Abstract
Objective
The safety of minimally invasive mitral valve surgery (MIMVS) in elderly patients is still debated. Our objective was to perform a systematic review and meta-analysis of studies comparing MIMVS with conventional sternotomy (CS) in elderly patients (≥65 years old).
Methods
We searched PubMed, EMBASE, Web of Science, clinicaltrials.gov, and Cochrane Central Register of Controlled Trials for trials and observational studies comparing MIMVS with CS in patients ≥65 years old presenting for mitral valve surgery. We performed a random-effects meta-analysis of all outcomes.
Results
The MIMVS group had lower odds of acute renal failure (odds ratio [OR] 0.27; 95% CI 0.10 to 0.78), prolonged intubation (>48 h; OR 0.47; 95% CI 0.31 to 0.70), less blood product transfusion (weighted mean difference [WMD] −0.82 units; 95% CI −1.29 to −0.34 units), shorter ICU length of stay (LOS; WMD −2.57 days; 95% CI −3.24 to −1.90 days) and hospital LOS (WMD −4.06 days; 95% CI −5.19 to −2.94 days). There were no significant differences in the odds of mortality, stroke, respiratory infection, reoperation for bleeding, and postoperative atrial fibrillation. MIMVS was associated with longer cross-clamp (WMD 11.8 min; 95% CI 3.5 to 20.1 min) and cardiopulmonary bypass times (WMD 23.0 min; 95% CI 10.4 to 35.6 min).
Conclusions
MIMVS in elderly patients is associated with lower postoperative complications, blood transfusion, shorter ICU, and hospital LOS, and longer cross-clamp and bypass times.
Keywords: mitral surgery, meta-analysis, minimally invasive
Central Message.
Minimally invasive mitral valve surgery in elderly patients is associated with lower postoperative complications, blood transfusion, and shorter intensive care unit and hospital length of stay.
Introduction
In recent years, a large body of evidence has shown that minimally invasive techniques can be used in mitral valve repair safely with good results in experienced hands. Repair rates with minimally invasive mitral valve surgery (MIMVS) have been shown to be superior as compared with a conventional sternotomy (CS).1 With better cosmesis, faster healing, shorter hospital length of stay, and quicker return to work, MIMVS has seen increasing adoption and is becoming the standard of care.2 Elderly patients represent a large proportion of patients presenting with mitral valve disease; in fact, the incidence of at least moderate regurgitation in patients aged 70 to 83 years is more than 10%.3,4 This patient population is believed to be at an increased perioperative surgical risk5 and has therefore been excluded from the major studies that compared MIMVS to CS approaches. Therefore, it is currently unclear if elderly patients benefit from the minimally invasive techniques. To address this question, we performed a systematic review and meta-analysis of observational studies comparing MIMVS with CS in elderly patients (≥65 years old). We hypothesized that MIMVS would yield noninferior outcomes if performed at experienced centers.
Methods
Data Sources and Study Selection
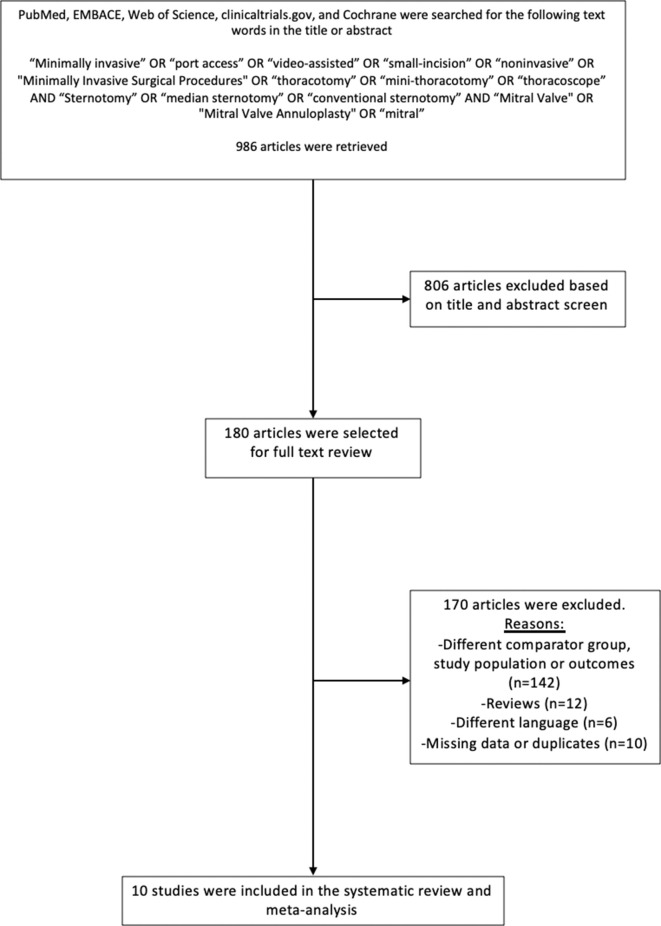
We performed a systematic search in PubMed, EMBACE, Web of Science, clinicaltrials.gov, and Cochrane using the search words “Minimally invasive” OR “port access” OR “video-assisted” OR “small-incision” OR “noninvasive” OR "Minimally Invasive Surgical Procedures" OR “thoracotomy” OR “mini-thoracotomy” OR “thoracoscope” AND “Sternotomy” OR “median sternotomy” OR “conventional sternotomy” AND “Mitral Valve” OR “Mitral Valve Annuloplasty” OR “mitral.” The “age” of the patients or their “elderly” status were not specifically included in the search strategy in order to increase the sensitivity of our search results, therefore minimizing the exclusion of any potential study that did not highlight “age” or “elderly.” We included all studies examining elderly patients (≥65 years old) undergoing mitral valve surgery with stratification on whether it was a minimally invasive versus a sternotomy approach. We excluded non-English studies, nonhuman studies, studies with patients <65 years old, meta-analyses, case reports, and any study that did not provide a comparison analysis.
