Abstract
Background
Global obesity estimates show a steadily increasing pattern across socioeconomic and geographical divides, especially among women. Our analysis tracked and described obesity trends across multiple equity dimensions among women of reproductive age (15–49 y) in 11 sub-Saharan African (SSA) countries during 1994–2015.
Methods
This study consisted of a cross-sectional series analysis using nationally representative demographic and health surveys (DHS) data. The countries included were Cameroon, Comoros, Congo, Cote d'Ivoire, Ghana, Kenya, Lesotho, Nigeria, Senegal, Zambia and Zimbabwe. The data reported are from a reanalysis conducted using the WHO Health Equity Assessment Toolkit that assesses inter- and intra-country health inequalities across socioeconomic and geographical dimensions. We generated equiplots to display intra- and inter-country equity gaps.
Results
There was an increasing trend in obesity among women of reproductive age across all 11 SSA countries. Obesity increased unequally across wealth categories, place of residence and educational measures of inequality. The wealthiest, most educated and urban dwellers in most countries had a higher prevalence of obesity. However, in Comoros, obesity did not increase consistently with increasing wealth or education compared with other countries. The most educated and wealthiest women in Comoros had lower obesity rates compared with their less wealthy and less well-educated counterparts.
Conclusion
A window of opportunity is presented to governments to act structurally and at policy level to reduce obesity generally and prevent a greater burden on disadvantaged subpopulation groups in sub-Saharan Africa.
Keywords: Equity analysis, Obesity, Women of reproductive age-group, sub-Saharan Africa
Introduction
The WHO defines obesity as a body mass index (BMI) of ≥30 kg/m2.1 Adult obesity is a complex disease with multifactorial determinants that is strongly associated with multiple comorbidities.2 Genetic factors, sedentariness, diet and socioeconomic factors are common determinants of adult obesity.3 The comorbidities associated with obesity including cardiovascular and cerebrovascular events, as well as the economic implications for healthcare systems, make obesity a topical issue of global health importance.2 In countries of the global North, for example, the USA, the annual medical spending on obesity and obesity-related complications is ∼US$190 billion according to one estimate.4 Over the last 2 decades, the prevalence of obesity has dramatically increased worldwide, especially among women,5 and is primarily attributed to increases in the consumption of cheap calorie-dense foods, physical inactivity, rapid urbanisation and economic growth.6 Together, these factors drive the global obesity burden,7,8 with 2.1 billion people estimated to be either overweight or obese.9
Obesity is currently a major contributor to the global burden of disease. Although initially considered a health challenge of the global North, obesity is increasingly prevalent in countries of the global South.10,11 Indeed, sub-Saharan Africa is recognised as having a ‘double burden’ of malnutrition, that is, the coexistence of undernutrition (wasting/stunting) and overnutrition (overweight/obesity).12 Nevertheless, investments in preventive health have traditionally focused on undernutrition and food insecurity while neglecting the problem of excess adiposity, which continues to be perceived as less prevalent in sub-Saharan African (SSA) contexts.13 Interestingly, whether considered from a global or Afro-centric epidemiological perspective, the obesity burden has not remained static over the years, with obesity estimates showing a varying but steadily increasing pattern across socioeconomic, urban-rural, intra- and inter-country divides.5 How these patterns vary across equity dimensions in diverse contexts remains an understudied area.
The study of obesity patterns has benefitted from temporal analysis, with some authors tracking obesity trends in Latin American and Caribbean countries,14 while others have focused on Europe and North America.15 These studies tend to reveal that there is an increase in the prevalence of obesity with an unequal distribution and burden across socioeconomic groups. One large SSA study that tracked obesity trends using nationally representative data during 1980–2014 reported increasing trends in BMI values for various countries on the continent16; however, it did not consider socioeconomic equity dimensions of these trends. Other SSA studies analysing the differential prevalence of adult obesity across socioeconomic domains have focused mainly on measures of income inequality. These studies found that wealthier segments of the population are more likely to be obese compared with their poorer counterparts.17,18 To our knowledge, there is no analysis of obesity trends among women of reproductive age across multi-dimensional measures of socioeconomic and geographical inequities exclusively in SSA countries.
Tracking obesity trends in SSA contexts across various equity dimensions is important and timely, especially because of policy commitments made by the WHO to end the upsurge in obesity in Africa by 2025.13 Extant evidence suggests that as the burden of obesity increases in resource-limited countries, people in socioeconomically disadvantaged subpopulations tend to be disproportionately represented.18 In a landscape of relatively weak and fragile health systems that are prevalent in several SSA countries that are already devoting significant resources to curtail threats from infectious diseases, an uncontrolled increase in obesity could overwhelm those systems. Our study tracked and described obesity trends across multiple equity dimensions in 11 SSA countries during 1994–2015 using nationally representative health survey data across three time periods.
Methods
Study design and data source
We conducted a cross-sectional series analysis of prevalence of obesity using nationally representative Demographic and Health Survey (DHS) data from 1994 to 2015 unpacked across socioeconomic and geographical equity dimensions. We extracted and used reanalysed and disaggregated DHS data from the WHO Health Equity Assessment Toolkit (HEAT).19 The HEAT is an online tool developed by the WHO to aid assessment of intra- and inter-country health equity gaps.20 The tool uses nationally representative data and also provides multi-country equity comparisons of health outcomes, thus is considered a useful tool for monitoring and tracking cross-country inequities. The disaggregated nationally representative data, available through HEAT, are the product of reanalyses of publicly available datasets from the DHS, multiple indicator cluster and reproductive health surveys. The data included in this analysis come from DHS datasets that are large-scale, nationally representative household surveys implemented in >90 low- and middle-income countries worldwide.21 The surveys are conducted through standardised face-to-face interviews and they report standard global health and population health indicators, including data with which to assess obesity in selected countries.21 We restricted our study to 11 SSA countries with reanalysed obesity data for at least two time periods in the HEAT database, namely, Cameroon, Comoros, Congo, Cote d'Ivoire, Ghana, Kenya, Lesotho, Nigeria, Senegal, Zambia and Zimbabwe.
