Abstract
Impaired sense of smell occurs in a fraction of patients with COVID-19 infection, but its effect on cerebral activity is unknown. Thus, this case report investigated the effect of COVID-19 infection on frontotemporal cortex activity during olfactory stimuli. In this preliminary study, patients who recovered from COVID-19 infection (n = 6) and healthy controls who never contracted COVID-19 (n = 6) were recruited. Relative changes in frontotemporal cortex oxy-hemoglobin during olfactory stimuli was acquired using functional near-infrared spectroscopy (fNIRS). The area under curve (AUC) of oxy-hemoglobin for the time interval 5 s before and 15 s after olfactory stimuli was derived. In addition, olfactory function was assessed using the Sniffin’ Sticks 12-identification test (SIT-12). Patients had lower SIT-12 scores than healthy controls (p = 0.026), but there were no differences in oxy-hemoglobin AUC between healthy controls and patients (p > 0.05). This suggests that past COVID-19 infection may not affect frontotemporal cortex function, and these preliminary results need to be verified in larger samples.
Keywords: COVID-19, functional near-infrared spectroscopy (fNIRS), olfactory stimuli, sniffin’ sticks 12-identification test
1. Introduction
Globally, as of May 6, 2021, there have been 154,640,649 confirmed cases of Coronavirus disease-2019 (COVID-19), including 3,232,285 deaths, reported to the World Health Organization (WHO) [1]. Since the outbreak of the COVID-19 pandemic, medical professionals have a better understanding of the pathogenesis and clinical features of COVID-19 infection. COVID-19 creates severe respiratory distress and other systemic complications involving multiple organ systems, due to a cascade of immunological responses [2]. Patients who suffered from COVID-19 infection may develop neurological complications, including acute myelitis, cerebrovascular accidents, cerebral venous thrombosis, Guillain-Barré syndrome, meningoencephalitis, posterior reversible encephalopathy syndrome and seizures [3]. Common neuropsychiatric symptoms of COVID-19 infection include change in mental state, delirium, giddiness, gustatory impairment, myalgia, headache [3] and cognitive impairment [4]. In addition to the above symptoms, COVID-19 infection is known to cause olfactory dysfunction [5]. Recent studies have focused on developing questionnaires and a smell identification test that assess olfactory dysfunction [6,7]. It has been reported that the prevalence of olfactory dysfunction is 73.1%, with a male to female ratio of 1:3 [8]. It was also reported that complete recovery of olfactory dysfunction occurs in 31.8% of COVID-19 survivors [8].
Olfactory dysfunction may be due to olfactory cleft opacification and olfactory bulb degeneration, detected by magnetic resonance imaging (MRI) of the olfactory bulb and computer tomography of the paranasal sinus [9]. Furthermore, there has been a report on the association between opacification in the olfactory cleft and the degree of loss of smell [10]. Olfactory dysfunction is thought to manifest when viral replication in the non-neural olfactory cells indirectly cause damage to the olfactory receptor nerves [11]. The COVID-19 virus binds to the human angiotensin converting enzyme ACE2 receptor, and it may thus target other cells that express this protein, such as neurons in the brain [5]. Viruses have been shown to be transported along synapses connecting the peripheral olfactory epithelium and the central nervous system. The first target regions are part of the olfactory system, including the olfactory bulb and amygdala. The virus may then spread to other tissues and induce neurodegenerative symptoms such as epilepsy, motor and cognitive symptoms [5]. In addition, recent studies have linked the incidence of acute respiratory failure with COVID-19 infection of the brainstem. It has been postulated that the COVID-19 virus causes dysfunction of the respiratory center by spreading from the olfactory bulb to the olfactory nerves, the rhinencephalon and, finally, the brainstem [12].
Despite the potential neuropathogenesis, neuroimaging studies on patients with COVID-19 and other respiratory infections are limited. Electroencephalography of patients with COVID-19 infection have shown frontal lobe abnormalities [13,14], while positron emission tomography (PET) of these patients has identified altered glucose metabolism in several brain areas. These include hypometabolism in the bilateral parahippocampal and fusiform gyri, left insula [15], dorsolateral prefrontal cortex, bilateral frontal eye fields and right anterior cingulate cortex, as well as hypermetabolism in the left orbitofrontal cortex, right posterior parietal cortex and right thalamus [16]. Grey matter volume loss detected by MRI occurred in the right orbitofrontal cortex of patients with post-infectious olfactory loss [17], decreased functional connectivity of the chemosensory network occurred in patients with chronic peripheral smell loss [17] and hypometabolism of the medial and lateral temporal cortex occurred in patients with olfactory dysfunction after an upper respiratory tract infection [18]. Taken together, the literature suggests that COVID-19 infection may affect brain function and that viral-associated loss of smell may be linked to long-term changes in the brain. Still, there is a gap in the literature about the neurophysiological response to direct olfactory stimulation in patients with viral-associated smell loss. Hence, neurobiological investigations with technologies that allow neuroimaging data to be acquired during direct olfactory stimulation, such as functional near-infrared spectroscopy (fNIRS), are needed.
