Abstract
Although most patients recover from acute COVID-19, some experience postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection (PASC). One subgroup of PASC is a syndrome called “long COVID-19,” reminiscent of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). ME/CFS is a debilitating condition, often triggered by viral and bacterial infections, leading to years-long debilitating symptoms including profound fatigue, postexertional malaise, unrefreshing sleep, cognitive deficits, and orthostatic intolerance. Some are skeptical that either ME/CFS or long COVID-19 involves underlying biological abnormalities. However, in this review, we summarize the evidence that people with acute COVID-19 and with ME/CFS have biological abnormalities including redox imbalance, systemic inflammation and neuroinflammation, an impaired ability to generate adenosine triphosphate, and a general hypometabolic state. These phenomena have not yet been well studied in people with long COVID-19, and each of them has been reported in other diseases as well, particularly neurological diseases. We also examine the bidirectional relationship between redox imbalance, inflammation, energy metabolic deficits, and a hypometabolic state. We speculate as to what may be causing these abnormalities. Thus, understanding the molecular underpinnings of both PASC and ME/CFS may lead to the development of novel therapeutics.
Keywords: COVID-19, chronic fatigue syndrome, myalgic encephalomyelitis, redox, mitochondria
Acute COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), can be a severe and even fatal disease. Beyond the acute illness, some survivors of COVID-19, even those who are only moderately ill during the acute infection, experience postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection (PASC). They report persisting, debilitating symptoms that last for months (1). In some people, these symptoms may be secondary to COVID-19–induced damage to the lung (hypoxia) and heart (reduced cardiac output) (2), skeletal muscle (3), kidneys (abnormal acid-base or fluid balance), or brain (small infarcts or hemorrhages) (4). However, some of these PASC patients, without apparent organ damage, also have persisting, debilitating symptoms (an illness called “long COVID-19”) that are similar to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) (5).
ME/CFS is a complex, multisystem disorder leading to debilitating symptoms including profound fatigue, postexertional malaise, unrefreshing sleep, cognitive deficits, and orthostatic intolerance. The US Centers for Disease Control and Prevention and the US National Academy of Medicine estimate that 836,000 to 2.5 million people have ME/CFS in the United States alone (6). Many cases occur following what appears to be a common, infectious-like illness. However, diagnostic tests are rarely performed to document the responsible infectious agents. Postinfectious fatigue syndromes also follow in the wake of well-documented acute infections with multiple viruses, bacteria, and even parasites (5).
In this review, we speculate that the symptoms of both long COVID-19 and ME/CFS may stem from redox imbalance—which in turn, is linked to inflammation and energy metabolic defects.
Redox Imbalance Occurs in Both COVID-19 and ME/CFS
Oxidative and Nitrosative Stress.
Oxidative and nitrosative stress have been reported in both acute COVID-19 and ME/CFS. Oxidative stress involves imbalance between reactive oxygen species (ROS) and antioxidant defense mechanisms. Nitrosative stress is characterized by excess reactive nitrogen species (RNS), such as peroxynitrite (ONOO−), generated by reaction of nitric oxide (NO) with superoxide anions (O2·−). NO has important physiological functions (including vasodilation and neurotransmission). However, increased RNS with excessive NO production can be at least as damaging as ROS and also can directly attack several antioxidant enzymes, including catalase (7). Thus, oxidative stress and nitrosative stress are linked bidirectionally.
Like NO, ROS mediates physiologic cellular signaling and defense against pathogens. However, excessive ROS, when not adequately countered by antioxidants, damage cellular components including proteins, lipids, and DNA (8, 9).
Redox Imbalance in Acute COVID-19.
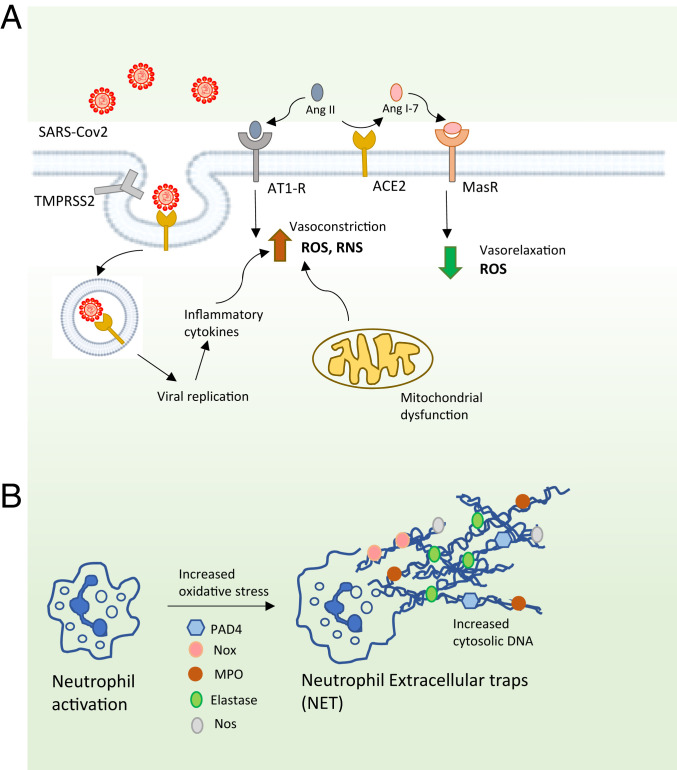
Multiple examples of redox dysregulation have been reported in acute COVID-19, as is typical of many viral infections (10, 11). Overall levels of serum thiols are decreased in the serum of COVID-19 patients (12). As depicted in Fig. 1A, COVID-19 induces redox imbalance, in part because SARS-CoV-2 uses the angiotensin converting enzyme 2 (ACE2) receptor to enter cells (13, 14). This leads to accumulation of O2·− as well as ROS and RNS by inducing mitochondrial dysfunction and production of proinflammatory cytokines (15).
Fig. 1.
Oxidative stress in COVID-19. (A) The ACE2 pathway. SARS-CoV-2 infects cells harboring ACE2 and the protein transmembrane protease, serine 2 (TMPRSS2); together, these molecules prime the viral spike protein S, facilitating its entry by endocytosis. ACE2 converts angiotensin II (Ang II) to angiotensin 1 to 7 (Ang 1–7). This decreases ACE2 and elevates Ang II, which acts through the angiotensin 1 receptors (AT1-Rs), causing accumulation of superoxide radicals (O2•−) leading to hypertension and inhibition of vasodilation. Ang 1–7 binds the G-protein–coupled Mas receptor MasR, mediates vasorelaxation, and decreases O2•− production. SARS-CoV-2 induces formation of reactive oxygen radicals (ROS) and RNS by eliciting mitochondrial dysfunction and production of proinflammatory cytokines. (B) The NETs. NETs are web-like structures extruded from activated neutrophils, comprising proteins assembled on a scaffold of decondensed chromatin, which target invading pathogens. The component proteins include oxidative and proinflammatory enzymes such as NADPH oxidase (Nox), neutrophil elastase, myeloperoxidase (MPO), NOS, and peptidyl arginine deiminase 4 (PAD4), which deaminates arginine to citrulline, resulting in the formation of citrullinated proteins (such as histone H3, causing its dissociation from DNA). Excessive accumulation of NETs causes inflammation and damage in COVID-19.
In a computational study, binding affinity was significantly impaired when the disulfide bonds of both ACE2 and SARS-CoV-2 spike protein, which binds ACE2, were reduced to thiol groups (16). The spike protein has 40 cysteine residues, some of which contribute to the stability of interaction with the ACE2 receptor on the host (17). Analysis of the crystal structure of the spike protein with the ACE2 receptor revealed that the Cys480–Cys488 pair of the spike protein participates directly in binding to the ACE2 (18, 19). Similarly, certain cysteine residues on the ACE2 protein of the host play key roles in the interaction between the two proteins. A disulfide bond between Cys133 and Cys141 is present at the dimer interface, which has been linked to susceptibility to COVID-19 (17). Cattle and swine have a leucine residue at position 133 and are resistant to SARS-CoV-2.
Elderly subjects are more vulnerable to severe COVID-19. A linear oxidation of the plasma cysteine/cystine redox state over the entire age span and that of reduced glutathione/oxidized glutathione (GSH/GSSG) occur after ∼45 y (20). The age-dependent decrease in thiol/disulfide ratio of extracellular fluids could modulate interaction of CoV-2 with the host cell in the airways. This redox-modulated binding is expected to affect the risk of severe infection in an age-dependent manner (21). Similarly, low levels of the antioxidant enzyme, alveolar Type II cell superoxide dismutase 3 (SOD3), in the lungs of the elderly correlate with severity of COVID-19 (12).
Redox Imbalance in ME/CFS.
In people with ME/CFS, there are multiple biomarkers of oxidative stress: reduced levels of antioxidants (22); decreased levels of α-tocopherol (23); increased levels of peroxides and superoxide that correlate with severity of symptoms (24); increased levels of isoprostanes, both at rest and after exercise (25); and reduced levels of thiobarbituric acid reactive substances and malondialdehyde levels, as well as reduced ascorbic acid and glutathione levels (26–30). These markers of redox imbalance also correlate with severity of symptoms (24, 31, 32). Brain magnetic resonance spectroscopy (MRS) reveals elevated levels of ventricular lactic acid consistent with oxidative stress (33–35).
