Abstract
Introduction
Pelvic ultrasounds are commonly performed for various clinical indications in female patients presenting to the hospital. A survey of the kidneys is routinely included as part of the examination, but there is limited justification for their inclusion in the assessment of every female presenting for a pelvic ultrasound.
Method
We examined the utility of surveying the kidney ultrasound during pelvic ultrasonography by reviewing the records of 1009 pelvic ultrasound examinations in 1000 women.
Results
In total, 46 incidental findings were identified, but 91% of these were clinically inconsequential. Only four patients had incidental findings of high clinical priority requiring specialist treatment. Of these, two patients were symptomatic and had urinary tract obstruction due to stones. The other two patients harboured asymptomatic renal cell carcinomas. The overall incidence of renal incidental findings of high clinical priority in asymptomatic patients was two in 1009 examinations (1999 kidneys).
Conclusion
Indiscriminate uncritical screening of the kidneys in women presenting for pelvic ultrasound is not evidence‐based and represents a low‐yield examination with extremely low rate of incidental findings of clinical significance.
Keywords: incidentaloma, kidney ultrasound, pelvic sonography, pelvic ultrasound examination, renal survey
Introduction
Pelvic ultrasound is one of the most common ultrasound examinations. There is a good level of agreement between different professional organisations internationally on how pelvic ultrasound should be performed and what should be included.1, 2, 3, 4 One point of difference is whether a survey of the kidneys should be routinely performed. While the Australasian Society for Ultrasound in Medicine (ASUM) advocates kidney survey in every woman presenting for pelvic ultrasound,4 other organisations do not, including the American College of Radiology (ACR), American College of Obstetrics and Gynecology (ACOG), Society of Pediatric Radiology (SPR), American Institute of Ultrasound In Medicine (AIUM), Society of Radiologists in Ultrasound (SRU) and British Medical Ultrasound Society (BMUS).1, 5 In the Standards of Practice documentation, ASUM does not provide a justification or external references for the inclusion of the kidneys during pelvic ultrasonography.
There may be reasonable clinical rationale to extend the pelvic examination and survey the kidneys in select patients presenting for pelvic ultrasound. First, large pelvic masses such as a fibroids,6, 7, 8, 9 ovarian10 or other masses,11 ureteric endometriosis12, 13, 14, 15, 16 or pelvic malignancy (gynaecological or other) may cause ureteric compression or invasion and result in obstruction. Pelvic organ prolapse is also sometimes associated with upper tract dilation.17 Second, in patients with lower abdominal pain, renal pathology may be present.18 Pain may be due to a renal problem, such as stones, or pelvic pain can be related to urinary tract infection necessitating review of the kidneys in some cases.19, 20, 21, 22 Third, patients with congenital variants or anomalies of the uterus have an increased likelihood of harbouring coexisting congenital renal anomalies.23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36 The knowledge of the presence or absence of such anomalies and their effect on the morphology and function of the kidney may be of clinical value.34
While the above scenarios provide reasonable clinical justifications for a kidney survey during pelvic ultrasound in specific patients, the majority of pelvic ultrasound examinations are performed for different reasons including irregular or heavy bleeding, characterisation of masses found on pelvic examination or other imaging, pelvic infection, characterisation of ovaries for polycystic morphology and others. These clinical scenarios provide no clinical justification for routine inclusion of the kidneys. The prevalence of renal incidental findings on cross‐sectional imaging is low.37, 38 The significance of these findings depends on the clinical context, and the value of screening for such lesions is debatable.37, 38, 39, 40, 41, 42 The prevalence of incidental findings in female patients presenting specifically for pelvic sonography is unknown.
In this paper, we summarise the outcomes of 1009 pelvic ultrasound examinations in 1000 female patients presenting for pelvic ultrasound with a concurrent examination of the kidneys. The incidence, spectrum and severity of renal findings are categorised. The outcome of significant renal findings was determined by review of patient records for the 12 calendar months following the ultrasound.
Methodology
We performed a retrospective sequential audit of 1009 ultrasound examinations in 1000 non‐pregnant female patients presenting for ultrasound imaging of the pelvis to Waikato District Health Board (DHB) Ultrasound service (Waikato Hospital, Hamilton and Thames Hospital, Thames, New Zealand) between the dates of 1 January 2017 and 14 July 2017. Pelvic ultrasound examinations were identified using a sequential search of our radiology picture archiving and communication system (PACS) – Philips PACS Enterprise. All patients had concurrent ultrasound imaging of the kidneys or recent imaging of the kidneys performed within the last month. All patients had been examined by either (i) qualified sonographers with postgraduate diploma or master's level qualifications or (ii) by trainee sonographers or radiology registrars under the direct supervision of a qualified sonographer. The ultrasound machines used were Philips Epiq 7 or Philips IU22.
Patient demographics and referral details were recorded. Ultrasound reports were reviewed, and the examination outcomes were analysed. Urinary tract findings were separated into clinically significant and clinically not significant (Table 1). The clinical outcome of patients with significant findings was determined by reviewing patient's clinical records for the 12 calendar months following the pelvic ultrasound.
Table 1.