Data Extraction
Two reviewers (A.H., S.G.) independently reviewed abstracts and full texts using the “Covidence” online screening tool based on the above-mentioned inclusion and exclusion criteria (Fig. 1). A third reviewer (F.H.) resolved any disagreement on study inclusion. Once the appropriate articles were selected, the 3 reviewers (A.H., F.H., S.G.) then independently extracted data including publication details, patient demographics, surgical approach, operative details, and postoperative outcomes. One study by Hawkins et al. met all of the inclusion criteria, except that the average age was 62 years.6 We contacted the corresponding author of the study and he provided us with an adjusted analysis restricted to age ≥65 years.
Fig. 1.
Flow chart for the search strategy employed in the meta-analysis.
Quality Assessment
We used the Newcastle-Ottawa quality assessment scale for cohort studies to assess the quality of the 10 studies that were included in our systematic review and meta-analysis.7 The Newcastle-Ottawa scale allows the assessment of 3 main domains: (1) Selection of the included studies; (2) comparability of the study groups; (3) assessment and reporting of the outcomes. Each of these domains is evaluated with a set of questions, and the scores are then converted to an overall quality score ranging from good, fair, or poor, based on the Agency for Healthcare Research and Quality standards.
Statistical Analysis
All analyses were performed using the meta package in Stata version 16 (StataCorp LP, College Station, TX) and random-effects models using Sidik-Jonkman because of the setting of rare outcomes. We pooled crude data from the different studies under the assumption that the individual studies had balanced baseline characteristics. For binary outcomes, we extracted the number of events and calculated log odds ratio (OR) via Peto’s method. When comparing continuous outcomes, we calculated the weighted mean difference (WMD) between both study groups. The heterogeneity between studies was assessed using I2, which allowed us to estimate the percentage of total variability that is due to between-studies heterogeneity rather than chance alone. Meta-regression was performed in order to assess if some of the variation between the studies (such as different proportion of degenerative mitral disease and different proportion of mitral repair) influenced the main results of the analysis.
Results
Characteristics of Included Studies and Quality Assessment
There were 10 retrospective observational cohort studies providing a head-to-head comparison between MIMVS and CS in elderly patients (≥65 years old), with a total of 1,897 patients (929 patients in the MIMVS group and 968 patients in the CS group).4,6,8-16 We had access to the full texts of 7 studies4,6,8-12 and only to the abstracts of 3 studies.13-16 After reviewing these 3 abstracts along with their accompanying materials, it was believed that we had access to enough information to make an assessment of the quality of the studies and to extract the appropriate information for our systematic review and meta-analysis. However, given that we did not have access to the full manuscripts, these 3 studies were only included in a separate sensitivity analysis.
All of the studies were single-center cohorts. The studies were relatively recent with the oldest study published in 2011 and the most recent one published in 2019. The smallest study reported on 45 patients12 and the largest study reported on 340 patients.16 All of the studies provided a comparison between elderly patients (≥65 years old) undergoing mitral valve surgery through a minimally invasive versus a sternotomy approach.
