Abstract
Small cell lung cancer (SCLC) is exceptionally responsive to chemotherapy and radiotherapy. In relapsed patients, particularly in resistant/refractory cases, the progression of disease occurs rapidly with second-line agents. Topotecan (TOPO), a camptothecin analog, is the only agent able to increase overall survival (OS) compared with the best supportive care alone. However, the efficacy of platinum-based chemotherapy rechallenge or other agents has not been systematically explored. In the present review, published articles, which evaluated outcome and toxicity associated with TOPO or non-TOPO-based chemotherapy in patients with SCLC from inception to September 2020 were systematically searched and identified by searching the PubMed, EMBASE and Cochrane Library databases. The primary outcome of interest was the risk of death (OS), and the secondary endpoints were risk of progression progression-free survival (PFS), overall response rate (ORR) and G3-4 hematological toxicities. A total of nine studies were included in quantitative synthesis for a total of 1,689 patients. They included platinum-based rechallenge, anthracycline-based combinations or camptothecin analogs. TOPO did not improve OS with respect to other therapies [hazard ratio (HR), 0.92; 95% confidence interval (95% CI), 0.78-1.09; P=0.33]. Similarly, PFS was similar in the two arms (HR, 1.1; 95% CI, 0.72-1.67; P=0.66). The ORR was not statistically higher with non-TOPO agents (relative risk, 1.53; 95% CI, 0.95-2.48). In subgroup analysis, combination chemotherapy was associated with an improved PFS but not OS or ORR compared with TOPO alone (HR, 1.85; 95% CI, 1.52-2.24; P<0.01). The rates of G3-4 anemia, febrile neutropenia and neutropenia were similar. In conclusion, in patients with relapsed SCLC, TOPO was associated with a similar survival, PFS and ORR as other agents. However, polychemotherapy was associated with improved PFS.
Keywords: small cell lung cancer, topotecan, survival, meta-analysis
Introduction
Small cell lung cancer (SCLC) is an aggressive lung cancer disease with a dismal prognosis in advanced stages. It is highly responsive to chemotherapy and radiotherapy but usually recurs within a few months in patients with extensive-stage SCLC. Recently, a first-line platinum plus etoposide-based chemotherapy with atezolizumab improved outcomes in first-line settings (1,2). In relapsed patients, in particular for resistant/refractory cases (during or within three months from the last day of upfront therapy), the progression of disease occurs rapidly with second-line agents (3). Topotecan, a camptothecin analog, has been demonstrated to increase overall survival (OS) compared with the best supportive care alone and results in greater symptom management relative to polychemotherapy regimens (3,4). The primary toxicities of TOPO are hematologic, with most patients experiencing grade [G]3 or 4 neutropenia, anemia, or thrombocytopenia. Recently, a phase III study compared TOPO alone with a combination of carboplatin/etoposide as a rechallenge schedule in patients with sensitive relapsed SCLC (5). Although a combination did not increase median OS, it provided a two-month benefit in progression-free survival (PFS) and showed similar rates of severe (G3-4) hematological toxicities. Despite platinum-based combinations may have a role in platinum-sensitive SCLC TOPO remain one of the referent treatment in relapsed disease. Recently it has been compared with platinum-etoposide-based doublets and triplets so it is reasonable to consider TOPO a pivotal comparator as second line agent.
To update the current state of the art, we performed a systematic review and meta-analysis of second-line studies comparing TOPO with other agents in patients with relapsed SCLC.