Criteria for significant and clinically not significant renal findings
| Urinary tract findings considered clinically significant | Urinary tract findings considered clinically not significant |
|---|---|
| New diagnosis of Bosniak 2F – 4 cyst | Simple cyst (Bosniak 1) |
| New finding of angiomyolipoma | Minimally complex cyst (Bosniak 2) |
| New diagnosis of renal cell carcinoma (RCC) | Known and stable angiomyolipoma |
| New diagnosis of urinary tract dilation | Known and stable urinary tract dilation |
| Progressive urinary tract dilation | Extrarenal pelvis |
| New diagnosis of urinary retention, post‐void bladder volume >100ccs | Known urolithiasis |
| New diagnosis of urolithiasis (obstructive, non‐obstructive) | Non‐obstructing renal calculus <10 mm |
| New diagnosis of renal scarring | Known and unchanging renal scarring |
| New observation of echogenic renal parenchyma | Known and unchanging echogenic renal parenchyma |
| New diagnosis of medullary nephrocalcinosis | Known and unchanging nephrocalcinosis |
| New diagnosis of lobar nephronia, renal abscess or perinephric abscess | Stable or reducing renal abscess |
| New diagnosis of reduced parenchymal thickness | Known and unchanging renal atrophy |
| New diagnosis of renal atrophy | Anatomical variant with no complications (duplex kidney) |
| New diagnosis of an anatomical variant with complications | Known and unchanging anatomical variant |
| New diagnosis of bladder TCC |
Exclusion criteria were as follows:
Targeted or incomplete pelvic examination with kidneys not included on ultrasound or other imaging
Repeat pelvic examination in <1 month
Positive pregnancy test at time of examination including women with retained products of conception
Post‐partum pelvic examinations within 1 month of delivery
The study was approved by Waikato DHB Clinical Audit Support Group.
Results
The results of 1000 female patients presenting for 1009 pelvic ultrasound examinations to a tertiary‐level ultrasound service (Waikato DHB) were reviewed. Patients ranged in age from 6 months to 93 years with a mean age of 43 and median age of 44 years. At the time of examination, 62% of patients were below the age of 50. Pelvic ultrasonography was requested for a wide variety of clinical indications with some women being referred with a combination of indications, for example pain and bleeding. In total, 1230 clinical indications were encountered on referrals for pelvic ultrasonography. The most common indications were as follows: pelvic pain in 412 (33%) cases, post‐menopausal bleeding in 203 (17%), menorrhagia in 149 (12%), surveillance of ovarian cyst in 62 (5%), assessment of pelvic mass identified on other imaging in 31 (2.5%) and palpable mass in 31 (2.5%). In the 412 instances where pain was a presenting symptom, the pain was reported in right iliac fossa in 177 (43%), left iliac fossa in 65 (16%), right flank in four (1%), left flank in six (1.5%), central in 29 (7%) and unspecified or generalised pain in 131 (32%).
A summary of the indications for pelvic ultrasonography in our cohort is provided in Figure 1. We encountered a high prevalence of pathology in our patients with 58% of examinations featuring at least one abnormality. In total, 710 abnormal findings were recorded. The most common diagnoses were as follows: fibroids in 190 (19%) cases, endometrial thickening in 104 (10%), simple ovarian cyst in 68 (7%), haemorrhagic ovarian cyst in 42 (4%), free fluid in 38 (4%), endometrial polyp(s) in 32 (3%), complex ovarian cyst in 25 (3%), dermoid in 21 (2.0%), polycystic ovarian morphology in 19 (1.9%), adenomyosis in 16 (1.6%), ovarian cystic neoplasm in 13 (1.3%) and other pathologies (Figure 2).
Figure 1.
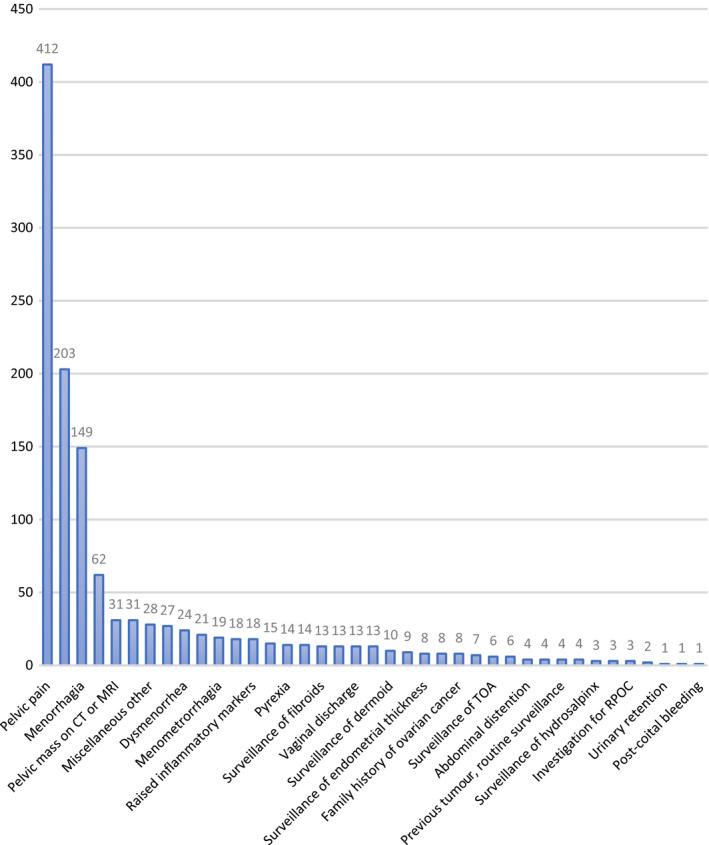
Indications for Pelvic Ultrasound.
Figure 2.
