Abstract
Background
Social networking platforms offer a wide reach for public health interventions allowing communication with broad audiences using tools that are generally free and straightforward to use and may be combined with other components, such as public health policies. We define interactive social media as activities, practices, or behaviours among communities of people who have gathered online to interactively share information, knowledge, and opinions.
Objectives
We aimed to assess the effectiveness of interactive social media interventions, in which adults are able to communicate directly with each other, on changing health behaviours, body functions, psychological health, well‐being, and adverse effects.
Our secondary objective was to assess the effects of these interventions on the health of populations who experience health inequity as defined by PROGRESS‐Plus. We assessed whether there is evidence about PROGRESS‐Plus populations being included in studies and whether results are analysed across any of these characteristics.
Search methods
We searched CENTRAL, CINAHL, Embase, MEDLINE (including trial registries) and PsycINFO. We used Google, Web of Science, and relevant web sites to identify additional studies and searched reference lists of included studies. We searched for published and unpublished studies from 2001 until June 1, 2020. We did not limit results by language.
Selection criteria
We included randomised controlled trials (RCTs), controlled before‐and‐after (CBAs) and interrupted time series studies (ITSs). We included studies in which the intervention website, app, or social media platform described a goal of changing a health behaviour, or included a behaviour change technique. The social media intervention had to be delivered to adults via a commonly‐used social media platform or one that mimicked a commonly‐used platform. We included studies comparing an interactive social media intervention alone or as a component of a multi‐component intervention with either a non‐interactive social media control or an active but less‐interactive social media comparator (e.g. a moderated versus an unmoderated discussion group).
Our main outcomes were health behaviours (e.g. physical activity), body function outcomes (e.g. blood glucose), psychological health outcomes (e.g. depression), well‐being, and adverse events. Our secondary outcomes were process outcomes important for behaviour change and included knowledge, attitudes, intention and motivation, perceived susceptibility, self‐efficacy, and social support.
Data collection and analysis
We used a pre‐tested data extraction form and collected data independently, in duplicate. Because we aimed to assess broad outcomes, we extracted only one outcome per main and secondary outcome categories prioritised by those that were the primary outcome as reported by the study authors, used in a sample size calculation, and patient‐important.
Main results
We included 88 studies (871,378 participants), of which 84 were RCTs, three were CBAs and one was an ITS. The majority of the studies were conducted in the USA (54%). In total, 86% were conducted in high‐income countries and the remaining 14% in upper middle‐income countries. The most commonly used social media platform was Facebook (39%) with few studies utilising other platforms such as WeChat, Twitter, WhatsApp, and Google Hangouts. Many studies (48%) used web‐based communities or apps that mimic functions of these well‐known social media platforms.
We compared studies assessing interactive social media interventions with non‐interactive social media interventions, which included paper‐based or in‐person interventions or no intervention. We only reported the RCT results in our 'Summary of findings' table. We found a range of effects on health behaviours, such as breastfeeding, condom use, diet quality, medication adherence, medical screening and testing, physical activity, tobacco use, and vaccination. For example, these interventions may increase physical activity and medical screening tests but there was little to no effect for other health behaviours, such as improved diet or reduced tobacco use (20,139 participants in 54 RCTs). For body function outcomes, interactive social media interventions may result in small but important positive effects, such as a small but important positive effect on weight loss and a small but important reduction in resting heart rate (4521 participants in 30 RCTs). Interactive social media may improve overall well‐being (standardised mean difference (SMD) 0.46, 95% confidence interval (CI) 0.14 to 0.79, moderate effect, low‐certainty evidence) demonstrated by an increase of 3.77 points on a general well‐being scale (from 1.15 to 6.48 points higher) where scores range from 14 to 70 (3792 participants in 16 studies). We found no difference in effect on psychological outcomes (depression and distress) representing a difference of 0.1 points on a standard scale in which scores range from 0 to 63 points (SMD ‐0.01, 95% CI ‐0.14 to 0.12, low‐certainty evidence, 2070 participants in 12 RCTs).
We also compared studies assessing interactive social media interventions with those with an active but less interactive social media control (11 studies). Four RCTs (1523 participants) that reported on physical activity found an improvement demonstrated by an increase of 28 minutes of moderate‐to‐vigorous physical activity per week (from 10 to 47 minutes more, SMD 0.35, 95% CI 0.12 to 0.59, small effect, very low‐certainty evidence). Two studies found little to no difference in well‐being for those in the intervention and control groups (SMD 0.02, 95% CI ‐0.08 to 0.13, small effect, low‐certainty evidence), demonstrated by a mean change of 0.4 points on a scale with a range of 0 to 100.
Adverse events related to the social media component of the interventions, such as privacy issues, were not reported in any of our included studies.
We were unable to conduct planned subgroup analyses related to health equity as only four studies reported relevant data.
Authors' conclusions
This review combined data for a variety of outcomes and found that social media interventions that aim to increase physical activity may be effective and social media interventions may improve well‐being. While we assessed many other outcomes, there were too few studies to compare or, where there were studies, the evidence was uncertain. None of our included studies reported adverse effects related to the social media component of the intervention. Future studies should assess adverse events related to the interactive social media component and should report on population characteristics to increase our understanding of the potential effect of these interventions on reducing health inequities.
Keywords: Adolescent, Adult, Humans, Young Adult, Behavior Therapy, Behavior Therapy/methods, Bias, Controlled Before-After Studies, Exercise, Fruit, Health Behavior, Health Equity, Heart Rate, Interrupted Time Series Analysis, Randomized Controlled Trials as Topic, Social Media, Social Networking, Treatment Outcome, Vegetables, Weight Loss
Plain language summary
Can programmes on social media help people to improve their health?
Key messages
Programmes on social media (such as Facebook or Twitter) that aim to increase physical activity may help people to become more physically active and may improve people's well‐being.
Future studies are needed to find out if there are any unwanted effects associated with taking part in interactive social media programmes.
What is social media?
Social media are computer‐based technologies that help people to share ideas, thoughts and information by building virtual networks and communities on the Internet; examples include, Facebook, Twitter or WhatsApp. Social media networks are 'interactive': the user communicates directly with a computer, or other device, to share and receive information.
What did we want to find out?
People who use social media can exchange ideas and share updates about their behaviours, such as becoming more active or eating more healthily. We wanted to find out if health programmes using interactive social media could change people's behaviours and improve their health.
What did we do?
We searched for studies that tested the effects of interactive social media programmes on people's health. We were interested in how the programmes might affect people's:
‐ health behaviours (such as smoking, drinking alcohol, breastfeeding, dieting, physical activity; seeking and using health services);
‐ health (such as physical fitness, lung function, asthma episodes);
‐ mental health (such as measures of depression, stress, coping);
‐ well‐being; and
‐ whether people reported any unwanted effects related to interactive social media programmes.
How up to date is this review?
We included evidence published up to 1 June 2020.
What did we find?
We found 88 studies involving 871,378 adults (aged 18 years and older). Most studies (49) took place in the USA; all studies took place in either high‐income countries or upper middle‐income countries. Facebook was the most commonly used social media platform; others included WeChat, Twitter, WhatsApp and Google Hangouts.
In most studies the effects of interactive social media programmes were compared against non‐interactive programmes, including paper‐based or in‐person programmes, or no programme. Ten studies compared two social media programmes against each another; for these studies we chose the more interactive of the two programmes as the 'interactive social media programme'.
What are the main results of our review?
Compared with non‐interactive programmes, social media programmes:
‐ may improve some health behaviours, such as increasing the number of daily steps taken, or taking part in screening tests, but may show little to no effect on other health behaviours, such as better diet or reducing tobacco use (evidence from 54 studies in 20,139 people).
‐ may cause small improvements in health, such as a small increase in amount of weight lost, and a small reduction in resting heart rate (evidence from 30 studies in 4521 people).
‐ may improve people's well‐being (evidence from 16 studies in 3792 people).
‐ may have little to no effect on people's mental health, such as depression (evidence from 12 studies in 2070 people).
No studies reported any unwanted effects related to using social media.
What are the limitations of the evidence?
Overall, our confidence in the evidence is low. Many studies did not report clearly how they were conducted. In most studies, people knew whether they were taking part in an interactive programme, and this may have affected the results of the study. Some of the studies did not report all their results, and there were wide variations in the results of some studies. Further research is likely to increase our confidence in the evidence.
Summary of findings
Summary of findings 1. Summary of findings ‐ Interactive Social Media compared to non‐interactive social media.
| Interactive social media compared with non‐interactive social media for public health | ||||||
|
Patient or population: adults Settings: h‐High and high‐middle income countries Intervention: interactive social media Comparison: non‐interactive social media | ||||||
| Outcomes | Absolute effect (95% CI)1 | Effect estimate (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Health behaviours | Overall, interactive social media interventions may improve health behaviours slightly. These effects varied according to the purpose of the intervention and ranged from, for example, a large increase in the number of daily steps (1377 more steps, from 708 to 2045 more) to little to no difference in diet quality (e.g. increase of 0.35 servings of fruits and vegetables per week (from 1.25 fewer servings to 1.96 more). | 20,139 (54 RCTs) | ⊕⊕⊝⊝ low2 | Health behaviours included: physical activity, diet quality, breastfeeding, calorie intake, condom use, health screening, medication, and vaccination uptake, and tobacco use. Additional details in Table 2 | ||
| Body function | Overall, interactive social media interventions may result in a small improvements in body function outcomes, for example, a small but important effect on weight loss (1.34 more kg (from 0.69 to 2.0 more kg) and a small but important effect on cardiorespiratory heart rate (reduction in resting heart rate by 2.50 beats per minute (from 6.17 beats per minute lower to 1.17 higher). | 4521 (30 RCTs) | ⊕⊝⊝⊝ very low3 | Body function outcomes included weight, blood glucose, blood pressure, BMI, cardiorespiratory fitness, dyspnoea, influenza‐like illness. Additional details in Table 3 | ||
| Well‐being Outcomes ‐ General well‐being and Quality of life | The mean well‐being score was 8.2 in the control group. | The mean well‐being score in the social media group was 3.77 points higher (from 1.15 higher to 6.48 points higher). | SMD 0.46 (0.14 to 0.79) | 3792 (16 studies RCTs) | ⊕⊕⊝⊝ low4 | Interactive social media interventions may improve well‐being scores slightly. Absolute effect calculated using Hutchesson 2018 (Quality of Life, Enjoyment and Satisfaction Questionnaire, scores range from 14‐70, higher scores indicate greater well‐being). Additional details in Table 4 |
| Psychological outcomes ‐ Distress and Depression | The mean depression score in the control group was 8.8. | The mean score in the social media group was 0.1 points lower (from 1.23 lower to 1.06 higher) | SMD ‐0.01 (‐0.14 to 0.12) | 2070 (12 studies) | ⊕⊕⊝⊝ low4 | Interactive social media interventions may have little to no effect on psychological outcomes. Absolute effect calculated using Wan 2017 (Beck Depression Inventory II, scores range from 0‐63, higher scores indicate greater degree of depression). Additional details in Table 4 |
| Adverse events | No adverse events were reported related to interactive social media. | ‐ | ⊕⊝⊝⊝ very low5 | Adverse events that were reported were not related to the social media components of the intervention, e.g. injuries related to physical activity, and no studies reported on online harassment or privacy concerns. | ||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1. Effect sizes were determined using the rule of thumb for SMDs: 0.2 represents a small effect, 0.5 a moderate effect and 0.8 a large effect
2. Downgraded by 2 for unclear risks of bias as well as inconsistency.
3. Downgraded by 3 for high risks of bias, inconsistency, and imprecision.
4. Downgraded by 2 for unclear risks of bias and inconsistency.
5. Downgraded by 3 because no studies reported on this outcome.
1. 'Summary of findings' table: health behaviours.
| Any interactive social media intervention compared with non‐interactive social media on health behaviours (RCTs) | ||||||
|
Patient or population: adults Settings: high and high‐middle income countries Intervention: interactive social media Comparison: non‐interactive social media | ||||||
| Outcomes | Absolute effect (95% CI) | Effect estimate (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Physical activity | Adults in the control group had 3770 steps per day | The mean number of steps per day increased by 74 steps for the intervention group (from 32 to 116 more steps) | SMD 0.28 (0.12 to 0.44) | 6250 (29 RCTs) | ⊕⊕⊝⊝ low1 | Absolute effect calculated using Wan 2017 |
| Diet quality | Adults in the control group consumed an average of 22.7 servings of fruit and vegetables per week. | The participants in the intervention increased their weekly fruit and vegetable intake by 0.35 servings (from 1.25 fewer servings to 1.96 more servings per week. | SMD 0.11 (‐0.25 to 0.47) | 1240 (8 RCTs) | ⊕⊕⊝⊝ low2 | Absolute effect calculated using Bantum 2014 |
| Calorie intake | The mean number of calories was 53.75 lower in the intervention group (from 172.48 lower to 44.97 higher | MD ‐53.75 (‐172.48 to 44.97) | 131 (3 RCTs) | ⊕⊕⊕⊝ moderate3 | ||
| Tobacco use | 12.72% of participants in the control group abstained from smoking. | 12.47% of intervention group participants abstained from smoking (from 9.4 to 16.4%). | RR 0.98, 95% CI 0.74, 1.29) | 2433 (4 RCTs) | ⊕⊕⊕⊝ moderate4 | Absolute effect calculated using Ramo 2015 |
| Condom use | The participants in the control group reporting condom use frequency of 3.28 on a scale of 1 (never) to 5 (always). | The intervention group reported condom use frequency 0.34 higher (from 0.51 fewer to 1.17 more). | SMD 0.22 (‐0.33 to 0.76) | 848 (2 RCTs) |
low5 ⊕⊕⊝⊝ |
Absolute effect calculated using Sun 2017 |
| Health screening, medication, vaccination uptake | The mean uptake was 86.8% for the control group. | The mean uptake in the social media group was 2.08% higher (from 1.32% lower to 5.62% higher). | SMD 0.11 (‐0.07, 0.30) | 3016 (8 RCTs) | ⊕⊕⊕⊝ moderate6 | Absolute effect calculated using Horvath 2013 |
| Adverse events | Not assessed | ‐‐ | 0 (0 studies) | ‐‐ | ||
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1. Downgraded by 1 for high heterogeneity (I2 = 84%) and unclear risk of bias.
2. Downgraded by 2 for high heterogeneity (I2 = 86%) and imprecision.
3. Downgraded by 1 for unclear risk of bias.
4. Downgraded by 1 because of high risk of bias.
5. Downgraded by 2 because of high risk of bias and imprecision.
6. Downgraded by 1 because of unclear risks of bias.
2. 'Summary of findings' table: body functions.
| Any interactive social media intervention compared with non‐interactive social media on body function | |||||
|
Patient or population: adults Settings: high and high‐middle income countries Intervention: interactive social media Comparison: non‐interactive social media | |||||
| Outcomes | Absolute effect (95% Cl) | Effect estimate (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Weight (kg) | Participants receiving the social media intervention lost 1.34 more kg (from 0.69 to 2.0 more kg) than those in the control group. | MD ‐1.34 kg (‐2.0 to ‐0.69) | 1963 (16 RCTs) | ⊕⊕⊝⊝ low1 | |
| BMI | Participants receiving the social media intervention reduced their BMI by 0.51 kg/m2 compared to the control group (from 0.10 to 0.92 kg/m2) more. | MD ‐0.51 (‐0.92 to ‐0.10) | 323 (4 RCTs) | ⊕⊕⊝⊝ low1 | |
| Blood glucose | The mean blood glucose level was 1.74 mmol/L lower (from 0.68 to 2.79 mmol/L lower) for the social media group compared to the control group. | MD ‐1.74 mmol/L (‐2.79 to ‐0.68) | 773 (4 RCTs) | ⊕⊕⊝⊝ low2 | |
| Cardiorespiratory fitness | The cardiorespiratory fitness was 2.50 heart beats per minute lower for the participants in the social media group (from 6.17 beats per minute lower to 1.17 higher) | MD ‐2.5 heart beats per minute (‐6.17 to 1.17) | 89 (1 RCT) | ⊕⊝⊝⊝ very low3 | |
| Insomnia | Insomnia scores for the social media group were 0.90 points lower (from 0.56 to 1.24 points lower) than the control group on an insomnia scale assessing how often a person has had trouble falling or staying asleep on 5‐point Likert scale. | MD ‐0.90 (‐1.24 to ‐0.56) | 303 (1 RCT) | ⊕⊕⊝⊝ low4 | |
| Dyspnoea | Dyspnea scores were 0.20 points lower for participants in the social media group (from 3.10 points lower to 2.7 points higher) on a scale of 0‐4.. | MD ‐0.20 (‐3.1 to 2.70) | 109 (1 RCT) | ⊕⊝⊝⊝ verylow5 | |
| Adverse events | Not assessed | ‐‐‐ | 0 (0 studies) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: Mean Difference; KG: kilogram | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
1. Downgraded by 1 for inconsistency and unclear risk of bias.
2. Downgraded by 1 for inconsistency and high risk of bias.
3. Downgraded by 3 for very serious imprecision and inconsistency
4. Downgraded by 2 for small sample size and unclear risks of bias.
5. Downgraded by 2 for high risks of bias and imprecision.
3. 'Summary of findings' table: well‐being and psychological outcomes.
| Any interactive social media intervention compared with non‐interactive social media on well‐being | ||||||
|
Patient or population: adults Settings: high and high‐middle income countries Intervention:iInteractive social media Comparison: non‐interactive social media | ||||||
| Outcomes | Absolute effect (95% CI) | Effect estimate (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Well‐being outcomes ‐ General well‐being and Quality of life | The mean well‐being score was 8.2 in the control group. | The mean well‐being score in the social media group was 3.77 points higher (from 1.15 lower to 6.48 points higher) where 14 points is the minimum possible score and 70 is the maximum. | SMD 0.46 (0.14 to 0.79) | 3792 (16 RCTs) | ⊕⊕⊝⊝ low1 | Absolute effect calculated using Hutchesson 2018 |
| Psychological outcomes ‐ Distress and Depression | The mean depression score in the control group was 8.8. | The mean score in the social media group was 0.1 points lower (from 1.23 lower to 1.06 higher) on a scale using cut‐offs for which a score of 0–13 is considered minimal depression, 14–19 is mild, 20–28 is moderate, and 29–63 is severe. | SMD ‐0.01 (‐0.14 to 0.12) | 2070 (12 RCTs) | ⊕⊕⊝⊝ low2 | Absolute effect calculated using Wan 2017 |
| Adverse events | Not reported in studies | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; SMD: Standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1. Downgraded by 2 for unclear risks of bias and inconsistency.
2. Downgraded by 2 for unclear risks of bias and inconsistency.
Background
Description of the condition
Social networking platforms present an opportunity to reach large numbers of Internet users quickly with health information. For public health authorities, health promotion agencies, non‐governmental organisations, and others, social media offers an especially attractive opportunity to communicate with target audiences. These tools are generally easy and free to use and may allow organisations to reach various populations, providing they have Internet access, including rural and remote populations. These interventions also allow for tailoring to reach those who may usually be considered hard‐to‐reach. Furthermore, social media allows target audiences for health‐related interventions to share information and comments on topics that are of interest to them. In this way, organisations with relevant and informative health‐related campaigns may reach broader audiences through the social networks of users who follow them.
For the purpose of this review, we have defined social media as "activities, practices, and behaviours among communities of people who gather online to share information, knowledge, and opinions using conversational media…that make it possible to create and easily transmit content in the form of words, pictures, videos, and audios" (Safko 2012). We have outlined the types of interactive social media interventions that are eligible for this review in Table 5.
4. Types of interactive social media interventions.
| Social media format | Included | Excluded |
| Blogs and microblogs (e.g. Twitter) | If the intervention includes multi‐way interaction between users (e.g. Twitter that promotes discussion) | Blogs would almost always be excluded since they usually have limited interaction. One‐way messages and posts or direct contact with a healthcare provider. |
| Content communities (e.g. YouTube, Pinterest) | If the intervention includes multi‐way interaction | One‐way messages and posts or direct contact with a healthcare provider |
| Mobile applications (apps) | Apps that allow for communication and interaction with a group of people | Apps that allow a person to track and monitor their progress (e.g. weight loss, blood sugar, etc.) without a social component or apps used to communicate with a healthcare provider |
| Virtual social networks (e.g. Facebook, Odnoklassniki) | If the intervention includes multi‐way interaction | One‐way messages and posts or direct contact with a healthcare provider |
| Web pages and Wikis | If the web site/Wiki allows for multi‐way interaction | One‐way communication (e.g. education) |
Globally, over 4.5 billion people use the Internet and over 3.8 billion use social media (We Are Social 2020). It is important to note that Internet access and usage vary within and between countries and world regions, as evidenced by the fact that the International Telecommunication Union (ITU) estimates that, as of 2019, total Internet users range from a high of 83% in Europe to a low of 28% in Africa (See Figure 1) (ITU 2019). Additionally, global estimates indicate Internet use among men is higher at 58% compared to only 48% of women (ITU 2019). In countries such as Canada and the USA, income has been shown to be a key source of digital inequality and is not only a significant determinant of Internet access, but also online activity level (Haight 2014). There is a risk that people who experience health inequity may face barriers to the use of social media, such as access, reading literacy and/or electronic health literacy (NCCHPC 2015; Welch 2016). Social media use is lower in low‐ and middle‐income countries. A 2014 survey of 32 emerging and developing nations found that those who read or speak English are more likely to access the Internet and Internet access and smartphone ownership rates were found to be greatest among the well‐educated and 18‐ to 34‐year‐olds (Pew Research Center 2015).
1.
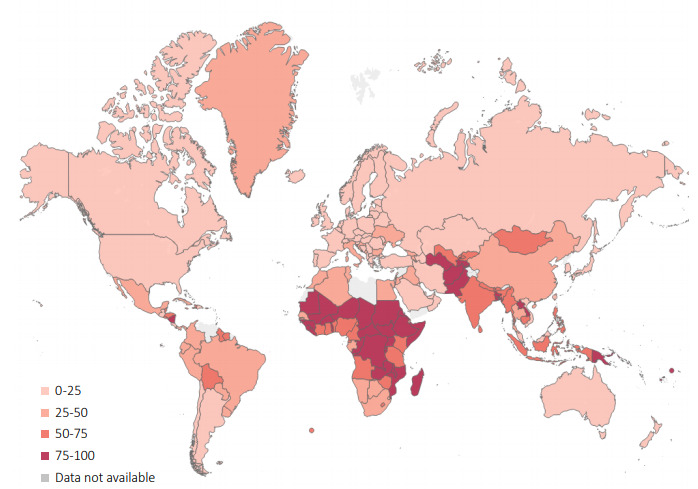
Percentage of the population not using the internet (ITU 2019)
Health inequities are differences in health that are avoidable and unfair (Whitehead 2006). For the purpose of this review, we use the PROGRESS‐Plus framework to consider socially stratifying characteristics that are associated with inequities in health (O'Neill 2014; Welch 2016). Coined by Evans to describe characteristics that may contribute to health inequity, PROGRESS stands for Place of residence, Race/ethnicity/culture/language, Occupation, Gender/sex, Religion, Education, Socioeconomic status, and Social capital (Evans 2003). 'Plus' represents personal characteristics that are associated with discrimination (e.g. age, disability), features of a relationship (e.g. smoking parents, excluded from school), time‐dependant relationships (e.g. leaving the hospital, respite care) and other circumstances that may be related to health inequities (Gough 2012). Social media interventions may inadvertently exacerbate health inequities if those who are most disadvantaged are excluded from participation due to issues such as lack of access or low literacy or electronic health literacy. Reducing health inequities is a major focus of both policy and research organisations from the local to the global level, such as the World Health Organization (WHO).
Social networking sites popular at the time of this review, like Facebook, Instagram, Twitter, WeChat, WhatsApp, and YouTube, as well as related apps, are designed to promote the sharing of information and opinions. Figure 2 maps the most common social media platforms used in different countries around the world. These social networking sites allow information and opinions to be shared in the form of text, images, and video among friends, family, acquaintances, and associates as well as public figures, businesses, and other organisations with whom users associate by 'following' and 'liking' pages or accounts. Health‐specific social media interventions have utilised the most popular features and platforms of social media to provide support for people who share an interest in a particular health concern, such as survivors of cancer. There is evidence that social media use may create a sense of community among people, giving users a feeling of being supported and accepted (Dyson 2015). As noted by Vitak 2014, numerous researchers have found a positive correlation between social media use and social capital, "a construct that encompasses both actual and potential resources available within a given network". Social media may also be used as part of a wider campaign to change cultural norms and behaviours, such as increasing proper hand washing, as seen by the Centers for Disease Control and Prevention's Handwashing: Clean Hands Save Lives campaign (https://www.cdc.gov/handwashing/heroes.html).
2.
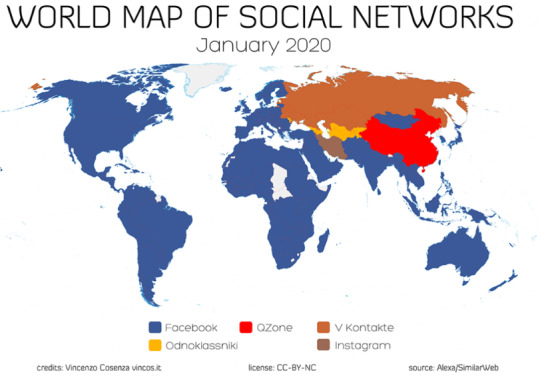
World map of most commonly used social media platforms, 2020
However, with the speed and reach of social media‐based communication come attendant risks that may compromise health, such as the potential for equally rapid diffusion of misinformation or information that is not evidence‐based. For example, the anti‐vaccination Facebook page vactruth.com is 'liked' by almost 125,000 Facebook users and some of its posts are shared hundreds of times, meaning that its content may be seen by many more people than the number of page followers would suggest. Social media may be used to change cultural norms and behaviours in harmful ways, such as the use of social media in campaigns by the alcohol industry in countries such as Australia (Westberg 2016). In addition, the use of social media itself may be associated with adverse outcomes unrelated to the actual intervention or social media platform, such as perceived social isolation, depression and anxiety, and cyberbullying. There are also privacy concerns related to the unsolicited sharing of personal information or images (O'Keeffe 2011; Tromholt 2016; Primack 2017).
Description of the intervention
Health‐related interactive social media interventions for adults use social networking platforms to promote a message that may influence health service uptake, health behaviour change (such as smoking, physical activity, or diet), and health outcomes such as weight loss, depression, or quality of life.
Young 2015 provides an example of a social media‐based intervention aiming to improve a health behaviour among a vulnerable group: uptake of free HIV testing among men who have sex with men. This randomised trial was developed by researchers at the University of California, Los Angeles in partnership with a local community clinic in Lima, Peru to test the efficacy of peer mentorship offered through Facebook. Investigators created non‐public intervention and control Facebook groups. The intervention groups included trained peer leaders who attempted to discuss with other members the importance of HIV prevention and testing. In contrast, the control group had no peer leaders, and participants simply received HIV testing information. Thus, intervention groups were subject to more interactive social media than control groups.
Another example of a social media intervention is described by Maher (Maher 2015). A free, 50‐day team‐based Facebook app called Active Team was developed by a team at the University of South Australia. As part of a randomised controlled trial, insufficiently active adult participants were recruited and allocated to either the intervention group or the control group. In the intervention group, participants were given a pedometer and encouraged to take 10,000 steps per day as part of a team of three to eight existing Facebook friends who the app encourages to engage in friendly rivalry and peer encouragement and support. The app includes a calendar for logging daily step counts, a dashboard showing step‐logging feedback on progress, awards, and gifts, and a team tally board so that users can monitor personal progress and their friends' progress. It also includes a team message board where team members can communicate and receive daily tips for increasing physical activity. Control group members were wait‐listed for the app‐based intervention and followed up with the same measurements as the intervention group.
How the intervention might work
For this review, we focused on 'interactive social media' in which the intervention allows for two‐way communication between peers or the public. This interactive functionality of social media offers a tremendous opportunity for increasing the reach of health interventions and enhancing a person's ability to engage in healthful behaviours. In addition to its potential to facilitate interactions between institutional providers and populations, social media allows lay people to create health‐focused groups to communicate with peers (Ali 2015; Myneni 2016). Furthermore, widespread use of mobile phones and other smart devices coupled with access to high‐speed Internet have considerably increased the ubiquitous functionality of social media while undermining limitations related to geographical locations, times, and social and economic status (Uskov 2015). In addition, because of the penetration of social media globally, people have experience using these interfaces that may allow them to take advantage of their functionality for finding, sharing, and using information.
Interactive social media has the potential to uphold health endeavours in various ways. Recent studies have reported the use of social media in strategies aimed at influencing individual health behaviours, informing health research, supporting health advocacy groups, and promoting health services (Brusse 2014; Seltzer 2015; Rhodes 2016; Sinnenberg 2016; Wong 2016). While the use of social media is common for supporting public health activities, very few organisations have reported consistent strategies describing how public health interventions sustained through social media have helped achieve their health equity goals (Thackeray 2012; Osborne 2013; Chauvin 2016; Ndumbe‐Eyoh 2016).
The logic model, developed by our team for this review, displayed in Figure 3 illustrates the components of interactive social media interventions. These include material and human resources and behaviour change techniques (BCTs) implemented through social media and non‐social media interventions as well as the expected intermediate outcomes (e.g. on knowledge, attitudes, self‐efficacy, motivation, emotions) leading to changes in health behaviours and, ultimately, health outcomes including health equity (Edberg 2015; Han 2017; Latkin 2015; Yoon 2014). We have also explored the potential for adverse effects (Rehfuess 2018; Rohwer 2016). We adapted the Funnel of Attrition to describe the mechanism of action of social media interventions on outcomes of interest (see Figure 4) (White 2018).
3.
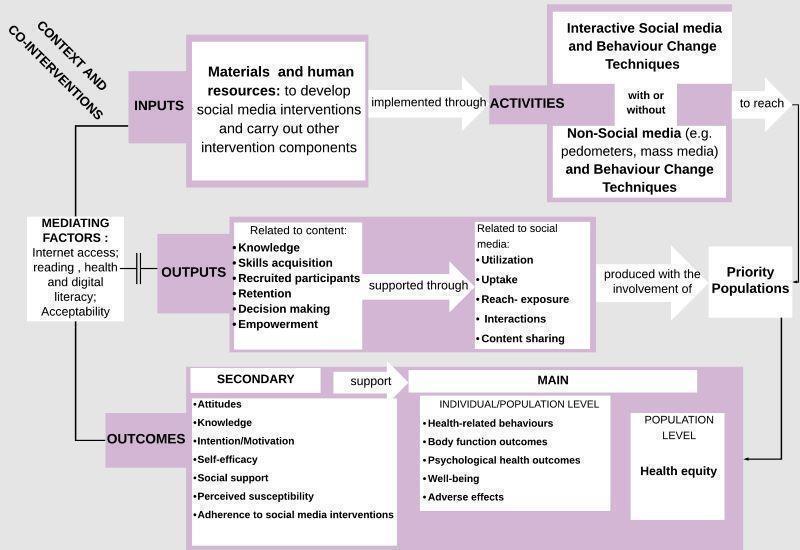
Logic Model
4.
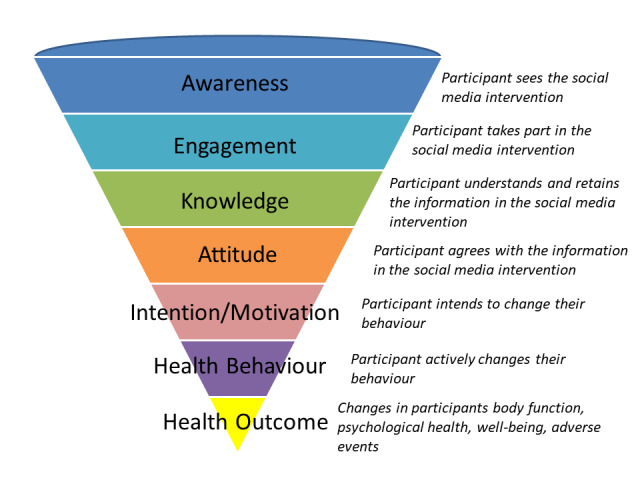
Funnel of Attrition
One of the reasons for using social media to deliver public health interventions is its capacity to build and reinforce social support for improving health outcomes (Osborne 2013; Vassilev 2014; Rhodes 2016; Rice 2016). Enabling social support through interactive social media has been linked to positive impacts on health outcomes by influencing knowledge, motivation, self‐efficacy (one's perceived ability to perform a behaviour), and other beliefs and cognitions towards health behaviours (Bandura 2000; Rhodes 2016; Rice 2016; Wong 2016). When used as a means for strengthening social networks, interactive social media may help promote public health and health equity by fostering collective efficacy (Greene 2011; Phua 2013; Di Bitonto 2015). Collective efficacy, a construct of social cognitive theory, is defined as "people's shared beliefs in their collective power to produce desired results" (Bandura 2000). Additional to the structure and the goal of the group, achieving group efficacy may be fostered by self‐efficacy, social comparison, or other specific rules governing the overall functioning of the group as one unit (Bandura 2000; MacAlister 2008; Ross 2010; Zhang 2016). Given the difficulty of anticipating the structure of participating communities in interactive social media interventions and the dynamic underpinning the functioning of online groups, collective efficacy was not included in the proposed logic model, however, we planned to collect information on collective efficacy, if it was reported.
Social media is often used in public health as a platform or setting for sharing knowledge, building skills, expanding the reach of public health interventions, fostering empowerment, and facilitating decision‐making among priority populations (Seltzer 2015; Hudnut‐Beumler 2016; Ndumbe‐Eyoh 2016). The logic model (Figure 3) acknowledges that interventions that involve social media are often complex interventions (Craig 2008), involving multiple components including offline intervention components to reinforce the message of the health‐related campaign.
Nevertheless, varied levels of interest in, access to, and acceptance of e‐technologies have been reported as affecting the uptake and effectiveness of interactive social media interventions for public health (Thackeray 2012; Antheunis 2013; Merolli 2013; Uskov 2015). Other studies have highlighted the mediating effect of characteristics such as social position, familiarity with social media, and literacy (reading, health, and digital literacy) in boosting the effect of interactive social media interventions on health outcomes (Korda 2013; Merolli 2013; Osborne 2013; Real 2015; Rice 2016). These elements have relevance for the replication of the interventions studied and should be factored into any description of the effects of interactive social media interventions on health outcomes.
Other concurrent public health initiatives, such as campaigns or community mobilisation, and the context in which interactive social media interventions are implemented may also impact the effectiveness of such interventions towards achieving health equity (Hudnut‐Beumler 2016; Ndumbe‐Eyoh 2016; Rice 2016). Thus, the effects of social media combined with campaigns should be interpreted with caution and their adaptation should be based on a thorough analysis of the needs of priority populations and assets available within the communities of interest.
Adverse and unintended effects from communication campaigns may arise due to stigmatisation and other reasons. For example, stigmatisation may be reported in interventions that use mechanisms such as self‐presentation and social comparison to promote healthy behaviours. Self‐presentation is described as "behavior that attempts to convey some information or image of oneself to other people" and it is often motivated by situational factors (Baumeister 1987). On the other hand, social comparison consists of drawing on others' behaviours to make comparison with one's performance (White 2006). Self‐presentation and social comparison have been reported as beneficial in interventions delivered online aimed at promoting healthy behaviours in the context of HIV prevention and physical activity, respectively (Byron 2013; Zhang 2016). While serving positive functions such as avoiding harms and encouraging healthy behaviours, self‐presentation and social comparison may also generate stigmatisation and embarrassment when strategies like manipulation and exemplification are used (Baumeister 1987; White 2006; Byron 2013). For example, someone may present themselves in such a way that they appear competent, dangerous, or morally virtuous (Baumeister 1987). Other adverse or unintended effects of communication campaigns can include confusion and misunderstanding about health risks and risk prevention and 'boomerang' (the reaction of the audience is the opposite of what was intended) (Cho 2007).
Fear of the consequences of privacy breaches and exposure of one's vulnerability through participating in the intervention may deter some individuals from enrolling. In order to avoid unwanted behaviours and to preserve the reputation of the interventions, organisers may establish consent processes that contain warnings to remove anybody deemed behaving inappropriately from the group. This situation may have the perverse effect of further excluding individuals who may have otherwise benefited from the public health intervention if the latter was not delivered through social media. Based on concerns over data security on social networking platforms and researchers' experience with an HIV education intervention delivered through social media, it has been suggested that health researchers familiarise themselves with current privacy settings available in order to help protect participants, and that they educate participants on how to better safeguard their privacy (Bull 2012). Thus, privacy breaches are one potential adverse effect that may be of special interest for the purpose of health interventions delivered online, especially for sensitive topics like sexual practices.
Lack of understanding of the research process and informed consent on the part of participants may influence participation in social media interventions and may differ for specific population groups (e.g. low literacy), especially in studies where this information was provided to participants online rather than with the direct involvement of research study personnel. For example, in the Harnessing Online Peer Education randomised trial (Young 2015), participants received information about the study and completed informed consent online. Chiu 2016 found that younger HOPE study participants, who generally had less experience with research studies than older participants, were less likely to indicate that they had understood the consent form and study process.
Why it is important to do this review
Although there are other systematic reviews of interactive social media interventions, these reviews have concluded that there is a gap in knowledge on the effects of modern social media (Maher 2014; Merolli 2013), and their narrower scope limited their ability to explore the mechanisms of action and possible effect modifiers across different type of behaviours (Laranjo 2015; Williams 2014). Heffernan 2017 have a forthcoming Cochrane title on whether social media influences attitudes and uptake of vaccines; however, this review will focus solely on vaccination, which has a set of issues that may not be generalisable to other areas of public health. Hamm 2014 reviewed the use and effectiveness of social media in child health. Thus, this review focused on adult social media users.
There are several Cochrane and non‐Cochrane systematic reviews on the effects of mass media interventions on topics as diverse as alcohol consumption, smoking prevention and cessation, HIV testing, mental health stigma, uptake of health services, and preventing non‐communicable diseases (Bala 2017; Carson‐Chahhoud 2017; Clement 2013; Grilli 2002; Mosdøl 2017; Siegfried 2014; Vidanapathirana 2005). Our review differs from these because we focused on interactive social media interventions that allow exchange of ideas, not mass media.
A number of reviews have examined equity impacts of health interventions, including those relating to physical activity (Humphreys 2013), prevention, management, or reduction of obesity (Bambra 2015), under‐nutrition (Kristjansson 2015), and healthy eating (McGill 2015). However, the effects of interactive social media interventions on disadvantaged populations have not been assessed in previous reviews. On one hand, interactive social media interventions have the potential to reach geographically dispersed populations, whereas on the other, there may be barriers such as the digital divide, language, literacy, acceptability, and risk of intervention‐generated inequities. Thus, it is important to assess the effects of interactive social media interventions on the health of disadvantaged populations.
Objectives
The main objective of this review was to assess the effects of interactive social media interventions aiming to change health behaviour for adults on health behaviours, physical and psychological health outcomes, and any reported adverse effects.
The secondary objectives were:
to assess the effects of interactive social media interventions that aim to change health behaviour across population subgroups (defined using PROGRESS‐Plus) to assess effects on health equity;
to explore heterogeneity of effects to identify other reasons for differences in effects.
Methods
Criteria for considering studies for this review
Types of studies
Some types of social media, such as peer‐initiated social media, are not conducive to randomisation. Therefore, we limited this review to Cochrane Effective Practice and Organisation of Care recommended study designs (EPOC 2017a), as follows.
Randomised controlled trials (RCTs): these studies consist of randomly assigning participants to receive one of the interventions studied. Participants may be assigned to interventions individually or by group (cluster‐RCTs). The interventions are usually described as treatment group (individuals who receive the intervention) and control group (individuals who do not receive the intervention).
Controlled before‐and‐after (CBA): these studies consist of measuring outcomes before and after the implementation of an intervention in both the treatment group and control group. Study investigators are not involved in the assignment of participants to either treatment or control group. Allocation is usually determined by other factors outside the control of the investigators. To be eligible, CBAs needed to have at least two intervention and two control sites.
Interrupted time series (ITS): these studies consist of measuring outcomes at multiple time points before and after an intervention ('the interruption') with the intent to capture whether the trends persist or there is a change in the outcomes measured after the intervention. When outcomes are assessed at regular intervals in the same participants, the ITS is called a repeated measures study (RMS). To be eligible, ITSs needed to have at least three data points before and three data points after the intervention.
RCTs with stepped‐wedge designs (treatments begun at different times for different groups of participants) were also eligible, however none were identified. We excluded all other study types.
Types of participants
A previous systematic review examined the use and effectiveness of social media in child health (Hamm 2014), therefore we only included members of the general population aged 18 years and older. We included studies with mixed populations (e.g. youth aged 15 to 24), if we were able to obtain disaggregated data for participants aged 18 years and older, or if the study reported that the population is mostly over 18 years of age (i.e. 70% or more of the population is 18 years of age or older). We included people from the general population, as well as participants with an identified health condition.
Given that we are also interested in the effect of social media interventions on health equity, we included studies that focused on or presented disaggregated data across 'PROGRESS‐Plus' characteristics.
Types of interventions
We used the Safko definition of social media: "activities, practices, and behaviours among communities of people who gather online to share information, knowledge, and opinions using conversational media…that make it possible to create and easily transmit content in the form of words, pictures, videos, and audios" (Safko 2012).
To be included in our review, the social media intervention must have allowed for interaction including two‐way communication between the user and peers. We excluded interventions that only offered one‐way communication as well as those that only offered one‐to‐one communication. We restricted inclusion to studies that focused on changing one or more behaviours. We assessed this using the following criteria:
the study purpose is focused on changing one or more behaviours (e.g. exercise, tobacco use); or
the web site/app or platform of the intervention tool described a goal of changing behaviour; or
the components of the intervention included a behaviour change technique that could be described using the Behaviour Change Technique taxonomy (Michie 2013; Presseau 2015).
We only included interactive social media interventions using commonly used social media tools (e.g. Facebook, Twitter) or those mimicking their interface (e.g. Quitnet) and related applications (apps). We excluded web‐based chat rooms designed by researchers or others since these are no longer used; they do not have a user interface like these other commonly used tools, and they have been synthesised in our overview (Welch 2016). Furthermore, because these web‐based chat rooms are not familiar to users, they require a learning curve and an extra effort to engage with them that is not required by tools such as Facebook or Twitter, with which users have familiarity and are likely already using. Examples of the types of interactive social media interventions to be included in this review are summarised in Table 5 (adapted from Welch 2016). We included peer‐initiated interventions as well as interventions initiated by organisations such as public health organisations or private organisations (e.g. Weight Watchers). We excluded studies assessing e‐health or telemedicine interventions that use technology to deliver health care. We also excluded studies that assess mobile health (e.g. apps that track clinical information with communication between an individual and their healthcare provider) and content that is transmitted unidirectionally (e.g. text message reminder interventions in which the recipient is unable to reply, podcasts in which health information is provided with no opportunity for two‐way communication) or which only allows for comments without sharing functionality, such as blogs. We excluded studies that assess online interventions that are based on exchange between a single care provider and a single participant such as online cognitive behavioural therapy, as they are covered within other reviews as telemedicine or e‐health interventions. Advertisements on social media (e.g. on Facebook) were ineligible if they did not have sharing functionality. We also excluded studies of virtual gaming interventions as we considered these to have a different mechanism of action.
We excluded studies of 'beta' interfaces that are aimed at assessing usability and improving the interface. These studies have limited applicability to understanding how social media can be used to influence health.
We included studies comparing interactive social media interventions with any comparison. We classified these as non‐interactive social media control, which included no intervention, usual care, or a non‐interactive social media‐based intervention. These would include, for example, paper‐ or in person‐based interventions or those delivered one‐on‐one via social networking platforms but without providing an opportunity for interaction amongst participants. We grouped these comparators together because we are interested in the effect of the interaction aspect of the social media interventions and are less interested in differences in effectiveness compared to 'no intervention' or 'in‐person' or paper‐based interventions. We also included active social media comparators if one arm received a more interactive social media intervention. Active comparators included those such as an unmoderated Facebook group compared to a moderated Facebook group. For these interventions, we considered the less interactive intervention to be the control.
Types of outcome measures
Primary outcomes
Our main outcomes were health behaviours, impairments of body function, psychological health, well‐being, mortality, and adverse effects (e.g. stigmatisation, exclusion, or harmful health behaviours). We expected the different outcome measures to be different across studies and therefore we did not pre‐specify the outcome measures within each of our outcome domains. We included only those assessed using measurement tools which had been used previously and we extracted data from the longest follow‐up reported.
Health behaviours included alcohol consumption, breastfeeding, dietary changes, physical activity, medication adherence, illicit drug use, sexual behaviours, smoking, and seeking and using health services.
Body functions as defined by the WHO ICF (WHO 2002) such as body mass index (BMI), physical fitness, lung function, or asthma episodes.
Psychological health included measures of depression, stress, coping, and other measures.
Well‐being included measures of quality of life.
Adverse effects included any reported adverse outcomes or unintended consequences associated with interactive social media interventions, such as online harassment and privacy concerns related to discussing or otherwise revealing health issues or health status online, and ethical issues pertaining to participants' privacy.
Table 6 provides a description of the main outcomes as well as the types of outcomes and measures used for each.
5. Specific outcome measures for each outcome category.
| Main outcome categories | Outcome type | Outcome measures |
| 1. Health behaviours | Breastfeeding | Exclusive breastfeeding |
| Dietary behaviour | Diet quality; calorie intake; infant feeding style | |
| Physical activity | Steps per day; total weekly moderate‐vigorous activity; MET min per week; calories expended; attendance at physical activity sessions | |
| Medication adherence | Medication adherence | |
| Health screening | HIV testing; colorectal cancer screening | |
| Vaccination | Vaccination uptake | |
| Safe food handling | Safe food handling | |
| Sexual behaviours | Condom use | |
| Tobacco use | Smoking cessation; smoking rate | |
| 2. Body functions | Body mass index (BMI) | BMI |
| Weight | Weight; infant weight gain; weight control practices | |
| Blood glucose | HbA1c (Mmol/L) | |
| Fat mass | Fat mass | |
| Physical health status | Physical health status score | |
| Cardiorespiratory fitness | Heart beats/minute | |
| Flu‐like illness | Flu‐like illness | |
| Dyspnoea | Dyspnoea score | |
| Insomnia | Insomnia | |
| 3. Psychological health | Depression | Depression score |
| Distress | Distress score | |
| Self‐worth | Self‐worth score | |
| 4. Well‐being | Quality of life | Quality of life score |
| General well being | Well‐being score |
BMI: body mass index; MET: metabolic equivalent
1. Outcome categories were prespecified and the outcome measures include what was reported in our studies.
Secondary outcomes
Secondary outcomes included process outcomes related to the main outcomes of interest and included: attitudes, intention and motivation, knowledge, perceived susceptibility, self‐efficacy, and social support. We also included measures of adherence, as reported by the study authors. We classified adherence as 'good' when the study authors reported 70% or more of participants engaged with or adhering to the social media intervention.
To assess potential impact on health equity, we collected data on population‐specific effects across PROGRESS‐Plus characteristics, when available.
Search methods for identification of studies
Electronic searches
We adapted a search strategy developed by an information specialist (TR), who also worked on the search strategy for our overview (Welch 2016), and used this to search the following electronic databases: CENTRAL, MEDLINE, Embase, and PSYCINFO (all via OVID) and CINAHL via Ebsco). See Appendix 1 for all search strategies.
We searched for studies published between 2001 up to the end of 1 June 2020, because most of the commonly used social media platforms were developed in 2001 or later (e.g. Facebook, Twitter), and our previous overview showed no earlier studies using these commonly used social media applications (Welch 2016).
We did not include a language limit on the searches. Our team is able to collect data from studies in English, Spanish, Catalan, and French. If required, we would have sought help using Cochrane Task Exchange for studies in other languages.
Searching other resources
We searched for unpublished studies or reports using a focused search within Google and Web of Science, as well as searching websites of public health governmental and non‐governmental organisations, including the Public Health Agency of Canada, the World Health Organization (WHO), the Asian Development Bank, and the Inter‐American Development Bank up to the end of May 2020. We also searched clinical trials registries (ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP)) for relevant studies. Finally, we searched the reference lists of our included studies.
Data collection and analysis
Selection of studies
Two review authors independently screened titles and abstracts to identify relevant studies meeting our pre‐specified inclusion criteria. We screened the full text of studies identified as potentially relevant independently, in duplicate. We discussed and resolved disagreements by consensus or with a third member of the research team when necessary.
Data extraction and management
Two independent review authors extracted data on the population (including PROGRESS‐Plus characteristics, where applicable), study design, intervention, comparison, outcomes, context/setting, and implementation such as adherence and exposure to the social media‐based interventions and delivery of the intervention. Disagreements were resolved through discussion with a third member of the team.
Due to the magnitude of outcomes reported in our included studies, we implemented data extraction criteria to prioritise outcomes. Review authors extracted all reported adverse effects and one outcome per the remaining categories of impairment of body function, psychological health, well‐being, and health behaviours. For health behaviours, review authors prioritised outcomes that matched the stated purpose of the intervention. When more than one outcome was stated as the primary behaviour (e.g. physical activity and nutrition), both outcomes were extracted.
The outcome extraction criteria included: 1) use of a validated measurement tool, 2) author‐reported primary outcomes, 3) used in a sample size calculation, and 4) patient‐important outcome. We applied the same criteria to our secondary outcomes of knowledge, attitudes, motivation and self‐efficacy, and other theory‐based constructs related to behaviour change. If an outcome was measured using a validated scale, only the global score was extracted, if a global score was not provided, we extracted all subscales for that outcome. Outcomes were considered to be patient‐important if they affect a person’s daily functioning (e.g. mortality, disability, pain) rather than biomarkers (HbA1c, haemoglobin, etc.) (Boers 2014; WHO 2002). However, biomarkers were extracted when considered relevant to the intervention’s objective (e.g. diabetes management).
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias using the Cochrane 'Risk of Bias' tool for randomised trials, to collect details on how the study was designed and we judged the studies as low, unclear, or high risk of bias for each domain using the guidance in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Additionally, we included the domains of the EPOC 'Risk of bias' tool (EPOC 2017b), which also assesses whether baseline outcome measurements and baseline characteristics are similar and whether there was protection against contamination. We felt that these additional domains were required to ensure that the groups included in our study had similar social media knowledge and use which would affect their use of the interactive social media interventions, as well as similar behaviours at baseline, such as physical activity, since this is important for comparing behaviour changes. For controlled before‐after studies (CBAs) and interrupted time series studies (ITSs), we used the modified EPOC 'Risk of bias' tool (EPOC 2017b). Most of our outcomes were self‐reported and therefore we applied the same 'Risk of bias' ratings for all outcomes as we judged the risks to be similar.
For ITS studies, we used the Cochrane Handbook chapter on assessing bias in non‐randomised studies which includes additional domains: bias due to confounding, bias in selection of participants into the study, bias in classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in measurement of the outcome, and bias in selection of the reported result (Sterne 2020).
Measures of treatment effect
We expected considerable heterogeneity in methods of measurement (e.g. self‐reported, computer‐collected) as well as measurement tools. In consultation with our clinical and statistical experts, we assessed whether it was appropriate to combine these different outcomes, based on conceptual similarity, using standardised mean differences (SMDs), as described in the analysis section below.
We expected that the mechanism of intervention would be similar for these different types of outcomes (see Figure 4), and, although we expected considerable heterogeneity in methods of measurement and in measurement tools, we planned to focus on broad outcome categories (e.g. health behaviours) with less emphasis on the specific outcome types (e.g. physical activity, tobacco use). However, when pooled, there was significant heterogeneity for our main outcomes and the effects could not be described in a meaningful way. In consultation with our knowledge users, we decided to present the results of the broad outcomes narratively, in Table 1 and present disaggregated data outcome type to ensure that the data are useful for those who may need to use these results. We have classified the broad outcomes as our 'main outcome categories' (e.g. health behaviours). These have been further described by 'outcome type' (e.g. breastfeeding, health screening, physical activity), and, when there were more than 10 studies reporting on an outcome type, we conducted an additional post hoc subgroup analysis by the specific outcome measure (e.g. steps per day, total weekly moderate‐vigorous activity). We have described these classifications in Table 6.
When a study included more than one measurement of our outcome classification above, we sought to assess which outcome was considered primary in the trial, based on whether it was named as a primary outcome, used in a sample size calculation or reported more prominently in the abstract or results. We recognised that this may not be possible since some studies have multiple measures of the same concept (e.g. we have identified over 15 measures of exercise behaviour modification such as frequency, intensity, and type of activity, and some studies reported three or more measures). Therefore, we documented how these decisions were made and reported on the additional outcomes available in the study in our Characteristics of included studies table.
As with the main outcomes, we expected heterogeneity in how our secondary outcomes were measured. We only included validated measures of these concepts. We classified all outcomes according to these categories, then conducted subgroup analyses according to the health behaviour each secondary outcome was related to (e.g. physical activity‐related self‐efficacy).
We analysed continuous outcomes as mean differences (MDs) in change from baseline, where possible. For some analyses we used standardised mean differences (SMDs) when different scales assessing the same outcome were used (e.g. well‐being). If baseline and end of study data were available, we calculated the change from baseline and associated standard deviation, using the methods in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2020a). We analysed dichotomous outcomes, such as tobacco use, as risk ratios (RRs).
Unit of analysis issues
We analysed studies at the level of allocation. For cluster‐randomised trials where groups of people were allocated to interventions, we assessed these studies for unit of analysis errors. We detected unit of analysis issues for two of the seven cluster trials (Cheung 2015, Young 2013). For these studies, we identified an intra‐cluster correlation coefficient (ICC) from a similar trial and used it to inflate the standard deviation using the variance inflation factor for each intervention arm, as described in the Cochrane Handbook for Systematic Reviews of Interventions. For dichotomous outcomes, we used the methods in the Cochrane Handbook for Systematic Reviews of Interventions to adjust the numerator and denominator for unit of analysis errors.
Dealing with missing data
We documented how the included studies handled missing data from participants in our data extraction form. We did not impute values for missing participants. If standard deviations were not reported, we calculated them using other methods such as the confidence interval and exact P values using the formulae in the Cochrane Handbook for Systematic Reviews of Interventions, when possible (Higgins 2020a). For studies that met the eligibility criteria but did not report sufficient information for meta‐analyses, we contacted authors (e.g. to request standard deviations or numbers of participants, if not provided). We received additional data from two study authors (Duncan 2014, Greene 2013). If we did not receive a reply or the authors stated that the data could not be provided, we summarised the results narratively.
For dichotomous and continuous outcomes, we analysed using intention‐to‐treat, therefore we used the full number of randomised individuals as the denominator.
Assessment of heterogeneity
We assessed heterogeneity with the I2 statistic and visual inspection of the forest plots. We explored heterogeneity using pre‐planned subgroup and sensitivity analyses, as described below.
Assessment of reporting biases
Publication bias was assessed using funnel plots based on outcomes for each comparator with more than 10 studies. We were able to construct funnel plots for three of our main outcomes.
Data synthesis
As stated above, our initial aim was to group all outcomes according to the five domains described above: health behaviours, well‐being, body function, psychological outcomes, and adverse events. However, based on consultations with our advisory group, we have analysed the outcome types separately, grouped as appropriate, and in consultation with our content experts.
We used Review Manager software (RevMan 2020) to conduct meta‐analyses using random‐effects models. We assessed individually‐randomised trials and cluster‐randomised trials in the same analyses, taking into account unit of analysis issues as above, and we assessed CBA and ITS studies separately.
We conducted separate comparisons based on the type of control group. We classified control groups as non‐interactive social media control when the control was no intervention or a non‐interactive social media control, and we classified those which included an interactive social media comparator in the control arm as having 'active social media controls'. For these studies, we considered the most intense intervention (e.g. social media plus other components) to be the 'intervention' (e.g. compared to social media alone).
Finally, for studies in which the same social media intervention was provided in both arms, we considered the control to be non‐interactive social media (e.g. a Facebook group addressing the health condition of interest compared to a different Facebook group on another topic). In these studies, the outcomes of interest were related to the content for the intervention arm, and participants needed to be active on the social media platform of interest to be eligible. Therefore, the content provided in the control group would be similar to what the participants would be exposed to through their usual social media use so classifying the control groups as non‐interactive social media is appropriate.
We analysed continuous outcomes as standardised mean differences (SMDs), using change from baseline as the measure of effect. For our main outcomes, we re‐expressed these SMDs as mean differences (MDs) in natural units using the most representative study and the most commonly reported outcome for that category. We analysed dichotomous outcomes as risk ratios (RRs) , using the intention‐to‐treat analyses. We calculated the absolute % change as the difference in change divided by the baseline of the intervention group of the most representative study and have included this information in the 'Summary of findings' tables.
We recorded decisions about the classification of outcomes, methods of measurement and selection from amongst multiple measures of the same concept as described above and have reported these in the Characteristics of included studies table.
For studies with multiple arms, we selected the intervention arm considered to have the highest intensity of social media interaction (e.g. most frequent interaction or most frequent reminders). When more than one arm included a social media component, we combined these groups using the methods recommended in the Cochrane Handbook for Systematic Reviews of Interventions. Similarly, for the control arm, we selected the arm that had the least exposure to an intervention (e.g. we selected 'usual care' over information provided via website). For interventions in which there were multiple intervention arms, we assessed those which included a social media component versus the arm designated by the authors as the 'control'.
We planned, but did not have enough data, to construct harvest plots to assess the presence of gradients in effects across sex, ethnicity, socioeconomic status, and other PROGRESS‐Plus characteristics for each outcome (Ogilvie 2008).
Subgroup analysis and investigation of heterogeneity
As above, for outcomes reported by 10 or more studies, we assessed heterogeneity to decide whether statistical meta‐analysis is appropriate. For meta‐analyses, we assessed heterogeneity using visual inspection of forest plots and the I2 statistic for heterogeneity.
We conducted the following planned subgroup analyses.
Type of population (general population, at‐risk, or with a health condition) since having a health condition may provide additional incentive for behaviour change (classified in Table 7).
Presence of co‐interventions such as campaigns that may magnify the impact of interactive social media interventions if combined.
6. Population subgroups.
| Population subgroup | Examples |
| Targeted at general population (universal) | Adults, college students, African American women, employees of a company, pregnant women |
| Targeted at those with a health condition or at‐risk of a health condition | Cancer patients/survivors, Type 2 diabetes, asthma, COPD/bronchitis/emphysema, HIV, trauma patients, rehabilitation patients, smokers, overweight/obese adults, men who have sex with men, low income mothers |
COPD: chronic obstructive pulmonary disease
We used the test for subgroup interaction in Review Manager 5.3 to perform these analyses.
We planned but were unable to conduct the following subgroup analyses.
Specific equity characteristics (sex/gender, ethnicity, socioeconomic status, and age are considered the most important for this question). Our included studies did not provide enough information to conduct subgroup analyses based on equity but we have summarised the available information from studies which were aimed at a potentially disadvantaged group.
Behaviour change techniques (BCTs) used (i.e. we planned to assess each BCT used in at least two studies as a potential mediator of the effect). We did not assess effectiveness of BCTs and instead described which BCTs were used. We present the major results of that analysis here but have published the complete results in a separate paper to allow more detail (Simeon 2020).
Participants (e.g. smokers, under‐users). We did not have enough information for subgroup analyses for specific participant characteristics but have reported subgroup analyses on the populations of the studies in general.
Intensity of interactive social media intervention (e.g. high versus low frequency of interaction, or automatic reminder messages versus no reminders). We were unable to conduct subgroup analyses for intensity because this type of information could not be combined across studies. We have instead provided data for the adherence to the intervention, as reported by the study authors.
Through consultation with our knowledge users, we also presented disaggregated data by outcome type, such as different health behaviours (e.g. physical activity, calorie intake, tobacco use) and have disaggregated these further when there were more than 10 studies assessing these using the same outcome measure (e.g. daily step counts, weekly minutes of moderate‐vigorous physical activity) (see Table 6 for description).
Sensitivity analysis
We conducted sensitivity analysis across risk of bias (i.e. allocation concealment and blinding of participants) by including only those assessed as low risk of bias. We also conducted a sensitivity analysis according to engagement with and adherence to the interactive social media intervention, defined as 70% or greater adherence as reported by the study authors.
Summary of findings and assessment of the certainty of the evidence
We present the evidence from randomised controlled trials (RCTs) for our main outcomes for the comparison of interactive social media to non‐interactive social media control in a Table 1. We assessed the certainty of the body of evidence for each outcome presented in our 'Summary of findings' tables using the GRADE methodology (Guyatt 2011). We presented our level of certainty as high, moderate, low, or very low. GRADE assessments were completed independently, in duplicate and disagreements were resolved with a third review author. We downgraded studies for imprecision when there was substantial heterogeneity and when the confidence intervals were wide. We downgraded due to risk of bias when the overall risks of bias of the studies were determined to be high or unclear based on whether any of the 'Risk of bias' domains were high (assessed as high overall) or unclear (Higgins 2020b). We would have downgraded for indirectness but did not judge there to be any differences between our studies. We assessed publication bias using funnel plots for outcomes with data from 10 or more studies.
Results
Description of studies
Results of the search
Our search yielded 66,249 results and we identified 88 studies from other sources. After de‐duplicating, we screened 39,615 titles and abstracts and excluded 39,062. We retrieved and screened 553 full‐text articles and excluded 265. We included a total of 88 studies (871,378 participants), reported in 156 papers. See Figure 5 for our PRISMA flow diagram. We identified 61 potentially eligible ongoing studies (reported in 66 papers) and 19 potentially eligible studies which are awaiting assessment as more information regarding study design or intervention is needed. The Characteristics of studies awaiting classification and Characteristics of ongoing studies tables provide additional details on these.
5.
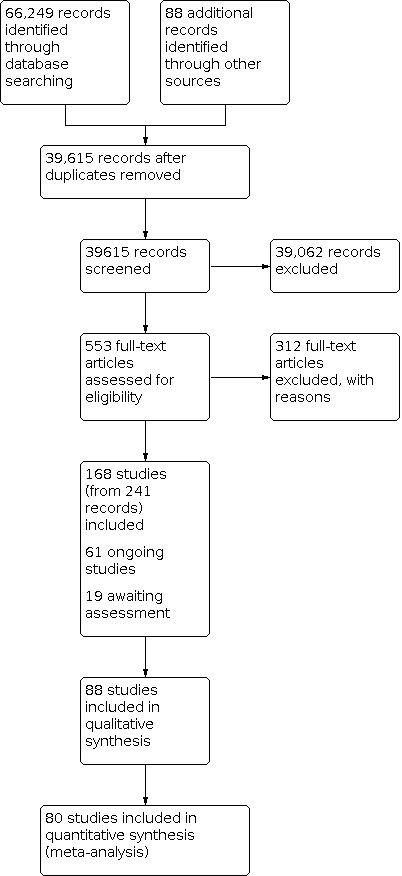
Study flow diagram.
Included studies
Refer to Characteristics of included studies.
The majority of the 88 included studies were conducted in the USA (n = 49, 56%) with other studies conducted in Australia (n = 14, 16%), China (n = 10, 11%), Canada (n = 3, 3%), South Korea (n = 2, 2%) and one study in each of Brazil, Germany, Ireland, Italy, Malaysia, the Netherlands, Peru, Singapore, Sweden, and the UK. We included 84 randomised controlled trials (RCTs,) of which 7 were cluster randomised, three controlled before‐after studies (CBAs), and one interrupted time series (ITS). A summary of the included studies is provided in Table 8. We have provided a summary of the important characteristics of each study in our Overview of Synthesis and Included Studies table (Table 9).
7. Summary of included studies.
| Study characteristics | N=88 | (%) |
| Country | ||
| USA | 49 | 56 |
| Australia | 14 | 16 |
| China | 10 | 11 |
| Canada | 3 | 3 |
| South Korea | 2 | 2 |
| Brazil | 1 | 1 |
| Germany | 1 | 1 |
| Ireland | 1 | 1 |
| Italy | 1 | 1 |
| Malaysia | 1 | 1 |
| the Netherlands | 1 | 1 |
| Peru | 1 | 1 |
| Singapore | 1 | 1 |
| Sweden | 1 | 1 |
| United Kingdom | 1 | 1 |
| High‐income countries | 76 | 86 |
| Upper‐middle‐income countries | 12 | 14 |
| Study design | ||
| RCT | 83 | 94 |
| Controlled before‐and‐after study | 4 | 5 |
| Interrupted time series | 1 | 1 |
| Type of social media | ||
| Web‐based community | 42 | 48 |
| 34 | 39 | |
| 5 | 6 | |
| 3 | 3 | |
| What's App | 2 | 2 |
| Google Hangouts | 1 | 1 |
| 1 | 1 | |
| Targeted population | ||
| Adults | 28 | 32 |
| Students | 14 | 16 |
| Patients who are overweight or obese, with Type 2 diabetes or coronary heart disease | 10 | 11 |
| Smokers | 8 | 9 |
| Pregnant women | 7 | 8 |
| Cancer patients and survivors | 6 | 7 |
| Men who have sex with men | 5 | 6 |
| Patients with COPD, bronchitis, asthma | 2 | 2 |
| Parents of overweight/obese children | 2 | 2 |
| Parents of children with ADHD | 1 | 1 |
| Haemodialysis patients | 1 | 1 |
| Mothers with PPD symptoms | 1 | 1 |
| Rehab patients | 1 | 1 |
| Trauma patients | 1 | 1 |
8. Overview of synthesis and included studies.
| Study | Study design | Overall risk of bias (study level) | Population category (healthy, at‐risk) | Type of intervention (social media alone, multi‐components) | Comparator | Outcome domains | Specific outcomes | If clustered, was clustering accounted for? |
| Ahmad 2018 | RCT | High | Targeted | Multi‐component | No intervention | Body function | BMI | ‐ |
| Ahmad 2020 | RCT | Unclear | General | Multi‐component | No intervention | Health behaviour Psychological health Well‐being | Mindfulness Depression Quality of life | ‐ |
| Ashton 2017 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | Health behaviour Body function Psychological health Well‐being | Steps Diet quality Weight Depression Well‐being | ‐ |
| Bai 2015 | cRCT | High | General | Multi‐component | Non‐social media | Health behaviour | Medication adherence | ‐ |
| Baker 2011 | RCT | High | Targeted | Multi‐component | Non‐social media | *not included in analysis | *not included in analysis | ‐ |
| Bantum 2014 | RCT | Unclear | Targeted | Social media only | Non‐social media | Health behaviour Body function Psychological health Well‐being | MVPA Diet quality Insomnia Depression | ‐ |
| Bender 2017 | RCT | High | Targeted | Multi‐component | Non‐social media | Health behaviour Body function | Steps Weight | ‐ |
| Booth 2018 | ITS | General | Social media only | No intervention | Health behaviours | Outpatient mental health visits | ‐ | |
| Boyd 2019 | RCT | High | Targeted | Social media only | Non‐social media | Psychological health | Depression | ‐ |
| Bull 2012 | cRCT | High | General | Social media only | Active social media comparator | Health behaviour | Condom use | Yes |
| Castillo 2013 | CBA | High | Targeted | Multi‐component | Non‐social media | Body function Psychological health | Physical health status Depression | ‐ |
| Cavalcanti 2019 | RCT | HIgh | General | Multi‐component | Non‐social media | Health behaviours | Breastfeeding | ‐ |
| Cavallo 2012 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviours | Calorie expenditure | ‐ |
| Chai 2018 | CBA | High | Targeted | Multi‐component | No intervention | health behaviours | Smoking rate | ‐ |
| Chen 2019 | RCT | Unclear | Targeted | Social media only | Non‐social media | Body function Well‐being | HbA1c Quality of life | ‐ |
| Cheung 2015 | cRCT | High | Targeted | Multi‐component | Non‐social media | Health behaviours | Smoking relapse | We calculated using ICC 0.148 |
| Cobb 2014 | RCT | High | General | Social media only | Non‐social media | Well‐being | Well‐being | ‐ |
| Coffeng 2014 | cRCT | High | General | Multi‐component | No intervention | Health behaviours Psychological health | MVPA Need for recovery | ‐ |
| Dadkhah 2014 | RCT | Unclear | General | Social media only | Non‐social media | Health behaviour Body function | MVPA Diet quality Weight | ‐ |
| Dahl 2019 | RCT | High | General | Multi‐component | Active social media comparator | Health behaviours Body function | Weight | ‐ |
| Daly 2017 | RCT | High | Targeted | Multi‐component | Non‐social media | Body function | Weight (gestational) | ‐ |
| Dehlendorf 2020 | RCT | High | General | Social media only | Active social media comparator | Health behaviour | IUD use | ‐ |
| Duncan 2014 | RCT | Unclear | General | Social media only | Non‐social media | Health behaviour | MVPA Diet quality | ‐ |
| Edney 2020 | RCT | High | General | Multi‐component | No intervention | Health behaviours Psychological health Well‐being | MVPA Depression Quality of life | ‐ |
| Fiks 2017 | RCT | High | Targeted | Multi‐component | Non‐social media | Health behaviours | Diet quality | ‐ |
| George 2013 | RCT | Unclear | General | Social media only | Non‐social media | *not included in analysis | *not included in analysis | ‐ |
| Glanz 2017 | RCT | Unclear | General | Social media only | Non‐social media | Health behaviour | Vaccination | ‐ |
| Gnagnarella 2016 | RCT | Unclear | Targeted | Social media only | Non‐social media | Health‐behaviour Psychological health Well‐being | Diet quality Distress Quality of life | ‐ |
| Godino 2016 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | Body function | Weight | ‐ |
| Graham 2011 | RCT | high | Targeted | Multi‐component | Non‐social media | Health behaviours | Tobacco use | ‐ |
| Graham 2018 | RCT | High | Targeted | Social media only | Non‐social media | Health behaviours | Tobacco use | ‐ |
| Greene 2013 | RCT | High | General | Multi‐component | Non‐social media | Health behaviours Body function | MVPA Weight | ‐ |
| Hammersley 2019 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviours | Parent modelling | ‐ |
| Herring 2014 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | Body function | Weight | ‐ |
| Herring 2017 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | Body function | Weight | ‐ |
| Horvath 2013 | RCT | High | Targeted | Social media only | Non‐social media | Health‐behaviours | Medication adherence | ‐ |
| Hutchesson 2018 | RCT | Unclear | Targeted | Multi‐component | No intervention | Health behaviours Body function Well‐being | MVPA Calorie intake Weight Quality of life | ‐ |
| Hwang 2013 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviour | Screening | ‐ |
| Jane 2017 | RCT | High | Targeted | Social media only | Non‐social media | Health behaviours Body function Psychological health Well‐being | Weight Calorie intake Depression Quality of life | ‐ |
| Joseph 2015 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviours Body function | MVPA BMI | ‐ |
| Kernot 2019 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviours Body function Psychological health Well‐being | MVPA BMI Depression Quality of Life | ‐ |
| Kim 2019 | RCT | High | Targeted | Multi‐component | No intervention | Health behaviours Body function | Self‐care HbA1c | ‐ |
| Kolt 2017 | RCT | High | General | Multi‐component | Non‐social media | Health behaviours | MVPA | ‐ |
| Koufopoulos 2016 | RCT | High | Targeted | Social media only | Non‐social media | Health behaviours | Medication adherence | ‐ |
| Lau 2012 | RCT | Unclear | General | Multi‐component | No intervention | Health behaviours | Vaccination Influenza‐like illness | ‐ |
| Li 2017 | RCT | Unclear | Targeted | Social media only | Active social media comparator | psychological health well‐being secondary outcomes | Depression Well‐being | ‐ |
| Li 2020 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviours | Maternal care utilization | ‐ |
| Liao 2020 | RCT | High | General | Social media only | No intervention | health behaviours secondary outcomes | Vaccination | ‐ |
| Linden 2017 | RCT | High | Targeted | Multi‐component | Non‐social media | body function psychological health well‐being secondary outcomes | HbA1c Distress Well‐being | ‐ |
| Looyestyn 2018 | RCT | High | General | Social media only | Non‐social media | health behaviours body function secondary outcomes | Cardiorespiratory fitness | ‐ |
| Lytle 2017 | RCT | High | General | Multi‐component | Non‐social media | health behaviours body function | MVPA Weight | ‐ |
| Maher 2015 | cRCT | High | General | Multi‐component | No intervention | health behaviours well‐being | MVPA Quality of life | Yes |
| Mailey 2016 | RCT | High | General | Social media only | Active social media comparator | health behaviours psychological health secondary outcomes | Physical activity Physical self‐worth | ‐ |
| Mascarenhas 2018 | RCT | High | General | Social media only | No intervention | health behaviours body function psychological health | MVPA | ‐ |
| Morris 2015 | RCT | High | General | Social media only | Non‐social media | psychological health | Depression | ‐ |
| Moy 2010 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | *not included in analysis | *not included in analysis | ‐ |
| Moy 2015 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | health behaviours well‐being | Steps Quality of life | ‐ |
| Nam 2015 | RCT | Unclear | Targeted | Social media only | No intervention | well‐being secondary outcomes | Quality of life | ‐ |
| Nam 2020 | RCT | Unclear | General | Multi‐component | Non‐social media | health behaviours body function | PMS score | ‐ |
| Namkoong 2017 | RCT | Unclear | General | Social media only | Active social media comparator | *not included in analysis | *not included in analysis | ‐ |
| Napolitano 2013 | RCT | Unclear | General | Social media only | No intervention | Body function | Weight | ‐ |
| O’Neil 2016 | RCT | High | Targeted | Multi‐component | Non‐social media | Body function | HbA1c | ‐ |
| Owen 2015 | RCT | High | Targeted | Multi‐component | No intervention | Psychological health | Distress | ‐ |
| Petrella 2017 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | Health behaviours Well‐being Body function Secondary outcomes | Steps BMI Quality of life | ‐ |
| Ramo 2015 | RCT | High | Targeted | Multi‐component | Non‐social media | Health behaviours | Tobacco use | ‐ |
| Ramo 2018b | RCT | High | Targeted | Social media only | Active social media comparator | Health behaviours | Tobacco use | ‐ |
| Ren 2019 | RCT | High | Targeted | Multi‐component | No intervention | Health behaviours Mortality Secondary outcomes | Self‐care | ‐ |
| Richardson 2010 | RCT | High | Targeted | Social media only | Non‐social media | Health behaviours | Steps | ‐ |
| Rote 2015 | RCT | High | General | Social media only | Non‐social media | Health behaviours Body function Secondary outcomes | Steps Weight | ‐ |
| Rouf 2020 | RCT | High | Young adults | Multi‐component | Non‐social media | health behaviours secondary outcomes | Calcium intake | ‐ |
| Rovniak 2016 | cRCT | High | General | Social media only | Non‐social media | *not included in analysis | *not included in analysis | *not included in analysis |
| Schaller 2017 | RCT | High | Targeted | Multi‐component | Non‐social media | Health behaviours | MVPA | ‐ |
| Schneider 2015 | cRCT | High | General | Multi‐component | Non‐social media | *not included in analysis | *not included in analysis | *not included in analysis |
| Stoddard 2008 | RCT | High | Targeted | Social media only | Non‐social media | health behaviours secondary outcomes | Tobacco use | ‐ |
| Sun 2017 | RCT | High | General | Social media only | Non‐social media | health behaviours secondary outcomes | Condom use | ‐ |
| Turner‐McGrievy 2011 | RCT | High | Targeted | Social media only | Non‐social media | Health behaviours Body function Secondary outcomes | Diet quality Weight | ‐ |
| Valle 2013 | RCT | High | Targeted | Social media only | Active social media comparator | Health behaviours Body function Well‐being Secondary outcomes | Physical activity Weight Quality of life | ‐ |
| Vandelanotte 2017 | RCT | High | General | Social media only | Active social media comparator | Health behaviours Body function Well‐being | MVPA BMI Quality of life | ‐ |
| Vogel 2019 | RCT | High | Targeted | Social media only | Active social media comparator | Health behaviours | Tobacco use | ‐ |
| Wan 2017 | RCT | Unclear | Targeted | Multi‐component | Non‐social media | Health behaviours Psychological health Well‐being Secondary outcomes | Steps Dyspnoea Depression Quality of life | ‐ |
| Wang 2015 | CBA | Unclear | General | Multi‐component | No intervention | Health behaviours | Physical activity | ‐ |
| Washington 2017 | RCT | Unclear | Targeted | Social media only | Non‐social media | health behaviours secondary outcomes | Screening | ‐ |
| Willcox 2017 | RCT | High | General | Multi‐component | No intervention | Health behaviours Body function | MVPA Weight | ‐ |
| Willis 2017 | RCT | High | Targeted | Multi‐component | Non‐social media | Health behaviours Body function | MVPA Calorie intake Weight | ‐ |
| Yang 2019 | RCT | High | Targeted | Multi‐component | Active social media comparator | Psychological health | Depression Anxiety | ‐ |
| Young 2013 | cRCT | High | Targeted | Social media only | Non‐social media | Health behaviours | Screening | We adjusted based on ICC 0.05 |
| Young 2015 | cRCT | Unclear | Targeted | Social media only | Active social media comparator | Health behaviours | Screening | Yes |
| Zhang 2016 | RCT | Unclear | General | Multi‐component | Non‐social media | Health behaviours | Exercise classes attended | ‐ |
BMI: body mass index; MPVA: moderate‐to‐vigorous physical activity
Many comparators included non‐interactive social media interventions, such as standard care or written or online materials. Ten included studies compared an interactive social media intervention to another social media intervention. For these, we classified the most interactive intervention as the 'intervention' group and the other as the 'control'. For example, the study by Mailey and colleague, included an online discussion board in both arms of the study, but the intervention participants had access to additional features and were placed into small groups for discussion and sent reminder emails to prompt discussion (Mailey 2016). The study by Vogel and colleagues assessed a culturally‐tailored Facebook intervention compared to a standard, non‐tailored version of the same intervention (Vogel 2019).
Excluded studies
Refer to Characteristics of excluded studies.
We assessed the full text of 481 papers and excluded 312. Studies were mainly excluded because they did not include a control group, did not aim to change a health behaviour, did not assess an intervention with an interactive social media component, or focused on beta‐testing of a platform.
Risk of bias in included studies
See Figure 6 for the 'Risk of bias' assessment summary. Details of the risk of bias assessments can be found in Characteristics of included studies.
6.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation
Most studies (n = 62) were assessed as low risk of bias for random sequence generation while 20 studies did not report on the method of randomisation and were assessed as unclear.
The remaining five studies were assessed as high risk of bias, although three of these were controlled before‐after studies (CBAs).
Allocation concealment
For allocation concealment, 26 studies were assessed as low risk of bias and five studies were assessed as high risk of bias. The majority of studies (n = 56) were unclear.
Blinding
Blinding of personnel
We assessed 13 studies as low risk of bias for blinding of study personnel. The majority of studies (n = 46) were high risk of bias due to non‐blinded study personnel. The remaining studies (n = 28) did not report on blinding of personnel and were assessed as unclear.
Blinding of participants
Only 10 studies were assessed as low risk of bias for blinding of participants. We assessed 31 studies as high risk of bias because participants were unblinded. The remaining studies (n = 46) were unclear.
Blinding of outcome assessment (detection bias): all outcomes
The risk of bias for blinding of outcome assessment was unclear in most studies (n = 48). Nineteen studies were assessed as high risk of bias for blinding of outcome assessment due to non‐blinding. The remaining 20 studies adequately blinded the outcome assessment and were assessed as low risk of bias.
Incomplete outcome data
We assessed 27 studies as high risk of bias for incomplete outcome data and 45 studies as low risk. Fifteen studies were unclear.
Selective reporting
Sixteen studies were assessed as low risk of bias for selective outcome reporting. We assessed 34 studies as high risk of bias because additional outcomes had been reported in the study protocol or trial registration that were not reported within the included papers. The remaining 37 studies were unclear.
We were able to construct funnel plots for three of our main outcomes: physical activity (Figure 7), body function outcomes (Figure 8), and well‐being (Figure 9). All of the outcomes assessed displayed symmetrical funnel plots, therefore studies do not suggest publication bias.
7.