Materials and methods
Identification of trials and inclusion criteria
Trials were identified through a comprehensive systematic search of Pubmed, EMBASE, and The Cochrane Library from inception, up to September 12th, 2020. All randomized clinical trials reporting on SCLC patients that examined the efficacy of TOPO compared with other agents or best supportive care as second-line therapy for relapsed (sensitive or refractory/resistant) disease and were published in the English language were identified. The search terms used to identify studies for the meta-analysis were: (‘small-cell lung carcinoma’[MeSH Major Topic] OR ‘small-cell lung cancer’[All Fields] OR ‘small-cell lung carcinoma’[All Fields] OR ‘sclc’[All Fields]) AND (‘recurrence’[MeSH Terms] OR ‘recurrence’[All Fields] OR ‘relapse’[All Fields] OR ‘relapses’[All Fields] OR ‘relapsing’[All Fields] OR ‘relapsed’[All Fields] OR ‘relapser’[All Fields] OR ‘relapsers’[All Fields] OR ‘previously treated’[All Fields] OR (‘recurrance’[All Fields] OR ‘recurrence’[MeSH Terms] OR ‘recurrence’[All Fields] OR ‘recurrences’[All Fields] OR ‘recurrencies’[All Fields] OR ‘recurrency’[All Fields] OR ‘recurrent’[All Fields] OR ‘recurrently’[All Fields] OR ‘recurrents’[All Fields]) OR ‘second line’[All Fields] OR (‘pretreat’[All Fields] OR ‘pretreated’[All Fields] OR ‘pretreating’[All Fields] OR ‘pretreatment’[All Fields] OR ‘pretreatments’[All Fields])) AND (‘topotecan’[MeSH Terms] OR ‘topotecan’[All Fields] OR (‘topotecan’[MeSH Terms] OR ‘topotecan’[All Fields])). Studies were excluded if they 1) were comparative observational series, 2) were phase 1 trials, and 3) compared different schedules or administration routes of TOPO.
Data extraction and risk of bias assessment
Two review authors (A.G. and F.P.) determined eligibility by reading the abstract of each study identified by the search. A third author (A.L.) independently read these studies and reached an agreement for trial inclusion. The primary outcome was OS defined as any death that occurred from the randomization date. The secondary outcomes were progression-free survival (PFS), overall response rate (ORR) and severe (grade [G] 3-4) adverse hematological events (anemia, thrombocytopenia, febrile neutropenia [FN] and neutropenia). Type of study, number of patients, median age, rate of PS 0-1 patients included, treatment setting, schedule of TOPO and the experimental arm, the HR for OS and PFS for TOPO vs. experimental arms, rate of overall response defined as the sum of partial and complete response, and rate of G3-4 hematological toxicities were extracted by two authors (F.P. and A.G.) independently from each study. For each trial, we assessed the risk of bias (‘low risk,’ ‘some concerns,’ or ‘high risk’) in the overall effect of TOPO on the outcome and serious adverse events using version 2 of the Cochrane Risk of Bias Assessment Tool (6). Risk of bias assessments were carried out independently by three of the investigators (A.G., F.P. and A.L.), with disagreements resolved through discussion. We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to assess the certainty of the evidence that TOPO increased OS compared with other agents in patients with relapsed SCLC (7).