Study population
The study population included non-pregnant women of reproductive age (15–49 y) in the 11 SSA countries. We chose the age group of 15–49 y for reasons of data availability and comparability, as the reanalysed DHS survey data in HEAT were complete for this subpopulation across all 11 SSA countries. All surveys used for analysis included de-identified datasets. Ethical approval was not sought for this analysis since it involved secondary data. The DHS study protocols were reviewed and approved by the inner city fund (ICF) International Institutional Review Board and each country's ethics board before commencement of the surveys.22
Data analysis
The primary outcome for our analysis was obesity and this was defined as BMI≥30 kg/m2 (i.e. body weight in kilograms divided by height in metres squared).23 In the datasets used, the prevalence of obesity was disaggregated by three socioeconomic equity indicators, family economic status, education index and area of residence. The DHS ascertains family economic status as a composite household wealth index of living standards, calculated based on ownership of specific household items and access to specific services.24 The DHS wealth index generates quintiles ranging from the poorest to the richest (i.e. Q1–Q5). The DHS generates education indexes (E1–E3) using the total number of formal years of education for an individual broken down into the least (E1) and most educated (E3). Area of residence is reported as rural or urban across all countries in DHS datasets.
Gaps in the prevalence of obesity were assessed using a single summary measure of absolute difference in the prevalence of obesity (in percentage points) between the highest and lowest extremes within each socioeconomic equity indicator.14,20 Median prevalence of obesity across the 11 SSA countries was computed across three time periods (1994–2004, 2005–2009 and 2010–2015) to show obesity trends from 1994 to 2015. We report inequalities for obesity and trends in the national prevalence of obesity across these time periods (including the latest available datasets) across the 11 SSA countries. All equiplots (to display socioeconomic inequalities in obesity) and graphs were created using Microsoft Excel (Microsoft Corp., Redmond, WA, USA).
Results
Trends in obesity across 11 SSA countries, 1994–2015
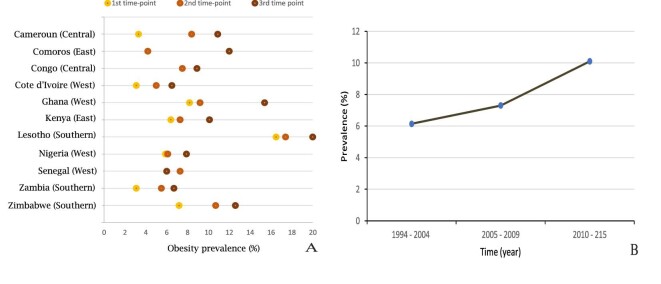
During 1994–2015, every country included in the analysis (except for Senegal) saw an overall increase in the age- and gender-specific prevalence of obesity over time, with prevalence across countries increasing at different rates (Figure 1). The lowest national prevalence values recorded at a single point in time were in Cote D'Ivoire (3.1% in 1994) and Zambia (3.1% in 2001), while the highest was in Lesotho (20% in 2014). The most rapid increase within two time periods occurred in Ghana (2008–2014), where the prevalence of obesity increased from 9.2 to 15.4% (Table 1). In Comoros, there was an increase from 4.2 to 12.0%, although this occurred over 16 y (1996–2012). In Senegal, the only country in our analysis where the prevalence of obesity appeared to be reducing, prevalence decreased from 7.3 to 6.0% during 2005– 2010. Nigeria saw only a marginal increase between 2003 and 2008 (from 5.9 to 6.1%), although the later data showed a more rapid increase.
Figure 1.
(A) Country-level trends in the prevalence of obesity; (B) median prevalence of obesity trends across three time periods (1994–2004, 2005–2009 and 2010–2015) in 11 sub-Saharan African countries. First time period: Cameroon (DHS 1998), Cote d'Ivoire (DHS 1994), Ghana (DHS 2003), Kenya (DHS 2003), Lesotho (DHS 2004), Nigeria (DHS 2003), Zambia (DHS 2001) and Zimbabwe (DHS 2005). Second time period: Cameroon (DHS 2004), Comoros (DHS 1996), Congo (DHS 2005), Cote d'Ivoire (DHS 1998), Ghana (DHS 2008), Kenya (DHS 2008), Lesotho (DHS 2009), Nigeria (DHS 2008), Senegal (DHS 2005), Zambia (DHS 2007) and Zimbabwe (DHS 2010). Third time period: Cameroon (DHS 2011), Comoros (DHS 2012), Congo (DHS 2011), Cote d'Ivoire (DHS 2011), Ghana (DHS 2014), Kenya (DHS 2014), Lesotho (DHS 2014), Nigeria (DHS 2013), Senegal (DHS 2010), Zambia (DHS 2013) and Zimbabwe (DHS 2015).
Table 1.