Funnel plot of comparison: 1 Overall ‐ any interactive social media intervention compared to non‐interactive social media control, outcome: 1.1 Health behaviours ‐ physical activity.
8.

Funnel plot of comparison: 1 Overall ‐ any interactive social media intervention compared to non‐interactive social media control, outcome: 1.18 Body functions ‐ weight (Kgs).
9.

Funnel plot of comparison: 1 Overall ‐ any interactive social media intervention compared to non‐interactive social media control, outcome: 1.28 well‐being outcomes.
Other potential sources of bias
Baseline characteristics
Most of our included studies reported similar baseline characteristics (e.g. the population characteristics of the participants, such as their age and social media use) for the intervention and control groups (n = 54). We assessed 17 studies as high risk of bias because of differences in population characteristics between groups. The remaining 16 studies were unclear.
Baseline outcome measurements
We also assessed whether the groups were similar at baseline for our outcome, such as physical activity, weight, or depression scores. The majority of our included studies (n = 38) were assessed as low risk of bias for differences in baseline outcome measurements. We assessed 18 studies as high risk and the remaining 31 were unclear.
Protection against contamination
We assessed 31 studies as low risk of bias for contamination. Eleven studies were assessed as high risk of bias. The remaining 45 studies were unclear.
Risk of bias for interrupted time series (ITS) study
We included one ITS study (Booth 2018) and assessed different domains specific for this study design.
Bias due to confounding
We assessed the Booth study as moderate for this domain because the study spans nine years and the authors have not reported on any other confounding situations that may have also taken place during this time.
Bias in selection of participants into the study
The Booth study is low risk for selection bias as the study compares access to mental health care before and after a health promotion campaign.
Bias in classification of interventions
The Booth study is moderate risk for bias related to the intervention. The authors did not measure whether the intervention was received by all participants. The intervention was mass released on social media but exposure to the messages were not assessed by those receiving care.
Bias due to deviations from intended interventions
The Booth study is low risk for bias related to deviations from the intervention.
Bias due to missing data
We assessed this study as moderate as data were missing for fewer than 0.1% of visits per year but participants were excluded based on missing information related to sex.
Bias in measurement of the outcome
The Booth study was low for bias in measurement of the outcomes.
Bias in selection of the reported result
We assessed the study as low for bias in selection of the reported results as the results correspond to the planned analysis.
Effects of interventions
See: Table 1
The interventions included in this review were quite different, however, we grouped them as planned into two comparisons: 1) social media compared to non‐interactive social media comparator, and 2) social media compared to active social media comparator. We grouped similar outcomes within our main outcome domains. We have reported the results for the main broad outcomes narratively in Table 1 and have reported more details about different outcome types in additional tables (Table 2, SoF: health behaviours, Table 3, Additional SoF: body function outcomes, and Table 4, Additional SoF: well‐being and psychological outcomes) and for comparison 2 in Table 10, Additional SoF: Active comparator, all outcomes. We explored the heterogeneity for these outcomes with subgroup and sensitivity and analyses as described above. Only the results from the RCTs were included in the Summary of Findings tables.
9. 'Summary of findings' table: all outcomes, active comparator.
| Any interactive social media intervention compared with an active social media comparator | |||||
|
Patient or population: adults Settings: High and high‐middle income countries Intervention: interactive social media Comparison: avctive social media comparator | |||||
| Outcomes | Absolute effect (95% CI) | Effect estimate (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Health behaviours ‐ Physical activity | The intervention group increased total weekly physical activity by 28 minutes (from 9 to 47 minutes more) | SMD 0.35 (0.12 to 0.59) | 1523 (4 RCTs) | ⊕⊝⊝⊝ very low1 | Absolute calculated using Valle 2013 |
| Body function outcomes ‐ Weight (kg) | The intervention group lost 4.70 kg more weight than the control group (from 1 kg to 8 kg more) | MD ‐4.70 kg (‐8.31 to ‐1.09) | 66 (1 RCT) | ⊕⊝⊝⊝ very low2 | |
| Body function outcomes ‐ BMI | The intervention group reduced BMI by 1.20 kg/m2 more (from 0.99 to 1.41 to ‐0.99 kg/m2 more). | MD ‐1.20 kg/m2 (‐1.41 to ‐0.99) | 1328 (1 RCT) | ⊕⊕⊝⊝ low3 | |
| Well‐being | The mean well‐being score on the RAND 36 scale was 69.3. The mean in the interactive social media group was 0.4 points higher (from 1.5 lower to 2.5 higher) (scale from 0‐100) | SMD 0.02 (‐0.08 to 0.13) | 2082 (2 RCTs) | ⊕⊕⊝⊝ low4 | Absolute calculated using Vandelanotte 2017 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: Mean difference; SMD: Standardised mean difference | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
1. Downgraded by 3 for high heterogeneity (inconsistency), indirectness (studies included working women and discussion groups or involved walking activities among healthy adults or cancer patients), and imprecision.
2. Downgraded by 3 very serious imprecision and high risk of bias.
3. Downgraded by 1 for single study and unclear risks of bias.
4. Downgraded by 2 for inconsistency and unclear risks of bias.
A brief description of each is provided below. The results are presented by comparison. There was considerable heterogeneity for many outcomes, as expected, because the interventions had different co‐interventions, different populations, and different outcomes. We have also conducted subgroup analyses to assess whether there are differences in effectiveness of the intervention depending on whether the intervention is aimed at the general population or at a population with or at‐risk of a health condition.
Six of our included studies could not be included in our meta‐analyses due to missing data: Baker 2011, George 2013, Namkoong 2017, Moy 2010, Rovniak 2016, Schneider 2015. The authors were contacted but they either did not reply or reported that the data were no longer available.
Comparison 1: Any interactive social media intervention compared to non‐interactive social media
Health behaviours
Physical activity
Physical activity can be measured in many different ways. We presented the combined results of the reported outcomes for these but also separated them by outcome type because of the differences in the aims of the interventions. Daily step counts and weekly minutes of moderate‐to‐vigorous activity were the most frequently reported physical activity outcomes, however, they correspond to different aims. Step counts aim to get people moving whereas minutes of moderate‐to‐vigorous activity aim to improve fitness. Therefore we decided it was appropriate to separate these studies by outcome type due their different implications for policy and programming. We have also separated the results by population group and intervention type (whether social media was delivered alone or as a component of a multi‐component intervention). See Table 2.
We included 29 studies (n = 6250) assessing increases in physical activity. When combined, the data from these studies indicated that interactive social media interventions may increase physical activity ( standardised mean difference (SMD) 0.29, 95% confidence interval (CI) 0.13 to 0.45; low‐certainty evidence, small effect size) when compared to a non‐interactive social media intervention. However, there was substantial heterogeneity between interventions (I2 = 84%). This represents an increase of 74 more steps per day for the intervention group (95% CI from 32 to 116 more steps per day) (Analysis 1.1).
1.1. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 1: Health behaviours ‐ physical activity
Disaggregated by outcome type
We disaggregated the data by outcome type. Seven studies (n = 861) assessed changes in the mean number of steps per day and found that interactive social media may increase daily step counts (mean difference (MD) 1376.81 steps (95% CI 708.43 to 2045.18, substantial heterogeneity (I2 = 83%) ) (Analysis 2.1).
2.1. Analysis.

Comparison 2: Disaggregated by outcome type ‐ any interactive social media intervention compared to non‐social media control, Outcome 1: Physical Activity (Steps per day)
Sixteen studies (n = 2365) assessed changes in the mean number of daily minu tes of moderate‐to‐vigorous physical activity. These studies found that interactive social media may increase daily activity (MD 15.81 minutes, 95% CI ‐2.98 to 34.59), but the results are uncertain. Again, there was substantial heterogeneity (I2=86%) (Analysis 2.2).
2.2. Analysis.

Comparison 2: Disaggregated by outcome type ‐ any interactive social media intervention compared to non‐social media control, Outcome 2: Physical Activity (total weekly minutes moderate‐vigorous activity)
When disaggregated, two studies found that interactive social media interventions may increase mean metabolic equivalent (MET) minutes per week (MD ‐833.93 MET‐min/week, 95% CI ‐5398.37 to 3730.52, substantial heterogeneity (I 2 = 95%) ) ( Analysis 2.3. A MET is the amount of oxygen consumed at rest.
2.3. Analysis.

Comparison 2: Disaggregated by outcome type ‐ any interactive social media intervention compared to non‐social media control, Outcome 3: Physical Activity (MET‐min/wk)
Two studies (n = 162) assessed changes in physical activity by assessing energy spent (e.g. calories expended). These studies found that interactive social media interventions may increase calorie expenditure slightly (MD 194.89 calories spent, 95% CI ‐38.38 to 428.15, no important heterogeneity (I2=0%)) but the results are uncertain (Analysis 2.4).
2.4. Analysis.

Comparison 2: Disaggregated by outcome type ‐ any interactive social media intervention compared to non‐social media control, Outcome 4: Physical Activity (calories expended)
One study (n = 592) assessed changes in attendance at physical activity classes and found that interactive social media may increase attendance slightly (MD 0.31 classes, 95% CI ‐0.34 to 0.96) but the results are uncertain (Analysis 2.5).
2.5. Analysis.

Comparison 2: Disaggregated by outcome type ‐ any interactive social media intervention compared to non‐social media control, Outcome 5: Attendance at physical activity sessions (number of classes)
Subgroup analyses
When there were 10 or more studies reporting on an outcome, we explored heterogeneity using planned subgroup analyses for the different population groups and intervention type (social media alone compared to social media as a component of a multi‐component intervention).
Regarding populations, we assessed studies of the general population and those including participants with a condition or at‐risk of a condition. We found that there were no subgroup differences (Chi² = 0.02, P = 0.90, I² = 0%) with an increase of 73 steps per day for the intervention group (95% CI 13 to 134 steps more) among general populations (SMD 0.8, 95% CI 0.05 to 0.51, substantial heterogeneity (I2 = 88%), large effect) and 87 more steps per day (95% CI 8 to 166 more steps per day) among populations with a condition or at risk of a condition (SMD 0.28, 95% CI 0.00 to 0.57, substantial heterogeneity (I2 = 81%), small effect) (Analysis 3.1).
3.1. Analysis.

Comparison 3: Subgroup by population ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 1: Health behaviour ‐ All Physical Activity
We conducted planned subgroup analyses by intervention type and outcome and found no differences (Chi² = 0.01, P = 0.92, I² = 0%) in daily step counts. (Analysis 4.1). There were also no subgroup differences in weekly minutes of physical activity for social media interventions alone compared to those included in a component of a multi‐component intervention (Chi² = 2.45 , P = 0.1 2, I² = 5 9.2 %) (Analysis 4.2).
4.1. Analysis.

Comparison 4: Subgroup by outcome type and intervention type ‐ Interactive social media intervention compared to non‐interactive social media control, Outcome 1: Physical Activity (Steps per day)
4.2. Analysis.

Comparison 4: Subgroup by outcome type and intervention type ‐ Interactive social media intervention compared to non‐interactive social media control, Outcome 2: Physical Activity (total weekly minutes moderate‐vigorous activity)
Sensitivity analyses
When 10 or more studies reported on the same outcome, we conducted a sensitivity analysis to assess the studies for which there was low risk of bias for allocation concealment. The combined data for these 10 studies found that interactive social media interventions may improve physical activity (SMD 0.38, 95% CI 0.07 to 0.69) which is consistent with the main findings (Analysis 5.1). Only one study was assessed as low risk of bias for blinding of participants. This study found a small improvement in physical activity but the results are uncertain (SMD 0.31, 95% CI ‐0.34, 0.96) (Analysis 5.2).
5.1. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 1: Health behaviours ‐ physical activity, Low ROB for allocation concealment
5.2. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 2: Health behaviours ‐ physical activity, Low ROB for blinding of participants
We also conducted planned sensitivity analyses based on adherence. We used the authors' reports of engagement with social media (e.g. Facebook posts) or adherence to the intervention (e.g. step count uploads) to assess adherence and considered 70% engagement or adherence to be "good". Six studies reported good adherence to the social media component of the intervention and found that interactive social media may improve physical activity (SMD 0.26, 95% CI ‐0.04 to 0.55), similar to the main findings (Analysis 5.3) (Table 11).
5.3. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 3: Health behaviours ‐ physical activity, Good adherence
10. Engagement and adherence outcomes.
| Study | Social Media Intervention Component | Outcome | Result | Good adherence (assessed as >70% engagement with or adherence to the social media intervention) |
| Ahmad2018 | Facebook and WhatsApp | Participation in WhatsApp (accessing information) | 96.9% of parents participated in WhatsApp. | Good adherence |
| Participation in Facebook groups (accessing information) | 81.3% of parents participated in Facebook. | |||
| Ahmad 2020 | Web‐based | Watching videos | 65% (24/37) watched 7 to 12 videos from “start to finish". | Cannot assess adherence by watching videos or responding not applicable to the appropriateness, supportiveness, and informativeness of exchanges in discussion forums. |
| Exchanges on discussion forums | 18.9% (7/27) of participant chose “not applicable” for questions on the appropriateness, supportiveness or informativeness of the discussion forum, indicating their nonuse. | |||
| Ashton 2017 | Step count app | App use and step count uploads | Step counts were uploaded for an average of 48 (SD 19) out of the available 65 days (range of 10–65 days per participant). | 48/65 days =74%, 75% read posts Good adherence |
| Facebook group | Facebook posts | All participants (100%, n = 24) joined the Facebook group, with a total of 23 posts, of which 22 were posted by the moderator. Average of 20 views and 1.8 ‘likes’ per post. In total, 75% (n = 18) reported reading the weekly Facebook posts. |
||
| Bai 2015 | Professional‐guided online community | Not reported | Not reported | Not reported |
| Baker 2011 | Online discussion board | Not reported | Not reported | Not reported |
| Bantum 2014 | Web‐based program | Number of sessions attended Website posts |
Number of sessions ever attended (logged on at least once) was mean 5.3 (SD 1.28, range 0‐6) 67.0% (203/303) of participants attended all six sessions, and 86.8% (263/303) attended 4 or more. Average of 46 posts per participant over the six‐week intervention period (total of 8016 posts) |
87% attended 4 or more sessions Good adherence |
| Bender 2017 | Wearing Ftibit | 97% (21/22) wore Fitbit at least 5 days per week. | Good adherence | |
| Logging weight | 79% (17/22) logged weight a least once per week. | |||
| Logging food/calorie intake | 89% (20/22) logged food/calorie intake at least once per week. | |||
| Booth 2018 | Not reported | Not reported | Not reported | |
| Boyd 2019 | Session attendance | 100% (n=12) of mothers in the social media group attended at least one online session. Average attendance was 83%. | Good adherence | |
| Comments | Average participant commenting was 73%. | |||
| Bull 2012 | Loyal visitors on Just/Us | 93 individuals (10%) were “loyal” visitors who posted regularly to the page Total of 277 posts by visitors to the page during the study period. |
Low adherence | |
| Castillo 2013 | Website | Not reported | Not reported | Not reported |
| Cavalcanti 2019 | Not reported | Not reported | Not reported | |
| Cavallo 2012 | Posts | Intervention participants who posted more than once (n=37) had on average 8.0 Facebook interactions during the intervention. 81 (32%) interactions were to the discussion board and 130 (50%) were posts or responses to the group wall. |
Cannot assess adherence by number of posts | |
| Chai 2018 | WeChat messenger | Not reported | Not reported | Not reported |
| Chen 2019 | Not reported | Not reported | Not reported | |
| Cheung 2015 | Posts | Mean posts was 21.0 (SD 34.4) in the Facebook social groups. 58% (23/40) of the Facebook participants did not post any (median 0, IQR 2.3). Posts were sharing of smoking or quitting experiences (81/123 posts, 65.9%) and simple reply to the moderator’s inquiry (82/123 posts, 66.7%). |
Low adherence | |
| Posts | Mean number of posts was 55.0 (SD 50.7). The WhatsApp social groups had more moderators’ posts (median 60, IQR 25 vs median 31.5, IQR 7; P=.05) and participants’ posts than Facebook (median 35, IQR 50 vs median 6, IQR 9; P=.07). 23 of 42 (54.8%) WhatsApp participants posted 1 to 9 times in the social group (median 3, IQR 7). The majority of posts were sharing of smoking or quitting experiences (151/384 posts, 39.3%) and simple reply to the moderator’s inquiry (WhatsApp: 131/384 posts, 34.1%). |
|||
| Cobb 2014 | E‐mail‐, web‐, and mobile‐based intervention | Not reported | Not reported | Not reported |
| Coffeng 2014 | Social media platform | Not reported | Not reported | Not reported |
| Dadkhah 2014 | Not reported | Not reported | Not reported | |
| Dahl 2019 | Website and app | Group based interactions | The frequency of participant posts (daily on 5 of 7 days in a week) did not generate much discussion between members, except for one study team. | Cannot assess adherence by frequency of posts. |
| Daly 2017 | Not reported | Not reported | Not reported | |
| Dehlendorf | Online community | Logins | Participants had an average of 7.90 logins during the study period (SD 6.89), with number of logins ranging from 0–63. 59 participants (12.1%) never logged in. Number of logins and percentage of participants who never logged in were not differential by arm. | Cannot assess adherence by number of logins |
| Duncan 2014 | Interactive web site | Self‐monitoring entries | Median number of self‐monitoring entries per week at 3 months and 9 months was 1.00 (IQR 20.0) and 1.00 (IQR 21.5). The average number of self‐monitoring entries at 3 months and 9 months was 16.69 (SE 2.38) and 22.51 (SE 3.79), respectively. Following the initial reduction in usage between week 1 and week 3, usage continued to decline throughout the intervention period. No measure of usage of the IT‐based platform was associated with any of the behaviours examined. |
Cannot assess adherence based on median entries |
| “Mate” feature | 21 participants (10%) used the Mate feature. No participants using this feature had more than 1 mate. | |||
| Edney 2020 | App | Logging steps | Participants logged steps for an average of 72 (SD=35) out of 100 days in the gamified app. | 72/100 days of logged steps = 72%. 89/100 days of gamified usage = 89%. Good adherence |
| Usage | The gamified group used the additional gamified app features an average of 89 (SD=118) times during the 100‐day intervention. | |||
| Fiks 2017 | Facebook Posts | 100% of participants joined and posted in their assigned Facebook group. Group members posted a mean of 30 times per group per week, which is more than twice the rate of posting that we had defined as ‘‘active engagement’’ (an average of 2 posts/group/day, or 14/week). In regression analyses, individual participation was inversely associated with weight‐for‐length z‐score (P = 0.007), but not other parent or child characteristics. Participants were most active in the groups around the perinatal period. During the prenatal curriculum (7 weeks), there were 1953 participant posts across the 4 groups; then 1802 from 0 to 3 months postnatal, 1074 from 3 to 6 months, and from 6 to 9 months, when curriculum content was posted less frequently, there were 553. |
100% joined and posted in the group which met study authors' criteria for active engagement. Good adherence | |
| Posts | Conversations about feeding (63 total conversations across all groups; 31 were mother initiated and not moderator initiated), infant sleep (29 total, 9 mother initiated), infant activity (40 total, 12 mother initiated), and maternal well‐being (51 total, 19 mother initiated). | |||
| Glanz 2017 | Website and interactive web site | Usage | Over the study period, the interactive web site offered 59 blog entries and 31 chat sessions. Participants contributed 90 comments and questions but a majority of the interaction was between participants and the research team rather than between participants. | Cannot assess adherence by number of comments |
| Gnagnarella 2016 | Website | Participation – ‘social actions’ | Participants actively participated to the discussion forum, blog and content with 293 total social actions including 97 messages or comments. | Cannot assess adherence by 'social actions' |
| Godino 2016 | Engagement | Median (IQR) engagement with the intervention declined over time: 98 (9–265) interactions at 6 months, 76 (0–222) at 12 months, 41 (0–198) at 18 months, and 12 (0–161) at 24 months. Participants with high levels of engagement did not achieve greater weight loss than participants with low levels of engagement (P > 0·05 at all time points). |
Cannot assess adherence by interactions | |
| Graham 2018 | Online social network | Community use | The social networking feature increased community use by 15.3% (P < .001). In the arms receiving nicotine replacement therapy, the social network feature increased community use by a total of 14% points (P < .001). | Cannot assess adherence by community use |
| Graham 2011 | Interactive web site | Not reported | Not reported | Not reported |
| George 2013 | Not reported | Not reported | Not reported | |
| Greene 2013 | Online social network | Not reported | Not reported | Not reported |
| Hammersley 2019 | Module completion | At least 5 of the 6 modules were completed by 29 participants (69%). 26 participants (61.90%) completed all 6 modules. | Cannot assess adherence by module completion. | |
| Herring 2014 | Not reported | Not reported | Not reported | |
| Herring 2017 | Facebook posts | 11% of participants commented or “liked” posts, the average number of weekly coach posts was 1.7 ± 0.9, which waned over time. | Low adherence | |
| Horvath 2013 | Interactive web site | Intervention use | Participants updated their medication graph 3,935 times. | Cannot assess adherence by medication graph updates |
| Hutchesson 2018 | Web‐based (website, app, email, text messages and social media) | Website logins | 96.6% of participants (n = 28) logged‐on to the website. | Good adherence for logins to website |
| Webpage visits | Webpage visits was 52 ± 29, ranging from 0–135. Most participants (89.6%) accessed the website in the first week of the program, with the proportion logging‐in declining thereafter. | |||
| App usage | 58.6% participants used the Easy Diet Diary application to self‐monitor their food (164 ± 312 entries), exercise (6.7 ± 11.1 entries) and/or weight (1.1 ± 2.2 entries). Engagement with the app declined until around Week 10, where it appears a more consistent group of users was established with 10.3% of participants using the app for nine of the remaining weeks. | |||
| Opening email newsletters | On average, participants opened 10.0 ± 4.4 of the 19 email newsletters. | |||
| Reading text‐messages | 52.4% of participant reported reading text‐messages regularly. | |||
| Facebook posts | The mean number of posts by participants was 1.8 ± 2.5. | |||
| Facebook comments | The mean number of comments by participants was 12.4 ± 19.8. | |||
| Instagram likes | There were 54 ‘likes’ with a mean number of likes of 1.9 ± 4.7 per participant, with no comments made | |||
| Hwang 2013 | Online discussion forum | Forum messages | 60% of participants posted at least one message; 27 posted only one message. | Low adherence |
| Jane 2017 | N/A | N/A | Not reported | |
| Joseph 2015 | Not reported | Not reported | Not reported | |
| Kernot 2019 | Facebook and app | App visits | Participants visited the app on average 26 times (95% confidence interval [CI] = 21.5 to 30.5). | 48/50 days of logged steps = 96%. Good adherence. Cannot assess adherence for other outcomes. |
| Logging steps | Participants logged steps for 48/50 days (95% CI = 45.9 to 50.0) on average. | |||
| Wall posts | Mean number of posts on the group message wall was 9 (95% CI = 5.9 to 12.1). | |||
| Vitrual gifts | The mean number of virtual gifts sent to teammates was 7 (95% CI = 4.2 to 9.8). | |||
| Kim 2019 | Naver Band | Not reported | Not reported | Not reported |
| Kolt 2017 | Interactive web site | Average days with step comment per week | At 12‐18 months, interactive web site compared to basic web site: mean 0.03 (SD 0.15) vs. mean 0.06 (SD 0.39) | Cannot assess adherence based on days with comments |
| Koufopoulos 2016 | Online community | Comments or posts | Total of 861 comments or posts left by users on intervention web site. 33 of 82 participants (40%) posted something on the site that was not purely a preventer post (i.e. posts about symptoms, questions about asthma, answer or reply comments) and there were a mean 3.24 (SD 0.94) non‐preventer posts over the 9 weeks of the intervention. Eight of 82 participants (10%) explicitly asked questions of the community and tended to post more frequently (mean number of non‐preventer posts in this subgroup was 5.38, SD 3.50). |
Low adherence |
| Site adherence | 41.7% adherence in the control condition compared to 11.3% site adherence in the intervention condition at week 1. | |||
| Lau 2012 | Interactive web site | Not reported | Not reported | Not reported |
| Li 2017 | Tencent QQ | Posted three good things | 23.2% (n=23) posted their three good things messages <1 day/week on QQ, 31.3% (n=31) posted 1‐4 day/week, and 16.2% (n=16) posted ≥5 days/week. | Low adherence. |
| Reviewed posts by others | 31.3% (n=31) reviewed messages posted by other members <1 day/week, 32.3% (n=32) 1‐4 day/week, and 26.3% (n=29) ≥5 days/week. | |||
| Provided positive feedback | 67.7% (n=67) provided positive feedbacks to other group members during the intervention period (55.6% provided 1‐10/week and 12.1% provided >10/week). | |||
| Li 2020 | Not reported | Not reported | Not reported | |
| Liao 2020 | Participation in the discussion group | Overall, 58.1% (93/160) of the participants who joined the WhatsApp discussion groups participated in the online discussion, on average 3.08 posts (SD 5.90) per participant. A total of 434 posts from participants were retrieved over eight weeks, on average 13.6 posts per group per week. | Good adherence for reading the discussion posts. Low adherence for participation in discussion group. | |
| Reading discussion posts | Of the 117 participants of the intervention groups who completed the outcome assessment, 115 (98.3%) reported reading the discussion posts at least several times a week during the intervention period and 105 (89.7%) had read more than one half of all discussion posts | |||
| Linden 2017 | Web‐based support | Number of entries to the self‐care diary | Median (min.; max.): 1 (0; 5850) | Low adherence |
| Looyestyn 2018 | Facebook interaction | The mean total number of interactions with the Facebook group in response to posts was 34.7 (SD 40.7; median 15 [interquartile range 62.3]; range 0‐158). 11/41 (27%) participants had more than 50 interactions |
Cannot assess adherence by number of interactions | |
| Lytle 2017 | Social network web site. | Logins | 50%–60% of participants logged in at the beginning of the study and self‐monitored their weight at least once a month; by 24 months only about 30% were regularly logging their weight. | Low adherence |
| Maher 2015 | Logging steps | 28 (55%) logged steps for all 50 days of the program, 35 (69%) logged steps for 36 days or more. These steps were logged across a mean of 18 unique logins (SD 13.3, range 0‐46). |
Low adherence | |
| Discussion posts | Participants made a mean of 2.7 wall posts to their team discussion wall (SD 3.4, range 0‐13). | |||
| Mailey 2016 | Website discussion board and podcasts | Website engagement | Discussion board use was higher in the enhanced group throughout the 8‐week intervention. | Low adherence |
| Podcast engagement | 85% (n = 37) reported listening to the podcasts during weeks 1 and 2, compared to 55% during weeks 7 and 8. | |||
| Mascarenhas 2018 | Google Hangout | Session attendance | Women in the intervention arm (n=30) attended 2.8 (SD 1.17) group video sessions per week on average for over 8 weeks. Participants attended 3.3 sessions per week in the first half of the study and 2.4 sessions per week in the second half. | Cannot assess adherence by number of sessions attended per week. |
| Morris 2015 | Online social network | Overall engagement | Engagement was higher for the online social network group (mean 137.10, SD 20.93) than the control (expressive writing) (mean 122.29, SD 20.81). | Cannot assess adherence by number of posts. |
| Posts | Intervention group mean 2.72 (SD 2.76) compared to control mean 6.62 (SD 8.76) | |||
| Moy 2015 | Online social network | Online community forum | 83.8% of the participants (129/154) used the online community forum at some point during the 12‐month study; 66.2% (102/154) of participants directly viewed an online community forum thread or entry, and 17.5% (27/154) of participants posted a new topic or a reply at least once. | Low adherence (17.5% posted) |
| Moy 2010 | Interactive web site | Not reported | Not reported | Not reported |
| Nam 2015 | Tweets | Mean total tweets 79.66, relational tweets 47.48, self‐contained tweet 19.17, Twitter usability 4.06 (SD: 1.45) | Cannot assess adherence by number of tweets | |
| Nam 2020 | App | Not reported | Not reported | Not reported |
| Namkoong 2017 | Facebook use | 37/101 (36.6%) posted at least one campaign idea, 50/101 (49.5%) made comments, and 74 /101(73.3%) “liked” others’ posts during the 3 weeks of the intervention period. There was a total of 160 posts (M = 1.29, SD = 3.04), 1,015 comments (M = 10.05, SD = 30.85), and 9,046 “likes” (M = 89.56, SD = 217.87). |
Good adherence | |
| Napolitano 2013 | Facebook Plus | Likes | 22.2% (4/18) of the participants ‘‘liked’’ the study‐related posts on the Facebook group. These participants ‘‘liked’’ the post once throughout their programs | >70% posted or commented at least once. Good adherence |
| Posts | 77.8% (14/18) posted or commented on the study‐related content at least once. The average number of posts per person among those who posted or commented was 1.3 | |||
| RSVP | 72.2% (13/18) responded to the event invitations at least once during the program. The average number of RSVPs within those who responded was 8.56. | |||
| O’Neil 2016 | Interactive web site | Not reported | Not reported | Not reported |
| Owen 2015 | Interactive web site | Social networking component | Discussion board all users (n=296): mean 142.9 (SD 243) Personal pages all users (n=296): mean 132.4 (SD 243) Webmail all users (n=296): mean 1.8 (SD 6.2) |
Low adherence |
| Petrella 2017 | Online social network | Not reported | Not reported | Not reported |
| Ramo 2015 | Comments | 77% (n = 192) commented at least once to their Facebook group. Median commenting was 13 [interquartile range (IQR) = 1–66], and among those who commented at least once was 31 (IQR = 7–84); 101 participants (40.6%) commented at least once during a live counselling session. Groups with an incentive had higher comment volume than no‐incentive, and monthly and weekly incentives had the highest volumes (none: median = 5; IQR = 0–25; monthly: median = 30; IQR: 2–87; weekly: median = 31; IQR: 2–94; daily: median = 11; IQR = 1–50). | Good adherence | |
| Ramo 2018b | Comments | Among TSP participants, 77% (n = 192) commented at least once to their Facebook group. Median commenting among the full TSP sample was 13 [interquartile range (IQR) = 1–66], and among those who commented at least once was 31 (IQR = 7–84). Comments were greater among those in pre‐contemplation (median = 22; IQR = 3–82) and preparation (median = 23; IQR = 2–70) than contemplation (median = 7; IQR = 0–57). Groups with an incentive had higher comment volume than no‐incentive, and monthly and weekly incentives had the highest volumes (none: median = 5; IQR = 0–25; monthly: median = 30; IQR: 2–87; weekly: median = 31; IQR: 2–94; daily: median = 11; IQR = 1–50). | Good adherence | |
| CBT session attendance | Ten (15.9% of participants in preparation) participated in one or more CBT treatment sessions during the 90‐day intervention period. | |||
| Ren 2019 | Not reported | Not reported | Not reported | |
| Richardson 2010 | Online social network | Posts | 65% (165/254) of participants were using the online community, either as posters or “lurkers” (readers who did not post). | Low adherence |
| Step data | The group with access to the online community uploaded valid pedometer data on more days than the control group (87% compared to 75% of days). | |||
| Rote 2015 | Facebook posts | Total of 196 posts (range 6‐32 per participant). Average of 7.1 (SD 4.5) posts per participant) Week 1 – 46 posts, week 2 – 30 posts, week 8 – 13 posts |
Cannot assess adherence based on posts | |
| Rouf 2020 | Seeing and reading Facebook posts | On average, Facebook posts were seen by 19.9 (SD=3.6) for the Facebook only group and 26.9 (SD = 5.0) for the Facebook plus text group. 21.7% (n=10) and 45.5% (n=20) of participants reported reading the Facebook posts all the time for the Facebook group and Facebook plus text group, respectively. 37.0% (n=17) and 25% (n=11) reported reading the messages more than once a week for the Facebook group and Facebook plus text group, respectively. | Low adherence for reading Facebook posts all of the time. Cannot assess adherence for other outcomes. | |
| Facebook likes | On average, Facebook likes were 1.1 (SD 1.4) for the Facebook only group and 3.6 (2.4) for the Facebook plus text group. | |||
| Facebook comments | In the Facebook group, 3 participants made comments on posts (mean 0.1, SD 0.5), whereas 4 participants in the Facebook plus text group commented on posts (mean 0.2, SD 0.9). | |||
| Facebook sharing | No participants shared their own content in the Facebook group for the Facebook group only. However, 9% (n=4) participants in the Facebook plus text group shared their own content in the Facebook group. | |||
| Reading text messages | 79.5% (n=20) of participants reported reading the text messages for the Facebook plus text group all the time and 15.9% reported more than once per week. | |||
| Text replies | For the Facebook plus text group, the mean number of replies from participants was 3.8 out of a maximum 21 (range 1‐18). Of 75 participants, 12 made no reply texts. The highest number of replies was to the yes/no response as to whether they had set a goal on the app (n=22). | |||
| Rovniak 2016 | Online social network | Engagement | Participants in the social network group performed a mean of 3.9 (SD = 2.6) of the 12 social networking activities targeted over the 12‐week intervention. Between the 3‐ and 9‐month assessments, 8.7 % of participants posted a discussion comment on the study’s online networking site; no other online networking activities were observed. | Low adherence |
| Schaller 2017 | Online social network | Not reported | Not reported | Not reported |
| Schneider 2015 | Online social network | Comments | 42.9% reported that they never commented on the Meetup web site. | Low adherence |
| Step uploads | 39.3% of participants reporting that they used activity monitoring 5 times or less and 35.7% reporting daily or almost daily use; 60.7% of participants reported that they never recorded their steps on the web site | |||
| Stoddard 2008 | Online social network | Time on Website | The average number of minutes spent for either condition was 14.4 minutes (n = 1083). Time on the web site was higher for those assigned to the social network condition (min 18.0, number 526) versus the control (min 11.1, number 557), those who reported abstinence (vs still smoking), and those who made a serious quit attempt by abstaining for at least 24 hours (vs those who did not). The longest time spent on the web site (30 minutes) was for those whose quit attempt began in the 5 days prior to registering for the study. | Low adherence |
| Bulletin Board Use | Only 242 opted to look at the Bulletin Board feature by clicking on the link, and of those visiting the link, 81/242 either selected an individual message to view or posted a message. This low utilization rate 81/684 (11.8%) limited our ability to analyse the impact of bulletin board use on cessation. | |||
| Sun 2017 | Facebook use | 159 Facebook interactions were recorded among 96 users. During the 6‐week intervention period, there were 144 “likes,” 13 comments, and 2 participant‐initiated posts. The posts on the Facebook group were viewed, on average, by 77% (74/96) of participants. |
Cannot assess adherence by views | |
| Turner‐McGrievy 2011 | Twitter and podcasts | Twitter posts | 94% (n = 44) posted at least once to Twitter and 64% (n = 30) posted at least weekly during the first 3 months and 28% (n = 13) posted weekly or more during months 3–6. Participants made a mean of 2.1 (SD 3.1) posts to Twitter per week, with significantly more posts being made in the first 3 months (2.8, SD 3.6 posts/week) than in months 3–6 (1.3, SD 3.0 posts/week; P < .001). |
Good adherence |
| Podcasts | Mean number of podcasts downloaded at 0–3 months podcast only group: 14.5 (7.6) or podcasts plus Twitter 16.4 (7.2), at 3–6 months podcast only: 8.2 (8.6), podcast plus Twitter: 9.0 (9.1) P‐value.67 Number of downloads per podcast episode per person at 0–3 months podcast only: 1.51 (0.65), podcast plus Twitter 2.00 (0.52), at 3–6 months podcast only: 0.66 (0.15), podcast plus Twitter: 0.87 (0.20) |
|||
| Valle 2013 | Facebook posts | Participants posted a total of 153 Facebook comments to the group wall over 12 weeks compared with 188 comments by control group participants. There was no difference in mean number of posts over the 12‐week program (intervention=3.4 (4.6) vs. control=4.6 (7.8), and almost half of participants in both groups made two or more Facebook posts over the course of the study period (intervention, 48.9 % (n=22); control, 48.8 % (n=20)) | 62.5% of the intervention group Low adherence |
|
| Vandelanotte 2017 | Interactive web site | Not reported | Not reported | Not reported |
| Vogel 2019 | Comment volume | Comment volume mean (SD) for the SGM‐tailored group (POP) was 60.2 (SD 41.0) and 78.4 (SD 35.1) for the TSP‐SGM group. On average, TSP‐SGM participants responded to posts with significantly more comments throughout the intervention than did POP participants. | Cannot assess frequency by mean volume of comments | |
| Wan 2017 | Online social support | Not reported | Not reported | Not reported |
| Wang 2015 | Not reported | Not reported | Not reported | |
| Washington 2017 | Not reported | Not reported | Not reported | |
| Willcox 2017 | Facebook and interactive web site | Facebook Page | Fourteen participants (31%) joined the private Facebook page. These women recorded 558 views, a mean of 40 per participant, submitted seven posts and two questions, and indicated 18 likes. | Low adherence |
| Willis 2017 | Online social network | Likes | The average number of ‘likes’ per person each week was 1.3 on study‐related posts and posts by a peer. | Cannot assess adherence by number of likes/comments |
| Comments | The average number of comments per person each week was 3.2 | |||
| Yang 2019 | Number of mindfulness sessions | The mean (SD) number of mindfulness meditations per week was 3.25 (1.45) times over the 8‐week intervention. | Cannot assess adherence by frequency or minutes of mediations per week. | |
| Minutes spent on meditation | The mean (SD) number of minutes spent on meditation each time was 21.23 (16.16) minutes. | |||
| Young 2013 | Messages | Participants who responded to messages during period 1: intervention 54/57 (94.7%), control 38/55 (69.1%) Period 2: intervention 52/57 (91.2%), control 34/55 (61.8%) Period 3: intervention 44/57 (77.2%), control 30/55 (54.5%) |
Good adherence | |
| Wall posts | Participants who responded to wall posts during period 1: intervention 39/57 (68.4%), control 40/55 (72.7%) Period 2: intervention 26/57 (45.6%), control 34/55 (61.8%) Period 3: intervention 27/57 (47.4%), control 28/55 (50.9%) |
|||
| Chat | Participants who responded to chat during period 1: intervention 43/57 (75.4%), control 14/55 (25.5%) Period 2: intervention 41/57 (71.9%), control 11/55 (20.0%) Period 3: intervention 36/57 (63.2%), control 11/55 (20.0%) |
|||
| Young 2015 | Not reported | Not reported | Not reported | |
| Zhang 2016 | Online social network | Website Engagement | Average of 22.8 logins (SD = 47.2) across all conditions during the program. Participants in the social support condition generated 81 online messages and participants in the combined condition generated 80 messages. | Cannot assess adherence by number of logins |
Dietary behaviour
Eight studies (n = 1240) assessed mean changes to self‐reported diet quality using various scales, such as the Australian Eating Survey or daily consumption of fruits and vegetables. The combined data from these studies indicates that there may be little to no difference in effect for those receiving an interactive social media intervention (SMD 0.11, 95% CI ‐0.25 to 0.47, substantial heterogeneity (I2 = 86%), low‐certainty evidence, small effect) (Analysis 1.2). Re‐expressed using weekly consumption of fruits and vegetables, this represents an increase of 0.35 servings (from 1.25 fewer servings to 1.96 more servings per week).
1.2. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 2: Health behaviours ‐ diet quality
Disaggregated by outcome type
Three studies n = 131) assessed mean changes in caloric intake and found that there is probably little to no difference in effect for those who received the interactive social media intervention (MD ‐53.75, 95% CI ‐152.48 to 44.97), no important heterogeneity (I2=0%), moderate‐certainty evidence). These studies used food diaries to assess daily consumption of calories (Analysis 1.3).
1.3. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 3: Health behaviours ‐ calorie intake
One study (n = 209) found that interactive social media may improve calcium intake (RR 1.97, 95% CI 1.31 to 2.98) (Analysis 1.4). Another study n = 73) found that social media may improve infant feeding style (MD 0.75, 95% CI 0.32 to 1.18; low‐certainty evidence) assessed using the Infant Feeding Style Questionnaire (Analysis 1.5).
1.4. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 4: Health behaviour ‐ increased calcium intake
1.5. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 5: Health behaviours ‐ healthy infant feeding behaviour score
Breastfeeding
One study (n = 251) assessed breastfeeding and found that interactive social media improves breastfeeding (RR 3.95, 95% CI 2.06, 7.58) (Analysis 1.6).
1.6. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 6: Health behaviours ‐ breastfeeding
Tobacco use
Four studies (n = 2433) compared an interactive social media intervention to a non‐interactive social media intervention and aimed to increase smoking cessation. The pooled effect indicates that there is probably a reduction in tobacco use but the results are uncertain (RR 0.98, 95% CI 0.74, 1.29, no important heterogeneity (I2 = 0%), moderate‐certainty evidence) (Analysis 1.7).
1.7. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 7: Health behaviours ‐ tobacco use
Condom use
Two studies (n = 848) assessed condom use. The combined effect size for these studies indicates that there may be little to no difference (SMD 0.22, 95% CI ‐0.33 to 0.76; substantial heterogeneity (I2 = 81%), low‐certainty evidence, small effect) (Analysis 1.8). This represents an increased frequency of 0.34 higher on a scale of 1 (never) to 5 (always) (from 0.51 fewer to 1.17 more). Both of these studies included general populations, such as college students.
1.8. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 8: Health behaviours ‐ condom use frequency
Screening, medication use, vaccination uptake
Finally, eight studies assessed interventions aimed at increasing uptake of screening, medication, or vaccination programs. These included HIV testing, colorectal cancer screening, medication adherence, and influenza vaccine uptake. Overall, the results indicate a small positive effect but the result is uncertain (SMD 0.11, 95% CI ‐0.07 to 0.30, no important heterogeneity (I2 = 0%), moderate‐certainty evidence, small effect) (See Table 2).
Disaggregated by outcome type
Three studies assessed interventions to improve medication adherence (for ADHD, asthma, and HIV) and found little to no difference for those receiving an interactive social media intervention (SMD 0.11, 95% CI ‐0.24 to 0.46, moderate heterogeneity (I2=42%), moderate‐certainty evidence). This represents a mean uptake of 2.08% higher in the social media group (from 1.32% lower to 5.62% higher) (Analysis 1.9).
1.9. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 9: Health behaviours ‐ Medication adherence
Two studies found that interactive social media may increase vaccination uptake (SMD 0.38, 95% CI ‐0.25 to 1.00, no important heterogeneity (I2= 0%)) but the result is uncertain (Analysis 1.10). This represents an increase in vaccination uptake by 1.5% for the social media group (from 1.1% to 3.2% more). Similarly, one study (Liao 2020) assessed seasonal influenza vaccine uptake and found that a What's App intervention may improve uptake but the evidence is uncertain (RR 1.12, 95%CI 0.84 to 1.49) (Analysis 1.11).
1.10. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 10: Health behaviours ‐ Vaccination (frequency)
1.11. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 11: Health behaviours ‐ vaccination uptake
Finally, four studies assessed screening uptake (for colorectal screening, and HIV testing) and found that interactive social media probably improves screening rates (RR 1.64, 95% CI (1.21 to 2.24), no important heterogeneity (I2=10%)) (Analysis 1.12).
1.12. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 12: Health behaviours ‐ screening test
Self care
Two studies (n = 186) assessed self‐care behaviours (for diabetes and haemodialysis) and found that interactive social media probably has no effect in improving self‐care (SMD 0.06, 95 % CI ‐0.55 to 0.67, moderate heterogeneity (I2 = 77%), small effect), but the evidence is uncertain (Analysis 1.13).
1.13. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 13: Health behaviours ‐ self‐care
Other health behaviours
Mindfulness was assessed by one study (n = 77) using the Five‐Facet Mindfulness Questionnaire‐Short Form. This study reported that interactive social media interventions may improve mindfulness scores (MD 7.60, 95% CI 4.57 to 10.63) (Analysis 1.14).
1.14. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 14: Health behaviours ‐ mindfulness
One study (n = 78) assessed found that interactive social media interventions may improve parent role‐modelling of healthy eating (MD 0.17, 95% CI 0.01 to 0.33) (Analysis 1.15).
1.15. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 15: Health behaviours ‐ parent modeling of healthy eating
One study (n = 1039) found that interactive social media may improve maternal health care utilisation (RR 1.12, 95% CI 1.06 to 1.19) (Analysis 1.16).
1.16. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 16: Health behaviours ‐ maternal care utilisation
Controlled before‐and‐after (CBAs) studies
Tobacco
Additionally, one CBA study found that social media interventions may increase the smoking rate (SMD 0.47, 95% CI ‐0.14 to 1.08) (Chai 2018) (Analysis 1.17).
1.17. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 17: Health behaviours, CBA
Interrupted time series (ITS) study
Primary and psychiatric care visits
We included one ITS study that assessed monthly mental health visits for young adults 18‐24 years old following a Twitter campaign aimed at increasing dialogue about mental health. The campaign was initiated in 2012 and data from 2006 to 2016 were available. The slope change (change in the rate of visits between the two time periods) for new primary health care visits for females was 0.04 (95% CI 0.02 to 0.08) and 0.01 (95% CI 0.002 to 0.03) for males (Booth 2018). The level change (change in magnitude of visits) was ‐0.49 for females and ‐0.41 for males. For new psychiatric service visits, there was no slope change for females or males. The level change was 0.005 for females and ‐0.01 for males.
Body function outcomes
We included 29 studies which assessed body functions.
Weight
The pooled data for 16 studies (n = 1963) assessing weight indicate that interactive social media interventions may lead to greater mean weight loss (MD ‐1.33 kilograms, 95% CI ‐2.00 to ‐0.67, substantial heterogeneity, I2 = 76%, low‐certainty evidence) (Analysis 1.18).
1.18. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 18: Body functions ‐ Weight (kg)
We conducted planned subgroup analyses for different population groups and found no subgroup differences for studies of the general population or studies of those with or at risk of a condition (Chi² = 0.16, P = 0.69, I² = 0%). Studies that included general populations found that interactive social media interventions may lead to greater mean weight loss (MD ‐1.78 kg, 95% CI ‐2.78 to ‐0.78, no important heterogeneity (I2=19%)) (Analysis 3.2). Similarly, studies that targeted participants with a condition or at‐risk of a condition found that interactive social media interventions lead to greater mean weight loss (MD ‐1.48 kg, 95% CI ‐2.53 to ‐0.43, substantial heterogeneity (I2 = 74%)).
3.2. Analysis.

Comparison 3: Subgroup by population ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 2: Body function ‐ Weight
We also conducted a planned subgroup analyses by intervention type and found no subgroup differences (Analysis 4.3). We included five studies which assessed the effect of interactive social media alone on mean weight loss and 11 studies which included social media within a multi‐component intervention and found no subgroup differences (Chi² = 1.49, P = 0.22, I² = 33.1%).
4.3. Analysis.

Comparison 4: Subgroup by outcome type and intervention type ‐ Interactive social media intervention compared to non‐interactive social media control, Outcome 3: Weight (kg)
We explored heterogeneity using planned sensitivity analyses. When only studies in which participants had good adherence to the interactive social media intervention were included in the meta‐analysis the results were similar to the main analysis and suggest that interactive social media may lead to mean weight loss (MD ‐1.07 kg, 95% CI ‐1.93 to ‐0.21, no important heterogeneity (I2=0%)) (Analysis 5.4). Similarly, when only those studies in which there was low risk of bias for allocation concealment, interactive social media probably leads to mean weight loss (MD ‐1.77 kg, 95% CI ‐2.66 to ‐0.88 substantial heterogeneity (I2=81%)) (Analysis 5.5).
5.4. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 4: Body function ‐ weight, Good adherence
5.5. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 5: Body function ‐ weight, Low ROB for allocation concealment
Gestational weight gain
One study assessed differences in gestational weight and found that interactive social media may leader to less weight gain but the results are uncertain (MD ‐3.50 kg, 95% CI ‐7.07 to 0.07) (Analysis 1.19).
1.19. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 19: Body functions ‐ gestational weight gain
BMI
The pooled data from four studies found social media interventions may reduce BMI (MD ‐0.51 kg/m2, 95% CI ‐0.92 to ‐0.10, considerable heterogeneity (I2=92%), low‐certainty evidence) (Analysis 1.20).
1.20. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 20: Body functions ‐ BMI kg/m2
Blood glucose
We included four studies (n = 773) reporting on blood glucose levels. The combined data for these studies indicates that interactive social media interventions may reduce HbA1c levels (MD ‐1.74, 95% CI ‐2.79 to ‐0.68, considerable heterogeneity (I2 = 93%), low‐certainty evidence) (Analysis 1.21).
1.21. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 21: Body Functions ‐ Blood glucose mmol/L
Other body function outcomes
Other body function outcomes were reported by single studies and found varying effects ranging from small but important benefits for improving insomnia scores (MD ‐0.90, 95% CI ‐1.24 to ‐0.56), premenstrual syndrome (PMS) score (MD ‐54.59, 95% CI ‐70.43 to ‐38.75) and reducing flu‐like illness (MD 1.10, 95% CI 0.85 to 1.41), and small but important benefits for which the evidence is uncertain (cardiorespiratory fitness (MD ‐2.50, 95% CI ‐6.17 to 1.17), dyspnoea (MD ‐0.20, 95% CI ‐3.10 to 2.70) (Analysis 1.22; Analysis 1.23; Analysis 1.24 ; Analysis 1.25 ; Analysis 1.26).
1.22. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 22: Body functions ‐ Insomnia
1.23. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 23: Body functions ‐ PMS Score
1.24. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 24: Body function ‐ Dyspnoea
1.25. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 25: Body functions ‐ Cardiorespiratory fitness (heart beats/min)
1.26. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 26: Body function ‐ Influenza‐like illness
Controlled before‐and‐after (CBAs) studies
Physical health status
One CBA (n = 190) assessed changes in physical health status scores (using the SF‐12 scale) and found a small positive effect for the interactive social media group (MD 1.40, 95% CI ‐2.13 to 4.93) but the evidence is uncertain (Analysis 1.27).
1.27. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 27: Body Function outcomes ‐ physical health status, CBA
Well‐being
Seventeen studies assessed well‐being and quality of life and the combined data for these studies found that interactive social media interventions may improve well‐being (SMD 0.37, 95% CI 0.00 to 0.73, substantial heterogeneity (I2 = 96%), low‐certainty evidence, moderate effect) (Analysis 1.28). This represents a mean difference in well‐being score, using the Quality of Life Enjoyment and Satisfaction Questionnaire, that is 3.77 points higher (from 1.15 lower to 6.48 points higher) for the social media group (14 points is the minimum and 70 points is the maximum score).
1.28. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 28: Well‐being outcomes
Twelve of these studies assessed mean changes in quality of life scores. The combined data for these studies found that participants who received interactive social media interventions probably experience improved quality of life (SMD 0.50, 95% CI 0.16 to 0.83, substantial heterogeneity (I2=89%), moderate effect). These studies included a mix of patients with or at‐risk of conditions, such as cancer patients, those with COPD/emphysema/bronchitis, or overweight or obese adults.
When we considered the populations of these studies, we found no subgroup differences (Chi² = 0.16, P = 0.69, I² = 0%) for general populations or those with or at‐risk of a condition (Analysis 3.3).
3.3. Analysis.

Comparison 3: Subgroup by population ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 3: Well‐being
For these 12 studies, we also conducted a planned subgroup analysis by outcome type and found no subgroup difference for studies in which interactive social media was provided alone or as a component of a multi‐component intervention (Chi² = 1.36, P = 0.24, I² = 26.3%) (Analysis 4.4).
4.4. Analysis.

Comparison 4: Subgroup by outcome type and intervention type ‐ Interactive social media intervention compared to non‐interactive social media control, Outcome 4: Quality of Life score
We explored heterogeneity with planned sensitivity analyses. When we only combined data from studies with good adherence to the social media intervention, we found that the result was similar to the main findings; interactive social media interventions probably improves well‐being (SMD 0.33, 95% CI 0.07 to 0.59, moderate heterogeneity (I2 = 37%), small effect) (Analysis 5.7). Similarly, for studies with low risk of bias for allocation concealment, we found that interactive social media interventions may improve well‐being (SMD 0.25, 95% CI ‐0.09 to 0.59, substantial heterogeneity (I2=81%), small effect) (Analysis 5.8).
5.7. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 7: Well‐being ‐ Good adherence
5.8. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 8: Well‐being ‐ Low ROB for allocation concealment
Psychological outcomes
Twelve studies assessed psychological outcomes. These studies found that there may be little to no difference in depression or distress scores (SMD, ‐0.15, 95% CI ‐0.38 to 0.08, substantial heterogeneity (I2 = 79%), low‐certainty evidence) (Analysis 1.29). This represents mean difference in Beck's Depression Scale score of 0.1 points higher (from 1.23 lower to 1.06 higher) for the social media group.
1.29. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 29: Psychological outcomes
There were no subgroup differences by population (Chi² = 0.55, P = 0.46, I² = 0%) (Analysis 3.4). These studies included general populations (SMD ‐0.25, 95% CI ‐0.67 to 0.16, substantial heterogeneity, I2 = 84%) and those with or at‐risk of a condition, such as cancer, COPD/emphysema/chronic bronchitis, diabetes, or overweight or obesity (SMD ‐0.05, 95% CI ‐0.38 to 0.27, substantial heterogeneity, I2=80%).
3.4. Analysis.

Comparison 3: Subgroup by population ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 4: Psychological outcomes
Two additional studies (one RCT and one CBA) also measured psychological outcomes but could not be combined in the main analysis, although the results were comparable (Analysis 1.30; Analysis 1.31).
1.30. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 30: Psychological outcomes ‐ probable depression
1.31. Analysis.

Comparison 1: Overall ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 31: Psychological outcomes ‐ CBA
Adverse events
None of our included studies reported on adverse events related to the social media components of the interventions, such as online harassment and privacy issues.
Six studies assessed possible adverse effects of the intervention. Five studies reported adverse events linked to the physical activity programs that the social media components were supporting.
Looyestyn and colleagues reported that five participants (two from the intervention group and three from the control group) reported musculoskeletal injuries (Looyestyn 2018).
Moy and colleagues reported that all serious adverse events were unrelated to the research (two deaths in the intervention group) (Moy 2015). There were 41 musculoskeletal events in the intervention group and three in the control group. There were also six pulmonary, three cardiac and five ‘other’ (e.g. falls, foot blisters) adverse events in the intervention group and one pulmonary, one cardiac, and three ‘others’ in the control group. In addition, there were nine COPD‐related events.
There were no serious adverse events reported by the participants of the study by Petrella and colleagues (Petrella 2017). Most adverse events were musculoskeletal (11 of 12), two of which were considered to be related to the intervention. Only one adverse event was experienced by a participant of the control group.
In the study by Schneider and colleagues there were 19 adverse events (five in the intervention group and 14 in the control group), and 15 were considered to be related to the dog‐walking the intervention (Schneider 2015). No additional details were provided.
Wan and colleagues reported that there were 24 serious adverse events reported by 17 participants (eight in the control group, nine in the intervention group). (Wan 2017) These adverse events included abdominal pain, anxiety, mental health crisis, headache, congestion, ear pain, rash, skin abscess, kidney problems, broken toe. There were 24 pulmonary adverse events reported by eight control and 13 intervention participants. None of these were considered to be related to the intervention.
Secondary outcomes
We have grouped all secondary outcomes by broad category and have also presented disaggregated data by target health behaviour.
Knowledge
Changes in knowledge scores were assessed in nine RCTs and one CBA study. The combined data from nine RCTs (n = 908) found that interactive social media had a positive effect, but the results are uncertain (SMD 0.90, 95% CI 0.22 to 1.58; considerable heterogeneity (I2= 95%); large effect) (Analysis 6.1).
6.1. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 1: Change in knowledge
For the CBA, there was positive effect but the results are uncertain (MD 0.86, 95% CI ‐2.56 to 4.28) (Analysis 6.2).
6.2. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 2: Knowledge (CBA)
The topics for which changes in knowledge were assessed included exercise, ADHD, food safety, haemodialysis, nutrition and weight/physical activity, tobacco, chronic obstructive pulmonary disease (COPD), diabetes, and colorectal cancer.
Attitudes
Changes in attitude were assessed by three RCTs and one CBA. The combined RCT data found a small negative effect but the results are uncertain (SMD ‐0.11, 95% CI ‐0.48 to 0.26, substantial heterogeneity (I2=66%), small effect) (Analysis 6.3). Similarly, one CBA study assessed attitude and a small positive effect, but the results are uncertain (MD 1.10, 95% CI ‐3.38 to 5.58) (Analysis 6.4).
6.3. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 3: Change in attitude
6.4. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 4: Change in attitude (CBA) ‐ Tobacco attitudes
Our included studies assessed attitudes related to condom use, exercise, medication, food safety, and tobacco.
Self‐efficacy
Data on changes in self‐efficacy were extracted for 14 RCTs (n = 2349) . The combined data found a small positive effect on self‐efficacy, but the results are uncertain (SMD 0.10, 95% CI ‐0.13 to 0.34, substantial heterogeneity (I2 = 85%)) (Analysis 6.5).
6.5. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 5: Change in self‐efficacy
Self‐efficacy for a variety of health behaviours was assessed in our included studies, such as physical activity and nutrition, exercise, diabetes care, condom use, smoking, medication adherence, weight loss, hypertension, patient activation, and cancer‐related self ‐ efficacy.
One CBA (n = 190) assessed changes in general self‐efficacy and found little to no difference for between the groups (MD 0.18, 95% CI ‐0.10 to 0.47) (Analysis 6.6).
6.6. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 6: Change in self‐efficacy (CBA) ‐ general self‐efficacy
Norms
Two studies (n = 893) that assessed changes in subjective norms also found a small positive effect but the results are uncertain (SMD 1.12, 95% CI ‐1.40 to 3.64; considerable heterogeneity I2 = 99%). (Analysis 6.7) These studies assessed changes in subjective norms for medication and condom use .
6.7. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 7: Change in subjective norms
Perceived control
One study (n = 89) assessed changes in perceived direct control and found that participants in the social media arm had higher control than the control group (MD 8.00, 95% CI 6.72, 9.28) (Analysis 6.8). One CBA study also assessed changes in direct control and found that there was a small positive effect for the comparator but the results are uncertain (MD ‐0.09, 95% CI ‐0.43 to 0.24) (Analysis 6.9).
6.8. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 8: Change in direct control
6.9. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 9: Change in direct control (CBA) ‐ exercise
Changes in direct control focused on medication behaviour and exercise.
Intention and motivation
Four studies assessed changes in intention. The combined data from three (n = 1087) indicate that the participants in the interactive social media intervention groups reported greater intention (SMD 1.00, 95% CI 0.04 to 1.96), which represents a small effect size with considerable heterogeneity (I2 = 97%) (Analysis 6.10). Two studies assessed changes in contraceptive use intention and one study focused on medication adherence intention. The fourth study (n = 291) assessed changes in intention to vaccinate children for seasonal influenza and found a small positive effect for those in the intervention group (RR 1.24, 95% CI 0.95 to 1.62) (Analysis 6.11).
6.10. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 10: Change in intention
6.11. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 11: Intention to vaccinate children
Two studies (n = 318) assessed changes in motivation and found little to no difference between the social media intervention group and the control (SMD ‐0.01, 95% CI ‐0.24 to 0.22) (Analysis 6.12).
6.12. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 12: Change in motivation
Two studies (n = 823) assessed likelihood of higher motivation. The combined data from these studies found little to no difference between intervention and control groups (RR 0.98, 95% CI 0.90, 1.06; no important heterogeneity, I2= 0%)) (Analysis 6.13). These studies assessed motivation to quit smoking and motivation for colorectal cancer screening.
6.13. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 13: Change in motivation (higher motivation)
Susceptibility
One study (n = 258) found that the control group had greater increases in perceived susceptibility to colorectal cancer compared to the group receiving the interactive social mediaintervention (SMD ‐0.09, 95% CI ‐0.17 to ‐0.01) (Hwang 2013) (Analysis 6.14).
6.14. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 14: Change in perceived susceptibility ‐ colorectal cancer
Social support
We extracted data from seven studies (n = 875) that assessed changes in perceived social support. The combined data indicate a small positive effect but the results are uncertain (SMD0.15, 95% CI ‐0.04 to 0.35). This represents a small effect size and moderate heterogeneity (I2= 48%) (Analysis 6.15). Our included studies assessed changes in social support in general or specific to physicalactivity, colorectal cancer screening, or cancer.
6.15. Analysis.

Comparison 6: Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media, Outcome 15: Change in social support
Comparison 2: Social media intervention compared to an active comparator
Health behaviours
Physical activity
Four studies (n = 1523) assessed mean changes in physical activity for studies which compared one form of interactive social media intervention to another, for example, comparing Facebook groups with moderated versus unmoderated discussions or an interactive social media intervention and an enhanced version of the same intervention with additional interactive features. The combined data found that social media may increase physical activity but the evidence is very uncertain (SMD 0.35, 95% CI 0.12 to 0.59, moderate heterogeneity (I2=40%), very low‐certainty evidence, small effect) (Analysis 7.1).
7.1. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 1: Health behaviours ‐ Physical activity
Healthy eating
One study compared an intervention aimed at healthy eating and physical activity using a website and app to the same intervention aimed at stress reduction and management assessed changes and found that the intervention may improve healthy eating scores (MD 1.40 95% CI 1.21 to 1.59) (Analysis 7.2).
7.2. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 2: Health behaviours ‐ healthy eating
IUD use
One study (n = 87) assessed intrauterine device (IUD) use for those in a social media group with IUD and non‐IUD users to non‐IUD users only and found that the intervention resulted in little to no difference (RR 0.88, 95% CI 0.16 to 4.75) (Analysis 7.3).
7.3. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 3: Health behaviours ‐ IUD use
Tobacco use
Two studies compared social media interventions and their effect on tobacco use. These two studies used similar interventions in which the intervention group received access to a Facebook and live group chats but Ramo 2018b compared the intervention to a quit smoking website and Vogel 2019 compared a culturally tailored intervention to the intervention assessed by Ramo. The combined data from these studies found that the more interactive social media intervention had little to no difference in smoking rates (RR 0.98, 95% CI 0.90 to1.07, substantial heterogeneity (I2 = 71%)) (Analysis 7.4).
7.4. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 4: Health behaviours ‐ tobacco use
Mindfulness
One study (n= 123) compared a WeChat‐based mindfulness intervention to WeChat group without the mindfulness component and found that there may be little to no difference in mindfulness behaviours (MD 0.52, 95 % CI ‐1.18 to 2.22) for those receiving the intervention, but the evidence is uncertain (Yang 2019) (Analysis 7.5).
7.5. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 5: Health behaviours ‐ mindfulness
Weight
Valle 2013 (n = 66) assessed changes in weight and found that more interactive social media may lead to greater weight loss compared to a less interactive social media intervention but the results are very uncertain (MD ‐4.70 kg, 95% CI ‐8.31 to ‐1.09, very low certainty) (Analysis 7.6). Vandelanotte 2017 (n ‐ 1328) assessed BMI and also found that more interactive social media interventions may lead to reduction in BMI (MD ‐1.20 kg/m2, 95% CI ‐1.41 to ‐0.99, low‐certainty evidence). Dahl 2019 (n = 87) assessed maternal weight gain and found little to no difference but the evidence is uncertain (MD 0.94 kg, 95% CI ‐2.36 to 4.24) (Analysis 7.7).
7.6. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 6: Body function outcomes
7.7. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 7: Body function ‐ total gestational weight gain (kg)
Well‐being
One study found there may be little to no difference for well‐being scores for participants receiving interactive social media (MD ‐2.00, 95% CI ‐5.10 to 1.10) and another found there may be an improvement in quality of life scores but the evidence is uncertain (MD 0.70, 95% CI‐1.37 to 2.77, low certainty) (Analysis 7.8).
7.8. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 8: Well‐being
Psychological outcomes
One study assessed self‐worth and found that participants in the interactive social media arm had worse self‐worth scores than the control group (MD ‐1.22, 95% CI ‐2.25 to ‐0.19) (Analysis 7.9). The study by Yang 2019 (n = 123) found that the mindfulness‐based WeChat intervention may improve depression and anxiety symptoms more than a WeChat group without mindfulness training but the evidence is uncertain (MD ‐2.94, 95% CI ‐3.39 to ‐2.49 (Analysis 7.10), and MD‐2.62, 95% CI ‐3.04 to ‐2.20 (Analysis 7.11), respectively).
7.9. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 9: Psychological outcomes ‐ Self‐worth
7.10. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 10: Psychological outcomes ‐ depression
7.11. Analysis.

Comparison 7: Overall ‐ Any interactive social media intervention compared to active social media comparator, Outcome 11: Pyschological outcomes ‐ anxiety
Adverse Events
None of the studies in this comparison reported on adverse events.
Secondary outcomes
Knowledge
None of the studies in this comparison reported on knowledge.
Attitudes
None of the studies in this comparison reported on attitudes.
Self efficacy
Data on changes in exercise self‐efficacy were extracted for two RCTs (n = 123) and the combined data indicates a small negative effect but the results are uncertain (SMD ‐0.05, 95%CI ‐0.52 to 0.42). This represents a small effect size with no important heterogeneity (I2=0%) (Analysis 8.1).
8.1. Analysis.

Comparison 8: Secondary Outcomes ‐ Interactive social media vs. active social media comparator, Outcome 1: Change in exercise self‐efficacy
Norms
No studies with this comparison assessed changes in norms.
Perceived control
None of our included studies with this comparison assessed changes this outcome.
Intention
None of the studies in this comparison assessed this outcome.
Susceptibility
None of the studies in this comparison assessed susceptibility.
Social support
One study (n = 86) assessed changes in physical activity social support and found a small effect favouring the active comparator but the results are uncertain (MD ‐1.16, 95% CI ‐3.55 to 1.23) (Analysis 8.2).
8.2. Analysis.