Statistical analysis
We classified the trials according to the setting of the intervention (refractory or sensitive disease). The convention-sensitive disease was considered, as progression occurred at least three months after the end of first-line, platinum-based chemotherapy. The primary analysis was an inverse variance-weighted fixed or random-effect meta-analysis of HRs for OS and PFS and an inverse variance-weighted fixed or random-effect analysis using risk ratios (RRs) for ORR and rates of toxicity. We used Parmar's method if HRs were not reported in the study (8). We quantified inconsistency in associations among the trials using the I2 statistic and derived P-values for heterogeneity using the Cochran Q statistic. We report precise P-values. A P-value <0.05 denoted statistical significance. A meta-regression analysis was performed to examine the potential effect of the number of sensitive SCLC cases and death. All analyses were conducted using RevMan statistical software version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
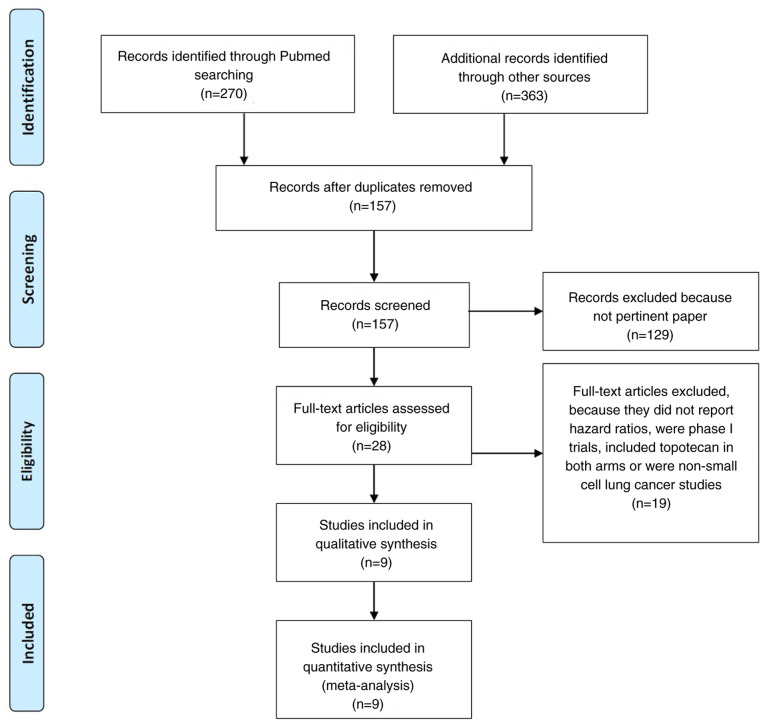
Results
Of 633 articles that met the preliminary criteria, we found nine eligible articles (4,5,9-14), which included five phase 3 and four phase 2 randomized trials that compared TOPO with other regimens (Fig. 1 and Table I). Overall, 1689 patients were included in these studies. In most of the studies, patients had a performance status of 0 or 1. The mean or median age was 64 years. Usually, the sensitive disease was considered when it recurs after 90 days. Intravenous, three-weekly TOPO was used in all studies except one where oral formulation was used. Combination chemotherapy was the experimental arm in n=3 trials, single agent in n=5, while best supportive care was the comparator arm in n=1 study. Sensitive disease ranged from 45 to 100% of included patients (median, 57.3%).
Figure 1.
Flow diagram of included studies.
Table I.
Characteristics of included studies.
| First author/s, year | Type of study | Patients, n | Setting (%) | PS 0-1, % | Median age, years | Topotecan schedule, mg/m2 | Exp arm | OS, months (Ctr vs. Exp) | PFS, months (Ctr vs. Exp) | ORR, % (Ctr vs. Exp) | G3-4 anemia, % (Ctr vs. Exp) | G3-4 thrombocy topenia, % (Ctr vs. Exp) | FN, % (Ctr vs. Exp) | G3-4 neutropenia, % (Ctr vs. Exp) | Risk of bias | (Refs.) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baize, 2020 | Phase 3 | 162 | Sensitive (100) | 92.5 | 64.5 | Oral 2.3 d1-5 q21 | Carboplatin + Etoposide | - | 2.7 vs. 4.7 | 25 vs. 49 | 21 vs. 24 | 36 vs. 31 | 13 vs. 6 | 24 vs. 13 | Low | (5) |
| Chiappori, 2016 | Phase 2 | 44 | Refractory (54.6); sensitive (45.4) | 36 | 64 | iv 1.5 d1-5 q21 | Linsitinib | 5.3 vs. 3.4 | 3 vs. 1.2 | 13.3 vs. 0 | 7.1 vs. 3.6 | 28.6 vs. 7.1 | - | 28.6 vs. NR | Uncertain | (14) |