The prevalence of obesity among women aged 15–49 y by country, year and equity dimensions
| Wealth quintile index | Educational attainment | Residence | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gap, per- | Gap, per- | Rural | Urban | Gap, per- | ||||||||||
| National | Q1 (95% | Q2 (95% | Q3 (95% | Q4 (95% | Q5 (95% | centage | E1 (95% | E2 (95% | E3 (95% | centage | (95% | (95% | centage | |
| Country | Rate | CI) | CI) | CI) | CI) | CI) | points | CI) | CI) | CI) | points | CI) | CI) | points |
| Cameroon | ||||||||||||||
| 2011 | 10.9 | 0.9 (0.5 to 1.6%) | 5.3 (4.0 to 7.0%) | 8.3 (6.7 to 10.2%) | 14.8 (13.0 to 16.7%) | 19 (17. 2 to 20.9%) | 18.1 | 3.8 (2.8 to 5.2%) | 11.6 (10.3 to 13.1%) | 13.1 (11.9 to 14.4%) | 9.3 | 4.8 (4.1 to 5.7%) | 15.8 (14. 6 to 17.1%) | 11.0 |
| 2004 | 8.4 | 1.6 (0.9 to 2.9%) | 2.4 (1.5 to 4.0%) | 6.7 (5.3 to 8.3%) | 12.3 (10.3 to 14.7%) | 15.1 (13.0 to 17.5%) | 13.5 | 3.4 (2.2 to 5.1%) | 8.9 (7.6 to 10.3%) | 10.5 (9.2 to 12.0%) | 7.1 | 3.3 (2.6 to 4.2%) | 12.5 (11.2 to 14%) | 9.2 |
| 1998 | 3.3 | - (-) | 0.8 (0.2to 3.1%) | 1.5 (0.7 to 3.6%) | 5.9 (4.0 to 8.8%) | 9.2 (6.5 to 12.9%) | 8.4 | 0.0 (0.0 to 0.0%) | 3.1 (1.9 to 5.0%) | 7.7 (5.5 to 10.7%) | 7.7 | 1.7 (0.9 to 3.0%) | 7.7 (5.5 to 10.8%) | 6.0 |
| Comoros | ||||||||||||||
| 2012 | 12 | 10.2 (7.5 to 13.8%) | 9.5 (7.6 to 11.9%) | 14.6 (12.2 to 17.4%) | 11.2 (9.2 to 13.7%) | 13.6 (11.2 to 16.5%) | 5.1 | 15.8 (13.5 to 18.4%) | 12.2 (9.7 to 15.4%) | 9.5 (8.3 to 10.9%) | 6.3 | 10.3 (8.8 to 11.9%) | 15.3 (13.5 to 17.2%) | 5.0 |
| 1996 | 4.2 | 1.2 (0.3 to 5.0%) | 1.9 (0.6 to 5.7%) | 3.3 (1.3 to 8.0%) | 5.7 (2.9 to 10.9%) | 11.2 (7.1 to 17.2%) | 10.0 | 3.7 (2.4 to 5.7%) | 3.8 (1.6 to 8.5%) | 7.0 (3.3 to 14.3%) | 6.3 | 2.4 (1.3 to 4.3%) | 9.7 (7.3 to 12.8%) | 7.3 |
| Congo | ||||||||||||||
| 2011 | 8.9 | 2.2 (1.6 to 3.0%) | 5.6 (3.6 to 8.6%) | 9.4 (6.8 to 12.7%) | 10.6 (7.5 to 14.8%) | 15.4 (12.4 to 19.0%) | 13.2 | 4.1 (2.0 to 7.9%) | 6.1 (4.1 to 8.9%) | 10.3 (8.6 to 12.4%) | 6.2 | 3.8 (2.6 to 5.4%) | 11.3 (9.6 to 13.3%) | 7.5 |
| 2005 | 7.5 | 1.8 (0.8 to 4.0%) | 3.3 (1.8 to 6.0%) | 5.5 (4.0 to 7.4%) | 9.0 (7.6 to 10.6%) | 15.3 (13.3 to 17.7%) | 13.5 | 6.7 (4.6 to 9.7%) | 5.2 (3.6 to 7.6%) | 8.7 (7.7 to 9.8%) | 3.5 | 3.4 (2.0 to 5.9%) | 10.5 (9.4 to 11.6%) | 7.1 |
| Cote D'Ivoire | ||||||||||||||
| 2011 | 6.5 | 1.3 (0.6 to 2.9%) | 3.7 (2.3 to 5.8%) | 5.9 (3.9 to 8.8%) | 9.0 (7.0 to 11.5%) | 10.6 (7.9 to 14.0%) | 9.3 | 6.4 (5.1 to 8.0%) | 7.3 (5.7 to 9.4%) | 5.9 (4.2 to 8.3%) | 1.4 | 2.8 (2.0 to 3.9%) | 10.1 (8.4 to 12.2%) | 7.3 |
| 1998 | 5.0 | 0.0 (0.0 to 0.0%) | 2.3 (1.1 to 4.8%) | 3.2 (1.5 to 6.8%) | 6.8 (5.1 to 9.0%) | 9.8 (8.1 to 11.7%) | 9.8 | 4.0 (2.9 to 5.5%) | 6.1 (4.6 to 8.1%) | 6.5 (4.7to 8.9%) | 2.5 | 2.5 (1.6 to 4.0%) | 8.2 (7.1 to 9.6%) | 5.7 |
| 1994 | 3.1 | 0.7 (0.3 to 1.9%) | 1.7 (1.0 to 2.9%) | 2.0 (1.1 to 3.6%) | 3.7 (2.3 to 5.9%) | 8.7 (6.7 to 11.1%) | 8.0 | 2.5 (1.7 to 3.4%) | 3.9 (2.7 to 5.5%) | 5.3 (2.9 to 9.5%) | 2.8 | 1.3 (0.9 to 2.0%) | 6.2 (4.9 to 7.9%) | 4.9 |
| Ghana | ||||||||||||||
| 2014 | 15.4 | 1.7 (1.0 to 2.9%) | 5.5 (3.8 to 7.8%) | 13.4 (11.1 to 16.1%) | 20.7 (17. 2 to 24.8%) | 29.0 (25.7 to 32.4%) | 27.3 | 8.8 (6.7 to 11.5%) | 15.2 (12.1 to 18.8%) | 17.4 (15.6 to 19.4%) | 8.6 | 8.7 (7.3 to 10.2%) | 20.1 (18.5 to 23.6%) | 11.4 |
