Abstract
Several factors associated with graft preparation for the surgery of the anterior cruciate ligament (ACL) like the wrong thawed, prophylaxis, bone cuts, excessive bone removal as well as positioning problems like a tunnels-graft mismatch, insufficient harvesting of the donor's tendon, size graft limitations (length and diameter), uncontrolled rotation of graft in their longitudinal axis, over or under tensioned graft, fixation mistakes, bone defects, secondary arthrofibrosis or morbidity of the donor site, and others factors importantly affect the outcomes of the ACL surgery. In this sense, the Achilles tendon Allograft is an advantageous technique where many of the previous limitation factors described can be controlled during an appropriate preparation. However, to obtain the maximum potentialities of the graft a detailed knowledge of the preparation is required. Hence, we aimed to describe how to prepare the Achilles tendon Allograft to control the graft's length and diameter, bone removal, and fixation requirements.
Technique Video
Over a sterile field into the surgeon’s room, the dimensions of the thawed allograft are measured. The width is marked from the tendon to the distal edge of the bone. This measure is reassessed before it is cut. The cut must be perpendicular, as can be seen in the procedure. Then, the thickness is symmetrically drawn. A cut of 90° must be controlled. The next step is to draw the tendon thickness with the same measurement of the bone thickness. Sectioning the tendon with the scalpel yields the patient’s tendon and the remnant allograft. The remnant tendon could be used for extra-articular tenodesis in front of residual rotational instability. The surgeon should remove the excessive surrounding bone tissue until cylindrical shape is obtained. The bone end is tested into the graft-sizing block until it reaches the targeted patient’s diameter (10 mm). The allograft should pass freely through the graft-sizing block. The last part involves a bullet-shape allograft that must fit into the femoral tunnel. A Kirschner wire is located at the center of the bone end to guide the transtibial technique. Prior to the allograft fixation, the surgeon should confirm that the bone diameter has not changed by dilation. The obtained dimensions serve to define the femoral tunnel length. Finally, the femoral fixation is guided using a Kirschner wire. The adequate femoral insertion is controlled and confirmed by arthroscopy.
Introduction
The restoration of the knee biomechanics is an important concern in anterior cruciate ligament (ACL) reconstruction.1 Generally, the ACL reconstruction is a successful technique with good results between 80% and 95% of patients and 81% of athletes return to sports at 6 years mean follow-up.2,3 However, during primary and revision reconstruction surgery of ACL, several factors like tunnel-graft length mismatch, insufficient harvesting of the donor’s tendon, size graft limitations (length and diameter), wrong graft fixation, bone defects, secondary arthrofibrosis, and morbidity of the donor site, secondary neuromuscular deficits, and other factors may compromise the outcomes of the surgery.
An ideal graft needs to achieve sufficient strength, positioning, healing advantages,4 and good clinical outcomes.5 The strength of the graft mainly depends on the quality of the tissue source that involves the stiffness and deformation capacity of the selected tissue.6 Nevertheless, the final strength of the ACL reconstruction can be affected dramatically by the insufficient length and diameter of the graft7 or by a wrong positioning, which can affect the mechanical properties of the reconstruction.8 For the Achilles allograft, additional mechanical advantages are given by a bone block on one side of the graft.7 However, technical aspects can affect the Achilles allograft quality, such as block shape, bone cuts, diameter and length estimation, angulation of fixations, or erroneous fixation due to incorrect screwing during the reconstruction.9
The decision for using Achilles allograft is based upon its ease of use, its resistance, bone stock supply to fill eventual bone defects, the possibility to split the same specimen for more than one ligament reconstruction (i.e., ligament augmentation), and its good clinical outcomes. Nevertheless, to obtain the maximum potentialities, detailed knowledge on graft preparation is required. Here, we describe how to prepare the Achilles tendon allograft requirements.
Surgical Technique
A video for the Achilles allograft preparation is available (Video 1), and the technique’s recommendations are shown in Table 1.
Table 1.
Recommendations for Achilles Tendon Preparation ACL Reconstruction
|
|
|
|
|
|
|
|
|
|
|
ACL, anterior cruciate ligament.
Allograft
All grafts should be supplied by tissue banks accredited under strict policies for serologic and microbiologic tests, according to the Food and Drug Administration regulations. In our case, we use the Achilles tendon, with calcaneus bone (MTF Biologics, USA). A detailed clinical record and disease screening of donors should be added for each allograft. Blood cultures for human immunodeficiency virus, syphilis B and C, and hepatitis tests must performed on all donors. Validate tissue cleaning and disinfecting process without adversely affecting their mechanical or biological performance should be considered. Allografts may receive a low dose (b2 mRad) of radiation and should be stored within two sealed envelopes and frozen at −80°C.
Eligibility Criteria
There is not a particular restriction to use the Achilles allograft as primary reconstruction, but it has mainly been used for revision surgeries, multiligament injuries, and for patients over 40 years old.
