Abstract
Background
Tension-type headache (TTH) has been ranked the second most prevalent health condition worldwide. Non-pharmacological treatments for TTH are widely used as a supplement or an alternative to medical treatment. However, the evidence for their effects are limited. Therefore, the aim of this study was to review the evidence for manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture and patient education as treatments for TTH on the effect of headache frequency and quality of life.
Methods
A systematic literature search was conducted from February to July 2020 for clinical guidelines, systematic reviews, and individual randomised controlled trials (RCT). The primary outcomes measured were days with headache and quality of life at the end of treatment along with a number of secondary outcomes. Meta-analyses were performed on eligible RCTs and pooled estimates of effects were calculated using the random-effect model. The overall certainty of evidence was evaluated using the Grading of Recommendations, Assessment, Development, and Evaluation approach (GRADE). In addition, patient preferences were included in the evaluation.
Results
In all, 13 RCTs were included. Acupuncture might have positive effects on both primary outcomes. Supervised physical activity might have a positive effect on pain intensity at the end of treatment and headache frequency at follow-up. Manual joint mobilisation techniques might have a positive effect on headache frequency and quality of life at follow-up. Psychological treatment might have a positive effect on stress symptoms at the end of treatment. No relevant RCTs were identified for patient education. The overall certainty of evidence was downgraded to low and very low. No serious adverse events were reported. A consensus recommendation was made for patient education and weak recommendations for the other interventions.
Conclusion
Based on identified benefits, certainty of evidence, and patient preferences, manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture, and patient education can be considered as non-pharmacological treatment approaches for TTH. Some positive effects were shown on headache frequency, quality of life, pain intensity and stress symptoms. Few studies and low sample sizes posed a challenge in drawing solid conclusions. Therefore, high-quality RCTs are warranted.
Supplementary Information
The online version contains supplementary material available at 10.1186/s10194-021-01298-4.
Keywords: Headache, Exercise, Manual therapy, Mindfulness, Dry needling, Non-pharmacological treatment
Background
Headache was ranked third among causes of years lived with disability [1], and tension-type headache (TTH) was ranked the second most prevalent health condition worldwide in 2010 [2]. Current TTH has a global prevalence of 38% [3], and an estimated one-year prevalence from 38 to 87% [4–7]. Infrequent episodic TTH has a one-year prevalence of 19%, frequent episodic TTH 22%, and chronic TTH 3% [4]. Although the cause of TTH is unresolved, muscular factors, especially from pericranial muscles, stress and central sensitization all seem to play a role in the pathophysiology of TTH [8].
TTH has an economic impact on both society and the individual. The mean per-person annual indirect and direct costs was €303 which included lost productivity, absenteeism, outpatient care etc. The main direct annual costs was outpatient care (which accounted for 44% (€11) of the total direct annual costs) which amongst others included professional advice from a nurse, physiotherapist, osteopath, and chiropractor, followed by investigations, acute medications, hospitalisation and prophylactics [9].
Even though non-pharmacological treatments for TTH are widely used and the direct financial costs associated with non-pharmacological treatments are high, the evidence for their effects is limited. In 2010, a European expert panel recommended non-pharmacological treatment for TTH such as psychological approaches that included EMG biofeedback, cognitive-behavioural therapy and relaxation as well as physical therapy and acupuncture [10]. In 2012, The National Clinical Guideline Centre, commissioned by the National Institute for Health and Care Excellence (NICE), published a clinical guideline for the management of primary headache disorders (NICE CG150) [11]. The NICE CG150 found some evidence for acupuncture but found no evidence for manual therapy, exercise, psychological therapies, and education and self-management. Therefore, there is a need for a systematic evaluation of the latest research associated with these non-pharmacological approaches.
Non-pharmacological treatment should be considered for TTH management [10]. It can be considered as a supplement to medical treatment or as an alternative to medical treatment [12]. Therefore, non-pharmacological treatment may also be considered if TTH-patients suffer from unpleasant side effects and/or perceive the medical treatment as not effective.
Previous systematic reviews, published after the release of ICHD-2 [13] have evaluated the effectiveness of manual therapy compared to conservative or conventional treatments [14, 15], effectiveness of trigger point manual therapy [16], several modalities [17, 18] or a solely focus on quality of life [19]. We need a focus on modalities that used manual joint mobilisation techniques rather than including manual therapies as massage, trigger point therapy or cranio-sacral therapy.
To our knowledge, no previous systematic review has evaluated the literature for the evidence of physical activity for TTH such as strength training and aerobic exercises. Systematic reviews have evaluated the effect of exercises in combination with manual therapies [20] and of yoga exercise [21]. Yoga exercise showed potential positive effects on TTH frequency and pain intensity, however, a part of these yoga programmes included relaxation and meditation which may have had an independent effect.
Previous systematic reviews have evaluated the effect of psychological treatment on headache disorders [22–25]. However, these studies primarily reported results on headache rather than separately for TTH.
Acupuncture has shown a positive effect on TTH frequency [26, 27]. Though, we need a literature evaluation of the latest evidence for acupuncture excluding acupuncture with electrical stimulation as intervention and sham acupuncture with needle insertion as comparator.
Self-management programs have shown positive effects on headache such as pain intensity, mood and disability [28]. We need a literature search for programs on TTH that included disease specific education that also included education about medication in order to avoid medication-overuse headache.
With this review we aimed at gathering the evidence for these five areas to evaluate them in relation to the same outcomes in order to produce recommendations for a National Clinical Guideline (NCG). Which may facilitate the path for health professionals in identifying and directing the patient with TTH to the appropriate treatment strategy targeting the patient’s needs and resources.
Thus, the aim of the current study was to conduct a systematic review with meta-analyses and summarise the evidence for the following five separate treatment approaches for TTH: manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture, and patient education compared to other than the respective investigated modality on the effect of headache frequency and quality of life.
