Abstract
Background Lung ultrasound (LUS) and computed tomography (CT) can both be used for diagnosis of interstitial pneumonia caused by coronavirus disease 2019 (COVID-19), but the agreement between LUS and CT is unknown. Purpose to compare the agreement of LUS and CT in the diagnosis of interstitial pneumonia caused by COVID-19. Materials and Methods We searched PubMed, Cochrane library, Embase, Chinese Biomedicine Literature, and WHO COVID-19 databases to identify studies that compared LUS with CT in the diagnosis of interstitial pneumonia caused by COVID-19. We calculated the pooled overall, positive and negative percent agreements, diagnostic odds ratio (DOR) and the area under the standard receiver operating curve (SROC) for LUS in the diagnosis of COVID-19 compared with CT. Results We identified 1896 records, of which nine studies involving 531 patients were finally included. The pooled overall, positive and negative percentage agreements of LUS for the diagnosis of interstitial pneumonia caused by COVID-19 compared with CT were 81% (95% confidence interval [CI] 43–99%), 96% (95% CI, 80–99%, I2 = 92.15%) and 80% (95%CI, 60–92%, I2 = 92.85%), respectively. DOR was 37.41 (95% CI, 9.43–148.49, I2 = 63.9%), and the area under the SROC curve was 0.94 (95% CI, 0.92–0.96). The quality of evidence for both specificity and sensitivity was low because of heterogeneity and risk of bias. Conclusion The level of diagnostic agreement between LUS and CT in the diagnosis of interstitial pneumonia caused by COVID-19 is high. LUS can be therefore considered as an equally accurate alternative for CT in situations where molecular tests are not available.
Keywords: COVID-19, systematic review, POCUS, lung ultrasound, computed tomography
1. Background
During the first year of the pandemic, Coronavirus Disease 2019 (COVID-19) has caused substantial harm in all aspects of life and a great loss of human, material, and financial resources. Diagnosis is a critical step for the treatment and prognosis of COVID-19. Currently, the reverse-transcriptase polymerase chain reaction (RT-PCR) for viral load is considered as the gold standard in the diagnosis of COVID-19 [1]. However, receiving the results of RT-PCR can take at least several hours, and in some circumstances, particularly in emergency situations, more rapid diagnostic methods are needed. Other common diagnostic methods for COVID-19 include chest computed tomography (CT), X-ray. Each of these methods has advantages in some aspects in the detection of COVID-19. However, one single study has shown that all of them have a low specificity compared with RT-PCR in diagnosing COVID-19 [2]. The use of imaging for patients with acute or severe COVID-19 is also inconvenient for the patients.
Lung ultrasound (LUS) refers to the application of ultrasound technology in the diagnosis and screening of respiratory diseases. LUS can be used to evaluate pleural abnormalities, to guide thoracentesis and related procedures, and to improve the accuracy and safety of identifying pleural disease and performing transpleural access-related procedures [3]. Compared to traditional pleural radiography, LUS has a multitude of advantages: it is radiation-free, uses portable equipment, the imaging is real-time and can be displayed dynamically [4]. Point-of-care ultrasonography (POCUS), a LUS tool widely used in emergency and critical care departments, is particularly practical as it can be used at the patient’s bedside, saving time and capacity. LUS and CT can both be used for diagnosis, assessment of disease severity, and evaluation of prognosis of interstitial pneumonia caused by COVID-19. In this systematic review, we aim to comprehensively identify the diagnostic agreement between LUS and CT in the diagnosis of interstitial pneumonia caused by COVID-19. We present this article in accordance with the PRISMA-DTA statement [5].
2. Methods
We have registered this systematic review at OSF REGISTRIES and the registration DOI is 10.17605/OSF.IO/ZY7FU.
2.1. Inclusion and Exclusion Criteria
2.1.1. Inclusion Criteria
We limited the search to studies that compared LUS with CT in the diagnosis of interstitial pneumonia caused by COVID-19. We included peer-reviewed papers published in English or Chinese that met the following conditions: (1) participants were patients with confirmed or suspected COVID-19 or asymptomatic SARS-CoV-2 infection; (2) the diagnostic method was ultrasound diagnosis (including POCUS) in the intervention group, and CT in the control group; and (3) a two-by-two contingency table comparing the diagnosis results with LUS and CT could be calculated.
2.1.2. Exclusion Criteria
We excluded narrative reviews, letters, and conference abstracts; duplicate publications; studies with insufficient data; and studies from which data could not be extracted.
