [Google Scholar]
- 16.Zou L, Wang H, Xiao Z, et al. Tai chi for health benefits in patients with multiple sclerosis: a systematic review. PLoS One 2017;12:e0170212. 10.1371/journal.pone.0170212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jahnke R, Larkey L, Rogers C, et al. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot 2010;24:e1–25. 10.4278/ajhp.081013-LIT-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Irwin MR, Olmstead R, Carrillo C, et al. Tai chi chih compared with cognitive behavioral therapy for the treatment of insomnia in survivors of breast cancer: a randomized, partially blinded, noninferiority trial. J Clin Oncol 2017;35:2656–65. 10.1200/JCO.2016.71.0285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McQuade JL, Prinsloo S, Chang DZ, et al. Qigong/tai chi for sleep and fatigue in prostate cancer patients undergoing radiotherapy: a randomized controlled trial. Psychooncology 2017;26:1936–43. 10.1002/pon.4256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang L-L, Wang S-Z, Chen H-L, et al. Tai chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manage 2016;51:504–11. 10.1016/j.jpainsymman.2015.11.020 [DOI] [PubMed] [Google Scholar]
- 21.Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933–40. 10.1002/sim.4780141709 [DOI] [PubMed] [Google Scholar]
- 22.Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health 2008;31:180–91. 10.1002/nur.20247 [DOI] [PubMed] [Google Scholar]
- 23.Campo RA, O'Connor K, Light KC, et al. Feasibility and acceptability of a tai chi chih randomized controlled trial in senior female cancer survivors. Integr Cancer Ther 2013;12:464–74. 10.1177/1534735413485418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao L-Q, Tan J-Y, Turner C, et al. Development and validation of a tai chi intervention protocol for managing the fatigue-sleep disturbance-depression symptom cluster in female breast cancer patients. Complement Ther Med 2021;56:102634. 10.1016/j.ctim.2020.102634 [DOI] [PubMed] [Google Scholar]
- 25.Berger AM, Mooney K, Alvarez-Perez A, et al. Cancer-related fatigue, version 2.2015. J Natl Compr Canc Netw 2015;13:1012–39. 10.6004/jnccn.2015.0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Department of health at the government of Western Australia . Resources. Available: https://www.health.gov.au/resources
- 27.Berger AM, Mooney K, Alvarez-Perez A. National comprehensive cancer network. cancer-related fatigue, version 2. J Natl Compr Canc Netw 2015;13:1012–39. 10.6004/jnccn.2015.0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berger AM, Mitchell SA, Jacobsen PB, et al. Screening, evaluation, and management of cancer-related fatigue: ready for implementation to practice? CA Cancer J Clin 2015;65:190–211. 10.3322/caac.21268 [DOI] [PubMed] [Google Scholar]
- 29.Li M, Fitzgerald P, Rodin G. Evidence-based treatment of depression in patients with cancer. J Clin Oncol 2012;30:1187–96. 10.1200/JCO.2011.39.7372 [DOI] [PubMed] [Google Scholar]
- 30.Mendoza TR, Wang XS, Cleeland CS, et al. The rapid assessment of fatigue severity in cancer patients: use of the brief fatigue inventory. Cancer 1999;85:1186–96. [DOI] [PubMed] [Google Scholar]
- 31.Nunes AF, Bezerra CO, Custódio JDS, et al. Clinimetric properties of the brief fatigue inventory applied to oncological patients hospitalized for chemotherapy. J Pain Symptom Manage 2019;57:297–303. 10.1016/j.jpainsymman.2018.10.508 [DOI] [PubMed] [Google Scholar]
- 32.Wang XS, Hao X-S, Wang Y, et al. Validation study of the Chinese version of the brief fatigue inventory (BFI-C). J Pain Symptom Manage 2004;27:322–32. 10.1016/j.jpainsymman.2003.09.008 [DOI] [PubMed] [Google Scholar]
- 33.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 34.Tsai P-S, Wang S-Y, Wang M-Y, et al. Psychometric evaluation of the Chinese version of the Pittsburgh sleep quality index (CPSQI) in primary insomnia and control subjects. Qual Life Res 2005;14:1943–52. 10.1007/s11136-005-4346-x [DOI] [PubMed] [Google Scholar]
- 35.Smith RP, Zigmond AS. The hospital anxiety and depression scale manual. Windsor: NFER—Nelson, 1994. [Google Scholar]
- 36.Wang W, Chair SY, Thompson DR, et al. A psychometric evaluation of the Chinese version of the hospital anxiety and depression scale in patients with coronary heart disease. J Clin Nurs 2009;18:1908–15. 10.1111/j.1365-2702.2008.02736.x [DOI] [PubMed] [Google Scholar]
- 37.Wan C, Zhang D, Yang Z, et al. Validation of the simplified Chinese version of the FACT-B for measuring quality of life for patients with breast cancer. Breast Cancer Res Treat 2007;106:413–8. 10.1007/s10549-007-9511-1 [DOI] [PubMed] [Google Scholar]
- 38.Portney LG, Watkins MP. Foundations of clinical research: applications to practice (Vol. 892). upper saddle river. NJ: Pearson/Prentice Hall, 2009. [Google Scholar]