Technique
The patients are positioned supine with flexion of hip and knee (90°) using sedation, anesthesia, and tourniquet for knee arthroscopy technique. All patients receive antibiotic prophylaxis (Cefazolin 1 g or Clindamycin 600 mg in case of known penicillin or cephalosporin allergies) 30 min before surgery and three additional doses to complete 24 hours of prophylaxis. The ACL disruption is confirmed by arthroscopy examination using conventional antero-medial and antero-lateral portals. Thereafter, not exclusively limited to a unique technique, we use the Achilles allograft under a hybrid transtibial technique.10,11 We drill the tibial tunnel 1-2 mm lower than the Achilles bone diameter, followed by enlargement to 1-2 mm using a dilator tunnel instrument (Arthrex, Inc., Naples, FL) to obtain a compacted tibial tunnel wall.12 Then, a femoral tunnel is drilled near the footprint using a guide typically 1-2 mm longer than the bone end length. The femoral tunnel had a depth enough to cover the whole bone end of the Achilles tendon allograft with the same diameter of the bone block. The ACL reconstruction is made by the senior surgeon (R.Y.).
Prior to the ACL surgery with sterile technique, the sealed envelopes of the Achilles allograft are open. The frozen allograft (MTF Biologics, Edison, NJ) is placed in 250 mL warm saline solution 0.9 % (usually 37°C to 41°C) with vancomycin 1 gram until the defrost (usually 10-15 minutes);13 see Fig 1. At this moment, a sample for common culture should be obtained for posterior clinical management. All required instruments to prepare the allograft are summarized in Fig 1.
Fig 1.

Preparation of instruments for Achilles tendon allograft. The allograft is warmed usually between 37°C and 41°C to defrost the allograft in 250 mL of 0.9 % saline solution with 1 gram vancomycin, usually for 10-15 minutes. The surgical instruments comprise an oscillating saw, graft-sizing block, sterile marker, and millimeter latex-free ruler, scalpel, scissors, and forceps.
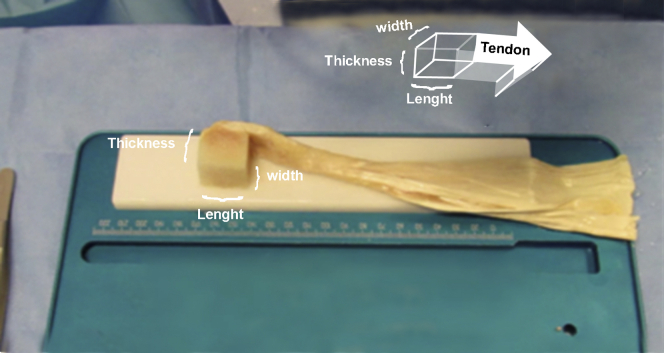
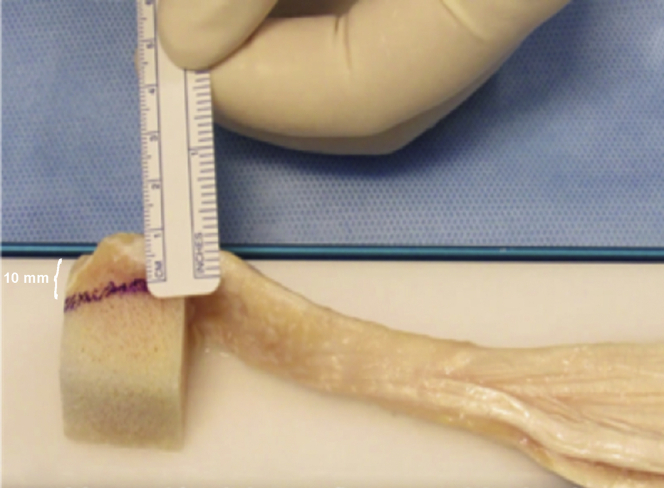
The second surgeon (H.Z.) or any other surgeon assistant can prepare the allograft (typically between 10 and 15 minutes), while the surgeon reams the tunnels. Over a sterile table, the bone end is measured by its width, length, and thickness through a latex-free millimeter ruler (Medline Industries, Inc., Waukegan, IL), see Fig 2. The bone end is marked through a sterile regular latex-free tip surgical marker (Medline Industries) from the tendon edge toward the bone block with 10 mm (Fig 3).
Fig 2.
Dimensions of the bone block. The thickness, length, and width are measured.
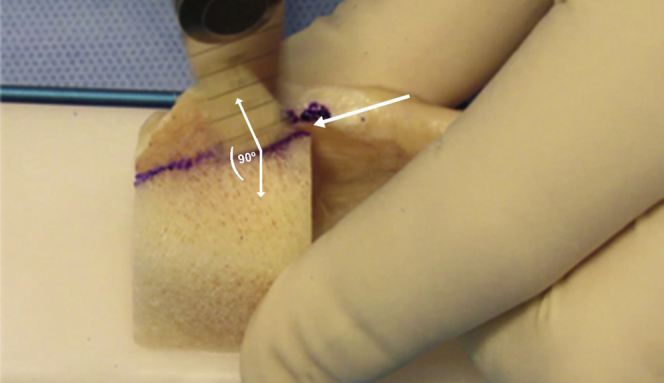
Fig 3.
The thickness measure is drawn with 10 mm across the bone end.