The overall quality was judged to be “Good” for 8 out of the 10 included studies (Supplemental Table 1). One study15 was judged to be of “Poor” quality, mainly because it did not demonstrate enough evidence of the comparability of the study groups (minimally invasive vs sternotomy groups) at baseline. The other study was judged to be of “Fair” quality, mainly because it did not provide an extensive description of the baseline demographics (Supplemental Table 1).16
Patient Characteristics
Patient preoperative characteristics are presented in Table 1. Within individual studies, the patients’ baseline characteristics were largely similar. All the minimally invasive procedures were performed through a lateral minithoracotomy. The proportion of degenerative mitral disease varied among studies, ranging from 60%6 to 93%.11 The proportion of mitral repair also varied among studies and ranged from 0%12 to 100%.11
Table 1.
Patient Preoperative Characteristics.
| Study | Patients | Age, yr | Male | Stroke | COPD | Cr, umol/L | LVEF, % | PVD | HTN | Diabetes | BMI, kg/m2 | Proportion of degenerative mitral disease | Proportion of mitral repair | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | MI | CS | Overall cohort | Overall cohort | |
| Seven studies included in main analysis | ||||||||||||||||||||||||
| Holzhey et al. (2011)8 | 143 | 143 | 76 ± 3.9 |
76 ± 3.6 |
102 (71) | 98 (69) | 12 (8) | 9 (6) | 13 (9) | 12 (8) | – | – | 58 ± 15 | 58 ± 15 | 21 (15) | 18 (13) | – | – | 32 (22) | 35 (24) | – | – | 83% | 56% |
| Santana et al. (2011)9 | 64 | 96 | 69.4 ± 11 |
64.7 ± 11.5 | 35 (55) | 54 (56) | 3 (5) | 17 (18) | 26 (41) | 34 (35) | 108 ± 44 | 108 ± 44 | 54 ± 13 | 50 ± 14 | 5 (8) | 16 (17) | 60 (94) | 88 (92) | 25 (39) | 35 (36) | 34.8 ± 5.3 | 34.9 ± 4.8 | – | – |
| Lamelas et al. (2011)4 | 119 | 84 | 80.6 ± 4.4 | 79.7 ± 4.4 | 47 (39) | 37 (44) | 19 (16) | 9 (11) | – | – | 94 ± 27 | 94 ± 27 | 58 ± 10 | 54 ± 10 | 7 (6) | 8 (10) | 109 (92) | 80 (95) | 32 (27) | 20 (24) | 26.4 ± 3.9 | 26.4 ± 3.9 | – | – |
| Iribarne et al. (2012)10 | 70 | 105 | 78.6 ± 3.3 | 79.4 ± 3.9 | 43 (61) | 70 (67) | 3 (4) | 9 (9) | 4 (8) | 13 (12) | 88 ± 4 | 97 ± 4 | 52 ± 12 | 50 ± 12 | 2 (3) | 2 (2) | – | – | 5 (7) | 7 (7) | 24 ± 0.5 |
24.5 ± 0.4 | 65% | 61% |
| Hawkins et al. (2018)6 | 47 | 184 | 73.8 ± 6.8 | 73.8 ± 6.1 | 23 (49) | 85 (46) | 2 (4) | 39 (21) | 5 (11) | 31 (17) | 97 ± 46 | 117 ± 97 | 58 ± 10 | 56 ± 10 | 2 (4) | 18 (10) | 2 (4) | 18 (10) | 9 (19) | 49 (27) | – | – | 60% | 42% |
| Losenno et al. (2019)11 | 121 | 41 | 73.9 ± 6.7 | 75.8 ± 6.8 | 71 (59) | 31 (76) | 8 (7) | 5 (12) | 5 (4) | 7 (17) | 86 ± 23 | 102 ± 41 | 62 ± 7 | 61 ± 8 | 5 (4) | 5 (12) | 7 (6) | 7 (17) | 26 ± 5 |
28.4 ± 7.9 | 93% | 100% | ||
| Chen et al. (2019)12 | 20 | 25 | 68.3 ± 2.6 | 69.1 ± 3.6 | 8 (40) | 11 (44) | 0 | 0 | – | – | 99 ± 12 | 106 ± 15 | 51 ± 7 | 50 ± 8 | – | – | 7 (35) | 10 (40) | 5 (25) | 8 (32) | 19.1 ± 2.2 | 18.7 ± 3.1 | – | 0% |
| Three additional studies included in sensitivity analysis | ||||||||||||||||||||||||
| Chen et al. (2017)13,14 | 50 | 50 | 82.9 ± 2.8 | 82.6 ± 2.2 | 27 (54) | 27 (54) | 8 (16) | 7 (14) | – | – | 97 ± 35 | 115 ± 88 | – | – | – | – | 36 (72) | 40 (80) | 2 (4) | 7 (14) | 24 ± 3.8 |
24.6 ± 4 |
– | 80% |
| Peterson et al. (2018)15 | 50 | 145 | 74.5 ± 2.5 | 75 ± 4 |
– | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 100% | |
| Van laeken et al. (2019)16 | 245 | 95 | 68 ± 16 |
72 ± 14 |
117 (48) | 37 (39) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |
Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease; Cr, preoperative creatinine; CS, conventional sternotomy; HTN, hypertension; LVEF, left ventricular ejection fraction; MI, minimally invasive; PVD, peripheral vascular disease.
