Abstract
Behavioural interventions can support the adoption of healthier lifestyles and improve physical health outcomes, but it is unclear what factors might drive success of such interventions in people with serious mental illness (SMI). We systematically identified and reviewed evidence of the association between determinants of physical health self-management behaviours in adults with SMI. Data about American Association of Diabetes Educator's Self-Care Behaviours (AADE-7) were mapped against the novel Mechanisms of Action (MoA) framework. Twenty-eight studies were included in the review, reporting evidence on 104 determinant-behaviour links. Beliefs about capabilities and beliefs about consequences were the most important determinants of behaviour, especially for being physically active and healthy eating. There was some evidence that emotion and environmental context and resources played a role in determining reducing risks, being active, and taking medications. We found very limited evidence associated with problem solving, and no study assessed links between MoAs and healthy coping. Although the review predominantly identified evidence about associations from cross-sectional studies that lacked validated and objective measures of self-management behaviours, these findings can facilitate the identification of behaviour change techniques with hypothesised links to determinants to support self-management in people with SMI.
Systematic Review Registration: PROSPERO, registration CRD42018099553.
Keywords: self-management, behaviour change, serious mental illness, determinant, theory
Introduction
Adults with serious mental illness (SMI), such as schizophrenia or bipolar disorder, experience considerable inequalities in health outcomes compared with the general adult population. Life expectancy for individuals with SMI is 10–20 years shorter and the mortality rate 3.7 times higher than in the general population (1–4). Furthermore, this mortality gap is widening (5). It is estimated that two thirds of these deaths are attributable to preventable long-term physical conditions such as cardiovascular disease, respiratory disease, diabetes and hypertension (1, 6). There is at least a 2-fold greater prevalence of obesity, diabetes, and cardiovascular disease in adults with SMI compared with the general adult population (6–8).
Supported self-management is critical to prevention and improving outcomes of long-term physical conditions and there is robust evidence that behavioural interventions can effectively support people in the general population to self-manage their health (9). Self-management refers to activities undertaken by individuals, typically to mitigate the effects of a long-term condition and maximise quality of life. Self-management of physical health comprises a range of health behaviours that include diet, physical activity, smoking abstinence, self-monitoring, and seeking appropriate professional help.
The evidence for behavioural interventions to support self-management in people with SMI is limited. There is some evidence that prescribed and directly administered exercise interventions that include up to 90 min a week of moderate-to-vigorous exercise can improve physical fitness and cardiometabolic risk as well as reduce psychiatric symptoms in people with schizophrenia (10). However, there is limited evidence that behavioural interventions positively affect physical activity in people with SMI. Findings from a systematic review of 32 studies of behavioural interventions to promote physical activity and reduce sedentary behaviours in people with schizophrenia were inconsistent and based on low quality evidence from controlled and uncontrolled trials (11). The evidence that behavioural approaches that include lifestyle interventions to support dietary change and physical activity to reduce weight in people with SMI is similarly equivocal. Naslund et al. reported small but significant treatment effects across 17 experimental and quasi-experimental studies of lifestyle weight loss interventions in overweight and obese people with SMI (12). However, findings from a Danish trial that tested an intensive lifestyle coaching intervention plus care coordination for people with schizophrenia-spectrum disorder and obesity which failed to show any positive results for 10-year cardiovascular risk factors or weight reduction (13). Efforts to target multiple cardiovascular risk factors using manualised and supported behavioural interventions in people with SMI have also proven ineffective (14). The STEPWISE trial tested the effectiveness of a group-based intervention, with 1:1 fortnightly telephone support, to identify and encourage ways to achieve dietary and physical activity goals in people with schizophrenia. The intervention was based on self-regulation and self-efficacy theories and a relapse prevention model, and was co-designed in partnership with people with lived experience of SMI, mental health professionals and behaviour change experts. However, weight reduction did not differ between intervention and control groups, and other key indicators of self-management, such as physical activity, remained unchanged (15).
Living with SMI may pose significant barriers to engaging in self-management of physical health. Individuals with SMI spend less time being physically active (16), are less likely to eat a healthy diet (17), and more likely to smoke than other people (18). There are a number of potential reasons for this, including how psychiatric symptoms can inhibit self-management behaviours. People with SMI experience deficits that are commonly referred to as negative symptoms; these include avolition, psychomotor retardation, blunted affect, alogia and anhedonia (19). People with SMI also experience positive symptoms of psychosis, including delusions and hallucinations. Negative symptoms have been shown to predict poorer cardiorespiratory fitness, larger waist circumference, higher HbA1c, and lower high-density lipoprotein in overweight people with schizophrenia (20). Both negative and positive symptoms can influence a person's ability to engage in health behaviours, either by directly impacting their motivation and their ability to understand the importance of these behaviours, or through triggering the use of unhealthy behaviours to cope with symptomatic episodes (21). The presence of psychiatric symptoms has been shown to overshadow diabetes self-management in people with SMI (22). Additionally, antipsychotic medications are commonly used to manage psychosis and are associated with increased risk of obesity, excessive weight gain and metabolic derangement (23, 24). Antipsychotics can also make self-management more difficult through unwanted side-effects, such as increased appetite and sedation (25, 26).
Over and above individual level factors, social and community level factors also underscore health inequalities experienced by people with SMI. People with SMI are more likely to experience higher levels of deprivation than the general population (27) and SMI increases the odds of living in poverty (28). Indeed, inequalities in mental health outcomes can in part be explained by neighbourhood and area of residence (29) and recent spatial analyses at small area level across England has shown higher prevalence of SMI in socially fragmented and socially deprived areas (30).
Intervention Development Methods and Theoretical Framework
To maximise the chance that behavioural interventions to support physical health self-management in people with SMI are effective and sustainable, an approach that draws on the science of behaviour change is needed. Intervention development in such an approach proceeds by the description of behavioural targets that drive risk factors, identification of mechanisms of action through which behaviour change might occur, followed by the identification of specific techniques that might alter the target, and the formulation of process measures that can measure the extent to which the intervention was successful (31). Our approach draws on a phased based approach underpinned by the Medical research Council Framework for developing and evaluating complex interventions (32). In the context of the science of behaviour change our work methodologically maps to the Behaviour Change Wheel (33) and the Obesity-Related Behavioural Interventions Trials or ORBIT model (34). These approaches within the science of behaviour change are well-suited to an emphasis on the early phases of intervention development, starting with the identification of hypothesised pathways that might mediate behaviour change and a clinical outcome, and the refinement and preliminary testing of an intervention in readiness for definitive phase III testing.
In order to design appropriate and effective supported physical health self-management interventions for people with SMI, it is essential to first identify modifiable determinants of behaviour change in this population. There is currently effort underway to develop ontologies as a means of building toward unifying different health psychological theories that speak to the range of influences upon behaviour (35). Contributing toward this, behavioural science has developed methods to systematically describe potentially active intervention components to support development, implementation, and evaluation of interventions (36). To facilitate intervention development, there is a need to identify and map evidence about the relationship between determinants and behaviours in a way that can guide the selection of appropriate intervention components. Interventions that address modifiable determinants might be more effective in changing behaviour. The Theoretical Domains Framework (TDF) contains 14 domains based on an integration of behavioural theories that relate to individual processes and characteristics of the physical and social environment that may act as determinants of (health) behaviour (37). The framework is itself an elaboration of the Capability—Opportunity—Motivation—Behaviour (COM-B) model that underpins the widely used Behaviour Change Wheel intervention development framework (33). Capability relates to a person's psychological and physical capacity to undertake a behaviour, including know-how and skills to do so. Opportunity concerns all the available social and physical factors within a person's environment that make the behaviour possible, while Motivation is specified as both reflective processes associated with planning and automatic processes associated with emotional responses, reactions, and impulses. The COM-B model proposes that capability and opportunity can influence motivation, to bring about behaviour through both direct and indirect paths. There is emerging evidence that COM-B outperforms other more established models of behaviour such as the theory of planned behaviour, theory of reasoned action, and the health belief model, in explaining the variance in delivery of opportunistic behaviour change interventions and the variance in time spent delivering interventions (38). Because the COM-B model forms the hub of the behaviour change wheel it can be used to identify potentially relevant intervention functions that could be deployed to target determinants of behaviours.
More recently, Michie et al. have combined the TDF components with 12 other mechanisms which did not overlap with the TDF and were identified in a literature review of 83 behaviour change theories. This process resulted in 26 Mechanisms of Action (MoAs) with expert rated links to 56 frequently used behaviour change techniques (39, 40). The findings from the literature review and expert consensus exercise were then triangulated to systematically produce evidence of 92 hypothesised behaviour change techniques (BCT)-MoA links with the potential to be targeted by interventions, along with evidence about where links do not exist or are inconclusive (41). This evidence has been distilled into an online tool known as the Theory and Techniques Tool which offers a comprehensive and efficient system to identify intervention techniques that are purported to operate through theoretically informed MoAs (41). Given the multiple theories that offer frameworks with which to identify processes by which behaviour change interventions operate (42), synthesis of theoretical approaches is required to avoid narrowing the available evidence (43). We applied the MoA framework to integrate evidence that spans a variation in populations, context, and behaviour (44). To be useful as an evidence synthesis tool for intervention development, it is necessary that that any theoretical framework or theory for identifying mechanisms of action also provides a taxonomy of behaviour change intervention techniques with which to support integration of evidence for both the mechanisms and the technique that targeted it. With a view to informing the identification and potential adaptation of behaviour change interventions to support self-management of physical health in people with SMI, we therefore aimed to systematically review the literature to identify the MoAs that determine self-management behaviours in adults with SMI, including those who have co-morbid long-term physical health conditions.
Methods
Protocol and Registration
This systematic review forms the first phase of work of the DIAMONDS research programme that is dedicated to developing, piloting, and then definitively testing a supported self-management intervention based on evidence based behaviour change techniques for people with SMI and diabetes (45). Our review maps to Phase 1a of the ORBIT model for developing behavioural interventions. The protocol was prospectively registered with PROSPERO, registration CRD42018099553. Amendments to the protocol are summarised in Table 1. The review addressed two questions:
Table 1.