| Evans, 2015 | Phase 2 | 179 | Refractory (49); sensitive (51) | 99.4 | 61 | iv 1.5 d1-5 q21 | Cabazitaxel | 6.8 vs. 5.2 | 3 vs. 1.4 | 10.1 vs. 0 | 26.1 vs. 3.4 | 45.5 vs. 4.5 | 22.7 vs. 18 | 78.4 vs. 56.8 | Moderate | (13) |
| Goto, 2016 | Phase 3 | 180 | Sensitive (100) | 97.2 | 64 | iv 1 d1-5 q21 | Cisplatin + Etoposide + Irinotecan | 12.5 vs. 18.2 | 3.6 vs. 5.7 | 25.5 vs. 33.8 | 27 vs. 85 | 28 vs. 41 | 7 vs. 31 | 85 vs. 84 | Low | (12) |
| Inoue, 2008 | Phase 2 | 59 | Refractory (39); sensitive (61) | 85 | 69 | iv 1 d1-5 q21 | Amrubicina | 8.4 vs. 8.4 | 2.2 vs. 3.5 | 13 vs. 38 | 30 vs. 21 | 40 vs. 28 | 3 vs. 14 | 87 vs. 93 | Moderate | (11) |
| Jotte, 2011 | Phase 2 | 76 | Sensitive (100) | 89.4 | 65.5 | iv 1.5 d1-5 q21 | Amrubicina | 7.6 vs. 9.2 | 3.3 vs. 4.5 | 15.4 vs. 44 | 30 vs. 25 | 61 vs. 39 | 9 vs. 10 | 78 vs. 71 | Moderate | (10) |
| O'Brien, 2006 | Phase 3 | 141 | Refractory (54); sensitive (46) | 70.2 | 59.2 | Oral 2.3 d1-5 q21 | BSC | 6.4 vs. 3.4 | 4 vs. NR (TTP) | 7 vs. 0 | 25 vs. 0 | 38 vs. 0 | 3 vs. 0 | 61 vs. 0 | Low | (3) |
| Von Pawel, 1999 | Phase 3 | 211 | Sensitive (100) | 78.6 | - | iv 1.5 d1-5 q21 | Cyclophosp hamide + Doxorubicin + Vincristine (CAV) | 6.2 vs. 6.1 | 3.3 vs. 3 (TTP) | 24.3 vs. 18.3 | 42.3 vs. 19.8 | 57.6 vs. 14.9 | - | 88.5 vs. 86.9 | Low | (4) |
| Von Pawel, 2014 | Phase 3 | 637 | Refractory (46.4); sensitive (53.6) | 97.9 | 61.5 | iv 1.5 d1-5 q21 | Amrubicina | 7.8 vs. 7.5 | 3.5 vs. 4.1 | 16.9 vs. 31.1 | 31 vs. 16 | 54 vs. 21 | 3 vs. 10 | 54 vs. 41 | Low | (9) |
PS, performance status; OS, overall survival; PFS, progression-free survival; ORR, overall response rate; FN, febrile neutropenia; TTP, time to progression; NR, not reported.
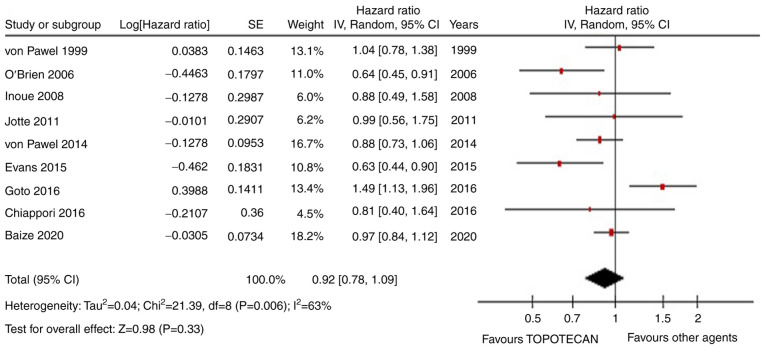
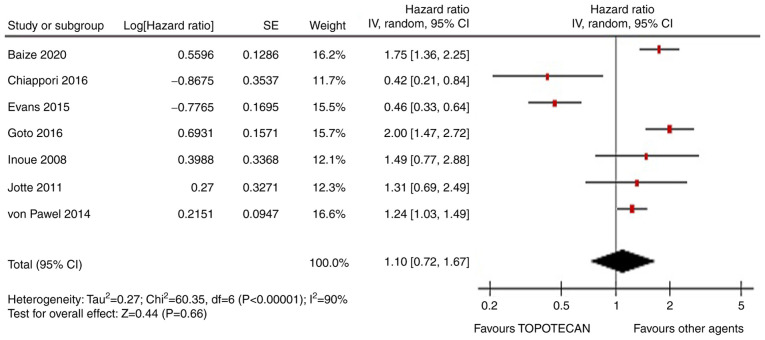
OS was not improved by TOPO with respect to other therapies (HR=0.92, 95% CI, 0.78-1.09; P=0.33; Fig. 2). Similarly, PFS was similar in the two arms (HR=1.1, 95% CI, 0.72-1.67; P=0.66; Fig. 3). The ORR was not statistically higher with non-TOPO agents (RR=1.53, 95% CI, 0.95-2.48; Fig. S1). In the meta-regression analysis, the rate of sensitive SCLC patients enrolled in each trial was significantly associated with OS (P=0.01). This means that agents different from TOPO are better in exquisite sensitive disease. In subgroup analysis, combination chemotherapy was associated with a better PFS but not OS or ORR than TOPO alone (HR=1.85, 95% CI, 1.52-2.24; P<0.01). The rates of G3-4 anemia, FN and neutropenia were similar. Instead, G3-4 thrombocytopenia was inferior in the experimental arms (RR=0.44, 95% CI, 0.26-0.74; P<0.01) (Fig. S2, Fig. S3, Fig. S4 and Fig. S5). In the primary analysis, both Begg's and Egger's tests were not significant for publication bias. There is little evidence that TOPO has a similar outcome to other agents in a mixed population of SCLC patients. However, we can recommend that in platinum-sensitive disease, combination agents are probably better and similarly or even less toxic than TOPO.