fNIRS enables real-time monitoring of hemodynamic changes in the cerebral cortex, because light in the near-infrared spectrum has the unique property of passing though tissues and being preferentially absorbed by hemoglobin in the cerebral cortex [19]. The absorbance spectra of hemoglobin is dependent on its binding with oxygen, which enables fNIRS devices to continuously detect relative changes in both oxy-hemoglobin and deoxy-hemoglobin in the cortical regions being studied [20]. According to a phenomenon called neurovascular coupling, fNIRS signals are believed to be a surrogate measure of the underlying neural activity [21]. Regional neuron activity triggers an increase in blood flow and volume that is many times higher than the metabolic demand. Therefore, cerebral hemodynamic response typically involves a large increase in oxy-hemoglobin and a simultaneous slight decrease in deoxy-hemoglobin [22]. Since there is a net change in oxy-hemoglobin, oxy-hemoglobin is used as a marker of cerebral activity [23].
Although near-infrared light cannot reach brain areas below the cortex, fNIRS has several practical advantages in both research and clinical settings compared to conventional neuroimaging modalities, such as functional magnetic resonance imaging (fMRI). Both fMRI and fNIRS are non-invasive and non-ionizing modalities that map brain activity by measuring changes in haemoglobin concentration. Studies that have used fNIRS and fMRI concurrently to measure activity during mental tasks have found that fNIRS signals are highly correlated with fMRI blood oxygen level-dependent (BOLD) signals recorded in the same neuroanatomical regions [24]. fNIRS offers an alternative to fMRI for olfactory research, because it is economical, quiet, does not require restraints, tolerant to motion, does not exclude special populations (such as individuals with claustrophobia or metal implants) [19] and does not require special equipment to deliver odorants [25]. Importantly, abnormal fNIRS signals during various olfactory stimuli have been reported in the frontal, temporal and/or parietal cortex of patients with chronic sinusitis [26], multiple chemical sensitivity [27], attention-deficit/hyperactivity disorder [28], subjective memory complaints, mild cognitive impairment and very mild Alzheimer’s disease [29], relative to healthy controls.
To the best of our knowledge, no research article has been published on fNIRS of individuals with COVID-19 infection since the outbreak of the pandemic. Such an instigation may identify abnormalities in olfactory and cerebral cortex function induced by the COVID-19 virus. Due to the lockdown and other social measures, we were not able to carry out large scale recruitment or recruit patients while they were infected with COVID-19. Thus, we compared fNIRS signals during olfactory stimuli between individuals with and without a history of COVID-19 infection in this case report. Among the regions of the brain associated with olfactory processing, the role of the orbitofrontal cortex is the most well established [25]. Hence, we hypothesized that oxy-hemoglobin changes during olfactory stimuli in the frontotemporal cortex would be lower in patients who recovered from COVID-19 infection than healthy controls.
2. Materials and Methods
2.1. Participants
This pilot case report included six healthy controls and six patients who had recovered from COVID-19 infection. All participants were at least 21-years old. Healthy controls were recruited from the community, while patients were recruited from and managed at our tertiary institution, the National University Hospital, Singapore, between 1 April to 31 October 2020. COVID-19 patients were contacted after they were discharged from the hospital and posed no significant risk of infecting others, including the researchers. The inclusion criterion for patients was a confirmed diagnosis of COVID-19 infection and a positive real-time reverse-transcription polymerase chain reaction assay of throat swab samples. Healthy controls were included if they had never contracted COVID-19 and had a negative COVID-19 swab test. The exclusion criteria for all participants were a history of neurological illnesses; traumatic brain injury; psychiatric disorder; intellectual disability; active cerebrovascular, respiratory, hepatic, renal disease, malignancy, chronic nasal conditions and previous nasal surgery. In addition, participants with rhinitis, history of sinunasal disease or known hyposmia for reasons other than past COVID-19 infection were excluded.
This study complied with the ethical standards of the Declaration of Helsinki and the ethical principles in the Belmont Report. It was approved by the Domain Specific Review Board (DSRB) of the National Healthcare Group, Singapore (protocol number 2020/00832). Written informed consent was obtained from participants prior to the commencement of the study.
