Abstract
Introduction
Knee Osteoarthritis (OA) is a degenerative joint disease that needs consistent exercise and an accurate understanding of the condition for long-term maintenance. While the accessibility of outpatient care is essential for disease management, many patients lack the resources to receive adequate healthcare. To address this challenge, we developed a not-for-profit interactive mobile application that provides a disease-specific educational background and a structured exercise regimen to patients.
Material and methods
“Rak Kao” (English translation: Love-Your-Knee) mobile application was designed to analyze the questionnaire data to assess the stage of knee OA and generate a personalized recommendation of treatment and exercise type using rule-based and Artificial Intelligence (AI) techniques. A single-blinded study was conducted with patients (n = 82) who were randomly assigned to the mobile application group (M-group) and the handout group (H-group). Patient groups were controlled for age, gender, BMI, onset of pain, grade of disease, education level, and occupation. Accuracy in performance of three prescribed knee exercises (catch-bend-down, stretch-touch-feet, and sit-stretch-hold) was evaluated. Clinical outcomes were evaluated before and after the 4-weeks program to assess the range of motion, symptoms, pain, physical activity, and quality of life via the KOOS and KSS scores.
Results
Completion of the study led to significantly more overall exercise accuracy in the M-group (76.2%) than the H-group (52.5%). Activities of daily life, quality of life, ability to do sports and recreational activities were significantly more improved in the M-group than the H-group (p < .01). No difference in the range of motion between groups. Satisfaction of patients’ experience was higher in the M-group than the H-group (p = .001) after the 4-week regimen.
Conclusions
With the better accuracy and outcomes for rehabilitation in the M-group than the H-group, we strongly recommend using our mobile application as a better alternative than handouts for exercises and information for patients with knee OA.
Trial registration
ClinicalTrials.gov: NCT03666585
Keywords: Knee osteoarthritis, Mobile application, Smartphone application, Knee exercises, Rehabilitation
Introduction
Knee osteoarthritis (OA) is a degenerative joint disorder that affects approximately 16% of adults, globally [1]. OA is characterized by the progressive degradation of cartilage in joints and causes pain and reduces joint mobility [2]. Currently, curative options for OA are surgical joint replacement and pharmacological treatment. Exercise and physical therapy are critical for disease management [3, 4]. However, most patients lack access to instruction or the motivation to adhere to an exercise regimen [5, 6]. Accordingly, there is an unmet need to develop a cost-effective strategy to mitigate disease progression that is accessible to most patients.
As mobile platforms have become increasingly accessible, the development of mobile applications (apps) has leveraged powerful computation, usability, and portability. This consistent innovation presents mobile apps as a powerful vehicle for health solutions. Currently, approximately 20 health apps per year are evaluated for US Food and Drug Administration approval [7]. The continual innovation of health apps offers a broad range of tools to the user, such as disease tracking, treatment options, relevant medical information, and consistent encouragement [8–10]. In the context of physical therapy for OA, the use of a mobile app has been shown to improve pain control and decrease opiate usage for patients in the postoperative setting [11]. Moreover, the ongoing COVID-19 pandemic has severely limited options for face-to-face training sessions with a therapist, negatively impacting the outcomes of patient rehabilitation [6, 12, 13]. Mobile apps have the potential to personalize educational programs and to monitor the patient's progress while still adhering to social-distancing restrictions. Therefore, we have developed “Rak Kao” (English translation: love your knee) as user-friendly health, not-for-profit mobile app to overcome some of these barriers [14].
The primary aim of this study was to evaluate if the use of this mobile app could improve the accuracy of rehabilitation of knee OA patients, compared to conventional educational handouts. The second aim was to compare the clinical outcomes between mobile app use and conventional educational handouts use in knee OA patients.
Materials and methods
App design and development
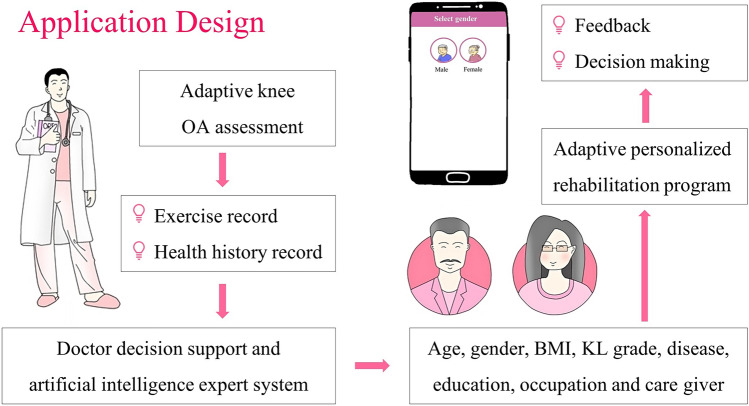
This mobile app was a collaboration between OA professionals and computer researchers. The app features four principles of knee OA in separate modules: (1) basic knowledge of the disease and symptoms, (2) available treatment options, (3) personalized assessment of the stage of severity, and (4) appropriate exercise instructions (Fig. 1). The education and disease assessment portions of the mobile app were designed to include important facts and common questions from the patients. One of the integral modules offers an adaptive test to assess patient symptoms from the questionnaire results. For instance, an adaptive knee OA assessment in module 3 evaluates the patient’s disease stage, ranging from mild to severe, according to the results of decision tree classification (Fig. 2).