Amendments to protocol.
| Section | Original protocol | Revised protocol | Rationale |
|---|---|---|---|
| Review question | What are the determinants of self-management in adults with SMI? | What are the determinants of physical health self-management in adults with SMI? | The number of included studies exceeded expectations and physical health self-management was prioritised to address the SMI mortality gap |
| Inclusion criteria | Inclusion of qualitative study designs | Inclusion of quantitative research only | Included studies were grouped by quantitative/qualitative design and a separate synthesis of qualitative evidence undertaken for pragmatic reasons, i.e., to ensure the work was feasible according to available resources |
| Inclusion criteria | Exclusion of non-English language reports | No exclusions on language | To maximise retrieval of all relevant studies and utilise local translation services |
| Inclusion criteria | No restrictions on setting | Exclusion of studies of inpatients | The inpatient setting is likely to involve different determinants of self-management |
| Quality appraisal | Assessment of study quality using a framework developed for mixed methods reviews | Use of the NICE quality appraisal checklist for quantitative studies reporting correlations and associations | Use of a tool appropriate for the design of included studies |
| Data extraction | Extraction of a random 20% sample of data independently by a second reviewer to identify any discrepancies | A second reviewer extracted data independently from 4 studies which was checked by the first reviewer to identify any discrepancies | To make use of data that had already been extracted from studies of individuals with a long term physical condition that were prioritised to inform the intervention to be developed as part of the wider project |
| Data synthesis | Synthesis of determinates of self-management using the Capabilities, Opportunities, Motivations and Behaviours (COM-B) system | Synthesis of determinates of self-management using the Mechanisms of Action (MoAs) framework | The Theory and Techniques tool was published since the review protocol and provides evidence-based links between the MoAs and behaviour change techniques, therefore the MoAs were deemed more useful than the COM-B in informing intervention content |
What are the determinants of self-management behaviours that underpin physical health in adults with SMI?
How do these determinants differ for people with SMI who have co-morbid long-term physical health conditions?
Eligibility Criteria
Studies were eligible if they reported determinants of self-management of physical health in adults with SMI. In this review physical health relates to a dynamic state related to a person's ability to self-manage and restore functional capacity and well-being (46). Determinants of self-management were first identified using the COM-B model (capability, opportunity, motivation, and behaviour) (33). Self-management behaviours were defined as “all the actions undertaken by people to recognise, treat and manage their own healthcare independently of or in partnership with the healthcare system” and were drawn from the American Association of Diabetes Educator's self-care behaviours (AADE-7) (47). We used the AADE-7 framework because it is an evidence-based model to promote self-management behaviours that underpin good physical health in people with diabetes and other long-term conditions (48). We did not exclude studies that reported behaviours associated with healthcare utilisation but where this was the focus of a study we mapped the behaviour against the most proximate AADE-7 behaviour. Studies that exclusively assessed adherence to psychotropic medication in people with SMI were not included as this topic has previously been reviewed (49). SMI was defined as a diagnosis of schizophrenia, affective disorders (psychotic), bipolar disorder, paranoid disorders, or psychosis (ICD codes F20–29, F30–31, F32.3, or F33.3).
In keeping with previous systematic reviews where populations with mixed diagnoses and age groups might be identified (50) we excluded studies if >70% of participants were aged over 18 years, >70% had SMI, or if the reporting of participant diagnoses was insufficient to determine eligibility. Studies with a control group of people without SMI that separately reported data from an eligible group of those with SMI were included. We included evidence from groups with or without diagnoses of long-term physical illness, with a focus on community settings. Studies of inpatient populations were excluded because they are likely to experience different determinants of self-management from individuals living in the community. Case studies, case series, conference abstracts, and dissertations were all excluded. Studies that reported on reduction or cessation of tobacco, alcohol or illicit substance use were eligible; studies that reported only on initiation or general consumption of tobacco, alcohol or illicit substances were excluded.
Because we wanted to use the findings from this systematic review to inform the development of behaviour change interventions for people with SMI and diabetes in a high-income health service context we restricted studies to those reported in English and conducted in high income countries according to 2018 OECD Country Classifications (51). There were no restrictions by date. Studies of any quantitative or mixed methods design were eligible; however experimental intervention studies were excluded because we were interested in determinants of behaviour in a naturalistic context.
Information Sources
We searched the following databases:
CINAHL (EBSCO) 1981- 25/07/2018
Conference Proceedings Citation Index- Science (Clarivate Analytics Web of Science) 1990 - 25/07/2018
Evidence Search (NICE), all available years - 25/07/2018
HMIC Health Management Information Consortium (Ovid) 1983 - 25/07/2018
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily 1946 to August 26, 2020
PsycINFO (Ovid) 1806 to August Week 3 2020
We also checked relevant systematic reviews identified in the search for additional eligible primary studies.
Search
All databases were searched on 25th July 2018. Update searches were conducted on 21st November 2019 and 27th August 2020 in the two databases that generated the most eligible studies in the original searches (MEDLINE and PsycINFO). A comprehensive search was designed using textwords, synonyms and indexing-terms. The searches were peer-reviewed by a second information specialist. An example search strategy for Ovid MEDLINE is shown in Table 2. A Medline search strategy is available as an online Supplementary Material.
Table 2.
Ovid medline search strategy.
| Database: Ovid MEDLINE(R) <1946 to July Week 2 2018> |
|---|
| 1 (bipolar adj (disorder* or disease* or illness*)).tw,kf. (21737) |
| 2 exp schizophrenia/ (97897) |
| 3 Affective disorders, psychotic/ (2204) |
| 4 Bipolar disorder/ (37267) |
| 5 paranoid disorders/ (3973) |
| 6 exp psychotic disorders/ (48180) |
| 7 schizo*.tw,kf. (119094) |
| 8 (mani* adj3 depress*).tw,kf. (8267) |
| 9 (psychotic* adj3 depress*).tw,kf. (2369) |
| 10 (severe* adj3 affective*).tw,kf. (207) |
| 11 (severe* adj3 mental*).tw,kf. (9026) |
| 12 (severe* adj3 depress*).tw,kf. (8801) |
| 13 (psychos#s adj3 depress*).tw,kf. (3368) |
| 14 (serious* adj3 affective*).tw,kf. (39) |
| 15 “serious mood*”.tw,kf. (24) |
| 16 (serious* adj3 mental*).tw,kf. (3957) |
| 17 (serious* adj3 depress*).tw,kf. (616) |
| 18 or/1-17 [Serious Mental Illness] (223362) |
| 19 self care/ (30488) |
| 20 self administration/ (10593) |
| 21 Self Medication/ (4458) |
| 22 Self Efficacy/ (17300) |
| 23 Self-Management/ (556) |
| 24 Self help groups/ (8641) |
| 25 blood glucose self-monitoring/ (5606) |
| 26 (self adj2 (efficac* or help or care* or cure* or manage* or directed or monitor* or medicat* or treat* or inject* or remed*)).tw,kf. (65658) |
| 27 (selfefficac* or selfhelp or selfcare or selfcure* or selfmanage* or selfdirected or selfmonitor* or selfmedicat* or selftreat* or selfinject* or selfremed*).tw,kf. (185) |
| 28 (self administ* not (self administ* adj2 (interview? or survey? or questionnaire?))).tw,kf. (15986) |
| 29 or/19-28 [Self Management only terms] (119143) |
| 30 life style/ or exp healthy lifestyle/ or life change events/ or sedentary lifestyle/ (81876) |
| 31 exp Diet Therapy/ or exp Diet/ or exp Food/ or exp Feeding Behavior/ (1407344) |
| 32 exp Exercise/ (167064) |
| 33 smoking cessation/ or smoking reduction/ (25689) |
| 34 Alcohol Abstinence/ (457) |
| 35 *health promotion/ or *healthy people programs/ or *weight reduction programs/ (45563) |
| 36 ((behavio?r or lifestyle or “life style” or habit?) adj2 (chang* or improv* or modif*)).tw,kf. (41849) |
| 37 ((diet* or eating) adj2 (healthy or improv*)).tw,kf. (13706) |
| 38 (physical adj1 (activit* or exercise*)).tw,kf. (89158) |
| 39 ((Smoking or cigar* or tobacco or alcohol*) adj2 (cessation or stop* or quit* or reduc* or abstinen* or withdrawal*)).tw,kf. (42214) |
| 40 (weight adj (loss or reduction)).tw,kf. (70109) |
| 41 exp “treatment adherence and compliance”/ (215866) |
| 42 ((adher* or non-adher* or compliance or non-compliance) adj2 (treatment? or medication*)).tw,kf. (21050) |
| 43 (screening adj5 (health* or cancer*)).tw,kf. (47461) |
| 44 or/30-43 [Healthy lifestyle] (2041439) |
| 45 *Patient Education as Topic/ (36279) |
| 46 exp Social Support/ (64039) |
| 47 (social adj2 support*).tw,kf. (30139) |
| 48 Patient care planning/ (37203) |
| 49 or/45-48 [Patient Knowledge] (147247) |
| 50 barrier?.ti,kf. (44604) |
| 51 difficult*.ti,kf. (26242) |
| 52 weakness*.ti,kf. (3988) |
| 53 participat*.ti,kf. (31623) |
| 54 facilitat*.ti,kf. (31063) |
| 55 enabler*.ti,kf. (365) |
| 56 strength*.ti,kw. (37766) |
| 57 determinant*.ti,kf. (44930) |
| 58 ((“Theoretical Domain?” or “Implementation Research” or Ecological or “Knowledge to Action” or “COMB B”) adj4 (Framework* or model? or system?)).tw,kf. (6077) |
| 59 motivat*.ti,kf. (16867) |
| 60 promot*.ti,kf. (142138) |
| 61 goal?.ti,kf. (15048) |
| 62 uptake.ti,kf. (62745) |
| 63 problem?.ti,kf. (179071) |
| 64 ((tackl* or address* or solv* or resolv* or sort*) adj1 problem*).tw,kf. (18324) |
| 65 Problem Solving/ (23501) |
| 66 exp Motivation/ (155294) |
| 67 or/50-66 [Barriers or Motivators] (783038) |
| 68 or/44,49 [Healthy lifestyle or patient knowledge] (2157107) |
| 69 67 and 68 [Barriers to healthy lifestyle or knowledge] (125499) |
| 70 (barriers adj4 care).ti. (1230) |
| 71 29 or 69 or 70 [Self Management or Barriers to lifestyle change] (237043) |
| 72 18 and 71 [SMI and SM or barriers to lifestyle change] (3836) |
| 73 Comment/ (678448) |
| 74 letter/ (937414) |
| 75 editorial/ (411497) |
| 76 note/ (1988) |
| 77 news/ (174511) |
| 78 newspaper article/ (18274) |
| 79 (comment* or letter? or editorial? or note?).ti. (163738) |
| 80 case reports/ (1881218) |
| 81 or/73-80 (3456232) |
| 82 Published Erratum/ or Retraction of Publication/ (5530) |
| 83 81 not 82 [Comments/Letters] (3455452) |
| 84 72 not 83 [SMI and SM or barriers to lifestyle change editorials etc. removed] (3531) |
| 85 exp Animals/ not exp Humans/ (4473346) |
| 86 (adolescent/ or child/ or infant/) not exp adults/ (1425928) |
| 87 84 not (85 or 86) [SMI and SM or barriers to lifestyle change - editorials/children/animals removed] (3280) |
Study Selection
Unique records identified by the search were imported into Covidence (52). Two reviewers independently screened titles and abstracts and then assessed full text eligibility; conflicts were resolved in discussion or through referral to a third reviewer.