2.2. Olfactory Assessment and Assessment of Other Symptoms
All participants refrained from smoking, eating and drinking 30 min prior to participating in this study. Olfactory function was assessed with the Sniffin’ Sticks 12-identification test (SIT-12; MediSense, Groningen, The Netherlands) [30]. The SIT-12 is a psychophysical, semi-objective assessment of olfactory performance [31] that has been validated in previous studies involving COVID-19 patients [32]. The test consists of 12 Sniffin’ sticks that resemble the 12 different odorants, including peppermint, fish, coffee, banana, orange, rose, lemon, pineapple, cinnamon, cloves, leather and licorice. Each Sniffin’ stick resembles a felt-tip pen containing a tampon and a liquid odorant dissolved in propylene glycol (4% dilution with a total volume of 4 mL) [28]. Sniffin’ Sticks were sequentially placed 2–3 cm in front of the subject’s nose for 3 s, and participants needed to choose one item out of four items on a card that was most closely associated with the scent [33]. The total number of correctly identified odorants was recorded as the SIT-12 score [33]. Scores from 0–6, 7–10 and 11–12 indicate anosmia, hyposmia and normosmia, respectively [34].
2.3. fNIRS Measurements
A 52-channel fNIRS system (ETG-4000. Hitachi Medical Co., Tokyo, Japan) was used in this study. This fNIRS device used two near-infrared light wavelengths (695 and 830 nm) to measure relative oxy-hemoglobin and deoxy-hemoglobin changes at a sampling rate of 10 Hz. Emitter and detector optodes were placed 3 cm apart. The cortical areas between each emitter and detector pairs are known as a channel. Anatomically, channels correspond to cortical regions 2–3 cm beneath the skin and scalp surface [35]. Optodes were placed on the forehead and scalp, with the lowest optodes placed along the T4-Fpz-T3 line, defined by the 10/20 system. This arrangement allowed for hemoglobin changes in the bilateral prefrontal cortex, frontopolar cortex and the anterior regions of the superior and middle temporal cortices to be measured. These approximate channel locations were based on the anatomical craniocerebral correction of the international 10/20 system.
2.4. Olfactory Stimuli
Olfactory stimuli during fNIRS measurements began with a 30-s rest period, followed by four 10-s olfactory stimulus periods that alternated with four 50-s rest periods [28]. A different odorant was presented for each stimulus period using Sniffin’ Sticks (Burghart Instruments, Germany) that were held 1 cm in front of the participant’s nostrils. The odorants were apple, garlic, chocolate and sesame oil [36], and these were presented in this order. Participants were asked to keep their eyes closed, keep their head and body still and breathe naturally throughout the fNIRS measurement.
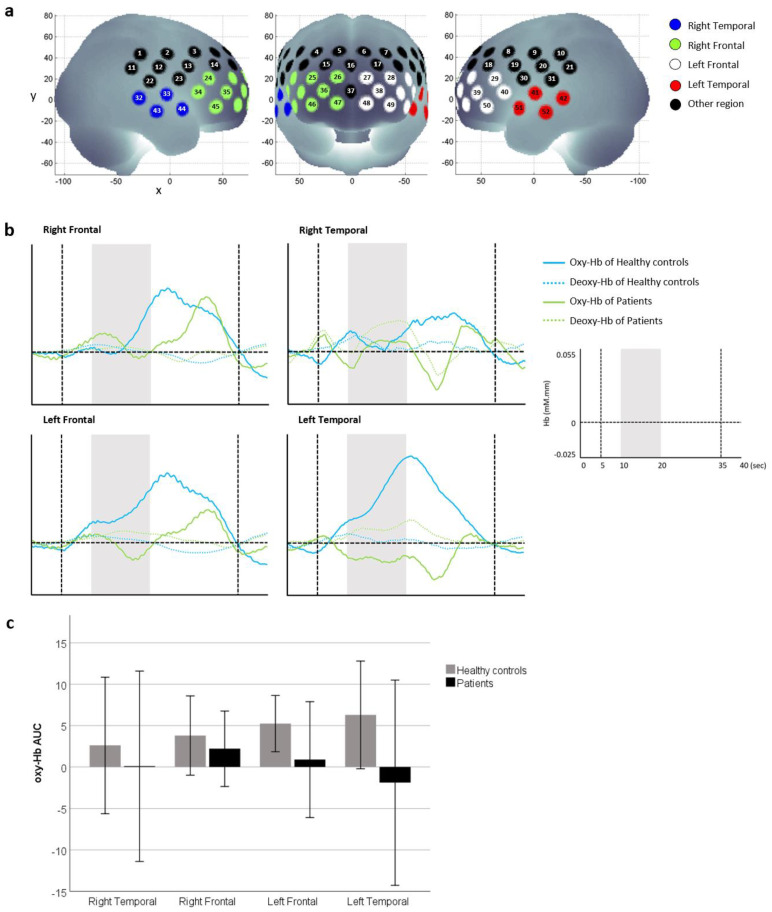
2.5. fNIRS Signal Processing
The fNIRS signals were processed according to the method described by Schecklmann et al. [28]. Oxy-hemoglobin, deoxy-hemoglobin and total hemoglobin were derived from optical densities using the modified Beer–Lambert law. A moving average factor of five was applied to remove short-term motion artefacts. Slow drifts were removed using linear fitting between a 10-s baseline at the end of the pre-stimulus rest period and a 10-s post-stimulus baseline period that begins 10 s into the post-stimulus rest period. Channels with body movement artefacts or high and low frequency noise were removed from further analysis. An average oxy-hemoglobin and deoxy-hemoglobin waveform of the four stimulus periods was generated for remaining channels. Since oxy-hemoglobin is typically used as a marker of cortical activity, the area under curve (AUC) of oxy-hemoglobin for the time interval 5 s before and 15 s after olfactory stimuli [28] was derived for each participant and region. The four regions of interest were the left and right frontal and temporal cortex (Figure 1a). The AUC of oxy-hemoglobin was used in further statistical analysis.
