Abstract
Background
Chronic kidney disease (CKD) has become a global public health problem. Accumulating evidence suggested that vitamins play important roles in the progression of CKD.
Methods
A cross-sectional study was conducted to investigate the vitamin status of patients with CKD at stage 1–5. The serum concentrations of 9 vitamins, vitamin A, B1, B2, B6, B9, B12, C, D, and E were measured by electroanalytical method with a Multi-Vitamin Analyzer. Pearson correlation and multiple linear regression between serum level of vitamins were analyzed.
Results
The median levels of vitamin A, B1, B2, B6, B9, B12, C and E were within the reference ranges or on the borderline. Vitamin D deficiency was found in all patients. Weak correlation was found between vitamin A or vitamin D and estimated glomerular filtration rate (eGFR). The Pearson correlation coefficient were − 0.21766 and 0.19752, respectively. Hypertension, diabetes mellitus, and atherosclerosis were the major comorbidities.
Conclusions
For the first time, the serum levels of 9 vitamins were measured simultaneously in patients with CKD at different stages. Vitamin D deficiency was found in all patients. Weak correlation between vitamin A or vitamin D and eGFR was found.
Keywords: Chronic kidney disease, Glomerular filtration rate, Vitamin, Deficiency, Cross-sectional study
Background
Chronic kidney disease (CKD) refers to kidney damage and decreased renal function, which can be classified into 5 stages according to KDOQI guidelines [1]. The global prevalence of CKD (stage 1–5) was estimated as 13.4 % with a 95 % confidence interval (CI) from 11.7 to 15.1 %. The prevalence of stages 3 to stage 5 was 10.6 % (95 %CI: 9.2-12.2 %) [2]. In China, about 119 million people are suffering from CKD [3]. Individuals with CKD are facing an increased risk for kidney failure, cardiovascular disease, and mortality despite standard interventions for managing the conventional risk factors associated with it [4]. CKD has been recognized as one of the most serious health problems worldwide, increasing the global burden of morbidity and mortality, as well as consuming scarce health resources. Therefore, deeper understanding of its mechanism and new intervention approaches based on non-traditional risk factors are of great importance [3–6].
Over the years, both basic research and clinical trials have improved our understanding of the interaction between disordered vitamins and CKD [7, 8]. CKD has been identified as a risk factor for vitamin D deficiency, which is highly prevalent in patients with CKD, especially those with end-stage renal disease (ESRD) and kidney transplant recipients [9]. The deficiency of serum 25(OH)D3 (the major circulating form of vitamin D) is present in all subsequent stages of CKD [10], and the prevalence increases as kidney function declines [11]. Individuals with 25(OH)D3 levels lower than 37.5 nM (15 ng/mL) had a higher risk for all-cause mortality despite adjustments for CKD stage and confounding factors [12]. To date, no randomized clinical trial (RCT) aiming to verify the beneficial effect of 25(OH)D3 supplementation on the outcomes of CKD has been identified [13]. The correlation between vitamin D and the prognosis of CKD needs further verification.
Renal dysfunction of CKD patients is reportedly associated with a decrease in plasma vitamin C level. Moreover, decreased vitamin C may cause endothelial dysfunction via an increase in oxidative stress in non-diabetic chronic kidney disease patients [14]. Hyperhomocysteinemia (hHcy) is recognized as a novel risk factor that contributes to the increased incidence of cardiac event among CKD patients. hHcy occurs in about 85 % of chronic kidney disease (CKD) patients, mainly because of the deficiency of vitamin В6, В9 and В12 [15]. It is therefore reasonable to assume that lowering homocysteine by B vitamin supplementation would finally lead to a reduction of cardiovascular complication and mortality. However, interventional studies through B vitamin supplementation to reduce homocysteine level did not show favorable clinical outcomes [16]. Despite this, folic acid (vitamin B9) treatment was associated with a significant reduction in the odds of CKD progression among mild to moderate CKD patients. A large RCT in China showed statistically significant reductions in the risk of first stroke and CKD progression with the addition of folic acid to Enalapril in adults with hypertension [17]. Recently, the genetic polymorphisms in vitamin metabolism have received great attention, suggesting that the evaluation of vitamin status from different gene polymorphisms may not be comparable [18]. Taken together, it is of great importance to study the pathophysiological role of the vitamins and discuss their correlation with CKD progression under different genetic background. This study aimed to investigate the vitamin status of patients with CKD in China and evaluate the correlation between serum vitamin level and progression of renal function.
Methods
Study design
CKD was defined as abnormalities of kidney structure or function, present for more than 3 months, with implications for health (Not graded). The diagnostic thresholds were estimated glomerular filtration rate (eGFR) of less than 60 mL/min per 1.73 m2 and an albumin-creatinine ratio (ACR) of 30 mg/g or greater were retained [19, 20] CKD was classified into five stages per the KDOQI guidelines using thresholds of estimated glomerular filtration rate (eGFR) within the CKD range and/or evidence of structural renal changes [21]. The eGFR value for different CKD stages were: eGFR ≥ 90 (stage 1), 60 ≤ eGFR < 90 (stage 2); 30 ≤ eGFR < 60 (stage 3); 15 ≤ eGFR < 30 (stage 4); and eGFR < 15 (stage 5).
From May 2018 to September 2019, consecutive patients with primary diagnosis of CKD and hospitalized at the Department of Nephrology, the First Medical Center of the General Hospital of People’s Liberation Army, were invited to participate the study. Exclusion criteria were (1) acute kidney injury (any of the following: increase in serum creatinine (sCr) by ≥ 0.3 mg/dl (≥ 26.5 µmol/l) within 48 h; or an increase in serum creatinine to ≥ 1.5 times baseline for 7 days; or a urine volume < 0.5 ml/kg/h for 6 h.); [22] (2) younger than 18 years old; (3) have participated in other kidney disease-pertinent clinical trial; (4) history of organ or bone marrow transplantation; (5) missed important analytic variables.
The study was approved by ethics committee of First Medical Center of Chinese People’s Liberation Army General Hospital and carried out in accordance with the declaration of Helsinki.
