Abstract
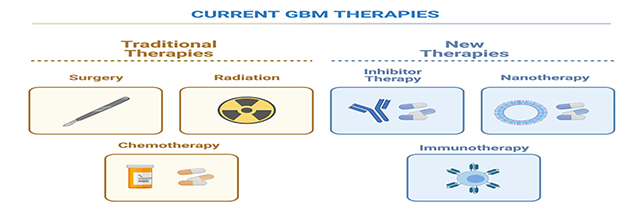
Glioblastoma multiforme (GBM) is a WHO grade IV glioma and the most common malignant, primary brain tumor with a 5-year survival of 7.2%. Its highly infiltrative nature, genetic heterogeneity, and protection by the blood brain barrier (BBB) have posed great treatment challenges. The standard treatment for GBMs is surgical resection followed by chemoradiotherapy. The robust DNA repair and self-renewing capabilities of glioblastoma cells and glioma initiating cells (GICs), respectively, promote resistance against all current treatment modalities. Thus, durable GBM management will require the invention of innovative treatment strategies. In this review, we will describe biological and molecular targets for GBM therapy, the current status of pharmacologic therapy, prominent mechanisms of resistance, and new treatment approaches. To date, medical imaging is primarily used to determine the location, size and macroscopic morphology of GBM before, during, and after therapy. In the future, molecular and cellular imaging approaches will more dynamically monitor the expression of molecular targets and/or immune responses in the tumor, thereby enabling more immediate adaptation of tumor-tailored, targeted therapies.
Keywords: glioblastoma, radiotherapy, chemotherapy, targeted therapy, nanotherapy, immunotherapy
Graphical Abstract
2. Introduction
2.1. The epidemiology and etiology of GBM
Glioblastoma multiforme (GBM) is a WHO grade IV brain tumor which represents one of the most lethal human cancers. The incidence of GBM increases with age and shows the highest incidence in the 75 to 84-year old age group in the United States(1). The incidence is higher in men than women, as well as in Caucasians than in other ethnicities(2). According to gene profile analysis and genetic modeling of GBM in mice, there is evidence that GBM is derived from neural stem cells (NSCs), NSC-derived astrocytes, and oligodendrocyte precursor cells (OPCs)(3). GBM tumors derived from different cellular origins show different behaviors in animal models(3)(Fig.1). Exposure of the central nervous system (CNS) to ionizing radiation has been associated with an increased risk to develop malignant brain gliomas, excess relative risk (ERR) estimates for brain/CNS tumors ranged per Gy from 0.19 (95% confidence interval [CI]: 0.03, 0.85) to 5.6 (95% CI: 3.0, 9.4) (4).
Fig.1.

Cellular origin and heterogeneity of glioblastoma multiform (GBM). GBM tumors originate from three types of cells in the brain parenchyma: neural stem cells (NSCs), NSC-derived astrocytes, and oligodendrocyte precursor cells (OPCs). GBM is characterized by extensive intertumor and intratumor heterogeneity, and has, therefore, been divided into four sub-groups: mesenchymal, classical, proneural, and neural.
2.2. The ongoing challenges of GBM treatment
Standard therapy for GBM encompasses surgical resection followed by chemoradiotherapy, using temozolomide (TMZ)(5). However, 5-year survival is only 7.2% in the United States according to CBTRUS Statistical Report 2020(6). Despite maximal surgical resection and aggressive adjuvant therapy, almost all GBM tumors locally recur after treatment(7). Ongoing challenges to GBM treatment include its incomplete resection, high degree of genetic heterogeneity, exclusive blood brain barrier (BBB), and immunosuppressive microenvironment.
2.2.1. High infiltration
The highly infiltrative nature of GBM makes complete resection at the cellular level nearly impossible(8). Also, abundant hypoxic regions provide perivascular niches for glioma initiating cells (GICs). These self-renewing cells can yield potentially more aggressive recurrent tumors that are radioresistant and chemoresistant (9, 10).
2.2.2. Intertumor and intratumor heterogeneity
Large intertumor and intratumor heterogeneity have complicated targeted therapy development(11). Based on their genetic and epigenetic markers, GBMs were previously classified by The Cancer Genome Atlas (TCGA) into four clusters: mesenchymal, classical, proneural, and neural(12, 13). Mesenchymal GBMs are characterized by the neurofibromin 1 (NF1) tumor suppressor gene mutation as well as by frequent mutations in the PTEN and TP53 tumor suppressor genes. The classical subtype is highly proliferative and characterized by EGFR amplification, but no TP53 mutation. Meanwhile proneural GBM is frequently associated with TP53 mutation, and uniquely with IDH1 and PDGFRA mutations. The neural subtype is characterized by many genes which also exist in the brain’s normal noncancerous neurons(12, 14). Another GBM tumor transcriptome analysis described only three subtypes: proneural, classical, mesenchymal. The authors proposed that the neural subtype may be due to contamination of the original samples with non-tumor cells(13, 15). The mesenchymal and classical subtypes are typically more aggressive tumors, while the proneural subtype is less aggressive and more often seen in younger patients(13). The proneural-to-mesenchymal phenotype transition is associated with GBM resistance (16). Even though TCGA has categorized GBM into four subgroups, recent studies show that different GBM subgroups vary spatially and temporally within the same tumor(17). Patel et al. showed with single cell RNA sequencing that a single tumor can include a diversity of cells that comprise all the GBM subgroups(18)(Fig. 1).
2.2.3. Blood brain barrier (BBB)
Another challenge to GBM treatment is delivering chemotherapeutic drugs across the blood brain barrier (BBB). The BBB is a protective boundary between the circulatory system and the extracellular space of the central nervous system. The BBB is mainly composed of endothelial cells that form a tight barrier along the wall of blood vessels and selectively limit the compounds that can cross into the parenchyma(19). Tight junctions are less than 1 nm in size and prohibit penetration of >98% of small molecules. Unlike in healthy brain tissue, the BBB in GBM exhibits enhanced permeability due to poorly formed, leaky blood vessels, upregulated transporter proteins, and downregulated tight junction proteins(20, 21). However, the disruption of the BBB is not uniform throughout a given tumor, with some areas exhibiting blood vessels with higher permeability and other tumor areas with more intact vessels and/or vascular shunts. Even if a chemotherapeutic drug managed to extravasate into the tumor tissue, it can often not gain therapeutic levels in tumor cells due to upregulation of efflux pumps by glioblastoma cells (22). Ultimately there remains a substantial proportion of GBM with locoregional intact BBB and upregulated efflux pumps (23, 24).
2.2.4. Immunosuppressive microenvironment
The microenvironment of GBM creates treatment challenges. Some authors refer to GBM with an immunosuppressive microenvironment as “cold tumors”. These tumors lack pre-existing tumor T cell infiltration which results in tumor resistance to immune checkpoint inhibitors (25). These tumors are further characterized by their lack of tumor antigens, defects in antigen presentation, and high accumulation of immunosuppressive cells (26, 27). Treatment with immune checkpoint inhibitors shows limited efficacy (28). In contrast, “hot tumors” are infiltrated with swarms of T cells, and thus more immunogenic. Turning “cold” to “hot” may be achieved by combinatorial approaches that boost anti-tumor immunity (27).
Given the genomic complexity and global alterations of multiple signaling pathways in GBM, consistent effort has been put forth to improve systemic therapies for glioblastoma. In the following sections, we will address how pharmacologic therapies have evolved, how mechanisms of resistance develop, and how new strategies have emerged.
3. GBM traditional therapy and resistance
3.1. Traditional therapy
3.1.1. Surgical resection
Surgical resection of brain tumors was revolutionized in the late ‘80s and early ‘90s with the development of frameless stereotaxy. It enabled the very precise placement of surgical instruments using image guidance and has been modernized with new imaging technologies(29). Additionally, cerebral cortical stimulation has enabled intraoperative localization of eloquent cortex regions of the brain that need be avoided during surgery. This technique, or “brain mapping” accounts for individual variations in anatomy or tissue reorganization to remove tumor in areas of great functional importance and that are responsible for quality of life(30, 31).
The extent of tumor resection has been positively correlated with survival time, with gross total resection (GTR) being desirable when possible(1, 32–36). There are, however, major challenges to achieving GTR, including successful identification of tumor margins as well as avoiding adjacent eloquent cortex. Even though the tumor margins can be roughly determined through imaging, GBM grows with microscopic, finger-like projections, imperceptible to presurgical or even intraoperative imaging techniques(37).
Imaging is an increasingly important tool for GBM resection(29). Images can guide biopsies(38–40), identify tumor margins(41–43), and localize critical brain structures that need to be spared(44). Computed tomography (CT) is valuable for emergent imaging, while MRI is the gold standard for brain tumor imaging due to its the higher anatomical resolution and higher soft tissue contrast. Depending on the MRI contrast and pulse sequence used, important features of the tumor and brain tissue can be elucidated including blood vessels, tumor necrosis, and hemorrhage (T1-weighted with contrast), cerebrospinal fluid (T2-weighted), blood perfusion (dynamic susceptibility contrast (DSC), dynamic contrast enhanced (DCE) and arterial spin labeling (ASL)(45, 46). Some studies have advocated supramaximal resection, thereby resecting beyond the T1 contrast enhancing portion(47).
Both intraoperative fluorescence imaging and MR imaging can help to address the challenging phenomenon of “brain shift” or movement of the brain during surgery, which can lead to discrepancies between the location of the tumor and critical brain structures on preoperative imaging studies and in the operating room. Some shifts can be up to 2 cm in distance and result from causes that are physical (e.g., patient position, gravity), surgical (types of equipment used, tissue/fluid loss during procedure), or biological (e.g., tumor type/location, drugs used to manage intracranial pressure). Unfortunately, this phenomenon worsens with increasing duration of the surgery and cannot be corrected for using neuronavigational devices that derive stereotaxic capabilities from pre-operative MRI images(48).
Fluorescent imaging has been performed with fluorescein, indocyanine green (ICG), and 5-aminolevulinic acid (5-ALA)(49–52). Fluorescein is of historical relevance, as it is one of the first intraoperative imaging adjuncts. While fluorescein does not typically cross an intact the BBB, it does penetrate high grade gliomas (HGGs) in areas of enhanced permeability(53). Likewise, ICG has been of historical value, primarily for angiography and vessel delineation rather than parenchymal margins. Currently, 5-aminolevulinic acid (5-ALA) has become the standard of care among intraoperative fluorescent agents and has received regulatory approval in the US and Europe(49). 5-ALA is a precursor to heme that can cross the BBB and converts to the fluorescent compound protoporphyrin IX in the mitochondria. The mechanisms underlying its accumulation in brain tumors are still not well understood. It exhibits higher specificity over fluorescein (67% vs 33%)(54). Studies have also shown that GTR or near-GTR rate is higher in patients that underwent fluorescence-guided surgery with 5-ALA compared to patients that were operated under white light only (65% vs 36%)(50). Additional clinical trials are now being performed using IRDye800CW and ZW800–1 for targeted imaging(55, 56),
Intraoperative MRI and ultrasound (iMRI and iUS, respectively) help surgeons identify residual cancer in surgeries (57, 58). The surgeon resects a brain tumor, then performs a contrast-enhanced MRI in the operating room on an intraoperative MRI scanner. If residual enhancing tissue is found, then this residual tissue is removed in the same surgery.
3.1.2. Chemotherapy
3.1.2.1. Cytotoxic chemotherapy
The standard post-surgical treatment regimen includes 6 weeks of concomitant TMZ (75 mg/m2) and radiation followed by adjuvant TMZ (150–200 mg/m2) for 5 days every 28 days for six cycles(59). TMZ, the most widely used chemotherapeutic drug for GBM, is a small molecular alkylating agent that directly damages tumors by methylating the purine bases of DNA(60). The key cytotoxic action is through formation of O6-methylguanine lesions which results in apoptosis, autophagy, and cellular senescence(61–64). In addition, it was discovered that TMZ has radiation-sensitizing properties. It increases the likelihood of radiation-induced DNA double strand breaks and cell death when the drug is administered at the same time as radiation therapy(65).
The most common side effect from TMZ is hematologic toxicity(66). Thrombocytopenia has been identified in 10–20% of patients. In a Phase II clinical trial, the addition of a thrombopoietin receptor agonist, Romiplostin to adjuvant CCRT (concurrent chemoradiation therapy) has increased the rate of completed regimens(67). Nonhematologic toxicities from TMZ are less common and include nausea, anorexia, fatigue, and hepatotoxicity(68).
Several nitrosourea reagents have also been explored for GBM treatment. Carmustine (also known as BCNU) is a small nitrogen mustard compound and alkylating agent. It induces interstrand crosslinks between the guanine and cytosine bases in DNA(69). Carmustine rose to prominence with the advent of Gliadel® wafers, which are FDA (U.S. Food and Drug Administration Agency)-approved biodegradable discs that are intraoperatively placed in the resection cavity to provide a slow release of drug over two weeks(70). The alkylating therapeutic effects of carmustine can be reversed by the enzyme alkyl guanine transferase (AGT). Therefore, carmustine is sometimes used in concert with AGT inhibitors to ensure therapeutic efficacy(71). Side effects include abnormal wound healing and intracranial infections since the wafers present as foreign bodies(72). Another alkylating anti-tumor reagent is lomustine. Due to its high lipophilicity and small size, lomustine can cross the BBB. Thus, lomustine can be given orally(73). Fotemustine, another molecule in this family of drugs, has been used for melanoma and is now tested for its efficacy with recurrent glioblastoma(74).
3.1.2.2. Anti-angiogenic chemotherapy
Bevacizumab is a humanized monoclonal antibody with anti-angiogenic properties and is administered intravenously. It binds to and inhibits vascular endothelial growth factor A (VEGF-A) which initiates growth of new blood vessels when bound to its receptor. The levels of VEGF-A in GBM are estimated to be approximately 30 times higher than in low grade astrocytomas making it an attractive therapeutic target. While bevacizumab appears to improve progression-free survival, it does not significantly improve overall survival for patients with newly diagnosed glioblastoma(75). Therefore, it is predominantly used to treat recurrent glioblastomas. The use of bevacizumab with irinotecan a small molecular prodrug that is converted a topoisomerase I inhibitor, is being explored(76, 77). Bevacizumab’s side effects most commonly include hypertension and leukopenia(74, 78).
3.1.3. Radiation therapy (RT)
Radiation therapy can be utilized in several forms (e.g., x-ray photons, gamma photons, protons), but not all have become validated for standard of care (Table 1). Conceptually, it can be administered to help provide local control for the microscopic disease unaddressed by surgical resection. In CCRT, patients receive 3D conformal RT which uses x-ray photons that are directed at the tumor target from several different angles. CT and MRI images are used to plan the delivery of the therapeutic dose to the tumor site. Radiation therapy is usually distributed over 6 weeks in 2 gray (Gy) fractions for a total dose of 40–60 Gy(79). A typical device for RT possesses elaborate multi-leaf collimators which allow very specific shaped beams to target the tumor and provide a small (1–2 cm) margin around the periphery. Treatment with x-rays confers low linear energy transfer which results in both direct and indirect biological damage. Direct damage to DNA makes up approximately one-third of the treatment effect, and indirect effects (namely, ionization of water to produce free radicals which damage DNA), make up approximately two-thirds(80).
Table 1.
Summary of therapeutic strategies to treat GBM.
| Treatment | Biological Action | Notes |
|---|---|---|
| Image-guided Surgery | ||
| Intraoperative ultrasonography | tumor removal | Routine clinical use. Used in ORs for maximal safe resection of brain tumors since the 1980s. |
| Intraoperative MRI | tumor removal | Routine clinical use. The first iMRI system was installed in 1994 at Brigham and Women’s Hospital. |
| Intraoperative fluorescence imaging | tumor removal | New clinical use. In 2017, Gleolan® (5-aminolevulinic acid) was FDA-approved for intraoperative fluorescence imaging. |
| Chemotherapy (small Molecules) | ||
| Temozolomide | alkylates DNA base pairs | Routine clinical use. Approved by the FDA in 1999 as a monotherapy and again in 2005 for use in newly diagnosed GBM concomitantly with radiotherapy and as maintenance treatment. |
| Carmustine (BCNU) | alkylates DNA base pairs | Routine clinical use. Gliadel® wafers were approved by the FDA for recurrent GBM in 1997 and for the newly diagnosed high-grade gliomas (III and IV) in 2003. |
| Lomustine (CCNU) | alkylates DNA base pairs | Routine clinical use. FDA approved in 2014 for patients with brain tumors following surgery and/or radiotherapy. |
| Fotemustine | alkylates DNA base pairs | Approved in Europe but not in the US. Phase II clinical trials have shown therapeutic benefit in recurrent GBM. |
| Radiation therapy (RT) | ||
| 2D conventional RT | creates DNA double-strand breaks and ROS | Routine clinical use. Largely being phased out for brain RT. Still used in some instances of uncomplicated bone metastases. |
| 3D conformal RT | creates DNA double-strand breaks and ROS | Routine clinical use. Good for advanced and inoperable tumors; used post-operatively. |
| Intensity-modulated RT | creates DNA double-strand breaks and ROS | Routine clinical use as adjuvant therapy after surgical tumor resection. |
| Stereotactic radiosurgery (SRS) | creates DNA double-strand breaks and ROS | Routine clinical use with either a gamma emitter (e.g., Gamma Knife) or a linear accelerator (e.g., Cyber Knife). |
| Brachytherapy | creates DNA double-strand breaks and ROS | Clinical adoption is slow due to adverse events and risk of exposure to people in close proximity to the patient. |
| Particle RT (Proton therapy) | creates DNA double-strand breaks and ROS | FDA approved but reimbursement for the procedure is low. Phase II clinical trials are underway to evaluate the efficacy of proton versus photon irradiation (NCT02179086, NCT01854554). |
| Inhibitor Therapy | ||
| Bevacizumab (mAb) | inhibits VEGF-A | Routine clinical use. FDA approved for recurrent GBM in 2009. |
| Irinotecan (CPT-11) (small molecule) | inhibits topoisomerase I | Phase I/II trials for recurrent GBM showed mixed results. Phase II clinical trials for combination therapies are under way for recurrent and pediatric GBM (NCT04267978, NCT02192359). |
| Veliparib (ABT-888) (small molecule) | inhibits PARP | Phase II trials in adults with recurrent (NCT01026493) and new (NCT00770471, NCT02152982) GBM showed limited benefit. A phase I/II study of veliparib with RT and TMZ in children with diffuse intrinsic pontine glioma reported little to no survival benefit (NCT01514201). |
| Olaparib (AZD-2281, MK-7339) (small molecule) | inhibits PARP | Phase II trials in recurrent GBM are ongoing (NCT03212274). Olaparib exacerbated hematological toxicities when used with TMZ in patients with recurrent GBM (NCT01390571). Further studies are warranted to understand potential clinical benefit. |
| Niraparib (MK-4827) (small molecule) | inhibits PARP | A phase I trial evaluated niraparib and TMZ in advanced cancer but with few GBM patients (NCT01294735). A phase II trial evaluating niraparib with TTFs in recurrent GBM is underway (NCT04221503). May be good treatment option for tumors over-expressing EGFR. |
| Pamiparib (BGB-290) (small molecule) | inhibits PARP | Phase I/II trials are underway studying pamiparib with TMZ in new and recurrent GBM (NCT03914742, NCT03150862). |
| Cediranib (AZD-2171) (small molecule) | inhibits VEGFR | Phase II-III trials in recurrent GBM showed little to no benefit. Some studies may be underpowered or lack proper patient selection (NCT00777153, NCT01310855, NCT00305656). A phase II trial is comparing cediranib and olaparib to bevacizumab for recurrent GBM (NCT02974621). |
| Gossypol (AT-101) (small molecule) | binds with and inhibits Bcl-2, Bcl-xL and Mcl-1 | Phase II trials were performed in recurrent and new GBM (NCT00390403, NCT00540722). Very little follow-up data exists. |
| Cabozantinimb (XL-184) (small molecule) | tyrosine kinase inhibitor | Phase II trial in adult patients with recurrent GBM showed modest clinical activity (NCT00704288). Phase II trial in pediatric patients with recurrent or progressive high grade gliomas is ongoing (NCT02885324). |
| Erlotinib | EGFR inhibitor | Phase II studies in recurrent GBM as monotherapy (NCT00337883,) and in combination with other therapies (NCT00039494, NCT00445588, NCT00525525 NCT00335764). Also evaluated in new GBM (NCT00187486, NCT00720356). Clinical results have not confirmed benefit. |
| Gefitinib | EGFR inhibitor | Phase II trials in new and recurrent GBM for both adult and pediatric patients (NCT00052208, NCT00014170, NCT00025675, NCT00042991). |
| Depatuxizumab mafodotin (ABT-414) | Ab targets EGFR and drug inhibits tubulin | Phase III trial was halted when no survival benefit for new GBM patients could be demonstrated over placebo plus TMZ/radiation (NCT02573324). |
| Imatinib | multi-targeted tyrosine kinase inhibitor | Phase II trials in new and recurrent GBM showed no clinical activity. Drug has poor BBB penetration. |
| Dasatinib | multi-targeted tyrosine kinase inhibitor | Phase I/II clinical trials in recurrent GBM failed to show treatment efficacy and have been limited by toxicity, especially when used in combination with a second chemotherapy (NCT00948389, NCT00423735). |
| Sorafenib | multi-targeted protein kinase inhibitor | Clinical trials to date have not been promising. Ongoing phase I/II trial evaluating sorafenib + everolimus (NCT01434602) and sorafenib, valproic acid, and sildenafil (NCT01817751) in recurrent high grade gliomas. |
| Sunitinib | multi-targeted protein kinase inhibitor | Several phase II clinical trials have not shown anti-glioma effects. There are no ongoing clinical trials known currently. |
| Temsirolimus (CCI-779) | inhibits mTOR | Phase I/II trials as a mono- and co-therapy mostly for recurrent GBM (NCT00329719, NCT00112736, NCT00022724). Little added benefit. |
| Everolimus | inhibits mTOR | Underway: Phase II trial evaluating combination with sorafenib (NCT01434602), Phase I trial evaluating combination with ribociclib in children (NCT03355794). |
| Liposomes | ||
| 2B3–101 PEGylated liposomes | Target GSH/GSH transporters | Phase I/IIa trial to explore the preliminary antitumor activity of 2B3-101 in brain metastases or recurrent malignant glioma (NCT01386580). |
| SGT-53 Cationic liposomes | Target Scfv/TfR | Phase II trial of combined temozolomide and SGT-53 for treatment of recurrent glioblastoma (NCT02340156). |
| Liposomal irinotecan | convection enhanced delivery (CED) | Phase II trial of convection-enhanced, image-assisted delivery of liposomal-irinotecan in recurrent high grade glioma (NCT02022644). |
| Immunotherapy | ||
| Cemiplimab | checkpoint inhibitor that binds to PD-1 | Phase II trials are underway for recurrent (NCT04006119) and newly diagnosed (NCT03491683) GBM. |
| Nivolumab | checkpoint inhibitor that binds to PD-1 | Phase III trials are underway for recurrent (NCT02017717) and newly diagnosed (NCT02617589, NCT02667587) GBM. |
| Rindopepimut peptide vaccine | targets EGFR deletion mutation EGFRvIII | Phase III clinical trial is ongoing (NCT01480479). |
| DCVax®-L | DCs are primed to recognize tumor-specific antigens | Ongoing phase III clinical trial (NCT00045968). |
| VB-111 (Ofranergene obadenovec) gene therapy using an adenovirus type 5 vector | Virus carries a trans-gene for chimeric death receptor that connects Fas to hTNF receptor 1. | Phase I/II trials showed statistically significant improvement for VB-111 monotherapy in recurrent GBM (NCT01260506). Phase III trial using dual administration of VB-111 and bevacizumab failed to improve outcomes in recurrent GBM. (NCT02511405). |
| CAR T cell therapy | T cells are engineered to express receptors against specific tumor markers | There are currently 19 clinical trials listed under clinicaltrials.gov, including ongoing studies NCT04385173, NCT04077866, NCT04045847, NCT04045847, NCT04214392, NCT04003649, NCT02937844, NCT03392545, NCT02208362, NCT0338923 |
| Misc. Therapies | ||
| Laser interstitial thermal therapy (LITT) | thermal ablation of tumor tissue | Studied for its applications toward tumor therapy and treatment of radiation necrosis. Current clinical trials: NCT02970448 (Phase I: LITT + chemoradiation for new HGGs), NCT03341806 (Phase 1: LITT + avelumab for recurrent GBM), NCT04699773/ NCT04181684 (LITT + hypofractionated RT for new/recurrent GBM) |
| Tumor Treating Fields (TTF) | disrupts mitotic cell division | May be good for recurrent GBM, inoperable tumors, and/or effective supplement to chemo/radiotherapy |
Conformal RT has been preferred in the clinic over whole brain radiation since recurrent gliomas tends to appear within 2 cm from the original tumor site in 80–90% of cases(81). Thus, conformal RT is designed to target the majority of residual GBM cells while sparing healthy brain tissue and thereby, minimize cognitive side effects. Intensity-modulated RT also uses multi-leafed collimators, but can redistribute ionizing radiation across the target depending on its location and sensitivity(82). This strategy has the added complexity of employing several collimated beams in order to avoid injury to critical structures including the cornea, optic nerves, and brainstem(83).
Another form of focal radiation includes stereotaxic radiosurgery (SRS) where even larger radiation doses can be applied by delivering multiple non-parallel, converging radiation beams. The dose is given in fewer fractions (1–5) and at higher doses per fraction (15+ Gy). The gamma radiation is derived from a cobalt-60 source and directed at the tumor through collimators(84). The heat transfer properties of gamma rays enable high doses of radiation to be delivered very specifically at the tumor target while sparing adjacent healthy tissues(85). SRS has been commonly used for brain metastases, particularly to avoid the cognitive side effects of whole brain RT, and may be appropriate in some cases of GBM(86).
Brachytherapy is being explored and involves local implantation of one or more radioactive vectors into the tumor bed at the time of surgery. The most common isotopes used for brachytherapy in brain tumors are iodine125 (t1/2 = 59.5 days) and iridium-192 (t1/2 = 73.8 days)(87). Unfortunately, two major trials by Laperriere et al. and Selker et al. did not show a statistically significant differences in survival between patients receiving brachytherapy and those that did not(88, 89). Another Phase I trial was halted early due to high toxicity(90). Adverse effects have included symptomatic radiation necrosis, vascular injury, and radiation exposure to close contacts(91).
Charged heavy proton radiotherapies such as carbon ion irradiation spares normal tissue and concentrates energy deposition on the tumor(92). This disrupts GIC viability(93) through the induction of pro-apoptotic pathways and thereby provides an antiangiogenic and immunopermissive tumor environment(94). Tumor regression and long-term local control were identified in xenograft mouse models and a clinical study of 50 patients with grade III and IV glioma measured an 18-month overall survival of 73% with dose equivalents of ≥ 60 gray appearing to be safe (93, 95). Indeed, combination therapies of carbon proton irradiation with TMZ treatment led to enhanced overall survival and progression-free survival compared to patients subjected to combination of TMZ with photon-induced irradiation(95).
An important impediment of effective RT is the hypoxic tumor environment. Oxygen generally enhances the response of cells to low linear energy transfer radiation. When tissue is irradiated and DNA radicals form, oxygen can react with the radicals to create permanent cell damage. In hypoxic tumor environments, the damaged DNA has added time to repair and reduce radiation injury(80). Hypoxic tissue is thought to require approximately three times the radiation dose to achieve the same therapeutic benefit(96).
3.2. GBM therapy resistance
3.2.1. DNA repair mechanism
3.2.1.1. Methyl guanine methyl transferase (MGMT)
TMZ causes tumor cytotoxicity by transferring methyl groups to DNA (70% at N7-guanine sites, 10% at N3-adenine sites and 5% at O6-guanine sites)(97). The O6 site alkylation on guanine leads to attachment of a thymine rather than a cytosine during the DNA replication process. The altered configuration is the primary cause of cell death(98). This alkylation damage can be reversed by the DNA repair enzyme MGMT (O6-methylguanine-DNA methyltransferase) by removing O6-methylguanine adducts. Thus, the methylation status of the MGMT gene promoter has great clinical significance(99, 100). MGMT promoter methylation is more prevalent in recurrent GBMs compared to primary GBMs (75% vs. 36%)(101). The level of MGMT protein expression has been associated with the efficacy of alkylating drugs to cancer cells in glioma tumor models (98, 102). GBM with MGMT promoter methylation (evaluated by methylation-specific PCR (MS-PCR)) and its subsequent loss of MGMT protein expression (measured by immunohistochemical staining) showed better response to TMZ therapy(103). MGMT inactivation or silencing is associated with significantly improved overall survival and progression-free survival (PFS)(104–106). The role of TMZ in CCRT has made MGMT one of the most pertinent prognostic markers.