When compared with healthy control subjects, people with ME/CFS also have multiple biomarkers of nitrosative stress: increased inducible nitric oxide synthase (NOS) with consequent increased NO, peroxynitrite, and nitrate, particularly following exercise (36, 37).
Immune responses to oxidized fatty acids (oleic, palmitic, and myristic acids) and markers of lipid peroxidation (such as malondialdehyde, acetylcholine, S-farnesyl-l-cysteine, and several NO-modified amino acids) also are significantly greater in ME/CFS patients as compared with controls (38, 39).
Metabolomic studies in plasma from ME/CFS subjects are consistent with these findings, revealing altered plasma levels of choline, carnitine, and complex lipid metabolites—consistent with oxidative stress and mitochondrial dysfunction (40–43).
Elevated Levels of Prooxidants in COVID-19 and ME/CFS
As summarized in Table 1, increased levels of prooxidants have been reported in both acute COVID-19 and ME/CFS.
Table 1.
Redox-related alterations shared by both COVID-19 and ME/CFS
| Redox-related alteration | COVID-19 | ME/CFS |
| Iron and heme metabolism | Hyperferritinemia (171–174) | Decreased serum transferrin, elevated heme (26, 43) |
| Elevated biliverdin levels (175) | ||
| Decreased bilirubin (176) | ||
| Homocysteine | Increased blood levels (177, 178) | Increased cerebrospinal fluid levels (179) |
| Elevated superoxide levels | Negative correlation between decreased SOD3 in lungs of elderly patients with COVID-19 and disease severity (12) | Decreased expression and activity of SOD (27, 180) |
| Neutrophil response | In severe disease, elevated numbers of neutrophils and a high neutrophil to lymphocyte ratio; high ratio positively correlated with mortality (90, 120, 181); NETs observed | Neutropenia and a reduced oxidative burst (182), possibly secondary to an initially aggressive neutrophil response, had led to neutrophil exhaustion, similar to lymphocyte exhaustion seen (182) |
| NO | NOS2 is significantly up-regulated in patients with severe disease (58) | High levels of NO (27, 38); citrulline, a product of arginine metabolism by NOS, also increased (59) |
| H2S | Survivors have higher serum levels of H2S and higher numbers of circulating lymphocytes (70), perhaps because H2S stimulates T cell proliferation (71) | Dysregulation of H2S may play a role in ME/CFS (73) |
| H2S can induce a torpor-like state in mice (74) | ||
| No studies yet of H2S regulation in humans | ||
| Tryptophan metabolites | Decreased tryptophan, serotonin, and indolepyruvate levels and increased kynurenine, kynurenic acid, picolinic acid, and nicotinic acid (183) | Nicotinamide phosphoribosyl transferase levels altered in peripheral blood mononuclear cells from ME/CFS patients (129) |
| NAD metabolome depressed in SARS-CoV-2–infected cells and patient samples, and levels of NAD biosynthetic enzymes also are elevated in SARS-CoV-2–infected cells, possibly as a compensatory mechanism (184) | ||
| Glutathione | Low blood levels of GSH in severe disease (185); severity of COVID-19 linked to decreased levels of vitamin D (185, 186) | Low GSH levels in the cortex of the brain and plasma (33, 187) |
| Decreased SOD, catalase, glutathione peroxidase, and glutathione reductase activities in erythrocytes (27) | ||
| Cysteine | Cysteine levels decreased in serum, while levels of oxidized cysteine are higher (183) | Low levels of cystine, the oxidized form of cysteine, and increased levels of cystine and methionine (methionine sulfoxide) in the peripheral blood mononuclear cells of people with ME/CFS (188) |
| Cystine and methionine (methionine sulfoxide) increased (183) | ||
| Selenium | Selenium levels low (189) and negatively correlated with recovery (189–191) | Unstudied |
| Vitamin C/ascorbate | Low plasma levels (192) | Low plasma levels (31, 193) |
| NAD metabolism | Nicotinamide phosphoribosyl transferase and nicotinamide riboside kinase increased (194) | Nicotinamide phosphoribosyl transferase levels increased (97) |
| Vitamin E levels | Low serum levels in pregnant women (195) | Decreasing serum levels correlate with severity of symptoms and levels increase in remissions (23, 196) |
| Also, decreased levels in pediatric cases (193) |
Dysregulated Heme and Iron Homeostasis.
Increased levels of free iron in cells (44) and increased ferritin levels (45) both can cause oxidative damage (44). Iron stored in heme molecules is degraded via the bilirubin pathway, an important component of antioxidant defense (46, 47). Evidence of dysregulated heme and iron homeostasis has been reported in acute COVID-19 and ME/CFS (Table 1).
Homocysteine.
Elevated levels of the amino acid homocysteine, seen in both acute COVID-19 and ME/CFS (Table 1), cause increased oxidative stress and are a risk factor for various cardiovascular diseases and dementia. Elevated homocysteine levels may indicate suboptimal activities of reverse transsulfuration enzymes or dysregulation of their cofactors and/or regulators (44, 48, 49).
Neutrophil Extracellular Traps.
Neutrophils attack invading pathogens by forming neutrophil extracellular traps (NETs) and generating both ROS and RNS (50–53) (Fig. 1B). Abnormalities of neutrophil biology have been reported in both acute COVID-19 and ME/CFS (Table 1).
Abnormal Metabolism Involving the Gaseous Signaling Molecules NO and Hydrogen Sulfide.
The major gaseous signaling molecules include NO, carbon monoxide, and hydrogen sulfide (H2S). They play key roles in the regulation of blood pressure, inflammation, and neurotransmission (54, 55). Under physiological conditions, both NO and H2S have anti-inflammatory effects (48, 56). However, both deficient and excess production of these gaseous signaling molecules can create brain pathology, immune dysfunction, and redox imbalance (56, 57).
NO.
NOS2 is significantly up-regulated in patients with severe and critical COVID-19 (58). There is evidence of nitrosative stress and disordered NO metabolism in people with ME/CFS (38). Levels of NO are higher in ME/CFS patients, which can accelerate nitrosative stress (27). Citrulline, a product of arginine metabolism by NOS, also is increased in ME/CFS (59).
H2S.
Normal H2S metabolism protects against inflammation and redox imbalance (48, 60, 61). One of the modes by which H2S functions is by a posttranslational modification termed persulfidation or sulfhydration (48, 62), which prevents irreversible oxidation of proteins (63, 64). H2S metabolism is disrupted in Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease and also, during aging (63, 65–67). H2S inhibits tau-phosphorylation, which may explain, in part, its role in protecting against Alzheimer’s disease (68, 69).
Dysregulated H2S metabolism has been reported in acute COVID-19. Survivors reportedly exhibit higher serum levels of H2S and higher numbers of circulating lymphocytes (70); H2S stimulates T cell proliferation (71). Indeed, exogenous H2S therapy may be beneficial in mild to moderate COVID-19 disease (72).
Dysregulation of H2S may play a role in ME/CFS since the gas can affect adenosine triphosphate (ATP) production from oxidative phosphorylation (73). H2S can induce a torpor-like state in mice (74). However, studies of H2S regulation in people with ME/CFS have not yet been reported.
Altered Levels of Tryptophan Metabolites.
Tryptophan serves as a precursor for nicotinamide adenine dinucleotide (NAD+) biosynthesis, making it important in redox balance. Abnormalities in the pathways by which tryptophan is transformed into serotonin or kynurenine pathway metabolites (75) have been reported in both acute COVID-19 and ME/CFS (Table 1), and can cause both oxidative stress and excitotoxicity (27).
Reduced Levels of Small Molecule Antioxidants in Acute COVID-19 and ME/CFS
As summarized in Table 1, decreased levels of antioxidants have been reported in both acute COVID-19 and ME/CFS. Foremost among these small molecules is glutathione, which helps modulate immune activation (76, 77). Glutathione also enhances vitamin D metabolism (78) and vitamin D, in turn, reciprocally increases glutathione and decreases oxidative stress and levels of inflammatory cytokines and chemokines (79). The antioxidant small molecules also include cysteine, a semiessential amino acid synthesized endogenously via the reverse transsulfuration pathway (80) (SI Appendix, Fig. S1); selenium, an essential micronutrient incorporated into various selenoproteins which have antioxidant roles; vitamin C/ascorbate, which exerts antiviral and immunomodulatory effects (81) and vitamin E compounds, which have free radical scavenging and antiinflammatory activities (82).
Impaired Energy Metabolism in COVID-19 and ME/CFS
Impaired Energy Metabolism in Acute COVID-19.
Mitochondrial dysfunction has long been associated with fatigue (83), causes elevated oxidative stress, and could contribute to the symptoms of fatigue found in both acute COVID-19 and ME/CFS (84).