2.2. Search Strategy
We systematically searched Medline, Embase, The Cochrane Library, Chinese Biomedicine Literature, and WHO COVID-19 database from 1 January 2020 to 15 January 2021 to identify studies on the use of LUS in the diagnosis of COVID-19. We used the following search strategy, adapted for the requirements of each database if necessary: (“COVID-19” OR “2019-nCov” OR “SARS-CoV-2”) AND (“ultrasonography” OR “ultrasound” OR “echography” OR “ultrasonics” OR “ultrasonic diagnosis” OR “ultrasonic echo” OR “ultrasonic examination” OR “ultrasonic scanning”). We also searched the reference lists of the identified articles to find additional studies. The details of the search strategy are shown in Supplementary Material 1.
2.3. Article Selection and Data Extraction
Two reviewers first screened all titles and abstracts, and then the full texts of articles deemed potentially eligible, independently according to the inclusion and exclusion criteria. Disagreements were solved by consensus or consultation with a third reviewer. The following information was extracted: (1) basic information (the first author, publication date, country or region of participants, and sample size), (2) patient information (age, gender, enrollment time of patients, setting where the study was conducted), and (3) the values of the two-by-two contingency table comparing the diagnostic outcomes with LUS and CT. If the contingency table could not be extracted from the article, we contacted the corresponding author for the information. If we could not retrieve the necessary data despite contacting the authors, the article was excluded.
2.4. Assessment of Risk of Bias and Quality of Evidence
Two investigators used the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool to assess the risk of bias in the included studies independently [6]. The QUADAS-2 tool covers both risk of bias and applicability. The risk of bias section consists of four domains (patient selection, index test, reference standard, and flow and timing) and the applicability section of three domains (patient selection, index test, and reference standard). The risk of bias or concerns in applicability in each domain are rated as either “low”, “high”, or “unclear”. Review Manager (RevMan) Version 5.4. (The Cochrane Collaboration, 2020) was used to present the results. In case of disagreement consensus was reached by discussion or consultation with a third researcher.
The quality of evidence was evaluated using the GRADE approach. For outcomes on diagnostic accuracy, the assessment starts by assuming high quality of evidence, which is then downgraded according to the risk of bias, indirectness, inconsistency, impreciseness, and publication bias, and upgraded for dose-response effect, large residual effects, and lack of bias and confounding [7].
2.5. Statistical Analysis
We calculated the pooled overall percent agreement, positive percent agreement, and negative percent agreement comparing LUS in the diagnosis of COVID-19 with CT as the reference. The overall percent agreement is the proportion of all test results that were in agreement with the two methods. The positive and negative percent agreements are equivalent to sensitivity and specificity, respectively, in situations where the reference is not necessarily the gold standard. The I2 statistics and Q test were used to measure and interpret the heterogeneity. Meta-analysis was performed after we had confirmed that there was no statistical heterogeneity. We used either the fixed or randomized effect model according to the guidance in the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy. We also calculated the diagnostic odds ratio (DOR) and area under the summary receiver operating characteristic (SROC) curve assuming CT as the reference standard. The analyses were performed in STATA 14 (Stata/MP 14.0 for Mac (64-bit Intel), Revision 22 April 2015, Copyright 1985–2015 StataCorp LP) software. The significance level of the meta-analysis was set at α = 0.05.
3. Results
3.1. Literature Selection Process
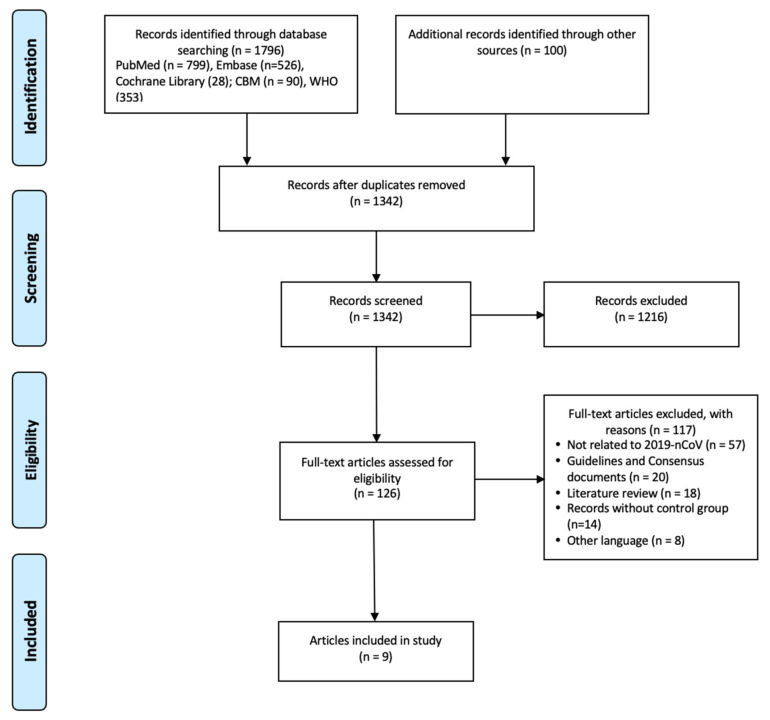
A total of 1896 documents were retrieved. After reading the titles, abstracts, and full text of the documents, nine articles were included in the analysis [8,9,10,11,12,13,14,15,16] (Figure 1).