Fig. 1.
Overview of mobile application design and criteria that serves OA patients
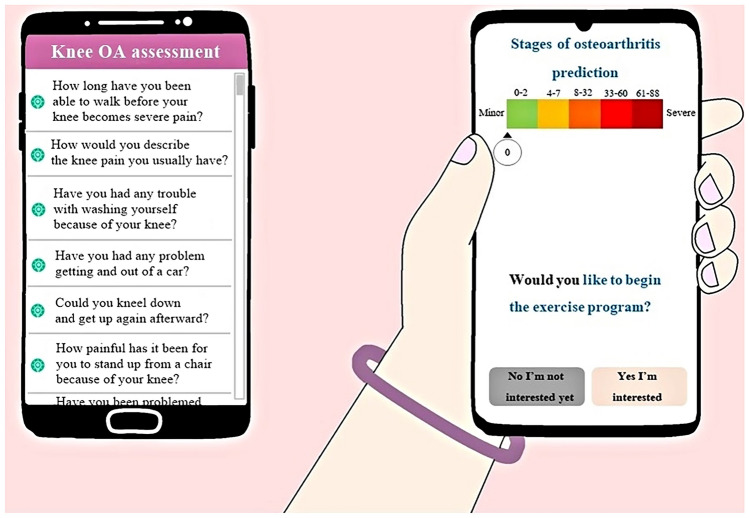
Fig. 2.
“Love your knee” app modules for education and assessment for the stage of disease
Adaptive knee osteoarthritis assessment
To assess the stage of OA, Love-Your-Knee uses an adaptive assessment, based on decision tree, to determine the disease stage. Once the disease stage is determined, the system recommends the appropriate exercise types and the number of sets as well as provides the basic knowledge for OA symptom management. With its ability to facilitate the information exchange between the patient and the doctor, the app can be effectively utilized as a personalized solution for assessing the stage of knee OA, monitoring disease progression, and promoting physical therapy and rehabilitation exercise.
Study design
This prospective single-blind randomized controlled trial (RCT) was approved by the institutional review board committee at our institution (COA034/2561), registered at clinicaltrials.gov (NCT03666585), and conducted between September 2018 and June 2019. Informed consent was obtained from all patients prior to participation. Participants were not given compensation nor were there any competing interests on behalf of the study investigators. A patent application of this mobile app was filed in our country under No. 1801005898. Data from this study are available upon reasonable request.
Patient inclusion criteria
Patients who were included in this study ranged from 40–80 years old and diagnosed with either unilateral or bilateral primary knee OA according to the American College of Rheumatology (ACR) criteria [15]. Additionally, the patients must own and be able to use smartphones with an Android operating system. Patients were excluded if they have had knee replacement surgery, if they had significant medical comorbidities that interfere with the rehabilitation exercise (previous stroke, cardiac diseases, severe hypertension, severe obesity, chronic obstructive pulmonary disease, low back pain, chronic pain, depression, and visual or hearing impairments), or if they have been instructed to our particular exercises prior to the study recruitment period.
