Abstract
Objectives
Due to the significant mortality and morbidity consequences of the coronavirus disease 2019 (COVID-19) pandemic among older adults, these individuals were urged to avoid going out in public and socializing with others, among other major disruptions to daily life. While these significant and often unavoidable disruptions have been shown to bear consequences for mental health, less attention has been devoted to behavioral changes, such as changes to sleeping or eating due to the COVID-19 pandemic, and their implications for emotional well-being.
Methods
We utilized data from a nationally representative survey of Medicare beneficiaries (aged 65 and older), which was administered between June and October 2020 (n = 3,122). We examine the relationship between self-reported changes to daily behaviors (e.g., sleep, drinking alcohol, and exercise) and emotional impacts of the COVID-19 pandemic (i.e., feelings of depression and anxiety about the COVID-19 pandemic) using stepwise hierarchical multivariable Poisson regression.
Results
We found that worse sleep quality, sleeping more or less, watching more television, and walking less were associated with more feelings of depression and anxiety about the COVID-19 pandemic.
Discussion
Previous research has shown a connection between the significant and often unavoidable disruptions to daily life due to the COVID-19 pandemic (e.g., sheltering in place) and adverse mental health symptoms. Less attention has been paid to potentially modifiable behaviors, such as sleep and exercise. Our findings highlight the behavioral changes associated with adverse emotional impacts among older adults during the COVID-19 pandemic. Future research may evaluate whether behavioral interventions may aim to attenuate the impact of pandemics on daily, modifiable behaviors to buffer against adverse emotional impacts.
Keywords: COVID-19, Life changes, Lifestyle, Mental health
The coronavirus disease 2019 (COVID-19) pandemic has at times presented profound insecurity, uncertainty, confusion, and isolation among the global population (Pfefferbaum & North, 2020). Research on previous infectious disease outbreaks has shown immediate adverse mental and emotional impacts (e.g., feelings of fear and anxiety), some of which attenuate with time, and others of which manifest as longer-term or chronic concerns, including depressive and anxiety disorders (Brooks et al., 2020). Several large, nationally representative surveys of adults in the United States have shown an increase in the prevalence of symptoms of depression and anxiety disorders concomitant with the COVID-19 pandemic (Bruine de Bruin, 2021; Czeisler et al., 2020; Ettman et al., 2020). Interestingly, these studies found that symptoms of those mental health disorders were particularly pronounced among young adults (Bruine de Bruin, 2021; Czeisler et al., 2020; Ettman et al., 2020), with a comparatively smaller proportion of older adults exhibiting these symptoms. Some gerontologists have suggested that lower prevalence of these symptoms of mental health disorders during the COVID-19 pandemic in older adults when compared with young adults may be in part due to resiliency that comes with older age (Vahia et al., 2020), but this does not mean the pandemic itself has not had any emotional impacts on older adults. To assess this would require examining feelings of depression and anxiety about the COVID-19 pandemic itself among older adults, as distinct from instruments designed to assess the prevalence of symptoms of depression and anxiety disorders in this population.
Why Older Adults May Be Depressed or Anxious About the COVID-19 Pandemic Itself
There are many reasons why older adults (aged 65 and older) may be anxious or depressed about the COVID-19 pandemic. First, the risk of death and serious illness due to the pandemic was at least two orders of magnitude higher among older adults than among young adults (Dowd et al., 2020; Undurraga et al., 2021). Thus, we could expect that older adults may well have experienced emotional impacts, such as fears and worry about their risks of dying or a loved one dying from COVID-19. In addition, with more than 1% of those older than 80 years of age having died from COVID-19, this age group is far more likely to have experienced a loss due to COVID-19 (Undurraga et al., 2021). Second, perhaps driven by fear or anxiety about becoming infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), older people have been much more compliant with stringent mitigation measures since the outset of the pandemic, such as quarantining and sheltering in place (Czeisler, Howard et al., 2021). Previous research conducted amidst the 2003 SARS outbreak in Canada found that the duration of quarantine (ranging from 2 to 66 days) was a strong predictor of the development of depression and anxiety postoutbreak (Hawryluck et al., 2004; Reynolds et al., 2008). Quarantine lasted far longer for most people during the COVID-19 pandemic, with older adults among those most strongly encouraged to abide by mitigation practices. It is therefore possible that the emotional impacts of the COVID-19 pandemic and its extended durations of quarantine increased the risk for feelings of depression and anxiety about the outbreak.
One nationwide survey administered in China examined emotional impacts of the pandemic, including feelings of depression and anxiety about the COVID-19 pandemic and its mitigation, and found that rates of these feelings were highest among both young adults (aged 18–30 years) and older adults (aged 60 and older; Qiu et al., 2020). Surveillance of a range of emotional impacts of the COVID-19 pandemic, such as feelings of depression and anxiety about the pandemic itself, particularly among groups at high risk for severe COVID-19 such as older adults, is critical to understand how this group is faring amidst the pandemic. Identifying the emotional impacts of the pandemic could facilitate efforts to attenuate their subsequent development into mental health disorders.