| 2008 | 9.2 | 2.1 (1.1 to 3.8%) | 3.2 (2.2 to 4.7%) | 4.7 (3.4 to 6.4%) | 11.8 (9.8 to 14.2%) | 19.7 (17.3 to 22.5%) | 17.6 | 5.2 (3.8 to 7.0%) | 9.1 (7.3 to 11.4%) | 10.7 (9.5 to 12.0%) | 5.5 | 4.7 (3.8 to 5.7%) | 14.0 (12.5 to 15.6%) | 9.3 |
| 2003 | 8.2 | 1.3 (0.7 to 2.3%) | 2.0 (1.1 to 3.4%) | 4.3 (3.0 to 6.1%) | 9.2 (7.3 to 11.5%) | 18.4 (16.2 to 20.1%) | 17.1 | 4.6 (3.4 to 6.4%) | 7.1 (5.5 to 9.0%) | 10.4 (9.0 to 11.9%) | 5.8 | 3.7 (2.7 to 4.9%) | 12.8 (11.3 to 14.5%) | 9.1 |
| Kenya | ||||||||||||||
| 2014 | 10.1 | 1.9 (1.4 to 2.5%) | 4.8 (3.8 to 5.9%) | 6.4 (5.4 to 7.6%) | 12.5 (10. 9 to 14.4%) | 19.4 (17. 2 to 21.7%) | 17.5 | 5.8 (4.1 to 8.0%) | 9.1 (8.1 to 10.0%) | 12.1 (10. 8 to 13.4%) | 6.3 | 7.1 (6.5 to 7.8%) | 14.7 (13. 2 to 16.4%) | 7.6 |
| 2008 | 7.3 | 1.5 (0.8 to 3.0%) | 2.7 (1.8 to 4.2%) | 6.2 (4.9 to 7.9%) | 8.7 (7.0 to 10.8%) | 13.4 (9.9 to 18.0%) | 11.9 | 2.5 (1.5 to 4.4%) | 6.3 (5.2 to 7.3%) | 10.0 (8.0 to 12.4%) | 7.5 | 5.6 (4.8 to 6.7%) | 12.1 (8.7 to 16.7%) | 6.5 |
| 2003 | 6.4 | 1.6 (0.9 to 2.9%) | 2.4 (1.5 to 3.7%) | 4.7 (3.5 to 6.3%) | 6.4 (5.2 to 7.9%) | 13.3 (11.6 to 15.1%) | 11.7 | 4.3 (3.0 to 6.2%) | 4.5 (3.8 to 5.3%) | 10.8 (9.2 to 12.6%) | 6.5 | 4.4 (3.6 to 5.3%) | 12.4 (10.8 to 14.2%) | 8.0 |
| Lesotho | ||||||||||||||
| 2014 | 20.0 | 6.2 (4.4 to 8.7%) | 16.1 (12.4 to 20.5%) | 16.2 (13.0 to 20.0%) | 25.5 (21.4 to 30.1%) | 27.3 (23.2 to 31.9%) | 21.1 | 19.1 (6.1 to 46.2%) | 18.6 (16.0 to 21.4%) | 20.9 (18.5 to 23.5%) | 2.3 | 18.3 (16.3 to 20.6%) | 22.9 (18.8 to 27.5%) | 4.6 |
| 2009 | 17.4 | 7.1 (4.8 to 10.5%) | 12.9 (10.2 to 16.0%) | 12.8 (10.1 to 16.1%) | 16.2 (13.8 to 19.1%) | 29.9 (26.2 to 33.9%) | 22.8 | 12.4 (5.6 to 25.1%) | 15.8 (13.9 to 17.9%) | 19.0 (16.8 to 21.4%) | 6.6 | 14.2 (12.8 to 15.7%) | 24.0 (20.7 to 27.8%) | 9.8 |
| 2004 | 16.5 | 8.1 (5.5 to 11.8%) | 9.9 (7.6 to 12.7%) | 14.8 (11.5 to 18.8%) | 18.4 (15.0 to 22.3%) | 24.1 (21.2 to 27.2%) | 16.0 | 13.4 (7.1 to 23.7%) | 15.7 (13.9 to 17.7%) | 17.8 (15.4 to 20.4%) | 4.4 | 15.6 (14.2 to 17.2%) | 19.1 (16.0 to 22.7%) | 3.5 |
| Nigeria | ||||||||||||||
| 2013 | 7.6 | 1.9 (1.2 to 3.0%) | 3.0 (2.5 to 3.6%) | 5.1 (4.5 to 5.8%) | 8.8 (8.0 to 9.6%) | 16.0 (15.0 to 17.1%) | 14.1 | 3.6 (3.1 to 4.3%) | 8.9 (7.9 to 10.0%) | 10.1 (9.4 to 10.8%) | 6.5 | 4.5 (4.0 to 5.1%) | 11.5 (10.8 to 12.2%) | 7.0 |
| 2008 | 6.1 | 1.8 (1.4 to 2.2%) | 2.3 (1.9 to 2.8%) | 4.2 (3.7 to 4.8%) | 6.9 (6.2 to 7.8%) | 12.8 (11.7 to 14.1%) | 11.0 | 3.2 (2.8 to 3.6%) | 6.7 (5.9 to 7.5%) | 8.0 (7.2 to 8.7%) | 4.8 | 4.0 (3.6 to 4.5%) | 9.6 (8.7 to 10.6%) | 5.6 |
| 2003 | 5.9 | 2.1 (1.2 to 3.6%) | 2.8 (1.6 to 4.8%) | 5.0 (3.6 to 6.9%) | 5.8 (4.4 to 7.7%) | 11.7 (9.6 to 14.1%) | 9.6 | 3.6 (2.8 to 4.7%) | 6.1 (4.5 to 8.2%) | 7.9 (6.3 to 9.9%) | 4.3 | 3.8 (2.9 to 4.8%) | 9.7 (8.1 to 11.5%) | 5.9 |
| Senegal | ||||||||||||||
| 2010 | 6.0 | 2.6 (1.7 to 3.8%) | 3.3 (2.3 to 4.7%) | 6.3 (4.6 to 8.4%) | 5.9 (4.1 to 8.5%) | 9.6 (7.1 to 12.9%) | 7.0 | 5.7 (4.6 to 7.0%) | 7.5 (5.6 to 9.8%) | 5.2 (3.5 to 7.7%) | 2.3 | 3.1 (2.5 to 3.7%) | 8.8 (7.1 to 10.9%) | 5.7 |