Randomization
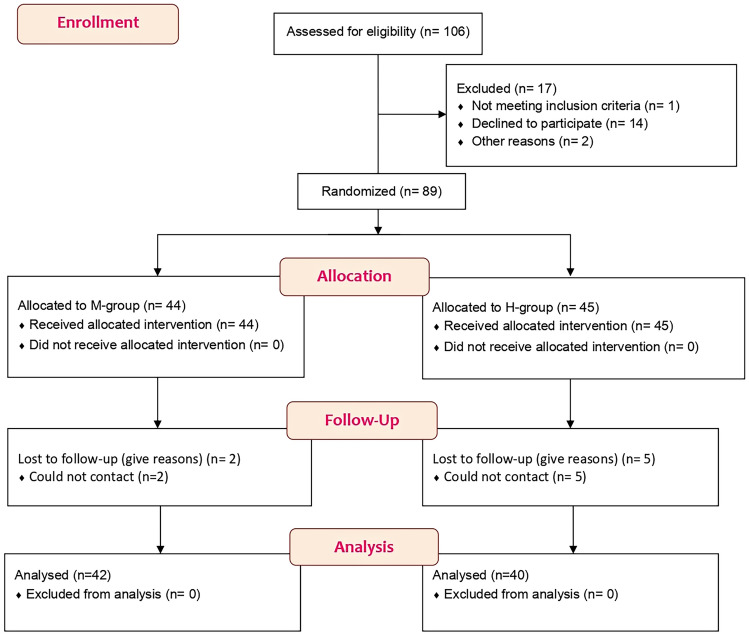
Eligible patients were randomized into 2 groups: mobile app self-directed exercise guidance group (M-group) and conventional education handout self-directed exercise guidance group (H-group) (n = 44 and 45, respectively) (Fig. 3). At the time of enrollment, each patient was assigned a computer-generated number. Patients were randomized into groups based on this number; those who received an even number were assigned to the M-group and those who received an odd number were assigned to the H-group. Demographics including age, gender, side, body mass index (BMI), onset of knee pain, education level, Kellgren and Lawrence grading from radiography (KL grade) [16], range of motion (ROM), the Knee injury and Osteoarthritis Outcome Score (KOOS) [17], and the Knee Society scores (KSS) [18] were recorded. Patients in both groups received the same information regarding knee OA disease background and exercise instruction.
Fig. 3.
Patient enrollment, eligibility, and randomization into H (handout)-group and M (mobile application)-group
Intervention
After group assignment, patients received instruction of exercise via mobile app for M-group and handouts for H-group. The standard instruction of three exercises includes (1) catch-bend-down, (2) stretch-touch-feet, and (3) sit-stretch-hold (Fig. 4). Catch-bend-down is a partial squat in which the patient holds the backrest of a chair with both hands and slowly bends both of his/her knees to 90-degree flexion. The patient was then asked to hold the squat for 10 s before slowly recovering to stand (Fig. 4a). Stretch-touch-feet is a hamstring stretch in which the patient sits on the floor with both knees fully extended, and then hinges forward from their hips to reach towards their feet (Fig. 4b). Patients were asked to hold the stretch for 10 s, and then slowly recover to a normal posture. Sit-stretch-hold is a knee extension exercise, in which the patient sits on a chair and then slowly raises his/her foot to contract their quadriceps. Patients were asked to hold for the extension 10 s before they slowly release (Fig. 4c).
Fig. 4.
Instruction of three exercises for H (handout)-group and M (mobile application)-group
Outcome measurement
All outcomes were evaluated at 4 weeks of self-guided practice by another clinician who was blinded to the trial intervention. The primary measurement of this study was the patient’s ability to correctly perform the three prescribed exercises. Patients were asked to perform the three exercises 10 times each. The exercise was considered to be performed correctly if the patient accurately completed 8 out of 10 repetitions. The secondary measurement was clinical outcomes in terms of ROM, KOOS [17] categories (symptoms, pain, activities of daily living, sports and recreation activities, and quality of life), and KSS [18] categories (objective knee score, satisfaction, expectation, and functional activity). The ROM was measured using a goniometer with a patient in the supine position.
Statistical analysis
The present study’s sample size was calculated based on the reported accuracy of rehabilitation exercise in knee OA patients [19] to be 25 knees per group to ensure sufficient power of 80 with a significant difference (P = 0.05, 2-sided significance level). To compensate for potential losses to follow-up of 20%, at least 32 knees per group should be recruited. All comparisons were analyzed by independent t tests and chi-square tests (SPSS version 23; SPSS Inc, Chicago, IL). The normal distribution of the data was verified before parametric tests were applied. Welch’s correction was used to correct for comparisons with unequal variances. All data were presented as mean ± standard deviation and comparisons were considered statistically significant if the p value was less than 0.05, two-tailed.
Results
Eighty-nine patients met the inclusion criteria for this study: 44 patients were allocated to the M-group and 45 patients were allocated to the H-group. There were 2 patients (4.5%) in the M- group and 5 patients (11.1%) in the H group who did not follow-up and thus were excluded from the final results. Table 1 outlines the demographics of the patients in this RCT. Patients on this trial were age, gender, side, BMI, and the onset of knee pain-matched: the average age of patients in the M group was 62.2 ± 6.8 years and that in the H group was 63.0 ± 9.7 years. Females constituted 85.7% of the M group and 92.5% of the H group. The average BMI of individuals in the M group was 27.1 ± 4.7, and that in the H group was 26.4 ± 5.2. Additionally, patients were matched for education level with the majority of patients from both groups have received at least junior high school level education. Overall, approximately 40, 37 and 20% of patients in both groups had a KL grade [16] of 2, 3, and 4, respectively. Finally, patients between the two groups were also matched for the ROM, KOOS [17] categories, and KSS [18] categories.