COVID-19-Related Disruptions to Daily Life and Adverse Emotional Impacts Among Older Adults
Public health COVID-19 mitigation policies, while vitally important to curb the spread of the highly contagious SARS-CoV-2, heralded significant disruptions to daily life, such as spending less time out in public and less time socializing (Courtemanche et al., 2020). These recommendations were widely adhered to among older adults. For instance, one study conducted by Krendl et al. of community-dwelling older adults found that 94% reported sheltering in place at the time of the interview, and 79% reported their social interactions were significantly disrupted due to the pandemic (Krendl & Perry, 2020).
Unfortunately, these significant disruptions to daily life associated with the mitigation of COVID-19 have been associated with adverse impacts on emotional and psychological well-being among older adults. The study conducted by Krendl et al. demonstrating high rates of compliance with COVID-19 mitigation measures among older adults also found that depression symptoms among this cohort were markedly higher in 2020 than in 2019 (Krendl & Perry, 2020). Another study among older adults found an association between the significant changes to daily life associated with mitigation of the COVID-19 pandemic and worries about COVID-19, such as fear of dying from COVID-19 (Barber & Kim, 2021).
The COVID-19 pandemic presented clear and significant barriers to daily life, some of which were not modifiable, such as policies imposing restrictions on going out in public and social distancing. While research has examined the relationship between these significant disruptions to daily life imposed by the pandemic and their emotional and psychological impacts, less attention has been paid to other daily behavioral changes, some of which may have been modifiable, such as changes to sleep, exercise, and other daily behavioral disruptions. One prospective cohort study of older adults in Spain found that good sleep quality was inversely associated with loneliness during the COVID-19 pandemic (Losada-Baltar et al., 2021). Similarly, another study among older adults in Israel found that sleep problems were positively associated with feelings of loneliness during the COVID-19 pandemic (Grossman et al., 2021). Therefore, research suggests that sleep disruptions during the pandemic are associated with more loneliness. However, less attention has been devoted to other behavioral domains affected by the pandemic, such as exercise and television watching.
Current Study
In this study, we assess the extent to which older adults reported changes to a comprehensive set of daily behaviors affected by the COVID-19 pandemic, including sleep, watching television, exercise, alcohol consumption, eating, and smoking or vaping, and their relationship to feelings of depression and anxiety about the COVID-19 pandemic. We also examine demographic factors, including gender, marital status, living alone, race/ethnicity, and age as potential mechanisms that might explain the relationship between changes to daily behaviors and feelings of depression and anxiety about the COVID-19 pandemic among older adults.
Method
We utilized data from the COVID-19 supplement to the National Health and Aging Trends Study (NHATS), an annual in-home, longitudinal, nationally representative survey of Medicare beneficiaries (aged 65 and older). The NHATS COVID-19 supplement was administered between June and October 2020 (Freedman & Hu, 2020). Of 3,188 of 3,961 eligible invited adults who responded to the COVID-19 supplement (response rate = 80.5%), 3,122 (97.9%) responded to the primary variables, including the daily behavior change and feelings of depression and anxiety about COVID-19 variables, and were therefore included in this analysis.
Measures
We examined changes to eight daily behaviors attributed to the COVID-19 pandemic (i.e., sleep quality, sleep duration, watching television, walking as exercise, doing vigorous activities, consuming alcohol, eating, and smoking or vaping) using either three-item scales for sleep duration, eating (more, less, and about the same), and sleep quality (better, worse, or about the same) or 4-point scales for walking for exercise, doing vigorous activities, consuming alcohol, and smoking or vaping (more, less, about the same, or did not do before or during). Responses of “did not do before or during” and “same amount” to walking for exercise, doing vigorous activities, consuming alcohol, and smoking or vaping were combined to indicate the behavior was unchanged or not practiced during the COVID-19 pandemic.
Emotional impacts of the COVID-19 pandemic broadly (i.e., regardless of whether someone was affected with COVID-19) were measured by assessing subjective feelings of distress about the COVID-19 pandemic. Specifically, NHATS participants were asked to report feelings of depression about COVID-19 (“During the COVID-19 outbreak, in a typical week, how sad or depressed have you felt about the outbreak”) and feelings of anxiety about the COVID-19 pandemic (“During the COVID-19 outbreak, in a typical week, how worried or anxious have you felt about the outbreak”). This is consistent with previous research assessing psychological trauma and symptoms (Hansen et al., 2010). Responses to feelings of depression and anxiety about the COVID-19 pandemic were assessed using 4-point Likert-type scales (not at all, mild, moderate, severe). We defined the outcomes as responding either “moderate” or “severe” to the questions assessing feelings of depression or anxiety about COVID-19 to facilitate interpretation of the results.
Statistical Analysis
Adjusted prevalence ratios (aPRs) estimating the association between changes to daily behaviors and whether feelings of depression and anxiety about the COVID-19 pandemic were generated using multivariable Poisson regression with robust standard errors, adjusted for demographic factors and health conditions. Hierarchical backward stepwise selection was used to select daily behavior changes most strongly associated with feelings of depression and anxiety about the COVID-19 pandemic. The threshold for model retention was set at p < .20.