| 2005 | 7.3 | 2.2 (1.3 to 3.5%) | 2.7 (1.8to 4.0%) | 6.6 (4.7 to 9.1%) | 9.8 (7.5 to 12.9%) | 11.5 (9.2 to 14.3%) | 9.3 | 5.8 (4.7 to 7.1%) | 9.6 (7.5 to 12.3%) | 8.9 (6.3 to 12.5%) | 3.8 | 3.4 (2.7 to 4.3%) | 11.0 (9.3 to 13.0%) | 7.6 |
| Zambia | ||||||||||||||
| 2013 | 6.7 | 0.8 (0.5 to 1.3%) | 1.9 (1.4 to 2.6%) | 3.7 (3.0 to 4.7%) | 9.3 (8.1 to 10.7%) | 13.7 (12.1 to 15.5%) | 12.9 | 3.2 (2.2 to 4.8%) | 5.2 (4.6 to 6.0%) | 8.9 (7.9 to 9.9%) | 5.7 | 3.0 (2.5 to 3.5%) | 10.9 (9.9 to 11.9%) | 7.9 |
| 2007 | 5.5 | 0.9 (0.4 to 1.8%) | 0.7 (0.3 to 1.6%) | 2.4 (1.6 to 3.6%) | 6.2 (4.8 to 7.9%) | 13.1 (11.0 to 15.5%) | 12.2 | 2.2 (1.2 to 3.9%) | 4.5 (3.7 to 5.6%) | 7.9 (6.4 to 9.7%) | 5.7 | 2.1 (1.6 to 2.8%) | 9.9 (8.3 to 11.8%) | 7.8 |
| 2001 | 3.1 | 0.3 (0.1 to 0.9%) | 0.4 (0.2 to 1.0%) | 1.4 (0.8 to 2.4%) | 3.0 (2.1 to 4.3%) | 8.3 (6.7 to 10.1%) | 8.0 | 2.0 (1.1 to 3.5%) | 2.3 (1.8 to 2.9%) | 4.9 (3.9 to 6.2%) | 2.9 | 1.1 (0.8 to 1.6%) | 5.7 (4.6 to 7.1%) | 4.6 |
| Zimbabwe | ||||||||||||||
| 2015 | 12.6 | 3.4 (2.5 to 4.6%) | 6.4 (5.2 to 7.9%) | 8.8 (7.4 to 10.4%) | 15.2 (13.4 to 17.1%) | 23.4 (21.2 to 25.8%) | 20.0 | 9.2 (4.7 to 17.1%) | 8.0 (6.8 to 9.3%) | 14.3 (13.2 to 15.6%) | 6.3 | 7.9 (7.9 to 9.0%) | 20.2 (18.5 to 22.1%) | 12.3 |
| 2010 | 10.7 | 4.1 (3.0 to 5.6%) | 6.7 (5.3 to 8.6%) | 8.4 (6.9 to 10.3%) | 13.7 (11.9 to 15.7%) | 17.0 (15.1 to 19.0%) | 12.9 | 10.4 (5.7 to 18.3%) | 9.7 (8.5 to 11.0%) | 11.2 (10.1 to 12.4%) | 1.5 | 7.6 (6.6 to 8.7%) | 15.8 (14.2 to 17.5%) | 8.2 |
| 2005 | 7.2 | 2.7 (1.9 to 3.7%) | 2.9 (2.1 to 3.9%) | 4.8 (3.7 to 6.3%) | 7.9 (6.6 to 9.5%) | 13.8 (12.4 to 15.2%) | 11.1 | 10.0 (6.4 to 15.2%) | 5.8 (4.9 to 6.8%) | 7.8 (6.9 to 8.7%) | 4.2 | 4.3 (3.7 to 4.9%) | 11.6 (10.4 to 13.1%) | 7.3 |
Inequalities in obesity in the 11 SSA countries
Table 1 presents the prevalence of obesity across time in the 11 SSA countries by various equity dimensions (wealth quintile, educational attainment, place of residence). Percentage gaps (percentage points) between the highest and lowest values within each equity dimension are shown.
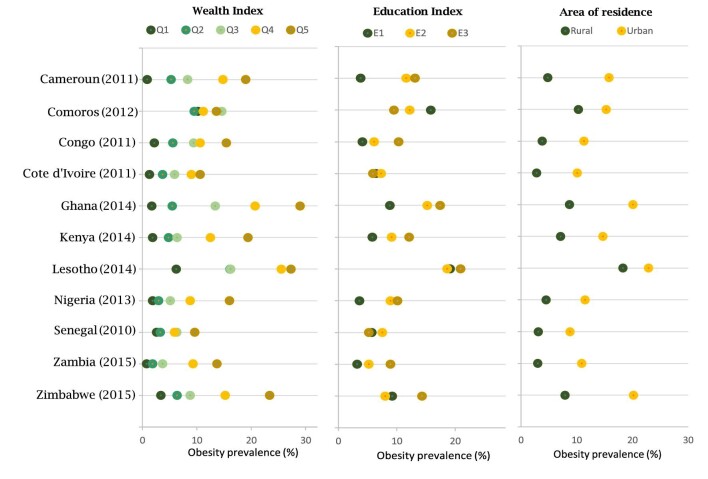
Inequality by wealth quintile
During 1994–2015, the highest prevalence within the wealth quintile category occurred in the fifth (wealthiest) quintile in Lesotho in 2009, where the rate was 29.9%; the highest rate based on the latest data was in the fifth quintile in Ghana in 2014, where the prevalence was 29.0%. In all 11 SSA countries analysed, the prevalence of obesity increased with wealth, except in Comoros. In Comoros, the highest prevalence in 2012 was in the third quintile (14.6%) and the lowest was in the second quintile (9.5%). In most countries, the percentage difference between the first and second quintiles was frequently small (<5%) but the difference between the third and fourth or fifth quintiles was larger (Figure 2).
Figure 2.
Inequalities in the prevalence of obesity among women aged 15–49 y in 11 sub-Saharan African countries, 2010–2015. Cameroon (DHS 2011), Comoros (DHS 2012), Congo (DHS 2011), Cote d'Ivoire (DHS 2011), Ghana (DHS 2014), Kenya (DHS 2014), Lesotho (DHS 2014), Nigeria (DHS 2013), Senegal (DHS 2010), Zambia (DHS 2013) and Zimbabwe (DHS 2015).