Figure 1.
Flowchart of the literature search and screen.
3.2. Characteristics of the Included Studies
A total of nine studies involving 531 patients were included, of which, three studies were from Turkey, and one each from the United States, Germany, Spain, Belgium, Italy, and China (Table 1). The study subjects included in the study were recruited between February and May of 2020 with sample sizes ranging from nine to 131. Four studies contained patients suspected for COVID-19, four contained patients with confirmed case of COVID-19, and one contained asymptomatic patients suspected to be infected with SARS-CoV-2. Only one study reported that they used high-resolution CT.
Table 1.
Characteristics of the included studies.
| Research ID | Journals | Country/Area | Publication Date | Patients | Female, N (%) | Age (year) | Patients Enrolled Time | Setting | Sample Size | Ultrasound | CT | TP | FP | FN | TN |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Şan et al. [8] | Notfall and Rettungsmedizin | Turkey | 2 December 2020 | Confirmed COVID-19 | 20 (50.0%) | Mean ± SD 43.8 ± 16.6 | 1–30 April 2020 | ED | 40 | LUS | CT | 20 | 3 | 12 | 5 |
| Schmid et al. [9] | BMC Emergency Medicine | Germany | 7 December 2020 | Suspected COVID-19 | NA | NA | 1–25 April 2020 | ED | 31 | LUS | CT | 13 | 3 | 7 | 8 |
| Karagöz et al. [10] | Ultrasound Quarterly | Turkey | 1 December 2020 | Suspected COVID-19 | 31 (43.0%) | Mean 51 (range 20–96) | 1–15 April 2020 | ED | 72 | BLUS | CT | 32 | 3 | 1 | 36 |
| Hizal et al. [11] | Pediatr Pulmonol | Turkey | 21 October 2020 | Confirmed COVID-19 | NA | Children | April–May 2020 | Hospital | 30 | LUS | CT | 11 | 1 | 2 | 16 |
| Chen et al. [12] | Ultrasound Med Biol | Spain | 13 July 2020 | Confirmed COVID-19 | 23 (45.1%) | Mean ± SD 61.4 ± 17.7 | March–April 2020 | ED | 51 | LUS | CT | 37 | 3 | 0 | 11 |
| Narinx et al. [13] | Emergency Radiology | Belgium | 10 September 2020 | Suspected COVID-19 | 49 (54.4%) | Mean ± SD 50.4 ± 16.3 | 28 March–20 April 2020 | ED | 90 | POCUS | CT | 22 | 51 | 0 | 17 |
| Dacrema et al. [14] | Internal and Emergency Medicine | Italy | 11 January 2021 | Suspected COVID-19 | 32 (24.4%) | Mean ± SD 64.3 ± 14.3 | 21 February–15 March 2020 | ED | 131 | LUS | HRCT | 129 | 0 | 1 | 1 |
| Walsh et al. [15] | Western Journal of Emergency Medicine | USA | 28 September 2020 | COVID-19 | NA | ≥14 | 4 March–19 May 2020 | ED | 77 | LUS | CT | 12 | 13 | 0 | 52 |
| Lin et al. [16] | Advanced Ultrasound in Diagnosis and Therapy | China | 6 September 2020 | Asymptomatic SARS-CoV-2 infected patients | 4 (44.4%) | Mean ± SD 34.0 ± 17.9 | 22–23 February 2020 | Hospital | 9 | LUS | CT | 2 | 0 | 1 | 6 |
LUS: Lung Ultrasound; CT: Computed Tomography; HRCT: High-resolution Computed Tomography; POCUS: Point-of-care Ultrasonography; BLUS: Bedside Lung Ultrasound; ED: Emergency Department.
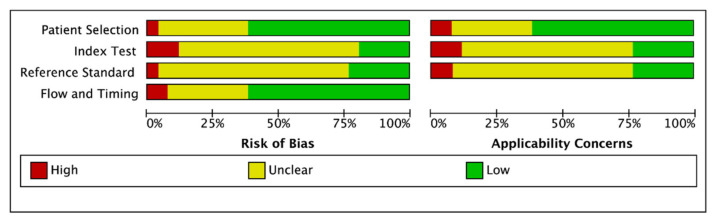
3.3. Risk of Bias in the Included Studies
The results of risk of bias in the included studies are shown in detail in Figure 2. Four studies had a high or unclear risk of bias in patient selection, four studies in flow and timing, seven studies in reference standard, and seven studies in index test.