Methods
The current review and NCG were based on the Population, Intervention, Comparison and Outcome (PICO) framework, with the methodology following the Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) approach. This review adhere to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and its protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) in 2020, ID: CRD42020220124.
Organization of the work
The Danish Knowledge Centre on Headache Disorders invited a multidisciplinary expert group with the purpose of developing a NCG for non-pharmacological treatment for patients with TTH as an aid to assist healthcare professionals and patients with TTH to identify and seek the most relevant non-pharmacological treatment strategies. The study process was led by the Danish Knowledge Centre on Headache Disorders (CVH, LNC, JMH) assisted by a specialist in literature search (KB) and a research methodologist (HEC). Members of the multidisciplinary expert group were appointed by Danish societies, i.e. the Chiropractor Association, the Osteopath Association, the Society for Physiotherapy, the Psychologist Association, the Medical Acupuncture, and the Neurological Society. Patient organizations and other representatives from the Danish health care system were included as a reference group. They provided feedback on the questions investigated, patient preferences, and on the final recommendations. The draft of the NCG was peer-reviewed by two external reviewers and disseminated for public feedback i.e. to relevant stakeholders.
Clinical questions
Five PICO questions were constructed in order to investigate the effect of specific non-pharmacological interventions for patients diagnosed with TTH.
Population
Patients diagnosed with TTH according to the International Classification of Headache Disorder 2nd-3rd edition (ICHD 2–3) [13, 29] were included. The study population was aged 18 years or older. Studies of patients suffering from both TTH and migraine were also included but only if results were reported separately for TTH. We excluded studies of any other primary or secondary headache disorders. If studies of cervicogenic headache also included patients with TTH, there had to be a clear distinction between these two classifications based on ICHD 2–3 for both headache disorders and/or the classification proposed by Sjaastad et al. for cervicogenic headache [30].
Intervention
The investigated interventions included: 1) manual joint mobilisation techniques 2) supervised physical activity 3) psychological treatment 4) acupuncture and 5) patient education.
Comparator
1) Maunal joint mobilisation techniques compared to no manual joint mobilisation techniques, other treatment than manual joint mobilisation techniques, treatment as usual, placebo, sham intervention or waitlist; 2) Supervised physical activity compared to no supervised physical activity, other treatment than physical activity, treatment as usual, placebo, sham intervention or waitlist; 3) Psychological treatment compared to no psychological treatment, other treatment than psychological treatment, treatment as usual, placebo, sham intervention or waitlist; 4) Acupuncture compared to no acupuncture, other treatment than acupuncture, treatment as usual, placebo, sham intervention (studies that only used sham acupuncture with skin penentration as control group were excluded) or waitlist; 5) Patient education compared to no patient education, other treatment than patient education, treatment as usual, placebo, sham intervention or waitlist.
Outcomes
Two primary outcomes were selected for each PICO question: headache frequency in days per month and quality of life, both measured at the end of treatment. Additional primary outcomes were selected for psychological treatment (functioning) and patient education (degree of increased knowledge about illness and treament). A complete list of primary and secondary outcomes for each PICO question can be found in the Additional file 1 (Table 1).
Definitions
Manual joint mobilisation techniques
Manual joint mobilisation techniques were defined as all manual techniques, mobilisation or manipulation within the normal range of motion of the joint, aimed at affecting the joints, muscles and connective tissues of the neck, chest and lower back.
Supervised physical activity
Supervised physical activity was defined as planned, repeated and structured physical activity [43].
Psychological treatment
Phychological treatment refers to approaches that address self-efficacy to decrease negative effect of reduced functioning and improve quality of life despite headache pain and headache related disability.
Acupuncture
Acupuncture was defined as a treatment where thin needles are inserted into the body including dry-needling and trigger point acupuncture excluding electroacupuncture.
Patient education
A disease-specific education aiming at improving the understanding of the disorder and treatment options, thus improving both knowledge and skills to master the life with recurring headache. Disease specific education can be conducted individually and in classes and also address family members containing information about the disease, its treatment, medication overuse, self-care, lifestyle, physical activity, regular diet and sleep. The intervention had to be conducted by a trained professional.
Literature search and study selection
A systematic search was made on February 2020 to July 2020. Databases included EMBASE, PsycINFO, MEDLINE, CINAHL and PEDRO. The search was performed for Randomised Controlled Trials (RCT) included in existing guidelines and systematic reviews. Subsequently, an individual search for RCTs was performed, with the search date limited to the date of the latest search in identified existing systematic reviews. There was no restriction regarding publication status. The studies had to be published in English, Swedish, Norwegian or Danish. The search protocol can be found in Additional file 2.
The title and abstract of studies were independently screened by one review author followed by an assessment of full text of potential studies by two review authors. Any disagreement was recognised and resolved. The authors evaluating the studies were not blinded.
Data extraction, risk of bias and quality assessment
Systematic reviews or existing clinical guidelines were identified and the methodological quality was evaluated using the AMSTAR [44] and AGREE [45] tools, respectively. Only systematic reviews and guidelines of sufficient quality were included, followed by data extraction of individual RCTs mentioned in the review and/or clinical guideline. Data including population demographics, intervention and control details, outcome and time measurement were independently extracted, by two review authors, from relevant RCTs. Risk of bias within individual RCTs was independently assessed by two review authors using the Cochrane risk of bias tool [46]. Any discrepancy was resolved through discussion. The review authors were not blinded.
Summary measures
Meta-analysis for each outcome were performed if data, in the included RCTs, was comparable. Data was extracted in the online software program, Covidence [47] and subsequently exported to RevMan5 [48], where pooled estimates of effects were calculated using the random-effect model. Dichotomous outcomes were calculated as relative risks (RR) and continous outcomes as mean differences (MD). If different scales were used in the measurement of continuous outcomes, a standardised mean difference (SMD) was applied. A 95% confidence interval was calculated for both dichotomous and continuous outcomes. I2 statistics were used for quantification of statistical heterogeneity (I2 > 50% was considered substantial heterogeneity). There was insufficient data to allow for any subgroup analysis. Results were displayed in forest plots for each outcome.