Figure 1.
(a) Four regions called the right and left frontal and temporal regions were studied. (b) Average oxy-hemoglobin and deoxy-hemoglobin waveforms of patients who recovered from COVID-19 infection and healthy controls who never contracted COVID-19 were generated for each region. Grey areas indicate the olfactory stimulus period, and vertical dotted lines indicate the time period used to calculate the AUC of oxy-hemoglobin. (c) Comparison of oxy-hemoglobin AUC between healthy controls and patients. Data are presented as mean ± SD. There were no differences between groups when oxy-hemoglobin AUC at each region were compared using Mann–Whitney U tests (p > 0.05).
2.6. Statistical Analysis
The effect of diagnostic group (i.e., COVID-19 infection vs. healthy controls) on continuous and categorical variables was determined using Mann–Whitney U test and Pearson’s chi-squared test, respectively. Continuous variables were age, SIT-12 score and AUC of oxy-hemoglobin at each region of interest. Categorical variables were gender and handedness. All tests were two-tailed, with a significance of p ≤ 0.05. Statistical analysis was performed using SPSS (Version 26, Armonk, NY, USA: IBM Corp).
3. Results
3.1. Sample Characteristics
Healthy controls and patients who had recovered from COVID-19 infection did not differ in gender (p = 1.0) and handedness (p = 1.0) (see Table 1). Compared to healthy controls, patients were older but within the adult age range, and had lower SIT-12 scores (p = 0.002). The median time between recovery from COVID-19 infection to fNIRS measurement was 20.6 (range 16.6–27.6) weeks. Amongst healthy controls, five were normosmic (83.3%), and one was dysosmic (16.7%). Amongst patients, two were normosmic (33.3%), two were dysosmic (33.3%) and two were anosmic (33.3%).
Table 1.
Demographic and clinical variables.
| Healthy Controls (n = 6) | Patients Who Had Recovered from COVID-19 Infection (n = 6) | p-Value | |
|---|---|---|---|
| Median age in years (range) | 32 (30–33) | 39.5 (36–48) | 0.002 |
| Gender | 1.000 | ||
| Male n (%) | 4 (66.7%) | 4 (66.7%) | |
| Female n (%) | 2 (33.3%) | 2 (33.3%) | |
| Handedness | 1.000 | ||
| Right n (%) | 6 (100%) | 5 (83.3%) | |
| Left n (%) | 0 | 1 (16.7%) | |
| Median SIT-12 score (range) | 11.5 (10–12) | 7.5 (4–11) | 0.026 |
| Median duration in weeks between recovery from the COVID-19 infection and fNIRS measurement (range) | 20.6 (16.6–27.6) |
p ≤ 0.05 are in bold.
3.2. Cortical Oxy-Haemoglobin during Olfactory Stimuli
Averaged oxy-hemoglobin waveforms (see Figure 1b) showed that relative oxy-hemoglobin changes during and after olfactory stimuli may have been higher in healthy controls than patients who recovered from COVID-19 infection, particularly in the left frontal and temporal region. However, there was no difference in oxy-hemoglobin AUC between healthy controls and patients in any region (see Figure 1c).
4. Discussion
Research on COVID-19-associated smell loss is important, because olfactory dysfunction has been linked to reduced mortality, quality of life, appetite and immunity. Loss of smell may also worsen medical illnesses and raises safety concerns, due to the inability to detect noxious environmental elements, such as fire, gas leaks and spoiled food [37]. This pilot case report found that patients who recovered from COVID-19 infection demonstrated lower olfactory function than healthy controls. Reduced SIT-12 scores in this sample of patients is consistent with previous studies that reported a persistent loss of smell even after patients with this symptom recovered from COVID-19 infection [38,39]. The cellular basis for these observations may be explained by a study describing the presence of virus transcripts and of SARS-CoV-2-infected cells in the olfactory mucosa of patients with long-term persistence of COVID-19-associated loss of smell [40].