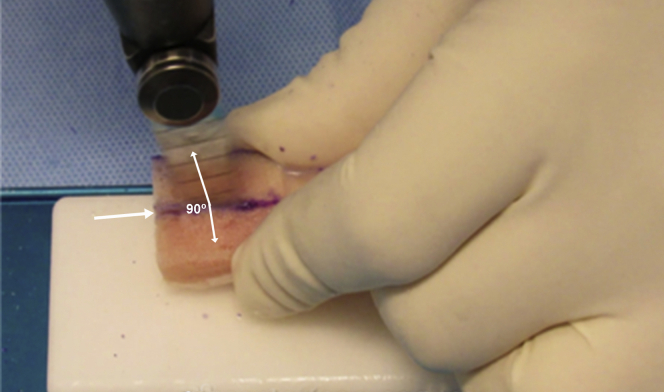
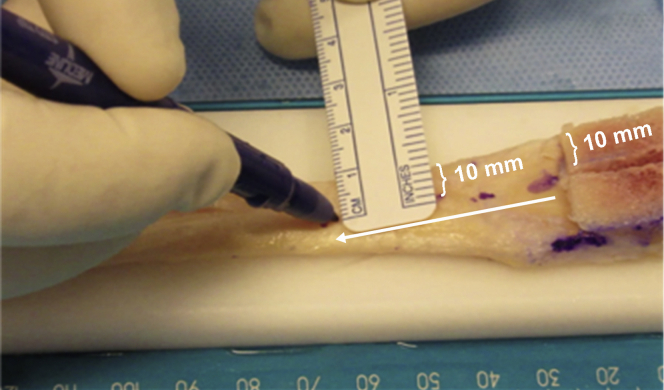
The thickness requirements are determined according to the anatomy of the patients and the femoral tunnel, but usually 10 mm and 11 mm are sufficient for both women and men,8 respectively (Fig 3). Never should diameters lower than 8 mm for both genders be used. Then, with an oscillating saw (DePuy Synthes, Raynham, MA), perpendicular to the bone block, the first cut is performed following the drawn marks (Fig 4). Immediately, to guarantee a symmetrical bone block, the same 10-mm thickness is used for marking the width of the bone block (Fig 5). Afterward, the second perpendicular cut is performed (Fig 6). At this moment, the surgeon should draw over the tendon the width (10 mm) following by a longitudinal dissection using a scalpel (Fig 7). As a result, the allograft and a remnant tendon are obtained (Fig 8). The remnant tendon might be used for augmentation procedures, according to the surgery plan.
Fig 4.
Perpendicular cut of the bone block. Note that the white arrow indicates the direction of the cut, which should be perpendicular.
Fig 5.
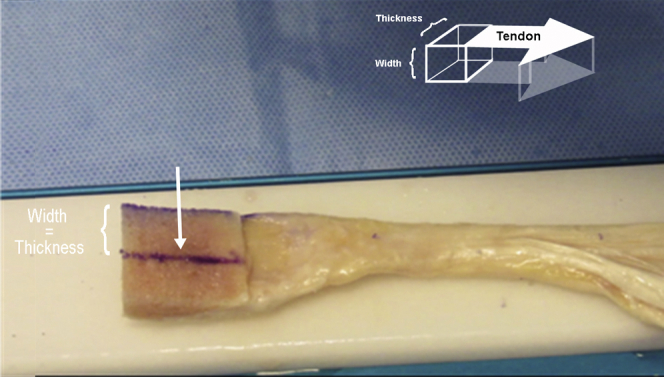
Width drawing of the bone block. Note the width and thickness have the same measurement (10 mm). The white arrow indicates the newly drawn line on the longitudinal axis of the allograft.
Fig 6.
Second cut on the bone block. Note that the cut is made perpendicular to the bone end following the drawn line (white arrow).
Fig 7.
Tendon marks for dissection. Note that the same measure drawn in the bone end should be replicated in the tendon. The white arrow indicates the direction of the marking.
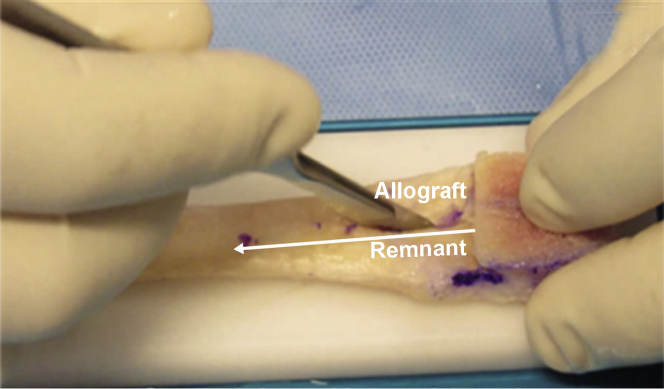
Fig 8.
Tendon dissection. A complete dissection of the tendon from bone end toward the tendon end is made with a scalpel. The white arrow indicates the direction of the dissection.
The next stage involves the cylindrical and cone shaping by bone removal to fit with the graft-sized block (Arthrex, Inc.). Follow the bone cuts a rectangular prism is obtained. However, to fit with the cylindrical femoral tunnel, the surgeon should obtain a cylindrical shape for the bone block by bone removal (Fig 9). Nonetheless, the removal of bone tissue must never achieve finger point support. However, forceps could hold the bone end as an alternative, but damage by compression should be avoided. The shaped bone is systematically tested into the graft-sizing block (Arthrex, Inc.) to obtain an appropriate diameter by removing excessive bone tissue (Fig 10). The rechecking with the graft-sizing block (Arthrex, Inc.) guides how much remnant osseous tissue is still needed to remove (Fig 11). When the cylindrical shape is reached, the allograft must pass freely through the graft-sizing block (Arthrex, Inc.), see Fig 12. At the end of this stage, the surgeon should remove around 3-5 mm with a slope angle of 60° to obtain a cone or bulleting15 shape of the distal bone block for fitting assumption with the femoral tunnel (Fig 13). As previously suggested, the removal of bone tissue never must achieve finger point support.