Data Extraction
Relevant data were extracted by one reviewer into a table organised by determinants and behaviours. Using the MoA definitions (Table 3), each determinant was mapped to a MoA using descriptions reported by study authors. Some determinants were deemed to overlap with more than one MoA. We allocated evidence to the more specific MoA wherever possible. A second senior reviewer checked the extracted data and decided on determinants that had insufficient description or overlapped multiple MoAs, resulting in allocation of each data item to a single MoA.
Table 3.
Mechanisms of action and their definition.
| Mechanism of Action | Definition [Reproduced from (39)] |
|---|---|
| Knowledge | An awareness of the existence of something |
| Skills | An ability or proficiency acquired through practice |
| Social/Professional Role and Identity | A coherent set of behaviours and displayed personal qualities of an individual in a social or work setting |
| Beliefs about Capabilities | Beliefs about one's ability to successfully carry out a behaviour |
| Optimism | Confidence that things will happen for the best or that desired goals will be attained |
| Beliefs about Consequences | Beliefs about the consequences of a behaviour (i.e., perceptions about what will be achieved and/ or lost by undertaking a behaviour, as well as the probability that a behaviour will lead to a specific outcome) |
| Reinforcement | Processes by which the frequency or probability of a response is increased through a dependent relationship or contingency with a stimulus or circumstance |
| Intentions | A conscious decision to perform a behaviour or a resolve to act in a certain way |
| Goals | Mental representations of outcomes or end states that an individual wants to achieve |
| Memory, Attention, and Decision Processes | Ability to retain information, focus on aspects of the environment, and choose between two or more alternatives |
| Environmental Context and Resources | Aspects of a person's situation or environment that discourage or encourage the behaviour |
| Social Influences | Those interpersonal processes that can cause oneself to change one's thoughts, feelings, or behaviours |
| Emotion | A complex reaction pattern involving experiential, behavioural, and physiological elements |
| Behavioural Regulation | Behavioural, cognitive, and/or emotional skills for managing or changing behaviour |
| Norms | The attitudes held and behaviours exhibited by other people within a social group |
| Subjective Norms | One's perceptions of what most other people within a social group believe and do |
| Attitude toward the Behaviour | The general evaluations of the behaviour on a scale ranging from negative to positive |
| Motivation | Processes relating to the impetus that gives purpose or direction to behaviour and operates at a conscious or unconscious level |
| Self-image | One's conception and evaluation of oneself, including psychological and physical characteristics, qualities, and skills |
| Needs | Deficit of something required for survival, well-being, or personal fulfilment |
| Values | Moral, social or aesthetic principles accepted by an individual or society as a guide to what is good, desirable, or important |
| Feedback Processes | Processes through which current behaviour is compared against a particular standard |
| Social Learning/Imitation | A process by which thoughts, feelings, and motivational states observed in others are internalised and replicated without the need for conscious awareness |
| Behavioural Cueing | Processes by which behaviour is triggered from either the external environment, the performance of another behaviour, or from ideas appearing in consciousness |
| General Attitudes/Beliefs | Evaluations of an object, person, group, issue, or concept on a scale ranging from negative to positive |
| Perceived Susceptibility/Vulnerability | Perceptions of the likelihood that one is vulnerable to a threat |
Each behaviour was then mapped to one AADE-7 category: healthy eating; being active; monitoring; taking medication; problem solving; reducing risks (e.g., smoking cessation), and healthy coping. Once a data item was mapped as described, an MoA and AADE-7 determinant-behaviour link was formed.
Data Items
Quantitative findings describing determinants of self-management behaviours in individuals with SMI were the data of interest. Where studies included a non-SMI control group only the SMI group data were extracted.
Quality Appraisal of Individual Studies
The methodological quality of the included studies was assessed by one reviewer using the NICE quality appraisal checklist for quantitative studies reporting correlations and associations (53), which produces separate ratings for internal and external validity. All ratings were checked by a second reviewer. We incorporated certainty of evidence in the synthesis by including cumulative ratings of internal and external validity across studies for each reported MoA and AADE-7 link. In line with GRADE ratings (54), certainty of evidence was rated as high (all positive ratings), moderate (majority positive ratings), low (balance between positive and negative ratings), and very low (all negative ratings).
Synthesis of Results
We performed a narrative synthesis as data were too heterogenous to allow for meta-analysis of statistical tests of associations between determinants and behaviours. Studies reporting statistical tests of associations were prioritised in the synthesis. Where a study performed a multivariable analysis of determinants we opted to use the univariate associations to enhance comparability with other studies that did not include multivariate analyses. We mapped links between MoAs and AADE-7 self-management behaviours against the superordinate COM-B framework. This allowed for MoAs that derive from the TDF to be easily identifiable within the COM-B framework and offers the means to identify candidate intervention functions associated with MoAs using the behaviour change wheel (33). Links were reported as positive or negative. Where results were inconclusive we reported these as having no association.
Results
Study Selection
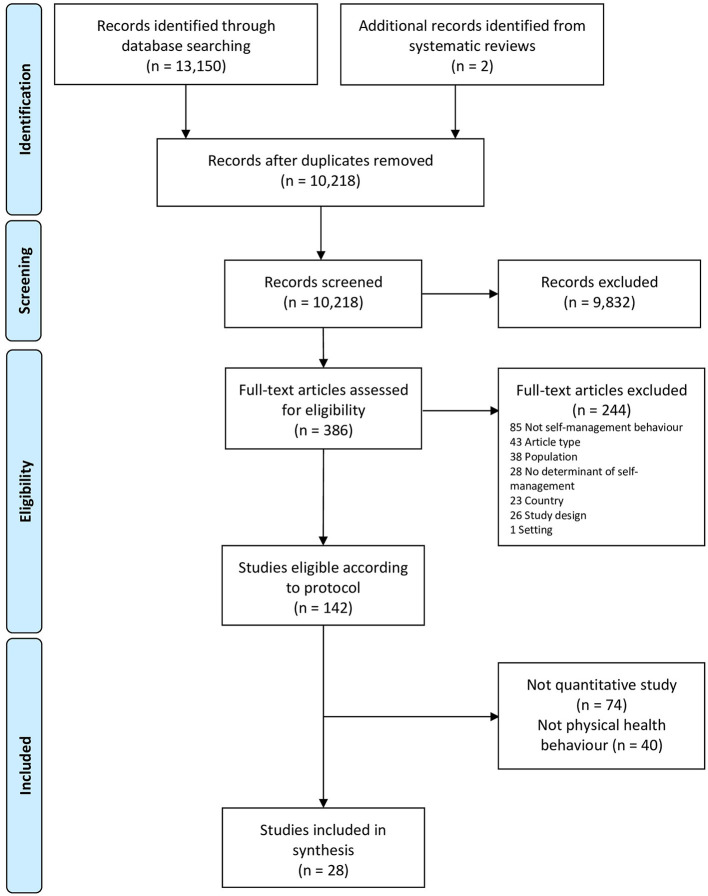
A flowchart of study selection in the context of the overarching review is shown in Figure 1. Of the 10,218 unique studies identified from searches, 386 were assessed as potentially eligible based on titles and abstracts and 28 studies were included.
Figure 1.
PRISMA flowchart.
Study Characteristics
Characteristics of the included studies are shown in Table 4. Twenty-four studies were of people with SMI and four studies were of people with SMI and diabetes (63, 69, 71, 77). We did not identify any study that met eligibility criteria that included populations of people with SMI and other long-term physical conditions. There were no studies of the perspective of clinicians or carers about determinants for individuals with SMI. Twenty-six studies used a cross-sectional design and two used a prospective cohort design. Nine studies were conducted in the USA, five in the UK, four in Canada, two each in Australia and Belgium, one each in Israel, Ireland, Italy, Japan and the Netherlands, and one study in both the Netherlands and Belgium.
Table 4.
Characteristics of included studies.