Figure 2.
Forest plot for overall survival of topotecan vs. other agents. SE, standard error; IV, inverse variance; df, degree of freedom; 95% CI, 95% confidence interval.
Figure 3.
Forest plot for progression-free survival of topotecan vs. other agents. SE, standard error; IV, inverse variance; df, degree of freedom; 95% CI, 95% confidence interval.
Discussion
SCLC is a subtype of lung cancer burdened by high mortality. The treatment of advanced SCLC has not changed over the years due to the high aggressiveness and refractoriness of the disease. Recently, two studies in a first-line setting with chemotherapy plus anti-programmed cell death ligand-1 (PDL-1) therapy showed an improved OS vs. chemo alone (1,2).
Most patients progressed after first-line treatment, and the best second-line strategy remains to be elucidated. Topotecan is the only drug approved for second-line treatment due to the head-to-head comparison with cyclophosphamide-doxorubicin-vincristine triplet (CAV regimen) and a placebo-controlled trial with oral administration. However, there is still a debate about the magnitude of its clinical benefit, and this meta-analysis shows how the use of drugs other than TOPO could give comparable outcomes. Based on our analysis, TOPO performs worse than other drugs in sensitive diseases, and combination therapy gives better response rates compared with a single agent. TOPO, as a second-line strategy, remains controversial, with conflicting evidence regarding its superiority in terms of survival, toxicity and response rates. TOPO seems to give less thrombocytopenia, while other toxicities are similar to combination therapies across the studies.
As second-line treatments in relapsed small-cell lung cancer are usually considered ‘palliative,’ the question remains whether using a standard drug is still a choice to be considered in young and fit older patients. Based on the literature, discouraging results have come from all agents tested, and superiority data do not support the use of TOPO over the others in common clinical practice. Even if combination regimens have more toxicity, the benefits are small and not durable. The rechallenge strategy with etoposide + platinum-based chemotherapy, however, at least in sensitive diseases, is a reasonable choice to have better response rates and progression-free survival with manageable toxicities (5). In this setting, the combination chemotherapy has shown high response rates (40-55%). For patients with refractory/resistant disease and a good performance status, inclusion in clinical trials is the preferred choice. Other agents as camptothecin analogues (irinotecan) have been tested in progressive disease (Table II). Despite a relatively high number of tumor responses in particular for combinations (range 12-52.9%) and median OS up to 10 months, neutropenia was consistent and this agent is not currently approved for use in western countries (15-24).
Table II.