Comparison 8: Secondary Outcomes ‐ Interactive social media vs. active social media comparator, Outcome 2: Change in physical activity social support
Adherence
We aimed to assess adherence to the interactive social media intervention. However, adherence to the social media intervention was often reported in terms of engagement with social media (e.g. Facebook posts) with few studies reporting outcomes such as step count uploads which are a more accurate measure of adherence to the behaviour change. We have summarised these outcomes as reported by the study authors in Table 11 . We classified 16 studies as achieving good adherence based on the authors' reports of adherence or engagement with the social media components of the intervention.
Equity
Only four of our included studies reported on the effects of the intervention on health equity.
Castillo and colleagues conducted a regression analysis for Patient Health Questionnaire scores and male sex and found no important difference with or without controlling for baseline social support scores (Castillo 2013). Greene and colleagues conducted regression analyses of online activity, physical activity, and participants characteristics, including gender, age, and obesity. The authors reported that none of these characteristics were related to changes in walking or weight (Greene 2013). The study by Liao and colleagues assessed whether seasonal influenza vaccination uptake differs by participants' educational attainment, income, and work status (full‐time and part‐time/unemployed). The authors reported that vaccination update may be greater among participants with a full‐time job suggesting that work status could be an effect modifier (Liao 2020).
Finally, Schaller and colleagues conducted subgroup analyses to assess potential differences related to age, gender, or highest level of education and found no important differences(Schaller 2017). Other studies reported on the demographics of study participants but did not explore differential effectiveness of the intervention.
Funnel of attrition analysis
We were unable to analyse our results according to our funnel of attrition. The measures of awareness and engagement were inconsistently reported and could not be meta‐analysed (Table 12). When reported, awareness was assessed using measures such as website visits or logins and email openings. Engagement outcomes were often assessed as a proxy for adherence to the intervention using measures such as Facebook posts or comments. We included 14 studies which assessed changes in knowledge, seven studies which assessed changes in attitudes, and seven studies which assessed changes in intention or motivation. As summarised above, we found small but positive effects for interactive social media interventions. Similarly, as reported above, we found small but positive results for health behaviours and health outcomes.
11. Funnel of attrition outcomes.
| Study | Social Media Intervention Component | Awareness | Engagement | Knowledge | Attitude | Intention/ Motivation |
| Ahmad 2018 | Facebook and WhatsApp | ✔ | ||||
| Ahmad 2020 | Web‐based | ✔ | ||||
| Ashton 2017 | eHealth support website Facebook group |
✔ | ✔ | |||
| Bai 2015 | Professional‐guided online community | ✔ | ✔ | ✔ | ||
| Baker 2011 | Online discussion board | |||||
| Bantum 2014 | Web‐based program | ✔ | ||||
| Bender 2017 | ✔ | |||||
| Booth 2018 | ||||||
| Boyd 2019 | ✔ | ✔ | ||||
| Bull 2012 | ✔ | ✔ | ✔ | |||
| Castillo 2013 | Website | ✔ | ||||
| Cavalcanti 2019 | ||||||
| Cavallo 2012 | ✔ | ✔ | ||||
| Chai 2018 | WeChat messenger | ✔ | ✔ | |||
| Chen 2019 | ||||||
| Cheung 2015 | Facebook |
✔ | ||||
| Cobb 2014 | E‐mail‐, web‐, and mobile‐based intervention | ✔ | ||||
| Coffeng 2014 | Social media platform | |||||
| Dadkhah 2014 | ✔ | ✔ | ||||
| Dahl 2019 | Website and app | ✔ | ✔ | ✔ | ||
| Daly 2017 | ||||||
| Dehlendorf 2020 | Online community | ✔ | ✔ | ✔ | ||
| Duncan 2014 | Interactive website | ✔ | ✔ | |||
| Edney 2020 | App | ✔ | ||||
| Fiks 2017 | ✔ | |||||
| Glanz 2017 | Website and interactive website | ✔ | ✔ | |||
| Gnagnarella02016 | Website | ✔ | ✔ | |||
| Godino 2016 | ✔ | |||||
| Graham 2018 | Online social network | ✔ | ||||
| Graham 2011 | Interactive web site | ✔ | ||||
| George 2013 | ||||||
| Greene 2013 | Online social network | |||||
| Hammersley 2019 | ✔ | |||||
| Herring | ||||||
| Herring | ✔ | |||||
| Horvath 2013 | Interactive website | ✔ | ✔ | |||
| Hutchesson 2018 | Web‐based (website, app, email, text messages and social media) | ✔ | ||||
| Hwang 2013 | Online discussion forum | ✔ | ✔ | |||
| Jane 2017 | ||||||
| Joseph 2015 | ✔ | |||||
| Kernot 2019 | Facebook and app | ✔ | ||||
| Kim 2019 | Naver Band | ✔ | ||||
| Kolt 2017 | Interactive website | ✔ | ✔ | |||
| Koufopoulos 2016 | Online community | ✔ | ||||
| Lau 2012 | Interactive website | |||||
| Li 2017 | Tencent QQ | ✔ | ||||
| Li 2020 | ||||||
| Liao 2020 | ✔ | ✔ | ✔ | |||
| Linden 2017 | Web‐based support | ✔ | ✔ | ✔ | ||
| Looyestyn 2018 | ✔ | ✔ | ✔ | |||
| Lytle 2017 | Social network website. | ✔ | ✔ | |||
| Maher 2015 | ✔ | ✔ | ||||
| Mailey 2016 | Website discussion board and podcasts | ✔ | ✔ | |||
| Mascarenhas 2018 | Google Hangouts | ✔ | ||||
| Morris 2015 | Online social network | ✔ | ✔ | |||
| Moy 2015 | Online social network | ✔ | ✔ | |||
| Moy 2010 | Interactive website | |||||
| Nam 2015 | ✔ | |||||
| Nam 2020 | App | |||||
| Namkoong 2017 | ✔ | |||||
| Napolitano 2013 | Facebook Facebook Plus |
✔ | ||||
| O’Neil 2016 | Interactive website | |||||
| Owen 2015 | Interactive website | ✔ | ✔ | |||
| Petrella 2017 | Online social network | |||||
| Ramo 2015 | ✔ | |||||
| Ramo 2018b | ✔ | |||||
| Ren 2019 | ✔ | |||||
| Richardson 2010 | Online social network | ✔ | ✔ | |||
| Rouf 2020 | ✔ | ✔ | ✔ | |||
| Rovniak 2016 | Online social network | ✔ | ||||
| Rote 2015 | ✔ | |||||
| Schaller 2017 | Online social network | |||||
| Schneider 2015 | Online social network | ✔ | ✔ | |||
| Stoddard 2008 | Online social network | ✔ | ✔ | |||
| Sun 2017 | ✔ | ✔ | ✔ | |||
| Turner‐McGrievy 2011 | Twitter and podcasts | ✔ | ✔ | ✔ | ||
| Valle 2013 | ✔ | ✔ | ||||
| Vandelanotte 2017 | Interactive website | ✔ | ||||
| Vogel 2019 | ✔ | |||||
| Wan 2017 | Online social support | ✔ | ✔ | ✔ | ||
| Wang 2015 | ||||||
| Washington 2017 | ||||||
| Willcox 2017 | Facebook and interactive website | ✔ | ✔ | |||
| Willis 2017 | Online social network | ✔ | ✔ | |||
| Yang 2019 | ✔ | |||||
| Young 2013 | ✔ | |||||
| Young 2015 | ||||||
| Zhang 2016 | Online social network | ✔ | ✔ |
Discussion
Summary of main results
We aimed to provide an overview of the effectiveness of interactive social media interventions for public health. We included 88 studies assessing many types of public health interventions and targeted health behaviours, such as physical activity, diet and nutrition, condom use, vaccination, and cancer screening, among others. As planned, we considered these outcomes to be sufficiently similar. However, the interventions assessed in our included studies were quite different and had a mix of comparators. There was substantial heterogeneity for many of our outcomes and it remained high even when explored through planned subgroup analyses by population of the studies or the intervention type (e.g. social media alone versus social media as a component of a multi‐component intervention).
However, despite high heterogeneity, our results are promising. Overall, our findings indicate that interactive social media interventions when compared to non‐interactive social media interventions, including no intervention, may increase physical activity (low‐certainty evidence), may lead to greater weight loss (low‐certainty evidence), and may improve well‐being scores (low‐certainty evidence). The evidence was uncertain for many of the other health behaviours, and body function or psychological outcomes. Interactive social media interventions, especially those included in multi‐component interventions, are complex and we do not know which ingredient is the active ingredient. It is possible that the mechanism of action in the control and intervention arms were not different enough to explain the effect of the social media components.
We also compared interactive social media interventions with active social media controls. For this comparison, we found that the more interactive intervention may improve physical activity and weight loss, however, we had fewer studies with this comparison and there was high heterogeneity.
Few of our included studies assessed adverse events and these were related to the other intervention components, such as injuries from physical activity, and not to interactive social media. None of the studies reported on expected adverse events such as privacy concerns.
Overall completeness and applicability of evidence
As indicated by our 'Summary of findings' table, we found that social media interventions may increase physical activity. Our data also suggest that social media interventions may improve weight loss. These studies included a broad range of interventions and a variety of populations, including adults in general, as well as specific populations, such as those with a health condition or those at‐risk of a health condition. The outcomes assessed by these studies were quite varied and although we aimed to group all outcomes across our pre‐defined broader domains (e.g. health behaviours, body function, well‐being, and psychological outcomes), we also separated the results by the different outcome types for ease of interpretation and usefulness to our knowledge users. For our secondary outcomes, those which are considered process outcomes, we found little to no difference in the effectiveness of the intervention (e.g. on self‐efficacy, knowledge, etc.) indicating that for studies assessing process measures, other mechanisms of change may explain any observed effects on main outcomes.
We grouped comparisons of interactive social media interventions and non‐interactive social media with those compared with no intervention but separately analysed those with an active social media comparator. The rationale for this is based on our focus on the interactivity of the social media interventions. However, this may be a limitation of our review as there could be differences in effect for comparators in which no intervention was provided and those with an intensive non‐social media based intervention.
Another limitation of our review is that we excluded studies that did not include two‐way interaction amongst participants. For this reason, we excluded a study by Rhodes and colleagues which assessed HIV testing rates amongst men who have sex with men and transgender persons who are existing users of various social media platforms (Rhodes 2016). In this study, the intervention utilised a health educator and allowed anyone who viewed his profile to initiate a conversation while the control group received no intervention. While this study did not fit our inclusion criteria, we acknowledge that this type of intervention may be more commonly utilised for potentially stigmatising conditions and may be potentially useful for public health program planners who are interested in utilising social media to improve health outcomes.
We included randomised as well as controlled before‐and‐after (CBA) and interrupted time series (ITS) studies because we expected there to be different types of interactive social media interventions that may utilise these different study designs. However, we identified only a small number of non‐randomised studies and we have therefore reported only the randomised controlled trials ( RCTs) in our' Summary of findings' table. Future updates of this review will use the ROBINS‐I tool for assessing risk of bias (Sterne 2016).
A strength of our approach is that we grouped physical activity outcomes to assess whether there were differences in the effectiveness of social media interventions for general populations compared to those with a condition or at‐risk of a condition. We did not separate by outcome type as there would have been too few studies for each outcome and population group for us to assess whether there was a difference. There was high heterogeneity for many of our outcomes. However, for outcomes with 10 or more studies, we explored this heterogeneity using preplanned subgroup analyses by population and intervention type. We also conducted sensitivity analyses by adherence and risks of bias for allocation concealment and blinding of participants. There may be additional factors contributing to heterogeneity that we were unable to assess, such as the dose or intensity of the interactive social media components. We also aimed to assess whether adherence influenced the effectiveness of the interventions. However, adherence was not consistently reported in our studies with many studies not assessing it at all. Differences in adherence may have also contributed to heterogeneity between studies.
Quality of the evidence
Our 'Summary of findings' table indicates that, overall, the certainty of the evidence is low. This is mainly related to unclear risks of bias and substantial heterogeneity. Many of our included studies had unclear risks of bias. We rated every study as unclear for at least one domain. Due to the nature of some of the interventions, blinding of the participants was not possible and for some outcomes, this could lead to a high risk of bias. It was also unclear in many of the studies whether there were any methods for protecting against contamination beyond the use of private Facebook groups. We rated 35 studies as high risk of bias for selective outcome reporting, and 43 studies as unclear because no protocol or trial registration could be located.
Potential biases in the review process
While we made all efforts to identify published and unpublished studies, there is a possibility that we may have missed some eligible studies. However, we screened over 25,000 records identified through multiple electronic databases. We were very inclusive at title and abstract stage and retrieved the full text of any study that was potentially assessing the effectiveness of an interactive social media intervention. We wanted to review full text to determine the interactivity of the social media intervention and did not rely on the title and abstract to make this judgement.
We prioritised outcomes for extraction based on the hierarchy described above. The vast number of similar outcomes assessed in each study made it unfeasible to extract all outcomes. Our review aimed to provide an overview of the general effectiveness of interactive social media interventions for behaviour change and health outcomes and therefore we feel that extracting one outcome for our main outcome domains is more meaningful than extracting all relevant outcomes reported. This allowed us to combine data across all of our included studies while also allowing for subgroup analyses to explore differences for specific outcomes and population groups. However, this means that our meta‐analyses do not include all data available for our main and secondary outcomes from our included studies.
We collected but did not analyse data related to the funding sources of our included studies.
Agreements and disagreements with other studies or reviews
Our results are similar to those of other systematic reviews assessing social media interventions on health outcomes. For example, Williams and colleagues assessed social media for diet and exercise behaviour and found mixed results, with little to no difference in physical activity or weight but a reduction in dietary fat consumption among those receiving the social media intervention (Williams 2014). A review by Laranjo and colleagues found that social networking platforms improve health‐related behaviours but the interventions are quite varied with high heterogeneity (Laranjo 2015). This review included seven studies that were also included in our review. Similarly, a review by Klassen and colleagues assessed the use of social media interventions for nutrition outcomes among young adults (Klassen 2018). This review included five studies included in our review and the authors found that the majority of studies found little to no difference for weight, body mass index (BMI), and dietary intake for the participants receiving a social media intervention compared to controls. In this review, engagement with the intervention varied greatly ranging from 3% to 69%. A review by Carson‐Chahhoud and colleagues included one study assessing a social media campaign aimed at preventing smoking in young people and found that the intervention did not have an effect on smoking rates (Carson‐Chahhoud 2017).
These reviews identified similar challenges in isolating the impact of the interactive social media intervention in comparison to the other intervention components (Hamm 2014; Laranjo 2015; Williams 2014; Klassen 2018).
Authors' conclusions
Implications for practice.
Our review found that interactive social media interventions may increase physical activity, and may improve weight loss and well‐being. However, our overall certainty of evidence is low due to high heterogeneity and unclear risks of bias. Public health practitioners who implement an interactive social media intervention should plan to evaluate the effectiveness of the intervention.
In addition, our included studies did not report on adverse events related to interactive social media intervention components even though there are studies that suggest that possible harms associated with social media use may impact adherence to these interventions.
Implications for research.
The outcomes assessed in our included studies varied and although we combined data across outcome domains, the differences between outcomes meant that we often had only a small number of studies reporting on many outcome types. Standardised outcomes or core outcome sets for studies aimed at changing health behaviours, body function, psychological health, or well‐being would improve our ability to meaningfully combine data across studies. Future studies should aim to identify which component is the active ingredient when interactive social media is combined with additional co‐interventions.
Future research may need to consider newer social media platforms, especially depending on the target audience. The most commonly used platform among our included studies was Facebook, although the use of Facebook may be decreasing among certain populations (e.g. in Europe, among those aged under 25). In 2020, other popular social media platforms included Snapchat, LinkedIn, Instagram, and TikTok, however, none of these platforms were utilised in our included studies.
Our review found that there was little to no difference in social support scores for those receiving interactive social media interventions compared to non‐interactive social media. Interestingly, five of the 10 studies which assessed social support had also assessed changes in physical activity. It is possible that the measures used for social support are not fit for purpose or the mechanism of effect for interactive social media may not actually be social support. It is also possible that social support as a behaviour change technique was addressed by the intervention. In addition, we found that most of the behaviour change techniques applied to the intervention arm were also applied to the control arm, which may have made the comparisons too similar to identify an effect. Future studies should provide a better description of social support as a behaviour change technique which would enable us to better understand the effect of social support on behaviour change through interactive social media interventions.
Adverse events related to the interactive social media interventions were not reported. Future studies should aim to assess the possible adverse events specifically related to social media, such as privacy concerns, in addition to the adverse events from the other intervention components.
Finally, only four of our included studies reported specific equity considerations. As interactive social media has the potential to reach diverse populations, better reporting of the population characteristics and disaggregating results by these characteristics, when appropriate, can increase our understanding of interactive social media interventions and their potential effect on health inequities.
What's new
| Date | Event | Description |
|---|---|---|
| 17 June 2021 | Amended | Typographical errors introduce via technical glitch corrected in Effects of interventions section text. |
History
Protocol first published: Issue 2, 2018 Review first published: Issue 5, 2021
Notes
This Cochrane review will be co‐published by Campbell Knowledge Translation and Implementation Coordinating Group.
Acknowledgements
This title is co‐registered with the Campbell Knowledge Translation and Implementation Group. The authors are grateful for the assistance of Christian Charbonneau (CC), Alexandra Sokolovski (AS) and Jennifer Ogborogu (JO) as well as the input of Cochrane Public Health, especially Miranda Cumpston, and Campbell Knowledge Translation and Implementation (Lorraine Tudor Car). We thank our advisory group, especially Heather Manson, Justin Thiellman and the staff at Public Health Ontario for their advice on grouping of outcomes. We thank Howard White for his advice on our Funnel of Attrition. We also acknowledge the contribution of Jennifer Vincent in the early stages of protocol development.
Appendices
Appendix 1. Search Strategies
Database: Ovid MEDLINE(R) ALL <1946 to June 01, 2020>
Search Strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp Social Media/
2 Blogging*.mp.
3 Blogging/
4 Communications Media/
5 Social Networking/
6 (social adj2 media).tw.
7 ((virtual or online) adj2 (communit$ or network$)).tw.
8 "Web 2.0".tw.
9 Facebook.tw.
10 Twitter.tw.
11 MySpace.tw.
12 Tumblr.tw.
13 instagram.tw.
14 pinterest.tw.
15 wiki$.tw.
16 YouTube.tw.
17 vimeo.tw.
18 Flickr.tw.
19 Delicious.tw.
20 blog$.tw.
21 (linkedin or linked in).tw.
22 (sixdegrees or six degrees).tw.
23 weibo.tw.
24 curediva.tw.
25 connectedliving.tw.
26 patientslikeme.tw.
27 wego.tw.
28 caringbridge.tw.
29 crowd sourc$.tw.
30 crowdsourc$.tw.
31 hash tag$.tw.
32 hashtag$.tw.
33 microblog$.tw.
34 push technolog$.tw.
35 facetime$.tw.
36 Friendster.tw.
37 Gchat.tw.
38 g‐chat.tw.
39 google maps.tw.
40 Kik.tw.
41 reddit$.tw.
42 subreddit$.tw.
43 snapchat$.tw.
44 tweet$.tw.
45 wechat$.tw.
46 whatsapp$.tw.
47 MXit.tw.
48 QQ.tw.
49 Qzone.tw.
50 baidu.tw.
51 viber.tw.
52 Vkontakte.tw.
53 Odnoklassniki.tw.
54 Facenama.tw.
55 (YY and (social adj2 network$)).tw.
56 (QQ and (social adj2 network$)).tw.
57 (vine and (social adj2 network$)).tw.
58 (LINE and (social adj2 network$)).tw.
59 or/1‐58
60 limit 59 to yr="2001‐ Current"
61 (pre‐intervention$ or preintervention$ or pre intervention$ or post‐intervention$ or postintervention$ or post intervention$).ti,ab.
62 demonstration project$.ti,ab.
63 (pre‐post or pre test$ or pretest$ or posttest$ or post test$ or (pre adj5 post)).ti,ab.
64 trial.ti. or ((study adj3 aim$) or our study).ab.
65 (before adj10 (after or during)).ti,ab.
66 (quasi‐experiment$ or quasiexperiment$ or quasi random$ or quasirandom$ or quasi control$ or quasicontrol$ or ((quasi$ or experimental) adj3 (method$ or study or trial or design$))).ti,ab,hw.
67 (time points adj3 (over or multiple or three or four or five or six or seven or eight or nine or ten or eleven or twelve or month$ or hour$ or day$ or more than)).ab.
68 (time series adj2 interrupt$).ti,ab,hw.
69 pilot.ti.
70 Pilot projects/ or "Controlled Before‐After Studies"/ or "Interrupted Time Series Analysis"/
71 (clinical trial or controlled clinical trial or multicenter study or randomised controlled trial or pragmatic clinical trial).pt.
72 (multicentre or multicenter or multi‐centre or multi‐center).ti.
73 random$.ti,ab. or controlled.ti.
74 (control adj3 (area or cohort$ or compare$ or condition or design or group$ or intervention$ or participant$ or study)).ab.
75 evaluation studies as topic/ or prospective studies/ or retrospective studies/ or non‐randomized controlled trials as topic/ or interrupted time series analysis/ or controlled before‐after studies/
76 (during adj5 period).ti,ab.
77 ((strategy or strategies) adj2 (improv$ or education$)).ti,ab.
78 (rat or rats or cow or cows or chicken$ or horse or horses or mice or mouse or bovine or animal$).ti.
79 exp animals/ not humans.sh.
80 (or/61‐77) not (or/78‐79)
81 60 and 80
PsycInfo
Database: APA PsycInfo <1806 to May Week 4 2020>
Search Strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp Social Media/
2 Blog/
3 communications media/
4 Computer Mediated Communication/
5 Online Social Networks/
6 (social adj2 media).tw.
7 ((virtual or online) adj2 (communit$ or network$)).tw.
8 "Web 2.0".tw.
9 Facebook.tw.
10 Twitter.tw.
11 MySpace.tw.
12 Tumblr.tw.
13 instagram.tw.
14 pinterest.tw.
15 wiki?.tw.
16 YouTube.tw.
17 vimeo.tw.
18 Flickr.tw.
19 Delicious.tw.
20 blog?.tw.
21 linkedin.tw.
22 sixdegrees.tw.
23 weibo.tw.
24 curediva.tw.
25 connectedliving.tw.
26 patientslikeme.tw.
27 wego.tw.
28 caringbridge.tw.
29 crowd sourc*.tw.
30 crowdsourc*.tw.
31 hash tag*.tw.
32 hashtag*.tw.
33 microblog*.tw.
34 push technolog*.tw.
35 facetime*.tw.
36 Friendster.tw.
37 Gchat.tw.
38 g‐chat.tw.
39 google maps.tw.
40 Kik.tw.
41 reddit*.tw.
42 subreddit*.tw.
43 snapchat*.tw.
44 tweet*.tw.
45 vine.tw.
46 wechat*.tw.
47 whatsapp*.tw.
48 MXit.tw.
49 QQ.tw.
50 Qzone.tw.
51 baidu.tw.
52 viber.tw.
53 Vkontakte.tw.
54 (YY and (social adj2 network*)).tw.
55 (QQ and (social adj2 network*)).tw.
56 (vine and (social adj2 network*)).tw.
57 (LINE and (social adj2 network*)).tw.
58 or/1‐56
59 limit 58 to ("comment/reply" or editorial or letter or review‐book or review‐media or review‐ software & other or reviews) [Limit not valid in APA PsycInfo; records were retained]
60 58 not 59
61 (double‐blind or random* assigned or control).tw.
62 60 and 61
63 intervention*.ti.
64 (collaborativ* or collaboration* or tailored or personali?ed).ti,ab.
65 demonstration project*.ti,ab.
66 (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or (pre adj5 post)).ti,ab.
67 ((study adj3 aim?) or "our study").ab.
68 (before adj10 (after or during)).ti,ab.
69 ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) adj3 (method* or study or trial or design*))).ti,ab,hw.
70 ("time series" adj2 interrupt*).ti,ab,hw.
71 (time points adj3 (over or multiple or three or four or five or six or seven or eight or nine or ten or eleven or twelve or month* or hour? or day? or "more than")).ab.
72 pilot.ti.
73 intervention/
74 clinical trials/
75 (multicentre or multicenter or multi‐centre or multi‐center).ti.
76 random*.ti,ab. or controlled.ti.
77 (control adj3 (area or cohort? or compar? or condition or group? or intervention? or participant? or study)).ab.
78 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77
79 60 and 78
80 79 not 62
81 limit 80 to yr="2001‐Current"
82 limit 58 to ("column/opinion" or "comment/reply" or editorial or letter or review‐book or review‐media or review‐software & other or reviews)
83 79 or 62
84 limit 83 to yr="2001 ‐Current"
85 84 not 81
CENTRAL
1 exp Social Media/
2 Blogging/
3 Communications Media/
4 Social Networking/
5 (social adj2 media).tw.
6 ((virtual or online) adj2 (communit$ or network$)).tw.
7 "Web 2.0".tw.
8 Facebook.tw.
9 Twitter.tw.
10 MySpace.tw.
11 Tumblr.tw.
12 instagram.tw.
13 pinterest.tw.
14 wiki?.tw.
15 YouTube.tw.
16 vimeo.tw.
17 Flickr.tw.
18 Delicious.tw.
19 blog?.tw.
20 linkedin.tw.
21 sixdegrees.tw.
22 weibo.tw.
23 curediva.tw.
24 connectedliving.tw.
25 patientslikeme.tw.
26 wego.tw.
27 caringbridge.tw.
28 crowd sourc*.tw.
29 crowdsourc*.tw.
30 hash tag*.tw.
31 hashtag*.tw.
32 microblog*.tw.
33 push technolog*.tw.
34 facetime*.tw.
35 Friendster.tw.
36 Gchat.tw.
37 g‐chat.tw.
38 google maps.tw.
39 Kik.tw.
40 reddit*.tw.
41 subreddit*.tw.
42 snapchat*.tw.
43 tweet*.tw.
44 vine.tw.
45 wechat*.tw.
46 whatsapp*.tw.
47 MXit.tw.
48 QQ.tw.
49 Qzone.tw.
50 baidu.tw.
51 viber.tw.
52 Vkontakte.tw.
53 (YY and (social adj2 network*)).tw.
54 (QQ and (social adj2 network*)).tw.
55 (vine and (social adj2 network*)).tw.
56 (LINE and (social adj2 network*)).tw.
57 or/1‐56
58 limit 57 to yr="2001 ‐Current"
Embase
Database: Embase Classic+Embase <1947 to 2020 June 01>
Search Strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp *Social Media/
2 Blogging*.mp.
3 *Blogging/
4 *mass medium/
5 *Social Network/
6 (social adj2 media).tw.
7 ((virtual or online) adj2 (communit$ or network$)).tw.
8 "Web 2.0".tw.
9 Facebook.tw.
10 Twitter.tw.
11 MySpace.tw.
12 Tumblr.tw.
13 instagram.tw.
14 pinterest.tw.
15 wiki$.tw.
16 YouTube.tw.
17 vimeo.tw.
18 Flickr.tw.
19 Delicious.tw.
20 blog$.tw.
21 (linkedin or linked in).tw.
22 (sixdegrees or six degrees).tw.
23 weibo.tw.
24 curediva.tw.
25 connectedliving.tw.
26 patientslikeme.tw.
27 wego.tw.
28 caringbridge.tw.
29 crowd sourc$.tw.
30 crowdsourc$.tw.
31 hash tag$.tw.
32 hashtag$.tw.
33 microblog$.tw.
34 push technolog$.tw.
35 facetime$.tw.
36 Friendster.tw.
37 Gchat.tw.
38 g‐chat.tw.
39 google maps.tw.
40 Kik.tw.
41 reddit$.tw.
42 subreddit$.tw.
43 snapchat$.tw.
44 tweet$.tw.
45 vine.tw.
46 wechat$.tw.
47 whatsapp$.tw.
48 MXit.tw.
49 QQ.tw.
50 Qzone.tw.
51 baidu.tw.
52 viber.tw.
53 Vkontakte.tw.
54 Odnoklassniki.tw.
55 Facenama.tw.
56 (YY and (social adj2 network$)).tw.
57 (QQ and (social adj2 network$)).tw.
58 (vine and (social adj2 network$)).tw.
59 (LINE and (social adj2 network$)).tw.
60 or/1‐59
61 (animal model$ or animal experiment$ or animal study$ or animal trial$ or canine or feline or bovine or cow or cows or mice or dog$ or cat or cats or rabbit$ or rat or rats or veterinar$).ti. or (animal or veterinary).hw.
62 (editorial or letter or note or "review" or trade or survey).pt.
63 meta‐analysis/ or systematic review/ or "literature review".ti. or "systematic review".ti. or (meta‐analy$ or metaanalyt$).ti.
64 61 or 62 or 63
65 60 not 64
66 randomised controlled trial/ or (randomised or randomised).tw. or experiment*.tw. or (time adj series).tw. or (pre test or pretest or posttest or post test).tw. or impact.tw. or intervention?.tw. or chang*.tw. or evaluat*.tw. or effect?.tw. or compar*.tw. or (controlled adj study).tw.
67 (random sampl* or random digit* or random effect* or random survey or random regression).ti,ab. not randomised controlled trial/
68 65 and 66
69 68 not 67
70 (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) and (human/ or normal human/ or human cell/)
71 (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) not 70
72 69 not 71
77 limit 72 to yr="2001‐Current"
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
Database; CINAHL (via Ebsco)
CINAHL
S1
MH social media+
S2
MH blog
Search modes ‐ SmartText Searching
S3
MH social networking
S4
TX (social N2 media)
S5
TX ((virtual or online) N2 (communit* or network*))
(3,755)
S6
TX Web 2.0
S7
TX Facebook
S8
TX Twitter
S9
TX Myspace
S10
TX Tumblr
S11
TX instagram
S12
TX pinterest
S13
TX wiki*
S14
TX YouTube
S15
TX vimeo
S16
TX Flickr
S17
TX Delicious
S18
TX blog*
S19
TX LinkedIn
S20
TX sixdegrees
S21
TX weibo
S22
TX curediva
Search modes ‐ SmartText Searching
S23
TX connectedliving
S24
TX patientslikeme
S25
TX wego
S26
TX caringbridge
S27
TX crowdsourc* or TX crowd sourc*
S28
TX hash tag* or TX hashtag*
S29
TX microblog*
S30
TX push technolog*
S31
TX facetime*
S32
TX Friendster*
S33
TX Gchat or TX g‐chat
Search modes ‐ SmartText Searching
S34
TX Gchat or TX g‐chat
Search modes ‐ SmartText Searching
S35
TX google maps
S36
TX Kik
S37
TX reddit* or TX subreddit*
S38
TX snapchat*
S39
TX tweet*
S40
TX vine
S41
TX wechat*
S42
TX whatsapp*
S43
TX MXit
S44
TX QQ
S45
TX Ozone
S46
TX baidu
S47
TX viber
S48
TX Vkontakte
S49
TX (YY and (social N2 network*))
S50
TX (QQ and (social N2 network*))
(2)
S51
TX (vine and (social N2 network*))
S52
TX (Line and (social N2 network*))
S53
TI ( postintervention* or post‐intervention* or preintervention* or pre‐intervention* ) or AB ( postintervention* or post‐intervention* or preintervention* or pre‐intervention* )
S54
TI ( pre‐test* or pretest* or posttest* or post‐test* ) or AB ( pre‐test* or pretest* or posttest* or "post test* )
S55
TI ( ( quasi‐experiment* or quasiexperiment* or quasi‐random* or quasirandom* or quasi control* or quasicontrol* or quasi* W3 method* or quasi* W3 study or quasi* W3 studies or quasi* W3 trial or quasi* W3 design* or experimental W3 method* or experimental W3 study or experimental W3 studies or experimental W3 trial or experimental W3 design* ) ) or AB ( ( quasi‐experiment* or quasiexperiment* or quasi‐random* or quasirandom* or quasi control* or quasicontrol* or quasi* W3 method* or quasi* W3 s ...
S56
TI ( (time point*) or (period* n4 interrupted) or (period* n4 multiple) or (period* n4 time) or (period* n4 various) or (period* n4 varying) or (period* n4 week*) or (period* n4 month*) or (period* n4 year*) ) or AB ( (time point*) or (period* n4 interrupted) or (period* n4 multiple) or (period* n4 time) or (period* n4 various) or (period* n4 varying) or (period* n4 week*) or (period* n4 month*) or (period* n4 year*) 58,880 )
(88,093)
S57
TI ( before* n10 during or before n10 after ) or AB ( before* n10 during or before n10 after )
S58
TI (time series) or AB (time series)
S59
AB "before‐and‐after"
S60
(MH "Pilot Studies")
S61
TI pilot
S62
TI ( demonstration project OR demonstration projects OR preimplement* or pre‐implement* or post‐ implement* or postimplement* ) or AB ( demonstration project OR demonstration projects OR preimplement* or pre‐implement* or post‐implement* or postimplement* )
S63
TI ( trial or (study n3 aim) or "our study" ) or AB ( (study n3 aim) or "our study" )
S64
TI random* OR controlled
S65
TI ( multicentre or multicenter or multi‐centre or multi‐center )
S66
TI ( (control w3 area) or (control w3 cohort*) or (control w3 compar*) or (control w3 condition) or (control w3 group*) or (control w3 intervention*) or (control w3 participant*) or (control w3 study) ) or AB ( (control w3 area) or (control w3 cohort*) or (control w3 compar*) or (control w3 condition) or (control w3 group*) or (control w3 intervention*) or (control w3 participant*) or (control w3 study) )
S67
TI ( (time points n3 over) or (time points n3 multiple) or (time points n3 three) or (time points n3 four) or (time points n3 five) or (time points n3 six) or (time points n3 seven) or (time points n3 eight) or (time points n3 nine) or (time points n3 ten) or (time points n3 eleven) or (time points n3 twelve) or (time points n3 month*) or (time points n3 hour*) or (time points n3 day*) or (time points n3 "more than") ) or AB ( (time points n3 over) or (time points n3 multiple) or (time points n3 ...
Search modes ‐ SmartText Searching
S68
(MM "Clinical Trials+")
S69
TI ( “clinical study” or “clinical studies” ) or AB ( “clinical study” or “clinical studies” )
S70
TI random* or AB random*
S71
TI controlled or AB controlled
S72
TI ( “control* N1 clinical” or “control* N1 group*” or “control* N1 trial*” or “control* N1 study” or “control* N1 studies” or “control* N1 design*” or “control* N1 method*” ) or AB ( “control* N1 clinical” or “control* N1 group*” or “control* N1 trial*” or “control* N1 study” or “control* N1 studies” or “control* N1 design*” or “control* N1 method*” )
Search modes ‐ SmartText Searching
S73
S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72
S74
S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52
S75
S73 AND S74
S76
S73 AND S74
Limiters ‐ Published Date: 20000101‐20200331
Data and analyses
Comparison 1. Overall ‐ any interactive social media intervention compared to non‐interactive social media control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Health behaviours ‐ physical activity | 29 | Std. Mean Difference (IV, Random, 95% CI) | 0.29 [0.13, 0.45] | |
| 1.2 Health behaviours ‐ diet quality | 8 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.25, 0.47] | |
| 1.3 Health behaviours ‐ calorie intake | 3 | 131 | Mean Difference (IV, Random, 95% CI) | ‐53.75 [‐152.48, 44.97] |
| 1.4 Health behaviour ‐ increased calcium intake | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.5 Health behaviours ‐ healthy infant feeding behaviour score | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6 Health behaviours ‐ breastfeeding | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.7 Health behaviours ‐ tobacco use | 4 | 2433 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.74, 1.29] |
| 1.8 Health behaviours ‐ condom use frequency | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.33, 0.76] | |
| 1.9 Health behaviours ‐ Medication adherence | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.24, 0.46] | |
| 1.10 Health behaviours ‐ Vaccination (frequency) | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.25, 1.00] | |
| 1.11 Health behaviours ‐ vaccination uptake | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.12 Health behaviours ‐ screening test | 4 | 579 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [1.21, 2.24] |
| 1.13 Health behaviours ‐ self‐care | 2 | 186 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.55, 0.67] |
| 1.14 Health behaviours ‐ mindfulness | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.15 Health behaviours ‐ parent modeling of healthy eating | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.16 Health behaviours ‐ maternal care utilisation | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.17 Health behaviours, CBA | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.17.1 Physical Activity | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.17.2 Smoking rate | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.18 Body functions ‐ Weight (kg) | 16 | 1963 | Mean Difference (IV, Random, 95% CI) | ‐1.34 [‐2.00, ‐0.69] |
| 1.19 Body functions ‐ gestational weight gain | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.20 Body functions ‐ BMI kg/m2 | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐0.92, ‐0.10] |
| 1.21 Body Functions ‐ Blood glucose mmol/L | 4 | 773 | Mean Difference (IV, Random, 95% CI) | ‐1.74 [‐2.79, ‐0.68] |
| 1.22 Body functions ‐ Insomnia | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.22.1 Insomnia | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.23 Body functions ‐ PMS Score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.23.1 PMS score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.24 Body function ‐ Dyspnoea | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.24.1 Dyspnoea | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.25 Body functions ‐ Cardiorespiratory fitness (heart beats/min) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.26 Body function ‐ Influenza‐like illness | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.27 Body Function outcomes ‐ physical health status, CBA | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.28 Well‐being outcomes | 17 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [0.00, 0.73] | |
| 1.28.1 General well‐being | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.60, 1.08] | |
| 1.28.2 Quality of life | 12 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.16, 0.83] | |
| 1.28.3 Fatigue | 1 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐0.95, ‐0.49] | |
| 1.29 Psychological outcomes | 12 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.38, 0.08] | |
| 1.29.1 Depression | 9 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.58, 0.07] | |
| 1.29.2 Distress | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.22, 0.23] | |
| 1.30 Psychological outcomes ‐ probable depression | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.31 Psychological outcomes ‐ CBA | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only |
Comparison 2. Disaggregated by outcome type ‐ any interactive social media intervention compared to non‐social media control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Physical Activity (Steps per day) | 7 | 861 | Mean Difference (IV, Random, 95% CI) | 1376.81 [708.43, 2045.18] |
| 2.2 Physical Activity (total weekly minutes moderate‐vigorous activity) | 16 | 2365 | Mean Difference (IV, Random, 95% CI) | 15.81 [‐2.98, 34.59] |
| 2.3 Physical Activity (MET‐min/wk) | 2 | 208 | Mean Difference (IV, Random, 95% CI) | ‐833.93 [‐5398.37, 3730.52] |
| 2.4 Physical Activity (calories expended) | 2 | 162 | Mean Difference (IV, Random, 95% CI) | 194.89 [‐38.38, 428.15] |
| 2.5 Attendance at physical activity sessions (number of classes) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. Subgroup by population ‐ any interactive social media intervention compared to non‐interactive social media control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Health behaviour ‐ All Physical Activity | 27 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1.1 General Population | 17 | 2257 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [0.07, 0.54] |
| 3.1.2 Targeted at a population with or at‐risk of a condition | 10 | 1322 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [‐0.00, 0.57] |
| 3.2 Body function ‐ Weight | 14 | 1757 | Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐2.39, ‐0.80] |
| 3.2.1 General Population | 5 | 575 | Mean Difference (IV, Random, 95% CI) | ‐1.78 [‐2.78, ‐0.78] |
| 3.2.2 Targeted at a population with or at‐risk of a condition | 9 | 1182 | Mean Difference (IV, Random, 95% CI) | ‐1.48 [‐2.53, ‐0.43] |
| 3.3 Well‐being | 15 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [0.07, 0.72] | |
| 3.3.1 General Population | 6 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [‐0.00, 0.95] | |
| 3.3.2 Targeted at a population with or at‐risk of a condition | 10 | Std. Mean Difference (IV, Random, 95% CI) | 0.35 [‐0.05, 0.75] | |
| 3.4 Psychological outcomes | 12 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.38, 0.10] | |
| 3.4.1 General population | 5 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.67, 0.16] | |
| 3.4.2 Targeted at a population with or at‐risk of a condition | 7 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.38, 0.27] |
Comparison 4. Subgroup by outcome type and intervention type ‐ Interactive social media intervention compared to non‐interactive social media control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Physical Activity (Steps per day) | 7 | 861 | Mean Difference (IV, Random, 95% CI) | 1376.81 [708.43, 2045.18] |
| 4.1.1 Social media alone | 2 | 376 | Mean Difference (IV, Random, 95% CI) | 1469.63 [‐725.31, 3664.57] |
| 4.1.2 Social media as component of a multi‐component intervention | 5 | 485 | Mean Difference (IV, Random, 95% CI) | 1357.78 [663.61, 2051.94] |
| 4.2 Physical Activity (total weekly minutes moderate‐vigorous activity) | 16 | 2348 | Mean Difference (IV, Random, 95% CI) | 8.80 [‐1.14, 18.74] |
| 4.2.1 Social media alone | 4 | 614 | Mean Difference (IV, Random, 95% CI) | 37.66 [8.69, 66.63] |
| 4.2.2 Social media as component of a multi‐component intervention | 12 | 1734 | Mean Difference (IV, Random, 95% CI) | 4.64 [‐24.83, 34.11] |
| 4.3 Weight (kg) | 16 | 2005 | Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐1.91, ‐0.61] |
| 4.3.1 Social media alone | 5 | 382 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.78, 0.35] |
| 4.3.2 Social media as component of a multi‐component intervention | 11 | 1623 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐2.54, ‐0.66] |
| 4.4 Quality of Life score | 12 | 1276 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.14, 0.86] |
| 4.4.1 Social media alone | 4 | 393 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [‐0.02, 1.80] |
| 4.4.2 Social media as component of a multi‐component intervention | 8 | 883 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.01, 0.64] |
Comparison 5. Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Health behaviours ‐ physical activity, Low ROB for allocation concealment | 10 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [0.07, 0.69] | |
| 5.2 Health behaviours ‐ physical activity, Low ROB for blinding of participants | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.3 Health behaviours ‐ physical activity, Good adherence | 6 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.04, 0.55] | |
| 5.4 Body function ‐ weight, Good adherence | 5 | 284 | Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.93, ‐0.21] |
| 5.5 Body function ‐ weight, Low ROB for allocation concealment | 6 | 737 | Mean Difference (IV, Random, 95% CI) | ‐1.77 [‐2.66, ‐0.88] |
| 5.6 Body function ‐ weight, Low ROB for blinding of participants | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.7 Well‐being ‐ Good adherence | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [0.07, 0.59] | |
| 5.8 Well‐being ‐ Low ROB for allocation concealment | 7 | Std. Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.09, 0.59] | |
| 5.9 Well‐being ‐ Low ROB for blinding of participants | 1 | Odds Ratio (IV, Random, 95% CI) | Subtotals only |
5.6. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 6: Body function ‐ weight, Low ROB for blinding of participants
5.9. Analysis.