| Study ID Design, sample size | Country setting | SMI diagnoses of study sample | Mean age % female | Ethnicity |
|---|---|---|---|---|
| Arbour-Nicitopoulos et al. (55)Prospective cohort, N = 101 | Canada Community setting |
Schizophrenia 67.3% Schizoaffective 31.7% Psychosis not otherwise specified 1.0% |
41.5 years 40.6% |
White 57.4% African 18.8% South Asian 5.9% Asian 6.9% Other 10.9% |
| Ashton et al. (56) Cross-sectional, N = 1,043 |
Australia Smoking cessation programme within adult MH services |
Schizophrenia 37.1% Depression and/or anxiety 20.5% Bipolar disorder 18.3% Schizoaffective disorder 16.7% Other* 7.4% (percentages are of n = 868 with a recorded diagnosis) |
41.9 years (men) 45.1 years (women) 49.6% |
NR |
| Berti et al. (57) Cross-sectional, N = 193 |
Italy Community MH service |
Schizophrenia or related psychosis 78% Affective psychosis 22% |
48 years 47% |
NR |
| Bezyak et al. (58) Cross-sectional, N = 92 |
USA Outpatient treatment program |
Schizophrenia 55.8% Schizoaffective disorder 33.7% Bipolar disorder 6.3% Other mood disorders 3.2% Other psychotic disorders 1.1% |
Range 18–70 years 25.3% |
NR |
| Campion et al. (59) Cross-sectional, N = 43 |
UK Rehabilitation centre and outpatient depot clinic |
“The majority had a formal diagnosis of schizophrenia” | 52.6 years 39% |
NR |
| Dickerson et al. (60) Cross-sectional, N = 78 |
USA Outpatient MH services |
Schizophrenia or schizoaffective disorder 64% Bipolar disorder 22% Major depression 13% Other 1% |
50.0 years 40% |
Caucasian 72% African American 27% Other 1% |
| Faulkner et al. (61) Cross-sectional, N = 109 |
Canada Smoking cessation clinic within an MH and Addiction facility |
Currently receiving treatment for mental health disorders (e.g., schizophrenia or depression) 92.7% Did not respond 6.3% |
46.5 years 46.8% |
White 91.0% Black/Asian 3.6% Aboriginal 1.8% Hispanic 0.9% Not identified 2.7% |
| Filia et al. (62) Cross-sectional, N = 43 |
Australia Community MH settings |
Schizophrenia 53.5% Schizoaffective disorder 25.6% Bipolar affective disorder 13.9% Other non-organic psychotic syndrome 7.0% |
36.3 years 41.9% |
Australian born 90.7% |
| Gorczynski et al. (63) Cross-sectional, N = 63 |
Canada Outpatient psychiatric facility |
Schizophrenia 52.4% Schizoaffective disorder 23.8% Bipolar 1 disorder 17.5% Major depressive disorder with psychosis 3.2% Other forms of psychosis 3.1% |
50.2 years 38.1% |
White 58.7% Black 19.0% Asian 12.7% |
| Kelly et al. (64) Cross-sectional, N = 100* |
USA Psychiatric research centre outpatient and inpatient programs |
Individuals with a diagnosis of schizophrenia or schizoaffective disorder recruited but characteristics of sample not reported | 43.3 years 29% |
Caucasian 61% African American 37% Other 2% |
| Klingaman et al. (65) Cross-sectional, N = 5,388 |
USA Veterans Affairs weight management program |
Schizophrenia 100% | Median 55 years 14.1% |
Race White 49.2% Black 32.2% Other 5.5% Unknown 13.1% Ethnicity Hispanic 11.3% |
| Kreyenbuhl et al. (66) Cross-sectional, N = 44* |
USA Public and private outpatient MH clinics in urban and suburban communities |
Schizophrenia-spectrum disorder 70% Major mood disorder 30% |
51.1 years 55% |
Non-Caucasian 41% |
| Matthews et al. (67) Cross-sectional, N = 105 |
Ireland Rehabilitation and recovery mental facilities |
Schizophrenia 44% Affective disorder 39% Majority of sample taking antipsychotic medication (70%) |
52 years 29% |
NR |
| Mishu et al. (68) Cross-sectional, N = 3,287 |
UK Large SMI research cohort recruited from primary and secondary care |
Individuals with diagnosis of schizophrenia or other psychotic disorders, bipolar disorder or depression with psychotic features eligible for study but characteristics of sample not reported | 47.7 years 40.1% |
White British 85.7% Other 14.3% |
| Mulligan et al. (69) Cross-sectional, N = 77 |
UK National Health Service, charities and service user networks |
Schizophrenia 36.4% Schizoaffective disorder 16.9% Depression with psychotic features 22.1% Bipolar disorder 41.6% (may have more than one diagnosis) |
52.3 years 46.8% |
Ethnicity White, British 61.0% White, other 9.1% South Asian 10.4% Black African Caribbean 7.8% Other 10.4% Missing 1.3% Missing 24.7% |
| Muralidharan et al. (70) Cross-sectional, N = 17,826 |
USA Veterans Affairs weight management program |
Schizophrenia or bipolar disorder (proportions not reported) | 54 and younger 49.3% 55 and older 50.7% 21.3% |
Race White 59.9% Black 23.7% Other 4.9% Unknown/missing 11.6% Ethnicity Hispanic 9.2% |
| Ogawa et al. (71) Cross-sectional, N = 38 |
Japan Outpatient psychiatric care |
Schizophrenia 100% | 53.9 years 39.5% |
NR |
| Peckham et al. (72) Cross-sectional, N = 97 |
UK Primary and secondary care |
Schizophrenia or other psychotic illness 59% Bipolar disorder 31% Schizoaffective disorder 10% |
Median 47.2 40.2% |
NR |
| Prochaska et al. (73) Cross-sectional, N = 685 |
USA Online mood disorder peer-support network |
Bipolar disorder 100% | 26–50 years 67% Not reported 33% 67% |
Non-Hispanic Caucasian 89% Not reported 11% |
| Romain and Abdel-Baki (74) Cross-sectional, N = 43 |
Canada Physical activity programme (baseline data) |
Schizophrenia 30.2% Bipolar disorders 23.3% Psychosis other 20.9% Schizo-affective disorders 14% Major depressive disorders 9.3% Severe anxiety disorders 2.3% |
29.0 years 32.3% |
NR |
| Roosenschoon et al. (75) Cross-sectional, N = 187 |
Netherlands Outpatient MH services |
Psychotic disorders 57% Mood disorder 33% Personality disorder 35% (Total >100% because participants had multimorbidity) |
44.3 years 47% |
NR |
| Shor and Shalev (76) Cross-sectional, N = 86 |
Israel Community MH facilities |
Schizophrenia 70% Bipolar disorder 16% Depression 14% |
39.4 years 52% |
NR |
| Spivak et al. (77) Cross-sectional, N = 271 |
USA Inner-city outpatient MH centres |
Primary diagnosis Schizophrenia 33% Mood disorder with psychotic features 60% Psychotic disorder not otherwise specified 7% |
42 years 53% |
Black 54% White 34% Other 12% |
| Twyford and Lusher (78) Cross-sectional, N = 105* |
UK Community MH services |
Schizophrenia 100% | 38.3 years 21% |
NR |
| Vancampfort et al. (79) Cross-sectional, N = 69* |
Belgium Psychiatric centres |
Schizophrenia 100% | 40.6 years 34.1% |
NR |
| Vancampfort et al. (80) Cross-sectional, N = 29* |
Belgium Psychiatric centres |
First-episode psychosis 100% | Men mean 25.0 years Women mean 23.7 years 35.7% |
NR |
| Vermeulen et al. (81) Prospective cohort, N = 1,094 |
Netherlands and Belgium University medical centres and associated mental health-care institutions |
Schizophrenia 66% Others not reported |
NR | NR |
| Zechner and Gill (82) Cross-sectional, N = 120 |
USA Outpatient MH services |
Bipolar disorder 35.0% Schizophrenia 29.2% Schizoaffective disorder 8.3% Depression 35.8% (Total >100% because participants had multimorbidity) |
47.5 years 40% |
Black 50.8% White 37.5% Hispanic 5.0% American Indian 1.7% Asian 1.7% Other 3.3% |
Table 5 shows the links between outcomes and AADE-7 self-management behaviours and between measured determinants and MoAs across all included studies. Six studies reported determinants of multiple self-management behaviours, two of which focused on a range of diabetes self-management activities (69, 71); the other four reported behaviours including physical activity, healthy eating, reducing risks (smoking cessation and alcohol consumption) (57, 59, 61, 65). Of the studies that focused on a single behaviour, eleven reported determinants of being active (55, 58, 63, 67, 68, 70, 74, 76, 78–80, 82), seven were about reducing risks [smoking cessation (56, 60, 62, 64, 72, 73, 81), seeking professional help (77), alcohol or drug use (75)], and one was about taking medications (66). Studies reported evidence aligning with a mean of five different MoAs (range 1–14) and there was evidence identified for 21 of 26 MoAs. The links between reported health outcomes and AADE-7 self-management behaviours and the links between reported determinants and MoAs are shown in Table 3.
Table 5.
Links between outcomes and AADE7 self-management behaviours and between measured determinants and MoAs.
| Study IDDesign, sample size | Outcome measure | AADE7 Behaviour (s) | Determinant (s) and measures | Mechanism of Action |
|---|---|---|---|---|
| Arbour-Nicitopoulos et al. (55) | Accelerometer | Physical activity | Intentions Action planning Coping planning Maintenance self-efficacy Health Action Process Approach inventory for adults with schizophrenia Social support Multidimensional Scale of Perceived Social Support |
Intentions Behavioural cueing Behavioural regulation Beliefs about Capabilities Environmental context and resources |
| Ashton et al. (56) | Pre-programme questionnaire for the Tobacco Free programme | Reducing risks – smoking cessation | Fitness; Impact on others Financial reasons Wanting freedom from addiction Health concerns Stigma Questionnaire (origin not reported) |
Beliefs about consequences Environmental context and resources Goals Perceived susceptibility/vulnerability Subjective norms |
| Berti et al. (57) | PASSI Questionnaire developed for the PASSI project | Physical activity Reducing risks—smoking cessation; alcohol consumption |
Employment status Client Sociodemographic and Service Receipt Inventory (CSSRI-EU) |
Environmental context and resources |
| Bezyak et al. (58) | The Physical Activity Scale for Individuals with Physical Disabilities (PASIPD), modified to refer to mental illness | Physical activity | Self-efficacy Multidimensional Self-Efficacy Questionnaire (MSEQ) Perceived pros and cons Decisional Balance for Exercise Adoption Relationships with program staff An exploratory question asked whether relationships with treatment program staff encouraged them to be physically active |
Beliefs about capabilities Beliefs about capabilities Social influences |
| Campion et al. (59) | Reported Health Behaviours Checklist. Interviews (yes/no questions) based on stages of change model |
Physical activity Reducing risks—smoking cessation |
Time; opportunity; expense Enjoyment; stress reduction Doctor's advice Social activity Prevent health problems Injury/weakness Media influence Questions based on dimensions of the Health Belief Model Interest in the behaviour Time of day |
Environmental context and resources Reinforcement Social influences Needs Perceived susceptibility/vulnerability Beliefs about capabilities Subjective norms Motivation Behavioural cueing |
| Dickerson et al. (60) | Structured interviews relating to smoking cessation | Reducing risks—smoking cessation | Health concerns Cost of cigarettes; experience of smoking restrictions in hospital; smoking restrictions at home or work Suggestion or advice from a doctor; suggestion or advice from others Example of family members who had died from a smoking-related illness; example of friends who quit Structured interview developed by authors |
Perceived susceptibility/vulnerability Environmental context and resources Social influences Social learning/imitation |
| Faulkner et al. (61) | Survey assessing perceived interest in physical activity Number of attempts to quit smoking |
Physical activity Reducing risks - smoking cessation |
Various perceived advantages of (e.g., it would improve my muscle tone) and barriers to (e.g., it would leave me feeling tired) becoming more physically active Improve how I feel about myself Improve my health or reduce my risk of disease; I might injure myself I would have to do it by myself; it would take time away from other things; it would cost too much I would worry about what other people think of me; I would be worried that I would not be very good at it I don't know how to do it It would be difficult to find out what to do and where to do it Decisional balance measure devised for the study Interest in physical activity (as a determinant of smoking cessation) |
Beliefs about consequences Self-image Perceived susceptibility/vulnerability Environmental context and resources Emotion Knowledge Beliefs about capabilities Motivation |
| Filia et al. (62) | Opiate treatment index (OTI) Fagerstrom Test for Nicotine dependence Breath levels of carbon monoxide |