Figure 2.
The risk of bias in the included studies.
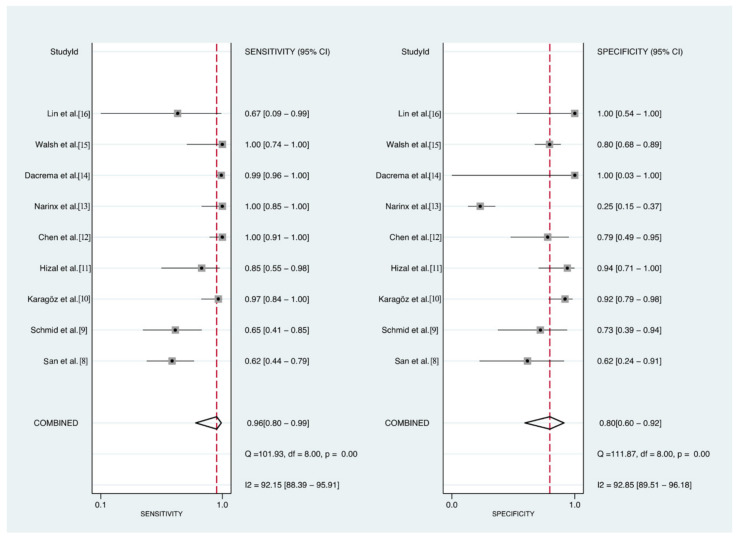
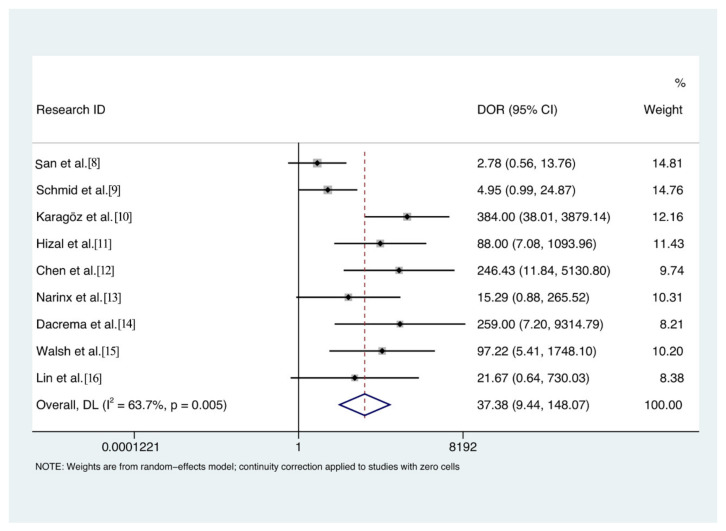
3.4. Agreement of LUS for the Diagnosis of COVID-19
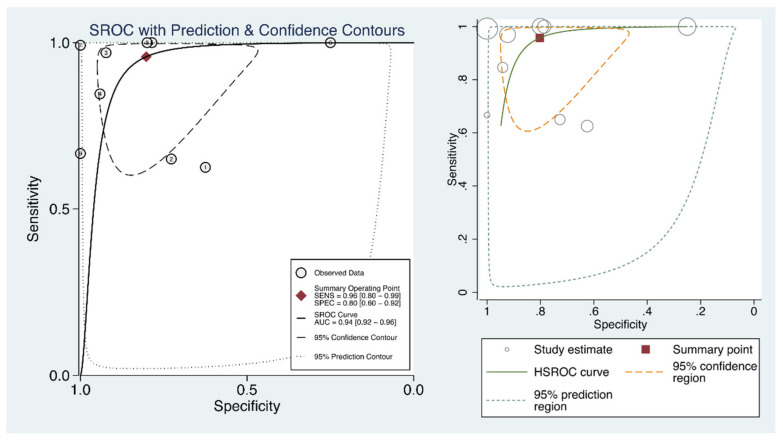
The pooled overall percent agreement was 81% (95% confidence interval [CI], 43–99%), positive percent agreement 96% (95% CI, 80–99%, I2 = 92.15%), and negative percent agreement 80% (95%CI, 60–92%, I2 = 92.85%) (Figure 3). The DOR was 37.4 (95% CI, 9.4–148.5, I2 = 63.9%) (Figure 4), and the area under the SROC curve 0.94 (95% CI, 0.92–0.96) (Figure 5). The quality of evidence for both positive and negative percent agreement was low because of heterogeneity and risk of bias.
Figure 3.