Mitochondrial dysfunction also has been linked to the pathogenesis of COVID-19. SARS-CoV-2 hijacks mitochondrial function and alters host metabolic pathways and immune response to facilitate pathogenesis. For instance, mitochondrial dysfunction triggered by SARS-CoV-2 causes accumulation of mitochondrial DNA (mtDNA) in the cytosol, leading to mtDNA-induced inflammasome activation and suppression of innate and adaptive immunity (85). The virus interferes with the RIG1-MAVS pathway to decrease type I interferon (IFN) production (86). SARS-CoV-2 infection of white blood cells leads to elevated glycolysis, increased mitochondrial reactive oxygen species (mtROS) production, and dysregulated mitochondrial bioenergetics (87, 88). In this study, the role of redox imbalance secondary to mitochondrial dysfunction in SARS-CoV-2 pathology was apparent; two potent antioxidants reduced viral load and proinflammatory cytokines. Elevated levels of lactate dehydrogenase (LDH) were also reported in COVID-19 (89, 90), which could reflect mitochondrial dysfunction.
Impaired Energy Metabolism in ME/CFS.
Metabolomic studies have reported evidence of impaired ATP production from oxygen, glucose, fatty acids, and amino acids in multiple cell types (41, 42, 91–94). Not just oxidative phosphorylation but also glycolysis—and possibly, the citric acid and urea cycles—are incriminated. In people with ME/CFS, there also is a more general hypometabolic state as previously proposed (73), characterized by depressed levels of most metabolites, as occurs in hibernating animals (41). Later, we speculate as to the cause of this hypometabolic state.
Both structural and functional mitochondrial abnormalities have been found in ME/CFS. Branching and fusion of mitochondrial cristae are observed in muscle biopsies of some patients (84). Although some studies have reported deletions of mtDNA genes, the most extensive controlled study using contemporary technology did not find mtDNA variants that correlated with susceptibility to ME/CFS—although it did find a correlation between specific haplogroups and mtDNA single-nucleotide polymorphisms and specific symptoms (95). Other reports have identified a deficit in Complex V (ATP synthase) activity of the electron transport chain (ETC) in lymphocytes, with a compensatory up-regulation of respiratory capacity (96, 97), and a decrease in mitochondrial membrane potential in CD8+ T cells (98). Serum from ME/CFS patients reportedly contains a factor that induces mitochondrial fragmentation (99).
Clinical studies also indicate mitochondrial dysfunction. People with ME/CFS have significantly higher blood lactate levels after exercise as compared with controls, indicative of reduced oxidative phosphorylation and a switch to anaerobic glycolysis (100–102). Elevated lactate levels also have been reported in the ventricles of ME/CFS patient brains (33–35, 103). As in COVID-19, elevated serum LDH levels also are seen (104). LDH is a critically important enzyme in energy metabolism, catalyzing the bidirectional conversion of lactate to pyruvate and NAD+ to reduced NAD+ (NADH). Thus, an elevated level in the blood of subjects in a resting state could indicate a system struggling to generate energy. Alternatively, the elevated blood levels of LDH could indicate tissue destruction, such as occurs in malignancies or red blood cell hemolysis.
Finally, people with ME/CFS reportedly have significantly decreased levels of plasma coenzyme Q10 (CoQ10), whose levels correlate inversely with the degree of fatigue, impaired concentration and memory, and symptoms of autonomic dysfunction (105, 106). CoQ10/ubiquinone, a component of the ETC, can have both prooxidant and antioxidant effects, as well as anti-inflammatory effects (107).
The causes of mitochondrial dysfunction in people with ME/CFS remain speculative. Viral infection surely can cause impairment of mitochondrial structure (99) and function (97, 108), and impairment of mitochondrial function, in turn, encourages viral replication and T cell exhaustion (108). Immune activation, with the generation of proinflammatory cytokines, also can cause mitochondrial fragmentation, hyperpolarization of the mitochondrial membrane, and the generation of ROS (109).
Connecting Redox Imbalance to Inflammation in COVID-19 and ME/CFS
Connections between Inflammation and Redox Imbalance.
Systemic inflammation and neuroinflammation are seen in both acute COVID-19 and ME/CFS. Inflammation, in turn, is bidirectionally linked to redox imbalance (110); inflammation generates ROS and RNS, and redox imbalance causes cellular damage that evokes an inflammatory response, leading to vicious cycles (111, 112).
Glutathione plays a particularly important role in enabling and modulating the immune response (76). It is vital for proliferation of T lymphocytes; T cell activation, in turn, generates glutathione, which counters ROS levels and mediates a metabolic shift toward aerobic glycolysis and glutaminolysis (113)
Other connections between inflammation and redox imbalance exist as well. Higher interleukin-2 (IL-2) levels stimulate NO production (114, 115), and IL-6 and tumor necrosis factor-α (TNF-α) stimulate cells to produce O2•− (116, 117). Mitochondrial dysfunction also leads to increased proinflammatory responses and increased ROS levels.
Inflammation in COVID-19 and Redox Imbalance.
The cytokine storm seen in severe cases of COVID-19 has been well characterized (118, 119). The nucleotide-binding oligomerization domain-like receptor containing pyrin domain 3 (NLRP3) inflammasome plays a key role in the effects of the cytokine storm; NLRP3, in turn, is activated by oxidative stress (118). Increased levels of the proinflammatory markers, C-reactive protein and IL-6, were associated with the disease (120).
Immunologic factors that correlated with more severe disease and higher mortality include neutrophilia, lymphocytopenia, low CD4+ T cells, decreased C3, very low human leukocyte antigen D–related expression, and low numbers of CD19 lymphocytes and natural killer (NK) cells (121). In addition to these changes, COVID-19 is associated with inadequate Type I and Type III IFN responses and elevated chemokine expression (122–124). Finally, T cell exhaustion is commonly seen in COVID-19 and could be explained by low levels of glutathione (125).
Inflammation in ME/CFS and Redox Imbalance.
The fatigue and cognitive deficits in people with ME/CFS are associated with neuroinflammation; positron emission tomography imaging reveals increased activation of microglia, astrocytes, and elevated levels of cytokines in the brain and spinal cord (126, 127). Increased levels of various cytokines can trigger many of the symptoms of ME/CFS (and post–COVID-19 syndrome), as became clear in the 1980s when various cytokines were synthesized and used as treatments. For example, when IFN I-α is given as antiviral therapy, it induces persistent fatigue in patients with chronic hepatitis C virus infection (128).
In ME/CFS, the systemic circulation often contains elevated levels of inflammatory biomarkers—proinflammatory cytokines like IL-1 and TNF-α (106). Also, circulating lymphocytes often produce increased transcripts of these cytokines (129). Both COVID-19 and ME/CFS are associated with activation of the protein kinase R and 2- to 5A synthetase antiviral IFN response pathways (130–132).
People with ME/CFS often have increased numbers of CD8+ T cells bearing activation antigens (133), although persistent T cell activation then may lead to exhaustion (134). Another characteristic finding in people with ME/CFS is impaired NK cell function (135). Redox imbalance leading to increased levels of l-kynurenine and lactate can impair NK cell function (136).
Connecting Redox Imbalance, Inflammation, and Energy Metabolism
Viral infection triggers increased mitochondrial function and sometimes, mitochondrial damage. In either case, increased ROS are produced. ROS, in turn, damage mtDNA and proteins, including those comprising the ETC, causing a decrease in ATP production (137, 138). In COVID-19, damage to endothelial cells results in chronic inflammation, thrombosis, atherosclerosis, and lung injury. Endothelial mitochondria modulate these inflammatory pathways via redox signaling, involving mtROS. However, continued elevation of mtROS leads to senescence, promoting inflammation and chronic endothelial dysfunction, culminating in vicious cycles that involve ROS, inflammation, and mitochondrial dysfunction (139, 140).
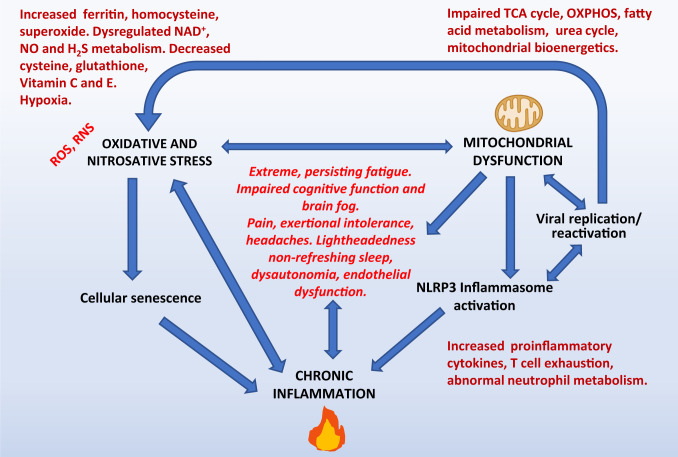
A mode by which mitochondrial dysfunction causes inflammation is by activating the NLRP3 inflammasome in immune cells. The NLRP3 inflammasome participates in the processing and release of inflammatory cytokines, such as IL-1β and IL-18 (141). Damaged ROS-generating mitochondria can elicit persistent inflammation via NLRP3 inflammasome-dependent inflammatory pathways (142). Additionally, damaged mitochondria mount inflammatory responses by releasing mtDNA into the cytosol; the DNA and its purinergic components function as a damage-activated molecular pattern to trigger the innate immune system (143, 144). Finally, mitochondria also modulate both adaptive and innate immune responses (143, 145, 146). In COVID-19, a dysregulation of the innate immune system has been observed, causing aberrant engagement of antiviral signaling cascades, which facilitates evasion of the host immune system and which is linked to mitochondrial function as described earlier (85, 86, 147). Thus, infection and inflammation are intimately linked to energy metabolism and redox imbalance (Fig. 2).
