Abstract
Background
Acne vulgaris is a skin problem affecting many people of different ages. Phototherapy is one of the acne treatment options. The aim of the study was to assess the effect of near-infrared low-level laser therapy on acne lesions.
Materials and Methods
The prospective study involved a total number of 27 women, aged 18 to 45 years, with mild to severe acne. All the participants underwent a series of six treatments with the use of a 785 nm low-level laser with the power density 80mW/cm2, performed every two weeks. The analysis of the effectiveness of the performed procedures was based on sebumetric examination, photographic documentation and assessment of the change in the number of acne lesions.
Results
Significant improvements in acne lesions (assessed as non-inflammatory and inflammatory lesion counts) and a significant decrease in skin sebum excretion were observed after the treatment. No adverse effects were reported.
Conclusion
A series of six treatments using a near-infrared low-level laser represents a safe and effective non-invasive therapy option for acne vulgaris.
Keywords: low-level laser therapy, acne, near infrared, sebum
Introduction
The research conducted in 2010 for the Global Burden of Disease Study shows that acne vulgaris is the eighth most commonly diagnosed skin disease. Considering all age groups, it affects almost 10% of the world’s population.1 More and more often, acne eruptions persist up to the fifth decade of life as the so-called “adult acne”.2,3
Acne eruptions, their causes, severity, location and impact on mental health of patients are a serious therapeutic problem. Acne vulgaris treatment usually includes systemic or topical therapies and possibly supportive measures. The latter include, for example, light therapy.4 Light therapy offers many options that support the treatment of acne vulgaris. There are high- and low-power lasers, intense pulsed light or LED lamps.5,6 In our study, we assessed the effectiveness of treatments using a laser representing a group of low-energy devices.
LLLT (Low-Level Laser Therapy) involves the use of devices emitting radiation with a maximum power of 500 mW. Considering that the first Food and Drug Administration (FDA) authorization for the use of LLLT in dermatological therapy, specifically in the treatment of ulcers, was only issued in 2002, it may be concluded that this type of treatment is still a developing branch of phototherapy.7 The photon beam produced during the procedure is absorbed by tissues and transformed into mitochondria with intracellular energy. This phenomenon is called photobiomodulation (PBM). The action of light induces an enhancement of cell signaling and the synthesis of growth factors, and reduces oxidative stress.8 As a result, this type of therapy stimulates physiological regenerative processes in irradiated structures, and has anti-inflammatory and antibacterial effects. The last two are the basis for the use of LLLT/PBM in acne-reducing treatments.9 Particular attention should also be paid to the action of porphyrins produced within the hair-sebaceous unit by anaerobic Cutibacterium acnes. Porphyrins, as photoactive compounds, can be excited by light, leading to the production of reactive oxygen species, which in turn is highly toxic to the bacteria described.10
The aim of the study was to determine whether the treatment method would improve the skin condition of patients with acne vulgaris, in terms of reduction of acne lesions and decrease in the amount of sebum produced. The phototherapy used in our research was not associated with any other form of treatment, whether systemic or topical. However, it is possible to use low-power phototherapy in combination with appropriately selected pharmacological supportive treatment.
The use of a low-level laser in our study was dictated by a search for alternative methods of treating acne vulgaris, with potentially fewer side effects as compared to other therapeutic options, such as antibiotics, oral or topical retinoids. Moreover, an additional factor prompting the analysis of the effectiveness of the low-level laser in the treatment of acne lesions was the relatively small number of studies with a similar profile published so far.
Materials and Methods
For the study, we recruited women with mild to severe acne according to the IGA (Investigator’s Global Assessment) scale, where the severity of acne and the type of lesions assigned to it are presented in Table 1.11–13
Table 1.
Investigator’s Global Assessment Scale of Acne Severity11–13
| Acne Severity Scale | Type of Lesions |
|---|---|
| 0 Clear skin | No inflammatory and non-inflammatory lesions |
| 1 The skin is almost unchanged | Few comedones and ≤ 1 small inflammatory lesion |
| 2 Mild severity | A dozen comedones, ≤ several inflammatory lesions |
| 3 Moderate severity | Many comedones, > several inflammatory lesions, ≤ 1 nodule |
| 4 Severe severity | Many comedones and inflammatory lesions, ≤ several nodules and cysts |
All persons signed their informed consent to participate in the research procedure and to publish the data. The study was positively recommended by the bioethics committee. All experimental protocols were approved by the Medical University of Lodz Bioethics Committee. The study complies with the Declaration of Helsinki.