Anthropometric data collection
Following our standardized protocols, demographic data and anthropometric measurements were collected by trained investigators. eGFR was calculated by the CKD Epidemiology Collaboration (CKD-EPI) equation [23]. Body mass index (BMI) was calculated as body weight (kg)/squared height (m2). Complete blood count, alkaline phosphatase (ALP), calcium, phosphorus, iron, albumin, creatinine, cystatin C, total cholesterol (CHOL), triglyceride (TG), high‑density lipoprotein (HDL), low‑density lipoprotein (LDL), homocysteine (Hcy) and other biochemical and clinical tests were performed as routine investigations. Renal biopsy was performed to investigate the possible etiology of CKD.
The analysis of serum vitamins
Serum concentrations of 9 vitamins, vitamin A, B1, B2, B6, B9, B12, C, D and E were measured by electroanalytical method with Multi-Vitamin Analyzer (LK3000V, Tianjin Lanbiao Electronic Technology Development Co. Ltd, China) following the manufacturer’s instructions. Briefly, 10ml venous blood sample was collected after 12-hour fasting and was centrifuged at 3000 rpm for 10 min quickly after collection. The separated serum sample were stored at 4 °C for testing. Vitamin E had to be tested within 24 h of sample collection, while other vitamins could be tested within 3 days. Sample preparation solution and vitamin standard solution for calibration were provided by the Tianjin Lanbiao Electronic Technology Development Co. Ltd, China. The detection limitation for different vitamins were vitamin A: 8.5 × 10− 10 mol/L, vitamin B1: 3.4 × 10− 9 mol/L, vitamin B2: 4.3 × 10− 8 mol/L, vitamin B6: 1.5 × 10− 10 mol/L, vitamin B9: 2.3 × 10− 10 mol/L, vitamin B12: 1.7 × 10− 12 mol/L, vitamin C: 2.8 × 10− 6 mol/L, vitamin D: 3.8 × 10− 9 mol/L, vitamin E: 6.0 × 10− 6 mol/L.
The concentration of a specific vitamin in serum sample below the following reference value was defined as deficiency, vitamin A: 0.70 µM, vitamin B1: 80.3 nM, vitamin B2: 106 nM, vitamin B6: 20 nM, vitamin B9: 10 nM, vitamin B12: 150 pM, vitamin C: 11 µM, vitamin D: 50 nM, and vitamin E: 23 µM. Normal value of serum homocysteine is below 15 µM [24–31].
Statistical analyses
All statistical analyses were performed using SAS (version 9.3; Cary, NC). Each variable was tested for normality before statistical analysis. Data were presented as median (interquartile range, IQR) or frequency (%). The difference between two groups were analyzed by the chi-squared test, Fisher’s Exact test, Kruskal-Wallis test or Student-Newman-Keuls test where appropriate. Pearson correlation coefficient was calculated to characterize the correlation between two variables. Multiple linear regression analysis was performed to examine the correlation between significant variables and eGFR. All p-values were two-tailed and those less than 0.05 were considered statistically significant.
Results
In total, 759 CKD patients were included in this study. Based on their eGFR values, the participants were assigned to 5 different stages according to the classification criteria described in the Methods section. The demographic and clinical characteristics of the cohort by different CKD stages were presented in Table 1. About three quarters of the patients were from stage 1 to stage 3, while the rest were from stage 4 and stage 5 equally. Patients in advanced stages were older than those in the lower stages (p < 0.001). More female patients were found in stage 1, whilst more males were found in other stages (p < 0.001). No statistically significant difference was found in the body mass index (BMI) of different stages. Serum concentrations of prealbumin, cystatin-C, alkaline phosphatase (ALP), creatinine, Hcy, urine protein, blood urea nitrogen (BUN), and uric acid increased along with the severity of CKD. The Hcy of patients with CKD at stage 1 were within the normal range, though it started increasing from stage 2 until stage 5, when Hcy levels were 2.58 times that of stage 1. Other indicators, such as hemoglobin (Hb), urine osmolality, and total iron binding capacity (TIBC) followed a decreasing trend in relation to the increasing severity of CKD.
Table 1.
Demographic and Clinical characteristics of CKD patients
| Variable | CKD | p-value | ||||
|---|---|---|---|---|---|---|
| Stage 1 (n = 179) |
Stage 2 (n = 187) |
Stage 3 (n = 201) |
Stage 4 (n = 97) |