Reducing risks—smoking cessation | Health concerns Self-control (to prove I can; to feel in control; can do other things) Reinforcement (I won't smell; to save money; won't burn holes in clothes) Social influence Reasons for quitting questionnaire Stress reduction (relaxation; to take a break; reduce stress); addiction (habit; craving); arousal (peps me up; weight control; enjoyment; to help concentration); mental illness |
Perceived susceptibility/vulnerability Self-image Beliefs about consequences Social influences |
| Partner smoking Reasons for smoking questionnaire |
Reinforcement Behavioural cueing |
|||
| Gorczynski et al. (63) | International Physical Activity Questionnaire (IPAQ) | Physical activity | Self-efficacy Perceived barriers Perceived benefits Patient-Centered Assessment and Counseling for Exercise (PACE) questionnaire Negative symptoms of psychosis (alogia; affective blunting; avolition-apathy; anhedonia-asociality; attentional impairment) Scale for the Assessment of Negative Symptoms (SANS) |
Beliefs about capabilities Attitude toward the behaviour Beliefs about consequences Motivation |
| Kelly et al. (64) | Fagerström Test for Nicotine Dependence | Reducing risks—smoking cessation | Health concerns Self-control (to prove I can; to feel in control; can do other things) Reinforcement (I won't smell; to save money; won't burn holes in clothes) |
Perceived susceptibility/vulnerability Self-image |
| Social pressure Reasons for quitting questionnaire |
Beliefs about consequences Social influences |
|||
| Klingaman et al. (65) | MOVE!23, a multidimensional assessment of factors related to weight management. | Physical activity Diet |
Eating from restaurants/convenience stores/vending machines; too much high calorie food at home/work; too little time to prepare and eat healthy food; too little money to buy healthy food; job/work schedule; no place to walk/be active; no transportation; lack of support/encouragement | |
| Feeling hungry much of the time; too tired Used to eating a certain way Stress/depression Being with others who overeat Safety concerns Do not like the behaviour Daily routines “MOVE!23,” a multidimensional assessment of factors related to weight management |
Environmental context and resources Motivation Behavioural regulation Emotion Subjective norms Perceived susceptibility/vulnerability Attitude toward the behaviour Behavioural cueing |
|||
| Kreyenbuhl et al. (66) | Brief Medication Questionnaire | Medication adherence | Motivation barrier (how well does your diabetes medication work for you?) Recall barrier Access barrier Brief Medication Questionnaire Beliefs about the necessity of diabetes medications for controlling the illness; concerns about the adverse consequences of taking the medications |
Beliefs about consequences Memory, attention, and decision processes Environmental context and resources |
| Beliefs about Medication Questionnaire: Specific Version (BMQ-Specific) HbA1c |
Beliefs about consequences Behavioural Regulation |
|||
| Matthews et al. (67) | 3Q physical activity assessment | Physical activity | Environmental resources Motivation and goals Beliefs about capabilities Knowledge Skills Emotion Social influences Beliefs about the consequences Action planning Coping planning Goal conflict The Determinants of Physical Activity Questionnaire (DPAQ) |
Environmental context and resources Motivation, Goals Beliefs about capabilities Knowledge Skills Emotion Social influences Beliefs about consequences Behavioural cueing Behavioural regulation Goals |
| Mishu et al. (68) Cross-sectional |
Self-reported participation in regular physical activity | Physical activity | Employment status Self-rated health Health problem limiting activity Importance of maintaining healthy lifestyle Would like to take more exercise Closing the Gap: The Lifestyle Health and Well-being (HWB) survey |
Environmental context and resources Self-image Beliefs about capabilities Values Attitude toward the behaviour |
| Mulligan et al. (69) Cross-sectional |
Summary of Diabetes Self-Care Activities (SDSCA) | Control—self-monitoring of blood glucose Medication adherence General diet Specific diet (eating fruit and vegetables and high fat foods) Physical activity Reducing risks—checking feet; smoking |
Psychological distress CORE-10 Knowledge Skills Social/professional role and identity Beliefs about capabilities; most difficult self-management behaviour Optimism Beliefs about consequences Reinforcement Intentions Goals Memory, attention and decision processes Environmental context and resources; employment status Social influences Emotion Behavioural regulation Questionnaire based on the Theoretical Domains Framework (TDF) |
Emotion Knowledge Skills Social/Professional role and identity Beliefs about capabilities Optimism Beliefs about consequences Reinforcement Intention Goals Memory, attention an decision processes Environmental context and resources Social influences Emotion Behavioural regulation |
| Muralidharan et al. (70) Cross-sectional |
“MOVE!23,” a multidimensional assessment of factors related to weight management | Physical activity | Physical health barriers Too little money; lack of support/encouragement; too little time; job/work schedule; no transportation; no place to walk/be active Too tired Stress/depression Safety concerns Do not like the behaviour Daily routines “MOVE!23,” a multidimensional assessment of factors related to weight management |
Beliefs about capabilities Environmental context and resources Motivation Emotion Perceived susceptibility/vulnerability Attitude toward the behaviour Behavioural cueing |
| Ogawa et al. (71) | Summary of Diabetes Self-Care Activities Questionnaire—Japanese version (SDSCA-J) | Physical activity Medication adherence Control - blood sugar testing; foot care |
Symptom severity Brief Psychiatric Rating Scale (BPRS) |
Emotion |
| Cross-sectional | Psychosocial functioning Global Assessment of Functioning Scale (GAF) |
Skills | ||
| Food Frequency Questionnaire Based on Food Groups (FFQg) | Diet | HbA1c Most recent test in medical records |
Behavioural regulation | |
| Peckham et al. (72) Cross-sectional |
Standardised interview about reasons for smoking and wanting to quit | Reducing risks–smoking cessation | Helps to cope with stress; helps to relax; bad for my health; makes me less fit; bad for the health of people near me; bad example for children; unpleasant for people near me; makes my clothes and breath smell; I enjoy it; breaks up working time | Beliefs about consequences |
| Something to do when bored Stops withdrawal symptoms Something to do with friends Stops me putting on weight I don't like feeling dependent on cigarettes Expense People around me disapprove Standardised interview about reasons for smoking and wanting to quit |
Behavioural cueing Reinforcement Social influences Goals Self-image Environmental context and resources Subjective norms |
|||
| Prochaska et al. (73) Cross-sectional |
Survey developed for the study about tobacco use, attempts to quit and tobacco-related attitudes and intentions | Reducing risks—smoking cessation | Gets in the way of living the life that I want Stress; craving Tobacco use by family and friends; support from family and friends; encouragement from healthcare providers Belief I can quit Pleasure of behaviour; concerns it would make my mental illness worse To treat my mental illness; being in good mental health Survey developed for the study about tobacco use, attempts to quit and tobacco-related attitudes and intentions |
Goals Emotion Environmental context and resources Beliefs about capabilities Beliefs about consequences Motivation |
| Romain and Abdel-Baki (74)Cross-sectional | Global Physical Activity Questionnaire | Physical activity |
Self-efficacy French translation of a scale developed by Bandura (83) Perceived advantages and inconveniences of the behaviour Decisional Balance Scale for Exercise |
Beliefs about capabilities Beliefs about consequences |
| Roosenschoon et al. (75)Cross-sectional | Single item from Addiction Severity Index (ASI) | Reducing risks—problems with alcohol/drug use | Social support Multidimensional Scale of Perceived Social Support (MSPSS) |
Environmental context and resources |
| Shor and Shalev (76)Cross-sectional | Scales designed to measure participants' perception of the barriers to and benefits of involvement in physical activities | Physical activity | Knowledge Accessibility Thoughts that the behaviour will not improve the person's condition; fear that the behaviour will have a negative effect on one's health; improvement of mental health and health Improvement of feelings about body Side effects of psychiatric medications; weight and associated co-morbid health problems Mental health Scales designed to measure participants' perception of the barriers to and benefits of involvement in physical activities |
Knowledge Environmental context and resources Beliefs about consequences Self-image Beliefs about capabilities Emotion |
| Spivak et al. (77)Cross-sectional | Delays in seeking medical care over the past 12-month period were assessed by using seven items, five of which were derived from the National Health Interview Survey | Reducing risks—seeking professional help | Couldn't get through on the telephone; couldn't get an appointment soon enough; once you get there you have to wait too long to see a doctor; the (clinic/doctor's) office wasn't open when I could get there; didn't have transportation; did not have health insurance or could not afford to receive care Concerns about being treated differently because of mental illness Questions partly derived from the National Health Interview Survey |
Environmental context and resources Subjective norms |
| Twyford and Lusher (78)Cross-sectional | A questionnaire adapted from Godin and Shephard's (84) Leisure-Time Activity Questionnaire (GLTEQ) | Physical activity | Behavioural beliefs Attitudes Subjective norms Perceived behavioural control; Self-efficacy Intention A questionnaire adapted from Ajzen's (85) guide to constructing a Theory of Planned Behaviour questionnaire Living situation; employment status; health professional support |
Beliefs about consequences Attitude toward the behaviour Subjective norms Beliefs about capabilities Intentions Environmental context and resources |
| Vancampfort et al. (79)Cross-sectional | Behavioural Regulation in Exercise Questionnaire 2 (BREQ-2) | Physical activity |
Amotivation External regulation Introjected regulation Autonomous regulation Behavioural Regulation in Exercise Questionnaire 2 (BREQ-2) |
Motivation Social influences Values Reinforcement |
| Vancampfort et al. (80)Cross-sectional | Patient-Centred Assessment and Counseling for Exercise | Physical activity | Amotivation External regulation Introjected regulation Autonomous regulation Behavioural Regulation in Exercise Questionnaire 2 (BREQ-2) |
Motivation Social influences Values Reinforcement |
| Vermeulen et al. (81)Prospective cohort | Composite International Diagnostic Interview (CIDI) | Reducing risks—smoking initiation and cessation | Symptom frequency Community Assessment of Psychotic Experience (CAPE) Symptom severity Emotional distress Positive And Negative Syndrome Scale (PANSS) Quality of life WHO Quality of Life (WHOQOL) schedule |
Motivation Motivation Emotion Self-image |
| Zechner and Gill (82)Cross-sectional | International Physical Activity Questionnaire—Short Form (IPAQ) | Physical activity | Social support Social Support for Exercise Scale Self-efficacy Self-efficacy for Exercise Scale Outcome expectations Outcome Expectations for Exercise Scale Goal-setting, self-monitoring, problem solving Exercise Goal-Setting Scale Psychological distress due to psychiatric symptoms Brief Symptom Inventory |
Environmental context and resources Beliefs about capabilities Beliefs about consequences Behavioural regulation Emotion |
Quality Appraisal of Individual Studies
Quality appraisal ratings are shown in Table 6. Five studies were rated as having high internal validity (55, 63, 71, 77, 81), but no studies were rated as having both high internal and external validity. Six studies were rated as having both low internal and low external validity (56, 59, 61, 62, 65, 76).
Table 6.