As a sensitivity analysis, we explored the relationship between the emotional impact measures employed in this study (i.e., feelings of depression and anxiety about COVID-19) from the COVID-19 supplement and measures of adverse mental health symptoms administered in the prior survey wave (2019), including depression and anxiety as measured by the Patient Health Questionnaire-2 (PHQ-2) and the General Anxiety Disorder-2 (GAD-2). The PHQ-2 assesses depression symptoms by asking “Over the last month, how often have you had little interest or pleasure in doing things” and “… felt down, depressed, or hopeless.” The GAD-2 assesses anxiety symptoms by asking participants “Over the last month, how often have you felt nervous, anxious, or on edge” and “… been unable to stop or control worrying?” All response categories are 0 (not at all), 1 (several days), 2 (more than half the days), and 3 (nearly every day). Items for both the PHQ-2 and GAD-2 are summed for separate scales, and scores of 3 or higher indicate further diagnostic evaluation is needed (Kroenke et al., 2003; Spitzer et al., 2006), yet we retain the six-level variables for the sensitivity analysis. We used longitudinal data from previous survey responses to examine whether feelings of depression or anxiety prior to the pandemic were associated with current feelings of depression or anxiety about the COVID-19 pandemic. Logistic regression models did not detect a significant association between prepandemic response to the PHQ-2 and feelings of depression about the COVID-19 pandemic (p = .378) or prepandemic response to the GAD-2 and feelings of anxiety about the COVID-19 pandemic (p = .349). Taken together, these findings suggest that the measures of feelings of depression and anxiety about the COVID-19 pandemic may be distinct from prior symptoms of depression and anxiety disorders as measured by the PHQ-2 and GAD-2 in 2019.
Potential interactions between demographic factors (married or living with a partner vs. widowed, divorced, or never married; living alone vs. with others; gender; race/ethnicity; and age older than 75 vs. younger), daily behavior changes, and feelings of depression and anxiety about the COVID-19 pandemic were examined. Next, we conducted stratified analyses to examine daily behavior changes and feelings of depression and feelings of anxiety about the COVID-19 pandemic by demographic factors (gender, marital status, living alone, race/ethnicity, and age). All models controlled for gender and health conditions that were noted to have a significant univariate association with the outcome, with the exception of stratified analyses by gender, which only adjusted for health conditions. Significance was considered at p < .05. All analyses were conducted in Stata version 16 (College Station, TX).
Results
The prevalences of older adults who reported feelings of depression and anxiety about COVID-19 were 22.7% and 28.3%, respectively. Women reported both more feelings of depression and anxiety about COVID-19 than did men (depression, 69.3% vs. 30.7%, p < .001; anxiety, 63.9% vs. 36.1%, p < .001). Regarding health conditions, those with arthritis reported more feelings of depression and anxiety about COVID-19 than did those without arthritis (depression, 30.9% vs. 18.5%, p < .01); those with osteoporosis reported more feelings of depression and anxiety about COVID-19 than did those without osteoporosis (depression, 41.3% vs. 19.2%; anxiety, 33.3% vs. 22.6%, p < .001); those with lung disease reported less depression and anxiety than those without lung disease (depression, 20.0% vs. 21.6%; anxiety, 25.0% vs. 27.0%, p < .01); those with dementia or Alzheimer’s disease reported more feelings of depression about COVID-19 (22.5% vs. 23.2%, p < .05) but less feelings of anxiety (12.8% vs. 29.1%, p < .001). Demographic characteristics by feelings of depression and anxiety about COVID-19 are displayed in Table 1.
Table 1.
Demographic and Health Condition Characteristics of the Sample by Feelings of Depression and Anxiety About the COVID-19 Pandemic (N = 3,122)
| Feelings of depression about the COVID-19 pandemic | Feelings of anxiety about the COVID-19 pandemic | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 3,116) | No feelings of depression about COVID-19 (n = 2,409) | Feelings of depression about COVID-19 (n = 707) | Chi-square | p | Total (n = 3,119) | No feelings of anxiety about COVID-19 (n = 2,237) | Feelings of anxiety about COVID-19 (n = 882) | Chi-square | p | |||||