Stage 5 (n = 95) |
||
| Age (year) | 41 (30, 49) | 45 (33, 55) | 48 (36, 59) | 51 (40, 62) | 50 (36, 60) | 0.000 |
| Sex (M/F) | 57/122 | 124/62 | 148/53 | 70/27 | 69/26 | 0.000 |
| BMI (kg/m2) | 25.14 (22.04, 27.61) | 25.39 (23.46, 28.06) | 25.68 (22.84, 28.59) | 24.52 (23.13, 26.71) | 25.32 (23.05, 27.99) | 0.166 |
| Ca (mM) | 2.16 (2.08, 2.25) | 2.20 (2.09, 2.29) | 2.19 (2.08, 2.30) | 2.20 (2.11, 2.26) | 2.11 (1.95, 2.19) | 0.000 |
| Fe (mM) | 14.00 (9.60, 19.30) | 15.90 (12.55, 20.05) | 14.40 (11.00, 18.35) | 12.60 (9.70, 16.20) | 9.75 (6.90, 14.20) | 0.000 |
| P (mM) | 1.21 (1.09, 1.33) | 1.19 (1.05, 1.35) | 1.21 (1.07, 1.37) | 1.26 (1.12, 1.43) | 1.85 (1.56, 2.20) | 0.000 |
| WBC (109/L) | 6.72 (5.47, 8.26) | 6.48 (5.57, 8.05) | 6.65 (5.38, 8.0) | 6.57 (5.37, 7.7) | 6.78 (5.63, 8.43) | 0.834 |
| Hb (g/L) | 128 (116, 140) | 138 (124, 150) | 128 (115, 146) | 114 (102, 127) | 89 (80, 101) | 0.000 |
| CRP (mg/L) | 0.9 (0.5, 1.0) | 0.9 (0.6, 1.0) | 0.9 (0.6, 1.1) | 0.9 (0.6, 1.8) | 1.0 (0.7, 2.7) | 0.003 |
| Prealbumin (mg/L) | 272.0 (229.5, 338.0) | 299.0 (251.0, 363.0) | 307.5 (250.0, 371.0) | 333.0 (264.0, 394.0) | 336.0 (288.5, 431.0) | 0.000 |
| Urine protein (g/d) | 1.23 (0.40, 2.89) | 1.17 (0.49, 3.15) | 1.50 (0.40, 3.18) | 1.84 (0.79, 3.50) | 2.80 (1.60, 4.34) | 0.000 |
| Albumin (g/L) | 35.3 (30.3, 40.6) | 36.6 (29.7, 41.3) | 38.0 (32.2, 42) | 38.8 (29.7, 41.4) | 37.0 (33.0, 40.9) | 0.084 |
| Creatinine (µM) | 63.4 (56.7, 70.8) | 86.0 (80.0, 92.5) | 125.7 (112.5, 146.5) | 218.4 (190.8, 252.7) | 615.3 (443.4, 851.5) | 0.000 |
| BUN (nM) | 4.31 (3.59, 5.19) | 5.34 (4.56, 6.14) | 7.43 (6.11, 9.12) | 11.33 (9.72, 14.38) | 22.58 (17.85, 28.93) | 0.000 |
| Uric acid (µM) | 326.2 (269.9, 376.0) | 372.8 (324.4, 437.2) | 397.1 (335, 470.2) | 401.4 (336.3, 474.5) | 434.9 (349.2, 516) | 0.000 |
| ALP (U/L) | 53.5 (43.9, 62.9) | 55.7 (45.2, 69.4) | 60.4 (46.4, 73.8) | 63.4 (50.2, 75.2) | 67.0 (51.4, 82.0) | 0.000 |
| TC (mM) | 4.53 (3.82, 5.63) | 4.40 (3.71, 5.62) | 4.18 (3.61, 5.28) | 3.85 (3.32, 4.69) | 3.96 (3.24, 5.01) | 0.000 |
| TG (mM) | 1.67 (1.18, 2.55) | 1.8 (1.26, 2.46) | 1.85 (1.23, 2.83) | 1.75 (1.26, 2.69) | 1.82 (1.26, 2.33) | 0.779 |
| HDLC (mM) | 1.12 (0.98, 1.43) | 1.10 (0.88, 1.36) | 1.02 (0.85, 1.29) | 0.96 (0.80, 1.26) | 0.94 (0.81, 1.14) | 0.000 |
| LDLC (mM) | 2.91 (2.26, 3.79) | 2.75 (2.22, 3.53) | 2.62 (1.99, 3.67) | 2.17 (1.72, 3.10) | 2.32 (1.70, 3.00) | 0.000 |
| Hcy (µM) | 10.7 (8.6, 13.4) | 13.9 (11.8, 17.7) | 18.6 (15.4, 24.2) | 23.3 (17.2, 31.5) | 27.6 (19.6, 36.9) | 0.000 |
| Cystatin-C (mg/L) | 0.86 (0.74, 0.95) | 1.04 (0.91, 1.17) | 1.58 (1.33, 1.86) | 2.47 (2.21, 2.94) | 4.43 (3.79, 5.36) | 0.000 |
| TIBC (µM) | 46.8 (40.7, 52.6) | 44.9 (39.7, 50.6) | 44.0 (36.8, 49.5) | 40.8 (36.3, 46.3) | 40.6 (34.7, 47.5) | 0.000 |
| HbA1c (%) | 5.50 (5.20, 6.05) | 5.50 (5.20, 5.80) | 5.85 (5.25, 6.50) | 6.10 (5.40, 6.80) | 5.50 (5.20, 6.20) | 0.008 |
| IgA (mg/dl) | 227 (177, 325) | 239 (188, 338) | 247 (188, 321) | 219 (170, 300) | 220 (168, 285) | 0.206 |
| IgM (mg/dl) | 97.9 (67.8, 132.0) | 84.9 (62.5, 121.0) | 90.5 (62.8, 118.0) | 92.4 (54.5, 133.0) | 68.4 (48.8, 96.3) | 0.002 |
| IgG (mg/dl) | 931 (684, 1114) | 933 (661, 1190) | 997 (779, 1250) | 1040 (783, 1290) | 995 (748, 1220) | 0.029 |
| C3 (mg/dl) | 109.0 (92.7, 122.0) | 108.0 (93.8, 120.0) | 102.0 (86.9, 116.0) | 94.4 (81.7, 111.0) | 88.5 (71.2, 106.0) | 0.000 |
| C4 (mg/dl) | 23.4 (18.8, 29.4) | 24.7 (20.6, 29.2) | 26.0 (21.5, 30.7) | 26.1 (21.9, 33.6) | 26.7 (22.4, 32.0) | 0.004 |
Note: results were from blood samples unless otherwise specified; data were expressed as median (IQR); BMI body mass index; WBC white blood cell; Hb hemoglobin; CRP C-reactive protein; BUN blood urea nitrogen; ALP alkaline phosphatase; TC total cholesterol; TG triglyceride; HDLC high-density lipoprotein cholesterol; LDLC low-density lipoprotein cholesterol; Hcy homocysteine; TIBC total iron binding capacity; HbA1c glycated hemoglobin; C3 complement component 3; C4 complement component 4
Based on the results of renal biopsy, the pathological classification of CKD patients was displayed in Table 2. The pathological subgroups of CKD were not distributed equally in different stages (p < 0.001). The major pathological type of CKD in this cohort was IgA nephropathy (40.6 %) followed by membranous nephropathy at a prevalence of 31.5 %.
Table 2.