Inequalities by educational attainment
Obesity generally increased with higher levels of education in many countries, however, the gaps between the least and most educated were minimal compared with those associated with wealth differences. In 2012 in Comoros, the prevalence of obesity decreased as education levels increased (Figure 2 and Table 1). Also deviating from the general pattern of increasing prevalence with increasing education were Lesotho and Zimbabwe. In Lesotho in 2014, the highest prevalence of obesity was in E3 (20.9%) followed by E1 (19.1%) then E2 (18.6%). In Zimbabwe in 2015, the highest prevalence was in E3 (14.3%) followed by E1 (9.2%) then E2 (8.0%).
Inequalities by place of residence (urban vs rural)
All countries at every point in time saw higher rates of obesity in urban compared with rural dwellers although the gaps between the two varied across countries and time. The widest gap was in Zimbabwe in 2015, where the rural prevalence was 7.9% compared with an urban prevalence of 20.2% (Table 1). The second widest gap was in Ghana in 2014, where the rural prevalence was 8.7% compared with an urban prevalence of 20.09%. The smallest gap was in Lesotho in 2004, where the rural prevalence was 15.6% compared with an urban prevalence of 19.1%.
Discussion
Overall, our results show an increasing trend of obesity during 1994–2015 across the SSA countries analysed (with the notable exception of Senegal). This increasing trend in obesity was unequal across wealth quintiles, place of residence and educational measures of inequality, as those in the wealthiest quintile, the most educated and women resident in urban centres in most countries had a higher prevalence of obesity. Our findings underscore the WHO's declaration of overweight and obesity as a worldwide epidemic of equal concern to populations in the global North and South.1 Interestingly, earlier community-based surveillance and nationally representative time-trend analysis data up until the early 1990s suggest that obesity was not a significant health concern or was even non-existent in sub-Saharan Africa.25,26
The increase in obesity in sub-Saharan Africa has been linked to several factors including the impact of the nutrition transition and its consequences, occasioned by rapid economic growth and urbanisation in many SSA countries since the early 1990s.27,28 Economic growth in Africa has resulted in increased access to technology with a resultant reduction in energy expenditure in the more labour-intensive activities like farming, as well as in the less energy-intensive sectors such as services and manufacturing.29 Furthermore, changes in transportation and reduced time and space for exercise due to urbanisation have also led to reduced physical activity. The combination of these factors (an imbalance in energy intake through diet and energy expenditure) is believed to be driving the increasing trend in obesity over the last 3 decades in sub-Saharan Africa.29 Several health systems on the continent currently struggle to deal with threats from infectious diseases, maternal-child health issues, undernutrition and its complications. If urgent and sustained actions are not taken to address the rising curve of obesity on the continent then health systems across many SSA countries may undergo an increased burden of non-communicable diseases (NCDs) associated with obesity.
Lesotho, a landlocked south African country, consistently had the highest prevalence of obesity during the three time periods considered. This trend is consistent with previous systematic reviews that found that countries in southern Africa, in comparison with their counterparts in other parts of sub-Saharan Africa, tend to have a higher prevalence of obesity, especially among women.30,31 By contrast, Senegal (in western Africa) had the lowest overall prevalence of obesity based on the latest available data. Furthermore, the differences in prevalence were narrow across wealth categories compared with Lesotho, which had wide and increasing gaps in obesity between the poorest and wealthiest subpopulations. Our finding of decreasing prevalence of obesity in Senegal is supported by data from two studies conducted in 2009 and 2017, which found no statistically significant increases in obesity rates during the 9 y under study.32,33 The difference between Lesotho (southern Africa) and Senegal (western Africa) could be due to different genetic factors that determine obesity, environmental and socioeconomic influences and differences in cultural perceptions of body size, as obesity may be viewed differently in these two settings. Our findings suggest that different SSA countries may be at different stages of nutritional and epidemiological transitions.34
Across the intra-country equity dimensions explored in this analysis, place of residence and wealth were consistently associated with differences in the prevalence of obesity. Obesity was consistently higher in the urban and wealthier subpopulations. These findings agree with previous studies that have shown that urbanisation in sub-Saharan Africa has been accompanied by an upward trend in obesity rates among wealthy and urban dwellers.35,36 Increased globalisation over the last 3 decades has led to the popularisation of highly processed, energy-dense take-away foods and sugar-sweetened beverages across the continent, especially in urban settings. These foods, which are relatively cheap and easy to access in the global North, are disproportionately more expensive in sub-Saharan Africa and, consequently, are more likely to be accessed by the wealthy.37 Furthermore, urban areas have adopted more highly processed foods due to a greater availability of non-traditional foods and the increased attraction for western products, the attainment of which may be seen as a status symbol.35 This is also complicated by cultural beliefs in Africa that a bigger body is admirable and a sign of wealth.38,39 These explanations are important for understanding the higher obesity rates among people in higher income brackets and urban dwellers in our analysis. The fact that increasing levels of education did not consistently show decreasing trends in obesity is an interesting finding that needs to be explored further. One would ordinarily expect more educated subgroups to be less obese based on their knowledge of the adverse effects of increasing adiposity.
We also found that in Comoros, obesity did not increase consistently with increasing wealth or education. Indeed, for the latest time period, the most educated had the lowest prevalence of obesity, while the least educated had the highest prevalence of obesity. Furthermore, those in the third wealth quintile (middle class) had the highest prevalence of obesity compared with those in the fourth and fifth (high income) wealth quintiles. The trend in Comoros mirrors the trend in most high-income countries such as Australia, where the risk of obesity is more than doubled among the poorest and least educated subpopulations.40 We do not have an immediate explanation for this apparent trend in Comoros, which is in the same United Nations income group as many of the other countries included in this study, although it had the smallest population size of them. The trend witnessed for Comoros suggests that it may be at a later stage of the epidemiological and nutrition transition and might already be reflecting the reality in high-income countries, where obesity trends are higher among socioeconomically disadvantaged subpopulations.40 The trend in Comoros is likely to be the norm in coming decades in many SSA countries as globalisation may lead wealthier people to prefer western standards of body weight. This projected reversal of the current trend implies that lower socioeconomic groups already disproportionately represented by the burden of infectious diseases in SSA countries will experience an even greater burden of obesity-related complications.