- 39.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 40.Fitzgerald P, Lo C, Li M, et al. The relationship between depression and physical symptom burden in advanced cancer. BMJ Support Palliat Care 2015;5:381–8. 10.1136/bmjspcare-2012-000380 [DOI] [PubMed] [Google Scholar]
- 41.Oh H, Seo Y, Jeong H, et al. The identification of multiple symptom clusters and their effects on functional performance in cancer patients. J Clin Nurs 2012;21:2832–42. 10.1111/j.1365-2702.2011.04057.x [DOI] [PubMed] [Google Scholar]
- 42.Qiang WM, Dong FQ, Yan L. Comparison of two different exercise programs in breast cancer patients after postoperative adjuvant chemotherapy. Chin J Nurs 2011;46:e540:537. [Google Scholar]
- 43.Jiang MY. Influence of shadowboxing on improving cancer-related fatigue and sleeping quality of patients with advanced lung cancer. Chin Nurs Res 2013;27:420. [Google Scholar]
- 44.Larkey LK, Roe DJ, Weihs KL, et al. Randomized controlled trial of Qigong/Tai chi easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med 2015;49:165–76. 10.1007/s12160-014-9645-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tadros G, Ormerod S, Dobson-Smyth P, et al. The management of behavioural and psychological symptoms of dementia in residential homes: does tai chi have any role for people with dementia? Dementia 2013;12:268–79. 10.1177/1471301211422769 [DOI] [PubMed] [Google Scholar]
- 46.Li F, Fisher KJ, Harmer P, et al. A simpler eight-form easy tai chi for elderly adults. J Aging Phys Act 2003;11:206–18. 10.1123/japa.11.2.206 [DOI] [Google Scholar]
- 47.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new medical research council guidance. BMJ 2008;337:a1655. 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.HL M, Tan JY, Yang LH. Current evidence on traditional Chinese exercises for cancer-related fatigue: a quantitative synthesis of randomized controlled trials. Eur J Integr Med 2016;8:707–14. 10.1016/j.eujim.2016.05.007 [DOI] [Google Scholar]
- 49.Wayne PM, Lee MS, Novakowski J, et al. Tai chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv 2018;12:256–67. 10.1007/s11764-017-0665-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Song S, Yu J, Ruan Y, et al. Ameliorative effects of tai chi on cancer-related fatigue: a meta-analysis of randomized controlled trials. Support Care Cancer 2018;26:2091–102. 10.1007/s00520-018-4136-y [DOI] [PubMed] [Google Scholar]
- 51.Van Vu D, Molassiotis A, Ching SSY, et al. Effects of Qigong on symptom management in cancer patients: a systematic review. Complement Ther Clin Pract 2017;29:111–21. 10.1016/j.ctcp.2017.09.005 [DOI] [PubMed] [Google Scholar]
- 52.Xiang Y, Lu L, Chen X, et al. Does tai chi relieve fatigue? a systematic review and meta-analysis of randomized controlled trials. PLoS One 2017;12:e0174872. 10.1371/journal.pone.0174872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yao L-Q, Tan J-Y, Turner C, et al. Traditional Chinese exercise for cancer-related sleep disturbance: a systematic review and descriptive analysis of randomized controlled trials. Complement Ther Clin Pract 2020;40:101197. 10.1016/j.ctcp.2020.101197 [DOI] [PubMed] [Google Scholar]
- 54.Zeng Y, Xie X, Cheng ASK. Qigong or tai chi in cancer care: an updated systematic review and meta-analysis. Curr Oncol Rep 2019;21:48. 10.1007/s11912-019-0786-2 [DOI] [PubMed] [Google Scholar]
- 55.Ni X, Chan RJ, Yates P, et al. The effects of tai chi on quality of life of cancer survivors: a systematic review and meta-analysis. Support Care Cancer 2019;27:3701–16. 10.1007/s00520-019-04911-0 [DOI] [PubMed] [Google Scholar]
- 56.Hilfiker R, Meichtry A, Eicher M, et al. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br J Sports Med 2018;52:651–8. 10.1136/bjsports-2016-096422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bower JE, Irwin MR. Mind-body therapies and control of inflammatory biology: a descriptive review. Brain Behav Immun 2016;51:1–11. 10.1016/j.bbi.2015.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Larkey L, Jahnke R, Etnier J, et al. Meditative movement as a category of exercise: implications for research. J Phys Act Health 2009;6:230–8. 10.1123/jpah.6.2.230 [DOI] [PubMed] [Google Scholar]
- 59.Committee of Chinese Sports College Textbook . Chinese Wushu textbook (Part I). Beijing: People’s Sports Publishing House of China, 2003. [Google Scholar]
- 60.Jia X, Jiang C, Tao J, et al. Effects of core strength training combined with tai chi chuan for the musculoskeletal system and cardiopulmonary function in older adults: a study protocol for a randomized controlled trial. Medicine 2018;97:e12024. 10.1097/MD.0000000000012024 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