Understanding the regulation of MGMT may improve the development of targeted therapies. An important gene related to MGMT expression is p53, a negative regulator of MGMT in GBM tumors (107–109). Clinically, GBM patients with lower MGMT expression have better prognoses with proneural phenotypes expressing p53(110). The proline-rich domain of p53 has been confirmed to be non-essential for MGMT-dependent DNA repair(111). However, p53 may down-regulate MGMT via interaction with the Sp1 transcription factor(112). This was supported when BACH overexpression competitively interfered with p53 and Sp1 binding, and antagonized MGMT expression(108). Sp1 is an imperative nuclear transcription factor, which suggests the role of transcriptional factors in regulating MGMT expression. In silico analysis by Transcription Elements Search System (TESS, http://www.cbil.upenn.edu/tess) identified putative consensus sequences for the binding of nuclear transcription factors in the promoter region of MGMT. These include Sp1, NF-κB, CEBP, AP-1, AP-2 and NF-IL6 at CpG dinucleotides. The literature has also supported Sp1(112–114), AP-1(102, 115), NF-κB(116, 117) in the activated transcription of MGMT. Thus, methylation of CpG dinucleotides may hinder the binding of these transcription and compress the transcriptional activation of the MGMT gene(102, 118, 119). Other transcription factors, such as hypoxia-inducible factor-1 (HIF-1), when activated in the hypoxic GICs niche, will enhance MGMT expression(120–122).
Besides transcriptional factors, epigenetic modifications of MGMT have also shown a relevant role in MGMT regulation(123, 124). Acetylation of lysine residues on histones H3 and H4 (H3Ac and H4Ac) is correlated with high MGMT expression(125) while di-methylation of lysine 9 of histone 3 (H3me2K9) leads to silencing of MGMT expression(102).
Thus, targeting transcriptional factors or epigenetic modifications related to MGMT activation may be options in GBM therapy.
3.2.1.2. Mismatch repair (MMR)
O6-methylguanine (O6-MeG) generated by therapeutic alkylating agents is the dominant cytotoxic lesion. It can either be removed by MGMT or tolerated by MMR deficiency, to induce prominent therapy resistance(126). MMR addresses inappropriate nucleotide base pairing to maintain DNA replication fidelity. MMR is collectively achieved by several proteins including MLH1, MLH3, MSH2, MSH3, MSH6, PMS1, and PMS2(127). Outside the context of TMZ treatment, MMR deficiency or epigenetic silencing of MMR gene expression leads to cancer development(128, 129). MMR deficiency results in strong resistance to the alkylating agents, such as the alkylating agents N-methyl-N′-nitro-N-nitrosoguanidine (MNNG), TMZ, or procarbazine. When MGMT is not present to remove the methyl group, thymine is erroneously inserted opposite O6-MeG by DNA polymerase. The O6-MeG:T mismatch is recognized by the MMR complex, and bound by MutSα (an MSH2•MSH6 heterodimer), subsequently, a gap is generated in a new stretch of single-stranded DNA, DNA polymerase once again inserts thymine to complete mismatch repair. It is highly likely that the futile repair generates double strand breaks leading to cell cycle arrest and cell death(130).
Perazzoli et al. noticed an interesting inverse correlation between MGMT and MMR (131). In vitro studies investigating an MGMT-methylated GBM cell line (U251), which survived TMZ treatment, ultimately developed MMR deficiency(132). Studies from TCGA suggest that at least one of the MMR genes - MLH1, MSH2, MSH6 or PMS2 - possess a methylated MGMT promoter(133). MSH6 inactivation exhibited a crucial role in conferring tolerant tumor cell growth. It has been shown that a modest decrease of MMR components MSH2 and MSH6 is associated with TMZ sensitivity(134). Sun et al reported that a large cohort of GBM clinical samples have enhanced expression of MMR genes especially MSH6 after long-term TMZ treatment(135). Whether the incidence of MSH6 mutation is induced by therapy is still unknown and remains controversial. The German Glioma network noticed significantly lower MSH2, MSH6, and PMS2 protein expression in recurrent GBM compared to primary GBM tumors(136), which is in line with some additional investigations(137). Meanwhile, recurrent GBM tumors frequently possess MMR6 mutations coinciding with microsatellite instability(138).
3.2.2. Glioma initiating cells (GICs)
A subpopulation of cells in GBM described as “cancer stem cell (CSC)” or “glioma initiating cells (GICs)” is speculated to possess specific characteristics that support tumor development, recurrence, and therapeutic resistance(10, 139, 140). GICs are believed to be a distinct subgroup of cells, that can undergo self-renewal and initiate tumorigenesis. Singh et al. first described a population of CD133+ cells, but not CD133- cells, that initiated tumor growth in NOD-SCID (non-obese diabetic, severe combined immunodeficient) mouse brains(141). Although CD133 is a recognized marker of GICs, it is also expressed in normal neural stem cells(142). Therefore, multiple surface markers are needed to characterize GICs. Other recognized markers of GICs include CD44 and ATP binding cassette transporters (143–145). We further elaborate on the molecular mechanisms of resistance in GICs.
3.2.2.1. Enhanced DNA repair capacity
In addition to protective responses by MGMT and MMR expression following chemotherapy, GICs may exhibit sensitizing mechanisms to radiation(146). Checkpoint kinases (Chks), in particular Chk1 and Chk2, play primary roles in cell cycle control. In response to DNA damage, Chk1 signal will be activated and holds the cells in the G2 phase until DNA is repaired and ready for the mitotic phase, whereas Chk2 is activated under double stranded break (DSB) and prevents cells from dividing in an uncontrolled manner. Bao et al reported that GBM displayed aberrant DNA damage response to radiotherapy. They observed that the addition of specific inhibitors of Chk1 and Chk2 checkpoint kinases restored the radiosensitivity of GICs(147). More recently, Ahmed, et al. observed that GICs have a prolonged cell cycle arrest at the G2 phase and noted that the inhibition of the Chk1 pathway induced double stranded breaks under ionizing radiation, in an ATM- and ATRdependent manner(148).
The polycomb group protein, BMI1, also shows enhanced expression in CD133+ GBM cells, BMI1 coprecipitated with DNA DSB response proteins, and preferentially associated with NHEJ repair proteins. This interaction enormously improved DNA damage response to radiation and cell viability(149).
Additionally, homologous recombination (HR) defects can contribute concurrently to the radioresistance of GICs. The inhibition of DNA repair protein RAD51 homolog 1 (RAD51) has been found to delay G2 cell cycle arrest, thereby sensitizing GICs to radiation(150). Due to the prominent cellular DNA damage response of GICs, targeting DNA repair pathways may provide a beneficial therapeutic approach for eliminating GICs.
3.2.2.2. ATP binding cassette (ABC) transporter
ABC transporters are ubiquitous and one of the largest transmembrane protein pump families. Normally, ABC transporters move endogenous bile acids, cholesterol, ions, and peptides across cell membranes. GICs express high levels of ABC transporters that are normally inactive in mature cells. In GICs, overexpression of ABC transporters further hinders drug delivery. ABC transporters promote therapy resistance by promoting efflux of exogenous compounds, such as TMZ, at the cellular and BBB level, in order to detoxify cells(151, 152).
ABC transporters include 49 members classified into seven gene subfamilies, designated ABCA–G. Thus far, ABCB1 (MDR1), ABCC1 (MRP1), and ABCG2 (BCRP1) are the most well-known pumps that have been identified in tumor stem-like cells. ABCG2 was first identified and associated with subpopulations of cells that are stem-like and multidrug resistant(153). ABCC1 is assumed to be another cause for GBM recurrence since the blockage of ABCC1 improved therapeutic response in GBMs(154, 155). GICs are enriched in hypoxic niches of the tumor(156). Low oxygen levels further promote the expression of MGMT, ABCC1 and ABCB1, and thereby lead to chemoresistance(157). Very recently, Lee, et al., proposed ABCB5 as a new marker for CD133+ GICs in chemoresistant GBM. The knockdown of ABCB5 inhibited GBM proliferation and sensitized the GBM cells to TMZ treatment(158).
Multiple pathways (SHH, Wnt-β-catenin pathway, Bcl-2, Akt, survivin, etc.) have been associated with the role of ABC transporters in therapy resistant GICs(151), which suggests that the ABC transporter is yet another target for which new therapies could be developed.
3.2.2.3. Hypoxia and autophagy
Tumor hypoxia is consistently associated with poor prognosis across multiple cancer types(159–161). GBM is characterized by extensive tissue hypoxia(162) and the hypoxic microenvironment has been regarded as an indispensable environmental cue for the preservation of GICs(120). In response to the reduction of oxygen tension, hypoxia-inducible factor 1 (HIF-1) is stabilized to maintain GICs and promote their tumorigenic ability(163, 164). In tumor tissue, microvascular thromboses congest vessels, further boosting intratumoral hypoxia. GICs can be found in the perivascular niche and the tumor core region, where are usually less oxygenated (1.25% O2) than peritumoral areas (2.5% O2)(165). The poorly oxygenated tumor tissue creates a perfect GIC niche and can stimulate downstream oncogenic pathways resulting in heterogeneity, invasiveness, and therapy resistance. Overall, the density and aggressiveness of GICs are negatively correlated with oxygen tension.
Several studies suggest that autophagy is induced by hypoxia as a cytoprotective mechanism, which is complementary to the ubiquitin system(166, 167). Autophagy is a survival-promoting process that contributes to the clearance of damaged proteins and organelles to maintain cellular homeostasis and genomic integrity. Moreover, it has been shown that autophagy supports cellular metabolism by generating metabolic precursors such as amino acids and lipids, which further supports the function of autophagy as an adaptive mechanism responding to metabolic stress(168, 169). In GBM, protective autophagy is triggered in GICs when challenged by cytotoxic therapies(168, 169).
It has been of great interest to investigate how autophagy sustains tumor growth and contributes to therapy resistance. Gene-9/Syntenin (MDA-9) is associated with advanced tumor grades in various cancer types. A recent study showed that MDA-9 is critical to maintaining GICs by regulating essential autophagy-related molecules, including BCL-2 and EGFR(170). Huang, et al., found that radiotherapy increases the level of MST4, which phosphorylates ATG4B and leads to autophagy. The inhibition of ATG4B significantly improved the survival benefit in radiation-treated mice(171). Inhibition of autophagy increased the massive accumulation of lipid peroxides and enhanced the sensitivity of GBM to TMZ treatment, which indicates initiation of ferroptosis in GICs(172). However, we observed an opposite role of autophagy. Aldehyde dehydrogenase 1A3 (ALDH1A3) has been regarded as a biomarker for various kinds of cancer stem cells, including GICs. We found that ALDH1A3 confers chemoresistance to GICs by deactivating toxic active aldehydes produced by lipid peroxidation under low concentrations of TMZ treatment. However, under high concentrations (500 μM) of TMZ, autophagy is induced, ALDH1A3 binds to p62 (an autophagic substrate) and is degraded along with ubiquitin cargo, ultimately enhancing the susceptibility of GICs to TMZ(173, 174).
The autophagy inhibitor chloroquine could reduce GBM resistance to anti-angiogenic therapy(175). It also has been shown that chloroquine-treated patients have better median survival in adjuvant settings in a phase III clinical trial(176). Although the role of autophagy in GBM progression is controversial, nevertheless, it provides a new insight for targeted therapy and conquering therapy resistance of GICs.
3.2.2.4. Epigenetic regulation
There is growing evidence that non-genetic determinants, associated with epigenetic modifications, contribute to functional heterogeneity and maintenance of GIC hierarchies(177–180). Epigenetic regulation includes alterations in the chromatin structure as well as DNA methylation and post translational histone modification or even changes in noncoding RNAs including long noncoding RNAs and miRNAs (181, 182). Specifically, the subpopulation of CD133+ cells, which are generally regarded as GICs, were found to be H3K9me2 negative, while the majority of cancer cells expressed strong H3K9me2. This data indicates that H3K9me2 is an important switch for maintaining stemness of GICs by regulating CD133(183). In a study based on histone modification expression analysis of 230 tumor samples, patients were divided into 10 separate prognostic groups. The 10 groups showed significantly different progression-free (P < 0.0001) and overall survival (P < 0.0001), demonstrating that aberrant histone modifications are critical prognostic factors for GBMs(184).
Epigenetic deregulation of multiple GIC-related pathways enables cancer cells to gain self-renewal and drug resistance properties. Wnt/β-catenin signaling can be activated by DNA methylation and aberrant histone modifications (185). Wnt/β-catenin signaling stabilized the epigenetic regulator KDM4C, and enhanced tumorigeneses and survival of human GBM cells(186). Another pathway that regularly interacts with epigenetic regulators is Notch signaling. DNA methylation of NOTCH1 and NOTCH3 inhibits GBM cell proliferation(187). Another study used sodium butyrate (NaB), a DNA methylating agent, to induce GBM apoptosis by decreasing HEY1 expression, suggesting that promoter methylation may regulate Notch signaling(188). In parallel to Wnt/β-catenin and Notch signaling, GICs also have high Sonic Hedgehog (SHH) signaling which is associated with better epigenetic memory. Hedgehog signaling can be epigenetically triggered in CSCs by Shh promoter hypomethylation and HDAC1 expression induction(179). BRD4, a wellcharacterized “epigenetic reader”, is also a critical regulator of GLI1 and GLI2 transcription(189). Lysine acetyltransferase 2B (PCAF/KAT2B) is another epigenetic modulator which is important in regulating SHH signaling in GBM (190). Collectively, a sophisticated network of signaling pathways can be deregulated as a result of aberrant epigenetic modifications in GICs. These genetic alterations uphold the stemness of GICs and promote tumor progression (Fig. 2).
Fig. 2.

The molecular mechanisms of resistance in glioma initiating cells (GICs). GBM is characterized by extensive intratumoral hypoxia. GIC niches are most commonly to be found in tumor core regions that are lessoxygenated. GICs are generally resistant to therapies and mostly due to following mechanisms: 1) Enhanced DNA repair capacity. Cell cycle arrest at G2 phase in GICs allows the DNA repair and further enter mitotic phase. 2) GICs express higher level of ABC transporters which promote efflux of therapeutic compounds. 3) The poorly oxygenated tumor tissue creates perfect GIC niches, which induce autophagy to maintain cellular homeostasis. Protective autophagy can also be triggered in GICs when challenged by cytotoxic therapies. 4) Epigenetic modifications contribute to functional heterogeneity and maintenance of GIC hierarchies. Multiple GICs-related signaling pathways (Wnt/β-catenin, Sonic Hedgehog (SHH), Notch) can be epigenetically regulated to gain self-renewing capabilities and drug resistance properties(179, 191, 192).
A better understanding of the mechanisms underlying GICs therapy resistance would improve the development of more effective therapies against GBM.
4. New therapies
Despite aggressive therapeutic measures, GBMs invariably continue to grow. Therefore, a broad search is underway for new and targeted therapies, such as inhibitors of specific molecular processes, nanoparticle carriers, and immunotherapy (Table.1 and Fig. 3).
Fig. 3.

New therapies described in this review.
4.1. Inhibitor therapy
Targeted inhibitors have been an additional therapeutic strategy for treating GBM(193). Inhibitors usually target a single biomarker or family of biomarkers that are markedly upregulated in malignant over healthy tissues. In general, inhibitors are developed either for extracellular targets like cell surface receptors or intracellular targets involved in signaling and activation of oncogenic pathways(193). These therapies have been tested alone and as a co-treatment with established therapeutics like TMZ or bevacizumab with varying but usually limited benefit.
4.1.1. PARP inhibitors
Poly (ADP ribose) polymerase (PARP) is a family of 17 nuclear enzymes that catalyze the cleavage of NAD+ molecules leading to the addition of ADP-ribose to acceptor proteins(194). The PARP1 enzyme is a prognostic marker and its elevated expression is associated with poor survival in some cancer patients(194). PARP is important for repair of DNA nicks, cell death, and genomic stability(195). Cancer therapies like radiation and alkylating agents rely on DNA breaks for their anti-tumor effect. Small molecule PARP inhibitors have been developed to improve the clinical efficacy of these therapies(196). PARP inhibitors can cause direct cytotoxic effects and potentiate the efficacy of alkylating agents. There is evidence to suggest that PARP inhibitors are most effective for GBM tumors with hypermethylated MGMT gene. In addition, PARP inhibitors can increase tumor sensitivity to TMZ chemotherapy, if the tumor has not previously been exposed to TMZ(196, 197). In addition to enhancing chemotherapy, PARP inhibitors synergize with radiation therapy because PARP1 activity increases 500-fold in the presence of DNA damage(198, 199). While several PARP inhibitors have been tested in vitro, only a few have been evaluated in GBM patients. A Veliparib-TMZ treatment regimen was evaluated in patients with recurrent GBM who had been previously treated with TMZ. Combination of TMZ and ABT-888 (veliparib) did not significantly improve PFS6 for either the bevacizumab-naïve or bevacizumab-failure patients (200). Similarly, co-treatment of children with diffuse intrinsic pontine glioma with veliparib, RT and TMZ did not show survival benefits(201). A phase I trial evaluating the safety and tolerability of cotreatment with olaparib and TMZ showed modest activity. Encouragingly, olaparib was found to have penetrated brain tumors both at the core and at the margins suggesting that the BBB was penetrated(202). Additional PARP inhibitors meriting further clinical study include niraparib and talazoparib (203–205). Many of these inhibitors show limited BBB penetration in preclinical models but evidence suggests the preclinical data might not faithfully predict clinical results(202, 204, 206). The true benefit, if any, of PARP inhibitor therapy for GBM patients remains to be determined.
4.1.2. Protein kinase inhibitors
Protein kinases are a involved in biochemical phosphate transfer reactions. Receptor tyrosine kinases are a family of high affinity cell surface receptors that have an extracellular domain with a ligand-binding site for many polypeptides, including growth factors and cytokines(207). Receptor tyrosine kinase pathways are known oncogenic drivers for malignant cancers(208). Several tyrosine kinase receptors, including vascular endothelial growth factor receptor (VEGFR), platelet derived growth factor (PDGF), fibroblast growth factor receptor (FGFR), and epidermal growth factor receptor (EGFR), are mutated and/or upregulated in GBM and have become attractive targets for novel therapy development(209–213). GBM is known to have high levels of VEGF expression resulting in highly angiogenic tumors and abnormal vessel formation(214). Inhibition of VEGFR or its substrates aims to stymie the growth of new blood vessels and starve the tumor of needed nutrients. Cediranib, an inhibitor of VEGF receptor tyrosine kinases has been evaluated in recurrent GBM as a monotherapy(215) or in combination with cilengitide(216), lomustine(217) or gefitinib(218), but has yet to receive FDA approval. Cediranib has the advantage of oral administration, targeting of multiple tyrosine kinases, and the ability to target intracellular VEGF receptors(215). Cediranib has been shown to help normalize tumor vascularization in a subset of patients which improved perfusion, oxygenation, and response to therapy. These patients had higher overall survival (OS) than the non-responding cohort(219). It was also recently discovered that cediranib sensitizes tumors to PARP inhibitors by downregulating homology-directed DNA repair(220). This discovery may encourage further investigations of combined anti-angiogenic and PARP inhibitor chemotherapies. Unfortunately, to date, the use of anti-angiogenic therapies for GBM has shown limited efficacy in clinical trials. One reason may include inadequate patient selection (221). Lu-Emerson, et al., summarized results from recent anti-angiogenic trials for GBM and how to use biomarkers to select for patients in future trials(222).
Erlotinib is an inhibitor of EGFR and has been approved to treat non-small cell lung and pancreatic cancers. It garnered excitement as a possible therapy for GBM in the early 2000s with encouraging in vitro results. However, several clinical trials have failed to reproduce the positive results obtained in initial experimental studies or improve survival of patients with GBM(223–227). Gefitinib, another EGFR inhibitor, has similarly been tested with and without other therapies. A phase II trial showed some evidence of activity of gefitinib for recurrent GBM in a subset of patients. However, survival was worse for the majority of patients compared to treatment with TMZ at the first sign of relapse(228). Other clinical trials using gefitinib alone or with cotreatments have shown no significant improvements over currently approved therapies(229–231). While most clinicians agree that combination therapies will be needed to treat recurrent GBM, there has been little further investigation of these two EGFR inhibitors in recent years.
There are also a number of small molecular multi-targeted protein kinase inhibitors that have been evaluated in new and recurrent GBM. Imatinib was evaluated in phase II clinical trials in newly diagnosed GBM (inoperable or not fully resected) and recurrent GBM, with and without concurrent radiation, but showed no clinical activity(232–234). Imatinib was well-tolerated but suffered from poor BBB penetration, even after radiation therapy. Again, it is possible that lack of proper patient selection for tumors overexpressing the targeted protein kinases may have contributed to the trial’s unfavorable results. Phase II trials of imatinib with the addition of hydroxyurea, which inhibits ribonucleotide reductase, again showed little to no anti-tumor activity(235–237). Dasatinib is another small molecular multi-targeted tyrosine kinase inhibitor. An early phase I/II clinical trial in recurrent GBM demonstrated toxicity issues and was underpowered such that clinical efficacy could not be determined(238). A trial evaluating the efficacy of adding dasatinib to bevacizumab did not have any added treatment benefit in patients with recurrent GBM compared to bevacizumab alone(239). Dasatinib was also tested in pediatric patients with progressive/recurrent GBM or diffuse intrinsic pontine gliomas with crizotinib, an oral c-Met inhibitor, but was poorly tolerated such that further investigation was discouraged in this patient population(240). Co-administration of dasatinib with lomustine (CCNU) unfortunately led to significant hematological toxicity(241). Sorafenib is another multi-targeted protein kinase inhibitor that has been tested in GBM patients(242). Several studies have evaluated the use of sorafenib with TMZ. Only one of these studies met its primary endpoint with 26% of patients achieving PFS at 6 months(243). The remaining trials with TMZ, bevacizumab, or erlotinib demonstrated safety of the combined therapy but no significant therapeutic efficacy(225, 244–246). Possible reasons leading to unfavorable study results included extensive prior therapy of some of the study participants and lack of selection of patients with tumors that expressed molecular targets for sorafenib (i.e., VEGFR, Raf-1 and wild-type B-Raf, PDGFR, c-KIT, and Flt-3A). Additional studies combining sorafenib with temsirolimus, an inhibitor of mammalian target of rapamycin (mTOR) or tipifarnib, a farnesyltransferase inhibitor, led to significant toxicities(247, 248). Recent evidence suggests that sorafenib may sensitize GBM cells to tumor-treating fields (249). Sunitinib is a similar multi-targeted protein kinase inhibitor that has been FDA-approved for the treatment of renal cell carcinoma but has failed to show efficacy for recurrent GBM in several clinical trials(250–252). Cabozantinib, another multi-targeted protein kinase inhibitor approved for the treatment of kidney cancer was evaluated in phase II trials for recurrent GBM and was welltolerated but did not meet predetermined statistical measures for success. Trials for pediatric patients are underway(253, 254).
4.1.3. Miscellaneous inhibitors
Additional molecular targets for inhibitors include myeloid cell leukemia-1 (MCL-1), and topoisomerase I inhibitors. MCL-1 is associated with PTEN deletion/mutation which occurs in 30–60% of GBM patients(255). Loss of PTEN in GBM cells led to upregulation of MCL-1 which is associated with resistance to apoptosis. There is preclinical evidence that the use of MCL-1 inhibitors in GBM may be an effective therapeutic strategy(255–257). A few MCL-1 inhibitors have gone to clinical trial (e.g., AZD5991, S64315, AMG 176, and AMG 397) mostly for the treatment of blood cancers but some have been halted due to concerns with cardiac toxicity(256, 257). Gossypol (AT-101), a polyphenolic compound that permeates cells and inhibits several dehydrogenase enzymes, has shown modest benefit in treating recurrent GBM, though few subsequent clinical trials have been initiated(258). Another biomarker under investigation is mTOR. Temsirolimus and everolimus are small molecular inhibitors that have been developed for mTOR which plays a role in glioma induction, growth, and progression(259). With these inhibitors, little to no radiographic improvements or benefit to progression-free survival have been observed when used as monotherapy and no added benefit was observed when used with bevacizumab or when compared against TMZ for patients with unmethylated MGMT promoters(260–265). The addition of everolimus and bevacizumab to radiation and TMZ as first-line treatment for GBM gave similar results compared to other phase II trials where bevacaizumab was added to first-line treatment(266). Additional mTOR inhibitors are currently being evaluated as potential cancer therapies (e.g., AZD-8055, OSI-027, and CC-115)(267). Irinotecan is a small molecular prodrug that, upon hydrolysis, is converted to SN-38, a topoisomerase I inhibitor(76). As a monotherapy, irinotecan has shown little to no benefit(268). It has been shown to have some activity in recurrent GBM although with some toxicity concerns(269–271). Use of irinotecan with TMZ for newly diagnosed GBM following concurrent chemoradiation therapy did not improve OS compared to TMZ alone and resulted in significant toxicities(272).
Targeted therapies for GBM have largely failed in clinical trials. A greater emphasis is now being placed on selecting patients whose tumors express the specific biomarkers targeted by the therapy(273, 274).
4.2. Immunotherapy
Immunotherapy has seen great success in the treatment of numerous cancers, but GBM has not been among the immunotherapy success stories. Several candidate therapies spanning antibodies and vaccines have reached phase III trials but yielded only modest gains in terms of clinical endpoints and survival. These experiences have underscored that additional interventions may be needed to achieve robust immune activation, potent effector cell activity, and durable treatment response. Here, we describe some of the most advanced immunotherapies studied to date for GBM and the specific mechanisms of resistance that accompany each strategy.
4.2.1. Checkpoint inhibitors
Checkpoint inhibitors are among the most successful innovations in immunotherapy. They are monoclonal antibodies designed to interrupt binding of regulatory receptors on T cells. In the normal cell, downstream signaling by these activated checkpoint receptors exist to prevent excessive inflammation(275). However, tumor cells can also produce the corresponding ligand, thereby abrogating and eluding an immune response that would lead to tumor clearance. Hence, such receptors are sometimes considered markers of T cell exhaustion, as they are no longer able to mount an immune response despite their successful tumor infiltration(276). A number of these receptors and inhibitors have since been identified, with anti-CTLA4 (cytotoxic T-lymphocyte-associated protein 4), anti-PD-1(programmed cell death protein 1), and anti-PDL1 already being used in the clinic (Fig. 4).
Fig.4.

The inhibition of CTLA-4 and PD-1 in GBM immunotherapy. Dendritic Cells (DCs) traffic between CNS tumors and the cervical lymph nodes to prime T cells against tumor neo-antigens. T cells receive effective activation signals with the engagement of two T cell receptors, antigen-specific T-cell receptor (TCR) and CD28, simultaneously. TCR binds to tumor-associated antigens (TAA) presented on major histocompatibility complex (MHC) molecule while CD28 interact with CD80/CD86(B7–1/2 receptors) costimulatory molecules on the surface of DCs. T cell activation leads to upregulation of checkpoint molecule CTLA-4(cytotoxic Tlymphocyte-associated protein 4). The interaction of CTLA-4 and CD80/CD86 of DCs results in blockage of T cell activation. The effector T cells can proliferate and migrate to the tumor microenvironment, leading to tumor eradication via MHC-I/TCR interaction. Some GBM cells and TAM-BMDMs express high levels of checkpoint molecules including transmembrane protein PD-L1. PD-L1 binds to PD-1 receptors on T cells, which leads to attenuation of TCR and CD28 signals, and subsequently promotes T cell apoptosis and functional exhaustion. Cytotoxic T cell responses are further inhibited by immune-suppressive cytokines by Tregs, astrocytes and neurons(277, 278). Immune checkpoint blockade (ICB) is based on a range of monoclonal antibody-based therapies, especially checkpoint inhibitors that block CTLA-4, PD-1, or PD-L1. Anti-CTLA-4 antibodies restore T cell activation in the lymph nodes, and PD-1/PD-L1 antibodies enhance the functional properties of effector T cells at the tumor site(279, 280). TAM: tumor-associated macrophage, BMDMs: bone marrow–derived macrophages, TCR: antigen-specific T-cell receptor.
For GBM, the greatest translational success has been seen with anti-PD-1 agents, nivolumab and pembrolizumab. When PD-1 binds to its ligand, there is downregulation of T cell activation(275). A trial from Dana-Farber Cancer Institute revealed patients who received pembrolizumab prior to surgery showed significant improvement in overall survival(281). However, in a Phase 3 clinical trial, CheckMate 143, nivolumab monotherapy failed to demonstrate an increase in overall survival versus bevacizumab (9.8 vs 10 months) for recurrent GBM(282). Additionally, monotherapy was found to be better tolerated than dual therapy with anti-CTLA4. Further findings in phase III trials, CheckMate 498 and CheckMate 548, also did not identify improvement in overall survival for standard therapy with and without anti-PD-1 in patients with MGMTmethylated GBM(283, 284).