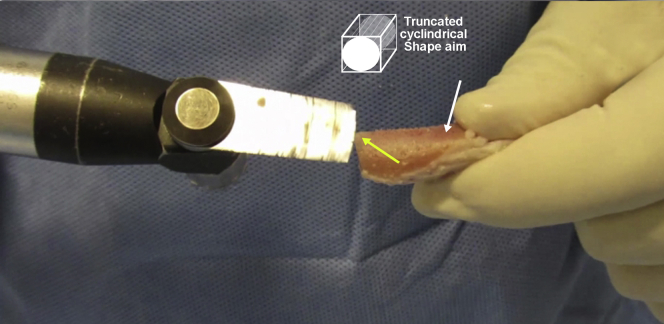
Fig 9.
Bone removal to obtain a truncated cylindrical shape. Note that the bone removal using an oscillating saw (yellow arrow) must never reach the finger point support (white arrow). As an alternative, a forceps could be used to hold the bone end, but tissue damage by compression should be avoided.
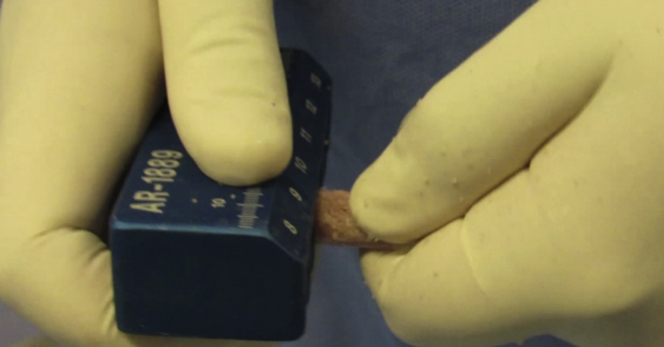
Fig 10.
Systematic testing into the graft-sizing block.
Fig 11.
Bone removal until the appropriate diameter is achieved to pass through the graft-sizing block. Note that the bone removal must never reach the finger point support. A forceps could be used as an alternative to hold the bone end, but tissue damage by compression should be avoided.
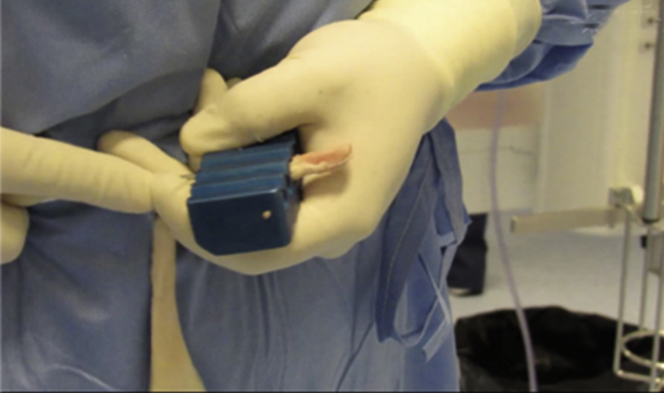
Fig 12.
Free pass through the graft-sizing block.
Fig 13.
Cone or bulleting shaping of the bone block. Note that the bone removal must never achieve the finger point support. Typically, 3-5 mm with a slope angle of 60° is removed for femoral tunnel fit. A forceps could be used as an alternative to hold the bone end, but tissue damage by compression should be avoided.