Fig. 2.
The interactions between redox imbalance, mitochondrial dysfunction, chronic inflammation, and related symptoms. As explained in the text, redox imbalance, mitochondrial dysfunction, and inflammation are bidirectionally related to each other and may cause some of the symptoms of both long COVID-19 and ME/CFS. The bidirectional connections mean that an initial abnormality in one component can trigger abnormalities in other components and can precipitate a persistent, self-reinforcing pathological process.
Hypometabolic State, the Cell Danger Response, and Integrated Stress Response
What might cause the hypometabolic state reported in ME/CFS? Dysregulated H2S production can induce a hypometabolic, torpor-like state in mice (73, 74). In addition, any of several stressors, including viral infection and oxidative stress, can trigger evolutionarily conserved protective responses that operate at the level of both the cell (the cell danger response) (148) and the whole organism (the integrated stress response, hibernation, and the state of dauer in Caenorhabditis elegans) (121, 149, 150). These protective responses generally are reversible when the stressor no longer is present. Since dysregulated H2S production can induce a hypometabolic, torpor-like state in mice (74), H2S production may be one potential switch (73). Since protein translation consumes considerable ATP, a reduction in protein translation thereby makes ATP available for repair of injury and preservation of vital functions.
The hypometabolic state seen in ME/CFS (and that may be seen in PASC) could be secondary to a persisting stressor (such as redox imbalance or viral infection), or it could result from a defect in the “switch” that turns off the protective state. Abnormalities in purinergic signaling secondary to mitochondrial damage (151, 152) and mitochondrial dysfunction of any cause (153) are often associated with cellular and organism stress responses, and each has been linked to a wide variety of neurological disorders.
Potential Redox-Based Therapeutics
Several therapies targeting redox imbalance already have been utilized or proposed for the treatment of disease. NO inhibits the replication of SARS-CoV-2 in vitro (154) and improves oxygenation in people with COVID-19 when administered by inhalation (155). Small studies of ubiquinol (156) and of a combination of NADH and CoQ10 (157) have reported clinical benefit. Many other potential treatments targeting redox imbalance also deserve consideration: for example, glutathione (and glutathione donors), N-acetyl cysteine, cysteamine, sulforaphane, ubiquinol, nicotinamide, melatonin, selenium, vitamin C, vitamin D, vitamin E, melatonin plus pentoxyfylline, disulfiram, ebselen, and corticosteroids. In two cases of acute COVID-19, glutathione administered therapeutically counteracted dyspnea associated with COVID-19 pneumonia and reduced pulmonary inflammation (158).
In rodents, administering H2S donors reduced inflammation and oxidative stress and attenuated ventilator-induced lung injury as well as injury induced by pneumonia (159, 160). In addition, the H2S donor, GYY4137, suppressed replication of enveloped RNA viruses like SARS-CoV-2 (161–163). Additionally, the H2S donor, sodium hydrosulfide, inhibits platelet activation, NET formation, DNA, and ROS levels while decreasing SOD in the hyperhomocysteinemia (HHcy) group (164). Thus, treatment of acute COVID-19 with H2S donors may be efficacious (165).
A screen for inhibitors of the main protease of SARS-CoV-2 identified ebselen, an organoselenium compound, as a potential inhibitor for the protease, Mpro or NSP5, and a therapeutic agent for COVID-19 (166, 167).
In general, however, oral therapies directed at restoring redox balance have not produced dramatic improvements in conditions associated with redox imbalance (168). No single antioxidant can scavenge or neutralize the wide variety of ROS and RNS singlehandedly. Hence, up-regulating pathways that counteract multiple abnormalities and bolster antioxidant defense and balance may be more beneficial. The timing of intervention may also be critical.
Concluding Remarks
People with acute COVID-19 and people with ME/CFS share redox imbalance, systemic inflammation and neuroinflammation, impaired production of ATP and other abnormalities in common (Fig. 2), abnormalities that have bidirectional connections (169).
The syndrome of long COVID-19 that can develop in some COVID-19 survivors (people called “long haulers”) is very similar to ME/CFS, so it may well be that the group of abnormalities seen in acute COVID-19 and in ME/CFS also will be seen in long COVID-19. Presumably, redox abnormalities in COVID-19 are secondary to the infection with SARS-CoV-2. The same may be true among those ME/CFS patients whose illness began with an “infectious-like” illness.
Clearly, COVID-19–induced permanent damage to the lungs (chronic hypoxia), heart (congestive failure), and kidneys (fluid and acid-base abnormalities) could cause some of the persisting symptoms seen in long COVID-19. In both long COVID-19 and ME/CFS other symptoms (e.g., fatigue, brain fog) may be generated by neuroinflammation, reduced cerebral perfusion due to autonomic dysfunction, and autoantibodies directed at neural targets, as summarized elsewhere (170).
As many as 2.5 million people suffer from ME/CFS in the United States (6). The COVID-19 pandemic may generate a similar number of cases of long COVID-19 in the coming 1 to 2 y (5). It therefore is imperative that increased research be focused on both long COVID-19 and ME/CFS. Fortunately, the United States and several other countries have committed substantial funding to study chronic illnesses following COVID-19, one of which is long COVID-19. Two registries and associated biobanks of people with long COVID-19 and/or ME/CFS are available to aid research.* We suggest that the study of the connections between redox imbalance, inflammation, and energy metabolism in long COVID-19 and in ME/CFS may lead to improvements in both new diagnostics and therapies.
Supplementary Material
Acknowledgments
This work was supported by Solve ME/CFS Initiative Grant 90089823 (to B.D.P.); the American Heart Association/Paul Allen Frontiers Group Project 19PABH134580006 (to B.D.P., S.H.S., and associates); US Public Health Service Grant 5U54AI138370 (to A.L.K.); and US Public Health Service Grant DA044123 (to S.H.S.). We acknowledge BioRender for the use of icons in figures and thank Julia Lemle for her artistic input in Fig. 2. A.L.K. thanks Jill Mazzetta for help in collecting pertinent literature. We thank the reviewers for several valuable suggestions.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission. M.R.H. is a guest editor invited by the Editorial Board.
*They are the You + M.E. Registry (https://youandmecovid.com/home) and NIH (https://searchmecfs.org/).
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2024358118/-/DCSupplemental.
Data Availability
There are no data underlying this work.
References
- 1.Al-Aly Z., Xie Y., Bowe B., High-dimensional characterization of post-acute sequalae of COVID-19. Nature 594, 259–264 (2021). [DOI] [PubMed] [Google Scholar]
- 2.Zhang X., et al., Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int. J. Infect. Dis. 94, 81–87 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Disser N. P., et al., Musculoskeletal consequences of COVID-19. J. Bone Joint Surg. Am. 102, 1197–1204 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee M. H., et al., Microvascular injury in the brains of patients with COVID-19. N. Engl. J. Med. 384, 481–483 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Komaroff A. L., Bateman L., Will COVID-19 lead to myalgic encephalomyelitis/chronic fatigue syndrome? Front. Med. (Lausanne) 7, 606824 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institute of Medicine , Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness (National Institutes of Health, Washington, DC, 2015).