Comparison 5: Sensitivity analysis ‐ any interactive social media intervention compared to non‐interactive social media control, Outcome 9: Well‐being ‐ Low ROB for blinding of participants
Comparison 6. Secondary Outcomes ‐ Interactive social media intervention vs. non‐interactive social media.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Change in knowledge | 9 | 908 | Std. Mean Difference (IV, Random, 95% CI) | 0.90 [0.22, 1.58] |
| 6.1.1 Parents' ADHD knowledge | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 4.53 [3.74, 5.33] |
| 6.1.2 Diabetes coherence | 1 | 143 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.12, 0.54] |
| 6.1.3 Colorectal cancer screening salience and coherence | 1 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.27, 0.22] |
| 6.1.4 COPD knowledge | 1 | 109 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.43, 0.32] |
| 6.1.5 Nutrition and weight knowledge | 2 | 159 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.55, 0.08] |
| 6.1.6 Haemodyalyss patient knowledge | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.28, 0.58] |
| 6.1.7 Parental competence | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | 7.95 [5.06, 10.85] |
| 6.1.8 Exercise coherence | 1 | 45 | Std. Mean Difference (IV, Random, 95% CI) | 1.06 [0.22, 1.90] |
| 6.2 Knowledge (CBA) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.2.1 Tobacco knowledge | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3 Change in attitude | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3.1 Condom use attitudes | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3.2 Exercise attitude | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3.3 Attitude to medication (ADHD) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.4 Change in attitude (CBA) ‐ Tobacco attitudes | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.5 Change in self‐efficacy | 14 | 2349 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.13, 0.34] |
| 6.5.1 General self‐efficacy | 1 | 209 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.29, 0.29] |
| 6.5.2 Diabetes self‐efficacy | 1 | 143 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.28, 0.38] |
| 6.5.3 Condom self‐efficacy | 1 | 804 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.20, 0.07] |
| 6.5.4 Medication‐taking self‐efficacy (ADHD) | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 1.58 [1.10, 2.06] |
| 6.5.5 Exercise self‐efficacy | 5 | 358 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.12, 0.35] |
| 6.5.6 Colorectal cancer screening self‐efficacy | 1 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.35, 0.14] |
| 6.5.7 Weight loss self‐efficacy | 1 | 96 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.50, 0.30] |
| 6.5.8 Patient activation | 1 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐1.47, ‐0.64] |
| 6.5.9 Cancer‐related self‐efficacy | 1 | 206 | Std. Mean Difference (IV, Random, 95% CI) | 0.54 [0.26, 0.81] |
| 6.5.10 Chronic disease self‐efficacy | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.24, 0.62] |
| 6.6 Change in self‐efficacy (CBA) ‐ general self‐efficacy | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.7 Change in subjective norms | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.7.1 Medication norms (ADHD) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.7.2 Condom norms | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.8 Change in direct control | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.8.1 Medication behaviour | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.9 Change in direct control (CBA) ‐ exercise | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.10 Change in intention | 3 | 1087 | Std. Mean Difference (IV, Random, 95% CI) | 1.00 [0.04, 1.96] |
| 6.10.1 Contraceptive use intention | 2 | 998 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.11, 0.73] |
| 6.10.2 Medication adherence intention (ADHD) | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 2.46 [1.91, 3.02] |
| 6.11 Intention to vaccinate children | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.12 Change in motivation | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.12.1 Motivation to exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.12.2 Motivation to increase calcium intake | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.13 Change in motivation (higher motivation) | 2 | 823 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.90, 1.06] |
| 6.14 Change in perceived susceptibility ‐ colorectal cancer | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.15 Change in social support | 7 | 875 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.04, 0.35] |
| 6.15.1 Physical activity social support | 4 | 302 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.17, 0.47] |
| 6.15.2 Colorectal cancer screening social support | 1 | 258 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.24, 0.24] |
| 6.15.3 Cancer social support | 1 | 206 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.16, 0.72] |
| 6.15.4 General social support | 1 | 109 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.34, 0.41] |
Comparison 7. Overall ‐ Any interactive social media intervention compared to active social media comparator.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Health behaviours ‐ Physical activity | 4 | 1523 | Std. Mean Difference (IV, Random, 95% CI) | 0.35 [0.12, 0.59] |
| 7.2 Health behaviours ‐ healthy eating | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.3 Health behaviours ‐ IUD use | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.4 Health behaviours ‐ tobacco use | 2 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.90, 1.07] |
| 7.5 Health behaviours ‐ mindfulness | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.6 Body function outcomes | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.6.1 Weight (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.6.2 BMI | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.7 Body function ‐ total gestational weight gain (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.8 Well‐being | 2 | 2082 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐2.99, 2.20] |
| 7.8.1 Well‐being | 1 | 1328 | Mean Difference (IV, Random, 95% CI) | 0.70 [‐1.37, 2.77] |
| 7.8.2 Quality of Life | 1 | 754 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐5.10, 1.10] |
| 7.9 Psychological outcomes ‐ Self‐worth | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.10 Psychological outcomes ‐ depression | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.11 Pyschological outcomes ‐ anxiety | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 8. Secondary Outcomes ‐ Interactive social media vs. active social media comparator.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Change in exercise self‐efficacy | 2 | 123 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.52, 0.42] |
| 8.2 Change in physical activity social support | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahmad 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: parents of overweight/obese school‐aged children from urban Malaysia primary government schools (N = 134).
Age range: children were 7 to 10 years of age and mean (SD) age in years of parents was 39.8 (3.6) for the intervention group and 41.3 (5.7) for the control group. Recruitment: brochures were sent to all five primary government schools in urban area of Malaysia. Eligibility: attending one of 5 schools, aged 7‐10, BMI z‐score more than 1 SD, parent‐child dyads of Malay ethnicity who were computer literate, had access to the Internet, were willing to use social media for interaction and children 7 to 10 years of age were recruited. Country: Malaysia |
|
| Interventions |
Intervention: multi‐component (n = 67) The REDUCE (REorganise Diet, Unnecessary sCreen time and Exercise) 4‐week intervention trained parents on children's nutrition, physical activity, behaviour modification techniques and parenting skills delivered via face‐to‐face (two sessions) and Facebook (two weeks). A What's App group was used for a 12‐week for booster phase to strengthen parents’ knowledge and skills. Control: no intervention (n = 67) Waitlist control condition. |
|
| Outcomes | Children's BMI z score, waist circumference percentile and percentage of total body fat. | |
| Equity | Upper middle‐income country, urban area, Malay ethnicity, high prevalence of childhood obesity. | |
| Notes | Health behaviours: not applicable. Body function: children's BMI z‐score was reported as the primary outcome and the most related to parental practices. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: no adverse events experienced. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Quote: "Each parent‐child dyad from all five schools was number coded by the first author and sent to a research assistant who performed a computer generated randomized list which allocated parents into intervention or wait‐list control groups." |
| Blinding of personnel | High risk | Quote: "The list was then provided to the first author to invite the intervention group for the REDUCE intervention program" |
| Blinding of participants | Unclear risk | Quote: "Participating parents were informed that the intervention would be done in stages." Parents would have the understanding that some of them would be participating earlier than others. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High response rate. Quote: "There was no significant difference between parents who remained in the study and parents who dropped out in terms of sociodemographic characteristics, parental BMI and the anthropometric measurements of the children." |
| Selective reporting (reporting bias) | High risk | Additional outcomes were reported in the protocol: parents' knowledge and practices, parents' self‐efficacy, parental feeding styles, physical activity and sedentary behaviours, child eating behaviours, dietary intake. |
| Baseline characteristics similar | Low risk | Quote: "There were no significant differences between the intervention and control groups at baseline" |
| Baseline outcome measurements similar | Unclear risk | BMI‐z scores of school children were not available at baseline. |
| Protection against contamination | Unclear risk | Quote: "the intervention group was informed not to share their social media experience with other parents, in addition they did not know who were in the wait‐listed group, hence minimizing contamination." However, there is a possibility they could have shared information. |
Ahmad 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: undergraduate university students (N = 119). Age range: ≥18 years of age, overall mean (SD) age in years was 24.8 (6.5). Recruitment: recruited participants on York University Campus through posters, class visits on permission of course directors, and email invitations via listserves of student associations in the Faculty of Health and Faculty of Liberal Arts. Eligibility: minimal age of 18 years, English language fluency, self‐reported high level of confidence to complete the study, and current undergraduate student status, ability to use a computer and smartphone and Internet literacy were assumed to be de facto skills. Country: Canada |
|
| Interventions |
Intervention: multi‐component intervention (n = 40) 8‐week Web‐based Full Mindfulness Virtual Community (MVC) interventions. For the first 4 weeks, there were 12 video‐based modules (youth‐specific mental health education and mindfulness‐practice modules, delivered via video recordings), peer‐to‐peer discussion forums (anonymous, asynchronous), and brief guided video conferences (20‐min live video conferences (group‐based) on module topics guided by a mental health professional); and in the second 4 weeks there was continued access to the video‐based modules. Control: no intervention (n = 40) Waitlist control group continued as usual care during the 8‐week period without access to additional resources. |
|
| Outcomes | Symptoms of depression, anxiety, and stress, quality of life, life satisfaction, mindfulness, self‐perceived change in the academic performance and in class attendance/absenteeism. module use (number of videos watched in full, average frequency of watching each video), exchanges during discussion forums (for appropriateness, supportiveness, and informativeness), and videoc onferences (for ease in access, convenience, help in understanding personal mindfulness practice and mental well‐being, and help via the direct messaging feature). | |
| Equity | High income country, undergraduate university studies. | |
| Notes | Health behaviours: mindfulness was the only outcome reported for this category. Body function: mot applicable. Psychological health: depression and anxiety were the first two reported outcomes (not alphabetically) for this category. Well‐being: quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: no instance of distress warranting support occurred during the trial period. Secondary outcomes: not applicable. Note: waitlist control group extracted as control since there was minimal interaction between participants/researcher. The Web‐based P‐MVC intervention was 8 weeks long and included all the video material of the F‐MVC intervention following a similar release schedule, but it did not offer any video conferences or discussion forums (n=39). A fourth group of face‐to‐face CBT mindfulness is presented elsewhere, study authors reported that the manuscript is under review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Quote "The randomization allocation sequence was computer‐generated" |
| Allocation concealment (selection bias) | Low risk | "Quote "The randomization allocation sequence was computer‐generated by an off‐site team member who concealed it in sequentially numbered, opaque envelopes. These envelopes were opened only after a written consent, keeping participants and research assistants blind to allocation." |
| Blinding of personnel | Low risk | "Quote "envelopes were opened only after a written consent, keeping participants and research assistants blind to allocation." |
| Blinding of participants | High risk | "Quote "envelopes were opened only after a written consent, keeping participants and research assistants blind to allocation." Unable to keep the participants blind to the intervention and control conditions once they opened the allocation envelopes after consenting. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were self‐reported and participants were aware of assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis used. Low attrition and similar across groups but reasons not provided. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Baseline characteristics similar | Unclear risk | "Quote "participant and other characteristics seemed to be similarly distributed between the control and intervention groups" but access to health insurance, self‐rated health, and weekly physical activity were lower in control group |
| Baseline outcome measurements similar | Unclear risk | Some variations in baseline depression and stress outcomes. |
| Protection against contamination | Unclear risk | Not reported except that passwords were changed after the first login while IDs remained the same to prevent the possibility of creating multiple accounts or identities |
Ashton 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: young adult males from the Hunter region of New South Wales (n = 50). Age range: 18–25 years. Recruitment: recruited via flyers distributed around the local university, technical colleges, workplaces, sports clubs and a barber shop. Country: Australia. |
|
| Interventions |
Intervention: multi‐component (n = 26)
‘HEYMAN’ (Harnessing Ehealth to enhance Young men’s Mental health, Activity and Nutrition) is a multi‐ component comprising of, A responsive website, A Jawbone wearable physical activity tracker, One‐hour weekly face‐to‐face sessions at the university, Personalised food and nutrient report comparing intakes to Australian food and nutrient recommendations, A private Facebook discussion group to facilitate social support, A Gymstick™ resistance band, for home‐based strength training, A TEMPlate™ dinner disc to guide main meal portion size for main meal components, to improve eating habits, activity levels, overall well‐being and healthy lifestyle program for men. Control: non‐social media (n = 24) Control participants were asked to continue their usual lifestyle for 3 months and offered the HEYMAN program once follow‐up assessments were completed. |
|
| Outcomes | Feasibility of research procedures (recruitment, randomisation, data collection and retention) and of the intervention components (program usage, attractiveness, comprehension, usability, support, satisfaction and ability to persuade). Physical activity level, diet quality, subjective‐well‐being, weight, fat, mass, skeletal mass, height, BMI, waist circumference, energy intake, self‐reported moderate to vigorous physical activity, fasting total cholesterol, HDL‐cholesterol, LDL‐cholesterol and triglycerides, systolic and diastolic blood pressure, resting heart rate and augmentation index, hazardous drinking, psychological stress, mental health, well‐being. | |
| Equity | High‐income country, Young men not living a healthy lifestyle | |
| Notes | Health behaviours: physical activity level and diet were both reported as primary outcomes. Body function: weight considered most patient‐important compared to other physical outcomes, many of which were biomarkers (BMI, HDL‐cholesterol, triglycerides, etc.). Psychological health: Depression, Anxiety and Stress was considered the most patient‐important outcome reported for this category. Well‐being: subjective‐well‐being was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was generated by a computer based random number algorithm. |
| Allocation concealment (selection bias) | Low risk | Quote: "Complete separation was achieved between the research assistant who generated the randomisation sequence, those who concealed allocation and from those involved in implementation of assignments." |
| Blinding of personnel | Low risk | Quote: "All measurements were performed by trained research assistants who were blinded to group allocation." Randomisation codes were not accessible by those assessing participants or completing data entry. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All measurements were performed by trained research assistants who were blinded to group allocation." Randomisation codes were not accessible by those assessing participants or completing data entry. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Less than 10% lost to follow‐up in both arms. All outcomes seem to be reported but no protocol available. |
| Selective reporting (reporting bias) | Low risk | Primary outcomes from the Trial Registration are not primary outcomes in this report (physical health, diet, well‐being versus feasibility as reported here) ‐‐ this paper reports on the feasibility and preliminary effectiveness for the actual trial which will assess the effects on health. |
| Baseline characteristics similar | High risk | Much higher university education among intervention group, much higher obesity in intervention group. |
| Baseline outcome measurements similar | High risk | There was a significant difference between groups for steps/day at baseline, with the intervention group reporting significantly more steps per day. |
| Protection against contamination | Unclear risk | Not reported |
Bai 2015.
| Study characteristics | ||
| Methods | cRCT | |
| Participants |
Participants: parents of ADHD Children, (n = 89) Age range: 6‐16 years Recruitment: patients and their families were recruited when they came to the hospital and got their assessment. Eligibility: children and adolescents aged 6‐16 years, Diagnosed as having ADHD with diagnoses based on DSM‐IV and then validated with a semi‐structured interview with parents and the child using Barkey's Clinical Diagnostic Interview Scale, First referral to the hospital, Medication prescription with parents agreement on the prescription. Country: China |
|
| Interventions |
Intervention: multi‐component (n = 44) Expert‐guided lecture; parent manual; parent group activities; online community for parents to communicate, share experiences and receive counsel. Control: non‐social media (n = 45) Received general clinical counselling without psychoeducation program. |
|
| Outcomes | Parents knowledge about ADHD, Adherence behaviour (assessed by measuring components of the Theory of Planned Behaviour Model), Medication adherence, ADHD symptoms, Satisfaction with the program. | |
| Equity | Upper middle‐income country, primary caregivers of children diagnosed as having ADHD | |
| Notes | Health behaviours: several measures of medication adherence reported. Medication possession ratio (the percentage of days the patient complied with the prescription in a specific period) was considered the most‐patient important for this category. Body function: not applicable. Psychological health: several ADHD measures reported but were focused on children's psychological health outcomes and therefore were not included in our analysis. Well‐being: not applicable Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: affectional attitude, functional attitude, subjective norms, direct control, indirect control, intention, knowledge, and self‐efficacy were the outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reports quote: "the present study used a cluster randomized control design" but does not describe sequence generation. |
| Allocation concealment (selection bias) | High risk | "Quote The allocation scheme was performed by the primary investigator...The other investigator was informed of the allocation result after recruitment was done." |
| Blinding of personnel | High risk | The allocation scheme was performed by the primary investigator and the other investigator was informed after recruitment. The clinical assistants managed the online community and maintained almost daily interaction with the parents. |
| Blinding of participants | Unclear risk | Participants were aware of their assignment (although unaware of the education materials received by the other group). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessments were reported by parents/participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Reports outcome data for all outcomes measures listed but no protocol is available. |
| Baseline characteristics similar | Low risk | Characteristics were similar. |
| Baseline outcome measurements similar | Low risk | Measures were similar. |
| Protection against contamination | Low risk | "Quote "possible contamination was avoided by arranging the groups' visits to the hospital for separate times" |
Baker 2011.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: women with breast cancer (N = 450) Age range: 50‐60 Recruitment: 1034 women from patient pools at the three sites were approached for study participation in the two experiments; women were approached for participation in either the current experiment or the companion experiment. Eligibility: standard inclusion criteria were used at all sites: women were >17 years old, able to read and understand English, and were within 2 months of a diagnosis of primary breast cancer or recurrence at the time of recruitment. Country: USA |
|
| Interventions |
Intervention: multi‐component CHESS info n = 118, CHESS info+support n = 109, Full CHESS n = 111.
The first CHESS condition (CHESS Information) received only the Information services; the second condition (CHESS Information and Support) received both the Information and Support services, while the third condition received all three types of CHESS services (Information, Support, and Coaching: Full CHESS). Control: non‐social media (n = 112) Internet Only |
|
| Outcomes | Cancer Information Competence, Emotional processing, Functional well‐being, Wisconsin social support scale, Constructs or outcomes that were exploratory in nature (e.g. measures of quality of life comprising physical health system and mobility items), Healthcare competence, Positive coping, Breast cancer concerns, Satisfaction with professional. | |
| Equity | High‐income country. Breast cancer patients | |
| Notes | Means provided with no SD, SE, or confidence intervals. Authors were contacted but reported that these data have been archived. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised via a computer‐generated list. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Research staff informed the patient about the resources to which she had been randomised and asked whether she needed a laptop computer or Internet service. |
| Blinding of participants | High risk | Research staff informed the patient about the resources to which she had been randomised and asked whether she needed a laptop computer or Internet service. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Patient withdrawal rates were low at 8% |
| Selective reporting (reporting bias) | High risk | Data collected at 12 months post‐treatment are not reported. |
| Baseline characteristics similar | Low risk | The groups did not differ significantly except for income (P = 0.025), with one condition (Information + Support) showing slightly lower incomes than the Full CHESS condition. These differences were not significant when using Shaffer’s correction for multiple tests |
| Baseline outcome measurements similar | Unclear risk | Patient outcomes not measured prior to the intervention |
| Protection against contamination | Unclear risk | Not reported |
Bantum 2014.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: cancer survivors,(n = 352) Age range: 18 years of age or older Recruitment: from oncology clinics, a tumour registry, as well as through online mechanisms, such as Facebook and the Association of Cancer Online Resources (ACOR). Eligibility: cancer survivors were eligible if they had completed their primary cancer treatment from 4 weeks to 5 years before enrolment, diagnosis with only one cancer and no recurrence, access to the Internet and ability to read English. Country: USA |
|
| Interventions |
Intervention: social media only (n = 176)
Six weeks online program (Examples include improving diet by making healthier food choices, increasing exercise, stress management via relaxation training, improving communication with healthcare providers) etc. patient education course adopting the underlying principle that people with similar health conditions can help each other improve their health behaviours. Control: non‐social media (n = 176) No access to the intervention. |
|
| Outcomes | Fatigue, insomnia, minutes per week of physical activity (categorised as strenuous plus moderate aerobic, strenuous aerobic, moderate aerobic, mild aerobic, and stretching), servings of fruits and vegetables eaten per week, and depression, website use. | |
| Equity | High‐income country | |
| Notes | Health behaviours: exercise and weekly fruit/vegetable intake were both stated as primary outcomes and were both selected for this category as per our outcome selection criteria. Several exercise outcomes were reported ‐ minutes per week of strenuous or moderate aerobic exercise was selected for this category as it was considered the most patient‐important. Body function: insomnia was the only physical health outcome reported and was classified as such because the questions in the Women’s Health Initiative Insomnia Rating Score were related to falling in staying asleep. Psychological health: depression was the only psychological health outcome reported and was measured using a validated tool. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Once 40 to 50 participants had completed their baseline questionnaire, they were numbered in the order of completion and then randomised, using a random number table, half to treatment and half to wait‐list control. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported ‐ all measures are self‐report related to exercise and diet behaviours |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition low, predictors for dropout provided and there were no differences between groups. |
| Selective reporting (reporting bias) | High risk | Protocol has additional outcomes not discussed in this paper including health care utilisation, quality of life, and interaction with oncologists |
| Baseline characteristics similar | Low risk | With the exception of age, no significant differences were found among the two groups. Double the number of non‐Hodgkins lymphoma patients in control group. |
| Baseline outcome measurements similar | Low risk | Additionally, there were no significant differences between the control and treatment groups on all outcomes measures at baseline Depression scores higher in control group at baseline, Minutes per week of strenuous exercise and stretching higher among intervention group, but absolute changes reported |
| Protection against contamination | Low risk | Not reported but participants are cancer survivors across multiple sites and recruited via tumour registries, Facebook etc. |
Bender 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: overweight Filipino Americans with type 2 diabetes (N = 45). Age range: ≥18 years of age, overall mean (SD) age in years was 57.6 (9.8). Recruitment: recruited from the San Francisco Bay Area primarily through word of mouth, community events, and snowball methods. Online recruitment strategies included San Francisco Bay Area Craigslist, a dedicated study Facebook website, and an institutional website. Eligibility: self‐identified Filipino, ≥18 years, BMI >23 kg/m2 for Asians, physician diagnosis of T2D (non‐insulin dependent), own a smartphone, tablet, or laptop with Internet access, and English language proficient. Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 22) Philipino Americans Go4Health (PilAm Go4Health) 6‐month intervention with access to private Facebook group for the first 3‐months for virtual social support, coaching, and weekly education topics. For the total 6‐month intervention, participants received a Fitbit accelerometer and associated mobile app for health behavior tracking (steps, food/calories, and weight) and attended monthly in‐person meetings for tailored feedback, coaching, and support. Control: non‐social media control (n = 23) Active waitlist control condition. Waitlist participants received Fitbit accelerometer and training only. |
|
| Outcomes | Feasibility, adherence, percentage weight change, BMI, waist circumference, plasma glucose, HbA1c, step counts. | |
| Equity | High‐income country, Filipino Americans, diagnosed with Type 2 Diabetes. | |
| Notes | Health behaviours: step counts was the only outcome reported for this category.
Body function: percentage weight change was reported as a secondary outcome by study authors and all other physical function outcomes were considered other outcomes.
Psychological health: not applicable.
Well‐being: not applicable.
Mortality: not applicable.
Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | "Quote "Due to the nature of a lifestyle intervention, only the lab technicians and statistician were blinded, but research investigators, staff, and participants were not". |
| Blinding of participants | High risk | "Quote Due to the nature of a lifestyle intervention, only the lab technicians and statistician were blinded, but research investigators, staff, and participants were not". In phase 2, at the 3‐month office visit, wait‐list control participants were transitioned to receive the PilAm Go4Health intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The lab technicians and statisticians were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no missing data for the 2 groups. |
| Selective reporting (reporting bias) | High risk | Missing dietary fat and sugar‐sweetened beverage intake which are outcomes reported in protocol. Primary outcome was originally secondary. |
| Baseline characteristics similar | Low risk | "Quote "The only sociodemographic variable with a difference between the 2 groups was "years lived in the United States" |
| Baseline outcome measurements similar | Low risk | Outcome measures similar at baseline. |
| Protection against contamination | Unclear risk | Private Facebook group and then the waitlist control group received the intervention at 3 months. Unclear whether in‐person visits could lead to contamination. |
Booth 2018.
| Study characteristics | ||
| Methods | ITS | |
| Participants |
Participants: young adults who received outpatient mental health services (N = 839,544 (primary health care mental health visits) and 142,122 (outpatient psychiatric visits)) Age range: 10 to 24 years of age (only those 18 to 24 years of age included) Recruitment: OHIP billing records, all Ontario residents are identifiable through healthcare administrative records held by the Institute for Clinical Evaluative Sciences (ICES). Eligibility: between 10‐24 years of age with valid OHIP status and accessed outpatient mental health services from Jan 1 2006 ‐ Dec 31 2015 in Ontario. Country: Canada |
|
| Interventions |
Intervention: social media only Bell Let's Talk campaign aimed at increasing dialogue on mental health and support mental health awareness, each mention of the campaign led to a donation of $0.05 CAD to mental health research and programming. Primary goal was to invite Canadians to talk about mental health in an effort to break down stigma. Control: not applicable. |
|
| Outcomes | Rate of outpatient mental health visits to primary health care or psychiatric services and new mental health visits to primary health care or psychiatric services. | |
| Equity | High‐income country, mental health service utilisation. | |
| Notes | Health behaviours: mental health visits to primary health care or psychiatric services were reported as the primary outcomes. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
Boyd 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants:mothers with postpartum depression (N = 24). Age range: parents ≥15 years of age with a child between 1 and 3 months old. Mean (SD) parents age in years was 26.4 (1.9) for the intervention group and 26.3 (1.8) for the control group. Recruitment: three urban paediatric primary care clinics in areas with high proportion of African American and recent immigrant patients. Recruited using advertisements at participating practices and through direct referrals from clinicians. Eligibility: at least 15 years old, have a child between 1 and 3 months old, have Internet access on a computer or a smartphone, and screen positive for depressive symptoms. Country: USA |
|
| Interventions |
Intervention: social media only (n = 12) Parents Interacting with Infants social media intervention included eight weekly sessions with topics focused on depression psychoeducation and behavioural activation, infant temperament (personality), play, feeding, safety, sleep, parent–child interactions (laughter) and reading. Each weekly session included a narrated PowerPoint presentation, a video clip, questions for sharing experiences, an exercise, follow‐up questions and a summary. The content was uploaded on the Facebook secret user group in three instalments over the course of a week to allow participants the time to read the material, practise the exercises and post comments/ answers to the questions posed by the facilitator. Control: non‐social media control (n = 12) The in‐person intervention was held weekly over 8 weeks with the same weekly topics as the social media group. Each session began with an introduction to the topic, series of questions, dyadic activity, and a wrap‐up and discussion of homework. Weekly reminder calls and/or texts were sent about the upcoming session. |
|
| Outcomes | Feasibility, severity of depression symptoms, and perceptions of parental competence. | |
| Equity | High‐income country, area with a large number of African American and recent immigrant families who live below the poverty line, mothers with postpartum depression. | |
| Notes | Health behaviours: not applicable. Body function: not applicable. Psychological health: severity of depression symptoms was the only outcome reported for this category. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: perceptions of parental competence was the only outcome reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Quote "Randomisation sequences were generated using computer‐generated numbers prior to enrolment with assignments contained in sequential sealed opaque envelopes." |
| Allocation concealment (selection bias) | Low risk | "Quote "Randomisation sequences were generated using computer‐generated numbers prior to enrolment with assignments contained in sequential sealed opaque envelopes." |
| Blinding of personnel | High risk | Trial registration describes this 'open label' |
| Blinding of participants | High risk | Trial registration describes this 'open label' |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Trial registration describes this 'open label' |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No attrition in intervention group but 30% of control group did not complete follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes listed in trial registration do not match those in the published report, e.g. acceptability, attendance at 6 or more sessions, feasibility, change in parenting stress, change in social support, change in parenting discipline. |
| Baseline characteristics similar | Unclear risk | "Quote "The in‐person group was more likely to have a family income of <$15,000 than the social media group" which may have influenced participant ability to adhere to the intervention. |
| Baseline outcome measurements similar | High risk | "Quote "Mothers in the in‐person group reported significantly higher levels of parenting competence than the mothers in the social media group. Our results showed that the mean total depression scores on the BDIII for social media group was within the moderate range of clinical severity; however the score for the in‐person group fell within the severe range." |
| Protection against contamination | Unclear risk | Secret Facebook group. No other details provided. |
Bull 2012.
| Study characteristics | ||
| Methods | cRCT | |
| Participants |
Participants: AfricanAmerican and Latino youth (n = 652) Age range: 16‐25 years Recruitment: individuals (seeds) recruited in multiple settings (online, via newspaper ads and face‐to‐face) were asked to recruit three friends, who in turn recruited additional friends, extending three waves from the seed. Seeds and waves of friends were considered networks and exposed to either the intervention or control condition. Eligibility: aged 16–25 years, a U.S. resident, owner of a Facebook page, willing to complete study behavioural risk assessments, and able to read and write in English" ‐‐ Therefore “liking” the intervention or control Facebook page was an eligibility criterion Country: United States |
|
| Interventions |
Intervention: Social media only (n = 340) Just/Us, a Facebook page developed with youth input, which included 8 broad topics related to sexual health Control: active social media comparator (n = 312) Facebook page sharing what was interesting in the news to those aged 18 –24 years. The intent was to avoid sexual health content. |
|
| Outcomes | 1) Condom use at last sex, 2) proportion of sex acts protected by condoms in the past 60 days.1) number of sex partners in the past 2 months, 2) intention to use condoms at the next sexual encounter, 3) whether the most recent sex partner was considered a “main” or primary partner or a casual partner, 4) whether participants were drunk or high during their last sexual experience;5) whether their friends on Facebook were likely to use condoms (peer norms for condom use); 6) whether they were confident they could use condoms (self‐effocacy for condom use). | |
| Equity | High‐income country, African‐ Amercian and Latino youth | |
| Notes | Health behaviours: condom use was used in a sample size calculation and was considered to be more patient‐important than other sexual health behavioural outcomes reported. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: condom intention, condom norms, and condom self‐efficacy were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Does not report how sequence was generated |
| Allocation concealment (selection bias) | High risk | These participants were considered seeds and assigned at random to the 18 24 News page (control, n 312) or the Just/Us page (intervention, n 340) and asked to recruit their Facebook friends to participate. Referrals would have been known at allocation (602 in intervention arm vs 324 in control) |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Quote "Just under 70% of the sample completed a 2‐month follow‐up (439 controls, 69%; and 653 intervention, 69%) and retention declined to 59% for controls at 6 months (n377) and 45% for intervention participants (n427). A total of 75% of participants completed any follow‐up (i.e., either 2 or 6 months; 484 control participants and 711 intervention participants). The number completing a 6‐month assessment in the 1824 News group was significantly greater than those from Just/Us at 6 months." |
| Selective reporting (reporting bias) | Low risk | As reported in trial registration |
| Baseline characteristics similar | High risk | Significant differences at age and sexual history at baseline (as well as some ethnicity, geographical regions) |
| Baseline outcome measurements similar | Low risk | No significant differences |
| Protection against contamination | High risk | "Quote "Finally, at the 6‐month follow‐up, participants were asked to indicate whether they “liked” numerous Facebook pages, embedding Just/Us among three other choices to assess contamination—if controls “liked” Just/Us in large numbers, there would be a concern that they had been exposed to intervention content. There were 43 participants in the control group (6.8%) who reported “liking” Just/Us; this should be compared to 100% of the participants in the intervention arm who “liked” Just/Us (because liking the page was a condition of eligibility as noted above)" |
Castillo 2013.
| Study characteristics | ||
| Methods | CBA | |
| Participants |
Participants:Trauma Patients (n=251) Age range: 18 ‐69 years Recuitment:Patients admitted to The R Adams Cowley Shock Trauma Center (STC) at the University of Maryland in the year before implementation of the TSN and enrolled in the study served as the control cohort (n = 125). Patients admitted to the hospital in the year following implementation of the TSN and enrolled into the study served as the experimental cohort (n = 126). Eligibility: Discharged alive, ages 18 years to 69 years, no serious brain injury as defined by an Abbreviated Injury Scale (AIS) score head injury of severity greater than 3, English speaking and not in jail or homeless, sustained one ormore lower/upper‐extremity injuries, and access to a computer at home, work, or school, and computer literate (defined as having used the computer in the past year to e‐mail someone or to order something over the Internet). Country: United States |
|
| Interventions |
Interventions: Multi‐component (n=126) Received the same standard of care, plus access to the TSN (Trauma Survivors Network) program. TSN consists of peer support (including internet peer support), self management, information and resources, and provider training Control: No interactive social media (n=125) recieved the same standard of care, no access to TSN program |
|
| Outcomes | Outcomes evaluated at 6 months included depression, anxiety, health status Other outcomes measured were self‐efficacy and patient activation (an aggregate concept encompassing broad areas of beliefs, motivation, locus of control, and self‐efficacy), and Self‐reported use of services | |
| Equity | High income country, Patients admitted to The R Adams Cowley Shock Trauma Center | |
| Notes | Health behaviours: Not applicable. Body function: Physical health status was the only outcome reported for this category. Psychological health: Both depression and anxieity were selected for this category as both were reported as primary outcomes. Well‐being: Not applicable. Mortality: Not applicable. Adverse effects: Not applicable. Secondary outcomes: Self‐efficacy and pateint activation were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled before‐after |
| Allocation concealment (selection bias) | Unclear risk | All patients received the intervention if enrolled after its implementation. The control group participants were enrolled before the intervention was implemented. |
| Blinding of personnel | High risk | Personnel would be aware of implementation |
| Blinding of participants | Unclear risk | Participants consented to take part but unclear whether they knew that the program was new and whether that would have an effect |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes were self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 75% followup, reasons for attiriton not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol but all outcomes reported in the methods and study aims were reported in the results. |
| Baseline characteristics similar | High risk | More men in the treatment group, treatment group had higher education |
| Baseline outcome measurements similar | High risk | social support scores for friends, family, and total were higher for the control group at baseline |
| Protection against contamination | High risk | "Although most of the follow‐up interviews for the control group occurred before TSN implementation, a few patients who were difficult to reach received follow‐up interviews after TSN implementation activities began. There is a possibility that some of these control patients may have been inadvertently exposed to TSN activities if they made return visits to the hospital." |
Cavalcanti 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: mothers with a newborn child (N = 251 mother‐child pairs). Age range:over 18 years of age. Most women were between 20 and 34 years of age (78% of the intervention group and 77.3% of the control group). Recruitment: maternity ward of the Hospital Universitário Lauro Wanderley. Eligibility: gave birth during the recruitment period, between August 2016 and February 2017, were over 18 years of age, knew how to read and write, used the online social network Facebook, and were discharged from the hospital together with their child. Country: Brazil |
|
| Interventions |
Intervention: multi‐component intervention (n = 123) Routine guidance from care team, a booklet on the practice of breastfeeding with explanations, and inclusion in a closed group called Projeto Amamenta Mamãe (Mama Breastfeeding Project) on Facebook (tagged in a post, corresponding to a topic of the booklet once per week). Control: non‐social media control (n = 128) Routine guidance from care team and a booklet on the practice of breastfeeding with explanations. |
|
| Outcomes | Exclusive breastfeeding | |
| Equity | Upper middle‐income country, mothers | |
| Notes | Health behaviours: exclusive breastfeeding was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Quote "One nutritionist of the project team performed the random assignment of the mother‐child pairing in the CG or IG based on a list of random, binary numbers drawn up before the beginning of the study, using the function 'random between 0 and 1' of the Microsoft Excel software" |
| Allocation concealment (selection bias) | Unclear risk | "Quote "The correspondence of the recruitment order with the order of the numbers from the predefined list determined in which group the woman would be assigned, with the value of '0' being assigned to the CG and '1' to the IG". |
| Blinding of personnel | High risk | "Quote "One limitation of this randomised study was that the research team knew which participants were included in each group. The study could not be double‐blinded because of the health professionals' need for communication,both over the phone with all women, and through the virtual online social network with the women in the IG." |
| Blinding of participants | Low risk | "Quote "The participant mothers were not aware that there were two groups in the study and also did not know to which group they had been assigned" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Self‐reported outcome, quote: "The participant mothers were not aware that there were two groups in the study and also did not know to which group they had been assigned" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants analysed ‐ intervention group had more losses at follow‐up with reasons including refusal, medical contraindication, death of baby |
| Selective reporting (reporting bias) | Unclear risk | No protocol available, all outcomes as reported in methods. |
| Baseline characteristics similar | High risk | Characteristics were similar but the number of prenatal consultations was significantly higher in the intervention group which may influence breastfeeding rates. |
| Baseline outcome measurements similar | Low risk | No baseline outcomes to assess |
| Protection against contamination | Unclear risk | Closed Facebook group. No other details provided. |
Cavallo 2012.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: female undergraduate students ( n =134) Age Range: < 25 years Recruitment: female undergraduate students (n = 134) at a large Southeastern public university were directed to an online screener through print and electronic communications including e‐mail, Facebook, and Twitter. Eligibility: currently enrolled female undergraduates, aged < 25 years, reported < 30 minutes of daily physical activity, and > 30 minutes of daily use of Facebook. Country: USA |
|
| Interventions |
Intervention:mMulti‐component (n = 67) Access to (INSHAPE) website, which provided educational information related to physical activity and a self‐monitoring tool that allowed participants to set goals, track their daily physical activity, and view a chart depicting their progress relative to their goal. Invited to join a Facebook group using their existing Facebook account for social support. Control: Non‐social media (n = 67) Access to a limited version of the INSHAPE website, which excluded self‐monitoring, and received e‐mails throughout the study with links to the same news stories related to physical activity that were provided to the Facebook group. |
|
| Outcomes | Social support for physical activity and self‐reported physical activity.The Facebook Intensity Scale was used to measure participants’ overall engagement in Facebook. A post‐intervention questionnaire was used to measure unobservable behavior in the Facebook group, such as visiting but not posting to the group, and intervention participants’ attitudes toward the Facebook component of the intervention. | |
| Equity | High‐income country. Female undergraduate students | |
| Notes | Health behaviours: physical activity (total kcal) was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: perceived social support (companionship) was the only outcome reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | From dissertation: "Computer generated permuted‐block randomization was used to randomize participants into two groups" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Blinding of personnel not possible since a moderator posted to Facebook and sent emails to both groups. |
| Blinding of participants | Unclear risk | Not reported ‐ unclear whether participants knew whether they were assigned to intervention or control |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes were self‐reported but blinding of participants not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | low attrition, ITT analysis, reasons for attrition described |
| Selective reporting (reporting bias) | Low risk | No protocol but all outcomes discussed in thesis and separate papers are the same |
| Baseline characteristics similar | High risk | Control group included those with higher Facebook intensity scores who were more likely to be completers than non‐completers. |
| Baseline outcome measurements similar | Unclear risk | not reported |
| Protection against contamination | Unclear risk | Not reported and all participants were female students at one university |
Chai 2018.
| Study characteristics | ||
| Methods | CBA | |
| Participants |
Participants: migrant workers/ smokers (n = 315) Age range: ≥16 years old Recruitment: four manufacturing factories were selected from the list of factories provided by the government and were allocated to intervention and control groups according to the willingness to cooperate of these factories. Eligibility: labour‐intensive manufacturing factories, the managers should be willing to adhere to the planned intervention.In each selected factory, we recruited migrant workers who were ≥16 years old and willing to participate in the study Country: China |
|
| Interventions |
Intervention: multi‐component (n = 149) Participants in the intervention factories (n = 2) received adapted 5A group counselling (Ask, Advise, Assess, Assist, Arrange and a 5Rs Relevance, Risks, Rewards, Roadblocks, Repeated),regularly supported by social‐media (WeChat) and traditional health education approaches in improving migrant workers’ knowledge of smoking and anti‐smoking attitudes to stop smoking attitudes in migrant workers. Control: No intervention (n = 166) The control factories (n = 2) were not provided any new intervention. |
|
| Outcomes | Change of smoking rate among migrant workers based on the salivary cotinine concentrate and changes in tobacco related knowledge and attitudes. | |
| Equity | Upper middle‐income country. Migrant workers | |
| Notes | Health behaviours: smoking rate was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: tobacco knowledge and tobacco attitude were the only outcomes reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Four manufacturing factories were selected from the list of factories provided by the government and were allocated to intervention and control groups according to the willingness to cooperate of these factories. Allocation of participants by factory allocation. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Quote "The laboratory technicians were blind to participants’ smoking status" but no mention of blinding for arm |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar numbers were lost to follow‐up in both intervention and control groups. Intention‐to‐treat (ITT) approach. "Quote "A multiple imputations by chained equation (MICE) analysis was used to correct for bias in the intervention effect, under the assumption that data were missing at random given the observed covariates. Analyses followed the intention‐to‐treat (ITT) principle, and all migrant workers that were recruited and provided data at baseline were included in the effectiveness analysis of this intervention." |
| Selective reporting (reporting bias) | High risk | Paper states "quote "study was conducted in accordance with the study protocol" but the protocol includes additional outcomes e.g. the Satisfaction rate was to be assessed through a questionnaire and in‐depth interviews. |
| Baseline characteristics similar | High risk | The intervention arm had a higher proportion of participants who were male, aged over 36 years old, had a monthly income of 2000–4000 Yuan RMB. |
| Baseline outcome measurements similar | High risk | At the baseline, the smoking rate based on the salivary cotinine was higher in the intervention arm than the control arm. The average daily cigarette consumption was also higher in the intervention arm. |
| Protection against contamination | Unclear risk | It is possible that participants in the control group could have been exposed to intervention components (e.g. join the WeChat room, saw the educational materials‐poster, leaflet etc.). |
Chen 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: hospital patients diagnosed with Type 2 Diabetes (N = 90). Age range: 19‐64 years of age. Recruitment: patients with T2DM admitted to The Linyi Central Hospital. Eligibility: patients who were diagnosed with T2DM in accordance with the 1999 WHO guidelines, the duration of T2DM is no more than 10 years, the patient had self‐care ability and was able to use WeChat on a mobile phone independently. Country: China |
|
| Interventions |
Intervention: social media only (n = 45) Interactive health education based on the WeChat platform. Patients could subscribe to the WeChat public service account and join the patient support group by scanning a QR code. The public WeChat group included disease education, daily life guidelines, and patient consultation with at least 2 popular science articles, audios, or videos on T2DM every week. Consultations were at fixed times every week with lectures and public activities being scheduled regularly. Each patient was encouraged to share experiences in the WeChat group. Control: Non‐social media control (n = 45) Routine health education, dietary instructions, and blood glucose monitoring with telephone or clinic visits every 2 weeks. |
|
| Outcomes | Blood glucose level (fasting blood glucose, 2‐hour postprandial blood glucose, glycated haemoglobin), medical coping modes questionnaire score (coping modes of confrontive, avoidant and resigned), summary of diabetes self‐care activities measure score (self‐management ability of diet, medication, blood glucose testing, exercise and foot care), health status questionnaire score (quality of life), nursing satisfaction. | |
| Equity | Upper middle‐income country, hospital patients with a diagnosis of type 2 diabetes. | |
| Notes | Health behaviours: not applicable. No baseline data reported for Summary of Diabetes Self‐Care Activities. Body function: glycated haemoglobin (HbA1c) for blood glucose level has a high specificity in diagnosing T2DM and was therefore, considered the most patient‐important outcome for this category. Psychological health: not applicable. Well‐being: quality‐of‐life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: only confrontational coping was extracted as it is most related to behaviour change. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The patients were randomly divided into a control group and an experimental group |
| Allocation concealment (selection bias) | Unclear risk | The patients were randomly divided into a control group and an experimental group |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All those randomised are analysed but attrition is not described |
| Selective reporting (reporting bias) | Unclear risk | No protocol available, outcomes reported as described in methods |
| Baseline characteristics similar | Low risk | Characteristics similar at baseline. |
| Baseline outcome measurements similar | Low risk | Outcome measures are similar at baseline |
| Protection against contamination | Unclear risk | Methods for protection against contamination not specified. Was not clear if the WeChat group was controlled. Hypothetically speaking, anyone could scan the QR code and subscribe to the WeChat public service account and join the patient support group. |
Cheung 2015.
| Study characteristics | ||
| Methods | cRCT | |
| Participants |
Participants: smokers (n = 136) Age range: 18 or older Recruitment: all participants were clients of the Tung Wah Group of Hospitals Integrated Centre of Smoking Cessation (ICSC) in China Hong Kong. At 8‐week follow‐up during telephone or face‐to‐face counselling, clients were asked by the ICSC counsellors if they had quit. Eligibility: self‐reported quitters were then screened with the criteria for eligibility, including (1) daily smoker at first entry to the ICSC, (2) aged 18 years or older, (3) received 3 to 8 smoking cessation counselling sessions provided by the ICSC, (4) reported tobacco abstinence for at least 7 days, (5) able to communicate in Cantonese and read and write Chinese, (6) had a mobile phone through a local network, and (7) were able to access the Internet by mobile phone Country: China |
|
| Interventions |
Intervention: multi‐component WhatsApp (n = 42), Facebook (n = 40) a) What's app and self‐help booklet and (b) Facebook and self help booklet (22‐page booklet related to quitting and healthy diet). Control: non‐social media (n = 54). Received only the same self‐help booklet and were advised to contact ICSC’s counsellors when they faced high‐risk situations or had smoking lapses (usual care). |
|
| Outcomes | Self‐reported relapse rate, which was defined as the proportion of participants who self‐reported smoking at least 5 cigarettes in 3 consecutive days in the past 2 months at the 2‐month follow‐up. 4‐month relapse rate at 6‐month follow‐up. Secondary outcomes (1) self‐reported any smoking incidence (i.e, smoking lapse), 2) self‐reported smoking in the past 7 days, and 3) biochemically‐validated abstinence at the 2 follow‐ups. | |
| Equity | Upper middle‐income country | |
| Notes | Health behaviours: smoking relapse rate was selected for this category as it was reported as a primary outcome and was considered more patient‐important than other health behaviour outcomes. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: smoking self‐efficacy was the only outcome of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation based on week of recruitment but each week randomised using computer‐generated sequence |
| Allocation concealment (selection bias) | High risk | Each week was randomised to group A, B, and C using numbers generated on a website for generating random variables. The ICSC counsellors who screened and enrolled participants were notified of the group allocation on Monday of each recruitment week. Participants were not aware of the allocation sequence. |
| Blinding of personnel | Low risk | Interviewers were blinded to the group assignment |
| Blinding of participants | Low risk | All participants received a specific relapse prevention intervention, but they did not know what the other interventions were. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Quote "All assessors of outcomes were blinded to the RCT group of each participant." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 86.8% were successfully followed at 2‐month follow‐up and the overall retention rate at 6‐month follow‐up was 73.5%. The reasons for loss to follow‐ups were (1) unable to reach via telephone, (2) refusal to follow‐up, and (3) incomplete survey. |
| Selective reporting (reporting bias) | Low risk | Outcomes as reported in trial registration NCT02007369 |
| Baseline characteristics similar | High risk | Facebook group younger than other groups and more likely to be married, and have higher income |
| Baseline outcome measurements similar | High risk | Higher daily consumption of cigarettes among controls, lower attempts to quit smoking previously |
| Protection against contamination | Unclear risk | Not reported |
Cobb 2014.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: U.S.‐based adults (n = 1503) Age range: 18 and older Recruitment: advertisements were placed within Facebook, running 82 different ads over 47 days. Advertisements did not mention the trial itself. Individuals registered for the product using Facebook‐enabled authentication, which provided their name, e‐mail address, and information on their Facebook friends. Participants were recruited to take part in the trial during product registration. Eligibility: adults living in the USA who were age 18 or older (19 or older if residing in Alabama or Nebraska). Country: USA |
|
| Interventions |
Intervention: Social media only (n = 752) A multimodal e‐mail‐, web‐, and mobile‐based intervention (Daily Challenge), in which participants receive daily suggestions of small health actions that they complete in a social environment. Control: non‐social media (n = 751) A traditional weekly health newsletter served as control. |
|
| Outcomes | Overall well‐being, Social support | |
| Equity | High‐income country | |
| Notes | Health behaviours: not applicable. Body function: not applicable. Psychological health: not applicable. Well‐being: well‐being was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: social support was the only outcome reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Quote "randomization was automated and gender‐stratified (permutation within strata)." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Low risk | Investigators were blinded to group assignments. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition, although ITT used. Unclear whether those who were lost are similar to completers. Higher unsubscribe rates in intervention group. |
| Selective reporting (reporting bias) | Low risk | As reported in trial registration NCT01586949 |
| Baseline characteristics similar | Low risk | No significant differences between groups |
| Baseline outcome measurements similar | Low risk | Baseline similar but slightly higher for intervention participants |
| Protection against contamination | High risk | "Quote "Control participants received a generic health newsletter by e‐mail once a week (no social interactivity or calls to action) and otherwise had no access to the Daily Challenge system" BUT "Daily Challenge is a freely accessible e‐mail‐, web‐, and mobile‐ based intervention. Members are encouraged to recruit individuals from their real‐life social network and connect with them within Daily Challenge." |
Coffeng 2014.
| Study characteristics | ||
| Methods | cRCT | |
| Participants |
Participants: office employees from a financial service provider (n = 412)
Age range: ≥18 years Recruitment: interviews with stakeholders, with the main aim to specify current physical activity and relaxation behaviour of the target population. Questionnaires, which were distributed among the target population to affirm the results of the interviews with the stakeholders, regarding physical activity and relaxation behaviour. Focus‐group interviews, in which the key determinants of physical activity and relaxation behaviour during work hours of the target population were identified. Eligibility: employees (≥18 years), working at the Dutch financial service provider. For this study, team leaders and their employees from 19 departments are eligible to participate. inclusion criterion of not being on sick leave for more than four weeks. Country: the Netherlands |
|
| Interventions |
Intervention:mMulti‐component (Social environment n = 118, Physical environment n = 96, Physical and social environment n = 92) Participants were allocated to the combined social and physical interventions, to the social intervention only, to the physical intervention only (not extracted). Social environment intervention consisted of Group Motivational Interviewing (GMI) (supported by social media platform) derived from Motivational Interviewing (MI), while Vitality in Practice (VIP) zones were created: (1) the VIP Coffee Corner Zone (2) the VIP Open Office Zone (3) the VIP Meeting Zone and (4) the VIP Hall Zone Control: no intervention.(n = 106) |
|
| Outcomes | Need for recovery,1) work‐related stress (validated), 2) small breaks, 3) physical activity, 4) sedentary behaviour | |
| Equity | High‐income country, Employees of a financial service provider | |
| Notes | Health behaviours: physical activity (moderate) was the only outcome reported for this category. A global score was not provided, therefore moderate‐to‐vigorous PA was prioritised as per our criteria. Body function: not applicable. Psychological health: need for recovery selected over work related stress as it was reported as a primary outcome and used in a sample size calculation. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | From protocol: "Quote "Within these strata, the departments will be randomized to GMI or no GMI by means of tossing a coin." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | "Quote "Blinding of the participants and intervention providers for the social environment intervention was impossible, although none of them had received information about our design involving three intervention groups." |
| Blinding of participants | High risk | "Quote "Blinding of the participants and intervention providers for the social environment intervention was impossible, although none of them had received information about our design involving three intervention groups." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Differences in reasons for attrition between groups not reported |
| Selective reporting (reporting bias) | High risk | Some outcomes mentioned in the protocol are not reported (e.g. absenteeism, work performance). PA listed as primary outcome in trial registry |
| Baseline characteristics similar | Low risk | Differences regarding age, gender, education, marital status, ethnicity, working hours, general health, job demands, supervisor support were observed between the intervention groups and control group. However, among the participants, males were slightly over represented (60%) and the majority was highly educated (57%). |
| Baseline outcome measurements similar | High risk | Control group had higher light and moderate physical activity at baseline and combined group had lower active commuting. social environment group had lower physical activity at work |
| Protection against contamination | Low risk | Blinding of the participants and intervention providers for the social environment intervention was impossible, although none of them had received information about our design involving three intervention groups. |
Dadkhah 2014.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: university students (n = 216)
Age range: 17 to 22 years Recruitment: recruitment strategies included publishing announcements on Today@Colorado State University (a convenient, one‐stop source for campus announcements at http://www.today.colostate.edu); sending e‐mails through different students Listserv; posting flyers throughout campus, including in freshmen residence halls and at the door of freshmen classes; presenting the information in freshmen classes; and spreading by word of mouth. The majority of participants were recruited from six recruitment stations run by volunteer nutrition or health and exercise students (mainly seniors) at six different dining halls during mealtimes. Eligibility: healthy, full‐time, first‐year students admitted to Colorado State University in 2012 who were from 17 to 22 years of age at the time of the recruitment Country: USA |
|
| Interventions |
Intervention: social media only (n = 115) CSU Fit (intervention group) Facebook page. CSU Fit was an experimental pretest‐posttest to attenuate weight gain in first‐year CSU students with a primary focus on increasing their walking by 2000 steps/day, or decreasing their energy intake by 100 Kcal/d. CSU Fit included a Facebook page component, group sessions, and feedback designed to prevent weight gain in first‐year students of CSU, with a 7‐month follow‐up. Control: non‐social media (n = 101) The Association for Student Activity Programming (ASAP) at CSU (control group) Facebook page |
|
| Outcomes | Physical activity; dietary intake (calorie, total fat, saturated fat, MUFA, PUFA, trans fat, protein, carbohydrate, dietary fibre, sugar, cholesterol, Vitamin A, Vitamin C, sodium, calcium); Weight ‐ body composition, including percentage of body fat (percentage BF), fat mass (FM) , and fat‐free mass (FFM) waist, hip, and thigh circumferences triceps skinfold thickness; Systolic and diastolic blood pressures; daily physical activity other than walking; self‐efficacy (combined self‐efficacy; nutrition and physical activity knowledge; combined self‐efficacy; physical activity; self‐efficacy; and healthy eating self‐efficacy) and satisfaction | |
| Equity | High‐income country, college students | |
| Notes | Health behaviours: both dietary intake and physical activity (total leisure time PA) were selected for this category as both were reported as primary outcomes. Body function: weight was considered to be the most‐patient important physical health outcome reported. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy (combined) was selected over other self‐efficacy outcomes because it provided a total score, per our criteria. Knowledge (nutrition and PA) was the only other outcome of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Three participants in the control group 54 joined the CSU Fit page on Facebook without invitation; thus, the researcher later assigned them to the intervention group. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Approximately 25% attrition in each group, no reasons reported. Baseline characteristics for the completers and dropout participants were analysed for potential attrition bias and none was found |
| Selective reporting (reporting bias) | Unclear risk | No protocol but all outcomes reported in methods reported in results |
| Baseline characteristics similar | Low risk | The intervention and control groups were not significantly different in ethnicity at baseline, with the exception that there were more Hispanic‐Latino and fewer White participants in the control group. Age similar, gender similar. |
| Baseline outcome measurements similar | Unclear risk | Not reported |
| Protection against contamination | High risk | Considering that both intervention and control groups were recruited from CSU, cross‐contamination was possible. Three participants in the control group joined the CSU Fit page on Facebook without invitation; thus, the researcher later assigned them to the intervention group |
Dahl 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: healthy pregnant women (N = 140). Age range: 20‐35 years of age. Recruitment: recruited through paid, targeted advertisements on Facebook and Twitter. Eligibility: singleton pregnancy, within the first half of pregnancy (< 20 weeks gestation), ages 20‐35 years, pre‐pregnancy BMI greater than 18.5 kg/m2 , current resident of the USA, owner of a smartphone, owner of a bathroom scale, able to read and speak English, willing to download and use a mobile app for the duration of the intervention (12 weeks), access to regular and consistent Wi‐Fi or a data plan. Country: USA |
|
| Interventions |
Intervention: multi‐component intervention (n = 77) Healthy Eating and Physical Activity (HEPA) intervention delivered on MakeMe mobile app and website. The app used 12 weekly group‐based challenges to reach a common customisable goal. The website included an outcome tracking tool, a leader board, weekly pregnancy tips and resources as well as 10 informational podcasts related to HEPA topics and overcoming barriers in pregnancy. Control: active social media comparator (n = 63) Same intervention as the HEPA group but the content and tracking activities were related to Stress Reduction and Management (SRAM). |
|
| Outcomes | Gestational weight gain, proportion of women with adequate gestational weight gain, healthy eating behaviours, physical activity, weight‐related knowledge (recommended weight gain for pre‐pregnancy BMI) and behaviours (self‐weighing frequency) (PRAMS), levels of perceived social support for healthy eating and exercise, perceived confidence to change exercise behaviours, motivation to change eating and exercise behaviours, and resources used for pregnancy health‐related information, usability of the mobile app, weekly challenges, and group‐based interactions and features (perceived social support from teammates, points achieved, and “bumps” of positive reinforcement shared), delivery outcomes form collected after delivery requested birth outcome data such as the baby’s length, weight, birth date, gender, presence of macrosomia, small‐ or large‐for‐gestational‐age, delivery method (vaginal versus cesarean). | |
| Equity | High‐income country. Pregnant women. | |
| Notes | Health behaviours: healthy eating and physical activity were selected as both were reported secondary outcomes by study authors and considered patient‐important. Body function: gestational weight gain was reported as primary outcome. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: weight‐related knowledge, levels of perceived social support for healthy eating and exercise, perceived confidence to change exercise behaviours, and motivation to change eating and exercise behaviours were the only outcomes of interest reported for this category; however, there were no data available for us to extract. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information of methods for randomisation not specified. Consent form states: "Quote A computer program will place you in one of the two conditions." Randomisation was stratified by the dichotomous pre‐pregnancy BMI value to ensure equal representation of BMI across the conditions. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | The research team set up the weekly challenge via the MakeMe app. The GWG graph was personalised using baseline survey data including pre‐pregnancy BMI, gestational age, and photo‐verified weight at baseline. The research team entered this information into the user profile on the back‐end to generate an appropriate GWG chart with accurate IOM recommendations based on pre‐pregnancy BMI and weekly rate of weight gain. Research team entered information onto participants profile, therefore they would be aware of their assignment. |
| Blinding of participants | Unclear risk | Not specified. Consent form describes the intervention groups in detail, possible participants could ascertain which group they belonged to based on the description provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Self‐reported measures were used. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rates among young, pregnant samples. "Quote"Several potential explanations for the high attrition rate of participants including, but not limited to, our inability to reach the participants after several attempts, potential complications with their pregnancy, cell phone service cancellation, or lack of external motivation to participate given the online nature of the study. Additionally, dropout may have been due to lack of interest or engagement with the intervention post randomisation. The baseline stress levels may have contributed to higher drop‐out among the SRAM participants, given the lack of need for a stress management program." |
| Selective reporting (reporting bias) | High risk | Not all outcomes (e.g. weight‐related knowledge, physical activity levels, dietary assessment, levels of perceived social support for healthy eating and exercise, perceived confidence to change exercise behaviours, motivation to change eating and exercise behaviours) included in the methods section are not sufficiently reported. |
| Baseline characteristics similar | Low risk | Groups are similar except for parity ‐ control group had much higher proportion of multiparous women (57.5% compared to 27.7% of intervention women.Therefore, parity was used as a covariate in the statistical models |
| Baseline outcome measurements similar | Unclear risk | Baseline values not reported for most outcomes. |
| Protection against contamination | Low risk | "Quote "Participants enrolled in the intervention study were asked to create a profile on the MakeMe app. Participants were then randomly assigned to a group of 8‐10 participants and when a group was “full,” participants in the group received a challenge code via email to enter into the MakeMe app." Participants in the control condition were unable to access the intervention materials on the study website and vice versa. |
Daly 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: obese pregnant women (n = 88) Age range: not reported Recruitment: women were recruited from Coombe Women and Infants University Hospital, Dublin, Ireland. Eligibility: eligible women had BMIs at their first prenatal visit of 30 or greater, underwent ultrasound confirmation of an ongoing pregnancy less than 17 weeks of gestation, understood English, were older than 18 years, and were able to give consent. Country: Ireland |
|
| Interventions |
Intervention: multi‐component (n =4 4) A medically supervised exercise intervention with routine prenatal care. Women in the intervention arm were invited to a secret Facebook group to create a sense of community among participants, to share healthy lifestyle advice, and to improve compliance with the exercise intervention. Control: non‐social media (n = 44) The control group received standard hospital written information on exercise. all women receive a pamphlet with information on healthy eating based on our national guidelines for nutrition and pregnancy. |
|
| Outcomes | Reduction in the mean fasting plasma glucose in the intervention group by 6.9 mg/dL (0.4 mmol/L) when compared with the control group; effects of the exercise intervention on longitudinal fasting plasma glucose concentrations; incidence of GDM at the time of the OGTT at 24–28 weeks of gestation; birth outcomes: induction of labour, mode of delivery and length of labor, birth weight, birth weight centile less than 10th and greater than 90th centiles, gestational age at delivery, preterm births, admission to neonatal intensive care unit, abnormal Apgar scores less than 7 at 1 and 5 minutes; gestational weight gain: mean gestational weight gain at 24–28 and 36 weeks of gestation, excessive gestational weight gain greater than 9.1 kg at 36 weeks of gestation, and mean postpartum weight retention at 6 weeks postpartum | |
| Equity | High‐income country. Pregnant women | |
| Notes | Health behaviours: not applicable. Body function: although the primary outcome reported was fasting plasma glucose, gestational weight was selected for this category as it was considered to be the most patient‐important physical health outcome. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was computer generated by an independent statistician and was stratified by parity and World Health Organization BMI category. |
| Allocation concealment (selection bias) | Low risk | Sequentiall‐ numbered opaque sealed envelopes were prepared by an independent research administrator |
| Blinding of personnel | Low risk | Women were randomised by another independent research administrator into either the exercise intervention or control arm. The clinical teams caring for the women were blinded to the randomisation result |
| Blinding of participants | Unclear risk | Women were informed that this was a RCT of closely supervised exercise during pregnancy to evaluate its ability to improve maternal glycaemia. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The research sample was blinded to clinical and research teams and reported to the research team at the end of the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 44 women randomised to the exercise group, five women did not participate. Four were nulliparous; mean age was 30.067.3 years, mean weight was 86.7619.3 kg, and mean BMI was 33.2 (range 30.4– 40.7). Two women cited lack of time and three did not explain why. Four of the five attended the clinical team for their OGTT and the results were analysed by ITT. |
| Selective reporting (reporting bias) | High risk | Trial registration notes several secondary outcomes not reported in study such as maternal body composition at 24‐28 weeks and 35‐38 weeks gestation and at 6 weeks postpartum; physical activity as measured by RT6 accelerometer at 24‐28 and 35‐38 weeks gestation and at 6 weeks postpartum; strength at 6 weeks postpartum; fitness at 6 weeks postpartum; among others. |
| Baseline characteristics similar | Low risk | There were no differences in the characteristics of the women between the two arms of the study |
| Baseline outcome measurements similar | Low risk | There were no differences between the two arms of the study |
| Protection against contamination | Unclear risk | Not reported |
Dehlendorf 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: women who have never used an IUD and women who used an IUD to serve as informational sources in the intervention arm (N = 628 ‐ 488 non‐IUD users and 140 IUD users). Age range: 18‐45 years of age. Recruitment: social media and forum‐based websites were used to recruit IUD non‐user participants. Email flyers were used to recruit IUD users through professional and social networks with stated interests in reproductive health. Eligibility: non IUD user eligibility: women between the ages of 18 to 45 who had ever been sexually active with men, desired pregnancy prevention, and had never used an IUD. IUD user eligibility: women age 18–45 who were satisfied with the IUD as a contraceptive method. Country: USA |
|
| Interventions |
Intervention: social media only (n = 340 ‐ 174 non‐IUD users and 140 IUD users, 35 groups of 9) Birth Control Connect groups dedicated to discussion of member experiences and perspectives related to contraception. Members were both IUD and non‐IUD users. Control: active social media comparator (n = 314 non‐IUD users, 35 groups of 9) Birth Control connect control groups are identical to those in the intervention arm, except no participants in the control arm are IUD users. |
|
| Outcomes | Initiation of IUD use, IUD attitudes (hormonal and non‐hormonal use for self and for women of same age), IUD knowledge (safe, effective at preventing pregnancy, more effective than the pill at preventing pregnancy), perceived informational support (group gave information about the IUD they did not have before, group gave them a better idea of what it would be like to have an IUD), other reported sources of IUD information accessed during the study period (online, healthcare provider, other women), frequency of Birth Control Connect logins during the study period. | |
| Equity | High‐income country, sexually active women. | |
| Notes | Health behaviours: initiation of IUD use was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: IUD attitudes of hormonal and non‐hormonal use as a contraceptive method for self was selected as it is most applicable to behaviour change. IUD knowledge and perceived informational support were the only outcomes of interest reported for this category. However, no estimates of precision were provided for IUD knowledge and only endline values were provided for perceived informational support. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Research team members randomised IUD non‐user participants using an electronic random number generator. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | The research team’s facilitation methods were identical between arms. Although facilitation was described to be identical, research team posted prompts to elicit discussion. It is possible that the level of prompts differed between groups. |
| Blinding of participants | Low risk | Trial registration reports participants were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Self reported outcomes, participants blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Quote "Loss to follow up of 29%, although baseline characteristics and study arm did not predict loss to follow up. While unmeasured factors may have influenced attrition, we hypothesize that risk of biased results due to attrition is relatively low" |
| Selective reporting (reporting bias) | High risk | Original primary outcome measures (Intention to change birth control method, Current birth control method, Acceptability of IUC, IUC information‐seeking, Normative beliefs about IUC, IUC Knowledge) differ from published measures (IUD use), as listed in the manuscript. |
| Baseline characteristics similar | Low risk | There were no significant differences in demographics by arm |
| Baseline outcome measurements similar | Unclear risk | Only baseline attitudes were reported |
| Protection against contamination | Low risk | The online discussion groups were closed. |
Duncan 2014.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: participants were adult males living in 2 regional cities in Queensland, who could access the Internet, owned a mobile phone, and were able to increase their activity level (n = 317). Age range: 35‐54 years Recruitment: to recruit participants, advertisements in local newspapers, trading magazines,face‐to‐face information sessions with local businesses, and distribution of leaflets and posters to local businesses, medical clinics, and offices of allied health professionals were used. Eligibility: males aged 35 to 54 years who owned a mobile telephone, had access to the Internet, did not have a mobility impairment, resided in the cities of Gladstone or Rockhampton (Queensland, Australia), and were classified as low risk to increase physical activity according to established guidelines were eligible to participate in the study Country: Australia |
|
| Interventions |
Intervention: Social media (n = 214) The ManUp challenges consisted of 6 physical activity and a multi‐component healthy eating challenge. Each challenge had 3 different “strengths” (light, mid, full), which varied the duration and the amount of activity or healthy eating that males were asked to achieve to complete the challenge. To complete a challenge, participants had to record the required number of minutes/distance/steps for activities or the number of healthy eating goals before the end of the challenge period; failure to do this meant the challenge was not completed. The variation between challenge strengths was intended to provide participants with an appropriate target relative to their current level of physical activity or healthy eating, or to provide a progression toward engaging in higher levels of physical activity or healthy eating. Control: non‐social media (n = 103) Participants in the print‐based group received a hard‐copy booklet that provided the same educational materials (including content from the My Weight section) and ManUp challenges as those provided to participants in the IT‐based intervention |
|
| Outcomes | Physical activity, sitting time, nutrition behaviours, physical activity and nutrition literacy, perceived health status | |
| Equity | High‐income country, Insufficiently active adults | |
| Notes | Health behaviours: physical activity (total minutes) and dietary score were selected as both reported as primary outcomes. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation lists were generated using freely available software |
| Allocation concealment (selection bias) | High risk | Randomisation lists were generated using freely available software (www.randomisation.com) and participants were allocated to intervention arms by project staff using an e‐mail with website URL, username and password trial registration. |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | High risk | Participants were blinded to group allocation until after baseline assessments were completed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants completed online surveys but were unblinded to assignment. A randomly selected subsample attended one of the trial centres for an in‐person assessment at each time point. During in‐person assessments, participants completed the online survey, received an accelerometer for the objective measurement of physical activity, and had their height, weight and waist circumference measured by a trained research assistant. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Completers were not significantly different in terms of baseline minutes and sessions of physical activity, dietary score, and type of bread consumed but differed from noncompleters in terms of age, the proportion working in professional level occupations, the proportion reporting a university‐level education, the proportion reporting to consume low‐fat milk, the proportion reporting that at least 20 minutes of vigorous intensity physical activity 3 times per week is essential to improve health, and nutritional literacy. A sensitivity analysis using baseline observation carried forward (BOCF) for participants with missing data at follow‐up time points was performed for physical activity, dietary behaviours and health literacy outcomes which found little difference in magnitude for these outcomes. All analyses followed ITT principles. |
| Selective reporting (reporting bias) | Unclear risk | Occupational sitting, leisure sitting, sedentary behaviours, perceived health status, waist circumference, weight reported in protocol but not in other papers. Possible these outcomes were just intended for baseline measures but unclear. |
| Baseline characteristics similar | Low risk | At baseline, intervention group consumed a significantly lower number of servings of red meat in the previous week, compared to the intervention group. No other significant between‐group differences were observed at baseline. |
| Baseline outcome measurements similar | High risk | There were no significant baseline differences between the groups for any behavioral or health literacy variable, except there were fewer participants who agreed that 30 minutes of physical activity is enough to improve health in the intervention group compared to the control group and more in the intervention group agreed that 20 minutes of vigorous activity per day is essential. |
| Protection against contamination | Low risk | Password‐protected ManUp website, Participants in the intervention group were emailed details to access the intervention platform, including website uniform resource locator (URL), username, and password; participants in the control group provided their mailing address to receive the print‐based intervention materials. |
Edney 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: non physically active adults (n = 444). Age range: 16 ‐ 65 years of age. Recruitment: participants were recruited using Facebook advertising, free advertisements within Facebook‐based community groups, and flyers placed around local university campuses. Eligibility: aged 18 −65 years, used Facebook weekly, spoke English, reported currently completing <150 minutes of MVPA per week, lived in Australia, and owned a smartphone (iPhone or Android). Before enrolment, participants were required to assemble a team of 3−8 Facebook friends, using an invitation feature within the registration section of the app. Country: Australia |
|
| Interventions |
Intervention: multi‐component intervention (n = 141) Active Team a 100‐day gameified smartphone app with interlinked social and gamified features (links to Facebook profile, post photographs and messages, unlock badges and virtual gifts, send and receive virtual gifts, and send and compete in mini challenges). Participants received a wrist‐worn pedometer to measure their daily step counts and could track their progress using the app. Participants also received a weekly e‐mail with a summary of their step count progress and encouragement to use the app, a daily push notification to remind them to log their steps, and a push notification when a friend interacted with them in the app. Control:nNo intervention (n = 140) Waitlist control group: no intervention. |
|
| Outcomes | Daily minutes MVPA at 3 months (objectively through accelerometers), self‐reported physical activity, health‐related quality of life (physical and mental), depression, anxiety, and stress, overall psychological well‐being, engagement with the app. | |
| Equity | High‐income country. | |
| Notes | Health behaviours: objective daily minutes of MVPA was reported as the primary outcome and considered the most patient‐important outcome for this category. Body function: not applicable. Psychological health: depression was the first outcome (not alphabetically) reported for this category. Well‐being: physical health related quality of life was considered most relevant to the primary outcome of MVPA. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. Note: waitlist control group extracted as control since there was minimal interaction between participants/researcher. Basic app group included the Active Team self‐monitoring features, a wrist‐worn pedometer, a weekly e‐mail with a summary of their steps, a daily push notification with a reminder to log their step count, and no access to social or gamified features (n = 160). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Quote "An independent allocation officer determined block sizes and allocation sequence using an electronic random number generator" |
| Allocation concealment (selection bias) | Low risk | "Quote "Block size and allocation sequence were concealed from study personnel enrolling participants in the trial" |
| Blinding of personnel | High risk | "Quote "Given the nature of the study, study personnel were aware of the allocated group once each team was formally enrolled" |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Retention was high. Intention‐to‐treat analysis: "Quote "missing data will be selected after inspecting the amount and pattern of missingness." There were no statistically significant differences in demographic characteristics between study completers and non completers. |
| Selective reporting (reporting bias) | High risk | Sleep quality and quantity (secondary outcome in protocol) and social‐cognitive theory constructs (secondary outcome in protocol) were not assessed. However, article states no deviations from the prespecified protocol during the trial. |
| Baseline characteristics similar | Low risk | There were no statistically significant differences in demographic characteristics between the 3 groups at baseline |
| Baseline outcome measurements similar | Unclear risk | Unclear whether differences in outcome measurements were assessed at baseline. No apparent differences at baseline exist. Although the study targeted inactive adults, this was assessed as a single‐item question at the time of joining the study (Are you currently doing less than 150 minutes of PA [e.g., walking, running] per week?) and people who went on to exceed this at baseline were not excluded. |
| Protection against contamination | Low risk | "Quote "To prevent contamination between experimental conditions, waitlist control and basic experimental condition participants will be blocked from receiving notifications from Facebook friends in the socially‐enhanced experimental condition, if they have such friends." |
Fiks 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: pregnant women who had a BMI >/=25 (overweight or obese) (n = 87) Age range: ≥18 years old Recruitment: mothers were recruited from two high‐volume, Philadelphia obstetric clinics from March to August 2014. We used limited characteristics available in the medical record (e.g. weeks of gestation) to prescreen for potentially eligible women and then approached them during appointments Eligibility: women who began pregnancy overweight or obese (body mass index (BMI) ‡25 kg/m2), were Medicaid insured, Women were ≥18 years old, English speaking,a singleton pregnancy between 20–32 weeks of gestation at the time of enrolment, owned a smartphone with a data plan, able to take photos and videos using the phone. Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 43) Grow2Gether participants joined a private Facebook group of 9– 13 women from 2 months before delivery until infant age 9 months. A psychologist facilitated groups featuring a curriculum of weekly videos addressing feeding, sleep, parenting, and maternal well‐being. Control: non‐social media (n = 44) Participants in control group received text message reminders for recommended infant primary care visits. The control group received no additional intervention |
|
| Outcomes | Feasibility, acceptability, impact on behaviours, Infant feeding practices, infant feeding beliefs, breastfeeding (ever breastfed, exclusively breastfed), introduction of solid foods and sugar‐sweetened beverages, infant sleep behaviours, parenting self‐efficacy, positive parenting behaviours (screen time, TV use, tummy time), maternal self‐care behaviours, maternal social support, maternal stress, infant weight and growth | |
| Equity | High‐income country. Pregnant women who had a BMI >/=25 (overweight or obese) | |
| Notes | Health behaviours: maternal infant feeding practices was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A randomly permuted randomisation sequence with randomly varying block sizes of 2 and 4 was computer generated by the study statistician. |
| Allocation concealment (selection bias) | Low risk | Sealed, sequentially‐numbered security envelopes concealed treatment allocation from study staff involved in recruitment before enrolment. |
| Blinding of personnel | High risk | Neither the study team nor participants were blinded to group assignment. |
| Blinding of participants | High risk | Neither the study team nor participants were blinded to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 98% retention. Eighty‐seven pregnant women (43 intervention; 44 control) completed the run‐in period and were randomised; 85 provided evaluable data. |
| Selective reporting (reporting bias) | High risk | Trial registration reports additional outcomes: Contraceptive use: Intent and behaviours, Maternal weight and height, Maternal depression. Only reports outcomes with statistically significant results. |
| Baseline characteristics similar | High risk | Significance not assessed, intervention group had higher proportion of participants with less than high school education, control group had highest proportion of participants who were high‐school graduates. Many more in control reported being food insecure. |
| Baseline outcome measurements similar | Unclear risk | Not assessed. |
| Protection against contamination | Low risk | Several procedures were established to protect participant privacy and safety, including use of ‘‘secret’’ Facebook groups, which are invisible to outsiders |
George 2013.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: medical students (n = 95) Age range: mean age 23 (intervention group only) Recruitment: all first year medical students were invited to participate Eligibility: all first year medical students Country: USA |