There were no differences in oxy-hemoglobin AUC during olfactory stimuli between healthy controls and patients, suggesting that frontotemporal function is not affected by past COVID-19 infection. Still, several routes by which the brain may be infected have been proposed, including entry through the olfactory nerve, transsynaptic transfer across infected neurons, vascular endothelium infection and migration of leukocytes across the blood–brain barrier [41]. Furthermore, previous reports have demonstrated that the COVID-19 virus can infect cells and cause neuronal death in vitro. On the other hand, analysis of cerebral spinal fluid samples and post-mortem brain tissues has provided inconsistent evidence for the neuroinvasion of COVID-19 [42]. When reviewing findings from animal models, Butowt et al. [43] concluded that the evidence for the olfactory route to brain infection is weak, and that the loss of smell does not indicate that the virus has entered the brain. In short, the mechanisms behind the neurological symptoms in COVID-19 infection and the potential for neuroinvasion of the virus in humans is still not clear [44]. Given that the available data on how the COVID-19 virus interacts with the brain and its vasculature is limited, the basic question of whether neurological manifestations of COVID-19 reflects brain invasion remains unanswered [42]. Continued efforts to study the acute and long-term effects of COVID-19 infection on the brain, using various techniques, including neuroimaging, is essential to enhance our understanding of the neurogenesis of this virus. Thus, repeating the fNIRS measurements during olfactory stimuli in a larger sample of individuals with and without a history of COVID-19 infection may be relevant. Furthermore, olfactory training is currently the only evidence-based therapy available for patients who have not regained their sense of smell after one month since the onset of COVID-19 induced olfactory dysfunction [37]. Future neuroimaging research on the effect of olfactory training may be of interest as well.
There are several limitations in this preliminary fNIRS study. Firstly, a small sample of participants were recruited due to quarantine measures during the pandemic. Consequently, this case report did not have adequate power to demonstrate statistically significant differences in cortical oxy-hemoglobin AUC between healthy controls and patients who recovered from COVID-19 infection. Secondly, patients were older than healthy controls. Regardless, all participants were within the adult age range, and the median age of healthy controls and patients who recovered from COVID-19 was under 40 years. Interestingly, a recent study reported that young adults who recovered from COVID-19 infection were prone to develop olfactory dysfunction [45]. Hence, we believe the effect of older age on measured outcomes was minimal. Thirdly, participants in this preliminary study were not exposed to a control odor during fNIRS measurements. Therefore, the findings of increased oxy-hemoglobin during olfactory stimuli in healthy controls need to be verified in a larger sample of individuals who are exposed to both experiment and control odors. Fourthly, the SIT-12 is a screening tool that does not have the same diagnostic accuracy as the standard Sniffin’ Sticks test, which comprises of threshold, discrimination and identification subtests. Fifthly, not all healthy controls were normosmic, and a fraction of patients were normosmic. Lastly, the median time of the fNIRS scan and recovery of COVID-19 infection was 20.6 weeks and not immediate after COVID-19 infection. A recent study found that there was a time-dependent increase in smell scores in healthcare workers who had recovered from COVID-19 infection [46]. We could not recruit patients soon after they were discharged from the hospital due to safety measures and concerns over the spread of COVID-19 to the research team and healthy controls. Despite these limitations, this has been the first functional neuroimaging case report on patients with who recovered from COVID-19 infection.
5. Conclusions
A history of COVID-19 infection was found to be associated with lower olfactory function assessed by the SIT-12, but not frontotemporal cortex hemodynamic response to olfactory stimuli measured with fNIRS. Nevertheless, fNIRS investigations on a larger sample of individuals with and without a history of COVID-19 infection may provide additional objective evidence to support the persistence of olfactory dysfunction detected by semi-objective smelling tests and self-reported questionnaires.
Acknowledgments
The authors would like to thank all study participants and Hitachi Medical Systems Singapore for their kind contribution of the ETG-4000 system.