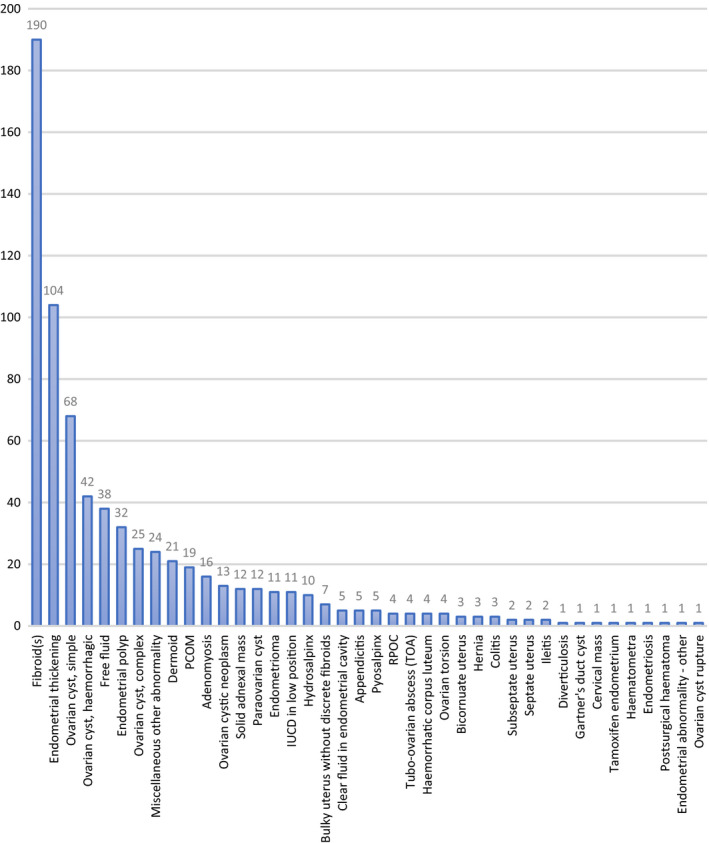
Spectrum of Diagnoses Made on Pelvic Ultrasound.
In the studied population of 1000 women, 1999 kidneys were available for review. One patient had had a nephrectomy in the past. Kidney survey revealed no significant finding in 96% of examinations. Forty‐six significant kidney findings were identified in 44 patients (Figure 3) including angiomyolipomas (14), renal dilation (9), urolithiasis (8), parenchymal thinning (4), complex renal cyst (3), renal scarring (3), renal atrophy (2), renal cell carcinoma (RCC, 2) and nephrocalcinosis (1). The overall prevalence of significant renal incidental findings was 4.6%.
Figure 3.
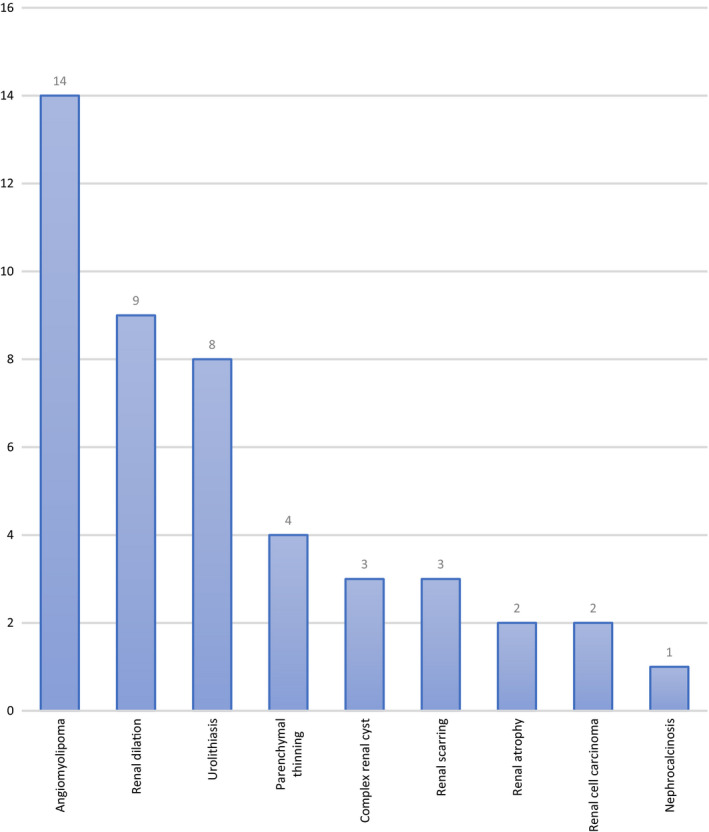
Type and Number of Renal Incidental Findings Per 1000 Patients With 1999 Kidneys.
Angiomyolipomas represented the most frequent incidental finding. A new diagnosis of angiomyolipoma was made in 14 patients (1.4%). Angiomyolipomas ranged in size from four to 45 mm (mean = 11.2 mm, median = 7.5 mm). None were referred for repeat surveillance imaging. None required any change in clinical management.
Renal dilation represented the second most frequent incidental finding. A new diagnosis of renal dilation was made in nine patients. The cause of dilation was a non‐visualised stone in three (33%) cases, large ovarian mass in two (22%), enlarged fibroid uterus in one (11%) and mild pelviureteric junction (PUJ) stricture in one (11%) case. In total, gynaecological causes accounted for renal dilation in three (33%) cases. In one case, dilation seen on ultrasound resolved and was not identified on subsequent computed tomography (CT) imaging. In another case, the cause of mild renal dilation was unknown and did not change on interval CT imaging. Seven of the nine patients (78%) with renal dilation required no treatment. Two patients (22%) required urological intervention. Clinical outcomes of patients with renal dilation are provided in Table 2.
Table 2.