|
| Interventions |
Intervention: social media only (n = 47)
Facebook group in which medical students posted content (e.g. video links, discussion prompts) Control: non‐social media (n = 48) In‐person stress management |
|
| Outcomes | Facebook use, experience with Facebook intervention | |
| Equity | High‐income country, medical students | |
| Notes | Control group data not reported. Author contacted and replied to state that the data was no longer available. No outcome data has been extracted for our review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "using simple randomization". Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Focus groups facilitated by someone not involved in the Facebook intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data on control group provided |
| Selective reporting (reporting bias) | High risk | No data on control group provided |
| Baseline characteristics similar | Unclear risk | No data on control group provided |
| Baseline outcome measurements similar | Unclear risk | No data on control group provided |
| Protection against contamination | Unclear risk | Not reported |
Glanz 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: Pregnant women (n = 1093) Age range: 18 years or old Recruitment: all participants were members of the KPCO health plan, a nonprofit managed care organization. Beginning of each wave, we used electronic health records to identify pregnant women in the third trimester of pregnancy (13–6 weeks from delivery). Eligibility: pregnant women had to be age 18 years or older, English speaking, have Internet access, be enrolled in the KPCO health plan Country: USA |
|
| Interventions |
Intervention: Social media only (VSM n = 542) (VI n = 371) Website with vaccine information (VI) (not extracted for this review) Web site with vaccine information and interactive social media components (VSM) ‐ multidirectional communication model, a social marketing strategy with 3 components: 1) standard, top‐down process in which Website developers create and present content to users, 2) bottom‐up process that allows users to create content and interact with Web site developers, 3)a side‐to‐side process in which users can interact with each other and share information. Participants in the VSM arm had access to social media technologies that included a blog, discussion forum, chat room, and “Ask a Question” portal through which participants could directly ask our experts questions about vaccination. Control: non‐social media UC (usual care) (UC = 180) Previsit informational sheet listing the vaccines recommended at each visit as well as Vaccine Information Statements |
|
| Outcomes | Days undervaccinated, up‐to‐date vaccination status | |
| Equity | High‐income country. Pregnant women | |
| Notes | Health behaviours: days under vaccinated was the primary outcome but we have extracted up to date vaccination as this is a more common measure. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done using the SAS/ STAT (SAS Institute, Inc, Cary, NC) procedure Proc Plan. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Although the study team was not blinded to study arm assignment, the study team was blinded to participants’ hesitancy status. |
| Blinding of participants | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Approximately 20% of data missing in each group with similar reasons. A lack of outcome data led to the exclusion of 205 infants (18.8%). Among participants lost to follow‐up, median vaccine hesitancy scores were not significantly different across the arms. |
| Selective reporting (reporting bias) | Unclear risk | No protocol.but all relevant outcomes in the methods section are reported in the results. |
| Baseline characteristics similar | Low risk | Baseline characteristics were evenly distributed across study arms |
| Baseline outcome measurements similar | Low risk | No differences were detected between study groups. |
| Protection against contamination | Low risk | To enhance security and prevent contamination, participants randomly assigned to the VSM and VI arms were required to create a login and password for the Website. |
Gnagnarella 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: cancer patients experiencing eating and nutritional problems (n = 138) Age range: >18 years Recruitment: cancer patients seeking information about nutritional problems on Internet web sites of the study partners and social network pages: Organisation of European Cancer Institutes (OECI; www.oeci‐eeig.org), the Italian Association for cancer patients, their families and friends (Associazione Italiana dei Malati di Cancro (AIMaC); www.aimac.it) and the Italian Federation of Volunteer‐Based Cancer Organizations (Federazione italiana delle Associazioni di Volontariato di Oncologia (FAVO); www.favo.it). In addition, printed leaflets have been distributed at the European Institute of Oncology. Eligibility: inclusion criteria were age >18 years, Italian residency, cancer diagnosis, Internet access and e‐mail account over the study period. Country: Italy |
|
| Interventions |
Intervention: social media only (n = 64) Access to the website, which included a series of contents and reports about cancer, nutritional problems and advice to better cope with them. Participants could also interact and ask questions to a group of experts established for the study. In addition, some interactive activities were planned for the intervention (polls, chat room to talk to the expert). Control: non‐social media (n = 61) Did not have access to the website; they were provided with PDF versions of the contents by e‐mail. |
|
| Outcomes | Change in knowledge on nutritional problems during cancer, psychological distress the quality of life | |
| Equity | High‐income country. Cancer patients experiencing eating and nutritional problems | |
| Notes | Health behaviours: nutrition (global score) was selected as per our outcome criteria. Body function: not applicable. Psychological health: psychological distress was the only outcome reported for this category. Well‐being: quality of life was the only outcome reported for this category Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: nutrition and cancer knowledge was the only outcome of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Eligibleparticpants were allocated to one of two study groups using a computer‐generated scheme. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Reports that participants in intervention arm could interact and ask questions to a group of experts established for the study. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 28% dropout without reasons or comparison to completers |
| Selective reporting (reporting bias) | Low risk | No protocol but preliminary results paper reports same outcomes as final paper |
| Baseline characteristics similar | Low risk | No differences between groups. |
| Baseline outcome measurements similar | Low risk | More women in the control group, weight loss and tumour site differed. |
| Protection against contamination | Low risk | Only intervention group had access to the website. |
Godino 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: overweight or obese college students from three universities in San Diego (n = 404) Age range: 18‐35 years Recruitment: students were recruited at the three college campuses via a combination of print (e.g. newspapers, flyers, posters, and magnets) and digital (e.g. emails, electronic bulletins, websites, and Facebook) advertisements. Additionally, in‐person recruitment was done at student orientations and health fairs and was coordinated with real‐time monitoring of online interest form submissions. Eligibility: eligible students were adults aged 18–35 years. They had a BMI of between 25·0 kg/m² and 34·9 kg/m², used Facebook or were willing to begin, owned a personal computer, owned a smartphone, used text messaging, and were willing to attend measurement visits in San Diego over 2 years. Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 202) Weight loss intervention delivered via Facebook, mobile apps, text messaging, emails, a website, and technology‐mediated communication with a health coach (the SMART intervention). Control: non‐social media (n = 202) Participants allocated to the control group were given access to a different website than intervention participants and were sent quarterly newsletters via email. |
|
| Outcomes | Main: Weight, BMI (kg/m²), waist circumference (cm), arm circumference (cm), systolic blood pressure (mm Hg), diastolic blood pressure (mm Hg), heart rate (beats per min), and the level of engagement (i.e. amount of use). Other outcomes measured: physical activity, sedentary behaviours, total dietary intake, eating behaviours related to weight management, sugar‐sweetened beverage consumption, eating away from home, quality of life, depression, self‐esteem,body image, psychosocial constructs related to physical activity and diet, social support and social network composition with Facebook data |
|
| Equity | High‐income country. Young adults | |
| Notes | Health behaviours: not applicable. Authors report that intervention effects on physical activity and diet will be reported in another manuscript at a later date. Body function: weight was considered the most patient‐important outcome reported for this category. Psychological health: not applicable. Authors report that intervention effects on depression will be reported in another manuscript at a later date. Well‐being: not applicable. Authors report that intervention effects on quality of life will be reported in another manuscript at a later date. Mortality: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A statistician allocated participants using computer‐based permuted‐block randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed from the participants, study staff, and investigators until the intervention was assigned. |
| Blinding of personnel | High risk | It was not possible to mask participants or the study staff that delivered the intervention |
| Blinding of participants | High risk | It was not possible to mask participants or the study staff that delivered the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Study staff who measured participants and investigators who analysed study outcomes remained masked to the allocation throughout the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16% were lost to follow‐up ‐ all analyses were done using an intention‐to‐treat framework and included all participants. To assess the potential effect of missing data on the primary outcome, a sensitivity analysis was done using an inclusive strategy. |
| Selective reporting (reporting bias) | Unclear risk | The primary aim of the intervention in the protocol is stated as 5% to 10% weight loss at 24 months but in the final report, this is reported in the secondary outcomes table. |
| Baseline characteristics similar | Low risk | The groups did not differ according to key demographic characteristics |
| Baseline outcome measurements similar | Low risk | The groups did not differ |
| Protection against contamination | High risk | Facebook data revealed that at least 30% participants in the control group were friends with one or more participants in the SMART intervention group. Depending on individual privacy settings, the control group could have viewed intervention‐related posts, comments, or likes. |
Graham 2011.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: current adult smokers who smoked 5 or more cigarettes per day (n = 2005) Age range: mean (SD) age of 35.9 (10.8) years Eligibility: eligibility criteria included US residence, current smoking of 5 or more cigarettes per day, age of 18 years or older, and no prior use of the QuitNet Web site as confirmed by the absence of a tracking cookie. Recruitment: Internet users from the USA were recruited based on use of the terms quit(ting) smoking or stop(ping) smoking in a major search engine query (AOL, MSN, Yahoo, Google) and no known prior visit to QuitNet (no cookie detected). When a user clicked on a link to QuitNet in the results of a search engine query, an intercept page appeared inviting them to participate in a study. Country: USA |
|
| Interventions |
Intervention: multi‐component Enhanced Iinternet ‐ access to the full version of QuitNet.com, an interactive website including online social network (n = 651) Enhanced Internet and telephone combined ‐ same as above plus telephone counselling (n = 675) These intervention groups have been combined for our analysis. Control: non social media Basic Internet ‐ access to a static, information only website with the same content as QuitNet (679) |
|
| Outcomes | 30‐day point prevalence abstinence determined at each follow‐up | |
| Equity | High‐income country. Adult smokers | |
| Notes | Health behaviours: smoking abstinence was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted via random numbers table. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Follow‐up telephone assessments were completed by research assistants who were not masked to treatment assignment but did not provide any form of intervention |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Follow up rates ranged from 76% at 3 months to 68% at 18 months. Reasons not provided. |
| Selective reporting (reporting bias) | High risk | Trial registration has 7‐day point prevalence abstinence at 12 months following treatment but paper reports 30 day point prevalence abstinence. |
| Baseline characteristics similar | Low risk | Reports no significant differences for any demographic variables between groups |
| Baseline outcome measurements similar | Low risk | Reports no significant differences for any smoking or psychosocial variables between groups. |
| Protection against contamination | Unclear risk | Not reported |
Graham 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: adult smokers (n = 5290)
Age range: 18 years and older Recruitment: participants were new registered users of BecomeAnEX.org, a free, publicly available smoking cessation Web site.. Immediately following registration on BecomeAnEX, participants were shown an invitation that briefly describes the study. Participants were recruited following website registration and completed online eligibility screening, informed consent, and a baseline survey Eligibility: Eligibility criteria are current smoking, age 18 years or older, and US residence. Country: USA |
|
| Interventions |
Intervention: social media only Group 2 (WEB + SN) (n = 1323) Social Network Intervention (SN): proactive communications from three established members of BecomeAnEX (“Integrators”) who were longstanding, very active members of the community to facilitate the integration of new members into the BecomeAnEX online social network. Group 3 (WEB + NRT) (n = 1313) Nicotine Replacement Therapy Intervention (NRT): free 4‐week supply of the NRT product of their choice (patch, gum, or lozenge) and a printed calendar for participants to record product use. Group 4 (WEB + SN + NRT) (n = 1317) Access to 4 weeks of NRT and the SN protocol as described in the sections above. Control: non‐social media ( n = 1337) Group 1: WEB: Access to website 'BecomeAnEX' with the following components: a series of Addiction Videos which provides information on pharmacotherapy; a Quit Date tool that assists users in selecting a quit date; a Build Your Support System exercise to identify helpful supporters; a Beat Your Smoking Triggers exercise to identify strategies to dissociate cigarettes from triggers; a Cigarette Tracker exercise to identify smoking triggers; a Choose a Quit Smoking Aid exercise, in which users indicate their plans for pharmacotherapy use; and Community, a large online network of current and former smokers who communicate via private messages and public posts in blogs, groups, forums, and on member profile pages. |
|
| Outcomes | Treatment adherence, defined and measured as (a) overall treatment “dose” received (general Web site utilization metrics), (b) use of skills training treatment components (interaction with static and interactive features on the Web site), (c) exposure to intratreatment social support (engagement in the online community), and (d) use of pharmacotherapy. | |
| Equity | High‐income country. Adult smokers | |
| Notes | Health behaviours: smoking abstinence and medication use were both selected as both were reported as primary outcomes. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Within‐strata randomisation assignments were automated using a computer algorithm. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Phone surveys conducted by research staff blind to treatment condition. Facilitators were blind to treatment condition in that they do not know whether participants are also receiving NRT. |
| Blinding of participants | Unclear risk | Trial registration reports participant blinded but not other details are provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes are self‐reported. Phone surveys are conducted by research staff blind to treatment condition. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 62.3% response rate at 3 months and 57.1% at 9 months. Response rate lower among those who did not receive medication. Reasons not provided. |
| Selective reporting (reporting bias) | High risk | The protocol reports additional secondary outcomes (motivation to quit and continuous abstinence) for which no results are reported. |
| Baseline characteristics similar | High risk | Statistically significant differences in ethnicity, employment, age. Proportion smoking 20 cigarettes or more and having received cessation advice from a healthcare provider were both higher among trial participants. Differences in gender, education, daily smoking, and quit attempts had medium effect sizes. |
| Baseline outcome measurements similar | Unclear risk | Abtinence rates not relevant at baseline however, more intervention participants had received cessation advice from a healthcare provider |
| Protection against contamination | Unclear risk | All study participants were able to send and receive public and private communications with other members. |
Greene 2013.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: PeaceHealth Oregon employees and family members (n = 513) Age range: 18‐79 years Eligibility: 1) participants were between 18 and 79 years old, had stable medication for 3 months and had expressed concern about their weight or health in an online screener survey. Recruitment: recruited from PeaceHealth Oregon employees and their family Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 180) The iWell OSN combined an online platform for social networking with an accelerometer and a weight scale that both wirelessly uploaded data for tracking over time. All participants received printed lifestyle guidelines. Control: non‐social media (n = 169) Received printed lifestyle guidelines on diet and exercise during their first study visit. |
|
| Outcomes | Weight loss, physical activity, number of messages participants sent to individuals in the iWell OSN, number of uploads of accelerometer data, commuting (walking/ cycling), activities at work (light/intense), household activities (light/intense), Leisure time (walking/cycling/gardening/odd jobs/ sports) | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: weight was classified as the most patient‐important physical health outcome reported. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation was not specified |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 68% participated for the full 6 months and were included in the analysis. Equal percentages of intervention and control group participants dropped out of the study. Those who stopped participating were not significantly different from those who continued in terms of baseline physical activity levels, clinical indicators, or gender but they did have higher baseline BMI than those who participated for the full 6 months and they were younger. |
| Selective reporting (reporting bias) | High risk | Does not report blood pressure as listed in trial registration (NCT01325376) |
| Baseline characteristics similar | High risk | More obese participants in control, more women, more participants aged < 40 and fewer > 60. |
| Baseline outcome measurements similar | Unclear risk | 100 minutes per week less leisure time walking in control group but unclear whether this is an important difference |
| Protection against contamination | Low risk | unlikely that control received online intervention Quote: "Intervention participants were provided access to the iWell OSN and were given an accelerometer that allowed them to capture their physical activity or “steps” for upload to the iWell OSN and a wireless weight scale for uploading weight data" |
Hammersley 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: parents with a child at or above the WHO 50th percentile for body mass index for their age and sex (n = 86). Age range: Overall parent’s age in years mean (SD) was 35.17 (4.80) and child's age in years mean (SD) was 3.46 (0.92). Recruitment: flyers distributed at early childhood education and care centres, general practices/primary healthcare centres, early childhood health centres, playgroups, and local sporting groups. Flyers were also displayed on community notice boards (e.g. libraries, shopping centres, children’s activity centres), and articles were placed in the University of Wollongong and Local Health District newsletters and posted on Facebook. Media releases were also sent to local media outlets. Eligibility: had access to the Internet, had a Facebook account or agreed to create one, and had a child that was 2 to 5 years old (and not yet attending school) who was at or above the WHO fiftieth percentile for BMI for their age and sex. Country: Australia |
|
| Interventions |
Intervention: multi‐component intervention (n = 42) Time2bHealthy intervention ‐ 6 modules relevant to multiple behaviours (nutrition, physical activity, screen time, and sleep) and delivered over 11 weeks. Each module included readings, videos, activities, quizzes, and a goal‐setting component. Participants also received access to a secret Facebook group to communicate with each other and the dietician. Participants received feedback from dietician and email reminders to login to website. Control: non‐social media control (n = 44) Emails every 2 weeks directing parents to resources on government website covering similar topics. |
|
| Outcomes | Change in child BMI 6‐month post baseline, child dietary intake (kJ/kg of body weight, kJ from sugar, kJ from saturated fat, servings of fruit, servings of vegetables, discretionary food frequency score), physical activity (sedentary time, light/moderate/vigorous physical activity and MPVA), screen time (week day, weekend day), sleep (duration, latency, sleep reluctance), child‐feeding practices (restriction and pressure), parent nutrition self‐efficacy, and parent role modelling. | |
| Equity | High‐income country. Parents with children at or above the WHO 50th percentile for body mass index for their age and sex. | |
| Notes | Health behaviours: parental modelling was the outcome most related to parental practices. Body function: not applicable. Children's BMI was reported but because it focused on children's physical function outcomes we did not include it in our analysis. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: nutrition self‐efficacy was the only outcome reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"Randomization was performed in a 1:1 ratio using a computerized random number generator" |
| Allocation concealment (selection bias) | Unclear risk | Not reported. Quote: "A data manager with no other involvement in the study conducted the randomization." |
| Blinding of personnel | Low risk | The researcher responsible for implementing the intervention was the only person who was informed about group allocation. However, outcomes are unlikely to be influenced by lack of blinding |
| Blinding of participants | Unclear risk | Blinding of participants not specified. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote:"At the follow‐up data collection time points, height and weight measurements were taken by trained data collectors blinded to group allocation." However, some outcomes were reported by parents and blinding of participants was not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate and similar across groups. Reasons for missing data (loss to follow‐up and technology issues) unlikely to be related to the true outcome. Intention‐to‐treat principles used |
| Selective reporting (reporting bias) | Low risk | All outcomes in protocol a priori were measured and reported |
| Baseline characteristics similar | Unclear risk | Differences in characteristics not assessed. There appear to be some differences, however unclear if significant (e.g. parental education, weight status of parent, martial status, income) |
| Baseline outcome measurements similar | Unclear risk | Differences in characteristics not assessed. There appear to be some differences, however unclear if significant including median BMI percentile range of child. |
| Protection against contamination | Low risk | Participants randomised to the intervention group were provided with an individual log‐in to access the Time2bHealthy program. |
Herring 2014.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: Urban, Low‐income mothers (n=18) Age range: Mean age was 24.2 ± 5.1 years Recruitment: recruited from the waiting rooms of two large outpatient practices (obstetrics, pediatrics) which served primarily Medicaid‐insured patients Eligibity: age ≥ 18, singleton infant delivered within the last 2 weeks to 12 months, early pregnancy (first trimester) body mass index (BMI) greater than or equal to 25 kg/m2 via prenatal records, weight at enrollment that exceeded early pregnancy weight by at least 5 kg, cell phone ownership with unlimited text messaging, and member of Facebook. Country: United States |
|
| Interventions |
Intervention: Multi‐component (n=9) Technology‐based intervention, which included empirically‐supported behavior change strategies, daily skills and self monitoring text messages with personalized feedback, biweekly counseling calls from a health coach, and access to a Facebook support group. Control: Non‐social media (n=9) Participants randomized to usual care received the current standard of care offered to postpartum mothers from their primary care providers or through the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). |
|
| Outcomes | change in body weight (kg) at 14 weeks from baseline, changes in weight‐related dietary and physical activity targets, relationship between adherence to the intervention (assessed by the number of self monitoring texts sent and number of coach calls completed) with weight loss among intervention participants, and program satisfaction | |
| Equity | High income country, urban, low‐income mothers | |
| Notes | Health behaviours: Not applicable. Diet and physical activity were reported as secondary outcomes; however, there was no data available for us to extract. Body function: Weight was the only outcome reported for this category. Psychological health: Not applicable. Well‐being: Not applicable. Mortality: Not applicable. Adverse effects: Not applicable. Secondary outcomes: Not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized using computer‐generated numbers |
| Allocation concealment (selection bias) | Low risk | In sealed envelopes |
| Blinding of personnel | Unclear risk | No mention if health coach was blinded |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Staff that assessed outcomes were not blinded, However, strict protocols on completion of anthropometric measures and delivery of questionnaires were used. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All but one participant (17/18) completed baseline and 14‐week follow‐up measures; for this participant, a weight measured at 8 weeks post‐scheduled follow‐up was used in intent‐to‐treat analyses. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. For secondary outcomes the background says "related dietary and physical activity targets" and results presented include consumption of sugary drinks, fried/fast foods, chips, less food, and number of days spent walking. |
| Baseline characteristics similar | Low risk | There were no differences between treatment groups on demographic characteristics. |
| Baseline outcome measurements similar | Low risk | There were no differences between treatment groups on weight, weight‐related behaviors, or mood. |
| Protection against contamination | Unclear risk | Discussion states that participation in text4baby not collected but does not describe what this means. Text4baby is a CDC text message service that sends texts to improve mom and baby's health so control participants may have had access to this service which is similar to the intervention group. |
Herring 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: obese African American women who were at or below their early pregnancy weights by 6 months postpartum (n = 66) Age range: ≥ 18 years Recruitment: study staff used Temple’s electronic medical record to identify potential participants by BMI and age, and then approached them in waiting rooms to evaluate trial interest Eligibility: age ≥ 18 years, self‐identification as African American, gestational age < 20 weeks, first trimester BMI 25 to kg/m2 45 kg/m2, Medicaid recipient (income proxy), cell phone ownership with unlimited text messaging and Facebook member Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 33) Technology‐based, behavioral intervention including: 1) daily skill‐building text messages, 2) weekly Facebook posts with links to websites and videos, 3) weekly to monthly 15‐minute calls with a health coach to problem solve barriers, provide support, and build participant self‐efficacy for behaviour change. Control: non‐social media (n = 33) Standard obstetrical care at Temple University, which included:1) an initial visit in the first trimester, during which obstetric providers completed a comprehensive patient history, physical exam, ultrasound, and blood work; 2) follow‐up visits monthly until week 24 and every 2 to 3 weeks until week 36, where providers assessed patient weight, blood pressure, urine protein, and fetal heart rate; and 3) weekly visits from week 36 until delivery. |
|
| Outcomes | Proportion of women at (within 0.9 kg) or below their early pregnancy weights by 6 months postpartum, proportion of women at or below their early pregnancy weights by 12 months postpartum, intervention engagement (e.g., the proportion of participants who responded to ≥50% of the self‐monitoring text prompts and number of coach calls completed), and treatment acceptability assessed via survey at 6‐month postpartum follow‐up | |
| Equity | High‐income country, obese African American women who were at or below their early pregnancy weights by 6 months postpartum | |
| Notes | Health behaviours: not applicable. Body function: maternal weight‐gain was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was computer‐generated |
| Allocation concealment (selection bias) | Low risk | Randomisation status was concealed in opaque envelopes |
| Blinding of personnel | Low risk | Clinic staff were blind to randomisation assignment |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Clinic staff were blind to randomization assignment; so any measurement bias would likely be non‐differential across treatment groups." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing postpartum weights at 6 months (n = 3) and 12‐months (n = 4) were additionally filled with EMR data (weights were accepted ± 30 days of planned 6‐month and ± 60 days of planned 12‐month postpartum assessments) |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Outcomes reported in methods match those in results. |
| Baseline characteristics similar | Low risk | No statistically significant differences in maternal demographic characteristics at baseline. |
| Baseline outcome measurements similar | Low risk | No differences in weight and BMI between groups at baseline. |
| Protection against contamination | Unclear risk | Not reported |
Horvath 2013.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: HIV‐positive gay men or bisexual men (n = 123) Age range: 18 years or older Recruitment: through a variety of online venues: 42% of participants from a prior online survey [18] were contacted via e‐mail and re‐screened for inclusion in the current study; 21% were recruited using online banner ads on HIV‐related websites (e.g. Poz.com; AIDSMeds.com); 11% were recruited using online banner ads placed on websites that target the gay/bisexual MSM community; and 1% via Facebook. Nearly one‐quarter (24%) of the sample came through other sources, such as word‐of‐mouth or hearing about the study at their clinic. Eligibility: HIV‐positive test result, male gender, gay or bisexual sexual orientation, 18 years of age or older, US resident, less than 100% ART adherence in the past 30 days, availability to participate in the study in the subsequent 16 weeks and (8) reported being somewhat to very interested (on a 1–4 point scale) in quote:“participating in a health and wellness website in which you would be interacting with other people living with HIV.” Country: United States |
|
| Interventions |
Intervention: Social media only (n = 66) TWM intervention ‐ TWM homepage consisted of an interface for participants to asynchronously interact with one other by posting messages and replying to other participants’ messages. The third major component of the intervention was intervention content addressing issues about living with HIV.Intervention content took one of 3 forms: video segments provided by the Positive Project (http://www.thepositiveproject.org/#) were chosen based on a prior analysis of topics HIV‐positive MSM would find most interesting, brief articles about HIV‐related topics and medication adherence written by study staff and links to other HIV‐related websites and webpages. Control: Non‐social media (n = 57) Received usual care, were not asked to participate in any activities; however, they were sent one interim e‐mail message reminding them of the upcoming follow‐up survey |
|
| Outcomes | Internet knowledge, Depression, Perceived Stress, Life Chaos, HIV Stigma, risk for alcohol dependency or hazardous alcohol consumption, illicit drugs use, intervention acceptability, ART medication use and adherence | |
| Equity | High‐income country, HIV‐positive gay men or bisexual men | |
| Notes | Health behaviours: medical adherence was a primary outcome and the only outcome reported for this category with baseline and endline measures. Body function: not applicable. Psychological health: not applicable. Depression was only reported at baseline. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: no outcomes of interest could be extracted as they were only reported at baseline. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using a random number generator. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | The intervention group was monitored daily by study staff to identify any concerns (e.g. hostile interactions; suicidal ideation; ART or HIV‐related misinformation) and to respond to participants’ questions or concerns about the intervention |
| Blinding of participants | High risk | Participants were given information describing the study arm to which they were randomised but were unaware of the activities of the other arm |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants self‐reported ART adherence and knew of their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Overall retention in the TWM study was 90%, with only a slight difference in retention between those randomised to the intervention arm (88%) and the control arm (93%). Reasons for loss to follow‐up not given. Participants with missing data were excluded from analysis. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available but reports outcomes as described in methods section |
| Baseline characteristics similar | Low risk | Baseline characteristics were similar between groups |
| Baseline outcome measurements similar | Unclear risk | Medication regimen complexity was higher in control than intervention. |
| Protection against contamination | Low risk | Only men randomised to the intervention arm were given access to the intervention |
Hutchesson 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: young females who are overweight (n = 57). Age range: 18‐35 years of age. Recruitment:rRecruited via media releases from the University of Newcastle and Hunter Medical Research Institute, posters at the university campus, local technical colleges, local businesses and organisations known to engage with the target group and the social media pages of these settings. An email invitation was also sent to consenting participants of a previous research study in young women. Eligibility: Female, aged 18–35 years, body mass index (BMI) 25.0–34.9 kg/m2, email and Internet access, iPhone model 4s or newer, social media accounts willing to be used for the study and able to attend measurement sessions. Country: Australia |
|
| Interventions |
Intervention: multi‐component intervention (n = 29) Be Positive Be Healthe (BPBH): 6‐month weight‐loss program delivered using e‐Health technologies only, comprising five delivery modes (website, app, email, text messages and social media). All resources promoted the BPBH 10 key weight‐loss messages related to key eating behaviours and physical activities and evidenced‐based weight loss strategies (i.e. self‐monitoring, stimulus control, cognitive restructuring and social support). During the first 12 weeks of the program, a different topic was covered each week in email newsletters, text messages and social media. Control: No intervention (n = 28) Waitlist control. |
|
| Outcomes | Weight change, BMI, waist circumference, body fat (kg and %), blood pressure (systolic and diastolic), total HDL and LDL cholesterol and triglycerides, physical activity (MPVA minutes/week, MPA minutes/week, VPA minutes/week), sitting time (week day, weekend day, total), dietary intake (fruit % and grams, vegetable % and grams, alcohol % and grams, takeaway %, % energy from non‐core or core foods), quality of life, program acceptability and satisfaction. | |
| Equity | High‐income country, females,BMI 25.0 kg/m2 to 34.9 kg/m2. | |
| Notes | Health behaviours: physical activity and energy intake were both considered the most patient‐important outcomes for this category. Body function: weight change was reported as primary outcome. Psychological health: not applicable. Well‐being: quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"The allocation sequence was generated by a computer‐based random number algorithm" |
| Allocation concealment (selection bias) | Low risk | Quote:"A researcher not involved in the study prepared concealed envelopes, which were distributed following completion of baseline assessments, by a researcher not involved in data collection." |
| Blinding of personnel | Unclear risk | Given that the Facebook group was facilitated, it is likely that there was no blinding of research personnel |
| Blinding of participants | Unclear risk | Not specified |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote:"Assessment sessions were held at the University of Newcastle, NSW, Australia, and conducted by trained, blinded assessors at baseline and after six months. Participants who were unable to attend assessment sessions in person at six months were invited to complete the online survey and provide a self‐reported weight." Self‐report assessments were included and blinding was unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Same loss to follow‐up numbers across groups, with similar reasons for missing data. Intention‐to‐treat analyses used. |
| Selective reporting (reporting bias) | Low risk | Deviations from protocol including not assessing physical activity with a pedometer, and self‐esteem using Body Esteem Scale for Adolescents and Adults. However, these values are provided in supplementary table. |
| Baseline characteristics similar | Unclear risk | Analyses not conducted. Does not appear to be differences with the exception of education and income. |
| Baseline outcome measurements similar | Unclear risk | Analyses not conducted. Appear to be differences between control and intervention groups for MVPA minutes/week, Energy intake (kJ/day), Vegetables (grams/day). However, unclear if these differences are significant. |
| Protection against contamination | Unclear risk | Possible that control group participants could access the website,Facebook group and Instagram, or downloaded self‐monitoring app. Not specification on protection of these accounts. |
Hwang 2013.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: members of an online weight‐loss community who were not up‐to‐date with Colorectal cancer screening (n = 306)
Age range: 50‐75 years old Recruitment: recruitment of Narrators for the Enhanced Group: Fifteen narrators were recruited from the SparkPeople online weight‐loss community who indicated in the prior survey19 that they were up‐to‐date with CRC screening and expressed interest in sharing their CRC narratives with unscreened members of the same community. Recruitment of study participants: SparkPeople administrators sent a recruitment e‐mail on July 27, 2011, to members aged ≥50 years who had logged in at least once in the previous 20 days (n = 51,847). The 20‐day time frame was chosen to reach approximately 50,000 members. The e‐mail invited members to click on a link to eligibility questions (with entrance into a random drawing for a $200 Amazon.com gift certificate) and learn about Eligibility: aged 50–75 years, residing in the USA, having no prior diagnosis of CRC, having no history of inflammatory bowel disease and not being up‐to‐date with CRC screening (i.e. having had no FOBT within the past year, sigmoidoscopy within the past 5 years, or colonoscopy within the past 10 years). Eligible individuals were required to submit an e‐mail address in order to enrol Country: United StatesUSA |
|
| Interventions |
Intervention: Multi‐component (n = 153) Participants in the Enhanced group received the same educational information as those in the Basic group. They also were invited to join the private, study‐specific online “SparkTeam” to access the narratives and interact with the narrators and other Enhanced group participants. Control: non‐social media (n = 153) Participants in the Basic group were sent an e‐mail link inviting them to view educational information about CRC adapted from the “Screen for Life” National Colorectal Cancer Action Campaign by the CDC. Topics included general information about CRC, risk factors, prevalence, benefit of screening, and types of screening tests. |
|
| Outcomes | Engagement, psychosocial outcomes (knowledge (not validated), motivation (not validated), attitudes (validated), salience and coherence, cancer worries, Perceived susceptibility, response efficacy, social influence of others, social influence of SparkPeople members, self‐efficacy, worries about screening, and self‐report CRC screening | |
| Equity | High‐income country | |
| Notes | Health behaviours: colorectal cancer screening was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: motivation, knowledge, perceived susceptibility, social influence of others, and salience and coherence were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated with a computer‐generated randomisation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote:"Allocation was concealed from investigators at the time of enrollment. Study participants were not informed of the differences between the two interventions." |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Study participants were not informed of the differences between the two interventions |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote:"Allocation was concealed from investigators at the time of enrollment" but no mention of blinding at outcome assessments |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only 87 of 153 (57%) of the participants in the intervention group joined and remained on the SparkTeam until the 6‐month assessment. |
| Selective reporting (reporting bias) | Low risk | Reports on all stated outcomes from trial registration (feasibility and colon cancer screening attitudes) with additional outcomes colorectal cancer screening, psychosocial outcomes and user engagement. NCT01411826 |
| Baseline characteristics similar | High risk | Most participants were female, white, married, employed, and had health insurance. Groups were similar at baseline, except that more participants in the control group reported a visit with their primary care provider in the past year. |
| Baseline outcome measurements similar | High risk | Control group was more likely to have visited with primary care provider in the last year and to have had a health maintenance exam |
| Protection against contamination | Unclear risk | All participants were members of the SparkPeople online weight‐loss community. Unclear whether any measures were taken to prevent contamination. |
Jane 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: overweight and obese individuals with a body mass index (BMI) between 25 kgm2 – 40 kg/m2 (n = 137) Age range: 21‐65 years Recruitment: recruited from the Perth community via advertisements in the West Australian Newspaper and Community Newspapers Eligibility: 0verweight and obese individuals with a body mass index (BMI) between 25 ± 40 kg/m2 and aged between 21 and 65 years. required to have access to a computer, laptop, tablet or Smartphone Country: Australia |
|
| Interventions |
Intervention: Social media only FG (n = 46) PG (n = 46) The two intervention groups were instructed to follow identical weight‐management program. One group received the program within a Facebook group, along with a support network with the group, and the other intervention group received the same program in a booklet, but both group followed the Total Wellbeing Diet developed by the Commonwealth Scientific and Industrial Research Organisation, following rigorous scientific testing and proven to result in weight loss. Control: non‐social media (n = 45) The control group was given standard care which was to follow the Australian Government dietary guidelines as well as the National Physical Activity Guidelines for Adults. |
|
| Outcomes | Weight loss, blood pressure, waist circumference, hip circumference, fasting blood glucose, lipids, insulin, dietary intake, physical activity, step count, three‐day food record, protein, carbohydrate, fat, alcohol, fibre), three‐day physical activity record, step count. | |
| Equity | High‐income country. Overweight and obese individuals with a body mass index (BMI) between 25 khm2–40 kg/m2 | |
| Notes | Health behaviours: both physical activity and diet were selected as both were reported as primary outcomes. Body function: weight was reported as the primary outcome and was classified as the most patient‐important outcome for this category. Psychological health: psychological health was the only outcome reported for this category. Well‐being: quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using online research randomising software (i.e. random number generator). |
| Allocation concealment (selection bias) | Unclear risk | Recruited participants were enrolled and assigned a three‐digit number in chronological order by the study co‐ordinator. Participants were blinded; randomisation and group allocation was undertaken by the study co‐ordinator |
| Blinding of personnel | High risk | Participants were blinded; randomisation and group allocation was undertaken by the study co‐ordinator. |
| Blinding of participants | Low risk | Participants were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Most outcomes were self‐reported quote:"The discrepancies between weight loss and changes to dietary intake may be explained by inaccurate dietary intake self‐reporting, a common problem in weight management trials" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition after baseline clinic visit, possibly due to intervention burden. Differences between completers and non‐completers not described |
| Selective reporting (reporting bias) | High risk | Changes to mental well‐being, depression, anxiety, stress scales, Quality of life, self‐control, self‐efficacy, social media survey, survey of weight management program, Personality and Individual Difference Questionnaire all listed in trial registration but not reported (ACTRN12614000536662). |
| Baseline characteristics similar | Unclear risk | Facebook group was younger, |
| Baseline outcome measurements similar | High risk | Weight, waist/hip circumference was higher among controls |
| Protection against contamination | Low risk | recruited from the Perth community via advertisements in the West Australian Newspaper and Community Newspapers between 2 July and 11 November 2014. The Facebook group was secret |
Joseph 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: African‐American women (n = 29) Age range: 24 to 49 years Recruitment: email distribution lists, fliers posted at local businesses, advertisements in a local African American newspaper, posting on a local social event website Eligibility: self‐identified as African‐American and female, were sufficiently inactive (<150 minutes/week of moderate‐intensity activity assessed by the short version of the international physical activity questionnaire, were 24‐49 years, had an active Facebook account, could read and write in English Country: United States |
|
| Interventions |
Intervention: multi‐component (n = 14) Participants receive one of two multi‐component physical activity interventions over 8 weeks: a culturally‐relevant, Social Cognitive Theory‐based, intervention delivered by Facebook and text message. Control: non‐social media (n = 15) Non‐culturally tailored print‐based intervention consisting of promotion brochures mailed to their home, not delivered by Facebook. |
|
| Outcomes | Physical activity, self‐reported physical activity, Physical activity, Participant satisfaction, self‐efficacy for physical activity, social support for exercise, self‐regulation for physical activity, outcome expectations for physical activity, BMI, feasibility and acceptability | |
| Equity | High‐income country. African‐American women | |
| Notes | Health behaviours: physical activity was reported as the primary outcome and was considered the most patient‐important outcome reported for this category. Body function: BMI was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy, social support, self‐regulation, outcome expectations were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Personnel provided training to the intervention group |
| Blinding of participants | High risk | Participants were notified of the group assignment by telephone. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reports 100% retention but 1 participant from the intervention group is missing from the results section for physical activity and no reason is provided |
| Selective reporting (reporting bias) | Unclear risk | No protocol but reports all outcomes as described in the methods. |
| Baseline characteristics similar | Low risk | No statistically significant differences in demographic characteristics between groups at baseline. |
| Baseline outcome measurements similar | Low risk | No statistically significant differences but BMI was higher among the intervention group. |
| Protection against contamination | Low risk | Separate group orientations were held for each study arm as participants were blinded to the differences in physical activity promotion materials between arms (i.e. culturally relevant versus non‐culturally relevant). The Facebook group was private. |
Kernot 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: postpartum women (n = 120, 23 captains and 97 invitees). Age range: mean (95% CI) age in years was 31.8 (30.8 to 32.4) Recruitment: A variety of advertising methods (newspapers, Facebook, flyers, and a recruitment agency) were used to aid recruitment. Eligibility:wWomen had to be up to 12 months postpartum, whether with their first or subsequent child, be current Facebook users, be able to read and understand English, and live in greater metropolitan Adelaide (capital city of South Australia, with a population of 1.3 million). Country: Australia |
|
| Interventions |
Intervention: multi‐component intervention (n = 41 ‐ 8 teams) Mums Step it Up Program (MSIU) intervention: Participants were given a pedometer and access to the MSIU Facebook app, a new 50‐day walking challenge where postpartum women were encouraged to team up to each to achieve half a million steps (per person). The app also included a daily physical activity tip (which appeared on the dashboard/main page of the app) and automated e‐mails. Control: non‐social media control (n = 39, 8 teams) Pedometer Condition (Alternative Intervention): participants in the pedometer condition were given a pedometer and a printed log book to record their daily steps over 50 days. There was no group/team component for the pedometer condition. |
|
| Outcomes | MVPA (accelerometer), accelerometer‐derived total activity counts, self reported MVPA and walking, sleep, depressive symptoms, quality of life, BMI. | |
| Equity | High‐income country. Ppostpartum women. | |
| Notes | Health behaviours: accelerometer MVPA was reported as primary outcome. Body function: BMI was the only outcome reported for this category. Psychological health: depressive symptoms was the only outcome reported for this category. Well‐being: quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: no adverse effects were reported. Secondary outcomes: not applicable. Note: Pedometer only condition extracted as control since there was minimal interaction between participants/researcher. The study control condition included written advice on increasing physical activity through email (n = 40, 7 teams). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Teams were randomized (by J.K.) following baseline assessment using a computer‐generated allocation sequence (http://www.randomizer.org/form.htm)" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Quote:"To reduce the chance of bias (blinding of participants and assessors was not possible), most instruments were self‐administered." |
| Blinding of participants | High risk | Quote:"To reduce the chance of bias (blinding of participants and assessors was not possible), most instruments were self‐administered." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote:"To reduce the chance of bias (blinding of participants and assessors was not possible), most instruments were self‐administered." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis used, reasons for dropouts provided Quote:"Twenty‐four participants withdrew from the study after the baseline assessment (MSIU [n = 8], pedometer [n = 6], and control [n = 10]), resulting in an overall retention rate of 82%. Reasons for withdrawal included being too busy (n = 9), not being contactable (n = 6), and falling pregnant (n = 9)." |
| Selective reporting (reporting bias) | Low risk | Outcomes as reported in trial registration and protocol |
| Baseline characteristics similar | Unclear risk | Data provided but differences between groups not reported |
| Baseline outcome measurements similar | Unclear risk | Data provided but differences between groups not reported ‐ There appear to be differences across groups at baseline across MPVA outcomes. |
| Protection against contamination | Unclear risk | Not described ‐ intervention required being on a team and recruited by a Facebook friend but possible that those in control used a pedometer, joined the MSIU app on their Facebook account or was forwarded tips or emails from intervention participants. |
Kim 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: adults with type 2 diabetes (N = 155). Age range: median (IQR) age in years for SM‐HL was 46 (15.50) and control 56 (10). Recruitment: participants were recruited from endocrinology outpatient units at two general hospitals, which were equipped with 940 and 603 beds, respectively, located in the southeast region of South Korea. Eligibility: diagnosed with Type 2 diabetes, poor diabetes control (HbA1c > 7.0%), can read Korean, and owns a smartphone. Country: South Korea |
|
| Interventions |
Intervention: multi‐component intervention (n = 52) Social media–based, health literacy–sensitive diabetes management 8‐week intervention (SM‐HL): Recieved easy‐to‐read diabetes educational materials using teach‐back methods as well as access to social media–based self‐management support (Mastering Diabetes). The social media included group announcement, instant messaging, member feedback, weekly action planning, weekly information on diabetes self‐management (video and easy‐to‐read text formats), and question and answer whenever needed. Comparator: no intervention (n = 52) Usual care: nurses delivered the usual education using a conventional diabetes education brochure. |
|
| Outcomes | Patient activation level (self‐reported knowledge, skills, and confidence related to the self‐management of health condition), diabetes self‐care, HbA1c. | |
| Equity | High‐income country. Diagnosed with type 2 diabetes. | |
| Notes | Health behaviours: diabetes self‐care was the only outcome reported for this category. Body function: HbA1c was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: Not applicable. Adverse effects: not applicable. Secondary outcomes: patient activation level was the only outcome reported for this category. Notes: usual care condition extracted as control since there was minimal interaction between participants/researcher. Telephone‐based, health literacy–sensitive diabetes management intervention (TEL‐HL) was an alternate intervention in which participants received diabetes self‐management education, easy‐to‐read diabetes education brochure and teach‐back method, and telephone self‐management support (weekly action planning and feedback, question and answer, whenever needed). This intervention was not extracted for our review (n = 51) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a web‐based randomisation tool (www.randomizer.org) |
| Allocation concealment (selection bias) | Low risk | Each participant’s allocation assignment was sealed in an envelope and kept from the participants. |
| Blinding of personnel | High risk | Diabetes nurse educator provided initial education and instructions to participants. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote:"The data collector, who assessed all of the outcomes but did not participate in the intervention, was blinded to the study. All outcomes were assessed by a data collector who was unaware of the patients’ group allocation." Self‐report instruments used, however, unclear whether participants were blinded to their assignment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote:"There were no significant differences in the baseline characteristics between patients who dropped out and those who did not, except in the control group, as those not treated with an oral glycemic agent were more likely to have dropped out at the 12‐week follow‐up (χ2 = 9.25, p = .008)." |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Baseline characteristics similar | High risk | "Baseline patient characteristics were similar with regard to sex, income, duration of illness, presence of diabetes complications, use of insulin upon enrollment, and use of an oral glycemic agent among each of the groups (Table S2). However, age, education, HbA1c, and health literacy level at baseline differed among the groups. Patients in the SM‐HL group were younger and more educated, and had poorer glycemic control and higher health literacy." |
| Baseline outcome measurements similar | High risk | Quote:"Baseline patient characteristics were similar with regard to sex, income, duration of illness, presence of diabetes complications, use of insulin upon enrollment, and use of an oral glycemic agent among each of the groups (Table S2). However, age, education, HbA1c, and health literacy level at baseline differed among the groups. Patients in the SM‐HL group were younger and more educated, and had poorer glycemic control and higher health literacy." |
| Protection against contamination | Unclear risk | Not specified. Used a closed social media service, which allowed the registered study participants to access, share, and view posts but possibility of contamination not described |
Kolt 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: insufficiently active adults (n = 504) (328 women, 126 men) Age range: 50. 8± 13.1 (mean ± SD) years Recruitment: permission was obtained from the Australian Electoral Commission to access an extract of 14,000 names and addresses, with accompanying age and gender details, 7000 from each of the Federal electoral divisions of Capricornia (Rockhampton, QLD) and Werriwa (Southwestern Sydney, NSW). Personalized invitation letters were posted to persons on the extract, initially in three batches of 1000 to test the response rate. Eligibility: individuals must live or work in South Western Sydney (New South Wales) or Rockhampton (Queensland), be willing to increase the amount of physical activity that they are currently taking part in, and be over 18 years of age. Country: Australia |
|
| Interventions |
Intervention: multi‐component Web 2.0 (n = 168),Web 1.0 (n = 165) Web 2.0 group participated physical activity intervention including user‐to‐user interaction through social networking capabilities. Web 1.0 group participated in the existing 10,000 Steps programme. Control: non‐social media (n = 171) Paper‐based Logbook |
|
| Outcomes | Physical activity levels, weight, height, abdomen girth, psychosocial correlates, intention, subjective norm, perceived behavioural control, attitude,outcome expectations, self efficacy, barriers to self efficacy, self reported Internet self‐efficacy, user satisfaction, website usability and usage | |
| Equity | High‐income country. Insufficiently active adults | |
| Notes | Health behaviours: physical activity was the only outcome of interest reported for this category. Body function: Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable Secondary outcomes: |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated algorithm |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | ActiGraph GT3X activity monitor and all remaining outcome measures were assessed by a blinded assessor. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition and many for unknown reasons. |
| Selective reporting (reporting bias) | High risk | Not all outcomes are completely reported ‐ e.g. no endline BMI or QoL or pyschosocial correlates, or secondary outcomes |
| Baseline characteristics similar | Low risk | No differences between groups. |
| Baseline outcome measurements similar | High risk | There were no significant between‐group differences for height or waist girth, however, significant differences were reported for weight, BMI and BMI categories. |
| Protection against contamination | Unclear risk | To avoid contamination in cases where participants reside in the same household, the first participant will be randomly assigned to a trial arm and the other participants from that household will also be allocated to the same trial arm. Web 2.0 intervention required access. No mention of how control group was kept out of web 1.0 site |
Koufopoulos 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Asthmatic adults from the who were prescribed an inhaled corticosteroid preventer (n = 216) Participants: participants were excluded if they didn't complete the eligibility questionnaire or baseline measures, did not have asthma, were not prescribed an inhaled corticosteroid preventer inhaler for a weekly regimen of at least one dose per week, did not provide informed consent, or had previously participated in the pilot study. Age range: mean age 28.1 (SD 9.7) Recruitment: emails requesting participants for a study on asthma management were sent out to department secretaries of the 40 largest universities in the UK Eligibility: Asthmatic adults from the who were prescribed an inhaled corticosteroid preventer Country: UK |
|
| Interventions |
Intervention: social media only (n = 99) “AsthmaVillage,” an online community for patients with asthma with which they could leave comments and see who else was online Control: non‐social media (n = 117) “AsthmaDiary,” an online diary for recording inhaled corticosteroid preventer use with no access to the posts of other participants and no way to interact online |
|
| Outcomes | Medication adherence, adherence to the intervention (total number of preventer puffs used to determine site adherence,site activity via community posts and comments | |
| Equity | High‐income country. Individuals who have asthma | |
| Notes | Health behaviours: medication adherence was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | The experimenters manually separated the two lists and emailed both groups log‐in instructions. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐reported outcomes but unclear if participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 60% of intervention participants and 45% of control participants dropped out of the study. Reasons were not provided. Used intention‐to‐treat (ITT) analyses. |
| Selective reporting (reporting bias) | Unclear risk | No protocol but all outcomes in the methods section are reported in the results section |
| Baseline characteristics similar | Low risk | No important differences were present across study groups |
| Baseline outcome measurements similar | Unclear risk | Significance was not tested between study groups. Other important baseline measures were taken and not reported in the study. |
| Protection against contamination | High risk | Quote:"It was not possible to determine whether an individual operated multiple accounts on AsthmaVillage or the online diary. Account passwords were screened by the experimenters for duplicates in an attempt to mitigate this possibility." |
Lau 2012.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: university students and staff (n = 742) Age range: 18 years and above Recruitment: students and staff were approached via mailing lists and advertisements in online print publications, which described the study and invited participants to complete an online pre‐study survey. Eligibility: aged 18 or above and access to the Internet, and email at least on a monthly basis Country: Australia |
|
| Interventions |
Intervention: multi‐component (n = 372) The PCHMS (personally controlled health management system ) called Healthy.me integrated an untethered personal health record with consumer care pathways, social forums, and messaging links with a health service provider‐ Healthy.me Control: no intervention (n = 370) Could use the system after 6 months, when the trial had concluded. |
|
| Outcomes | Influenza vaccination, participants visiting the UHS during the study, symptoms of Influenza‐Like Illness (ILI) during the study, using medications or remedies due to ILI symptoms, participants visiting a healthcare professional due to ILI symptoms, impairment in work or study due to ILI symptoms, number of days absent from work or study due to ILI symptoms, reasons for receiving (or not receiving) influenza vaccine, patterns of usage and feedback concerning PCHMS | |
| Equity | High‐income country | |
| Notes | Health behaviours: proportion of participants obtaining influenza vaccination was considered the most patient‐important outcome for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence |
| Allocation concealment (selection bias) | Low risk | Allocation occurred automatically at enrolment. Participants received the next consecutive allocation in the random number sequence. |
| Blinding of personnel | Low risk | Investigators and clinicians were blinded to group allocation. |
| Blinding of participants | High risk | Group allocation was revealed to participants after obtaining their consent to participate and completion of the pre‐study survey |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigators and clinicians were blinded to group allocation. Only administrative staff at the practice would receive requests for appointments facilitated by Healthy.me; no clinical staff assessing patient outcomes and/or administrating influenza vaccination would receive these appointment requests. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for exclusion from analysis provided for all those with missing data (e.g. received influenza vaccination prior to study, possible contamination) |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in protocol included in the results and/or supplementary data |
| Baseline characteristics similar | Low risk | No significantly significant differences between the groups. |
| Baseline outcome measurements similar | Low risk | No significantly significant differences between the groups. |
| Protection against contamination | Low risk | To minimise contamination of the control group, the intervention group was asked to not share their access details with others. Four participants who reported being influenced by other participants were excluded from the analysis. |
Li 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: HIV positive men who have sex with men (N = 214). Age range: 56.1% of participants were ≤30 years of age Recruitment: posters displayed in the public area of the NGO and social media of their service users. The four peer fieldworkers approached prospective participants by making phone calls and reaching them through social media. Eligibility: men who have had anal sex with at least one men in the last six months, more than 18 years‐old, diagnosed as HIV positive for at least three months (as newly diagnosed PLWH tends to be unstable), with intention to stay in Chengdu in the coming six months, and a regular QQ user (use QQ for at least once a week). Country: China |
|
| Interventions |
Intervention: social media only (n = 105) Three Good Things with social networking (TGT‐SN) 1 month intervention: Participants posted brief messages on three goods things that they experienced and felt grateful for daily on Tencent QQ. They could read and provide feedback to other participants. Control: active social media comparator (n = 109) Received information about mental health promotion from research assistants via Tencent QQ once a week during the one‐month intervention period. No QQ group was formed for the control group. |
|
| Outcomes | Probable case of mild to severe depression, depressive symptoms, probable general anxiety disorder, gratitude, positive affect and negative affect, happiness, satisfaction with life, social support, self‐stigma, enacted stigma, and perceived stress. | |
| Equity | Upper middle‐income country. HIV‐positive men who have sex with men. | |
| Notes | Health behaviours: not applicable. Body function: not applicable. Psychological health: probable depression cases was reported as primary outcome. Well‐being: satisfaction with life was the only outcome of interest reported for this category. Mortality: not applicable. Adverse effects: no observable adverse events took place during the intervention period. Secondary outcomes: social support was the only outcome of interest reported for this category, but could not be included as it was not measured using a validated tool. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"Block randomization (size =6) was used, and randomization was performed using a computerized random number generator." |
| Allocation concealment (selection bias) | Low risk | Quote:"Allocation was concealed by sealed and sequentially numbered envelopes from all participants and field workers" |
| Blinding of personnel | High risk | Quote:"The research assistants sent two ‘LIKE’ feedbacks to each member every week on different weekday to ensure everyone was getting some positive feedback" |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition, similar between groups. Reasons provided. |
| Selective reporting (reporting bias) | Unclear risk | No protocol, At time of trial registration anxiety was listed as the primary indicator (not depression) |
| Baseline characteristics similar | Low risk | Quote:"All baseline background characteristics and baseline outcome measures were well balanced between the two study arms as indicated by the nonsignificant differences in background characteristics between the two groups." |
| Baseline outcome measurements similar | Low risk | Quote:"All baseline background characteristics and baseline outcome measures were well balanced between the two study arms as indicated by the nonsignificant differences in background characteristics between the two groups." |
| Protection against contamination | High risk | Quote:"Among the 105 participants in the control group, 87 (82.9%) have never heard about the TGT exercise; 10 (9.5%) have heard about the TGT exercise but never practiced it; and 8 (7.7%) have conducted the TGT exercise during the study period. Among the 99 participants in the TGT‐SN group who have completed the follow‐up survey at T1, 24 (24.2%) have told the exercise to other MSM who also participated in the study" |
Li 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: pregnant women (N = 1050). Age range: 18‐45 years of age. Recruitment: continuous sampling of pregnant women with early intrauterine pregnancy in the three Maternal and Child Hospitals. Eligibility: women aged 18–45 years old, permanent residents in Chengdu, confirmed being pregnant and were at <13 weeks of gestation, did not register to the antenatal care system before 13 weeks of gestation, no history of extra uterine pregnancy, hypertension, diabetes, heart disease, anaemia, and recurrent abortion, had a WeChat account and used it often (i.e., ‡3 times/week), and consented to be randomly assigned to either of the four groups. Country: China |
|
| Interventions |
Intervention: multi‐component intervention (n = 700) WeChat ‐ Health education information about maternal health care at least every 2 weeks via WeChat (n = 350) and WeChat plus Specialist Team with at least 5 phone calls from the specialist team during pregnancy and one time postpartum (team reminded women to take prenatal examinations and postpartum check‐ups, provided referral of high‐risk pregnancies, and provided postpartum visits) (n = 350). Control: non‐social media control (n = 350) Routine maternal healthcare control. |
|
| Outcomes | Satisfaction rate of participants, rate of early pregnancy care, rate of maternal system management and rate of postpartum visit. | |
| Equity | Upper middle‐income country. Pregnant women. | |
| Notes | Health behaviours: maternal system management was selected for this category as it incorporated other health behaviour outcomes reported (i.e., pregnant women who attended the service package including the first antenatal care visit within the first trimester, five times antenatal care visits, and delivered baby in a health facility and postnatal visit) and was considered the most patient‐important.
Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. Note: usual care condition extracted as control since there was minimal interaction between participants/researcher. Specialist team intervention included 5 or more phone calls during pregnancy and once during postpartum (n = 350). This intervention was not extracted for our review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"In a quiet room in front of a computer, the participant was informed to click on the ‘‘start’’ button of the software, which randomly generates a number between 0 and 3. The number 0, 1, 2, and 3 indicates an assignment to the SAU, WC, ST, and WC‐ST group, respectively" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition, reasons provided |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available, results as reported in methods |
| Baseline characteristics similar | Low risk | At baseline, participants in the four groups did not show significant differences in their age, education, family income, gravidity, and parity |
| Baseline outcome measurements similar | Low risk | No differences in satisfaction rates across groups, postpartum maternal health care service utilization could not be measured at baseline |
| Protection against contamination | Unclear risk | Quote:"Another concern is possible contamination from the WC and WC‐ST participants who may forward the WC information to the other two groups, although they were required and agreed not to share the WC information with others." |
Liao 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: mothers with at least one child aged 6 to 72 months (N = 365). Age range: 58.7%, 51.2% and 57.3% of parents were between 18 ‐ 34 years of age for the intervention group with a time component, intervention without a time component and control group, respectively. children were between the ages of 6 and 72 months old. Recruitment: recruited from previous samples of population‐based random‐dialled household telephone surveys and community outreach conducted by a commercial polling company. Eligibility: mothers with at least one child aged 6‐72 months as well as Chinese communication fluency, having a Hong Kong network‐connected smartphone with Internet access, and having installed or being willing to install WhatsApp on their mobile phone. Country: China |
|
| Interventions |
Intervention: social media only (n = 160) 8‐week intervention with weekly reminders, with (n = 80) or without (n = 80) a time pressure component, for seasonal influenza vaccination via WhatsApp discussion groups. Intervention groups were encouraged to share their positive vaccination decisions and experiences. Control: No intervention (n = 205) |
|
| Outcomes | Children’s SIV uptake before and during the 2017/18 influenza season, intention to take child for influenza vaccination, parental perceptions about vaccination. | |
| Equity | Upper middle‐income country. Mothers. | |
| Notes | Health behaviours: vaccination uptake was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: intention and attitudes were the only outcomes reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"Before each telephone interview, the interviewer opened a sealed envelope which contained a random allocation sequence generated by computer to determine the subject’s group allocation." |
| Allocation concealment (selection bias) | Low risk | Quote:"Before each telephone interview, the interviewer opened a sealed envelope which contained a random allocation sequence generated by computer to determine the subject’s group allocation." |
| Blinding of personnel | High risk | Quote:"The moderator also addressed any questions, concerns or misunderstandings raised about influenza and influenza vaccination, if these were not first addressed by other mothers within the groups" |
| Blinding of participants | High risk | Quote:"Participants could not be blinded to subject allocation. Subjects who were allocated to an intervention group were notified that they would be participating in a WhatsApp discussion group during the intervention period to receive weekly vaccination reminders and share their views and experiences about SIV with other mothers and a group moderator" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote:"The interviewers who conducted baseline assessment were blind to the interventions arm (with or without time pressure) participants occupied. The assessor of the primary outcome was blinded to all participant group allocation. However, participants, whom were unblinded, self‐reported their vaccination uptake (primary outcomes). Data on children’s SIV uptake were reported by parents and could not be validated from children’s medical records and may be subject to social desirability bias." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote:"Participants of the intervention groups were more likely to drop out from the outcome assessment than were the control (χ222=8.0, P=.02), but those who completed the baseline assessment and outcome assessment did not differ by intervention condition in terms of their demographics, their target child’s characteristics, past SIV uptake, baseline SIV perceptions, and intention to take child for SIV. Difference could be related to vaccination status (e.g., those in intervention group were not intending to vaccinate their child and therefore, did not care to receive education and support on vaccination topics)." "Intention‐to‐treat analysis was used as a conservative and sensitivity analysis by treating the lost outcomes as not vaccinated over the specific CIVSS campaign to compare with the complete case analysis." Intention to treat results not provided for secondary outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available, all outcomes described in methods section are reported in results |
| Baseline characteristics similar | Low risk | Those who completed the baseline assessment and the outcome assessment did not differ by intervention condition in terms of their demographics, their target child’s characteristics, past SIV uptake, baseline SIV perceptions and intention to take child for SIV |
| Baseline outcome measurements similar | Low risk | Those who completed the baseline assessment and the outcome assessment did not differ by intervention condition in terms of their demographics, their target child’s characteristics, past SIV uptake, baseline SIV perceptions and intention to take child for SIV |
| Protection against contamination | Unclear risk | WhatsApp discussion group messages (e.g., weekly vaccination reminders, number of days remaining for the recommended vaccination timing) could have been communicated to other study participants. Methods for protection of ensuring the group remained closed were not described. |
Linden 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: women with Type 1 diabetes were recruited between November 2011 and December 2014 in their first or early second trimester of pregnancy (n = 174) Age range: >18 years Recruitment: women with Type 1 diabetes were recruited in their first or early second trimester of pregnancy and registered at one of the six participating study centres. Eligibility: literate and Swedish speaking pregnant women aged >18 years with a diagnosis of Type 1 diabetes and registered at one of the six participating study centres. Country: Sweden |
|
| Interventions |
Intervention: multi‐component (n = 83) Web support with evidence‐based information, self‐care diary and communication with pregnant women with Type 1 diabetes in addition to standard care Control: non‐social media (n = 91) Standard care during pregnancy, childbirth and immediately after. Standard care varied, although all clinics offered frequent contact with midwives, obstetricians and endocrinologists during pregnancy, and one follow‐up visit after childbirth. |
|
| Outcomes | The primary outcomes (mean difference, measured at 6 months after childbirth) were well‐being and diabetes management.The secondary outcomes were psychometric scales measuring psychosocial variables and medical outcomes including Hypoglycemia fear, Diabetes‐related distress, and self‐perceived health. HbA1c values The intervention group evaluated the web‐based support using a structured questionnaire also containing a free‐text alternative. | |
| Equity | High‐income country. Pregnant women with a diagnosis of Type 1 diabetes | |
| Notes | Health behaviours: not applicable. Body function: HbA1c was the only outcome reported for this category. Psychological health: diabetes distress was the only outcome reported for this category. Well‐being: well‐being was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy in diabetes management, self‐perceived health, sense of coherence, and fear of hypoglycaemia were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence generation not described. The authors state "randomly allocated (1:1) by the study midwife to the intervention group or the control group, using block randomization" |
| Allocation concealment (selection bias) | Low risk | Quote:"Using block randomization with prepared closed envelopes" |
| Blinding of personnel | Low risk | The diabetes midwives in charge of the random allocated sequence at the centres are not involved in the preparation of the envelopes, the use of web‐based support or in the statistical analyses. |
| Blinding of participants | High risk | Due to the nature of this trial it is not possible to blind the participants. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | One limitation of the study is that it is not feasible to blind members of the healthcare team to group allocation. Some outcomes are self‐reported and participants were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The dropout rate was high but not unexpected, and increased with miscarriages, neonatal and infant deaths. The participants included in the intention‐to‐treat analysis consisted of 158 women (intervention group, n = 78; control group, n = 80) |
| Selective reporting (reporting bias) | High risk | Outcomes in protocol but not in paper: self‐rated health, breastfeeding rate, experiences of nursing. |
| Baseline characteristics similar | Low risk | In the intervention 74.4% administered insulin via multiple injections versus 53.8% in the control group (P = 0.01). Adjusted for in analysis |
| Baseline outcome measurements similar | High risk | Well‐being measured with WBQ12 differed at baseline (i.e. in early pregnancy), with the control group scoring lower (P = 0.05; Table 2). Not adjusted for in analysis. |
| Protection against contamination | High risk | The research group has no way of monitoring and/or limiting access to other web‐based forums in relation to diabetes or childbearing during the study period. |
Looyestyn 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Age range: adults aged 18 to 50 years (n = 89) Recruitment: recruited through a variety of advertising methods including online (via Facebook advertising) and via print media Eligibility: (1) aged between 18 and 50 years, (2) Australian residents, (3) current Facebook users, (4) able to read and understand English, and (5) not participating in a regular running program Country: Australia | |
| Interventions |
Intervention: social media only (n = 41) UniSA Run Free program, an 8‐week Web‐based beginners’ running intervention, delivered via a closed Facebook group that included daily interactive posts (information with links, motivational quotes, opinion polls, or questions) and details of the running session Control: non‐social media (n = 48) The control group who received a hard copy of the running program |
|
| Outcomes | Self‐reported MVPA and cardiorespiratory fitness, self‐efficacy, exercise attitudes, and social support, adverse effects, engagement and feasibility | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: cardiorespiratory fitness was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: all reported adverse effects were selected as per our criteria. Secondary outcomes: self‐efficacy, attitude, and social support were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence with allocation concealment |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes were used for allocation concealment |
| Blinding of personnel | High risk | Upon enrolment, they were randomly allocated (by the primary researcher. |
| Blinding of participants | High risk | Blinding of participants was not possible because of the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self reported outcomes and participants were aware of assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar numbers of participants did not complete the 5 month assessment with similar reasons. ITT analysis. |
| Selective reporting (reporting bias) | Unclear risk | Not reported. Protocol not available. |
| Baseline characteristics similar | High risk | The intervention group included 90% women compared to 71% in the control group and had a higher proportion of participants with university or higher education compared to high school and diploma or further education certificate. |
| Baseline outcome measurements similar | High risk | The control group reported moderate‐vigorous physical activity than the intervention group at baseline. |
| Protection against contamination | Low risk | The Facebook group was a closed group and recruitment took place online through advertisements and participants could be located anywhere in Australia.. |
Lytle 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: colleges students in Minnesota (n = 441) Age range: 18–35 years Recruitment: CHOICES study staff recruited students to participate in the study with help from the administrative offices at the colleges using a variety of approaches, including e‐mail invitations, posters and table tents in the college, and information tables staffed by CHOICES staff. Eligilibity: (1) being aged 18–35 years; (2) having a BMI between 20 and 34.9 kg/m2; and (3) planning to live in the geographic area for at least 2 years. A BMI of ≥20 was chosen as the lower cut point to help guard against unhealthy weight loss. Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 187) A social network website designed for the CHOICES study was introduced in the course and encouraged self‐monitoring, goal setting, and interaction around the same health behaviours taught in the course. Incentives in the form of points for participation were provided and could be redeemed for a variety of wellness‐related products such as yoga mats and cooking utensils Control: Non‐social media (n = 179) Students randomised to the control condition received health assessments with their measurement visits as well as basic health promotion information on a quarterly basis |
|
| Outcomes | Change in body mass index (BMI). weight, body fat percentage, waist circumference, weight status, diet (fast food, sugary beverages, breakfast, at‐home meal preparation), physical activity/screen time (minutes and energy expenditure in leisure time physical activity, television viewing, leisure time computer use) and sleep (hours of sleep, time required to fall asleep, days not getting enough rest, difficulty staying awake). | |
| Equity | High‐income country. College students (young adults) | |
| Notes | Health behaviours: physical activity was considered to be the most patient‐important outcome for this category. Body function: both BMI and weight were reported as primary outcomes. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not clear how participants were randomised. States: "The data management team used a random allocation sequence to assign participants to either condition." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Trial registration states that there was no masking. |
| Blinding of participants | High risk | Trial registration states that there was no masking. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Trial registration states that there was no masking. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Women in the intervention condition were slightly more likely to drop out as compared with women in the control condition (data not shown). Those lost to follow‐up were more likely to be non‐white and have a higher income or not report their income. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported in trial registration reported in papers. Additional outcomes also reported (e.g. body fat percentage, waist circumference, behaviour outcomes). |
| Baseline characteristics similar | Low risk | There were no statistically significant differences by treatment condition, |
| Baseline outcome measurements similar | Low risk | There were no statistically significant differences for BMI, weight, waist circumference, or body fat percentage. |
| Protection against contamination | Unclear risk | Students were blocked by college but unclear whether there were other measures to prevent contamination. |
Maher 2015.
| Study characteristics | ||
| Methods | cRCT | |
| Participants | Age range: adults aged 18 to 65 years (n = 110 participants, 25 teams) Recruitment: 'Snowball style' recruiting. Participants were recruited through a Facebook advertising campaign, media stories (local newspaper and television news), and distribution of flyers at the University of South Australia campuses. Participants invited eligible Facebook friends to form a team. Eligibility: (1) were between the ages of 18 and 65 years, (2) considered themselves insufficiently active (i.e.not currently achieving the Australian guidelines of 150 min of MVPA/week), (3) were current Facebook users, (4) did not have an existing medical condition for which they had been advised by a doctor to avoid exercise, and (5) were able to speak English Country: Australia | |
| Interventions |
Intervention: multi‐component (n = 51 individuals, 12 teams) Team‐based Facebook app for encouraging physical activity. Participants were provided a pedometer and encouraged to achieve 10,000 steps per day and work in teams of 3 to 8 existing Facebook friends. Control: no intervention (n = 59 individuals, 13 teams) A wait‐listed control condition. |
|
| Outcomes | Self‐reported total weekly moderate‐vigorous physical activity, physical activity types/intensities separately (1. weekly walking time, other moderate physical activity, and vigorous physical activity; all derived from the AAS), and quality of life, feasibility. | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence with blocking |
| Allocation concealment (selection bias) | Unclear risk | States: "computer‐generated randomization sequence with blocking ...with allocation concealment" but no details provided. |
| Blinding of personnel | Unclear risk | Not reported, but does report that single blinding of outcome assessors was achieved |
| Blinding of participants | High risk | Blinding of participants was not possible. Participants received an automated email informing them of which condition they were enrolled in and when their Active Team challenge would begin. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Single blinding was achieved, in that the outcome measures were administered by computer. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 15% attrition. Missing data were imputed for the small number of individuals using baseline observations carried forward. |
| Selective reporting (reporting bias) | High risk | Outcomes are slightly different than those listed on trial registration, for example, the primary outcome for the trial registration is number of steps using pedometer but the paper reports minutes of moderate‐vigorous physical activity assessed by survey as primary outcome. |
| Baseline characteristics similar | Low risk | Similar between groups |
| Baseline outcome measurements similar | Low risk | Similar between groups |
| Protection against contamination | Low risk | Teams allocated to the intervention condition received access to the full Active Team app and were mailed a pedometer. |
Mailey 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: working mothers (n = 69) Age range: not reported Recruitment: nationally by contacting schools, childcare centres, newspapers, bloggers, and moms groups and asking if they would consider posting a blurb about the study in a newsletter, on their Facebook page, or on their website Eligibility: mothers working at least 30 hours/week, with a child under the age of 12 living at home, and engaging in less than 150 minutes/week of moderate‐to‐vigorous physical activity. Country: USA |
|
| Interventions |
Intervention: social media only (n = 33) Same intervention as control with additional interactive features including group dynamics content on the discussion board each week and participants were placed in small discussion groups with weekly tasks (e.g. set a group physical activity goal) and received several weekly discussion prompts. Control: less intense social media (n = 36) 8‐week intervention delivered online including a weekly email containing tasks for the week, such as listening to a podcast, completing an assignment in their workbook and communicating with other participants through the website's discussion board. |
|
| Outcomes | Physical activity (both GLTEQ and MAQ scores), self‐worth, exercise motivation, self‐efficacy, website use | |
| Equity | High‐income country. Working mothers. | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: not applicable. Psychological health: physical self‐worth was the only outcome reported for this category. However data provided in the tables conflicted with the data in the text. We contacted authors to ask for clarification. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy was considered to be more patient‐important than perceived motivation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random digit generator. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Self‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants who completed the study reported higher introjected regulation and lower self‐efficacy at baseline than those who dropped out. Reasons for missing outcome data were not provided. Completers and dropouts did not differ on any demographic variables at baseline. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available but all outcomes reported in the methods are reported in results |
| Baseline characteristics similar | Low risk | No significant differences between groups. |
| Baseline outcome measurements similar | High risk | Physical activity was higher in the control group at baseline |
| Protection against contamination | Low risk | Intervention was entirely online and participants did not know each other when they enrolled in the study |
Mascarenhas 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: women with children (N = 64). Age range: 18‐60 years of age. Recruitment: participants were recruited using advertisements that included a link to our study website in parent‐specific Facebook groups and email listservs. Eligibility: women needed to be between the ages of 18 and 60 years, speak and understand English, be able to give consent, and have at least 1 child under the age of 12 years. Participants were also required to have access and understand how to operate 2 devices, one with videoconferencing capacity and one with mobile app capacity. Participants had to be capable of exercising safely. Country: USA |
|
| Interventions |
Intervention: social media only (n = 30) The Moms Online Video Exercise (MOVE): Joined daily group exercise sessions (2 to 5 participants) that lasted no more than 30 minutes for 8 weeks using Google Hangouts videoconferencing. Participants were connected to their group members via email. Control: no intervention (n = 34) Waitlist control. |
|
| Outcomes | Physical activity (MVPA minutes per week), weight, social support for physical activity, physical activity self‐efficacy, anxiety, sleep disturbance, depression, and fatigue, participant adherence and acceptability. | |
| Equity | High‐income country. Women with children. | |
| Notes | Health behaviours: physical activity (MPVA) was reported as primary outcome. Body function: weight was considered the most patient‐important outcome for this category. However, only data on treatment effect was available Psychological health: anxiety and depression were both considered patient‐important outcomes for this category. However, only data on treatment effecst were available. Well‐being: not applicable. Mortality: Nnt applicable. Adverse effects: not applicable. Secondary outcomes: social support for physical activity and physical activity self‐efficacy were the only outcomes of interest reported for this category. However, only data on treatment effect were available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"Our statistician generated a stratified block random sequence using Stata 14 (StataCorp, Texas, USA) and stored it in Research Electronic Data Capture (REDCap), a secure, Web‐based database application hosted at the University of California, San Francisco" |
| Allocation concealment (selection bias) | Low risk | Quote:"The sequence was concealed from the primary investigator who used REDCap to reveal the computer‐assigned randomization once participants were enrolled." |
| Blinding of personnel | High risk | Quote:"The assignment was not blinded to investigators or participants." |
| Blinding of participants | High risk | Quote:"The assignment was not blinded to investigators or participants." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote:"We relied on a self‐report measure of physical activity, which though validated and widely used, could have introduced bias." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis. Low attrition. |
| Selective reporting (reporting bias) | High risk | Additional outcomes described in Clinicaltrials.gov that are not reported on: Change in exercise enjoyment, Change in global health (PROMIS Global Health 7 measure ‐ in study reported short form) |
| Baseline characteristics similar | High risk | Number of children which was unbalanced at baseline. |
| Baseline outcome measurements similar | Unclear risk | Appear to be differences in MPVA, significance not assessed |
| Protection against contamination | Unclear risk | Methods for containment not described. Intervention group received a link to their respective Google Hangouts videoconferencing group calls. Possibly could have been forwarded to control participants. |