Certainty of evidence and recommendations
The GRADE approach was applied to assess the certainty of evidence obtained for each outcome. One of four possible rating was possible; high, moderate, low or very low. If needed, downgrading the certainty of evidence was done based on the extent of risk of bias, inconsistency, indirectness, imprecision, and publication bias. The overall certainty of evidence for each clinical question was based on the lowest rating of the primary outcome.
If evidence was available for a given clinical question, either a strong or weak recommendation, for or against an intervention was made. If no evidence was available, a consensus recommendation was made. Recommendations were based on a combined evaluation of the certainty of evidence, patient preferences, and the identified benefits and harms.
Patient preferences and consensus recommendation
The Danish Knowledge Centre on Headache Disorders performed a survey on patients’ expectations concerning treatments offered by chiropractors, physiotherapists, psychologists, acupuncturists and courses about knowledge on illness and treatment. They were also asked whether they would seek this treatment again. The headache population was recruited by a modified snowball sampling via facebook and patient organizations.
Patient preferences and consensus recommendation were based on direct patient involvement based on responses from the survey, direct feedback from chairmen (ABO, BOL) and board member (JB) representing Danish Migraine Association, Denmark’s Patient Society for People with Headache, and the Migraine and Headache Society, respectively. Additionally, patient preferences were based on expert opinion of the multidisciplinary working group formed by their experience in working with patients in daily practice.
Results
Literature search and study selection
One relevant guideline was identified [11] and considered of high methodological quality in accordance with the AGREE-II tool. From this guideline one relevant RCT [32], concerning manual joint mobilisation techniques, was identified. This was followed by a search for existing systematic reviews; 11 relevant reviews were identified [14, 16, 17, 19, 22–27, 49], and rated using the AMSTAR tool. From the included systematic reviews, ten relevant RCTs were identified (six concerning manual joint mobilisation techniques [31–36]; three concerning psychological treatment [39–41]; one concerning acupuncture [42]. The AGREE-II and AMSTAR assessments can be found in Additional file 1 (Figure 1 and Table 2). An individual search for RCTs identified two additional studies, both concerning supervised physical activity [37, 38]. PRISMA flow charts of identified clinical guidelines, systematic reviews and primary studies can be seen in Additional file 1 (Figures 2–12).
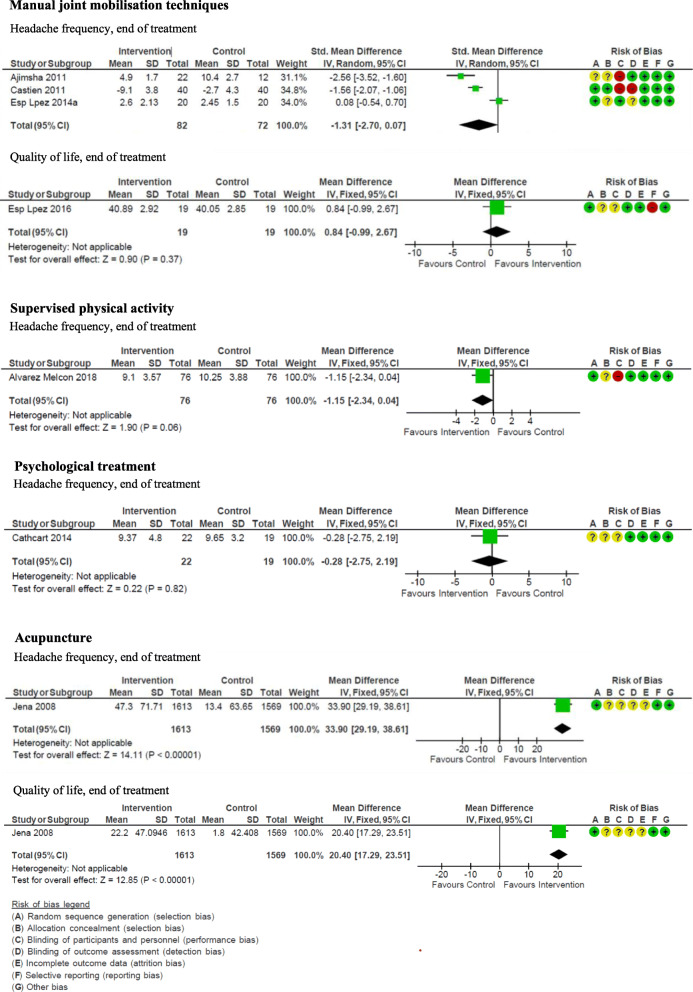
Estimated effect and recommendations
The RCTs included for each PICO and the outcomes assessed can be found in Table 1. The meta-analyses of primary outcomes can be seen in Fig. 1. Meta-analyses of secondary outcomes can be found in Additional file 1 (Figures 13–16). An overview of the recommendations can be found in Table 2.
Table 1.
