Abstract
Purpose
Clarithromycin is commonly prescribed for H. pylori infection. Domain V mutations are responsible for clarithromycin resistance. This study was aimed to characterize the clarithromycin resistance and its associated mutations in clinical isolates of H. pylori in Pakistan.
Materials and Methods
Infection was diagnosed in 93 patients’ biopsies using culture, rapid urease test, 16S rRNA, and vacA gene multiplex PCR. Clarithromycin resistance was assessed by the agar dilution method. Mutations were detected by PCR-RFLP using 46 (1.4 kb) domain V fragments. Sequencing was executed for 13 domain V fragments, of which 12 showed unusual amplicon size (1.2 kb) and 01 had a new MboII RFLP pattern.
Results
A total of 48 (83%) strains were obtained from 58 (62.3%) PCR H. pylori-positive samples. Resistance (MIC ≥ 0.001 mg/mL) and intermediate resistance phenotype (MIC = 0.0005 mg/mL) was observed in 22 (46%), and 10 (21%) isolates, respectively. The primary resistance was found in 23 (39.6%) samples. PCR-RFLP detected A2142G, A2143G, and double mutations in 19, 04, and 01 resistant strain, respectively. Sequencing of 10 amplicons obtained from intermediated resistant strains and 03 amplicons from resistant strains showed 138 new mutations. Among them, T2182C was also seen in 04 intermediated resistant isolates, whereas A2142G, A2143G, and A2143C were observed in resistant isolates. The new MboII RFLP pattern in an intermediated resistant strains was due to A1761G mutation.
Conclusion
H. pylori domain V mutations showed extensive diversity. Multiple mutations in domain V may give endurance to H. pylori against clarithromycin. Further investigations on the molecular mechanism of antibiotic resistance in H. pylori seem crucial at this stage.
Keywords: 23S rRNA gene, Helicobacter pylori, clarithromycin resistance, domain V multiple point mutations
Introduction
Helicobacter pylori, an infectious agent of human chronic active gastritis and also associated with other gastric ailments such as peptic ulcer, gastric cancer, and mucosa-associated lymphoid tissue lymphoma.1 Clarithromycin is considered the best option among other antibiotics for the management of this bacterial infection.2 However, increasing resistance against this antibiotic has declined its eradication rates.
H. pylori possess two genes of 23S rRNA and mutation in any one gene confers clarithromycin resistance phenotype.3 The most frequent and well-studied molecular pathway for clarithromycin resistance is due to A2142G and A2143G point mutations in domain V of the 23S rRNA gene.4 Other mutations like A2142C, G1939A, A2115G, G2141A, A2144G, A2144T, C2147G, T2182C, G2224A, and T2215C vary geographically and found to mediate resistance phenotype.1,3,5
This study on the characterization of 23S rRNA gene mutations in clinical isolates of H. pylori in Pakistan found three new features of domain V. First, a new MboII RFLP pattern was found. Second, 1.2 kb long amplicons of domain V instead of 1.4 kb with a specific primer set were obtained. Third, multiple new point mutations were observed in intermediate resistant isolates.
Previously, no data were available on the 23S rRNA gene mutations other than at 2142 and 2143 positions from this region. In this study, besides the prevalence of clarithromycin resistance-associated mutations A2142G, A2143G, A2143C, other multiple point mutations in the domain V of 23S rRNA gene of H. pylori, and their effect on clarithromycin minimum inhibitory concentration (MIC) are reported.
Materials and Methods
Patients
This cross-sectional study comprised 93 dyspeptic patients enrolled for upper esophageal-gastroduodenoscopy (OGD) at two hospitals in Karachi, Pakistan. This study was conducted in accordance with the Declaration of Helsinki, and written informed consent was obtained from each enrolled patient before endoscopy for the collection of biopsies. Moreover, study methodology was approved by the Board of Advance Studies and Research, University of Karachi. From each patient, six biopsies were obtained, ie, two from antrum, two from corpus, and two from fundus. A total of 558 biopsies were collected from 93 patients. A structured questionnaire was also used to obtain the information about the earlier use of any anti-H. pylori treatment.
H. pylori Culture
Gastric biopsies were transported in Stuart transport medium (CM111; Oxoid) at 4°C. One biopsy of antrum, corpus, and fundus from each patient was directly rubbed against the surface of Columbia blood agar plates (CM331; Oxoid) supplemented with 10% sheep blood, Nalidixic acid (0.01 mg/mL), Vancomycin (0.006 mg/mL), Amphotericin B (0.006 mg/mL), Cefsulodine (0.005 mg/mL), and Tetrazolium chloride (0.04 mg/mL). Plates were placed in an anaerobic jar (AN25; Oxoid) with a Campygen microaerophilic gas generating kit (CN25; Oxoid). The anaerobic jar was placed in an incubator at 37°C for up to 7 days. After 72 hours of incubation, plates were daily checked for the appearance of H. pylori golden pigmented colonies due to the reduction of tetrazolium chloride. After 7 days plates with no growth were discarded and considered as culture negative. Golden pigmented colonies were further Gram-stained and checked for urease test. The agar dilution method was used to check the clarithromycin susceptibility as described by the Clinical and Laboratory Standards Institute (CLSI) guidelines.6 Briefly, using Muller-Hinton agar (CM337; Oxoid) supplemented with 5% sheep blood, two-fold serial dilutions of clarithromycin concentrations were prepared (0.004 mg/mL to 0.000125 mg/mL). Clarithromycin MICs breakpoints were noted according to the CLSI criteria (≤0.00025 mg/mL, susceptible; 0.0005 mg/mL, intermediate; ≥0.001 mg/mL, resistant).
Rapid Urease Test
Each patient also contributed the antrum, corpus, and fundus biopsies that were immersed separately in urease test tubes and incubated at room temperature for 12 hrs. Tubes were inspected for color change from yellow to bright magenta. Rapid urease test tubes were prepared as described previously.7 Briefly, the following components were mixed, filter sterilized, and stored at −20°C: yeast extract (10 mg), KH2PO4 (9.1mg), Na2HPO4 (9.5 mg), urea (4000 mg instead of 2000 mg), and 15 drops of phenol red (0.5% solution).