Pathological diagnosis of CKD patients
| Pathological subgroup |
CKD | p-value | ||||
|---|---|---|---|---|---|---|
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | Stage 5 | ||
| IgAN | 37 (17.05) | 62 (28.57) | 80 (36.87) | 26 (11.98) | 12 (5.53) | 0.000 |
| MN | 71 (42.26) | 64 (38.09) | 26 (15.48) | 6 (3.57) | 1 (0.60) | ---- |
| FSGS | 1 (2.86) | 5 (14.28) | 23 (65.72) | 4 (11.43) | 2 (5.71) | ---- |
| OPN | 16 (36.36) | 12 (27.27) | 9 (20.45) | 3 (6.81) | 4 (9.09) | ---- |
| SN | 17 (24.29) | 13 (18.57) | 23 (32.86) | 11 (15.71) | 6 (8.57) | ---- |
Note: data were expressed as frequency (%); MN membranous nephropathy; IgAN IgA nephropathy; FSGS focal segmental glomerulosclerosis; OPN other primary nephropathy; SN secondary nephropathy
Hypertension was the most common comorbidity in this cohort. 437 (75.47 %) patients were suffering from hypertension. Its incidence increased along with the increase of CKD severity, ranging from 29 % of stage 1 patients to 87 % of stage 5 patients. 140 (18.44 %) and 81 (10.67 %) patients had diabetes mellitus (DM) and atherosclerosis, respectively. The incidence rates of hypertension, DM, and atherosclerosis were higher in advanced stages than in lower stages (p < 0.001). The incidence rates of other comorbidities, such as liver disease (14.23 %), gastrointestinal diseases (11.86 %), respiratory diseases (10.93 %), cancer (5.80 %), and coronary heart disease (5.40 %) were relatively low, and no difference was found in different stages. More details of the common comorbidities in this cohort were shown in Table 3.
Table 3.
Common comorbidities in CKD patients at different stages
| Comorbidity | CKD | p-value | ||||
|---|---|---|---|---|---|---|
| Stage 1 (n = 179) |
Stage 2 (n = 187) |
Stage 3 (n = 201) |
Stage 4 (n = 97) |
Stage 5 (n = 95) |
||
| Hypertension | 52 (29.05) | 86 (45.99) | 136 (67.66) | 80 (82.47) | 83 (87.37) | 0.000 |
| Diabetes mellitus | 19 (10.61) | 15 (8.02) | 43 (21.39) | 30 (30.93) | 33 (34.74) | 0.000 |
| Atherosclerosis | 9 (5.03) | 20 (10.70) | 16 (7.96) | 20 (20.62) | 16 (16.84) | 0.000 |
| Liver disease | 17 (9.50) | 32 (17.11) | 37 (18.41) | 11 (11.34) | 11 (11.58) | 0.071 |
| Gastrointestinal diseases | 17 (9.50) | 20 (10.70) | 27 (13.43) | 12 (12.37) | 14 (14.74) | 0.653 |
| Respiratory diseases | 26 (14.53) | 19 (10.16) | 24 (11.94) | 6 (6.19) | 8 (8.42) | 0.235 |
| Cancer | 13 (7.26) | 11 (5.88) | 5 (2.49) | 10 (10.31) | 5 (5.26) | 0.078 |
| Coronary heart disease | 6 (3.35) | 7 (3.74) | 8 (3.98) | 11 (11.34) | 9 (9.47) | 0.011 |
Note: data were expressed as frequency (%)
The serum level of 9 vitamins were exhibited in Table 4. Most of the patients had their serum vitamin concentration above the reference levels. Few of them had their vitamin A levels on the borderline or below the reference value. It is worth noting that vitamin D deficiency was found in all of the participants. The concentration of vitamin D started decreasing from stage 3, and its level in stage 5 was lower than in stage 4, the concentration in the latter was lower than in stage 3 (p < 0.001). The changing of vitamin D level was associated with the severity of eGFR staging (p < 0.001), age (p = 0.004) and sex (p = 0.024). The concentration of vitamin A increased from stage 1 to stage 5. However, the changing of vitamin A level was only correlated with eGFR staging (p < 0.001) and sex (p = 0.002). No statistical difference was noticed in vitamin B9, C or E between different stages.
Table 4.
Serum concentrations of vitamins in CKD patients
| Vitamin | CKD | p-value | ||||
|---|---|---|---|---|---|---|
| Stage 1 (n = 179) |
Stage 2 (n = 187) |
Stage 3 (n = 201) |
Stage 4 (n = 97) |
Stage 5 (n = 95) |
||
| Vit A (µM) | 0.69 (0.54, 0.92) | 0.73 (0.60, 0.98) | 0.85 (0.64, 1.04) | 0.81 (0.67, 1.03) | 1.01 (0.77, 1.34) | 0.000 |
| Vit B1 (nM) | 82.91 (76.47, 91.04) | 87.27 (77.65, 97.09) | 86.11 (78.77, 95.79) | 89.33 (80.49, 101.68) | 83.81 (76.87, 92.79) | 0.004 |
| Vit B2 (nM) | 11.50 (10.73, 12.36) | 11.37 (10.68, 12.43) | 11.29 (10.63, 12.30) | 10.84 (10.26, 11.77) | 11.05 (10.47, 12.01) | 0.000 |