- 7.Pérez-Torres I., Manzano-Pech L., Rubio-Ruíz M. E., Soto M. E., Guarner-Lans V., Nitrosative stress and its association with cardiometabolic disorders. Molecules 25, E2555 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sies H., Berndt C., Jones D. P., Oxidative stress. Annu. Rev. Biochem. 86, 715–748 (2017). [DOI] [PubMed] [Google Scholar]
- 9.Sies H., Jones D. P., Reactive oxygen species (ROS) as pleiotropic physiological signalling agents. Nat. Rev. Mol. Cell Biol. 21, 363–383 (2020). [DOI] [PubMed] [Google Scholar]
- 10.Khomich O. A., Kochetkov S. N., Bartosch B., Ivanov A. V., Redox biology of respiratory viral infections. Viruses 10, E392 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chernyak B. V., et al., COVID-19 and oxidative stress. Biochemistry (Mosc.) 85, 1543–1553 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abouhashem A. S., Singh K., Azzazy H. M. E., Sen C. K., Is low alveolar type II cell SOD3 in the lungs of elderly linked to the observed severity of COVID-19? Antioxid. Redox Signal. 33, 59–65 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffmann M., et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181, 271–280.e8 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajagopalan S., et al., Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. Contribution to alterations of vasomotor tone. J. Clin. Invest. 97, 1916–1923 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silvagno F., Vernone A., Pescarmona G. P., The role of glutathione in protecting against the severe inflammatory response triggered by COVID-19. Antioxidants 9, E624 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hati S., Bhattacharyya S., Impact of thiol-disulfide balance on the binding of COVID-19 spike protein with angiotensin-converting enzyme 2 receptor. ACS Omega 5, 16292–16298 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh J., Dhindsa R. S., Misra V., Singh B., SARS-CoV2 infectivity is potentially modulated by host redox status. Comput. Struct. Biotechnol. J. 18, 3705–3711 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lan J., et al., Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature 581, 215–220 (2020). [DOI] [PubMed] [Google Scholar]
- 19.Yan R., et al., Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 367, 1444–1448 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones D. P., Mody V. C. Jr., Carlson J. L., Lynn M. J., Sternberg P. Jr., Redox analysis of human plasma allows separation of pro-oxidant events of aging from decline in antioxidant defenses. Free Radic. Biol. Med. 33, 1290–1300 (2002). [DOI] [PubMed] [Google Scholar]
- 21.Giustarini D., Santucci A., Bartolini D., Galli F., Rossi R., The age-dependent decline of the extracellular thiol-disulfide balance and its role in SARS-CoV-2 infection. Redox Biol. 41, 101902 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fukuda S., et al., A potential biomarker for fatigue: Oxidative stress and anti-oxidative activity. Biol. Psychol. 118, 88–93 (2016). [DOI] [PubMed] [Google Scholar]
- 23.Miwa K., Fujita M., Fluctuation of serum vitamin E (alpha-tocopherol) concentrations during exacerbation and remission phases in patients with chronic fatigue syndrome. Heart Vessels 25, 319–323 (2010). [DOI] [PubMed] [Google Scholar]
- 24.Maes M., Kubera M., Uytterhoeven M., Vrydags N., Bosmans E., Increased plasma peroxides as a marker of oxidative stress in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Med. Sci. Monit. 17, SC11–SC15 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson M., et al., Plasma IL-6, its soluble receptors and F2-isoprostanes at rest and during exercise in chronic fatigue syndrome. Scand. J. Med. Sci. Sports 20, 282–290 (2010). [DOI] [PubMed] [Google Scholar]
- 26.Manuel y Keenoy B., Moorkens G., Vertommen J., De Leeuw I., Antioxidant status and lipoprotein peroxidation in chronic fatigue syndrome. Life Sci. 68, 2037–2049 (2001). [DOI] [PubMed] [Google Scholar]
- 27.Kurup R. K., Kurup P. A., Hypothalamic digoxin, cerebral chemical dominance and myalgic encephalomyelitis. Int. J. Neurosci. 113, 683–701 (2003). [DOI] [PubMed] [Google Scholar]
- 28.Smirnova I. V., Pall M. L., Elevated levels of protein carbonyls in sera of chronic fatigue syndrome patients. Mol. Cell. Biochem. 248, 93–95 (2003). [DOI] [PubMed] [Google Scholar]
- 29.Jammes Y., Steinberg J. G., Mambrini O., Brégeon F., Delliaux S., Chronic fatigue syndrome: Assessment of increased oxidative stress and altered muscle excitability in response to incremental exercise. J. Intern. Med. 257, 299–310 (2005). [DOI] [PubMed] [Google Scholar]
- 30.Brkic S., Tomic S., Maric D., Novakov Mikic A., Turkulov V., Lipid peroxidation is elevated in female patients with chronic fatigue syndrome. Med. Sci. Monit. 16, CR628–CR632 (2010). [PubMed] [Google Scholar]
- 31.Fenouillet E., et al., Association of biomarkers with health-related quality of life and history of stressors in myalgic encephalomyelitis/chronic fatigue syndrome patients. J. Transl. Med. 14, 251 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jammes Y., Steinberg J. G., Guieu R., Delliaux S., Chronic fatigue syndrome with history of severe infection combined altered blood oxidant status, and reduced potassium efflux and muscle excitability at exercise. Open J. Int. Med. 3, 98–105 (2013). [Google Scholar]
- 33.Shungu D. C., et al., Increased ventricular lactate in chronic fatigue syndrome. III. Relationships to cortical glutathione and clinical symptoms implicate oxidative stress in disorder pathophysiology. NMR Biomed. 25, 1073–1087 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murrough J. W., et al., Increased ventricular lactate in chronic fatigue syndrome measured by 1H MRS imaging at 3.0 T. II. Comparison with major depressive disorder. NMR Biomed. 23, 643–650 (2010). [DOI] [PubMed] [Google Scholar]
- 35.Mathew S. J., et al., Ventricular cerebrospinal fluid lactate is increased in chronic fatigue syndrome compared with generalized anxiety disorder: An in vivo 3.0 T (1)H MRS imaging study. NMR Biomed. 22, 251–258 (2009). [DOI] [PubMed] [Google Scholar]
- 36.Suárez A., et al., Nitric oxide metabolite production during exercise in chronic fatigue syndrome: A case-control study. J. Womens Health (Larchmt.) 19, 1073–1077 (2010). [DOI] [PubMed] [Google Scholar]
- 37.Morris G., Maes M., Oxidative and nitrosative stress and immune-inflammatory pathways in patients with myalgic encephalomyelitis (ME)/chronic fatigue syndrome (CFS). Curr. Neuropharmacol. 12, 168–185 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morris G., et al., Nitrosative stress, hypernitrosylation, and autoimmune responses to nitrosylated proteins: New pathways in neuroprogressive disorders including depression and chronic fatigue syndrome. Mol. Neurobiol. 54, 4271–4291 (2017). [DOI] [PubMed] [Google Scholar]
- 39.Maes M., Mihaylova I., Leunis J. C., Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins. Neuroendocrinol. Lett. 27, 615–621 (2006). [PubMed] [Google Scholar]
- 40.Nagy-Szakal D., et al., Insights into myalgic encephalomyelitis/chronic fatigue syndrome phenotypes through comprehensive metabolomics. Sci. Rep. 8, 10056 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naviaux R. K., et al., Metabolic features of chronic fatigue syndrome. Proc. Natl. Acad. Sci. U.S.A. 113, E5472–E5480 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Germain A., Ruppert D., Levine S. M., Hanson M. R., Metabolic profiling of a myalgic encephalomyelitis/chronic fatigue syndrome discovery cohort reveals disturbances in fatty acid and lipid metabolism. Mol. Biosyst. 13, 371–379 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Germain A., Ruppert D., Levine S. M., Hanson M. R., Prospective biomarkers from plasma metabolomics of myalgic encephalomyelitis/chronic fatigue syndrome implicate redox imbalance in disease symptomatology. Metabolites 8, E90 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sbodio J. I., Snyder S. H., Paul B. D., Redox mechanisms in neurodegeneration: From disease outcomes to therapeutic opportunities. Antioxid. Redox Signal. 30, 1450–1499 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Recalcati S., Invernizzi P., Arosio P., Cairo G., New functions for an iron storage protein: The role of ferritin in immunity and autoimmunity. J. Autoimmun. 30, 84–89 (2008). [DOI] [PubMed] [Google Scholar]
- 46.Sedlak T. W., et al., Bilirubin and glutathione have complementary antioxidant and cytoprotective roles. Proc. Natl. Acad. Sci. U.S.A. 106, 5171–5176 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vasavda C., et al., Bilirubin links heme metabolism to neuroprotection by scavenging superoxide. Cell Chem. Biol. 26, 1450–1460.e7 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Paul B. D., Snyder S. H., H2S signalling through protein sulfhydration and beyond. Nat. Rev. Mol. Cell Biol. 13, 499–507 (2012). [DOI] [PubMed] [Google Scholar]
- 49.Kaye A. D., et al., Folic acid supplementation in patients with elevated homocysteine levels. Adv. Ther. 37, 4149–4164 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Laforge M., et al., Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat. Rev. Immunol. 20, 515–516 (2020). Erratum in: Nat. Rev. Immunol. 20, 579 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Middleton E. A., et al., Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood 136, 1169–1179 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Papayannopoulos V., Neutrophil extracellular traps in immunity and disease. Nat. Rev. Immunol. 18, 134–147 (2018). [DOI] [PubMed] [Google Scholar]