Author Contributions
Conceptualization, R.C.H., V.K.S., S.F.H. and A.C.Y.C.; methodology, R.C.H., S.F.H., B.X.T. and Q.-H.P.; formal analysis, R.C.H., S.F.H., B.X.T. and Q.-H.P.; data curation, B.Y.Q.T., A.Y.Y.N. and Y.-S.L.; writing—original draft preparation, R.C.H., V.K.S., S.F.H. and A.C.Y.C.; writing—review and editing, R.S.M., C.S.H., B.Y.Q.T., A.C.Y.C., Y.-S.L., B.X.T. and Q.-H.P.; funding acquisition, R.C.H. and B.X.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NUS iHeathtech Other Operating Expenses (R-722-000-004-731) and the Vingroup Innovation Foundation, under project code VINIF.2019.DA14.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and it was approved by the Domain Specific Review Board of the National Healthcare Group, Singapore (protocol number 2020/00832).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be obtained from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization WHO Coronavirus Disease (COVID-19) Dashboard. [(accessed on 6 May 2021)]; Available online: https://covid19.who.int/
- 2.Ashraf O., Young M., Malik K.J., Cheema T. Systemic Complications of COVID-19. Crit. Care Nurs. Q. 2020;43:390–399. doi: 10.1097/CNQ.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 3.Harapan B.N., Yoo H.J. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19) J. Neurol. 2021:1–13. doi: 10.1007/s00415-021-10406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alnefeesi Y., Siegel A., Lui L.M., Teopiz K.M., Ho R., Lee Y., Nasri F., Gill H., Lin K., Cao B. Impact of SARS-CoV-2 Infection on Cognitive Function: A Systematic Review. Front. Psychiatry. 2021;11:1629. doi: 10.3389/fpsyt.2020.621773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rebholz H., Braun R.J., Ladage D., Knoll W., Kleber C., Hassel A.W. Loss of Olfactory Function—Early Indicator for Covid-19, Other Viral Infections and Neurodegenerative Disorders. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.569333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim J.-W., sang Kim H., Kim M., Kim S.H., Cho S.-W., Kim J.Y. Validation of Olfactory Questionnaire in Koreans: An Alternative for Conventional Psychophysical Olfactory Tests. J. Korean Med. Sci. 2021;36:e34. doi: 10.3346/jkms.2021.36.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boscolo-Rizzo P., Menegaldo A., Fabbris C., Spinato G., Borsetto D., Vaira L.A., Calvanese L., Pettorelli A., Sonego M., Frezza D. Six-month psychophysical evaluation of olfactory dysfunction in patients with COVID-19. Chem. Senses. 2021;46 doi: 10.1093/chemse/bjab006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andrews P.J., Pendolino A.L., Ottaviano G., Scarpa B., Grant J., Gaudioso P., Bordin A., Marchese-Ragona R., Leoni D., Cattelan A. Olfactory and taste dysfunction among mild-to-moderate symptomatic COVID-19 positive health care workers: An international survey. Laryngoscope Investig. Otolaryngol. 2020;5:1019–1028. doi: 10.1002/lio2.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kandemirli S.G., Altundag A., Yildirim D., Sanli D.E.T., Saatci O. Olfactory bulb MRI and paranasal sinus CT findings in persistent COVID-19 anosmia. Acad. Radiol. 2021;28:28–35. doi: 10.1016/j.acra.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yıldız E., Balcı A., Selendili O., Kuzu S. Olfactory Cleft Opacification in COVID-19 Related Smell Loss: CT Findings and Correlation With Objective Testing. Ear Nose Throat J. 2021 doi: 10.1177/01455613211011285. [DOI] [PubMed] [Google Scholar]
- 11.Yazdanpanah N., Saghazadeh A., Rezaei N. Anosmia: A missing link in the neuroimmunology of coronavirus disease 2019 (COVID-19) Rev. Neurosci. 2020;31:691–701. doi: 10.1515/revneuro-2020-0039. [DOI] [PubMed] [Google Scholar]
- 12.Machado C., DeFina P.A., Chinchilla M., Machado Y., Machado Y. Brainstem Dysfunction in SARS-COV-2 Infection can be a Potential Cause of Respiratory Distress. Neurol. India. 2020;68:989–993. doi: 10.4103/0028-3886.299165. [DOI] [PubMed] [Google Scholar]