| Vit B6 (nM) | 31.30 (29.67, 33.12) | 31.46 (29.44, 32.93) | 31.28 (29.16, 33.21) | 32.11 (29.16, 34.02) | 33.67 (30.98, 34.92) | 0.000 |
| Vit B9 (nM) | 20.51 (15.76, 24.88) | 18.51 (14.76, 24.65) | 18.2 (13.97, 23.45) | 19.34 (15.41, 24.85) | 19.24 (14.35, 23.87) | 0.150 |
| Vit B12 (pM) | 418.5 (361.7, 448.1) | 403.0 (363.0, 445.3) | 390.4 (355.3, 430.8) | 417.3 (381.2, 445.3) | 438.2 (390.0, 464.7) | 0.000 |
| Vit C (µM) | 35.44 (33.29, 38.96) | 35.54 (34.04, 37.76) | 35.82 (33.46, 38.38) | 35.7 (34.37, 38.66) | 36.36 (34.35, 38.45) | 0.733 |
| Vit D (nM) | 35.68 (29.41, 42.47) | 35.65 (30.03, 42.29) | 35.24 (28.80, 40.78) | 30.01 (24.74, 34.98) | 26.12 (20.86, 30.27) | 0.000 |
| Vit E (µM) | 25.72(25.03, 26.37) | 25.98 (25.17, 26.58) | 25.66 (24.96, 26.51) | 25.56 (24.98, 26.33) | 25.84 (25.10, 26.75) | 0.177 |
Note: data were expressed as median (IQR)
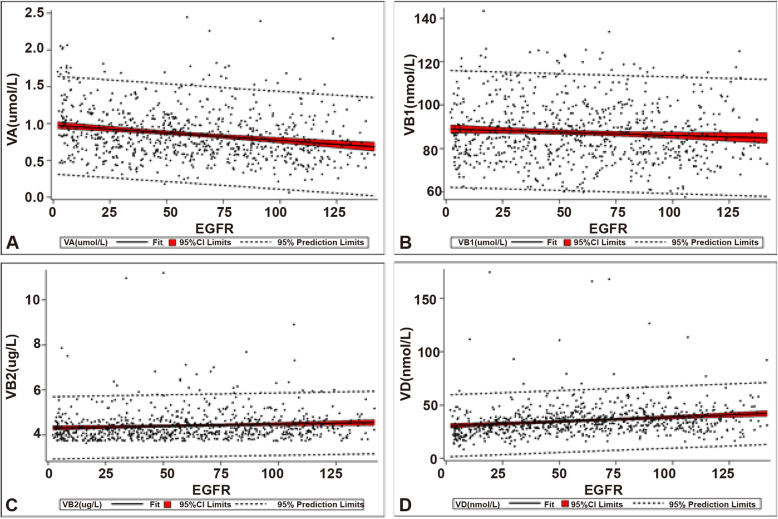
No difference in vitamin levels was observed between different pathological subgroups (Table 5), suggesting no correlation between the vitamin level and pathological subgroups of CKD. Details of the correlation analysis and multiple linear regression analysis between serum levels of each vitamin and eGFR was listed in Table 6. Based on the significance tests, significant but weak correlation was found between vitamin A, B1, or D and eGFR. However, the coefficient of vitamin B1 (-0.07844, p = 0.0307) was too small to be practically meaningful. Vitamin A was inversely associated with eGFR (-0.21766, p < 0.0001), whilst vitamin D (0.19752, p < 0.001) was positively associated (Fig. 1).
Table 5.
Serum concentrations of vitamins in CKD patients of different pathological subgroups
| Vitamin | CKD | p-value | ||||
|---|---|---|---|---|---|---|
| MN | IgAN | FSGS | OPN | SN | ||
| Vit A (µM) | 0.75 (0.57, 0.96) | 0.82 (0.64, 1.06) | 0.78 (0.68, 0.99) | 0.79 (0.61,1.04) | 0.73 (0.55, 0.94) | 0.063 |
| Vit B1 (nM) | 83.93 (76.82,95.16) | 84.51 (75.70, 96.26) | 87.23 (78.40,96.22) | 83.09 (80.42,88.56) | 85.59 (78.59,90.02) | 0.885 |
| Vit B2 (nM) | 11.34 (10.68, 12.36) | 11.42 (10.68, 12.33) | 11.41 (10.63, 12.41) | 11.34 (10.44, 12.22) | 11.42 (10.44, 12.14) | 0.912 |
| Vit B6 (nM) | 31.25 (29.37,32.73) | 31.26 (28.96,32.99) | 31.15 (27.95,33.18) | 32.27 (29.59,34.53) | 31.67 (29.94,33.63) | 0.057 |
| Vit B9 (nM) | 19.81 (14.76,24.16) | 19.43 (15.36,24.77) | 17.90 (12.96,20.93) | 19.40 (13.92,25.62) | 18.28 (14.94,24.75) | 0.472 |
| Vit B12 (pM) | 417.2 (364.6, 445.5) | 413.3 (363.7, 448.1) | 377.0 (353.6, 419.0) | 408.2 (371.4, 446.5) | 412.9 (354.0, 449.2) | 0.260 |
| Vit C (µM) | 35.33 (33.25,38.41) | 35.82 (34.00,38.46) | 35.87 (33.68,37.59) | 35.13 (32.69,38.81) | 35.56 (34.10,37.77) | 0.616 |
| Vit D (nM) | 33.56 (27.32,39.92) | 35.58 (29.88, 41.45) | 36.73 (28.88,43.06) | 33.46 (28.19,40.51) | 33.51 (27.58,39.09) | 0.255 |
| Vit E (µM) | 25.91 (25.14, 26.54) | 26.24 (25.07, 26.68) | 25.63 (24.89, 26.26) | 25.70 (24.94, 26.44) | 25.61 (25.05, 26.40) | 0.396 |
Note: data were expressed as median (IQR); MN membranous nephropathy; IgAN IgA nephropathy; FSGS focal segmental glomerulosclerosis; OPN other primary nephropathy; SN secondary nephropathy
Table 6.
The correlation and regression analysis between different vitamins and estimated glomerular filtration rate (eGFR)
| Variable | Pearson correlation | Multiple linear regression | |||
|---|---|---|---|---|---|
| Coefficient | p-value | Parameter | SE of parameter | p-value | |
| Vit A | -0.21766 | < 0.0001 | -23.45440 | 3.63941 | < 0.0001 |
| Vit B1 | -0.07844 | 0.0307 | -0.20342 | 0.09237 | 0.0280 |
| Vit B2 | 0.08720 | 0.0163 | 0.69456 | 1.98502 | 0.7265 |
| Vit B6 | -0.06300 | 0.0828 | -0.12628 | 0.31433 | 0.6880 |
| Vit B9 | 0.06546 | 0.0715 | 0.33561 | 0.21735 | 0.1230 |
| Vit B12 | -0.05781 | 0.1115 | ---- | ---- | ---- |
| Vit C | -0.03097 | 0.3943 | ---- | ---- | ---- |
| Vit D | 0.19752 | < 0.0001 | 0.46360 | 0.09356 | < 0.0001 |
| Vit E | 0.00177 | 0.9611 | ---- | ---- | ---- |
| Intercept | ---- | ---- | 76.19669 | 16.60018 | < 0.0001 |
Fig. 1.