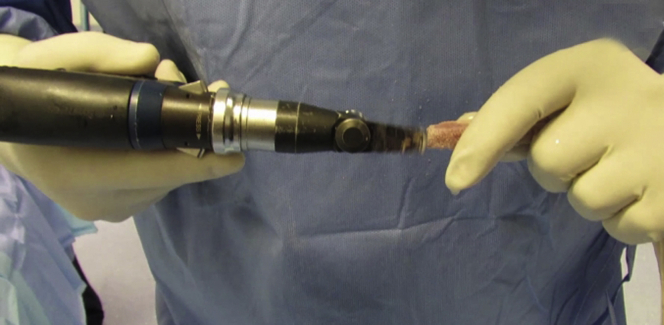
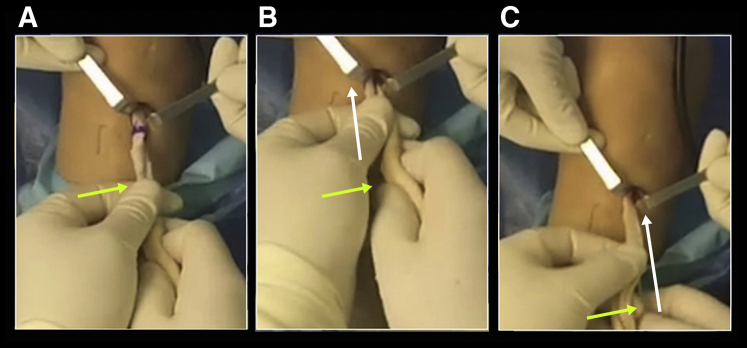
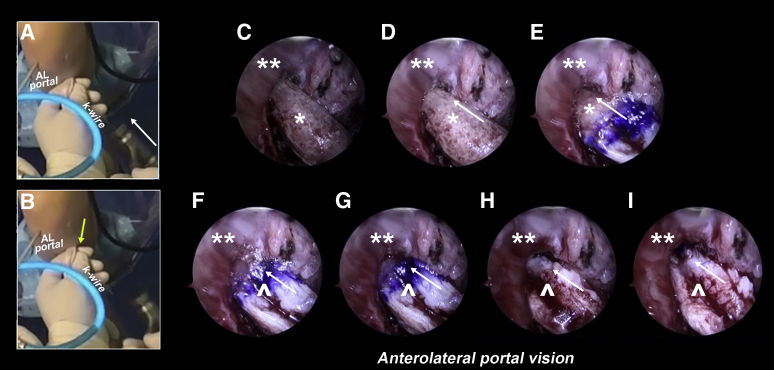
The final stage of preparation involves the bone block fit with the femoral tunnel. Here, a Kirschner wire (K-wire) of 1.6 mm is located at the center of the bone block in the longitudinal axis until 2/3 of its length to guide the transtibial technique (Fig 14). Free passage of the allograft through the graft-sizing block (Arthrex, Inc.) must be rechecked because of the possible dilation of the bone block when placing the K-wire (Fig 15). Then, the Allograft is inserted into the tunnels based on obtained dimensions (Fig 16). If necessary, soft tapings over the K-wire could be performed for better insertion (Figs 17 and 18). Finally, we fix the bone-tendon end of the graft through a metal interference screw (Arthrex, Inc.). For the tibial fixation, we use the combination of a sheath and screw for the free tendon end (AperFix II, Zimmer Biomet, Parsippany, NJ).16,17 The tendon is cut flush at the end of the tibial bone tunnel. Finally, the preparation details of the Allograft are written in the record of the patient.
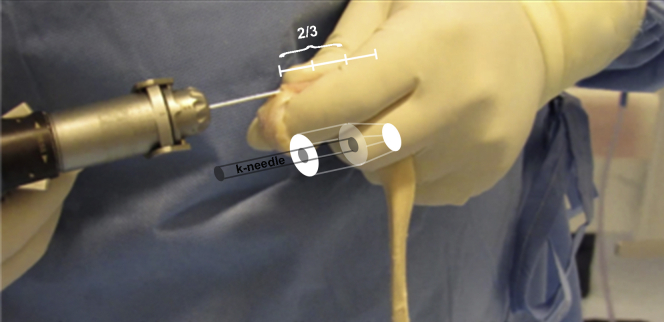
Fig 14.
Longitudinal insertion of a Kirschner wire of 1.6 mm in the bone block centered at 2/3 of its length. Note that the bone removal must never reach the finger point support. A forceps could be used as an alternative to hold the bone end, but tissue damage by compression should be avoided.
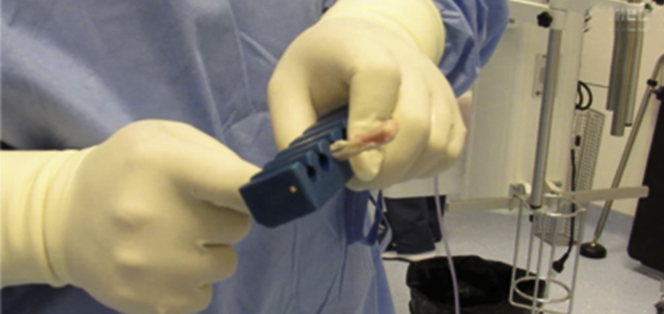
Fig 15.
Diameter testing for the bone block with Kirschner wire.
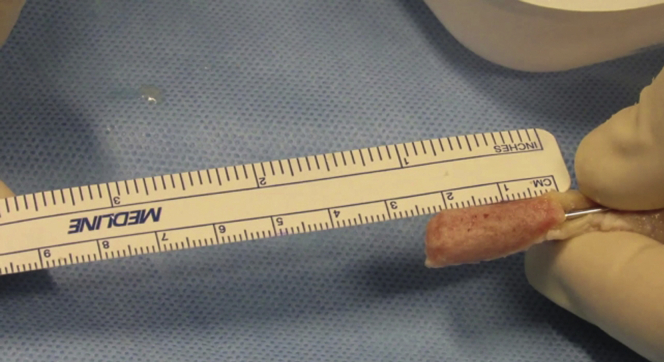
Fig 16.
Measurement and recording of the resultant bone block dimensions. Note the dimensions are used to plan the femoral tunnel dimension. Typically, 1-2 mm more length than the bone end length for the femoral tunnel is drilled.
Fig 17.
Transtibial technique for allograft using a Kirschner wire. The yellow arrow shows how the surgeon guides the bone end fit, and the white arrow shows the direction of the movement made by the surgeon. (A-C) Progressive insertion of the Achilles allograft.
Fig 18.