Irinotecan studies in pretreated small cell lung cancer.
| First author/s, year | Type of study | Patients, n | Setting (%) | PS 0-1, % | Median age, years | Schedule, mg/m2 | OS, months | PFS, months | ORR, % | G3-4 anemia, % | G3-4 thrombocyt openia,% | FN,% | G3-4 neutropenia, % | (Refs.) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kondo, 2018 | Phase 2 | 30 | Sensitive (40); resistant (60) | 100 | 67 | CPT-11 100d1, 8 q21 | 10.4 | 4.1 | 43 | 13.3 | 3.3 | 6.6 | 36.7 | (15) |
| Trafalis, 2016 | Phase 2 | 32 | Resistant (100) | 82 | 63.5 | CPT-11 175 + bevacizumab 7.5 mg/kg q14 | 6 | 3 | 25 | 0 | 0 | 3.5 | 7.1 | (16) |
| Xenidis, 2011 | Phase 2 | 31 | Refractory (100) | 84 | 64 | CPT-11 125 + PLD 15 d1,14 q 28 | 3.16 | 1.86 | 12.9 | 3.2 | 0 | 6.5 | 0 | (17) |
| Ramalingam, 2010 | Phase 2 | 55 | Sensitive (51); refractory (49) | 95 | 61 | CPT-11 50 d1,8 + PAC 75 d1,8 q21 | 7.6 and 5.5a | 3 and 2a | 19.5 | 2 | 0 | 0 | 11 | (18) |
| Chen, 2009 | Phase 2 | 40 | Sensitive (100) | 85 | 65 | CPT-11 150 + CBDCA AUC5 d1 q 21 | 10 | - | 50 | 15 | 23 | 3 | 55 | (19) |
| Pallis, 2009 | Randomized phase 2 | 69 | Sensitive (52 vs. 35); refractory (47 vs. 64) | 85 vs. 94 | 60 vs. 65 | CPT-11 300 d8 + GEM 1000 d1, 8 q21 vs. CPT-11 300 d1 q21 | 8.6 and 5.7a (sensitive) vs. 8.6 and 3.8 (refractory) | 4.3 and 2.5 vs. 1.7 and 1.1 (sensitive and refractory) | 23.7 vs. 0 | 5.3 vs. 3.2 | 21 vs. 9.7 | 2.6 vs. 6.4 | 23 vs. 33 | (20) |
| Ohyanagi, 2008 | Phase 2 | 30 | Sensitive (66); refractory (34) | 65 | 90 | CPT-11 150 q21 + GEM 1000 d1,14 q21 | 14.4 | 3 | 36.7 | 3.3 | 3.3 | 0 | 43 | (21) |
| Rocha Lima, 2007 | Phase 2 | 71 | Sensitive (50); refractory (50) | 85 | 62 | CPT-11 100 d1,8 + GEM 1000 d1,8 q21 | 7.1 and 3.5a | 3.1. and 1.6 | 21 | 7.5 | 31 | 4.5 | 38.5 | (22) |
| Schuette, 2005 | Phase 2 | 35 | Sensitive (57); refractory (43) | 86 | 63 | CPT-11 100 d1,8 + GEM 1000 d1, 8 q 21 | 5.8 | 3.4 | 17 | 8.6 | 11.4 | 0 | 5.7 | (23) |
| Ichiki, 2003 | Phase 2 | 34 | Sensitive (71); refractory (29) | 68 | 69 | CPT-11 80 d1,8,15 + IFO 1,5 g/m2 d1-3 q 28 | 7.2 | - | 52.9 | 29.4 | 11.8 | 0 | 52.9 | (24) |
aSensitive and refractory disease. CPT-11, irinotecan; GEM, gemcitabine; IFO, Ifosfamide; CBDCA, carboplatin; PAC, paclitaxel; PDL, pegylated lyposomal doxorubicin; PS, performance status; OS, overall survival; PFS, progression-free survival; ORR, overall response rate; FN, febrile neutropenia.
In conclusion, TOPO is not better than other agents in relapsed SCLC, but there is weak evidence that it is inferior to platinum-based combinations in sensitive diseases.