Morris 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: adults (n = 217) Age range: 18‐35 Recruitment: participants were recruited from various universities, Internet websites (craigslist, research portals), and through social media channels (Facebook, Twitter). Participants signed up on the Web, by submitting their emails on the study recruitment website. Eligibility: participants needed to be native English speakers between the ages of 18 and 35. Country: USA |
|
| Interventions |
Intervention: social media only (n = 108) A web‐based peer‐to‐peer cognitive reappraisal platform designed called Panoply was used to allow participants to post negative thoughts and situations and receive responses from other participants. Control: Non‐social media (n = 109) 'Expressive writing' ‐ The visual and interface design for the control condition was built to mirror the Panoply intervention. The instructions for describing stressful situations and negative thoughts were exactly the same but the participants did not receive feedback from the crowd and were not given the opportunity to provide feedback to others. |
|
| Outcomes | Symptoms of depression, reappraisal frequency, and maladaptive rumination, engagement, activity levels | |
| Equity | High‐income country | |
| Notes | Health behaviours: not applicable. Body function: not applicable, depressive symptoms was the only outcome reported for this category. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The randomisation sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Experimenters were not blind to the random assignment of participants so that they would be able to answer questions about either intervention. During the study, only 4 participants emailed for technical support or clarification. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition, reasons provided, but were not reported per group. |
| Selective reporting (reporting bias) | High risk | Trial registration includes additional outcomes: subjective happiness scale, positive and negative affect schedule |
| Baseline characteristics similar | Low risk | No significant differences in baseline characteristics |
| Baseline outcome measurements similar | Low risk | No significant differences in baseline scores for the different outcome measures. |
| Protection against contamination | Low risk | Participants were asked to use their study IDs to create an anonymous account on their assigned platform |
Moy 2010.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: patients with self‐reported emphysema, asthma, or bronchitis (n = 24) Age range: not reported Recruitment: not reported Eligibility: patients with self‐reported emphysema, asthma, or bronchitis and at least one of: Type 2 diabetes, coronary artery disease, or BMI >25 Country:USA | |
| Interventions |
Intervention: multi‐component (n not reported)
Walking intervention with pedometer and step count feedback, goal setting, website with, and an online discussion board to communicate with other participants. Control: non‐social media (n not reported) Same as the intervention but without access to the online community |
|
| Outcomes | Step counts | |
| Equity | High‐income country, People with COPD | |
| Notes | Notes that analyses showed no difference between groups for step count and therefore data presented for all participants as a separate group. Authors contacted to provide data by group assignment but did not respond. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Baseline characteristics similar | Unclear risk | Not reported |
| Baseline outcome measurements similar | Unclear risk | Not reported |
| Protection against contamination | Unclear risk | Not reported |
Moy 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: veterans with COPD (n = 239) Age range: mean age 67 (SD 9 years) Recruitment: potential participants were identified from a national database of veterans who had received medical services in the previous year Eligibility: COPD diagnosis, able to walk a minimum of one block, sedentary, has a health‐care provider who can give medical clearance, competent to give informed consent, checks e‐mail weekly, has access to a computer with an Internet connection, a USB port, and not involved in another pedometer‐based walking program Country:USA |
|
| Interventions |
Intervention: multi‐component (n = 155) The intervention arm receives iteratived step‐count feedback; individualised step‐count goals, motivational and informational messages, and access to an online community. Control: non‐social media (n = 84) Instructed to wear the pedometer every day,upload step‐count data at least monthly, and report adverse events ‐ no instructions about exercise, were not assigned step‐count goals, and had access to a web page that only showed a count of what week they were in the study. At the end of the 12‐month study, they were given the option to participate in the Internet‐mediated intervention. |
|
| Outcomes | Change in Saint George’s Respiratory Questionnaire ‐ health related QoL,hospitalizations for COPD‐related adverse events, self‐reported dyspnoea, change in average daily step counts, adverse events | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: health‐related quality of life was considered to be the most patient‐important outcome for this category. Mortality: not applicable. Adverse effects: all reported adverse effects were selected as per our criteria. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group assignment was computer generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | All participants who are randomised to the intervention arm have access to the study staff for questions, which could be initiated by sending an email or directly on the website through a form. Participants can also call the staff on a toll‐free number |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported, outcomes were self‐reported online |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention to treatment and only 1 individual was excluded from analysis (from intervention group). The analysis excluded one outlier whose change for St. George's respiratory Questionnaire was 4.0 standard deviations greater than the mean for change. |
| Selective reporting (reporting bias) | High risk | Some secondary outcomes were not reported: hospitalisations for COPD‐related adverse events, self‐reported dyspnoea |
| Baseline characteristics similar | Low risk | There was no significant between‐group difference for all characteristics |
| Baseline outcome measurements similar | Low risk | There was no significant between‐group difference for all outcome measures |
| Protection against contamination | Unclear risk | Not reported |
Nam 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: cancer patients (n = 337) Age range: mean 38.9 (SD 14.6 years) Recruitment: recruited through a public ad posted on Facebook and Twitter and online pages that support cancer management and awareness. Eligibility: having been diagnosed with cancer or being in a state of survival, at least 18 years old, own a smartphone or mobile device with internet and app functionality, active on social media and use their phones or mobile devices daily for text messages Country: USA |
|
| Interventions |
Intervention: Social media only (n=164) Private Twitter‐based cancer support group, each with 17 to 20 recruited subjects. Control: No intervention (n=173) Participants assigned to the control group did not participate in the Twitter‐based support program. |
|
| Outcomes | health status: (1) whether each patient was confident with his/her cancer treatment, (2) had become better at managing his/her cancer‐related condition, (3) had become more optimistic about his/her cancer‐related condition, (4) had felt an increase in self‐esteem, and (5) had discovered an enhanced feeling of health and well‐being; social capital: bridging and bonding social capital, social support; Self‐efficacy | |
| Equity | High‐income country. Diagnosed with cancer or being in a state of survival | |
| Notes | Health behaviours: not applicable. Body function: not applicable. Psychological health: not applicable. Well‐being: cancer‐related coping skills and quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: social support and self‐efficacy were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | The researcher created a group account on Twitter for each support group and marked it protected. Participants were instructed to follow the group account on Twitter and the researcher manually approved each follower and followed them back. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition, most measures had 5% to 15% missing data. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available and all outcomes from methods presented in results. |
| Baseline characteristics similar | Low risk | Baseline charactersitics similar. |
| Baseline outcome measurements similar | Unclear risk | Not reported |
| Protection against contamination | Low risk | Participants could only access the private Twitter account when manually approved by the research team. |
Nam 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: university women experiencing Premenstrual Syndrome (PMS) (N = 68). Age range: mean (SD) age in years of was 22.25 (1.88) for the intervention group and 21.66 (2.19) for the control group. Recruitment: posted flyers on Campus. Eligibility: menstruating university students not on hormone therapy. Country: South Korea |
|
| Interventions |
Intervention: multi‐component intervention (n = 34) Social‐media‐based support for 4‐weeks through Fitbit Flex (Fitbit’s smartphone application), text messages, and e‐mail. Intervention included general and tailored information on PMS and physical activity through a smartphone application and text messages and support groups of 6‐10 participants through smartphone applications twice a week. Control: Non‐social media control (n = 34) Provided information about PMS and physical activity. |
|
| Outcomes | Premenstrual Syndrome levels (total score and 18 different symptom presentations) and physical activity (MET minutes/week, walking days, walking minutes, moderate days, moderate‐intensity activity minutes, vigorous days, vigorous‐intensity activity minutes). | |
| Equity | High‐income country. University women who experience PMS. | |
| Notes | Health behaviours: physical activity MET min/week was selected over other physical activity outcomes because it provided a total score, per our criteria. Body function: total PMS scores was selected over other PMS level outcomes because it provided a total score, per our criteria. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | SPSS random number generator by simple randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Participants received encouragement from the researchers twice a week |
| Blinding of participants | Unclear risk | Not specified. However, quote: "Participants had one‐on‐one meetings with a researcher before entering the study to learn the study purpose and procedures and sign informed consent forms." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 dropouts per arm, reasons provided |
| Selective reporting (reporting bias) | Unclear risk | No protocol, outcomes as reported in methods |
| Baseline characteristics similar | Low risk | No significant demographic differences |
| Baseline outcome measurements similar | Low risk | No differences between group |
| Protection against contamination | Unclear risk | Not reported ‐ however, control participants could theoretically be using the Fitbit Flex app, they could additionally be interacting with intervention participants through the app. |
Namkoong 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: university students (n = 201)
Age range: not reported
Recruitment: undergraduate students enrolled in a Southeastern university via e‐mail invitations
Eligibility: undergraduate students over the age of 18 who had active Facebook accounts Country: USA |
|
| Interventions |
Intervention: social media only (n = 101) Facebook page to which a researcher posted messages every day for three weeks on anti‐smoking. Participants were invited to contribute by posting their ideas related to the posts as well as their own relevant messages (e.g. videos, text, photos), discuss with others, and "like" posted content. Control: active social media intervention (n = 100) Facebook page with the same content as the intervention group but without the interactivity features. |
|
| Outcomes | Attitude, descriptive and subjective norms, behavioural control, behavioural intention, information‐seeking related to smoking | |
| Equity | High‐income country. Students | |
| Notes | Data presented as a path analysis and therefore could not be used. Authors contacted but no response. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Baseline characteristics similar | Unclear risk | Not reported |
| Baseline outcome measurements similar | Unclear risk | Not reported |
| Protection against contamination | Unclear risk | Not reported |
Napolitano 2013.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: college students (n = 52) Age range: 18‐29 years Recruitment: recruited from a large, urban university in the eastern United States. University media outlets (e.g., online newspaper), posting flyers, broadcasting electronic announcements on websites, Facebook, and listservs, and partnering with campus and student organisations. Eligibility: (i) age 18‐29 years; (ii) body mass index (BMI) of 25 kg/m2 to 50 kg/m2; (iii) healthy enough to participate in physical activity and lose weight safely determined by an in‐person physical with a physician; (iv) a mobile phone plan that included unlimited texting; and (v) an active Facebook user. Country: USA |
|
| Interventions |
Intervention: social media only Facebook (n = 17) and Facebook Plus text messaging and personalized feedback (i.e., Facebook Plus) (n =18) Control: no intervention (n = 17) Waiting List control group |
|
| Outcomes | Weight loss after 8 weeks, physical activity behavior, goal setting and planning, Physical activity self‐efficacy, 4) Weight self‐efficacy, 5) Adapted social support for diet and exercise, 6) Engagement/compliance, 7) Consumer satisfaction | |
| Equity | High‐income country. University students | |
| Notes | Health behaviours: not applicable. Individual data for behaviour outcomes were not reported. Body function: weight loss was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. Individual data for social support and self‐efficacy were not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Participants in the intervention group were invited to join the group and had to accept the request. |
| Blinding of participants | Unclear risk | Participants had to accept the invitation to join the group but unclear if they were aware what the other arms received. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High retention. 100% at 4‐week assessment, and 96% at 8‐weeks. |
| Selective reporting (reporting bias) | Unclear risk | No protocol. Data for secondary outcomes of physical activity and psychosocial measures not presented and instead the report just mentions that ANCOVAs with pos‐hoc contracts found no significant differences. |
| Baseline characteristics similar | Low risk | There were no differences between groups. |
| Baseline outcome measurements similar | Unclear risk | Baseline outcome measurements not reported |
| Protection against contamination | Low risk | Facebook participants received information about the private Facebook group and privacy settings and separate groups were used for the Facebook and Facebook Plus participants to limit cross contamination. |
O'Neil 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: Adults with Type 2 Diabetes (n=563) Age range: 18‐70 yeras Recruitment: not reported Eligibility: Participant‐reported diagnosis of type 2 diabetes mellitues, HbA1c between 7–11%, fasting blood glucose 18 to 70 years; diabetes management by a non‐study physician; stable regimen of all medications for at least 3 months; and willingness to attend weekly Weight Watchers meetings in the community and to use Weight Watchers online tools. Country: United States |
|
| Interventions |
Intervention: Multi‐component (n=279) Weight Watchers program including in‐person meetings and online tools, including social media, combined with telephone and email consultations.WW participants were provided free access to the ongoing, weekly, in‐person Weight Watchers meetings in their communities and the standard online tools. Included in this education was guidance regarding risk factors for and symptoms of hypoglycemia and recommendations for preventing and treating any such occurrences. Control: Non‐social media (n=284) Standard diabetes nutrition counseling and education. |
|
| Outcomes | HbA1c, weight, BMI, waist circumference, fasting blood glucose, cardiovascular risk markers (lipid measures, blood pressure, C‐Reactive Protein), diabetes medications. | |
| Equity | High income country, adults with type 2 diabetes | |
| Notes | Health behaviours: Not applicable. Body function: HbA1c was reported as the primary outcome. Psychological health: Not applicable. Well‐being: Not applicable. Mortality: Not applicable. Secondary outcomes: Not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Low risk | Weight Watchers meeting staff were unaware participants had diabetes or were participating in the study |
| Blinding of participants | High risk | Participants were blinded at baseline but authors state that "the necessarily unblinded nature of the trial may have contributed to differential patient expectations about the efficacy of their assigned intervention" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blood samples were obtained and shipped to a central laboratory for blinded analyses. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The primary study outcome, HbA1c, was investigated using a mixed model/hierarchical linear (HLM) model approach with HLM6 software [1]. HLM is a practical strategy for analyzing data from large‐scale multisite, multiple time‐point studies because the method does not assume equal numbers of observations or fixed time points of measurement, and given |
| Selective reporting (reporting bias) | High risk | One additional secondary outcome, change in various mental health assessments, is reported in trial registration but not included in published paper. |
| Baseline characteristics similar | Low risk | Characteristics were similar between groups. |
| Baseline outcome measurements similar | Low risk | There were no statistically significant group differences. |
| Protection against contamination | Low risk | 16 U.S. sites across 13 states and control participants weren't involved in the Weight Watchers program |
Owen 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: cancer survivors with distress (n = 296) Age range: (SD) 53.1 (10.9) Recruitment: recruited through the Loma Linda University tumour registry, as well as a number of online websites (cancer‐related forums, Facebook, and cancer‐related websites) Eligibility: participants were required to be at least 18 years of age, have consistent Internet access, be able to read and write in English, and have a minimum score of a 4 on the Distress Thermometer Country: USA |
|
| Interventions |
Intervention: multi component Low‐engaged users (n = 113), Moderate‐highly engaged users (n = 124) 12‐week distress management intervention (health‐space.net) multiple components. Primary components of healthspace.net were weekly guidance modules; a live weekly, facilitated chat; a discussion board; personal profiles; and webmail (i.e. confidential private messaging with other group members or facilitators via the study website). Weekly guidance modules contained 10 to 12 pages of educational materials and activities for participants, such as quizzes and exercises in which a participant was asked to describe ways in which they were currently engaging with each weekly guidance module. Control: No intervention (n = 59) Wait list control group. |
|
| Outcomes | Measures of quality of life, psychological well‐being, distress, psychological functioning, depression, and trauma‐related anxiety symptoms and social support. Secondary outcomes were fatigue and vigour. | |
| Equity | High‐income country | |
| Notes | Health behaviours: not applicable. Body function: not applicable. Psychological health: psychological functioning was selected as it was reported as a global score that incorporated other psychological outcomes reported (i.e. depression, anxiety). Well‐being: not applicable. No data reported for quality of life. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. No data reported for social support. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Not reported but trial registration states no masking |
| Blinding of participants | High risk | Not reported but trial registration states no masking |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported but trial registration states no masking |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Differences in attrition rates based on recruitment source with 75% of registry‐recruited participants completing the 3‐month follow‐up compared to only 64% of Internet‐recruited participants. |
| Selective reporting (reporting bias) | Low risk | Outcomes as reported in trial registration |
| Baseline characteristics similar | Low risk | No baseline differences between treatment and control groups. |
| Baseline outcome measurements similar | Low risk | Treatment and control groups did not differ at baseline with respect to any of the primary outcomes. |
| Protection against contamination | Unclear risk | Not reported |
Petrella 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: overweight and obese men 35–65 years old (n = 80) Age range: 35–65 years Recruitment: variety of methods (e.g. hockey team e‐mail blasts and social media accounts, study Web site (http://hockeyfansintraining.org/), posters, traditional media advertisements, word of mouth, direct contact at team arena) Eligibility: male 35–65 years old with a BMI of 28 kg/m2, meeting physical activity safety requirements Country: Canada |
|
| Interventions |
Intervention: multi‐component (n=40) Hockey FIT includes a 12 week active phase (weekly, coach‐led group meetings including provision of dietary information, practice of behavior change techniques, and safe exercise sessions plus incremental pedometer walking) and a 40‐wk minimally supported phase involving a smartphone app for sustaining physical activity, private online social network, and standardised e‐mails. Control: Non‐social media (n = 40) Men were instructed to continue with usual daily activities without any restrictions from the research team and with minimal intervention (i.e. only contacted to schedule 12‐week measurements). |
|
| Outcomes | Mean weight loss (kg), percentage weight change from baseline to 12 weeks, BMI, waist circumference, resting systolic and diastolic blood pressure, Self‐reported physical activity (average steps per day), sedentary time (typical week day in minutes), self‐reported eating (healthful eating score, fatty food score, as well as sugary food and fruit/ vegetable consumption) and alcohol consumption, self‐esteem score, positive and negative affect scores, health‐related quality of life (self‐rated health), and adverse events | |
| Equity | High‐income country, Male | |
| Notes | Health behaviours: diet quality and physical activity (steps per day) were selected as both were reported as intervention aims.
Well‐being: self‐rated health was the only outcome reported for this category. Body function: BMI was selected for this category as weight was not measured directly at both baseline and endline. BMI was considered most patient‐important compared to other outcomes reported for this category (eg. waist circumference). Psychological health: not applicable. Mortality: not applicable. Adverse effects: all reported adverse effects were selected as per our criteria. Secondary outcomes: self‐esteem was the only outcome of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated using SAS software version 9.4 |
| Allocation concealment (selection bias) | Low risk | concealed using sequentially numbered and sealed opaque envelopes |
| Blinding of personnel | High risk | It was not possible to blind participants or coaches |
| Blinding of participants | High risk | It was not possible to blind participants or coaches |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | objective measurement was used for our planned primary outcome (weight) and a blinded assessor conducted weight measurements in a separate, private area, to reduce the likelihood that group allocation would be revealed. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 13 men who did return for the 12‐week measurement session, We analysed the data using likelihood‐based methods, which are well known to provide unbiased results under the more general assumption of missing at random (i.e. the probability of missing may depend not only on the covariates but also on the observed outcomes). This assumption is tenable because we did not find any differences between these men and the 67 who attended the 12‐week measurement sessions on characteristics such as age, weight, steps per day, healthful eating, and self‐rated health. We did not adopt the method of last observation carried forward because it makes a very restrictive assumption that the outcome will be stable from the point of dropout to trial completion. One may still suspect that the data are missing not at random (i.e. the probability that a man did not return for measurement depends on his unobserved true weight). |
| Selective reporting (reporting bias) | Low risk | No evidence outcomes selectively reported |
| Baseline characteristics similar | Unclear risk | Significance not determined. At baseline, groups were balanced on most demographic and health history characteristics, as well as study outcomes |
| Baseline outcome measurements similar | Unclear risk | Significance not determined. At baseline, groups were balanced on most demographic and health history characteristics, as well as study outcomes |
| Protection against contamination | Low risk | Hockey FIT social network, a secure Web‐based network tailored to each site and including only group members and coaches. |
Ramo 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: smokers (n = 501) Age range: 18 and 25 years, Recruitment: primarily recruited from Facebook advertising campaign Eligibility: Smoke ≥100 cigarettes in their lifetime and currently smoke at least 1 cigarette per day on 4 or more days of the week, have had at least one heavy episode of drinking in the last month, read English, use Facebook at least 3 times a week. Country: USA |
|
| Interventions |
Intervention: multi‐component (n = 251) Participants in the Tobacco Status Project intervention are allocated to private Facebook groups according to readiness to quit smoking (i.e. ready to quit smoking or not ready to quit smoking). The Facebook groups include smoking cessation posts, tailored to readiness, delivered daily for 90 days. The posts include images, videos, and text to reflect the experience of young adults and all pose a question to elicit participant response. There were weekly live sessions delivered by a study counsellor who provides content for discussions, answers questions and provides supplemental support. Referrals to more intensive treatment can be provided by the study counsellors. Comparator: non‐social media (n = 249) Participants had access to the Tobacco Status Project website. |
|
| Outcomes | Biochemically verified 7‐day point prevalence abstinence over 12 months, biochemically verified abstinence at treatment end (3 months), reported 7‐day abstinence from cigarettes (including all reports of abstinence not verified biochemically), reduction of cigarette consumption by 50% or more (yes/no) between baseline and each follow‐up, presence of at least one 24‐hour tobacco quit attempt in the assessment time period (yes/no), proportion of participants in preparation, action or maintenance stages of change | |
| Equity | High‐income country | |
| Notes | Health behaviours: smoking abstinence was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment sequence generated by the study biostatistician |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Random sequence generation developed by study biostatistician, randomisation table held by study author, and the research assistants obtained the group assignment once the baseline assessment was completed, |
| Blinding of participants | High risk | Not reported but trial registration states no masking. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported but trial registration states no masking. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reasons for dropouts were not reported. Dropout rates were highest among those in the pre‐contemplation stage compared to those in contemplation or preparation. |
| Selective reporting (reporting bias) | High risk | Trial registration includes additional outcomes, such as health risk behaviours. |
| Baseline characteristics similar | Low risk | Groups were similar. |
| Baseline outcome measurements similar | Low risk | Groups were similar. |
| Protection against contamination | Unclear risk | Not reported |
Ramo 2018b.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: young adults who smoke cigarettes (N = 500). Age range: 18–25 years of age. Recruitment: participants were primarily recruited through a Facebook advertising campaign. Eligibility: English‐literate young adults, aged 18–25 years, who reported smoking ≥ 100 cigarettes in their life‐times; and at the time of recruitment reported smoking at least one cigarette per day on 3 or more days of the week on average, regular Facebook use (≥ 4 days per week) and access to a digital camera (e.g. on a phone or computer) to send a picture as part of the biochemical validation procedure. Country: USA |
|
| Interventions |
Intervention: Social media only (n = 251) Tobacco Status Project (TSP): 12‐month smoking cessation program using Facebook and weekly live group counselling. Daily Facebook posts containing evidence‐based smoking cessation strategies tailored to participants' readiness to quit smoking were posted for 90 days. Participants who were in the preparation groups received additional intervention components (e.g. additional CBT sessions). Control: active social media comparator (n = 241) Referral to smokefree.gov website. Features include a website tailored to readiness to quit smoking, a texting program, Smartphone application, on‐line live chat and a Facebook page. |
|
| Outcomes | Biochemically verified 7‐day point prevalence abstinence from tobacco, biochemically verified abstinence at treatment end (3 months), reported 7‐day abstinence from cigarettes, reduction of cigarette consumption by 50% or more, presence of at least one 24‐hour tobacco quit attempt in the assessment time period, proportion of participants in preparation, action or maintenance stages of change at all time point, and treatment acceptability/engagement. | |
| Equity | High‐income country. Young adults who smoke cigarettes. | |
| Notes | Health behaviours: biochemically verified 7‐day point prevalence abstinence from tobacco was reported as primary outcome. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote:"A stratified random assignment program was developed and participants are assigned from within stratified blocks immediately after completing the baseline assessment. Participants are stratified on stage of change (pre‐contemplation, contemplation, preparation) and smoking pattern (daily versus non‐daily), variables known to be related to outcomes and addressed by the intervention" |
| Allocation concealment (selection bias) | Unclear risk | Quote:"The randomization table was held by D.E.R. and the research assistants obtained the group assignment once the baseline assessment was completed." |
| Blinding of personnel | Unclear risk | Clinicaltrials.gov: None (0pen‐label) |
| Blinding of participants | High risk | Clinicaltrials.gov: None (open‐label): therefore knowledge of the assigned intervention may affect smoking behaviour |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Objective measure used for tobacco cessation, outcome measurement is not likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 70% completion at 12 months, no difference in follow up between groups, those who did not report abstinence were assumed to be smokers |
| Selective reporting (reporting bias) | High risk | Primary outcome in protocol was biochemically‐verified 7‐day point prevalence abstinence at 3, 6 months, as well but reasons for only including 12 months are justified in the paper ‐ recommended by the Society for Research on Nicotine and Tobacco Workgroup on abstinence measures). However, abstinence goal reported in protocol) not reported in results, additional outcomes in trial registration (prevalence rates of health‐risk behaviours other than smoking including recent alcohol and illicit drug use, poor sleep quality, sedentary behaviour, poor diet, depression, and high‐risk sexual behavior) were not reported in results. |
| Baseline characteristics similar | Unclear risk | Groups seem similar but not compared statistically |
| Baseline outcome measurements similar | Unclear risk | Groups seem similar but not compared statistically |
| Protection against contamination | Low risk | ‘Secret’ (i.e. entirely private) Facebook groups. The Dr. Is In sessions delivered in Facebook events and events are scheduled in each group separately. |
Ren 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: haemodialysis patients (N = 120). Age range: ≥18 years of age, overall mean (SD) age in years was 48.86 (4.75). Recruitment: patients were recruited for study participation at a tertiary hospital in southern China. Eligibility: 18 years or older, had more than 3 months of treatment duration, had undergone dialysis at least twice a week, had the ability to communicate in both oral and written formats without assistance and were willing to use the WeChat software. Country: China |
|
| Interventions |
Intervention: multi‐component intervention (n = 60) 3‐month WeChat health education programme in addition to routine care. Health education texts were added in the WeChat group daily. Patients were also encouraged to participate in regular seminars. Control: no intervention (n = 60) Waitlist control with routine care during the first 3 months. |
|
| Outcomes | Self‐management (combined, partnership, problem‐solving skills, self‐care, emotion management), haemodialysis patient knowledge, and chronic disease self‐efficacy. | |
| Equity | Upper middle‐income country. Patients undergoing haemodialysis. | |
| Notes | Health behaviours: self‐managment combined was selected over other self‐management outcomes because it provided a total score, per our criteria. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: 5 participants died during the course of the study (2 in intervention and 3 in control) (reasons for death not specified). Adverse effects: Nnt applicable. Secondary outcomes: haemodialysis patient knowledge and chronic disease self‐efficacy were the only outcomes reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"All eligible patients were labelled from 001‐120, according to the hospitalization number from lowest to highest. Then, three digits ranging from 001‐120 were produced by the random number table without duplication" |
| Allocation concealment (selection bias) | Unclear risk | Chief nurse randomly assigned the patients into one of two groups according to a random number table with a ratio of 1:1. All eligible patients were labelled from 001‐120, according to the hospitalisation number from lowest to highest. Then, three digits ranging from 001‐120 were produced by the random number table without duplication. The patients whose numbers corresponded to the first 60 valid digits were assigned to group 1 and the rest were assigned to group 2. |
| Blinding of personnel | High risk | Likely not blinded given that the personnel would remind participants to participate in the intervention and also provide routine care. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate, differences between control and intervention groups ‐ especially in the control group 39% of which many 'refused to participate (24%). Authors report: Quote:"The participants who withdrew from the study may have been more likely to be older with more serious conditions and had heavy economic burdens from the disease due to the inability to work." |
| Selective reporting (reporting bias) | Low risk | Biochemical Indexes not reported as a secondary outcome as reported in trial registration. All outcomes described in methods are reported in results |
| Baseline characteristics similar | High risk | 78% controls compared to 22% of intervention group were not working and mean ages of control was 56 compared to 44 in intervention group. |
| Baseline outcome measurements similar | Unclear risk | Not reported |
| Protection against contamination | Unclear risk | Both groups encouraged to participate in regular seminars held at the centre. Possible that participants discussed components of their intervention with others. |
Richardson 2010.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: adults with type 2 diabetes or coronary artery disease or are overweight (n = 324) Age range: 24 to 82 years Recruitment: a list was obtained of all patients who received treatment from a University of Michigan Health System provider within the previous 6 months with at least 1 of the following: body mass index (BMI) ≥ 25, type 2 diabetes, or coronary artery disease. Individuals diagnosed with quadriplegia or paraplegia or as having been pregnant within the previous year were excluded. word‐of‐mouth were referred to the study website. Eligibility: sedentary, ambulatory adults who used email regularly and had at least 1 of the following: overweight (BMI ≥ 25), Type 2 diabetes, or coronary artery disease Country: USA |
|
| Interventions |
Intervention: social media only (n = 254) Participants in the “online community” arm had access to online community features embedded in their intervention webpage. Control: non‐social media (n = 70) Control participants allocated to the ”no online community” arm could not read or post messages to other control‐arm participants. |
|
| Outcomes | Participant attrition, average daily step counts over 16 weeks, online community use, social support and motivation for walking. | |
| Equity | High‐income country. Adults with Type 2 diabetes or coronary artery disease or overweight | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: Not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Automated randomisation algorithm |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Research staff contributed to online community to stimulate involvement |
| Blinding of participants | High risk | The informed consent form described the two study arms. Quote: "This study will include about 300 participants, 240 in the group that can post messages to each other online, and 60 in the group that cannot." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants and personnel knew of assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline values were carried forward for those who did not complete the program. The intervention arm had statistically significantly higher completion rates than the control arm.The time to last pedometer upload was shorter in the control group indicating earlier drop out than the intervention group. |
| Selective reporting (reporting bias) | High risk | Additional outcomes reported in trial registration but not in paper. Additional outcomes presented in the results that were not reported in the methods. |
| Baseline characteristics similar | Low risk | No significant difference between arms |
| Baseline outcome measurements similar | High risk | Baseline step counts were significantly higher in the online community arm than the no online community arm. This difference required control for baseline step counts in all analyses. |
| Protection against contamination | Low risk | Participants in both arms were given a user name and password that allowed them to access a personalised intervention webpage. |
Rote 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: female freshman at a large, urban university in the Midwest.(n = 63) Age range: 18.6 ± 0.7 years Recruitment: announcements made in large university classes and via individual e‐mails gained through a university list‐serve. Eligibility: a) currently living in on‐campus dormitories; b) a Facebook user; and c) insufficiently active, which was defined as obtaining less than 7500 steps/day Country: USA | |
| Interventions |
Intervention: social media only (n = 32) Facebook Social Support Intervention plus the standard intervention.The individuals randomised to the Facebook Social Support Group received feedback on their baseline physical activity level (i.e. average steps/day), a pedometer, 8 paper logs to record steps taken per day, and a weekly personalized step goal of increasing steps/day by 10% of the previous week’s average steps/day; recommendations were not to exceed 15,000 steps/day. Each week of the intervention, participants received a personal Facebook message from the intervention leader requesting a report of their steps/day for the previous week. Based on their average steps/day, participants received an additional Facebook message with their new step goal and feedback. Control: non‐social media (n = 31) Standard Walking Intervention (no social support) including a pedometer, 8 paper logs to track steps/day, and a weekly personalised goal of increasing steps/day by 10% of the previous week’s average steps/day. |
|
| Outcomes | Physical activity (steps per day), physical activity stage of change, social support, decisional balance, and self‐efficacy with regard to physical activity. | |
| Equity | High‐income country. Female freshmen | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: weight was the only outcome of interest reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: social support and self‐efficacy were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised using 'Urn' randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | The lead study author was the intervention leader for all groups, added weekly posts to each Facebook page, and sent messages directly to intervention participants. There was also face‐to‐face contact at baseline and post‐intervention assessments. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants were required to track their own steps and report these back to the intervention leader. The authors report: quote:"tracking and reporting of steps may have been subject to social desirability bias." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Steps per day analysed for all those assigned to the groups, the rate of attrition did not differ significantly between the groups. |
| Selective reporting (reporting bias) | High risk | Measures of height, weight, and waist circumference were assessed at follow‐up but were not completely reported in results. Quote:"There were no significant changes in anthropometric variables in response to the intervention for women in the Standard Walking Intervention. Women in the Facebook Social Support Group significantly decreased waist circumference t(2,24) = 3.25, P = .003) by 1.1 cm at the completion of the intervention compared with baseline." |
| Baseline characteristics similar | Unclear risk | Baseline characteristics not provided by group. |
| Baseline outcome measurements similar | Unclear risk | Not reported. |
| Protection against contamination | Unclear risk | Private Facebook group but all students at the same university in which friends may have enrolled together |
Rouf 2020.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: young adults (N = 211). Age range: 18‐25 years of age. Recruitment: social media (posts to friends and paid advertising on Facebook), posting on University website (volunteer for research study), flyers (on campus notice boards), volunteers on a research database (previous volunteers who took part in nutrition research and agreed for contact in the future), and active face‐to‐face recruitment. Eligibility: young adults (males and females) aged 18 to 25 years who owned a smartphone and a Facebook account. Country: Australia |
|
| Interventions |
Intervention: multi‐component intervention (n = 141) 6‐week Facebook intervention (Facebook) (n = 65) and Facebook intervention plus text messages (Facebook plus text) (n = 76) focused calcium education. Text messages (every alternate day) and Facebook posts (every alternate day to the text) were sent to participants to remind them to set goals and track progress. Participants were encouraged to use smartphone apps to track progress. Control: non‐social media control (n = 70) Emailed an e‐leaflet containing information on calcium intake. |
|
| Outcomes | Calcium intake (cups of milk and other calcium‐rich foods), knowledge of calcium recommendations and serving sizes, self‐efficacy, motivation, habit formation, engagement with the platform, feedback regarding the acceptability of the program, intervention experience and uptake of content as well as frequency and reason for engagement. | |
| Equity | High‐income country. Young adults. | |
| Notes | Health behaviours: number of cups of milk were reported for calcium intake as it was reported as the primary outcome and considered the most patient‐important. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy and motivation were the only outcomes of interest reported for this category. Knowledge was assessed using a researcher‐designed questionnaire and no validated questionnaire could be found. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote:"A randomized sequence generation was used to allocate the participants. The randomization was performed by 2 independent researchers who were not study investigators." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | Unclear risk | Not reported but blinding unlikely as posts were made every alternate day by the researcher. |
| Blinding of participants | Unclear risk | Not specified in manuscript. In the CONSORT Checklist. Quote: "Participants were not aware which group they were in as the Facebook groups were kept separate." However, it is unclear whether participants knew they were in one of the intervention groups or control. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Effect size among missing outcomes enough to induce clinically relevant bias in observed effect size ‐ quote:"The analysis on completers‐only data demonstrated a significant increase in milk intake in the Facebook plus text messages group compared with the control group (OR 4.99, 95% CI 1.63‐15.28). Imputed data‐set non‐significant. an intention‐to‐treat analysis with multiple imputations for missing values was used. The GEE indicated that females had lower adjusted odds ratio (OR) than males of have missing data, adjusted for all other sociodemographic variables. No other sociodemographic variables were associated with missing outcome values. All participants were from the same arm (Facebook plus text) and opted out by sending a text—an option not available to other participants who could only opt out passively." |
| Selective reporting (reporting bias) | Unclear risk | The primary outcome is stated as change in calcium intake with a focus on milk intake but protocol only mentions calcium |
| Baseline characteristics similar | Unclear risk | Differences in characteristics not assessed. There appear to be some differences, however unclear if significant (occupation, SES, income, purchaser of groceries) |
| Baseline outcome measurements similar | Unclear risk | Not assessed |
| Protection against contamination | Unclear risk | Facebook and Facebook plus text groups were invited to join a closed Facebook group. The 2 Facebook groups were kept separate to avoid potential contamination between groups. Possible that text messages could have been forwarded to other participants (i.e. in Facebook only or control) |
Rovniak 2016.
| Study characteristics | ||
| Methods | cRCT | |
| Participants | Participants: physically inactive adults (n = 308) Age range: 34‐65 years Recruitment: to recruit participants, a list of households in each of the study sites with at least one person within the study’s age range was generated from a commercial marketing database (InfoUSA). Eligibility: age 35–64 years; physically inactive, i.e. < 150 minutes/week of self‐reported moderate‐to‐vigorous physical activity (MVPA) for exercise; able to speak English; able to engage in moderate intensity physical activity; and Internet access Country: USA | |
| Interventions |
Intervention: social media only. Activity group (n = 108), Social networks group (n = 104) Activity group received weekly emailed tip plus an evidence‐based online fitness walking intervention (not extracted for this review) Social Networks group received the activity group intervention plus access to an online networking site for walking as well as prompting social networking for walking/activity across diverse settings. Control: non‐social media (n = 96) Received weekly emailed tips but no other contact between program staff and participants. |
|
| Outcomes | Accelerometer‐measured MVPA, aerobic fitness, body mass index (BMI), waist circumference, and blood pressure. | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity (MVPA) was considered the most patient‐important outcome reported for this category. Body function: BMi was considered the most patient‐important outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated permuted block randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Quote: All assessments were single‐blinded (participants), except for aerobic fitness, which was double‐blinded (participants, staff)." |
| Blinding of participants | Low risk | Participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessments were single‐blinded (participants) including, BMI, blood pressure, accelerometer readings, except for aerobic fitness, which was double‐blinded (participants, staff), assessed using treadmill test. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High retention and reasons for missing data provided (missing accelerometer data). |
| Selective reporting (reporting bias) | High risk | Some outcomes reported in protocol not presented. |
| Baseline characteristics similar | Low risk | Participants in the three intervention groups did not differ significantly at baseline on all measured variables, except for race/ethnicity |
| Baseline outcome measurements similar | Low risk | Participants in the three intervention groups did not differ significantly at baseline on all measured variables. |
| Protection against contamination | High risk | Quote: "As treatment contamination was 8.1 % at post‐program, we conducted sensitivity analyses to examine the intervention effect on primary and secondary outcomes among the subgroup of participants not reporting treatment contamination." |
Schaller 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: rehab inpatients (n = 412) Age range: 18 to 65 years Recruitment: participants were recruited from an inpatient medical rehabilitation centre Eligibility: aged 18 to 65 years and starting an inpatient medical rehabilitation treatment due to low back pain. Country: Germany |
|
| Interventions |
Intervention: multi‐component (n = 71) (Movement Coaching) included three different components: face‐to‐face contact (small group intervention, three times during inpatient rehabilitation), tailored telephone aftercare (8 weeks and 12 weeks after rehabilitation) and an Internet‐based aftercare (web 2.0 platform; available up to six months after rehabilitation). Control: non‐social media (n = 73) Two general presentations on health‐enhancing physical activity (30 minutes each) during inpatient rehabilitation which could be downloaded from a homepage during aftercare. |
|
| Outcomes | Total physical activity (MET‐minutes/week), the subscales leisure time (MET‐minutes/week), workplace (MET‐minutes/week) and transportation physical activity (MET‐minutes/week) | |
| Equity | High‐income country. Rehab inpatients | |
| Notes | Health behaviours: total physical activity was considered the most patient‐important outcome for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator. |
| Allocation concealment (selection bias) | Low risk | An independent administrative assistant performed and controlled the randomisation |
| Blinding of personnel | High risk | Personnel not blinded ‐ the therapist conducted both interventions. |
| Blinding of participants | Low risk | Participants were blinded ‐ they were aware there were 2 physical activity interventions but were unaware of the differences between the 2. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants self‐reported but the therapist conducted both interventions. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Very high attrition rate with reasons provided. Both intention‐to‐treat and per‐protocol analyses performed. Younger age and lower leisure time activity were associated with not replying to the follow‐up surveys. |
| Selective reporting (reporting bias) | High risk | Additional outcomes reported in protocol (e.g. pain, healthcare utilisation, complications, barriers) |
| Baseline characteristics similar | Unclear risk | Characteristics similar but only reported by group for completers |
| Baseline outcome measurements similar | High risk | Intervention group much more physically active at baseline, only reported at baseline for completers |
| Protection against contamination | Unclear risk | Not reported |
Schneider 2015.
| Study characteristics | ||
| Methods | cRCT | |
| Participants | Participants: sedentary dog owners (n = 102) Age range: age mean (SD): 49.20 (13.72) intervention and 47.49 (12.26) control Recruitment: participants were recruited from January to May 2012 via flyers sent to registered dog owners in Worcester and Lowell, flyers posted in veterinary clinics, pet stores and other community locations, Craigslist advertisements and advertisements in local newspapers. Students and employees of the University of Massachusetts were recruited through ads posted on the intranet, in emailed newsletters and on bulletin boards within the institution.Interested individuals called to learn about the study and complete an initial eligibility screening. Interested individuals provided their home address so that the research assistant could determine if they resided in an included neighbourhood Eligibility: owning a healthy dog that was considered a pet, ≥ 21 years old and home Internet access Country: USA | |
| Interventions |
Intervention: multi‐component (n = 45) The 'Meetup' intervention was delivered over 6 months and consisted of newsletters, dog walks, community events and an activity monitor. The intervention was delivered via a Meetup group, which is a freely available online social network. Meetup includes a message board where members can post comments and questions. Control: non‐social media (n = 57) 6‐monthly emails with encouragement to begin walking and a link from the AHA (American Heart Association )website for starting a physical activity program |
|
| Outcomes | Steps, social support for walking, sense of community, perceived dog‐walking outcomes, barriers to dog walking and feasibility of the intervention (intervention receipt, participant satisfaction, adverse events, contamination, sustainability) | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity (steps) was considered the most patient‐important outcome for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: all reported adverse effects were selected as per our criteria. Secondary outcomes: social support was the only outcome of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator.. |
| Allocation concealment (selection bias) | Unclear risk | States that the project director allocated neighbourhoods but not mention of methods of concealment. |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data similar between groups and intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol but outcomes from methods are reported in results |
| Baseline characteristics similar | High risk | Participants in the intervention group reported greater neighbourhood aesthetics and less crime than participants in the control group |
| Baseline outcome measurements similar | High risk | At baseline, participants in the intervention group walked significantly more compared to participants in the control group. |
| Protection against contamination | Low risk | None of the control participants reported that they knew someone who was a member of the intervention group, participated in a neighbourhood walk or viewed any newsletters. |
Stoddard 2008.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: all participants were adult federal employees or contractors to the federal government who responded to an email and indicated a willingness to quit smoking in 30 days (n = 1375) Age range: mean (SD) 43.6 (10.3) years Recruitment: approximately 120,000 invitations to review the smokefree.gov website were sent out in 2 phases. federal employees received an email invitation asking them to participate. The second series of emails was sent to a different group of federal employees and contractors. Eligibility: 1) federal employee or contractor, 2) were a minimum of 18 years old, 3) and had a willingness to quit smoking, 4) those over 18 years of age who were ready to quit in the next 30 days or who had begun an initiation attempt within 5 days before enrolment. Country: USA | |
| Interventions |
Intervention: Social media only (n = 684) BB condition (bulletin board) a forum where participants could respond to some seeded categories posted on the board or start their own message. Control: non‐social media (n = 691) The publicly available version and usual care. |
|
| Outcomes | Smoking abstinence for 7 consecutive days and 24 hours at 1, 3, and 6 months, satisfaction with the resources provided, use of other cessation aids during the study period, extent of perceived social support, motivation and number of minutes of website use, visits to the website after registration at 1, 3, and 6 months | |
| Equity | High‐income country | |
| Notes | Health behaviours: smoking abstinence was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: perceived social support was the only outcome of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer algorithm (.ie. random number generator) generated the sequence. |
| Allocation concealment (selection bias) | Unclear risk | All invitations were sent blind to the receiver’s smoking status; thus the majority was sent to nonsmokers. Concealment not reported. |
| Blinding of personnel | Low risk | States that the research team was blinded to the assignments. |
| Blinding of participants | Low risk | Participants knew they were being randomised to one of 2 versions of the website without knowing what potential differences were. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Approximately 40% dropouts but similar in both groups. Reasons for loss to follow‐up were not provided. ITT analysis which treated all those who did not complete a follow‐up survey as smokers. |
| Selective reporting (reporting bias) | High risk | only reports abstinence at 3 months but clinicaltrials.gov states endline is 6 months. Social support was not documented in clinical trial submission, but measured in study |
| Baseline characteristics similar | Unclear risk | Quote: "Initial analyses revealed no differences between treatment groups" but characteristics table not disaggregated by arm so unclear if similar |
| Baseline outcome measurements similar | Unclear risk | Quote: "Initial analyses revealed no differences between treatment groups" but tobacco dependency outcomes were not disaggregated by arm. |
| Protection against contamination | High risk | Quote: "we cannot rule out possible contamination between conditions." To reduce the risk, the authors looked for similar demographics, smoking histories, usernames, and times of entry. The only suspicious entries (same date, similar time, and similar demographics/smoking history) were removed this record from the dataset. |
Sun 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: college students (n = 196) Age range: 17 to 25 years Recruitment: recruited from three different colleges in Hong Kong. The research was promoted to the students through mass emails, student societies, posters around campus, and social media. Eligibility: undergraduate student and aged under 25 years Country: China |
|
| Interventions |
Intervention: social media only (n = 96) Peer‐led, safer sex Facebook group as the intervention. Control: non‐social media (n = 100) Sex education website link of the Hong Kong Family Planning Association. |
|
| Outcomes | Condom use, attitude, contraceptive use behavioral intention, changes in behavioural skill and behaviour frequency of condom use, online visiting frequency, online engagement and usage | |
| Equity | Upper middle‐income country. College students | |
| Notes | Health behaviours: condom use was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: attitude, behavioural intention, and perceived difficulty and ease of use of contraceptive were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The online survey software randomised the participants into one of the two groups |
| Allocation concealment (selection bias) | Unclear risk | The online survey software randomly assigned participants upon completion of the baseline survey. |
| Blinding of personnel | High risk | Secret Facebook group in which only those invited could join. Researchers recorded the only usage of each participant. |
| Blinding of participants | Unclear risk | Not reported but 2 participants from the intervention group quote: "decided to join the Facebook group" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Firstly, outcome variables rely on self‐reported measures. Although validated scales were adopted, there is still potential for bias. Social desirability bias is possible, as the baseline of the outcome variables was high, and some participants even achieved full marks at baseline assessment." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High retention rate (12% dropouts) but many more from the control group than the intervention group. |
| Selective reporting (reporting bias) | Unclear risk | No protocol. Outcomes in the methods section are reported in the results section |
| Baseline characteristics similar | Low risk | No significant difference between the intervention and control groups at baseline was found. |
| Baseline outcome measurements similar | Low risk | No significant difference between the intervention and control groups at baseline was found. |
| Protection against contamination | High risk | Quote: "There was a contamination issue between the control and intervention groups, with some of the students signing up together but then being randomized into different groups. Although the participants were asked to maintain confidentiality on the assignment of groups and the intervention content, 2 of the participants assigned to the control group joined the Facebook group and were removed from the study." |
Turner‐McGrievy 2011.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: overweight and obese men and women (n = 96) Age range: 18–60 years old Recruitment: television advertisements and email listservs in the Raleigh‐Durham, North Carolina metropolitan area Eligibility: overweight and obese men and women (BMI 25 kg/m2 to 45 kg/m2 18 to 60 years old) Country: USA | |
| Interventions |
Intervention: social media only (n = 47) Podcast plus enhanced mobile media intervention (Podcast+Mobile). Both groups received 2 podcasts per week for 3 months and 2 mini podcasts per week for months 3–6. In addition to the podcasts. The Podcast+Mobile group was also instructed to use a diet and physical activity monitoring application (app) on their mobile device and to interact with study counsellors and other participants on Twitter Control: non‐social media (n = 49) The Podcast group received a book with calorie and fat gram amounts of food to assist them in monitoring their dietary intake |
|
| Outcomes | Change in body weight, dietary intake, physical activity, self‐efficacy (Weight Efficacy Life‐Style Questionnaire [WEL]) and eating behaviours (Eating Behavior Inventory [EBI]) | |
| Equity | High‐income country. Overweight and obese men and women | |
| Notes | Health behaviours: eating behaviours was considered the most patient‐important outcome for this category. Intentional physical activity was not selected because it is a step towards behaviour change, rather than a behaviour change itself. Body function: weight was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy (weight‐loss), knowledge (weight‐loss) and social support were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random numbers generator |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Neither study participants nor investigators were blind to treatment assignment |
| Blinding of participants | High risk | Neither study participants nor investigators were blind to treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Neither study participants nor investigators were blind to treatment assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High response rate and intention‐to‐treat by using imputation (baseline observation carried forward) |
| Selective reporting (reporting bias) | Unclear risk | No protocol available but outcomes reported in methods are assessed in results. |
| Baseline characteristics similar | Low risk | There were no significant differences in baseline demographics between the two groups except that more intervention group participants reported previously downloading a health‐related podcast or installing a healthy diet‐related app to their mobile device |
| Baseline outcome measurements similar | High risk | No significant differences between groups. |
| Protection against contamination | Low risk | Participants had access to a group‐specific podcast site |
Valle 2013.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: young adults with cancer (n = 86) Age range: Fitnet 30.8 (5.7); control 32.7 (4.2) years Recruitment: interested organisations posted recruitment advertisements through various mass distribution channels, such as Facebook, Twitter, listservs, flyers, and e‐mail Eligibility: young adults between ages 21 and 39 diagnosed with cancer (excluding non‐melanoma skin cancer) at age 18 or older; ≥1 year beyond date of diagnosis with no evidence of progressive disease or second primary cancers; completed cancer treatment; English speaking and writing; no pre‐existing medical condition(s) or contraindications that preclude adherence to an unsupervised exercise program; access to the Internet and an active Facebook account Country: USA | |
| Interventions |
Intervention: social media only (n = 45) Received a pedometer to monitor steps to record walking steps and physical activity type, duration, and intensity, 12 weekly Facebook messages,weekly goal setting and charts providing feedback on performance relative to weekly exercise goal, previous weeks and overall intervention goal, Facebook group with moderated discussion prompts to encourage support, links, and weekly reminders. The Facebook group received an expanded lesson and more specific guidance on physical activity than the control. Intervention participants also had access to a separate website with goal setting‐tools and physical activity diary. Control: active social media comparator (n = 41) Received a pedometer to monitor steps to record walking steps and physical activity type, duration, and intensity, 12 weekly Facebook messages,weekly goal setting and charts providing feedback on performance relative to weekly exercise goal, previous weeks and overall intervention goal, Facebook group with unmoderated discussion. |
|
| Outcomes | Self‐reported moderate‐vigorous physical activity minutes per week at 12 weeks. body weight, BMI, and quality of life | |
| Equity | High‐income country. Young adult cancer patients | |
| Notes | Health behaviours: physical activity was the only outcome reported for this category. Body function: weight was considered the most patient‐important outcome for this category. Psychological health: not applicable. Well‐being: overall quality of life was considered the most patient‐important outcome reported for this category. Mortality:not applicable. Adverse effects: not applicable. Secondary outcomes: self‐efficacy (making time) was considered more patient‐important than self‐efficacy (sticking to it) for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers list |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Study administrator invited participants to the Facebook groups |
| Blinding of participants | High risk | Not reported but trial registration indicates no masking. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported but trial registration indicates no masking. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 70% to 80% retention, higher in the control group than the intervention. Noncompleters were less likely to be married and were closer to their diagnosis than completers. Reasons for loss to follow‐up provided. |
| Selective reporting (reporting bias) | Unclear risk | Trial registration reports only physical activity as primary outcome while the paper reports both physical activity and feasibility. |
| Baseline characteristics similar | Low risk | No differences between groups except that the intervention group reported more daily Facebook use |
| Baseline outcome measurements similar | Low risk | The groups were similar but the control group was a bit more physically active at baseline (significance not tested). |
| Protection against contamination | Low risk | Invitation to join secret Facebook groups |
Vandelanotte 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: adults (n = 1803) Age range: 18 and older Recruitment: adults 18 years of age or older spontaneously signing up for the freely available and Web‐based 10,000 Steps program, asked during the registration process whether they wanted to participate in a research study from November 2012 to June 2014. Eligibility: adults 18 years of age or older spontaneously signing up for the freely available and Web‐based 10,000 Steps program Country: Australia | |
| Interventions |
Intervention: Social media only (n = 868) Access to Walk 2.0 which is similar to Web 1.0 with additional features: messaging and group publishing tools implemented in a social networking setting. The self‐monitoring features also have additional functionality: status updates, internal emails, requesting ‘friends’, personalised profile pages which allow for opportunities for interactivity and communication between participants. Control: social media active comparator (n = 899) Walk 1.0 Website, Participants allocated to this condition will be able to log their daily activities, in terms of type and duration of activity and/ or number of steps as well as access the website library for information concerning PA and other health behaviours. sharing of stories, ask questions or make comments in the discussion forum. |
|
| Outcomes | Physical activity, weight and height, user engagement and retention, self‐reported quality of life, emotional well‐being, social functioning, bodily pain, general health perceptions, website usage: | |
| Equity | High‐income country | |
| Notes | Health behaviours: physical activity (total weekly minutes) was the only outcome reported for this category. Body function: BMI was considered the most patient‐important outcome reported for this category. Psychological health: not applicable. Well‐being: quality of life was the term used for the following outcome variables (i.e. no data exist for QoL alone): Physical functioning, Role limitations due to physical health problems, Role limitation due to personal or emotional problems, Energy/fatigue, Emotional well‐being, Social functioning, Bodily pain, General health perceptions, Body mass index (kg/m2). Emotional well‐being was selected for this category as it most likely described the term "well‐being". Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated algorithm. |
| Allocation concealment (selection bias) | Low risk | Quote: "All actions, from study invitation to completion, were fully automated with no interaction from the research team at any point." |
| Blinding of personnel | Low risk | No interaction between the research team and the participants. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Outcomes were self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 13% and 20% follow‐up at 3 months, even less at 12 months, reasons not provided. Authors report that those who were likely to complete the 3 month survey were control group participants, male, aged 45 years or older, and not obese, as well as those having a higher education, professional occupation, and higher income. |
| Selective reporting (reporting bias) | Low risk | Reports outcomes included in trial registration with the addition of quality of life. |
| Baseline characteristics similar | Low risk | There were no significant differences between groups. |
| Baseline outcome measurements similar | Low risk | There were no significant differences between groups. |
| Protection against contamination | Low risk | Unlikely that those in the control group could have accessed the Web 2.0 intervention. |
Vogel 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: young adults who self‐identify as a sex/gender minority (SGM) who smokes tobacco (N = 165). Age range: 18‐25 years of age. Recruitment: targeted Facebook advertising campaign with ads targeted toward SGM smokers using rainbow imagery and keywords such as “LGBT”. Eligibility: English literacy, age 18–25 years, self‐identification as sex/gender minority, using Facebook at least 4 days/week, and smoking at least 100 cigarettes in their lives and currently smoking at least 1 cigarette per day, 4+ days per week. Country: USA |
|
| Interventions |
Intervention: Social media only (n = 84) Culturally‐tailored Put it Out Project (POP) 90‐day intervention using secret Facebook group. Intervention included daily Facebook posts and weekly “The Doctor Is In” live group chat tailored to the characteristics of the target population. Control: active social media comparator (n = 81) Identical as intervention except did not contain culturally tailored content. |
|
| Outcomes | Biochemically verified abstinence from smoking cigarettes, self‐reported 7‐day abstinence, reduction in cigarettes per week by at least 50%, presence of 24‐hour quit attempt, stage of change for quitting, intervention acceptability and engagement. | |
| Equity | High‐income country. Sexual and Gender Minorities, young adults who smoke. | |
| Notes | Health behaviours: biochemically verified abstinence was reported as primary outcomes Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. Note: Please see Ramob for more information on The Put It Out Project (POP) Facebook Intervention. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The principal investigator (DR) held the randomisation table. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. The principal investigator (DR) held the randomisation table. |
| Blinding of personnel | High risk | The principal investigator (DR) held the randomisation table and reported group assignment to study staff after each participant completed the baseline assessment. Open‐label |
| Blinding of participants | High risk | None ‐ Open‐label |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Saliva cotinine test |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat ‐ no reported dropout |
| Selective reporting (reporting bias) | High risk | Trial registration includes slightly different secondary outcomes (e.g. stage of change for quitting versus readiness to quit and thoughts about quitting in trial registration). |
| Baseline characteristics similar | Low risk | No significant differences |
| Baseline outcome measurements similar | Low risk | Outcomes for control and intervention groups were similar at baseline. |
| Protection against contamination | Low risk | “Secret” Facebook groups (i.e., entirely private groups for which the existence is not visible to non‐members) |
Wan 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: veterans who are smokers with diagnosis of COPD, emphysema or chronic bronchitis (n = 114) Age range: mean age 68.6 ± 8.3 years Recruitment: participants were recruited from the general pulmonary clinics at VA Boston. Eligibility: a) adults 40 years old, b) Diagnosis of COPD, emphysema or chronic bronchitis, as defined by FEV1/FVC <0.70 or CT evidence of emphysema, c) Have at least a 10 pack‐year history of smoking, d) Able to walk a minimum of one block, e) Approval and medical clearance from health care provider, f) Competent to give informed consent, g) Have access to a computer with an Internet connection, a USB port, and any Windows operating system or be willing to come to the VA to use computers once a week, h) >90% accuracy by Omron to detect step counts as compared to manual step counts during baseline clinic testing Country: USA | |
| Interventions |
Intervention: multi‐component (n = 60) A pedometer and website which provided goal‐setting, feedback, disease‐specific education, and an online community forum Control: non‐social media (n = 54) Pedometer and written materials about exercise. Participants were not given a step‐count goal but were instructed to wear the pedometer daily while awake and to upload step counts at least monthly via the website. The website had no content except a display of the study week. |
|
| Outcomes | Daily step count, exercise adherence, health‐related quality of life, dyspnoea, depression, COPD knowledge, exercise self‐efficacy, social support, motivation and confidence to exercise daily, adverse events | |
| Equity | High‐income country. Smokers with diagnosis of COPD, emphysema or chronic bronchitis | |
| Notes | Health behaviours: daily step count was the only outcome reported for this category. Body function: not applicable ‐ no endline data reported for dyspnoea. Psychological health: depression was the only outcome reported for this category. Well‐being: health‐related quality of life was the only outcome reported for this category. Mortality: not applicable. Adverse effects: all reported adverse effects were selected as per our criteria. Secondary outcomes: COPD knowledge, self‐efficacy (exercise), social support, and motivation were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer algorithm |
| Allocation concealment (selection bias) | Low risk | Randomisation assignments were generated with random block sizes which were not disclosed to study staff. |
| Blinding of personnel | High risk | Assignments were communicated to study staff. |
| Blinding of participants | High risk | Participant blinding was not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The research staff conducting assessments at the study conclusion were blinded to group assignments and outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Very high retention, similar number lost in each group. Reasons not provided. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available but outcomes from methods were reported in results section. |
| Baseline characteristics similar | Low risk | No significant differences in age, BMI, pack‐years or other characteristics. |
| Baseline outcome measurements similar | Low risk | No significant differences between groups. |
| Protection against contamination | Unclear risk | Not reported. |
Wang 2015.
| Study characteristics | ||
| Methods | CBA | |
| Participants | Participants: Undergraduate students with equal gender distribution. (n = 62) Age range: 19‐25 years (mean age= 22.30 years, SD = 1.51) Recruitment: recruited from undergraduate students in a local university Eligibility: students between 19 to 25 years of age were recruited Country: Singapore | |
| Interventions |
Intervention: multi‐component Group B: (n = 17) Participants of this group participated in a 3 hour physical fitness class each week for eight weeks (not extracted). Group C: (n = 14) received the Group B intervention, plus the participants in this group were linked through Facebook. Regular posts were updated on the Facebook wall page including polls, articles related to physical fitness and health, discussion topics, sharing of photographs and videos Group D: (n = 24), participants participated voluntarily in a 1 hour physical exercise program each week. Participants were linked via Facebook Control: No intervention Group A (n = 7), did not receive any intervention |
|
| Outcomes | Physical activity level, perceived autonomy, perceived competence, relatedness, perceived enjoyment and vitality. | |
| Equity | High‐income country. College students | |
| Notes | Health behaviours: physical activity (total MET‐minutes/week) was the only outcome reported for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: perceived competence and perceived autonomy were the only outcomes of interest reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were assigned into four groups, no randomisation. |
| Allocation concealment (selection bias) | High risk | Non‐random assignment. |
| Blinding of personnel | Unclear risk | Not reported. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rates not provided. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Baseline characteristics similar | Unclear risk | Not reported |
| Baseline outcome measurements similar | Unclear risk | Not reported |
| Protection against contamination | Unclear risk | Not reported. Study does not report measures to prevent the control group from accessing the Facebook page. |
Washington 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: black men who have sex with men (BMSM; N = 42) Age range: 18‐30 years Recruitment: recruited in person at community‐based organisations serving Black males at high risk and online via social media (e.g. Facebook, Twitter, Black Gay Chat). Eligibility: Black/African American male, aged 18–30 years, had sex with a man in the past 3 months by self‐report, HIV status unknown and have not tested for HIV at least within the past six months, resident of Los Angeles County, California, had condomless receptive or insertive anal sex at least once in lifetime, English speaking, and a valid e‐mail address Country: USA | |
| Interventions |
Intervention: social media only (n = 22) The intervention group participants were asked to review five 60‐second intervention videos, weekly. Participants were asked to post comments on the group page in reaction or response to the video content about HIV prevention and HIV testing uptake messages Control: non‐social media (n = 20) Participants in the control group viewed standard HIV text information sent weekly. |
|
| Outcomes | Self‐reported HIV testing, sexual practices, HIV knowledge (including substance use as risk), drug using behaviour | |
| Equity | High‐income country. Black males at high risk for HIV, men who have sex with men | |
| Notes | Health behaviours: HIV testing was selected for this category as it was reported as the primary outcome. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: HIV knowledge was the only outcome reported for this category. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | The intervention was conducted online with monitoring by a systems analyst and the research team. |
| Blinding of participants | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was similar for both groups (n = 8 intervention, n = 6 control). Reasons for loss to follow‐up were not provided. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Baseline characteristics similar | Low risk | No significant differences between groups. |
| Baseline outcome measurements similar | Low risk | No significant differences between groups |
| Protection against contamination | Unclear risk | Participants had to 'like' the Facebook group to which they had been assigned but study does not mention how this was managed and whether it was possible for participants to like the group to which they were not assigned. |
Willcox 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: pregnant women who were overweight or obese prior to pregnancy (n = 91) Age range: mean age 32.5 (SD3.4) years Recruitment: eligible women were identified at their first hospital antenatal visit to a university‐affiliated maternity hospital in Melbourne, Australia. Eligibility: eligibility criteria included women with a singleton, live gestation between 100 and 176 weeks; self‐reported pre‐pregnancy BMI >25 kg/m2 ; able to speak, read and write English; and owning a mobile phone. Country: Australia | |
| Interventions |
Intervention: multi‐component (n = 45) The multi‐modality‐delivered intervention included tailored text messages, access to a responsive information website viewable on mobile devices, video messages, and chat room interaction via Facebook. Control: No intervention (n = 46) Usual maternity care ‐ mailed brief information brochures containing advice regarding diet and physical activity prior to the first hospital visit and were also encouraged to weigh at first visit. |
|
| Outcomes | Feasibility, gestational weight gain, diet and physical activity | |
| Equity | High‐income country. Women attending hospital antenatal visit | |
| Notes | Health behaviours: physical activity was considered the most patient‐important outcome for this category. Body function: weight was the only outcome reported for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Quote: "Numbered cards allocating women to either the intervention or control groups were placed in opaque, sequentially numbered envelopes." |
| Blinding of personnel | Unclear risk | Not reported |
| Blinding of participants | Unclear risk | Quote: "Given the nature of the intervention, participants could not be blinded to group assignment". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The participant group allocation was re‐coded by an independent researcher to ensure that the data analyst was blinded to allocation.The outcome assessors will be blinded to participant allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 91% retention rate. Participants who did not complete the study (n = 9) differed only by being recruited earlier in pregnancy than those who completed. 1 withdrawal due to dislike or intervention others due to pregnancy complications and miscarriage. |
| Selective reporting (reporting bias) | High risk | Some outcomes reported in protocol but not reported in results: Knowledge. attitude to gestational weight gain, self‐efficacy. |
| Baseline characteristics similar | Low risk | Baseline characteristics similar. |
| Baseline outcome measurements similar | Unclear risk | Differences between groups were not measured. |
| Protection against contamination | Unclear risk | The videos and website were intentionally coded so as not to be searchable on search engines, but they were not password protected and could have been accessed by those outside the intervention group. |
Willis 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Participants: 70 adults with obesity (body mass index [BMI] = 30.0 kg/m2 to 5.0 kg/m2 ) (n = 70) Age range: 21–70 years Recruitment: participants were recruited using university broadcast emails, flyers, the General Medicine Clinic at the University of Kansas Medical Center and the wait list for participation in the Center for Physical Activity and Weight Management's Weight Control Research Projects. Potential participants were asked to contact study staff via phone or email. Interested individuals were directed to complete an initial eligibility questionnaire through Research Electronic Data Capture (REDCap) version 6.4.4 hosted at The University of Kansas Medical Center. Participants provided self‐reported height and weight (BMI), medication use, previous attempts at weight loss, presence of chronic disease, current physical activity level, and special diet restrictions. Eligibility: participants excluded if they were unable to participate in moderate intensity PA (i.e. walking), were regularly exercising (> 90 minutes/week) or at serious medical risk Country: USA | |
| Interventions |
Intervention: multi‐component (n = 34) Online social network intervention and Phone conference call sessions Control: non‐social media (n = 36) Phone conference call sessions 60‐minute group phone conference meetings of 12–18 participants were conducted one evening per week (total 24 meetings) for 6 months. |
|
| Outcomes | Weight loss at 6 months, waist circumference, dietary intake, physical activity | |
| Equity | High‐income country. Adults with obesity | |
| Notes | Health behaviours: physical activity and dietary intake were selected as both were reported as primary aims of the study. Body function: weight loss was considered the most patient‐important outcome for this category. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of personnel | High risk | Inability to blind health educators is reported as a limitation. |
| Blinding of participants | High risk | Inability to blind participants is reported as a limitation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Overall blinding not reported ‐ some outcomes, e.g. daily step count are low risk because recorded by Fitbit, but weekly weight and diet were self‐reported by unblinded participants (high risk). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reasons for missing data were not reported. Proportion of missing data was similar and greater than 80% retention at 6 months. Baseline data not provided for all participants |
| Selective reporting (reporting bias) | High risk | Additional outcomes reported in the paper not described in methods (e.g. quality of life, exercise self‐efficacy, moderators and mediators of diet and physical activity, changes in social support) |
| Baseline characteristics similar | Low risk | There were no baseline differences between participants. |
| Baseline outcome measurements similar | Low risk | No significant group differences were observed for BMI and waist circumference. |
| Protection against contamination | Unclear risk | Not reported |
Yang 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants |
Participants: pregnant women experiencing symptoms of depression or anxiety (N = 123). Age range: over 18 years of age. Mean (SD) age in years was 31.31 (4.97) for the intervention group and 30.38 (3.91) for the control group. Recruitment:cConducted in the obstetrics clinic of the Women’s Hospital School of Medicine at Zhejiang University. Eligibility: women aged more than 18 years, 24 to 30 weeks’ gestation, low‐risk pregnancy at the start of the intervention, Internet access, fluent in Chinese and able to complete the questionnaires, and elevated depressive or anxious symptoms as determined by either a PHQ‐9 score of more than 4 or a GAD‐7 score of more than 4. Country: China |
|
| Interventions |
Intervention: multi‐component intervention (n = 52) The 8‐week mindfulness intervention program included 4 x 40‐minute mindfulness sessions over the course of 8 weeks. Mindfulness sessions recorded and uploaded on WeChat and women were encouraged to interact and share experiences. Nurses contacted all participants through Wechat video or telephone to address specific training problems and to understand their experience of mindfulness practice. Control: active social media comparator (n = 50) Routine care and were also enrolled in a Wechat group to interact with each other, but received no mindfulness training during the intervention period. |
|
| Outcomes | Adherence to the intervention, symptoms of depression, level of general anxiety, and level of mindfulness (combined, observing, describing, acting with awareness, non judgment, and non reactivity). | |
| Equity | Upper middle‐income country. Pregnant women, symptoms of depression and/or anxiety. | |
| Notes | Health behaviours: not applicable. Body function: not applicable. Psychological health: depression and anxiety were selected as both were reported as intervention aims and considered the most patient‐important outcomes for this category. Well‐being: not applicable. Mortality: not applicable. Adverse effects: none specifically reported, however 1 woman in the intervention group and 3 in the control group discontinued the intervention because of an increase in depressive symptoms. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization sequence was computer generated, and group assignment was done by staff not associated with the study using opaque, sealed envelopes" |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomization sequence was computer generated, and group assignment was done by staff not associated with the study using opaque, sealed envelopes" |
| Blinding of personnel | High risk | Quote: "The midwife and another nurse were responsible for Wechat group management, including correcting inappropriate information, encouraging homework practice, and tracking training adherence." |
| Blinding of participants | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Researchers blinded to the group allocation collected the outcome data and checked the questionnaires immediately after collection. If any problems were apparent, they guided participants to complete or revise the answers." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analyses were conducted based on an intention‐to‐treat approach. The multiple imputation method was used for missing data. Similar attrition across groups. However, missing outcome data likely to be related to outcome: 5 intervention participants dropped out of the study because of the burden of daily mindfulness practice ‐ one woman in the intervention group and 3 in the control group discontinued the intervention because of an increase in depressive symptoms. |
| Selective reporting (reporting bias) | Unclear risk | Protocol unavailable. All outcomes outlined in methods reported in results. |
| Baseline characteristics similar | Low risk | No significant differences in the demographic or maternal health variables were observed between these groups (Table 2). |
| Baseline outcome measurements similar | Low risk | No significant differences in the baseline PHQ‐9 or GAD‐7 scores were observed between the 2 groups. |
| Protection against contamination | Unclear risk | Methods for protection against contamination not described. Possible communication across participants or control group received mindfulness through other means (e.g., app). |
Young 2013.
| Study characteristics | ||
| Methods | cRCT | |
| Participants | Participants: men who have sex with men and living in the Los Angeles, California area (n = 105) Age range: mean 31.5 (SD 10.2) Recruitment: Internet and social networking sites through paid, targeted banner ads on social networking sites such as Facebook; recruitment posts on the personals and jobs sections on Craigslist in the greater Los Angeles area; and a Facebook fan page with study information taken from community fliers Eligibility: African American or Latino man, age 18 years or older, has a Facebook account, self‐reported living in the Los Angeles area, and had sex with a man in the past 12 months Country: USA | |
| Interventions |
Intervention: social media only (n = 52) HIV information delivered via Facebook with peer leaders who were instructed to communicate about HIV prevention and testing Control: non‐social media comparator (n = 53) General health information delivered via Facebook with peer leaders instructed to communicate about importance of exercising, healthy eating, and maintaining a low‐stress lifestyle |
|
| Outcomes | Request for a home‐based testing kit, returning the kit, and following up for test results; self‐reported reduction in number of sexual partners and observed and self‐reported communication using the social networking community; feasibility and acceptability of using social networking as a health research platform; social network metrics | |
| Equity | High‐income country. African American and Latino men who have sex with men | |
| Notes | Health behaviours: HIV testing was considered the most patient‐important outcome for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. Note: this study reports the same trial registration number (NCT01701206) as Young 2015. However, we have chosen to treat these as two separate studies, one conducted in the US and one conducted in Peru because the participants were not the same in the two studies. The papers that we refer to as Young 2013 do not report on the participants from the Peru location. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | Quote: "concealed allocation" but method not described.C |
| Blinding of personnel | Unclear risk | Peer leaders were informed about study goals but were asked to not disclose this information to participants |
| Blinding of participants | Low risk | Participants were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High retention rate, but reasons for attrition and differences between completers and non‐completers were not described. |
| Selective reporting (reporting bias) | High risk | Trial registration only lists requesting of HIV testing kit. Paper reports additional outcomes (e..g. reduction in number of sexual partners) |
| Baseline characteristics similar | High risk | The control group had more single participants than the intervention group and the intervention group had more persons who completed post secondary education than the control group. |
| Baseline outcome measurements similar | Low risk | Request for HIV tests not applicable at baseline. |
| Protection against contamination | Unclear risk | Peer leaders could have exposed intervention elements to control group. Quote: "Peer leaders were informed about study goals but were asked to not disclose this information to participants" |
Young 2015.
| Study characteristics | ||
| Methods | cRCT | |
| Participants | Participants: men who have sex with men (MSM) (n = 498) Age range: 18 and older Recruitment: online banner advertisements on three of the major Peruvian gay websites: gayperu.com, peruesgay.com and perugay.com, and from targeted advertisements (displaying advertisements only to participants who matched targeted criteria) on Facebook. Online advertisements notified participants that UCLA was conducting a study with Epicentro and participants should click on the ad to be screened Eligibility: 1) male, 2) sex with a man in the past 12 months, 3) 18 years of age or older, 4) living in the Greater Lima Metropolitan area, 5) HIV negative or serostatus unknown, and 6) had a Facebook account or willing to create one. Peer leaders: 1) 18 years of age or older, 2) had had sex with a man in the past 12 months, 3) had a Facebook account or willing to set one up, 4) reported by staff as being friendly and well‐respected among the MSM community, and 5) interested in educating others about health. Potential peer leaders visited the study website for an online eligibility screening Country: Peru | |
| Interventions |
Intervention: social media only (n = 252) Harnessing Online Peer Education (HOPE) social media intervention. Participants were assigned to secret and private Facebook groups and 2 peer leaders per group attempted to interact with participants about the importance of HIV prevention and testing via Facebook messages, chats and posts. Control:active social media comparator (n = 246) Standard offline HIV prevention available in Peru as well as participation in Facebook groups without peer leaders that provided study updates and HIV testing information |
|
| Outcomes | Requesting an HIV test by the end of follow‐up | |
| Equity | Upper middle‐income country. | |
| Notes | Health behaviours: HIV testing was considered the most patient‐important outcome for this category. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. Note: this study reports the same trial registration number (NCT01701206) as Young 2013. However, we have chosen to treat these as two separate studies, one conducted in the US and one conducted in Peru because the participants were not the same in the two studies. The study we refer to as Young 2015 does not report on the American participants who are included in Young 2013. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | Reports that allocation was concealed and that no participants or peer leaders were involved in randomisation but method of concealment not reported. |
| Blinding of personnel | Unclear risk | Quote: "Peer leaders who satisfied enrolment criteria were informed about the study design and study goals but were asked to not disclose this information to participants." |
| Blinding of participants | Low risk | Participants were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High retention (88% to 90%). Those lost to follow‐up did not complete the final survey but reasons not provided. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available but all outcomes from methods section are reported in results. |
| Baseline characteristics similar | Low risk | There were no significant differences found in baseline characteristics between groups. |
| Baseline outcome measurements similar | Low risk | The participants were not allowed to participate if already tested. |
| Protection against contamination | Unclear risk | Peer leaders were informed about the study design and study goals but were asked to not disclose this information to participants. Peer leaders but were allowed to interact with group participants who they had not been assigned. However, this would have just been among intervention groups as control did not have peer leaders. |