DNA Extraction
Cell lysate of H. pylori culture was prepared as described previously,8 and directly used in the PCR reaction. Genomic DNA from urease test biopsies was also extracted using the previously described method.9,10 The DNA pellet was re-suspended in 10–15 µL of TE (Tris-HCl 10mM (pH: 8.00), EDTA 1mM), and stored at −20°C until use.
Amplification of H. pylori DNA
H. pylori detection in gastric biopsies was performed using the 16S rRNA gene Helicobacter genus-specific PCR and the vacA gene multiplex PCR for signal (s) and middle (m) region alleles.11–13 Samples found positive in both PCR methods were further used for the amplification of 1.4 kb long region of domain V of the 23S rRNA gene. The amplified fragments of the domain V were purified using Quantum Prep Freeze N Squeeze DNA gel extraction spin columns (Fermentas, Thermo Fisher Scientific, Waltham, Massachusetts, USA), and further used in H. pylori-specific nested PCR to amplify the 696bp internal region of the domain V as previously described.12 PCR reaction volume was 50µL and the mixture consisted of 5 µL template DNA (3.2 ng), 1µM each primer, 200µM each dNTPs, 1.5mM MgCl2, 1x buffer, and 1.5U of Taq polymerase (Fermentas, Thermo Fisher Scientific, Waltham, Massachusetts, USA). Amplification was performed in the Applied Biosystems, GeneAmp PCR, 2400. Summary of oligonucleotides and PCR cycle conditions is presented in Table 1.
Table 1.
Primer Pairs and PCR Cycle Conditions Used to Amplify H. pylori Various Gene Fragments from Gastric Biopsies
| Primer Name | Sequence | Target | Amplicon (bp) | PCR Reaction Conditions | Reference No. |
|---|---|---|---|---|---|
| C97 | GCTATGACGGGTATCC | 16S rDNA | 422 | 6min at 94°C; 40 cycles for 30sec at 94°C, 1min at 50°C then 3min at 72°C and final extension for 10min at 72°C | [12] |
| C98 | GATTTTACCCCTACACCA | ||||
| VAI-F | ATGGAAATACAACAAACACAC | vacA s1/vacA s2 | 259/286 | 1 min at 94°C; 35 cycles of 1 min at 94°C, 1 min at 55°C, 1min at 72°C | [11,13] |
| VAI-R | CTGCTTGAATGCGCCAAAC | ||||
| VAG-F | CAATCTGTCCAATCAAGCGAG | vacA m1/vacA m2 | 567/642 | 1 min at 94°C; 35 cycles of 1 min at 94°C, 1 min at 55°C, 1min at 72°C | [11,13] |
| VAG-R | GCGTCAAAATAATTCCAAGG | ||||
| 18 HP | AGTCGGGACCTAAGGCGAG | 23S rRNA | 1402 | 6min at 94°C; 40 cycles for 30sec at 94°C, 1min at 50°C then 3min at 72°C and final extension for 10min at 72°C | [8] |
| 21 HP | TTCCCGCTTAGATGCTTTCAG | ||||
| 18 HP | AGTCGGGTCCCTAAGCCGAG | 23S rRNA | 1402 | 6min at 94°C; 40 cycles for 30sec at 94°C, 1min at 50°C then 3min at 72°C and final extension for 10min at 72°C | [12] |
| 21 HP | TTCCTGCTTAGATGCTTTCAG | ||||
| HPRP-1 | ATCGCTGATACCGTCGTGCC | 23S rRNA | 696 | 6min at 94°C; 40 cycles for 30sec at 94°C, 1min at 50°C then 3min at 72°C and final extension for 10min at 72°C | [12] |
| HPRP-2 | CTTTTTAGGAGCGACCGCCCC |
PCR-RFLP for the Detection of Point Mutations
The 1.4 kb long domain V fragments from gastric biopsies and culture isolates were analyzed for mutation detections using the polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) technique. Amplicons were treated with MboII and BsaI restriction endonucleases (Fermentas, Thermo Fisher Scientific, Waltham, Massachusetts, USA) for the detection of A2142G and A2143G mutations, respectively. Digestion reaction consisted of 10 ul PCR products, 1x buffer, 10 and 20 units of MboII and BsaI restriction enzymes, respectively, according to the manufacturer’s recommendations. PCR products were digested during 10-hours of incubation at 37°C. Restriction digestion products were separated by electrophoresis on a 1.2% agarose gel with 100-bp DNA molecular weight marker (Fermentas, Thermo Fisher Scientific, Waltham, Massachusetts, USA). Endonuclease MboII digested PCR products having A2142G mutation are expected to yield two fragments of 710 bp and 692 bp that comigrate in agarose gel. Endonuclease BsaI digested PCR products having A2143G mutation should yield three fragments of 700 bp, 400 bp, and 300bp.
Sequencing for the Detection of Point Mutations
The commercial sequencing facility from Macrogen Inc. Seoul, Korea, using an ABI 3730XL sequencer was used for DNA sequencing. A total of thirteen 696 bp nested amplicons of domain V were sequenced.
Nucleotides Sequence Analysis
The 696 bp long domain V sequences were aligned with the reference sequences of the 23S rRNA gene of H. pylori strains 26695, J99, and U27270 (GenBank accession No.). The numbering of nucleotides was done as described previously.14
Nucleotides Sequence Accession Numbers
The nucleotide sequences reported in this study have been deposited in GenBank under the accession numbers KY353088 to KY353100.
Results
Bacterial Culture and Clarithromycin Susceptibility Testing
A total of 93 dyspeptic patients participated in this study. Among them, anti-H. pylori treatment history was found in 08 (8.6%) patients. The culture showed positive results in 48 (51%) patients. Of these strains, 46 (96%) were recovered from untreated and 02 (4%) from clarithromycin-treated patients. Of the 48 H. pylori isolates, 22 (46%) were categorized as clarithromycin resistant (MIC ≥ 0.001 mg/mL), 10 (21%) as intermediate resistant (MIC= 0.0005 mg/mL), and 16 (33%) isolates were considered as susceptible (MIC ≤ 0.00025 mg/mL).
Rapid Urease Test
A positive urease test was found in 48 (51.6%) culture-positive biopsies and in 02 (2%) culture-negative biopsies. Overall, 50 (53.7%) biopsies showed a positive urease test.
PCR Based H. Pylori Detection
H. pylori infection was confirmed by using 16S rRNA gene Helicobacter genus-specific and H. pylori-specific vacA gene PCR. Samples were considered positive for H. pylori DNA only if they showed positive results in both PCR methods. Both targeted genes, 16S rRNA and vac A, were present in all cultures and urease test positive biopsies. However, 08 (8%) culture and urease test negative and 02 (2%) culture-negative samples also showed positive results in PCR methods. Overall, both PCR methods detected infection in 58 (62%) samples.
Helicobacter 16S rRNA gene PCR also showed positive amplification in 13 (13.9%) urease test, culture, and vacA gene PCR negative samples, while all tests were found negative in 22 (23.6%) patients. The 16S rRNA gene PCR results were presented in Supplementary Material.
Of the 58 (62%) H. pylori-infected patients, vacA genotype s1m1 was found in 20 (34%) clinical isolates, s1m2 in 08 (13.7%), s2m1 in 05 (8.6%), and s2m2 genotype was detected in 25 (43%)H. pylori isolates. The vacA gene PCR results are presented in Supplementary Material.
Amplification of 23S rRNA Gene Fragments
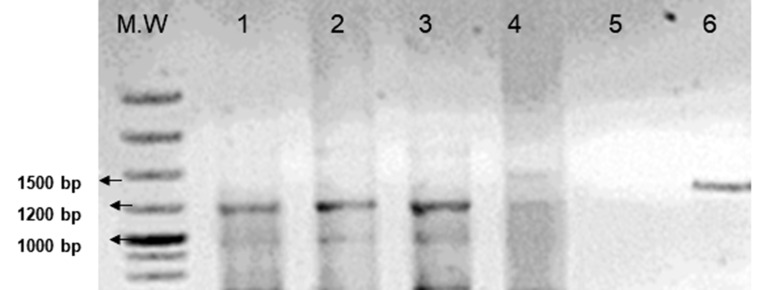
H. pylori isolates and PCR positive samples were used to amplify the domain V of the 23S rRNA gene. Two sets of 23S rRNA gene primers proposed previously were used.8,12 Both these primer sets have been reported to give a 1.4 kb amplicon. In this study, 46 (79%) samples produced 1.4 kb amplicons with both primer sets. Of these amplicons, 19 (41%) were obtained from clarithromycin-resistant isolates, 16 (34.7%) from susceptible isolates, 01 (2%) from clarithromycin intermediate resistant isolate, and 10 (21.7%) amplicons were obtained from culture-negative samples. Furthermore, 12 (20.6%) culture and PCR positive samples yielded around 1.2 kb amplicons with only one primer set proposed by Versalovic et al8 (Figure 1). Of these amplicons, 03 (25%) were obtained from clarithromycin-resistant isolates, and 09 (75%) were obtained from strains that showed intermediate resistance. Nested PCR using 1.4 kb and 1.2 kb amplicons as templates gave the expected 696bp internal part of domain V of the 23S rRNA gene from all 58 (100%) H. pylori-positive samples. See Supplementary Material, for nested PCR results.
Figure 1.
PCR amplification of 1200bp amplicons of domain V of the 23S rRNA gene of H. pylori using Versalovic et al8 primer pair. M.W, 1kb molecular weight marker; Lane 1 to 3, 1200bp amplified fragments; Lane 4, H. pylori-negative biopsy DNA; Lane 5, Negative Control (No DNA only PCR reaction mix); Lane 6, Standard 1400 bp amplicon obtained from the same primer set using different H. pylori-positive biopsy DNA.
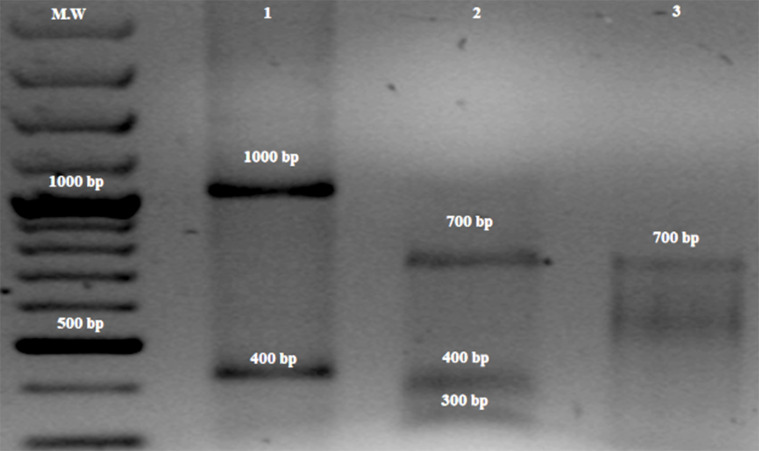
PCR-RFLP for the Detection of A2142G and A2143G Mutations
Restriction analyses were performed using 1.4 kb amplicons of domain V, as the restriction fragments of clarithromycin sensitive and resistant strains of H. pylori are well established.8,15 The MboII restriction endonuclease-mediated digestion detected A2142G mutation in 19 (41%) samples (Figure 2). Of these 19 samples, 15 (79%) were obtained from culture-positive resistant isolates and 04 (21%) from culture-negative strains with anti-H. pylori treatment history. Moreover, 01 (2%) amplicon from intermediate resistance phenotype strain showed a new MboII restriction profile, ie, instead of 700bp and 696 bp fragments in the presence of A2142G mutation, the approximately 400bp, and 1000bp fragments were seen (Figure 2). The BsaI restriction endonuclease-mediated digestion detected A2143G mutation in 04 (8.6%) culture-positive resistant strains (Figure 2). Also, 01 (2%) amplicon from a culture-negative clarithromycin treated strain showed both A2142G and A2143G mutations.
Figure 2.
PCR-RFLP based detection of mutations A2142G and A2143G in 1400 kb amplicon of 23S rRNA gene of H. pylori with BsaI and MboII restriction enzymes, respectively. Lane 1 shows the new MboII RFLP pattern, ie, approximately 1000bp and 400 bp fragments appears in the presence of A1761G mutation and sequencing also confirmed this mutation (see Figure 3); Lane 2 shows the clarithromycin resistant restriction profile with BsaI, ie, 700bp, 400bp and 300bp fragments indicate the presence of A2143G mutation; Lane 3 shows the clarithromycin resistant profile with MboII, ie, 710bp and 690 fragments indicate the presence of A2142G mutation, M.W, 100bp molecular weight marker.
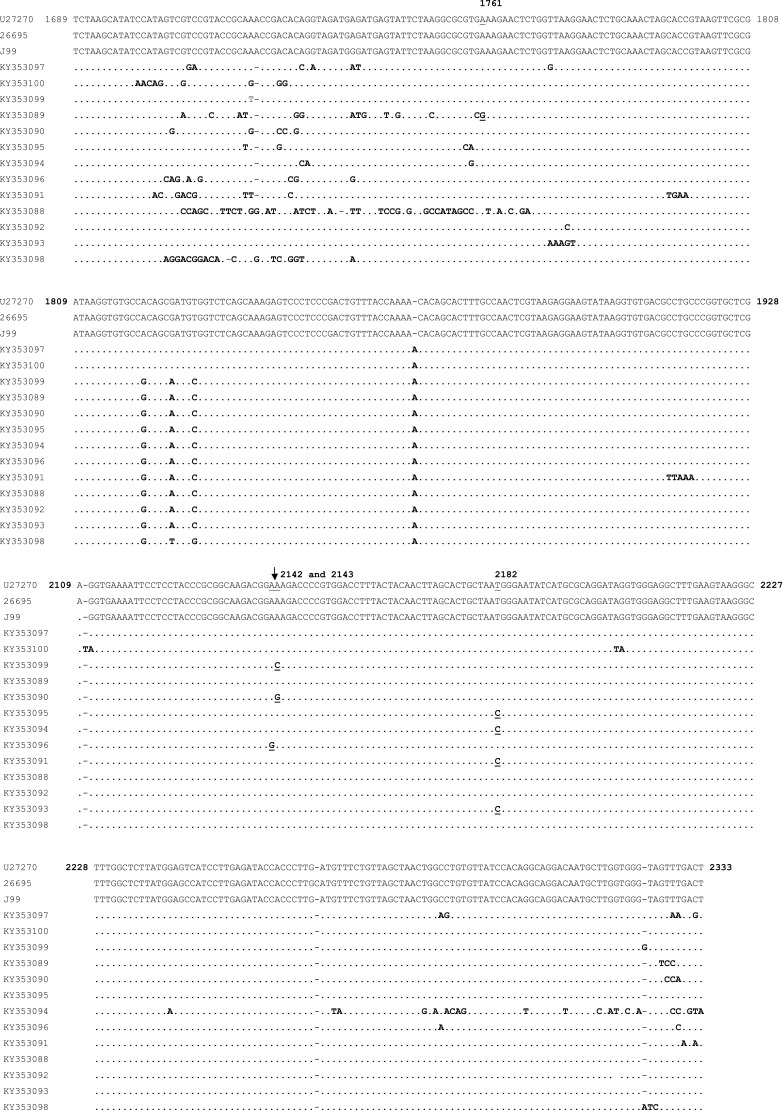
Sequencing for the Detection of Point Mutations
Of the 13 sequenced amplicons, 03 (23%) were obtained from the resistant strains and they all showed multiple new mutations and clarithromycin resistance-associated mutations like A2142G, A214 3G, and A2143C, respectively (Figure 3). While 10 (77%) amplicons were amplified from intermediate resistance isolates. All of them showed multiple new mutations. Among them, 04 (4%) also showed T2182C mutation. Moreover, a new MboII RFLP pattern (approximately 400bp and 1000bp) was due to the A1761G mutation.
Figure 3.
Multiple sequence alignment of thirteen 696 bp long domain V sequences of 23S rRNA gene of H. pylori (KY353089 to KY353100; GenBank Accession No.) obtained in the present study with the reference domain V sequences of H. pylori strains 26695, J99, and U27270 (GenBank accession No.). The nucleotide numbering was done according to Taylor et al.14 This figure only shows the nucleotide’s positions which are mutated. Similarity among the sequences is represented by (.) and gaps are represented by (-).
Primary and Secondary Clarithromycin Resistance
Primary and secondary resistance against clarithromycin was correlated using the questionnaire information obtained from each patient. Clarithromycin resistance-associated mutations were found in 27 (46%) H. pylori isolates. Among them, primary clarithromycin resistance was observed in 18 (31%), 04 (7%), and 01 (2%) isolates due to A2142G, A2143G, and A2143C mutations, respectively. The secondary resistance was noted in 02 (3%) isolates due to A2142G, in 01 (2%) isolate due to A2143G, whereas both mutations were found responsible for secondary resistance in 01 (2%) isolate. The overall primary resistance rate was 23 (39.6%) and the secondary resistance rate was 04 (7%). See Table 2 for primary and secondary clarithromycin resistance results.
Table 2.
Domain V Mutations Associated with Primary and Secondary Clarithromycin Resistance
| H. pylori-Infected Patients (N=58) | Antibiotic Treatment History | Domain V Mutations Detected Through PCR-RFLP and Sequencing | ||
|---|---|---|---|---|
| A2142G | A2143G | A2143C | ||
| 3 | MTZ + AMX+ PPI | + | - | - |
| 1 | MTZ+CLR+AMX+ PPI | + | + | - |
| 1 | CLR+AMX+CPF+PPI | + | - | - |
| 1 | MTZ+CLR+AMX+ PPI | - | + | - |
| 1 | MTZ+CLR+AMX+ PPI | - | - | - |
| 1 | CLR+AMX+PPI | + | - | - |
| 15 | No antibiotic treatment | + | - | - |
| 4 | No antibiotic treatment | - | + | - |
| 1 | No antibiotic treatment | - | - | + |
| 4 | No antibiotic treatment | - | - | - |
| 26 | No antibiotic treatment | - | - | - |
| Overall mutations frequency in H. pylori positive samples | (A2142G) 36% (21/58) | (A2143G) 10% (6/58) | (A2143C) 2% (1/58) | |
Abbreviations: MTZ, metronidazole; AMX, amoxicillin; CLR, clarithromycin; PPI, proton pumps inhibitor; CPF, ciprofloxacin; PCR-RFLP, polymerase chain reaction-restriction fragment length polymorphism; A2142G (36%), 23S rRNA domain V mutation from Adenine to Guanine at position 2142 and its corresponding frequency in H. pylori positive samples; A2143G (10%), 23S rRNA domain V mutation from Adenine to Guanine at position 2143 and its corresponding frequency in H. pylori positive samples; A2143C (2%), 23S rRNA domain V mutation from Adenine to Cytosine at position 2143 and its corresponding frequency in H. pylori positive samples.
Discussion
Escalating resistance against antibiotics in H. pylori is a concern, especially in developing countries like Pakistan, where more than 80% of the population is infected.16 Clarithromycin-based regimes have been recommended by many experts as the first-line treatment.17 However, the worldwide occurrence of clarithromycin resistance is a major threat in the management of this bacterial infection.18
This study was performed to explore the prevalence of clarithromycin resistance and its associated mutations in the 23S rRNA gene of H. pylori isolated from the clinical samples of dyspeptic patients in Pakistan. The presence of H. pylori was confirmed by the culture, rapid urease test, Helicobacter genus-specific 16S rRNA gene PCR, and H. pylori-specific vacA gene multiplex PCR as reported earlier.7,12,13
The culture was found positive in 48 (51%) samples and negative in 10 (11%) rapid urease test and PCR positive samples. Culturing has low sensitivity, and successful recovery depends on several factors like transportation conditions, prior antibiotic treatment, number of bacteria in samples, biopsy processing procedure, exposure to atmospheric oxygen, etc, so negative results might be related to any of these factors. The PCR test of both genes of H. pylori showed positive results in all 50 (100%) rapid urease test positive biopsies and in 08 (19%) urease test negative biopsies. The negative urease test in eight PCR positive samples might be related to low bacterial count because the sensitivity of the urease test depends on the number of bacteria present in the biopsy. Moreover, the use of proton pump inhibitors (PPI) also reduces its sensitivity. A study by Yakoob et al19 reported the low sensitivity of rapid urease tests in patients with prior use of PPI. In the present study, patients’ clinical history also revealed that 27 (46%) of the 58 H. pylori-positive patients had been on such medications before endoscopy (data not shown).
Helicobacter genus-specific 16S rRNA gene PCR also showed positive results in 13 (13.9%) urease test and vacA gene PCR negative samples. These patients might be infected with some other Helicobacter species as reported earlier.12,20 The identity of these species is being pursued by 16S rRNA gene sequencing.
The confirmation of H. pylori infection was performed using the vacA gene multiplex PCR as described previously.13 The reason behind using vacA primer pairs for H. pylori detection is that these primers were redesigned using the sequence information of the Asian H. pylori strains.11 In this study, the most frequent detected vacA genotype was s2m2 (43%) followed by s1m1 (34%), s1m2 (13.7%), and s2m1 (8.6%). The distribution of vacA genotypes in the present study was different from another study of Pakistan,21 where the most frequent genotype was s1m1. This variability reflects the intra-regional genetic diversity within the H. pylori genome.
The phenotypic clarithromycin resistance was assessed by the agar dilution method as reported previously.6 The breakpoints for clarithromycin are well established, reproducible, and categorized the strains into three types, ie, sensitive (MIC ≤0.00025 mg/mL), intermediate resistant (MIC 0.0005 mg/mL), and resistant (MIC ≥ 0.001mg/mL). In this study, 46% of isolates were categorized as resistant, 21% as intermediate, and 33% of isolates were found susceptible. These results showed a high prevalence of clarithromycin resistance in clinical isolates of H. pylori. Earlier, another study from Pakistan also reported a high clarithromycin resistance rate.21
To investigate the clarithromycin resistance-associated mutations A2142G and A2143G sequencing and PCR-RFLP techniques were used. The PCR-RFLP is still being used, an accurate, rapid, and low-cost method.22,23 Both techniques showed that all phenotypic clarithromycin-resistant isolates had either A2142G, A2143G, or A2143C mutations. The prevalence of A2142G was 36% (21/58), A2143G 10% (6/58), and A2143C was 1.7% (1/58). In other words, 78% (21/27) of mutations found in our study were categorized as A2142G and 22% (6/27) were A2143G and 3.7% (1/27) were A2143C.
The prevalence of A2142G and A2143G mutations varies geographically. A study from a west neighbor country, ie, Iran reported A2142G in 90% of clarithromycin-resistant isolates.24 However, studies from east and northeast neighbors, ie, India and China reported a high percentage of A2143G mutation.18,25 Data from the other regions also reported variability in the prevalence of these mutations. In Europe, the observed percentage of A2143G was 44% to 67%, and from 23% to 33% for A2142G.26,27 In Japan, 90% of H. pylori isolates showed A2143G mutation.28 In U.A.E., 60% of A2143G and 40% of A2142G mutations were observed in clarithromycin-resistant isolates.29 In Korea, 71% of resistant isolates showed A2143G whereas 29% showed A2142G.30 A recent study from Turkey reported 33.4% A2142G and 45.8% of A2143G in clarithromycin resistance isolates.5 Conversely, data from US studies reported the high frequency of A2142G (53%) as compared to A2143G (45%).31
The clinical importance of these mutations has been studied extensively. Research have shown that A2142G mutation was associated with the increased clarithromycin MIC as compared to A2143G, and the presence of either mutation increased the likelihood of treatment failure. The study of Lee et al31 and Yakoob et al32 reported the low eradication rates of H. pylori in the presence of these mutations.
In this study, the overall prevalence of genotypic and phenotypic clarithromycin-resistant due to A2142G, A2143G, and A2143C was 48.2%, of which the primary resistance rate was 39.6%. Such a high percentage of primary resistance was beyond the standard accepted range, which is less than 15 to 20%.17 In this situation, it is advised to perform clarithromycin susceptibility testing before the initiation of treatment. The prevalence of primary clarithromycin resistance in our study is higher than that reported in Malaysia (2.1%),33 Germany (2.2%),34 Canada (less than 4%),35 Hong-Kong (4.5%),36 Korea (5% to 6%),37 Europe (9.9%),38 USA (10% to 15%),39 Iran (17%),40 and in Turkey (24.8%).41 This geographical variability reflects the local consumption of antibiotics. Frequent consumption of macrolide not only in the management of H. pylori infection but also in the treatment of respiratory tract diseases, resistance to clarithromycin has been surfaced in many regions of the world.42 A recent study by Klein et al43 reported that from 2000 to 2015 antibiotics consumption in Pakistan has been increased by 65% from 800 million defined daily doses (DDD) to 1.3 billion. Moreover, the usage of macrolides (clarithromycin) 12% of total DDD has been increased by 119%. High consumption of macrolides has been resulting in high levels of primary clarithromycin resistance in this region.
This study also reported the two new features of domain V including a new MboII RFLP pattern and around 1.2 kb long amplicons which were further investigated using DNA sequencing. Sequencing showed a new mutation A to G at position 1761 which created a new MboII restriction pattern. A previous study also reported a new restriction pattern of domain V with MboII, ie, 505 bp, 205 bp, and 692 bp fragments due to G to A change at position 1939 in Chilean clarithromycin-resistant isolates.44 In the present study, the new RFLP pattern was obtained from an isolate that showed an intermediate resistance.
DNA sequencing also indicated multiple point mutations and clarithromycin resistance-associated mutations A2142G, A2143G, and A2143C. Mutation A2143C is a rare substitution. So far, this mutation has not been observed in any H. pylori clinical isolates in Pakistan. Recent study from Korea45 reported this mutation and its association with clarithromycin resistance. Moreover, mutation T2182C which confers clarithromycin-resistant phenotype in H. pylori isolates of Bangladesh,46 and Korea47 also seen in the present study in four samples. However, the association of T2182C with clarithromycin resistance in H. pylori clinical isolates is still unclear in this region. Further studies are required to investigate the role of T2182C in Pakistan. This study also found other mutations like A1821G, G1826A, and T1830C which were previously reported in clarithromycin sensitive and resistant isolates of H. pylori from Bangladesh.46
Besides the known domain V mutations, 138 new mutation points also appeared in the strains that showed intermediate resistance. A study by Gomez et al48 reported that “the ribosomal mutations promote the evolution of antibiotic resistance”. Accumulation of mutations in domain V which is the target site of many antibiotics may make H. pylori more prone to develop resistance against multiple antibiotics, and it is also possible that the intermediate resistance phenotype is the initial stage towards the development of complete resistance. In addition to this, self-medication and excessive consumption of antibiotics have been reported in Pakistan,43 it is also conceivable that to sustain in the multidrug environment H. pylori might have developed such ribosomal RNA mutations.
Conclusion
In conclusion, H. pylori 23S rRNA domain V mutations exhibited wide diversity. The presence of such a large number of multiple point mutations reveals the genetic heterogeneity of H. pylori strains in this part of the world and may indicate the existence of a different molecular mechanism to survive in the multi drugs surroundings. The rate of primary clarithromycin resistance is also alarming. Therefore, it is mandatory to customize the first-line therapy on the information of the individual H. pylori antibiotic resistance profile. Further research on the molecular mechanism of antibiotic resistance in H. pylori seems essential at this stage.
Acknowledgments
We are thankful to Dr. Sajida Qureshi, Dr. Shahriyar Ghazanfar, Dr. Aftab, Dr. Ali Taj from Surgical Unit IV, Civil Hospital, Karachi, and Dr. Arif Siddiqui from Patel Hospital, Karachi, for providing biopsies, endoscopic findings of each patient. We are also thankful to all the staff members of the endoscopy unit for their cooperation and assistance during this work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ng HK, Goh KL, Chuah KH, et al. Sequencing-based detection of 23S rRNA domain V mutations in treatment-naïve Helicobacter pylori patients from Malaysia. J Glob Antimicrob Resist. 2020;23:345–348. doi: 10.1016/j.jgar.2020.10.012.Epub 2020 Nov 1 [DOI] [PubMed] [Google Scholar]
- 2.Albasha AM, Elnosh MM, Osman EH, et al. Helicobacter pylori 23S rRNA gene A2142G, A2143G, T2182C, and C2195T mutations associated with clarithromycin resistance detected in Sudanese patients. BMC Microbiol. 2021;21:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marques AT, Vitor JMB, Santos A, et al. Trends in H. pylori resistance to clarithromycin: from phenotypic to genomic approaches. Microbial Genomics. 2020 Mar;6(3):e000344.doi: 10.1099/mgen.0.000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vazirzadeh J, Falahi J, Moghim S, et al. Molecular assessment of resistance to clarithromycin in Helicobacter pylori strains isolated from patients with dyspepsia by fluorescent in situ hybridization in the center of Iran. Biomed Res Int. 2020 Mar 27;2020:2304173.. doi: 10.1155/2020/2304173.eCollection2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kocazeybek B, Sakli MK, Yuksel P, et al. Comparison of new and classical point mutations associated with clarithromycin resistance in H. pylori strains isolated from dyspeptic patients and their effects on phenotypic clarithromycin resistance. J Med Microbiol. 2019;68(4):566–573. doi: 10.1099/jmm.0.000944 [DOI] [PubMed] [Google Scholar]
- 6.Clinical and laboratory Standards Institute (CLSI). Methods for Antimicrobial Dilutions and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria. 3rd ed. CLSI guideline M45. Wayne, PA: Clinical and Laboratory Standards Institute; 2016. [DOI] [PubMed] [Google Scholar]
- 7.Mattar R, Laudanna AA. Helicobacter pylori genotyping from positive CLOtest in patients with duodenal ulcer. Rev Hosp Clin. 2000;55(5):155–160. doi: 10.1590/S0041-87812000000500001 [DOI] [PubMed] [Google Scholar]
- 8.Versalovic J, Shortridge D, Kibler K, et al. Mutations in 23S rRNA are associated with clarithromycin resistance in Helicobacter pylori. J Antimicrob Chemother. 1996;40:477–480. doi: 10.1128/AAC.40.2.477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chisholm SA, Owen RJ, Teare EL, et al. PCR-based diagnosis of Helicobacter pylori infection and real-time determination of clarithromycin resistance directly from human gastric biopsy samples. J Clin Microbiol. 2001;39:1217–1220. doi: 10.1128/JCM.39.4.1217-1220.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sambrook J, Fritsch EF, Maniatis T. Molecular Cloning: A Laboratory Manual. 2nd ed. New York: Cold Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 11.Atherton JC, Cao P, Peek RM, et al. Mosaicism in vacuolating cytotoxin alleles of H. pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1999;270:17771–17777. doi: 10.1074/jbc.270.30.17771 [DOI] [PubMed] [Google Scholar]
- 12.Pena AJ, Fox JG, Ferraro MJ, et al. Molecular resistance testing of Helicobacter pylori in gastric biopsies. Arch Pathol Lab Med. 2001;125:493–497. doi: 10.5858/2001-125-0493-MRTOHP [DOI] [PubMed] [Google Scholar]
- 13.Chattopadhyay S, Patra R, Ramamurthy T, et al. Multiplex PCR assay for rapid detection and genotyping of H. pylori directly from biopsy specimens. J Clin Microbiol. 2004;42(6):2821–2824. doi: 10.1128/JCM.42.6.2821-2824.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor DE, Ge Z, Purych D, et al. Cloning and sequence analysis of two copies of a 23S rRNA gene from H. pylori and association of clarithromycin resistance with 23S rRNA mutations. Antimicrob Agents Chemother. 1997;41:477–480. doi: 10.1128/AAC.41.12.2621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Veralsovic J, Osato MS, Spakovsky K, et al. Point mutations in the 23S rRNA gene of Helicobacter pylori-associated with different levels of clarithromycin resistance. J Antimicrob Chemother. 1997;40:283–286. doi: 10.1093/jac/40.2.283 [DOI] [PubMed] [Google Scholar]
- 16.Hooi JKY, Lai WY, Ng WK, et al. Global prevalence of H. pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153:420–429. doi: 10.1053/j.gastro.2017.04.022 [DOI] [PubMed] [Google Scholar]
- 17.Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection-the maastricht IV/ florence consensus report. Gut. 2012;61:646–664. doi: 10.1136/gutjnl-2012-302084 [DOI] [PubMed] [Google Scholar]
- 18.Gehlot VS, Mahanta AK, Mukhopadhyay KD, et al. Low level of clarithromycin-resistant H. pylori isolates with an A2143G point mutation in the 23S rRNA gene in North India. J Glob Antimicrob Resist. 2016;6:39–43. doi: 10.1016/j.jgar.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 19.Yakoob J, Jafri W, Abid S, et al. Role of rapid urease test and histopathology in the diagnosis of Helicobacter pylori infection in a developing country. BMC Gastroenterol. 2005;5:38. doi: 10.1186/1471-230X-5-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yakoob J, Abbas Z, Khan R, et al. Prevalence of non-Helicobacter pylori species in patients presenting with dyspepsia. BMC Gastroenterol. 2012;12:3. doi: 10.1186/1471-230X-12-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rasheed F, Campbell BJ, Alfizah H, et al. Analysis of clinical isolates of H. pylori in Pakistan reveals high degrees of pathogenicity and high frequencies of antibiotic resistance. Helicobacter. 2014;19:387–399. doi: 10.1111/hel.12142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tran VH, Ha TMT, Le PTQ, et al. Characterization of point mutations in domain V of 23S rRNA gene of clinical strains of H. pylori and clarithromycin-resistant phenotype in central Vietnam. J Glob Antimicrob Resist. 2018;16:87–91. doi: 10.1016/j.jgar.2018.09.012 [DOI] [PubMed] [Google Scholar]
- 23.Nyi KN, Soe AM, Htut ZM. Molecular detection of genotypic clarithromycin-resistant strains and its effect on the eradication rate of concomitant therapy in H. pylori infection. GastroHep. 2021;00: 1-7. doi: 10.1002/ygh2.476 [DOI] [Google Scholar]
- 24.Khashei R, Dara M, Bazargani A, et al. The high rate of A2142G point mutation associated with clarithromycin resistance among Iranian H. pylori clinical isolates. APMIS. 2016;124(9):787–793. doi: 10.1111/apm.12567 [DOI] [PubMed] [Google Scholar]
- 25.Zhen-Hua Z, De-qiang H, Yong X, et al. Characterization of 23S rRNA gene mutation in primary and secondary clarithromycin-resistant H. pylori strains from East China. Turk J Gastroenterol. 2013;24:5–9. doi: 10.4318/tjg.2013.0525 [DOI] [PubMed] [Google Scholar]
- 26.Van-doorn LJ, Glupczynski Y, Kusters JG, et al. Accurate prediction of macrolide resistance in Helicobacter pylori by a PCR line probe assay for detection of mutations in the 23S rRNA gene: multicentre validation study. Antimicrob Agents Chemother. 2001;45:1500–1504. doi: 10.1128/AAC.45.5.1500-1504.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alacorn T, Domingo D, Prieto N, et al. PCR using 3ʹ-mismatched primers to detect A2142C mutation in 23S rRNA conferring resistance to clarithromycin in Helicobacter pylori clinical isolates. J Clin Microbiol. 2000;38:923–925. doi: 10.1128/JCM.38.2.923-925.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rimbara E, Noguchi N, Kijima H, et al. Mutations in the 23S rRNA gene of clarithromycin-resistant Helicobacter pylori from Japan. Int J Antimicrob Agents. 2007;30:250–254. doi: 10.1016/j.ijantimicag.2007.04.009 [DOI] [PubMed] [Google Scholar]
- 29.Alfaresi MS, Elkoush AA. Characterization of clarithromycin resistance in isolates of Helicobacter pylori from the U. A. E. Indian J Gastroenterol. 2010;29:116–120. doi: 10.1007/s12664-010-0034-z [DOI] [PubMed] [Google Scholar]
- 30.Lee HK, Chae HS, Kang JO, et al. Multicentre study for the frequency of 23S rRNA point mutations associated with clarithromycin resistance in H. pylori in Korea. Korean J Clin Microbiol. 2008;11:12–15. doi: 10.5145/KJCM.2008.11.2.84 [DOI] [Google Scholar]
- 31.Lee HJ, Kim JI, Cheung DY, et al. Eradication of H. pylori according to 23S ribosomal RNA point mutations associated with clarithromycin resistance. J Infect Dis. 2013;208:1123–1130. doi: 10.1093/infdis/jit287 [DOI] [PubMed] [Google Scholar]
- 32.Yakoob J, Jaffari W, Abbas Z, et al. Risk factors associated with H. pylori infection treatment failure in a high prevalence area. Epidemiol Infect. 2011;139:581–590. doi: 10.1017/S0950268810001226 [DOI] [PubMed] [Google Scholar]
- 33.Ahmad N, Zakaria WR, Abdullah SA, et al. Characterization of clarithromycin resistance in Malaysian isolates of Helicobacter pylori.. World J Gastroenterol. 2009;15:3161–3165. doi: 10.3748/wjg.15.3161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolle K, Leodolter A, Malfertheiner P, et al. Antibiotic susceptibility of Helicobacter pylori in Germany: stable primary resistance from 1995 to 2000. J Med Microbiol. 2002;51:705–709. doi: 10.1099/0022-1317-51-8-705 [DOI] [PubMed] [Google Scholar]
- 35.Fellone CA. Epidemiology of the antibiotic resistance of Helicobacter pylori in Canada. Can J Gastroenterol. 2000;14:879–882. doi: 10.1155/2000/562159 [DOI] [PubMed] [Google Scholar]
- 36.Ling TKW, Leung WK, Lee CC, et al. The antimicrobial susceptibility of Helicobacter pylori in Hong Kong (1997–2001). Helicobacter. 2002;7:327–329. doi: 10.1046/j.1523-5378.2002.00101_1.x [DOI] [PubMed] [Google Scholar]
- 37.Kim JJ, Reddy R, Lee M, et al. Analysis of metronidazole, clarithromycin, and tetracycline resistance of H. pylori isolates from Korea. J Antimicrob Chemother. 2001;47:459–461. doi: 10.1093/jac/47.4.459 [DOI] [PubMed] [Google Scholar]
- 38.Lerang F, Moum B, Haug JB, et al. Highly effective twice-daily triple therapies for Helicobacter pylori infection and peptic ulcer disease: does in vitro metronidazole resistance have any clinical relevance? Am J Gastroenterol. 1997;92:248–253. [PubMed] [Google Scholar]
- 39.Laine L, Fennerty MB, Osato M, et al. Esomeprazole-based Helicobacter pylori eradication therapy and the effect of antibiotic resistance: results of three US multicenter, double-blind trials. Am J Gastroenterol. 2000;95:3393–3398. doi: 10.1111/j.1572-0241.2000.03349.x [DOI] [PubMed] [Google Scholar]
- 40.Mohammedi M, Doroud D, Massarrat S, et al. Clarithromycin resistance in Iranian Helicobacter pylori strains before the introduction of clarithromycin. Helicobacter. 2003;8:79–80. [DOI] [PubMed] [Google Scholar]
- 41.Kocazeybek B, Tokman HB. Prevalence of primary antimicrobial resistance of H. pylori in Turkey: a systematic review. Helicobacter. 2015. doi: 10.1111/hel.12272 [DOI] [PubMed] [Google Scholar]
- 42.Ghotaslou R, Leylabadlo HE, Asl YM. Prevalence of antibiotic resistance in H. pylori: a recent literature review. World J Methodol. 2015;5:164–174. doi: 10.5662/wjm.v5.i3.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klein EY, VanBoeckel TP, Martinez EM, et al. Global increase, and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci. 2018;115(15):E3463–E3470. doi: 10.1073/pnas.1717295115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garrido L, Toledo H. Novel genotypes in Helicobacter pylori involving domain V of the 23S rRNA gene. Helicobacter. 2007;12(5):505–509. doi: 10.1111/j.1523-5378.2007.00506.x [DOI] [PubMed] [Google Scholar]
- 45.Seo SI, Do BJ, Kang JG, et al. Helicobacter pylori eradication according to sequencing-based 23S rRNA point mutation associated with clarithromycin resistance. J Clin Med. 2020;9:54. doi: 10.3390/jcm9010054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khan R, Nahar S, Sultana J, et al. T2182C mutation in 23S rRNA is associated with clarithromycin resistance in H. pylori isolates obtained in Bangladesh. Antimicrob Agents Chemother. 2004;48(9):3567–3569. doi: 10.1128/AAC.48.9.3567-3569.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim KS, Kang JO, Eun CS, et al. Mutations in the 23S rRNA gene of Helicobacter pylori-associated with clarithromycin resistance. J Korean Med Sci. 2002;17:599–603. doi: 10.3346/jkms.2002.17.5.599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gomez JE, Kaufmann-Malaga BB, Wivagg CN, et al. Ribosomal mutations promote the evolution of antibiotic resistance in a multidrug environment. eLife. 2017;6:e20420. doi: 10.7554/eLife.20420 [DOI] [PMC free article] [PubMed] [Google Scholar]