Identified randomised controlled trials (RCTs) for non-pharmacological treatments for tension-type headache. Studies were found in existing guidelines and systematic reviews, or via a search for individual RCTs
| Non-pharmacological treatment | Number of RCTs identified | Intervention | Comparison | Outcomes assessed in the studies |
|---|---|---|---|---|
| Manual joint mobilisation techniques | 6 (Ajimsha et al. [31]); Castien et al. [32]; Espi-Lopez et al. 2014a [33]; Espi-Lopez et al. 2014b [34]; Espi-Lopez et al. 2016 [35]; Rolle et al. [36]) | Direct myofascial release technique (Ajimsha et al.), manual therapy (Castien et al.), osteopathic manual therapy (Rolle et al.), suboccipital muscle manipulation (Espi-Lopez 2014a, 2014b, 2016). | Sham intervention (Ajimsha et al.; Rolle et al.), treatment as usual (Castien et al.), no treatment (Espi-Lopez 2014a, 2014b, 2016). |
• Headache frequency (at the end of treatment and at follow-up) • Quality of life (at the end of treatment and at follow-up) • Headache intensity • Serious adverse events |
| Supervised physical activity | 2 (Alvarez-Melcon et al .[37]; Andersen et al. [38]) | Training program for the neck and relaxation (Alvarez-Melcon et al.) and training of neck and shoulder using an elastic band (Andersen et al.). | Relaxation (Alvarez-Melcon et al.) and weekly information on health (Andersen et al). |
• Headache frequency (at the end of treatment and at follow-up) • Headache intensity • The use of attack-medicine/analgesics |
| Psychological treatment | 3 (Cathcart et al. [39]; Holroyd et al. [40]; Omidi et al. [41]) | Mindfulness-based therapy (Cathcart et al.), cognitive behavioural stress management (Holroyd et al.) and mindfulness-based stress reduction (Omidi et al.). | Waiting list (Cathcart et al.), placebo (Holroyd et al.) and medical treatment as usual (Omidi et al.). |
• Headache frequency • Stress symptoms |
| Acupuncture | 1 (Jena et al. [42]) | Acupuncture | No treatment |
• Quality of life • Number of days with migraine • Serious adverse events |
| Patient education | None identified | – | – | – |
Fig. 1.
Non-pharmacological treatments for tension-type headache. Meta-analyses of primary outcomes: headache frequency and quality of life at end of treatment of manual joint mobilisation techniques, supervised physical activity, psychological treatment, and acupuncture. No randomized controlled trials were found for patient education. SD: standard deviation. CI: confidence interval
Table 2.
Overview of the recommendations for the use of non-pharmacological treatments for patients with tension-type headache
| Intervention | Certainty of evidence | Patient preferences | Recommendation |
|---|---|---|---|
| Manual joint mobilisation techniques | Very Low | Variability in patient preferences is expected | Weak recommendation for |
| Supervised physical activity | Very low | No substantial variability in patient preferences is expected | Weak recommendation for |
| Psychological treatment | Very low | Variability in patient preferences is expected | Weak recommendation for |
| Acupuncture | Low | Variability in patient preferences is expected | Weak recommendation for |
| Patient education | None identified | No substantial variability in patient preferences is expected | Consensus based recommendation |
Manual joint mobilisation techniques
Six relevant RCTs were identified [31–36]. In the study by Ajimsha et al. [31], direct myofascial release and sham intervention were included in the meta-analysis. In the studies by Espi-Lopez et al. [33–35], suboccipital muscle manipulation and no treatment were included in the meta-analysis. In the study by Rolle et al. [36], data could not be included in the analysis as data were reported visually in figures.
Results showed that manual joint mobilisation techniques have a potential positive effect on headache frequency (SMD -1.31 (95% CI -2.70 - 0.07)) and quality of life (MD 0.84 (95% CI -0.09 - 2.67)) when measured at follow-up. The certainty of the evidence was very low due to risk of bias, inconsistency and imprecision. We expect that there would be variability in the number of patients who would prefer this intervention. Based on these findings, a weak recommendation is made for manual joint mobilisation techniques which can be considered as a supplement to medical treatment for patients with TTH.
Supervised physical activity
Two relevant RCTs were identified [37, 38]. In the study by Andersen et al. [38], data were not presented in a form that could be used in the meta-analysis.
Results showed a potential positive effect of headache intensity at the end of treatment (MD -0.61 (95% CI -1.09 - -0.13)) and headache frequency at follow-up (MD -1.15 (95% CI -2.34 - 0.04)). The certainty of evidence was very low due to risk of bias and imprecision. We expect that most patients would prefer this intervention. Based on these findings, a weak recommendation is made for supervised physical activity which can be considered as a supplement to medical treatment for patients with TTH.
Psychological treatment
Three relevant RCTs were identified [39–41]. In the study by Holroyd et al. [40], the data could not be included in the meta-analysis as they were depicted visually in figures.
Results showed that psychological treatment potentially has a positive effect on stress symptoms at the end of treatment (MD -0.28 (95% CI -2.75 - 2.19)). The certainty of evidence was very low due to risk of bias and imprecision. We expect that there would be variability in the number of patients who would prefer this intervention. Based on these findings, a weak recommendation is made for psychological treatment which can be considered as a supplement to medical treatment for patients with TTH.
Acupuncture
One relevant RCT was identified [42]. Results showed that acupuncture potentially has a positive effect on headache frequency (MD 33.90 (95% CI 29.19–38.61)) and quality of life (MD 20.40 (95% CI 17.29–23.51)) at the end of treatment. The certainty of evidence was low due to risk of bias and imprecision. We expect that there would be variability in the number of patients with TTH who would prefer this intervention. Based on these findings, a weak recommendation is made for acupuncture which can be considered as a supplement to medical treatment for patients with TTH.
Patient education
No relevant RCTs were identified, and therefore the recommendation is solely based on consensus from experts. Based on clinical experience, patient education provided as systematic information and counseling, may have a positive effect on the patient’s ability to manage their disease and their life with chronic illness thereby reducing the overall symptom burden. We expect that the majority of patients would like to receive this intervention. Based on consensus, it is recommended to consider using patient education as a supplement to medical treatment for patients with TTH.
No serious adverse events were identified for any of the non-pharmacological treatment approaches.