| n | n | % | n | % | n | n | % | n | % | |||||
| Total (n = 3,116) | No feelings of depression about COVID-19 (n = 2,409) | Feelings of depression about COVID-19 (n = 707) | Chi-square | p | Total (n = 3,119) | No feelings of anxiety about COVID-19 (n = 2,237) | Feelings of anxiety about COVID-19 (n = 882) | Chi-square | p | |||||
| n | n | % | n | % | n | n | % | n | % | |||||
| Gender | 49.1 | <.001 | 18.2 | <.001 | ||||||||||
| Male | 1,313 | 1,096 | 45.5 | 217 | 30.7 | 1,312 | 994 | 44.4 | 318 | 36.1 | ||||
| Female | 1,803 | 1,313 | 54.5 | 490 | 69.3 | 1,807 | 1243 | 55.6 | 564 | 63.9 | ||||
| Age (years) | 6.9 | .232 | 9.3 | .097 | ||||||||||
| 65–69 | 39 | 32 | 1.3 | 7 | 1.0 | 39 | 30 | 1.3 | 9 | 1.0 | ||||
| 70–74 | 694 | 533 | 22.1 | 161 | 22.8 | 696 | 473 | 21.1 | 223 | 25.3 | ||||
| 75–79 | 866 | 692 | 28.7 | 174 | 24.6 | 868 | 630 | 28.2 | 238 | 27.0 | ||||
| 80–84 | 699 | 534 | 22.2 | 165 | 23.3 | 697 | 506 | 22.6 | 191 | 21.7 | ||||
| 85–89 | 504 | 387 | 16.1 | 117 | 16.5 | 505 | 379 | 16.9 | 126 | 14.3 | ||||
| 90+ | 314 | 231 | 9.6 | 83 | 11.7 | 314 | 219 | 9.8 | 95 | 10.8 | ||||
| Marital status | 12.0 | .038 | 7.3 | .197 | ||||||||||
| Married | 1,496 | 1,179 | 49.0 | 317 | 44.8 | 1,499 | 1,067 | 47.7 | 432 | 49.0 | ||||
| Living with a partner | 60 | 47 | 2.0 | 13 | 1.8 | 60 | 44 | 2.0 | 16 | 1.8 | ||||
| Separated | 40 | 30 | 1.2 | 10 | 1.4 | 40 | 25 | 1.1 | 15 | 1.7 | ||||
| Divorced | 377 | 284 | 11.8 | 93 | 13.2 | 376 | 270 | 12.1 | 106 | 12.0 | ||||
| Widowed | 1,036 | 776 | 32.2 | 260 | 36.8 | 1,038 | 744 | 33.3 | 294 | 33.3 | ||||
| Never married | 106 | 92 | 3.8 | 14 | 2.0 | 105 | 86 | 3.8 | 19 | 2.2 | ||||
| Worked for pay recently | 0.7 | .691 | 4.2 | .125 | ||||||||||
| Yes | 365 | 288 | 12.7 | 77 | 11.9 | 366 | 276 | 13.2 | 90 | 10.9 | ||||
| No | 2,231 | 1728 | 76.1 | 503 | 77.7 | 2,233 | 1582 | 75.5 | 651 | 79.0 | ||||
| Retired | 321 | 254 | 11.2 | 67 | 10.4 | 320 | 237 | 11.3 | 83 | 10.1 | ||||
| Race | 5.4 | .374 | 5.4 | .364 | ||||||||||
| White, non-Hispanic | 2,367 | 1,831 | 77.1 | 536 | 76.6 | 2,372 | 1,715 | 77.8 | 657 | 75.3 | ||||
| Black, non-Hispanic | 514 | 396 | 16.7 | 118 | 16.9 | 512 | 362 | 16.4 | 150 | 17.2 | ||||
| Other* | 65 | 55 | 2.3 | 10 | 1.4 | 65 | 43 | 2.0 | 22 | 2.5 | ||||
| Hispanic | 128 | 92 | 3.9 | 36 | 5.1 | 128 | 84 | 3.8 | 44 | 5.0 | ||||
| Heart attack | 2.6 | .107 | 1.3 | .250 | ||||||||||
| Yes | 57 | 39 | 68.4 | 18 | 31.6 | 57 | 37 | 64.9 | 20 | 35.1 | ||||
| No | 3,054 | 2,365 | 77.4 | 689 | 22.6 | 3,057 | 2,196 | 71.8 | 861 | 28.2 | ||||
| Heart disease | 2.0 | .362 | 1.5 | .484 | ||||||||||
| Yes | 70 | 52 | 74.3 | 18 | 25.7 | 70 | 49 | 70.0 | 21 | 30.0 | ||||
| No | 2,346 | 1,827 | 77.9 | 519 | 22.1 | 2,348 | 1,696 | 72.2 | 652 | 27.8 | ||||
| High blood pressure | 0.5 | .782 | 0.6 | .751 | ||||||||||
| Yes | 43 | 34 | 79.1 | 9 | 20.9 | 44 | 30 | 68.2 | 14 | 31.8 | ||||
| No | 816 | 624 | 76.5 | 192 | 23.5 | 818 | 581 | 71.0 | 237 | 29.0 | ||||
| Arthritis | 13.4 | .001 | 18.3 | <.001 | ||||||||||
| Yes | 81 | 56 | 69.1 | 25 | 30.9 | 81 | 54 | 66.7 | 27 | 33.3 | ||||
| No | 831 | 677 | 81.5 | 154 | 18.5 | 831 | 643 | 77.4 | 188 | 22.6 | ||||
| Osteoporosis | 49.2 | <.001 | 27.5 | <.001 | ||||||||||
| Yes | 75 | 44 | 58.7 | 31 | 41.3 | 75 | 40 | 53.3 | 35 | 46.7 | ||||
| No | 2,046 | 1,654 | 80.8 | 392 | 19.2 | 2,049 | 1,523 | 74.3 | 526 | 25.7 | ||||
| Diabetes | 1.2 | .555 | 1.9 | .394 | ||||||||||
| Yes | 18 | 12 | 66.7 | 6 | 33.3 | 18 | 11 | 61.1 | 7 | 38.9 | ||||
| No | 2,241 | 1,735 | 77.4 | 506 | 22.6 | 2,245 | 1,622 | 72.2 | 623 | 27.8 | ||||
| Lung disease | 7.8 | .020 | 10.5 | .005 | ||||||||||
| Yes | 872 | 32 | 80.0 | 8 | 20.0 | 40 | 30 | 75.0 | 10 | 25.0 | ||||
| No | 872 | 1,893 | 78.4 | 523 | 21.6 | 2,417 | 1,765 | 73.0 | 652 | 27.0 | ||||
| Stroke | 0.0 | .988 | 0.0 | .891 | ||||||||||
| Yes | 62 | 48 | 77.4 | 14 | 22.6 | 62 | 44 | 71.0 | 18 | 29.0 | ||||
| No | 3,049 | 2,358 | 77.3 | 691 | 22.7 | 3,052 | 2,190 | 71.8 | 862 | 28.2 | ||||
| Dementia or Alzheimer’s | 7.0 | .030 | 16.1 | <.001 | ||||||||||
| Yes | 40 | 31 | 77.5 | 9 | 22.5 | 39 | 34 | 87.2 | 5 | 12.8 | ||||
| No | 2,922 | 2,245 | 76.8 | 677 | 23.2 | 2,925 | 2,073 | 70.9 | 852 | 29.1 | ||||
| Cancer | 0.0 | .910 | 0.4 | .550 | ||||||||||
| Yes | 192 | 149 | 77.6 | 43 | 22.4 | 192 | 134 | 69.8 | 58 | 30.2 | ||||
| No | 2,919 | 2,255 | 77.3 | 664 | 22.7 | 2,922 | 2,098 | 71.8 | 824 | 28.2 | ||||
Note: COVID-19 = coronavirus disease 2019.
*Other races included American Indian, Asian, and Hawaiian Islander.
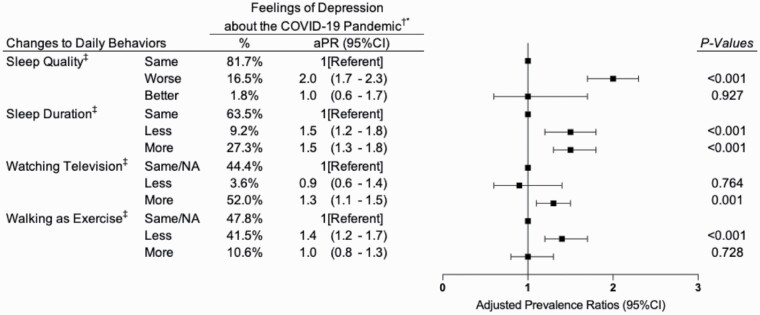
Eight daily behaviors were entered into the covariate-adjusted stepwise multivariable Poisson regression. Four behaviors met the criteria for inclusion in the final adjusted models: sleep quality, sleep duration, walking as exercise, and watching television. Changes to daily life associated with feeling depressed about COVID-19 were worse sleep quality (aPR, 2.0 [95% CI, 1.7–2.3]), sleeping less (aPR, 1.5 [95% CI, 1.2–1.8]), sleeping more (aPR, 1.5 [95% CI, 1.3–1.8]), watching more television (aPR, 1.3 [95% CI, 1.1–1.5]), and doing less walking as exercise (aPR, 1.4 [95% CI, 1.2–1.7]; Figure 1).
Figure 1.
Hierarchical stepwise covariate-adjusted Poisson regression models with robust standard errors examining changes to daily behaviors and feelings of depression about the coronavirus disease 2019 (COVID-19) pandemic (N = 3,122). Notes: *Adjusted prevalence ratios (aPRs) represent models that adjust for confounders identified in bivariate analyses, including gender and health conditions (arthritis, osteoporosis, lung disease, and Alzheimer’s disease or dementia). †For sleep quality, sleep duration, and eating (including snacks), the reference category is “Same amount,” now labeled as “Same.” For drinking alcohol, smoking or vaping, watching TV, walking for exercise, and doing vigorous activities, the response option “Did not do before or during,” which was combined with “Same amount” as the reference category, is now labeled as “Same/NA.”
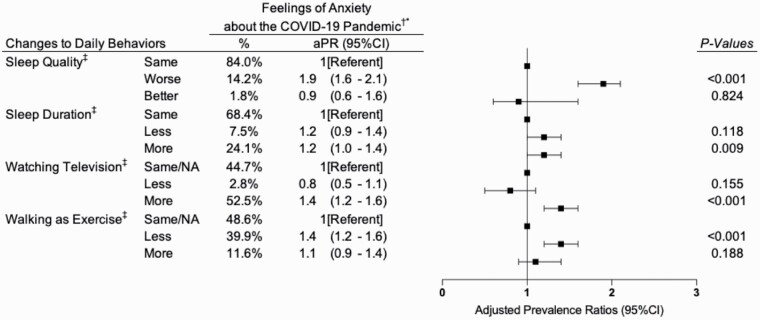
Changes to daily life associated with feeling anxious about COVID-19 were worse sleep quality (aPR, 1.9 [95% CI, 1.6–2.1]), sleeping more (aPR, 1.2 [95% CI, 1.0–1.4]), watching more television (aPR, 1.4 [95% CI, 1.2–1.6]), and doing less walking as exercise (aPR, 1.4 [95% CI, 1.2–1.6]; Figure 2).
Figure 2.
Hierarchical stepwise covariate-adjusted Poisson regression models with robust standard errors examining changes to daily behaviors and feelings of anxiety about the coronavirus disease 2019 (COVID-19) pandemic (N = 3,122). Notes: *Adjusted prevalence ratios (aPRs) represent models that adjust for confounders identified in bivariate analyses, including gender and health conditions (arthritis, osteoporosis, lung disease, and Alzheimer’s disease or dementia). †For sleep quality, sleep duration, and eating (including snacks), the reference category is “Same amount,” now labeled as “Same.” For drinking alcohol, smoking or vaping, watching TV, walking for exercise, and doing vigorous activities, the response option “Did not do before or during,” which was combined with “Same amount” as the reference category, is now labeled as “Same/NA.”