Data presented as mean ± SD or n (%).
Postoperative Outcomes
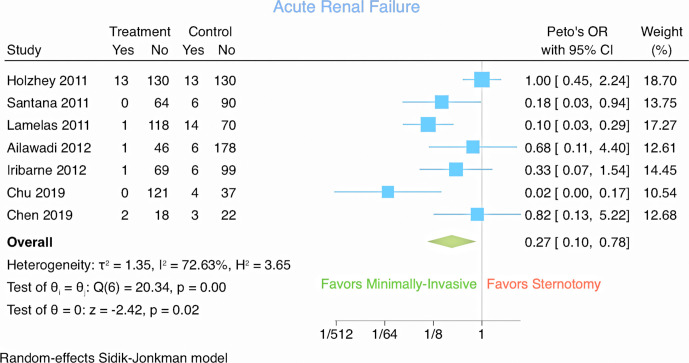
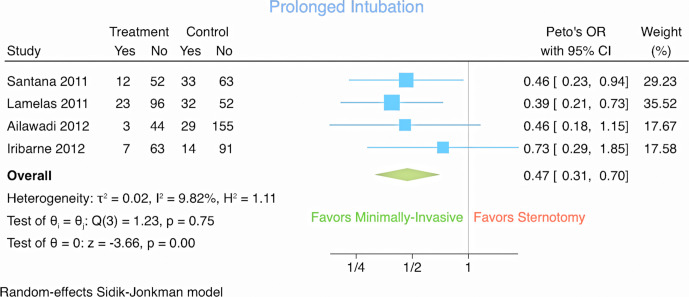
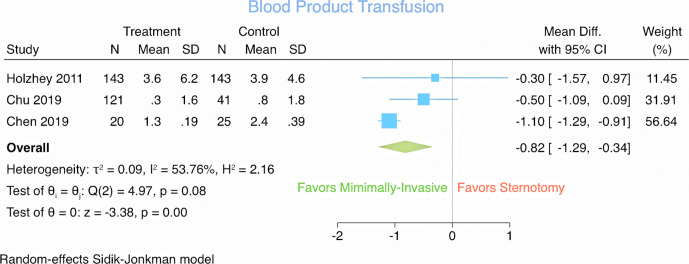
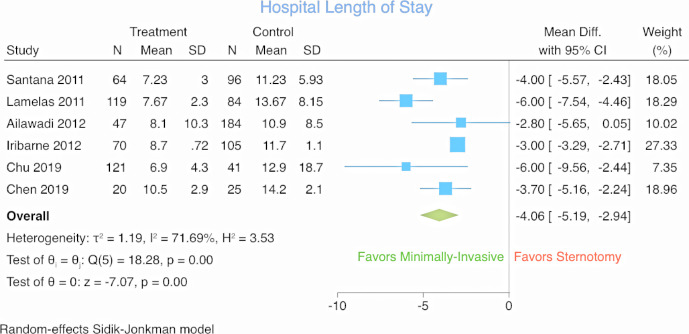
When we restricted the analysis to the 7 studies to which we had access to the full manuscripts, we found that the MIMVS group had significantly lower odds of acute renal failure (7 studies, 1,262 patients: OR 0.27; 95% CI 0.10 to 0.78; I2 = 72.6%; Fig. 2), prolonged intubation (>48 h; 4 studies, 729 patients: OR 0.47; 95% CI 0.31 to 0.70; I2 = 9.8%; Fig. 3), and also less blood product transfusion (3 studies, 493 patients: WMD −0.82 units; 95% CI −1.29 to −0.34 units; I2 = 53.8%; Fig. 4), shorter intensive care unit (ICU) length of stay (LOS; 4 studies, 786 patients: WMD −2.57 days; 95% CI −3.24 to −1.90 days; I2 = 50.8%), and hospital LOS (6 studies, 976 patients: WMD −4.06 days; 95% CI −5.19 to −2.94 days; I2 = 71.7%; Fig. 5) favoring MIMVS.