Quality appraisal ratings for individual studies.
| Population | Method of selection of exposure (or comparison) group | Outcomes | Analyses | Summary | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| References | 1.1 Is the source population or source area well-described? | 1.2 Is the eligible population or area representative of the source population or area? | 1.3 Do the selected participants or areas represent the eligible population or area? | 2.1 Selection of exposure (and comparison) group. How was selection bias minimised? | 2.2 Was the selection of explanatory variables based on a sound theoretical basis? | 2.3 Was the contamination acceptably low? | 2.4 How well were likely confounding factors identified and controlled? | 2.5 Is the setting applicableto the UK? | 3.1 Were the outcome measures and procedures reliable? | 3.2 Were the outcome measurements complete? | 3.3 Were all the importantoutcomes assessed? | 3.4 Was there a similar follow-up time in exposure and comparison groups? | 3.5 Was follow-up meaningful? | 4.1 Was the study sufficiently powered to detect an intervention effect (if one exists)? | 4.2 Were multiple explanatory variables considered in the analyses? | 4.3 Were the analytical methods appropriate? | 4.4 Was the precision of association given or calculable? Is association meaningful? | 5.1 Are the study results internally valid (i.e., unbiased)? | 5.2 Are the findings generalisable to the source population (i.e., externally valid)? |
| Arbour-Nicitopoulos et al. (55) | + | NR | + | NA | ++ | NA | + | + | ++ | - | NA | + | ++ | NA | ++ | ++ | ++ | ++ | + |
| Ashton et al. (56) | ++ | – | – | NA | ++ | NA | – | + | – | – | NA | NA | NA | NA | – | – | – | – | – |
| Berti et al. (57) | ++ | ++ | + | NA | + | NA | – | + | – | NR | NA | NA | NA | NA | + | + | – | + | + |
| Bezyak et al. (58) | + | + | + | NA | ++ | NA | NA | – | – | + | NA | NA | NA | NA | – | – | – | – | + |
| Campion et al. (59) | + | – | – | NA | ++ | NA | NR | + | – | NR | NA | NA | NA | NA | + | NR | – | – | – |
| Dickerson et al. (60) | + | + | – | NA | – | NA | – | + | – | + | NA | NA | NA | NA | – | – | – | – | + |
| Faulkner et al. (61) | – | – | – | NA | – | NA | – | + | – | + | NA | NA | NA | NA | – | – | – | – | – |
| Filia et al. (62) | + | + | – | NA | + | NA | – | + | – | ++ | NA | NA | NA | NA | – | – | – | – | – |
| Gorczynski et al. (63) | – | NR | NR | NA | ++ | NA | + | + | + | ++ | NA | NA | NA | NA | ++ | + | ++ | ++ | – |
| Kelly et al. (64) | + | + | + | NA | + | NA | – | + | – | NR | NA | NA | NA | NA | – | – | – | – | + |
| Klingaman et al. (65) | + | – | + | NA | NR | NA | NR | – | – | – | NA | NA | NA | NA | – | – | – | – | – |
| Kreyenbuhl et al. (66) | + | – | + | NA | ++ | NA | NA | – | – | ++ | NA | NA | NA | NA | ++ | + | ++ | + | + |
| Matthews et al., (67) | + | + | – | NA | ++ | NA | – | + | + | ++ | NA | NA | NA | NA | – | + | – | + | + |
| Mishu et al. (68) | + | + | + | NA | NR | NA | – | ++ | – | – | NA | NA | NA | NA | ++ | + | ++ | + | + |
| Mulligan et al. (69) | + | ++ | + | NA | ++ | NA | – | ++ | – | ++ | NA | NA | NA | NA | ++ | + | ++ | + | + |
| Muralidharan et al. (70) | + | + | + | NA | + | NA | NA | – | – | ++ | NA | NA | NA | NA | + | – | – | – | + |
| Ogawa et al. (71) | + | + | + | NA | + | NA | ++ | + | + | + | NA | NA | NA | NA | ++ | ++ | ++ | ++ | + |
| Peckham et al. (72) | + | + | + | NA | NR | NA | – | ++ | – | – | NA | NA | NA | NA | + | – | – | – | + |
| Prochaska et al. (73) | + | + | + | NA | – | NA | – | + | – | + | NA | NA | NA | NA | – | – | – | – | + |
| Romain and Abdel–Baki (74) | – | NR | + | NA | ++ | NA | NA | + | NR | ++ | NA | NA | NA | NA | ++ | – | + | + | – |
| Roosenschoon et al. (75) | + | + | + | NA | ++ | NA | – | + | – | ++ | NA | NA | NA | NA | + | + | + | + | + |
| Shor and Shalev (76) | + | + | – | NA | + | NA | – | + | – | + | NA | NA | NA | NA | – | – | + | – | – |
| Spivak et al. (77) | + | + | + | NA | NR | NA | ++ | – | – | + | NA | NA | NA | NA | ++ | ++ | ++ | ++ | + |
| Twyford and Lusher (78) | + | – | – | NA | ++ | NA | NA | ++ | – | NR | NA | NA | NA | NA | ++ | – | + | + | – |
| Vancampfort et al. (79) | + | + | NR | NA | ++ | NA | NA | + | – | ++ | NA | NA | NA | NA | – | – | – | – | + |
| Vancampfort et al. (80) | + | + | + | NA | ++ | NA | – | + | + | ++ | NA | NA | NA | NA | + | ++ | ++ | + | + |
| Vermeulen et al. (81) | – | + | + | NA | ++ | NA | ++ | + | + | + | NA | + | + | NA | ++ | + | ++ | ++ | + |
| Zechner and Gill (82) | – | – | NR | NA | ++ | NA | + | – | + | – | NA | NA | NA | NA | + | + | + | + | + |
Synthesis of Findings About Links Between MoAs and AADE-7 Self-Management Behaviours
Twenty-one MoAs were identified as determinants of self-management behaviours for people with SMI and people with SMI and diabetes. Table 7 reports evidence of positive (green), negative (red), and no significant associations (amber) between MoAs and AADE-7 self-management behaviours. MoAs are grouped under the super-ordinate categories used in the COM-B framework.
Table 7.
Associations between mechanisms–of–action and AADE-7 self-management behaviours.
| COM-B: Mechanism of Action | Positive Association | Certainty of evidence | Negative Association | Certainty of evidence | Inconclusive | Certainty of evidence |
|---|---|---|---|---|---|---|
| Capability | ||||||
| Knowledge | Healthy eating (69) | Moderate | Being active (67) | Moderate | ||
| Memory, attention, and decision processes | Healthy eating (69) | Moderate | ||||
| Behavioural regulation | Monitoring, problem solving, being active (82) | Moderate | Healthy eating, monitoring (69) | Moderate | Being active (55, 67); taking medications (66) | Moderate |
| Skills | Being active (67, 71); Monitoring (69, 71); taking medication, healthy eating, reducing risks (71) | Moderate | ||||
| Opportunity | ||||||
| Social influences | Healthy eating, being active (69) | Moderate | Being active (67); Monitoring, taking medication, reducing risk (69) | Moderate | ||
| Environmental context and resources | Being active (69, 82); healthy eating, taking medication | Moderate | Being active (55) | Moderate | Being active (67, 78); Monitoring, reducing risks (69) | Moderate |
| (69); reducing risk (75) | ||||||
| Behavioural cueing | Being active (55, 67) | Moderate | ||||
| Motivation | ||||||
| Reinforcement | Healthy eating, being active (69) | Moderate | Monitoring, taking medication, reducing risks (69) | Moderate | ||
| Emotion | Reducing risks (69, 71, 81); being active (69, 82); healthy eating, monitoring (69) | Moderate | Being active (67) | Moderate | ||
| Beliefs about capabilities | Being active (55, 58, 61, 63, 68, 69, 74, 78, 82); healthy eating (69) | Moderate | Being active (67) | Moderate | ||
| Beliefs about consequences | Being active (58, 61, 67, 74, 78, 82); healthy eating (69) | Low to Moderate | Monitoring, taking medication, reducing risks (69) | Moderate | ||
| Motivation | Being active (67); Reducing risks (61) | Low to Moderate | Being active (63) | Moderate | Reducing risks (81) | Moderate |
| Intentions | Being active (69, 78); healthy eating (69) | Moderate | Monitoring; taking medication; reducing risks (69) | Moderate | ||
| Goals | Healthy eating (69); being active (67, 69) | Moderate | Taking medication, monitoring, reducing risks (69) | Moderate | ||
| Subjective norms | Being active (78) | Low | ||||
| Attitude toward the behaviour | Being active (63) | Moderate | Being active (68) | Moderate | ||
| Self-image | Being active (61, 68) | Low | Reducing risks (81) | Moderate | ||
| Values | Being active (68) | Moderate | ||||
| Perceived susceptibility/vulnerability | Being active, reducing risks (61) | Very low | ||||
| Optimism | Healthy eating (69) | Moderate | Being active, monitoring; taking medication; reducing risks (69) | Moderate | ||
| Social/Professional Role and Identity | Monitoring, healthy eating, taking medication; being active, reducing risks (69) | Moderate | ||||
Green highlighted text indicates a positive association between mechanism-of-action and self-management behaviour; red highlighted text indicates a negative association between mechanism-of-action and self-management behaviour; and amber highlighted text indicates that the evidence was inconclusive to determine an association between a mechanism-of-action and a self-management behaviour.
Capability
Nineteen tests of association between MoAs and self-management behaviours were identified in six studies that could be grouped under the Capability domain. There was only limited evidence from one cross-sectional study about barriers to effective diabetes management in people with SMI, which reported that knowledge was positively associated with the frequency of following a healthy eating plan (69). This same study showed that memory, attention and decision processes and behavioural regulation were negatively associated with healthy eating. A non-significant association in either direction was observed for skills in relation to healthy eating.
There was mixed evidence that behavioural regulation was associated with monitoring, with one result showing a positive association with this behaviour (82), and another reporting a negative association (69). Evidence that skills are associated with monitoring was equivocal, with no association between this MoA and behaviour reported in two cross-sectional studies (69, 71). Additionally, memory, attention, and decision processes were not reported as being significantly associated with monitoring.
Behavioural regulation was positively associated with being active in a cross-sectional study of predictors of physical activity in people with a wide range of SMI (82); however there was no evidence of association between this MoA and behaviour in a longitudinal study of physical activity intentions in people with schizophrenia (55). There was descriptive evidence that lack of knowledge about how to do physical activities was the third highest ranked of eight barriers to being active (76), but another cross-sectional study found no association between knowledge and physical activity (67). Memory, attention, and decision processes were not significantly associated with being active (69).
Cross-sectional data from a study about glycaemic control and diabetes self-care in people with schizophrenia did not show either a positive or negative relationship between skills and behaviours associated with reducing risks (71). Memory, attention, and decision processes were also not significantly associated with reducing risks (69). Neither memory, attention, and decision processes (69), behavioural regulation (66), or skills (71) were significantly associated with taking diabetes medication (71). Furthermore, memory, attention, and decision processes were cited as a barrier among 75% of participants in a comparative cross-sectional study of taking diabetes medications in people with and without SMI (66). Only one significant association was observed for problem solving, with one study showing a positive association between behavioural regulation and this behaviour (82).