Summary of patients diagnosed with renal tract dilation
| Age | Dilation side and grade | Further imaging of kidneys required? | Further specialist or hospital treatment for renal finding required? | Clinical details |
|---|---|---|---|---|
| 44 | Mild bilateral renal dilation | No | No |
Reason for referral: recent urinary retention thought to be due to constipation Ultrasound pelvis: enlarged fibroid uterus (300 cc) Renal function: normal |
| 34 | Mild bilateral renal dilation | No | No |
Reason for referral: abdominal distension with palpable mass, ultrasound pelvis: large 33 cm pelvic cyst Outcome: benign cystadenoma Renal function: normal |
| 88 | Mild right renal dilation | No | No |
Reason for referral: post‐menopausal bleeding Ultrasound pelvis: endometrial thickening Outcome: high‐grade endometrial carcinoma CT staging: renal dilation unchanged Renal function: normal |
| 76 | Mild bilateral renal dilation | No | No |
History: stage IV colon cancer with Krukenberg tumours Reason for referral: post‐menopausal bleeding Ultrasound pelvis: 10 cm solid adnexal mass CT reimaging post‐operatively: dilation resolved Renal function: normal |
| 66 | Mild right renal dilation | Yes (CT) | No |
Reason for referral: palpable pelvic mass Ultrasound pelvis: non‐enlarged fibroid uterus (60 cc) CT reimaging: minor PUJ stricture, no change |
| 22 | Mild right renal dilation | Yes (CT) | No |
Reason for referral: RIF pain Ultrasound pelvis: normal CT: renal dilation resolved, normal examination Ultrasound pelvis 10 months later: normal examination |
| 18 | Mild right renal dilation and hydroureter | Yes (CT) | No |
Reason for referral: right‐sided pain, raised WCC, haematuria, vomiting Ultrasound pelvis: normal CT: 5 mm obstructing calculus Outcome: Patient passed calculus, hydronephrosis resolved Renal function: renal function |
| 35 | Moderate right renal dilation and hydroureter | Yes (Nuclear Medicine) | Yes |
Reason for referral: pelvic pain, past history of cyst Ultrasound pelvis: normal Nuclear medicine: moderate reduction in right renal function Outcome: stent, cystoscopy–ureteroscopy, laser for stone, stent, recovered Nuclear medicine: improvement in right renal function Renal function: mild renal impairment, creatinine 98 μmol/L |
| 50 | Mild right renal dilation | Yes (CT) | Yes |
Reason for referral: RIF pain, clinically septic Ultrasound pelvis: endometrial thickening CT: 6 mm right ureteric calculus Outcome: cystoscopy–ureteroscopy, stent Renal function: impaired when septic, normal renal function after recovery |
Urolithiasis represented the third most frequent incidental finding. A new diagnosis of urolithiasis was made in eight (0.8%) patients. Six of the eight patients (75%) had asymptomatic non‐obstructing calculi. Two patients had ureteric calculi with mild renal dilation. Both were referred for pelvic ultrasound because of pain, and the pain was attributable to the renal calculi in both cases. No patient required specialist or hospital treatment for calculi. Detailed outline of the clinical outcome of patients with urolithiasis is provided in Table 3.
Table 3.
Summary of patients diagnosed with urolithiasis
| Age | Stone size and associated findings | Further imaging of kidneys required? | Further specialist or hospital treatment for renal finding required? | Clinical management actions were taken with regard to the renal finding |
|---|---|---|---|---|
| 77 |
9 mm non‐obstructing right renal calculus |
No | No |
Reason for referral: post‐menopausal bleeding Ultrasound pelvis: normal Outcome: no action Renal function: normal |
| 55 |
8 mm non‐obstructing left renal calculus |
Yes (X‐ray, CT) | No |
Reason for referral: palpable abdominal mass Ultrasound pelvis: normal Outcome: conservative management Renal function: not tested |
| 57 |
5 mm non‐obstructing left renal calculi |
No | No |
Reason for referral: post‐menopausal bleeding Ultrasound pelvis: endometrial thickening Outcome: hysteroscopy, polypectomy, benign Renal function: normal |
| 25 |
6 mm non‐obstructing left renal calculus |
No | No |
Reason for referral: Investigation for PCOM Ultrasound pelvis: PCOM Outcome: no action Renal function: normal |
| 26 |
3 mm non‐obstructing left renal calculus |
No | No |
Reason for referral: menorrhagia Ultrasound pelvis: normal Outcome: no action Renal function: not tested |
| 53 |
13 mm non‐obstructing left renal calculus |
Yes (X‐ray, CT) | No |
Reason for referral: post‐menopausal bleeding Ultrasound pelvis: endometrial thickening Outcome: no endometrial cancer, conservative management for urolithiasis Renal function: background of CKD stage 4, creatinine 171–209 μmol/L |
| 28 |
5 mm left VUJ calculus with mild upper tract dilation |
Yes (X‐ray) | No |
Reason for referral: left flank pain Ultrasound pelvis: normal Outcome: pain resolved, patient did not attend specialist clinic appointments Renal function: normal |
| 24 |
5.5 mm right ureteric calculus with mild upper tract dilation |
Yes (X‐ray x2) | No |
Reason for referral: RIF pain Ultrasound pelvis: normal Outcome: conservative management, passed calculus Renal function: normal |
Parenchymal thinning was incidentally detected in four patients. They ranged in age from 69 to 76 years with a mean age of 70. Two of the four patients had mild renal impairment (creatinine level: 98–144 and 97 μmol/L). None received further imaging for this finding. None required any change in clinical management.
Cystic renal masses were characterised by using the Bosniak classification system.43 A complex renal cyst was incidentally detected in three patients, including Bosniak 2F lesions and one indeterminate lesion. The patients ranged in age from 45 to 68 years. Two patients received contrast CT, and the renal lesions were downgraded to simple cysts or a cluster of simple cysts (Bosniak 1). One patient with a Bosniak 2F lesion did not receive repeat surveillance imaging because the recommendation to do so was not actioned by the referrer. None of the three patients required any change in clinical management.
Renal parenchymal scarring was incidentally detected in three patients. They ranged in age from 42 to 49 years. None received further imaging for this finding. None required any change in clinical management.
Unilateral renal atrophy was detected in two patients. They were aged 53 and 64 years. One patient had normal renal function, and the other had known stage four chronic kidney disease. Neither received further imaging for this finding. Neither required any change in clinical management.