Several checkpoint inhibitor-specific mechanisms of resistance have been described across cancers and may generalize for GBM. One transcriptome analysis of melanoma biopsies found an “innate PD-1 resistance gene signature” that could predict response to anti-PD-1(285). In this study, resistant tumors exhibited increased expression of genes regulating mesenchymal transition, cell adhesion, extracellular matrix remodeling, angiogenesis, and wound healing. Other work in a lung tumor model has shown that anti-inflammatory immune cells in the tumor microenvironment (TME) can decrease the efficacy of checkpoint inhibitors. For example, tumor-associated macrophages (TAMs) have been observed to remove anti-PD1 antibodies bound to CD8+ T cells (286). Additional preclinical studies on several cell lines have suggested that Treg apoptosis due to TME-related oxidative stress can generate adenosine release and anti-PD-L1 resistance(287).
Various mechanisms also prevent checkpoint inhibitors from generating a robust or durable T cell response. This is, in part, due to impaired epigenetics and memory cell formation, resulting in T cell exhaustion and immune evasion of the tumor(288, 289). Furthermore, several other checkpoint molecules may compensate for blocked PD-1 function(290). LAG3 is one example found on CD4, CD8, and Tregs. Like PD1, LAG3 normally inhibits T cell receptor activation and cytokine production(291). TIM3 is another promising checkpoint target, seen during the late stages of disease and T cell exhaustion. Binding to its ligand can lead to effector T cell apoptosis(292). Both LAG3 and TIM3 inhibitors are being assessed in combination with anti-PD1 in GBM Phase I clinical trials. (NCT02658981, NCT03961971). Given the complex interplay of checkpoint regulators, clinical trials have also begun to explore combination therapies.
4.2.2. Vaccines
Vaccines can be largely divided into peptide-based vaccines and cell-based vaccines. While the vehicles may differ, both ultimately require antigen presentation and T cell activation. Much of the early enthusiasm for cancer vaccines has since been redirected due to their limited success. Nevertheless, cancer vaccines have provided important insights on immune responses of GBM and are continuously investigated, especially in conjunction with multimodal treatment regimens.
4.2.2.1. Peptide-based vaccines
The most studied peptide-based vaccine, rindopepimut, targets the EGFRvIII variant. Wildtype EGFR of the ErbB family of kinase receptors is activated by EGF signal for cell proliferation, cell migration, and apoptosis inhibition(293). In approximately 20–30% of GBMs, EGFRvIII has a truncated extracellular domain, which prevents binding and leads to constitutive activation. The resulting amino acid sequence spanning across the deleted portion is tumor-specific, not found in any normal tissues(294). This specific epitope led to the development of rindopepimut (CDX-110-KLH), a 14 amino acid peptide, enhanced by the keyhole limpet hemocyanin carrier protein.
Rindopepimut underwent several early clinical trials, ultimately reaching a phase III trial (ACT IV) assessing vaccine efficacy in GBM patients with minimal residual disease. The control arm surpassed expectations and was statistically insignificant from rindopepimut, with a median OS of 20.0 and 20.1 months, respectively(295). The investigators had previously used historical controls during their phase I and II trials, which might have led to an overestimation of rindopepimut’s efficacy. Reasons for subsequently noted lower performance of the vaccine in GBM included variable responses to human leukocyte antigen (HLA) haplotype and antigen escape (296). One study reported that 82% of treated GBMs did not express EGFRvIII at the time of tumor recurrence(297). Since then, one small phase II trial (ReACT) combined rindopepimut with bevacizumab for recurrent GBM and reported a small survival benefit of the experimental group (12 months) compared to the control group (8.8 months)(298).
4.2.2.2. Cell-based vaccines
Among cell-based vaccines, the DCVax is possibly the most prominent. In this strategy, dendritic cells (DCs) generated ex vivo from patient derived peripheral blood are pulsed with different sources of tumor-associated antigens (TAAs), such as autologous tumor lysates, antigen peptide, and TAA-encoding RNA. These naturally-derived, mature DCs showed stronger antigen presentation potential(299). Moreover, the DCVax enabled customized targeting of multiple tumor antigens for potentially durable response. This approach has been cautiously monitored for the theoretical risk of developing an immune response to normal tissue antigens(300). Multiple early clinical trials were able to identify GBM patients for safe DCVax application, culminating in a phase III study. Although the study has yet to be formally completed, median overall survival has been reported at 23.1 months(301).
Several challenges unique to DCs have precluded the efficiency of cell-based vaccines. Interestingly, one group described that mature DCs in melanoma may be more motile and capable of migration to lymph nodes(302). Additionally, the immune suppressive environment can hinder a desirable DC-NK cross talk, whereby DC maturation leads to enhancement of NK cytotoxicity and IFN-y production. This has led to consideration of vaccine adjuvants such as, alpha-galactosylceramide or poly(I:C) to enhance NKT and DC activity in GBM treatment(303–305). Current clinical trials continue to incorporate these adjuvants while optimizing the antigen selection with personalized strategies. In addition, combination strategies with checkpoint inhibitors such as anti-PD-1 are also being considered at the preclinical phase in glioma(306).
4.2.3. Virotherapy
Over the past few decades, virotherapy has evolved from a primarily oncolytic to a broader viroimmunotherapeutic approach. Previously, treatment was designed to infiltrate the tumor, mitigate tumor defenses and induce a rapid, large-scale tumor cell death. Now, the focus of the field has shifted from direct oncolysis (payloads of virus) to immunostimulatory effects to induce long-lasting antitumor immune response (307). There are a variety of oncolytic viruses that can be armed with immunoregulatory inserts, like IL14, GMCSF, OX40 ligand or INFbeta to increase safety (308–311).The release of tumor associated antigens or damage-associated molecules can lead to durable and systemic effects, as evidenced in metastatic melanoma(312). Some parallels have been seen in GBM, where the application of an oncolytic adenovirus has led to CD8 effector T cell activation and downregulation of checkpoint inhibitors (313).
A challenge of therapy with oncolytic viruses is to achieve adequate replication of the virus in the tumor and tumor lysis. Viral vectors must avoid triggering an inflammatory response that would invite early elimination(314). Combination regimens have been proposed to avoid this premature viral clearance. Chemotherapies, radiation, and steroids are all post-operative steps that can temporarily suppress the innate immunity and support viral infection and dissemination(315, 316).
Several virotherapies have been investigated in clinical trials for the treatment of GBM, most notably vocimagene amiretrorepvec (Toca 511), which depends on a non-lytic strategy. In this model, a replicating retrovirus encoded with a cytosine deaminase is injected into the tumor bed with the goal to achieve preferential tumor cell infection over several weeks. At that time, the encoded virus converts a prodrug, Toca FC, to 5-fluorouracil which will in turn impair thymidylate synthase and cell replication(317). Several weeks later, when viral infection has been achieved, this prodrug-converting enzyme can convert valaciclovir into a nucleotide analogue and interrupt tumor cell replication(318). Early clinical trials reported a median overall survival of 13.6 months for recurrent or progressive GBM, which is promising when compared to historical controls. Additional viral studies have been performed with alternative vectors as adenovirus, poliovirus, cytomegalovirus and herpes virus(319). ASPECT is one such Phase III clinical trial for patients with operable high-grade glioma currently underway which assesses the use of an adenovirus encoded with herpes-simplexvirus thymidine kinase(320).
4.2.4. Chimeric antigen receptor T (CAR T) cells
Treatment with CAR T cells involves collection of allogeneic T cells from peripheral blood, ex vivo genetic engineering of the cells to express receptors against specific tumor associated antigens, and adoptive transfer of the tumor-targeted T cells. CAR T cells can bind the tumor antigen without antigen processing and independent of HLA-mediated antigen presentation. Immune cell activation signals are derived from CD3 and co-stimulatory receptors, such as CD28 or TNFRSF9/4–1BB (321). Several early phase clinical trials with tumortargeted CAR-T cells have been completed, targeting various tumor antigens such as EGFRvIII, HER2, and IL13R α2(322–324) in GBM. It remains to be seen whether there are significant and durable survival benefits for patients with GBM(322, 323). Several other targets for GBM are also actively being evaluated including CD147, also known as extracellular matrix metalloproteinase inducer, as well as B7-H3, an immune checkpoint transmembrane protein overexpressed in GBM(325). (NCT04045847, NCT04385173)
As with other therapies, CAR T cell therapies are subject to many barriers affecting a robust T cell response such as adequate T cell infiltration and activation. Tumor plasticity, antigen loss and heterogeneity continuously counteract CAR T cell therapies(326). Decreased expression of the target antigen, presence of splice variants and epitope modifications after treatment have all been observed(327). Additionally, not all tumor cells express the targeted antigen at any given time, while current versions of CAR T cells have a limited receptor repertoire. Recent work has described the expansion into bispecific T cell engager (BiTE) and trivalent CAR T cells, enabling recognition of multiple tumor antigens. Unfortunately, immunosuppressive features of the tumor microenvironment, Tregs and TAMs can counteract the efficacy of CAR T cells or promote T cell exhaustion (328). Finally, intrinsic pathways can interrupt sustained therapeutic activity of CAR T cells, such as chronic antigen exposure and tonic CAR signaling, which can also lead to T cell exhaustion.
Overall, many approaches for immunotherapy of GBM rely on activated T cells. Unlike other solid malignancies, GBM treatment is uniquely challenged by its immune-privileged state(326). Intrinsic characteristics of tumor cells can block this activation, leading to a “cold” tumor(329). For example, continuous changes in the tumor cell’s mutational profile can lead to loss of neoantigens that are initial targets for therapeutic T-cells (330). This differs from many hematologic malignances which exhibit more clonal cell populations(331). Meanwhile, extrinsic mechanisms can also hinder immune cell infiltration and coordinate an immunosuppressive tumor microenvironment. This can contribute to tumor-promoting resident immune cell populations and secreted factors in the tissue space. While immunotherapy alone fails to provide significant survival benefits for brain cancer patients, accumulating evidence shows that adjuvant radiation can prime and activate immune cells to tumor-derived antigens, induce presentation of neo-antigens in the tumor, and improve immune-suppressive environment, all of which sensitize brain cancers to immunotherapies by converting the immune environment from “cold” to “hot”(278, 332) (Fig.5). We found that irradiation improves IL-8 secretion by tumors, thus, we constructed IL-8 receptor-modified CD70CAR T cells to migrate into the tumor and induce an enhanced antitumor response in GBM(333). Additionally, Murty et al. found concurrent irradiation improved intravenous adoptive T-cell administration in the treatment of GBM in a preclinical immunocompetent GBM model(334).
Fig.5.

Immune modulatory effects of radiotherapy. The localized cytotoxic effects of radiation have been shown to cause immunogenic cell death (ICD). Radiation can induce all three arms of ICD: upregulation of the release of adenosine triphosphate (ATP), the extracellular release of “danger signal” high motility group box 1 (HMGB1) and translocation of “eat me” signal calreticulin (CRT) to the cell surface. Additionally, radiation regimens unmask the tumor by upregulating major histocompatibility complex (MHC) on the tumor cell, which enhances neo-antigen presentation in tumor cells for recognition by cytotoxic T-cells. Besides the effects on tumor cells, irradiation also affects tumor-associated stromal cells, such as reactive astrocytes, and the recruitment of microglia, which further contribute to the establishment of radiation-induced immune responses.
4.3. Nanotherapy
Conventional therapies for GBM can only marginally prolong the survival of patients with GBM. The vast majority of patients with GBM will die within 1–2 years after their diagnosis. Some challenges to successful treatment include the difficulty of complete tumor resection, the inefficient delivery of chemotherapeutic drugs, and the incomplete eradication of GICs. To overcome these obstacles, the application of nanoparticulate anti-GBM drugs has been proposed.
4.3.1. Passive tumor targeting: EPR effect
Nanoscale drug systems are based on polymeric micelles, liposomes, inorganic nanoparticles, nanotubes, or dendrimers(335, 336) (Fig.6) with attached or internalized chemotherapeutic drugs, sensitizers, or RNA(337). A limited permeability of the blood brain barrier (BBB) is the major obstacle in traditional GBM treatment. As a result of the angiogenesis process, the blood vessels in a tumor may develop a leaky endothelium which allows the entry of macromolecules, such as nanoparticles. After intravenous administration, nanoparticles diffuse into tumor tissue. While small molecular drugs extravasate more easily into tumors, they can also diffuse quickly back into the blood. By contrast, the large size of nanomaterials prevents diffusion of extravasated macromolecules back into the blood. This phenomenon is known as the enhanced permeability and retention (EPR) effect(338–340). The size of macromolecular drugs is critically important to achieve an ideal compromise between vascular extravasation and tumor retention. Xu et al. compared the tumor targeting efficiency of nanoparticles between 3 nm and 30 nm. The study showed that 3 nm nanoparticles exhibited much greater tumor targeting efficiency and penetration compared to the 30 nm nanoparticles(341). Bort et al developed ultrasmall polysiloxane-based nanoparticles with a hydrodynamic diameter of approximately 4 nm, which extravasated into rodent tumors and have recently been further developed towards a phase I clinical trial in patients with brain metastases(342).
Fig.6.

Advanced delivery platforms and delivery mechanisms of nanoparticulate anti-GBM drugs. Nanocarriers have been proposed based on various materials and principles as shown in the figure (a-g). Ligand-installed nanocarriers achieve therapeutic effects by actively targeting the surface marker or signaling pathway of cancer cells. Stimuli-responsive nanocarriers can release drug by responding to internal/external stimuli, which enable specific delivery cargos into the tumor microenvironment.
4.3.2. Active tumor targeting
The EPR effect is highly dependent on the permeability of blood vessels within a tumor, to improve tumor targeting, nanoparticle carriers have been decorated with specific antibodies, peptides, or aptamers, which can be actively targeted to specific surface markers of tumor cells (Fig.6).
Nanocarriers can transport RNA inhibitors such as siRNAs, miRNAs and LncRNAs(343–347), can be targeted against specific surface markers such as Cx43, CD133, CD44, CD163, CD15, CD49f, CD90 or target signaling pathways such as Hedgehog, Notch, PI3K/Akt/PTEN/mTOR, cAMP-Epac, NF-κB, Jak/STAT(337, 348, 349). Specific tumor targeting is commonly associated with certain nanocarriers. PEG-modified liposomes allow the attachment of functional groups targeting tumor tissues and reduce uptake by the reticuloendothelial system (350). In one case, Pep-1-conjugated PEGylated nanoparticles loaded with paclitaxel (Pep-NP-PTX) improved anti-glioma efficacy with a median survival time of 32 days in mouse models, which was significantly longer than that of control mice treated with PTX-NP (23 days) and Taxol® (22 days)(351). Grafals-Ruiz et al developed gold-liposome nanoparticles conjugated with the brain targeting peptides apolipoprotein E (ApoE) and rabies virus glycoprotein (RVG). Spherical nucleic acids (SNAs)-Liposome-ApoE were able to cross the BBB and showed a high accumulation in brain tumor tissues. Furthermore, SNA-Liposome-ApoE specifically targeted a highly abundant miRNA (miR-92b), which is aberrantly overexpressed in GBM (352). Belhadj et al developed a multifunctional liposomal glioma-targeted drug delivery system (c(RGDyK)/pHA-LS) modified with cyclic RGD (c(RGDyK)) and p-hydroxybenzoic acid (pHA). In their study, c(RGDyK)/pHA-LS/DOX showed a median survival time of 35 days, which was 2.31-, 1.76- and 1.5-fold higher than that of LS/DOX, c(RGDyK)-LS/DOX, and pHA-LS/DOX, respectively(353).
4.3.3. Stimuli-responsive drug release
Although various delivery platforms, such as PEGylated nanocarriers, have been developed to prolong circulation and improve drug solubility, the delivery efficacy of most nanocarriers is still quite low(354). Thus, stimuli-responsive nanocarriers are rationally designed to deliver and release drugs by responding to internal stimuli, such as pH, hypoxia, reactive oxygen species, enzyme activity, etc., or external stimuli, including ultrasound, light (e.g., laser), temperature (i.e., thermal) and magnetic field, etc (336, 355) (Fig.6). can specifically delivery cargos to the tumor microenvironment.
GBMs are characterized by extensive tissue hypoxia and various nanocarriers have been designed to target hypoxic tumors (356). Liu et al developed hypoxia-responsive ionizable liposomes, which showed enhanced therapeutic efficacy of small interference RNA (siRNA) anticancer drugs when exposed to low pH and hypoxic tumor microenvironment in glioma(357). GBMs are known for their resistance to radiotherapy due to intratumoral hypoxia. Hua et al have designed angiopep-2-lipid-poly-(metronidazoles)n (ALP-(MIs)n) hypoxic radiosensitizer-polyprodrug nanoparticles (NPs), which enhanced the radiotherapy sensitivity of gliomas(358). Enzyme activity is another internal stimuli to be considered. We developed a cross-linked iron oxide nanoparticle conjugated to azademethylcolchicine (CLIO-ICT), which is specifically activated by the enzyme, matrix-metalloproteinase 14 (MMP-14). Since MMP-14 is highly expressed in GBM, but not in the normal brain or normal visceral organs, it provides cancer-specific therapy with little or no side effects. Upon-cleavage by MMP-14, CLIO-ICT releases azademethylcolchizine in the tumor tissue, which disrupted the tumor vasculature and killed tumor cells and GIC in GBM (359, 360). Our study showed that treatment with CLIO-ICT plus TMZ and irradiation lead to significantly improved tumor growth inhibition and overall survival of mice with GBM when compared to controls that received monotherapy. In addition, the iron core of CLIO-ICT enabled in vivo drug tracking with MR imaging, demonstrating in vivo tumor drug accummulation.
External stimuli also have been studied extensively to improve nanodrug delivery in GBM. Although the BBB is disrupted in GBM patients, overwhelming clinical evidence demonstrates the existence of an intact BBB in all GBM, which limit therapeutics delivery and efficacy (361). The combination of focused ultrasound (FUS)-BBB opening and externally applied magnetic field (MT) could deliver nanodrugs more effectively to deepseated GBM tumors(362, 363). Most recently, Curley et al. used MRI–FUS and microbubbles to deliver “brainpenetrating” nanoparticle (BPN), which yielded markedly augmented interstitial tumor flow and enhanced BPN penetration in GBM(364). Fan et al. developed boron-containing polyanion [polyethylene glycol-b-poly((closododecaboranyl)thiomethylstyrene) (PEG-b-PMBSH)] nanoparticles (295 ± 2.3 nm in aqueous media) and coupled them with microbubble-assisted FUS for GBM treatment. They found the combination may improve boron neutron capture therapy (BNCT) in GBM(365). Li et al. developed polysorbate 80- modified paclitaxel-loaded PLGA nanoparticles (PS- 80- PTX- NPs, PPNP), which showed significantly stronger anti-tumor efficacy in the tumor- bearing mice when combined with FUS(366). Furthermore, magnetic hyperthermiamediated cancer therapy (MHCT) has shown promising results in the preclinical studies. MHCT has applied magnetic nanoparticles to heat tumor tissues, which is based on an alternating magnetic field (AMF)(367, 368). Gupta et al. have developed manganese-doped magnetic nanoclusters for hyperthermia and photothermal GBM therapy, they observed oxidative stress produced in the cellular environment and confirmed the ROS-dependent apoptosis of GBM cells via the mitochondrial pathway(369). Mamani et al. found magnetic hyperthermia effectively decreased cell viability (about 20% and 100% after 10- and 30-minutes therapy) with a GBM 3D cells culture model(370).
4.3.4. Different administration routes for drug delivery
An intranasal route of drug administration can enable therapeutic compounds to reach GBM tumors in significantly higher doses than with intravenous administration. Sousa et al. developed BCZ-loaded PLGA nanoparticles and intranasally injected them into a GBM mouse model. The drug was found to be efficiently delivered to the brain with very limited off-target delivery to visceral organs, such as the lung and liver(371). Khan et al established nano-lipid chitosan hydrogel formulations for a nose-to-brain delivery of TMZ. After intranasal administration, TMZ release to GBM was 60% within 24 h and Wistar rats showed an increased drug targeting efficiency (DTE) of 326% and a direct transport percentage (DTP) of 93% compared to the intranasal administration of nano-lipid formulation as a control (DTE, 113.36% and DTP, 71.74%)(372). Similarly, the concomitant intranasal administration of chitosan nanoparticles attached with a Gal-1 siRNA enhanced the efficacy of anti-PD-1 antibodies with a median survival of 51.5 days, which is significantly higher than the control groups (17.5 and 30 days for untreated mice and anti-PD-1 antibodies alone, respectively)(373).
Intratumor administration can also be effective in cases of a solitary tumor which cannot be surgically removed. The injection can be carried out with a syringe or catheter at the tumor location or with the help of convection enhanced delivery (CED). CED is a technique which can precisely control the infusion rates of anti-GBM compound towards GBM tumors by maintaining a hydrostatic pressure gradient(374). CED was first introduced in 1994(375) and applied widely in clinical trials for the non-nano-formulated anti-cancer compounds(376–380). CED involves drilling a small burr hole into the skull and stereotactically positioning catheters to the interstitial space next to the tumor using image guidance. Once in position, the catheter can deliver many different kinds of therapeutic or imaging contrast agents to the site (e.g., small molecules, proteins, viruses, liposomes, nanoparticles, etc.)(381, 382). This technique ensures delivery to the tumor without needing to bypass the blood-brain barrier (BBB), but it failed mostly due to insufficient drug distribution(383). Later, it was tested with nano-formulated drugs and showed high retention time in tumors. Polymeric nanoparticles such as poly(lactide-coglycolide) (PLGA) nanoparticles were used for CED. CED of carboplatin nanoparticles conferred greater tumor cytotoxicity and reduced neuronal toxicity in rat and porcine models(374). Finbloom et al found that the CED of virus-like particles (VLPs) and nanophage filamentous rods modified with doxorubicin (DOX) required smaller doses than traditional intravenous routes to achieve comparable survival outcomes(384).
Several potential benefits of anti-GBM nano-drugs have been identified: 1) Improving surgical tumor removal. Most recently, fluorescence guided resection of GBM after intravenous administration of a fluorescent mini nanoimaging agent (NIA) or fluorescent silica coated iron oxide nanoparticles greatly improved the intraoperative delineation of GBM(385, 386). 2) Improving the efficacy of chemotherapy and reducing side effects. As described above, nano-scale drugs have a greater blood circulation half-life and can be predominantly delivered to the tumor via the EPR effect or active delivery systems. Targeting specific markers of tumor cells reduces toxicity to healthy cells and thus decreases side effects(339) 3) Enhancing the efficacy of radiotherapy. Recent studies have shown that nanodrugs that kill GICs can enhance the efficacy of radiotherapy(360, 387). Radiation therapy could, in turn, enhance nanotherapy by affecting the prevalence and polarization of tumor-associated macrophages(388). 4) The nanoparticle carrier can be designed to actively induce an immune response (389, 390). Our group showed that the iron oxide nanoparticle ferumoxytol induced pro-inflammatory macrophage polarization and thus inhibited tumor growth(391). Overall, nanotherapeutics have many advantages for treating GBM, which can enhance the efficacy of traditional therapy.
4.4. Miscellaneous therapies
4.4.1. Laser interstitial thermal therapy (LITT)
LITT is a method for delivering thermal energy to GBM using a stereotaxic device with the goal to ablate the tumor tissue. A small burr hole is drilled into the skull through which an optical fiber is threaded and guided to the center of the tumor. The fiber creates heat which burns and kills the tumor tissue. The heat generated can be monitored using MR-thermometry to ensure safe use and no harm to healthy adjacent tissue. Advantages of LITT over standard surgery include the minimally invasive approach and feasibility to treat inoperable tumors. This technology has been used with other types of brain lesions and was particularly useful for high grade gliomas(392). After treatment with LITT, patients with smaller tumors (<4 cm3) demonstrated higher survival rates and fewer perioperative complications compared to patients with larger tumors (>4 cm3)(392, 393). Despite promising results, side effects from LITT can include swelling and inflammation which can cause neurological side effects. Traditional surgery also leads to inflammation; however, the effect is mitigated since there is space left where tissue was removed. With LITT, the dead treated tissue is still present. There is still no clear guidance on who should receive this treatment, but it is a useful tool to supplement existing treatment strategies.
4.4.2. Tumor-treating fields (TTFields)
Tumor treating fields are a new treatment modality for GBM. It was approved by the FDA in 2011 for recurrent GBM and in 2015 for newly diagnosed GBM. More recently, TTFields has been approved by the FDA for the treatment of patients with pleural malignant mesothelioma(394). The treatment requires the patient to wear a device on their shaved head that delivers low-intensity, intermediate frequency, alternating electric fields(395). The alternating electric fields produce antimitotic effects that are selective for rapidly dividing cells with the maximal benefit occurring when the electric fields are parallel to the axis of cell division(396). Given that cells in a tumor are turned in many different directions, the treatment is most effective when two or more orthogonal pairs of transducer arrays are used. One major benefit to TTFields is the limited toxicity and mild side effects (usually only skin irritation that can be managed with topical treatments). The greatest determinant of treatment success is patient compliance in wearing the device since the treatment is only working when the device is worn and the electric fields are “on”. This technology has been slow to gain traction in the clinic possibly due to the sparse scientific literature and variable compliance of patients to shave their head, wearing the device > 75% of the time, and carrying around a large battery pack. However, the benefits of TTFields are clear. In a phase III multi-center clinical trial, it was shown that in a population of nearly 700 patients, those that received TTField therapy in addition to TMZ had a significantly enhanced progression-free survival (~5 months) and significantly enhanced overall survival(397). Optimization of therapy will come from further examination of the mechanisms of actions of TTFields. For instance, it has been shown that TTFields can disrupt the membrane composition and permeability of cancer cells(398) and this could explain the synergistic effects of combination therapies of TTFields with chemotherapeutics such as Withaferin A (399).
5. Future therapeutic strategies
In 2005, when Stupp et al. demonstrated a major pharmaceutical progress for GBM management by combining radiotherapy and adjuvant TMZ therapy(5). Since then, there have been advances in understanding genetic drivers of tumor development and progression. Many of these molecular characteristics were included in the World Health Organization (WHO) 2016 updated classification of tumors of the central nervous system including IDH mutant/wildtype status, 1p/19q deletions, EGFR amplification, and mutations in TP53, PTEN, ATRX, and TERT promoters(400). There have been improved 2- and 3- year survival rates, but 5-year survival rates remain poor(401). Advances in precision medicine, surgical techniques, and combination therapies will shape the future directions for GBM treatment.
5.1. Precision medicine
Ideally, a given patient’s brain tumor would be screened for specific biomarkers that could be paired with selective drugs. Only patients having high expression of the biomarker would receive a targeted drug. The treatment plan would likely change over time as the tumor evolves and would also look different for patients with different tumor characteristics. For example, O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation has already been shown to predict tumor response to TMZ therapy (402). Exosomes, extracellular vesicles, and microRNA assays are also being used as biomarkers for GBM (403–406). Intraoperatively, mass spectrometry (MS) can sensitively and specifically identify molecules in the tumor(407), aiding the surgeon in defining the tumor margin and determining the most effective systemic therapy.
GBM is marked by extensive inter- and intra-individual heterogeneity in driver mutations and molecular subtypes (408). Identification of new biomarkers is also important for treatment of recurrent GBM as 90% of druggable targets are differentially expressed in a recurrent tumor compared to the tumor at initial diagnosis(409). Patients may need to receive new therapies over the course of their disease. Le Rhun et al. provided an in depth summary of known GBM-specific biomarkers(410). Many GIC markers are also being explored, including CD133, CD44, CD15, CD70, S100A4, ALDH1A3, NANOG, OCT-4, SOX-2, and NESTIN(411–414).
Tools that aid discovery and understanding of biochemical pathways will likely include new genetic screening techniques(415, 416), next generation sequencing and epigenetic studies(417). In addition, machine learning algorithms and bioinformatics analyses of tumor omics data will enable correlations of complex multi-factorial clinical information with tailored treatment options(418, 419). Machine learning algorithms could be designed to predict responses to treatment and support treatment decisions(420). Furthermore, organoids gain more and more attention in recent years. Organoids possess greater predictive power compared to assays of single cell monolayers and can be used to test patient-specific therapies(421, 422). They are especially useful in situations where patient samples are difficult to obtain(423, 424). Some organoid models have even been shown to exhibit stage-specific neural development and yield pathology results similar to resected patient tumors(425).