Fig. 2.
Forest plot for acute renal failure.
Fig. 3.
Forest plot for prolonged intubation.
Fig. 4.
Forest plot for blood transfusion.
Fig. 5.
Forest plot for hospital length of stay.
There were no statistically significant differences in the odds of stroke (6 studies, 1,117 patients: OR 0.79; 95% CI 0.27 to 2.31; I2 = 53.6%; Supplemental Fig. 1), respiratory infection (3 studies, 677 patients: OR 0.30; 95% CI 0.03 to 3.04; I2 = 69.2%), postoperative atrial fibrillation (3 studies, 656 patients: OR 0.61; 95% CI 0.33 to 1.13; I2 = 60.2%), mortality (6 studies, 1,217 patients: OR 0.59; 95% CI, 0.20 to 1.77; I2 = 64.6%; Supplemental Fig. 2), and reoperation for bleeding (6 studies, 1,100 patients, OR 0.58; 95% CI 0.25 to 1.39; I2 = 51.1%; Supplemental Fig. 3).
MIMVS was associated with significantly longer cross-clamp (7 studies, 1,262 patients: WMD 11.8 min; 95% CI 3.5 to 20.1 min; I2 = 90.1%) and cardiopulmonary bypass times (7 studies, 1,262 patients: WMD 23.0 min; 95% CI 10.4 to 35.6 min; I2 = 91.7%).
We performed 3 additional sensitivity analyses. The first sensitivity analysis consisted of including the 3 abstracts into the meta-analysis (yielding a total of 10 studies). The second sensitivity analysis consisted of performing meta-regression to assess whether the variations between the studies in the proportion of degeneration mitral disease or the proportion of mitral repair influenced the results. The third sensitivity analysis examined the influence of the inclusion of propensity-matched studies versus unmatched studies on the postoperative outcomes.
For the first sensitivity analysis, when all 10 studies where included for analysis, MIMVS group had significantly lower odds of acute renal failure (8 studies, OR 0.29; 95% CI 0.11 to 0.75; I2 = 67.5%), prolonged intubation (>48 h; 4 studies, OR 0.47; 95% CI 0.31 to 0.70; I2 = 9.8%), wound infection (3 studies, OR 0.14; 95% CI 0.05 to 0.44; I2 = 17.1%), and also less blood product transfusion (4 studies, WMD −0.96 units; 95% CI −1.61 to −0.30 units; I2 = 75.7%), shorter ICU LOS (6 studies, WMD −1.69 days; 95% CI −2.68 to −0.70 days; I2 = 89.2%) and hospital LOS (8 studies, WMD −3.12 days; 95% CI −4.62 to −1.62 days; I2 = 92.2%) favoring MIMVS. There were no statistically significant differences in the odds of stroke (9 studies, OR 0.60; 95% CI 0.22 to 1.63), respiratory infection (4 studies, OR 0.31; 95% CI 0.06 to 1.53), postoperative atrial fibrillation (3 studies, OR 0.61; 95% CI 0.33 to 1.13), mortality (9 studies, OR 0.56; 95% CI, 0.23 to 1.36), or reoperation for bleeding (7 studies, OR 0.58; 95% CI 0.25 to 1.39). MIMVS was associated with significantly longer cross-clamp (10 studies, WMD 14.2 min; 95% CI 7.4 to 21.0 min) and cardiopulmonary bypass times (10 studies, WMD 28.9 min; 95% CI 18.0 to 39.8 min).
Meta-regression revealed that the differences/similarities in outcomes between MIMVS and CS were not influenced by the variation in the proportion of degenerative mitral disease nor the proportion of mitral repair between the studies that were included in the meta-analysis (Table 2).
Table 2.