- 53.Zuo Y., et al., Neutrophil extracellular traps in COVID-19. JCI Insight 5, 138999 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mustafa A. K., Gadalla M. M., Snyder S. H., Signaling by gasotransmitters. Sci. Signal. 2, re2 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ignarro L. J., Nitric oxide as a unique signaling molecule in the vascular system: A historical overview. J. Physiol. Pharmacol. 53, 503–514 (2002). [PubMed] [Google Scholar]
- 56.Ignarro L. J., Physiology and pathophysiology of nitric oxide. Kidney Int. Suppl. 55, S2–S5 (1996). [PubMed] [Google Scholar]
- 57.Paul B. D., Snyder S. H., Modes of physiologic H2S signaling in the brain and peripheral tissues. Antioxid. Redox Signal. 22, 411–423 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Karki R., et al., Synergism of TNF-α and IFN-γ triggers inflammatory cell death, tissue damage, and mortality in SARS-CoV-2 infection and cytokine shock syndromes. Cell 184, 149–168.e17 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pall M. L., Levels of nitric oxide synthase product citrulline are elevated in sera of chronic fatigue syndrome patients. J. Chronic Fatigue Syndr. 10, 37–41 (2002). [Google Scholar]
- 60.Filipovic M. R., Zivanovic J., Alvarez B., Banerjee R., Chemical biology of H2S signaling through persulfidation. Chem. Rev. 118, 1253–1337 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yuan S., Shen X., Kevil C. G., Beyond a gasotransmitter: Hydrogen sulfide and polysulfide in cardiovascular health and immune response. Antioxid. Redox Signal. 27, 634–653 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mustafa A. K., et al., H2S signals through protein S-sulfhydration. Sci. Signal. 2, ra72 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zivanovic J., et al., Selective persulfide detection reveals evolutionarily conserved antiaging effects of S-sulfhydration. Cell Metab. 30, 1152–1170.e13 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dóka É., et al., Control of protein function through oxidation and reduction of persulfidated states. Sci. Adv. 6, eaax8358 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Paul B. D., Snyder S. H., Gasotransmitter hydrogen sulfide signaling in neuronal health and disease. Biochem. Pharmacol. 149, 101–109 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paul B. D., et al., Cystathionine γ-lyase deficiency mediates neurodegeneration in Huntington’s disease. Nature 509, 96–100 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vandiver M. S., et al., Sulfhydration mediates neuroprotective actions of parkin. Nat. Commun. 4, 1626 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Giovinazzo D., et al., Hydrogen sulfide is neuroprotective in Alzheimer’s disease by sulfhydrating GSK3β and inhibiting Tau hyperphosphorylation. Proc. Natl. Acad. Sci. U.S.A. 118, e2017225118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Paul B. D., Neuroprotective roles of the reverse transsulfuration pathway in Alzheimer’s disease. Front. Aging Neurosci. 13, 659402 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Renieris G., et al., Serum hydrogen sulfide and outcome association in pneumonia by the SARS-CoV-2 coronavirus. Shock 54, 633–637 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Miller T. W., et al., Hydrogen sulfide is an endogenous potentiator of T cell activation. J. Biol. Chem. 287, 4211–4221 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dominic P., et al., Decreased availability of nitric oxide and hydrogen sulfide is a hallmark of COVID-19. Redox Biol. 43, 101982 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lemle M. D., Hypothesis: Chronic fatigue syndrome is caused by dysregulation of hydrogen sulfide metabolism. Med. Hypotheses 72, 108–109 (2009). [DOI] [PubMed] [Google Scholar]
- 74.Blackstone E., Morrison M., Roth M. B., H2S induces a suspended animation-like state in mice. Science 308, 518 (2005). [DOI] [PubMed] [Google Scholar]
- 75.Cervenka I., Agudelo L. Z., Ruas J. L., Kynurenines: Tryptophan’s metabolites in exercise, inflammation, and mental health. Science 357, eaaf9794 (2017). [DOI] [PubMed] [Google Scholar]
- 76.Dröge W., Breitkreutz R., Glutathione and immune function. Proc. Nutr. Soc. 59, 595–600 (2000). [DOI] [PubMed] [Google Scholar]
- 77.Dröge W., et al., Functions of glutathione and glutathione disulfide in immunology and immunopathology. FASEB J. 8, 1131–1138 (1994). [PubMed] [Google Scholar]
- 78.Jain S. K., Parsanathan R., Achari A. E., Kanikarla-Marie P., Bocchini J. A. Jr., Glutathione stimulates vitamin D regulatory and glucose-metabolism genes, lowers oxidative stress and inflammation, and increases 25-hydroxy-vitamin D levels in blood: A novel approach to treat 25-hydroxyvitamin D deficiency. Antioxid. Redox Signal. 29, 1792–1807 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jain S. K., Micinski D., Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem. Biophys. Res. Commun. 437, 7–11 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sbodio J. I., Snyder S. H., Paul B. D., Regulators of the transsulfuration pathway. Br. J. Pharmacol. 176, 583–593 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mousavi S., Bereswill S., Heimesaat M. M., Immunomodulatory and antimicrobial effects of vitamin C. Eur. J. Microbiol. Immunol. (Bp.) 9, 73–79 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schneider C., Chemistry and biology of vitamin E. Mol. Nutr. Food Res. 49, 7–30 (2005). [DOI] [PubMed] [Google Scholar]
- 83.Filler K., et al., Association of mitochondrial dysfunction and fatigue: A review of the literature. BBA Clin. 1, 12–23 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Behan W. M., More I. A., Behan P. O., Mitochondrial abnormalities in the postviral fatigue syndrome. Acta Neuropathol. 83, 61–65 (1991). [DOI] [PubMed] [Google Scholar]
- 85.Singh K. K., Chaubey G., Chen J. Y., Suravajhala P., Decoding SARS-CoV-2 hijacking of host mitochondria in COVID-19 pathogenesis. Am. J. Physiol. Cell Physiol. 319, C258–C267 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wu J., et al., SARS-CoV-2 ORF9b inhibits RIG-I-MAVS antiviral signaling by interrupting K63-linked ubiquitination of NEMO. Cell Rep. 34, 108761 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ajaz S., et al., Mitochondrial metabolic manipulation by SARS-CoV-2 in peripheral blood mononuclear cells of patients with COVID-19. Am. J. Physiol. Cell Physiol. 320, C57–C65 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Codo A. C., et al., Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1alpha/glycolysis-dependent axis. Cell Metab. (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Santos C. S., et al., Determinants of COVID-19 disease severity in patients with underlying rheumatic disease. Clin. Rheumatol. 39, 2789–2796 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang D., et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061–1069 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tomas C., Elson J. L., Newton J. L., Walker M., Substrate utilisation of cultured skeletal muscle cells in patients with CFS. Sci. Rep. 10, 18232 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tomas C., Elson J. L., Strassheim V., Newton J. L., Walker M., The effect of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) severity on cellular bioenergetic function. PLoS One 15, e0231136 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fluge Ø., et al., Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome. JCI Insight 1, e89376 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yamano E., et al., Index markers of chronic fatigue syndrome with dysfunction of TCA and urea cycles. Sci. Rep. 6, 34990 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Billing-Ross P., et al., Mitochondrial DNA variants correlate with symptoms in myalgic encephalomyelitis/chronic fatigue syndrome. J. Transl. Med. 14, 19 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Missailidis D., et al., An isolated complex V inefficiency and dysregulated mitochondrial function in immortalized lymphocytes from ME/CFS patients. Int. J. Mol. Sci. 21, E1074 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sweetman E., et al., A SWATH-MS analysis of myalgic encephalomyelitis/chronic fatigue syndrome peripheral blood mononuclear cell proteomes reveals mitochondrial dysfunction. J. Transl. Med. 18, 365 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mandarano A. H., et al., Myalgic encephalomyelitis/chronic fatigue syndrome patients exhibit altered T cell metabolism and cytokine associations. J. Clin. Invest. 130, 1491–1505 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schreiner P., et al., Human herpesvirus-6 reactivation, mitochondrial fragmentation, and the coordination of antiviral and metabolic phenotypes in myalgic encephalomyelitis/chronic fatigue syndrome. Immunohorizons 4, 201–215 (2020). [DOI] [PubMed] [Google Scholar]
- 100.Snell C. R., Stevens S. R., Davenport T. E., Van Ness J. M., Discriminative validity of metabolic and workload measurements for identifying people with chronic fatigue syndrome. Phys. Ther. 93, 1484–1492 (2013). [DOI] [PubMed] [Google Scholar]
- 101.Vermeulen R. C., Vermeulen van Eck I. W., Decreased oxygen extraction during cardiopulmonary exercise test in patients with chronic fatigue syndrome. J. Transl. Med. 12, 20 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lien K., et al., Abnormal blood lactate accumulation during repeated exercise testing in myalgic encephalomyelitis/chronic fatigue syndrome. Physiol. Rep. 7, e14138 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mueller C., Lin J. C., Sheriff S., Maudsley A. A., Younger J. W., Evidence of widespread metabolite abnormalities in myalgic encephalomyelitis/chronic fatigue syndrome: Assessment with whole-brain magnetic resonance spectroscopy. Brain Imaging Behav. 14, 562–572 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fegan K. G., Behan P. O., Bell E. J., Myalgic encephalomyelitis: Report of an epidemic. J. R. Coll. Gen. Pract. 33, 335–337 (1983). [PMC free article] [PubMed] [Google Scholar]