- 13.Vellieux G., Sonneville R., Vledouts S., Jaquet P., Rouvel-Tallec A., d’Ortho M.P. COVID-19-Associated Neurological Manifestations: An Emerging Electroencephalographic Literature. Front. Physiol. 2021;11 doi: 10.3389/fphys.2020.622466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kopańska M., Banaś-Ząbczyk A., Łagowska A., Kuduk B., Szczygielski J. Changes in EEG Recordings in COVID-19 Patients as a Basis for More Accurate QEEG Diagnostics and EEG Neurofeedback Therapy: A Systematic Review. J. Clin. Med. 2021;10:1300. doi: 10.3390/jcm10061300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donegani M.I., Miceli A., Pardini M., Bauckneht M., Chiola S., Pennone M., Marini C., Massa F., Raffa S., Ferrarazzo G., et al. Brain Metabolic Correlates of Persistent Olfactory Dysfunction after SARS-Cov2 Infection. Biomedicines. 2021;9:287. doi: 10.3390/biomedicines9030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niesen M., Trotta N., Noel A., Coolen T., Fayad G., Leurkin-Sterk G., Delpierre I., Henrard S., Sadeghi N., Goffard J.C., et al. Structural and metabolic brain abnormalities in COVID-19 patients with sudden loss of smell. Eur. J. Nucl. Med. Mol. Imaging. 2021;48:1890–1901. doi: 10.1007/s00259-020-05154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kollndorfer K., Jakab A., Mueller C., Trattnig S., Schöpf V. Effects of chronic peripheral olfactory loss on functional brain networks. Neuroscience. 2015;310:589–599. doi: 10.1016/j.neuroscience.2015.09.045. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y.K., Hong S.-L., Yoon E.J., Kim S.E., Kim J.-W. Central presentation of postviral olfactory loss evaluated by positron emission tomography scan: A pilot study. Am. J. Rhinol. Allergy. 2012;26:204–208. doi: 10.2500/ajra.2012.26.3759. [DOI] [PubMed] [Google Scholar]
- 19.Lai C.Y.Y., Ho C.S.H., Lim C.R., Ho R.C.M. Functional near-infrared spectroscopy in psychiatry. BJPsych Adv. 2017;23:324–330. doi: 10.1192/apt.bp.115.015610. [DOI] [Google Scholar]
- 20.Ho C.S., Zhang M.W., Ho R.C. Optical Topography in Psychiatry: A Chip Off the Old Block or a New Look Beyond the Mind-Brain Frontiers? Front. Psychiatry. 2016;7:74. doi: 10.3389/fpsyt.2016.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gsell W., De Sadeleer C., Marchalant Y., MacKenzie E.T., Schumann P., Dauphin F. The use of cerebral blood flow as an index of neuronal activity in functional neuroimaging: Experimental and pathophysiological considerations. J. Chem. Neuroanat. 2000;20:215–224. doi: 10.1016/S0891-0618(00)00095-8. [DOI] [PubMed] [Google Scholar]
- 22.Scholkmann F., Kleiser S., Metz A.J., Zimmermann R., Pavia J.M., Wolf U., Wolf M. A review on continuous wave functional near-infrared spectroscopy and imaging instrumentation and methodology. Neuroimage. 2014;85:6–27. doi: 10.1016/j.neuroimage.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 23.Ferrari M., Quaresima V. A brief review on the history of human functional near-infrared spectroscopy (fNIRS) development and fields of application. Neuroimage. 2012;63:921–935. doi: 10.1016/j.neuroimage.2012.03.049. [DOI] [PubMed] [Google Scholar]
- 24.Cui X., Bray S., Bryant D.M., Glover G.H., Reiss A.L. A quantitative comparison of NIRS and fMRI across multiple cognitive tasks. Neuroimage. 2011;54:2808–2821. doi: 10.1016/j.neuroimage.2010.10.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olofsson J.K., Freiherr J. Neuroimaging of smell and taste. Handb. Clin. Neurol. 2019;164:263–282. doi: 10.1016/b978-0-444-63855-7.00017-4. [DOI] [PubMed] [Google Scholar]
- 26.Kobayashi E., Karaki M., Kusaka T., Kobayashi R., Itoh S., Mori N. Functional optical hemodynamic imaging of the olfactory cortex in normosmia subjects and dysosmia subjects. Acta Oto-Laryngol. 2009;129:79–84. doi: 10.1080/00016480902964325. [DOI] [PubMed] [Google Scholar]
- 27.Azuma K., Uchiyama I., Takano H., Tanigawa M., Azuma M., Bamba I., Yoshikawa T. Changes in cerebral blood flow during olfactory stimulation in patients with multiple chemical sensitivity: A multi-channel near-infrared spectroscopic study. PLoS ONE. 2013;8:e80567. doi: 10.1371/journal.pone.0080567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schecklmann M., Schenk E., Maisch A., Kreiker S., Jacob C., Warnke A., Gerlach M., Fallgatter A.J., Romanos M. Altered frontal and temporal brain function during olfactory stimulation in adult attention-deficit/hyperactivity disorder. Neuropsychobiology. 2011;63:66–76. doi: 10.1159/000323448. [DOI] [PubMed] [Google Scholar]
- 29.Fladby T., Bryhn G., Halvorsen O., Rosé I., Wahlund M., Wiig P., Wetterberg L. Olfactory response in the temporal cortex of the elderly measured with near-infrared spectroscopy: A preliminary feasibility study. J. Cereb. Blood Flow Metab. 2004;24:677–680. doi: 10.1097/01.WCB.0000119966.74298.5C. [DOI] [PubMed] [Google Scholar]