Survey of patient expectations
The survey was answered by 380 patients. Regarding the different intervention, the largest part of patients expected reduced number of headache days (chiropractor 72%, physiotherapist 71%, psychologist 12%, acupuncture 79%, and education (lectures/ classes) 9% respectively). Subsequently, improved quality of life (chiropractor 46%, physiotherapist 47%, psychologist 69%, acupuncture 40%, education (lectures/classes) 44% respectively), and reduced use of analgesics (chiropractor 43% physiotherapist 41%, psychologist 6%, acupuncture 47%, and education (lectures/classes) 10% respectively). Moreover, 86% of the patients expected education to result in increased knowledge about headache and headache treatment. Psychological treatment was expected to result in improved pain coping strategies (63%) and positive impact on depression, anxiety and stress (58%). Regarding the likelihood with which patients would ask for a specific intervention again, there was a certain amount of variability relating to interventions by chiropractors, physiotherapists, acupuncture and psychologists, whereas 54% of the patients would ask for education again. Additional file 1 (Figure 17).
Discussion
The current study presented a systematic review of the evidence for manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture, and patient education as non-pharmacological treatment strategies for TTH regarding headache related outcomes, quality of life and disability.
The findings reveal that non-pharmacological treatment approaches for TTH were safe and showed a number of positive effects. In summary, in relation to primary outcomes, a potential positive effect on headache frequency and quality of life at the end of treatment were found for acupuncture. In relation to secondary outcomes, a potential positive effect was found for headache frequency (manual joint mobilisation techniques and supervised physical activity) and quality of life (manual joint mobilisation techniques) at follow-up; pain intensity (supervised physical activity) and stress symptoms (psychological treatment) at the end of treatment.
According to the GRADE approach, there was very low certainty of evidence for supervised physical activity and psychological treatment owing to risk of bias and imprecision. There was very low certainty of evidence for manual joint mobilisation techniques owing to risk of bias, inconsistency and imprecision. There was low certainty of evidence for acupuncture owing to risk of bias and imprecision. No relevant RCTs were found regarding patient education. There were no identified serious adverse events for any of the investigated interventions. A consensus recommendation was made for patient education and weak recommendations for the other interventions.
To the best of our knowledge, no former guideline, applying a similar systemtic approach, has been publised since the NICE CG150 was publiched in 2012. In line with the current review, the NICE CG150 [11] reviewed the evidence for manual therapies, exercise, psychological therapies, acupuncture, and patient education and self-management also applying the GRADE approach. There are similarities between the findings from the NICE CG150 and the current review. The NICE CG150 found some evidence for acupuncture as preventive treatment for TTH and made a recommendation for this treatment. We based our recommendation on one large RCT which was rated with low certainty of evidence. The NICE CG150 found low to very low certainty of evidence for manual therapy, but did not find enough evidence to form a recommendation. We formed a recommendation; however, the overall certainty of evidence was also rated very low. In contrast to the current review, the NICE CG150 did not find any relevant RCTs evaluating the effect of exercise on TTH. We based our recommendation on one study that could be included in the meta-analysis. The included study was based on university students with a mean age of 20 years, limiting the external validity. In line with the NICE CG150, that found low to very low certainty of evidence for psychological treatment but were not able to form a recommendation. We formed a recommendation but found an overall certainty of evidence that also was rated very low. In line with our review, the NICE CG150 did not find any evidence for self-management and educational programs for TTH.
Overall, direct comparison with other systematic reviews is challenging due to methodological variations, especially regarding variability in the intervention and comparison groupings as well as grouping in the analyses. However, in line with our results, earlier reviews reported potential positive effects for manual therapies on headache frequency [16, 18] and quality of life [14, 19]. All studies found low to very low level of evidence or inconclusive results [14–19]. However, these studies represent a variety of different treatment modalities. We included studies which directed the treatment towards affecting the joints, muscles and connective tissues of the neck, chest and lower back.
No previous systematic reviews were identified evaluating the effect of physical activity for TTH. We identified only RCT studies that evaluated the effect of exercises such as strength training, but no studies were identified evaluating aerobic exercise. Therefore, future studies may investigate the effect of a combination of these exercise treatments.
Regarding psychological treatment, Lee et al. (2019) [25] reported in a subgroup analysis that patients with TTH showed positive effects on headache index (reflecting diverse aspects of headache suffering [25]). We found positive effects on stress symptoms, which may indicate that this treatment approach could contribute to positive effects on both headache and psychological symptoms.
In line with previous systematic reviews on acupuncture [26, 27], we found positive effects on headache frequency. We excluded studies using electroacupuncture as intervention and studies using sham acupuncture with needle insertion and identified only one RCT study. Therefore, further studies using these criteria are needed to confirm these results.
There is a major gap in the quality of research related to patient education. Ashina et al. (2021) [12] indicated that all patients with TTH benefit from education that includes healthy lifestyle habits. Patient education aims to provide patients, who experience an impaired quality of life, with a better understanding and knowledge about their disease together with strategies for self-care and self-management. Based on clinical experience, the multidisciplinary expert group of this review recommended patient education for patients with frequent and chronic TTH as they often seek knowledge about their disorder and tools to manage their life with chronic illness. However, there is a need for more research in various programs within the field of headache.
The recommendations from the current review were also formed by an assessment of patient preferences with respect to non-pharmacological treatment. There may be variations in individuals’ need for treatment depending on the degree of headache and the impact on their daily living and quality of life. The patients with TTH should be informed, by healthcare professionals, about options for relevant forms of treatment and about realistic expectations of their effects. Lack of possibility of reimbursement may limit some patients’ access to non-pharmacological treament. Ideally, non-pharmacological treatments should be subjected to cost-effectiveness analysis in future guidelines.
The internal validity of the included studies needs to be addressed. In several studies, the reporting of headache classification was inconsistent and unclear. It was not clear who diagnosed the participants and how their diagnosis was obtained even if it was stated that the diagnosis was based on ICHD criteria. Currently, there are validated tools to classify primary headaches, however, there is a lack of tools that can be used by non-experts in primary care settings [50]. It is recommended to aid the diagnosis of headache by keeping a headache diary [11, 29].
Since the published guideline from the NICE CG150 in 2012 and updates in 2015, we found few studies matching each PICO. As a result, further research is warranted. It is recommended that future studies use uniform outcome measures and follow the designs of clinical trials as recommended by the guidelines from the International Headache Society [51], and follow the CONSORT statement for reporting randomised controlled trials [52].