Meta-Regression Examining Influence of Variation in Proportion of Mitral Repair and Proportion of Degenerative Mitral Disease Between the Studies on Postoperative Outcomes.
| Outcomes | Regression coefficient | 95% CI | P value |
|---|---|---|---|
| Acute renal failure | Mitral repair: 0.05 | −6.98 to 7.09 | 0.98 |
| Degenerative regurgitation: −3.99 | −55.75 to 47.77 | 0.51 | |
| Prolonged intubation | Mitral repair: IS | — | — |
| Degenerative regurgitation: IS | — | — | |
| Blood transfusion | Mitral repair: 0.65 | −3.23 to 4.53 | 0.28 |
| Degenerative regurgitation: IS | — | — | |
| ICU length of stay | Mitral repair: IS | — | — |
| Degenerative regurgitation: IS | — | — | |
| Hospital length of stay | Mitral repair: −0.64 | −8.98 to 7.70 | 0.77 |
| Degenerative regurgitation: 10.39 | −91.06 to 70.29 | 0.35 | |
| Stroke | Mitral repair: 2.75 | −6.67 to 12.17 | 0.34 |
| Degenerative regurgitation: 3.61 | −10.42 to 17.64 | 0.38 | |
| Respiratory infection | Mitral repair: IS | — | — |
| Degenerative regurgitation: IS | — | — | |
| Postoperative AF | Mitral repair: 1.02 | −6.57 to 8.61 | 0.34 |
| Degenerative regurgitation: 2.05 | −12.91 to 17.01 | 0.33 | |
| Mortality | Mitral repair: IS | — | — |
| Degenerative regurgitation: IS | — | — | |
| Reoperation for bleeding | Mitral repair: IS | — | — |
| Degenerative regurgitation: IS | — | — |
Abbreviations: AF, atrial fibrillation; CI, confidence interval; ICU, intensive care unit; IS, insufficient studies.
In the third sensitivity analysis where we examined the influence of the inclusion of propensity-matched studies versus unmatched studies on the postoperative outcomes, meta-regression revealed that the differences/similarities in outcomes between MIMVS and CS were not influenced by the inclusion of both propensity-matched studies and unmatched studies (Table 3).
Table 3.
Meta-Regression Examining Influence of the Inclusion of Propensity-Matched Studies Versus Unmatched Studies on Postoperative Outcomes.
| Outcomes | Regression coefficient | 95% CI | P value |
|---|---|---|---|
| Acute renal failure | −1.30 | −4.29 to 1.70 | 0.26 |
| Prolonged intubation | 0.31 | −2.31 to 2.92 | 0.66 |
| Blood transfusion | 0.57 | −9.54 to 10.68 | 0.61 |
| ICU length of stay | 1.51 | −3.20 to 6.21 | 0.30 |
| Hospital length of stay | 1.42 | −3.98 to 6.81 | 0.51 |
| Stroke | −0.60 | −2.78 to 1.57 | 0.44 |
| Respiratory infection | insufficient studies | — | — |
| Postoperative AF | −0.44 | −4.62 to 3.74 | 0.41 |
| Mortality | −0.59 | −28.72 to 27.54 | 0.83 |
| Reoperation for bleeding | −0.32 | −8.28 to 7.63 | 0.70 |
| Cross-clamp time | 4.15 | −21.68 to 29.98 | 0.70 |
| CPB time | 16.14 | −17.33 to 49.62 | 0.27 |
Abbreviations: AF, atrial fibrillation; CI, confidence interval; CPB, cardiopulmonary bypass; ICU, intensive care unit.
Discussion
We present the first meta-analysis to compare the outcomes of MIMVS versus CS in elderly patients. We found that MIMVS is associated with lower odds of acute renal failure, prolonged intubation (>48 h), less blood product transfusion, and shorter ICU and hospital LOS. There was also no significant difference in mortality, stroke, respiratory infection, postoperative atrial fibrillation, or reoperation for bleeding. As expected, MIMVS was associated with longer cross-clamp and cardiopulmonary bypass times. All of these findings were consistent whether we included or excluded the 3 studies to which we only had access to their abstracts. Also, these findings were not influenced by the variation in the proportion of degenerative mitral disease or the proportion of mitral repair in the studies that were included.
Minimally invasive techniques have been applied to mitral repair for nearly 2 decades with good results in experienced hands. Repair rates and early and late durability with an endoscopic, right minithoracotomy approach have been shown to be excellent and equally as good as sternotomy in centers of expertise.2 However, most of the studies comparing MIMVS to CS included younger patients, most commonly in their fifth decade of life.17-22
Concerns have been previously raised that MIMVS has additional unique complications, including phrenic nerve palsy, unilateral pulmonary edema, and retrograde aortic dissection which may be potentially increased in a frail elderly population.23 In a Society of Thoracic Surgeons Database analysis of over 28,000 patients undergoing mitral repair, they found a significantly increased risk for perioperative stroke in patients undergoing less invasive mitral operations but concluded that these may be related to beating or fibrillating heart techniques.23 Our results are reassuring for stroke risk in MIMVS in that there was no increased risk or even signal towards more strokes in the MIMVS group. With respect to other complications, our findings were also reassuring with lower odds of many of these complications in the MIMVS group.