Summary of Findings for Capability
The certainty of evidence for associations between MoAs and AADE-7 health behaviours within the Capability domain was rated as moderate across all studies. Only two studies reported positive associations: one for healthy eating (knowledge) and one for monitoring, problem solving, and being active (behavioural regulation). One study reported negative associations for healthy eating with memory, attention and decisional processes and behavioural regulation and also with monitoring for behavioural regulation. The majority of associations in this domain were inconclusive for five of the seven health behaviours.
Opportunity
Eighteen tests of association between MoAs and self-management behaviours were identified in studies that could be grouped under the Opportunity domain. Cross-sectional data from one study showed that social influences and environmental context and resources were positively associated with healthy eating (69). Environmental context and resources, defined as aspects of the situation and surroundings that influence engagement in health behaviours, were also implicated in predicting physical activity. Evidence from two studies showed that social support and support from health professionals was positively associated with being active in people with SMI (82) and also in people with SMI and diabetes (69). Data from a Canadian prospective cohort study (55) showed that support from family, friends, and significant others was not associated with physical activity and a UK cross-sectional study (78) showed health professional support explained variance in exercise intention but not behaviour in people with schizophrenia. There was evidence from multiple studies that physical activity was more frequent in the employed than the unemployed (57, 68, 69, 78). Additionally behavioural cuing was not significantly associated with being active (55, 67). Tests of associations between monitoring and MoAs were observed in only one study. Mulligan et al. showed that social influences and environmental context and resources were not significantly associated with monitoring in a population with SMI (69). Reducing risks associated with alcohol and drug use was positively associated with environmental context and resources in one cross-sectional study in people with a range of psychotic and mood disorders and personality disorder (75). There were more equivocal findings in one other study which found no evidence for a significant association between either environmental context and resources or social influences and reducing risks (69). There was scant evidence of associations between MoAs aligned with Opportunity and taking medications. Findings from one cross-sectional study showed that access to health services was positively associated with taking diabetes medication, suggesting that environmental context and resources are important drivers of this behaviour (69).
Summary of Findings for Opportunity
The certainty of evidence for associations between MoAs and AADE-7 health behaviours within the Opportunity domain was rated as moderate across all studies. There was more inconclusive evidence for the importance of social influences being associated with behaviours, with only one study showing a positive association for this MoA with healthy eating and being active. The role of environmental context and resources appears to be important with four studies reporting positive associations for four behaviours (being active; healthy eating; taking medication; and reducing risk). Two studies reported negative associations with being active and environmental context and resources. There was little conclusive evidence about the role of behavioural cueing in prompting behaviours.
Motivation
Sixty-three tests of association between MoAs and self-management behaviours were identified in twelve studies that could be grouped under the Motivation domain. The most consistent evidence was observed between MoAs and healthy eating, with positive associations observed in one cross-sectional study for reinforcement, emotion, beliefs about capabilities, beliefs about consequences, intentions, goals, and optimism (69). This study also reported non-significant associations between healthy eating and social/professional role identity.
Evidence about the links between MoAs and monitoring was also drawn from the same cross-sectional study, but findings were equivocal. A positive significant association was reported for the link between emotion and monitoring, but no significant associations were observed for reinforcement, beliefs about consequences, intentions, goals, optimism, and social/professional role identity with this behaviour (69).
The most evidence was observed for determinants of being active. Eleven MoAs were positively associated with being active across ten studies (55, 58, 61, 63, 67–69, 74, 78, 82). The most commonly reported MoAs were beliefs about capabilities (nine positive associations) and beliefs about consequences (six positive associations). Other commonly reported positive determinants of being active were emotion (69, 86), intentions (69, 78), and self-image (61, 68). Positive associations with being active were also observed in relation to reinforcement and goals (67, 69), subjective norms (78), values (68), and perceived susceptibility/vulnerability (61). A negative association between motivation and attitudes toward the behaviour and being active was reported in one study (63). Additionally a large UK study of people with mixed SMI reported no significant association between attitudes toward the behaviour and being active and (68). There was similarly no evidence that social/professional role and identity was a significant determinant of being active (69).
Two cross-sectional studies reported positive associations between emotion and reducing risks associated with smoking and diabetic foot problems (69, 71), and one prospective cohort study reported positive associations between emotion and reducing risk of smoking (81). Goals were negatively associated with reducing risks in one study (69). Cross-sectional data from one study showed no significant association between reinforcement, beliefs about consequences, intention, optimism, and social/professional role identity and reducing risks behaviours (69). Additionally longitudinal data from one prospective cohort study showed no significant association between motivation or self-image and reducing risks (87).
No positive associations were reported for links between determinants of taking medications. All observations were drawn from one cross-sectional study (69). Goals were negatively associated with taking diabetes medication. No significant associations were reported for reinforcement, beliefs about consequence, intentions, optimism, and social/professional role identity and taking medications.
There was no evidence found for links between AADE-7 self-management behaviours and these MoAs: norms, needs, social learning/imitation, feedback processes, and general attitudes/beliefs.
Summary of Findings for Motivation
The certainty of evidence for associations between MoAs and AADE-7 health behaviours within the Motivation domain was generally rated as moderate, but some evidence for positive associations was drawn from studies with low and very low ratings. The bulk of the evidence about determinants of behaviours was captured within this domain, with 44 links between four behaviours (healthy eating; being active; reducing risks; monitoring) and 11 MoAs being reported as positive. Results for being active and healthy eating clustered around beliefs about capabilities and beliefs about consequences. Goals and intentions were also linked three times with these behaviours. There was less inconclusive evidence within this domain with only four studies reporting no associations across four behaviours. Negative associations were reported for motivation (being active), goals (taking medication; monitoring; reducing risks, and attitude toward the behaviour (being active), but these findings were reported in just two studies.
Discussion
Using the novel MoA framework that comprehensively captures processes known to be associated with behaviour change, this review aimed to identify the determinants of self-management behaviours that underpin physical health in adults with SMI. The bulk of the evidence for associations between MoAs and self-management behaviours clustered around the super-ordinate Motivation domain in the COM-B framework. This finding lends further empirical support to the proposition that Motivation (which includes reflective and automatic processes) sits at the centre of the COM-B model and mediates behaviour via Capability and Opportunity (88). In keeping with the expert consensus exercise that mapped MoAs with behaviour change techniques (39), our review showed that being active mostly operated through beliefs about capabilities and beliefs about consequences. This finding is also consistent with evidence that the COM-B constructs of psychological capability and reflective motivation predict moderate-to-vigorous physical activity in healthy adults (88). Reflective motivation also underscores intentions, self-image, and perceived risk or perceived susceptibility which were also shown to be positively associated with being active in people with SMI alone and people with SMI and diabetes.
Outside of the capability and motivation constructs we also showed that environmental context and resources were important determinants of being active. Previous reviews have shown that lower self-efficacy and social isolation are correlated with lower physical activity participation in people with schizophrenia (89) and bipolar disorder (90). We found that physical activity in people with SMI is reported to be more frequent in those who are employed than unemployed. Social support from friends might also be important in promoting engagement with physical activity in people with SMI. However, access to employment and social support is likely to be closely linked with an individual's experience of SMI, as people who are experiencing low mood or acute psychosis (91), and who do not adequately respond to treatment (92), are less likely to access social support and employment (93).
There was less evidence and less consistency across available evidence about determinants of other self-management behaviours. Ten MoAs were linked with healthy eating, but none were reported more than once. It is worth noting that memory, attention, and decision processes, and behavioural regulation were negatively associated with healthy eating in people with SMI and diabetes. Both these MoAs include higher level cognitive processing that some people with SMI might find challenging. Cognitive deficits associated with attention and working memory are considered a central feature of schizophrenia (94). These deficits can make it difficult for people with schizophrenia to encode and arrange information, making self-evaluative tasks that require attention to multiple streams and sources of information and feedback difficult.
Reducing risks, monitoring, and taking medication are critical behaviours to self-managing long-term conditions, and this is especially the case in the context of SMI. We identified four studies of self-management in people with diabetes and SMI. Lower diabetes related distress was associated with less smoking and more frequent blood glucose monitoring among people with SMI and diabetes. People with SMI are three times as likely as the general population to smoke (95) and are more likely to become nicotine dependent and develop smoking related illnesses (96). Furthermore, people with SMI commonly hold the belief that smoking relieves their depression and anxiety (97). There is good evidence that bespoke smoking cessation interventions that include behavioural support from mental health practitioners and pharmacological therapies can help people with SMI to quit smoking and that such approaches are not detrimental to mental health (98). The role of emotion in determining engagement with self-management behaviours suggests that managing mood, and symptoms of SMI, could be important to successful behaviour change such as reducing risks of smoking. The prevalence of depression is about 40% in people with schizophrenia and is known to negatively affect quality of life, psychosocial functioning, and medication adherence (99). A meta-analysis by Firth et al. of motivators and barriers to physical activity in SMI reported the most important motivators were losing weight, improving mood and reducing stress. It found barriers were related to mental health symptoms such as depression and stress (100). The ability to self-manage emotional well-being is captured by the healthy coping behaviour in the AADE-7 framework. However, we did not identify any studies that measured associations between determinants and healthy coping, possibly because our focus was mainly on determinants of physical health behaviours. However, healthy coping may be an important determinant of physical health behaviours, as the revised version of the AADE-7 framework places healthy coping at the centre of this self-management model on the basis that a positive attitude toward diabetes and self-management is critical to the mastery of the other six behaviours (48). Additionally, qualitative research has highlighted that people with SMI use unhealthy coping strategies, such as smoking (101), eating unhealthy foods (102), drinking alcohol and using illicit substances (103), to cope with the symptoms of mental illness (21) Going forwards, there is scope to better understand how the promotion of healthy coping in people with SMI might underpin successful engagement with other AADE-7 self-management behaviours associated with good health outcomes.
We also did not identify much evidence about what determines medication taking, but there was some signal that environmental context in the form of access to health services might play an important role in driving this behaviour among people with SMI and diabetes. Adherence to oral hypoglycaemic medication is known to be higher among adults with diabetes who take three or more other medications and have more frequent physical health checks (104). In the UK, primary care has been incentivised to offer physical health checks to people with SMI with the potential to improve the quality of care (105). However, in recent years many of these physical health indicators have been removed and the impact of this on people with SMI is unknown (106). Further research about which MoAs are likely to support people with SMI and long-term conditions to engage with health services is warranted. Here, the perspectives of health professionals and carers might be insightful as there may be some mechanisms that people with SMI are less likely to self-report (107). Furthermore, by focusing on evidence originating from people with SMI alone, the relationship between self-management and the organisation and delivery of care may be overlooked (87).