Allograft fitting in the femoral tunnel using a Kirschner wire. (A and B) Small tapings on the Kirschner wire for complete insertion of the bone end into the femoral tunnel. (C-I) Progressive fitting of the bone end from the antero-lateral portal vision. Note that the white arrow shows the fitting direction, and the yellow arrow shows how the surgeon can use the Kirschner wire for better guiding of the Allograft. ∗∗ denotes the femoral wall; ∗ denotes the prepared bone end of the Allograft; ˆ denotes the tendon tissue of the allograft with a Kirschner wire.
Discussion
The graft preparation whether it is autograft or allograft has not received wide attention. Unfortunately, inadequate allograft preparation may affect the restoration of the knee biomechanics despite the important Achilles Allograft resistance.18, 19, 20, 21 The critical problems during the preparation relate to mismatched dimensions; incorrect thawed, prophylaxis; bone marks and cuts; excessive bone removal; fracture of the bone block by dilation; or allograft contamination. However, support for the important use advantages of the Achilles allograft is given in Table 2, advantages that include a standardized preparation (Table 1) that helps provide adequate dimension of the allograft,4 easy manipulation in the operative room, fast procedure, nonmorbidity by the donor site, high strength, healing advantages, multiple-ligament reconstruction capacity, potential to fill bone defects,14 a high rate of a successful return to sports,3 and diminished chance of graft tunnel mismatch.
Table 2.
Advantages and Limitations of the Technique
| Advantages |
| Standardizing technique permits obtain the maximum potentialities of the graft Easy adaptation for the ACL reconstruction patient’s requirements (diameter) Easy to size Predictable size of the bone block previous to surgery No tunnel and graft length mismatch Decreasing surgical time28 No donor site morbidity28 Graft length allows direct traction over the tendon during the insertion of the tibial implant Fixation without needing sutures or traction. Anatomical fixation by bone-to-bone at the femoral insertion (healing advantages) Multiple-ligament reconstruction14 The bone block allows filling bone defects (mainly revision cases)14 Avoid a two-stage ACL revision Allows free tendon fixation in case of bone block loss No lower clinical differences in ACL reconstructions compared with other allografts29,30 High rate of successful sport returns up to 81% of athletes at 6 years mean follow-up3 Allows primary and revision surgery High tensile resistance of the allograft19 |
| Limitations |
| Disease transmission, i.e., the immunodeficiency virus reported 1 case of 1.6 million cases (a small risk)23 Slower time for graft integration like any bone-to-bone healing24 In some centers, it could be an expensive procedure Fracture of the bone block by dilation |
ACL, anterior cruciate ligament.
This Technical Note has described how to prepare the Achilles tendon allograft, especially how to control the dimensions of the graft, the techniques necessary to fit the bone block with the tunnels, and how to improve the tunnels’ passages. These assumptions facilitate the fixation of the bone block, and the use of the K-wire facilitates the guide of the allograft fit into the femoral tunnel. Also, perforations on the bone block could be performed to pass sutures and pull out, if needed. In addition, the possibility of performing a multiligament reconstruction, such as collateral ligament augmentation to improve valgus instability or extra-articular tenodesis to improve a rotational instability after ACL rupture gives additional advantages.1,22
The Achilles allograft is not out of limitations (Table 2). The disease transmission may be the most important limitation. However, a low risk of transmission has been reported as one case of 1.6 million cases for immunodeficiency virus.23 A completed record of the donor from approved tissue banks (accredited under strict policies for serologic and microbiologic tests regulations) and extended screening permits diminish this risk. The other relevant limitation involves the bone time integration.24 In our center, variation in signal intensity signs for bone integration between 3 and 5 months in T2-enhanced magnetic resonance is assessed25 to diminish the risk of rerupture because patients have a quicker postoperative rehabilitation, which may lead to an incorrect decision to return to a sport before sufficient biological healing.26 The literature especially shows early rerupture of allograft for young athletes.26 Hence, we focus on patient education and clinical follow-up during the rehabilitation for good management of the operated ACL with Achilles allograft,27 using physical therapy and biomechanics services.
In conclusion, a standardized and appropriate Allograft preparation allows improved ACL reconstruction capable of controlling the length, width, bone removal, filling defects, multiligament reconstruction, and better tunnel location through a k-wire guide.
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Institution Social Medias:
@clinicameds (Instagram)
@medschile (Facebook)
@clinicaMEDS (Twitter)
Author social medias:
@drhectorzamorano (Instagram)
@dr.gaston.caracciolo (Instagram)
@ drfjvergara (Instagram)
@totiyanezrojo (Instagram)
@sebaa_valdes (Instagram)
Carlos-De-La-Fuente-3 (Researchgate)
Supplementary Data
Over a sterile field into the surgeon’s room, the dimensions of the thawed allograft are measured. The width is marked from the tendon to the distal edge of the bone. This measure is reassessed before it is cut. The cut must be perpendicular, as can be seen in the procedure. Then, the thickness is symmetrically drawn. A cut of 90° must be controlled. The next step is to draw the tendon thickness with the same measurement of the bone thickness. Sectioning the tendon with the scalpel yields the patient’s tendon and the remnant allograft. The remnant tendon could be used for extra-articular tenodesis in front of residual rotational instability. The surgeon should remove the excessive surrounding bone tissue until cylindrical shape is obtained. The bone end is tested into the graft-sizing block until it reaches the targeted patient’s diameter (10 mm). The allograft should pass freely through the graft-sizing block. The last part involves a bullet-shape allograft that must fit into the femoral tunnel. A Kirschner wire is located at the center of the bone end to guide the transtibial technique. Prior to the allograft fixation, the surgeon should confirm that the bone diameter has not changed by dilation. The obtained dimensions serve to define the femoral tunnel length. Finally, the femoral fixation is guided using a Kirschner wire. The adequate femoral insertion is controlled and confirmed by arthroscopy.