Table 1.
Patient demographics
| M-group (n = 42) | H-group (n = 40) | p value | |
|---|---|---|---|
| Agea (yrs) | 62.2 ± 6.8 | 63.0 ± 9.7 | 0.673 |
| Genderb (%) | |||
| Male | 6 (14.3) | 3 (7.5) | 0.266 |
| Female | 36 (85.7) | 37 (92.5) | |
| Sideb (%) | |||
| Left | 9 (21.4) | 10 (25.0) | 0.451 |
| Right | 33 (78.6) | 30 (75.0) | |
| BMIa (kg/m2) | 27.1 ± 4.7 | 26.4 ± 5.2 | 0.531 |
| Time in yrs since the onset of knee painb (%) | |||
| < 2 yrs | 19 (45.2) | 20 (50.0) | 0.417 |
| ≥ 2 yrs | 23 (54.8) | 20 (50.0) | |
| KL gradeb (%) | |||
| KL grade 2 | 17 (40.5) | 17 (42.5) | 0.515 |
| KL grade 3 | 15 (35.7) | 16 (40.0) | 0.432 |
| KL grade 4 | 10 (23.8) | 7 (17.9) | 0.441 |
| Education levelb (%) | |||
| < Junior high school | 14 (33.3) | 11 (27.5) | 0.370 |
| ≥ Junior high school | 21 (50.0) | 25 (62.5) | 0.180 |
| ≥ bachelor | 7 (16.7) | 4 (10.0) | 0.289 |
| Occupationb (%) | |||
| Housewife | 27 (64.3) | 22 (55.0) | 0.264 |
| Professional and administration | 8 (19.0) | 8 (20.0) | 0.567 |
| Merchant and employee | 7 (16.7) | 10 (25.0) | 0.255 |
| Care giverb (%) | 1 (2.4) | 2 (5.0) | 0.611 |
| ROMa (o) | 126.3 ± 7.3 | 124.0 ± 5.9 | 0.537 |
| KOOSa | |||
| Symptoms | 67.3 ± 13.3 | 62. 0 ± 4.1 | 0.150 |
| Pain | 72.0 ± 6.8 | 69.3 ± 5.9 | 0.261 |
| Activities of daily living | 71.6 ± 9.0 | 67.1 ± 6.9 | 0.102 |
| Sports and recreational activities | 70.5 ± 5.2 | 68.2 ± 10.1 | 0.393 |
| Quality of life | 69.5 ± 6.2 | 64.7 ± 8.7 | 0.066 |
| KSSa | |||
| Objective knee score | 29.5 ± 14.2 | 27.4 ± 14.8 | 0.802 |
| Satisfaction score | 23.0 ± 3.0 | 22.4 ± 4.6 | 0.449 |
| Expectation score | 14.1 ± 0.6 | 14.0 ± 0.7 | 0.754 |
| Functional activity score | 56.3 ± 3.5 | 54.6 ± 14.6 | 0.779 |
BMI Body mass index, KL Kellgren and Lawrence system for classification of osteoarthritis of knee, ROM, range of motion, KOOS, Knee Injury and Osteoarthritis Outcome Score, KSS Knee Society score
aPresented as mean ± standard deviation
bPresented as number of patients
Although there was no significant improvement in the ROM of the knee in either group after 4 weeks of exercise, patients in both groups had improvement in functional outcomes measured by KOOS [17] and KSS [18] (Tables 2, 3). To assess the benefit of using the mobile app during rehabilitation, we compared KOOS [17] and KSS [18] of patients between the groups after the 4-week regimen. According to patient evaluations, patients in the M group had stronger overall functional outcomes than patients in the H group (Table 4). Specifically, patients in the M group reported better daily life, ability to do sports and recreation, higher satisfaction and expectation. Importantly, patients in the M group reported a significantly better quality of life than patients in the H group (p < 0.01).
Table 2.