Unfortunately, targeted therapies in clinical trials have had limited success thus far, partly due to the heterogeneity and plasticity of GBM but also due to practical limitations(193). A future clinical trial would likely have the following elements: i) strong evidence of anti-tumor activity in relevant pre-clinical models, ii) selection of patients with molecular enrichment for the drug target ideally with a non-invasive diagnostic technique, iii) a drug that by design or by delivery route accounts for the restrictive nature of the BBB, iv) inclusion of tissue collection or advanced molecular imaging during the treatment for analysis of pharmacodynamic markers, and v) close integration of advanced imaging technologies and treatment, including advanced imaging biomarkers for improved tumor detection, characterization and treatment monitoring.
5.2. Advances in surgical techniques
Given the importance of complete tumor resection toward positive patient outcomes, advances in surgical techniques and image guidance will be critical for the future of GBM treatment. LITT has shown efficacy in improving quality of life, cognition, and stabilization of Karnofsky Performance Status (KPS) score for patients suffering from radiation necrosis(426). Appropriate patient selection is important. LITT may not be appropriate for patients who are significantly functionally compromised(393). The development of novel fluorescent imaging agents and trelated equipment may improve the surgeon’s ability to see and remove the entire tumor. Only 5-aminolevulinic acid (5-ALA) is approved for intraoperative use in GBM resection(49, 427, 428). Unfortunately, the US was a full decade behind Europe in approving this clinical imaging agent(49). In addition, diffusion tensor imaging (DTI)-MRI has also shown promise to visually help locate important motor fibers which can be spared during tumor resection(429). In addition to improving tumor resection, emphasis should be placed equally on improving safety as new deficits after surgery can eliminate the survival benefits of surgery(430).
5.3. Combination therapies
Unfortunately, current combination therapies for the treatment of GBM are often rendered ineffective because the tumor can find redundant compensatory mechanisms. This was likely the reason why isolated studies that targeted PI3K/AKT/mTOR, p53/RB pathways, or EGFR gene amplification or mutation, have failed to improve outcomes(410). Therefore, to be successful, novel GBM therapies target distinct biological pathways and include novel methodologies such as electric field, viral, or cell-based therapeutic strategies. Tumor treating fields (TTFields) may be particularly suited for combination therapy(431). TTFields elicit a therapeutic effect by applying alternating electric fields that alter DNA repair, membrane permeability, and immunological responses(432).
Major considerations for combination therapies are the method of delivery, time of administration, and the order of therapy(433). Nanocarriers hold promise for delivery of multiple chemical therapeutics and/or a high payload to GBM tumors in a single dose. Nanoparticles are then often phagocytosed by tumor-associated macrophages which can create both limitations and opportunities (434). Encapsulating several agents in a single nanocarrier can deliver them together (435). For radiation therapy, fractionated doses are important for normal cell recovery and reoxygenation of acutely hypoxic tissues(436). In addition to DNA damage induced by radiation, the “abscopal effect” can prime and activate the innate immune system (437–439). The order of combination therapies also needs to be carefully evaluated. For example, a first therapy could be used to “prime” the tumor microenvironment and make it more receptive for a subsequent second therapy(440). “Priming” may include normalizing the vasculature, reducing stress associated with the large solid tumor mass, or degrading the extracellular matrix for better drug penetration (441).
6. Conclusion
GBM continues to be the most lethal tumor type with limited treatment options. Given the genomic complexity and multiple signaling pathways of GBM, a monotherapy will likely not be effective. An effective treatment approach for GBM will require combination therapies targeting distinct oncogenic pathways. A comprehensive understanding of the molecular biology of GBM, along with mechanisms of therapy resistance and effective integration of different therapy approaches will be key for the development of effective therapies. While histology and the identification of chromosomal deletions are important to estimate prognosis and plan targeted therapies, imaging can help in guiding surgeries and monitoring treatment response.
Acknowledgments:
We would like to dedicate this article to our late chair and long-term mentor Dr. Sanjiv Sam Gambhir, the Virginia and D.K. Ludwig Professor in Cancer Research and Chairman of the Department of Radiology at Stanford University from 2011–2020. Dr. Gambhir had dedicated his life to cancer research, with specific focus on glioblastoma. W.W. and H.D.L. are supported by a grant from the ReMission Alliance Against Brain Tumors (PI: Duane Mitchell, University of Florida; PI of subaward to Stanford: H. Daldrup-Link). In addition, H.D.L. is supported by a grant from the National Institute of Child Health and Development (R01HD103638) and the National Cancer Institute (P30CA124435; PI: Steven Artandi). M.Z. is supported by the Stanford Cancer Imaging Training Program (T32CA009695, PI S. Napel, Stanford University).
Footnotes
Declaration of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Oszvald A, Güresir E, Setzer M, Vatter H, Senft C, Seifert V, Franz K. Glioblastoma therapy in the elderly and the importance of the extent of resection regardless of age. Journal of Neurosurgery. 2012;116(2):357–364. [DOI] [PubMed] [Google Scholar]
- 2.Davis ME. Glioblastoma: Overview of Disease and Treatment. Clin J Oncol Nurs. 2016;20(5 Suppl):S2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yao M, Li S, Wu X, Diao S, Zhang G, He H, Bian L, Lu Y. Cellular origin of glioblastoma and its implication in precision therapy. Cell Mol Immunol. 2018;15(8):737–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braganza MZ, Kitahara CM, Berrington de Gonzalez A, Inskip PD, Johnson KJ, Rajaraman P. Ionizing radiation and the risk of brain and central nervous system tumors: a systematic review. Neuro Oncol. 2012;14(11):1316–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for R, Treatment of Cancer Brain T, Radiotherapy G, National Cancer Institute of Canada Clinical Trials G. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. [DOI] [PubMed] [Google Scholar]
- 6.Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2013–2017. Neuro Oncol. 2020;22(12 Suppl 2):iv1–iv96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ringel F, Pape H, Sabel M, Krex D, Bock HC, Misch M, Weyerbrock A, Westermaier T, Senft C, Schucht P, Meyer B, Simon M, group SNs. Clinical benefit from resection of recurrent glioblastomas: results of a multicenter study including 503 patients with recurrent glioblastomas undergoing surgical resection. Neuro Oncol. 2016;18(1):96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lara-Velazquez M, Al-Kharboosh R, Jeanneret S, Vazquez-Ramos C, Mahato D, Tavanaiepour D, Rahmathulla G, Quinones-Hinojosa A. Advances in Brain Tumor Surgery for Glioblastoma in Adults. Brain Sci. 2017;7(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garnier D, Renoult O, Alves-Guerra MC, Paris F, Pecqueur C. Glioblastoma Stem-Like Cells, Metabolic Strategy to Kill a Challenging Target. Front Oncol. 2019;9:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prager BC, Bhargava S, Mahadev V, Hubert CG, Rich JN. Glioblastoma Stem Cells: Driving Resilience through Chaos. Trends Cancer. 2020;6(3):223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramon YCS, Sese M, Capdevila C, Aasen T, De Mattos-Arruda L, Diaz-Cano SJ, Hernandez-Losa J, Castellvi J. Clinical implications of intratumor heterogeneity: challenges and opportunities. J Mol Med (Berl). 2020;98(2):161–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verhaak RG, Hoadley KA, Purdom E, Wang V, Qi Y, Wilkerson MD, Miller CR, Ding L, Golub T, Mesirov JP, Alexe G, Lawrence M, O’Kelly M, Tamayo P, Weir BA, Gabriel S, Winckler W, Gupta S, Jakkula L, Feiler HS, Hodgson JG, James CD, Sarkaria JN, Brennan C, Kahn A, Spellman PT, Wilson RK, Speed TP, Gray JW, Meyerson M, Getz G, Perou CM, Hayes DN, Cancer Genome Atlas Research N. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17(1):98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Behnan J, Finocchiaro G, Hanna G. The landscape of the mesenchymal signature in brain tumours. Brain. 2019;142(4):847–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sturm D, Bender S, Jones DT, Lichter P, Grill J, Becher O, Hawkins C, Majewski J, Jones C, Costello JF, Iavarone A, Aldape K, Brennan CW, Jabado N, Pfister SM. Paediatric and adult glioblastoma: multiform (epi)genomic culprits emerge. Nat Rev Cancer. 2014;14(2):92–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Q, Hu B, Hu X, Kim H, Squatrito M, Scarpace L, deCarvalho AC, Lyu S, Li P, Li Y, Barthel F, Cho HJ, Lin YH, Satani N, Martinez-Ledesma E, Zheng S, Chang E, Gabriel Sauve CE, Olar A, Lan ZD, Finocchiaro G, Phillips JJ, Berger MS, Gabrusiewicz KR, Wang G, Eskilsson E, Hu J, Mikkelsen T, DePinho RA, Muller F, Heimberger AB, Sulman EP, Nam DH, Verhaak RGW. Tumor Evolution of Glioma-Intrinsic Gene Expression Subtypes Associates with Immunological Changes in the Microenvironment. Cancer Cell. 2018;33(1):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fedele M, Cerchia L, Pegoraro S, Sgarra R, Manfioletti G. Proneural-Mesenchymal Transition: Phenotypic Plasticity to Acquire Multitherapy Resistance in Glioblastoma. Int J Mol Sci. 2019;20(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qazi MA, Vora P, Venugopal C, Sidhu SS, Moffat J, Swanton C, Singh SK. Intratumoral heterogeneity: pathways to treatment resistance and relapse in human glioblastoma. Ann Oncol. 2017;28(7):1448–1456. [DOI] [PubMed] [Google Scholar]
- 18.Patel AP, Tirosh I, Trombetta JJ, Shalek AK, Gillespie SM, Wakimoto H, Cahill DP, Nahed BV, Curry WT, Martuza RL, Louis DN, Rozenblatt-Rosen O, Suva ML, Regev A, Bernstein BE. Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science. 2014;344(6190):1396–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol. 2015;7(1):a020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greene C, Campbell M. Tight junction modulation of the blood brain barrier: CNS delivery of small molecules. Tissue Barriers. 2016;4(1):e1138017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liebner S, Dijkhuizen RM, Reiss Y, Plate KH, Agalliu D, Constantin G. Functional morphology of the blood-brain barrier in health and disease. Acta Neuropathol. 2018;135(3):311–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robey RW, Pluchino KM, Hall MD, Fojo AT, Bates SE, Gottesman MM. Revisiting the role of ABC transporters in multidrug-resistant cancer. Nat Rev Cancer. 2018;18(7):452–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gomez-Zepeda D, Taghi M, Scherrmann JM, Decleves X, Menet MC. ABC Transporters at the Blood-Brain Interfaces, Their Study Models, and Drug Delivery Implications in Gliomas. Pharmaceutics. 2019;12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang D, Wang C, Wang L, Chen Y. A comprehensive review in improving delivery of small-molecule chemotherapeutic agents overcoming the blood-brain/brain tumor barriers for glioblastoma treatment. Drug Deliv. 2019;26(1):551–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharma P, Allison JP. The future of immune checkpoint therapy. Science. 2015;348(6230):56–61. [DOI] [PubMed] [Google Scholar]
- 26.Bonaventura P, Shekarian T, Alcazer V, Valladeau-Guilemond J, Valsesia-Wittmann S, Amigorena S, Caux C, Depil S. Cold Tumors: A Therapeutic Challenge for Immunotherapy. Front Immunol. 2019;10:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lim M, Xia Y, Bettegowda C, Weller M. Current state of immunotherapy for glioblastoma. Nat Rev Clin Oncol. 2018;15(7):422–442. [DOI] [PubMed] [Google Scholar]
- 28.Brahm CG, van Linde ME, Enting RH, Schuur M, Otten RHJ, Heymans MW, Verheul HMW, Walenkamp AME. The Current Status of Immune Checkpoint Inhibitors in Neuro-Oncology: A Systematic Review. Cancers (Basel). 2020;12(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Azagury DE, Dua MM, Barrese JC, Henderson JM, Buchs NC, Ris F, Cloyd JM, Martinie JB, Razzaque S, Nicolau S, Soler L, Marescaux J, Visser BC. Image-guided surgery. Current Problems in Surgery. 2015;52(12):476–520. [DOI] [PubMed] [Google Scholar]
- 30.Watts C, Sanai N. Surgical approaches for the gliomas. Handbook of Clinical Neurology. 2016;134:51–69. [DOI] [PubMed] [Google Scholar]
- 31.Ojemann JG, Miller JW, Silbergeld DL. Preserved function in brain invaded by tumor. Neurosurgery. 1996;39(2):253–258; discussion 258–259. [DOI] [PubMed] [Google Scholar]
- 32.Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbusch SJ, Holland E, Hess K, Michael C, Miller D, Sawaya R. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. Journal of Neurosurgery. 2001;95(2):190–198. [DOI] [PubMed] [Google Scholar]
- 33.Sanai N, Berger MS. Glioma extent of resection and its impact on patient outcome. Neurosurgery. 2008;62(4):753–764; discussion 264–266. [DOI] [PubMed] [Google Scholar]
- 34.Sanai N, Polley M-Y, McDermott MW, Parsa AT, Berger MS. An extent of resection threshold for newly diagnosed glioblastomas. Journal of Neurosurgery. 2011;115(1):3–8. [DOI] [PubMed] [Google Scholar]
- 35.Ushio Y, Kochi M, Hamada J-i, Kai Y, Nakamura H. Effect of surgical removal on survival and quality of life in patients with supratentorial glioblastoma. Neurologia Medico-Chirurgica. 2005;45(9):454–460; discussion 460–461. [DOI] [PubMed] [Google Scholar]
- 36.Stummer W, Reulen H-J, Meinel T, Pichlmeier U, Schumacher W, Tonn J-C, Rohde V, Oppel F, Turowski B, Woiciechowsky C, Franz K, Pietsch T, Group AL-GS. Extent of resection and survival in glioblastoma multiforme: identification of and adjustment for bias. Neurosurgery. 2008;62(3):564–576; discussion 564–576. [DOI] [PubMed] [Google Scholar]
- 37.Kircher MF, de la Zerda A, Jokerst JV, Zavaleta CL, Kempen PJ, Mittra E, Pitter K, Huang R, Campos C, Habte F, Sinclair R, Brennan CW, Mellinghoff IK, Holland EC, Gambhir SS. A brain tumor molecular imaging strategy using a new triple-modality MRI-photoacoustic-Raman nanoparticle. Nature Medicine. 2012;18(5):829–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moore CM, Robertson NL, Arsanious N, Middleton T, Villers A, Klotz L, Taneja SS, Emberton M. Image-Guided Prostate Biopsy Using Magnetic Resonance Imaging–Derived Targets: A Systematic Review. European Urology. 2013;63(1):125–140 [DOI] [PubMed] [Google Scholar]
- 39.Kobayashi K, Bhargava P, Raja S, Nasseri F, Al-Balas HA, Smith DD, George SP, Vij MS. Image-guided Biopsy: What the Interventional Radiologist Needs to Know about PET/CT. RadioGraphics. 2012;32(5):1483–1501 [DOI] [PubMed] [Google Scholar]
- 40.Klimberg VS, Rivere A. Ultrasound image-guided core biopsy of the breast. Chinese Clinical Oncology. 2016;5(3):33. [DOI] [PubMed] [Google Scholar]
- 41.Hu S, Kang H, Baek Y, El Fakhri G, Kuang A, Choi HS. Real-Time Imaging of Brain Tumor for Image-Guided Surgery. Advanced Healthcare Materials. 2018;7(16):e1800066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barone DG, Lawrie TA, Hart MG. Image guided surgery for the resection of brain tumours. The Cochrane Database of Systematic Reviews. 2014(1):CD009685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jenkinson MD, Barone DG, Bryant A, Vale L, Bulbeck H, Lawrie TA, Hart MG, Watts C. Intraoperative imaging technology to maximise extent of resection for glioma. The Cochrane Database of Systematic Reviews. 2018;1:CD012788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whitney MA, Crisp JL, Nguyen LT, Friedman B, Gross LA, Steinbach P, Tsien RY, Nguyen QT. Fluorescent peptides highlight peripheral nerves during surgery in mice. Nature Biotechnology. 2011;29(4):352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Villanueva-Meyer JE, Mabray MC, Cha S. Current Clinical Brain Tumor Imaging. Neurosurgery. 2017;81(3):397–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pan JW, Moon CH, Hetherington HP. Cerebrospinal fluid-suppressed T2 -weighted MR imaging at 7 T for human brain. Magn Reson Med. 2019;81(5):2924–2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li YM, Suki D, Hess K, Sawaya R. The influence of maximum safe resection of glioblastoma on survival in 1229 patients: Can we do better than gross-total resection? Journal of Neurosurgery. 2016;124(4):977–988. [DOI] [PubMed] [Google Scholar]
- 48.Gerard IJ, Kersten-Oertel M, Petrecca K, Sirhan D, Hall JA, Collins DL. Brain shift in neuronavigation of brain tumors: A review. Medical Image Analysis. 2017;35:403–420. [DOI] [PubMed] [Google Scholar]
- 49.Hadjipanayis CG, Stummer W. 5-ALA and FDA approval for glioma surgery. Journal of Neuro-Oncology. 2019;141(3):479–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen H-J, Group AL-GS. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. The Lancet Oncology. 2006;7(5):392–401. [DOI] [PubMed] [Google Scholar]
- 51.Schebesch K-M, Brawanski A, Hohenberger C, Hohne J. Fluorescein Sodium-Guided Surgery of Malignant Brain Tumors: History, Current Concepts, and Future Project. Turkish Neurosurgery. 2016;26(2):185–194. [DOI] [PubMed] [Google Scholar]
- 52.Cho SS, Salinas R, Lee JYK. Indocyanine-Green for Fluorescence-Guided Surgery of Brain Tumors: Evidence, Techniques, and Practical Experience. Frontiers in Surgery. 2019;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Diaz RJ, Dios RR, Hattab EM, Burrell K, Rakopoulos P, Sabha N, Hawkins C, Zadeh G, Rutka JT, Cohen-Gadol AA. Study of the biodistribution of fluorescein in glioma-infiltrated mouse brain and histopathological correlation of intraoperative findings in high-grade gliomas resected under fluorescein fluorescence guidance. Journal of Neurosurgery. 2015;122(6):1360–1369. [DOI] [PubMed] [Google Scholar]
- 54.Della Puppa A, Munari M, Gardiman MP, Volpin F. Combined Fluorescence Using 5-Aminolevulinic Acid and Fluorescein Sodium at Glioblastoma Border: Intraoperative Findings and Histopathologic Data About 3 Newly Diagnosed Consecutive Cases. World Neurosurgery. 2019;122:e856–e863. [DOI] [PubMed] [Google Scholar]
- 55.Luo H, Hernandez R, Hong H, Graves SA, Yang Y, England CG, Theuer CP, Nickles RJ, Cai W. Noninvasive brain cancer imaging with a bispecific antibody fragment, generated via click chemistry. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(41):12806–12811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miller SE, Tummers WS, Teraphongphom N, van den Berg NS, Hasan A, Ertsey RD, Nagpal S, Recht LD, Plowey ED, Vogel H, Harsh GR, Grant GA, Li GH, Rosenthal EL. First-in-human intraoperative near-infrared fluorescence imaging of glioblastoma using cetuximab-IRDye800. Journal of Neuro-Oncology. 2018;139(1):135–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nimsky C, Ganslandt O, Hastreiter P, Fahlbusch R. Intraoperative compensation for brain shift. Surgical Neurology. 2001;56(6):357–364. [DOI] [PubMed] [Google Scholar]
- 58.Ohue S, Kumon Y, Nagato S, Kohno S, Harada H, Nakagawa K, Kikuchi K, Miki H, Ohnishi T. Evaluation of Intraoperative Brain Shift Using an Ultrasound-Linked Navigation System for Brain Tumor Surgery. Neurologia medico-chirurgica. 2010;50(4):291–300. [DOI] [PubMed] [Google Scholar]
- 59.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJB, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for R, Treatment of Cancer Brain T, Radiotherapy G, National Cancer Institute of Canada Clinical Trials G. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. The New England Journal of Medicine. 2005;352(10):987–996. [DOI] [PubMed] [Google Scholar]
- 60.Syro LV, Rotondo F, Camargo M, Ortiz LD, Serna CA, Kovacs K. Temozolomide and Pituitary Tumors: Current Understanding, Unresolved Issues, and Future Directions. Frontiers in Endocrinology. 2018;9:318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Knizhnik AV, Roos WP, Nikolova T, Quiros S, Tomaszowski K-H, Christmann M, Kaina B. Survival and death strategies in glioma cells: autophagy, senescence and apoptosis triggered by a single type of temozolomideinduced DNA damage. PloS One. 2013;8(1):e55665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aasland D, Götzinger L, Hauck L, Berte N, Meyer J, Effenberger M, Schneider S, Reuber EE, Roos WP, Tomicic MT, Kaina B, Christmann M. Temozolomide Induces Senescence and Repression of DNA Repair Pathways in Glioblastoma Cells via Activation of ATR-CHK1, p21, and NF-κB. Cancer Research. 2019;79(1):99–113. [DOI] [PubMed] [Google Scholar]
- 63.Kaina B, Ziouta A, Ochs K, Coquerelle T. Chromosomal instability, reproductive cell death and apoptosis induced by O6-methylguanine in Mex−, Mex+ and methylation-tolerant mismatch repair compromised cells: facts and models. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis. 1997;381(2):227–241 [DOI] [PubMed] [Google Scholar]
- 64.Meikrantz W, Bergom MA, Memisoglu A, Samson L. O6-alkylguanine DNA lesions trigger apoptosis. Carcinogenesis. 1998;19(2):369–372. [DOI] [PubMed] [Google Scholar]
- 65.Chakravarti A, Erkkinen MG, Nestler U, Stupp R, Mehta M, Aldape K, Gilbert MR, Black PM, Loeffler JS. Temozolomide-mediated radiation enhancement in glioblastoma: a report on underlying mechanisms. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2006;12(15):4738–4746. [DOI] [PubMed] [Google Scholar]
- 66.Gerber DE, Grossman SA, Zeltzman M, Parisi MA, Kleinberg L. The impact of thrombocytopenia from temozolomide and radiation in newly diagnosed adults with high-grade gliomas. Neuro-Oncology. 2007;9(1):47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Le Rhun E, Devos P, Houillier C, Cartalat S, Chinot O, Di Stefano AL, Lepage C, Reyns N, Dubois F, Weller M. Romiplostim for temozolomide-induced thrombocytopenia in glioblastoma: The PLATUM trial. Neurology. 2019;93(19):e1799–e1806. [DOI] [PubMed] [Google Scholar]
- 68.Dixit S, Baker L, Walmsley V, Hingorani M. Temozolomide-related idiosyncratic and other uncommon toxicities: a systematic review. Anti-Cancer Drugs. 2012;23(10):1099–1106. [DOI] [PubMed] [Google Scholar]
- 69.Brent TP, Remack JS. Formation of covalent complexes between human O6-alkylguanine-DNA alkyltransferase and BCNU-treated defined length synthetic oligodeoxynucleotides. Nucleic Acids Research. 1988;16(14B):6779–6788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grossman SA, Reinhard C, Colvin OM, Chasin M, Brundrett R, Tamargo RJ, Brem H. The intracerebral distribution of BCNU delivered by surgically implanted biodegradable polymers. Journal of Neurosurgery. 1992;76(4):640–647. [DOI] [PubMed] [Google Scholar]
- 71.Gajewski TF, Sosman J, Gerson SL, Liu L, Dolan E, Lin S, Vokes EE. Phase II trial of the O6-alkylguanine DNA alkyltransferase inhibitor O6-benzylguanine and 1,3-bis(2-chloroethyl)-1-nitrosourea in advanced melanoma. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2005;11(21):7861–7865. [DOI] [PubMed] [Google Scholar]
- 72.Bock HC, Puchner MJA, Lohmann F, Schütze M, Koll S, Ketter R, Buchalla R, Rainov N, Kantelhardt SR, Rohde V, Giese A. First-line treatment of malignant glioma with carmustine implants followed by concomitant radiochemotherapy: a multicenter experience. Neurosurgical Review. 2010;33(4):441–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bartzatt R Lomustine analogous drug structures for intervention of brain and spinal cord tumors: the benefit of in silico substructure search and analysis. Chemother Res Pract. 2013;2013:360624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Brandes AA, Finocchiaro G, Zagonel V, Reni M, Caserta C, Fabi A, Clavarezza M, Maiello E, Eoli M, Lombardi G, Monteforte M, Proietti E, Agati R, Eusebi V, Franceschi E. AVAREG: a phase II, randomized, noncomparative study of fotemustine or bevacizumab for patients with recurrent glioblastoma. Neuro-Oncology. 2016;18(9):1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ameratunga M, Pavlakis N, Wheeler H, Grant R, Simes J, Khasraw M. Anti‐angiogenic therapy for high‐grade glioma. The Cochrane Database of Systematic Reviews. 2018;2018(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WKA, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2009;27(28):4733–4740. [DOI] [PubMed] [Google Scholar]
- 77.Ozel O, Kurt M, Ozdemir O, Bayram J, Akdeniz H, Koca D. Complete response to bevacizumab plus irinotecan in patients with rapidly progressive GBM: Cases report and literature review. Journal of Oncological Sciences. 2016;2(2):87–94. [Google Scholar]
- 78.Diaz RJ, Ali S, Qadir MG, De La Fuente MI, Ivan ME, Komotar RJ. The role of bevacizumab in the treatment of glioblastoma. Journal of Neuro-Oncology. 2017;133(3):455–467. [DOI] [PubMed] [Google Scholar]
- 79.Cabrera AR, Kirkpatrick JP, Fiveash JB, Shih HA, Koay EJ, Lutz S, Petit J, Chao ST, Brown PD, Vogelbaum M, Reardon DA, Chakravarti A, Wen PY, Chang E. Radiation therapy for glioblastoma: Executive summary of an American Society for Radiation Oncology Evidence-Based Clinical Practice Guideline. Practical Radiation Oncology. 2016;6(4):217–225. [DOI] [PubMed] [Google Scholar]
- 80.Murshed H. Chapter 3 - Radiation Biology. In: Murshed H, editor. Fundamentals of Radiation Oncology (Third Edition): Academic Press; 2019. p. 57–87 [Google Scholar]
- 81.Hochberg FH, Pruitt A. Assumptions in the radiotherapy of glioblastoma. Neurology. 1980;30(9):907–911. [DOI] [PubMed] [Google Scholar]
- 82.Liu P, Liu G, Wang G, Zhou W, Sun Y, Chen W, Zeng Q, Hong J, Xie Q, Ou L, Wei R. Comparison of Dosimetric Gains Provided by Intensity-Modulated Radiotherapy, Volume-Modulated Arc Therapy, and Helical Tomotherapy for High-Grade Glioma. BioMed Research International. 2020;2020:4258989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Narayana A, Yamada J, Berry S, Shah P, Hunt M, Gutin PH, Leibel SA. Intensity-modulated radiotherapy in highgrade gliomas: clinical and dosimetric results. International Journal of Radiation Oncology, Biology, Physics. 2006;64(3):892–897. [DOI] [PubMed] [Google Scholar]
- 84.Ganz JC. The journey from proton to gamma knife. Progress in Brain Research. 2014;215:67–75. [DOI] [PubMed] [Google Scholar]
- 85.Leber KA, Berglöff J, Pendl G. Dose-response tolerance of the visual pathways and cranial nerves of the cavernous sinus to stereotactic radiosurgery. Journal of Neurosurgery. 1998;88(1):43–50. [DOI] [PubMed] [Google Scholar]
- 86.Redmond KJ, Mehta M. Stereotactic Radiosurgery for Glioblastoma. Cureus. 2015;7(12 ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Barbarite E, Sick JT, Berchmans E, Bregy A, Shah AH, Elsayyad N, Komotar RJ. The role of brachytherapy in the treatment of glioblastoma multiforme. Neurosurgical Review. 2017;40(2):195–211. [DOI] [PubMed] [Google Scholar]
- 88.Laperriere NJ, Leung PM, McKenzie S, Milosevic M, Wong S, Glen J, Pintilie M, Bernstein M. Randomized study of brachytherapy in the initial management of patients with malignant astrocytoma. International Journal of Radiation Oncology, Biology, Physics. 1998;41(5):1005–1011. [DOI] [PubMed] [Google Scholar]
- 89.Selker RG, Shapiro WR, Burger P, Blackwood MS, Arena VC, Gilder JC, Malkin MG, Mealey JJ, Neal JH, Olson J, Robertson JT, Barnett GH, Bloomfield S, Albright R, Hochberg FH, Hiesiger E, Green S, Brain Tumor Cooperative G. The Brain Tumor Cooperative Group NIH Trial 87–01: a randomized comparison of surgery, external radiotherapy, and carmustine versus surgery, interstitial radiotherapy boost, external radiation therapy, and carmustine. Neurosurgery. 2002;51(2):343–355; discussion 355–357. [PubMed] [Google Scholar]
- 90.Chen AM, Chang S, Pouliot J, Sneed PK, Prados MD, Lamborn KR, Malec MK, McDermott MW, Berger MS, Larson DA. Phase I Trial of Gross Total Resection, Permanent Iodine-125 Brachytherapy, and Hyperfractionated Radiotherapy for Newly Diagnosed Glioblastoma Multiforme. International Journal of Radiation Oncology*Biology*Physics. 2007;69(3):825–830 [DOI] [PubMed] [Google Scholar]
- 91.Parvez K, Parvez A, Zadeh G. The diagnosis and treatment of pseudoprogression, radiation necrosis and brain tumor recurrence. International Journal of Molecular Sciences. 2014;15(7):11832–11846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pompos A, Durante M, Choy H. Heavy Ions in Cancer Therapy. JAMA Oncol. 2016;2(12):1539–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chiblak S, Tang Z, Lemke D, Knoll M, Dokic I, Warta R, Moustafa M, Mier W, Brons S, Rapp C, Muschal S, Seidel P, Bendszus M, Adeberg S, Wiestler OD, Haberkorn U, Debus J, Herold-Mende C, Wick W, Abdollahi A. Carbon irradiation overcomes glioma radioresistance by eradicating stem cells and forming an antiangiogenic and immunopermissive niche. JCI Insight. 2019;4(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tomiyama A, Tachibana K, Suzuki K, Seino S, Sunayama J, Matsuda KI, Sato A, Matsumoto Y, Nomiya T, Nemoto K, Yamashita H, Kayama T, Ando K, Kitanaka C. MEK-ERK-dependent multiple caspase activation by mitochondrial proapoptotic Bcl-2 family proteins is essential for heavy ion irradiation-induced glioma cell death. Cell Death Dis. 2010;1:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kong L, Wu J, Gao J, Qiu X, Yang J, Hu J, Hu W, Mao Y, Lu JJ. Particle radiation therapy in the management of malignant glioma: Early experience at the Shanghai Proton and Heavy Ion Center. Cancer. 2020;126(12):2802–2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rockwell S, Dobrucki IT, Kim EY, Marrison ST, Vu VT. Hypoxia and radiation therapy: Past history, ongoing research, and future promise. Current molecular medicine. 2009;9(4):442–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yang Z, Wei D, Dai X, Stevens MFG, Bradshaw TD, Luo Y, Zhang J. C8-Substituted Imidazotetrazine Analogs Overcome Temozolomide Resistance by Inducing DNA Adducts and DNA Damage. Front Oncol. 2019;9:485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Verbeek B, Southgate TD, Gilham DE, Margison GP. O6-Methylguanine-DNA methyltransferase inactivation and chemotherapy. Br Med Bull. 2008;85:17–33. [DOI] [PubMed] [Google Scholar]
- 99.Weller M Assessing the MGMT status in glioblastoma: one step forward, two steps back? Neuro Oncol. 2013;15(3):253–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thon N, Kreth S, Kreth FW. Personalized treatment strategies in glioblastoma: MGMT promoter methylation status. Onco Targets Ther. 2013;6:1363–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Szopa W, Burley TA, Kramer-Marek G, Kaspera W. Diagnostic and Therapeutic Biomarkers in Glioblastoma: Current Status and Future Perspectives. Biomed Res Int. 2017;2017:8013575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cabrini G, Fabbri E, Lo Nigro C, Dechecchi MC, Gambari R. Regulation of expression of O6-methylguanine-DNA methyltransferase and the treatment of glioblastoma (Review). Int J Oncol. 2015;47(2):417–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pandith AA, Qasim I, Zahoor W, Shah P, Bhat AR, Sanadhya D, Shah ZA, Naikoo NA. Concordant association validates MGMT methylation and protein expression as favorable prognostic factors in glioma patients on alkylating chemotherapy (Temozolomide). Sci Rep. 2018;8(1):6704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Binabaj MM, Bahrami A, ShahidSales S, Joodi M, Joudi Mashhad M, Hassanian SM, Anvari K, Avan A. The prognostic value of MGMT promoter methylation in glioblastoma: A meta-analysis of clinical trials. J Cell Physiol. 2018;233(1):378–386. [DOI] [PubMed] [Google Scholar]
- 105.Meng W, Jiang Y, Ma J. Is the prognostic significance of O6-methylguanine- DNA methyltransferase promoter methylation equally important in glioblastomas of patients from different continents? A systematic review with meta-analysis. Cancer Manag Res. 2017;9:411–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Christians A, Hartmann C, Benner A, Meyer J, von Deimling A, Weller M, Wick W, Weiler M. Prognostic value of three different methods of MGMT promoter methylation analysis in a prospective trial on newly diagnosed glioblastoma. PLoS One. 2012;7(3):e33449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Forte IM, Indovina P, Iannuzzi CA, Cirillo D, Di Marzo D, Barone D, Capone F, Pentimalli F, Giordano A. Targeted therapy based on p53 reactivation reduces both glioblastoma cell growth and resistance to temozolomide. Int J Oncol. 2019;54(6):2189–2199. [DOI] [PubMed] [Google Scholar]
- 108.Nie E, Jin X, Wu W, Yu T, Zhou X, Zhi T, Shi Z, Zhang J, Liu N, You Y. BACH1 Promotes Temozolomide Resistance in Glioblastoma through Antagonizing the Function of p53. Sci Rep. 2016;6:39743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lotfi M, Afsharnezhad S, Raziee HR, Ghaffarzadegan K, Sharif S, Shamsara J, Lary S, Behravan J. Immunohistochemical assessment of MGMT expression and p53 mutation in glioblastoma multiforme. Tumori. 2011;97(1):104–108. [DOI] [PubMed] [Google Scholar]
- 110.He ZC, Ping YF, Xu SL, Lin Y, Yu SC, Kung HF, Bian XW. Lower MGMT expression predicts better prognosis in proneural-like glioblastoma. Int J Clin Exp Med. 2015;8(11):20287–20294. [PMC free article] [PubMed] [Google Scholar]
- 111.Baran K, Yang M, Dillon CP, Samson LL, Green DR. The proline rich domain of p53 is dispensable for MGMT-dependent DNA repair and cell survival following alkylation damage. Cell Death Differ. 2017;24(11):1925–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bocangel D, Sengupta S, Mitra S, Bhakat KK. p53-Mediated down-regulation of the human DNA repair gene O6-methylguanine-DNA methyltransferase (MGMT) via interaction with Sp1 transcription factor. Anticancer Res. 2009;29(10):3741–3750. [PMC free article] [PubMed] [Google Scholar]
- 113.Chang KY, Hsu TI, Hsu CC, Tsai SY, Liu JJ, Chou SW, Liu MS, Liou JP, Ko CY, Chen KY, Hung JJ, Chang WC, Chuang CK, Kao TJ, Chuang JY. Specificity protein 1-modulated superoxide dismutase 2 enhances temozolomide resistance in glioblastoma, which is independent of O(6)-methylguanine-DNA methyltransferase. Redox Biol. 2017;13:655–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aasland D, Reich TR, Tomicic MT, Switzeny OJ, Kaina B, Christmann M. Repair gene O(6) -methylguanine-DNA methyltransferase is controlled by SP1 and up-regulated by glucocorticoids, but not by temozolomide and radiation. J Neurochem. 2018;144(2):139–151. [DOI] [PubMed] [Google Scholar]
- 115.Christmann M, Kaina B. Transcriptional regulation of human DNA repair genes following genotoxic stress: trigger mechanisms, inducible responses and genotoxic adaptation. Nucleic Acids Res. 2013;41(18):8403–8420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Avci NG, Ebrahimzadeh-Pustchi S, Akay YM, Esquenazi Y, Tandon N, Zhu JJ, Akay M. NF-kappaB inhibitor with Temozolomide results in significant apoptosis in glioblastoma via the NF-kappaB(p65) and actin cytoskeleton regulatory pathways. Sci Rep. 2020;10(1):13352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yu Z, Chen Y, Wang S, Li P, Zhou G, Yuan Y. Inhibition of NF-kappaB results in anti-glioma activity and reduces temozolomide-induced chemoresistance by down-regulating MGMT gene expression. Cancer Lett. 2018;428:7789. [DOI] [PubMed] [Google Scholar]
- 118.Yu W, Zhang L, Wei Q, Shao A. O(6)-Methylguanine-DNA Methyltransferase (MGMT): Challenges and New Opportunities in Glioma Chemotherapy. Front Oncol. 2019;9:1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Medvedeva YA, Khamis AM, Kulakovskiy IV, Ba-Alawi W, Bhuyan MS, Kawaji H, Lassmann T, Harbers M, Forrest AR, Bajic VB, consortium F. Effects of cytosine methylation on transcription factor binding sites. BMC Genomics. 2014;15:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lo Dico A, Martelli C, Diceglie C, Lucignani G, Ottobrini L. Hypoxia-Inducible Factor-1alpha Activity as a Switch for Glioblastoma Responsiveness to Temozolomide. Front Oncol. 2018;8:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fidoamore A, Cristiano L, Antonosante A, d’Angelo M, Di Giacomo E, Astarita C, Giordano A, Ippoliti R, Benedetti E, Cimini A. Glioblastoma Stem Cells Microenvironment: The Paracrine Roles of the Niche in Drug and Radioresistance. Stem Cells Int. 2016;2016:6809105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Codrici E, Enciu AM, Popescu ID, Mihai S, Tanase C. Glioma Stem Cells and Their Microenvironments: Providers of Challenging Therapeutic Targets. Stem Cells Int. 2016;2016:5728438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Romani M, Pistillo MP, Banelli B. Epigenetic Targeting of Glioblastoma. Front Oncol. 2018;8:448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yang J, Zhu XB, He LX, Gu ZW, Jin MZ, Ji WY. Clinical significance of epigenetic silencing and re-expression of O6-methylguanine-DNA methyltransferase using epigenetic agents in laryngeal carcinoma. Oncol Lett. 2015;9(1):35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nowacka-Zawisza M, Wisnik E. DNA methylation and histone modifications as epigenetic regulation in prostate cancer (Review). Oncol Rep. 2017;38(5):2587–2596. [DOI] [PubMed] [Google Scholar]
- 126.Erasimus H, Gobin M, Niclou S, Van Dyck E. DNA repair mechanisms and their clinical impact in glioblastoma. Mutat Res Rev Mutat Res. 2016;769:19–35. [DOI] [PubMed] [Google Scholar]
- 127.Reyes GX, Schmidt TT, Kolodner RD, Hombauer H. New insights into the mechanism of DNA mismatch repair. Chromosoma. 2015;124(4):443–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gao D, Herman JG, Guo M. The clinical value of aberrant epigenetic changes of DNA damage repair genes in human cancer. Oncotarget. 2016;7(24):37331–37346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Modrich P, Lahue R. Mismatch repair in replication fidelity, genetic recombination, and cancer biology. Annu Rev Biochem. 1996;65:101–133. [DOI] [PubMed] [Google Scholar]
- 130.Noonan EM, Shah D, Yaffe MB, Lauffenburger DA, Samson LD. O6-Methylguanine DNA lesions induce an intra-S-phase arrest from which cells exit into apoptosis governed by early and late multi-pathway signaling network activation. Integr Biol (Camb). 2012;4(10):1237–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Perazzoli G, Prados J, Ortiz R, Caba O, Cabeza L, Berdasco M, Gonzalez B, Melguizo C. Temozolomide Resistance in Glioblastoma Cell Lines: Implication of MGMT, MMR, P-Glycoprotein and CD133 Expression. PLoS One. 2015;10(10):e0140131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Stritzelberger J, Distel L, Buslei R, Fietkau R, Putz F. Acquired temozolomide resistance in human glioblastoma cell line U251 is caused by mismatch repair deficiency and can be overcome by lomustine. Clin Transl Oncol. 2018;20(4):508–516. [DOI] [PubMed] [Google Scholar]
- 133.Network TC. Corrigendum: Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2013;494(7438):506. [DOI] [PubMed] [Google Scholar]
- 134.McFaline-Figueroa JL, Braun CJ, Stanciu M, Nagel ZD, Mazzucato P, Sangaraju D, Cerniauskas E, Barford K, Vargas A, Chen Y, Tretyakova N, Lees JA, Hemann MT, White FM, Samson LD. Minor Changes in Expression of the Mismatch Repair Protein MSH2 Exert a Major Impact on Glioblastoma Response to Temozolomide. Cancer Res. 2015;75(15):3127–3138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sun Q, Pei C, Li Q, Dong T, Dong Y, Xing W, Zhou P, Gong Y, Zhen Z, Gao Y, Xiao Y, Su J, Ren H. Up-regulation of MSH6 is associated with temozolomide resistance in human glioblastoma. Biochem Biophys Res Commun. 2018;496(4):1040–1046. [DOI] [PubMed] [Google Scholar]
- 136.Felsberg J, Thon N, Eigenbrod S, Hentschel B, Sabel MC, Westphal M, Schackert G, Kreth FW, Pietsch T, Loffler M, Weller M, Reifenberger G, Tonn JC, German Glioma N. Promoter methylation and expression of MGMT and the DNA mismatch repair genes MLH1, MSH2, MSH6 and PMS2 in paired primary and recurrent glioblastomas. Int J Cancer. 2011;129(3):659–670. [DOI] [PubMed] [Google Scholar]
- 137.Stark AM, Doukas A, Hugo HH, Hedderich J, Hattermann K, Maximilian Mehdorn H, Held-Feindt J. Expression of DNA mismatch repair proteins MLH1, MSH2, and MSH6 in recurrent glioblastoma. Neurol Res. 2015;37(2):95105. [DOI] [PubMed] [Google Scholar]
- 138.Yip S, Miao J, Cahill DP, Iafrate AJ, Aldape K, Nutt CL, Louis DN. MSH6 mutations arise in glioblastomas during temozolomide therapy and mediate temozolomide resistance. Clin Cancer Res. 2009;15(14):4622–4629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gimple RC, Bhargava S, Dixit D, Rich JN. Glioblastoma stem cells: lessons from the tumor hierarchy in a lethal cancer. Genes Dev. 2019;33(11–12):591–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Dirkse A, Golebiewska A, Buder T, Nazarov PV, Muller A, Poovathingal S, Brons NHC, Leite S, Sauvageot N, Sarkisjan D, Seyfrid M, Fritah S, Stieber D, Michelucci A, Hertel F, Herold-Mende C, Azuaje F, Skupin A, Bjerkvig R, Deutsch A, Voss-Bohme A, Niclou SP. Stem cell-associated heterogeneity in Glioblastoma results from intrinsic tumor plasticity shaped by the microenvironment. Nat Commun. 2019;10(1):1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB. Identification of human brain tumour initiating cells. Nature. 2004;432(7015):396–401. [DOI] [PubMed] [Google Scholar]
- 142.Glumac PM, LeBeau AM. The role of CD133 in cancer: a concise review. Clin Transl Med. 2018;7(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yan Y, Zuo X, Wei D. Concise Review: Emerging Role of CD44 in Cancer Stem Cells: A Promising Biomarker and Therapeutic Target. Stem Cells Transl Med. 2015;4(9):1033–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zinzi L, Contino M, Cantore M, Capparelli E, Leopoldo M, Colabufo NA. ABC transporters in CSCs membranes as a novel target for treating tumor relapse. Front Pharmacol. 2014;5:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Si D, Yin F, Peng J, Zhang G. High Expression of CD44 Predicts a Poor Prognosis in Glioblastomas. Cancer Manag Res. 2020;12:769–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.McCord AM, Jamal M, Williams ES, Camphausen K, Tofilon PJ. CD133+ glioblastoma stem-like cells are radiosensitive with a defective DNA damage response compared with established cell lines. Clin Cancer Res. 2009;15(16):5145–5153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB, Dewhirst MW, Bigner DD, Rich JN. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444(7120):756–760. [DOI] [PubMed] [Google Scholar]
- 148.Ahmed SU, Carruthers R, Gilmour L, Yildirim S, Watts C, Chalmers AJ. Selective Inhibition of Parallel DNA Damage Response Pathways Optimizes Radiosensitization of Glioblastoma Stem-like Cells. Cancer Res. 2015;75(20):4416–4428. [DOI] [PubMed] [Google Scholar]
- 149.Facchino S, Abdouh M, Chatoo W, Bernier G. BMI1 confers radioresistance to normal and cancerous neural stem cells through recruitment of the DNA damage response machinery. J Neurosci. 2010;30(30):10096–10111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tachon G, Cortes U, Guichet PO, Rivet P, Balbous A, Masliantsev K, Berger A, Boissonnade O, Wager M, Karayan-Tapon L. Cell Cycle Changes after Glioblastoma Stem Cell Irradiation: The Major Role of RAD51. Int J Mol Sci. 2018;19(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wijaya J, Fukuda Y, Schuetz JD. Obstacles to Brain Tumor Therapy: Key ABC Transporters. Int J Mol Sci. 2017;18(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Uribe D, Torres A, Rocha JD, Niechi I, Oyarzun C, Sobrevia L, San Martin R, Quezada C. Multidrug resistance in glioblastoma stem-like cells: Role of the hypoxic microenvironment and adenosine signaling. Mol Aspects Med. 2017;55:140–151. [DOI] [PubMed] [Google Scholar]
- 153.Westover D, Li F. New trends for overcoming ABCG2/BCRP-mediated resistance to cancer therapies. J Exp Clin Cancer Res. 2015;34:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Peignan L, Garrido W, Segura R, Melo R, Rojas D, Carcamo JG, San Martin R, Quezada C. Combined use of anticancer drugs and an inhibitor of multiple drug resistance-associated protein-1 increases sensitivity and decreases survival of glioblastoma multiforme cells in vitro. Neurochem Res. 2011;36(8):1397–1406. [DOI] [PubMed] [Google Scholar]
- 155.Tivnan A, Zakaria Z, O’Leary C, Kogel D, Pokorny JL, Sarkaria JN, Prehn JH. Inhibition of multidrug resistance protein 1 (MRP1) improves chemotherapy drug response in primary and recurrent glioblastoma multiforme. Front Neurosci. 2015;9:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Huang WJ, Chen WW, Zhang X. Glioblastoma multiforme: Effect of hypoxia and hypoxia inducible factors on therapeutic approaches. Oncol Lett. 2016;12(4):2283–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kolenda J, Jensen SS, Aaberg-Jessen C, Christensen K, Andersen C, Brunner N, Kristensen BW. Effects of hypoxia on expression of a panel of stem cell and chemoresistance markers in glioblastoma-derived spheroids. J Neurooncol. 2011;103(1):43–58. [DOI] [PubMed] [Google Scholar]
- 158.Lee CAA, Banerjee P, Wilson BJ, Wu S, Guo Q, Berg G, Karpova S, Mishra A, Lian JW, Tran J, Emmerich M, Murphy GF, Frank MH, Frank NY. Targeting the ABC transporter ABCB5 sensitizes glioblastoma to temozolomide-induced apoptosis through a cell-cycle checkpoint regulation mechanism. J Biol Chem. 2020;295(22):7774–7788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jing X, Yang F, Shao C, Wei K, Xie M, Shen H, Shu Y. Role of hypoxia in cancer therapy by regulating the tumor microenvironment. Mol Cancer. 2019;18(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gomez CR. Editorial: Tumor Hypoxia: Impact in Tumorigenesis, Diagnosis, Prognosis, and Therapeutics. Front Oncol. 2016;6:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Walsh JC, Lebedev A, Aten E, Madsen K, Marciano L, Kolb HC. The Clinical Importance of Assessing Tumor Hypoxia: Relationship of Tumor Hypoxia to Prognosis and Therapeutic Opportunities. Antioxidants & Redox Signaling. 2014;21(10):1516–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Monteiro AR, Hill R, Pilkington GJ, Madureira PA. The Role of Hypoxia in Glioblastoma Invasion. Cells. 2017;6(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kaur B, Khwaja FW, Severson EA, Matheny SL, Brat DJ, Van Meir EG. Hypoxia and the hypoxia-inducible-factor pathway in glioma growth and angiogenesis. Neuro Oncol. 2005;7(2):134–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kocaturk NM, Gozuacik D. Crosstalk Between Mammalian Autophagy and the Ubiquitin-Proteasome System. Front Cell Dev Biol. 2018;6:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Logun M, Zhao W, Mao L, Karumbaiah L. Microfluidics in Malignant Glioma Research and Precision Medicine. Adv Biosyst. 2018;2(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Daskalaki I, Gkikas I, Tavernarakis N. Hypoxia and Selective Autophagy in Cancer Development and Therapy. Front Cell Dev Biol. 2018;6:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Glick D, Barth S, Macleod KF. Autophagy: cellular and molecular mechanisms. J Pathol. 2010;221(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hewitt G, Korolchuk VI. Repair, Reuse, Recycle: The Expanding Role of Autophagy in Genome Maintenance. Trends Cell Biol. 2017;27(5):340–351. [DOI] [PubMed] [Google Scholar]
- 169.Jawhari S, Ratinaud MH, Verdier M. Glioblastoma, hypoxia and autophagy: a survival-prone ‘menage-a-trois’. Cell Death Dis. 2016;7(10):e2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Talukdar S, Pradhan AK, Bhoopathi P, Shen XN, August LA, Windle JJ, Sarkar D, Furnari FB, Cavenee WK, Das SK, Emdad L, Fisher PB. MDA-9/Syntenin regulates protective autophagy in anoikis-resistant glioma stem cells. Proc Natl Acad Sci U S A. 2018;115(22):5768–5773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Huang T, Kim CK, Alvarez AA, Pangeni RP, Wan X, Song X, Shi T, Yang Y, Sastry N, Horbinski CM, Lu S, Stupp R, Kessler JA, Nishikawa R, Nakano I, Sulman EP, Lu X, James CD, Yin XM, Hu B, Cheng SY. MST4 Phosphorylation of ATG4B Regulates Autophagic Activity, Tumorigenicity, and Radioresistance in Glioblastoma. Cancer Cell. 2017;32(6):840–855 e848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Buccarelli M, Marconi M, Pacioni S, De Pascalis I, D’Alessandris QG, Martini M, Ascione B, Malorni W, Larocca LM, Pallini R, Ricci-Vitiani L, Matarrese P. Inhibition of autophagy increases susceptibility of glioblastoma stem cells to temozolomide by igniting ferroptosis. Cell Death Dis. 2018;9(8):841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wu W, Schecker J, Wurstle S, Schneider F, Schonfelder M, Schlegel J. Aldehyde dehydrogenase 1A3 (ALDH1A3) is regulated by autophagy in human glioblastoma cells. Cancer Lett. 2018;417:112–123. [DOI] [PubMed] [Google Scholar]
- 174.Wu W, Wu Y, Mayer K, von Rosenstiel C, Schecker J, Baur S, Wurstle S, Liesche-Starnecker F, Gempt J, Schlegel J. Lipid Peroxidation Plays an Important Role in Chemotherapeutic Effects of Temozolomide and the Development of Therapy Resistance in Human Glioblastoma. Transl Oncol. 2020;13(3):100748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Hu YL, DeLay M, Jahangiri A, Molinaro AM, Rose SD, Carbonell WS, Aghi MK. Hypoxia-induced autophagy promotes tumor cell survival and adaptation to antiangiogenic treatment in glioblastoma. Cancer Res. 2012;72(7):1773–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sotelo J, Briceno E, Lopez-Gonzalez MA. Adding chloroquine to conventional treatment for glioblastoma multiforme: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2006;144(5):337–343. [DOI] [PubMed] [Google Scholar]
- 177.Wainwright EN, Scaffidi P. Epigenetics and Cancer Stem Cells: Unleashing, Hijacking, and Restricting Cellular Plasticity. Trends Cancer. 2017;3(5):372–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mishra A, Verma M. Epigenetics of solid cancer stem cells. Methods Mol Biol. 2012;863:15–31. [DOI] [PubMed] [Google Scholar]
- 179.Toh TB, Lim JJ, Chow EK. Epigenetics in cancer stem cells. Mol Cancer. 2017;16(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lapinska K, Faria G, McGonagle S, Macumber KM, Heerboth S, Sarkar S. Cancer Progenitor Cells: The Result of an Epigenetic Event? Anticancer Res. 2018;38(1):1–6. [DOI] [PubMed] [Google Scholar]
- 181.Wei JW, Huang K, Yang C, Kang CS. Non-coding RNAs as regulators in epigenetics (Review). Oncol Rep. 2017;37(1):3–9. [DOI] [PubMed] [Google Scholar]
- 182.Joh RI, Palmieri CM, Hill IT, Motamedi M. Regulation of histone methylation by noncoding RNAs. Biochim Biophys Acta. 2014;1839(12):1385–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Tao H, Li H, Su Y, Feng D, Wang X, Zhang C, Ma H, Hu Q. Histone methyltransferase G9a and H3K9 dimethylation inhibit the self-renewal of glioma cancer stem cells. Mol Cell Biochem. 2014;394(1–2):23–30. [DOI] [PubMed] [Google Scholar]
- 184.Liu BL, Cheng JX, Zhang X, Wang R, Zhang W, Lin H, Xiao X, Cai S, Chen XY, Cheng H. Global histone modification patterns as prognostic markers to classify glioma patients. Cancer Epidemiol Biomarkers Prev. 2010;19(11):2888–2896. [DOI] [PubMed] [Google Scholar]
- 185.Hussain M, Rao M, Humphries AE, Hong JA, Liu F, Yang M, Caragacianu D, Schrump DS. Tobacco smoke induces polycomb-mediated repression of Dickkopf-1 in lung cancer cells. Cancer Res. 2009;69(8):3570–3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chen Y, Fang R, Yue C, Chang G, Li P, Guo Q, Wang J, Zhou A, Zhang S, Fuller GN, Shi X, Huang S. WntInduced Stabilization of KDM4C Is Required for Wnt/beta-Catenin Target Gene Expression and Glioblastoma Tumorigenesis. Cancer Res. 2020;80(5):1049–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Huang YC, Lin SJ, Shih HY, Chou CH, Chu HH, Chiu CC, Yuh CH, Yeh TH, Cheng YC. Epigenetic regulation of NOTCH1 and NOTCH3 by KMT2A inhibits glioma proliferation. Oncotarget. 2017;8(38):63110–63120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Tsung AJ, Guda MR, Asuthkar S, Labak CM, Purvis IJ, Lu Y, Jain N, Bach SE, Prasad DVR, Velpula KK. Methylation regulates HEY1 expression in glioblastoma. Oncotarget. 2017;8(27):44398–44409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Allen BK, Stathias V, Maloof ME, Vidovic D, Winterbottom EF, Capobianco AJ, Clarke J, Schurer S, Robbins DJ, Ayad NG. Epigenetic pathways and glioblastoma treatment: insights from signaling cascades. J Cell Biochem. 2015;116(3):351–363. [DOI] [PubMed] [Google Scholar]
- 190.Malatesta M, Steinhauer C, Mohammad F, Pandey DP, Squatrito M, Helin K. Histone acetyltransferase PCAF is required for Hedgehog-Gli-dependent transcription and cancer cell proliferation. Cancer Res. 2013;73(20):63236333. [DOI] [PubMed] [Google Scholar]
- 191.Bazzoni R, Bentivegna A. Role of Notch Signaling Pathway in Glioblastoma Pathogenesis. Cancers (Basel). 2019;11(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Lee Y, Lee JK, Ahn SH, Lee J, Nam DH. WNT signaling in glioblastoma and therapeutic opportunities. Lab Invest. 2016;96(2):137–150. [DOI] [PubMed] [Google Scholar]
- 193.Touat M, Idbaih A, Sanson M, Ligon KL. Glioblastoma targeted therapy: updated approaches from recent biological insights. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2017;28(7):1457–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Rojo F, García-Parra J, Zazo S, Tusquets I, Ferrer-Lozano J, Menendez S, Eroles P, Chamizo C, Servitja S, Ramírez-Merino N, Lobo F, Bellosillo B, Corominas JM, Yelamos J, Serrano S, Lluch A, Rovira A, Albanell J. Nuclear PARP-1 protein overexpression is associated with poor overall survival in early breast cancer. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2012;23(5):1156–1164. [DOI] [PubMed] [Google Scholar]
- 195.Schreiber V, Dantzer F, Ame J-C, de Murcia G. Poly(ADP-ribose): novel functions for an old molecule. Nature Reviews Molecular Cell Biology. 2006;7(7):517–528. [DOI] [PubMed] [Google Scholar]
- 196.Gupta SK, Smith EJ, Mladek AC, Tian S, Decker PA, Kizilbash SH, Kitange GJ, Sarkaria JN. PARP Inhibitors for Sensitization of Alkylation Chemotherapy in Glioblastoma: Impact of Blood-Brain Barrier and Molecular Heterogeneity. Frontiers in Oncology. 2019;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Clarke MJ, Mulligan EA, Grogan PT, Mladek AC, Carlson BL, Schroeder MA, Curtin NJ, Lou Z, Decker PA, Wu W, Plummer ER, Sarkaria JN. Effective sensitization of temozolomide by ABT-888 is lost with development of temozolomide resistance in glioblastoma xenograft lines. Molecular Cancer Therapeutics. 2009;8(2):407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Malyuchenko NV, Kotova EY, Kulaeva OI, Kirpichnikov MP, Studitskiy VM. PARP1 Inhibitors: antitumor drug design. Acta Naturae. 2015;7(3):27–37. [PMC free article] [PubMed] [Google Scholar]
- 199.Lesueur P, Chevalier F, El-Habr EA, Junier M-P, Chneiweiss H, Castera L, Müller E, Stefan D, Saintigny Y. Radiosensitization Effect of Talazoparib, a Parp Inhibitor, on Glioblastoma Stem Cells Exposed to Low and High Linear Energy Transfer Radiation. Scientific Reports. 2018;8(1):3664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Robins HI, Zhang P, Gilbert MR, Chakravarti A, de Groot JF, Grimm SA, Wang F, Lieberman FS, Krauze A, Trotti AM, Mohile N, Kee AYJ, Colman H, Cavaliere R, Kesari S, Chmura SJ, Mehta M. A randomized phase I/II study of ABT-888 in combination with temozolomide in recurrent temozolomide resistant glioblastoma: an NRG oncology RTOG group study. Journal of Neuro-Oncology. 2016;126(2):309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Baxter PA, Su JM, Onar-Thomas A, Billups CA, Li X-N, Poussaint TY, Smith ER, Thompson P, Adesina A, Ansell P, Giranda V, Paulino A, Kilburn L, Quaddoumi I, Broniscer A, Blaney SM, Dunkel IJ, Fouladi M. A phase I/II study of veliparib (ABT-888) with radiation and temozolomide in newly diagnosed diffuse pontine glioma: a Pediatric Brain Tumor Consortium study. Neuro-Oncology. 2020;22(6):875–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Hanna C, Kurian KM, Williams K, Watts C, Jackson A, Carruthers R, Strathdee K, Cruickshank G, Dunn L, Erridge S, Godfrey L, Jefferies S, McBain C, Sleigh R, McCormick A, Pittman M, Halford S, Chalmers AJ. Pharmacokinetics, safety and tolerability of olaparib and temozolomide for recurrent glioblastoma: results of the phase I OPARATIC trial. Neuro-Oncology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Choi PJ, Cooper E, Schweder P, Mee E, Turner C, Faull R, Denny WA, Dragunow M, Park TIH, Jose J. PARP inhibitor cyanine dye conjugate with enhanced cytotoxic and antiproliferative activity in patient derived glioblastoma cell lines. Bioorganic & Medicinal Chemistry Letters. 2020;30(14):127252. [DOI] [PubMed] [Google Scholar]
- 204.Parrish KE, Cen L, Murray J, Calligaris D, Kizilbash S, Mittapalli RK, Carlson BL, Schroeder MA, Sludden J, Boddy AV, Agar NYR, Curtin NJ, Elmquist WF, Sarkaria JN. Efficacy of PARP Inhibitor Rucaparib in Orthotopic Glioblastoma Xenografts Is Limited by Ineffective Drug Penetration into the Central Nervous System. Molecular Cancer Therapeutics. 2015;14(12):2735–2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wu S, Gao F, Zheng S, Zhang C, Martinez-Ledesma E, Ezhilarasan R, Ding J, Li X, Feng N, Multani A, Sulman EP, Verhaak RG, de Groot JF, Heffernan TP, Yung WKA, Koul D. EGFR Amplification Induces Increased DNA Damage Response and Renders Selective Sensitivity to Talazoparib (PARP Inhibitor) in Glioblastoma. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2020;26(6):1395–1407. [DOI] [PubMed] [Google Scholar]
- 206.Kizilbash SH, Gupta SK, Chang K, Kawashima R, Parrish KE, Carlson BL, Bakken KK, Mladek AC, Schroeder MA, Decker PA, Kitange GJ, Shen Y, Feng Y, Protter AA, Elmquist WF, Sarkaria JN. Restricted Delivery of Talazoparib Across the Blood-Brain Barrier Limits the Sensitizing Effects of PARP Inhibition on Temozolomide Therapy in Glioblastoma. Molecular Cancer Therapeutics. 2017;16(12):2735–2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Robinson DR, Wu YM, Lin SF. The protein tyrosine kinase family of the human genome. Oncogene. 2000;19(49):5548–5557. [DOI] [PubMed] [Google Scholar]
- 208.Jin N, Bi A, Lan X, Xu J, Wang X, Liu Y, Wang T, Tang S, Zeng H, Chen Z, Tan M, Ai J, Xie H, Zhang T, Liu D, Huang R, Song Y, Leung EL-H, Yao X, Ding J, Geng M, Lin S-H, Huang M. Identification of metabolic vulnerabilities of receptor tyrosine kinases-driven cancer. Nature Communications. 2019;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Yamazaki H, Fukui Y, Ueyama Y, Tamaoki N, Kawamoto T, Taniguchi S, Shibuya M. Amplification of the structurally and functionally altered epidermal growth factor receptor gene (c-erbB) in human brain tumors. Molecular and Cellular Biology. 1988;8(4):1816–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Singh D, Chan JM, Zoppoli P, Niola F, Sullivan R, Castano A, Liu EM, Reichel J, Porrati P, Pellegatta S, Qiu K, Gao Z, Ceccarelli M, Riccardi R, Brat DJ, Guha A, Aldape K, Golfinos JG, Zagzag D, Mikkelsen T, Finocchiaro G, Lasorella A, Rabadan R, Iavarone A. Transforming fusions of FGFR and TACC genes in human glioblastoma. Science (New York, NY). 2012;337(6099):1231–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Weathers S-P, de Groot J. VEGF Manipulation in Glioblastoma. Oncology (Williston Park, NY). 2015;29(10):720727. [PubMed] [Google Scholar]
- 212.Barber TD, Vogelstein B, Kinzler KW, Velculescu VE. Somatic mutations of EGFR in colorectal cancers and glioblastomas. The New England Journal of Medicine. 2004;351(27):2883. [DOI] [PubMed] [Google Scholar]
- 213.Fleming TP, Saxena A, Clark WC, Robertson JT, Oldfield EH, Aaronson SA, Ali IU. Amplification and/or overexpression of platelet-derived growth factor receptors and epidermal growth factor receptor in human glial tumors. Cancer Research. 1992;52(16):4550–4553. [PubMed] [Google Scholar]
- 214.Guo P, Hu B, Gu W, Xu L, Wang D, Huang H-JS, Cavenee WK, Cheng S-Y. Platelet-Derived Growth Factor-B Enhances Glioma Angiogenesis by Stimulating Vascular Endothelial Growth Factor Expression in Tumor Endothelia and by Promoting Pericyte Recruitment. The American Journal of Pathology. 2003;162(4):1083–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Batchelor TT, Duda DG, di Tomaso E, Ancukiewicz M, Plotkin SR, Gerstner E, Eichler AF, Drappatz J, Hochberg FH, Benner T, Louis DN, Cohen KS, Chea H, Exarhopoulos A, Loeffler JS, Moses MA, Ivy P, Sorensen AG, Wen PY, Jain RK. Phase II study of cediranib, an oral pan-vascular endothelial growth factor receptor tyrosine kinase inhibitor, in patients with recurrent glioblastoma. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2010;28(17):2817–2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Gerstner ER, Ye X, Duda DG, Levine MA, Mikkelsen T, Kaley TJ, Olson JJ, Nabors BL, Ahluwalia MS, Wen PY, Jain RK, Batchelor TT, Grossman S. A phase I study of cediranib in combination with cilengitide in patients with recurrent glioblastoma. Neuro-Oncology. 2015;17(10):1386–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Batchelor TT, Mulholland P, Neyns B, Nabors LB, Campone M, Wick A, Mason W, Mikkelsen T, Phuphanich S, Ashby LS, DeGroot J, Gattamaneni R, Cher L, Rosenthal M, Payer F, Jürgensmeier JM, Jain RK, Sorensen AG, Xu J, Liu Q, van den Bent M. Phase III Randomized Trial Comparing the Efficacy of Cediranib As Monotherapy, and in Combination With Lomustine, Versus Lomustine Alone in Patients With Recurrent Glioblastoma. Journal of Clinical Oncology. 2013;31(26):3212–3218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Brown N, McBain C, Nash S, Hopkins K, Sanghera P, Saran F, Phillips M, Dungey F, Clifton-Hadley L, Wanek K, Krell D, Jeffries S, Khan I, Smith P, Mulholland P. Multi-Center Randomized Phase II Study Comparing Cediranib plus Gefitinib with Cediranib plus Placebo in Subjects with Recurrent/Progressive Glioblastoma. PloS One. 2016;11(5):e0156369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Batchelor TT, Gerstner ER, Emblem KE, Duda DG, Kalpathy-Cramer J, Snuderl M, Ancukiewicz M, Polaskova P, Pinho MC, Jennings D, Plotkin SR, Chi AS, Eichler AF, Dietrich J, Hochberg FH, Lu-Emerson C, Iafrate AJ, Ivy SP, Rosen BR, Loeffler JS, Wen PY, Sorensen AG, Jain RK. Improved tumor oxygenation and survival in glioblastoma patients who show increased blood perfusion after cediranib and chemoradiation. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(47):19059–19064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kaplan AR, Gueble SE, Liu Y, Oeck S, Kim H, Yun Z, Glazer PM. Cediranib suppresses homology-directed DNA repair through down-regulation of BRCA1/2 and RAD51. Sci Transl Med. 2019;11(492). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Hundsberger T, Reardon DA, Wen PY. Angiogenesis inhibitors in tackling recurrent glioblastoma. Expert Review of Anticancer Therapy. 2017;17(6):507–515. [DOI] [PubMed] [Google Scholar]
- 222.Lu-Emerson C, Duda DG, Emblem KE, Taylor JW, Gerstner ER, Loeffler JS, Batchelor TT, Jain RK. Lessons from anti-vascular endothelial growth factor and anti-vascular endothelial growth factor receptor trials in patients with glioblastoma. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2015;33(10):1197–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Karpel-Massler G, Westhoff MA, Kast RE, Wirtz CR, Halatsch M-E. Erlotinib in glioblastoma: lost in translation? Anti-Cancer Agents in Medicinal Chemistry. 2011;11(8):748–755. [DOI] [PubMed] [Google Scholar]
- 224.Raizer JJ, Giglio P, Hu J, Groves M, Merrell R, Conrad C, Phuphanich S, Puduvalli VK, Loghin M, Paleologos N, Yuan Y, Liu D, Rademaker A, Yung WK, Vaillant B, Rudnick J, Chamberlain M, Vick N, Grimm S, Tremont-Lukats IW, De Groot J, Aldape K, Gilbert MR, Brain Tumor Trials C. A phase II study of bevacizumab and erlotinib after radiation and temozolomide in MGMT unmethylated GBM patients. Journal of Neuro-Oncology. 2016;126(1):185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Peereboom DM, Ahluwalia MS, Ye X, Supko JG, Hilderbrand SL, Phuphanich S, Nabors LB, Rosenfeld MR, Mikkelsen T, Grossman SA, New Approaches to Brain Tumor Therapy C. NABTT 0502: a phase II and pharmacokinetic study of erlotinib and sorafenib for patients with progressive or recurrent glioblastoma multiforme. Neuro-Oncology. 2013;15(4):490–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Reardon DA, Desjardins A, Vredenburgh JJ, Gururangan S, Friedman AH, Herndon JE, Marcello J, Norfleet JA, McLendon RE, Sampson JH, Friedman HS. Phase 2 trial of erlotinib plus sirolimus in adults with recurrent glioblastoma. Journal of Neuro-Oncology. 2010;96(2):219–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Addeo R, Zappavigna S, Parlato C, Caraglia M. Erlotinib: early clinical development in brain cancer. Expert Opinion on Investigational Drugs. 2014;23(7):1027–1037. [DOI] [PubMed] [Google Scholar]
- 228.Rich JN, Reardon DA, Peery T, Dowell JM, Quinn JA, Penne KL, Wikstrand CJ, Van Duyn LB, Dancey JE, McLendon RE, Kao JC, Stenzel TT, Ahmed Rasheed BK, Tourt-Uhlig SE, Herndon JE, Vredenburgh JJ, Sampson JH, Friedman AH, Bigner DD, Friedman HS. Phase II trial of gefitinib in recurrent glioblastoma. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2004;22(1):133–142. [DOI] [PubMed] [Google Scholar]
- 229.Chakravarti A, Wang M, Robins HI, Lautenschlaeger T, Curran WJ, Brachman DG, Schultz CJ, Choucair A, Dolled-Filhart M, Christiansen J, Gustavson M, Molinaro A, Mischel P, Dicker AP, Bredel M, Mehta M. RTOG 0211: a phase 1/2 study of radiation therapy with concurrent gefitinib for newly diagnosed glioblastoma patients. International Journal of Radiation Oncology, Biology, Physics. 2013;85(5):1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Kreisl TN, Lassman AB, Mischel PS, Rosen N, Scher HI, Teruya-Feldstein J, Shaffer D, Lis E, Abrey LE. A pilot study of everolimus and gefitinib in the treatment of recurrent glioblastoma (GBM). Journal of Neuro-Oncology. 2009;92(1):99–105. [DOI] [PubMed] [Google Scholar]
- 231.Uhm JH, Ballman KV, Wu W, Giannini C, Krauss JC, Buckner JC, James CD, Scheithauer BW, Behrens RJ, Flynn PJ, Schaefer PL, Dakhill SR, Jaeckle KA. Phase II evaluation of gefitinib in patients with newly diagnosed Grade 4 astrocytoma: Mayo/North Central Cancer Treatment Group Study N0074. International Journal of Radiation Oncology, Biology, Physics. 2011;80(2):347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Sautter L, Hofheinz R, Tuettenberg J, Grimm M, Vajkoczy P, Groden C, Schmieder K, Hochhaus A, Wenz F, Giordano FA. Open-Label Phase II Evaluation of Imatinib in Primary Inoperable or Incompletely Resected and Recurrent Glioblastoma. Oncology. 2020;98(1):16–22. [DOI] [PubMed] [Google Scholar]
- 233.Raymond E, Brandes AA, Dittrich C, Fumoleau P, Coudert B, Clement PMJ, Frenay M, Rampling R, Stupp R, Kros JM, Heinrich MC, Gorlia T, Lacombe D, van den Bent MJ, European Organisation for R, Treatment of Cancer Brain Tumor Group S. Phase II study of imatinib in patients with recurrent gliomas of various histologies: a European Organisation for Research and Treatment of Cancer Brain Tumor Group Study. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2008;26(28):4659–4665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Razis E, Selviaridis P, Labropoulos S, Norris JL, Zhu M-J, Song DD, Kalebic T, Torrens M, Kalogera-Fountzila A, Karkavelas G, Karanastasi S, Fletcher JA, Fountzilas G. Phase II study of neoadjuvant imatinib in glioblastoma: evaluation of clinical and molecular effects of the treatment. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2009;15(19):6258–6266. [DOI] [PubMed] [Google Scholar]
- 235.Reardon DA, Egorin MJ, Quinn JA, Rich JN, Gururangan I, Vredenburgh JJ, Desjardins A, Sathornsumetee S, Provenzale JM, Herndon JE, Dowell JM, Badruddoja MA, McLendon RE, Lagattuta TF, Kicielinski KP, Dresemann G, Sampson JH, Friedman AH, Salvado AJ, Friedman HS. Phase II Study of Imatinib Mesylate Plus Hydroxyurea in Adults With Recurrent Glioblastoma Multiforme. Journal of Clinical Oncology. 2005;23(36):93599368. [DOI] [PubMed] [Google Scholar]
- 236.Reardon DA, Dresemann G, Taillibert S, Campone M, van den Bent M, Clement P, Blomquist E, Gordower L, Schultz H, Raizer J, Hau P, Easaw J, Gil M, Tonn J, Gijtenbeek A, Schlegel U, Bergstrom P, Green S, Weir A, Nikolova Z. Multicentre phase II studies evaluating imatinib plus hydroxyurea in patients with progressive glioblastoma. British Journal of Cancer. 2009;101(12):1995–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Dresemann G. Imatinib and hydroxyurea in pretreated progressive glioblastoma multiforme: a patient series. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2005;16(10):1702–1708. [DOI] [PubMed] [Google Scholar]
- 238.Lassman AB, Pugh SL, Gilbert MR, Aldape KD, Geinoz S, Beumer JH, Christner SM, Komaki R, DeAngelis LM, Gaur R, Youssef E, Wagner H, Won M, Mehta MP. Phase 2 trial of dasatinib in target-selected patients with recurrent glioblastoma (RTOG 0627). Neuro-Oncology. 2015;17(7):992–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Galanis E, Anderson SK, Twohy EL, Carrero XW, Dixon JG, Tran DD, Jeyapalan SA, Anderson DM, Kaufmann TJ, Feathers RW, Giannini C, Buckner JC, Anastasiadis PZ, Schiff D. A phase 1 and randomized, placebo-controlled phase 2 trial of bevacizumab plus dasatinib in patients with recurrent glioblastoma: Alliance/North Central Cancer Treatment Group N0872. Cancer. 2019;125(21):3790–3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Broniscer A, Jia S, Mandrell B, Hamideh D, Huang J, Onar-Thomas A, Gajjar A, Raimondi SC, Tatevossian RG, Stewart CF. Phase 1 trial, pharmacokinetics, and pharmacodynamics of dasatinib combined with crizotinib in children with recurrent or progressive high-grade and diffuse intrinsic pontine glioma. Pediatric Blood & Cancer. 2018;65(7):e27035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Franceschi E, Stupp R, van den Bent MJ, van Herpen C, Laigle Donadey F, Gorlia T, Hegi M, Lhermitte B, Strauss LC, Allgeier A, Lacombe D, Brandes AA. EORTC 26083 phase I/II trial of dasatinib in combination with CCNU in patients with recurrent glioblastoma. Neuro-Oncology. 2012;14(12):1503–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Wilhelm S, Carter C, Lynch M, Lowinger T, Dumas J, Smith RA, Schwartz B, Simantov R, Kelley S. Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Nature Reviews Drug Discovery. 2006;5(10):835–844. [DOI] [PubMed] [Google Scholar]
- 243.Zustovich F, Landi L, Lombardi G, Porta C, Galli L, Fontana A, Amoroso D, Galli C, Andreuccetti M, Falcone A, Zagonel V. Sorafenib plus daily low-dose temozolomide for relapsed glioblastoma: a phase II study. Anticancer Research. 2013;33(8):3487–3494. [PubMed] [Google Scholar]
- 244.Reardon DA, Vredenburgh JJ, Desjardins A, Peters K, Gururangan S, Sampson JH, Marcello J, Herndon JE, McLendon RE, Janney D, Friedman AH, Bigner DD, Friedman HS. Effect of CYP3A-inducing anti-epileptics on sorafenib exposure: results of a phase II study of sorafenib plus daily temozolomide in adults with recurrent glioblastoma. Journal of Neuro-Oncology. 2011;101(1):57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Hainsworth JD, Ervin T, Friedman E, Priego V, Murphy PB, Clark BL, Lamar RE. Concurrent radiotherapy and temozolomide followed by temozolomide and sorafenib in the first-line treatment of patients with glioblastoma multiforme. Cancer. 2010;116(15):3663–3669. [DOI] [PubMed] [Google Scholar]
- 246.Galanis E, Anderson SK, Lafky JM, Uhm JH, Giannini C, Kumar SK, Kimlinger TK, Northfelt DW, Flynn PJ, Jaeckle KA, Kaufmann TJ, Buckner JC. Phase II study of bevacizumab in combination with sorafenib in recurrent glioblastoma (N0776): a north central cancer treatment group trial. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2013;19(17):4816–4823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Schiff D, Jaeckle KA, Anderson SK, Galanis E, Giannini C, Buckner JC, Stella P, Flynn PJ, Erickson BJ, Schwerkoske JF, Kaluza V, Twohy E, Dancey J, Wright J, Sarkaria JN. Phase 1/2 trial of temsirolimus and sorafenib in the treatment of patients with recurrent glioblastoma: North Central Cancer Treatment Group Study/Alliance N0572. Cancer. 2018;124(7):1455–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Nghiemphu PL, Ebiana VA, Wen P, Gilbert M, Abrey LE, Lieberman F, DeAngelis LM, Robins HI, Yung WKA, Chang S, Drappatz J, Mehta MP, Levin VA, Aldape K, Dancey JE, Wright JJ, Prados M, Kuhn J, Cloughesy TF. Phase I study of sorafenib and tipifarnib for recurrent glioblastoma: NABTC 05–02. Journal of Neuro-Oncology. 2018;136(1):79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Jo Y, Kim EH, Sai S, Kim JS, Cho J-M, Kim H, Baek J-H, Kim J-Y, Hwang S-G, Yoon M. Functional Biological Activity of Sorafenib as a Tumor-Treating Field Sensitizer for Glioblastoma Therapy. International Journal of Molecular Sciences. 2018;19(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Pan E, Yu D, Yue B, Potthast L, Chowdhary S, Smith P, Chamberlain M. A prospective phase II single-institution trial of sunitinib for recurrent malignant glioma. Journal of Neuro-Oncology. 2012;110(1):111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Balaña C, Gil MJ, Perez P, Reynes G, Gallego O, Ribalta T, Capellades J, Gonzalez S, Verger E. Sunitinib administered prior to radiotherapy in patients with non-resectable glioblastoma: results of a phase II study. Targeted Oncology. 2014;9(4):321–329. [DOI] [PubMed] [Google Scholar]
- 252.Kreisl TN, Smith P, Sul J, Salgado C, Iwamoto FM, Shih JH, Fine HA. Continuous daily sunitinib for recurrent glioblastoma. Journal of Neuro-Oncology. 2013;111(1):41–48. [DOI] [PubMed] [Google Scholar]
- 253.Wen PY, Drappatz J, de Groot J, Prados MD, Reardon DA, Schiff D, Chamberlain M, Mikkelsen T, Desjardins A, Holland J, Ping J, Weitzman R, Cloughesy TF. Phase II study of cabozantinib in patients with progressive glioblastoma: subset analysis of patients naive to antiangiogenic therapy. Neuro-Oncology. 2018;20(2):249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Cloughesy TF, Drappatz J, de Groot J, Prados MD, Reardon DA, Schiff D, Chamberlain M, Mikkelsen T, Desjardins A, Ping J, Holland J, Weitzman R, Wen PY. Phase II study of cabozantinib in patients with progressive glioblastoma: subset analysis of patients with prior antiangiogenic therapy. Neuro-Oncology. 2018;20(2):259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Chen C, Zhu S, Zhang X, Zhou T, Gu J, Xu Y, Wan Q, Qi X, Chai Y, Liu X, Chen L, Yan J, Hua Y, Lin F. Targeting the synthetic vulnerability of PTEN-deficient glioblastoma cells with MCL1 inhibitors. Molecular Cancer Therapeutics. 2020. [DOI] [PubMed] [Google Scholar]
- 256.Wei AH, Roberts AW, Spencer A, Rosenberg AS, Siegel D, Walter RB, Caenepeel S, Hughes P, McIver Z, Mezzi K, Morrow PK, Stein A. Targeting MCL-1 in hematologic malignancies: Rationale and progress. Blood Reviews. 2020:100672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zhang X, Liu X, Zhou D, Zheng G. Targeting anti-apoptotic BCL-2 family proteins for cancer treatment. Future Medicinal Chemistry. 2020;12(7):563–565. [DOI] [PubMed] [Google Scholar]
- 258.Mehner M, Kubelt C, Adamski V, Schmitt C, Synowitz M, Held-Feindt J. Combined treatment of AT101 and demethoxycurcumin yields an enhanced anti-proliferative effect in human primary glioblastoma cells. Journal of Cancer Research and Clinical Oncology. 2020;146(1):117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Mecca C, Giambanco I, Donato R, Arcuri C. Targeting mTOR in Glioblastoma: Rationale and Preclinical/Clinical Evidence. Disease Markers. 2018;2018:9230479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Galanis E, Buckner JC, Maurer MJ, Kreisberg JI, Ballman K, Boni J, Peralba JM, Jenkins RB, Dakhil SR, Morton RF, Jaeckle KA, Scheithauer BW, Dancey J, Hidalgo M, Walsh DJ, North Central Cancer Treatment G. Phase II trial of temsirolimus (CCI-779) in recurrent glioblastoma multiforme: a North Central Cancer Treatment Group Study. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2005;23(23):5294–5304. [DOI] [PubMed] [Google Scholar]
- 261.Lassen U, Sorensen M, Gaziel TB, Hasselbalch B, Poulsen HS. Phase II study of bevacizumab and temsirolimus combination therapy for recurrent glioblastoma multiforme. Anticancer Research. 2013;33(4):1657–1660. [PubMed] [Google Scholar]
- 262.Wick W, Gorlia T, Bady P, Platten M, van den Bent MJ, Taphoorn MJB, Steuve J, Brandes AA, Hamou M-F, Wick A, Kosch M, Weller M, Stupp R, Roth P, Golfinopoulos V, Frenel J-S, Campone M, Ricard D, Marosi C, Villa S, Weyerbrock A, Hopkins K, Homicsko K, Lhermitte B, Pesce G, Hegi ME. Phase II Study of Radiotherapy and Temsirolimus versus Radiochemotherapy with Temozolomide in Patients with Newly Diagnosed Glioblastoma without MGMT Promoter Hypermethylation (EORTC 26082). Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2016;22(19):4797–4806. [DOI] [PubMed] [Google Scholar]
- 263.Geoerger B, Kieran MW, Grupp S, Perek D, Clancy J, Krygowski M, Ananthakrishnan R, Boni JP, Berkenblit A, Spunt SL. Phase II trial of temsirolimus in children with high-grade glioma, neuroblastoma and rhabdomyosarcoma. European Journal of Cancer (Oxford, England: 1990). 2012;48(2):253–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Chinnaiyan P, Won M, Wen PY, Rojiani AM, Werner-Wasik M, Shih HA, Ashby LS, Michael Yu H-H, Stieber VW, Malone SC, Fiveash JB, Mohile NA, Ahluwalia MS, Wendland MM, Stella PJ, Kee AY, Mehta MP. A randomized phase II study of everolimus in combination with chemoradiation in newly diagnosed glioblastoma: results of NRG Oncology RTOG 0913. Neuro-Oncology. 2018;20(5):666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Ma DJ, Galanis E, Anderson SK, Schiff D, Kaufmann TJ, Peller PJ, Giannini C, Brown PD, Uhm JH, McGraw S, Jaeckle KA, Flynn PJ, Ligon KL, Buckner JC, Sarkaria JN. A phase II trial of everolimus, temozolomide, and radiotherapy in patients with newly diagnosed glioblastoma: NCCTG N057K. Neuro-Oncology. 2015;17(9):12611269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Hainsworth JD, Shih KC, Shepard GC, Tillinghast GW, Brinker BT, Spigel DR. Phase II study of concurrent radiation therapy, temozolomide, and bevacizumab followed by bevacizumab/everolimus as first-line treatment for patients with glioblastoma. Clinical Advances in Hematology & Oncology: H&O. 2012;10(4):240–246. [PubMed] [Google Scholar]
- 267.Munster P, Mita M, Mahipal A, Nemunaitis J, Massard C, Mikkelsen T, Cruz C, Paz-Ares L, Hidalgo M, Rathkopf D, Blumenschein G, Smith DC, Eichhorst B, Cloughesy T, Filvaroff EH, Li S, Raymon H, de Haan H, Hege K, Bendell JC. First-In-Human Phase I Study Of A Dual mTOR Kinase And DNA-PK Inhibitor (CC-115) In Advanced Malignancy. Cancer Management and Research. 2019;11:10463–10476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Prados MD, Lamborn K, Yung WK, Jaeckle K, Robins HI, Mehta M, Fine HA, Wen PY, Cloughesy T, Chang S, Nicholas MK, Schiff D, Greenberg H, Junck L, Fink K, Hess K, Kuhn J, North American Brain Tumor C. A phase 2 trial of irinotecan (CPT-11) in patients with recurrent malignant glioma: a North American Brain Tumor Consortium study. Neuro Oncol. 2006;8(2):189–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Vredenburgh JJ, Desjardins A, Herndon JE, Marcello J, Reardon DA, Quinn JA, Rich JN, Sathornsumetee S, Gururangan S, Sampson J, Wagner M, Bailey L, Bigner DD, Friedman AH, Friedman HS. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2007;25(30):4722–4729. [DOI] [PubMed] [Google Scholar]
- 270.Vredenburgh JJ, Desjardins A, Reardon DA, Friedman HS. Experience with irinotecan for the treatment of malignant glioma. Neuro Oncol. 2009;11(1):80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Mesti T, Moltara ME, Boc M, Rebersek M, Ocvirk J. Bevacizumab and irinotecan in recurrent malignant glioma, a single institution experience. Radiology and Oncology. 2015;49(1):80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Lieberman FS, Wang M, Robins HI, Tsien CI, Curran WJ Jr., Werner-Wasik M, Smith RP, Schultz C, Hartford AC, Zhang P, Mehta MP. Phase 2 Study of Radiation Therapy Plus Low-Dose Temozolomide Followed by Temozolomide and Irinotecan for Glioblastoma: NRG Oncology RTOG Trial 0420. Int J Radiat Oncol Biol Phys. 2019;103(4):878–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Wick W, Dettmer S, Berberich A, Kessler T, Karapanagiotou-Schenkel I, Wick A, Winkler F, Pfaff E, Brors B, Debus J, Unterberg A, Bendszus M, Herold-Mende C, Eisenmenger A, von Deimling A, Jones DTW, Pfister SM, Sahm F, Platten M. N2M2 (NOA-20) phase I/II trial of molecularly matched targeted therapies plus radiotherapy in patients with newly diagnosed non-MGMT hypermethylated glioblastoma. Neuro-Oncology. 2019;21(1):95–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.D’Alessandris QG, Martini M, Cenci T, Di Bonaventura R, Lauretti L, Stumpo V, Olivi A, Larocca LM, Pallini R, Montano N. Tailored therapy for recurrent glioblastoma. Report of a personalized molecular approach. Journal of Neurosurgical Sciences. 2020. [DOI] [PubMed] [Google Scholar]
- 275.Sharpe AH, Pauken KE. The diverse functions of the PD1 inhibitory pathway. Nat Rev Immunol. 2018;18(3):153167. [DOI] [PubMed] [Google Scholar]
- 276.Woroniecka K, Fecci PE. T-cell exhaustion in glioblastoma. Oncotarget. 2018;9(82):35287–35288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Ribas A Tumor immunotherapy directed at PD-1. N Engl J Med. 2012;366(26):2517–2519. [DOI] [PubMed] [Google Scholar]
- 278.Sevenich L Turning “Cold” Into “Hot” Tumors-Opportunities and Challenges for Radio-Immunotherapy Against Primary and Metastatic Brain Cancers. Front Oncol. 2019;9:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Kelly WJ, Giles AJ, Gilbert M. T lymphocyte-targeted immune checkpoint modulation in glioma. J Immunother Cancer. 2020;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Seidel JA, Otsuka A, Kabashima K. Anti-PD-1 and Anti-CTLA-4 Therapies in Cancer: Mechanisms of Action, Efficacy, and Limitations. Front Oncol. 2018;8:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Cloughesy TF, Mochizuki AY, Orpilla JR, Hugo W, Lee AH, Davidson TB, Wang AC, Ellingson BM, Rytlewski JA, Sanders CM, Kawaguchi ES, Du L, Li G, Yong WH, Gaffey SC, Cohen AL, Mellinghoff IK, Lee EQ, Reardon DA, O’Brien BJ, Butowski NA, Nghiemphu PL, Clarke JL, Arrillaga-Romany IC, Colman H, Kaley TJ, de Groot JF, Liau LM, Wen PY, Prins RM. Neoadjuvant anti-PD-1 immunotherapy promotes a survival benefit with intratumoral and systemic immune responses in recurrent glioblastoma. Nat Med. 2019;25(3):477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Reardon DA, Brandes AA, Omuro A, Mulholland P, Lim M, Wick A, Baehring J, Ahluwalia MS, Roth P, Bahr O, Phuphanich S, Sepulveda JM, De Souza P, Sahebjam S, Carleton M, Tatsuoka K, Taitt C, Zwirtes R, Sampson J, Weller M. Effect of Nivolumab vs Bevacizumab in Patients With Recurrent Glioblastoma: The CheckMate 143 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020;6(7):1003–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Bristol-Myers Squibb Provides Update on Phase 3 Opdivo (nivolumab) CheckMate −548 Trial in Patients with Newly Diagnosed MGMT-Methylated Glioblastoma Multiforme. Available from: https://news.bms.com/news/corporate-financial/2019/Bristol-Myers-Squibb-Provides-Update-on-Phase-3-Opdivonivolumab-CheckMate--548-Trial-in-Patients-with-Newly-Diagnosed-MGMT-Methylated-GlioblastomaMultiforme/default.aspx.