Positive (left panel) and negative (right panel) percent agreement of lung ultrasound for the diagnosis of interstitial pneumonia caused by COVID-19.
Figure 4.
Diagnostic odds ratio of lung ultrasound for the diagnosis of interstitial pneumonia caused by COVID-19.
Figure 5.
The summary receiver operating characteristic curve of lung ultrasound for the diagnosis of interstitial pneumonia caused by COVID-19.
4. Discussion
4.1. Principal Findings
Our study identified nine studies comparing LUS with CT for the diagnosis of interstitial pneumonia caused by COVID-19 [8,9,10,11,12,13,14,15,16]. In four out of five cases the diagnoses done by LUS and CT were in agreement. In particular, LUS was able to detect COVID-19 in 96% of patients who were diagnosed positive with CT. The quality of evidence was however low. LUS and CT therefore have comparable reliability in diagnosing COVID-19 in patients at emergency departments.
Ultrasound can yield high resolution images of anatomical structures quickly and in a timely manner. It can also be applied to the examination of lungs, stomach, and other chest structures and to rapidly diagnosis or confirmation of the cause of hemodynamic instability [17]. As early as during the pandemic of influenza A in 2003, LUS was shown to yield results comparable with chest imaging tools for the early diagnosis of H1N1 at the emergency department.
In diagnosing pulmonary diseases or disorders, such as pneumothorax, pleural effusion, pneumonia, chronic obstructive pulmonary disease/asthma, pulmonary edema, and acute respiratory distress syndrome (ARDS), the sensitivity and specificity of LUS have been shown to be higher than those of CT [18]. In patients with ARDS, the capabilities of chest X-ray and LUS in identifying patients at high risk of death have been shown to be equivalent [19]. LUS has been commonly used in the diagnosis of acute respiratory failure as a basic tool that can help improve the diagnosis in intensive care setting. When combined with standard diagnostic methods, LUS can expedite the management of emergency care.
POCUS is one of the more common types of ultrasound, a compact equipment that can be used at the patient’s bedside for diagnostic or adjunctive confirmation of diseases [20]. POCUS is currently attracting a lot of attention in intensive care units (ICU) due to its many advantages. POCUS allows to delay or even avoid the need of transfer to the radiology department, and prevent exposure to radiation [21]. POCUS can also guide life-saving therapies in extreme emergencies. POCUS has a sensitivity of 85% (95%CI 84–87%) and specificity of 93% (95%CI 92–95%) for pneumonia, showing it is an accurate tool for the diagnosis of pneumonia [22]. In health care settings with limited medical resources and in primary care facilities, POCUS is feasible for detecting pulmonary manifestations of malaria and sepsis [23]. In addition, POCUS has been shown to have advantages and be effective in the diagnosis and evaluation of patients in the perioperative period in the emergency departments [24]. POCUS has also been used in emergency departments for rapid assessment of the patient’s lungs and chest [25]. Therefore, POCUS is an important diagnostic tool for pneumonia due to its simplicity, accessibility, low cost, and lack of radiological hazards.
LUS had been used for the diagnosis of lung disease for a long time. Early in the COVID-19 outbreak, LUS was found to show specific findings in patients with COVID-19: irregular pleural lines on the anterior and posterior thorax bilaterally, small subpleural consolidations, white areas and thick, confluent and irregular vertical artifacts (B lines), and the presence of stripped areas bilaterally, mixed with pathologic areas. This evidence suggested that LUS could be used to diagnose and evaluate COVID-19 [26]. As COVID-19 spread across the world, the use of ultrasound became widespread and is now recommended by several national and international guidelines. For example, the WHO guidelines suggest that ultrasound can be used as a complementary alternative method for diagnostic evaluation in pregnant women and children with infection prevention and control measures [27,28]. The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) updated their guidelines stating that ultrasound can be performed to examine the fetuses and pregnant women for the diagnosis and evaluation of COVID-19 with proper protection.
4.2. Strengths and Limitation
A total of 14 reviews or protocols assessing the use of LUS for the diagnosis of COVID-19 have been published prior to our study, including 12 narrative reviews [29,30,31,32,33,34,35,36,37,38,39,40], one systematic review and meta-analysis [41], and one systematic review proposal [42]. The narrative reviews analyzed the role of LUS in COVID-19 from different perspectives. However, most of the reviews did not search the literature systematically or analyze the risk of bias. The conclusions of the only systematic review so far were similar to ours [41], but our search covering five databases was broader and could thus include more studies and patients, strengthening the evidence.
Our study has also some limitations. We did not include preprints because we decided to restrict the review to peer-reviewed studies to assure high quality of the meta-analysis. In addition, we did not perform subgroup analyses because the differences in patient characteristics between the studies were minor. For the scoring of LUS, we did not calculate the scores of COVID-19 because of the different scoring systems. Finally, the overall quality of the included studies was low.