The overall certainty of evidence for the included studies assessed by using GRADE was low to very low owing to insufficient blinding of staff, participants and outcome assessors. Moreover, there were uncertainties about the random sequence generation and allocation concealment in some studies, which could skew the baseline parameters in the intervention arms. The effect estimates display imprecision mainly because of wide confidence intervals, few studies, and low sample sizes. Consequently, is it difficult to draw any solid conclusions. Future reviews may, therefore, come to different conclusions than the conclusions reported from our review.
Strengths and limitations
We have based our review on the best current standards for systematic reviews and meta-analyses which strengthens the resulting NCG. The work was based on the PICO framework and performed using transparent quality assessment instruments, the AGREE-II and AMSTAR tools for clinical guidelines and systematic reviews respectively. The Cochrane risk of bias tool was used for individual RCTs and the overall certainty of evidence was performed using the GRADE approach. The reporting of this review was based on the PRISMA statement and registered beforehand in the PROSPERO register. The multidisciplinary expert group was composed of relevant experts with both clinical and research experience, and the literature search was performed by an expert research librarian. Finally, this NCG was peer-reviewed by the professional and medical societies and by two independent and international experts.
There were some limitations of this review. The GRADE approach is prone to downgrade research that is not double-blinded, which is challenging for clinical non-pharmacological research. The literature search was limited to English and Scandinavian languages. The survey on headache patients’ expectations were based on a modified snowball sampling, therefore this population may not represent the total headache population. The aim of the survey was to have an overview of the use and preferences of non-pharmacological treatment as a starting point for this review. The target population was headache patients. Therefore, there were no distinction between headache types, headache frequency, demographics or psychiatric or other comorbidities that may have influenced the responses. The data presented in the meta-analyses are based on the published material. The authors of the included studies have not been contacted for further details. This review and recommendations are primarily based on an evaluation of the certainty of evidence in combination with consensus between the members of the multidisciplinary expert group, patient preferences, and benefits and harms.
Conclusion
Based on the identified benefits, the certainty of evidence, and patient preferences, the multidisciplinary expert group of this review concluded that manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture, and patient education can be considered as treatment approaches for TTH. No serious adverse events were identified for any of the included studies. Some positive effects were shown on headache frequency, quality of life, pain intensity and stress symptoms. Few studies and low sample sizes posed a challenge in drawing solid conclusions. Therefore, there is a need for high-quality RCTs in this field.
This NCG can be used by healthcare professionals as an aid in identifying and directing the patient with TTH to the appropriate treatment strategy targeting the patient’s needs and resources based on evidence.
Supplementary Information
Additional file 1. Additional tables and figures. Complete list of primary and secondary outcomes, AGREE and AMSTAR evaluations, flowcharts of litterature search and meta-analyses of secondary outcomes.
Acknowledgements
The authors wish to thank the following members of the reference group Anne Bülow-Olsen (Danish Migraine Association), Bent Ove Larsen (Denmark’s Patient Society for People with Headache), Jette Bach (Migraine and Headache Society), Lea Hegaard (The Danish Committee for Health Education), Beate Vesteskov and Ann Vilhelmsen (Danish Regions), Lise Holten (KL - Local Government Denmark), and Sonja Antic (Danish Regions).
Abbreviations
- DHA
Danish Health Authority
- ICHD
International Classification of Headache Disorders
- GRADE
Grading of Recommendation, Assessment, Development, and Evaluation
- MD
Mean Differences
- NCG
National Clinical Guideline
- NICE
National Institute for Health and Care Excellence
- PICO
Population, Intervention, Comparison and Outcome
- RCT
Randomised Clinical Trial
- RR
Relative Risk
- TTH
Tension-type Headache
Authors’ contributions
All authors constributed with study development. LSK contributed with drafting and revison of the manuscripts. HEC: contributed with statistics and data interpretation, KB: contributed with literature search. All authors commented on revised manuscripts and have read and approved the final version of the manuscript.
Funding
This study was supported by the Danish Health Authority.
Availability of data and materials
The datasets generated and analysed during the current study are available at the Danish Knowledge Centre on Headache Disorders webpage: https://videnscenterforhovedpine.dk/nkr/
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
DB is Advisory Board Member at: Novartis, Lilly, TEVA, conducted Clinical Trials for: Novartis, TEVA, Lilly, Lundbeck and received travel support from: Novartis, Allergan. HEC has reveived personal fees from Danish Knowledge Centre on Headache Disorders. HWC has reveived operating grants from Foundation for Chiropractic Research and Postgraduate Education. LNC has received grants from the Danish Health Authority. MJ is chairman of the board of the Danish Medical Acupuncture Society and owns an acupuncture clinic. LSK, KB, HW, HT, CVH and JMH declare that they have no competing interests.