The correlation between vitamins and estimated glomerular filtration rate (eGFR). A, inverse correlation between vitamin A and eGFR. Pearson correlation coefficient is -0.21766 (p < 0.0001); B, inverse correlation between vitamin B1 and eGFR. Pearson correlation coefficient is -0.07844 (p = 0.0307); C, correlation between vitamin B2 and eGFR. Pearson correlation coefficient is 0.08720 (p = 0.0163); D, correlation between vitamin D and eGFR. Pearson correlation coefficient is -0.19752 (p < 0.0001)
Discussion
CKD has become a grave public health problem worldwide, especially in developing countries. Being the largest developing country in this world, China has about 119.5 (112.9–125.0) million CKD patients [3]. The prevalence of CKD increases with age of the population [2]. In 2000, a cross-sectional study including 15,540 Chinese adults was carried out. The age-specific prevalence of CKD was 0.71 %, 1.69 %, 3.91 %, and 8.14 % among participants aged 35 to 44, 45 to 54, 55 to 64, and 65 to 74 years old, respectively [32]. In 2012, the results of a China’s national cross-sectional investigation showed that the average age of patients with CKD at stage 3–5 was 63.6 ± 14.7 [3]. In our study, the median age of CKD patients at stage 3–5 was only 50 years old, which was more than 10 years younger than in previous studies. The discrepancy in patients’ average ages may be due to the prevalence of comorbidities or the composition of pathological subgroups. For example, less than 10 % (70/759) of the patients were diagnosed with secondary nephropathy, which needs further study.
Hypertension, DM and CVD are common coexisting chronic diseases of CKD in clinical setting, where one is not necessarily more central than the other. CKD is not only a common cause of hypertension but also a complication of uncontrolled hypertension [33]. The prevalence of hypertension in patients with CKD could increase from 67 to 92 % along with the declining of eGFR in advanced stages [34]. The interaction between CKD and hypertension is complex, and is more likely to lead to poor CVD outcomes. Thus, lowing blood pressure can slow the decline of eGFR, delay the progression to end-stage renal disease (ESRD), and reduce the incidence of CVD in CKD patients as well [35]. DM is a recognized risk factor for CVD and is the leading cause of CKD. In America, the prevalence of CKD among patients with DM was about 36 %, which was more than 2 folds of general population [36]. In the present study, the prevalence of hypertension, DM, and atherosclerosis increased along with the decreasing of eGFR. For example, the prevalence of hypertension in stage 1 and stage 5 patients were 29.05 and 87.37 %, respectively. This finding was in line with previous studies [34]. In addition, the prevalence of hypertension and DM in patients with CKD at stage 3–5 was 76.1 and 26.2 %, which was much higher than a cross-sectional study reported in 2012 [3]. The higher prevalence of hypertension (76.1 % vs. 60.5 %) and DM (26.2 % vs. 19.1 %) could be one of the reasons leading to a younger median age of patients with CKD at stages 3–5 in the present study, also suggesting that patients’ ages may be on a downward trend.
Vitamins, water or fat-soluble, are important for normal cellular function as well as the growth and development of human body. Due to this, vitamin deficiency may cause severe health problem. It was reported that vitamins played important roles in the prognosis of CKD. Hyperhomocysteinemia (hHcy) was highly prevalent and strongly associated with renal function deterioration in patients with CKD. Vitamins B9 and B12 regulate the metabolism of homocysteine and reduce the odds of CKD progression by 83 % [17]. Vitamin D deficiency (VDD) had been reported to be as high as 80 % in patients with CKD, which was associated with albuminuria, faster progression of kidney disease and leading to increased all-cause mortality [13]. In this study, we investigated the status of vitamin status in 759 hospitalized patients with CKD at stage 1–5, and evaluated their association with eGFR. To our knowledge, this was the first of its kind that 9 vitamins associated with CKD were studied simultaneously. Based on the literature review, there was no consensus regarding the reference range for vitamin D deficiency. Some experts suggested serum vitamin D level should be equal or greater than 30 nmol/L, [30] while others proposed that serum level between 50 and 74 nmol/L as insufficiency, and less than 50 nmol/L as deficiency [37]. In light of the importance of vitamin D in the progression of CKD, we preferred to use a stricter reference value (50 nmol/L) to evaluate the status of vitamin D in patients with CKD. In this case, vitamin D deficiency was found in all patients of this study. A weak positive correlation (0.19752, p < 0.001) between vitamin D and eGFR was identified, indicating that circulating vitamin D concentrations were lower in patients of advanced stages and with lower eGFR. Vitamin D deficiency may be related to a decrease in intake from food, supplement, insufficient sunlight exposure, or generation of vitamin D3 from 7-DHC [38]. Due to the limitations of data collected in this study, it was difficult to confirm that vitamin D deficiency were attributed to the above mentioned reasons. However, it was worth noting that the urine protein of this cohort ranged from 1.23 g/d (stage 1) to 2.80 g/d (stage 5), high urinary loss of vitamin D-binding protein could be one of the reasons for vitamin D deficiency [39]. Since lower levels of vitamin D have been associated with poor outcomes of CKD, including an increased risk of progression and mortality, [11, 40] the management of vitamin D concentration should be of importance in the treatment of similar patients.
Except for vitamin D, the serum levels of other vitamins were all within the reference range or on the borderline. Circulating vitamin A and its metabolites are essential for cellular maintenance, gene regulation, lipid metabolism, and inflammatory response [41]. In the present study, an inverse relationship between vitamin A and eGFR (-0.21766, p < 0.0001) was identified, although the correlation was weak, which was in line with what was reported previously [41, 42]. Whether it was CKD or its related comorbidities that altered vitamin A homeostasis remains unknown [43–45]. To prevent toxicity, supplement of vitamin A is not recommended for CKD patients unless necessary [41]. It is notable that homocysteine level increased as the kidney function (eGFR) decreasing. In the meantime, the levels of vitamin B6, vitamin B9 and vitamin B12 didn’t show any association with Hcy, which was inconsistent with previous studies. As reported previously, plasma vitamin C concentration demonstrated a positive, linear relationship with eGFR in both diabetic and non-diabetic patients, suggesting renal dysfunction was associated with a decrease in plasma vitamin C level [14]. However, no correlation of vitamin C with eGFR was observed in this study.
The limitations to our research include (1) absence of data about dietary intake, enteral feeds, vitamin supplements, and medications related to bone and mineral metabolism of the patients, which made it difficult to test etiologic hypotheses. (2) The presence of a vitamin in serum may neither be able to reflect the adequacy and content at the tissue or cellular level nor the efficiency of utilization at the tissue or cellular level. Patients may exhibit functional deficiency of a vitamin despite normal serum content. (3) This was a single-center study conducted in a tertiary hospital. Multi-center studies with a large sample size, particularly if outpatients are included, should be carried out in the future to alleviate the possible biases and confounding factors.