- 30.Pinkhardt E.H., Liu H., Ma D., Chen J., Pachollek A., Kunz M.S., Kassubek J., Ludolph A.C., Huang Y., Chen H. Olfactory screening of Parkinson’s Disease patients and healthy subjects in China and Germany: A study of cross-cultural adaptation of the Sniffin’Sticks 12-identification test. PLoS ONE. 2019;14:e0224331. doi: 10.1371/journal.pone.0224331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rumeau C., Nguyen D.T., Jankowski R. How to assess olfactory performance with the Sniffin’ Sticks test®. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2016;133:203–206. doi: 10.1016/j.anorl.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 32.Bagnasco D., Passalacqua G., Braido F., Tagliabue E., Cosini F., Filauro M., Ioppi A., Carobbio A., Mocellin D., Riccio A.M. Quick Olfactory Sniffin’Sticks Test (Q-Sticks) for the detection of smell disorders in COVID-19 patients. World Allergy Organ. J. 2021;14:100497. doi: 10.1016/j.waojou.2020.100497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hummel T., Sekinger B., Wolf S.R., Pauli E., Kobal G. ‘Sniffin’sticks: Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem. Senses. 1997;22:39–52. doi: 10.1093/chemse/22.1.39. [DOI] [PubMed] [Google Scholar]
- 34.Hummel T., Konnerth C.G., Rosenheim K., Kobal G. Screening of olfactory function with a four-minute odor identification test: Reliability, normative data, and investigations in patients with olfactory loss. Ann. Otol. Rhinol. Laryngol. 2001;110:976–981. doi: 10.1177/000348940111001015. [DOI] [PubMed] [Google Scholar]
- 35.Okada E., Delpy D.T. Near-infrared light propagation in an adult head model. II. Effect of superficial tissue thickness on the sensitivity of the near-infrared spectroscopy signal. Appl. Opt. 2003;42:2915–2921. doi: 10.1364/AO.42.002915. [DOI] [PubMed] [Google Scholar]
- 36.Shu C.-H., Yuan B.-C. Assessment of odor identification function in Asia using a modified “Sniffin’Stick” odor identification test. Eur. Arch. Oto-Rhino-Laryngol. 2008;265:787–790. doi: 10.1007/s00405-007-0551-2. [DOI] [PubMed] [Google Scholar]
- 37.Mullol J., Alobid I., Mariño-Sánchez F., Izquierdo-Domínguez A., Marin C., Klimek L., Wang D.Y., Liu Z. The Loss of Smell and Taste in the COVID-19 Outbreak: A Tale of Many Countries. Curr. Allergy Asthma Rep. 2020;20:61. doi: 10.1007/s11882-020-00961-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Loftus P.A., Roland L.T., Gurrola J.G., Cheung S.W., Chang J.L. Temporal Profile of Olfactory Dysfunction in COVID-19. OTO Open. 2020;4:2473974×20978133. doi: 10.1177/2473974X20978133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Otte M.S., Eckel H.N.C., Poluschkin L., Klussmann J.P., Luers J.C. Olfactory dysfunction in patients after recovering from COVID-19. Acta Otolaryngol. 2020;140:1032–1035. doi: 10.1080/00016489.2020.1811999. [DOI] [PubMed] [Google Scholar]
- 40.de Melo G.D., Lazarini F., Levallois S., Hautefort C., Michel V., Larrous F., Verillaud B., Aparicio C., Wagner S., Gheusi G., et al. COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci. Transl. Med. 2021;13:eabf8396. doi: 10.1126/scitranslmed.abf8396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zubair A.S., McAlpine L.S., Gardin T., Farhadian S., Kuruvilla D.E., Spudich S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020;77:1018–1027. doi: 10.1001/jamaneurol.2020.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iadecola C., Anrather J., Kamel H. Effects of COVID-19 on the nervous system. Cell. 2020;183:16–27. doi: 10.1016/j.cell.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Butowt R., Meunier N., Bryche B., von Bartheld C.S. The olfactory nerve is not a likely route to brain infection in COVID-19: A critical review of data from humans and animal models. Acta Neuropathol. 2021;141:809–822. doi: 10.1007/s00401-021-02314-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mukerji S.S., Solomon I.H. What can we learn from brain autopsies in COVID-19? Neurosci. Lett. 2021;742:135528. doi: 10.1016/j.neulet.2020.135528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheng M.-Y., Hsih W.-H., Ho M.-W., Lai Y.-C., Liao W.-C., Chen C.-Y., Chen T.-C., Lee Y.-L., Liu P.-Y., Kao C.-C. Younger adults with mild-to-moderate COVID-19 exhibited more prevalent olfactory dysfunction in Taiwan. J. Microbiol. Immunol. Infect. 2021 doi: 10.1016/j.jmii.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao A.C., Nimmo Z.M., Mirza N., Cohen N.A., Brody R.M., Doty R.L. Objective screening for olfactory and gustatory dysfunction during the COVID-19 pandemic: A prospective study in healthcare workers using self-administered testing. World J. Otorhinolaryngol. Head Neck Surg. 2021 doi: 10.1016/j.wjorl.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be obtained from the corresponding author upon request.