Obesity presents an emerging threat to health equity as an individual's choices on what to eat, how much of it to eat and how much energy they can expend depends, to a large extent, on their socioeconomic circumstances. Thus, the approach to management of obesity in sub-Saharan Africa must be robust and responsive to the ongoing realities of socioeconomic inequalities in obesity trends and anticipated trends in the coming years. Governments should respond to the specific needs of local populations, contextualising global obesity prevention frameworks to reflect their country-level realities. Strategies that can be implemented include subsidisation of healthy foods (e.g. fruit and vegetables), adopting sugar taxes at country level and strong public health regulations on the numbers, availability and distribution of high-calorie fast food restaurants. These strategies should consider cultural and socioeconomic factors as well as geographical differences that can impact policy successes. The evidence on the policy approaches of SSA countries in general do not appear to indicate much success in innovatively adapting global NCD- and obesity-related frameworks.
Limitations
There are some limitations to our analysis that are worth considering. First, the end point of the latest time period was 2015, and emerging and recent data may show trends that vary from those reported. Nevertheless, our study contributes to the evidence base on obesity and health equities and helps to highlight a specific stage within the demographic and nutritional transition, where people from lower socioeconomic classes are less overweight and obese, hence the need to act urgently to prevent the possible reversal of this trend. Additionally, our study, which is based on a very specific demographic group (women aged 15–49 y), only covers a part of the overall situation, and equity dimensions of obesity for men or females younger or older than those included here may be different. Lastly, our data source, the WHO HEAT database, which provided a reanalysis of the DHS dataset for the chosen SSA countries, did not report on the subcategory of overweight (i.e. BMI= 25–29.9 kg/m2), but only provided data for obesity (BMI≥30 kg/m2). Tracking the trends in overweight, in addition to the data on obesity presented here, would be even more revealing on how the rise in obesity should be approached SSA.
Our study nonetheless is useful as it helps to highlight obesity trends among an extremely important demographic (females of reproductive age), and also highlights the possible negative challenge of a double burden within countries if the poorest women (who often already suffer higher rates of infectious diseases) have both greater obesity and NCDs. Future multi-country comparisons to understand the underlying social and behavioural patterns that determine a higher burden of obesity among particular subgroups (e.g. the richer, most educated and urban dwellers) should be conducted. Such research could utilise mixed (qualitative and quantitative) methodologies and would be important for understanding the contextual social and behavioural patterns that drive obesity trends among women of reproductive age across SSA.
Conclusion
There has been a general trend of increasing obesity among women of reproductive age in the 11 SSA countries studied. Our equity analyses suggest great variability in the prevalence of obesity by wealth and area of residence (i.e. urban vs rural) in the countries under study. Specifically, urban populations and those in the wealthiest quintile consistently maintained a higher prevalence than rural populations and those in the poorest quintile overall. Our findings provide evidence to guide policies and public health interventions, which can be focused on subpopulations of women of reproductive age with the highest burden of obesity, in this case the wealthiest and those in urban settings. A window of opportunity is presented to governments to act structurally and at the policy level to reduce obesity generally and prevent a greater burden on disadvantaged subpopulation groups.
Contributor Information
Oghenebrume Wariri, Medical Research Council (MRC) Unit The Gambia, at the London School of Hygiene and Tropical Medicine, Fajara, The Gambia.
Jacob Albin Korem Alhassan, Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan, Canada.
Godwin Mark, Department of Internal Medicine, Federal Teaching Hospital, Gombe, Nigeria.
Oyinkansola Adesiyan, Extra Care Charitable Trust, Coventry, UK.
Lori Hanson, Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan, Canada.
Authors’ contributions
OW conceived the study and study design together with JAKA, contributed to data analysis, developed the first draft of the manuscript and critically reviewed the final manuscript; JAKA led data analysis, developed the first draft of the manuscript and critically reviewed the final manuscript; GM contributed to data analysis, developed the first draft of the manuscript and critically reviewed the final manuscript; OA contributed to data analysis, developed the first draft of the manuscript and critically reviewed the final manuscript; and LH oversaw study design/implementation, critically reviewed and commented on all drafts of the manuscript. All the authors approved the final draft of the manuscript.
Funding
No external source of funding was received for this study.
Competing interests
None declared.
Ethical approval
This study was based on secondary analysis of already existing DHS data with no primary data collection involving patients or vulnerable groups. DHS surveys have been reviewed and approved by the ICF International Institutional Review Board and comply with the laws and the norms of the host country. The DHS obtained informed consent from all survey respondents.
Data availability
All data come from publicly available secondary data sources and are included in the article.