References
- 1.Abusleme S., Strömbäck L., Caracciolo G., et al. Lateral extra-articular tenodesis: A technique With an iliotibial band strand without implants. Arthroscopy Techniques. 2021;10:e85–e89. doi: 10.1016/j.eats.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bach B.R., Aadalen K.J., Dennis M.G., et al. Primary anterior cruciate ligament reconstruction using fresh-frozen, nonirradiated patellar tendon allograft: minimum 2-year follow-up. Am J Sports Med. 2005;33:284–292. doi: 10.1177/0363546504267347. [DOI] [PubMed] [Google Scholar]
- 3.Zaffagnini S., Grassi A., Marcheggiani Muccioli G.M., et al. Anterior cruciate ligament revision with Achilles tendon allograft in young athletes. Orthop Traumatol Surg Res. 2018;104:209–215. doi: 10.1016/j.otsr.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Gasser S., Uppal R. Anterior cruciate ligament reconstruction: a new technique for Achilles tendon allograft preparation. Arthroscopy. 2006;22:1365.e1-e3. doi: 10.1016/j.arthro.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 5.Poehling G.G., Curl W.W., Lee C.A., et al. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: Allograft versus autograft. Arthroscopy. 2005;21:774–785. doi: 10.1016/j.arthro.2005.04.112. [DOI] [PubMed] [Google Scholar]
- 6.la Fuente C.D., Cruz-Montecinos C., Schimidt H.L., Henríquez H., Ruidiaz S., Carpes F.P. Biomechanical properties of different techniques used in vitro for suturing mid-substance Achilles tendon ruptures. Clin Biomech (Bristol, Avon) 2017;50:78–83. doi: 10.1016/j.clinbiomech.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Kang S.H., Sohn K.M., Lee D.K., Lee B.H., Yang S.W., Wang J.H. Arthroscopic posterior cruciate ligament reconstruction: The Achilles tendon allograft versus the quadriceps tendon allograft. J Knee Surg. 2020;33:553–559. doi: 10.1055/s-0039-1681029. [DOI] [PubMed] [Google Scholar]
- 8.Samitier G., Marcano A.I., Alentorn-Geli E., Cugat R., Farmer K.W., Moser M.W. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015;3:220–240. [PMC free article] [PubMed] [Google Scholar]
- 9.Colvin A.C., Shen W., Musahl V., Fu F.H. Avoiding pitfalls in anatomic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:956–963. doi: 10.1007/s00167-009-0804-2. [DOI] [PubMed] [Google Scholar]
- 10.Trofa D.P., Saltzman B.M., Corpus K.T., Connor P.M., Fleischli J.E., Piasecki D.P. A hybrid transtibial technique combines the advantages of anteromedial portal and transtibial approaches: A prospective randomized controlled trial. Am J Sports Med. 2020;48:3200–3207. doi: 10.1177/0363546520956645. [DOI] [PubMed] [Google Scholar]
- 11.Jennings J.K., Leas D.P., Fleischli J.E., D’Alessandro D.F., Peindl R.D., Piasecki D.P. Transtibial versus anteromedial portal ACL reconstruction: Is a hybrid approach the best? Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117719857. 2325967117719857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gokce A., Beyzadeoglu T., Ozyer F., Bekler H., Erdogan F. Does bone impaction technique reduce tunnel enlargement in ACL reconstruction? Int Orthop. 2009;33:407–412. doi: 10.1007/s00264-007-0496-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lamplot J.D., Liu J.N., Hutchinson I.D., et al. Effect of vancomycin soaking on anterior cruciate ligament graft biomechanics. Arthroscopy. 2021;37:953–960. doi: 10.1016/j.arthro.2020.10.040. [DOI] [PubMed] [Google Scholar]
- 14.Maestro Fernández A., Pipa Muñiz I., Rodríguez García N. Two-stage anterior cruciate ligament reconstruction revision surgery for severe bone defects with anterolateral ligament reconstruction technique. Arthrosc Tech. 2020;9:e327–e337. doi: 10.1016/j.eats.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fanelli G.C., Larson R.V. Practical management of posterolateral instability of the knee. Arthroscopy. 2002;18(2 Suppl 1):1–8. doi: 10.1053/jars.2002.31779. [DOI] [PubMed] [Google Scholar]
- 16.Fu F.H., Bennett C.H., Lattermann C., Ma C.B. Current trends in anterior cruciate ligament reconstruction. Part 1: Biology and biomechanics of reconstruction. Am J Sports Med. 1999;27:821–830. doi: 10.1177/03635465990270062501. [DOI] [PubMed] [Google Scholar]
- 17.Aga C., Rasmussen M.T., Smith S.D., et al. Biomechanical comparison of interference screws and combination screw and sheath devices for soft tissue anterior cruciate ligament reconstruction on the tibial side. Am J Sports Med. 2013;41:841–848. doi: 10.1177/0363546512474968. [DOI] [PubMed] [Google Scholar]
- 18.Akpinar B., Baron S., Alaia M.J., Jazrawi L.M. Clinical and biomechanical outcomes following knee extensor mechanism reconstruction. Arthrosc Sports Med Rehabil. 2020;2:e553–e561. doi: 10.1016/j.asmr.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levitt R.L., Malinin T., Posada A., Michalow A. Reconstruction of anterior cruciate ligaments with bone-patellar tendon-bone and achilles tendon allografts. Clin Orthop Relat Res. 1994;303:67–78. [PubMed] [Google Scholar]