Outcomes of M-group at pre-test and after 4 weeks of the mobile app self-directed exercise
| Pre-test | 4 wk | p value | |
|---|---|---|---|
| ROMa (o) | 126.3 ± 7.3 | 129.0 ± 6.5 | 0.457 |
| KOOSa | |||
| Symptoms | 67.3 ± 13.3 | 70.7 ± 11.0 | 0.045* |
| Pain | 72.0 ± 6.8 | 73.3 ± 7.2 | 0.089 |
| Activities of daily living | 71.6 ± 9.0 | 80.4 ± 9.8 | 0.138 |
| Sports and recreational activities | 70.5 ± 5.2 | 80.9 ± 9.0 | < 0.001* |
| Quality of life | 69.5 ± 6.2 | 79.6 ± 10.7 | < 0.001* |
| KSSa | |||
| Objective knee score | 29.5 ± 14.2 | 32.8 ± 12.9 | 0.464 |
| Satisfaction score | 23.0 ± 3.0 | 25.2 ± 0.8 | < 0.001* |
| Expectation score | 14.1 ± 0.6 | 14.0 ± 0.8 | 0.189 |
| Functional activity score | 56.3 ± 3.5 | 59.5 ± 5.2 | 0.598 |
ROM range of motion, KOOS Knee Injury and Osteoarthritis Outcome Score, KSS Knee Society score
aPresented as mean ± standard deviation
*Indicates a statistically significant difference with p value < .05
Table 3.
Outcomes of H-group at pre-test and after 4 weeks of handout self-directed exercise
| Pre-test | 4 wk | p value | |
|---|---|---|---|
| ROMa (o) | 124.0 ± 5.9 | 125.9 ± 5.6 | 0.676 |
| KOOSa | |||
| Symptoms | 62.0 ± 4.1 | 65.3 ± 5.2 | 0.049* |
| Pain | 69.3 ± 5.9 | 70.7 ± 5.9 | 0.077 |
| Activities of daily living | 67.1 ± 6.9 | 71.2 ± 7.0 | 0.184 |
| Sports and recreational activities | 68.2 ± 10.1 | 71.8 ± 7.3 | 0.034* |
| Quality of life | 64.7 ± 8.7 | 71.2 ± 7.8 | 0.021* |
| KSSa | |||
| Objective knee score | 27.4 ± 14.8 | 29.3 ± 14.8 | 0.457 |
| Satisfaction score | 22.4 ± 4.6 | 23.6 ± 3.1 | 0.183 |
| Expectation score | 14.0 ± 0.7 | 13.5 ± 0.8 | 0.005* |
| Functional activity score | 54.6 ± 14.6 | 56.6 ± 13.7 | 0.781 |
ROM range of motion, KOOS Knee Injury and Osteoarthritis Outcome Score, KSS Knee Society score
aPresented as mean ± standard deviation
*Indicates a statistically significant difference with p value < .05
Table 4.
Comparison of outcomes between the two groups after 4 weeks
| M-group (n = 42) | H-group (n = 40) | p value | |
|---|---|---|---|
| ROMa (o) | 129.0 ± 6.5 | 125.9 ± 5.6 | 0.371 |
| KOOSa | |||
| Symptoms | 70.7 ± 11.0 | 65.3 ± 5.2 | 0.100 |
| Pain | 73.3 ± 7.2 | 70.7 ± 5.9 | 0.279 |
| Activities of daily living | 80.4 ± 9.8 | 71.2 ± 7.0 | 0.002* |
| Sports and recreational activities | 80.9 ± 9.0 | 71.8 ± 7.3 | 0.002* |
| Quality of life | 79.6 ± 10.7 | 71.2 ± 7.8 | 0.009* |
| KSSa | |||
| Objective knee score | 32.8 ± 12.9 | 29.3 ± 14.8 | 0.657 |
| Satisfaction score | 25.2 ± 0.8 | 23.6 ± 3.1 | 0.001* |
| Expectation score | 14.0 ± 0.8 | 13.5 ± 0.8 | 0.005* |
| Functional activity score | 59.5 ± 5.2 | 56.6 ± 13.7 | 0.634 |
ROM range of motion, KOOS Knee Injury and Osteoarthritis Outcome Score, KSS Knee Society score
aPresented as mean ± standard deviation
*Indicates a statistically significant difference with p value < .05
Finally, we evaluated the ability of each patient to correctly perform each of the three prescribed exercises at the end of the 4-week regimen. Overall, patients in the M group completed all of the exercises more accurately than those in the H group (p = 0.022) (Table 5). Among the three exercises, the M group significantly performed exercise 1 more accurately than the H group (p = 0.005) while not significantly in exercise 2 and 3 (p = 0.185 and p = 0.189, respectively).
Table 5.
Comparison of outcome exercise between the two groups
| M-group (n = 42) | H-group (n = 40) | p value | |
|---|---|---|---|
| Patient performing total exercisea (%) | |||
| Correct | 32 (76.2) | 21 (52.5) | 0.022* |
| Incorrect | 10 (23.8) | 19 (47.5) | |
| Patient performing correct exercise 1–3a (%) | |||
| Exercise 1 | 40 (95.2) | 29 (72.5) | 0.005* |
| Exercise 2 | 34 (81.0) | 28 (70.0) | 0.185 |
| Exercise 3 | 33 (78.6) | 27 (67.5) | 0.189 |
aPresented as number of patients
*Indicates a statistically significant difference with p value < .05
Discussion
This study investigated an interactive and user-friendly mobile app and assessed its effectiveness in delivering exercise instruction and disease education to patients and improving clinical outcomes and satisfaction. This RCT found that patients who had a rehabilitation regiment delivered by the mobile app had improved the accuracy of rehabilitation, activities of daily life, quality of life, and ability to do sports and recreational activities compared to conventional educational handouts. The mobile app also improved patient’s satisfaction and expectation in knee performance compared to traditional handouts.
Muscle-strengthening exercises for knee OA rehabilitation improve pain and functional capacity [20–22]. Osteoarthritis Research and Society International (OARSI) also recommended that osteoarthritis patients should be encouraged to undertake regular aerobic, muscle strengthening, and range of motion exercises [23, 24]. To ensure effective rehabilitation, the prescribed exercise regime must be performed accurately, and regularly [22]. Three exercises regularly prescribed to knee OA patients are catch-bend-down, stretch-touch-feet, sit-stretch-hold. With a mobile app, the patients completed these exercises with a significantly higher rate of accuracy which may suggest the ability of patients to continue appropriate rehabilitation in a long term [6, 25, 26]. In line with our findings, patients with musculoskeletal conditions who received exercise instruction by a mobile app had better adherence to their home exercises than those who received common paper handouts [27]. A different RCT compared adherence to home-based exercise between knee OA patients who used a mobile application and those who used handouts and found that those who used the mobile had a better adherence rate, lower VAS-pain scores, and stronger improvements of physical function and lower-limb muscle strength [28]. It is worthy to note that our trial assessed knee OA patients that did not require surgery; however, in the postoperative setting, the use of a mobile app during rehabilitation led to reduced opiate usage for pain management [11] and may become a promising tool in improving functional outcomes [29]. Thus, this developed mobile app has proven to be a valuable tool for OA patients for motivating patients to exercise, educating patients on disease progression and improving the accuracy of rehabilitation.
Although our RCT is a short-term study, we predict that this app will improve the long-term compliance with the rehabilitation program. This app not only provides instruction, but also insights into their personal condition. Our mobile app includes a list of common questions that are used to assess the degree of OA progression. Utilization of this questionnaire may provide knowledge of the physical condition and motivation to adhere to rehabilitation efforts. Additionally, this application has a section that provides the patients with an educational background of the disease, that may benefit the patients in a variety of ways, including increasing daily activities and reducing anxiety [30, 31].
It is important to consider the limitations of this study. First, the patients included in this study were able to efficiently use smartphones, which may not be reflective of a larger elderly population. Second, according to the structure of the study, it is impossible to blind the participants to their intervention. This knowledge can potentially skew self-reported outcomes. Third, the majority of the patients were females (89.0%). However, this gender bias is always observed in OA patients [32]. The gender bias may be solved by randomization according to gender in future study. Fourth, there is no consensus on the definition of a method to measure patients’ adherence to exercise [33, 34]. We believed that a patient's ability to accurately perform the exercises at the final follow-up reflects adherence to home exercise; however, this may not always be the case. Fifth, there is a lack of normative data of KSS to assess the patients. There are no reference values to differentiate which patients have improved significantly. Finally, a long-term follow-up study is needed to prove the sustained positive effect of the mobile application use on adherence to exercise and the health status of the patients on this trial.
Electronic health has been introduced recently to support patient’s adherence to home exercise programs and exercise interventions to reduce pain and improve physical function in OA patients [35–37]. A major advantage to mobile apps is that patients can easily access exercise information on their mobile phones. Therefore, patients can learn to perform the exercises at any time, not just when they are at home. Interactive features of this application, such as exercise tracking and motivational animations, are attributes that can engage and motivate the users. Future developments include introducing a social component to the rehabilitation program, which allows for patients who have improved symptoms and reduced pain over time to encourage newer users. Additional features include music, video instruction, alerts, and awards. This app has the potential to provide a healthy community of users to support each other and exercise together, promoting an effective way to manage knee OA.
Conclusion
This RCT supports the hypothesis that the developed mobile app is an effective way to deliver rehabilitation education and instruction to knee OA patients. The results show that OA patients using this app were able to exercise correctly and enjoyed usage their exercise regimen with significant improvement of symptom progression as indicated by KSS and KOOS category scores. Thus, the use of our mobile app for short-term disease maintenance and treatment of OA benefits patients and represents a potential approach for long-term rehabilitation.
Acknowledgements
The authors thank Ms Thikampa Wichai for help in collecting and organizing the data analyzed in this report.
Funding
This project was supported by the Navamindradhiraj University Research Fund grant numbers CEU/C 8/2561.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study has been performed in compliance with the Helsinki Declaration, has been approved by the ethical committee of Navamindradhiraj University COA034/2561) and registered at clinicaltrials.gov (NCT03666585).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587. doi: 10.1016/j.eclinm.2020.100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Middelkoop M, Bennell KL, Callaghan MJ, Collins NJ, Conaghan PG, Crossley KM, Eijkenboom J, van der Heijden RA, Hinman RS, Hunter DJ, Meuffels DE, Mills K, Oei EHG, Runhaar J, Schiphof D, Stefanik JJ, Bierma-Zeinstra SMA. International patellofemoral osteoarthritis consortium: consensus statement on the diagnosis, burden, outcome measures, prognosis, risk factors and treatment. Semin Arthritis Rheum. 2018;47(5):666–675. doi: 10.1016/j.semarthrit.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, Stansfield C, Oliver S. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018;4(4):CD010842. doi: 10.1002/14651858.CD010842.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins NJ, Hart HF, Mills KAG. Osteoarthritis year in review 2018: rehabilitation and outcomes. Osteoarthritis Cartilage. 2019;27(3):378–391. doi: 10.1016/j.joca.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Kanavaki AM, Rushton A, Efstathiou N, Alrushud A, Klocke R, Abhishek A, Duda JL. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open. 2017;7(12):e017042. doi: 10.1136/bmjopen-2017-017042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobson F, Bennell KL, French SD, Nicolson PJ, Klaasman RN, Holden MA, Atkins L, Hinman RS. Barriers and facilitators to exercise participation in people with hip and/or knee osteoarthritis: synthesis of the literature using behavior change theory. Am J Phys Med Rehabil. 2016;95(5):372–389. doi: 10.1097/phm.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 7.Administration UFaD Policy for devices software function and mobile medical application.
- 8.Mrklas KJ, Barber T, Campbell-Scherer D, Green LA, Li LC, Marlett N, Miller J, Shewchuk B, Teare S, Wasylak T, Marshall DA. Co-design in the development of a mobile health app for the management of knee osteoarthritis by patients and physicians: qualitative study. JMIR Mhealth Uhealth. 2020;8(7):e17893. doi: 10.2196/17893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P t. 2014;39(5):356–364. [PMC free article] [PubMed] [Google Scholar]
- 10.Rabin A, Dolkart O, Kazum E, Wengier R, Goldstein Y, Maman E, Chechik O. Shoulder assessment by smartphone: a valid alternative for times of social distancing. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-03762-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singler K, Roth T, Beck S, Cunningham M, Gosch M. Development and initial evaluation of a point-of-care educational app on medical topics in orthogeriatrics. Arch Orthop Trauma Surg. 2016;136(1):65–73. doi: 10.1007/s00402-015-2366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitchell HL, Hurley MV. Management of chronic knee pain: a survey of patient preferences and treatment received. BMC Musculoskelet Disord. 2008;9:123. doi: 10.1186/1471-2474-9-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holden MA, Nicholls EE, Young J, Hay EM, Foster NE. Role of exercise for knee pain: what do older adults in the community think? Arthritis Care Res (Hoboken) 2012;64(10):1554–1564. doi: 10.1002/acr.21700. [DOI] [PubMed] [Google Scholar]
- 14.Choi W, Zheng H, Franklin P, Tulu B. mHealth technologies for osteoarthritis self-management and treatment:a systematic review. Health Informatics J. 2019;25(3):984–1003. doi: 10.1177/1460458217735676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria committee of the american rheumatism association. Arthritis Rheum. 1986;29(8):1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 16.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64–64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. doi: 10.1097/00003086-198911000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Thiengwittayaporn S, Wetpiryakul P, Foosakun Y, Ngamsom T, Vathanavit P, Pintongtun J. Comparison of the accuracy of quadriceps isometric exercise between using quadriceps education device (QED) and not using QED for osteoarthritic knee patients: a randomized controlled trial. J Med Assoc Thai. 2009;92(Suppl 6):S33–38. [PubMed] [Google Scholar]