Conclusions
To our knowledge, for the first time the status of 9 vitamins were assessed in a single center study at one time. Except for vitamin D, vitamin deficiency was not a serious problem in this cohort. Weak correlation of vitamin A or D with the severity of renal function was identified. Patients’ ages have been decreasing from those in previous reports; whether it is correlated to the elevated prevalence of comorbidities, such as hypertension and/or diabetes, requires further study.
Acknowledgements
None.
Abbreviations
- CKD
Chronic kidney disease
- eGFR
Estimated glomerular filtration rate
- CI
Confidence interval
- hHcy
Hyperhomocysteinemia
- GFR
Glomerular filtration rate
- sCr
Serum creatinine
- eGFR
Estimated glomerular filtration rate
- CKD-EPI
CKD Epidemiology Collaboration
- ALP
Alkaline phosphatase
- CHOL
Total cholesterol
- TG
Triglyceride
- HDL
High‑density lipoprotein
- LDL
Low‑density lipoprotein
- Hcy
Homocysteine
- DM
Diabetes mellitus
Authors' contributions
Y W, Y Z and XM C carried out the studies, participated in collecting data, and drafted the manuscript. P C, S L and PF H performed the statistical analysis and participated in its design. XL S and GY C participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by ethics committee of First Medical Center of Chinese People’s Liberation Army General Hospital and carried out in accordance with the declaration of Helsinki. The study is retrospective study, Informed consents were exempted.
Consent for publication
Not applicable.
Competing interests
All of the authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yong Wang and Ying Zheng are co-first authors.
References
- 1.Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, et al. Chronic kidney disease as a global public health problem: approaches and initiatives - a position statement from Kidney Disease Improving Global Outcomes. Kidney Int. 2007;72(3):247–59. doi: 10.1038/sj.ki.5002343. [DOI] [PubMed] [Google Scholar]
- 2.Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis. PLoS One. 2016;11(7):e0158765. doi: 10.1371/journal.pone.0158765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379(9818):815–22. doi: 10.1016/S0140-6736(12)60033-6. [DOI] [PubMed] [Google Scholar]
- 4.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 5.Gaitonde DY, Cook DL, Rivera IM. Chronic Kidney Disease: Detection and Evaluation. Am Fam Physician. 2017;96(12):776–83. [PubMed] [Google Scholar]
- 6.Gluba-Brzózka A, Franczyk B, Rysz J. Vegetarian Diet in Chronic Kidney Disease-A Friend or Foe. Nutrients. 2017;9:4. doi: 10.3390/nu9040374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yadav AK, Kumar V, Kumar V, Banerjee D, Gupta KL, Jha V. The Effect of Vitamin D Supplementation on Bone Metabolic Markers in Chronic Kidney Disease. J Bone Miner Res. 2018;33(3):404–9. doi: 10.1002/jbmr.3314. [DOI] [PubMed] [Google Scholar]
- 8.Duranton F, Rodriguez-Ortiz ME, Duny Y, Rodriguez M, Daurès JP, Argilés A. Vitamin D treatment and mortality in chronic kidney disease: a systematic review and meta-analysis. Am J Nephrol. 2013;37(3):239–48. doi: 10.1159/000346846. [DOI] [PubMed] [Google Scholar]
- 9.Filipov JJ, Zlatkov BK, Dimitrov EP, Svinarov D. Relationship between vitamin D status and immunosuppressive therapy in kidney transplant recipients. Biotechnol Biotechnol Equip. 2015;29(2):331–5. doi: 10.1080/13102818.2014.995415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pilz S, Iodice S, Zittermann A, Grant WB, Gandini S. Vitamin D status and mortality risk in CKD: a meta-analysis of prospective studies. Am J Kidney Dis. 2011;58(3):374–82. doi: 10.1053/j.ajkd.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 11.Mehrotra R, Kermah DA, Salusky IB, Wolf MS, Thadhani RI, Chiu YW, et al. Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Int. 2009;76(9):977–83. doi: 10.1038/ki.2009.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webster AC, Nagler EV, Morton RL, Masson P. Chronic Kidney Disease Lancet. 2017;389(10075):1238–52. doi: 10.1016/S0140-6736(16)32064-5. [DOI] [PubMed] [Google Scholar]
- 13.Franca Gois PH, Wolley M, Ranganathan D, Seguro AC. Vitamin D Deficiency in Chronic Kidney Disease: Recent Evidence and Controversies. Int J Environ Res Public Health. 2018;15:8. doi: 10.3390/ijerph15081773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takahashi N, Morimoto S, Okigaki M, Seo M, Someya K, Morita T, et al. Decreased plasma level of vitamin C in chronic kidney disease: comparison between diabetic and non-diabetic patients. Nephrol Dial Transplant. 2011;26(4):1252–7. doi: 10.1093/ndt/gfq547. [DOI] [PubMed] [Google Scholar]
- 15.Cianciolo G, De Pascalis A, Di Lullo L, Ronco C, Zannini C, La Manna G. Folic Acid and Homocysteine in Chronic Kidney Disease and Cardiovascular Disease Progression: Which Comes First? Cardiorenal Med. 2017;7(4):255–66. doi: 10.1159/000471813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nigwekar SU, Kang A, Zoungas S, Cass A, Gallagher MP, Kulshrestha S, et al. Interventions for lowering plasma homocysteine levels in dialysis patients. Cochrane Database Syst Rev. 2016(5):Cd004683. [DOI] [PMC free article] [PubMed]
- 17.Li Y, Spence JD, Wang X, Huo Y, Xu X, Qin X. Effect of Vitamin B(12) Levels on the Association Between Folic Acid Treatment and CKD Progression: A Post Hoc Analysis of a Folic Acid Interventional Trial. Am J Kidney Dis. 2020;75(3):325–32. doi: 10.1053/j.ajkd.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 18.Obi Y, Hamano T, Isaka Y. Prevalence and prognostic implications of vitamin D deficiency in chronic kidney disease. Dis Markers. 2015;2015:868961. doi: 10.1155/2015/868961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levin A, Stevens PE. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49–61. doi: 10.1038/ki.2013.444. [DOI] [PubMed] [Google Scholar]