- 284.Company B-MS. Bristol-Myers Squibb Announces Phase 3 CheckMate −498 Study Did Not Meet Primary Endpoint of Overall Survival with Opdivo (nivolumab) Plus Radiation in Patients with Newly Diagnosed MGMTUnmethylated Glioblastoma Multiforme. Available from: https://news.bms.com/news/corporatefinancial/2019/Bristol-Myers-Squibb-Announces-Phase-3-CheckMate--498-Study-Did-Not-Meet-PrimaryEndpoint-of-Overall-Survival-with-Opdivo-nivolumab-Plus-Radiation-in-Patients-with-Newly-Diagnosed-MGMTUnmethylated-Glioblastoma-Multiforme/default.aspx.
- 285.Hugo W, Zaretsky JM, Sun L, Song C, Moreno BH, Hu-Lieskovan S, Berent-Maoz B, Pang J, Chmielowski B, Cherry G, Seja E, Lomeli S, Kong X, Kelley MC, Sosman JA, Johnson DB, Ribas A, Lo RS. Genomic and Transcriptomic Features of Response to Anti-PD-1 Therapy in Metastatic Melanoma. Cell. 2017;168(3):542. [DOI] [PubMed] [Google Scholar]
- 286.Arlauckas SP, Garris CS, Kohler RH, Kitaoka M, Cuccarese MF, Yang KS, Miller MA, Carlson JC, Freeman GJ, Anthony RM, Weissleder R, Pittet MJ. In vivo imaging reveals a tumor-associated macrophage-mediated resistance pathway in anti-PD-1 therapy. Sci Transl Med. 2017;9(389). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Maj T, Wang W, Crespo J, Zhang H, Wang W, Wei S, Zhao L, Vatan L, Shao I, Szeliga W, Lyssiotis C, Liu JR, Kryczek I, Zou W. Oxidative stress controls regulatory T cell apoptosis and suppressor activity and PD-L1blockade resistance in tumor. Nat Immunol. 2017;18(12):1332–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Sen DR, Kaminski J, Barnitz RA, Kurachi M, Gerdemann U, Yates KB, Tsao HW, Godec J, LaFleur MW, Brown FD, Tonnerre P, Chung RT, Tully DC, Allen TM, Frahm N, Lauer GM, Wherry EJ, Yosef N, Haining WN. The epigenetic landscape of T cell exhaustion. Science. 2016;354(6316):1165–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Pauken KE, Sammons MA, Odorizzi PM, Manne S, Godec J, Khan O, Drake AM, Chen Z, Sen DR, Kurachi M, Barnitz RA, Bartman C, Bengsch B, Huang AC, Schenkel JM, Vahedi G, Haining WN, Berger SL, Wherry EJ. Epigenetic stability of exhausted T cells limits durability of reinvigoration by PD-1 blockade. Science. 2016;354(6316):1160–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Thommen DS, Schreiner J, Muller P, Herzig P, Roller A, Belousov A, Umana P, Pisa P, Klein C, Bacac M, Fischer OS, Moersig W, Savic Prince S, Levitsky V, Karanikas V, Lardinois D, Zippelius A. Progression of Lung Cancer Is Associated with Increased Dysfunction of T Cells Defined by Coexpression of Multiple Inhibitory Receptors. Cancer Immunol Res. 2015;3(12):1344–1355. [DOI] [PubMed] [Google Scholar]
- 291.Long L, Zhang X, Chen F, Pan Q, Phiphatwatchara P, Zeng Y, Chen H. The promising immune checkpoint LAG-3: from tumor microenvironment to cancer immunotherapy. Genes Cancer. 2018;9(5–6):176–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Kim JE, Patel MA, Mangraviti A, Kim ES, Theodros D, Velarde E, Liu A, Sankey EW, Tam A, Xu H, Mathios D, Jackson CM, Harris-Bookman S, Garzon-Muvdi T, Sheu M, Martin AM, Tyler BM, Tran PT, Ye X, Olivi A, Taube JM, Burger PC, Drake CG, Brem H, Pardoll DM, Lim M. Combination Therapy with Anti-PD-1, Anti-TIM-3, and Focal Radiation Results in Regression of Murine Gliomas. Clin Cancer Res. 2017;23(1):124–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Singh AB, Harris RC. Autocrine, paracrine and juxtacrine signaling by EGFR ligands. Cell Signal. 2005;17(10):1183–1193. [DOI] [PubMed] [Google Scholar]
- 294.Choi BD, Archer GE, Mitchell DA, Heimberger AB, McLendon RE, Bigner DD, Sampson JH. EGFRvIII-targeted vaccination therapy of malignant glioma. Brain Pathol. 2009;19(4):713–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Weller M, Butowski N, Tran DD, Recht LD, Lim M, Hirte H, Ashby L, Mechtler L, Goldlust SA, Iwamoto F, Drappatz J, O’Rourke DM, Wong M, Hamilton MG, Finocchiaro G, Perry J, Wick W, Green J, He Y, Turner CD, Yellin MJ, Keler T, Davis TA, Stupp R, Sampson JH, investigators AIt. Rindopepimut with temozolomide for patients with newly diagnosed, EGFRvIII-expressing glioblastoma (ACT IV): a randomised, double-blind, international phase 3 trial. Lancet Oncol. 2017;18(10):1373–1385. [DOI] [PubMed] [Google Scholar]
- 296.Wu AH, Xiao J, Anker L, Hall WA, Gregerson DS, Cavenee WK, Chen W, Low WC. Identification of EGFRvIII-derived CTL epitopes restricted by HLA A0201 for dendritic cell based immunotherapy of gliomas. J Neurooncol. 2006;76(1):23–30. [DOI] [PubMed] [Google Scholar]
- 297.Sampson JH, Heimberger AB, Archer GE, Aldape KD, Friedman AH, Friedman HS, Gilbert MR, Herndon JE 2nd, McLendon RE, Mitchell DA, Reardon DA, Sawaya R, Schmittling RJ, Shi W, Vredenburgh JJ, Bigner DD. Immunologic escape after prolonged progression-free survival with epidermal growth factor receptor variant III peptide vaccination in patients with newly diagnosed glioblastoma. J Clin Oncol. 2010;28(31):4722–4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Reardon DA, Desjardins A, Vredenburgh JJ, O’Rourke DM, Tran DD, Fink KL, Nabors LB, Li G, Bota DA, Lukas RV, Ashby LS, Duic JP, Mrugala MM, Cruickshank S, Vitale L, He Y, Green JA, Yellin MJ, Turner CD, Keler T, Davis TA, Sampson JH, Re ACTti. Rindopepimut with Bevacizumab for Patients with Relapsed EGFRvIIIExpressing Glioblastoma (ReACT): Results of a Double-Blind Randomized Phase II Trial. Clin Cancer Res. 2020;26(7):1586–1594. [DOI] [PubMed] [Google Scholar]
- 299.Santos PM, Butterfield LH. Dendritic Cell-Based Cancer Vaccines. J Immunol. 2018;200(2):443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Bigner DD, Pitts OM, Wikstrand CJ. Induction of lethal experimental allergic encephalomyelitis in nonhuman primates and guinea pigs with human glioblastoma multiforme tissue. J Neurosurg. 1981;55(1):32–42. [DOI] [PubMed] [Google Scholar]
- 301.Liau LM, Ashkan K, Tran DD, Campian JL, Trusheim JE, Cobbs CS, Heth JA, Salacz M, Taylor S, D’Andre SD, Iwamoto FM, Dropcho EJ, Moshel YA, Walter KA, Pillainayagam CP, Aiken R, Chaudhary R, Goldlust SA, Bota DA, Duic P, Grewal J, Elinzano H, Toms SA, Lillehei KO, Mikkelsen T, Walbert T, Abram SR, Brenner AJ, Brem S, Ewend MG, Khagi S, Portnow J, Kim LJ, Loudon WG, Thompson RC, Avigan DE, Fink KL, Geoffroy FJ, Lindhorst S, Lutzky J, Sloan AE, Schackert G, Krex D, Meisel HJ, Wu J, Davis RP, Duma C, Etame AB, Mathieu D, Kesari S, Piccioni D, Westphal M, Baskin DS, New PZ, Lacroix M, May SA, Pluard TJ, Tse V, Green RM, Villano JL, Pearlman M, Petrecca K, Schulder M, Taylor LP, Maida AE, Prins RM, Cloughesy TF, Mulholland P, Bosch ML. First results on survival from a large Phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma. J Transl Med. 2018;16(1):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.De Vries IJ, Krooshoop DJ, Scharenborg NM, Lesterhuis WJ, Diepstra JH, Van Muijen GN, Strijk SP, Ruers TJ, Boerman OC, Oyen WJ, Adema GJ, Punt CJ, Figdor CG. Effective migration of antigen-pulsed dendritic cells to lymph nodes in melanoma patients is determined by their maturation state. Cancer Res. 2003;63(1):12–17. [PubMed] [Google Scholar]
- 303.Liu H, Chen L, Liu J, Meng H, Zhang R, Ma L, Wu L, Yu S, Shi F, Li Y, Zhang L, Wang L, Feng S, Zhang Q, Peng Y, Wu Q, Liu C, Chang X, Yang L, Uemura Y, Yu X, Liu T. Co-delivery of tumor-derived exosomes with alphagalactosylceramide on dendritic cell-based immunotherapy for glioblastoma. Cancer Lett. 2017;411:182–190. [DOI] [PubMed] [Google Scholar]
- 304.Dhodapkar KM, Cirignano B, Chamian F, Zagzag D, Miller DC, Finlay JL, Steinman RM. Invariant natural killer T cells are preserved in patients with glioma and exhibit antitumor lytic activity following dendritic cell-mediated expansion. Int J Cancer. 2004;109(6):893–899. [DOI] [PubMed] [Google Scholar]
- 305.Garzon-Muvdi T, Theodros D, Luksik AS, Maxwell R, Kim E, Jackson CM, Belcaid Z, Ganguly S, Tyler B, Brem H, Pardoll DM, Lim M. Dendritic cell activation enhances anti-PD-1 mediated immunotherapy against glioblastoma. Oncotarget. 2018;9(29):20681–20697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Antonios JP, Soto H, Everson RG, Orpilla J, Moughon D, Shin N, Sedighim S, Yong WH, Li G, Cloughesy TF, Liau LM, Prins RM. PD-1 blockade enhances the vaccination-induced immune response in glioma. JCI Insight. 2016;1(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Bridle BW, Stephenson KB, Boudreau JE, Koshy S, Kazdhan N, Pullenayegum E, Brunelliere J, Bramson JL, Lichty BD, Wan Y. Potentiating cancer immunotherapy using an oncolytic virus. Mol Ther. 2010;18(8):1430–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Zhang Q, Liu F. Advances and potential pitfalls of oncolytic viruses expressing immunomodulatory transgene therapy for malignant gliomas. Cell Death Dis. 2020;11(6):485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Kurokawa C, Iankov ID, Anderson SK, Aderca I, Leontovich AA, Maurer MJ, Oberg AL, Schroeder MA, Giannini C, Greiner SM, Becker MA, Thompson EA, Haluska P, Jentoft ME, Parney IF, Weroha SJ, Jen J, Sarkaria JN, Galanis E. Constitutive Interferon Pathway Activation in Tumors as an Efficacy Determinant Following Oncolytic Virotherapy. J Natl Cancer Inst. 2018;110(10):1123–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Menotti L, Avitabile E. Herpes Simplex Virus Oncolytic Immunovirotherapy: The Blossoming Branch of Multimodal Therapy. Int J Mol Sci. 2020;21(21). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Rius-Rocabert S, Garcia-Romero N, Garcia A, Ayuso-Sacido A, Nistal-Villan E. Oncolytic Virotherapy in Glioma Tumors. Int J Mol Sci. 2020;21(20). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Andtbacka RH, Kaufman HL, Collichio F, Amatruda T, Senzer N, Chesney J, Delman KA, Spitler LE, Puzanov I, Agarwala SS, Milhem M, Cranmer L, Curti B, Lewis K, Ross M, Guthrie T, Linette GP, Daniels GA, Harrington K, Middleton MR, Miller WH Jr., Zager JS, Ye Y, Yao B, Li A, Doleman S, VanderWalde A, Gansert J, Coffin RS. Talimogene Laherparepvec Improves Durable Response Rate in Patients With Advanced Melanoma. J Clin Oncol. 2015;33(25):2780–2788. [DOI] [PubMed] [Google Scholar]
- 313.Lang FF, Conrad C, Gomez-Manzano C, Yung WKA, Sawaya R, Weinberg JS, Prabhu SS, Rao G, Fuller GN, Aldape KD, Gumin J, Vence LM, Wistuba I, Rodriguez-Canales J, Villalobos PA, Dirven CMF, Tejada S, Valle RD, Alonso MM, Ewald B, Peterkin JJ, Tufaro F, Fueyo J. Phase I Study of DNX-2401 (Delta-24-RGD) Oncolytic Adenovirus: Replication and Immunotherapeutic Effects in Recurrent Malignant Glioma. J Clin Oncol. 2018;36(14):1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Spencer DA, Young JS, Kanojia D, Kim JW, Polster SP, Murphy JP, Lesniak MS. Unlocking the promise of oncolytic virotherapy in glioma: combination with chemotherapy to enhance efficacy. Ther Deliv. 2015;6(4):453–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Cerullo V, Diaconu I, Kangasniemi L, Rajecki M, Escutenaire S, Koski A, Romano V, Rouvinen N, Tuuminen T, Laasonen L, Partanen K, Kauppinen S, Joensuu T, Oksanen M, Holm SL, Haavisto E, Karioja-Kallio A, Kanerva A, Pesonen S, Arstila PT, Hemminki A. Immunological effects of low-dose cyclophosphamide in cancer patients treated with oncolytic adenovirus. Mol Ther. 2011;19(9):1737–1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, Xu Y, Frohlich MW, Schellhammer PF, Investigators IS. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–422. [DOI] [PubMed] [Google Scholar]
- 317.Perez OD, Logg CR, Hiraoka K, Diago O, Burnett R, Inagaki A, Jolson D, Amundson K, Buckley T, Lohse D, Lin A, Burrascano C, Ibanez C, Kasahara N, Gruber HE, Jolly DJ. Design and selection of Toca 511 for clinical use: modified retroviral replicating vector with improved stability and gene expression. Mol Ther. 2012;20(9):1689–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Wheeler LA, Manzanera AG, Bell SD, Cavaliere R, McGregor JM, Grecula JC, Newton HB, Lo SS, Badie B, Portnow J, Teh BS, Trask TW, Baskin DS, New PZ, Aguilar LK, Aguilar-Cordova E, Chiocca EA. Phase II multicenter study of gene-mediated cytotoxic immunotherapy as adjuvant to surgical resection for newly diagnosed malignant glioma. Neuro Oncol. 2016;18(8):1137–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Stepanenko AA, Chekhonin VP. Recent Advances in Oncolytic Virotherapy and Immunotherapy for Glioblastoma: A Glimmer of Hope in the Search for an Effective Therapy? Cancers (Basel). 2018;10(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Westphal M, Yla-Herttuala S, Martin J, Warnke P, Menei P, Eckland D, Kinley J, Kay R, Ram Z, Group AS. Adenovirus-mediated gene therapy with sitimagene ceradenovec followed by intravenous ganciclovir for patients with operable high-grade glioma (ASPECT): a randomised, open-label, phase 3 trial. Lancet Oncol. 2013;14(9):823–833. [DOI] [PubMed] [Google Scholar]
- 321.Jena B, Dotti G, Cooper LJ. Redirecting T-cell specificity by introducing a tumor-specific chimeric antigen receptor. Blood. 2010;116(7):1035–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.O’Rourke DM, Nasrallah MP, Desai A, Melenhorst JJ, Mansfield K, Morrissette JJD, Martinez-Lage M, Brem S, Maloney E, Shen A, Isaacs R, Mohan S, Plesa G, Lacey SF, Navenot JM, Zheng Z, Levine BL, Okada H, June CH, Brogdon JL, Maus MV. A single dose of peripherally infused EGFRvIII-directed CAR T cells mediates antigen loss and induces adaptive resistance in patients with recurrent glioblastoma. Sci Transl Med. 2017;9(399). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Ahmed N, Brawley V, Hegde M, Bielamowicz K, Kalra M, Landi D, Robertson C, Gray TL, Diouf O, Wakefield A, Ghazi A, Gerken C, Yi Z, Ashoori A, Wu MF, Liu H, Rooney C, Dotti G, Gee A, Su J, Kew Y, Baskin D, Zhang YJ, New P, Grilley B, Stojakovic M, Hicks J, Powell SZ, Brenner MK, Heslop HE, Grossman R, Wels WS, Gottschalk S. HER2-Specific Chimeric Antigen Receptor-Modified Virus-Specific T Cells for Progressive Glioblastoma: A Phase 1 Dose-Escalation Trial. JAMA Oncol. 2017;3(8):1094–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Bielamowicz K, Fousek K, Byrd TT, Samaha H, Mukherjee M, Aware N, Wu MF, Orange JS, Sumazin P, Man TK, Joseph SK, Hegde M, Ahmed N. Trivalent CAR T cells overcome interpatient antigenic variability in glioblastoma. Neuro Oncol. 2018;20(4):506–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Tang X, Zhao S, Zhang Y, Wang Y, Zhang Z, Yang M, Zhu Y, Zhang G, Guo G, Tong A, Zhou L. B7-H3 as a Novel CAR-T Therapeutic Target for Glioblastoma. Mol Ther Oncolytics. 2019;14:279–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Fecci PE, Sampson JH. The current state of immunotherapy for gliomas: an eye toward the future. J Neurosurg. 2019;131(3):657–666. [DOI] [PubMed] [Google Scholar]
- 327.Sotillo E, Barrett DM, Black KL, Bagashev A, Oldridge D, Wu G, Sussman R, Lanauze C, Ruella M, Gazzara MR, Martinez NM, Harrington CT, Chung EY, Perazzelli J, Hofmann TJ, Maude SL, Raman P, Barrera A, Gill S, Lacey SF, Melenhorst JJ, Allman D, Jacoby E, Fry T, Mackall C, Barash Y, Lynch KW, Maris JM, Grupp SA, ThomasTikhonenko A. Convergence of Acquired Mutations and Alternative Splicing of CD19 Enables Resistance to CART-19 Immunotherapy. Cancer Discov. 2015;5(12):1282–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Choi BD, Yu X, Castano AP, Bouffard AA, Schmidts A, Larson RC, Bailey SR, Boroughs AC, Frigault MJ, Leick MB, Scarfo I, Cetrulo CL, Demehri S, Nahed BV, Cahill DP, Wakimoto H, Curry WT, Carter BS, Maus MV. CAR-T cells secreting BiTEs circumvent antigen escape without detectable toxicity. Nat Biotechnol. 2019;37(9):10491058. [DOI] [PubMed] [Google Scholar]
- 329.Jackson CM, Choi J, Lim M. Mechanisms of immunotherapy resistance: lessons from glioblastoma. Nat Immunol. 2019;20(9):1100–1109. [DOI] [PubMed] [Google Scholar]
- 330.Anagnostou V, Smith KN, Forde PM, Niknafs N, Bhattacharya R, White J, Zhang T, Adleff V, Phallen J, Wali N, Hruban C, Guthrie VB, Rodgers K, Naidoo J, Kang H, Sharfman W, Georgiades C, Verde F, Illei P, Li QK, Gabrielson E, Brock MV, Zahnow CA, Baylin SB, Scharpf RB, Brahmer JR, Karchin R, Pardoll DM, Velculescu VE. Evolution of Neoantigen Landscape during Immune Checkpoint Blockade in Non-Small Cell Lung Cancer. Cancer Discov. 2017;7(3):264–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Kailayangiri S, Altvater B, Wiebel M, Jamitzky S, Rossig C. Overcoming Heterogeneity of Antigen Expression for Effective CAR T Cell Targeting of Cancers. Cancers (Basel). 2020;12(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Lhuillier C, Rudqvist NP, Elemento O, Formenti SC, Demaria S. Radiation therapy and anti-tumor immunity: exposing immunogenic mutations to the immune system. Genome Med. 2019;11(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Jin L, Tao H, Karachi A, Long Y, Hou AY, Na M, Dyson KA, Grippin AJ, Deleyrolle LP, Zhang W, Rajon DA, Wang QJ, Yang JC, Kresak JL, Sayour EJ, Rahman M, Bova FJ, Lin Z, Mitchell DA, Huang J. CXCR1- or CXCR2-modified CAR T cells co-opt IL-8 for maximal antitumor efficacy in solid tumors. Nat Commun. 2019;10(1):4016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Murty S, Haile ST, Beinat C, Aalipour A, Alam IS, Murty T, Shaffer TM, Patel CB, Graves EE, Mackall CL, Gambhir SS. Intravital imaging reveals synergistic effect of CAR T-cells and radiation therapy in a preclinical immunocompetent glioblastoma model. Oncoimmunology. 2020;9(1):1757360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Oswald JT, Patel H, Khan D, Jeorje NN, Golzar H, Oswald EL, Tang S. Drug Delivery Systems Using Surface Markers for Targeting Cancer Stem Cells. Curr Pharm Des. 2020;26(17):2057–2071. [DOI] [PubMed] [Google Scholar]
- 336.Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MDP, Acosta-Torres LS, Diaz-Torres LA, Grillo R, Swamy MK, Sharma S, Habtemariam S, Shin HS. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnology. 2018;16(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Alphandery E Nano-Therapies for Glioblastoma Treatment. Cancers (Basel). 2020;12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Shi Y, van der Meel R, Chen X, Lammers T. The EPR effect and beyond: Strategies to improve tumor targeting and cancer nanomedicine treatment efficacy. Theranostics. 2020;10(17):7921–7924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Golombek SK, May JN, Theek B, Appold L, Drude N, Kiessling F, Lammers T. Tumor targeting via EPR: Strategies to enhance patient responses. Adv Drug Deliv Rev. 2018;130:17–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Rosenblum D, Joshi N, Tao W, Karp JM, Peer D. Progress and challenges towards targeted delivery of cancer therapeutics. Nat Commun. 2018;9(1):1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Xu Y, Wu H, Huang J, Qian W, Martinson DE, Ji B, Li Y, Wang YA, Yang L, Mao H. Probing and Enhancing Ligand-Mediated Active Targeting of Tumors Using Sub-5 nm Ultrafine Iron Oxide Nanoparticles. Theranostics. 2020;10(6):2479–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Bort G, Lux F, Dufort S, Cremillieux Y, Verry C, Tillement O. EPR-mediated tumor targeting using ultrasmallhybrid nanoparticles: From animal to human with theranostic AGuIX nanoparticles. Theranostics. 2020;10(3):1319–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Jang E, Kim E, Son HY, Lim EK, Lee H, Choi Y, Park K, Han S, Suh JS, Huh YM, Haam S. Nanovesicle-mediated systemic delivery of microRNA-34a for CD44 overexpressing gastric cancer stem cell therapy. Biomaterials. 2016;105:12–24. [DOI] [PubMed] [Google Scholar]
- 344.Liu C, Zhao G, Liu J, Ma N, Chivukula P, Perelman L, Okada K, Chen Z, Gough D, Yu L. Novel biodegradable lipid nano complex for siRNA delivery significantly improving the chemosensitivity of human colon cancer stem cells to paclitaxel. J Control Release. 2009;140(3):277–283. [DOI] [PubMed] [Google Scholar]
- 345.Lopez-Bertoni H, Kozielski KL, Rui Y, Lal B, Vaughan H, Wilson DR, Mihelson N, Eberhart CG, Laterra J, Green JJ. Bioreducible Polymeric Nanoparticles Containing Multiplexed Cancer Stem Cell Regulating miRNAs Inhibit Glioblastoma Growth and Prolong Survival. Nano Lett. 2018;18(7):4086–4094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Ling H, Fabbri M, Calin GA. MicroRNAs and other non-coding RNAs as targets for anticancer drug development. Nat Rev Drug Discov. 2013;12(11):847–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Nawaz M Extracellular vesicle-mediated transport of non-coding RNAs between stem cells and cancer cells: implications in tumor progression and therapeutic resistance. Stem Cell Investig. 2017;4:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Glaser T, Han I, Wu L, Zeng X. Targeted Nanotechnology in Glioblastoma Multiforme. Front Pharmacol. 2017;8:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Basati G, Khaksarian M, Abbaszadeh S, Lashgarian HE, Marzban A. Cancer stem cells and nanotechnological approaches for eradication. Stem Cell Investig. 2019;6:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Chekhonin VP, Baklaushev VP, Yusubalieva GM, Belorusova AE, Gulyaev MV, Tsitrin EB, Grinenko NF, Gurina OI, Pirogov YA. Targeted delivery of liposomal nanocontainers to the peritumoral zone of glioma by means of monoclonal antibodies against GFAP and the extracellular loop of Cx43. Nanomedicine. 2012;8(1):63–70. [DOI] [PubMed] [Google Scholar]
- 351.Wang B, Lv L, Wang Z, Jiang Y, Lv W, Liu X, Wang Z, Zhao Y, Xin H, Xu Q. Improved anti-glioblastoma efficacy by IL-13Ralpha2 mediated copolymer nanoparticles loaded with paclitaxel. Sci Rep. 2015;5:16589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Grafals-Ruiz N, Rios-Vicil CI, Lozada-Delgado EL, Quinones-Diaz BI, Noriega-Rivera RA, Martinez-Zayas G, Santana-Rivera Y, Santiago-Sanchez GS, Valiyeva F, Vivas-Mejia PE. Brain Targeted Gold Liposomes Improve RNAi Delivery for Glioblastoma. Int J Nanomedicine. 2020;15:2809–2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Belhadj Z, Zhan C, Ying M, Wei X, Xie C, Yan Z, Lu W. Multifunctional targeted liposomal drug delivery for efficient glioblastoma treatment. Oncotarget. 2017;8(40):66889–66900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Chen H, Zhang W, Zhu G, Xie J, Chen X. Rethinking cancer nanotheranostics. Nat Rev Mater. 2017;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Mi P Stimuli-responsive nanocarriers for drug delivery, tumor imaging, therapy and theranostics. Theranostics. 2020;10(10):4557–4588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Liu Y, Jiang Y, Zhang M, Tang Z, He M, Bu W. Modulating Hypoxia via Nanomaterials Chemistry for Efficient Treatment of Solid Tumors. Acc Chem Res. 2018;51(10):2502–2511. [DOI] [PubMed] [Google Scholar]