Several other studies have investigated the differences in outcomes between MIMVS and CS in this elderly population; however, these studies were limited in generalizability and most importantly, their estimated results were restricted by the rarity of the postoperative outcomes/complications.
Study Limitations
Our study has some limitations. All of the studies included in our analysis were retrospective studies and were therefore limited by the intrinsic biases that they may carry, particularly the selection bias (confounding by indication) where patients had to be good candidates to undergo a minimally invasive approach. As in any meta-analysis combining/pooling results from different studies, it is expected to see differences in the characteristics of the individual studies that are included in the analysis. This explains why we have performed our meta-analysis using random-effects (rather than fixed effects) in order to account for the between-studies variabilities. Some of the outcomes have substantial heterogeneity. We have attempted to understand the source of this heterogeneity and have performed 3 meta-regressions (as part of sensitivity analyses) and found that this heterogeneity was neither influenced by the variation in the proportion of degenerative mitral disease, nor the proportion of mitral repair between the studies that were included in the meta-analysis, nor the inclusion of both propensity-matched studies and unmatched studies. Other elements that might be driving the heterogeneity could be the different definitions of outcomes among various studies (such as the case for acute renal failure) and the presence of other between-studies variations that were not accounted for in our analysis. An example of this could be the variations in some intraoperative variables, for example the use of central versus peripheral cannulation, that could have caused the significant heterogeneity in cross-time and bypass times. Our postoperative outcomes were limited to in-hospital complications and did not report on long-term outcomes, simply because the 10 studies included in this meta-analysis did not provide any long-term follow-up.
Conclusions
In the first meta-analysis in elderly patients comparing MIMVS to CS in elderly patients, we found that compared to CS, the minimally invasive approach when performed by experienced surgeons, was not associated with significantly different mortality, but was associated with significantly lower postoperative morbidities, blood transfusion, and shorter ICU and hospital LOS. Despite longer cross-clamp and bypass times, there does not appear to be a physiologic penalty and the risk of renal failure is in favor of MIMVS. Therefore, patients over 65 years presenting at experienced cardiac surgery centers should not be deprived from the advantages of a surgical mitral intervention, simply on the basis of their perceived “higher risk.”
Supplemental Material
Supplemental material, Supplementary Material 1, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Supplementary Material 2, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Supplementary Material 3, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Supplementary Material 4, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Visual Abstract, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MWC has received speaker’s honoraria from Medtronic, Edwards Lifesciences, Boston Scientific, and Abbott Vascular.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Statement: Institutional Review Board approval was not required for this study and no consent was obtained since it did not include any study participants.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Hawkins RB., Mehaffey JH., Mullen MGet al. A propensity matched analysis of robotic, minimally invasive, and conventional mitral valve surgery. Heart 2018; 104: 1970–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagendran J., Catrip J., Losenno KLet al. Minimally invasive mitral repair surgery: why does controversy still persist? Expert Rev Cardiovasc Ther 2017; 15: 15–24. [DOI] [PubMed] [Google Scholar]
- 3.Singh JP., Evans JC., Levy Det al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol 1999; 83: 897–902. [DOI] [PubMed] [Google Scholar]
- 4.Lamelas J., Sarria A., Santana Oet al. Outcomes of minimally invasive valve surgery versus median sternotomy in patients age 75 years or greater. Ann Thorac Surg 2011; 91: 79–84. [DOI] [PubMed] [Google Scholar]
- 5.Kolh P., Kerzmann A., Lahaye Let al. Cardiac surgery in octogenarians; peri-operative outcome and long-term results. Eur Heart J 2001; 22: 1235–1243. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins RB., Mehaffey JH., Kessel SMet al. Minimally invasive mitral valve surgery is associated with excellent resource utilization, cost, and outcomes. J Thorac Cardiovasc Surg 2018; 156: 611–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells GA., Shea B,., O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. ScienceOpen , https://www.scienceopen.com/document?vid=54b48470-4655-4081-b5d4-e8ebe8d1792e (2020, accessed 27 May 2020).