- 20.Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–30. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 21.Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80(1):17–28. doi: 10.1038/ki.2010.483. [DOI] [PubMed] [Google Scholar]
- 22.Kellum JA, Lameire N. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1) Crit Care. 2013;17(1):204. doi: 10.1186/cc11454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. [DOI] [PMC free article] [PubMed]
- 24.Timoneda J, Rodríguez-Fernández L, Zaragozá R, Marín MP, Cabezuelo MT, Torres L, et al. Vitamin A Deficiency and the Lung. Nutrients. 2018;10:9. doi: 10.3390/nu10091132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saka Y, Naruse T, Kato A, Tawada N, Noda Y, Mimura T, et al. Thiamine status in end-stage chronic kidney disease patients: a single-center study. Int Urol Nephrol. 2018;50(10):1913–8. doi: 10.1007/s11255-018-1974-y. [DOI] [PubMed] [Google Scholar]
- 26.Chen CH, Yeh EL, Chen CC, Huang SC, Huang YC. Vitamin B-6, Independent of Homocysteine, Is a Significant Factor in Relation to Inflammatory Responses for Chronic Kidney Disease and Hemodialysis Patients. Biomed Res Int. 2017;2017:7367831. doi: 10.1155/2017/7367831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hiraoka M, Kagawa Y. Genetic polymorphisms and folate status. Congenit Anom (Kyoto) 2017;57(5):142–9. doi: 10.1111/cga.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miranti EH, Stolzenberg-Solomon R, Weinstein SJ, Selhub J, Männistö S, Taylor PR, et al. Low vitamin B(12) increases risk of gastric cancer: A prospective study of one-carbon metabolism nutrients and risk of upper gastrointestinal tract cancer. Int J Cancer. 2017;141(6):1120–9. doi: 10.1002/ijc.30809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marik PE, Liggett A. Adding an orange to the banana bag: vitamin C deficiency is common in alcohol use disorders. Crit Care. 2019;23(1):165. doi: 10.1186/s13054-019-2435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pfeiffer CM, Schleicher RL, Johnson CL, Coates PM. Assessing vitamin status in large population surveys by measuring biomarkers and dietary intake - two case studies: folate and vitamin D. Food Nutr Res. 2012;56. [DOI] [PMC free article] [PubMed]
- 31.Okebukola PO, Kansra S, Barrett J. Vitamin E supplementation in people with cystic fibrosis. Cochrane Database Syst Rev. 2017;3(3):Cd009422. doi: 10.1002/14651858.CD009422.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen J, Wildman RP, Gu D, Kusek JW, Spruill M, Reynolds K, et al. Prevalence of decreased kidney function in Chinese adults aged 35 to 74 years. Kidney Int. 2005;68(6):2837–45. doi: 10.1111/j.1523-1755.2005.00757.x. [DOI] [PubMed] [Google Scholar]
- 33.Pugh D, Gallacher PJ, Dhaun N. Management of Hypertension in Chronic Kidney Disease. Drugs. 2019;79(4):365–79. doi: 10.1007/s40265-019-1064-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Cheung AK, Rahman M, Reboussin DM, Craven TE, Greene T, Kimmel PL, et al. Effects of Intensive BP Control in CKD. J Am Soc Nephrol. 2017;28(9):2812–23. doi: 10.1681/ASN.2017020148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lessey G, Stavropoulos K, Papademetriou V. Mild to moderate chronic kidney disease and cardiovascular events in patients with type 2 diabetes mellitus. Vasc Health Risk Manag. 2019;15:365–73. doi: 10.2147/VHRM.S203925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Holick MF, Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19(2):73–8. doi: 10.1016/j.annepidem.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacob AI, Sallman A, Santiz Z, Hollis BW. Defective photoproduction of cholecalciferol in normal and uremic humans. J Nutr. 1984;114(7):1313–9. doi: 10.1093/jn/114.7.1313. [DOI] [PubMed] [Google Scholar]
- 39.Denburg MR, Bhan I. Vitamin D-Binding Protein in Health and Chronic Kidney Disease. Semin Dial. 2015;28(6):636–44. doi: 10.1111/sdi.12422. [DOI] [PubMed] [Google Scholar]
- 40.Ravani P, Malberti F, Tripepi G, Pecchini P, Cutrupi S, Pizzini P, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75(1):88–95. doi: 10.1038/ki.2008.501. [DOI] [PubMed] [Google Scholar]
- 41.Jing J, Isoherranen N, Robinson-Cohen C, Petrie I, Kestenbaum BR, Yeung CK. Chronic Kidney Disease Alters Vitamin A Homeostasis via Effects on Hepatic RBP4 Protein Expression and Metabolic Enzymes. Clin Transl Sci. 2016;9(4):207–15. doi: 10.1111/cts.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Steiber AL, Kopple JD. Vitamin status and needs for people with stages 3–5 chronic kidney disease. J Ren Nutr. 2011;21(5):355–68. doi: 10.1053/j.jrn.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 43.Barazzoni R, Zanetti M, Semolic A, Pirulli A, Cattin MR, Biolo G, et al. High plasma retinol binding protein 4 (RBP4) is associated with systemic inflammation independently of low RBP4 adipose expression and is normalized by transplantation in nonobese, nondiabetic patients with chronic kidney disease. Clin Endocrinol (Oxf) 2011;75(1):56–63. doi: 10.1111/j.1365-2265.2011.03990.x. [DOI] [PubMed] [Google Scholar]
- 44.Henze A, Frey SK, Raila J, Tepel M, Scholze A, Pfeiffer AF, et al. Evidence that kidney function but not type 2 diabetes determines retinol-binding protein 4 serum levels. Diabetes. 2008;57(12):3323–6. doi: 10.2337/db08-0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Frey SK, Nagl B, Henze A, Raila J, Schlosser B, Berg T, et al. Isoforms of retinol binding protein 4 (RBP4) are increased in chronic diseases of the kidney but not of the liver. Lipids Health Dis. 2008;7:29. doi: 10.1186/1476-511X-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.