Supplementary Material
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
All datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
FP, AG and AL contributed equally to manuscript writing. Data authentication is not applicable. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Horn L, Mansfield AS, Szczȩsna A, Havel L, Krzakowski M, Hochmair MJ, Huemer F, Losonczy G, Johnson ML, Nishio M, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379:2220–2229. doi: 10.1056/NEJMoa1809064. [DOI] [PubMed] [Google Scholar]
- 2.Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, Statsenko G, Hochmair MJ, Özgüroğlu M, Ji JH, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): A randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394:1929–1939. doi: 10.1016/S0140-6736(19)32222-6. [DOI] [PubMed] [Google Scholar]
- 3.O'Brien ME, Ciuleanu TE, Tsekov H, Shparyk Y, Cuceviá B, Juhasz G, Thatcher N, Ross GA, Dane GC, Crofts T. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol. 2006;24:5441–5447. doi: 10.1200/JCO.2006.06.5821. [DOI] [PubMed] [Google Scholar]
- 4.Von Pawel J, Schiller JH, Shepherd FA, Fields SZ, Kleisbauer JP, Chrysson NG, Stewart DJ, Clark PI, Palmer MC, Depierre A, et al. Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol. 1999;17:658–667. doi: 10.1200/JCO.1999.17.2.658. [DOI] [PubMed] [Google Scholar]
- 5.Baize N, Monnet I, Greillier L, Geier M, Lena H, Janicot H, Vergnenegre A, Crequit J, Lamy R, Auliac JB, et al. Carboplatin plus etoposide versus topotecan as second-line treatment for patients with sensitive relapsed small-cell lung cancer: An open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2020;21:1224–1233. doi: 10.1016/S1470-2045(20)30461-7. [DOI] [PubMed] [Google Scholar]
- 6.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343(d5928) doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. GRADE Working Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–2834. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 9.Von Pawel J, Jotte R, Spigel DR, O'Brien ME, Socinski MA, Mezger J, Steins M, Bosquée L, Bubis J, Nackaerts K, et al. Randomized phase III trial of Amrubicin versus topotecan as second-line treatment for patients with small-cell lung cancer. J Clin Oncol. 2014;32:4012–4018. doi: 10.1200/JCO.2013.54.5392. [DOI] [PubMed] [Google Scholar]
- 10.Jotte R, Conkling P, Reynolds C, Galsky MD, Klein L, Fitzgibbons JF, McNally R, Renschler MF, Oliver JW. Randomized phase II trial of single-agent amrubicin or topotecan as second-line treatment in patients with small-cell lung cancer sensitive to first-line platinum-based chemotherapy. J Clin Oncol. 2011;29:287–293. doi: 10.1200/JCO.2010.29.8851. [DOI] [PubMed] [Google Scholar]
- 11.Inoue A, Sugawara S, Yamazaki K, Maemondo M, Suzuki T, Gomi K, Takanashi S, Inoue C, Inage M, Yokouchi H, et al. Randomized phase II trial comparing amrubicin with topotecan in patients with previously treated small-cell lung cancer: North Japan lung cancer study group trial 0402. J Clin Oncol. 2008;26:5401–5406. doi: 10.1200/JCO.2008.18.1974. [DOI] [PubMed] [Google Scholar]
- 12.Goto K, Ohe Y, Shibata T, Seto T, Takahashi T, Nakagawa K, Tanaka H, Takeda K, Nishio M, Mori K, et al. Combined chemotherapy with cisplatin, etoposide, and irinotecan versus topotecan alone as second-line treatment for patients with sensitive relapsed small-cell lung cancer (JCOG0605): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2016;17:1147–1157. doi: 10.1016/S1470-2045(16)30104-8. [DOI] [PubMed] [Google Scholar]
- 13.Evans TL, Cho BC, Udud K, Fischer JR, Shepherd FA, Martinez P, Ramlau R, Syrigos KN, Shen L, Chadjaa M, Wolf M. Cabazitaxel versus topotecan in patients with small-cell lung cancer with progressive disease during or after first-line platinum-based chemotherapy. J Thorac Oncol. 2015;10:1221–1228. doi: 10.1097/JTO.0000000000000588. [DOI] [PubMed] [Google Scholar]