5. Conclusions
The diagnostic agreement between LUS and CT in the diagnosis of interstitial pneumonia caused by COVID-19 is high. LUS can be therefore considered as an equally accurate alternative for CT in situations where molecular tests are not available. Particularly when performed with a point-of-care portable tool, LUS has great potential to support the diagnosis and evaluation of patients with COVID-19 in emergency or intensive care setting due to its simplicity, accessibility, low cost, and safety.
Acknowledgments
I would like to declare on behalf of my co-authors of this manuscript and the working group members participating in this research that our work described is original that has not been published previously, and not under consideration for publication elsewhere, in whole or in part.
Abbreviations
COVID-19 = coronavirus disease 2019, LUS = Lung Ultrasound, CT = Computed Tomography, HRCT = High-resolution Computed Tomography, POCUS = Point-of-care Ultrasonography, ED = Emergency Department.
Supplementary Materials
The following supplementary materials are available online at https://www.mdpi.com/article/10.3390/diagnostics11081351/s1.
Author Contributions
Conceptualization, literature retrieval, screening and data extraction, M.W., X.L., L.W. and J.T.; quality assessment, M.W., M.L. and Y.Z.; writing—original draft preparation, M.W. and X.L.; writing—review and editing, J.E., Q.W., X.X., Y.S., M.S.L., H.S.A., J.L. and J.T.; supervision, J.L. and J.T.; project administration, J.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Goudouris E.S. Laboratory diagnosis of COVID-19. J. Pediatr. 2021;97:7–12. doi: 10.1016/j.jped.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duarte M.L., Dos Santos L.R., Contenças A.C.D.S., Iared W., Peccin M.S., Atallah N. Reverse-transcriptase polymerase chain reaction versus chest computed tomography for detecting early symptoms of COVID-19. A diagnostic accuracy systematic review and meta-analysis. Sao Paulo Med. J. 2020;138:422–432. doi: 10.1590/1516-3180.2020.034306072020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soni N.J., Franco R., Velez M.I., Schnobrich D., Dancel R., Restrepo M.I., Mayo P.H. Ultrasound in the diagnosis and management of pleural effusions. J. Hosp. Med. 2015;10:811–816. doi: 10.1002/jhm.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bitar Z.I., Maadarani O.S., El-Shably A.M., Al-Ajmi M.J. Diagnostic accuracy of chest ultrasound in patients with pneumonia in the intensive care unit: A single-hospital study. Heal. Sci. Rep. 2018;2:e102. doi: 10.1002/hsr2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McInnes M.D., Moher D., Thombs B.D., McGrath T.A., Bossuyt P.M., Clifford T., Cohen J.F., Deeks J.J., Gatsonis C., Hooft L., et al. Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA. 2018;319:388396. doi: 10.1001/jama.2017.19163. [DOI] [PubMed] [Google Scholar]
- 6.Whiting P.F., Rutjes A.W., Westwood M.E., Mallett S., Deeks J.J., Reitsma J.B., Leeflang M.M., Sterne J.A., Bossuyt P.M. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 7.Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P., Schünemann H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Şan İ., Bekgöz B., Usul E., Yıldırım Ç., Gemcioğlu E., Kahraman A.F., Ay A.E. Role of lung ultrasonography in the diagnosis of COVID-19 patients admitted to the emergency department. Notf. Rett. 2020;2:1–6. doi: 10.1007/s10049-020-00807-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmid B., Feuerstein D., Lang C.N., Fink K., Steger R., Rieder M., Duerschmied D., Busch H.J., Damjanovic D. Lung ultrasound in the emergency department-a valuable tool in the management of patients presenting with respiratory symptoms during the SARS-CoV-2 pandemic. BMC Emerg. Med. 2020;20:1–7. doi: 10.1186/s12873-020-00389-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karagöz A., Sağlam C., Demirbaş H.B., Korkut S., Ünlüer E.E. Accuracy of Bedside Lung Ultrasound as a Rapid Triage Tool for Suspected Covid-19 Cases. Ultrasound Q. 2020;36:339–344. doi: 10.1097/RUQ.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 11.Hizal M., Aykac K., Yayla B.C.C., Yilmaz A., Altun D., Akkaya H.E., Bayhan G.I., Kurt A.N.C., Karakaya J., Ozsurekci Y., et al. Diagnostic value of lung ultrasonography in children with COVID-19. Pediatr. Pulmonol. 2020;56:1018–1025. doi: 10.1002/ppul.25127. [DOI] [PubMed] [Google Scholar]