Results from our analyses with interaction terms in the stepwise multivariable Poisson regression did not reveal any evidence of moderation by demographic variables. The level of significance for each interaction term was p > .05.
Stratified analyses examining daily behavioral changes and feelings of depression about COVID-19 and feelings of anxiety about COVID-19 by demographic factors revealed similar patterns within each demographic category to the overall, nonstratified stepwise multivariable-adjusted Poisson regression. Specifically, as seen in the nonstratified multivariable-adjusted Poisson regression, stratified analyses revealed that worse sleep quality was associated with feelings of depression and anxiety about COVID-19 for all demographic subgroups (p < .05). Stratified analyses also revealed that sleeping more or less was associated with feelings of depression and anxiety about COVID-19 in nearly all demographic categories (p < .05), as were both watching more television and walking less as exercise (p < .05). As a reference, results of the stratified analyses are displayed in Supplementary Material.
Discussion
Using data from the NHATS COVID-19 supplement, we examine the changes to daily life associated with the pandemic and their relationship to adverse emotional impacts, including feelings of depression and anxiety about the COVID-19 pandemic. Using hierarchical regression, we identified poor sleep quality, a change in sleep duration, increased television watching, and doing less walking as daily behavior changes associated with increased burden of feelings of depression or anxiety about the COVID-19 pandemic among older adults.
We did not find evidence that these relationships varied by demographic factors. Instead, stratified analyses revealed that daily behavioral changes identified in the covariate-adjusted stepwise Poisson regression were associated with feelings of depression and anxiety about the COVID-19 pandemic in each demographic category examined, suggesting that daily behavioral changes and their relationship to feelings of depression and anxiety about the COVID-19 pandemic had a profound impact on this population overall. Furthermore, demographic characteristics that previous work has shown to buffer against adverse mental health consequences, such as marital status (Stokes & Moorman, 2018), were not protective against adverse impacts of daily behavioral changes on feelings of depression or anxiety about COVID-19.
Our findings on daily lifestyle behaviors and mental health are consistent with and extend prior research. Previous studies outside the context of pandemics have demonstrated associations between both insomnia (Pigeon et al., 2017) and sedentary behavior (de Rezende et al., 2014) and diminished emotional well-being and symptoms of depression and anxiety. According to research conducted during the COVID-19 pandemic, changes to daily life, such as spending more time alone sheltering in place, were extremely common (>90%) among older adults during the early months of the COVID-19 pandemic, but also associated with depression symptoms (Krendl & Perry, 2020). On a positive note, according to research conducted by Losada-Baltar et al. (2021), older adults in Spain who were able to obtain favorable sleep quality during the COVID-19 pandemic demonstrated a lower risk for loneliness. Understanding factors that contribute to emotional health and well-being among older adults about the pandemic among older adults, such as daily behavioral changes, can guide future efforts to prevent symptom worsening.
It is striking that we observed that approximately one quarter to one third of older adults reported either feelings of depression and anxiety about the COVID-19 pandemic itself, respectively. Our sensitivity analyses revealed that the emotional impacts assessed in our study, including feelings of depression and anxiety about COVID-19, were distinct from other assessments of depression and anxiety symptoms that were available in the prior prepandemic wave of NHATS. On the one hand, these findings suggest that the emotional impacts assessed in this study may be distinct from the adverse mental health symptoms assessed using the PHQ-2 and GAD-2, but these measures were captured at different time points; therefore, their comparison warrants further exploration.
The strengths of this study include the large, representative sample of the NHATS study recruited using probabilistic methods and assessment of a range of demographic variables and daily behaviors with feelings of depression and anxiety about the COVID-19 pandemic. Limitations include that not all NHATS participants completed the COVID-19 supplement, so the analytic sample may not remain fully representative of U.S. Medicare beneficiaries. In addition, the questions assessing feelings of depression and anxiety about the COVID-19 pandemic are not yet validated to detect clinically relevant measures of depression. Nevertheless, these concerns in some cases could reflect clinically relevant mental health concerns or adverse mental health symptoms. Also, the feelings of depression and anxiety about the COVID-19 pandemic that we examined in this study could worsen to chronic mental health conditions, particularly as the COVID-19 pandemic continues. Finally, it is possible that the associations observed in this study between daily behavioral changes and feelings of depression or anxiety about COVID-19 are bidirectional. For example, it is possible that consuming news stories on television may exacerbate feelings of depression or anxiety about COVID-19 (Czeisler, Wiley et al., 2021).
In summary, this study presented evidence that more than one quarter of older adults are experiencing depression and anxiety about COVID-19. In addition, we identify the behavioral changes that had the strongest association with feelings of depression and anxiety due to COVID-19, which were worse sleep quality, sleeping more or less, watching television, and walking less, all as compared to before the COVID-19 pandemic. These relationships remained significant in analyses stratifying by demographic factors. Given the robust relationship observed in this study between worse sleep quality and feelings of depression and anxiety about COVID-19 in all demographic categories, future research is needed to evaluate whether behavioral interventions to improve sleep quality among older adults can reduce feelings of depression and anxiety due to the pandemic.
Supplementary Material
Acknowledgments
The authors respectfully acknowledge the early contribution of Ms. Allison Chou to this manuscript.
Contributor Information
Rebecca Robbins, Division of Sleep and Circadian Disorders, Brigham & Women’s Hospital, Boston, Massachusetts, USA; Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, USA.
Matthew D Weaver, Division of Sleep and Circadian Disorders, Brigham & Women’s Hospital, Boston, Massachusetts, USA; Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, USA.
Mark É Czeisler, Turner Institute for Brain and Mental Health, Monash University, Melbourne, Victoria, Australia; Institute for Breathing and Sleep, Austin Health, Melbourne, Victoria, Australia.
Laura K Barger, Division of Sleep and Circadian Disorders, Brigham & Women’s Hospital, Boston, Massachusetts, USA; Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, USA.
Stuart F Quan, Division of Sleep and Circadian Disorders, Brigham & Women’s Hospital, Boston, Massachusetts, USA; Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, USA.
Charles A Czeisler, Division of Sleep and Circadian Disorders, Brigham & Women’s Hospital, Boston, Massachusetts, USA; Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, USA.
Funding
This study was supported by grants from the National Institutes of Health and the National Institute for Occupational Health and Safety, Centers for Disease Control and Prevention (grant numbers: K01HL150339 [to R. Robbins], R01OH011773 [to M. D. Weaver, L. K. Barger, R. Robbins, and C. A. Czeisler], and R56HL151637 [to M. D. Weaver, L. K. Barger, R. Robbins, S. F. Quan, and C. A. Czeisler]). M. É. Czeisler reports funding from the CDC Foundation funded by BNY Mellon, WHOOP Inc., and Hopelab Inc., outside of the submitted work.
Competing Interests
R. Robbins reports personal fees from Sleep Cycle AB, Rituals Cosmetics B.V., Denihan Hospitality, With Deep Inc., Wave Sleep, and Bynacht. M. D. Weaver reports personal fees from the University of Pittsburgh and the National Sleep Foundation. S. F. Quan has served as a consultant for Best Doctors, Jazz Pharmaceuticals, and WhisperSom. M. É. Czeisler reports a grant from the Australian–American Fulbright Commission funded by The Kinghorn Foundation, along with personal fees from Vanda Pharmaceuticals. L. K. Barger reports personal fees from the University of Pittsburgh, CurAegis, Casis, Puget Sound Pilots, and Boston Children’s Hospital. C. A. Czeisler reports grants/contracts to BWH from Dayzz Live Well Ltd., Delta Airlines, FAA, Jazz Pharmaceuticals, NHLBI, NIA, NIOSH, NASA, Puget Sound Pilots, Regeneron Pharmaceuticals/Sanofi, and DOD; is/was a paid consultant or received lecture fees from Emory University, Inselspital Bern, UCLA, Institute of Digital Media and Child Development, Klarman Family Foundation, National Council for Mental Wellbeing, National Sleep Foundation, Physician’s Seal, Sleep Research Society Foundation, Tencent Holdings Ltd., Teva Pharma Australia, With Deep Inc., and Vanda Pharmaceuticals Inc., in which C. A. Czeisler also holds an equity interest; received travel support from Aspen Brian Institute, Bloomage International Investment Group, Inc., UK Biotechnology and Biological Sciences Research Council, Bouley Botanical, Dr. Stanley Ho Medical Development Foundation, European Biological Rhythms Society, German National Academy of Sciences (Leopoldina), National Safety Council, National Sleep Foundation, Stanford Medical School Alumni Association, Tencent Holdings Ltd., and Vanda Pharmaceuticals Inc.; receives research/education support through BWH from Arbor Pharmaceuticals, Avadel Pharmaceuticals, Bryte Foundation, Cephalon, Alexandra Drane, DR Capital Ltd, Eisai, Mary Ann & Stanley Snider via Combined Jewish Philanthropies, Harmony Biosciences LLC, Jazz Pharmaceuticals PLC Inc., Johnson & Johnson, NeuroCare, Inc., Optim, Philips Respironics Inc./Philips Homecare Solutions, Regeneron Pharmaceuticals, Regional Home Care, ResMed, San Francisco Bar Pilots, Teva Pharmaceuticals Industries Ltd., Sanofi SA, Optum, ResMed, San Francisco Bar Pilots, Sanofi, Sleep Cycle AB, Schneider, Simmons, Sleep Number, Sysco, Vanda Pharmaceuticals; is/was an expert witness in legal cases, including those involving Advanced Power Technologies, Aegis Chemical Solutions LLC, Amtrak; Casper Sleep Inc., C&J Energy Services, Catapult Energy Services Group, LLC, Covenant Testing Technologies, LLC, Dallas Police Association, Enterprise Rent-A-Car, Espinal Trucking/Eagle Transport Group LLC/Steel Warehouse Inc., FedEx, Greyhound Lines Inc./Motor Coach Industries/FirstGroup America, PAR Electrical Contractors Inc., Product & Logistics Services LLC/Schlumberger Technology Corp/Gelco Fleet Trust, Puckett Emergency Medical Services LLC, Puget Sound Pilots, Union Pacific Railroad, UPS, and Vanda Pharmaceuticals; serves as the incumbent of an endowed professorship provided to Harvard University by Cephalon, Inc.; and receives royalties from McGraw Hill, and Philips Respironics for the Actiwatch-2 and Actiwatch Spectrum devices. C. A. Czeisler’s interests were reviewed and are managed by the Brigham and Women’s Hospital and Mass General Brigham in accordance with their conflict of interest policies.