- 357.Liu HM, Zhang YF, Xie YD, Cai YF, Li BY, Li W, Zeng LY, Li YL, Yu RT. Hypoxia-responsive ionizable liposome delivery siRNA for glioma therapy. Int J Nanomedicine. 2017;12:1065–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Hua L, Wang Z, Zhao L, Mao H, Wang G, Zhang K, Liu X, Wu D, Zheng Y, Lu J, Yu R, Liu H. Hypoxia-responsive lipid-poly-(hypoxic radiosensitized polyprodrug) nanoparticles for glioma chemo- and radiotherapy. Theranostics. 2018;8(18):5088–5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Mohanty S, Chen Z, Li K, Morais GR, Klockow J, Yerneni K, Pisani L, Chin FT, Mitra S, Cheshier S, Chang E, Gambhir SS, Rao J, Loadman PM, Falconer RA, Daldrup-Link HE. A Novel Theranostic Strategy for MMP-14Expressing Glioblastomas Impacts Survival. Mol Cancer Ther. 2017;16(9):1909–1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Wu W, Klockow JL, Mohanty S, Ku KS, Aghighi M, Melemenidis S, Chen Z, Li K, Morais GR, Zhao N, Schlegel J, Graves EE, Rao J, Loadman PM, Falconer RA, Mukherjee S, Chin FT, Daldrup-Link HE. Theranostic nanoparticles enhance the response of glioblastomas to radiation. Nanotheranostics. 2019;3(4):299–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Sarkaria JN, Hu LS, Parney IF, Pafundi DH, Brinkmann DH, Laack NN, Giannini C, Burns TC, Kizilbash SH, Laramy JK, Swanson KR, Kaufmann TJ, Brown PD, Agar NYR, Galanis E, Buckner JC, Elmquist WF. Is the blood-brain barrier really disrupted in all glioblastomas? A critical assessment of existing clinical data. Neuro Oncol. 2018;20(2):184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Deng Z, Sheng Z, Yan F. Ultrasound-Induced Blood-Brain-Barrier Opening Enhances Anticancer Efficacy in the Treatment of Glioblastoma: Current Status and Future Prospects. J Oncol. 2019;2019:2345203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Fisher DG, Price RJ. Recent Advances in the Use of Focused Ultrasound for Magnetic Resonance Image-Guided Therapeutic Nanoparticle Delivery to the Central Nervous System. Front Pharmacol. 2019;10:1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Curley CT, Mead BP, Negron K, Kim N, Garrison WJ, Miller GW, Kingsmore KM, Thim EA, Song J, Munson JM, Klibanov AL, Suk JS, Hanes J, Price RJ. Augmentation of brain tumor interstitial flow via focused ultrasound promotes brain-penetrating nanoparticle dispersion and transfection. Sci Adv. 2020;6(18):eaay1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Fan CH, Wang TW, Hsieh YK, Wang CF, Gao Z, Kim A, Nagasaki Y, Yeh CK. Enhancing Boron Uptake in Brain Glioma by a Boron-Polymer/Microbubble Complex with Focused Ultrasound. ACS Appl Mater Interfaces. 2019;11(12):11144–11156. [DOI] [PubMed] [Google Scholar]
- 366.Li Y, Wu M, Zhang N, Tang C, Jiang P, Liu X, Yan F, Zheng H. Mechanisms of enhanced antiglioma efficacy of polysorbate 80-modified paclitaxel-loaded PLGA nanoparticles by focused ultrasound. J Cell Mol Med. 2018;22(9):4171–4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Gupta R, Sharma D. Evolution of Magnetic Hyperthermia for Glioblastoma Multiforme Therapy. ACS Chem Neurosci. 2019;10(3):1157–1172. [DOI] [PubMed] [Google Scholar]
- 368.Mahmoudi K, Bouras A, Bozec D, Ivkov R, Hadjipanayis C. Magnetic hyperthermia therapy for the treatment of glioblastoma: a review of the therapy’s history, efficacy and application in humans. Int J Hyperthermia. 2018;34(8):1316–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Gupta R, Sharma D. Manganese-Doped Magnetic Nanoclusters for Hyperthermia and Photothermal Glioblastoma Therapy. ACS Applied Nano Materials. 2020;3(2):2026–2037. [Google Scholar]
- 370.Mamani JB, Marinho BS, Rego GNA, Nucci MP, Alvieri F, Santos RSD, Ferreira JVM, Oliveira FA, Gamarra LF. Magnetic hyperthermia therapy in glioblastoma tumor on-a-Chip model. Einstein (Sao Paulo). 2020;18:eAO4954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Sousa F, Dhaliwal HK, Gattacceca F, Sarmento B, Amiji MM. Enhanced anti-angiogenic effects of bevacizumab in glioblastoma treatment upon intranasal administration in polymeric nanoparticles. J Control Release. 2019;309:37–47. [DOI] [PubMed] [Google Scholar]
- 372.Khan A, Aqil M, Imam SS, Ahad A, Sultana Y, Ali A, Khan K. Temozolomide loaded nano lipid based chitosan hydrogel for nose to brain delivery: Characterization, nasal absorption, histopathology and cell line study. Int J Biol Macromol. 2018;116:1260–1267. [DOI] [PubMed] [Google Scholar]
- 373.Van Woensel M, Mathivet T, Wauthoz N, Rosiere R, Garg AD, Agostinis P, Mathieu V, Kiss R, Lefranc F, Boon L, Belmans J, Van Gool SW, Gerhardt H, Amighi K, De Vleeschouwer S. Sensitization of glioblastoma tumor microenvironment to chemo- and immunotherapy by Galectin-1 intranasal knock-down strategy. Sci Rep. 2017;7(1):1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Arshad A, Yang B, Bienemann AS, Barua NU, Wyatt MJ, Woolley M, Johnson DE, Edler KJ, Gill SS. Convection-Enhanced Delivery of Carboplatin PLGA Nanoparticles for the Treatment of Glioblastoma. PLoS One. 2015;10(7):e0132266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Bobo RH, Laske DW, Akbasak A, Morrison PF, Dedrick RL, Oldfield EH. Convection-enhanced delivery of macromolecules in the brain. Proc Natl Acad Sci U S A. 1994;91(6):2076–2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Kunwar S, Chang S, Westphal M, Vogelbaum M, Sampson J, Barnett G, Shaffrey M, Ram Z, Piepmeier J, Prados M, Croteau D, Pedain C, Leland P, Husain SR, Joshi BH, Puri RK, Group PS. Phase III randomized trial of CED of IL13-PE38QQR vs Gliadel wafers for recurrent glioblastoma. Neuro Oncol. 2010;12(8):871–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Weaver M, Laske DW. Transferrin receptor ligand-targeted toxin conjugate (Tf-CRM107) for therapy of malignant gliomas. J Neurooncol. 2003;65(1):3–13. [DOI] [PubMed] [Google Scholar]
- 378.Kunwar S, Chang SM, Prados MD, Berger MS, Sampson JH, Croteau D, Sherman JW, Grahn AY, Shu VS, Dul JL, Husain SR, Joshi BH, Pedain C, Puri RK. Safety of intraparenchymal convection-enhanced delivery of cintredekin besudotox in early-phase studies. Neurosurg Focus. 2006;20(4):E15. [PubMed] [Google Scholar]
- 379.Lidar Z, Mardor Y, Jonas T, Pfeffer R, Faibel M, Nass D, Hadani M, Ram Z. Convection-enhanced delivery of paclitaxel for the treatment of recurrent malignant glioma: a phase I/II clinical study. J Neurosurg. 2004;100(3):472–479. [DOI] [PubMed] [Google Scholar]
- 380.Allard E, Passirani C, Benoit JP. Convection-enhanced delivery of nanocarriers for the treatment of brain tumors. Biomaterials. 2009;30(12):2302–2318. [DOI] [PubMed] [Google Scholar]
- 381.Center UB. Convection enhanced delivery. Available from: https://braintumorcenter.ucsf.edu/treatment/experimental-diagnostics-therapies/convection-enhanced-delivery
- 382.Souweidane MM, Kramer K, Pandit-Taskar N, Zhou Z, Haque S, Zanzonico P, Carrasquillo JA, Lyashchenko SK, Thakur SB, Donzelli M, Turner RS, Lewis JS, Cheung NV, Larson SM, Dunkel IJ. Convection-enhanced delivery for diffuse intrinsic pontine glioma: a single-centre, dose-escalation, phase 1 trial. Lancet Oncol. 2018;19(8):1040–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Sampson JH, Archer G, Pedain C, Wembacher-Schroder E, Westphal M, Kunwar S, Vogelbaum MA, Coan A, Herndon JE, Raghavan R, Brady ML, Reardon DA, Friedman AH, Friedman HS, Rodriguez-Ponce MI, Chang SM, Mittermeyer S, Croteau D, Puri RK, Investigators PT. Poor drug distribution as a possible explanation for the results of the PRECISE trial. J Neurosurg. 2010;113(2):301–309. [DOI] [PubMed] [Google Scholar]
- 384.Finbloom JA, Aanei IL, Bernard JM, Klass SH, Elledge SK, Han K, Ozawa T, Nicolaides TP, Berger MS, Francis MB. Evaluation of Three Morphologically Distinct Virus-Like Particles as Nanocarriers for Convection-Enhanced Drug Delivery to Glioblastoma. Nanomaterials (Basel). 2018;8(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Patil R, Galstyan A, Sun T, Shatalova ES, Butte P, Mamelak AN, Carico C, Kittle DS, Grodzinski ZB, Chiechi A, Ding H, Black KL, Ljubimova JY, Holler E. Polymalic acid chlorotoxin nanoconjugate for near-infrared fluorescence guided resection of glioblastoma multiforme. Biomaterials. 2019;206:146–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Lee C, Kim GR, Yoon J, Kim SE, Yoo JS, Piao Y. In vivo delineation of glioblastoma by targeting tumor-associated macrophages with near-infrared fluorescent silica coated iron oxide nanoparticles in orthotopic xenografts for surgical guidance. Sci Rep. 2018;8(1):11122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Morgenroth A, Vogg AT, Ermert K, Zlatopolskiy B, Mottaghy FM. Hedgehog signaling sensitizes glioma stem cells to endogenous nano-irradiation. Oncotarget. 2014;5(14):5483–5493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Miller MA, Chandra R, Cuccarese MF, Pfirschke C, Engblom C, Stapleton S, Adhikary U, Kohler RH, Mohan JF, Pittet MJ, Weissleder R. Radiation therapy primes tumors for nanotherapeutic delivery via macrophage-mediated vascular bursts. Sci Transl Med. 2017;9(392). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Yang B, Chen Y, Shi J. Reactive Oxygen Species (ROS)-Based Nanomedicine. Chem Rev. 2019;119(8):48814985. [DOI] [PubMed] [Google Scholar]
- 390.Yong SB, Chung JY, Song Y, Kim J, Ra S, Kim YH. Non-viral nano-immunotherapeutics targeting tumor microenvironmental immune cells. Biomaterials. 2019;219:119401. [DOI] [PubMed] [Google Scholar]
- 391.Zanganeh S, Hutter G, Spitler R, Lenkov O, Mahmoudi M, Shaw A, Pajarinen JS, Nejadnik H, Goodman S, Moseley M, Coussens LM, Daldrup-Link HE. Iron oxide nanoparticles inhibit tumour growth by inducing proinflammatory macrophage polarization in tumour tissues. Nat Nanotechnol. 2016;11(11):986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Kamath AA, Friedman DD, Hacker CD, Smyth MD, Limbrick DD, Kim AH, Hawasli AH, Leuthardt EC. MRI-Guided Interstitial Laser Ablation for Intracranial Lesions: A Large Single-Institution Experience of 133 Cases. Stereotactic and Functional Neurosurgery. 2017;95(6):417–428. [DOI] [PubMed] [Google Scholar]
- 393.Shao J, Radakovich NR, Grabowski M, Borghei-Razavi H, Knusel K, Joshi KC, Muhsen BeA, Hwang L, Barnett GH, Mohammadi AM. Lessons Learned in Using Laser Interstitial Thermal Therapy (LITT) for Treatment of Brain Tumors: A Case Series of 238 Patients from A Single Institution. World Neurosurgery. 2020. [DOI] [PubMed] [Google Scholar]
- 394.Ceresoli GL, Aerts JG, Dziadziuszko R, Ramlau R, Cedres S, van Meerbeeck JP, Mencoboni M, Planchard D, Chella A, Crino L, Krzakowski M, Russel J, Maconi A, Gianoncelli L, Grosso F. Tumour Treating Fields in combination with pemetrexed and cisplatin or carboplatin as first-line treatment for unresectable malignant pleural mesothelioma (STELLAR): a multicentre, single-arm phase 2 trial. Lancet Oncol. 2019;20(12):1702–1709. [DOI] [PubMed] [Google Scholar]
- 395.Burri SH, Gondi V, Brown PD, Mehta MP. The Evolving Role of Tumor Treating Fields in Managing Glioblastoma: Guide for Oncologists. American Journal of Clinical Oncology. 2018;41(2):191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Kirson ED, Dbalý V, Tovaryš F, Vymazal J, Soustiel JF, Itzhaki A, Mordechovich D, Steinberg-Shapira S, Gurvich Z, Schneiderman R, Wasserman Y, Salzberg M, Ryffel B, Goldsher D, Dekel E, Palti Y. Alternating electric fields arrest cell proliferation in animal tumor models and human brain tumors. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(24):10152–10157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Stupp R, Idbaih A, Steinberg DM, Read W, Toms S, Barnett G, Nicholas G, Kim C-Y, Fink K, Salmaggi A, Lieberman F, Zhu J, Taylor L, Stragliotto G, Hottinger A, Kirson ED, Weinberg U, Palti Y, Hegi ME, Ram Z. LTBK01: Prospective, Multi-center Phase III Trial Of Tumor Treating Fields Together With Temozolomide Compared To Temozolomide Alone In Patients With Newly Diagnosed Glioblastoma. Neuro-Oncology. 2016;18(Suppl 6):i1.26705298 [Google Scholar]
- 398.Chang E, Patel CB, Pohling C, Young C, Song J, Flores TA, Zeng Y, Joubert LM, Arami H, Natarajan A, Sinclair R, Gambhir SS. Tumor treating fields increases membrane permeability in glioblastoma cells. Cell Death Discov. 2018;4:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Chang E, Pohling C, Beygui N, Patel CB, Rosenberg J, Ha DH, Gambhir SS. Synergistic inhibition of glioma cell proliferation by Withaferin A and tumor treating fields. J Neurooncol. 2017;134(2):259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–820. [DOI] [PubMed] [Google Scholar]
- 401.Poon MTC, Sudlow CLM, Figueroa JD, Brennan PM. Longer-term (>/= 2 years) survival in patients with glioblastoma in population-based studies pre- and post-2005: a systematic review and meta-analysis. Sci Rep. 2020;10(1):11622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Wick W, Weller M, van den Bent M, Sanson M, Weiler M, von Deimling A, Plass C, Hegi M, Platten M, Reifenberger G. MGMT testing--the challenges for biomarker-based glioma treatment. Nature Reviews Neurology. 2014;10(7):372–385. [DOI] [PubMed] [Google Scholar]
- 403.Saadatpour L, Fadaee E, Fadaei S, Nassiri Mansour R, Mohammadi M, Mousavi SM, Goodarzi M, Verdi J, Mirzaei H. Glioblastoma: exosome and microRNA as novel diagnosis biomarkers. Cancer Gene Ther. 2016;23(12):415–418. [DOI] [PubMed] [Google Scholar]
- 404.Huang SW, Ali ND, Zhong L, Shi J. MicroRNAs as biomarkers for human glioblastoma: progress and potential. Acta Pharmacol Sin. 2018;39(9):1405–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Osti D, Del Bene M, Rappa G, Santos M, Matafora V, Richichi C, Faletti S, Beznoussenko GV, Mironov A, Bachi A, Fornasari L, Bongetta D, Gaetani P, DiMeco F, Lorico A, Pelicci G. Clinical Significance of Extracellular Vesicles in Plasma from Glioblastoma Patients. Clin Cancer Res. 2019;25(1):266–276. [DOI] [PubMed] [Google Scholar]
- 406.Touat M, Duran-Pena A, Alentorn A, Lacroix L, Massard C, Idbaih A. Emerging circulating biomarkers in glioblastoma: promises and challenges. Expert Rev Mol Diagn. 2015;15(10):1311–1323. [DOI] [PubMed] [Google Scholar]
- 407.Santagata S, Eberlin LS, Norton I, Calligaris D, Feldman DR, Ide JL, Liu X, Wiley JS, Vestal ML, Ramkissoon SH, Orringer DA, Gill KK, Dunn IF, Dias-Santagata D, Ligon KL, Jolesz FA, Golby AJ, Cooks RG, Agar NY. Intraoperative mass spectrometry mapping of an onco-metabolite to guide brain tumor surgery. Proc Natl Acad Sci U S A. 2014;111(30):11121–11126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Qian J, Rankin EB. Hypoxia-Induced Phenotypes that Mediate Tumor Heterogeneity. Advances in Experimental Medicine and Biology. 2019;1136:43–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Schafer N, Gielen GH, Rauschenbach L, Kebir S, Till A, Reinartz R, Simon M, Niehusmann P, Kleinschnitz C, Herrlinger U, Pietsch T, Scheffler B, Glas M. Longitudinal heterogeneity in glioblastoma: moving targets in recurrent versus primary tumors. J Transl Med. 2019;17(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Le Rhun E, Preusser M, Roth P, Reardon DA, van den Bent M, Wen P, Reifenberger G, Weller M. Molecular targeted therapy of glioblastoma. Cancer Treatment Reviews. 2019;80:101896. [DOI] [PubMed] [Google Scholar]
- 411.Pradhan AK, Maji S, Das SK, Emdad L, Sarkar D, Fisher PB. MDA-9/Syntenin/SDCBP: new insights into a unique multifunctional scaffold protein. Cancer Metastasis Rev. 2020;39(3):769–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Talukdar S, Pradhan AK, Bhoopathi P, Shen XN, August LA, Windle JJ, Sarkar D, Furnari FB, Cavenee WK, Das SK, Emdad L, Fisher PB. Regulation of protective autophagy in anoikis-resistant glioma stem cells by SDCBP/MDA-9/Syntenin. Autophagy. 2018;14(10):1845–1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Kegelman TP, Wu B, Das SK, Talukdar S, Beckta JM, Hu B, Emdad L, Valerie K, Sarkar D, Furnari FB, Cavenee WK, Wei J, Purves A, De SK, Pellecchia M, Fisher PB. Inhibition of radiation-induced glioblastoma invasion by genetic and pharmacological targeting of MDA-9/Syntenin. Proc Natl Acad Sci U S A. 2017;114(2):370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Hassn Mesrati M, Behrooz AB, A YA, Syahir A. Understanding Glioblastoma Biomarkers: Knocking a Mountain with a Hammer. Cells. 2020;9(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Yu C, Mannan AM, Yvone GM, Ross KN, Zhang YL, Marton MA, Taylor BR, Crenshaw A, Gould JZ, Tamayo P, Weir BA, Tsherniak A, Wong B, Garraway LA, Shamji AF, Palmer MA, Foley MA, Winckler W, Schreiber SL, Kung AL, Golub TR. High-throughput identification of genotype-specific cancer vulnerabilities in mixtures of barcoded tumor cell lines. Nat Biotechnol. 2016;34(4):419–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Xiu J, Piccioni D, Juarez T, Pingle SC, Hu J, Rudnick J, Fink K, Spetzler DB, Maney T, Ghazalpour A, Bender R, Gatalica Z, Reddy S, Sanai N, Idbaih A, Glantz M, Kesari S. Multi-platform molecular profiling of a large cohort of glioblastomas reveals potential therapeutic strategies. Oncotarget. 2016;7(16):21556–21569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Jovcevska I Next Generation Sequencing and Machine Learning Technologies Are Painting the Epigenetic Portrait of Glioblastoma. Front Oncol. 2020;10:798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Valdebenito J, Medina F. Machine learning approaches to study glioblastoma: A review of the last decade of applications. Cancer Rep (Hoboken). 2019;2(6):e1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Zhou Y, Yang L, Zhang X, Chen R, Chen X, Tang W, Zhang M. Identification of Potential Biomarkers in Glioblastoma through Bioinformatic Analysis and Evaluating Their Prognostic Value. Biomed Res Int. 2019;2019:6581576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Pan ZQ, Zhang SJ, Wang XL, Jiao YX, Qiu JJ. Machine Learning Based on a Multiparametric and Multiregional Radiomics Signature Predicts Radiotherapeutic Response in Patients with Glioblastoma. Behav Neurol. 2020;2020:1712604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Andreatta F, Beccaceci G, Fortuna N, Celotti M, De Felice D, Lorenzoni M, Foletto V, Genovesi S, Rubert J, Alaimo A. The Organoid Era Permits the Development of New Applications to Study Glioblastoma. Cancers (Basel). 2020;12(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Ruiz-Garcia H, Alvarado-Estrada K, Schiapparelli P, Quinones-Hinojosa A, Trifiletti DM. Engineering ThreeDimensional Tumor Models to Study Glioma Cancer Stem Cells and Tumor Microenvironment. Front Cell Neurosci. 2020;14:558381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Infinger LK, Stevenson CB. Re-Examining the Need for Tissue Diagnosis in Pediatric Diffuse Intrinsic Pontine Gliomas: A Review. Curr Neuropharmacol. 2017;15(1):129–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Tang K, Gardner S, Snuderl M. The Role of Liquid Biopsies in Pediatric Brain Tumors. J Neuropathol Exp Neurol. 2020;79(9):934–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Linkous A, Balamatsias D, Snuderl M, Edwards L, Miyaguchi K, Milner T, Reich B, Cohen-Gould L, Storaska A, Nakayama Y, Schenkein E, Singhania R, Cirigliano S, Magdeldin T, Lin Y, Nanjangud G, Chadalavada K, Pisapia D, Liston C, Fine HA. Modeling Patient-Derived Glioblastoma with Cerebral Organoids. Cell Rep. 2019;26(12):3203–3211 e3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Ahluwalia M, Barnett GH, Deng D, Tatter SB, Laxton AW, Mohammadi AM, Leuthardt E, Chamoun R, Judy K, Asher A, Essig M, Dietrich J, Chiang VL. Laser ablation after stereotactic radiosurgery: a multicenter prospective study in patients with metastatic brain tumors and radiation necrosis. J Neurosurg. 2018;130(3):804–811. [DOI] [PubMed] [Google Scholar]
- 427.Gandhi S, Tayebi Meybodi A, Belykh E, Cavallo C, Zhao X, Syed MP, Borba Moreira L, Lawton MT, Nakaji P, Preul MC. Survival Outcomes Among Patients With High-Grade Glioma Treated With 5-Aminolevulinic AcidGuided Surgery: A Systematic Review and Meta-Analysis. Front Oncol. 2019;9:620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Michael AP, Watson VL, Ryan D, Delfino KR, Bekker SV, Cozzens JW. Effects of 5-ALA dose on resection of glioblastoma. J Neurooncol. 2019;141(3):523–531. [DOI] [PubMed] [Google Scholar]
- 429.Dubey A, Kataria R, Sinha VD. Role of Diffusion Tensor Imaging in Brain Tumor Surgery. Asian J Neurosurg. 2018;13(2):302–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Rahman M, Abbatematteo J, De Leo EK, Kubilis PS, Vaziri S, Bova F, Sayour E, Mitchell D, Quinones-Hinojosa A. The effects of new or worsened postoperative neurological deficits on survival of patients with glioblastoma. J Neurosurg. 2017;127(1):123–131. [DOI] [PubMed] [Google Scholar]
- 431.Stupp R, Taillibert S, Kanner AA, Kesari S, Steinberg DM, Toms SA, Taylor LP, Lieberman F, Silvani A, Fink KL, Barnett GH, Zhu JJ, Henson JW, Engelhard HH, Chen TC, Tran DD, Sroubek J, Tran ND, Hottinger AF, Landolfi J, Desai R, Caroli M, Kew Y, Honnorat J, Idbaih A, Kirson ED, Weinberg U, Palti Y, Hegi ME, Ram Z. Maintenance Therapy With Tumor-Treating Fields Plus Temozolomide vs Temozolomide Alone for Glioblastoma: A Randomized Clinical Trial. JAMA. 2015;314(23):2535–2543. [DOI] [PubMed] [Google Scholar]
- 432.Rominiyi O, Vanderlinden A, Clenton SJ, Bridgewater C, Al-Tamimi Y, Collis SJ. Tumour treating fields therapy for glioblastoma: current advances and future directions. Br J Cancer. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Yang J, Shi Z, Liu R, Wu Y, Zhang X. Combined-therapeutic strategies synergistically potentiate glioblastoma multiforme treatment via nanotechnology. Theranostics. 2020;10(7):3223–3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Gustafson HH, Holt-Casper D, Grainger DW, Ghandehari H. Nanoparticle Uptake: The Phagocyte Problem. Nano Today. 2015;10(4):487–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Zhao M, van Straten D, Broekman MLD, Preat V, Schiffelers RM. Nanocarrier-based drug combination therapy for glioblastoma. Theranostics. 2020;10(3):1355–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Willers H, Heilmann HP, Beck-Bornholdt HP. [One hundred years of radiotherapy. Historical origins and development of fractionated irradiation in German speaking countries]. Strahlenther Onkol. 1998;174(2):53–63. [DOI] [PubMed] [Google Scholar]
- 437.Daguenet E, Louati S, Wozny AS, Vial N, Gras M, Guy JB, Vallard A, Rodriguez-Lafrasse C, Magne N. Radiationinduced bystander and abscopal effects: important lessons from preclinical models. Br J Cancer. 2020;123(3):339–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Ene CI, Kreuser SA, Jung M, Zhang H, Arora S, White Moyes K, Szulzewsky F, Barber J, Cimino PJ, Wirsching HG, Patel A, Kong P, Woodiwiss TR, Durfy SJ, Houghton AM, Pierce RH, Parney IF, Crane CA, Holland EC. Anti-PD-L1 antibody direct activation of macrophages contributes to a radiation-induced abscopal response in glioblastoma. Neuro Oncol. 2020;22(5):639–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Junko Zenkoh AG, Wang Yuzi, Miwa Yoshihiro, Ohno Tadao, Tsuboi Koji. The abscopal effect induced by in situirradiated peripheral tumor cells in a murine GL261 brain tumor model. Translational Cancer Research. 2016;6. [Google Scholar]
- 440.Khawar IA, Kim JH, Kuh HJ. Improving drug delivery to solid tumors: priming the tumor microenvironment. J Control Release. 2015;201:78–89. [DOI] [PubMed] [Google Scholar]
- 441.Jiang W, Chan CK, Weissman IL, Kim BYS, Hahn SM. Immune Priming of the Tumor Microenvironment by Radiation. Trends Cancer. 2016;2(11):638–645. [DOI] [PubMed] [Google Scholar]