- 105.Maes M., et al., Coenzyme Q10 deficiency in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is related to fatigue, autonomic and neurocognitive symptoms and is another risk factor explaining the early mortality in ME/CFS due to cardiovascular disorder. Neuroendocrinol. Lett. 30, 470–476 (2009). [PubMed] [Google Scholar]
- 106.Maes M., Twisk F. N., Why myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) may kill you: Disorders in the inflammatory and oxidative and nitrosative stress (IO&NS) pathways may explain cardiovascular disorders in ME/CFS. Neuroendocrinol. Lett. 30, 677–693 (2009). [PubMed] [Google Scholar]
- 107.Yang X., et al., Neuroprotection of coenzyme Q10 in neurodegenerative diseases. Curr. Top. Med. Chem. 16, 858–866 (2016). [DOI] [PubMed] [Google Scholar]
- 108.Fisicaro P., et al., Targeting mitochondrial dysfunction can restore antiviral activity of exhausted HBV-specific CD8 T cells in chronic hepatitis B. Nat. Med. 23, 327–336 (2017). [DOI] [PubMed] [Google Scholar]
- 109.Buoncervello M., et al., Inflammatory cytokines associated with cancer growth induce mitochondria and cytoskeleton alterations in cardiomyocytes. J. Cell. Physiol. 234, 20453–20468 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Muri J., Kopf M., Redox regulation of immunometabolism. Nat. Rev. Immunol. 21, 363–381 (2021). [DOI] [PubMed] [Google Scholar]
- 111.Mittal M., Siddiqui M. R., Tran K., Reddy S. P., Malik A. B., Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox Signal. 20, 1126–1167 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Biswas S. K., Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid. Med. Cell. Longev. 2016, 5698931 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Angelini G., et al., Antigen-presenting dendritic cells provide the reducing extracellular microenvironment required for T lymphocyte activation. Proc. Natl. Acad. Sci. U.S.A. 99, 1491–1496 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Li Y., Hu Y., Yu J., Ma T., Retrospective analysis of laboratory testing in 54 patients with severe- or critical-type 2019 novel coronavirus pneumonia. Lab. Invest. 100, 794–800 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hibbs J. B. Jr., et al., Evidence for cytokine-inducible nitric oxide synthesis from L-arginine in patients receiving interleukin-2 therapy. J. Clin. Invest. 89, 867–877 (1992). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tsujimoto M., Yokota S., Vilcek J., Weissmann G., Tumor necrosis factor provokes superoxide anion generation from neutrophils. Biochem. Biophys. Res. Commun. 137, 1094–1100 (1986). [DOI] [PubMed] [Google Scholar]
- 117.Kharazmi A., Nielsen H., Rechnitzer C., Bendtzen K., Interleukin 6 primes human neutrophil and monocyte oxidative burst response. Immunol. Lett. 21, 177–184 (1989). [DOI] [PubMed] [Google Scholar]
- 118.Mehta P.et al.; HLH Across Specialty Collaboration, UK , COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 395, 1033–1034 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Xu Z., et al., Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 8, 420–422 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhao Y., et al., Abnormal immunity of non-survivors with COVID-19: Predictors for mortality. Infect. Dis. Poverty 9, 108 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Klug B. J., Brigham R. M., Changes to metabolism and cell physiology that enable mammalian hibernation. Springer Sci. Rev. 3, 39–56 (2015). [Google Scholar]
- 122.Zhang Q.et al.; COVID-STORM Clinicians; COVID Clinicians; Imagine COVID Group; French COVID Cohort Study Group; CoV-Contact Cohort; Amsterdam UMC Covid-19 Biobank; COVID Human Genetic Effort; NIAID-USUHS/TAGC COVID Immunity Group , Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science 370, eabd4570 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bastard P.et al.; HGID Lab; NIAID-USUHS Immune Response to COVID Group; COVID Clinicians; COVID-STORM Clinicians; Imagine COVID Group; French COVID Cohort Study Group; Milieu Intérieur Consortium; CoV-Contact Cohort; Amsterdam UMC Covid-19 Biobank; COVID Human Genetic Effort , Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 370, eabd4585 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Blanco-Melo D., et al., Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell 181, 1036–1045.e9 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Khanfar A., Al Qaroot B., Could glutathione depletion be the Trojan horse of COVID-19 mortality? Eur. Rev. Med. Pharmacol. Sci. 24, 12500–12509 (2020). [DOI] [PubMed] [Google Scholar]
- 126.Natelson B. H., Weaver S. A., Tseng C. L., Ottenweller J. E., Spinal fluid abnormalities in patients with chronic fatigue syndrome. Clin. Diagn. Lab. Immunol. 12, 52–55 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Nakatomi Y., et al., Neuroinflammation in patients with chronic fatigue syndrome/myalgic encephalomyelitis: An 11C-(R)-PK11195 PET study. J. Nucl. Med. 55, 945–950 (2014). [DOI] [PubMed] [Google Scholar]
- 128.Russell A., et al., Persistent fatigue induced by interferon-alpha: A novel, inflammation-based, proxy model of chronic fatigue syndrome. Psychoneuroendocrinology 100, 276–285 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sweetman E., et al., Changes in the transcriptome of circulating immune cells of a New Zealand cohort with myalgic encephalomyelitis/chronic fatigue syndrome. Int. J. Immunopathol. Pharmacol. 33, 2058738418820402 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vojdani A., Lapp C. W., Interferon-induced proteins are elevated in blood samples of patients with chemically or virally induced chronic fatigue syndrome. Immunopharmacol. Immunotoxicol. 21, 175–202 (1999). [DOI] [PubMed] [Google Scholar]
- 131.Meeus M., et al., Unravelling intracellular immune dysfunctions in chronic fatigue syndrome: Interactions between protein kinase R activity, RNase L cleavage and elastase activity, and their clinical relevance. In Vivo 22, 115–121 (2008). [PubMed] [Google Scholar]
- 132.Bjørklund G., et al., Environmental, neuro-immune, and neuro-oxidative stress interactions in chronic fatigue syndrome. Mol. Neurobiol. 57, 4598–4607 (2020). [DOI] [PubMed] [Google Scholar]
- 133.Barker E., Fujimura S. F., Fadem M. B., Landay A. L., Levy J. A., Immunologic abnormalities associated with chronic fatigue syndrome. Clin. Infect. Dis. 18 (suppl. 1), S136–S141 (1994). [DOI] [PubMed] [Google Scholar]
- 134.Hornig M., et al., Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci. Adv. 1, e1400121 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Caligiuri M., et al., Phenotypic and functional deficiency of natural killer cells in patients with chronic fatigue syndrome. J. Immunol. 139, 3306–3313 (1987). [PubMed] [Google Scholar]
- 136.Riggan L., Shah S., O’Sullivan T. E., Arrested development: Suppression of NK cell function in the tumor microenvironment. Clin. Transl. Immunology 10, e1238 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Murphy M. P., How mitochondria produce reactive oxygen species. Biochem. J. 417, 1–13 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Abate G., et al., Mitochondria and cellular redox state on the route from ageing to Alzheimer’s disease. Mech. Ageing Dev. 192, 111385 (2020). [DOI] [PubMed] [Google Scholar]
- 139.Chang R., Mamun A., Dominic A., Le N. T., SARS-CoV-2 mediated endothelial dysfunction: The potential role of chronic oxidative stress. Front. Physiol. 11, 605908 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Saleh J., Peyssonnaux C., Singh K. K., Edeas M., Mitochondria and microbiota dysfunction in COVID-19 pathogenesis. Mitochondrion 54, 1–7 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sadatomi D., et al., Mitochondrial function is required for extracellular ATP-induced NLRP3 inflammasome activation. J. Biochem. 161, 503–512 (2017). [DOI] [PubMed] [Google Scholar]
- 142.Zhou R., Yazdi A. S., Menu P., Tschopp J., A role for mitochondria in NLRP3 inflammasome activation. Nature 469, 221–225 (2011). [DOI] [PubMed] [Google Scholar]
- 143.Mills E. L., Kelly B., O’Neill L. A. J., Mitochondria are the powerhouses of immunity. Nat. Immunol. 18, 488–498 (2017). [DOI] [PubMed] [Google Scholar]
- 144.Paul B. D., Snyder S. H., Bohr V. A., Signaling by cGAS-STING in neurodegeneration, neuroinflammation, and aging. Trends Neurosci. 44, 83–96 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Breda C. N. S., Davanzo G. G., Basso P. J., Saraiva Câmara N. O., Moraes-Vieira P. M. M., Mitochondria as central hub of the immune system. Redox Biol. 26, 101255 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Weinberg S. E., Sena L. A., Chandel N. S., Mitochondria in the regulation of innate and adaptive immunity. Immunity 42, 406–417 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Schultze J. L., Aschenbrenner A. C., COVID-19 and the human innate immune system. Cell 184, 1671–1692 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Naviaux R. K., Metabolic features and regulation of the healing cycle-A new model for chronic disease pathogenesis and treatment. Mitochondrion 46, 278–297 (2019). [DOI] [PubMed] [Google Scholar]
- 149.Costa-Mattioli M., Walter P., The integrated stress response: From mechanism to disease. Science 368, eaat5314 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Penkov S., et al., Integration of carbohydrate metabolism and redox state controls dauer larva formation in Caenorhabditis elegans. Nat. Commun. 6, 8060 (2015). [DOI] [PubMed] [Google Scholar]
- 151.Burnstock G., An introduction to the roles of purinergic signalling in neurodegeneration, neuroprotection and neuroregeneration. Neuropharmacology 104, 4–17 (2016). [DOI] [PubMed] [Google Scholar]
- 152.Zolkipli-Cunningham Z., et al., Metabolic and behavioral features of acute hyperpurinergia and the maternal immune activation mouse model of autism spectrum disorder. PLoS One 16, e0248771 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pei L., Wallace D. C., Mitochondrial etiology of neuropsychiatric disorders. Biol. Psychiatry 83, 722–730 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Akaberi D., et al., Mitigation of the replication of SARS-CoV-2 by nitric oxide in vitro. Redox Biol. 37, 101734 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lotz C., et al., Effects of inhaled nitric oxide in COVID-19-induced ARDS - Is it worthwhile? Acta Anaesthesiol. Scand. 65, 629–632 (2021). [DOI] [PubMed] [Google Scholar]
- 156.Fukuda S., et al., Ubiquinol-10 supplementation improves autonomic nervous function and cognitive function in chronic fatigue syndrome. Biofactors 42, 431–440 (2016). [DOI] [PubMed] [Google Scholar]
- 157.Castro-Marrero J., et al., Does oral coenzyme Q10 plus NADH supplementation improve fatigue and biochemical parameters in chronic fatigue syndrome? Antioxid. Redox Signal. 22, 679–685 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Horowitz R. I., Freeman P. R., Bruzzese J., Efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia: A report of 2 cases. Respir. Med. Case Rep. 30, 101063 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Faller S., et al., Pre- and posttreatment with hydrogen sulfide prevents ventilator-induced lung injury by limiting inflammation and oxidation. PLoS One 12, e0176649 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Evgen’ev M. B., Frenkel A., Possible application of H2S-producing compounds in therapy of coronavirus (COVID-19) infection and pneumonia. Cell Stress Chaperones 25, 713–715 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bazhanov N., Escaffre O., Freiberg A. N., Garofalo R. P., Casola A., Broad-range antiviral activity of hydrogen sulfide against highly pathogenic RNA viruses. Sci. Rep. 7, 41029 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Roblin X., Pofelski J., Zarski J. P., [Steatosis, chronic hepatitis virus C infection and homocysteine]. Gastroenterol. Clin. Biol. 31, 415–420 (2007). [DOI] [PubMed] [Google Scholar]
- 163.Deminice R., Silva T. C., de Oliveira V. H., Elevated homocysteine levels in human immunodeficiency virus-infected patients under antiretroviral therapy: A meta-analysis. World J. Virol. 4, 147–155 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhao X., et al., Exogenous hydrogen sulfide inhibits neutrophils extracellular traps formation via the HMGB1/TLR4/p-38 MAPK/ROS axis in hyperhomocysteinemia rats. Biochem. Biophys. Res. Commun. 537, 7–14 (2021). [DOI] [PubMed] [Google Scholar]
- 165.Bourgonje A. R., et al., N-acetylcysteine and hydrogen sulfide in coronavirus disease 2019. Antioxid. Redox Signal., 10.1089/ars.2020.8247 (2021). [DOI] [PubMed] [Google Scholar]
- 166.Jin Z., et al., Structure of Mpro from SARS-CoV-2 and discovery of its inhibitors. Nature 582, 289–293 (2020). [DOI] [PubMed] [Google Scholar]
- 167.Sies H., Parnham M. J., Potential therapeutic use of ebselen for COVID-19 and other respiratory viral infections. Free Radic. Biol. Med. 156, 107–112 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Barcelos I., Shadiack E., Ganetzky R. D., Falk M. J., Mitochondrial medicine therapies: Rationale, evidence, and dosing guidelines. Curr. Opin. Pediatr. 32, 707–718 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Stanculescu D., Larsson L., Bergquist J., Hypothesis: Mechanisms that prevent recovery in prolonged ICU patients also underlie myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Front. Med. (Lausanne) 8, 628029 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Komaroff A. L., Lipkin W. I., Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends Mol. Med., 10.1016/j.molmed.2021.06.002 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wang F., et al., The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight 5, 137799 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kappert K., Jahić A., Tauber R., Assessment of serum ferritin as a biomarker in COVID-19: Bystander or participant? Insights by comparison with other infectious and non-infectious diseases. Biomarkers 25, 616–625 (2020). [DOI] [PubMed] [Google Scholar]
- 173.Perricone C., et al., COVID-19 as part of the hyperferritinemic syndromes: The role of iron depletion therapy. Immunol. Res. 68, 213–224 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Colafrancesco S., Alessandri C., Conti F., Priori R., COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? Autoimmun. Rev. 19, 102573 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Song J. W., et al., Omics-driven systems interrogation of metabolic dysregulation in COVID-19 pathogenesis. Cell Metab. 32, 188–202.e5 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Shen B., et al., Proteomic and metabolomic characterization of COVID-19 patient sera. Cell 182, 59–72.e15 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yang Z., et al., Predictors for imaging progression on chest CT from coronavirus disease 2019 (COVID-19) patients. Aging (Albany NY) 12, 6037–6048 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ponti G., Ruini C., Tomasi A., Homocysteine as a potential predictor of cardiovascular risk in patients with COVID-19. Med. Hypotheses 143, 109859 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Regland B., et al., Increased concentrations of homocysteine in the cerebrospinal fluid in patients with fibromyalgia and chronic fatigue syndrome. Scand. J. Rheumatol. 26, 301–307 (1997). [DOI] [PubMed] [Google Scholar]
- 180.Pietrangelo T., et al., Transcription profile analysis of vastus lateralis muscle from patients with chronic fatigue syndrome. Int. J. Immunopathol. Pharmacol. 22, 795–807 (2009). [DOI] [PubMed] [Google Scholar]
- 181.Henry B., et al., Lymphopenia and neutrophilia at admission predicts severity and mortality in patients with COVID-19: A meta-analysis. Acta Biomed. 91, e2020008 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Brenu E. W., et al., Role of adaptive and innate immune cells in chronic fatigue syndrome/myalgic encephalomyelitis. Int. Immunol. 26, 233–242 (2014). [DOI] [PubMed] [Google Scholar]
- 183.Thomas T., et al., COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status. JCI Insight 5, 140327 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Heer C. D., et al., Coronavirus infection and PARP expression dysregulate the NAD metabolome: An actionable component of innate immunity. J. Biol. Chem. 295, 17986–17996 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Polonikov A., Endogenous deficiency of glutathione as the most likely cause of serious manifestations and death in COVID-19 patients. ACS Infect. Dis. 6, 1558–1562 (2020). [DOI] [PubMed] [Google Scholar]
- 186.Rhodes J. M., Subramanian S., Laird E., Griffin G., Kenny R. A., Perspective: Vitamin D deficiency and COVID-19 severity—plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2, and thrombosis. J. Intern. Med. 289, 97–115 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kennedy G., et al., Oxidative stress levels are raised in chronic fatigue syndrome and are associated with clinical symptoms. Free Radic. Biol. Med. 39, 584–589 (2005). [DOI] [PubMed] [Google Scholar]
- 188.Aoki T., Miyakoshi H., Usuda Y., Herberman R. B., Low NK syndrome and its relationship to chronic fatigue syndrome. Clin. Immunol. Immunopathol. 69, 253–265 (1993). [DOI] [PubMed] [Google Scholar]
- 189.Zhang J., Taylor E. W., Bennett K., Saad R., Rayman M. P., Association between regional selenium status and reported outcome of COVID-19 cases in China. Am. J. Clin. Nutr. 111, 1297–1299 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Hoffmann P. R., Berry M. J., The influence of selenium on immune responses. Mol. Nutr. Food Res. 52, 1273–1280 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Steinbrenner H., Al-Quraishy S., Dkhil M. A., Wunderlich F., Sies H., Dietary selenium in adjuvant therapy of viral and bacterial infections. Adv. Nutr. 6, 73–82 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Chiscano-Camón L., Ruiz-Rodriguez J. C., Ruiz-Sanmartin A., Roca O., Ferrer R., Vitamin C levels in patients with SARS-CoV-2-associated acute respiratory distress syndrome. Crit. Care 24, 522 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kennedy G., Khan F., Hill A., Underwood C., Belch J. J., Biochemical and vascular aspects of pediatric chronic fatigue syndrome. Arch. Pediatr. Adolesc. Med. 164, 817–823 (2010). [DOI] [PubMed] [Google Scholar]
- 194.Heer C. D., et al., Coronavirus infection and PARP expression dysregulate the NAD metabolome: An actionable component of innate immunity. J. Biol. Chem. 295, 17986–17996 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Erol S. A., et al., Evaluation of maternal serum afamin and vitamin E levels in pregnant women with COVID-19 and its association with composite adverse perinatal outcomes. J. Med. Virol. 93, 2350–2358 (2021). [DOI] [PubMed] [Google Scholar]
- 196.Vecchiet J., et al., Relationship between musculoskeletal symptoms and blood markers of oxidative stress in patients with chronic fatigue syndrome. Neurosci. Lett. 335, 151–154 (2003). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
There are no data underlying this work.