Zhang 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants | The SHAPE‐UP program was open to all graduate and professional students at the University who were 18 years or older (n = 790) Participants: Graduate and professional students at the University Age range: (mean age 25.2) Recruitment: participants were recruited through advertisements on the University's website, through the student email list, via advertisements from the graduate student association, and with paper flyers placed on billboards around campus Eligibility: eligibility for enrolment in the study was determined by a physical assessment conducted by the DRHS. Each participant completed a screening questionnaire (Canadian Society for Exercise Physiology (CSEP), 2002) designed to identify adults for whom physical activity might be inappropriate. The assessment lasted for 10 min and also measured participants' physical endurance, strength, and Body Mass Index (BMI). Logging in to the study website at least once after online registration Country: USA |
|
| Interventions |
Intervention: multi‐component Social comparison condition placed participants into 6‐person competitive social networks.(n = 198) Social support condition placed participants into 6‐person teams with peer support and a chatting feature.(n = 192) Combined condition with both supportive and competitive relationships placed participants into 6‐person teams, where participants could compare their team's performance to 5 other teams' performances.(n = 198) Control: non‐social media (n = 202) Participants were provided with no social motivations, and were rewarded at the end of the program based on their individual record of attendance at exercise classes. |
|
| Outcomes | Total number of exercise classes that participants attended throughout the 11‐week program, Change from baseline in participants' self‐reported physical activity level (outcome only reported for a subsample of participants in companion paper). | |
| Equity | High‐income country. University students | |
| Notes | Health behaviours: physical activity (number of exercise classes attended) was the only outcome reported for this category with complete data. Body function: not applicable. Psychological health: not applicable. Well‐being: not applicable. Mortality: not applicable. Adverse effects: not applicable. Secondary outcomes: not applicable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequences |
| Allocation concealment (selection bias) | Low risk | Upon logging into the website for the first time, participants were randomly assigned to one of four experimental conditions. |
| Blinding of personnel | Low risk | Class instructors were blind to experimental assignments. |
| Blinding of participants | Low risk | Participants were blind to experimental assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Attendance data for all classes recorded by class instructors. Participants reported physical activity levels. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | intention‐to‐treat principle. The attrition rates for participants receiving the treatment were statistically indistinguishable across all conditions, Between 4‐7% attrition. |
| Selective reporting (reporting bias) | Unclear risk | Some outcomes reported were not presented in results, e.g. change from baseline in participants' self‐reported physical activity level |
| Baseline characteristics similar | Low risk | There were no significant differences in participants' characteristics at baseline across conditions |
| Baseline outcome measurements similar | Unclear risk | Not applicable ‐ outcome of class attendance couldn't be measured at baseline. |
| Protection against contamination | Unclear risk | Not reported. |
ADHD: Attention deficit hyperactivity disorder; ART: antiretroviral therapy; BMI: body mass index; CBT: cognitive behavioural therapy; COPD: chronic obstructive pulmonary disease; cRCT: cluster randomised controlled trial; FOBT\; fecal occult blood test; HDL: high‐density lipoprotein; IQR: interquartile range; ITT: intention‐to‐treat; IUD: intrauterine device; LDL: low‐density lipoprotein; MPVA: moderate‐to‐vigorous physical activity; MUFA: monounsaturated fatty acids; OGTT: oral glucose tolerance test; PUFA: polyunsaturated fatty acids; QoL: quality of life; RCT: randomised controlled trial; SD: standard deviation; SE: standard error; T2D: Type 2 diabetes.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aiello 2015 | Intervention is not aimed at changing behaviour. |
| Al‐Eisa 2016 | Study design is not relevant (non‐randomised controlled trial) |
| Allman‐Farinelli 2016 | Intervention only included a blog as its social media feature |
| Bragadottir 2008 | Intervention is not aimed at changing behaviour but focuses on social support. |
| Bramlett Mayer 2012 | Study design is not relevant (non‐randomised controlled trial) |
| Brosseau 2015 | No real interaction between participants: quote: "participants were not actually connected to 132 other students". |
| Cadeiras 2014 | Social media used for social marketing campaign to increase organ donation, no interaction between participants via social media |
| Cao 2018 | Intervention is not aimed at changing behaviour. |
| Dam 2017 | Intervention is not aimed at changing behaviour but focuses on social support. |
| Epstein 2019 | Intervention is not aimed at changing behaviour. |
| Espie 2012 | Cognitive behavioural therapy and imagery relief therapy delivered by an animated personal therapist. No interaction between participants. |
| Hixson 2015 | No control group |
| Ho 2015 | No control group |
| Ho 2016 | Not an eligible study design |
| Kaur 2020 | Not interactive social media for all participants ‐ the intervention included a What's App component but not accessed by all, required participants to have access to a mobile phone or landline phone or Internet |
| Ko 2013 | Study design is not relevant (non‐randomised controlled trial) |
| Kofinas 2014 | Not interactive social media ‐ participants only had access to the Facebook page for 30 minutes. |
| Kondo 2019 | Intervention is not aimed at changing behaviour. |
| Kumar 2016 | Intervention is not aimed at changing behaviour. |
| Laws 2018 | Study design is not relevant (non‐randomised controlled trial) |
| Li 2019 | Study design is not eligible (only one cluster in control and intervention groups) |
| Lindsay 2009 | Social media platform is not well‐known and was developed by the authors for the purpose of the study; participants had to be provided computers and trained in using them. |
| Ling 2018 | Study design is not relevant (non‐randomised controlled trial) |
| Mingoia 2019 | Intervention is not aimed at changing behaviour |
| MotaPereira 2014 | Intervention is online cognitive behavioural therapy. |
| Muntaner‐Mas 2017 | Study design is not relevant (non‐randomised controlled trial) |
| Niela‐Viten 2016 | Intervention is not aimed at changing behaviour. |
| Po'e 2013 | No interactive social media. The protocol reports use of a blogging feature but the final report does not mention use of the blog or any other social media. |
| Pope 2018 | Both arms received content‐identical Facebook group but the intervention group also received a smart watch. |
| Rhodes 2016 | Communication is between the participant and the health educator via instant messaging or email and not amongst participants. |
| Rosser 2010 | No interaction between participants. Participants had virtual peers and simulated chats. |
| Smith 2012 | Intervention is not aimed at changing behaviour. |
| Tiermensma 2015 | Intervention is not aimed at changing behaviour. |
| van der Eijk 2012 | Beta testing of online community applications in clinical practice |
| Verduyn 2015 | Intervention is not aimed at changing behaviour. |
| West 2016 | Study design is not relevant (non‐randomised controlled trial) |
| Young 2018 | Intervention is not aimed at changing behaviour. |
| Yu 2014 | No control group |
Characteristics of studies awaiting classification [ordered by study ID]
Abdelkarim 2016.
| Methods | Non‐randomised controlled trial |
| Participants |
Participants: Egyptian patients with borderline personality disorder (BPD) (N=38).
Age range: not reported Recruitment: not reported Country: Egypt |
| Interventions |
Intervention: dialectical behaviour therapy skills training with parallel Facebook group to increase compliance Control: dialectical behaviour therapy skills training |
| Outcomes | Health behaviours: patient compliance |
| Notes | Conference abstract only |
Alghafri 2018.
| Methods | cRCT |
| Participants |
Participants: adults with Type 2 diabetes (N = 232).
Age range: 44.2 (8.1) years Recruitment: patients attending health centres for diabetes care for at least 6 months Country: Oman |
| Interventions |
Intervention: MOVEdiabetes with face‐to‐face consultations, pedometers, What's App group Control: usual care with diet and weight management but no focus on physical activity |
| Outcomes | Health behaviours: physical activity (MET.min/week) Body function: weight, BMI, blood pressure, HbA1c, lipid profile Secondary outcomes: self‐efficacy, social support |
| Notes | Very little detail on interactivity. Authors contacted for clarification. |
Bakirci‐Taylor 2019.
| Methods | RCT |
| Participants |
Participants: parents with children (N = 30).
Age range: 18‐45 years Recruitment: Parents with children recruited at story time at libraries Country: USA |
| Interventions |
Intervention: Jump2Health had 3 components: a mobile website, Facebook page, and short message service Control: text messages only |
| Outcomes | Health behaviours: fruit and vegetable consumption Body function: BMI, carotenoid levels |
| Notes | Auhors contacted ‐ need data for fruit and vegetable consumption using validated questionnaire, and BMI |
Bickel 2016.
| Methods | RCT |
| Participants |
Participants: individuals in recovery from substance addiction (N = 256).
Age range: not reported Recruitment: International Quit & Recovery Registry Country: USA |
| Interventions |
Intervention: Lattice social network (highly clustered networks with more adjacent social network friends) Control: Small‐world social network (redundant connections and fewer adjacent social network friends) |
| Outcomes | Secondary outcomes: engagement in social network activities |
| Notes | Abstract only, no start date reported |
Birnbrauer 2018.
| Methods | CBA |
| Participants |
Participants: individuals with T1 or T2 diabetes (N = not reported).
Age range: not reported Recruitment: not reported Country: USA |
| Interventions |
Intervention: Facebook Control: Facebook |
| Outcomes | Health behaviours: diabetes self‐management, medication adherence Secondary outcomes: Facebook participation and frequency of Facebook use |
| Notes | Abstract only, very little detail provided on intervention and control group components, no start date reported |
Chang 2018.
| Methods | 3 arm RCT |
| Participants |
Participants: undergraduate students (N = 140).
Age range: mean age was 22 years ± 0.5 Recruitment: not reported Country: China |
| Interventions |
Intervention: 8‐week intervention includes activity tracker, online game, and Facebook Control: activity tracker only and activity tracker plus online game |
| Outcomes | Health behaviours: moderate to vigorous physical activity Body function: body fat percentage, muscle mass |
| Notes | Abstract only, no start date reported |
Cheng 2018.
| Methods | Non‐randomised controlled trial |
| Participants |
Participants: prediabetic patients (N = not reported).
Age range: not reported Recruitment: third grade A hospital in Zhengzhou Country: China |
| Interventions |
Intervention: WeChat cluster based on network based on diet and blood glucose control Control: conventional health education |
| Outcomes | Health behaviours: Average daily intake rate Body function: body mass index (BMI), fasting blood glucose, glycosylated haemoglobin (HbA1c) |
| Notes | June 2016 start date |
Dulli 2020.
| Methods | RCT |
| Participants |
Participants: youth living with HIV in Nigeria who had been on antiretroviral therapy for less than 12 months (N = 349).
Age range: 15 to 24 years ‐ mean was 21 years of age (SD 2.3). Recruitment: patients who attended clinic visits at 14 health facilities Country: Nigeria |
| Interventions |
Intervention: SMART (Social Media to promote Adherence and Retention in Treatment) Connections delivered through secret Facebook groups led by an adult facilitator with lived HIV experience. Included social activities, interactive polls, facilitated discussions, word‐of‐the‐week and key messages. Intervention participants continued to receive standard services. Control: standard care ‐ routine clinical care for HIV treatment |
| Outcomes | Health behaviours: retention in HIV treatment, adherence to antiretroviral treatment Psychological health: depression Secondary outcomes: HIV knowledge and treatment literacy, social support, social isolation, HIV‐related stigma |
| Notes | Could not be reported in our review because no estimates of precision were provided for retention in HIV treatment. September 2018 ‐ November 2019. |
Ehde 2017.
| Methods | RCT |
| Participants |
Participants: adults aging with multiple sclerosis (MS) (N = 31).
Age range: older than 45 years of age Recruitment: not reported Country: USA |
| Interventions |
Intervention: 6‐week Everyday Matters intervention which teaches strategies for increasing happiness and resilience in people with MS. Everyday Matters was delivered via group teleconference and included an online private social media group. Control: waitlist group |
| Outcomes | Health behaviours: sleep Body function: pain, fatigue Psychological health: resilience, mood |
| Notes | Abstract only |
Elloumi 2018.
| Methods | RCT |
| Participants |
Participants: healthy individuals working or studying at the University of Twente (N = 103). Age: 25 and 55 years of age. Recruitment: University of Twente Facebook groups and University of Twente mailing lists (MIRA2 and CTIT3 institutes). Country: the Netherlands |
| Interventions |
Intervention: the TogetherActive system, a virtual community that provides social support to people during their daily physical activities. Intervention components include a physical activity sensor, a gateway (which can be a smartphone), and a portal where participants were asked to collaborate, communicate and compete with each other. Control: a basic version of the TogetherActive V2 system with a Fitbit. Control participants had no access to the virtual community functionalities. |
| Outcomes | Health behaviours: physical activity (steps). Secondary outcomes: participants’ usage of the platform functionalities. |
| Notes | Could not be reported in our review because no estimates of precision were provided, no start date provided. |
Gao 2015.
| Methods | RCT |
| Participants |
Participants: new hospital patients diagnosed with Type 2 diabetes (N = 46).
Age range: not reported Recruitment: hospital patients Country: China |
| Interventions |
Intervention: Cloud platform group ‐ used a Fumanduo metre T1 type and managed their diabetes through the glucose cloud platform combined with webchat interaction for diabetes management. Control: used an Abbott metre and participated in a remote interactive micro‐channel platform to improve their lifestyle and adjust their insulin dosage. |
| Outcomes | Body function: fasting plasma glucose, 2‐hour plasma glucose, HbA1c level (%) |
| Notes | Abstract only, no start date reported |
Hafiz 2018.
| Methods | 3‐arm RCT |
| Participants |
Participants: full‐time university students living away from home (N = 60).
Age range: mean age was 24.4 years (SD 3·7) Recruitment: not reported Country: Ireland |
| Interventions |
InterventionS: F&V: received fruits and vegetables for 4‐weeks. F&V + education: received fruits and vegetables plus nutrition education on Facebook. Control: no intervention |
| Outcomes | Health behaviours: fruit and vegetable consumption, compliance to fruit and vegetable consumption Secondary outcomes: Facebook engagement |
| Notes | Abstract only, 70 % of participants engaged with Facebook regularly. No start day reported. |
Li 2018.
| Methods | RCT |
| Participants |
Participants: patients with thyroid cancer treated with 131 I (N = 103)
Age range: not reported Recruitment: Qinghai Hospital of Traditional Chinese Medicine Country: China |
| Interventions |
Intervention: WeChat group was established for thyroid cancer patients to conduct daily communication and mutual assistance. Control: standard treatment and routine care |
| Outcomes | Psychological health: depression Well‐being: quality of life |
| Notes | Not in English |
Mahdi 2019.
| Methods | 4‐arm RCT |
| Participants |
Participants: patients with Type 2 diabetes (N = 80)
Age range: not reported Recruitment: diabetes treatment centres in Isfahan Country: Iran |
| Interventions |
Interventions: mobile social network‐based mindfulness performed in 45‐minute sessions daily for 8 weeks, eight 120‐minutes session mindfulness group intervention or acceptance and commitment group therapy intervention. Control: not described. |
| Outcomes | Psychological health: depression, anxiety, and stress |
| Notes | Not in English, Start date of Spring 2018 |
Maher 2018.
| Methods | RCT |
| Participants |
Participants: adults who were non‐runners (N = 89).
Age range: mean age of 35.2 years (SD 10.9) Recruitment: online advertising and mainstream media news articles Country: Australia |
| Interventions |
Intervention: 8‐week running program on private Facebook group which included 3× weekly interval training sessions and daily interactive posts Control: running program in print copy |
| Outcomes | Health behaviours: moderate to vigorous physical activity Body function: cardiorespiratory fitness Secondary outcomes: social support, exercise attitudes, self‐efficacy, compliance with the running program and engagement with the Facebook |
| Notes | Abstract only, no start date reported |
Petrovski 2016.
| Methods | RCT |
| Participants |
Participants: Type 1 diabetes patients on insulin pump with Hba1c of 7.9+/‐1.4% (N = 72).
Age range: mean age was 17.8 years +/‐4.2 years Recruitment: not reported Country: not reported |
| Interventions |
Intervention: Doctors' group: Viber in a group led by one doctor and one educator. Control: Patient group: Viber offered in a group led by two Type 1 diabetes patients. |
| Outcomes | Body function: Hba1c Secondary outcomes: communications per week |
| Notes | Abstract only, patients could interact with other patients about their diabetes management in Viber, no start date reported |
Trude 2018.
| Methods | RCT |
| Participants |
Participants: low‐income urban youths and their caregivers (N = 385).
Age range: average age of caregivers was 40 years and 12 years for youth. Recruitment: 28 low‐income zones in Baltimore Country: USA |
| Interventions |
Intervention: B'more Healthy Communities for Kids (BHCK), an obesity prevention program, which included corner store/carryout restaurants, social media/text messaging, and youth‐led nutrition education in recreation centres. Control: recreation centres nor small food stores received the nutrition education sessions and communication materials and caregiver– child dyads were not enrolled in the BHCK text‐messaging program. |
| Outcomes | Secondary outcomes: exposure scores (viewing of BHCK materials, participation in activities) |
| Notes | Not enough detail on interactivity. Authors contacted for clarification. July 2013 start date. |
Wu 2019.
| Methods | Non‐randomised controlled trial |
| Participants |
Participants: pregnant women who had at least 9 years of education and were in less than 12 weeks of gestation (N = 138).
Age range: over 20 years old. Mean age of intervention group was 32.79 (3.87) years and control group was 32.78 (3.82) years. Recruitment: medical centre in Taiwan Country: China |
| Interventions |
Intervention: the expectant mother club with a discussion forum and a library area for pregnancy‐related information Control: ordinary prenatal care |
| Outcomes | Body function: physical symptoms Psychological health: physical symptoms, depression Secondary outcomes: social support |
| Notes | Could not be reported in our review because only differences in outcome measurements of time and treatment interaction were reported. May 2012 start date. |
Yang 2016.
| Methods | 3‐arm RCT |
| Participants |
Participants: patients with COPD who are nicotine dependent (N = 146).
Age range: not reported Recruitment: COPD patients undergoing quitting smoking intervention were randomly selected between October 2014 and September 2015 by prospective design. Country: China |
| Interventions |
Intervention: drug (varenicline tartrate) with WeChat group Controls: drug group (varenicline tartrate) and non‐drug group |
| Outcomes | Health behaviours: 7‐day point withdrawal rates and sustained withdrawal rates |
| Notes | Not in English, very little detail provided on intervention and control group components as well as study methods, no start date reported |
BMI: body mass index; MET: metabolic equivalent; RCT: randomised controlled trial; SD: standard deviation.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12619000335190.
| Study name | Mi.spot (supportive, preventative, online and targeted): a moderated online intervention for young adults who have a parent with a mental illness and/or substance use concern: a study protocol for a randomised controlled trial |
| Methods | RCT |
| Participants | Young adults, who have a parent with a mental illness and/or substance use problem (age: 18–25). |
| Interventions | Intervention: mi.spot, an online 6‐week intervention with psychoeducational modules, a forum to interact with peers, one‐to‐one counselling chats, online diary, and weekly activities. Control: information about local and national services. |
| Outcomes | Main: well‐being levels (MHC‐SF), depression, anxiety and stress (DASS‐21). Secondary: levels of coping (COPE inventory), Levels of help seeking (General Help Seeking Questionnaire), levels of social connectedness (Social Connectedness Scale), self‐efficacy (10 item General Self‐Efficacy Scale), levels of psychoeducation (Mental Health Literacy Scale), attribution of responsibility measure. |
| Starting date | April 29, 2019 |
| Contact information | Andrea Reupert
Phone: +61 03 9902 4587 Email: Andrea.reupert@monash.edu |
| Notes |
ACTRN12619001785190.
| Study name | Talking about Aboriginal gambling: examining the effectiveness of Facebook groups to reduce gambling harm within Aboriginal communities in New South Wales, Australia |
| Methods | Stepped‐wedge RCT |
| Participants | Participants over 18 years of age who live in 10 communities in New South Wales, Austrailia. Included communities have a high representation of Aboriginal and/or Torres Strait Islander people. |
| Interventions | Intervention: community‐developed, co‐designed online health promotion platform (Facebook). The online content will consist of discussion prompts, information about gambling, and support services available (community‐generated videos, informational posts and forum discussions). Control: those who have not yet received the intervention. |
| Outcomes | Main: classification of being at risk of problem/moderate/low risk gambling (PGSI). Secondary: gambling frequency (by activity), Gambling expenditure (by activity), harm experienced by someone else’s gambling, reactions' to content and posts as shown through Facebook Analytics, how people have engaged and responded to the material. |
| Starting date | Anticipated date of first participant enrolment: February 3, 2020 |
| Contact information | Dr Marisa Paterson Phone: +61 436 811 151 Email: Marisa.paterson@anu.edu.au |
| Notes |
Arnold 2019.
| Study name | The Stepped Care intervention to suppress viral load in youth living with HIV: protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | Youth living with HIV (12‐24 years old) |
| Interventions | Intervention: Enhanced Stepped Care which has three levels of intervention ‐ Level 1, Enhanced Standard Care plus automated messaging and monitoring intervention (AMMI); Level 2, online peer support via social media (muut.com) plus AMMI plus Enhanced Standard Care; and Level 3, coaching plus online peer support via social media (muut.com) and AMMI plus Enhanced. Standard Care. Should participants HIV fail to be virally suppressed, they will be provided with the next level of intervention in addition to the other levels of care to which they were previously assigned. Control: Enhanced Standard Care, which includes standard clinical care plus an AMMI. |
| Outcomes | Main: HIV viral load. Secondary: Retention in care, Antiretroviral Therapy Adherence, Alcohol Use (Alcohol Use Disorders Identification Test), Substance Use (marijuana, synthetic marijuana, cocaine or crack, heroin, ecstasy, methamphetamines, prescription stimulants or amphetamines, gamma hydroxybutyric acid, ketamine, poppers, inhalants, hallucinogens, prescription painkillers not used as prescribed, and other prescription medications not used as prescribed), Sexual Behavior (the number of sexual partners (in total and partners who are HIV positive), the number of insertive and receptive anal sex acts, the frequency of condom use with sexual partners at each sexual encounter), Mental Health (12‐item Short Form Health Survey, Patient Health Questionnaire for adolescents, Generalized Anxiety Disorder 7‐item). Other: SMS survey outcomes, the number of responses to the AMMI surveys (Level 1), the number of peer support posts and logins (Level 2), and the number of coaching sessions (Level 3). |
| Starting date | June 2017 |
| Contact information | Elizabeth Mayfield Arnold, PhD Phone: 1 214 648 8140 Email: liz.arnold@utsouthwestern.edu |
| Notes |
Aschbrenner 2019.
| Study name | Randomized trial of a lifestyle intervention for young adults with serious mental illness in community mental health centers |
| Methods | RCT |
| Participants | Adults aged 18‐35 years with serious mental illness (SMI) and BMI ≥ 25 receiving services at community mental health centres. |
| Interventions | Intervention: PeerFIT ‐ group lifestyle intervention supported by mobile health technology (Fitbits, text messaging support) and social media (Facebook). Control: BEAT ‐ one‐on‐one basic education in fitness and nutrition supported by a wearable Activity Tracking device (Fitbit Zip) plus text message reminders and encouragement for self‐monitoring weight loss. |
| Outcomes | Main: cardiovascular risk reduction indicated by either clinically significant weight loss (5% or greater) or increased fitness (>50 m on the 6‐Minute Walk Test). Secondary: change in BMI, lipids, and haemoglobin A1c, perceived self‐efficacy for exercise and peer support. |
| Starting date | July 3, 2017 |
| Contact information | Kelly Aschbrenner, PhD Contact information not available |
| Notes |
Beleigoli 2018.
| Study name | Online platform for healthy weight loss in adults with overweight and obesity ‐ the “POEmaS” project: a randomized controlled trial |
| Methods | RCT |
| Participants | University students or employees aged 18‐60 years of age who classified as overweight or obese with the intention to lose weight. |
| Interventions | Intervention: Online platform ‐ access to the study website program (social network, gamification and short‐text sessions) with diet, physical activity behavior change recommendations for 24 weeks. Intervention: Online dietitian coaching ‐ same components as online platform group, but also includes online sessions with a dietitian specialist for 12 weeks. Control: four videos and an e‐book on diet, physical activity and behaviour change recommendations for 24 weeks and will receive access to the platform subsequently. |
| Outcomes | Main: weight and BMI change Secondary: changes in dietary habits, food‐related behaviours (TFEQ‐R21), physical activity habits and sedentary behaviours (IPAQ), health perception (12‐item Short‐Form Health Survey), online activity and users´ satisfaction. |
| Starting date | September 24, 2017 |
| Contact information | Alline Maria Beleigoli Email: abeleigoli@gmail.com |
| Notes |
Block 2014.
| Study name | Development and clinical trial of an eHealth program for pre‐diabetics |
| Methods | RCT |
| Participants | Individuals with Type 2 diabetes. |
| Interventions | Intervention: one‐year multimedia email‐web‐smartphone program (Alive‐Pre‐Diabetes). Control: delayed control. |
| Outcomes | Main: change in glucose and haemoglobin A1c. |
| Starting date | Not reported |
| Contact information | Gladys Block Contact information not available |
| Notes | Very little information provided on participant eligibility, intervention components, and outcomes. Abstract only. |
Bonar 2020.
| Study name | Social media interventions for risky drinking among adolescents and emerging adults:protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | Adolescents and emerging adults who are 16‐24 years of age with past 3 month at‐risk drinking/alcohol misuse. |
| Interventions | Intervention: SMI + I ‐ interaction between participants and coaches in secret Facebook group over 8‐weeks delivered with financial incentives for participation. Intervention: SMI ‐ interaction between participants and coaches in secret Facebook group over 8‐weeks delivered without financial incentives for participation. Control: Attention‐Control E‐News ‐ Facebook group on unrelated topics. |
| Outcomes | Main: changes in alcohol consumption (quantity, frequency, binge drinking using Timeline Follow‐Back), alcohol consequences (BYAACQ). Secondary: other drug use (30‐day daily cannabis use, tobacco, prescription medications using Tobacco, Alcohol, Prescription medications, and other Substance tool). Other: intervention engagement (counts of posts, status, comments to others’ posts, likes/shares), intervention acceptability and perceived helpfulness. |
| Starting date | January 5, 2017 |
| Contact information | Erin E Bonar, PhD Phone: 1 7347647936 Email: erinbona@med.umich.edu |
| Notes |
Boudreau 2016.
| Study name | Effectiveness of computer tailoring versus peer support web‐based Interventions in promoting physical activity among insufficiently active Canadian adults With Type 2 diabetes: protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | Quebec men and women with self‐reported Type 2 diabetes who do not meet the Canadian Diabetes Association guidelines on moderate‐intensity aerobic physical activity, do not have medical indications of limiting physical activity, can understand French, have access to the Internet and are between the ages of 18 to 65 years of age. |
| Interventions | Intervention: the Web‐based computer‐tailored intervention will include eight personalised computer motivational sessions, which will be tailored to participants physical activity cognitions and current physical activity level. All computer‐tailored motivational sessions will be interactive‐based. Intervention: the Web‐based peer support intervention will allow participants to visit the intervention website or to interact with other participants in a semi‐guided private Facebook group. The Facebook group will be moderated by a clinical nurse. Participants will be given the opportunity to discuss web articles with other participants on the Facebook group page. Control: participants will not receive any intervention. |
| Outcomes | Main: physical activity levels (GLTEQ). Secondary: physical activity related cognitions including attitude, social influence, self‐efficacy/perceived behavioral control, and intention, and type of motivation (BREQ‐2). |
| Starting date | Project was funded in 2011 and enrolment was completed in September 2014. |
| Contact information | François Boudreau, PhD Phone: 1 819 376 5011 ext 3465 Email: francois.boudreau@uqtr.ca |
| Notes |
Campbell 2016.
| Study name | The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) Program: a cluster‐randomized controlled trial of an early intervention to prevent childhood obesity |
| Methods | cRCT |
| Participants | First‐time parents who are part of a Maternal and Child Health Centres first‐time parent group and are literate in English. |
| Interventions | Intervention: the Melbourne InFANT Extend Program is an early obesity program that will be delivered to first time parent groups until a child is 18‐months of age. The intervention will be composed of six quarterly two‐hour sessions to provide anticipatory guidance, share information and develop skills. All intervention content will be available on an online web page. A first‐time parent Facebook group, facilitated by a nutrition expert, will also be created to promote parent engagement and reinforce session content. Newletters that contain web links to new content will be delivered to participants via email three times a month. Control: usual care from Maternal and Child Health nurses and general health newsletters every three months. |
| Outcomes | Main: Children’s anthropometry (i.e. height, weight, waist circumference, recumbent length, BMI). Secondary: child dietary intake (FFQ), child physical activity (ActiGraph accelerometer), child sedentary behaviour, parent diet (FFQ), parent physical activity (Active Australia Survey), parent television time, parent nutrition knowledge (Nutrition Knowledge Questionnaire), parent feeding style (Comprehensive Feeding Practices Questionnaire), parent modelling of healthy eating, home food availability, parental confidence, parent physical activity knowledge, parent interactions with their child around physical activity, audit checklist on the physical activity and sedentary home environment. Other: use of services related to infant’s or parent's own weight, diet/eating behaviours or physical activity, number of occasions of service use and any financial cost. |
| Starting date | Registered April 13, 2011. |
| Contact information | Karen Campbell, PhD Phone: +61 3 5227 8414 Email: karen.campbell@deakin.edu.au |
| Notes |
Cheung 2020.
| Study name | Effectiveness of WhatsApp online group discussion for smoking relapse prevention: protocol for a pragmatic randomized controlled trial. |
| Methods | RCT |
| Participants | Daily tobacco users over 18 years of age who are receiving smoking cessation service in 10 smoking cessation clinics in Hong Kong. |
| Interventions | Intervention: moderated Whatsapp social group and three text messages or videos a week for 8‐weeks Control: three mobile phone text messages each week for 8 weeks. No video clips and pictures will be sent and participants in this group will not interact with others. |
| Outcomes | Main: prevalence of carbon monoxide and saliva cotinine validated tobacco abstinence at 12‐month follow‐up. Secondary: prevalence of biochemically validated abstinence at the 6‐month follow‐up, self‐reported tobacco abstinence of 7 days, continuous abstinence, and the relapse rate. Other: time to relapse, number of posts made by participants in WhatsApp groups, change in frequency and intensity of smoking urges, change in the Minnesota Nicotine Withdrawal Scale (MNWS), and the change in EuroQoL 5‐dimension 5‐level (EQ‐5D‐5 L) health utility scores. |
| Starting date | October 4, 2018 |
| Contact information | Dr. Yee Tak Derek Cheung, PhD Phone: +852 39176652 Email: derekcheung@hku.hk |
| Notes |
Fereira 2017.
| Study name | Baseline characteristics from prep Chicago: A randomized controlled diffusion‐based network intervention for HIV prevention among young Black men who have sex with men |
| Methods | RCT |
| Participants | Young Black men who have sex with men. |
| Interventions | Intervention: small group peer change agent workshop and then booster phone calls. Control: group sex‐diary session. |
| Outcomes | Main: pre‐exposure prophylaxis uptake. |
| Starting date | Not reported |
| Contact information | Matthew Ferreira, DVM, MPH Contact information not available |
| Notes | Abstract only. |
Glover 2017.
| Study name | An innovative team‐based weightloss competition to reduce cardiovascular and diabetes risk among Māori and Pacific people: rationale and method for the study and its evaluation |
| Methods | RCT |
| Participants | Māori or Pacific people who 16 years of age or older, obese and either at risk of or already diagnosed with Type 2 diabetes or cardiovascular disease. |
| Interventions | Intervention: group use of an Internet‐based competition offering financial incentives, education and support. Control: No intervention. |
| Outcomes | Main: % of individual weight loss. Secondary: HbA1c and total cholesterol. |
| Starting date | June 2016 |
| Contact information | Marewa Glover Phone: +64 9 213 6059 Email: M.Glover@massey.ac.nz |
| Notes |
Herring 2019.
| Study name | Targeting pregnancy‐related weight gain to reduce disparities in obesity: baseline results from the Healthy Babies trial |
| Methods | RCT |
| Participants | Obstetric patients over 18 years of age who were in the first or early second trimesters of pregnancy. |
| Interventions | Intervention: technology‐based behavioural intervention program with behaviour change goals, daily text messages with feedback, web‐based weight gain graphs, health coaching, and a Facebook support group, in addition to regular care. Control: standard obstetric care. |
| Outcomes | Main: Revalence of excessive gestational weight gain. Secondary: Cardiometabolic risk factors, mode of delivery, infant birth weight and 6‐month postpartum weight retention. |
| Starting date | October 2014 |
| Contact information | Sharon J. Herring, MD, MPH Email: herris01@temple.edu |
| Notes |
ISRCTN14859844.
| Study name | Testing the short‐term effectiveness of online weight loss programmes |
| Methods | RCT |
| Participants | Over 18 years of age and a BMI of ≥30 kg/m2. |
| Interventions | Intervention: 3 separate online weight loss interventions (NHS weight loss programme which includes a 12‐week weight loss plan with meals apps and links; Slimming world online which includes 8‐weeks of featured recipes, food diaries, regular weight recording, group sessions, live chat support body magic challenges or; Rosemary online which includes 8‐weeks of weight monitoring tools, food and exercise diary, exercise ideas/ videos, blogs, videos and articles, access to online coaching, recipes, online community support, daily motivational reviews) focusing on different aspects of weight loss. Control: no intervention. |
| Outcomes | Main: Change in self‐reported weight from baseline to 8 weeks. Secondary: Engagement with the program, demographic data. |
| Starting date | January 1, 2019 |
| Contact information | Dr Michaela Noreik Email: michaela.noreik@phc.ox.ac.uk |
| Notes |
Jacobson 2020.
| Study name | Electronic Monitoring Of Mom's Schedule (eMOMS TM): protocol for a feasibility randomized controlled trial to improve postpartum weight, blood sugars, and breastfeeding among high BMI women. |
| Methods | RCT |
| Participants | Healthy pregnant woman who are 18 years of age or older and less than 16 weeks gestation at recruitment. |
| Interventions | Intervention: eMOMS1 ‐ Diabetes Prevention Program (one‐on‐one counselling sessions via telephone, use of private Facebook groups for delivery of educational content, email reminders, and answering of questions related to the topic of interest for that week) and educational breastfeeding videos and support. Intervention: eMOMS2 ‐ Diabetes Prevention Program only. Control: eMOMS3 ‐ usual care (no videos or Diabetes Prevention Program). |
| Outcomes | Main: maternal postpartum weight loss. Secondary: maternal haemoglobin A1C, maternal arterial blood pressure, breastfeeding status, maternal level of breastfeeding knowledge, maternal breastfeeding self‐efficacy, maternal diet quality, maternal physical activity levels, maternal depression. |
| Starting date | September 18, 2019 |
| Contact information | Lisette T. Jacobson, PhD Phone: 316‐293‐3484 Email: ljacobson@kumc.edu |
| Notes |
Jansson 2019.
| Study name | Integrating smartphone technology, social support and the outdoor built environment to promote community‐based aerobic and resistance‐based physical activity: rationale and study protocol for the ‘ecofit’ randomized controlled trial |
| Methods | RCT |
| Participants | Adults who do not meet current Australian aerobic and/or resistance‐based physical activity guidelines. |
| Interventions | Intervention: Ecofit app (includes standardised workouts, workout locations, workout categories, self‐monitoring function, exercise library and resources), social support (groups of up to four and the ecofit Facebook group), ‘Fixed’ and or ‘Trail based’ outdoor fitness equipment (installed in the park locations and detailed in the ecofit app), one introductory group session (90 minutes) with a qualified exercise specialist, an app manual and a ‘physical activity starter pack’. Control: wait‐list ‐ access to the ‘Fixed’ and ‘Trail‐based’ outdoor fitness equipment only. |
| Outcomes | Main: upper (degree push‐up test)and lower body muscular fitness (sit‐to‐stand test). Secondary: physical activity (accelerometry and self‐report using modified version of the validated Godin Leisure‐Time questionnaire), body composition ( dual‐energy x‐ray absorptiometry), aerobic fitness (YMCA step test), BMI, self‐reported resistance‐based physical activity (modified version of the validated Godin Leisure‐Time questionnaire), active travel (Global Physical Activity Questionnaire (GPAQ)), self‐report happiness, mental health outcomes (depression, anxiety and stress using DASS‐21). Other: physical activity self‐efficacy, resistance training self‐efficacy, implementation intention for resistance training, park use, perceived environment, social support, process measures (participants’ park use, participants’ goals and progress, participant satisfaction and feedback), objective audit of parks. |
| Starting date | August 28, 2019 |
| Contact information | Ronald Plotnikoff Phone: +61 2 49854465 Email: ron.plotnikoff@newcastle.edu.au |
| Notes |
Jaser 2019.
| Study name | Communication and coping intervention for mothers of adolescents with type 1 diabetes: rationale and trial design |
| Methods | RCT |
| Participants | Mother‐adolescent dyads ‐ adolescent must be 11‐17 years of age and have Type 1 diabetes for at least one year and mother must live with the adolescent at least 50% of the time and report either mild to moderate symptoms of depression or moderate diabetes distress. |
| Interventions | Intervention: communication and coping ‐ phone calls with a trained interventionist (content related to coping with diabetes‐related stress and positive parenting strategies) and a Facebook group to practice the skills from the phone sessions and receive reinforcement from their peers. Control: phone calls with a trained interventionist (content related to diabetes management) and a Facebook group with educational daily posts to reinforce concepts covered in the phone sessions. |
| Outcomes | Main: glycaemic control. Secondary: maternal depressive symptoms (patient Health Questionnaire (PHQ‐9), adaptive coping strategies (Responses to Stress Questionnaire (RSQ)), social support (Multidimensional Scale of Perceived Social Support (MSPSS)), parental involvement (Diabetes Family Conflict Scale (DFCS)), adolescent adherence (Self Care Inventory (SCI)), parent diabetes‐related distress (Parent Diabetes Distress Scale (DDS‐P)), diabetes‐ related knowledge (Revised Diabetes Knowledge Test), adolescent adjustment (Child Behavior Checklist (CBCL), Problem Areas in Diabetes (PAID), Youth Self Report (YSR)), adolescent quality of life (Pediatric Quality of Life 3.0 Type 1 Diabetes Module (PedsQL)). |
| Starting date | Not reported |
| Contact information | Sarah S. Jaser Email: sarah.jaser@vumc.org |
| Notes |
Kaylor‐Hughes 2017.
| Study name | Direct to public peer support and e‐Therapy program versus information to aid self‐management of depression and anxiety: protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | Residents 16 years of age or older from County of Nottinghamshire with a probable case of depression and/or anxiety and have access to the Internet. |
| Interventions | Intervention: participants will receive six months of free access to the Big White Wall web site. Participants will have access to web‐based mental and physical health assessments, moderated online peer support network, and various self‐managed and facilitated programs. Control: participants will be directed to Moodzone, a web site that provides information providing information on mental health. |
| Outcomes | Main: self‐rated well‐being (WEMWBS). Secondary: maintenance of well‐being, symptoms of anxiety (GAD‐7 scale), depression (PHQ‐9), health‐related quality of life (SF‐12v2), social support (MOS‐SS), social function (WSAS). Other: medical outcomes (Medical Outcomes Study Short Form health survey version 2.0), Client Service Receipt Inventory, RE‐AIM framework. |
| Starting date | Not reported |
| Contact information | Richard K Morriss, MB ChB, MRCPsych, MMedSci, MD, FRCPsych Phone: 44 01158232478 Email: richard.morriss@nottingham.ac.uk |
| Notes |
Kim 2017.
| Study name | Harnessing Facebook for smoking reduction and cessation interventions: Facebook user engagement and social support predict smoking reduction |
| Methods | RCT |
| Participants | Smokers between 18‐65 years of age and living in the USA. |
| Interventions | Intervention: participants were encouraged to share their thoughts and progress and support their peers on Facebook. A professional clinical expert joined the group to provide guidance and anti‐smoking materials were posted by the research team. Intervention: MTurk‐only condition not described. Control: email only. |
| Outcomes | Main: self‐reported smoking reduction. Secondary: anti‐smoking attitudes, readiness to quit, motivation to quit, self‐efficacy, perceived social support. |
| Starting date | November 2015 |
| Contact information | Sunny Jung Kim Phone: 1‐603‐646‐7041 Email: sunny.j.kim@dartmouth.edu |
| Notes | Published paper currently only reports outcomes for the Facebook group. We contacted the authors who said that a paper reporting outcomes for all groups was being submitted. |
McKeon 2019.
| Study name | A mental health informed physical activity program for first responders and their chosen support partners |
| Methods | Stepped‐wedge RCT |
| Participants | Sedentary first responders and their chosen support partner (age 18‐65, male and female participants). |
| Interventions | Intervention: group based physical activity through a private Facebook group, option to join a weekly call. Control: the same participants act as their own controls through the study design. |
| Outcomes | Main: psychological distress (Kessler 6). Secondary: Feasibility, Acceptability, Physical activity levels (Fitbit data and SIMPAQ), depression and anxiety (DASS21), PTSD symptoms (PCL‐5), Sleep Quality (Pittsburgh Sleep Quality Index), quality of life (AQoL‐6D), social support to exercise (social support and exercise survey), suicidal ideation (SIDAS), mental health service utilisation. |
| Starting date | June 21, 2019 |
| Contact information | Grace McKeon Phone: +61 434041357 Email: g.mckeon@unsw.edu.au |
| Notes |
NCT03021655.
| Study name | A pilot randomized control trial to help youth smokers to quit smoking |
| Methods | RCT |
| Participants | Hong Kong resident who has smoked in the last 30 days and is between 12‐25 years of age. |
| Interventions | Intervention: adventure‐based group ‐ one camp day which includes physical activity and health education on self‐efficacy, self‐esteem, emotion and smoking abstinence. Intervention: WhatsApp group ‐ messages about mood and stress management sent to a Whatsapp group each week for 6 months. Control: telephone counselling on quitting smoking. |
| Outcomes | Main: self‐reported 7‐day point prevalence Secondary: biochemical validated quit rate, depressive symptoms (CESDC), self‐esteem (RSES), quality of life (SF‐6D). |
| Starting date | December 2016 |
| Contact information | Dr. Li William Ho Cheung, PhD Phone: 852‐39176634 Email: william3@hku.hk |
| Notes |
NCT03078153.
| Study name | Effect of social media support and financial incentives on PrEP adherence |
| Methods | RCT |
| Participants | African American, Latino and Asian males (assigned at birth) between 18 to 24 years of age who are HIV negative and have had unprotected sex with a man in the last 6 months. |
| Interventions | Intervention: financial incentive ‐ receive incentive at follow‐up visits. Intervention: social media group ‐ Access to Facebook group with links to PrEP information and ability to ask questions and communicate experiences with PrEP. Control: no intervention. |
| Outcomes | Main: Adherence to Truvada. Secondary: New Cases of HIV, incidence of STIs. |
| Starting date | April 1, 2017 |
| Contact information | Mark Siegel, MD Contact information not provided |
| Notes |
NCT03109743.
| Study name | Group clinical visit adherence intervention for HIV+ women of color |
| Methods | RCT |
| Participants | HIV positive cis gender women who are 18 years of age or older, undergoing HIV treatment and report antiretroviral therapy adherence of less than 100% in the last 30 days. |
| Interventions | Intervention: Sisters‐GPS: weekly group clinical visits and participation in a private social media site. Control: one‐on‐one adherence counselling. |
| Outcomes | Main: antiretroviral therapy adherence (pill count, self‐report). Secondary: change in HIV viral load, HIV viral load suppression, antiretroviral therapy adherence. Other: antiretroviral therapy beliefs and attitudes (ARV beliefs and attitudes questionnaire), antiretroviral therapy knowledge ( HIV Treatment Knowledge Scale), medication side effects (Treatment Satisfaction Questionnaire for Medication), perceived self‐efficacy (ARV adherence Self‐Efficacy Scale), perceived HIV‐related stigma (HIV Stigma Scale), perceived social support (Scale of Perceived Social Support). |
| Starting date | May 17, 2017 |
| Contact information | Oni Blackstock Contact information not provided |
| Notes | The study was terminated early as funding was relinquished. |
NCT03143309.
| Study name | Physical activity intervention to promote walking among female university students |
| Methods | RCT |
| Participants | Females who are 18‐28 years of age and enrolled in University. |
| Interventions | Intervention: introductory session, pedometer instruction, daily pedometer use and enrolment in a Whatsapp group with health promotional content delivered 2‐3 times per week. Control: enrolled in Whatsapp group with non‐health related content delivered 2‐3 times per week. |
| Outcomes | Primary: walking (change in 7‐day average steps objectively). Secondary: self‐reported walking, body mass index, barriers to weight management. |
| Starting date | March 15, 2017 |
| Contact information | Abdulrahman Al‐Mohaimeed Contact information not provided |
| Notes |
NCT03149757.
| Study name | Connecting youth and young adults to optimize ART adherence: YouTHrive efficacy trial |
| Methods | RCT |
| Participants | HIV positive adolescents and young adults between 15‐24 years of age who have an antiretroviral therapy prescription with treatment non adherence (HIV care appointments or medication) or a detectable viral load. |
| Interventions | Intervention: YouTHrive ‐ a private social networking site that involves peer‐to‐peer interaction, daily monitoring of HIV medication adherence and mood, daily mixed‐media content with strategies to improve medication adherence' and goal setting and monitoring. Participants will also receive weekly SMS text messages to visit the site. Control: brief informational text and graphic‐based webpages released weekly via email. The 'newsletter' will contain static information on living with HIV but not ART adherence. |
| Outcomes | Main: sustained undetectable viral load. Other: self‐reported antiretroviral therapy adherence (Adherence Scale), ART adherence strengths and barriers ((IMB ART Adherence Questionnaire (IMB‐AAQ), self‐efficacy for adherence to HIV treatment plans (HIV ASES), adherence support, substance use (cocaine, phencyclidine, tobacco, alcohol, cannabis, amphetamines, inhalants, sedatives, hallucinogens, and opioids using 5‐panel screening test), mental health (depression using PHQ‐8, anxiety using GAD‐7, emotional regulation using Emotional Regulation Questionnaire, HIV stigma using stigma scale), relationship status, sexual behaviour, social support (PROMIS short‐form), technology adoption and use, intervention ease of use (System Usability Scale), acceptability, and satisfaction, user engagement. |
| Starting date | May 16, 2017 |
| Contact information | Keith J. Horvath, PhD Phone: 1 (612) 626 1799 Email: horva018@umn.edu |
| Notes |
NCT03163303.
| Study name | Smoking Tobacco and Drinking Study (STAND) |
| Methods | RCT |
| Participants | Individuals between 18 and 25 years of age who have smoked ≥100 cigarettes in their lives and currently smoke at least 1 cigarette per day on 4 or more days of the week and have had at least one heavy drinking episode (5+ for men, 4+ for women) in the past month. |
| Interventions | Intervention: Tobacco Status Project Intervention + Alcohol Intervention ‐ 90 days of Facebook messaging and weekly live sessions targeting tobacco use and alcohol use plus a 14‐day supply of nicotine patch. Control: Tobacco Status Project Intervention ‐ 90 days of Facebook messaging and weekly live sessions targeting tobacco use only plus a 14‐day supply of nicotine patch. |
| Outcomes | Main: 7‐day point prevalence abstinence Secondary: number of participants with a reduction in cigarettes smoked over time, number of participants whom attempted to quit tobacco use during the course of treatment, number of participants reporting a readiness to quit tobacco use over time, average score on the Thoughts About Abstinence questionnaire, average number of days of heavy episodic drinking over time, median number of drinks per week over time, average score on the Alcohol Use Disorder Identification Test ‐ Concise (AUDIT‐C) over time, alcohol quit attempt, readiness to change alcohol use over time, average score on the Thoughts About Abstinence Questionnaire (Heavy Episodic Drinking) over time, number of participants with reported combined use using tobacco or alcohol over time. |
| Starting date | December 18, 2017 |
| Contact information | Derek Satre, PhD Email: derek.satre@ucsf.edu |
| Notes |
NCT03169686.
| Study name | 'WeChat WeQuit' smoking cessation program |
| Methods | RCT |
| Participants | Daily Chinese cigarette smokers who 18 years of age or older and willing to make an attempt to quit smoking in the next month. |
| Interventions | Intervention: multiple messages will be sent daily to participants providing smoking cessation related information and encouragement to send peer support messages to WeChat group. Control: no smoking related messages. |
| Outcomes | Main: continuous abstinence at 24 weeks. Secondary: 7 day point‐prevalence abstinence, reductions in number of cigarettes smoked per day, rates of participation in and completion of smoking‐cessation programs. |
| Starting date | August 1, 2019 |
| Contact information | Yanhui Liao Phone: 8615116225099 Email: tangliaoyanhui@163.com |
| Notes |
NCT03253406.
| Study name | Health wearables and college student health |
| Methods | RCT |
| Participants | Individuals who are between 18‐29 years of age with a BMI ≥ 18.5 and are not currently getting enough physical activity as well as servings of fruits and vegetables per day. |
| Interventions | Intervention: Polar M400 + Facebook Group ‐ Polar M400 smartwatch with physical activity and nutritious eating tips on Facebook. Control: Facebook Only Group ‐ content‐identical Facebook group. |
| Outcomes | Main:pPhysical activity (Actigraph Link accelerometers). Secondary: cardiovascular fitness (YMCA 3‐minute step test), body composition (bioelectrical impedance), body weight, self‐efficacy, social support (Patient‐Centered Assessment and Counseling for Exercise questionnaire), enjoyment, barriers, outcome expectancy, intrinsic motivation (Intrinsic Motivation Inventory), nutritious eating behaviours (National Cancer Institute's Automated Self‐Administered (ASA) 24‐hour Dietary Recall), and Facebook‐delivered health intervention adherence. |
| Starting date | September 6, 2017 |
| Contact information | Zan Gao, PhD Contact information not provided |
| Notes |
NCT03257657.
| Study name | Helping Moms to be healthy after baby |
| Methods | RCT |
| Participants | Post‐partum females between 18‐50 years of age who are enrolled or has an infant enrolled in Women, Infants, Children (WIC) and has a pre‐pregnancy BMI of 25 ‐ 40 kg/m2 as well as a postpartum BMI between 25 and 50 kg/m2. |
| Interventions | Intervention: Lifestyle group ‐ visits and weekly phone coaching with WIC staff, text messages with informational and motivational content, and access to a private Facebook group. Control: Observation group ‐ regular WIC care, a packet of written materials on lifestyle interventions and access to a Registered Dietitian at 12 weeks. |
| Outcomes | Main: feasibility of recruitment, attrition rate, visit attendance, acceptability of a weight loss intervention, evaluation of the use of phone coaching. Secondary: change in weight between visits, changes in diet (Block Fat‐Sugar‐Fruit‐Vegetable Screener), changes in physical activity (Pregnancy Physical Activity Questionnaire), changes in diet and physical activity self‐efficacy (Eating Habits Confidence Survey and Exercise Confidence Survey), changes in motivations to eat (Eating Stimulus Index questionnaire), changes in readiness to change, (Readiness to Change questionnaire) changes in diet: intakes measured in cups, changes in diet: kcal intake (Block Fat‐Sugar‐Fruit‐Vegetable Screener). |
| Starting date | July 31, 2017 |
| Contact information | Darcy A Thompson, MD, MPH Phone: 303 724 7471 Email: darcy.thompson@ucdenver.edu |
| Notes |
NCT03259360.
| Study name | A Facebook intervention for young sexual and gender minority smokers (POP) |
| Methods | RCT |
| Participants | Young sexual and gender minorities between 18 to 25 years of age who smoke cigarettes |
| Interventions | Intervention: the Put It Out Project (POP) ‐ A 90‐day culturally tailored intervention tailored to sexual and gender minority young adults on Facebook which includes weekly live sessions targeting tobacco use. Control: non‐tailored Tobacco Status Project intervention delivered to groups of only sexual and gender minority participants on Facebook. |
| Outcomes | Main: 7‐day point prevalence abstinence at 3 months and 6 months. Secondary: reduction in cigarettes smoked by at least 50%, tobacco use quit attempts, readiness to quit tobacco and thoughts about tobacco abstinence. |
| Starting date | April 23, 2018 |
| Contact information | Gary L. Humfleet, PhD Contact information not provided |
| Notes |
NCT03387800.
| Study name | RCT for evaluation of online social networking intervention in smoking cessations |
| Methods | RCT |
| Participants | Current smokers who are 18 years of age or older. |
| Interventions | Intervention: basic health education messages sent through WeChat and WeChat online peer support groups. Control: basic health education messages sent through WeChat only. |
| Outcomes | Main: self reported 7‐day point prevalence quit rate. Secondary: number of cigarettes consumed per day as compared to that of the baseline, Positive and Negative Affect Scale score, Smoking Self‐Efficacy Questionnaire score, Subjective Norms Scale score, Attitude Towards Smoking Scale score. |
| Starting date | August 1, 2015 |
| Contact information | Zixin Wang, PhD Contact information not provided |
| Notes |
NCT03441321.
| Study name | Social‐media intervention in reducing indoor tanning in high‐risk indoor tanners |
| Methods | RCT |
| Participants | 18 to 25 year old females that are high risk indoor tanners (used an indoor tanning bed at least 10 times in the previous 12 month). |
| Interventions | Intervention: secret Facebook group focusing on avoiding indoor tanning and promoting a healthy body image. Control: secret Facebook group focusing on other health topics. |
| Outcomes | Main: number of indoor tanning sessions. Secondary: indoor tanning behavior, skin burns from indoor tanning, tanning intentions. |
| Starting date | June 1, 2019 |
| Contact information | Sharon Manne, PhD Phone: 732‐235‐6759 Email: mannesl@cinj.rutgers.edu |
| Notes |
NCT03456453.
| Study name | Social media HIV prevention intervention for high risk rural women |
| Methods | RCT |
| Participants | Incarcerated females 18 years of age and older who lived in a rural Appalachian county prior to incarceration with previous high‐risk drug use and engagement sexual risk behaviour. |
| Interventions | Intervention: the National Institute on Drug Abuse (NIDA) Standard via Facebook ‐ HIV prevention education focused on reducing risky sexual and drug use practices on Facebook. Control: re‐entry services as usual. |
| Outcomes | Main: study enrolment. Secondary: HIV risk behaviours. |
| Starting date | May 29, 2019 |
| Contact information | Michele Staton, PhD Phone: 859‐257‐2483 Email: mstaton@uky.edu |
| Notes |
NCT03553992.
| Study name | An extended Facebook intervention for young sexual and gender minority smokers (POP‐6) |
| Methods | RCT |
| Participants | Young sexual and gender minorities between 18 to 25 years of age who smoke cigarettes |
| Interventions | Intervention: the Put It Out Project (POP) ‐ A 90‐day culturally tailored intervention tailored to sexual and gender minority young adults on Facebook which includes weekly live sessions targeting tobacco use plus a 14‐day supply of nicotine patch. Control: non‐tailored Tobacco Status Project intervention delivered to groups of only sexual and gender minority participants on Facebook plus a 14‐day supply of nicotine patch. |
| Outcomes | Main: 7‐day point prevalence abstinence at 3 months and 6 months. Secondary: reduction in cigarettes smoked by at least 50%, tobacco use quit attempts (Smoking Questionnaire), readiness to quit tobacco and thoughts about tobacco abstinence (4‐item Thoughts About Abstinence Form). |
| Starting date | October 29, 2018 |
| Contact information | Gary L. Humfleet, PhD Contact information not provided |
| Notes |
NCT03556774.
| Study name | Boosting Chinese healthcare service providers' utilization of smoking cessation interventions by 'WeChat WeQuit' program |
| Methods | RCT |
| Participants | Chinese Health Service Providers (HSP). |
| Interventions | Intervention: 'WeChat WeQuit' smoking cessation training program with regular smoking cessation training program messages. Control: participants without smoking cessation training and will not receive any smoking cessation messages. |
| Outcomes | Main: effectiveness of 'WeChat WeQuit' training program (utilisation rate of behavioural and pharmacotherapy interventions by HSP for smoking patients). Secondary: prevalence of 7‐day point prevalence smoking abstinence. |
| Starting date | April 1, 2019 |
| Contact information | Yanhui Liao, MD Phone: 8615116225099 Email: tangliaoyanhui@163.com |
| Notes |
NCT03567226.
| Study name | Leveraging WeChat social‐media and messaging platform to increase physical activity in Chinese glaucoma patients |
| Methods | RCT |
| Participants | Glaucoma patients who are 40 years of age or older. |
| Interventions | Intervention: WeChat group which receives exercise reminders, health education materials, and interaction with others. Control: a handout and counselling of the benefits of exercise on eye health. |
| Outcomes | Main: number of daily steps (Accelerometer). Secondary: time spent in moderate to vigorous physical activity. |
| Starting date | June 25, 2018 |
| Contact information | David Friedman, MD, MPH, MPH Contact information not provided |
| Notes |
NCT03574012.
| Study name | SmART Heart: study of mHealth apps to reduce cancer‐treatment effects on the heart |
| Methods | RCT |
| Participants | Individuals between 18 to 55 years of age who are in remission with a prior diagnosis of leukaemia, lymphoma or hematopoietic cell transplantation and have at least one cardiovascular risk factor. |
| Interventions | Intervention: goal‐setting and coaching on physical activity and diet supplemented with peer support through the study's social media platform and access to mHealth apps (Fitbit, Healthwatch) Control: receive general information about physical activity and diet with access to Fitbit and Healthwatch only. |
| Outcomes | Main: Enrollment rate, retention rate, participation in Facebook group, Fitbit physical activity tracking and Healthwatch diet tracking. |
| Starting date | August 31, 2018 |
| Contact information | Eric Chow Contact information not provided |
| Notes |
NCT03658044.
| Study name | Social Media on Prescription for colorectal cancer patients (SMOP) |
| Methods | RCT |
| Participants | Adults 18 years of age or older with a colorectal cancer diagnosis within the last year. |
| Interventions | Intervention: participate in a closed weekly Internet forum with other participants. Control: access to the general website, but not the forum. |
| Outcomes | Main: self empowerment (12 months) (Cancer Behavior Inventory (CBI)). Secondary: self empowerment (3 months) (Cancer Behavior Inventory (CBI)), compliance to treatment, quality of life, usability of a health care platform. |
| Starting date | December 1, 2018 |
| Contact information | Eva Angenete, MD, PhD Phone: +46760514441 Email: eva.angenete@vgregion.se |
| Notes |
NCT03677739.
| Study name | Young melanoma family Facebook intervention or healthy lifestyle Facebook intervention in improving skin examination in participants with melanoma and their families |
| Methods | RCT |
| Participants | Melanoma patients between 18‐39 years of age who completed treatment at least 3 months prior with no concurrent cancer diagnosis. First degree relatives between 18‐80 years of age who do not have melanoma. |
| Interventions | Intervention: access to young melanoma family Facebook group. Control: access healthy lifestyle Facebook group. |
| Outcomes | Main: total cutaneous examination. Secondary: skin self‐exam (count response and comprehensiveness for relatives and patients), sun protection habits (relatives and patients) (Sun protection behaviours scale). Other: Normative influences, family and peer support, risks, benefits, barriers, self‐efficacy, use of change strategies, Melanoma risk factors, month of the year enrolled, Residential Latitude, Sex, patient disease stage, relationship to patient, Facebook engagement, social network use. |
| Starting date | September 1, 2019 |
| Contact information | Sharon Manne, PhD Phone: 732‐235‐6759 Email: mannesl@cinj.rutgers.edu |
| Notes |
NCT03678181.
| Study name | Increasing engagement and improving HIV outcomes via HealthMPowerment |
| Methods | RCT |
| Participants | Male (assigned at birth) between 15‐29 years of age who identify as Black/African American and/or Latino/Hispanic and have had a previous condomless anal sex act with a man. |
| Interventions | Intervention: HMP 2.0 Arm ‐ Knowledge Center focused on HIV prevention content, interactive forums, and a provider question & answer platform. Intervention: peer‐referred HMP network arm ‐ HMP 2.0 but participants can also refer and enrol 2 peers of their choosing into the study. Control: information only group ‐ HMP 1.0 Knowledge Center with tailored information and content for young Black or Latino men who have sex with men and transgender women but no engagement. |
| Outcomes | Main: Change in HIV testing behaviour, change in viral suppression. Secondary: Change in treatment adherence, change in Pre‐Exposure Prophylaxis (PrEP) uptake. |
| Starting date | July 20, 2020 |
| Contact information | Jose A Bauermeister, PhD Phone: 215‐898‐9993 Email: bjose@upenn.edu |
| Notes |
NCT03684070.
| Study name | Together we move: a multi‐component intervention to increase physical activity for ethnic minority older adults |
| Methods | RCT |
| Participants | Self‐identified Chinese or Chinese American who is 60 years of age or older |
| Interventions | Intervention: Fitbit and lifestyle counselling/education sessions plus WeChat motivational messages and peer interaction. Control: Fitbit and lifestyle counselling/education sessions only. |
| Outcomes | Main: physical activity (Fitbit steps). Secondary: self‐efficacy for physical activity (Self‐Efficacy for Exercise), qualitative feedback. |
| Starting date | May 18, 2018 |
| Contact information | Carina Katigbak, PhD Phone: 617‐552‐8718 Email: katigbac@bc.edu |
| Notes |
NCT03897049.
| Study name | Evaluation of the Trans Women Connected Mobile App for changes in sexual health‐related behavior among transgender women |
| Methods | RCT |
| Participants | Sexually active self‐identified trans women between 18‐49 years of age. |
| Interventions | Intervention: Trans Women Connected mobile app which includes more than 30 interactive activities (resource maps, PrEP/PEP content, and communication forums). Control: general health mobile app that contains sexual health information. |
| Outcomes | Main: self‐reported STI/HIV testing in past three months, receptive condomless anal intercourse or condomless vaginal intercourse. Secondary: use of a condom at last receptive anal intercourse or vaginal intercourse, sexual partners, unprotected, in last 3 months, health care visits, multidimensional Scale of Perceived Social Support, engaged as/with mentor, PrEP Uptake, self‐efficacy in decisions around safe sex behavior (HIV & Safer Sex: Self Efficacy Scale), patient communication self‐efficacy within clinical encounters (Ask,Understand, and Remember (AURA)), degree of comfort with external appearance as it relates to gender identity (Transgender Congruence Scale (TCS)), rumination in the context of gender identity (The Gender Identity Reflection and Rumination Scale). Other: Reactions to trans women connected. |
| Starting date | Estimated start: April 2020 |
| Contact information | Tamara Kuhn, MA Phone: 831.440.2104 Email: tamara.kuhn@dfusioninc.com |
| Notes |
NCT03907462.
| Study name | SMART 2.0: social mobile approaches to reducing weight in young adults (SMART 2) |
| Methods | RCT |
| Participants | Overweight or obese adults who are between 18‐35 years of age. |
| Interventions | Intervention: SMART 2.0 (a popular consumer‐level wearable, wireless scale, and corresponding app, tailored and interactive text messaging system, multiple social media streams, social network mechanisms of influence and technology‐mediated health coaching) with technology and personal health coaching treatment group. Intervention: SMART 2.0 technology alone treatment group. Control: consumer‐level wearable and scale with a corresponding app to use at their discretion. |
| Outcomes | Main: change in weight Secondary: change inBMI, per cent weight change, percentage of participants who lost at least 3% of their weight from baseline, percentage of participants who lost at least 5% of their weight from baseline, change in waist circumference, change in waist‐to‐hip ratio, change in body composition, change in bone mineral density, change in systolic blood pressure, change in diastolic blood pressure, change in cardiorespiratory fitness, change in flexibility, change in grip strength, physical activity (Fitbit, waist‐worn tri‐axial accelerometer and Global Physical Activity Questionnaire), sleep, change in sleep, resting heart rate, change in resting heart rate, sedentary behavior (Fitbit and waist‐worn tri‐axial accelerometer), change in sedentary behaviour, diet history, weight management practices, strategies for weight management, eating behaviours, daily meal patterns, healthy eating: change strategies, physical activity: change strategies, physical activity neighbourhood environment, social support for healthy eating habits, social support for physical activity, depression, anxiety, self‐esteem, quality of well‐being, body image. Other: Smoking & marijuana use, alcohol use. |
| Starting date | April 1, 2019 |
| Contact information | Shadia J Assi, MPH Phone: 8582463302 Email: sjassi@ucsd.edu |
| Notes |
NCT03959631.
| Study name | Effectiveness and cost‐effectiveness of a VCoP to empowerment of patients with ischaemic heart disease in PHC: cluster‐RCT |
| Methods | RCT |
| Participants | Adult patients with an active diagnosis of ischaemic heart disease. |
| Interventions | Intervention: Virtual Community of Practice on a web 2.0 platform. Control: usual care according to clinical practice guidelines. |
| Outcomes | Main: patient activation (Patient Activation Measure questionnaire). |
| Starting date | Estimated start date: September 1, 2020 |
| Contact information | Sofía Garrido Elustondo Phone: 913016400 ext 204 Email: sgarrido@salud.madrid.org |
| Notes |
NCT04010019.
| Study name | The facing pain study |
| Methods | RCT |
| Participants | Adults 18 years of age or older with chronic pain (i.e. pain for over 3 months). |
| Interventions | Intervention: enhanced Facebook condition ‐ psychoeducation on pain neurobiology, emotional validation training, facilitating patients' emotional disclosures, and prompts to engage participants in activities. Control: Facebook condition ‐ instruction on offering mutual support. |
| Outcomes | Main: change in pain severity and change in pain interference. Secondary: change in depression, change in anxiety, change in chronic pain social support, change in anger, change in self‐efficacy for managing pain, change in helplessness, change in self‐efficacy for managing emotions, change in social isolation, change in pain catastrophising, change in alexithymia, change in substance use (drinking / opioid use/marijuana use), and perceived emotional support within the Facebook group. Other: ambivalence over emotional expression, perceived social constraints, childhood adverse events, attachment style. |
| Starting date | September 27, 2019 |
| Contact information | Mark A. Lumley Contact information not provided |
| Notes |
NCT04045132.
| Study name | The parenting with depression study |
| Methods | RCT |
| Participants | Females with postpartum depression who are over the age of 18 years and have an infant less than 8 months old. |
| Interventions | Intervention: parenting program on Facebook (video vignettes, narrated PowerPoint presentations, written materials, comments on postings daily, provides feedback to participants) and MoodGym (an online cognitive behavioral treatment program with interactive exercises, workbooks, anxiety and depression quizzes, and downloadable relaxation audio files) with facilitator texting or email check‐ins. Control: MoodGym alone with facilitator texting or email check‐ins. |
| Outcomes | Main: the quality of affect and behaviour in parent‐child interactions (The Patient Child Early Relational Assessment (PCERA)). Secondary: change in depressive symptoms (the Edinburgh Postnatal Depression Scale (EPDS) and BDI‐II), change in parenting self‐esteem and confidence (Parenting Sense of Competence Scale (PSOC)), change in parenting stress (the Parenting Stress Index‐Short Form (PSI‐SF), and mental health service use (National Comorbidity Survey (NCS)). |
| Starting date | December 17, 2019 |
| Contact information | James Guevara, MD, MPH Phone: 215‐590‐1130 Email: guevara@email.chop.edu |
| Notes |
NCT04187989.
| Study name | Social media intervention for cannabis use in emerging adults |
| Methods | RCT |
| Participants | Adults between 18‐25 years of age who report using cannabis at least 3 times per week. |
| Interventions | Intervention: Facebook page with e‐coaches promoting well‐being and reducing risky behaviours. Control: Attention‐Control E‐News condition. |
| Outcomes | Main: change in frequency of cannabis use, change in quantity of cannabis used, change in consequences of cannabis use. Secondary: change in perceived risk of cannabis use, change in peer approval/disapproval of cannabis use, changes in cannabis impaired driving, change in other drug use, change in frequency of alcohol consumption, change in quantity of alcohol consumption. |
| Starting date | February 3, 2020 |
| Contact information | Erin Bonar Email: erinbona@med.umich.edu |
| Notes |
NCT04217759.
| Study name | Healthy lifestyle intervention on diabetes risk reduction among Bruneian young adults |
| Methods | RCT |
| Participants | Bruneian individuals between 18 to 29 years of age with a BMI of 25 to 39.99 and a diabetes risk score of 3 to 8. |
| Interventions | Intervention: healthy lifestyle intervention emphasising on physical activity and diet for 12 weeks via face‐to‐face sessions, Facebook and Whatsapp. Control: leaflets on healthy lifestyle with no further guidance. |
| Outcomes | Main: change in diabetes risk score (Finnish Diabetes Risk Score (FINDRISC) questionnaire). Secondary: change in weight (kg and %), height, change in body mass index, change in waist circumference, change in hip circumference, change in waist‐to‐hip ratio, change in fasting blood glucose, change in fasting blood total cholesterol, change in fasting blood triglycerides, change in systolic blood pressure, change in diastolic blood pressure, change in resting heart rate, change in vigorous physical activity metabolic task (short‐form international PA questionnaire (SF‐IPAQ), change in moderate physical activity metabolic task (SF‐IPQ), change in walking metabolic task (SF‐IPQ), change in total physical activity metabolic task (SF‐IPQ), change in sitting time (SF‐IPQ), change in intake of carbohydrates, change in intake of protein, change in intake of fruits, change in Intake of vegetables, change in intake of water, change in motivation score (University of Rhode Island Change Assessment (URICA)), change in social support (diet and physical activity) score (social cognitive theory (SCT) constructs scale), change in social support (physical activity) score (social cognitive theory (SCT) constructs scale), change in overcoming barriers (physical activity) score (social cognitive theory (SCT) constructs scale), change in moral disengagement (diet) score (social cognitive theory (SCT) constructs scale), change in outcome expectations (diet and physical activity) score (social cognitive theory (SCT) constructs scale), change in emotional coping (physical activity) score (social cognitive theory (SCT) constructs scale), change in self‐efficacy (physical activity) score (social cognitive theory (SCT) constructs scale), facilitation (physical activity) score (social cognitive theory (SCT) constructs scale). |
| Starting date | October 1, 2017 |
| Contact information | Alifah Nur'ain Haji Mat Rasil Contact information not provided |
| Notes |
NCT04286165.
| Study name | Brief peer supported webSTAIR compared to enhanced wait list |
| Methods | RCT |
| Participants | Veterans between 21 to 80 years of age who have Post Traumatic Stress Disorder (PTSD) and have experienced at least one traumatic event. |
| Interventions | Interventions: BPS webSTAIR, an online platform for teaching skills in emotion regulation with the support of peers. Control: no BPS webSTAIR‐ Waitlist. |
| Outcomes | Main: change on Difficulties in Emotion Regulation Scale, change on Personal Health Questionnaire Depression Scale, change in PTSD Checklist for DSM‐5 (PCL‐5), change on the Work and Social Adjustment Scale (WSAS), change on Clinically Administered PTSD Scale (CAPS), Life Events Checklist for DSM‐5 (LEC‐2). |
| Starting date | January 20, 2020 |
| Contact information | Adam D Jacobs, MA Phone: 650‐714‐3998 Email: adam.jacobs2@va.gov |
| Notes |
NCT04367506.
| Study name | Adapting a digital intervention to improve smoking cessation in persons with serious mental illness |
| Methods | RCT |
| Participants | Current smokers who are diagnosed with a serious mental illness, are interested in quitting smoking and are 18 years of age or older. |
| Interventions | Intervention: BecomeanEX which includes a website that provides education about smoking and quitting, text messaging real‐time digital coaching, and an online community plus usual care (two weeks of nicotine replacement therapy, brief individual counselling, and referral to the MD quit line). Control: Usual care. |
| Outcomes | Primary outcomes: feasibility of recruitment, feasibility of registration, acceptability (Services Satisfaction Questionnaire), website utilisation, 7‐day point prevalence smoking abstinence, craving (Tobacco Cravings Questionnaire), self‐efficacy (Smoking Situations Confidence Questionnaire), motivation to remain abstinent (Abstinence‐Related Motivational Engagement Scale). |
| Starting date | Estimated start date: July 2020 |
| Contact information | Melanie Bennett, PhD Phone: 410‐706‐2490 Email: mbennett@som.umaryland.edu |
| Notes |
Pagoto 2016.
| Study name | Engaging Moms on teen indoor tanning through social media: protocol of a randomized controlled trial |
| Methods | RCT |
| Participants | Mothers who live in Tennessee, have a daughter between the ages of 14 to 17, can read English and have a Facebook account or are willing to create one. Teen daughters will be enrolled in the study as well. |
| Interventions | Intervention: participants will have access to a private Facebook group name Health Chat with health messages (25% on preventing indoor tanning and 75% are on other health topics (e.g. nutrition, physical activity, etc). Posts will occur twice daily for 12 months. Control: participants will have access to a private Facebook group with health messages. These messages will not include any content about indoor tanning (25% on preventing prescription drug abuse and 75% on the same health topics as the intervention condition). |
| Outcomes | Main: mothers’ permissiveness for daughters to tan indoors, mothers' indoor tanning prevalence, daughters' indoor tanning prevalence, mothers' support for stricter bans on indoor tanning by minors. Other: overall health status, number of servings of fruits and of vegetables, number of times sugar sweetened drinks, body mass index, physical activity, alcoholic beverage intake, smoking behavior, mental health, human papillomavirus (HPV) vaccination status, abuse of prescription drugs, mothers’ engagement, maternal communication, mother‐daughter relationship quality, information sharing. |
| Starting date | Recruitment began in September 2016. |
| Contact information | Sherry L Pagoto, PhD Phone: 1 508 856 2092 Email: Sherry.Pagoto@umassmed.edu |
| Notes |
Patel 2018.
| Study name | Empowering with PrEP (E‐PrEP), a peer‐led social media‐based intervention to facilitate HIV preexposure prophylaxis adoption among young Black andLlatinx gay and bisexual men: protocol for a cluster randomized controlled trial. |
| Methods | RCT |
| Participants | Self‐identified Black or Latino males between 18‐29 years of age who have an HIV negative or unknown status and have had at risk sex with at least one male partner in the last year. |
| Interventions | Intervention: E‐PrEP‐ Peer‐Led Intervention about PrEP: Peer leaders recruit other participants to a private social media group to discuss PrEP, PrEP access, and other related health issues. Control: BxNow ‐ General Health Campaign: similar to intervention with private SM groups but information will focus on general health topics unrelated to HIV or sexual health. |
| Outcomes | Main: self‐reported PrEP uptake or intention, change on the PrEP motivational cascade at 12 weeks. Secondary: PrEP knowledge, PrEP‐related stigma, attitudes about PrEP, and access to primary or sexual health care. Other: changes in social network factors (e.g. social support) and whether social media engagement correlated with the primary and secondary outcomes. |
| Starting date | June 16, 2017 |
| Contact information | Viraj V Patel, MD, MPH Phone: 1 718 920 5256 Email: vpatel@montefiore.org |
| Notes |
Pechmann 2020.
| Study name | The use of web‐based support groups versus usual quit‐smoking care for men and women aged 21‐59 years: protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | Current smokers who are in the preparation stages of quitting and are between 21 ‐ 59 years of age. |
| Interventions | Intervention: NRT + Web Guide + Tweet2Quit‐Coed ‐ 90‐day quit smoking intervention that provides an online peer‐to‐peer support group (12 buddy pairs) on Twitter, daily automated texts providing feedback on their prior‐day tweeting behavior, Smokefree.gov quit guides emailed every 5 days plus 8 weeks of combination NRT. Intervention: NRT + Web Guide + Tweet2Quit‐Women ‐ same as other intervention group except Twitter group consists of women only. Control: Smokefree.gov quit guides emailed every 5 days plus 8 weeks of combination NRT. |
| Outcomes | Main: biochemically sustained abstinence. Secondary: percentage of participants with a 7‐day point prevalence abstinence. |
| Starting date | October 2016 |
| Contact information | Cornelia Ann Pechmann, MSc, MBA, PhD Phone: 1 3108920619 Email: cpechman@uci.edu |
| Notes |
Ramo 2018a.
| Study name | Tobacco status project |
| Methods | RCT |
| Participants | Young adults 18 to 25 years of age who have smoked ≥100 cigarettes in their lives and currently smoke. |
| Interventions | Intervention: participants in the Tobacco Status Project intervention are allocated to private Facebook groups according to readiness to quit smoking (i.e. ready to quit smoking or not ready to quit smoking). The Facebook groups include smoking cessation posts, tailored to readiness, delivered daily for 90 days. The posts include images, videos, and text to reflect the experience of young adults and all pose a question to elicit participant response. Control: participants in the Tobacco Status Project + Alcohol intervention are similarly allocated to private Facebook groups according to readiness to quit smoking. However, the content also targets heavy episodic drinking. |
| Outcomes | Main: biochemically‐verified 7‐day point prevalence abstinence from all tobacco products at 3, 6, and 12 months. Secondary: reduction in cigarettes smoked by at least 50%, quit attempts. Other: health risk behaviours (alcohol and illicit drug use, poor sleep quality, sedentary behavior, poor diet, depression, and high risk sexual behavior). |
| Starting date | October 2014 |
| Contact information | Danielle Ramo, PhD Email: danielle.ramo@ucsf.edu |
| Notes |
Siegmund 2017.
| Study name | Feasibility of a Facebook intervention for exercise motivation and cardiac rehabilitation adherence: study protocol |
| Methods | RCT |
| Participants | Men and women who qualify for cardiac rehabilitation (i.e. diagnosed with cardiovascular disease), are current and regular Facebook users, are 18 years of age or older, speak English, are entering cardiac rehabilitation the main campus of the tertiary care centre and live within 100 miles of this centre. |
| Interventions | Intervention: participants in the intervention group will be given access to a private Facebook group. Facebook posts, in the form of text, video or pictures, will be uploaded weekly to the group. The educational posts will include 12 health topics about preventative heart care and the provider posts will include support such as encouragement. Each participant will receive a text message prompt when a new post is added. Control: the control group will receive the same educational and provider support materials as the Facebook intervention group. However, these materials will be delivered to the participant in the form of handouts or email. Both groups are able to attend weekly education classes or peer interactions, with up to 3 hours of group cardiac rehabilitation per week. |
| Outcomes | Main: change in exercise motivation (BREQ‐3) and need satisfaction with exercise (PNSE scale). Secondary: percentage of cardiac rehabilitation sessions attended. Other: Facebook engagement and participants’ perceptions of the intervention. |
| Starting date | Project was funded in July 2017. |
| Contact information | Lee Anne Siegmund, RN, PhD Phone: 1 216 445 3457 Email: siegmul@ccf.org |
| Notes |
Sinicrope 2019.
| Study name | Social media intervention to promote smoking treatment utilization and cessation among Alaska Native people who smoke: protocol for the Connecting Alaska Native People to Quit Smoking (CAN Quit) pilot study |
| Methods | RCT |
| Participants | Alaska Natives over 19 years of age who are a currently smoke cigarettes as a main tobacco product and are considering or willing to make a quit attempt. |
| Interventions | Intervention: Facebook group moderated daily by a tobacco research counsellor, treatment referral information by mail and/or email and smokefree.gov quit smoking resources. Control: treatment referral information by mail and/or email and smokefree.gov quit smoking resources. |
| Outcomes | Main: feasibility indicators and biochemically verified smoking abstinence. Secondary: self‐reported other tobacco abstinence, smoking treatment utilisation, and interdependence as a culturally relevant mediator of intervention effectiveness. Other: social media engagement, usability, and satisfaction. |
| Starting date | No start date provided |
| Contact information | Pamela S Sinicrope, DrPH Phone: 1 507 266 1238 Email: Sinicrope.Pamela@mayo.edu |
| Notes |
Swendeman 2019.
| Study name | Text‐messaging, online peer support group, and coaching strategies to optimize the HIV prevention continuum for youth |
| Methods | RCT |
| Participants | Youth 12 to 24 years of age who test seronegative on HIV testing and are high risk for HIV. |
| Interventions | Intervention: Peer Support ‐ private, online peer support groups with peer supporters, coaches and project coordinators plus Automated Text Messaging and Monitoring (AMMI) which includes 1‐5 daily texts for 24 months to motivate, inform, and refer youth to health care and HIV service and a weekly monitoring survey. Intervention: coaching ‐ access to a dedicated Coach primarily through e‐mail, social media, text messages, and phone calls plus AMMI messages. Intervention: coaching + Peer Support ‐ online, private peer support groups, access to a Coach, and AMMI messages. Control: AMMI messages only. |
| Outcomes | Main: uptake and adherence to the HIV prevention continuum (HIV testing, STI testing, condom use frequency, PEP use/adherence, PREP use/adherence, sexual partners). Secondary: mental health symptoms (anxiety and depression), substance use (alcohol, marijuana, methamphetamines, opiates, cocaine. |
| Starting date | May 6, 2017 |
| Contact information | Dallas Swendeman, PhD, MPH Phone: (310) 794‐8128 Email: dswendeman@mednet.ucla.edu |
| Notes |
Wang 2017.
| Study name | Clinic versus online social network–delivered lifestyle interventions: protocol for the Get Social noninferiority randomized controlled trial |
| Methods | RCT |
| Participants | Participants who have a BMI between 27.0 and 45.0 kg/m2, are between the ages of 18 and 65 years, are a current social media user with a smartphone and interested in losing weight. |
| Interventions | Intervention: participants in the Get Social intervention will receive life counselling in a private Twitter group for 12 months. The intervention is based on the Diabetes Prevention Program, an evidence‐based weight loss program targeting lifestyle changes. Tweets will be in the form of text only; a combination of text and an image of an excerpt of the original materials; a combination of text and an image that reflects the content of the text, polls, and text; and a link to a study blog post or other online resource elaborating the topic. Participants will receive notifications (e.g., emails and pop‐ups) for new Tweets and are asked to report their weight change from the previous week by replying to the Tweets. Newsletters will be emailed weekly to encourage patients to engage in the Twitter group and to highlight content. Control: participants will receive 12 months of lifestyle counselling through 90 min session clinic‐based group meetings. this control is also based on the Diabetes Prevention Program, an evidence‐based weight loss program targeting lifestyle changes. |
| Outcomes | Main: weight loss (digital scale). Secondary: energy intake (24‐hour diet recall interviews ASA24), physical activity (74‐item Arizona Activity Frequency Questionnaire), administrative costs, interventionist costs, participant costs. Other: treatment retention, acceptability and burden. |
| Starting date | Recruitment began in August 2016. |
| Contact information | Sherry L Pagoto, PhD Phone: 1 860 486 2313 Email: sherry.pagoto@uconn.edu |
| Notes |
Waring 2019.
| Study name | Delivering a post‐partum weight loss intervention via Facebook or in‐person groups: protocol for a randomized feasibility pilot trial |
| Methods | RCT |
| Participants | Women 18 years of age or older who are overweight or obese and are 8 weeks to 12 months postpartum. |
| Interventions | Intervention: trained weight loss counsellor will deliver a lifestyle intervention based on Diabetes Prevention Program on a secret Facebook group (2 posts daily for the first 15 weeks, and 1 post daily for weeks 16 to 25), participants will receive calorie and physical activity goals, and use MyFitnessPal to track their energy intake, physical activity, and weight. Control: same intervention as above, but delivered in‐person through weekly 90‐minute group meetings for the first 15 weeks and then every other week in weeks 16 to 25. |
| Outcomes | Primary: feasibility of recruitment, sustained participation, contamination, retention, and feasibility of assessment procedures including measurement of costs. Other: 6‐ and 12‐month weight loss. |
| Starting date | September 2018 |
| Contact information | Molly E Waring, PhD Phone: 1 8604861446 Email: molly.waring@uconn.edu |
| Notes |
Wilcox 2018.
| Study name | A randomised controlled trial to prevent excessive gestational weight gain Rand promote postpartum weight loss in overweight and obese women: Health In Pregnancy and Postpartum (HIPP) |
| Methods | RCT |
| Participants | White or African American Women who are within the first 16 weeks of pregnancy, between the ages of 18‐44 years, have a prepregnancy BMI ≥ 25 kg/m2 and a prepregnancy weight ≤ 370 pounds, can read and speak English and has no plan to move outside of the geographic area in 18 months. |
| Interventions | Intervention: Participants in the lifestyle intervention will receive two one‐hour in‐depth counselling sessions, one during pregnancy and the other postpartum. The sessions will primarily focus on participants dietary intake and physical activity. Participants will receive a reports, a binder of study handouts, a pedometer for tracking physical activity and a bathroom scale. Weekly to biweekly 20‐minute telephone counselling, where participants weighs in and the interventionist refers to participant handouts. A total of 26 behavioural podcasts will be delivered to provide information weight gain in pregnancy, healthy eating and physical activity through dialogue and an audio blog. Finally, participants will have access to a private Facebook group for support and posts related to intervention content. Control: participants in the standard care group will receive regular clinic visits with prenatal care providers and standard nutrition counselling emphasising diet. Participants will also receive 12 study mailings focusing on development and 26 podcasts focusing on healthy pregnancy, fetal and infant development and parenting. |
| Outcomes | Main: total gestational weight gain. Secondary: gestational weight gain (Seca scale), postpartum weight retention, pregnancy and postpartum physical activity (SenseWear Armband, IPAQ), pregnancy and postpartum dietary intake (ASA24), health‐related quality of life (SF‐12), offspring adiposity Other‐ exercise social support (Friend Support for Exercise Habits Scale and the Family Support for Exercise Habits Scale), diet social support (Friend Support for Diet Scale and the Family Support for Diet), exercise self‐efficacy (Marcus and colleague's validated 5‐item questionnaire), diet self‐efficacy (10‐item Self‐Efficacy for Diet Questionnaire, exercise self‐regulation (EGS and Exercise Planning and Scheduling Scale), diet self‐regulation (22‐item scale from the HealthStyles survey), sociodemographic, health, and pregnancy‐related characteristics, satisfaction with body function and appearance, perceived stress (Perceived Stress Scale), depressive symptoms (10‐item Edinburgh Postnatal Depression Scale), general social support (Medical Outcomes Study Social Support Survey), physical activity environment (PANES), food environment, food insecurity (Household Food Security Scale), fast food consumption (Early Childhood Longitudinal Study). |
| Starting date | January 2015 |
| Contact information | Sara Wilcox, PhD Phone: 803‐777‐8141 Email: wilcoxs@mailbox.sc.edu |
| Notes |
Wysocki 2018.
| Study name | A web‐based coping intervention by and for parents of very young children with Type 1 diabetes: user‐centered design |
| Methods | RCT |
| Participants | Adult and child dyads, adults were eligible if they were parents of a child that was diagnosed with Type 1 diabetes before the age of 6, and their child is under 10 years of age. |
| Interventions | Intervention: the New Normal: a community of parents of young children with Type 1 diabetes website which includes a private social media platform enabling parents to interact around topics of shared interest or discuss website articles. Control: usual care. |
| Outcomes | Main: parental outcomes ‐ adjustment for managing their children’s T1D, treatment adherence, quality of life, psychiatric symptoms, social support, parenting self‐efficacy, T1D family routines, fear of hypoglycaemia, and benefit finding. Child outcomes ‐ haemoglobin A1c and general and T1D‐specific behavior problems. |
| Starting date | No start date provided |
| Contact information | Tim Wysocki Phone: 1 904 697 3483 Email: tim.wysocki@nemours.org |
| Notes |
BMI: body mass index; cRCT: cluster randomised controlled trial; RCT: randomised controlled trial; STI: sexually transmitted infection; T2D: type 2 diabetes;.
Differences between protocol and review
In our protocol, we only identified broad outcome domains of interest. Before starting data extraction, we decided to prioritise outcomes to make data analysis manageable. Review authors extracted all reported adverse effects and one outcome per the main outcome categories of body function, psychological health, well‐being, and health behaviours. The outcome extraction criteria included: 1) use of a validated measurement tool, 2) author‐reported primary outcomes, 3) used in a sample size calculation, and 4) patient‐important outcome. We applied the same criteria to our secondary outcomes of knowledge, attitudes, motivation and self‐efficacy, and other theory‐based constructs related to behaviour change.
In our analysis, we had planned to only report broad outcomes, however, our knowledge users indicated that disaggregated data by specific outcome would be useful. We therefore reported disaggregated data when there were 10 or more studies reporting on the same broad outcome (e.g. physical activity).
At the protocol stage, we reported that we would not include surrogate biochemical markers, such as haemoglobin. However, when discussing the prioritisation of outcomes with our author team and knowledge users, we decided that HbA1c is an important outcome for diabetic patients and therefore decided to extract and report on it when it met our other extraction criteria, as outlined above. We did not include any other surrogate biochemical markers.
In our protocol, we stated that we would conduct subgroup analyses based on the intensity of the social media intervention. However, we had stated that we would use frequency of interaction as criteria for intensity. Based on discussions with our knowledge users, we decided that this is more of an assessment of adherence to the intervention than a measure of the intensity. We reported this as 'adherence' in our review. Adherence was reported in many ways in our included studies. We decided to combine outcomes of engagement with the interactive social media intervention with adherence outcomes. We classified 'good adherence' as engagement with or adherence to the interactive social media intervention as 70% and higher (70% of participants).
We planned to document and characterise how these interventions aim to change behaviour, using the validated behaviour change techniques taxonomy (BCTTv1), developed by Michie 2013. The BCTTv1 is a comprehensive hierarchy of 93 behaviour change techniques (BCTs). However, we decided to present a detailed summary of the BCTs identified in our studies within a separate paper (Simeon 2020). We plan to explore the moderating effect of BCTs on social media interventions in a separate study.
Contributions of authors
Jennifer Petkovic (JPetkovic), Vivian Welch (VW), Rosiane Simeon (RS), Omar Dewidar (OD), Tamara Rader (TR), Jordi Pardo Pardo (JPP), Jessica Trawin (JT), Stephanie Duench (SD) drafted the review. TR developed the search strategy with the assistance of JPP and MY. Input on the review draft was provided by the advisory group, including Marie Des Meules (MDM), Diane Gagnon (DG), Lisa Hartling (LH), Heather Manson (HM), Janet Hatcher Roberts (JHR), Alomgir Hossain (AH), Justin Presseau (JPresseau), and Peter Tugwell (PT).
Study selection: MY, AS, SD, RS, JT, VW, CC, MT, OD, JV, JPetkovic
Extracting data from studies: MY, AS, JT, SD, OD, MT, RS, VW, JPetkovic
Entering data in RevMan: MY, CC, JT, JO, VW, JPetkovic, SD
Carrying out analysis: VW, JPetkovic, AH
Interpreting analysis: VW, JPP, RS, JPetkovic, JT, JPresseau + advisory group
Drafting final review: VW, RS, JPetkovic, JT
Disagreement resolution: VW, JPetkovic
Updating review: VW, JPetkovic
Sources of support
Internal sources
No sources of support provided
External sources
-
Canadian Institutes for Health Research (CIHR), Canada
Knowledge Synthesis Grant
Declarations of interest