Author Contributions
R. Robbins and M. D. Weaver had full access to the data and performed the statistical analysis. The study’s conceptual approach was developed with all authors’ feedback. R. Robbins and M. D. Weaver conducted the statistical analysis. The manuscript was drafted by R. Robbins. M. D. Weaver, L. K. Barger, S. F. Quan, and C. A. Czeisler, and M. É. Czeisler provided substantial intellectual contributions to the draft and critical revisions. All authors reviewed and approved the final version of this manuscript.
Data Availability
The data used in this study are publicly available (released: December 17, 2020; www.nhats.org).
References
- Barber, S. J., & Kim, H. (2021). COVID-19 worries and behavior changes in older and younger men and women. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e17–e23. doi: 10.1093/geronb/gbaa068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England), 395(10227), 912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin, W. (2021). Age differences in COVID-19 risk perceptions and mental health: Evidence from a national U.S. survey conducted in March 2020. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e24–e29. doi: 10.1093/geronb/gbaa074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche, C., Garuccio, J., Le, A., Pinkston, J., & Yelowitz, A. (2020). Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Affairs (Project Hope), 39(7), 1237–1246. doi: 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- Czeisler, M. É., Howard, M. E., Robbins, R., Barger, L. K., Facer-Childs, E. R., Rajaratnam, S. M. W., & Czeisler, C. A. (2021). Early public adherence with and support for stay-at-home COVID-19 mitigation strategies despite adverse life impact: A transnational cross-sectional survey study in the United States and Australia. BMC Public Health, 21(1), 503. doi: 10.1186/s12889-021-10410-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. doi: 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler, M. É., Wiley, J. F., Facer-Childs, E. R., Robbins, R., Weaver, M. D., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2021). Mental health, substance use, and suicidal ideation during a prolonged COVID-19-related lockdown in a region with low SARS-CoV-2 prevalence. Journal of Psychiatric Research, 140, 533–544. doi: 10.1016/j.jpsychires.2021.05.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Rezende, L. F. M., Rey-López, J. P., Matsudo, V. K. R., & do Carmo Luiz, O. (2014). Sedentary behavior and health outcomes among older adults: A systematic review. BMC Public Health, 14, 333. doi: 10.1186/1471-2458-14-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd, J. B., Andriano, L., Brazel, D. M., Rotondi, V., Block, P., Ding, X., Liu, Y., & Mills, M. C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences of the United States of America, 117(18), 9696–9698. doi: 10.1073/pnas.2004911117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686. doi: 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V., & Hu, M. (2020). COVID-19 supplement to the National Health and Aging Trends Study user guide. Beta release. Johns Hopkins Bloomberg School of Public Health. nhats.org [Google Scholar]
- Grossman, E. S., Hoffman, Y. S. G., Palgi, Y., & Shrira, A. (2021). COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators. Personality and Individual Differences, 168, 110371. doi: 10.1016/j.paid.2020.110371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen, M., Andersen, T. E., Armour, C., Elklit, A., Palic, S., & Mackrill, T. (2010). PTSD-8: A short PTSD inventory. Clinical Practice and Epidemiology in Mental Health, 6, 101–108. doi: 10.2174/1745017901006010101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck, L., Gold, W. L., Robinson, S., Pogorski, S., Galea, S., & Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases, 10(7), 1206–1212. doi: 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krendl, A. C., & Perry, B. L. (2020). The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(2), e53–e58. doi: 10.1093/geronb/gbaa110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2003). The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Losada-Baltar, A., Martínez-Huertas, J. Á., Jiménez-Gonzalo, L., Pedroso-Chaparro, M. del S., Gallego-Alberto, L., Fernandes-Pires, J., & Márquez-González, M. (2021). Longitudinal correlates of loneliness and psychological distress during the lockdown situation due to COVID-19. Effects of age and self-perceptions of aging. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 77(4), 652–660. doi: 10.1093/geronb/gbab012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. The New England Journal of Medicine, 383(6), 510–512. doi: 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Pigeon, W. R., Bishop, T. M., & Krueger, K. M. (2017). Insomnia as a precipitating factor in new onset mental illness: A systematic review of recent findings. Current Psychiatry Reports, 19(8), 44. doi: 10.1007/s11920-017-0802-x [DOI] [PubMed] [Google Scholar]
- Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds, D. L., Garay, J. R., Deamond, S. L., Moran, M. K., Gold, W., & Styra, R. (2008). Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiology and Infection, 136(7), 997–1007. doi: 10.1017/S0950268807009156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stokes, J. E., & Moorman, S. M. (2018). Influence of the social network on married and unmarried older adults’ mental health. The Gerontologist, 58(6), 1109–1113. doi: 10.1093/geront/gnx151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Undurraga, E. A., Chowell, G., & Mizumoto, K. (2021). COVID-19 case fatality risk by age and gender in a high testing setting in Latin America: Chile, March–August 2020. Infectious Diseases of Poverty, 10(1), 11. doi: 10.1186/s40249-020-00785-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahia, I. V., Jeste, D. V., & Reynolds, C. F.3rd. (2020). Older adults and the mental health effects of COVID-19. Journal of the American Medical Association, 324(22), 2253–2254. doi: 10.1001/jama.2020.21753 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study are publicly available (released: December 17, 2020; www.nhats.org).