Renal cell carcinoma represented the second least common incidental finding and was detected in two patients. They were aged 48 and 61 years. One patient was referred for surveillance of an ovarian cyst diagnosed at another institution. The other was referred for post‐menopausal bleeding. The size of the RCCs was 30 and 43 mm. One patient underwent partial nephrectomy and the other radical nephrectomy. Both RCCs were clear cell type on histology.
Nephrocalcinosis represented the least common incidental finding and was detected in one patient, aged 32 years. The patient did receive further imaging for this finding. The patient did not require any change in clinical management. Her renal function remains normal.
Two patients with a congenital renal anomaly (horseshoe kidney) did not feature associated gynaecological variants. Likewise, all nine patients with congenital uterine anomaly (three bicornuate uterus, four septate uterus and two subseptate uterus) featured normal kidneys.
Renal finding as a cause of pain
Pain was one of the presenting symptoms in 412 (40%) patients referred for pelvic ultrasound and in eight (2%) of those the renal finding accounted for the pain. Four patients had renal dilation subsequently confirmed to be caused by a stone on CT imaging, two had renal dilation with a stone detected on ultrasound, one had unexplained mild upper tract dilation that was unchanged on interval imaging and one had pyelonephritis with lobar nephronia. The latter case was not included in our analysis of significant incidental findings because the finding had been detected on a preceding CT scan on the same day and was subsequently reimaged by ultrasound. None of these women had coexisting pelvic pathology that would account for pain on the ipsilateral side. One patient had a haemorrhagic ovarian cyst on the contralateral side.
Inconsequential findings
Of the 46 incidental renal findings, 42 (91%) were inconsequential and required no change in patient management, no specialist treatment and no hospital admissions.
Findings of high clinical priority
In the 1009 examinations, only four (0.4%) renal findings were considered to be of high clinical priority because they were of immediate clinical concern or required intervention. These included two cases of renal dilation requiring intervention and two RCCs. Both patients with urinary dilation were symptomatic, and one of the two was septic. Both RCCs were clinically silent. Therefore, the overall prevalence of incidental findings of high clinical priority in asymptomatic patients was two (0.2%) in 1009 examinations or 0.1% in 1999 kidneys.
Discussion
The inclusion of a kidney survey during pelvic ultrasound is a common practice in Australia and New Zealand. It is most commonly motivated by protocol‐based, accreditation‐driven, uncritical compliance with the ASUM guideline4 and not by a genuine clinical need or sound clinical justification. The origin of the idea and motives behind the inclusion of a kidney survey in this guideline is unknown and unreferenced. The ASUM guideline is also vague on the issue because the only imaging requirement with regard to the kidneys is listed as ‘kidneys – position’. Apart from a congenital abnormality or a large mass displacing the kidney, the kidney would be expected in a normal position regardless of the presence of clinically significant renal findings including tumour, obstruction, stones or infection. Indeed, 99.9% of the 1999 kidneys in our series of 1000 patients were in normal position. Two patients had normally functioning horseshoe kidneys in an inferior anatomical location, but with no clinical sequelae identified or expected. It is perhaps due to these considerations that most individuals and practices have interpreted the ASUM guideline as requiring a complete examination of the kidneys rather than a simple identification of renal position.
We used a low threshold to identify renal findings as clinically significant. Using our criteria, the prevalence rate of renal incidental findings was 4.6%, but the vast majority (91%) were inconsequential. The prevalence of incidental findings of high clinical priority was only four in 1000 (0.4%). The prevalence of incidental findings of high clinical priority in asymptomatic patients was only two in 1009 examinations (0.2%). Our study confirms that the inclusion of a kidney survey during every pelvic ultrasound produces a vast predominance of VOMITS (victims of modern imaging technology),44, 45, 46 rather than uncovering clinically useful findings.
Rather than indiscriminate kidney imaging of all patients presenting for pelvic ultrasound, a better utilisation of sonography would be to include kidney survey only in patients with a sound clinical reason. Sonographers already carry the mandate to extend examination where clinically appropriate, so this would not represent a change to current clinical practice.5, 47, 48 Two of the four clinically concerning incidental findings in our study would have been detected by using this approach with exception of two clinically silent RCCs.
Renal cell carcinomas represent the most problematic incidentalomas. The majority of RCCs are clinically silent and are often incidentally detected on imaging.49 A large meta‐analysis by Rossi et al.37 estimated that at least one RCC would incidentally be detected in 1000 patients screened by sonography. This estimate agrees with our findings, with two RCCs detected in 1000 women (prevalence rate 0.2%). Both were small, and both were successfully surgically treated. While these two patients clearly benefited from the incidental discovery of RCC, the use of ultrasound in screening for RCC is controversial and has not been implemented.50, 51 A dedicated RCC screening programme would require a national approach and would most certainly include some form of prior selection of patients with increased pre‐test probability of kidney cancer.50 If the RCC screening algorithm proposed by Shea50 had been employed on our cohort of patients, one of the two RCCs would have been detected and the other missed.
Individuals and departments who wish to continue kidney screening of all women presenting for a pelvic examination should consider why they do not advocate such screening during other examinations such as thyroid, carotid or breast sonography where the probability of incidental discovery of significant renal incidentalomas is comparable or potentially higher on the account of older patient populations receiving these imaging procedures. In the case of pelvic, thyroid, carotid or breast ultrasonography, the additional examination of the kidneys requires a similar amount of time, effort and resources including changing of transducers (transvaginal to curvilinear, linear to curvilinear respectively), performance of the scanning procedure, interpretation of the finding by the sonographer, review of the finding by a radiologist or sonologist, and recording of the findings. Another relevant question would be whether instead of screening all women for associated renal abnormality, women over the age of 65 should be screened for other conditions such an abdominal aortic aneurysm. In our population of 1000 women, 132 were over the age of 65. Based on a published prevalence rate of 0.7%,52 we would have expected to identify one asymptomatic abdominal aortic aneurysms (AAA).
The addition of a kidney survey during pelvic ultrasound requires considerable investment of physical labour by the sonographer as well as cognitive burden for both the sonographer and the radiologist. Removing the requirement to image the kidneys would have the potential to improve the efficiency of the pelvic examination, significantly decrease the work burden on sonographers and allow more time for the assessment of the areas of clinical concern. The authors propose that the common practice to indiscriminately and uncritically image the kidneys in all women presenting for gynaecological ultrasound be abandoned. Instead, sonographers should exercise sound clinical judgement and examine the kidneys selectively, for instance in women with a large pelvic mass or unexplained unilateral pain. In our study, one‐third of the cases of renal dilation were associated with a pelvic mass. In women with pelvic pain, the prevalence of renal finding to account for pain was quite low (1.9%). Although pain was the most common presenting symptom in our cohort, unilateral pain necessitating extension of the examination was only encountered in 252 of 1009 examinations. Unnecessary examination of the kidneys could therefore be voided in at least 757 (75%) of cases.
The most common incidental findings in our study were angiomyolipomas. They were identified on 1.4% of all examinations. None were referred for repeat imaging within 1 year of the initial ultrasound even though a recommendation to do so was made on some reports. One of the caveats of the ultrasound diagnosis of angiomyolipoma is that it is a presumptive diagnosis based on anatomical location (parenchymal) and acoustic properties of the lesion (echogenic). Ultrasound does not provide tissue differentiation to positively identify angiomyolipomas. Between 2% and 5% of small echogenic parenchymal renal lesions are concerning or malignant in nature.53, 54 Sonographers, radiologists and clinicians should therefore exercise caution when interpreting small echogenic renal masses as benign entities. Larger angiomyolipomas (>20 mm) may require confirmatory imaging and surveillance for interval growth and haemorrhage.55, 56, 57
Our study has several limitations. First, we surveyed the clinical outcome of women for the 12 calendar months following the ultrasound. Second, we assessed hospital clinical records (admissions, discharge summaries, clinic letters, imaging records, laboratory results), but did not assess general practitioners’ (GP) records to determine whether the incidental findings had any effect on primary care visits and consultations. Third, it is possible that some of our incidental findings may become symptomatic in the future. This is particularly the case with urolithiasis. It is also possible that the knowledge of the incidental finding may lead to adjustments in lifestyle or diet that may have benefited the patients in the long term. Conversely, it is possible that the incidental discovery of a trivial finding may have created undue anxiety for the patient and their doctors.
Finally, we acknowledge that if renal imaging had not been performed, two RCCs would have been missed in our cohort and this may have led to adverse health outcomes. RCC represents the ninth most common cancer.50 While the mortality of RCC cannot be trivialised, patients with small renal masses (SRMs) generally do well.58 One of our patients fell into this category, and the other was just beyond the threshold of SRM.
Conclusion
Routine inclusion of a kidney survey during every pelvic ultrasound represents a low‐yield imaging investigation that is not clinically justified. In our study of 1009 pelvic examinations in 1000 female patients with 1999 kidneys, the prevalence of renal incidental findings was 4.6%. The vast majority (91%) were clinically inconsequential. The prevalence of renal incidental findings of high clinical priority was only four in 1000 (0.4%), and half of these were symptomatic.
Acknowledgements
The authors would like to thank the following individuals for their review of the manuscript, insights, comments and suggestions: Nicole Curtis, Karen Robertson, Katie Drummond, Cornelia Deakins (Hamilton), Dr Deborah McMurtrie (Tauranga), Kate Thomas (Dunedin), Mike Heath, Carol Bagnall (Auckland) and Angela Browne (Whangarei).
References
- 1.American College of Radiology . ACR–ACOG–AIUM–SPR–SRU Practice Parameter for the performance of ultrasound of the female pelvis [Internet]. 2014. [cited 2017 Dec 15]. Available from: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/us-pelvis.pdf?la=en
- 2.American College of Radiology . ACR appropriateness criteria [Internet]. 2015. [cited 2017 Dec 15]. Available from: https://acsearch.acr.org/docs/69503/Narrative/
- 3.American Institute of Ultrasound in Medicine . AIUM Practice parameter for the performance of Ultrasound of the female pelvis [Internet]. 2014. [cited 2017 Dec 15]. Available from: http://www.aium.org/resources/guidelines/femalepelvis.pdf
- 4.Australasian Society for Ultrasound and Medicine . Guidelines, Policies and Statements D8: Statement on the Performance of a Gynaecological Scan [Internet]. 2014. [cited 2017 Dec 15]. Available from: http://www.asum.com.au/files/public/SoP/D8-Guidelines-for-the-Performance-of-a-Gynaecological-Scan.pdf