References
- 1.WHO . Obesity: Preventing and managing the global epidemic. World Health Organization; Technical Report Series, no. 894;2000:252. [PubMed] [Google Scholar]
- 2.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lakerveld J, Mackenbach J.. The upstream determinants of adult obesity. Obes Facts. 2017;10(3):216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cawley J, Meyerhoefer C.. The medical care costs of obesity: An instrumental variables approach. J Health Econ. 2012;31(1):219–30. [DOI] [PubMed] [Google Scholar]
- 5.Di Cesare M, Bentham J, Stevens GA, et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . What are the causes? Available from https://www.who.int/dietphysicalactivity/childhood_why/en/ [accessed May 10, 2020]. [Google Scholar]
- 7.James WPT.The fundamental drivers of the obesity epidemic. Obes Rev. 2008;9(suppl. 1):6–13. [DOI] [PubMed] [Google Scholar]
- 8.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378:804–14. [DOI] [PubMed] [Google Scholar]
- 9.Kelly T, Yang W, Chen CS, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32(9):1431–7. [DOI] [PubMed] [Google Scholar]
- 10.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377(9765):557–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Popkin BM, Doak CM.. The obesity epidemic is a worldwide phenomenon. Nutr Rev. 2009;56(4):106–14. [DOI] [PubMed] [Google Scholar]
- 12.Wojcicki JM.The double burden household in sub-Saharan Africa: Maternal overweight and obesity and childhood undernutrition from the year 2000: Results from World Health Organization Data (WHO) and Demographic Health Surveys (DHS). BMC Public Health. 2014;14:1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO . Strategic plan to reduce malnutrition in Africa adopted by WHO Member States | WHO | Regional Office for Africa . Available from https://www.afro.who.int/news/strategic-plan-reduce-malnutrition-africa-adopted-who-member-states [accessed May 10, 2020]. [Google Scholar]
- 14.Jiwani SS, Carrillo-Larco RM, Hernández-Vásquez A, et al. The shift of obesity burden by socioeconomic status between 1998 and 2017 in Latin America and the Caribbean: a cross-sectional series study. Lancet Glob Heal. 2019;7(12):e1644–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garrido-Miguel M, Cavero-Redondo I, Álvarez-Bueno C, et al. Prevalence and trends of overweight and obesity in European children from 1999 to 2016: A systematic review and meta-analysis. JAMA Pediatr. 2019;173(10):e192430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collaboration NRFC (NCD-R-AWG . Trends in Obesity and Diabetes Across Africa From 1980 to 2014: An Analysis of Pooled Population-Based Studies - PubMed. Available from https://pubmed.ncbi.nlm.nih.gov/28582528/ [accessed May 10, 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alaba O, Chola L.. Socioeconomic inequalities in adult obesity prevalence in South Africa: A decomposition analysis. Int J Environ Res Public Health. 2014;11(3):3387–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reyes Matos U, Mesenburg MA, Victora CG. Socioeconomic inequalities in the prevalence of underweight, overweight, and obesity among women aged 20–49 in low- and middle-income countries. Int J Obes. 2020;44(3):609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO . Health Equity Assessment Toolkit Available from https://whoequity.shinyapps.io/HEAT/ [accessed May 10, 2020]. [Google Scholar]
- 20.Hosseinpoor AR, Schlotheuber A, Nambiar D, et al. Health Equity Assessment Toolkit Plus (HEAT Plus): software for exploring and comparing health inequalities using uploaded datasets. Glob Health Action. 2018;11(sup1):20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The DHS Program . The DHS Program - Quality information to plan, monitor and improve population, health, and nutrition programs. Available from: https://www.dhsprogram.com/ [accessed May 10, 2020]. [Google Scholar]
- 22.ICF . The DHS Program - Protecting the Privacy of DHS Survey Respondents. The DHS Program website. Funded by USAID https://dhsprogram.com/What-We-Do/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm [accessed May 10, 2020]. [Google Scholar]
- 23.National Institute of Health, Heart, Lung and BI . Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. 1998. [PubMed] [Google Scholar]
- 24.The DHS Program . The DHS Program - Research Topics - Wealth Index. Available from https://dhsprogram.com/topics/wealth-index/Index.cfm [accessed May 10, 2020]. [Google Scholar]
- 25.Martorell R, Kettel Khan L, Hughes ML, et al. Obesity in women from developing countries. Eur J Clin Nutr. 2000;54(3):247–52. [DOI] [PubMed] [Google Scholar]
- 26.Pelletier DL, Rahn M.. Trends in body mass index in developing countries. Food Nutr Bull. 1998;19(3):223–39. [Google Scholar]
- 27.Popkin BM.The nutrition transition and its health implications in lower-income countries. Public Health Nutr. 1998;1(1):5–21. [DOI] [PubMed] [Google Scholar]
- 28.Vorster HH, Kruger A, Margetts BM. The nutrition transition in Africa: can it be steered into a more positive direction? Nutrients. 2011;3:429–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haggblade S, Duodu KG, Kabasa JD, et al. Emerging Early Actions to Bend the Curve in Sub-Saharan Africa's Nutrition Transition. Food Nutr Bull. 2016;37(2):219–41. [DOI] [PubMed] [Google Scholar]
- 31.Stevens GA, Singh GM, Lu Y, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Macia E, Duboz P, Gueye L. Prevalence of obesity in Dakar. Obes Rev. 2010;11(10):691–4. [DOI] [PubMed] [Google Scholar]
- 33.Duboz P, Cohen E, Macia E, et al. Prevalence of obesity and body size perceptions in urban and rural Senegal: New insight on the epidemiological transition in West Africa. Cardiovasc J Afr. 2017;28(5):324–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Defo BK. Demographic, epidemiological, and health transitions: Are they relevant to population health patterns in Africa? Glob Health Action. 2014;7(suppl. 1):22443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: A problem of the rich or the poor? BMC Public Health. 2009;9(1):465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steyn NP, Mchiza ZJ.. Obesity and the nutrition transition in Sub-Saharan Africa. Ann N Y Acad Sci. 2014;1311(1):88–101. [DOI] [PubMed] [Google Scholar]
- 37.Rosenheck R. Fast food consumption and increased caloric intake: A systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9:535–47. [DOI] [PubMed] [Google Scholar]
- 38.Okop KJ, Mukumbang FC, Mathole T, et al. Perceptions of body size, obesity threat and the willingness to lose weight among black South African adults: A qualitative study. BMC Public Health. 2016;16(1):365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flynn KJ, Fitzgibbon M. Body images and obesity risk among black females: A review of the literature. Ann Behavior Med. 1998;20:13–24. [DOI] [PubMed] [Google Scholar]
- 40.Backholer K, Mannan HR, Magliano DJ, et al. Projected socioeconomic disparities in the prevalence of obesity among Australian adults. Aust N Z J Public Health. 2012;36(6):557–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data come from publicly available secondary data sources and are included in the article.