All the participants underwent a series of six treatments, performed every two weeks. The analysis of the effectiveness of the performed procedures was based on sebumetric examination, photographic documentation and assessment of the change in the number of acne eruptions, such as comedones, papules, pustules and post-inflammatory hyperpigmentation.
Before commencement of the tests, sebumetric measurements were performed on each female probe. Sebumeter (Courage + Khazaka electronic GmbH, Germany) is a device used to assess the degree of skin greasiness and the activity of sebaceous glands. For the measurement, a special head was applied to the skin for 30 seconds with a tape, which absorbs sebum. The measurement was repeated after the third and sixth treatments.
Photos, included in the photographic documentation, were taken before the procedure and two weeks after the end of the whole therapy.
The evaluation of the effectiveness of the therapy in terms of the number of lesions was carried out after the sixth treatment using a low-level laser as compared to the evaluation made on the first visit.
Each treatment involved irradiation of the skin affected by acne lesions with a low-level laser (Vitalaser®, Vitalaser Hannover GmbH). The radiation exposure time was 10 minutes. During the procedure, a device with a power of 360 mW emits infrared radiation with a wavelength of 785 nm and a power density of 80 mW/cm2. According to the protocol requirements, 27 individuals completed the observation.
All methods were carried out in accordance with relevant guidelines and regulations.
The sebumetric measurement of the forehead and the right cheek, depending on the time of measurement, was compared by an analysis of variance for repeated measurements. Fisher’s test was used as a post-hoc test, and a linear trend test was also carried out.
The number of lesions and IGA scales, depending on the measurement date, were compared by the t-student test for dependent variables.
Relationships between the forehead and right cheek sebumetric measurements, and the number of lesions and IGA were analyzed by estimating Pearson’s linear correlation coefficients.
Test probability at p < 0.05 was considered significant, and test probability at p < 0.01 was considered highly significant.
Results
The study involved a total number of 27 women, aged 18 to 45 years.
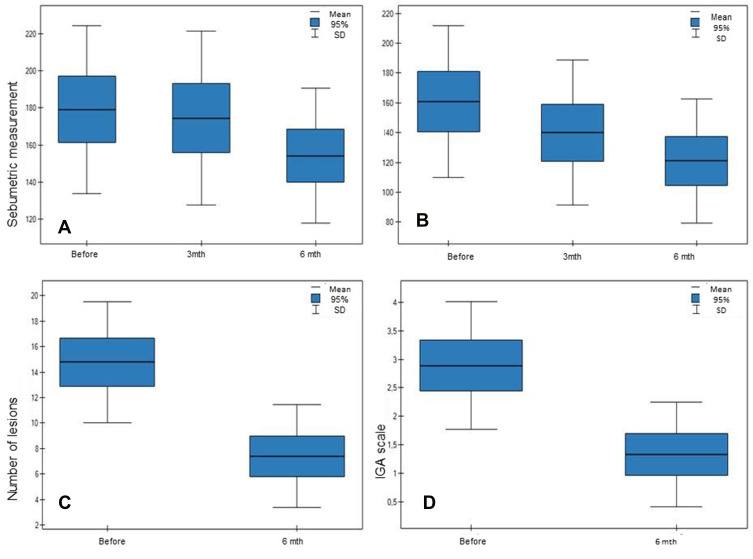
A series of six treatments using a low-level laser ultimately resulted in a statistically significant reduction in the secreted sebum. Considering the values recorded on the forehead, the highest average of the results of 179.1 was obtained before the beginning of the study, after three treatments, there was no significant (p > 0.05) decrease to the value of 174.5, whereas a high (p < 0.01) decrease was observed in the period between the third and sixth treatment. An average of 154.2 results was obtained at the end of the treatment. Similarly, on the right cheek, the highest value of 160.1 was found before the test. In this area, a highly significant (p < 0.01) decrease in the amount of sebum produced was obtained after three treatments and between the third and sixth laser exposure. The average results recorded then were 140 and 121.1, respectively (Figure 1).
Figure 1.
(A) Forehead sebumetric measurement. (B) Sebumetric measurement on the right cheek. (C) Number of lesions. (D) IGA scale.
In the case of a series of six treatments involving irradiation by low-level laser, statistically significant (p < 0.01) differences were also observed for the number of acne eruptions and the IGA scale. Both indicators decreased between the period before the beginning of the study and after six treatments. The average number of non-inflammatory lesions in the form of blackheads before the study was 23 (SD = 8093), while after the treatment series only 10 (SD = 6087). Taking into account inflammatory acne eruptions, the average amount calculated before the start of treatments was 12 (SD = 5483) and 9 (SD = 5078) for pustules and papules, respectively. These values decreased on average to 4 in the case of both pustular (SD = 2977) and papular (SD = 3067) lesions (Figures 2 and 3).
Figure 2.
Patient no. 1, a 19-year-old woman, before commencement of the study and two weeks after completion of the series of six treatments using a low level laser.
Figure 3.
Patient no. 2, a 19-year-old woman, before commencement of the study and two weeks after completion of the series of six treatments using a low level laser.
Prior to the study, significant (p < 0.05, r=0.4183; 0.4598) positive correlations were found between all measurable right-cheek values. It follows that the high sebumetric results were associated with a significant amount of acne eruptions and higher IGA scale values. For measurements made on the forehead, those correlations were lower and not significant (p > 0.05, r=0.2898; 0.2668).
After a series of six treatments, all previous correlations became smaller and insignificant (p > 0.05), r=0.2356; 0.1867; −0.0347). An important (p < 0.05, r = 0.3832) remained only the correlation between the amount of acne eruptions and the result from the measurement of the level of sebum secreted on the forehead.
Discussion
The ethiopathogenesis of acne is multifactorial. The contributing factors are increased sebum production, abnormal follicular keratinization, cutibacterium acnes overgrowth within the hair follicles, and inflammatory mediator release. A successful treatment should focus on several causative agents.
In the study, the procedures were performed with a low-level laser emitting near-infrared radiation, with a wavelength of 785 nm. As a result of a series of treatments, a highly significant (p < 0.01) change in the values determining the total number of acne eruptions and the severity of the disease according to the IGA scale were obtained.
The antibacterial effect was proved for light treatments, especially those based on blue light application.14 That is an approach to limit systemic antibiotic use in acne since administration of this group of medications may be associated with a variety of adverse outcomes including bacterial resistance and disruption of the microbiome. One of the mechanisms through which phototherapy affects acne is the absorption of light by porphyrins, which are produced by Cutibacterium acnes as a part of normal metabolism and which act as specific endogenous photosensitizers. This process triggers a photochemical reaction. Reactive free radicals and forms of singlet oxygen are produced, which in turn leads to the destruction of bacteria.14,15 The effect was also observed in strains resistant to antibiotic substances, such as clindamycin, tetracycline or erythromycin. This gives new, distinct therapeutic possibilities for patients in whom antibiotic therapy does not bring the expected results.16
Previous studies have also shown a positive interaction between light, specifically the wavelength corresponding to red radiation, and the release of anti-inflammatory cytokines, which is one of the mechanisms in the pathogenesis of acne.17 Colonization and proliferation of Cutibacterium acnes have been proven to be crucial for the development of inflammation.18 The peptide cell wall of Cutibacterium acnes initiates the release of cytokines such as IL-α, IL-1β, IL-8 and TNF-α from monocytes, which causes the development of an inflammatory response in the skin.19,20 It is worth mentioning here that compared to blue light, the red spectrum is characterized by deeper penetration into the irradiated tissues,21 and in our study, near-infrared was used which is known to have ever deeper penetration. Research on the use of low-energy LED radiation from the field of red light, conducted by Li et al demonstrated anti-inflammatory effect of the method used, by lowering the level of interleukin IL-α.22 It follows that therapy with low levels of red LED light can provide beneficial anti-inflammatory effects, which allows its use in anti-acne treatments.23–25 Similar effects were also obtained in studies using blue light. Tests performed on cell cultures showed a reduction in the production of pro-inflammatory interleukin-1α and ICAM-1 (intercellular adhesion molecule).21
It has also been proven that phototherapy can significantly affect the activity of sebaceous glands and reduce the keratosis of the hair follicles outlets.26,27 Li et al22 conducted a study on the biological effect of red LED radiation in acne, using an in vitro model and obtained normalization of keratinization within the sebaceous glands.22 In turn, Jung et al28 used light-emitting diodes (LEDs) emitting both blue (415nm) and red (630nm) light to verify their effect on lipid production in human sebaceous cells in vitro. They showed that blue light inhibits their proliferation and red radiation reduces lipid production, which is one of the acne pathogenetic factor.28
The data for infrared acne therapy are sparse. A clinical trial of infrared 1320-nm Nd:YAG laser therapy was carried out by Orringer et al.29 It was a split-face study, and there was no significant difference between the two sides in terms of inflammatory lesions count after the treatments, however, the authors described the effectiveness of the therapy in reducing non-inflammatory lesions. In our study, the near-infrared low level laser was used, and the reduction was seen not only in non-inflammatory lesions but also in inflammatory ones. The average number of non-inflammatory lesions in the form of blackheads before the study was 23, while after the treatment series only 10. Taking into account inflammatory acne eruptions, the average amount calculated before the start of treatments was 12 and 9 for pustules and papules, respectively. These values decreased on average to 4 in the case of both pustular and papular lesions. In our study, the used 785 nm is close to red light; hence, the effect may be more similar to red light, where the anti-inflammatory effect was observed.17 Paithankar et al30 used a 1450 nm laser to reach the depth of the sebaceous glands and a statistically significant decrease in acne lesions was reported.
Aziz-Jalali et al31 conducted a study comparing the effects of low-level laser therapy, including a device emitting a beam of red (630nm) and infrared (890nm) light. As a result of the performed procedure, a significant reduction in the number of acne lesions was observed on the side exposed to radiation with a wavelength of 630 nm, and a statistically insignificant improvement (p > 0.05) after irradiation with 890 nm beam. The discrepancy between the results obtained by Aziz-Jalali and those recorded in our study may be explained by a different wavelength of laser that we applied, as well as the number and frequency of procedures performed. Aziz-Jalali et al carried out a series of 12 treatments performed twice a week. In turn, our study covered only 6 procedures; however, they were repeated every 14 days, what is more comfortable for patients. In addition, no other form of therapy was implemented in the patients’ own study. In turn, in the Aziz-Jalali study, all the patients were treated topically with 2% clindamycin on both sides of the face.31
Research on the effectiveness of low-energy radiation was also conducted using a combination of blue LED (415nm) and near-infrared (830nm) light. Sadick32 performed a series of eight treatments twice a week. Nevertheless, this type of acne combination therapy has less satisfactory end effects than using a combination of blue and red light; however, the limitation of the study is small number of participants who completed it, which is 11. The author described the reduction of non-inflammatory lesions,32 which was also reflected by our results. In our study, a reduction in all types of acne lesions and a reduction in sebaceous gland activity (assessed by sebum measurement) were observed. In turn, in the blue and red LED therapy, the authors received a better therapeutic effect within inflammatory than non-inflammatory lesions.15,33
Apart from the lack of any form of procedure other than LLLT, an additional advantage of the therapy used in our study is undoubtedly the lack of side effects accompanying the irradiation. There are many reports confirming that the IPL procedure is accompanied by pain and burning, as well as significant postoperative redness of the skin.34,35 In our study, as it has already been emphasized, no such side effects were found.
It also seems very important that all the above-mentioned studies, including LED, IPL or LLLT, were based on counting acne lesions and assessing the final effect based on photographic documentation.15,31–34,36 In our study, due to sebumetric measurement, the effect of the performed procedures on the activity of sebaceous glands was also analyzed. Thus, it was proved that a series of six treatments using a low level near-infrared laser, apart from reducing all types of acne lesions, finally resulted in a statistically significant reduction in the amount of sebum secreted, which confirms the conclusions drawn earlier based on the research conducted by Jung et al in vitro study.28
The limitations of the study were the number of participants and the time of observation. Taking into consideration more participants maybe, we would be able to see side effects. Also, only women took part in our research. Because of acne recurrence, the time of observation is planned to be extended.
Conclusions
To sum up, a series of six treatments using a low-level laser for non-pharmacological reduction of acne lesions ultimately give satisfactory final results. It strongly encourages further research in the field of low-level laser therapy as it seems to be a good alternative to limit systemic antibiotic use in acne.
Funding Statement
This research was funded by the Medical University of Lodz (grant No. 503/3-066- 02/503-31-001 to EB).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Heng AHS, Chew FT. Systematic review of the epidemiology of acne vulgaris. Sci Rep. 2020;10:5754. doi: 10.1038/s41598-020-62715-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams C, Layton AM. Persistent acne in women: implications for the patient and for therapy. Am J Clin Dermatol. 2006;7(5):281–290. doi: 10.2165/00128071-200607050-00002 [DOI] [PubMed] [Google Scholar]
- 3.Rivera R, Guerra A. Management of acne in women over 25 years of age. Actas Dermosifiliogr. 2009;100(1):33–37. doi: 10.1016/S0001-7310(09)70054-7 [DOI] [PubMed] [Google Scholar]
- 4.Castillo DE, Keri JE. Chemical peels in the treatment of acne: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:365–372. doi: 10.2147/CCID.S137788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erkiert-Polguj A, Szymańska A, Zduńska K, Haliba A, Budzisz E, Rotsztejn H. Non-pharmacological acne treatment. Part II: light-based therapies. Derm Prakt. 2016;6(47):21–29. [Google Scholar]
- 6.Bariberi JS, Spaccarelli N, Margolis DJ, James WD. Approaches to limit systemic antibiotic use in acne: systemic alternatives, emerging topical therapies, dietary modification, and laser and light-based treatments. J Am Acad Dermatol. 2019;80(2):538–549. doi: 10.1016/j.jaad.2018.09.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim WS, Calderhead RG. Is light-emitting diode phototherapy (LED-LLLT) really effective? Laser Ther. 2011;20(3):205–215. doi: 10.5978/islsm.20.205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glass GE. Photobiomodulation: the clinical applications of low-level light therapy. Aesthet Surg J. 2021;41(6):723–738. doi: 10.1093/asj/sjab025 [DOI] [PubMed] [Google Scholar]
- 9.Sawhney MK, Hamblin MR. Low-level light therapy (LLLT) for cosmetics and dermatology. Proc SPIE. 2014;8932:89320X–1. [Google Scholar]
- 10.Ashkenazi H, Malik Z, Harth Y, Nitzan Y. Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light. FEMS Immunol Med Microbiol. 2003;35:17–24. doi: 10.1111/j.1574-695X.2003.tb00644.x [DOI] [PubMed] [Google Scholar]
- 11.Dreno B, Fischer TC, Perosino E, et al. Expert opinion: efficacy of superficial chemical peels in active acne management – what can we learn from the literature today? Evidence-based recommendations. J Eur Acad Dertmatol Venerol. 2011;25(6):695–704. doi: 10.1111/j.1468-3083.2010.03852.x [DOI] [PubMed] [Google Scholar]
- 12.Kainz JT, Berghammer G, Auer-Grumbach P, et al. Azelaic acid 20 % cream: effects on quality of life and disease severity in adult female acne patients. J Dtsch Dermatol Ges. 2016;14(12):1249–1259. [DOI] [PubMed] [Google Scholar]
- 13.Szymańska A, Budzisz E, Erkiert-Polguj A. Efficacy of 30% azelaic acid peel in the nonpharmacological treatment of facial acne. J Dermatol Treat. 2021;32(3):291–296. doi: 10.1080/09546634.2019.1657222 [DOI] [PubMed] [Google Scholar]
- 14.Avci P, Gupta A, Sadasivam M, et al. Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg. 2013;32(1):41–52. [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SY, You CE, Park MY. Blue and red light combination LED phototherapy for acne vulgaris in patients with skin phototype IV. Lasers Surg Med. 2007;39(2):180–188. doi: 10.1002/lsm.20412 [DOI] [PubMed] [Google Scholar]
- 16.Dunn K, Fassih A, Miksa D, Mohammed N, Desai P, Southall M. Antibacterial effect of low-level blue light on Propionibacterium acnes and antibiotic-resistant P acnes. J Am Acad Dermatol. 2019;81(4, suppl.1):AB433–AB433, 8461. Poster abstracts. [Google Scholar]
- 17.Cunliffe WJ, Goulden V. Phototherapy and acne vulgaris. Br J Dermatol. 2000;42:855–856. doi: 10.1046/j.1365-2133.2000.03528.x [DOI] [PubMed] [Google Scholar]
- 18.Shaheen B, Gonzalez M. Acne sans P. acnes. J Eur Acad Dermatol Venereol. 2013;27:1–10. doi: 10.1111/j.1468-3083.2012.04516.x [DOI] [PubMed] [Google Scholar]
- 19.Yoon JY, Kwon HH, Min SU, Thiboutot DM, Suh DH. Epigallocatechin-3-gallate improves acne in humans by modulating intracellular molecular targets and inhibiting P. acnes. J Invest Dermatol. 2013;133:429–440. doi: 10.1038/jid.2012.292 [DOI] [PubMed] [Google Scholar]
- 20.Chen Q, Koga T, Uchi H, et al. Propionibacterium acnes-induced IL-8 production may be mediated by NF-kB activation in human monocytes. J Dermatol Sci. 2002;29:97–103. doi: 10.1016/S0923-1811(02)00013-0 [DOI] [PubMed] [Google Scholar]
- 21.Schnitkind E, Yaping E, Geen S, Shalita AR, Lee WL. Antiinflammatory properties of narrow band blue light. J Drugs Dermatol. 2006;5:605–610. [PubMed] [Google Scholar]
- 22.Li WH, Fassih A, Binner C, Parsa R, Southall MD. Low-level red LED light inhibits hyperkeratinization and inflammation induced by unsaturated fatty acid in an in vitro model mimicking acne. Lasers Surg Med. 2018;50:158–165. doi: 10.1002/lsm.22747 [DOI] [PubMed] [Google Scholar]
- 23.Downie MM, Sanders DA, Kealey T. Modelling the remission of individual acne lesions in vitro. Br J Dermatol. 2002;147:869–878. doi: 10.1046/j.1365-2133.2002.04946.x [DOI] [PubMed] [Google Scholar]
- 24.Guy R, Green MR, Kealey T. Modeling acne in vitro. J Invest Dermatol. 1996;106:176–182. doi: 10.1111/1523-1747.ep12329907 [DOI] [PubMed] [Google Scholar]
- 25.Guy R, Kealey T. The effects of inflammatory cytokines on the isolated human sebaceous infundibulum. J Invest Dermatol. 1998;110:410–415. doi: 10.1046/j.1523-1747.1998.00143.x [DOI] [PubMed] [Google Scholar]
- 26.Rotunda AM, Bhupathy AR, Rohrer TE. The new age of acne therapy: light, lasers, and radiofrequency. J Cosmet Laser Ther. 2004;6(4):191–200. doi: 10.1080/14764170410008124 [DOI] [PubMed] [Google Scholar]
- 27.Sadick NS. Handheld LED array device in the treatment of acne vulgaris. J Drugs Dermatol. 2008;7(4):347–350. [PubMed] [Google Scholar]
- 28.Jung YR, Kim SJ, Sohn KC, et al. Regulation of lipid production by light-emitting diodes in human sebocytes. Arch Dermatol Res. 2015;307(3):265–273. doi: 10.1007/s00403-015-1547-1 [DOI] [PubMed] [Google Scholar]
- 29.Orringer JS, Kang S, Maier L, et al. A randomized, controlled, split-face clinical trial of 1320-nm Nd: YAGlaser therapy in the treatment of acne vulgaris. J Am Acad Dermatol. 2007;56(3):432–438. doi: 10.1016/j.jaad.2006.10.978 [DOI] [PubMed] [Google Scholar]
- 30.Paithankar DY, Ross EV, Saleh BA, Blair MA, Graham BS. Acne treatment with a 1450 nm wavelength laser and cryogen spray cooling. Lasers Surg Med. 2002;31(2):106–114. doi: 10.1002/lsm.10086 [DOI] [PubMed] [Google Scholar]
- 31.Aziz-Jalali MH, Tabaie SM, Djavid GE. Comparison of red and infrared low-level laser therapy in the treatment of acne vulgaris. Indian J Dermatol. 2012;57(2):128–130. doi: 10.4103/0019-5154.94283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sadick N. A study to determine the effect of combination blue (415 nm) and near-infrared (830 nm) light-emitting diode (LED) therapy for moderate acne vulgaris. J Cosmet Laser Ther. 2009;11(2):125–128. doi: 10.1080/14764170902777349 [DOI] [PubMed] [Google Scholar]
- 33.Goldberg DJ, Russell BA. Combination blue (415 nm) and red (633 nm) LED phototherapy in the treatment of mild to severe acne vulgaris. J Cosmet Laser Ther. 2006;8(2):71–75. doi: 10.1080/14764170600735912 [DOI] [PubMed] [Google Scholar]
- 34.Mokhtari F, Shajari A, Iraji F, et al. The effectiveness of adapalene 0.1% with intense pulsed light versus benzoyl peroxide 5% with intense pulsed light in the treatment of acne vulgaris: a comparative study. J Res Med Sci. 2019;24:101. doi: 10.4103/jrms.JRMS_398_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pei S, Inamadar AC, Adya KA, Tsoukas MM. Light-based therapies in acne treatment. Indian Dermatol Online J. 2015;6(3):145–157. doi: 10.4103/2229-5178.156379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joo Y, Kang H, Choi EH, Nelson JS, Jung B. Characterization of a new acne vulgaris treatment device combining light and thermal treatment methods. Skin Res Technol. 2012;18(1):15–21. doi: 10.1111/j.1600-0846.2011.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]