Vivian Welch ‐ VW is the Editor‐in‐Chief of Campbell and the review was co‐registered with Campbell and handled by independent editors. VW received a peer reviewed Canadian Institutes of Health Research grant as principal investigator for this work. The funder had no role in the design of this review.
Jennifer Petkovic ‐ No known conflict of interest.
Rosiane Simeon ‐ No known conflict of interest.
Justin Presseau ‐ No known conflict of interest.
Diane Gagnon ‐ No known conflict of interest.
Alomgir Hossain ‐ No known conflict of interest.
Jordi Pardo Pardo ‐ No known conflict of interest.
Kevin Pottie ‐ No known conflict of interest.
Tamara Rader ‐ No known conflict of interest.
Manosila Yoganathan ‐ No known conflict of interest.
Peter Tugwell ‐ No known conflict of interest.
Marie DesMeules ‐ No known conflict of interest.
Stephanie Duench ‐ No known conflict of interest.
Vivian Welch and Justin Presseau contributed equally to this review
Vivian Welch and Justin Presseau contributed equally to this review
Edited (no change to conclusions)
References
References to studies included in this review
Ahmad 2018 {published data only}
- Ahmad N, Shariff ZM, Mukhtar F, Lye M. Family-based intervention using face-to-face sessions and social media to improve Malay primary school children's adiposity: a randomized controlled field trial of the Malaysian REDUCE programme. Nutrition Journal 2018;17(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahmad 2020 {published data only}
- Ahmad F, El Morr C, Ritvo P, Othman N, Moineddin R, MVC Team. An eight-week, web-based mindfulness virtual community intervention for students' mental health: randomized controlled trial. JMIR Mental Health 2020;7(2):e15520. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ashton 2017 {published data only}
- Ashton LM, Morgan PJ, Hutchesson MJ, Rollo ME, Collins CE. Feasibility and preliminary efficacy of the ‘HEYMAN’ healthy lifestyle program for young men: a pilot randomised controlled trial. Nutrition Journal 2017;16(2):1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bai 2015 {published data only}
- Bai G, Wang Y, Yang L, Niu W. Effectiveness of a focused, brief psychoeducation program for parents of ADHD children: improvement of medication adherence and symptoms. Neuropsychiatric Disease and Treatment 2015;11:2721-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2011 {published data only}
- Baker TB, Hawkins R, Pingree S, Roberts LJ, McDowell HE, Shaw BR, et al. Optimizing eHealth breast cancer interventions: which types of eHealth services are effective? Translational Behavioral Medicine 2011;1:134-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namkoong K, McLaughlin B, Yoo W, Hull SJ, Shah DV, Kim SC, et al. The effects of expression: how providing emotional support online improves cancer patients’ coping strategies. Journal of the National Cancer Institute Monographs 2013;47:169-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bantum 2014 {published data only}
- Bantum E, Albright C, White K, Berenberg J, Layi G, Ritter P, et al. Surviving and thriving with cancer using a web-based health behavior change intervention: randomized controlled trial. Journal of Medical Internet Research 2014;16(2):e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bender 2017 {published data only}
- Bender MS, Cooper B. A feasible and effective mobile health weight loss lifestyle intervention for Filipinos with type 2 diabetes. Circulation 2017;135(Suppl 1):135. [Google Scholar]
- Bender MS, Cooper BA, Park LG, Padash S, Arai S. A feasible and efficacious mobile-phone based lifestyle intervention for Filipino Americans with type 2 diabetes: randomized controlled trial. JMIR Diabetes 2017;2(2):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Booth 2018 {published data only}
- Booth RG, Allen BN, Jenkyn KM, Li L, Shariff SZ. Youth mental health services utilization rates after a large-scale social media campaign: population-based interrupted time-series analysis. Journal of Medical Internet Research 2018;20(4):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyd 2019 {published data only}
- Boyd RC, Price J, Mogul M, Yates T, Guevara JP. Pilot RCT of a social media parenting intervention for postpartum mothers with depression symptoms. Journal of Reproductive and Infant Psychology 2019;37(3):290-301. [DOI] [PubMed] [Google Scholar]
Bull 2012 {published data only}
- Bull S, Levine D, Black S, Schmiege S, Santelli J. Social media–delivered sexual health intervention: a cluster randomized controlled trial. American Journal of Preventive Medicine 2012;43(5):467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castillo 2013 {published data only}
- Bradford AN, Castillo RC, Carlini AR, Wegener ST, Teter H, Mackenzie EJ. The trauma survivors network: Survive. Connect. Rebuild. Journal of Trauma: Injury, Infection, and Critical Care 2011;70(6):1557–60. [DOI] [PubMed] [Google Scholar]
- Castillo R, Wegener S, Newell M, Carlini A, Bradford A, Heins S, et al. Improving outcomes at level I trauma centers: an early evaluation of the trauma survivors network. Journal of Trauma and Acute Care Surgery 2013;74(6):1534-40. [DOI] [PubMed] [Google Scholar]
Cavalcanti 2019 {published data only}
- Cavalcanti DS, Cabral CS, Toledo Vianna RP, Osorio MM. Online participatory intervention to promote and support exclusive breastfeeding: randomized clinical trial. Maternal & Child Nutrition 2019;15(3):e12806. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cavallo 2012 {published data only}
- Cavallo DN, Jane D, Brown JD, Tate DF, DeVellis RF, Zimmer C, et al. The role of companionship, esteem, and informational support in explaining physical activity among young women in an online social network intervention. Journal of Behavioral Medicine 2014;37:955–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo DN, Tate DF, Ries AV, Brown JD, DeVellis RF, Ammerman AS. A social media–based physical activity intervention: a randomized controlled trial. American Journal of Preventive Medicine 2012;43(5):527–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo DN, Tate DF, Ward DS, DeVellis RF, Thayer LM, Ammerman AS. Social support for physical activity—role of Facebook with and without structured intervention. Translational Behavioral Medicine 2014;4:346–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo DN. Using Online Social Network Technology to Increase Social Support for Physical Activity:the Internet Support For Healthy Associations Promoting Exercise (inshape) Study. University of North Carolina at Chapel Hill, Department of Nutrition 2012.
Chai 2018 {published data only}
- Chai W, Zou G, Shi J, Chen W, Gong X, Wei X, et al. Evaluation of the effectiveness of a WHO5A model based comprehensive tobacco control program among migrant workers in Guangdong, China: a pilot study. BMC Public Health 2018;18(1):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2019 {published data only}
- Chen X, Jiang S, Xu Y, Tian Y. The effect of interactive health education based on the WeChat platform on diabetic outpatients. International Journal of Clinical and Experimental Medicine 2019;12(11):13154-62. [Google Scholar]
Cheung 2015 {published data only}
- Cheung YT, Chan CH, Lai CJ, Chan WV, Wang MP, William Li HC, et al. Using WhatsApp and Facebook online social groups for smoking relapse prevention for recent quitters: a pilot pragmatic cluster randomized controlled trial. Journal of Medical Internet Research 2015;17(10):e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cobb 2014 {published data only}
- Cobb NK, Poirier J. Effectiveness of a multimodal online well-being intervention: a randomized controlled trial. American Journal of Preventive Medicine 2014;46(1):41–8. [DOI] [PubMed] [Google Scholar]
Coffeng 2014 {published data only}
- Coffeng JK, Boot CR, Duijts SF, Twisk JW, Mechelen W, Hendriksen IJ. Effectiveness of a worksite social & physical environment intervention on need for recovery, physical activity and relaxation; results of a randomized controlled trial. PLOS One 2014;9(12):e114860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffeng JK, Hendriksen IJ, Duijts SF, Proper KI, Mechelen W, Boot CR. The development of the Be Active & Relax “Vitality in Practice” (VIP) project and design of an RCT to reduce the need for recovery in office employees. BMC Public Health 2012;12:592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffeng JK, Sluijs EM, Hendriksen IJ, Mechelen W, Boot CR. Physical activity and relaxation during and after work are independently associated with the need for recovery. Journal of Physical Activity and Health 2015;12:109-15. [DOI] [PubMed] [Google Scholar]
Dadkhah 2014 {published data only}
- Dadkhah M. Development and Evaluation of the America On the Move Program For University Students. Colorado State University, Department of Food Science and Human Nutrition 2013.
Dahl 2019 {published data only}
- Dahl AA. Healthy motivations for moms-to-be (healthy mom2b) study: a mobile health intervention targeting gestational weight gain among U.S. women. Dissertation Abstracts International: Section B: The Sciences and Engineering 2019;80(2-B(E)):1. [Google Scholar]
Daly 2017 {published data only}
- Daly N, Farren M, McKeating A, O'Kelly R, Stapleton M, Turner MJ. A medically supervised pregnancy exercise intervention on obese women. Obstetrics & Gynecology 2017;130(5):1001-10. [DOI] [PubMed] [Google Scholar]
Dehlendorf 2020 {published data only}
- Dehlendorf C, Fox E, Sharma AE, Zhang J, Tang S, Centola D. Birth Control Connect: a randomized trial of an online group to disseminate contraceptive information. Contraception 2020;101(6):376-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duncan 2014 {published and unpublished data}
- Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, George ES, et al. Effectiveness of a web- and mobile phone-based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. Journal of Medical Internet Research 2014;16(6):e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan MJ, Vandelanotte C, Rosenkranz RR, Caperchione CM, Ding H, Ellison M, et al. Effectiveness of a website and mobile phone based physical activity and nutrition intervention for middle-aged males: trial protocol and baseline findings of the ManUp study. BMC Public Health 2012;12:656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short CE, Vandelanotte C, Dixon MW, Rosenkranz R, Caperchione C, Hooker C, et al. Examining participant engagement in an information technology-based physical activity and nutrition intervention for men: the ManUp randomized controlled trial. JMIR Research Protocols 2014;3(1):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edney 2020 {published data only}
- Edney S, Plotnikoff R, Vandelanotte C, Olds Y, De Bourdeauhuij I, Ryan J, et al. "Active Team" a social and gamified app-based physical activity intervention: randomised controlled trial study protocol. BMC Public Health 2017;17(1):859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edney SM, Olds TS, Ryan JC, Vandelanotte C, Plotnikoff RC, Curtis RG, et al. A social networking and gamified app to increase physical activity: cluster RCT. American Journal of Preventive Medicine 2020;58(2):e51-62. [DOI] [PubMed] [Google Scholar]
Fiks 2017 {published data only}
- Fiks AG, Gruver RS, Bishop-Gilyard CT, Shults J, Virudachalam S, Suh AW, et al. A social media peer group for mothers to prevent obesity from infancy: the Grow2Gether randomized trial. Childhood Obesity 2017;13(5):356-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
George 2013 {published data only}
- George DR, Dellasega C, Whitehead MM, Bordon A. Facebook-based stress management resources for first-year medical students: a multi-method evaluation. Computers in Human Behavior 2013;29:559-62. [Google Scholar]
Glanz 2017 {published data only}
- Daley MF, Narwaney KJ, Shoup JA, Wagner NM, Glanz JM. Addressing parents’ vaccine concerns: a randomized trial of a social media intervention. American Journal of Preventive Medicine 2018;55(1):44-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz JM, Wagner NM, Narwaney KJ, Kraus CR, Shoup JA, Xu S, et al. Web-based social media intervention to increase vaccine acceptance: a randomized controlled trial. Pediatrics 2017;140(6):e20171117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary S, Wagner N, Narwaney K, Kraus C, Shoup JA, Xu S, et al. Effectiveness of a web-based intervention to increase uptake of maternal vaccines. Open Forum Infectious Diseases 2017;4(suppl 1):s457. [Google Scholar]
- O'Leary S, Wagner N, Narwaney K, Kraus C, Shoup JA, Xu S, et al. Efficacy of a web-based intervention to increase uptake of maternal vaccines: an RCT. American Journal of Preventive Medicine 2019;57(4):e125-e133. [DOI] [PubMed] [Google Scholar]
Gnagnarella 2016 {published data only}
- Gnagnarella P, Misotti AM, Santoro L, Akoumianakis D, Campo LD, De Lorenzo F, et al. Nutritional online information for cancer patients: a randomized trial of an Internet communication plus social media intervention. Journal of Cancer Education 2016;31:472-80. [DOI] [PubMed] [Google Scholar]
- Gnagnarella P, Misotti AM, Santoro L, Akoumianakis D, Milolidakis G, De Lorenzo F, et al. A dedicated website for cancer subjects, the nutritional support study: preliminary results. Ecancermedicalscience 2011;5:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Godino 2016 {published data only}
- Godino JG, Merchant G, Norman GJ, Donohue MC, Marshall SJ, Fowler JH, et al. Using social and mobile tools for weight loss in overweight and obese young adults (project SMART): a 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes & Endocrinology 2016;4:747-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merchant G, Weibel N, Pina L, Griswold WG, Fowler JH, Ayala GX, et al. Face-to-face and online networks: college students’ experiences in a weight-loss trial. Journal of Health Communication 2017;22(1):75-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K, Marshall SJ, Davila EP, Kolodziejczyk JK, Fowler J, Calfas KJ, et al. Design and implementation of a randomized controlled social and mobile weight loss trial for young adults (project SMART). Contemporary Clinical Trials 2014;37(1):10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Graham 2011 {published data only}
- Graham AL, Cobb NK, Papandonatos GD, Moreno JL, Kang H, Tinkelman DG, et al. A randomized trial of Internet and telephone treatment for smoking cessation. Archives of Internal Medicine 2011;171(1):46-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Papandonatos GD, Cobb CO, Cobb NK, Niaura RS, Abrams DB, et al. Internet and telephone treatment for smoking cessation: mediators and moderators of short-term abstinence. Nicotine & Tobacco Research 2015;17(3):299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Papandonatos GD, Erar B, Stanton CA. Use of an online smoking cessation community promotes abstinence: results of propensity score weighting. Health Psychology 2015;34:1286–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Stanton CA, Papandonatos GD, Erar B. Online community use predicts abstinence in combined Internet/phone intervention for smoking cessation. Journal of Consulting and Clinical Psychology 2016;84(7):633– 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Graham 2018 {published data only}
- Cha S, Erar B, Niaura RS, Graham AL. Baseline characteristics and generalizability of participants in an Internet smoking cessation randomized trial. Annals of Behavioral Medicine 2016;50(5):751-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Cha S, Cobb NK, Fang Y, Niaura RS, Mushro A. Impact of seasonability on recruitment, retention, adherence, and outcomes in a web-based smoking cessation intervention: randomized controlled trial. Journal of Medical Internet Research 2013;15(11):e249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Cha S, Papadonatos GD, Cobb NK, Mushro A, Fang Y, et al. Improving adherence to web-based cessation programs: a randomized controlled trial study protocol. Trials 2013;14:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Papandonatos GD, Cha S, Erar B, Amato MS. Improving adherence to smoking cessation treatment: smoking outcomes in a web-based randomized trial. Annals of Behavioral Medicine 2018;52(4):331-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Zhao K, Papadonatos GD, Erar B, Wang X, Amato MS, et al. A prospective examination of online social network dynamics and smoking cessation. PLOS One 2017;12(8):e0183655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson JL, Amato MS, Papandonatos GD, Zhao K, Erar B, Wang X, et al. Exposure to positive peer sentiment about nicotine replacement therapy in an online smoking cessation community is associated with NRT use. Addictive Behaviors 2018;87:36-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao K, Wang X, Cha S, Cohn AM, Papadonatos GD, Amato MS, et al. A multirelational social network analysis of an online health community for smoking cessation. Journal of Medical Internet Research 2016;18(8):e233. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greene 2013 {published and unpublished data}
- Greene J, Sacks R, Piniewski B, Kil D, Hahn JS. The impact of an online social network with wireless monitoring devices on physical activity and weight loss. Journal of Primary Care & Community Health 2013;4(3):189-94. [DOI] [PubMed] [Google Scholar]
Hammersley 2019 {published data only}
- Hammersley ML, Jones RA, Okely AD, Jones RA. An Internet-Based Childhood Obesity Prevention Program (Time2bHealthy) for Parents of Preschool-Aged Children: Randomized Controlled Trial. J Med Internet Res 2019;21(2):e11964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammersley ML, Jones RA, Okely AD. Time2bHealhy - an online childhood obesity prevention program for preschool-aged children: a randomised controlled trial protocol. Contemporary Clinical Trials 2017;61:73-80. [DOI] [PubMed] [Google Scholar]
Herring 2014 {published data only}
- Herring SJ, Cruice JF, Bennett GG, Davey A, Foster GD. Using technology to promote postpartum weight loss in urban, low-income mothers: a pilot randomized controlled trial. Journal of Nutrition Education and Behavior 2014;46(6):610-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Herring 2017 {published data only}
- Herring SJ, Cruice JF, Bennett GG, Darden N, Wallen JJ, Rose MZ, et al. Intervening during and after pregnancy to prevent weight retention among African American women. Preventive Medicine Reports 2017;7:119-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Horvath 2013 {published data only}
- Horvath KJ, Oakes JM, Rosser BR, Danilenko G, Vezina H, Amico KR, et al. Feasibility, acceptability and preliminary efficacy of an online peer-to-peer social support ART adherence intervention. AIDS and Behavior 2013;17(6):2031–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hutchesson 2018 {published data only}
- Hutchesson MJ, Calister R, Mogan PJ, Pranata I, Clarke ED, Skinner G, et al. A targeted and tailored eHealth weight loss program for young women: the Be Positive Be Healthe randomized controlled trial. Healthcare 2018;6(2):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hwang 2013 {published data only}
- Hwang KO, Ottenbacher AJ, Graham AL, Thomas EJ, Street RL, Vernon SW. Online narratives and peer support for colorectal cancer screening: a pilot randomized trial. American Journal of Preventive Medicine 2013;45(1):98–107. [DOI] [PubMed] [Google Scholar]
Jane 2017 {published data only}
- Jane M, Foster J, Hagger M, Ho S, Kane R, Pal S. Psychological effects of belonging to a Facebook weight management group in overweight and obese adults: results of a randomised controlled trial. Health & Social Care in the Community 2018;May:10.1111/hsc.12584. [DOI] [PubMed] [Google Scholar]
- Jane M, Foster J, Hagger M, Pal S. Using new technologies to promote weight management: a randomised controlled trial study protocol. BMC Public Health 2015;15:509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jane M, Hagger M, Foster J, Ho S, Kane R, Pal S. Effects of a weight management program delivered by social media on weight and metabolic syndrome risk factors in overweight and obese adults: a randomised controlled trial. PLoS One 2017;12(6):e0178326. [DOI] [PMC free article] [PubMed] [Google Scholar]
Joseph 2015 {published data only}
- Joseph RP, Keller C, Adams MA, Ainsworth BE. Print versus a culturally-relevant Facebook and text message delivered intervention to promote physical activity in African American women: a randomized pilot trial. BMC Women's Health 2015;15:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kernot 2019 {published data only}
- Kernot J, Lewis L, Olds T, Maher C. Effectiveness of a Facebook-delivered physical activity intervention for postpartum women: a randomized controlled trial. Journal of Physical Activity and Health 2019;16(2):125-33. [DOI] [PubMed] [Google Scholar]
- Kernot J, Olds T, Lewis LK, Maher C. Effectiveness of a Facebook-delivered physical activity intervention for post-partum women: a randomized controlled trial protocol. BMC Public Health 2013;13:518. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2019 {published data only}
- Kim SH, Utz S. Effectiveness of a social media-based, health literacy-sensitive diabetes self-management intervention: a randomized controlled trial. Journal of Nursing Scholarship 2019;Oct 17:661-9. [DOI] [PubMed] [Google Scholar]
Kolt 2017 {published data only}
- Alley SJ, Kolt GS, Caperchione CM, Savage TN, Maeder AJ, Rosenkranz RR, et al. The effectiveness of a web 2.0 physical activity intervention in older adults – a randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2018;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alley SJ, Kolt GS, Duncan MJ, Caperchione CM, Savage TN, Maeder AJ, et al. The effectiveness of a web 2.0 physical activity intervention in older adults – a randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2018;15(4):e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caperchione CM, Duncan MJ, Rosenkranz RR, Vandelanotte C, Van Itallie AK, Savage TN, et al. Recruitment, screening, and baseline participant characteristics in the WALK 2.0 study: a randomized controlled trial using web 2.0 applications to promote physical activity. Contemporary Clinical Trials Communications 2016;2:25-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolt GS, George ES, Rebar AL, Duncan MJ, Vandelanotte C, Caperchione CM, et al. Associations between quality of life and duration and frequency of physical activity and sedentary behaviour: baseline findings from the WALK 2.0 randomised controlled trial. PLOS One 2017;12(6):e0180072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolt GS, Rosenkranz RR, Savage TN, Maeder AJ, Vandelanotte C, Duncan MJ, et al. WALK 2.0 - using Web 2.0 applications to promote health-related physical activity: a randomised controlled trial protocol. BMC Public Health 2013;13:436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolt GS, Rosenkranz RR, Vandelanotte C, Caperchione CM, Maeder AJ, Tague R, et al. Using Web 2.0 applications to promote health-related physical activity: findings from the WALK 2.0 randomised controlled trial. British Journal of Sports Medicine 2017;51:1433–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koufopoulos 2016 {published data only}
- Koufopoulos JT, Conner MT, Gardner PH, Kellar I. A web-based and mobile health social support intervention to promote adherence to inhaled asthma medications: randomized controlled trial. Journal of Medical Internet Research 2016;18(6):e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lau 2012 {published data only}
- Lau AY, Sintchenko V, Crimmins J, Magrabi F, Gallego B, Coiera E. Impact of a web-based personally controlled health management system on influenza vaccination and health services utilization rates: a randomized controlled trial. Journal of the American Medical Informatics Association 2012;19:719-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau AY, Sintchenko V, Crimmins J, Magrabi F, Gallego B, Coiera E. Protocol for a randomised controlled trial examining the impact of a web-based personally controlled health management system on the uptake of influenza vaccination rates. BMC Health Services Research 2012;12:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2017 {published data only}
- Li J. A randomized controlled study to evaluate the efficacy of a positive psychology and social networking intervention in reducing depressive symptoms among HIV-infected men who have sex with men in China. Dissertation Abstracts International: Section B: The Sciences and Engineering 2017;77(9-B(E)).
Li 2020 {published data only}
- Li C, Tang L, Yang M, Lin Y, Liu C, Liu Y, et al. A study to evaluate the efficacy of different interventions for improving quality of maternal health care service in China. Telemedicine Journal and e-Health 2020;Jan 13:doi: 10.1089.tmj.2019.0230. [DOI] [PubMed] [Google Scholar]
Liao 2020 {published data only}
- Liao Q, Fielding R, Cheung YT, Lian J, Yuan J, Lam WW. Effectiveness and parental acceptability of social networking interventions for promoting seasonal influenza vaccination among young children: randomized controlled trial. Journal of Medical Internet Research 2020;22(2):e16427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linden 2017 {published data only}
- Adolfsson A, Linden K, Sparud-Lundin C, Larsson P, Berg M. A web-based support for pregnant women and new mothers with type 1 diabetes mellitus in Sweden (MODIAB-Web): study protocol for a randomized controlled trial. Trials 2014;15:513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden K, Berg M, Adolfsson A, Sparud-Lundin C. Person-centred, web-based support in pregnancy and early motherhood for women with type 1 diabetes mellitus: a randomized controlled trial. Diabetic Medicine 2017;35:232-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden K, Sparud-Lundin C, Adolfsson A, Berg M. Well-being and diabetes management in early pregnant women with type 1 diabetes mellitus. International Journal of Environmental Research and Public Health 2016;13:836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Looyestyn 2018 {published data only}
- Edney S, Looyestyn J, Ryan J, Kernot J, Maher C. Posts, pics, or polls? Which post type generates the greatest engagement in a Facebook physical activity intervention? Translational Behavioral Medicine 2018;8:953-7. [DOI] [PubMed] [Google Scholar]
- Looyestyn J, Kernot J, Boshoff K, Maher C. A web-based, social networking beginners’ running intervention for adults aged 18 to 50 years delivered via a Facebook group: randomized controlled trial. Journal of Medical Internet Research 2018;20(2):e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lytle 2017 {published data only}
- Laska MN, Lytle LA, Nanney MS, Moe SG, Linde JA, Hannan PJ. Results of a 2-year randomized, controlled obesity prevention trial: effects on diet, activity and sleep behaviors in an at-risk young adult population. Preventive Medicine 2016;89:230-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Laska MN, Linde JA, Moe SG, Nanney MS, Hannan PJ, et al. Weight gain reduction among 2-year college students: The CHOICES RCT. American Journal of Preventive Medicine 2017;52(2):183–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Moe SG, Nanney MS, Laska MN, Linde JA, Petrich CA, et al. Designing a weight gain prevention trial for young adults: the CHOICES study. American Journal of Health Education 2014;45:67-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maher 2015 {published data only}
- Maher C, Ferguson M, Vandelanotte C, Plotnikoff R, De Bourdeaudhuij I, Thomas S, et al. A web-based, social networking physical activity intervention for insufficiently active adults delivered via Facebook app: randomized controlled trial. Journal of Medical Internet Research 2015;17(7):e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mailey 2016 {published data only}
- Mailey EL, Huberty J, Irwin BC. Feasibility and effectiveness of a web-based physical activity intervention for working mothers. Journal of Physical Activity and Health 2016;13:822-9. [DOI] [PubMed] [Google Scholar]
Mascarenhas 2018 {published data only}
- Mascarenhas MN, Chan JM, Vittinghoff E, Blarigan EL, Hecht F. Increasing physical activity in mothers using video exercise groups and exercise mobile apps: randomized controlled trial.. Journal of Medical Internet Research 2018;20(5):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2015 {published data only}
- Morris RR, Schueller SM, Picard RW. Efficacy of a web-based, crowdsourced peer-to-peer cognitive reappraisal platform for depression: randomized controlled trial. Journal of Medical Internet Research 2015;17(3):e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moy 2010 {published data only}
- Moy ML, Janney AW, Nguyen HQ, Matthess KR, Cohen M, Garshick E, et al. Use of pedometer and Internet-mediated walking program in patients with chronic obstructive pulmonary disease. Journal of Rehabilitation Research and Development 2010;47(5):485-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moy 2015 {published data only}
- Martinez CH, Moy ML, Nguyen HQ, Cohen M, Kadri R, Roman P, et al. Taking healthy steps: rationale, design and baseline characteristics of a randomized trial of a pedometer-based Internet-mediated walking program in veterans with chronic obstructive pulmonary disease. BMC Pulmonary Medicine 2014;14:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy ML, Collins RJ, Martinez CH, Kadri R, Roman P, Holleman RG, et al. An Internet-mediated pedometer-based program improves health-related quality-of-life domains and daily step counts in COPD: a randomized controlled trial. CHEST 2015;148(1):128-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy ML, Martinez CH, Kadri R, Roman P, Holleman RG, Kim HM, et al. Long-term effects of an Internet-mediated pedometer-based walking program for chronic obstructive pulmonary disease: randomized controlled trial. Journal of Medical Internet Research 2016;18(8):e215. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nam 2015 {published data only}
- Nam Y. The effect of Twitter social support on health outcomes and its mediators: a randomized controlled trial of a social support intervention on Twitter for patients affected by cancer. University of Southern California 2015:1-120.
Nam 2020 {published data only}
- Nam SJ, Cha C. Effects of a social-media-based support on premenstrual syndrome and physical activity among female university students in South Korea. Journal of Psychosomatic Obstetrics & Gynecology 2020;41(1):47-53. [DOI] [PubMed] [Google Scholar]
Namkoong 2017 {published data only}
- Namkoong K, Nah S, Record RA, Van Stee SK. Communication, reasoning, and planned behaviors: unveiling the effect of interactive communication in an anti-smoking social media campaign. Health Communication 2017;32(1):41-50. [DOI] [PubMed] [Google Scholar]
Napolitano 2013 {published data only}
- Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity 2013;21(1):25-31. [DOI] [PubMed] [Google Scholar]
O'Neil 2016 {published data only}
- O’Neil PM, Miller-Kovach K, Tuerk PW, Becker LE, Wadden TA, Fujioka K, et al. Randomized controlled trial of a nationally available weight control program tailored for adults with type 2 diabetes. Obesity 2016;24(11):2269-77. [DOI] [PubMed] [Google Scholar]
Owen 2015 {published data only}
- Owen JE, Bantum EO, Criswell K, Stanton AL. Characterizing patterns of engagement with a social-networking intervention to treat cancer-related distress. Asia-Pacific Journal of Clinical Oncology 2012;8(3):142-3. [Google Scholar]
- Owen JE, Bantum EO, Gorlick A, Annette L, Stanton AL. Engagement with a social networking intervention for cancer-related distress. Annals of Behavioral Medicine 2015;49:154–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen JE, Bantum EO, Pagano IS, Stanton A. Randomized trial of a social networking intervention for cancer-related distress. Annals of Behavioral Medicine 2017;51:661–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petrella 2017 {published data only}
- Blunt W, Gill DP, Sibbald SL, Riggin B, Pulford RW, Scott R, et al. Optimization of the Hockey Fans in Training (Hockey FIT) weight loss and healthy lifestyle program for male hockey fans. BMC Public Health 2017;17(1):916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill DP, Blunt W, De Cruz A, Riggin B, Hunt K, Zou G, et al. Hockey Fans in Training (Hockey FIT) pilot study protocol: a gender-sensitized weight loss and healthy lifestyle program for overweight and obese male hockey fans. BMC Public Health 2016;16(1):1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrella RJ, Gill DP, Zou G, Cruz AD, Riggin B, Bartol C, et al. Hockey Fans in Training: a pilot pragmatic randomized controlled trial. Medicine & Science in Sports & Exercise 2017;49(12):2506–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramo 2015 {published data only}
- Ramo DE, Thrul J, Chavez K, Delucchi KL, Prochaska JJ. Feasibility and quit rates of the Tobacco Status Project: a Facebook smoking cessation intervention for young adults. Journal of Medical Internet Research 2015;17(12):e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramo 2018b {published data only}
- McKelvey K, Ramo D. Conversation within a Facebook smoking cessation intervention trial for young adults (Tobacco Status Project): qualitative analysis. JMIR Formative Research 2018;2(2):e11138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo D, Thrul J, Delucchi K, Hall SM, Ling P, Belohlavek A, et al. The Tobacco Status Project: three month outcomes for a randomized controlled trial of a Facebook smoking cessation intervention for young adults. Drug and Alcohol Dependence 2017;171:e2-226. [Google Scholar]
- Ramo DE, Thrul J, Delucchi KL, Hall S, Ling PM, Belohlavek A, et al. A randomized controlled evaluation of the Tobacco Status Project, a Facebook intervention for young adults. Addiction 2018;Nov 24:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Thrul J, Delucchi KL, Ling PM, Hall SM, Prochaska JJ. The Tobacco Status Project (TSP): study protocol for a randomized controlled trial of a Facebook smoking cessation intervention for young adults. BMC Public Health 2015;15:897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrul J, Meacham MC, Tice C, Kelly O, Ramo DE. Live counselor contact in a Facebook intervention predicts smoking cessation outcomes. Psychology of Addictive Behaviors 2020;34(2):360-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel EA, Ramo DE. Smoking cessation, metabolic risk behaviors, and stress management over time in a sample of young adult smokers. Translational Behavioral Medicine 2019;Oct 9:ibz139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel EA, Thrul J, Humfleet GL, Delucchi KL, Ramo DE. Smoking cessation intervention trial outcomes for sexual and gender minority young adults. Health Psychology 2018;38(1):12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ren 2019 {published data only}
- Ren Q, Lian M, Liu Y, Thomas-Hawkins C, Zhu L, Shen Q. Effects of a transtheoretical model‐based WeChat health education programme on self‐management among haemodialysis patients: a longitudinal experimental intervention study.. Journal of Advanced Nursing 2019;75(12):3554-65. [DOI] [PubMed] [Google Scholar]
Richardson 2010 {published data only}
- Richardson CR, Buis LR, Janney AW, Goodrich DE, Sen A, Hess ML, et al. An online community improves adherence in an Internet-mediated walking program. Part 1: results of a randomized controlled trial. Journal of Medical Internet Research 2010;12(4):e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rote 2015 {published data only}
- Rote AE, Klos LA, Brondino MJ, Harley AE, Swartz AM. The efficacy of a walking intervention using social media to increase physical activity: a randomized trial. Journal of Physical Activity and Health 2015;12(1):S18-S25. [DOI] [PubMed] [Google Scholar]
- Rote AE. Examining the efficacy of a Facebook-mediated intervention to increase steps per day in college freshmen. University of Wisconsin Milwaukee - UWM Digital Commons, Theses and Dissertations August 2013.
Rouf 2020 {published data only}
- Rouf A, Nour M, Allman-Farinelli M. Improving calcium knowledge and intake in young adults via social media and text messages: randomized controlled trial. JMIR mHealth and uHealth 2020;8(2):e16499. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rovniak 2016 {published data only}
- Rovniak LS, Lan Kong L, Hovell MF, Ding D, Sallis JF, Ray CA, et al. Engineering online and in-person social networks for physical activity: a randomized trial. Annals of Behavioral Medicine 2016;50(6):885-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovniak LS, Sallis JF, Kraschnewski JL, Sciamanna CN, Kiser EJ, Ray CA, et al. Engineering online and in-person social networks to sustain physical activity: application of a conceptual model. BMC Public Health 2013;13:753. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schaller 2017 {published data only}
- Schaller A, Dintsios C, Icks A, Reibling N, Froboese I. Promoting physical activity in low back pain patients: six months follow-up of a randomised controlled trial comparing a multicomponent intervention with a low intensity intervention. Clinical Rehabilitation 2016;30(9):865-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller A, Froboese I. Movement Coaching: study protocol of a randomized controlled trial evaluating effects on physical activity and participation in low back pain patients. BMC Musculoskeletal Disorders 2014;15:391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller A, Petrowski K, Pfoertner T, Froboese I. Effectiveness of a theory-based multicomponent intervention (Movement Coaching) on the promotion of total and domain-specific physical activity: a randomised controlled trial in low back pain patients. BMC Musculoskeletal Disorders 2017;18(1):431. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schneider 2015 {published data only}
- Schneider KL, Murphy D, Ferrara C, Oleski J, Panza E, Savage C, et al. An online social network to increase walking in dog owners: a randomized trial. Medicine & Science in Sports & Exercise 2015;47(3):631-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stoddard 2008 {published data only}
- Stoddard JL, Augustson EM, Moser RP. Effect of adding a virtual community (bulletin board) to Smokefree.gov: randomized controlled trial. Journal of Medical Internet Research 2008;10(5):e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2017 {published data only}
- Sun WH, Wong CH, Wong WC. A peer-led, social media-delivered, safer sex intervention for Chinese college students: randomized controlled trial. Journal of Medical Internet Research 2017;19(8):e284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner‐McGrievy 2011 {published data only}
- Turner-McGrievy G, Tate D. Tweets, apps, and pods: results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. Journal of Medical Internet Research 2011;13(4):e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valle 2013 {published data only}
- Valle CG, Tate DF, Mayer DK, Allicock M, Cai J. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. Journal of Cancer Survivorship 2013;7:355-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valle CG, Tate DF, Mayer DK, Allicock M, Cai J. Exploring mediators of physical activity in young adult cancer survivors: evidence from a randomized trial of a Facebook-based physical activity intervention. Journal of Adolescent and Young Adult Oncology 2015;4(1):26-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valle CG, Tate DF. Engagement of young adult cancer survivors within a Facebook-based physical activity intervention. Translational Behavioral Medicine 2017;7:667–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valle CG. Examining the use of online social networking to improve physical activity behaviours among young adult cancer survivors. University of North Carolina at Chapel Hill, Department of Nutrition. 2012.
Vandelanotte 2017 {published data only}
- Caperchione CM, Kolt GS, Savage TN, Rosenkranz RR, Maeder AJ, Vandelanotte C, et al. WALK 2.0: examining the effectiveness of Web 2.0 features to increase physical activity in a ‘real world’ setting: an ecological trial protocol. BMJ Open 2014;4:e006374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandelanotte C, Kolt G, Caperchione C, Savage T, Rosenkranz R, Maeder A, et al. Effectiveness of a Web 2.0 intervention to increase physical activity in real-world settings: randomized ecological trial. Journal of Medical Internet Research 2017;19(11):e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vogel 2019 {published data only}
- Vogel EA, Ramo DE, Meacham MC, Prochaska JJ, Delucchi KL, Humfleet GL. The Put It Out Project (POP) Facebook intervention for young sexual and gender minority smokers: outcomes of a pilot randomized controlled trial. Nicotine and Tobacco Research 2019;22(9):1614-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wan 2017 {published data only}
- Robinson SA, Shimada SL, Quigley KS, Moy ML. A web-based physical activity intervention benefits persons with low self-efficacy in COPD: results from a randomized controlled trial. Journal of Behavioral Medicine 2019;42:1082-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan ES, Kantorowski A, Homsy D, Teylan M, Kadri R, Richardson CR, et al. Promoting physical activity in COPD: insights from a randomized trial of a web-based intervention and pedometer use. Respiratory Medicine 2017;130:102-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Wang JC, Leng HK, Kee YH. Use of Facebook in physical activity intervention programme: a test of self determination theory. International Journal of Sport Psychology 2015;46(3):210-24. [Google Scholar]
Washington 2017 {published data only}
- Washington TA, Applewhite S, Glenn W. Using Facebook as a platform to direct young Black men who have sex with men to a video-based HIV testing intervention: a feasibility study. Urban Social Work 2017;1(1):36-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Willcox 2017 {published data only}
- Willcox JC, Campbell KJ, McCarthy EA, Wilkinson SA, Lappas M, Ball K, et al. Testing the feasibility of a mobile technology intervention promoting healthy gestational weight gain in pregnant women (txt4two) - study protocol for a randomised controlled trial. Trials 2015;16:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcox JC, Wilkinson SA, Lappas M, Ball K, Crawford D, McCarthy EA, et al. A mobile health intervention promoting healthy gestational weight gain for women entering pregnancy at a high body mass index: the txt4two pilot randomised controlled trial. BJOG 2017;124(11):1718-28. [DOI] [PubMed] [Google Scholar]
Willis 2017 {published data only}
- Willis EA, Szabo-Reed AN, Ptomey LT, Steger FL, Honas JJ, Al-Hihi EM, et al. Distance learning strategies for weight management utilizing online social networks versus group phone conference call. Obesity Science & Practice 2017;3(2):134-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis EA, Szabo-Reed AN, Ptomey LT, Steger FL, Honas JJ, Al-Hihi EM, et al. Distance learning strategies for weight management utilizing social media: a comparison of phone conference call versus social media platform. Rationale and design for a randomized study. Contemporary Clinical Trials 2016;47:282–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2019 {published data only}
- Yang M, Jia G, Sun S, Ye C, Zhang R, Yu X. Effects of an online mindfulness intervention focusing on attention monitoring and acceptance in pregnant women: a randomized controlled trial. Journal of Midwifery & Women's Health 2019;64(1):68-77. [DOI] [PubMed] [Google Scholar]
Young 2013 {published data only}
- Young SD, Cumberland WG, Lee S, Jaganath D, Szekeres G, Coates T. Social networking technologies as emerging tools for HIV prevention: a cluster randomized trial. Annals of Internal Medicine 2013;159(5):318-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SD, Holloway I, Jaganath D, Rice E, Westmoreland D, Coates T. Project HOPE: online social network changes in an HIV prevention randomized controlled trial for African American and Latino men who have sex with men. American Journal of Public Health 2014;104(9):1707-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SD, Jaganath D. Feasibility of using social networking technologies for health research among men who have sex with men: a mixed methods study. American Journal of Men's Health 2014;8(1):6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2015 {published data only}
- Young SD, Cumberland WG, Nianogo R, Menacho LA, Galea JT, Coates T. The HOPE social media intervention for global HIV prevention: a cluster randomized controlled trial in Peru. Lancet HIV 2015;2(1):e27–e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2016 {published data only}
- Zhang J, Brackbill D, Yang S, Becker J, Herbert N, Centola D. Support or competition? How online social networks increase physical activity: a randomized controlled trial. Preventive Medicine Reports 2016;4:453-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Brackbill D, Yang S, Centola D. Efficacy and causal mechanism of an online social media intervention to increase physical activity: results of a randomized controlled trial. Preventive Medicine Reports 2015;2:651–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Aiello 2015 {published data only}
- Aiello CP, Ferrari DV. Teleaudiology: efficacy assessment of an online social network as a support tool for parents of children candidates for cochlear implant. Codas 2015;27(5):411-8. [DOI] [PubMed] [Google Scholar]
Al‐Eisa 2016 {published data only}
- Al-Eisa E, Al-Rushud A, Alghadir A, Anwer S, Al-Harbi B, Al-Sughaier N, et al. Effect of motivation by "Instagram" on adherence to physical activity among female college students. BioMed Research International 2016;2016:1546013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Allman‐Farinelli 2016 {published data only}
- Allman-Farinelli M, Partridge SR, McGeechan K, Balestracci K, Hebden L, Wong A, et al. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): nine month outcomes of a randomized controlled trial. JMIR Mhealth Uhealth 2016;4(2):e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebden L, Balestraci K, McGeechan K, Denney-Wilson E, Harris M, Bauman A, et al. 'TXT2BFiT' a mobile phone-based healthy lifestyle program for preventing unhealthy weight gain in young adults: study protocol for a randomized controlled trial. Trials 2013;14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partridge SR, McGeechan K, Hebden L, Balestraci K, Wong AT, Denney-Wilson E, et al. Effectiveness of a mhealth lifestyle program with telephone support (TXT2BFiT) to prevent unhealthy weight gain in young adults: a randomized controlled trial. JMIR Mhealth and Uhealth 2015;3(2):e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bragadottir 2008 {published data only}
- Bragadottir H. Computer-mediated support group intervention for parents. Journal of Nursing Scholarship 2008;40(1):32-8. [DOI] [PubMed] [Google Scholar]
Bramlett Mayer 2012 {published data only}
- Bramlett Mayer A, Harrison J. Safe Eats: an evaluation of the use of social media for food safety education. Journal of Food Protection 2012;75(8):1453–63. [DOI] [PubMed] [Google Scholar]
Brosseau 2015 {published data only}
- Brosseau L, Wells G, Brooks-Lineker S, Bennell K, Sherrington C, Briggs A, et al. Internet-based implementation of non-pharmacological interventions of the "People Getting a Grip on Arthritis" educational program: an international online knowledge translation randomized controlled trial design protocol. JMIR Research Protocols 2015;4(1):1-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cadeiras 2014 {published data only}
- Cadeiras M, Soroya M, Patel S, Starling C, Lim G, Dong K, et al. Using social media as a method of increasing organ donation. Circulation 2014;130(Suppl 2):A18386. [Google Scholar]
Cao 2018 {published data only}
- Cao F, Li L, Lin M, Lin Q, Ruan Y, Hong F. Application of instant messaging software in the follow-up of patients using peritoneal dialysis, a randomised controlled trial. Journal of Clinical Nursing 2018;27(15-16):3001-7. [DOI] [PubMed] [Google Scholar]
Dam 2017 {published data only}
- Dam AE, Vugt ME, Boxtel MP, Verhey FR. Effectiveness of an online social support intervention for caregivers of people with dementia: the study protocol of a randomised controlled trial. BioMed Central 2017;18:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
Epstein 2019 {published data only}
- Epstein M, Oesterle S, Haggerty KP. Effectiveness of Facebook groups to boost participation in a parenting intervention. Prevention Science 2019;20:894-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
Espie 2012 {published data only}
- Espie CA, Kyle SD, Williams C, Ong JC, Douglas NK, Hames P, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep 2012;35(6):769-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hixson 2015 {published data only}
- Hixson JD, Barnes D, Parko K, Durgin T, Van Bebber S, Graham A, et al. Patients optimizing epilepsy management via an online community. Neurology 2015;85:129-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hixson JD. The POEM study: testing the impact of a digital health platform on U.S. veterans with epilepsy. Epilepsy and Behaviour 2015;46:53. [Google Scholar]
Ho 2015 {published data only}
- Ho K, Newton L, Boothe A, Novak-Lauscher H. Mobile Digital Access to a Web-Enhanced Network (mDAWN): assessing the feasibility of mobile health tools for self-management of type 2 diabetes. AMIA Annual Symposium Proceedings 2015;2015:621-9. [PMC free article] [PubMed] [Google Scholar]
Ho 2016 {published data only}
- Ho K, Novak Lauscher H, Newton L, Boothe A. Mobile Digital Access to a Web-Enhanced Network (mDAWN): MHealth for type-2 diabetes self-management and implications for emergency medicine. Canadian Journal of Emergency Medicine 2016;18:s99. [Google Scholar]
Kaur 2020 {published data only}
- Kaur J, Kaur M, Chakrapani V, Webster J, Santos JA, Kumar R. Effectiveness of information technology-enabled 'SMART Eating' health promotion intervention: a cluster randomized controlled trial. PLOS One 2020;15(1):e0225892. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ko 2013 {published data only}
- Ko N, Hsieh C, Wang M, Lee C, Chen C, Chung A, et al. Effects of Internet Popular Opinion Leaders (iPOL) among Internet-using men who have sex with men. Journal of Medical Internet Research 2013;15(2):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kofinas 2014 {published data only}
- Kofinas J, Varrey A, Sapra K, Kanj RV, Chervenak FA, Asfaw T. Randomized controlled trial of adjunctive social media for more effective contraceptive counseling. The American College of Obstetricians and Gynecologists 2014;123:doi: 10.1097/01.AOG.0000447049.82019.cb. [DOI] [PubMed] [Google Scholar]
Kondo 2019 {published data only}
- Kondo E, Tatah S, Sap S, Koki PO, Sobngwi E, Mbanya JC, et al. Effect of patient education through a social network in young patients with type 1 diabetes in a Sub‐Saharan context. Pediatric Diabetes 2019;20(3):361-5. [DOI] [PubMed] [Google Scholar]
Kumar 2016 {published data only}
- Kumar K, King EA, Muzaale AD, Konel JM, Bramstedt KA, Massie AB, et al. A smartphone app for increasing live organ donation. American Journal of Transplantation 2016;16:3548-53. [DOI] [PubMed] [Google Scholar]
Laws 2018 {published data only}
- Denney-Wilson E, Laws R, Russell CG, Ong K, Taki S, Elliot R, et al. Preventing obesity in infants: the growing healthy feasibility trial protocol. BMJ Open 2015;5:e009258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denney-Wilson E, Laws R, Russell CG, Ong KL, Taki S, Litterbach EK, et al. Preventing obesity in infants with a novel m-health intervention: the growing healthy feasibility trial. Obesity Reviews Populations and Population Health 2016;17(2):91-151. [Google Scholar]
- Laws RA, Denney-Wilson EA, Taki S, Russell CG, Zheng M, Litterbach E, et al. Key lessons and impact of the Growing Healthy mHealth program on milk feeding, timing of introduction of solids, and infant growth: quasi-experimental study. JMIR Mhealth and Uhealth 2018;6(4):e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell CG, Denney-Wilson E, Laws RA, Abbott G, Zheng M, Lymer SJ, et al. Impact of the Growing Healthy mHealth program on maternal feeding practices, infant food preferences, and satiety responsiveness: quasi-experimental study. JMIR Mhealth and Uhealth 2018;6(4):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2019 {published data only}
- Li X, Li T, Chen J, Xie Y, An X, Lv Y, et al. A WeChat-based self-management intervention for community middle-aged and elderly adults with hypertension in Guangzhou, China: a cluster-randomized controlled trial. International Journal of Environmental Research and Public Health 2019;16(21):4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lindsay 2009 {published data only}
- Lindsay S, Bellaby P, Smith S, Baker R. Enabling healthy choices: is ICT the highway to health improvement. Health 2008;12(3):313-31. [DOI] [PubMed] [Google Scholar]
- Lindsay S, Smith S, Bellaby P, Baker R. The health impact of an online heart disease support group: a comparison of moderated versus unmoderated support. Health Education Research 2009;24(4):646-54. [DOI] [PubMed] [Google Scholar]
Ling 2018 {published data only}
- Ling J, Robbins LB, Zhang N, Kerver JM, Lyons H, Wieber N, et al. Using Facebook in a healthy lifestyle intervention: feasibility and preliminary efficacy. Western Journal of Nursing Research 2018;40(12):1818-42. [DOI] [PubMed] [Google Scholar]
Mingoia 2019 {published data only}
- Mingoia J, Hutchinson AD, Gleaves DH, Wilson C. The impact of a social media literacy intervention on positive attitudes to tanning: a pilot study. Computers in Human Behavior 2019;90:188-95. [Google Scholar]
MotaPereira 2014 {published data only}
- Mota Pereira J. Facebook enhances antidepressant pharmacotherapy effects. Scientific World Journal 2014;2014:892048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Muntaner‐Mas 2017 {published data only}
- Muntaner-Mas A, Vidal-Conti J, Borràs PA, Ortega FB, Palou P. Effects of a WhatsApp-delivered physical activity intervention to enhance health-related physical fitness components and cardiovascular disease risk factors in older adults. Journal of Sports Medicine and Physical Fitness 2017;57(1-2):90-102. [DOI] [PubMed] [Google Scholar]
Niela‐Viten 2016 {published data only}
- Niela‐Vilén H, Axelin A, Melender H, Löyttyniemi E, Salanterä S. Breastfeeding preterm infants - a randomized controlled trial of the effectiveness of an Internet-based peer-support group. Journal of Advanced Nursing 2016;72(10):2495-507. [DOI] [PubMed] [Google Scholar]
Po'e 2013 {published data only}
- Po'e EK, Heerman WJ, Mistry RS, Barkin SL. Growing Right Onto Wellness (GROW): a family-centered community-based obesity prevention randomized controlled trial for preschool child-parent pairs. Contemporary Clinical Trials 2013;36(2):436-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pope 2018 {published data only}
- Pope ZC, Zeng N, Zhang R, Lee HY, Gao Z. Effectiveness of combined smartwatch and social media intervention on breast cancer survivor health outcomes: a 10-week pilot randomized trial. Journal of Clinical Medicine 2018;7:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rhodes 2016 {published data only}
- Rhodes SD, McCoy TP, Tanner AE, Stowers J, Bachmann LH, Nguyen AL, et al. Using social media to increase HIV testing among gay and bisexual men, other men who have sex with men, and transgender persons: outcomes from a randomized community trial. Clinical Infectious Diseases 2016;62:1450-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosser 2010 {published data only}
- Rosser BR, Oakes MJ, Konstan J, Hooper S, Horvath KJ, Danilenko GP, et al. Reducing HIV risk behavior of MSM through persuasive computing: results of the Men’s INTernet Study (MINTS-II). AIDS 2010;24(13):2099–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2012 {published data only}
- Smith GC, Nichole E, Dellman-Jenkins M, Nanna K, Palmieri PA. Reducing depression in stroke survivors and their informal caregivers: a randomized clinical trial of a web-based intervention. Rehabilitation Psychology 2012;57(3):196-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tiermensma 2015 {published data only}
- Tiemensma J, Rus H. The inhibitory effect of Facebook use on stress recovery: a pilot study. Psychoneuroendocrinology 2015;62:75. [Google Scholar]
van der Eijk 2012 {published data only}
- Eijk M, Faber MJ, Aarts JW, Kremer JA, Munneke M, Bloem BR. Using online health communities to deliver patient-centered care to people with chronic conditions. Journal of Medical Internet Research 2013;15(6):e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Verduyn 2015 {published data only}
- Verduyn P, Lee DS, Park J, Shablack H, Orvell A, Bayer J, et al. Passive Facebook usage undermines affective well-being: experimental and longitudinal evidence. Journal of Experimental Psychology: General 2015;144(2):480-8. [DOI] [PubMed] [Google Scholar]
West 2016 {published data only}
- West DS, Monroe CM, Turner-McGrievy G, Sundstrom B, Larsen C, Magradey K, et al. A technology-mediated behavioral weight gain prevention intervention for college students: controlled, quasi-experimental study. Journal of Medical Internet Research 2016;18(6):e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2018 {published data only}
- Young SD, Koussa M, Lee SJ, Perez H, Gill N, Gelberg L, et al. Feasibility of a social media/online community support group intervention among chronic pain patients on opioid therapy. Journal of Addictive Diseases 2018;37(1-2):96-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yu 2014 {published data only}
- Yu CH, Parsons J, Mamdani M, Lebovic G, Shah BR, Bhattacharyya O, et al. Designing and evaluating a web-based self-management site for patients with type 2 diabetes - systematic website development and study protocol. BMC Medical Informatics & Decision Making 2012;12:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu CH, Parsons JA, Hall S, Newton D, Jovicic A, Lottridge D, et al. User-centered design of a web-based self-management site for individuals with type 2 diabetes - providing a sense of control and community. BMC Medical Informatics & Decision Making 2014;14:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu CH, Parsons JA, Mamdani M, Lebovic G, Hall S, Newton D, et al. A web-based intervention to support self-management of patients with type 2 diabetes mellitus: effect on self-efficacy, self-care and diabetes distress. BMC Medical Informatics & Decision Making 2014;14:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Abdelkarim 2016 {published data only}
- Abdelkarim A, Nagui RD, Esmaiel M, Helal H. Social media group parallel to dialectical behavior therapy skills training group, the pros and cons. European Psychiatry 2016;33:s556. [Google Scholar]
Alghafri 2018 {published data only}
- Alghafri TS, Alharthi SM, Al-Farsi Y, Alrawahi AH, Bannerman E, Craigie AM, et al. 'MOVEdiabetes': a cluster randomized controlled trial to increase physical activity in adults with type 2 diabetes in primary health in Oman. BMJ Open Diabetes Research & Care 2018;6(1):e00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bakirci‐Taylor 2019 {published data only}
- Bakirci-Taylor AL, Reed DB, McCool B, Dawson JA. MHealth improved fruit and vegetable accessibility and intake in young children. Journal of Nutrition Education and Behaviour 2019;51(5):556-66. [DOI] [PubMed] [Google Scholar]
Bickel 2016 {published data only}
- Bickel WK, Chandrasekar P, Koffarnus MN, Fox EA, Franck CT, Bhandari S, et al. The social interactome of recovery: social media network typology influences relapse. Alcoholism: Clinical and Experimental Research 2016;40:e20. [Google Scholar]
Birnbrauer 2018 {published data only}
- Birnbrauer K. Applying the health belief model to investigate the effects of Facebook participation on diabetes self-management and medication adherence. Dissertation Abstracts International Section A: Humanities and Social Sciences 2018;79:2-A(E). [Google Scholar]
Chang 2018 {published data only}
- Chang Y, Lu S, Hsu Y. Efficacy of a game-based mobile application intervention in physical activity promotion and health management. Obesity Facts 2018;11(Suppl 1):326-7. [Google Scholar]
Cheng 2018 {published data only}
- Cheng Y, Qi M, Zhang X. Influence of WeChat cluster intervention on diet and blood glucose control in prediabetes patients. Chinese Nursing Research 2018;32(12):1882-5. [Google Scholar]
Dulli 2020 {published data only}
- Dulli L, Ridgeway K, Packer C, Murray KR, Mumuni T, Plourde KF, et al. A social media-based support group for youth living with HIV in Nigeria (SMART Connections): a randomized controlled trial. Journal of Medical Internet Research 2020;22(6):e18343. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ehde 2017 {published data only}
- Ehde DM, Arewasikpon A, Nelson IK, Molton IR, Alchuler KN. A pilot randomized controlled trial evaluating the effects of a resilience intervention on adults aging with multiple sclerosis. Multiple Sclerosis Journal 2017;23(3 Suppl):671-2. [Google Scholar]
Elloumi 2018 {published data only}
- Elloumi L, Beijnum BJ, Hermens H. Exploratory study of a virtual community for physical activity. Health and Technology 2018;8:81-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gao 2015 {published data only}
- Gao H, Feng F, Li J, Zhao Q, Ba J. The application of a glucose cloud platform combined with WeChat interaction in diabetes management. Diabetes/Metabolism Research and Reviews 2015;31:48. [Google Scholar]
Hafiz 2018 {published data only}
- Hafiz AA, Gallagher AM, Hill AJ. The influence of social networks in increasing fruit and vegetables consumption in university students: a randomised controlled study. Proceedings of the Nutrition Society 2018;77:OCE1. [Google Scholar]
Li 2018 {published data only}
- Li S, Lu R, Wang R, Zhao J, Li Y, Pu W. Effect of WeChat mutual help group on 131I treatment compliance and quality of life of thyroid cancer patients. Anti-Tumor Pharmacy 2018;8(6):1001-5. [Google Scholar]
Mahdi 2019 {published data only}
- Mahdi AM, Gholamreza M, Mohsen G. Comparison of the effectiveness of mobile social network-based mindfulness interventions, acceptance and commitment therapy, and mindfulness group therapy on depression, anxiety, and stress among type II diabetic patients. Journal of Diabetic Nursing 2019;7(2):775-92. [Google Scholar]
Maher 2018 {published data only}
- Maher C, Looyestyn J, Kernot J, Boshoff K. An 8 week beginners' running program delivered using via online social networking: a randomised controlled trial. Journal of Science and Medicine in Sport 2018;21(Suppl 1):s26. [Google Scholar]
Petrovski 2016 {published data only}
- Petrovski G, Zivkovik M, Ahmeti I, Adamova K. Mobile social media and diabetes: Viber communication improves glucose control in type 1 diabetes patients on insulin pump. Diabetes Technology and Therapeutics 2016;18:A97. [Google Scholar]
Trude 2018 {published data only}
- Trude AC, Kharmats AY, Jones-Smith JC. Exposure to a multi-level multi-component childhood obesity prevention community-randomized controlled trial: patterns, determinants, and implications. Trials 2018;19(1):287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2019 {published data only}
- Wu W, Hung C. Impact of a peer virtual community on pregnant women's well-being: a repeated-measure and quasi-experimental study. Journal of Advanced Nursing 2019;75(5):1099-107. [DOI] [PubMed] [Google Scholar]
Yang 2016 {published data only}
- Yang DX, Gu CJ, Ni L, Li N, Li QY, Zhou JP. Assessment of efficacy of medication combined with WeChat platform for quitting smoking in patients with chronic obstructive pulmonary disease. Journal of Shanghai Jiaotong University (Medical Science) 2016;36(3):385-9. [Google Scholar]
References to ongoing studies
ACTRN12619000335190 {published data only}
- Reupert A. Mi.spot (supportive, preventative, online and targeted): a moderated online intervention for young adults who have a parent with a mental illness and/or substance use concern: a study protocol for a randomised controlled trial. ANZCTR 2019;Available from: https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12619000335190.
ACTRN12619001785190 {published data only}
- Paterson M. Talking about Aboriginal gambling: examining the effectiveness of Facebook groups to reduce gambling harm within Aboriginal communities in New South Wales, Australia [2019]. ANZCTR;Available from: https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12619001785190.
Arnold 2019 {published data only}
- Alvarez M. Enhancing social functioning in young people at ultra high risk for psychosis: randomised controlled trial of a novel strengths-based online social therapy. ANZCTR 2019;Available from: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=376773.
- Arnold EM, Swendeman D, Harris D, Fournier J, Kozina L, Abdallan S, et al. The stepped care intervention to suppress viral load in youth living with HIV: protocol for a randomized controlled trial. JMIR Research Protocols 2019;8(2):e10791. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aschbrenner 2019 {published data only}
- Aschbrenner K, Naslind J, Gorin A, Mueser K, Bartels S. Randomized trial of a lifestyle intervention for young adults with serious mental illness in community mental health centers. Schizophrenia Bulletin 2019;45(Suppl 2):s135. [Google Scholar]
Beleigoli 2018 {published data only}
- Beleigoli AM, Andrade AQ, Diniz MD, Alvares RS, Fereira MH, Silva LA, et al. Protocol of a randomized clinical trial to test the efficacy of an online platform for weight loss in adults with overweight and obesity: POEmaS project. Obesity Facts 2018;11(Suppl 1):268. [Google Scholar]
- Beleigoli AM, Queiroz de Andrade A, Haueisen Diniz M, Alvares RS, Ribeiro AL. Online platform for healthy weight loss in adults with overweight and obesity - the "POEmaS" project: a randomized controlled trial. BMC Public Health 2018;18(1):945. [DOI] [PMC free article] [PubMed] [Google Scholar]
Block 2014 {published data only}
- Block G, Azar K, Block T, Block C, Palaniappan L. Development and clinical trial of an eHealth program for pre-diabetics. FASEB 2014;28(Suppl 1):1035.12. [Google Scholar]
Bonar 2020 {published data only}
- Bonar EE, Schneeberger DM, Bourque C, Bauermeister JA, Young SD, Blow FC, et al. Social media interventions for risky drinking among adolescents and emerging adults: protocol for a randomized controlled trial. JMIR Research Protocols 2020;9(5):e16688. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boudreau 2016 {published data only}
- Boudreau F, Moreau M, Côté J. Effectiveness of computer tailoring versus peer support web-based interventions in promoting physical activity among insufficiently active Canadian adults with type 2 diabetes: protocol for a randomized controlled trial. JMIR Research Protocols 2016;5(1):e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2016 {published data only}
- Campbell KJ, Hesketh KD, McNaughton SA, Ball K, McCallum Z, Lynch J, et al. The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) program: a cluster-randomized controlled trial of an early intervention to prevent childhood obesity. BMC Public Health 2016;16:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheung 2020 {published data only}
- Cheung YT, Chan CH, Ho KS, Fok WP, Conway M, Wong CK, et al. Effectiveness of WhatsApp online group discussion for smoking relapse prevention: protocol for a pragmatic randomized controlled trial. Addiction 2020;115(9):1777-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fereira 2017 {published data only}
- Fereira M, Young L, Schneider J. Baseline characteristics from prep Chicago: a randomized controlled diffusion-based network intervention for HIV prevention among young Black men who have sex with men. Open Forum Infectious Diseases 2017;4(Suppl 1):s439-40. [Google Scholar]
Glover 2017 {published data only}
- Glover M, Kira A, Kira G, McRobbie H, Breie BH, Kruger R, et al. An innovative team-based weightloss competition to reduce cardiovascular and diabetes risk among Māori and Pacific people: rationale and method for the study and its evaluation. BMC Nutrition 2017;3:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Herring 2019 {published data only}
- Herring SJ, Albert JJ, Dardeb N, Bailer B, Cruice J, Hassan S, et al. Targeting pregnancy-related weight gain to reduce disparities in obesity: baseline results from the Healthy Babies trial. Contemporary Clinical Trials 2019;87:105822. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN14859844 {published data only}
- Noreik M. Online weight loss. ISRCTN 2019;Available from: https://doi.org/10.1186/ISRCTN14859844.
Jacobson 2020 {published data only}
- Jacobson LT, Collins TC, Lucas M, Zackula R, Okut H, Nazir N, et al. Electronic Monitoring Of Mom's Schedule (eMOMS TM): protocol for a feasibility randomized controlled trial to improve postpartum weight, blood sugars, and breastfeeding among high BMI women. Contemporary Clinical Trials Communications 2020;18(101671157):100565. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jansson 2019 {published data only}
- Jansson AK, Lubans DR, Smith JJ, Duncan MJ, Bauman A, Attia J, et al. Integrating smartphone technology, social support and the outdoor built environment to promote community-based aerobic and resistance-based physical activity: rationale and study protocol for the ‘ecofit’ randomized controlled trial. Contemporary Clinical Trials Communications 2019;16:100457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jaser 2019 {published data only}
- Jaser SS, Hamburger ER, Pagoto S, Williams R, Meyn A, Jonas AC, et al. Communication and coping intervention for mothers of adolescents with type 1 diabetes: rationale and trial design. Contemporary Clinical Trials 2019;85:105844. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaylor‐Hughes 2017 {published data only}
- Kaylor-Hughes CJ, Rawsthorne M, Coulson NS, Simpson S, Simons L, Guo B, et al. Direct to public peer support and e-therapy program versus information to aid self-management of depression and anxiety: protocol for a randomized controlled trial. JMIR Research Protocols 2017;6(12):e231. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2017 {published data only}
- Kim SJ, Marsch LA, Brunette MF, Dallery J. Harnessing Facebook for smoking reduction and cessation interventions: Facebook user engagement and social support predict smoking reduction. Journal of Medical Internet Research 2017;19(5):e168. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKeon 2019 {published data only}
- McKeon G, Steel Z, Wells R, Newby JM, Hadzi-Pavlovic D, Vancampfort D, et al. Mental health informed physical activity for first responders and their support partner: a protocol for a stepped-wedge evaluation of an online, codesigned intervention. BMJ Open 2019;9(9):e030668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeon G. A mental health informed physical activity program for first responders and their chosen support partners [2019]. ANZCTR;Available: http://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=377720.
NCT03021655 {published data only}
- Cheung L. A pilot randomized control trial to help youth smokers to quit smoking. clinicaltrials.gov 2017;Available from:https://clinicaltrials.gov/ct2/show/ NCT03021655.
NCT03078153 {published data only}
- Siegel M. Effect of social media support and financial incentives on PrEP adherence. clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03078153.
NCT03109743 {published data only}
- Blackstock O. Group clinical visit adherence intervention for HIV+ women of color. clinicaltrials.gov 2018;available from: https://clinicaltrials.gov/ct2/show/ NCT03109743.
NCT03143309 {published data only}
- Saquib J. Physical activity intervention to promote walking among female university students. clinicaltrials.gov 2017;Available from: https://clinicaltrials.gov/ct2/show/ NCT03143309.
NCT03149757 {published data only}
- Horvath K. Connecting youth and young adults to optimize ART adherence: youTHrive efficacy trial. clincialtrials.gov 2017;Available from: https://clinicaltrials.gov/ct2/show/ NCT03149757. [DOI] [PMC free article] [PubMed]
NCT03163303 {published data only}
- Satre D. Smoking Tobacco and Drinking study (STAND). clincialtrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03163303.
NCT03169686 {published data only}
- Liao Y. 'WeChat WeQuit' smoking cessation program. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03169686.
NCT03253406 {published data only}
- Gao Z. Health wearables and college student health. clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03253406.
NCT03257657 {published data only}
- Thompson DA. Helping moms to be healthy after baby. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03257657.
NCT03259360 {published data only}
- Humfleet GL. A Facebook intervention for young sexual and gender minority smokers (POP). clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03259360. [DOI] [PMC free article] [PubMed]
NCT03387800 {published data only}
- Wang Z. RCT for evaluation of online social networking intervention in smoking cessations. clinicaltrials.gov 2018;Available from: https://clinicaltrials.gov/ct2/show/ NCT03387800.
NCT03441321 {published data only}
- Manne S. Social-media intervention in reducing indoor tanning in high-risk indoor tanners. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03441321.
NCT03456453 {published data only}
- Staton M. Social media HIV prevention intervention for high risk rural women. clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03456453.
NCT03553992 {published data only}
- Humfleet GL. An extended Facebook intervention for young sexual and gender minority smokers (POP-6). clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03553992. [DOI] [PMC free article] [PubMed]
NCT03556774 {published data only}
- Liao Y. Boosting Chinese healthcare service providers' utilization of smoking cessation interventions by 'WeChat WeQuit' program. clincialtrials.gov 2018;Available from: https://clinicaltrials.gov/ct2/show/ NCT03556774.
NCT03567226 {published data only}
- Friedman D, Liang Y. Leveraging WeChat social-media and messaging platform to increase physical activity in Chinese glaucoma patients. clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03567226.
NCT03574012 {published data only}
- Hutchinson F. SmART Heart: study of mHealth apps to reduce cancer-treatment effects on the heart. clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03574012.
NCT03658044 {published data only}
- Angenete E. Social media on prescription for colorectal cancer patients (SMOP). clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03658044.
NCT03677739 {published data only}
- Manne S. Young melanoma family Facebook intervention or healthy lifestyle Facebook intervention in improving skin examination in participants with melanoma and their families. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03677739.
NCT03678181 {published data only}
- Bauermeister JA, Golinkoff JM. Increasing engagement and improving HIV outcomes via HealthMPowerment. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03678181.
NCT03684070 {published data only}
- Katigbak C. Together we Move: a multi-component intervention to increase physical activity for ethnic minority older adults. clinicatrials.gov 2019;Available from: https://www.clinicaltrials.gov/ct2/show/ NCT03684070.
NCT03897049 {published data only}
- Kuhn T. Evaluation of the Trans Women Connected mobile app for changes in sexual health-related behavior among transgender women (TWC). clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03897049.
NCT03907462 {published data only}
- Godino J. SMART 2.0: social mobile approaches to reducing weight in young adults (SMART 2). clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03907462.
NCT03959631 {published data only}
- Elustondo SG. Effectiveness and cost-effectiveness of a VCoP to empowerment of patients with ischaemic heart disease in PHC: cluster-RCT (Empodera-dos). clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03959631.
NCT04010019 {published data only}
- Lumley MA. The facing pain study. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT04010019.
NCT04045132 {published data only}
- Children's Hospital of Philadelphia. The parenting with depression study. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT04045132.
NCT04187989 {published data only}
- Bonar E. Social media intervention for cannabis use in emerging adults. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT04187989. [DOI] [PMC free article] [PubMed]
NCT04217759 {published data only}
- Rasil AN. Healthy lifestyle intervention on diabetes risk reduction among Bruneian young adults. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT04217759.
NCT04286165 {published data only}
- Cloitre M. Brief peer supported webSTAIR compared to enhanced wait list (BPSwS). clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT04286165.
NCT04367506 {published data only}
- Bennett M. Adapting a digital intervention to improve smoking cessation in persons with serious mental illness. clincialtrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT04367506.
Pagoto 2016 {published data only}
- Pagoto SL, Baker K, Griffith J, Oleski JL, Palumbo A, Walkosz BJ, et al. Engaging moms on teen indoor tanning through social media: protocol of a randomized controlled trial. JMIR Research Protocols 2016;5(4):e228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2018 {published data only}
- Patel V, Ginsburg Z, Golub SA, Horvath K, Rios N, Mayer KH, et al. Empowering with PrEP (E-PrEP), a peer-led social media-based intervention to facilitate HIV preexposure prophylaxis adoption among young Black and Latinx gay and bisexual men: protocol for a cluster randomized controlled trial. JMIR Research Protocols 2018;7(8):e11375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel VV, Ginsburg Z, Golub SA, Horvath KJ, Rios N, Mayer KH, et al. Empowering with PrEP (E-PrEP), a peer-led social media-based intervention to facilitate HIV preexposure prophylaxis adoption among young Black and Latinx gay and bisexual men: protocol for a cluster randomized controlled trial. Journal of Medical Internet Research 2018;20(8):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel VV. Social media based peer-led intervention for HIV prevention. clinicaltrials.gov 2019;Available from: https://clinicaltrials.gov/ct2/show/ NCT03213366.
Pechmann 2020 {published data only}
- Pechmann CA, Calder D, Phillips C, Delucchi K, Prochaska JJ. The use of web-based support groups versus usual quit-smoking care for men and women aged 21-59 years: protocol for a randomized controlled trial. JMIR Research Protocols 2020;9(1):e16417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramo 2018a {published data only}
- Ramo DE, Kaur M, Corpuz ES, Satre DD, Delucchi K, Brown SA, et al. Using Facebook to address smoking and heavy drinking in young adults: protocol for a randomized, controlled trial. Contemporary Clinical Trials 2018;68:52-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siegmund 2017 {published data only}
- Siegmund LA, Ahmed HM, Crawford MT, Bena JF. Feasibility of a Facebook intervention for exercise motivation and cardiac rehabilitation adherence: study protocol. JMIR Research Protocols 2017;6(8):e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinicrope 2019 {published data only}
- Sinicrope PS, Koller KR, Prochaska JJ, Hughes CA, Bock MJ, Decker PA, et al. Social media intervention to promote smoking treatment utilization and cessation among Alaska Native people who smoke: protocol for the Connecting Alaska Native People to Quit Smoking (CAN Quit) pilot study. JMIR Research Protocols 2019;8(11):e15155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Swendeman 2019 {published data only}
- Swendeman D, Arnold EM, Harris D, Fournier J, Cornulada WS, Reback C, et al. Engaging seronegative youth to optimize HIV prevention continuum. JMIR Research Protocols 2019;8(8):e11165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2017 {published data only}
- Wang ML, Waring ME, Jake-Schoffman DE, Oleski JL, Michaels Z, Goetz JM, et al. Clinic versus online social network–delivered lifestyle interventions: protocol for the Get Social noninferiority randomized controlled trial. JMIR Research Protocols 2017;6(12):e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waring 2019 {published data only}
- Waring ME, Libby BA, Moore Simas TA, Bracken ML, Bibeau JL, Herrera V, et al. Delivering a post-partum weight loss intervention via Facebook or in-person groups: protocol for a randomized feasibility pilot trial. JMIR Research Protocols 2019;8(11):e15530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waring ME. The healthy moms study: comparison of a post-partum weight loss intervention delivered via Facebook or in-person groups. clinicaltrials.gov 2020;Available from: https://clinicaltrials.gov/ct2/show/ NCT03700736.
Wilcox 2018 {published data only}
- Wilcox S, Liu J, Addy CL, Turner-McGrievy G, Burgis JT, Wingard E, et al. A randomized controlled trial to prevent excessive gestational weight gain and promote postpartum weight loss in overweight and obese women: Health In Pregnancy and Postpartum (HIPP). Contemporary Clinical Trials 2018;66:51-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wysocki 2018 {published data only}
- Wysocki T, Pierce J, Caldwell C, Aroin K, Miller L, Farless R, et al. A web-based coping intervention by and for parents of very young children with type 1 diabetes: user-centered design. JMIR Diabetes 2018;3(4):e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Ali 2015
- Ali K, Farrer L, Gulliver A, Griffiths KM. Online peer-to-peer support for young people with mental health problems: a systematic review. JMIR Mental Health 2015;2(2):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Antheunis 2013
- Antheunis ML, Tates K, Nieboer TE. Patients' and health professionals' use of social media in health care: motives, barriers and expectations. Patient Education and Counseling 2013;92(3):426-31. [DOI] [PubMed] [Google Scholar]
Bala 2017
- Bala MM, Strzeszynski L, Topor-Madry R. Mass media interventions for smoking cessation in adults. Cochrane Database of Systematic Reviews 2017, Issue 1. Art. No: CD004704. [DOI: 10.1002/14651858.CD004704.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bambra 2015
- Bambra CL, Hillier FC, Cairns J-M, Kasim A, Moore HJ, Summerbell CD. How effective are interventions at reducing socioeconomic inequalities in obesity among children and adults? Two systematic reviews. Public Health Research 2015;3.1. [PubMed]
Bandura 2000
- Bandura A. Exercise of human agency through collective efficacy. Current Directions in Psychological Science 2000;9(3):75-8. [Google Scholar]
Baumeister 1987
- Baumeister RF, Hutton DG. Self-presentation theory: self-construction and audience pleasing. In: Mullen B, Goethals, GR, editors(s). Theories of Group Behavior. New York: Springer, 1987:71-87. [Google Scholar]
Boers 2014
- Boers M, Kirwan JR, Wells G, Beaton D, Gossec L, d'Agostino M, et al. Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. Journal of Clinical Epidemiology 2014;67(7):745-53. [DOI] [PubMed] [Google Scholar]
Brusse 2014
- Brusse C, Gardner K, McAullay D, Dowden M. Social media and mobile apps for health promotion in Australian Indigenous populations: scoping review. Journal of Medical Internet Research 2014;16(12):e280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Byron 2013
- Byron P, Albury K, Evers C. “It would be weird to have that on Facebook”: young people's use of social media and the risk of sharing sexual health information. Reproductive Health Matters 2013;21(41):35-44. [DOI] [PubMed] [Google Scholar]
Carson‐Chahhoud 2017
- Carson-Chahhoud KV, Ameer F, Sayehmiri K, Hnin K, Agteren JE, Sayehmiri F, et al. Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No: CD001006. [DOI: 10.1002/14651858.CD001006.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chauvin 2016
- Chauvin J, Perera Y, Clarke M. Digital technologies for population health and health equity gains: the perspective of public health associations. Journal of Public Health Policy 2016;37(2):232-48. [DOI] [PubMed] [Google Scholar]
Chiu 2016
- Chiu CJ, Menacho L, Young SD. The association between age and ethics-related issues in using social media for HIV prevention in Peru. Ethics & Behavior 2016;26(2):99-109. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cho 2007
- Cho H, Salmon CT. Unintended effects of health communication campaigns. Journal of Communication 2007;57:293-317. [Google Scholar]
Clement 2013
- Clement S, Lassman F, Barley E, Evans-Lacko S, Williams P, Yamaguchi S, et al. Mass media interventions for reducing mental health-related stigma. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD009453. [DOI: 10.1002/14651858.CD009453.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Craig 2008
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Di Bitonto 2015
- Di Bitonto P, Pesare E, Rossano V, Roselli T. Smart learning environments using social network, gamification and recommender system approaches in e-Health contexts. In: Uskov LV, Howlett R, Jain L, editors(s). Smart Education and Smart e-Learning. Vol. 41. Springer International Publishing, 2015:491-500. [Google Scholar]
Dyson 2015
- Dyson MP, Hartling L, Shulhan J, Chisholm A, Milne A, Sundar P, et al. A systematic review of social media use to discuss and view deliberate self-harm acts. PLOS One 2015;11(5):e-0155813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edberg 2015
- Edberg M. Essentials of Health Behavior: Social and Behavioral Theory in Public Health. 2nd Ed. edition. Jones & Barthlett Learning, 2015. [Google Scholar]
EPOC 2017a
- Cochrane Effective Practice and Organisation of Care (EPOC). What study designs should be included in an EPOC view? EPOC resources for review authors. Available at epoc.cochrane.org/epoc-resources-review-authors 2017.
EPOC 2017b
- Effective Practice and Organization of Care (EPOC). Suggested risk of bias criteria for EPOC reviews. EPOC resources for review authors. Available from: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/suggested_risk_of_bias_criteria_for_epoc_reviews.pdf.
Evans 2003
- Evans T, Brown H. Road traffic crashes: operationalizing equity in the context of health sector reform. Injury Control Safety Promotion 2003;10(1-2):11-2. [DOI] [PubMed] [Google Scholar]
Gough 2012
- Gough D, Oliver S, Thomas J. Introduction to Systematic Reviews. London: Sage, 2012. [Google Scholar]
Greene 2011
- Greene JA, Choudhry NK, Kilabuk E, Shrank WH. Online social networking by patients with diabetes: a qualitative evaluation of communication with Facebook. Journal of General Internal Medicine 2011;26(3):287-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grilli 2002
- Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database of Systematic Reviews 2002, Issue 1. Art. No: CD000389. [DOI: 10.1002/14651858.CD000389] [DOI] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2011;64(4):380–2. [DOI] [PubMed] [Google Scholar]
Haight 2014
- Haight M, Quan-Haase A, Corbett BA. Revisiting the digital divide in Canada: the impact of demographic factors on access to the Internet, level of online activity, and social networking site usage. Information, Communication & Society 2014;14(4):503-19. [Google Scholar]
Hamm 2014
- Hamm M, Shulhan J, Williams G, Milne A, Scott SD, Hartling L. A systematic review of the use and effectiveness of social media in child health. BMC Pediatrics 2014;14:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
Han 2017
- Han H, Pettee Gabriel K, Kohl HW 3rd. Application of the transtheoretical model to sedentary behaviors and its association with physical activity status. PLOS One 2017;12(4):e0176330. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heffernan 2017
- Heffernan C, et al. Social media interventions for impacting knowledge, attitudes and behaviours around vaccination uptake. Cochrane Database of Systematic Reviews in progress. [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Higgins 2020a
- Higgins JP, Li T, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect.. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1. Cochrane, 2020. [Google Scholar]
Higgins 2020b
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1. Cochrane, 2020. [Google Scholar]
Hudnut‐Beumler 2016
- Hudnut-Beumler J, Po'e E, Barkin S. The use of social media for health promotion in Hispanic populations: a scoping systematic review. JMIR Public Health and Surveillance 2016;2(2):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Humphreys 2013
- Humphreys DK, Ogilvie D. Synthesising evidence for equity impacts of population-based physical activity interventions: a pilot study. International Journal of Behavioral Nutrition and Physical Activity 2013;10:76. [DOI: 10.1186/1479-5868-10-76] [DOI] [PMC free article] [PubMed] [Google Scholar]
ITU 2019
- ITU. Measuring digital development: Facts and Figures 2019. International Telecommunication Union 2019;(Availablle from: https://www.itu.int/en/ITU-D/Statistics/Documents/facts/FactsFigures2019.pdf):accessed 30 March 2020.
Klassen 2018
- Klassen KM, Douglass CH, Brennan L, Truby H, Lim MS. Social media use for nutrition outcomes in young adults: a mixed methods systematic review. International Journal of Behavioral Nutrition and Physical Activity 2018;15(1):70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Korda 2013
- Korda H, Itani Z. Harnessing social media for health promotion and behavior change. Health Promotion Practice 2013;14(1):15-23. [DOI] [PubMed] [Google Scholar]
Kristjansson 2015
- Kristjansson E, Francis DK, Liberato S, Benkhalti Jandu M, Welch V, Batal M, et al. Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No: CD009924. [DOI: 10.1002/14651858.CD009924.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Laranjo 2015
- Laranjo L, Arguel A, Neves AL, Gallagher AM, Kaplan R, Mortimer N, et al. The influence of social networking sites on health behavior change: a systematic review and meta-analysis. Journal of the American Medical Informatics Association 2015;22:243–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Latkin 2015
- Latkin CA, Knowlton AR. Social network assessments and interventions for health behavior change: a critical review. Behavioral Medicine 2015;41(3):90-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacAlister 2008
- McAlister AL, Perry CL, Parcel GS. How individuals, environments and health behaviors interact: social cognitive theory. In: Glanz K, Rimer BK, Viswanath K, editors(s). Health Behaviors and Health Education. 4th edition. Jossey-Bass, 2008:169-75. [Google Scholar]
Maher 2014
- Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review. Journal of Medical Internet Research 2014;16(2):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGill 2015
- McGill R, Anwar E, Orton L, Bromley H, Lloyd-Williams F, O'Flaherty M, et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 2015;15:457. [DOI: 10.1186/s12889-015-1781-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Merolli 2013
- Merolli M, Gray K, Martin-Sanchez F. Health outcomes and related effects of using social media in chronic disease management: a literature review and analysis of affordances. Journal of Biomedical Informatics 2013;46:957-69. [DOI: 10.1016/j.jbi.2013.04.010] [DOI] [PubMed] [Google Scholar]
Michie 2013
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine 2013;46(1):81-95. [DOI] [PubMed] [Google Scholar]
Mosdøl 2017
- Mosdøl A, Lidal IB, Straumann GH, Vist GE. Targeted mass media interventions promoting healthy behaviours to reduce risk of non-communicable diseases in adult, ethnic minorities. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD011683. [DOI: 10.1002/14651858.CD011683.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Myneni 2016
- Myneni S, Cobb N, Cohen T. In pursuit of theoretical ground in behavior change support systems: analysis of peer-to-peer communication in a health-related online community. Journal of Medical Internet Research 2016;18(2):e28. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCCHPC 2015
- National Collaborating Centre for Healthy Public Policy. Social media in public health. http://www.ncchpp.ca/docs/2015_TC_KT_SocialMediaPH_en.pdf (accessed 15 November 2016) 2015.
Ndumbe‐Eyoh 2016
- Ndumbe-Eyoh S, Mazzucco A. Social media, knowledge translation, and action on the social determinants of health and health equity: a survey of public health practices. Journal of Public Health Policy 2016;37(2):249-59. [DOI] [PubMed] [Google Scholar]
O'Keeffe 2011
- O'Keeffe GS, Clarke-Pearson K. The impact of social media on children, adolescents, and families. Pediatrics 2011;127(4):800-4. [DOI] [PubMed] [Google Scholar]
O'Neill 2014
- O'Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of Clinical Epidemiology 2014;67:56-64. [DOI] [PubMed] [Google Scholar]
Ogilvie 2008
- Ogilvie D, Fayter D, Petticrew M, Sowden A, Thomas S, Whitehead M, et al. The harvest plot: a method for synthesising evidence about the differential effects of interventions. BMC Medical Research Methodology 2008;8:8. [DOI: 10.1186/1471-2288-8-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Osborne 2013
- Osborne K, Patel K. Evaluation of a website that promotes social connectedness: lessons for equitable e-health promotion. Australian Journal of Primary Health 2013;19(4):325-30. [DOI] [PubMed] [Google Scholar]
Pew Research Center 2015
- Pew Research Center. Internet seen as positive influence on education but negative on morality and emerging and developing nations. http://www.pewglobal.org/2015/03/19/Internet-seen-as-positive-influence-on-education-but-negative-influence-on-morality-in-emerging-and-developing-nations/ (accessed 20 November 2016) 2015.
Phua 2013
- Phua JJ. The reference group perspective for smoking cessation: an examination of the influence of social norms and social identification with reference groups on smoking cessation self-efficacy. Psychology of Addictive Behaviors 2013;27(1):102. [DOI] [PubMed] [Google Scholar]
Presseau 2015
- Presseau J, Ivers NM, Newham JJ, Knittle K, Danko KJ, Grimshaw JM. Using a behaviour change techniques taxonomy to identify active ingredients within trials of implementation interventions for diabetes care. Implementation Science 2015;10:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Primack 2017
- Primack BA, Shensa A, Sidani JE, Whaite EO, Lin LY, Rosen D, et al. Social media use and perceived social isolation among young adults in the US. American Journal of Preventive Medicine 2017 Mar 6 [Epub ahead of print]. [DOI: 10.1016/j.amepre.2017.01.010] [DOI] [PMC free article] [PubMed]
Real 2015
- Real B, McDermott AJ, Bertot JC, Jaeger PT. Digital inclusion and the Affordable Care Act: public libraries, politics, policy, and enrollment in "Obamacare". Public Library Quarterly 2015;13(1):36-44. [Google Scholar]
Rehfuess 2018
- Rehfuess EA, Booth A, Brereton L, Burns J, Gerharus A, Mozygemba K, et al. Towards a taxonomy of logic models in systematic reviews and health technology assessments: a priori, staged, and iterative approaches. Research Synthesis Methods 2018;9(1):13-24. [DOI] [PubMed] [Google Scholar]
RevMan 2020 [Computer program]
- Review Manager (RevMan). Version 5.4.1. Copenhagen: The Nordic Cochrane Centre, Cochrane, 2020.
Rice 2016
- Rice ES, Haynes E, Royce P, Thompson SC. Social media and digital technology use among Indigenous young people in Australia: a literature review. International Journal for Equity in Health 2016;15:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rohwer 2016
- Rohwer AA, Booth A, Pfadenhauer L, Brereton L, Gerhardus A, Mozygemba K, et al. Guidance on the use of logic models in health technology assessments of complex interventions. Integrate-HTA 2016:Available from: https://www.integrate-hta.eu/wp-content/uploads/2016/02/Guidance-on-the-use-of-logic-models-in-health-technology-assessments-of-complex-interventions.pdf.
Ross 2010
- Ross TP, Ross LT, Rahman A, Cataldo S. The bicycle helmet attitudes scale: using the health belief model to predict helmet use among undergraduates. Journal of American College Health 2010;59(1):29-36. [DOI] [PubMed] [Google Scholar]
Safko 2012
- Safko L, Brake D. The Social Media Bible: Tactics, Tools, and Strategies for Business Success. 3rd edition. Hoboken (US): Wiley, 2012. [Google Scholar]
Seltzer 2015
- Seltzer EK, Jean NS, Kramer-Golinkoff E, Asch DA, Merchant RM. The content of social media's shared images about Ebola: a retrospective study. Public Health 2015;129(9):1273-7. [DOI] [PubMed] [Google Scholar]
Siegfried 2014
- Siegfried N, Pienaar DC, Ataguba JE, Volmink J, Kredo T, Jere M, et al. Restricting or banning alcohol advertising to reduce alcohol consumption in adults and adolescents. Cochrane Database of Systematic Reviews 2014, Issue 11. Art. No: CD010704. [DOI: 10.1002/14651858.CD010704.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simeon 2020
- Simeon R, Dewidar O, Trawin J, Duench S, Manson H, Pardo Pardo J, et al. Behaviour change techniques (BCTs) included in reports of social media interventions for promoting health behaviours in adults: A study within a review. Journal of Medical Internet Research 2020;22(6):e16002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinnenberg 2016
- Sinnenberg L, DiSilvestro CL, Mancheno C, Dailey K, Tufts C, Buttenheim AM, et al. Twitter as a potential data source for cardiovascular disease research. JAMA Cardiology 2016;1(9):1032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2016
- Sterne JA, Heran MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2020
- Sterne JA, Hernán MA, McAleenan A, Reeves BC, Higgins JP. Chapter 25: Assessing risk of bias in a non-randomized study. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1. Cochrane, 2020. [Google Scholar]
Thackeray 2012
- Thackeray R, Neiger BL, Smith AK, Van Wagenen SB. Adoption and use of social media among public health departments. BMC Public Health 2012;12(1):242. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tromholt 2016
- Tromholt H. The Facebook experiment: quitting Facebook leads to higher levels of well-being. Cyberpsychology, Behavior and Social Networking 2016;19(11):661-6. [DOI] [PubMed] [Google Scholar]
Uskov 2015
- Uskov VL, Bakken JP, Pandey A. The ontology of next generation smart classrooms. In: Uskov VL, Howlett R, Jain L , editors(s). Smart Education and Smart e-Learning (Smart Innovation, Systems and Technologies). Vol. 41. Springer International Publishing, 2015:33-41.
Vassilev 2014
- Vassilev I, Rogers A, Kennedy A, Koetsenruijter J. The influence of social networks on self-management support: a metasynthesis. BMC Public Health 2014;14(1):719. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vidanapathirana 2005
- Vidanapathirana J, Abramson MJ, Forbes A, Fairley C. Mass media interventions for promoting HIV testing. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD004775. [DOI: 10.1002/14651858.CD004775.pub2] [DOI] [PubMed] [Google Scholar]
Vitak 2014
- Vitak J. Unpacking social media's role in resource provision: variations across relational and communicative properties. Societies 2014;4:561-86. [Google Scholar]
We Are Social 2020
- We Are Social. Digital 2020: Global Digital Overview. https://wearesocial.com/global-digital-report-2019 2020:accessed 24 February 2021.
Welch 2016
- Welch V, Petkovic J, Pardo Pardo J, Rader T, Tugwell P. Interactive social media interventions to promote health equity: an overview of reviews. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice 2016;36(4):63-75. [http://www.phac-aspc.gc.ca/publicat/hpcdp-pspmc/36-4/ar-01-eng.php] [DOI] [PMC free article] [PubMed] [Google Scholar]
Westberg 2016
White 2006
- White JB, Langer EJ, Yariv L, Welch JC. Frequent social comparisons and destructive emotions and behaviors: the dark side of social comparisons. Journal of Adult Development 2006;13(1):36-44. [Google Scholar]
White 2018
- White H. Theory-based systematic reviews. Journal of Development Effectiveness 2018;10(1):17-38. [Google Scholar]
Whitehead 2006
- Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: levelling up part 1. WHO Regional Office for Europe. Available at http://www.euro.who.int/__data/assets/pdf_file/0010/74737/E89383.pdf (accessed 31 January 2017) 2006.
WHO 2002
- World Health Organization. Towards a common language for functioning, disability and health; ICF. World Health Organization, Geneva 2002.
Williams 2014
- Williams G, Hamm MP, Shulhan J, Vandermeer B, Hartling L. Social media interventions for diet and exercise behaviours: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 2014;4:e003926. [DOI: 10.1136/bmjopen-2013-003926] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wong 2016
- Wong CA, Ostapovich G, Kramer-Golinkoff E, Griffis H, Asch DA, Merchant RM. How US children's hospitals use social media: a mixed methods study. Healthcare 2016;4(1):15-21. [DOI] [PubMed] [Google Scholar]
Yoon 2014
- Yoon HJ, Tourassi G. Analysis of online social networks to understand information sharing behaviors through social cognitive theory. Annual ORNL Biomedical Science and Engineering Center Conference 2014;1-2:Available from: https://doi.org/10.1109/BSEC.2014.6867744. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Welch 2018
- Welch V, Petkovic J, Simeon R, Presseau J, Gagnon D, Hossain A, et al. Interactive social media interventions for health behaviour change, health outcomes, and health equity in the adult population.. Cochrane Database of Systematic Reviews 2018, Issue 2. Art. No: CD012932. [DOI: 10.1002/14651858.CD012932] [DOI] [Google Scholar]