Footnotes
The original online version of this article was revised: Following the publication of the original article, we were notified that the quality for Figure 1 needed improvement.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
10/6/2021
A Correction to this paper has been published: 10.1186/s10194-021-01329-0
References
- 1.Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z. Migraine remains second among the world's causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020;21(1):137. doi: 10.1186/s10194-020-01208-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saylor D, Steiner TJ. The global burden of headache. Semin Neurol. 2018;38(2):182–190. doi: 10.1055/s-0038-1646946. [DOI] [PubMed] [Google Scholar]
- 3.Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, Steiner TJ, Zwart JA. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 4.Hagen K, Åsberg AN, Uhlig BL, Tronvik E, Brenner E, Stjern M, Helde G, Gravdahl GB, Sand T. The epidemiology of headache disorders: a face-to-face interview of participants in HUNT4. J Headache Pain. 2018;19(1):25. doi: 10.1186/s10194-018-0854-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R. Has the prevalence of migraine and tension-type headache changed over a 12-year period? A Danish population survey. Eur J Epidemiol. 2005;20(3):243–249. doi: 10.1007/s10654-004-6519-2. [DOI] [PubMed] [Google Scholar]
- 6.Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lanteri-Minet M, et al. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15(1):31. doi: 10.1186/1129-2377-15-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain. 2010;11(4):289–299. doi: 10.1007/s10194-010-0217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bendtsen L, Ashina S, Moore A, Steiner TJ. Muscles and their role in episodic tension-type headache: implications for treatment. Eur J Pain. 2016;20(2):166–175. doi: 10.1002/ejp.748. [DOI] [PubMed] [Google Scholar]
- 9.Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barre J, Katsarava Z, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–711. doi: 10.1111/j.1468-1331.2011.03612.x. [DOI] [PubMed] [Google Scholar]
- 10.Bendtsen L, Evers S, Linde M, Mitsikostas DD, Sandrini G, Schoenen J. EFNS guideline on the treatment of tension-type headache - report of an EFNS task force. Eur J Neurol. 2010;17(11):1318–1325. doi: 10.1111/j.1468-1331.2010.03070.x. [DOI] [PubMed] [Google Scholar]
- 11.Centre NCG. Headaches: Diagnosis and Management of Headaches in Young People and Adults : Commissioned by the National Institute for Health and Clinical Excellence. London: National Clinical Guideline Centre (UK); 2012. [Google Scholar]
- 12.Ashina S, Mitsikostas DD, Lee MJ, Yamani N, Wang SJ, Messina R, Ashina H, Buse DC, Pozo-Rosich P, Jensen RH, Diener HC, Lipton RB. Tension-type headache. Nat Rev Dis Primers. 2021;7(1):24. doi: 10.1038/s41572-021-00257-2. [DOI] [PubMed] [Google Scholar]
- 13.Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 14.Coelho M, Ela N, Garvin A, Cox C, Sloan W, Palaima M, Cleland JA. The effectiveness of manipulation and mobilization on pain and disability in individuals with cervicogenic and tension-type headaches: a systematic review and meta-analysis. Phys Ther Rev. 2019;24(1-2):29–43. doi: 10.1080/10833196.2019.1572963. [DOI] [Google Scholar]
- 15.Lozano López C, Mesa Jiménez J, de la Hoz Aizpurúa JL, Pareja Grande J, Fernández de Las Peñas C. Efficacy of manual therapy in the treatment of tension-type headache. A systematic review from 2000-2013. Neurologia. 2016;31(6):357–369. doi: 10.1016/j.nrl.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Falsiroli Maistrello L, Geri T, Gianola S, Zaninetti M, Testa M. Effectiveness of trigger point manual treatment on the frequency, intensity, and duration of attacks in primary headaches: a systematic review and meta-analysis of randomized controlled trials. Front Neurol. 2018;9:254. doi: 10.3389/fneur.2018.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cerritelli F, Lacorte E, Ruffini N, Vanacore N. Osteopathy for primary headache patients: a systematic review. J Pain Res. 2017;10:601–611. doi: 10.2147/JPR.S130501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kamonseki DH, Lopes EP, van der Meer HA, Calixtre LB (2020) Effectiveness of manual therapy in patients with tension-type headache. A systematic review and meta-analysis. Disabil Rehabil. 12:1–10. 10.1080/09638288.2020.1813817 [DOI] [PubMed]
- 19.Falsiroli Maistrello L, Rafanelli M, Turolla A. Manual therapy and quality of life in people with headache: systematic review and meta-analysis of randomized controlled trials. Curr Pain Headache Rep. 2019;23(10):78. doi: 10.1007/s11916-019-0815-8. [DOI] [PubMed] [Google Scholar]
- 20.Luedtke K, Allers A, Schulte LH, May A. Efficacy of interventions used by physiotherapists for patients with headache and migraine: systematic review and meta-analysis. Cephalalgia. 2016;36(5):474–492. doi: 10.1177/0333102415597889. [DOI] [PubMed] [Google Scholar]
- 21.Anheyer D, Klose P, Lauche R, Saha FJ, Cramer H. Yoga for treating headaches: a systematic review and meta-analysis. J Gen Intern Med. 2020;35(3):846–854. doi: 10.1007/s11606-019-05413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anheyer D, Leach MJ, Klose P, Dobos G, Cramer H. Mindfulness-based stress reduction for treating chronic headache: a systematic review and meta-analysis. Cephalalgia. 2019;39(4):544–555. doi: 10.1177/0333102418781795. [DOI] [PubMed] [Google Scholar]