- 5.Society and College of Radiographers and British Medical Ultrasound Society . Guidelines for Professional Ultrasound Practice [Internet]. 2015. [cited 2017 Jan 9]. Available from: https://www.sor.org/sites/default/files/document-versions/ultrasound_guidance.pdf
- 6.Derbent A, Turhan NO. Acute urinary retention caused by a large impacted leiomyoma. Arch Gynecol Obstet 2009; 280(6): 1045–7. [DOI] [PubMed] [Google Scholar]
- 7.Novi JM, Shaunik A, Mulvihill BHK, Morgan MA. Acute urinary retention caused by a uterine leiomyoma: a case report. J Reprod Med 2004; 49(2): 131–2. [PubMed] [Google Scholar]
- 8.Bansal T, Mehrotra P, Jayasena D, Okolo S, Yoong W, Govind A. Obstructive nephropathy and chronic kidney disease secondary to uterine leiomyomas. Arch Gynecol Obstet 2009; 279(6): 785–8. [DOI] [PubMed] [Google Scholar]
- 9.Yazdany T, Bhatia NN, Nguyen JN. Urinary retention and voiding dysfunction in women with uterine leiomyoma: a case series. J Reprod Med 2012; 57(9–10): 384–9. [PubMed] [Google Scholar]
- 10.Geisler JP, Perry RW, Ayres GM, Holland TF, Melton ME, Geisler HE. Ovarian cancer causing upper and lower urinary tract obstruction. Eur J Gynaecol Oncol 1994; 15(5): 343–4. [PubMed] [Google Scholar]
- 11.Advincula AP, Hernandez JC. Acute urinary retention caused by a large peritoneal inclusion cyst: a case report. J Reprod Med 2006; 51(3): 202–4. [PubMed] [Google Scholar]
- 12.Choi JI, Yoo JG, Kim SJ, Lee HN, Kim MJ. Acute renal failure due to obstructive uropathy secondary to ureteral endometriosis. Case Rep Obstet Gynecol 2015; 2015: 761348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pateman K, Holland TK, Knez J, Derdelis G, Cutner A, Saridogan E, et al. Should a detailed ultrasound examination of the complete urinary tract be routinely performed in women with suspected pelvic endometriosis? Hum Reprod 2015; 30(12): 2802–7. [DOI] [PubMed] [Google Scholar]
- 14.Yohannes P. Ureteral endometriosis. J Urol 2003; 170(1): 20–5. [DOI] [PubMed] [Google Scholar]
- 15.Donnez J, Nisolle M, Squifflet J. Ureteral endometriosis: a complication of rectovaginal endometriotic (adenomyotic) nodules. Fertil Steril 2002; 77(1): 32–7. [DOI] [PubMed] [Google Scholar]
- 16.Ponticelli C, Graziani G, Montanari E. Ureteral endometriosis: a rare and underdiagnosed cause of kidney dysfunction. Nephron Clin Pract 2010; 114(2): c89–94. [DOI] [PubMed] [Google Scholar]
- 17.Beverly CM, Walters MD, Weber AM, Piedmonte MR, Ballard LA. Prevalence of hydronephrosis in patients undergoing surgery for pelvic organ prolapse. Obstet Gynecol 1997; 90(1): 37–41. [DOI] [PubMed] [Google Scholar]
- 18.Kruszka PS, Kruszka SJ. Evaluation of acute pelvic pain in women. Am Fam Physician 2010; 82(2): 141–7. [PubMed] [Google Scholar]
- 19.Tsai J‐L, Tsai S‐F. Case report: a rare cause of complicated urinary tract infection in a woman with Herlyn–Werner–Wunderlich syndrome. Iran Red Crescent Med J 2016; 18(11): e40267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vandermeer FQ, Wong‐You‐Cheong JJ. Imaging of acute pelvic pain. Clin Obstet Gynecol 2009; 52(1): 2–20. [DOI] [PubMed] [Google Scholar]
- 21.Amirbekian S, Hooley RJ. Ultrasound evaluation of pelvic pain. Radiol Clin North Am 2014; 52(6): 1215–35. [DOI] [PubMed] [Google Scholar]
- 22.Ackerman SJ, Irshad A, Anis M. Ultrasound for pelvic pain II: nongynecologic causes. Obstet Gynecol Clin North Am 2011; 38(1): 69–83, viii. [DOI] [PubMed] [Google Scholar]
- 23.Takami M, Aoki S, Kurasawa K, Okuda M, Takahashi T, Hirahara F. A classification of congenital uterine anomalies predicting pregnancy outcomes. Acta Obstet Gynecol Scand 2014; 93(7): 691–7. [DOI] [PubMed] [Google Scholar]
- 24.Mansouri R, Sander JC, Janzen NK, Dietrich JE. A case of obstructed Hemivagina with ectopic ureter leading to severe hydrocolpos and contralateral renal outflow tract obstruction in a neonate. J Pediatr Adolesc Gynecol 2015; 28(5): e131–3. [DOI] [PubMed] [Google Scholar]
- 25.Li S, Qayyum A, Coakley FV, Hricak H. Association of renal agenesis and mullerian duct anomalies. J Comput Assist Tomogr 2000; 24(6): 829–34. [DOI] [PubMed] [Google Scholar]
- 26.Sajjad Y. Development of the genital ducts and external genitalia in the early human embryo. J Obstet Gynaecol Res 2010; 36(5): 929–37. [DOI] [PubMed] [Google Scholar]
- 27.Acién P, Acién M. Diagnostic imaging and cataloguing of female genital malformations. Insights Imaging 2016; 7(5): 713–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imai A, Takagi H, Matsunami K. Double uterus associated with renal aplasia; magnetic resonance appearance and three‐dimensional computed tomographic urogram. Int J Gynecol Obstet 2004; 87(2): 169–71. [DOI] [PubMed] [Google Scholar]
- 29.Dias JL, Jogo R. Herlyn–Werner–Wunderlich syndrome: pre‐ and post‐surgical MRI and US findings. Abdom Imaging 2015; 40(7): 2667–82. [DOI] [PubMed] [Google Scholar]
- 30.Behr SC, Courtier JL, Qayyum A. Imaging of Müllerian duct anomalies. Radiographics 2012; 32(6): E233–50. [DOI] [PubMed] [Google Scholar]
- 31.Robbins JB, Broadwell C, Chow LC, Parry JP, Sadowski EA. Müllerian duct anomalies: embryological development, classification, and MRI assessment. J Magn Reson Imaging 2015; 41(1): 1–12. [DOI] [PubMed] [Google Scholar]
- 32.Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod 2013; 28(8): 2032–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies. 2017 Dec 13 [cited 2017 Dec 13]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4753246/.