- 12.Tung-Chen Y., de Gracia M.M., Díez-Tascón A., Alonso-González R., Agudo-Fernández S., Parra M., Ossaba-Vélez S., Rodríguez-Fuertes P., Llamas-Fuentes R. Correlation between Chest Computed Tomography and Lung Ultrasonography in Patients with Coronavirus Disease 2019 (COVID-19) Ultrasound Med. Biol. 2020;46:2918–2926. doi: 10.1016/j.ultrasmedbio.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Narinx N., Smismans A., Symons R., Frans J., Demeyere A., Gillis M. Feasibility of using point-of-care lung ultrasound for early triage of COVID-19 patients in the emergency room. Emerg. Radiol. 2020;27:663–670. doi: 10.1007/s10140-020-01849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DaCrema A., Silva M., Rovero L., Vertemati V., Losi G., Piepoli M.F., Sacchi R., Mangiacotti M., Nazerian P., Pagani L., et al. A simple lung ultrasound protocol for the screening of COVID-19 pneumonia in the emergency department. Intern. Emerg. Med. 2021;19:1–9. doi: 10.1007/s11739-020-02596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh P., Hankins A., Bang H. Point-of-care Lung Ultrasound Is Useful to Evaluate Emergency Department Patients for COVID-19. West. J. Emerg. Med. 2020;21:24–31. doi: 10.5811/westjem.2020.8.49205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin H., Zhang B., Kou H., Zhao Y., Li K., Wu D., Ren L., Chen Z., Shan X., Huang Y., et al. Application Value of Lung Ultrasound in Asymptomatic Patients with Confirmed COVID-19. Adv. Ultrasound Diagn. Ther. 2020;4:67–72. doi: 10.37015/audt.2020.200025. [DOI] [Google Scholar]
- 17.Testa A., Soldati G., Copetti R., Giannuzzi R., Portale G., Gentiloni-Silveri N. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit. Care. 2012;16:R30. doi: 10.1186/cc11201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baston C., West T.E. Lung ultrasound in acute respiratory distress syndrome and beyond. J. Thorac. Dis. 2016;8:E1763–E1766. doi: 10.21037/jtd.2016.12.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.See K.C., Ong V., Tan Y.L., Sahagun J., Taculod J. Chest radiography versus lung ultrasound for identification of acute respiratory distress syndrome: A retrospective observational study. Crit. Care. 2018;22:1–9. doi: 10.1186/s13054-018-2105-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramsingh D., Bronshteyn Y.S., Haskins S., Zimmerman J. Perioperative Point-of-Care Ultrasound: From Concept to Application. Anesthesiology. 2020;132:908. doi: 10.1097/ALN.0000000000003113. [DOI] [PubMed] [Google Scholar]
- 21.Zompatori M., Ciccarese F., Fasano L. Overview of current lung imaging in acute respiratory distress syndrome. Eur. Respir. Rev. 2014;23:519–530. doi: 10.1183/09059180.00001314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alzahrani S.A., Al-Salamah M.A., Al-Madani W.H., Elbarbary M.A. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit. Ultrasound J. 2017;9:1–11. doi: 10.1186/s13089-017-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leopold S.J., Ghose A., Plewes K.A., Mazumder S., Pisani L., Kingston H.W., Paul S., Barua A., Sattar M.A., Huson M.A., et al. Point-of-care lung ultrasound for the detection of pulmonary manifestations of malaria and sepsis: An observational study. PLoS ONE. 2018;13:e0204832. doi: 10.1371/journal.pone.0204832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bainbridge D., McConnell B., Royse C. A review of diagnostic accuracy and clinical impact from the focused use of perioperative ultrasound. Can. J. Anesth. 2018;65:371–380. doi: 10.1007/s12630-018-1067-5. [DOI] [PubMed] [Google Scholar]
- 25.Choi W.J., Ha Y.R., Oh J.H., Cho Y.S., Lee W.W., Sohn Y.D., Cho G.C., Koh C.Y., Do H.H., Jeong W.J., et al. Clinical guidance for point-of-care ultrasound in the emergency and critical care areas after implementing insurance coverage in Korea. J. Korean Med. Sci. 2020;35:7. doi: 10.3346/jkms.2020.35.e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buonsenso D., Piano A., Raffaelli F., Bonadia N., Donati K.D.G., Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: A case report and potential applications during COVID-19 outbreak. J. Ultrasound Med. 2020;24:2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- 27.Akl E.A., Blažić I., Yaacoub S., Frija G., Chou R., Appiah J.A., Fatehi M., Flor N., Hitti E., Jafri H., et al. Use of chest imaging in the diagnosis and management of COVID-19: A WHO rapid advice guide. Radiology. 2020;298:E63–E69. doi: 10.1148/radiol.2020203173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buerke M., Gasser A., Suhai T. Medizinische Klinik–Intensivmedizin und Notfallmedizin. Med. Klin. Intensivmed. Notf. 2011;106:5. doi: 10.1007/s00063-011-0002-0. [DOI] [PubMed] [Google Scholar]