- 20.Tanaka R, Ozawa J, Kito N, Moriyama H. Efficacy of strengthening or aerobic exercise on pain relief in people with knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2013;27(12):1059–1071. doi: 10.1177/0269215513488898. [DOI] [PubMed] [Google Scholar]
- 21.Uthman OA, van der Windt DA, Jordan JL, Dziedzic KS, Healey EL, Peat GM, Foster NE. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. Br J Sports Med. 2014;48(21):1579. doi: 10.1136/bjsports-2014-5555rep. [DOI] [PubMed] [Google Scholar]
- 22.Brosseau L, Taki J, Desjardins B, Thevenot O, Fransen M, Wells GA, Mizusaki Imoto A, Toupin-April K, Westby M, Álvarez Gallardo IC, Gifford W, Laferrière L, Rahman P, Loew L, De Angelis G, Cavallo S, Shallwani SM, Aburub A, Bennell KL, Van der Esch M, Simic M, McConnell S, Harmer A, Kenny GP, Paterson G, Regnaux JP, Lefevre-Colau MM, McLean L. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part two: strengthening exercise programs. Clin Rehabil. 2017;31(5):596–611. doi: 10.1177/0269215517691084. [DOI] [PubMed] [Google Scholar]
- 23.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18(4):476–499. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 24.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16(2):137–162. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 25.Maly MR, Marriott KA, Chopp-Hurley JN. Osteoarthritis year in review 2019: rehabilitation and outcomes. Osteoarthritis Cartilage. 2020;28(3):249–266. doi: 10.1016/j.joca.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Pisters MF, Veenhof C, Schellevis FG, Twisk JW, Dekker J, De Bakker DH. Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res (Hoboken) 2010;62(8):1087–1094. doi: 10.1002/acr.20182. [DOI] [PubMed] [Google Scholar]
- 27.Lambert TE, Harvey LA, Avdalis C, Chen LW, Jeyalingam S, Pratt CA, Tatum HJ, Bowden JL, Lucas BR. An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: a randomised trial. J Physiother. 2017;63(3):161–167. doi: 10.1016/j.jphys.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 28.Alasfour M, Almarwani M. The effect of innovative smartphone application on adherence to a home-based exercise programs for female older adults with knee osteoarthritis in Saudi Arabia: a randomized controlled trial. Disabil Rehabil. 2020 doi: 10.1080/09638288.2020.1836268. [DOI] [PubMed] [Google Scholar]
- 29.Bäcker HC, Wu CH, Schulz MRG, Weber-Spickschen TS, Perka C, Hardt S. App-based rehabilitation program after total knee arthroplasty: a randomized controlled trial. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-03789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coleman S, Briffa NK, Carroll G, Inderjeeth C, Cook N, McQuade J. A randomised controlled trial of a self-management education program for osteoarthritis of the knee delivered by health care professionals. Arthritis Res Ther. 2012;14(1):R21. doi: 10.1186/ar3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khachian A, Seyedoshohadaei M, Haghani H, Amiri F. Effect of self-management program on outcome of adult knee osteoarthritis. Int J Orthop Trauma Nurs. 2020;39:100797. doi: 10.1016/j.ijotn.2020.100797. [DOI] [PubMed] [Google Scholar]
- 32.Bawa HS, Weick JW, Dirschl DR. Gender disparities in osteoarthritis-related health care utilization before total knee arthroplasty. J Arthroplasty. 2016;31(10):2115–2118.e2111. doi: 10.1016/j.arth.2016.03.044. [DOI] [PubMed] [Google Scholar]
- 33.Bailey DL, Holden MA, Foster NE, Quicke JG, Haywood KL, Bishop A. Defining adherence to therapeutic exercise for musculoskeletal pain: a systematic review. Br J Sports Med. 2020;54(6):326–331. doi: 10.1136/bjsports-2017-098742. [DOI] [PubMed] [Google Scholar]
- 34.Hall AM, Kamper SJ, Hernon M, Hughes K, Kelly G, Lonsdale C, Hurley DA, Ostelo R. Measurement tools for adherence to non-pharmacologic self-management treatment for chronic musculoskeletal conditions: a systematic review. Arch Phys Med Rehabil. 2015;96(3):552–562. doi: 10.1016/j.apmr.2014.07.405. [DOI] [PubMed] [Google Scholar]
- 35.Schäfer AGM, Zalpour C, von Piekartz H, Hall TM, Paelke V. The efficacy of electronic health-supported home exercise interventions for patients with osteoarthritis of the knee: systematic review. J Med Internet Res. 2018;20(4):e152. doi: 10.2196/jmir.9465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Safari R, Jackson J, Sheffield D. Digital self-management interventions for people with osteoarthritis: systematic review with meta-analysis. J Med Internet Res. 2020;22(7):e15365. doi: 10.2196/15365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Petersen W, Karpinski K, Backhaus L, Bierke S, Häner M. A systematic review about telemedicine in orthopedics. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-03788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]