- 34.Heckmann R, de la Fuente FA, Heiner JD. Pediatric urinary retention and constipation: vaginal agenesis with hematometrocolpos. West J Emerg Med 2015; 16(3): 418–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garel L, Dubois J, Grignon A, Filiatrault D, Van Vliet G. US of the pediatric female pelvis: a clinical perspective. Radiographics 2001; 21(6): 1393–407. [DOI] [PubMed] [Google Scholar]
- 36.Bocca SM, Abuhamad AZ. Use of 3‐dimensional sonography to assess uterine anomalies. J Ultrasound Med Off J Am Inst Ultrasound Med 2013; 32(1): 1–6. [DOI] [PubMed] [Google Scholar]
- 37.Rossi SH, Hsu R, Blick C, Goh V, Nathan P, Nicol D, et al. Meta‐analysis of the prevalence of renal cancer detected by abdominal ultrasonography. Br J Surg 2017; 104(6): 648–59. [DOI] [PubMed] [Google Scholar]
- 38.Meyer HJ, Pfeil A, Schramm D, Bach AG, Surov A. Renal incidental findings on computed tomography: frequency and distribution in a large non selected cohort. Medicine (Baltimore) 2017; 96(26): e7039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mazziotti S, Cicero G, D'Angelo T, Marino MA, Visalli C, Salamone I, et al. Imaging and management of incidental renal lesions. BioMed Res Int 2017; 2017: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sohaib A. Incidental solid cystic renal lesion. Cancer Imaging 2012; 12(2): 385–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takagi H, Matsunami K, Noda K, Furui T, Imai A. Magnetic resonance imaging in the evaluating of double uterus and associated urinary tract anomalies: a report of five cases. J Obstet Gynaecol J Inst Obstet Gynaecol 2003; 23(5): 525–7. [DOI] [PubMed] [Google Scholar]
- 42.Ha SC, Zlomke HA, Cost N, Wilson S. The past, present, and future in management of small renal masses. J Oncol 2015; 2015: 364807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Israel G, Hindman N, Bosniak M. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology 2004; 231(2): 365–71. [DOI] [PubMed] [Google Scholar]
- 44.Hayward R. VOMIT (victims of modern imaging technology)—an acronym for our times. BMJ 2003; 326(7401): 1273. [Google Scholar]
- 45.Lysdahl KB, Hofmann BM. What causes increasing and unnecessary use of radiological investigations? A survey of radiologists’ perceptions. BMC Health Serv Res 2009; 1(9): 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Booth TC, Najim R, Petkova H. Incidental findings discovered during imaging: implications for general practice. Br J Gen Pr 2016; 66(648): 346–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Australasian Society for Ultrasound and Medicine . Guidelines, Policies and Statements C2: Statement on the Practice of Ultrasound by Sonographers [Internet]. 2014. Available from: http://www.asum.com.au/files/public/SoP/C2-Statement-on-%20the-Practice-of-Ultrasound-by-Sonographers.pdf
- 48.Necas M. The clinical ultrasound report: guideline or sonographers. Australas J Ultrasound Med 2017; 21: 9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rabjerg M, Mikkelsen MN, Walter S, Marcussen N. Incidental renal neoplasms: is there a need for routine screening? A Danish single‐center epidemiological study. APMIS Acta Pathol Microbiol Immunol Scand 2014; 122(8): 708–14. [DOI] [PubMed] [Google Scholar]
- 50.Shea MW. A proposal for a targeted screening program for renal cancer. Front Oncol 2013; 3: 207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoffman A, Half EE. Update on screening for urological malignancies. Rambam Maimonides Med J 2017; 8(4): e0041. 10.5041/RMMJ.10318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DeRubertis BG, Trocciola SM, Ryer EJ, Pieracci FM, McKinsey JF, Faries PL, et al. Abdominal aortic aneurysm in women: prevalence, risk factors, and implications for screening. J Vasc Surg 2007; 46(4): 630–5.e1. [DOI] [PubMed] [Google Scholar]
- 53.Doshi AM, Ayoola A, Rosenkrantz AB. Do incidental hyperechoic renal lesions measuring up to 1 cm warrant further imaging? Outcomes of 161 lesions. Am J Roentgenol 2017; 209(2): 346–50. [DOI] [PubMed] [Google Scholar]
- 54.de Silva S, Copping R, Malouf D, Hutton A, Maclean F, Aslan P. Frequency of angiomyolipomas among echogenic nonshadowing renal masses (>4 mm) found at ultrasound and the utility of MRI for diagnosis. AJR Am J Roentgenol 2017; 209(5): 1074–80. [DOI] [PubMed] [Google Scholar]
- 55.Maclean DFW, Sultana R, Radwan R, McKnight L, Khastgir J. Is the follow‐up of small renal angiomyolipomas a necessary precaution? Clin Radiol 2014; 69(8): 822–6. [DOI] [PubMed] [Google Scholar]
- 56.Flum AS, Hamoui N, Said MA, Yang XJ, Casalino DD, McGuire BB, et al. Update on the diagnosis and management of renal angiomyolipoma. J Urol 2016; 195(4 Pt 1): 834–46. [DOI] [PubMed] [Google Scholar]
- 57.Chan KE, Chedgy E, Bent CL, Turner KJ. Surveillance imaging for sporadic renal angiomyolipoma less than 40 mm: lessons learnt and recommendations from the experience of a large district general hospital. Ann R Coll Surg Engl 2018; 16: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bensalah K, Pantuck AJ, Crepel M, Verhoest G, Méjean A, Valéri A, et al. Prognostic variables to predict cancer‐related death in incidental renal tumours. BJU Int 2008; 102(10): 1376–80. [DOI] [PubMed] [Google Scholar]