- 23.Gu Q, Hou JC, Fang XM. Mindfulness Meditation for Primary Headache Pain: A Meta-Analysis. Chin Med J. 2018;131:829–838. doi: 10.4103/0366-6999.228242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris P, Loveman E, Clegg A, Easton S, Berry N. Systematic review of cognitive behavioural therapy for the management of headaches and migraines in adults. Br J Pain. 2015;9(4):213–224. doi: 10.1177/2049463715578291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee HJ, Lee JH, Cho EY, Kim SM, Yoon S. Efficacy of psychological treatment for headache disorder: a systematic review and meta-analysis. J Headache Pain. 2019;20(1):17. doi: 10.1186/s10194-019-0965-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang J, Shen M, Qin X, Guo W, Li H. Acupuncture for the treatment of tension-type headache: an overview of systematic reviews. Evid Based Complement Alternat Med. 2020;2020:4262910. doi: 10.1155/2020/4262910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Shin BC, et al. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016;4:CD007587. doi: 10.1002/14651858.CD007587.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Probyn K, Bowers H, Mistry D, Caldwell F, Underwood M, Patel S, Sandhu HK, Matharu M, Pincus T, CHESS team Non-pharmacological self-management for people living with migraine or tension-type headache: a systematic review including analysis of intervention components. BMJ Open. 2017;7(8):e016670. doi: 10.1136/bmjopen-2017-016670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Headache Classification Subcommittee of the International Headache Society Headache classification Committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 30.Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic headache international study group. Headache. 1998;38(6):442–445. doi: 10.1046/j.1526-4610.1998.3806442.x. [DOI] [PubMed] [Google Scholar]
- 31.Ajimsha MS. Effectiveness of direct vs indirect technique myofascial release in the management of tension-type headache. J Bodyw Mov Ther. 2011;15(4):431–435. doi: 10.1016/j.jbmt.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 32.Castien RF, van der Windt DA, Grooten A, Dekker J. Effectiveness of manual therapy for chronic tension-type headache: a pragmatic, randomised, clinical trial. Cephalalgia. 2011;31(2):133–143. doi: 10.1177/0333102410377362. [DOI] [PubMed] [Google Scholar]
- 33.Brouwers MK, ME; Browman, GP; Cluzeau, F; Feder, G; Fervers, B; Hanna, S; Makarski, J; on behalf of the AGREE Next Step Consortium. Appraisal of guidelines for research & evaluation II: AGREE II instrument: update 2017. The AGREE Research Trust; 2009, 2013, 2017
- 34.Espí-López GV, Rodríguez-Blanco C, Oliva-Pascual-Vaca A, Benítez-Martínez JC, Lluch E, Falla D. Effect of manual therapy techniques on headache disability in patients with tension-type headache. Randomized controlled trial. Eur J Phys Rehabil Med. 2014;50(6):641–647. [PubMed] [Google Scholar]
- 35.Espí-López GV, Rodríguez-Blanco C, Oliva-Pascual-Vaca A, Molina-Martínez F, Falla D (2016) Do manual therapy techniques have a positive effect on quality of life in people with tension-type headache? A randomized controlled trial. Eur J Phys Rehabil Med 52(4):447–456. Accessed 7 June 2021 [PubMed]
- 36.Rolle G, Tremolizzo L, Somalvico F, Ferrarese C, Bressan LC (2014) Pilot trial of osteopathic manipulative therapy for patients with frequent episodic tension-type headache. J Am Osteopath Assoc 114(9):678–685. 10.7556/jaoa.2014.136. Accessed 7 June 2021 [DOI] [PubMed]
- 37.Álvarez-Melcón AC, Valero-Alcaide R, Atín-Arratibel MA, Melcón-Álvarez A, Beneit-Montesinos JV. Effects of physical therapy and relaxation techniques on the parameters of pain in university students with tension-type headache: a randomised controlled clinical trial. Neurologia. 2018;33(4):233–243. doi: 10.1016/j.nrl.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 38.Andersen LL, Mortensen OS, Zebis MK, Jensen RH, Poulsen OM. Effect of brief daily exercise on headache among adults--secondary analysis of a randomized controlled trial. Scand J Work Environ Health. 2011;37(6):547–550. doi: 10.5271/sjweh.3170. [DOI] [PubMed] [Google Scholar]
- 39.Cathcart S, Galatis N, Immink M, Proeve M, Petkov J. Brief mindfulness-based therapy for chronic tension-type headache: a randomized controlled pilot study. Behav Cogn Psychother. 2014;42(1):1–15. doi: 10.1017/S1352465813000234. [DOI] [PubMed] [Google Scholar]
- 40.Holroyd KA, Labus JS, Carlson B. Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: the role of disorder severity and psychiatric comorbidity. Pain. 2009;143(3):213–222. doi: 10.1016/j.pain.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Omidi A, Zargar F. Effects of mindfulness-based stress reduction on perceived stress and psychological health in patients with tension headache. J Res Med Sci. 2015;20(11):1058–1063. doi: 10.4103/1735-1995.172816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jena S, Witt CM, Brinkhaus B, Wegscheider K, Willich SN. Acupuncture in patients with headache. Cephalalgia. 2008;28(9):969–979. doi: 10.1111/j.1468-2982.2008.01640.x. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization . Global recommendations on physical activity for health. Geneva: WHO; 2010. [PubMed] [Google Scholar]
- 44.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7(1):10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brouwers MK, Kho ME, Browman GP, Cluzeau F, Feder G, Fervers B, Hanna S, Makarski J, on behalf of the AGREE, Consortium; NS Appraisal of guidelines for research & evaluation II: AGREE II instrument: updated 2013. The AGREE Research Trust 2009, p 2013
- 46.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Covidence Team. Covidence [Available from: https://covidence.org]
- 48.Review Manager (RevMan) [Computer program]: Version 5.3. Cochrane Collaboration; 2014
- 49.France S, Bown J, Nowosilskyj M, Mott M, Rand S, Walters J. Evidence for the use of dry needling and physiotherapy in the management of cervicogenic or tension-type headache: a systematic review. Cephalalgia. 2014;34(12):994–1003. doi: 10.1177/0333102414523847. [DOI] [PubMed] [Google Scholar]
- 50.Potter R, Probyn K, Bernstein C, Pincus T, Underwood M, Matharu M. Diagnostic and classification tools for chronic headache disorders: a systematic review. Cephalalgia. 2019;39(6):761–784. doi: 10.1177/0333102418806864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bendtsen L, Bigal ME, Cerbo R, Diener HC, Holroyd K, Lampl C, Mitsikostas DD, Steiner TJ, Tfelt-Hansen P, International Headache Society Clinical Trials Subcommittee Guidelines for controlled trials of drugs in tension-type headache: second edition. Cephalalgia. 2010;30(1):1–16. doi: 10.1111/j.1468-2982.2009.01948.x. [DOI] [PubMed] [Google Scholar]
- 52.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340(mar23 1):c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Additional tables and figures. Complete list of primary and secondary outcomes, AGREE and AMSTAR evaluations, flowcharts of litterature search and meta-analyses of secondary outcomes.
Data Availability Statement
The datasets generated and analysed during the current study are available at the Danish Knowledge Centre on Headache Disorders webpage: https://videnscenterforhovedpine.dk/nkr/