- 20.Kunze K.N., Burnett R.A., Shinsako K.K., Bush-Joseph C.A., Cole B.J., Chahla J. Trapezoidal Achilles tendon allograft plug for revision quadriceps tendon repair with a large tendon defect. Arthrosc Tech. 2019;8:e1031–e1036. doi: 10.1016/j.eats.2019.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paez C.J., Rebolledo B.J. Suture anchor repair with V-Y plasty and Achilles allograft augmentation for chronic quadriceps tendon injury. Arthrosc Tech. 2020;9:e1033–e1038. doi: 10.1016/j.eats.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hurley E.T., Manjunath A.K., Strauss E.J., Jazrawi L.M., Alaia M.J. Return to play after anterior cruciate ligament reconstruction with extra-articular augmentation: A systematic review. Arthroscopy. 2021;37:381–387. doi: 10.1016/j.arthro.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Buck B.E., Malinin T.I., Brown M.D. Bone transplantation and human immunodeficiency virus. An estimate of risk of acquired immunodeficiency syndrome (AIDS) Clin Orthop Relat Res. 1989;(240):129–136. [PubMed] [Google Scholar]
- 24.Scheffler S.U., Schmidt T., Gangéy I., Dustmann M., Unterhauser F., Weiler A. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy. 2008;24:448–458. doi: 10.1016/j.arthro.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 25.Araujo P., van Eck C.F., Torabi M., Fu F.H. How to optimize the use of MRI in anatomic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1495–1501. doi: 10.1007/s00167-012-2153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaeding C.C., Aros B., Pedroza A., et al. Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verma N.N., Beletsky A., Lu Y., et al. Time to achievement of clinically significant outcomes in anterior cruciate ligament reconstruction. Arthroscopy. 2021;37:e29–e30. doi: 10.1016/j.arthro.2020.12.059. [DOI] [Google Scholar]
- 28.Chehab E.L., Flik K.R., Vidal A.F., et al. Anterior cruciate ligament reconstruction using achilles tendon allograft: an assessment of outcome for patients age 30 years and older. HSS J. 2011;7:44–51. doi: 10.1007/s11420-010-9183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim S.-J., Bae J.-H., Lim H. Comparison of Achilles and tibialis anterior tendon allografts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:135–141. doi: 10.1007/s00167-012-2334-6. [DOI] [PubMed] [Google Scholar]
- 30.West R.V., Harner C.D. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197–207. doi: 10.5435/00124635-200505000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Over a sterile field into the surgeon’s room, the dimensions of the thawed allograft are measured. The width is marked from the tendon to the distal edge of the bone. This measure is reassessed before it is cut. The cut must be perpendicular, as can be seen in the procedure. Then, the thickness is symmetrically drawn. A cut of 90° must be controlled. The next step is to draw the tendon thickness with the same measurement of the bone thickness. Sectioning the tendon with the scalpel yields the patient’s tendon and the remnant allograft. The remnant tendon could be used for extra-articular tenodesis in front of residual rotational instability. The surgeon should remove the excessive surrounding bone tissue until cylindrical shape is obtained. The bone end is tested into the graft-sizing block until it reaches the targeted patient’s diameter (10 mm). The allograft should pass freely through the graft-sizing block. The last part involves a bullet-shape allograft that must fit into the femoral tunnel. A Kirschner wire is located at the center of the bone end to guide the transtibial technique. Prior to the allograft fixation, the surgeon should confirm that the bone diameter has not changed by dilation. The obtained dimensions serve to define the femoral tunnel length. Finally, the femoral fixation is guided using a Kirschner wire. The adequate femoral insertion is controlled and confirmed by arthroscopy.
Over a sterile field into the surgeon’s room, the dimensions of the thawed allograft are measured. The width is marked from the tendon to the distal edge of the bone. This measure is reassessed before it is cut. The cut must be perpendicular, as can be seen in the procedure. Then, the thickness is symmetrically drawn. A cut of 90° must be controlled. The next step is to draw the tendon thickness with the same measurement of the bone thickness. Sectioning the tendon with the scalpel yields the patient’s tendon and the remnant allograft. The remnant tendon could be used for extra-articular tenodesis in front of residual rotational instability. The surgeon should remove the excessive surrounding bone tissue until cylindrical shape is obtained. The bone end is tested into the graft-sizing block until it reaches the targeted patient’s diameter (10 mm). The allograft should pass freely through the graft-sizing block. The last part involves a bullet-shape allograft that must fit into the femoral tunnel. A Kirschner wire is located at the center of the bone end to guide the transtibial technique. Prior to the allograft fixation, the surgeon should confirm that the bone diameter has not changed by dilation. The obtained dimensions serve to define the femoral tunnel length. Finally, the femoral fixation is guided using a Kirschner wire. The adequate femoral insertion is controlled and confirmed by arthroscopy.