- 8.Holzhey DM., Shi W., Borger MAet al. Minimally invasive versus sternotomy approach for mitral valve surgery in patients greater than 70 years old: a propensity-matched comparison. Ann Thorac Surg 2011; 91: 401–405. [DOI] [PubMed] [Google Scholar]
- 9.Santana O., Reyna J., Grana Ret al. Outcomes of minimally invasive valve surgery versus standard sternotomy in obese patients undergoing isolated valve surgery. Ann Thorac Surg 2011; 91: 406–410. [DOI] [PubMed] [Google Scholar]
- 10.Iribarne A., Easterwood R., Russo MJet al. Comparative effectiveness of minimally invasive versus traditional sternotomy mitral valve surgery in elderly patients. J Thorac Cardiovasc Surg 2012; 143(4 Suppl): S86–S90. [DOI] [PubMed] [Google Scholar]
- 11.Losenno KL., Jones PM., Valdis Met al. Higher-risk mitral valve operations after previous sternotomy: endoscopic, minimally invasive approach improves patient outcomes. Can J Surg 2016; 59: 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen Q., Yu L-L., Zhang Q-Let al. Minimally invasive video-assisted mitral valve replacement with a right chest small incision in patients aged over 65 years. Braz J Cardiovasc Surg 2019; 34: 428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen CW., Chung JJ., Gaffey AC. The advantages of minimally-invasive mitral valve surgery can be safely translated to the elderly: a propensity-matched analysis. Innovations 2017; 12(Suppl 4): S172. [Google Scholar]
- 14.Chen CW., Auvil BJ,., Chung JJ, et al. The advantages of minimally-invasive mitral valve surgery can be safely translated to the elderly: a propensity score matched analysis. ePostersOnline , https://epostersonline.com/ismics2017/node/250 (2017, accessed 27 May 2020).
- 15.Petersen J., Naito S., Neumann Net al. Impact of minimally invasive mitral valve surgery in elderly patients. Thorac Cardiovasc Surg 2018; 66(S 01): S1–S110. [Google Scholar]
- 16.Van laeken E., Bové T,., Vandewiele K, et al. Minimally invasive thoracotomy is a ICU proven alternative approach for mitral valve surgery. Crit Care 2019; 23(Suppl 2): P122. [Google Scholar]
- 17.Grossi EA., LaPietra A., Ribakove GHet al. Minimally invasive versus sternotomy approaches for mitral reconstruction: comparison of intermediate-term results. J Thorac Cardiovasc Surg 2001; 121: 708–713. [DOI] [PubMed] [Google Scholar]
- 18.Suri RM., Schaff HV., Meyer SRet al. Thoracoscopic versus open mitral valve repair: a propensity score analysis of early outcomes. Ann Thorac Surg 2009; 88: 1185–1190. [DOI] [PubMed] [Google Scholar]
- 19.Ryan WH., Brinkman WT., Dewey TMet al. Mitral valve surgery: comparison of outcomes in matched sternotomy and port access groups. J Heart Valve Dis 2010; 19: 51–58. [PubMed] [Google Scholar]
- 20.Raanani E., Spiegelstein D., Sternik Let al. Quality of mitral valve repair: median sternotomy versus port-access approach. J Thorac Cardiovasc Surg 2010; 140: 86–90. [DOI] [PubMed] [Google Scholar]
- 21.Speziale G., Nasso G., Esposito Get al. Results of mitral valve repair for Barlow disease (bileaflet prolapse) via right minithoracotomy versus conventional median sternotomy: a randomized trial. J Thorac Cardiovasc Surg 2011; 142: 77–83. [DOI] [PubMed] [Google Scholar]
- 22.Goldstone AB., Atluri P., Szeto WYet al. Minimally invasive approach provides at least equivalent results for surgical correction of mitral regurgitation: a propensity-matched comparison. J Thorac Cardiovasc Surg 2013; 145: 748–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gammie JS., Zhao Y., Peterson EDet al. Less-invasive mitral valve operations: trends and outcomes from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg 2010; 90: 1401–1410. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary Material 1, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Supplementary Material 2, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Supplementary Material 3, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Supplementary Material 4, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery
Supplemental material, Visual Abstract, for Minimally Invasive Versus Sternotomy for Mitral Surgery in the Elderly: A Systematic Review and Meta-Analysis by Ali Hage, Fadi Hage, Hussein Al-Amodi, Suruchi Gupta, Stefania I. Papatheodorou, Robert Hawkins, Gorav Ailawadi, Murray A. Mittleman and Michael W. A. Chu in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery