About the NAM series on Emerging Stronger After COVID-19: Priorities for Health System Transformation
This discussion paper is part of the National Academy of Medicine’s Emerging Stronger After COVID-19: Priorities for Health System Transformation initiative, which commissioned papers from experts on how 9 key sectors of the health, health care, and biomedical science fields responded to and can be transformed in the wake of the COVID-19 pandemic. The views presented in this discussion paper and others in the series are those of the authors and do not represent formal consensus positions of the NAM, the National Academies of Sciences, Engineering, and Medicine, or the authors’ organizations.
Learn more: nam.edu/TransformingHealth

Introduction
Clinicians—who consist of physicians, nurses, pharmacists, and other allied health professionals involved in direct caregiving—are the foundation of the health care delivery system. While more than 17 million individuals in the American health system are employed in a clinical capacity and are critical members of care delivery teams nationwide, this paper will primarily focus on the experience of nurses (over 4 million) and physicians (1 million), who represent two of the largest professional groups in the health care workforce, prior to and during the COVID-19 pandemic [1,2].
Today, the professional responsibilities of clinicians encompass both the traditional domains of caregiving (e.g., diagnosis, treatment, symptom management) and an appropriately increased focus on supporting the unique social needs of their patients (e.g., addressing the social determinants of health by inquiring about and connecting patients with resources to increase food security, stable housing, and reliable transportation, among others). Yet even as the clinical purview is expanding and the complexity of patient care is increasing due to the growing burden of chronic diseases, clinical capacity remains unevenly distributed across the country, with more than 80 million Americans residing in a “Health Professional Shortage Area” [3]. The professional demands on practicing clinicians have also been exacerbated by an ever-increasing bevy of administrative requirements which contribute to record rates of burnout and declining mental health and well-being among clinicians [4,5].
These workforce trends frame the backdrop for many of the challenges facing clinicians during the CO-VID-19 pandemic. Physicians, nurses, and other allied health professionals represent the frontlines of the health care system, and have worked tirelessly to care for infected patients from the outset of the outbreak. Clinicians in COVID-19 epicenters had to rapidly develop best practices for treating patients infected with a novel pathogen, were frequently asked to care for patients with inadequate personal protective equipment (PPE), and in some cases were required to staff clinical settings that they had not worked or trained in for decades, or not at all. In tandem, public health measures to contain the outbreak disrupted non-COVID-19 care, requiring clinicians to quickly learn how to operate virtual platforms and adapt service delivery where possible to ensure the continuity of care.
Navigating this evolving workplace environment amidst a deadly, new, and infectious disease has taken its toll on clinicians, who faced the same COVID-19 stressors as other Americans—juggling child care, caring for loved ones who had fallen ill—in addition to the added anxieties of a higher risk of exposure to infection, the psychological burden from prolonged separation from their families due to self-isolation requirements, and the emotional anguish arising from caring for high volumes of acutely ill patients. Persistent PPE shortages left clinicians exposed to the virus when caring for infected patients, with nurses and physicians accounting for 49% of the more than 3,600 health care worker deaths attributed to COVID-19 as of April 2021 [6,7]. The extreme stress also led many clinicians to report symptoms of anxiety, depression, and post-traumatic stress disorder (PTSD), with burnout—defined as “a syndrome characterized by a high degree of emotional exhaustion and depersonalization (i.e., cynicism), and a low sense of personal accomplishment at work”—carrying tragic consequences, including suicide [8,9].
The public and government have lauded the critical role of health care workers during the pandemic, with clinicians frequently referred to as “heroes” for their service during COVID-19. And while clinicians have been remarkably adaptive, innovative, and resilient during the pandemic, verbal salutes alone are insufficient to address the systemic workforce challenges exacerbated by COVID-19. Instead, tangible and long-term investments in training, operations, and financing are needed to shore up the clinical capacity needed to care for future generations. A special focus on mental health, particularly efforts to reduce burnout and promote workforce well-being, will be needed following the pandemic.
This discussion paper will examine the clinician experience to date during COVID-19, identifying the challenges and lessons from pandemic response activities to inform a series of priority actions for revitalizing the sector’s capacity to address population health challenges, care for clinicians themselves, and respond to future public health emergencies.
The Clinician Response to COVID-19
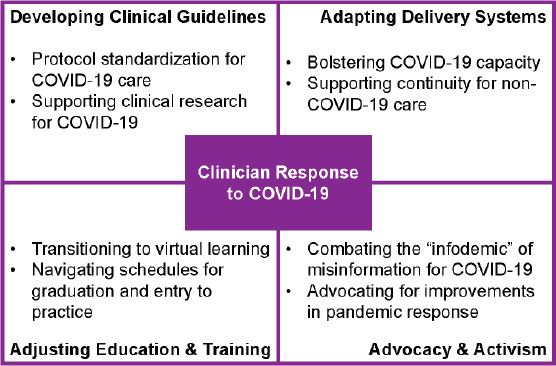
Beyond the basic frontline COVID-19 diagnosis and treatment responsibilities in hospitals and office practices nationwide, clinicians have worked to rapidly gather and synthesize evidence to inform care for exposed and infected patients and adapt care processes for non-COVID-19 care. In addition to their primary responsibilities of providing patient care, clinicians also engaged in other activities including modifying training programs and participating in public education and advocacy. Key elements of the clinician response include:
-
1.
Developing and updating clinical guidelines for COVID-19;
-
2.
Adapting delivery systems to support both CO-VID-19 and non-COVID-19 care;
-
3.
Adjusting education and training programs to the circumstances of the pandemic; and
-
4.
Leveraging advocacy and activism to inform the public and spotlight health system challenges (see Figure 1).
FIGURE 1. The Clinician Response to COVID-19.
Developing Clinician Guidelines for COVID-19
As a novel pathogen without a pre-defined evidence base, SARS-CoV-2 created an immediate challenge for health systems seeking to triage and treat the rapidly growing population of infected patients. However, it was challenging for clinicians to manage the sheer volume of new research—from the tens of thousands of preprints posted on servers such as medRxiv to peer-reviewed publications in academic journals—particularly considering the significant variation in methodological rigor and evidence quality. Consequently, to balance the urgency for new evidence with the need to uphold standards for quality, health systems and professional societies played an important role in both supporting COVID-19 studies and performing rapid and real-time syntheses of emerging evidence into guidelines to inform best practices for patient care.
Protocol Standardization
At the beginning of the pandemic, government agencies such as the National Institutes of Health (NIH) and global clinical partnerships such as the Surviving Sepsis Campaign worked quickly to extrapolate evidence from other viral infections into evidence-based guidelines for the management of COVID-19 [10]. As new evidence emerged, professional societies within the U.S. worked to update guidelines and communicate the latest evidence to clinicians.
For example, the Infectious Diseases Society of America (IDSA) published initial treatment guidelines in April 2020, and has updated the document more than a dozen times since then to include the latest evidence from trials of potential therapeutic agents [11]. Likewise, rapid recommendations from the Surviving Sepsis Campaign—a collaboration between the Society of Critical Care Medicine and the European Society of Intensive Care Medicine—in March 2020 helped provide clarity about best practices for preventing infection transmission within health care facilities (e.g., the use of fitted respirators by health care workers, the use of negative pressure rooms for infected patients) [12]. Furthermore, the American Association of Critical Care Nurses developed a number of procedure manuals to support trainings for COVID-19 (e.g., for intubation, for oral care practices), and in October 2020 launched an official micro-credential for COVID-19 Pulmonary and Ventilator Care with online verification to standardize and disseminate best practices across the health professions workforce [13,14]. Initiatives such as these were critical for helping clinicians distinguish between the signal and noise in the growing literature on CO-VID-19, and ensure that patient care was informed by the latest standards.
Supporting Clinical Research
Clinicians played a key role in supporting the generation of new evidence in how to treat and combat CO-VID-19, from authoring case reports to collaborating with researchers to support clinical trials for potential therapies and vaccines. However, clinician support for COVID-19 research encountered a variety of challenges.
First, frontline clinicians’ desire to do anything possible for acutely ill patients at risk for rapid deterioration often came into conflict with researchers’ efforts to design and complete randomized clinical trials for COVID-19 therapies [15]. Second, conflicting results from clinical trials, evolving regulatory guidance, and the politicization of science during the pandemic contributed to “panic prescribing,” or the off-label use of medications such as hydroxychloroquine for both CO-VID-19 prophylaxis and treatment [16,17]. To provide guidance to frontline clinicians and help combat panic prescribing, the American Medical Association (AMA), American Pharmacists Association, and American Society of Health-System Pharmacists issued a joint statement on ordering, prescribing, or dispensing COVID-19 medications in April 2020 [18]. To help engage clinicians in COVID-19 research, the federal government developed programs such as the Clinical Trials Improvement activity in the Merit-based Incentive Payment System to encourage clinicians to report COVID-19 data to clinical trials or patient registries [19].
Adapting Delivery Systems
With COVID-19 both increasing staffing demands at outbreak epicenters while disrupting care delivery for other diseases and elective procedures, health systems had to adapt care processes across all fronts to meet ongoing and emerging patient needs. Clinicians played a key role in supporting the adaptation of delivery systems, from flexible staffing for COVID-19 to the adoption of telehealth.
Bolstering COVID-19 Capacity
The surge in COVID-19 patients requiring intensive care soon outpaced the critical care capacity of even large academic medical centers. Although many health systems took steps to repurpose bed space and hospital units—so-called “surge capacity”—to meet patient needs, a key challenge was the shortage of clinicians with expertise in critical care [20,21]. To fill gaps in care capacity, clinicians from service lines which had been halted by the pandemic were often redeployed and retrained when possible using specialized modules to support COVID-19 care [22]. For example, professional societies for medicine (e.g., the American Thoracic Society, the Society for Critical Care Medicine) and nursing (e.g., the American Association of Critical Care Nurses) partnered together to develop online videos and courses on basic critical care management designed for non-critical care audiences. Additionally, with regulators providing temporary flexibilities for licensing and scope of practice, many clinicians volunteered to serve in COVID-19 hotspots to alleviate staffing shortages [23]. However, even as clinicians responded to the numerous calls to action, health systems struggled to procure the necessary PPE, creating persistent challenges for staff safety.
Supporting Care Continuity for Non-COVID-19 Care
The closure of many health care facilities and cancellation of in-person visits and elective procedures risked creating a second “hidden” pandemic through disruptions in chronic disease management [24]. With the Centers for Medicare & Medicaid Services (CMS) issuing temporary policies to support the expansion of telehealth and the Food and Drug Administration (FDA) providing regulatory flexibilities for the use of remote patient monitoring technologies, the locus of care delivery for non-COVID-19 services began shifting from traditional health care facilities to the home [25,26]. Clinicians and professional societies played an important role in supporting this transition, with providers and patients alike facing a rapid learning curve for telehealth.
While telehealth was an important stopgap, virtual care was not a perfect substitute. For example, early evidence comparing the use and content of virtual and in-person primary care visits found that telehealth visits were less likely to include assessments for chronic disease management (e.g., blood pressure measurement) [27]. Likewise, the transition to telehealth was more conducive for some specialties (e.g., behavioral health) as opposed to others (e.g., orthopedics) [28]. Additionally, clinicians encountered technical and operational challenges during the transition to telehealth, from poor integration of telehealth into electronic health records (EHRs) to the “digital divide” affecting the potential ability of marginalized populations to use telehealth [29,30,31]. In addition to telehealth, clinicians—particularly those in community practice—also explored alternative avenues for patient outreach and engagement, ranging from pop-up clinics to house calls [32].
Adjusting Education and Training Programs
Clinical education and training is embedded into the infrastructure of America’s health system. Consequently, as major academic medical centers pivoted to shore up capacity for COVID-19, health professions schools took steps to adjust education and training programs, from the suspension of in-person learning to the deployment of new pedagogical tools to reduce the impact of training disruptions for the next generation of clinicians.
Transitioning to Virtual Learning
In the spring of 2020, many institutions of higher education began transitioning to virtual learning following guidance from the Centers for Disease Control and Prevention (CDC) about recommended event cancellations and public health practices for slowing the transmission of COVID-19. In March 2020, national associations such as the Association of American Medical Colleges (AAMC) and the American Association of Colleges of Nursing (AACN) called on health professions schools to suspend or limit in-person clinical instruction by placing their clinical rotations on hold [33,34]. While each academic institution had to make independent decisions, the recommendations from AAMC and AACN were widely driven by the persistent shortages of PPE across the health system and the collective effort to “flatten the curve” by reducing the potential to spread COVID-19.
The rapid transition to remote learning required innovation at all levels of clinical pedagogy. For example, health professions schools needed to develop contingency plans for how to offer online simulation-based education, particularly for students scheduled to graduate during 2020. The Academic Service Learning opportunities offered by the American Red Cross for prelicensure nursing students or registered nurses working on their bachelor’s or post-graduate degrees are an example of one avenue for student engagement during the pandemic [35]. In addition to retrofitting established clinical curricula to virtual platforms, faculty were also focused on remaining up to date with the current local, state, and national guidelines to help prepare students for the uncertain and dynamic clinical environment they would be entering as new graduates. Reinforcements in public health, emergency preparedness, ethical decision-making, resilience and well-being strategies, and education on proper use of PPE became even more essential to prepare new providers entering the field.
Health professions schools did encounter several challenges during the transition to virtual learning, ranging from the variability in faculty comfort with remote learning platforms to gaps in access and support systems for students. Additionally, although schools sought to continue many non-hospital clinical experiences and create non-clinical volunteering opportunities for students, some students expressed concerns that cancellations of clinical rotations would negatively affect their career progression [36]. To help navigate the uncertainties of the pandemic, national associations and professional societies played a key role in providing guidance to educators and students and developing plans for the resumption of clinical instruction.
Graduation and Entry into Practice
Disruptions to in-person education created an atmosphere of confusion for clinical trainees during the early days of the pandemic, with health professions schools navigating the dual challenges of whether students scheduled to complete their training during 2020 would be able to graduate on time and what the appropriate role of health professions students should be in light of the frontline staffing needs in pandemic epicenters.
In the nursing profession, the Commission on Collegiate Nursing Education (CCNE) released guidance that recommended flexibility in the types of eligible experiences for students and the associated clinical hours as long as the outcomes were met [37]. While CCNE Guidelines for accreditation and the AACN Essentials, which guide nursing school curriculum, do not set clinical hour minimums for prelicensure baccalaureate programs, state boards of nursing vary in their requirements for in-person clinical rotations. This added a layer of complexity for students graduating during the pandemic. Exacerbating concern for an on-time graduation was the initial closure of in-person testing sites for the National Council Licensure Examination for Registered Nurses. Coordination by nursing leaders and professional societies enabled testing centers to reopen under limited capacity in line with the CDC guidelines. As the pandemic wore on, additional guidance was released by AACN to help support schools of nursing reopen safely, taking into consideration campus risk, state alert levels, testing strategies, and clinical placement interactions, among other tactics [38]. Spring of 2020 captured a moment in time that was shrouded by confusion as the entire academic infrastructure navigated federal and state guidance and emerging best practices, and ultimately made decisions based on how best to protect the health and safety of students, faculty, and staff given their assessment of the overall environment. With graduations occurring in May and December of 2020, the task at hand focused on how to re-envision curricula so that students, already critical to the health care system, could be additive to the most pressing demand—vaccination. Health professions schools proved themselves to be active partners in the pandemic response by preparing students for public health efforts such as community education campaigns and contact tracing and moving up training on intramuscular injections [39].
In the medical school community, questions began to arise related to early graduation as medical students were being removed from their fourth year clerkships. Several medical schools, particularly those in COVID-19 epicenters, did allow students who expressed a desire to volunteer on the frontlines to graduate early [40]. However, early graduations were not seamless, as the transition from medical school to graduate medical education is complicated by a myriad number of issues including regulation of licensure and oversight of reimbursement. In April 2020, the Accreditation Council for Graduate Medical Education (ACGME) ultimately released a statement that recommended against the early graduation of allopathic and osteopathic medical students, noting challenges to residency if not appointed to an ACGME-accredited program and the ramifications to early appointments related to CMS reimbursement of direct and indirect graduate medical education [41]. Recognizing the complexity of the situation for students and schools, the variation in medical center-specific staffing needs, and the physical and emotional pressures on trainees, the AMA also issued a series of recommended principles for medical students during COVID-19, including an emphasis that any early graduation initiatives should be voluntary and that such students should be designated as full providers with corresponding benefits to reduce physical risk and professional coercion [42]. ACGME also provided guidance for residents and fellows who may have been redeployed from their specialty area of training to fill staffing gaps in intensive care and meet other pandemic-specific patient needs.
Leveraging Advocacy and Activism
Clinicians have long been viewed as trusted voices of authority in American society. During the pandemic, clinicians often served as credible messengers to keep the public informed about public health best practices. Furthermore, clinician advocacy and activism, particularly on social media, played an important role in spotlighting challenges in the response to COVID-19, especially for issues such as PPE shortages and the impact of health inequities on COVID-19 outcomes. However, clinicians did experience challenges to their expertise and credibility due to the spread of misinformation and disinformation and the politicization of the pandemic [43].
Combating Misinformation
Researchers and health officials at the World Health Organization (WHO) have documented the presence of an “infodemic” during COVID-19, from misleading statements by elected officials to the spread of misinformation and disinformation on social media [44]. These trends were challenging within the clinician community as well, with the sharing of insights about CO-VID-19 on social media blurring the line between individual anecdotes and empirical evidence.
Internally within the clinician community, social media platforms and professional societies began to take an active role in filtering emerging evidence and disseminating updates to guidelines. For example, a private Facebook group called “COVID-19 USA Physicians and Advanced Practice Providers”—which required individuals to verify their provider credentials in order to participate—had over 150,000 members as of fall 2020 and served as a useful forum for discussion and evidence sharing. Likewise, professional societies such as the AMA and the American Nurses Association (ANA) created dedicated webpages to serve as resource centers for clinicians, including guides on topics ranging from a code of medical and nursing ethics for the pandemic to best practices on infection control curated from the CDC, WHO, and other trusted organizations [45,46,47].
Externally, many clinicians became trusted messengers both in their communities and on social media. For example, Twitter, in an effort to reduce misleading misinformation, decided to verify (noted visually on Twitter as a blue check mark next to a person’s username) health care professionals providing sound CO-VID-19 guidance so as to notify users and other health care professionals that the information was deemed reliable and that it was being provided by a person with the prerequisite expertise [48]. At all levels of government, clinicians frequently served an important role in communicating the latest evidence on COVID-19 to the public around testing, infection trends, and new medical products. These actions were important to emphasize public health best practices and evidence-based information, but in some cases carried personal (e.g., harassment on social media) and professional (e.g., potential penalties from employers) risks for clinicians [49,50].
Advocating for Pandemic Response
In addition to serving in an informational capacity, clinicians also organized at the national and grassroots levels to draw attention to the challenges of America’s pandemic response. For example, a key area of focus was the persistent shortage of PPE in hospitals and health care facilities [51]. In response, health care workers organized on social media using the hashtag #GetUsPPE, launching a survey to identify PPE shortages across the country and partnering with professional societies to coordinate last-mile distribution of PPE at various health care sites [52].
Clinician advocacy placed particular emphasis on highlighting the disparate impact of COVID-19 on communities of color. National organizations, including the AMA and ANA, played a leading role from the outset of the pandemic in advocating for improvements in the collection of race and ethnicity data to assess the impact of COVID-19 on marginalized populations [116]. Additionally, following the tragic deaths of George Floyd, Breonna Taylor, and many other Black Americans during the pandemic, coupled with the disparate impact of COVID-19 on communities of color, clinicians organized to draw attention to the role of racism as a public health crisis. Statements from numerous professional societies affirmed the health consequences of structural racism and the necessity of embedding a focus on equity into clinical education and practice, and the Rainbow PUSH Coalition and National Medical Association collaborated to develop the COVID-19 Public Health Manifesto [53,54,55]. Furthermore, amidst the growing number of reports of hate crimes against Asian Americans and Pacific Islanders during the pandemic, national organizations including the AMA and ANA spoke out to condemn xenophobia and racism, with the AMA highlighting the structural roots of present-day discrimination and the American Academy of Nursing issuing a statement identifying “Anti-Asian Discrimination as a Public Health Crisis” [117,118,119].
Lastly, a key focus of clinician advocacy was addressing hesitancy surrounding the development and authorization of COVID-19 vaccines. For example, Black doctors in the National Medical Association formed a panel to review clinical trial data and organized listening sessions in collaboration with community leaders from organizations such as churches, fraternities, and sororities to address misinformation [120]. Similarly, Black nurses and doctors formed the Black Coalition Against COVID-19, which compiled resources and coordinated virtual town halls with key government officials to keep communities informed about the vaccine [121]. While these examples of advocacy illustrate the role of clinicians as “trusted messengers,” they also highlight the elevated burden borne by minority clinicians during the pandemic, who have long been underrepresented across the health profession.
Key Challenges for the Clinician Sector During COVID-19
While clinicians have displayed remarkable resilience and innovation on the frontlines during the response to COVID-19, the pandemic has magnified many existing, systemic challenges across the sector. For example, the acute and prolonged stress of working under surge conditions has intensified the multiple, well-documented sources of chronic distress and “moral injury” already endemic among health professionals today, challenging the long-term well-being and stability of the clinician workforce. Likewise, the upheaval to clinician education, practice, and finances during the pandemic has highlighted certain long-standing, structural inadequacies of clinician training, staffing, and financing. This section examines the systemic vulnerabilities in the clinician sector exposed and exacerbated by CO-VID-19, with a key focus on the following:
-
1.
Clinician well-being and occupational distress;
-
2.
Staffing and operations;
-
3.
Disruptions to education and training; and
-
4.
Financial and administrative impacts (see Table 1).
TABLE 1. Key Challenges for the Clinician Sector.
| Challenge Area | Pre-Pandemic Trend | COVID-19 Experience |
|---|---|---|
| Clinician well-being and occupational distress |
|
|
| Staffing and operations |
|
|
| Disruptions to education and training |
|
|
| Financial and administrative impacts |
|
|
Clinician Well-Being and Burnout
Pre-Pandemic Trends in Burnout and Degraded Well-being
Over the past two decades, multiple complex factors have contributed to the growing challenge of occupational distress among health care professionals, which can manifest in a number of ways, including problems with work-life integration, fatigue and other physical symptoms, and moral distress and a loss of meaning in work [56]. One of the most common manifestations of work-related distress is burnout [5,57]. National studies prior to the COVID-19 pandemic suggest that between 35% and 45% of clinicians have high levels of occupational burnout [58,59,60]. Notably, nearly 20% of interprofessional clinicians reported they are considering leaving their jobs because of moral distress, which is the inability to translate moral choices into action, and is experienced by members of the clinical team in response to the ethical issues that threaten or violate their integrity [61,62,63]. These studies also suggest that burnout symptoms and challenges with work-life integration are more prevalent among clinicians compared to other sectors of the U.S. workforce [64].
As reviewed in the National Academy of Medicine’s (NAM) 2019 consensus study on clinician burnout, the causes of occupational distress are multifactorial and include excessive clinical demands, decreased control over work, inadequate time with patients, regulatory issues that create administrative burdens and lead to inefficiencies in care delivery, challenges integrating clinicians’ personal and professional lives, unresolved ethical issues, suboptimal teamwork and unprofessional behavior by some team members, and inefficiencies created by suboptimal technologic tools and isolation from their patients [5]. Mounting evidence has documented how these stressors can cause adverse personal (e.g., broken relationships, depression, thoughts of suicide) and professional (e.g., absenteeism, presenteeism, increased risk of medical errors, decreased clinical productivity, increased risk for turnover) consequences in health care professionals [65,66,67,68]. All of these consequences reduce the ability of delivery systems to achieve health care’s quadruple aim of better care experiences and population health at a lower cost while fostering clinician well-being [122].
COVID-19 Stressors
The pandemic introduced new dimensions of chronic stressors to the clinician workforce, summarized in Figure 2 [68].
FIGURE 2. COVID-19 Stressors for Clinicians.
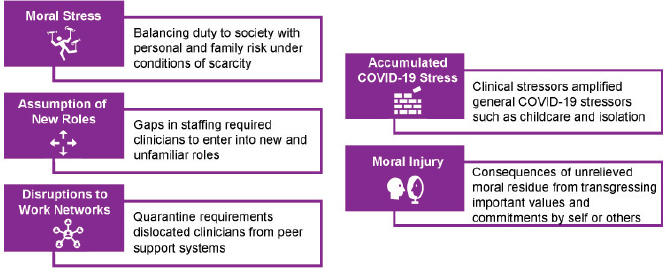
First, clinicians experienced moral stress in their attempt to balance their duty to society with personal health risks, particularly for older health care workers and those with health issues placing them at high risk for severe or fatal COVID-19 infection. Health care workers faced intensified concerns about the personal risk of becoming infected and the fear of being a vector of infection for their family members. The accumulated moral burden was often exacerbated by shortages of PPE, with many clinicians consequently considering quarantining themselves from their families despite their own needs for support and connection, further amplifying the experience of moral fatigue. Their moral stress was exacerbated by the introduction of novel ethical dilemmas created by models for allocating scarce resources, and intensified by new practice patterns and protocols, uncertainty or inconsistent decision-making, lack of health care worker protections, organizational structures for reporting concerns, and crisis management protocols that shifted decision-making from individual clinicians to triage officers.
Second, clinicians answering the call to action on the frontlines were frequently deployed outside their typical area of practice, forcing them to acquire new skills and raising concerns that they were not providing optimal care or were causing harm to their patients. Most organizations also adopted strict visitation guidelines aimed at protecting the health of patients, families, and staff, which had the unintended consequence of creating moral distress for clinicians who assumed new roles to bridge the gaps left by family member absence and witnessed patients dying alone.
Third, disruptions to the workplace environment unmoored clinicians from their professional support networks during a time of crisis. For example, for the thousands of health care workers who did contract the virus, the resulting quarantine requirements created additional stress by separating clinicians from their peer support systems at work and lead many health professionals to feel as though they were abandoning colleagues and patients in a time of need. Likewise, numerous clinicians went above and beyond their professional responsibilities only to be given notice of furloughs or layoffs when the crisis began to subside, disrupting team stability and cohesion at the precise time that health care workers were most reliant on support from one another. Social support, a key element of resilience, was also disrupted or dismantled.
Fourth, all of these occupation-specific challenges for clinicians were layered on top of the general social challenges of COVID-19 experienced by all Americans. Clinicians simultaneously had to navigate challenges such as childcare, family issues, and adjustments to shelter-in-place restrictions, all while lacking the ability to engage in many of the activities that health professionals traditionally relied on to recharge (e.g., recreation, social connection). Clinicians’ prolonged exposure to critically ill and dying patients coupled with the systemic failures of organizations and the government resulted in unacknowledged and unprocessed grief for health care workers alongside the collective grief of the pandemic itself.
Fifth, COVID-19 exacerbated moral injury, which involves the betrayal of what one believes is “right,” often in high stakes situations by those with legitimate authority or directly or indirectly by one’s own actions or those of others [69]. The preceding factors converged to create the conditions for what many clinicians experienced as an assault on their professional values and commitments [70,123,129]. Severe shortages of clinicians to treat the volume of patients with COVID-19, lack of governmental and organizational leadership and coordination, and systemic inequities that disproportionately impact people of color further eroded clinicians’ ability to fulfill their core professional values [123]. As the pandemic progressed, clinicians were confronted with patients who refused to accept their COVID-19 diagnosis and accused clinicians of deceit or malintent, adding to their sense of defeat, discouragement, and fatigue. Instead of receiving the strength to keep going from their patients, clinicians experienced significant emotional distress when realizing that they had sacrificed their own well-being to provide care and treatment for the unrelenting number of people who contracted the virus—some because of lack of adherence to public health guidelines or lack of belief in the truth of COVID-19’s existence. The moral residue of these unmet moral and ethical commitments has the potential to contribute even further to the physical and psychological burden of the pandemic.
Collectively, these challenges have resulted in massive acute stress and suffering for clinicians that is superimposed on the pre-existing occupational distress for the health profession. A number of studies have highlighted the increased rates of insomnia, anxiety, grief, depression, PTSD, and moral distress and injury among clinicians caring for COVID-19 patients during the pandemic [10,71]. Distressingly, the emerging evidence suggests that the risk of these conditions is greatest among clinicians who are women and who are nurses. These are also the individuals who typically bear the greatest burden of child and family caregiving, and as a consequence have experienced a dual burden of stress due to pandemic-induced disruptions to normal life [71].
The profound emotional, moral, and psychologic distress of clinicians during the pandemic, coupled with the erosion of trust in the health system due to failures of the COVID-19 response (e.g., shortages of PPE), the financial impact of the pandemic (e.g., pay cuts, furloughs, layoffs), and the misinformation spread by some elected officials (e.g., claims that clinicians were lying about or profiting from COVID-19), threaten the long-term well-being of the clinician workforce, and have systemic consequences for care delivery during and after the pandemic. COVID-19 is consequently a clarion call for the need to address clinician burnout, which long precedes the pandemic. Policymakers and health system leaders will need to take steps to develop holistic frameworks and multifaceted support systems that remodel delivery environments to promote clinician well-being [124].
Staffing and Operations
While clinicians mobilized rapidly on the frontlines to support the response to COVID-19, the growing pains of redeploying clinicians from different sectors, the technical challenges of sharing data and coordinating across teams, and the targeted gaps in capacity across key clinical domains highlighted a number of challenges for staffing and operations.
Staffing and Clinical Capacity
Researchers have long drawn attention to the shortage of various health care workers and providers in the U.S. A key area of neglect has been in critical care capacity, with frequent shortages among both intensivists and registered nurses in the ICU and in stepdown units due to the specialized training required to work in such environments and the high burnout rates reported by providers due to the harrowing experience of caring for acutely ill patients [21,72,73]. The consequence of these shortages was apparent during the COVID-19 pandemic, particularly given that between 12% and 33% of patients hospitalized with COVID-19 required ICU admission or mechanical ventilation [74,75,76].
While clinicians, as noted in the subsection on “Adapting Delivery Systems,” took steps to fill capacity by cross-training from different specialties or traveling to COVID-19 hotspots to volunteer at overwhelmed facilities, these temporary measures belie the systemic challenges facing the clinician workforce. From an operational perspective, pandemic-era innovations to centralize staffing and triage processes represent opportunities to improve the efficiency and flexibility of critical care both at baseline and during emergency situations. Additionally, evidence about the importance of collaborative clinical care during COVID-19 should encourage the adoption of integrated and multidisciplinary clinical teams across hospital service lines. From a capacity perspective, the sheer volume of staffing needs should be a call to action to invest in the pipeline of critical care clinicians and other specialties with long-standing staffing gaps.
Digital Infrastructure
Care delivery in the U.S. health system has long been fragmented, and a key challenge has been the lack of interoperability among data systems and EHRs. The importance of an interconnected and learning health system was evident during the COVID-19 pandemic, particularly due to the expansion of telehealth and remote patient monitoring. For example, challenges with electronic case reporting and differences in the type and quality of data collected within and across systems created challenges for clinicians caring for COVID-19 patients (e.g., delays in transmitting testing data affected decision-making for admissions and discharge). Likewise, variation in data systems and reporting capacity contributed to challenges for facile enrollment and follow-up for COVID-19 clinical trials. Furthermore, for non-COVID-19 care, gaps in the integration of telehealth and EHRs risked disrupting care continuity and care handoffs.
Clinicians did deploy technology throughout the pandemic to expand capacity, such as the development of virtual triage clinics and the creation of critical care command centers and tele-ICU teams [77]. However, shifting the modality of care delivery does not resolve the underlying shortages in the clinician workforce that will require attention. In addition, sustainably integrating telehealth into care delivery moving forward will require policymakers and health system leaders to address systemic shortcomings in existing digital and technical infrastructure, with a particular focus on promoting interoperability and adopting uniform standards for data collection.
Disruptions to Education and Training
While health professions schools and academic medical centers pivoted quickly to remote learning platforms and professional societies introduced guidelines and flexibilities for current and graduating students, the overall disruption to clinical education during the pandemic has created several challenges for the sector as a whole.
Impact on Training Programs
To preserve PPE, optimize staffing, and minimize infection risk, health professions schools had to adjust training programs, affecting the clinical education of health professions students.
First, many health professions schools paused clinical rotations for their students during the pandemic, interrupting an important period of clinical immersion for trainees [78]. Second, at many academic medical centers, staffing shortages led to the redeployment of residents and fellows. For example, in one New York City hospital, pediatric residents were deployed to care for adult patients [79]. While trainees rose to the occasion to meet the needs of patients, changes in clinical workflow posed challenges due to the rapid learning curve and have led to gaps in the clinical training of these trainees. Third, the training of physician- and nurse-scientists was disrupted as many research laboratories were either closed or repurposed for COVID19-related activities (e.g., to serve as processing centers for COVID-19 diagnostics), and trainees were in many cases redeployed to fill clinical needs [86]. Interruptions to the protected research time (for students) and laboratory start-up time (for early-career investigators and post-doctoral fellows) affected activities ranging from experiment completion to manuscript revisions to grant applications and renewals, all of which may carry consequences for future academic careers. Distressingly, the career costs of COVID-19’s disruption of research activities appear to have disproportionately affected female scientists, as evidenced by the widened gender gap in publications during the pandemic, threatening to exacerbate long-standing inequities in academic nursing and medicine [81,82].
Financial Impacts
Health care systems and institutions of higher education across the country have suffered severe financial impacts due to COVID-19. To stabilize university finances, many schools took actions such as issuing hiring freezes, furloughing faculty and staff, and introducing pay cuts, with these steps carrying short- and long-term implications for students and faculty.
First, from the perspective of faculty and newly minted clinicians interested in academic careers, many research programs at universities have been placed on hold during the pandemic as laboratory space and program resources were redirected to support pandemic activities. Many nurse- and physician-scientists paused their primary research focus to engage with the COVID-19 research response [83]. Furthermore, hiring freezes may create challenges for the next generation of clinician-researchers in entering academic life.
Second, from the perspective of students, a year of remote learning during an economic crisis without a commensurate change in tuition rates has once again spotlighted the increasingly unaffordable nature of health professions education in the U.S. To ensure the sustainability of education for incoming and current students, guidelines for financial aid and student loan programs need to be amended to address flexibility in their requirements while at the same time offering relief. In the long term, policymakers and education leaders will need to renew conversations around increasing the affordability and sustainability of financing clinical educations, with a number of preexisting programs for loan and debt forgiveness coupled with innovations in pedagogy (e.g., efforts to shorten training) providing opportunities for further consideration [83].
Disparities in Educational Access
Within the clinician workforce itself, students of color have been disproportionally impacted by COVID-19 as they attempt to cope with the disturbing effects of the pandemic in their communities. The emotional and mental strain of the pandemic compounds the existing challenges of institutional racism embedded in America’s education and health structures, which long predates COVID-19 [85]. For students already enrolled in a health professions school, the transition to virtual learning was uneven due to resource inequities. For example, students who lacked access to high-speed internet or institutions which had lesser technical capabilities not only experienced disparities in didactic instruction (e.g., lectures, exams) but also in their ability to take part in remote versions of clinical training (e.g., scribing, telehealth visits, volunteer opportunities) [86].
In addition to increased awareness about inequities within clinical education during the pandemic, the disparate impact of COVID-19 on marginalized populations coupled with broader public discussion on racism and social justice during 2020 spotlighted many of the longstanding disparities in health professions education writ large. For example, nearly one-third of all Americans are either Black (13%) or Latinx (19%) [125]. However, not a single medical specialty adequately reflects the racial and ethnic diversity of the broader U.S. population, despite evidence indicating improved health outcomes when patients are cared for by clinicians from a similar demographic background [87,88]. Likewise, the number of Black men matriculating to medical school remains largely unchanged over the past 30 years, even as the population of Black men in America grows, broadening this already existing disparity [89]. In baccalaureate nursing programs, only 11% of students are Black and 13% are Hispanic or Latinx [90]. While many health professions schools reaffirmed their commitment to addressing health disparities during the pandemic, the challenge for these institutions will be translating rhetoric into reality, including investments to diversify the clinician pipeline, policies to increase the affordability and accessibility of clinical education, and pedagogical interventions to introduce a meaningful focus on equity at all levels of clinical training [91].
Financial and Administrative Impacts
Despite their centrality to the pandemic response, clinicians experienced a paradox of extreme financial instability. Delays in non-COVID-19 care and the cancellation of non-emergent procedures cut off key revenue streams for physicians and highlighted the instability of a fee-for-service reimbursement system. Furthermore, physicians and nurses alike struggled to comply with administrative requirements due to the stress and workload of the pandemic. While regulatory flexibilities (e.g., reimbursement for telehealth) and financial relief (e.g., from the Provider Relief Fund) did help to alleviate the immediate impact of the pandemic, the financial and administrative challenges of COVID-19 highlight deeper vulnerabilities for the clinician sector.
Disruptions to Clinician Reimbursement
The majority of clinicians, including physicians and Advanced Practice Registered Nurses, continue to be reimbursed through inflexible payment models that often fail to support the deployment of high-value services such as team-based efforts to proactively manage preventative and chronic disease care outside the office. Early in the pandemic, temporary practice closures, deferred patient visits, and sustained volume reductions to support social distancing requirements and conserve PPE precipitated extraordinary and sudden drops in fee-for-service based clinician revenue. The financial impact was magnified after factoring in the expenses incurred from responding to COVID-19, including the cost of procuring PPE (which due to shortages, often required practices to pay significant markups), performing frequent cleanings, upgrading ventilation systems, and redesigning office environments to minimize infection risk. Indeed, 81% of physicians continued to report lower revenue compared to pre-pandemic levels as of August 2020, with an average decline of 32% [92].
However, federal relief funds appropriated through the Coronavirus Aid, Relief, and Economic Security (CARES) Act helped prevent insolvency, and health service volumes have rebounded to pre-pandemic utilization levels for some specialties [28]. Despite considerable improvement and stabilization in fall 2020 compared to spring 2020, clinicians continue to express concerns about the uneven nature of the recovery, with national surveys during the fall of 2020 indicating that a significant number of nurses (32%) and primary care physicians (43%) believe that the financial recovery from COVID-19 for clinicians would take over a year [93,194]. The escalation of the pandemic during the winter of 2020 increased the strain on clinicians, with 91% of practices reporting a personnel shortage even as 62% of clinicians reported an increase in patient complexity. The prolonged nature of the pandemic has taken a toll, with over half of physicians reporting greater problems with payments in December 2020 as compared to the spring of 2020 [95]. While the situation continues to evolve and trends for utilization and reimbursement remain dynamic, it is clear that the disruption induced by COVID-19 and the uncertain timeline for resolving the public health emergency have generated substantial pressure on the clinician sector.
Temporary policies from public and private payers to reimburse telehealth at parity with in-person visits for the duration of the public health emergency have offered a financial lifeline for many physicians and nurses, while sustaining access to care for some patients. However, surveys of physicians indicate that the growth in telehealth visits early in the pandemic did not fully compensate for the decline in in-person visits, contributing to gaps in revenue [92]. Additionally, the transition to telehealth came at an operational cost (e.g., digitizing processes, procuring necessary hardware and software, aligning health record systems). Furthermore, while payers have reimbursed telehealth at parity, physicians have found it challenging to keep up to date with rapid changes in payment processes across different plans [96].
A final challenge, related to the difficulties of billing, has been ensuring appropriate reimbursement for physicians providing COVID-19 care. Collaboration between the Current Procedural Terminology (CPT) Editorial Panel and the AMA and Specialty Society Relative Value Scale Update Committee helped create a new CPT code that appropriately quantifies the specific attributable costs for new infection control processes during the pandemic [97]. However, the time required to create and value the code and the delays in adoption by payers into their individual plan’s coverage policies further added to the financial challenges of physicians.
Changes in Administrative Requirements
Many national incentive programs for clinicians rely on quality measure reporting and data submission for attribution and risk adjustment. However, COVID-19 exacerbated long-standing challenges for clinicians with quality measurement requirements, which can often be burdensome, somewhat unaligned between payers, and provide only lagging feedback. Clinicians were further pressured during COVID-19 in fulfilling these administrative requirements (e.g., those required for Medicare’s Merit-based Incentive Payment System, or MIPS). Such disruptions posed a setback for the larger quality improvement enterprise and limited policymakers’ capacity to rapidly expand and target specific data collection for COVID-19.
The pandemic also illustrated how some administrative requirements in health care can constrain clinician decision-making and delay patient access to clinically appropriate care. A leading example of this is prior authorization, a well-intentioned tool for utilization management that has unfortunately created a significant administrative burden for clinicians, negatively affecting the timeliness and outcomes of care delivery, and increasingly shifting financial responsibility for necessary care onto patients [97,98,99].
During the pandemic, many payers worked to streamline some administrative requirements to avoid care delays. For example, a number of payers temporarily paused some quality measurement programs or waived prior authorization requirements for certain types of COVID-19 and non-COVID-19 care (e.g., prescription medications, in-network facility transfers). Additionally, several other administrative requirements (e.g., documentation and signature requirements for various medical orders) were also temporarily waived to remove bottlenecks to care delivery and avoid adding to clinicians’ already high rates of burnout during the pandemic [100].
These policies are generally time-limited and are expected to expire at the conclusion of the public health emergency. However, some pandemic flexibilities may provide an opportunity to address pre-pandemic concerns around the burden of administrative requirements, such as the potential negative consequences of prior authorization on the timeliness of care delivery and the financial responsibility borne by patients. In the aftermath of the pandemic, it will be critical for payers and policymakers to resist a “return to normal,” considering the significant body of evidence about the inefficiencies of existing administrative requirements and their association with clinician burnout. Consequently, clinicians should work to partner with leaders across other sectors to evaluate the experience from pandemic-era flexibilities to support the transformation of the quality measurement ecosystem and associated administrative processes.
Priority Actions and Policy Considerations
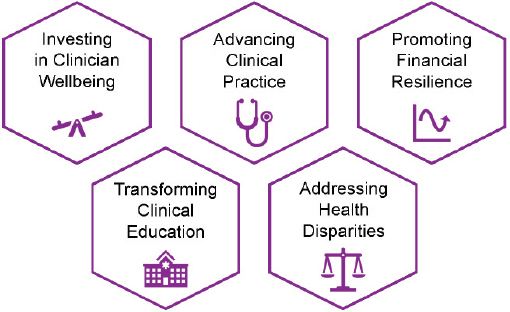
COVID-19 has illustrated the critical importance of a robust, healthy, and resilient clinician workforce to not only support the response to public health emergencies, but also meet urgent population health challenges such as the management of increasingly complex chronic diseases. To build on the innovations and adaptations of clinicians during COVID-19, regulators will need to implement policy and programmatic changes to improve the sector’s overall preparedness and efficiency. In tandem, given the heavy toll levied by the pandemic on clinicians’ morale and financial stability, it will be critical that policymakers and system leaders take steps to commit to long-term investments in workplace transformation and practice improvements to address systemic challenges facing the sector. This section outlines the priority actions and policy considerations for the clinician sector in the post-pandemic era, with key domains of focus including:
-
1.
Investing in clinician well-being;
-
2.
Advancing innovations in clinician practice;
-
3.
Promoting financial resilience for clinicians;
-
4.
Transforming education and training; and
-
5.
Developing policies and programs to address health disparities (see Figure 3)
FIGURE 3. Priority Areas for the Clinician Sector.
Investing in Clinician Well-being
A holistic assessment of the clinician workforce during COVID-19 requires acknowledging the mental, physical, and moral toll of the pandemic as well as the commitment, tenacity, creativity, and perseverance of health professionals. Many clinicians met both the sheer, physical requirement of caring for volumes of patients that exceeded clinical capacity and the mental and emotional strain of navigating system failures and profound and acute suffering with compassion and altruism. These examples of resilience and integrity should not be overlooked or taken for granted, and are a testament to the tremendous clinical leadership and clinician sacrifices undergirding America’s pandemic response.
Yet in tandem, celebrations of clinician resilience must be accompanied with an examination of the well-documented and quantified emotional, psychological, moral, and physical burden experienced by clinicians during the pandemic. COVID-19 has helped to increase awareness about the challenges of burnout and other forms of distress, and the importance of clinician well-being at both the organizational as well as the societal level. Creating space for this conversation has led to sober yet realistic assessments of the current inadequacies of support systems for clinicians and the negative consequences on care quality and outcomes when clinicians are experiencing burnout, moral distress, and in more extreme circumstances, moral injury. Importantly, the pandemic has also generated an impetus for change, with an increasing number of organizations committing themselves to advancing the welfare of their clinical care teams. Notably, COVID-19 has helped empower clinicians to be their own advocates, with numerous examples of health care workers identifying creative solutions to the acute challenges of burnout and systems failures during the pandemic, ranging from addressing shortages of PPE to managing the complexity of staffing to developing new strategies for communication with patients and families. These efforts have affirmed the importance of grounding clinical work in relationships with patients and fostering workplace environments that are diverse and collaborative spaces for clinicians to thrive.
BOX 1. Considerations for Investing in Clinician Well-Being.
Rebuild the trust that has been eroded during the pandemic by focusing on transparent communication and listening to and acting upon the concerns of frontline clinicians
Health care organizations should act on the recommendations in the NAM’s 2019 report on clinician well-being. In particular, health care organizations should prioritize the mitigation of burnout and contributing factors (e.g., moral distress, problems with teamwork, inefficiency, work-life integration issues, isolation), develop a strategy, infrastructure, and leadership (e.g., Chief Wellness Officers) to address the issue, and measure progress on improving well-being
Strengthen protections for clinicians to report safety and ethical concerns without retribution or retaliation. Create provisions for risk compensation, disability insurance, and life insurance protections for health care workers
Train senior leadership, supervisors, and managers in the leadership behaviors that cultivate well-being, promote equity and inclusion. Leaders should also be trained to proactively recognize symptoms of emotional and moral distress, mental health issues and functional impairment in health care workers and understand how to guide referrals to institutional or community resources
Remove stigma and barriers to the use of mental health resources, including by providing sufficient insurance coverage for ongoing mental health services and access to mental health providers who are not employed by the health care organization and are trained in trauma informed care
Building on this momentum and supporting the revitalization of the clinician workforce in the aftermath of COVID-19 will require addressing the long-standing drivers of chronic occupational distress and moral injury in the clinician workforce. The NAM’s 2019 consensus study on clinician well-being provides an important starting point for policymakers and system leaders to begin to take action to proactively monitor clinicians for symptoms of occupational distress and develop robust support systems for clinicians experiencing emotional, psychological, and moral distress, with attention to reducing the stigma associated with seeking mental health care and associated services [5]. Some examples of tangible organizational, associational, and policy actions that leaders can take to address drivers of distress include developing a robust monitoring system with validated measurement tools for burnout and other forms of distress, realigning educational incentives to ensure that training programs foster professional well-being, and reducing burdensome administrative and documentation requirements.
Leaders themselves at all levels of the organization, from managers to executive team members, will also need training in the behaviors that promote well-being, and will need to apply frameworks for cultivating more inclusive and nurturing cultures among all clinicians [126,127]. Modeling these behaviors by leadership is necessary to combat the high prevalence of stigma that clinicians report to be associated with seeking mental health resources. For example, a recent survey of nurses indicated that a lack of time and concerns around retribution, stigma, confidentiality, and licensing were among the leading deterrents to utilizing professional mental health support [128]. Leaders will also need to remain vigilant as many of the consequences of the pandemic on the health care workforce are still evolving, and the full impact of the pandemic will likely not be apparent for some time. To avoid further degradation of workforce well-being, policymakers and health systems need to act now and embrace a new paradigm of collaborative design with leaders and frontline clinicians to stem the tide of occupational distress, burnout, and moral suffering in health care.
Priority actions for investing in clinician well-being are summarized in Box 1.
BOX 2. Considerations for Advancing Innovations in Clinician Practice.
Advance frameworks that facilitate the ability of clinicians to be licensed in and care for patients in multiple states while following state licensure requirements
Implement effective recruitment and retention strategies to address workforce shortages in nursing and critical care
Encourage the use of system-wide standardized evidence-based protocols for critical care processes and encourage continuing education for clinicians related to key critical care functions
Within academic institutions, evaluate internal research review and oversight processes to reduce barriers and prioritize and accelerate needed research efforts during a crisis; for other trusted entities, publish evidence-based practice guidelines for clinicians rapidly and frequently during evolving public health emergencies
Invest in the infrastructure needed to achieve effective health data sharing, especially between health care organizations and public health departments and officials
Advancing Innovations in Clinician Practice
COVID-19 has demonstrated the value of regulatory flexibilities (e.g., the temporary removal of licensing barriers to interstate practice) and organizational innovations (e.g., the development and uptake of crisis standards of care) for adapting clinical practice to meet patient needs. However, the pandemic has also illustrated the need for improvements in clinical capacity and infrastructure to break down siloes (e.g., between clinicians and researchers) and improve coordination (e.g., between clinicians and public health departments and officials) to foster preparedness for future public health emergencies.
In the aftermath of COVID-19, professional societies will need to review both the process and outputs of guideline development during the pandemic to identify best practices for developing and disseminating guidelines for clinical practice during crisis situations in which the evidence base is rapidly evolving. For example, academic journals played a key role in accelerating the review and publication of new materials by adopting open access policies and receiving support from clinician researchers to expedite peer review. This in turn allowed for the rapid publication of and subsequent updates to clinical guidelines. A review of the clinical research experience during COVID-19 should also include a recognition of the fragmentation of many research efforts and the tensions that arose between clinical care and clinical research. Conversations and partnerships between health care organizations (e.g., Institutional Review Boards) and the research bodies (e.g., the NIH) to develop a dedicated infrastructure for large-scale platform trials, standards for data collection and exchange, and clear protocols would help improve coordination and ensure the sufficiency of study rigor (e.g., power, randomization). Beyond supporting research, bolstering clinical capacity for crises will require care organizations and professional societies to identify the potential skills and capacity gaps exposed by COVID-19 and work to accordingly update continuing education practices and support workforce development initiatives.
The pandemic has also illustrated the importance of digital tools and robust technological infrastructure for the future of clinical practice. Partnerships with policymakers will be key to ensuring that standards for the seamless exchange of data are implemented, guidelines for patient privacy are clarified, and resources to support the modernization of organizational competencies are available (particularly at the practice level, where the adoption of digital tools and telehealth has been uneven, especially among rural and safety net populations). Regulators will also need to collaborate with professional societies and clinicians to determine what lessons can be identified from COVID-19 flexibilities (e.g., around licensing) to maximize clinician capacity for the post-pandemic era. Central to these discussions will be balancing the need for appropriate oversight and credentialing with the recognition of pervasive capacity gaps in communities across America.
Priority actions for advancing innovations in clinical practice are summarized in Box 2.
Promoting Financial Resilience for Clinicians
With COVID-19 exposing the fragility of a volume-based reimbursement system, policymakers will need to implement payment reforms that drive improvements in quality, decrease spending, and promote financial resiliency for clinicians by transitioning to a more diverse set of payment models. Many examples of alternative payment models (APMs) have been trialed over the past decade, some of which may have been associated with modest cost savings pre-pandemic and improved financial positioning for clinicians during COVID-19. However, widespread adoption of such models has lagged. First, interested practices often lack the resources needed to invest in the tools and data systems needed to redesign care delivery. Second, the steep requirements for financial risk inherent in many APM models have posed barriers to participation. Third, the risk adjustment for many APMs has been perceived to be inadequate, particularly given emerging evidence demonstrating the financial losses incurred by providers who treat patients with greater medical and social needs [101].
BOX 3. Considerations for Promoting Financial Resilience for Clinicians.
Develop and implement innovative payment models that drive quality and value while building the resiliency and sustainability of clinical practices
Fund payment models that support high quality team-based care delivery and coordination in treatment planning and management
Build on COVID-19 reporting flexibilities to streamline future quality measurement and reduce the administrative burdens associated with prior authorization
Establish a standard approach for supporting patient access and continuity of health care during public health emergencies and natural disasters
Establish longer-term coverage and payment policies for telehealth services to promote continued availability of these services by medical practices post-COVID-19
To strengthen the health care system and make practices more resilient to future public health emergencies, regulators should take steps to redesign payment models and provide the necessary support to clinicians to facilitate the transition away from volume-based reimbursement. Increasing the accessibility of pilot programs (e.g., Medicare’s medical home models) for clinicians and fostering partnerships with payers may promote the adoption of new payment systems. Importantly, policymakers must also provide meaningful opportunities for clinicians to engage in the payment redesign process, particularly given the limited engagement by policymakers with existing advisory groups (e.g., the Physician-Focused Payment Model Technical Advisory Committee) [102]. Good faith, cross-sector collaborations—such as those formed during the pandemic—can help achieve consensus and spur the adoption of tangible reforms.
In addition to realigning financial incentives, policymakers, payers, and clinicians should work together to evaluate how COVID-19 flexibilities, where appropriate, could be iterated upon to reduce the administrative burden of clinicians. While quality measurement is critical to payment reform, measurement for the sake of measurement only adds to the administrative burden of clinicians. To improve and reinvent the quality measurement ecosystem for future pandemics, CMS and commercial payers should focus on streamlining measure sets to prioritize the most impactful metrics for patients and clinicians. Furthermore, transitioning to a selective approach for prior authorization, as proposed in a 2018 consensus statement issued by professional societies and industry associations, can help improve transparency, efficiency, and continuity of care beyond the pandemic [103].
As policymakers take steps to implement payment reforms, they must also recognize the fragile state of many practices following COVID-19. While the rapid allocation of federal relief funds helped temporarily stabilize many practices, assistance was fragmented, leaving out certain critical providers, and the duration of these measures remains inadequate to address ongoing revenue losses and increased expenses. In the short term, Congress and CMS could help accelerate providers’ recovery from the financial impact of COV-ID-19 by extending pandemic-era policies for telehealth reimbursement, while using the lens of value-based payment to develop telehealth payment policies for the long term. With a growing body of evidence from the pandemic illustrating that many clinical conditions could be effectively managed using virtual care modalities, regulatory actions—including permanently lifting originating site requirements, and continuing coverage of certain telehealth modalities—will help support the continued use of these delivery innovations. In the long term, policymakers should build on the recent experiences with advanced payments, provider relief funding, and cost sharing waivers to establish standard approaches to support patient access and continuity of medical care during future public health emergencies.
BOX 4. Considerations for Transforming Education and Training.
Address the drivers of inequities in resources and learner experiences in academic medicine and nursing, including structural racism
Address financial barriers to student access and progression in health professions education
Expand the prevalence of competency-based, time-variable education across health professions programs
Advance innovation in health professions education through technology and simulation for continuous learning
Priority actions for promoting financial resilience for clinicians are summarized in Box 3.
Transforming Education and Training
Pandemic-induced disruptions to and innovations in clinical education provide an important window for clinicians and professional societies to build upon existing momentum for reform to improve the affordability, accessibility, and equity of clinical education in the 21st century.
As a starting point, the broad inequities exposed by the COVID-19 pandemic illustrate the need for health professions schools to appropriately transform their curricula to prioritize attention to equity. In tandem, academic medicine and nursing will need to take a deliberate approach to rethinking pipeline recruitment, clinical training, hiring processes, and workforce organization to improve diversity across all axes of representation and create clinical environments that support the development of historically underrepresented and marginalized populations [91,104]. For example, the economic impact of the pandemic on both student and university finances should prompt a meaningful conversation about opportunities to improve the affordability of clinical education, and should merit consideration from policymakers to expand existing clinician pipeline programs, including the Health Career Opportunity Program and the National Health Service Corps [105,106,107]. Likewise, educators should incorporate lessons from COVID-19 to improve the equity of training and application processes, such as addressing the inequities created by the inconsistent availability of visiting clinical rotations in medical residency selection processes [108]. To operationalize this systems-based approach to improving equity in clinical education, health professions schools will need to develop systems for measuring and assessing progress toward diversity, equity, and inclusion [109].
Efforts to transform clinical curricula should also incorporate evidence from COVID-19 on different pedagogical innovations. For example, educators may seek to update their curricula to include a new focus on crisis communication, critical appraisal of scientific evidence, and experiential opportunities to enhance “webside” manner for a new generation of clinicians who are digital natives [110]. In the process, the trauma of COVID-19 should prompt educators to devote greater attention to issues of clinician well-being and ethical decision-making. The pandemic has also emphasized how clinical care is a “team sport,” and that interprofessional education for physicians, nurses, and other allied health professionals is critical for the delivery of safe, empathetic, and high-quality patient care.
Furthermore, COVID-19 has illustrated the value of competency-based, time-variable education, which creates flexibility for learning without compromising rigor or the expected performance standards for students and trainees [108]. Sustaining these innovations beyond the pandemic will require collaboration across health professions schools, professional societies, and policymakers. For example, scaling competency-based, time-variable education will not only necessitate investments in new education models, assessment tools, and faculty development programs, but also require academic institutions as well as licensing, certification, and regulatory bodies to shift their requirements from a time-based orientation (e.g., credit hours, program length) to an achievement-based orientation (e.g., mastery of required skills). Such partnerships will be critical for building on the momentum from COVID-19 to redirect the focus of clinical education away from process and towards outcomes.
BOX 5. Considerations for Addressing Health Disparities.
Develop fair, equitable, and transparent plans for resource allocation and access to testing, treatment, and nursing services. Plans should include adjustments for increasing access to people who are systematically disadvantaged, disabled, or otherwise vulnerable
All plans should be designed with a systematic inquiry into how racism might be at play in this decision or plan
Health care institutions and leaders should create ongoing methods of surveillance of the impact of their decisions and protocols on different types of professionals and staff and to proactively assess the unintended inequities or consequences that arise from them
Develop standardized protocols regarding participating in treatment decision-making or support by families, surrogates, and health care agents to patients during crisis situations that do not disadvantage certain groups or create barriers that disproportionately add burden to certain professions or roles
Priority actions for transforming education and training are summarized in Box 4.
Developing Policies and Programs to Address Health Disparities
The disparate impact of COVID-19 on marginalized populations is the result of long-standing disparities in population health in the U.S. for people made vulnerable by racism, socioeconomic disparities, geography, disability, and bias. Beyond the distressing gaps in access to affordable health care and the environmental challenges contributing to poorer health outcomes for marginalized populations, the pandemic has also demonstrated how inequities are embedded in various processes in health care (e.g., recruitment for clinical trials, guidelines for the allocation of medical products) [111,112].
Addressing health disparities will require a systems approach inclusive of all sectors of the health system. But as direct providers of care to patients in need, clinicians will play an important role at combating inequities on the frontlines. At the level of care delivery, clinicians and professional societies will need to use the lens of equity to address implicit biases within clinical practice (e.g., the use of race when estimating kidney function) [113,114]. Clinicians will need to also review guidelines for public health emergencies to ensure that such protocols do not disadvantage certain groups.
Of course, meaningful progress to redress the disparities in American health care will require embedding equity and the ethos of justice in all aspects of clinical training, practice, and operations, rather than treating issues of representation and racial bias in isolation. Indeed, each of the priority actions listed above in Box 1 through Box 4 can and should be centered around the principles of equity, whether it is a priority action to address clinician well-being (e.g., recognizing the association between racial bias and burnout) or a policy consideration for improving equity in clinician education (e.g., the chronic underrepresentation of communities of color in clinical practice) [115].
Priority actions for addressing health disparities are summarized in Box 5.
Conclusion
This discussion paper has sought to highlight the challenges and lessons for clinicians and professional societies during the COVID-19 pandemic. While this paper has focused primarily on the experience of physicians and nurses, which represent two of the largest segments of the health professions workforce, it is important to acknowledge the tremendous contributions of all health care workers, including a range of allied health professions who provide care in diverse clinical settings encompassing community clinics, long-term care facilities, and hospitals. The clinician sector has played a leading role during each stage of the response to CO-VID-19, from detecting and caring for the first infected patients at the beginning of the outbreak, to adapting care models to meet the needs of both COVID-19 and non-COVID-19 patients as the pandemic progressed, to more recently supporting vaccination campaigns by administering shots and organizing to address vaccine hesitancy. Beyond care delivery, clinicians also worked to navigate uncertain clinical environments and an evolving evidence base to develop clinical guidelines for COVID-19. Furthermore, clinicians have served as trusted messengers and voices for change throughout the pandemic, organizing at the national and grassroots levels to highlight the role of structural racism in pandemic disparities and advocate for improving the equity of both the pandemic response and the health care system writ large.
Yet the diverse contributions of clinicians during the pandemic—layered on top of their first and foremost responsibility of delivering empathetic and effective patient care—have taken their toll. Emerging evidence unequivocally indicates the tremendous physical, mental, emotional, and moral burden imposed by a prolonged public health emergency on the clinician workforce. Pandemic-era stressors spanning dangers to clinicians’ personal safety, to isolation from personal and professional support networks, to the persistent burden of working in understaffed and over-booked care delivery settings, to the role of structural racism in contributing to stark inequities in pandemic outcomes, have all exacerbated pre-pandemic trends of rising burnout, moral distress and deteriorating clinician well-being. COVID-19 has also exposed existing challenges for the clinician sector, from the instability of fee-for-service reimbursement to the gaps in clinical capacity for specific specialties (e.g., critical care) and populations (e.g., rural, safety net), to the inequities embedded into health professions training and clinical care. It has also illuminated the prevalence of moral injury associated with clinical care during the pandemic.
Although the pandemic remains ongoing at the time of this paper’s publication, the experiences of clinicians to date offer valuable insights for policymakers as the country works to navigate the next phase of the pandemic and future emergency preparedness. For example, a key lesson from the pandemic is how building a robust health care system capable of meeting both population health needs and emergency situations is predicated on a sufficiently resourced clinician workforce. In this discussion paper, leaders from the clinician sector have sought to review the experience to date of clinicians and present the priority actions for guiding COVID-19 response and recovery. Considerations for policymakers include investing in clinician well-being, advancing innovations in clinician practice, promoting financial resilience for clinicians, transforming education and training, and developing policies and programs to address health disparities. A resilient health care system begins with a resilient health care workforce, and by addressing the systemic challenges exposed and exacerbated by the pandemic, policymakers can support and revitalize the clinician workforce to meet the health and care needs of patients and communities across America for COVID-19 and beyond.
Funding Statement
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies.
Footnotes
Conflict-of-Interest Disclosures: Michelle Gong reports receiving grants from NIH, CDC, and AHRQ unrelated to this work, and receiving personal fees from Regeneron and Phillips Healthcare. Jack Resneck reports that he is a trustee of the American Medical Association and a director at the National Quality Forum. Tait Shanafelt reports that he is co-inventor of the Well-being Index Instruments and the Participatory Management Leadership Index. Mayo Clinic holds the copyright for these instruments and has licensed them for use outside of the Mayo Clinic, and Mayo Clinic pays Dr. Shanafelt a portion of any royalties received.
Contributor Information
James Madara, American Medical Association.
Suzanne Miyamoto, American Academy of Nursing.
Jason E. Farley, Johns Hopkins University School of Nursing and Johns Hopkins University School of Medicine.
Michelle Gong, Montefiore Medical Center and Albert Einstein College of Medicine.
Millicent Gorham, National Black Nurses Association, Inc..
Holly Humphrey, Josiah Macy Jr. Foundation.
Mira Irons, American Medical Association.
Ateev Mehrotra, Harvard Medical School and Beth Israel Deaconess Medical Center.
Jack Resneck, Jr., University of California San Francisco.
Cynda Rushton, Johns Hopkins School of Medicine, Berman Institute of Bioethics and School of Nursing.
Tait Shanafelt, Stanford Medicine and Stanford University.
Acknowledgments
This paper benefited from the thoughtful input of George Thibault, Harvard Medical School; Bernadette Melnyk, The Ohio State University; and Leon McDougle, The Ohio State University Wexner Medical Center.
Jennifer Lee and Kushal Kadakia from the National Academy of Medicine, Arjun Venktatesh from Yale University School of Medicine, Shannon K. McDevitt from the Health Resources and Services Administration, and Howard Bauchner provided valuable support to the development of this paper.
References
- 1.Salsberg E, Martiniano R. Health Affairs Blog. 2018. Health Care Jobs Projected To Continue To Grow Far Faster Than Jobs In The General Economy. [DOI] [Google Scholar]
- 2.American Association of Colleges of Nursing. Nursing Fact Sheet. 2019. [November 30, 2020]. https://www.aacnnursing.org/news-Information/fact-sheets/nursing-fact-sheet. [Google Scholar]
- 3.Kaiser Family Foundation. Primary Care Health Professional Shortage Areas. 2020. [November 30, 2020]. https://www.kff.org/other/state-indicator/primary-care-health-professional-shortage-areas-hpsas/?currentTimeframe=0&sortModel=%7B%22colId% 22:%22Location%22,%22sort%22:%22asc%22%7D. [Google Scholar]
- 4.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, Mata DA. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018;320:11:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press; 2019. [DOI] [PubMed] [Google Scholar]
- 6.National Academies of Sciences, Engineering, and Medicine. Rapid Expert Consultation on Understanding Causes of Health Care Worker Deaths Due to the COVID-19 Pandemic. Washington, DC: The National Academies Press; 2020. [December 10, 2020]. [DOI] [Google Scholar]
- 7.Kaiser Health News. Lost on the Frontline: Explore the Database. 2020. [November 30, 2020]. https://khn.org/news/lost-on-the-frontline-explore-the-database/ [Google Scholar]
- 8.Rossi R, Socci V, Pacitti F, Lorenzo G, Di Marco A, Siracusano A, Rossi A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Network Open. 2020;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Academy of Medicine. Action Collaborative on Clinician Well-Being and Resilience. 2021. [January 5, 2021]. https://nam.edu/initiatives/clinicianresilience-and-well-being/ [Google Scholar]
- 10.Poston JT, Patel BK, Davis AM. Management of Critically Ill Adults With COVID-19. JAMA. 2020;323:18:1839–1841. doi: 10.1001/jama.2020.4914. [DOI] [PubMed] [Google Scholar]
- 11.Infectious Diseases Society of America. Guidelines on the Treatment and Management of Patients with COVID-19. 2020. [November 30, 2020]. https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/#toc-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Surviving Sepsis Campaign. COVID-19 Guidelines. 2020. [November 30, 2020]. https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/COVID-19. [Google Scholar]
- 13.American Association of Critical Care Nurses. Procedure Manual: COVID-19 Resources. 2020. [December 8, 2020]. https://www.aacn.org/clinical-resources/covid-19/procedure-manual-covid-19-resources. [Google Scholar]
- 14.American Association of Critical Care Nurses. COVID-19 Micro-Credential Among First for Clinical Care. 2020. [December 8, 2020]. https://www.aacn.org/newsroom/covid-19-micro-credential-among-first-for-clinical-care. [Google Scholar]
- 15.Dominus S. New York Times. 2020. Aug 5, [November 30, 2020]. The Covid Drug Wars That Pitted Doctor vs. Doctor. https://www.nytimes.com/2020/08/05/magazine/covid-drug-wars-doctors.html. [Google Scholar]
- 16.Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, Brenner SK, Leon-berg-Yoo A, Schenck EJ, Radbel J, Reiser J, Bansal A, Srivastava A, Zhou Y, Sutherland A, Green A, Shehata AM, Goyal N, Vijayan A, Velez JCQ, Shaefi S, Parikh CR, Arunthamakun J, Athavale AM, Friedman AN, Short SAP, Kibbelaar ZA, Omar SA, Admon AJ, Donnelly JP, Gershengorn HB, Hernan MA, Semler MW, Leaf DE. Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US. JAMA Internal Medicine. 2020;180:11:1436–1446. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lynch HF, Bateman-House A, Caplan AL. Health Affairs Blog. 2020. ‘Panic Prescribing’ Untested Coronavirus Treatments: A Danger To Patients Today and Tomorrow. https://doiorg/10.1377/hblog20200330.265604. [Google Scholar]
- 18.American Medical Association. Joint Statement on Ordering, Prescribing or Dispensing CO-VID-19 Medications. 2020. [November 30, 2020]. https://www.ama-assn.org/delivering-care/public-health/joint-statement-ordering-prescribing-or-dispensing-covid-19. [Google Scholar]
- 19.Centers for Medicare & Medicaid Services. Trump Administration Champions Reporting of CO-VID-19 Clinical Trial Data through Quality Payment Program, Announces New Clinical Trials Improvement Activity. 2020. [November 30, 2020]. https://www.cms.gov/newsroom/press-releases/trump-administration-champions-reporting-covid-19-clinical-trial-data-through-quality-payment. [Google Scholar]
- 20.Spetz J. Health Affairs Blog. 2020. There Are Not Nearly Enough Nurses To Handle The Surge Of Coronavirus Patients: Here’s How To Close the Gap Quickly. [DOI] [Google Scholar]
- 21.Halpern NA, Pasores SM, Oropello JM, Kvetan V. Critical Care Medicine in the United States: Addressing the Intensivist Shortage and Image of the Specialty. Critical Care Medicine. 2013;41(12):2754–2761. doi: 10.1097/CCM.0b013e318298a6fb. [DOI] [PubMed] [Google Scholar]
- 22.Keeley C, Jimenez J, Jackson H, Boudourakis L, Salway RJ, Cineas N, Villaneuva Y, Bell D, Wallach AB, Schwartz DB, Mendez-Justiniano I, Long TG. Staffing Up For The Surge: Expanding The New York City Public Hospital Workforce During The COVID-19 Pandemic. Health Affairs. 2020;39(8):1426–1430. doi: 10.1377/hlthaff.2020.00904. [DOI] [PubMed] [Google Scholar]
- 23.American Medical Association. COVID-19 Volunteer Guide for Health Care Professionals. 2020. [November 30, 2020]. https://www.ama-assn.org/delivering-care/public-health/covid-19-volunteer-guide-healthcare-professionals. [Google Scholar]
- 24.Barnett ML. Washington Post. 2020. Apr 8, [November 30, 2020]. A Second, Hidden Pandemic Will Follow COVID-19. We Need to Be Ready For It. https://www.washingtonpost.com/opinions/2020/04/08/covid-19-pandemic-will-end-americas-next-health-crisis-is-already-starting/?arc404=true. [Google Scholar]
- 25.Centers for Medicare and Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. 2020. [November 30, 2020]. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. [Google Scholar]
- 26.U.S. Food and Drug Administration. Enforcement Policy for Non-Invasive Remote Monitoring Devices Used to Support Patient Monitoring During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency. 2020. [November 30, 2020]. https://www.fda.gov/media/136290/download. [Google Scholar]
- 27.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and Content of Primary Care Office-Based vs Telemedicine Care Visits During the COVID-19 Pandemic in the US. JAMA Network Open. 2020;3(10):e2021476. doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D, Schneider EC. The Impact of the COVID-19 Pandemic on Outpatient Care: Visits Return to Prepandemic Levels, but Not for All Providers and Patients. 2020. [November 30, 2020]. https://www.commonwealthfund.org/publications/2020/oct/impactcovid-19-pandemic-outpatient-care-visits-return-prepandemic-levels. [Google Scholar]
- 29.Jercich K. 2020. [November 30, 2020]. Most Clinicians Can’t Access Telehealth Directly From EHRs. https://www.healthcareitnews.com/news/most-clinicians-cant-access-telehealth-directly-ehrs. [Google Scholar]
- 30.Whaley CM, Pera MF, Cantor J, Chang J, Velasco J, Hagg HK, Sood N, Bravata DM. Changes in Health Services Use Among Commercially Insured US Populations During the COVID-19 Pandemic. JAMA Network Open. 2020;3(11):e2024984. doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roberts ET, Mehrotra A. Assessment of Disparities in Digital Access Among Medicare Beneficiaries and Implications for Telemedicine. JAMA Internal Medicine. 2020;180(10):1386–1389. doi: 10.1001/jamainternmed.2020.2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Katersky A, Kim SR. From House Calls to Drive-Thru Visits, Independent Physicians Adapt Amid COVID-19 Crisis. 2020. [November 30, 2020]. https://abcnews.go.com/US/house-calls-drive-visits-independent-physicians-adapt-amid/story?id=70131146. [Google Scholar]
- 33.American Association of Colleges of Nursing. Considerations for COVID-19 Preparedness and Response in U.S. Schools of Nursing. 2020. [November 30, 2020]. https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Considerations-for-COVID19-Nursing-Schools.pdf. [Google Scholar]
- 34.American Association of Medical Colleges. Updated Interim Guidance for Medical Students’ Participation in Patient Care During the Coronavirus (CO-VID-19) Outbreak. 2020. [November 30, 2020]. https://www.aamc.org/news-insights/press-releases/updated-interim-guidance-medical-students-participation-patient-care-during-coronavirus-covid-19. [Google Scholar]
- 35.American Red Cross. Academic Service Learning. 2020. [November 30, 2020]. https://www.redcross.org/aboutus/who-we-are/nursing-health/academic-service-learning.html. [Google Scholar]
- 36.Byrnes YM, Civantos AM, Go BC, McWilliams TL, Rajasekaran K. Effect of the COV-ID-19 pandemic on medical student career perceptions: a national survey study. Medical Education Online. 2020;25(1):1–19. doi: 10.1080/10872981.2020.1798088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Commission on Collegiate Nursing Education. Information Regarding Coronavirus Impact on CCNE Accredited Baccalaureate and Graduate Nursing Programs. 2020. [November 30, 2020]. https://www.aacnnursing.org/Portals/42/CCNE/News/CCNE-Statement-on-Coronavirus-Bacc-and-Grad.pdf. [Google Scholar]
- 38.American Association of Colleges of Nursing. Considerations for Reopening U.S. Schools of Nursing During COVID-19. 2020. [January 20, 2021]. https://www.aacnnursing.org/Portals/42/News/AACN-Guidance-Reopening-Schools-COVID-19-July-2020.pdf. [Google Scholar]
- 39.American Association of Colleges of Nursing. AACN Launches New National Campaign to Elevate Academic Nursing’s Role in Administering the COV-ID-19 Vaccine. 2021. [January 20, 2021]. https://www.aacnnursing.org/News-Information/Press-Releases/View/ArticleId/24761/national-campaign-covid-19-vaccine. [Google Scholar]
- 40.Orbey E. The New Yorker. 2020. May 6, [November 30, 2020]. The Medical Students Who Joined the Battle Against the Coronavirus. https://www.newyorker.com/science/medical-dispatch/the-medical-students-who-joined-the-battle-against-the-coronavirus. [Google Scholar]
- 41.Accreditation Council for Graduate Medical Education. ACGME Statement on Early Graduation from US Medical Schools and Early Appointment to the Clinical Learning Environment. 2020. [November 30, 2020]. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10184/ACGME-Statement-on-Early-Graduation-from-US-Medical-Schools-and-Early-Appointment-to-the-Clinical-Learning-Environment. [Google Scholar]
- 42.American Medical Association. AMA Guiding Principles to Protect Learners Responding to CO-VID-19. 2020. [January 5, 2021]. https://www.ama-assn.org/delivering-care/public-health/ama-guiding-principles-protect-learners-responding-covid-19. [Google Scholar]
- 43.Satariano A. The New York Times. 2020. Aug 17, [December 17, 2020]. Coronavirus Doctors Battle Another Scourge: Misinformation. https://www.nytimes.com/2020/08/17/technology/coronavirus-disinformation-doctors.html. [Google Scholar]
- 44.World Health Organization. Managing the COVID-19 Infodemic: Promoting Healthy Behaviours and Mitigating the Harm from Misinformation and Disinformation. 2020. [November 30, 2020]. https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation. [Google Scholar]
- 45.Petri CR, Brenner LN, Calhoun TF, Chivukula RR, Maley JH, Vinarsky V, Dudzinski DM, Hardin CC. The Fast Literature Assessment and Review (FLARE) Initiative. A Collaborative Effort for Timely Literature Appraisal during the Coronavirus Disease Pandemic. ATS Scholar. 2020;1(2):186–193. doi: 10.34197/ats-scholar.2020-0045IN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.American Medical Association. AMA COVID-19 Guides for Health Care Professionals. 2020. [November 30, 2020]. https://www.ama-assn.org/delivering-care/publichealth/ama-covid-19-guides-health-care-professionals. [Google Scholar]
- 47.American Nurses Association. Nurses, Ethics, and the Response to the COVID-19 Pandemic. 2020. [December 8, 2020]. https://www.nursingworld.org/~4981cc/globalassets/covid19/nurses-ethics-and-the-response-to-the-covid-19-pandemic_pdf-1.pdf. [Google Scholar]
- 48.Lunden I. 2020. [November 30, 2020]. Twitter Prioritizes Blue-Check Verifications to Confirm Experts on COVID-19 and the Novel Coronavirus. https://techcrunchcom/2020/03/21/twitter-prioritizes-blue-check-verifications-to-confirm-experts-on-covid-19-and-the-novel-coronavirus/ [Google Scholar]
- 49.Carville O, Court E, Brown KV. Bloomberg. 2020. Mar 31, [December 17, 2020]. Hospitals Tell Doctors They’ll Be Fired If They Speak Out About Lack of Gear. https://www.bloomberg.com/news/articles/2020-03-31/hospitals-tell-doctors-they-ll-be-fired-if-they-talk-to-press. [Google Scholar]
- 50.Roborgh S, Fast L. Healthcare Workers Are Still Coming Under Attack During The Coronavirus Pandemic. 2020. [December 17, 2020]. https://theconversation.com/healthcare-workers-are-still-coming-under-attack-during-the-coronavirus-pandemic-136573. [Google Scholar]
- 51.Glasser SB. The New Yorker. 2020. Apr 8, [November 30, 2020]. How Did the U.S. End Up with Nurses Wearing Garbage Bags? https://www.newyorker.com/news/letter-from-trumps-washington/the-corona-virus-and-how-the-united-states-ended-up-with-nurses-wearing-garbage-bags. [Google Scholar]
- 52.He S, Ojo A, Beckman AL, Gondi S, Betz M, Faust JS, Choo E, Kass D, Raja AS. The Story of #GetMePPE and GetUsPPE.org to Mobilize Health Care Response to COVID-19: Rapidly Deploying Digital Tools for Better Health Care. Journal of Medical Internet Research. 2020;22(7):e20469. doi: 10.2196/20469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.American Medical Association. New AMA Policy Recognizes Racism as a Public Health Threat. 2020. [November 30, 2020]. https://www.ama-assn.org/press-center/press-releases/new-ama-policy-recognizes-racism-public-health-threat. [Google Scholar]
- 54.American Academy of Nursing. Racism Affects Health and Wellness and It Must Be Addressed. 2020. [December 8, 2020]. https://www.aannet.org/news/pressreleases/position-statement-on-racism. [Google Scholar]
- 55.American Nurses Association. ANA’s Membership Assembly Adopts Resolution on Racial Justice for Communities of Color. 2020. [December 8, 2020]. https://www.nursingworld.org/news/news-releases/2020/ana-calls-for-racial-justice-for-communities-of-color/ [Google Scholar]
- 56.Van Mol MMC, Kompanje EJO, Benoit DD, Bakker J, Nijkamp MD. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. PLoS One. 2015;31(10):e0136955. doi: 10.1371/journal.pone.0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.West CP, Dyrbye LN, Shanafelt TD. Physician Burnout: Contributors, Consequences and Solutions. Journal of Internal Medicine. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 58.Shanafelt TD, West CP, Sinsky C, Rock-el MT, Tutty M, Satele DV, Carlasare LE, Dyrbye LN. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clinic Proceedings. 2019;94(9):1681–1694. doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 59.McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ Widespread Job Dissatisfaction, Burnout, and Frustration with Health Benefits Signal Problems for Patient Care. Health Affairs. 2011;30(2):202–210. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dyrbye LN, West CP, Johnson PO, Cipriano PF, Beatty DE, Peterson C, Major-Elechi B, Shanafelt T. Burnout and Satisfaction With Work-Life Integration Among Nurses. Journal of Occupational and Environmental Medicine. 2019;61(8):689–698. doi: 10.1097/JOM.0000000000001637. [DOI] [PubMed] [Google Scholar]
- 61.Dodek PM, Wong H, Norena M, Ayas N, Reynolds SC, Keenan SP, Hamric A, Rodney P, Stewart M, Alden L. Moral Distress in Intensive Care Unit Professionals is Associated with Profession, Age, and Years of Experience. Journal of Critical Care. 2016;31(1):178–182. doi: 10.1016/j.jcrc.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 62.Epstein EG, Whitehead PB, Prompahakul C, Thacker LR, Hamric AB. Enhancing Understanding of Moral Distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empirical Bioethics. 2019;10(2):113–124. doi: 10.1080/23294515.2019.1586008. [DOI] [PubMed] [Google Scholar]
- 63.Carse A, Rushton CH. Harnessing the Promise of Moral Distress: A Call for Re-Orientation. [January 28, 2021];Journal of Clinical Ethics. 2017 28(1):15–29. https://pubmed.ncbi.nlm.nih.gov/28436924/ [PubMed] [Google Scholar]
- 64.Dyrbye LN, West CP, Halasy M, O’Laughlin DJ, Satele D, Shanafelt T. Burnout and Satisfaction with Work-Life Integration Among PAs Relative to Other Workers. JAAPA. 2020;33(5):35–44. doi: 10.1097/01.JAA.0000660156.17502.e6. [DOI] [PubMed] [Google Scholar]
- 65.West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, Shanafelt TD. Association of Perceived Medical Errors with Resident Distress and Empathy: A Prospective Longitudinal Study. JAMA. 2006;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 66.Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, Sloan JA, Swensen SJ, Buskirk SJ. Longitudinal Study Evaluating the Association Between Physician Burnout and Changes in Professional Work Effort. Mayo Clinic Proceedings. 2016;91(4):422–431. doi: 10.1016/j.mayocp.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 67.Dyrbye LN, Shanafelt TD, Johnson PO, Johnson L, Satele D, West CP. A Cross-Sectional Study Exploring the Relationship Between Burnout, Absenteeism, and Job Performance Among American Nurses. BMC Nursing. 2019;18:57. doi: 10.1186/s12912-019-0382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shanafelt T, Ripp J, Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the CO-VID-19 Pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 69.Shay J. Moral Injury. Psychoanalytic Psychology. 2014;31(2):182–191. doi: 10.1037/a0036090. [DOI] [Google Scholar]
- 70.Dean W, Talbot S, Caplan A. Clarifying the Language of Clinician Distress. JAMA. 2020;323(10):923–924. doi: 10.1001/jama.2019.21576. [DOI] [PubMed] [Google Scholar]
- 71.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. https://doi.org/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Steichmiller JK. The Nursing Shortage in Acute and Critical Care Settings. AACN Clinical Issues. 2002;13(4):577–584. doi: 10.1097/00044067200211000-00011. [DOI] [PubMed] [Google Scholar]
- 73.Cecile M, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, Chevret S, Schlemmer B, Azoulay E. Burnout Syndrome in Critical Care Nursing Staff. American Journal of Respiratory and Critical Care Medicine. 2006;175(7):698–704. doi: 10.1164/rccm.200606-806OC. https:// doi.org/10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 74.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 75.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, Satlin MJ, Campion TR, Nahid M, Ringel JB, Hoffman KL, Alshak MN, Li HA, Wehmeyer GT, Rajan M, Reshetnyak E, Hubert N, Horn EM, Martinez FJ, Gulick RM, Safford MM. Clinical Characteristics of Covid-19 in New York City. New England Journal of Medicine. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Keene AB, Shiloh AL, Eisen L, Berger J, Karwa M, Fein D, Orsi D, Gong M. Critical Care Surge During the COVID-19 Pandemic: Implementation and Feedback From Frontline Providers. Journal of Intensive Care Medicine. 2021;36(2):233–240. doi: 10.1177/0885066620973175. [DOI] [PubMed] [Google Scholar]
- 78.Accreditation Council for Graduate Medical Education. ACGME Resident/Fellow Education and Training Considerations Related to Coronavirus (COVID-19) 2020. [December 19, 2020]. https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10085/ACGME-Resident-Fellow-Education-and-Training-Considerations-related-to-Coronavirus-COVID-19. [Google Scholar]
- 79.Biala D, Siegel EJ, Silver L, Schindel B, Smith KM. Deployed: Pediatric Residents Caring for Adults During COVID-19’s First Wave in New York City. Journal of Hospital Medicine. 2020;15(12):763–764. doi: 10.12788/jhm.3527. [DOI] [PubMed] [Google Scholar]
- 80.Wade C. AcademicMedicine. 2020. Physician-Scientists in the Era of CO-VID-19: Gone But Not Forgotten. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Spector ND, Overholser B. CO-VID-19 and the Slide Backward for Women in Academic Medicine. JAMA Network Open. 2020;3(9):e2021061. doi: 10.1001/jamanet-workopen.2020.21061. [DOI] [PubMed] [Google Scholar]
- 82.Gewin V. The Career Cost of COVID-19 to Female Researchers, and How Science Should Respond. 2020. [December 19, 2020]. https://www.nature.com/articles/d41586-020-02183-x. [DOI] [PubMed] [Google Scholar]
- 83.Pickler RH. Back to Science. Nursing Research. 2020;69(4):251. doi: 10.1097/NNR.0000000000000439. [DOI] [PubMed] [Google Scholar]
- 84.Asch DA, Grischkan J, Nicholson S. The Cost, Price, and Debt of Medical Education. New England Journal of Medicine. 2020;383:6–9. doi: 10.1056/NEJMp1916528. [DOI] [PubMed] [Google Scholar]
- 85.Anderson G. The Emotional Toll of Racism. 2020. [November 30, 2020]. https://www.insidehighered.com/news/2020/10/23/racism-fuels-poor-mental-health-outcomes-black-students. [Google Scholar]
- 86.Jumreornvong O, Yang E, Race J, Appel J. Academic Medicine. 2020. Telemedicine and Medical Education in the Age of COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Deville C, Hwang W, Burgos R, Chapman CH, Both S, Thomas CR. Diversity in Graduate Medical Education in the United States by Race, Ethnicity, and Sex, 2012. JAMA Internal Medicine. 2015;175(10):1706–1708. doi: 10.1001/jamainternmed.2015.4324. [DOI] [PubMed] [Google Scholar]
- 88.Alsan M, Garrick O, Graziani GC. Does Diversity Matter for Health? Experimental Evidence from Oakland. 2019. [January 5, 2021]. https://www.nber.org/system/files/working_papers/w24787/w24787.pdf. [Google Scholar]
- 89.Gallegos A. AAMC Report Shows Decline of Black Males in Medicine. 2016. [December 7, 2020]. https://www.aamc.org/news-insights/aamc-report-shows-decline-black-males-medicine. [Google Scholar]
- 90.American Association of Colleges of Nursing. Race/Ethnicity of Students Enrolled from Generic (Entry-Level) Baccalaureate, RN-to-Baccalaureate, Total Baccalaureate, Master’s, Research-Focused Doctoral, and DNP Programs in Nursing, 2010-2019. 2020. [January 20, 2021]. https://www.aacnnursing.org/Portals/42/News/Surveys-Data/EthnicityTbl.pdf. [Google Scholar]
- 91.Yousif H, Ayogu N, Bell T. The Path Forward — An Antiracist Approach to Academic Medicine. New England Journal of Medicine. 2020;383:e91. doi: 10.1056/NEJMpv2024535. [DOI] [PubMed] [Google Scholar]
- 92.American Medical Association. COVID-19 Physician Practice Financial Impact Survey Results. 2020. [November 30, 2020]. https://www.ama-assn.org/practicemanagement/sustainability/covid-19-physician-practice-financial-impact-survey-results. [Google Scholar]
- 93.American Nursing Association. Pulse on the Nation’s Nurses COVID-19 Survey Series: Financial. 2020. [December 7, 2020]. https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/financial-impact-survey/ [Google Scholar]
- 94.Primary Care Collaborative. Primary Care & COVID-19: Week 21 Survey. 2020. [November 30, 2020]. https://www.pcpcc.org/2020/10/01/primary-care-covid-19-week-21-survey. [Google Scholar]
- 95.Primary Care Collaborative. Primary Care & COVID-19: Week 24 Survey. 2021. [January 18, 2021]. https://www.pcpcc.org/2020/12/17/primary-care-covid-19-round-24-survey. [Google Scholar]
- 96.Primary Care Collaborative. Primary Care & COVID-19: Round 23 Survey. 2020. [November 30, 2020]. https://www.pcpcc.org/2020/11/23/primary-care-covid-19-round-23-survey. [Google Scholar]
- 97.American Medical Association. COVID-19 CPT Coding and Guidance. 2020. [November 30, 2020]. https://www.ama-assn.org/practice-management/cpt/covid-19-cpt-coding-and-guidance. [Google Scholar]
- 98.Gaines ME, Auleta AD, Berwick DM. Changing the Game of Prior Authorization. JAMA. 2020;323(8):705–706. doi: 10.1001/jama.2020.0070. [DOI] [PubMed] [Google Scholar]
- 99.American Medical Association. 2019 AMA Pri- or Authorization (PA) Physician Survey. 2020. [November 30, 2020]. https://www.ama-assn.org/system/files/2020-06/prior-authorization-survey-2019.pdf. [Google Scholar]
- 100.Sinsky C, Linzer M. Practice And Policy Reset Post-COVID-19: Reversion, Transition, Or Transformation? Health Affairs. 2020;39(8):1405–1411. doi: 10.1377/hlthaff.2020.00612. [DOI] [PubMed] [Google Scholar]
- 101.American Medical Association. Reducing Barriers to Physician-Focused Payment Models. 2017. [November 30, 2020]. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/about-ama/councils/Council%20Reports/council-on-medicalservice/issue-brief-reducing-barriers-physician-focused-payment-models.pdf. [Google Scholar]
- 102.Micklos J. Health Affairs Blog. 2018. Rethinking The Physician-Focused Payment Model Technical Advisory Committee. [DOI] [Google Scholar]
- 103.American Medical Association. Consensus Statement on Improving the Prior Authorization Process. 2018. [November 30, 2020]. https://edhub.ama-assn.org/data/Multimedia/10.1001ama.2018.0080supp1.pdf. [Google Scholar]
- 104.Coleman T. Anti-Racism in Nursing Education: Recommendations for Racial Justice Praxis. Journal of Nursing Education. 2020;59(11):642–645. doi: 10.3928/01484834-20201020-08. [DOI] [PubMed] [Google Scholar]
- 105.Nolen L. Congress: Don’t Eliminate Funding for the Diversity Creating Health Career Opportunity Program. 2019. [November 30, 2020]. https://www.statnews.com/2019/12/12/congress-dont-stop-funding-health-career-opportunity-program/ [Google Scholar]
- 106.Centers for Medicare and Medicaid Services. Graduate Nurse Education Demonstration. 2020. [November 30, 2020]. https://innovation.cms.gov/innovation-models/gne. [Google Scholar]
- 107.Heisler E. The National Health Service Corps. 2018. [November 30, 2020]. https://fas.org/sgp/crs/misc/R44970.pdf. [Google Scholar]
- 108.Lucey CR, Johnston SC. The Transformational Effects of COVID-19 on Medical Education. JAMA. 2020;324(11):1033–1034. doi: 10.1001/jama.2020.14136. [DOI] [PubMed] [Google Scholar]
- 109.Josiah Macy Jr. Foundation. Conference Recommendations: Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments. 2020. [December 7, 2020]. https://macyfoundation.org/assets/reports/publications/jmf_2020_confsummary_fin.pdf. [Google Scholar]
- 110.Chua IS, Jackson V, Kamdar M. Web-side Manner during the COVID-19 Pandemic: Maintaining Human Connection during Virtual Visits. Journal of Palliative Medicine. 2020;23(11) doi: 10.1089/jpm.2020.0298. [DOI] [PubMed] [Google Scholar]
- 111.Schmidt H. The New York Times. 2020. Apr 15, [November 30, 2020]. The Way We Ration Ventilators is Biased. https://www.nytimes.com/2020/04/15/opinion/covid-ventilator-rationing-blacks.html. [Google Scholar]
- 112.Chastain DB, Osae SP, Henao-Martinez AF, Franco-Paredes C, Chastain JS, Young HN. Racial Disproportionality in Covid Clinical Trials. New England Journal of Medicine. 2020;383:e59. doi: 10.1056/NEJMp2021971. [DOI] [PubMed] [Google Scholar]
- 113.Vyas DA, Eisenstein LG, Jones DS. Hidden in Plain Sight — Reconsidering the Use of Race Correction in Clinical Algorithms. New England Journal of Medicine. 2020;383(9):874–882. doi: 10.1056/NEJMms2004740. [DOI] [PubMed] [Google Scholar]
- 114.Eneanya ND, Yang W, Reese PP. Reconsidering the Consequences of Using Race to Estimate Kidney Function. JAMA. 2019;322(2):113–114. doi: 10.1001/jama.2019.5774. [DOI] [PubMed] [Google Scholar]
- 115.Dyrbye L, Herrin J, West CP, Wittlin NM, Dovidio JF, Hardeman R, Burke SE, Phelan S, Onyeador IN, Cunningham B, van Ryn M. Association of Racial Bias With Burnout Among Resident Physicians. JAMA Network Open. 2019;2(7):e197457. doi: 10.1001/jamanetworkopen.2019.7457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.American Medical Association, American Nurses Association, and American Pharmacists Association. Open Letter to America’s Health Care Professionals. 2021. Mar 2, [April 22, 2021]. https://searchlf.ama-assn.org/letter/documentDownload?uri=%2Funstructured%2Fbinary%2Fletter%2FLETTERS%2Frace-ethnicity-open-letter.pdf. [Google Scholar]
- 117.American Medical Association. AMA warns against racism, xenophobia amid COVID-19. 2020. May 4, [April 22, 2021]. https://www.ama-assn.org/presscenter/press-releases/ama-warns-against-racism-xenophobia-amid-covid-19. [Google Scholar]
- 118.Smith TM. AMA Population Care. 2020. Jul 28, [April 22, 2021]. 2020: Teachable moment in fight against anti-Asian, anti-Black racism. https://www.ama-assn.org/delivering-care/populationcare/2020-teachable-moment-fight-against-antiasian-anti-black-racism. [Google Scholar]
- 119.American Academy of Nursing. Anti-Asian Discrimination is a Public Health Crisis. 2021. Mar 4, [April 22, 2021]. https://www.aannet.org/news/pressreleases/position-statement-anti-asian-discrimination. [Google Scholar]
- 120.Boodman E. STAT. 2021. Jan 22, [April 22, 2021]. With painstaking effort, Black doctors’ group takes aim at Covid-19 vaccine hesitancy. https://www.statnews.com/2021/01/22/for-black-doctors-com-batting-covid-19-vaccine-hesitancy-starts-with-listening/ [Google Scholar]
- 121.Black Coalition Against COVID-19. Home. [April 22, 2021]. n.d. https://blackcoalitionagainstcovid.org/makingitplain/ [Google Scholar]
- 122.Bodenheimer T, Sinsky C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Annals of Family Medicine. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rushton CH, Turner K, Brock RN, Braxton JM. Invisible Moral Wounds of the CO-VID-19 Pandemic: Are We Experiencing Moral Injury? AACN Advanced Critical Care. 2021;32(1):119–125. doi: 10.4037/aacnacc2021686. [DOI] [PubMed] [Google Scholar]
- 124.Dzau VJ. Los Angeles Times. 2021. Mar 5, [April 23, 2021]. We need a national strategy to help health workers recover from the stress of the pandemic. https://www.latimes.com/opinion/story/2021-03-05/national-strategy-healthcare-workers-mental-health. [Google Scholar]
- 125.United States Census. QuickFacts. [April 23, 2021]. n.d. https://www.census.gov/quickfacts/fact/table/US/PST045219. [Google Scholar]
- 126.Shanafelt T, Trockel M, Rodriguez A, Logan D. Wellness-Centered Leadership: Equipping Health Care Leaders to Cultivate Physician Well-Being and Professional Fulfillment. Academic Medicine. 2021;96(5):641–651. doi: 10.1097/ACM.0000000000003907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shanafelt TD, Noseworthy JH. Executive Leadership and Physician Well-Being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clinic Proceedings. 2016;92(1):129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 128.American Nurses Foundation. Year One COVID-19 Impact Assessment Survey. 2020. [April 23, 2021]. https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/year-one-covid-19-impact-assessment-survey/ [Google Scholar]
- 129.Ulrich C, Rushton C, Grady C. Nursing Outlook. 2020. Nurses confronting the coronavirus: Challenges met and lessons learned to date. [DOI] [PMC free article] [PubMed] [Google Scholar]