- 29.Smith M.J., Hayward S.A., Innes S.M., Miller A.S. Point-of-care lung ultrasound in patients with COVID-19–a narrative review. Anaesthesia. 2020;75:1096–1104. doi: 10.1111/anae.15082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Convissar D.L., Gibson L.E., Berra L., Bittner E.A., Chang M.G. Narrative Review Article: Application of Lung Ultrasound During the COVID-19 Pandemic: A Narrative Review. Anesth. Analg. 2020;131:345. doi: 10.1213/ANE.0000000000004929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gutiérrez V.F., Azcárate J.A., Torres D.P., Zapata L., Yakushev A.R., Calvo A.O. Ultrasound in the management of the critically ill patient with SARS-CoV-2 infection (COVID-19): Narrative review. Med. Intensiva. 2020;2:11. doi: 10.1016/j.medin.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vetrugno L., Baciarello M., Bignami E., Bonetti A., Saturno F., Orso D., Girometti R., Cereser L., Bove T. The “pandemic” increase in lung ultrasound use in response to Covid-19: Can we complement computed tomography findings? A narrative review. Ultrasound J. 2020;12:1–11. doi: 10.1186/s13089-020-00185-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Youssef A., Cavalera M., Azzarone C., Serra C., Brunelli E., Casadio P., Pilu G. The use of lung ultrasound during the COVID-19 pandemic: A narrative review with specific focus on its role in pregnancy. J. Popul. Ther. Clin. Pharmacol. 2020;27:e64–e75. doi: 10.15586/jptcp.v27iSP1.743. [DOI] [PubMed] [Google Scholar]
- 34.Kharasch S., Duggan N.M., Cohen A.R., Shokoohi H. Lung Ultrasound in Children with Respiratory Tract Infections: Viral, Bacterial or COVID-19? A Narrative Review. Open Access Emerg. Med. 2020;12:275. doi: 10.2147/OAEM.S238702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gandhi D., Jain N., Khanna K., Li S., Patel L., Gupta N. Current role of imaging in COVID-19 infection with recent recommendations of point of care ultrasound in the contagion: A narrative review. Ann. Transl. Med. 2020;8:1094. doi: 10.21037/atm-20-3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gandhi D., Ahuja K., Grover H., Sharma P., Solanki S., Gupta N., Patel L. Review of X-ray and computed tomography scan findings with a promising role of point of care ultrasound in COVID-19 pandemic. World J. Radiol. 2020;12:195–203. doi: 10.4329/wjr.v12.i9.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Szabó I.A., Ágoston G., Varga A., Cotoi O.S., Frigy A. Pathophysiological background and clinical practice of lung ultrasound in COVID-19 patients: A short review. Anatol. J. Cardiol. 2020;24:76. doi: 10.14744/AnatolJCardiol.2020.33645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pata D., Valentini P., De Rose C., De Santis R., Morello R., Buonsenso D. Chest Computed Tomography and Lung Ultrasound Findings in COVID-19 Pneumonia: A Pocket Review for Non-radiologists. Front. Med. 2020;7:375. doi: 10.3389/fmed.2020.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Buda N., Segura-Grau E., Cylwik J., Wełnicki M. Lung ultrasound in the diagnosis of COVID-19 infection-A case series and review of the literature. Adv. Med. Sci. 2020;65:378–385. doi: 10.1016/j.advms.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sultan L.R., Sehgal C.M. A review of early experience in lung ultrasound in the diagnosis and management of COVID-19. Ultrasound Med. Biol. 2020;46:2530–2545. doi: 10.1016/j.ultrasmedbio.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mohamed M.F., Al-Shokri S., Yousaf Z., Danjuma M., Parambil J., Mohamed S., Mubasher M., Dauleh M.M., Hasanain B., AlKahlout M.A., et al. Frequency of abnormalities detected by point-of-care lung ultrasound in symptomatic COVID-19 patients: Systematic review and meta-analysis. Am. J. Trop. Med. Hyg. 2020;103:815–821. doi: 10.4269/ajtmh.20-0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang Y., Zhang D., Zhou C., Huang H., Wang R. Value of lung ultrasound for the diagnosis of COVID-19 pneumonia: A protocol for a systematic review and meta-analysis. BMJ Open. 2020;10:e039180. doi: 10.1136/bmjopen-2020-039180. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.