- 14.Chiappori AA, Otterson GA, Dowlati A, Traynor AM, Horn L, Owonikoko TK, Ross HJ, Hann CL, Abu Hejleh T, Nieva J, et al. A randomized phase II study of linsitinib (OSI·906) versus topotecan in patients with relapsed small·cell lung cancer. Oncologist. 2016;21:1163–1164. doi: 10.1634/theoncologist.2016-0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kondo R, Watanabe S, Shoji S, Ichikawa K, Abe T, Baba J, Tanaka J, Tsukada H, Terada M, Sato K, et al. A phase II study of irinotecan for patients with previously treated small-cell lung cancer. Oncology. 2018;94:223–232. doi: 10.1159/000486622. [DOI] [PubMed] [Google Scholar]
- 16.Trafalis DT, Alifieris C, Stathopoulos GP, Sitaras N. Phase II study of bevacizumab plus irinotecan on the treatment of relapsed resistant small cell lung cancer. Cancer Chemother Pharmacol. 2016;77:713–722. doi: 10.1007/s00280-016-2983-0. [DOI] [PubMed] [Google Scholar]
- 17.Xenidis N, Vardakis N, Varthalitis I, Giassas S, Kontopodis E, Ziras N, Gioulbasanis I, Samonis G, Kalbakis K, Georgoulias V. Α multicenter phase II study of pegylated liposomal doxorubicin in combination with irinotecan as second-line treatment of patients with refractory small-cell lung cancer. Cancer Chemother Pharmacol. 2011;68:63–68. doi: 10.1007/s00280-010-1427-5. [DOI] [PubMed] [Google Scholar]
- 18.Ramalingam SS, Foster J, Gooding W, Evans T, Sulecki M, Belani CP. Phase 2 study of irinotecan and paclitaxel in patients with recurrent or refractory small cell lung cancer. Cancer. 2010;116:1344–1349. doi: 10.1002/cncr.24753. [DOI] [PubMed] [Google Scholar]
- 19.Chen G, Huynh M, Fehrenbacher L, West H, Lara PN Jr, Yavorkovsky LL, Russin M, Goldstein D, Gandara D, Lau D. Phase II trial of irinotecan and carboplatin for extensive or relapsed small-cell lung cancer. J Clin Oncol. 2009;27:1401–1404. doi: 10.1200/JCO.2008.20.2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pallis AG, Agelidou A, Agelaki S, Varthalitis I, Pavlakou G, Gerogianni A, Papakotoulas P, Rapti A, Chandrinos V, Christophyllakis C, Georgoulias V. A multicenter randomized phase II study of the irinotecan/gemcitabine doublet versus irinotecan monotherapy in previously treated patients with extensive stage small-cell lung cancer. Lung Cancer. 2009;65:187–191. doi: 10.1016/j.lungcan.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Ohyanagi F, Horiike A, Okano Y, Satoh Y, Okumura S, Ishikawa Y, Nakagawa K, Horai T, Nishio M. Phase II trial of gemcitabine and irinotecan in previously treated patients with small-cell lung cancer. Cancer Chemother Pharmacol. 2008;61:503–508. doi: 10.1007/s00280-007-0496-6. [DOI] [PubMed] [Google Scholar]
- 22.Rocha-Lima CM, Herndon JE II, Lee ME, Lee ME, Atkins JN, Mauer A, Vokes E, Green MR. Phase II trial of irinotecan/gemcitabine as second-line therapy for relapsed and refractory small-cell lung cancer: Cancer and leukemia group B study 39902. Ann Oncol. 2007;18:331–337. doi: 10.1093/annonc/mdl375. Cancer and Leukemia Group B. [DOI] [PubMed] [Google Scholar]
- 23.Schuette W, Nagel S, Juergens S, Bork I, Wollschlaeger B, Schaedlich S, Blankenburg T. Phase II trial of gemcitabine/irinotecan in refractory or relapsed small-cell lung cancer. Clin Lung Cancer. 2005;7:133–137. doi: 10.3816/CLC.2005.n.029. [DOI] [PubMed] [Google Scholar]
- 24.Ichiki M, Rikimaru T, Gohara R, Koga T, Kawayama T, Matunami M, Oshita Y, Kamimura T, Aizawa H. Phase II study of irinotecan and ifosfamide in patients with advanced non-small cell lung cancer. Oncology. 2003;64:306–311. doi: 10.1159/000070286. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.