Despite there being good evidence for how health behaviour models might explain physical activity in the general population, few behaviour change interventions used in people with SMI are underpinned by theory. Only nine out of 32 studies included in a systematic review of behaviour change interventions to promote physical activity in people with SMI were based on theory (11). Social cognitive theory and self-determination theory accounted for over half of those studies that did use theory. Furthermore, only three of the 11 studies that reported positive outcomes for physical activity used theory, drawing on social cognitive theory, and in particular self-efficacy theory, and acceptance and commitment theory. Self-efficacy and intention of physical activity have previously been shown to be a determinant of physical activity in people with SMI and depression (108), but in people with schizophrenia alone there is no evidence that trans-theoretical model mediators of change, such as exercise self-efficacy, are predicative of physical activity (109). Moreover, the majority of intervention studies that aim to increase physical activity in people with SMI have failed to target motivation for physical activity. Studies that have attempted to incorporate motivational techniques within interventions have observed no change in physical activity in people with SMI, pointing to the need for the systematic appraisal of the theoretical determinants of motivation for behaviour change in people with SMI (110).
Strengths and Limitations
A major strength of this systematic review is that it has operationalised the novel MoA framework using the COM-B model, possibly for the first time, to synthesise published evidence about links between determinants of self-management behaviours in people with SMI, including people with SMI and diabetes. The strengths of the MoA framework stem from the fact that it is based on the result of evidence synthesis and expert consensus, with a series of subsequent triangulation studies that sought to integrate the previous findings quantitatively and through expert consensus. This approach has resulted in evidence that builds upon the previous BCT Taxonomy V1 (36) and provides evidence of 1,456 BCT–MoA links, with the nature of the link (link/non-link/inconclusive) and type of evidence available in a heatmap format in the web-based Theory and Technique Tool (41). This work is part of a broader effort toward an ontology of human behaviour change (111–113), that is extending into intervention source and intervention mode of delivery (114). As such, the MoA Framework explicitly offers the benefits of an ontological approach that links intervention content to behaviour change techniques. This information is key for both systematic reviewers and intervention developers seeking to inform and or evaluate intervention development (43). Our review identified evidence of associations between AADE-7 health behaviours and all 14 domains of the TDF, but we also found evidence of associations for seven additional determinants that have been proposed as part of the MoA framework. This expands the scope of mapping MoAs to BCTs to change target behaviours and affect clinical outcomes, thus supporting the utility of this extended framework over and above the TDF alone.
We did not find studies of people with other long-term conditions so we cannot be sure this evidence extends beyond diabetes. Methodological strengths of the review include independent assessment of study eligibility by two reviewers and checking of data extraction and quality appraisal by a second reviewer. We conducted comprehensive searches but it is possible some evidence was missed through exclusion of conference abstracts and dissertations and a top-up search was conducted in only two databases.
We did not rate quality of included studies based on sample size. Nor did we exclude studies that reported smaller sample sizes. There is little empirical evidence that sample size drives risk of bias and smaller studies can still make a significant contribution to innovative and translational research (115). Our review aimed to identify all relevant evidence about the association between MoAs and physical health self-management behaviours, including from smaller studies. This approach offered greater opportunities to synthesise findings across multiple studies and minimised reporting bias about how associations between determinants and self-management behaviours clustered around particular MoAs. Additionally, excluding studies with smaller samples might lose information about important sub-groups, including those with SMI and diabetes.
Using the MoA framework can make it difficult to maintain specificity in how determinants are identified, especially among those existing within broader domains such as environmental context and resources, with implications for the appropriateness of subsequent selection of behaviour change techniques. More descriptive and nuanced data about whether determinants acted as barriers or motivators could also have been lost through the methods used, pointing to the need for qualitative studies about drivers of self-management behaviours in people with SMI. Additionally, the framework does not describe relationships between mechanisms established by social cognition models of behaviour and behaviour change (116). Hypothesised links, such as between perceptions, cues and intentions, can be overlooked by amalgamating theories into an integrative framework. However, MoAs are accessible to an interdisciplinary audience and can be organised using the COM-B system to aid understanding of their similarities and differences (33). Nevertheless, use of the MoAs in conjunction with the COM-B system creates overlaps (such as motivation within motivation) and two MoAs (Social Learning/Imitation and Behavioural Cueing) belong to more than one of the three overarching COM-B domains. The new MoAs are less clearly specified and inclusive than MoAs that originated in the TDF, which might account for why the majority of evidence fell within domains that were previously captured by the TDF. Further specification of the MoAs, particularly those that were not previously described in the TDF and which have clear links to social cognition models would make coding and application of evidence arising from evidence synthesis more accessible and feasible. An additional limitation of the MoA framework is that it does not account for how symptoms and health status can impact on a person's ability to engage in behaviour change. Our review is therefore unable to discern how psychiatric symptoms might affect engagement in behaviour change interventions in people with SMI.
We assessed the strength and direction of associations using conventional measures of statistical significance for univariate analyses that assessed the relationship between MoAs and self-management behaviours. This approach might limit the robustness of the synthesis as tests of significance and non-significance are dependent on a range of factors such as sample size or quality which is not captured using these methods. Furthermore, many of the included studies had small sample sizes that precluded the use of multivariate regression analyses that would offer adjusted and more accurate assessments of predictors of self-management behaviours.
A further limitation of the review is that it included mainly moderate to low quality cross-sectional evidence that cannot attribute causality, but this was partly a result of excluding intervention studies to avoid including associations between determinants and behaviours that had been modified by behaviour change techniques. This approach effectively restricted the evidence base to single group cohort designs. Most of the included studies did not use valid measures of behaviour. This was especially true for physical activity. Only one study used an accelerometer to objectively measure activity but the small sample size precludes drawing firm conclusions. There were also studies which compared SMI groups to non-SMI control groups and only the SMI group data could be extracted from these studies. It was not always straightforward to extract and map behavioural determinants but mapping to MoAs was performed by researchers with past experience of applying the framework to evidence of behavioural determinants in SMI groups. We enhanced the internal validity of this process by consulting linked evidence, such as qualitative studies, to help pinpoint the most appropriate MoA, with a second reviewer checking all allocation of evidence to MoAs.
Implications for Research and Intervention Development
Our heat-map matrix of MoAs and self-management behaviours, organised under the broader COM-B model of behaviour change, allows for easier identification and possible adaptation of candidate behaviour change techniques using existing resources such as the online theory and techniques tool (117). Using this tool, we can map MoAs that appear to be important determinants of health behaviours in people with SMI to BCTs with evidential links, thereby informing the next phase of work to develop interventions to support self-management of physical health in people with SMI. By way of example, beliefs about consequences, beliefs about capabilities, environmental resources and context, emotion, intention, and motivation were MoAs that were most commonly associated with AADE-7 health behaviours. Based on the theory and techniques tool these six MoAs are linked with 28 BCTs that are organised under 12 super ordinate categories in the Behaviour Change Taxonomy v1 (36). Four of these BCTs are linked to more than one MoA suggesting that there are opportunities for targeting multiple MoAs with single BCTs.
Feedback and monitoring are among the BCTs linked to the MoAs that we identified as being associated with health behaviours under the Motivation domain of the COM-B. This finding tallies with the results of the STEPWISE process evaluation which showed that participants who wanted to lose weight wanted closer monitoring and healthcare professionals wanted to monitor weight outcomes too, but such a focus on monitoring lay outside the scope of the intervention. Going forwards, the advent of wearable technology to objectively measure physical activity, behaviour change applications for smartphones, and devices that allow continuous glucose monitoring are likely to transform the capacity of behaviour change interventions to facilitate monitoring. There is evidence that the use of wearable technology and digital applications are acceptable among adults who take part in facilitated and remotely delivered behaviour change interventions to reduce the risk of long-term conditions (118). The relevance of such approaches is, however, untested in people with SMI and future trials are needed to assess feasibility and acceptability of the use of such technology in the delivery and assessment of behaviour change interventions in these populations.
Conclusion
This review provides an evidential basis for the development of appropriate and theory-based behaviour change interventions for managing physical health in adults with SMI. We synthesised evidence about 21 determinants of physical health self-management behaviours known to be important in people with SMI and people with SMI and a long-term condition. Organisation of evidence within the MoA framework facilitates the identification of behaviour change techniques with hypothesised links to determinants. Many of these determinants overlap and stem from reflective and automatic motivational processes. Critical determinants for being active and healthy eating were beliefs about capabilities and beliefs about consequences. There was less evidence about what determines other self-management behaviours but emotion and environmental context and resources appear to be important determinants of reducing risks and taking medications. The next phase of research and development should involve drawing up a shortlist of candidate BCTs and the involvement of healthcare professionals and people with lived experience of SMI to support decisions about how they are delivered using methods such as expert consensus and co-design.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
NS, JT, PC, EP, IK, CK, SA, JW, and JL wrote the protocol. CK, JT, PC, SA, EP, JL, AB-K, BY, JBr, CC, and IK screened titles and abstracts. BY, AB-K, JBr, and CC screened full text records. CC, JBr, PC, AB-K, BY, and JT assessed quality of included studies. PC wrote the first complete draft of the manuscript. All authors edited the manuscript for substantive intellectual content.
Author Disclaimer
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NHS, NIHR, or the Department of Health and Social Care. URKI does not necessarily endorse the views expressed by the authors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
Funding. This paper reports work undertaken as part of DIAMONDS, which was funded by the National Institute for Health Research under its Programme Grants for Applied Research (project number RP-PG-1016-20003). PC was partly funded by the UK Research and Innovation Closing the Gap Network+ (ES/S004459/1) and the NIHR Applied Research Collaboration Yorkshire and Humber.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.723962/full#supplementary-material
References
- 1.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. (2015) 72:334–41. 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13:153–60. 10.1002/wps.20128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Management of Physical Health Conditions in Adults With Severe Mental Disorders. Geneva: World Health Organization; (2018). [PubMed] [Google Scholar]
- 4.NHS Digital . NHS Outcomes Framework Indicators. (2020). Available from: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-outcomes-framework/may-2020
- 5.Hayes JF, Marston L, Walters K, King MB, Osborn DPJ. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000–2014. Br J Psychiatry. (2017) 211:175–81. 10.1192/bjp.bp.117.202606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. (2017) 16:163–80. 10.1002/wps.20420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vancampfort D, Wampers M, Mitchell AJ, Correll CU, De Herdt A, Probst M, et al. A meta-analysis of cardio-metabolic abnormalities in drug naive, first-episode and multi-episode patients with schizophrenia versus general population controls. World Psychiatry. (2013) 12:240–50. 10.1002/wps.20069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. (2011) 10:52–77. 10.1002/j.2051-5545.2011.tb00014.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allegrante JP, Wells MT, Peterson JC. Interventions to support behavioral self-management of chronic diseases. Annu Rev Public Health. (2019) 40:127–46. 10.1146/annurev-publhealth-040218-044008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. (2015) 45:1343–61. 10.1017/S0033291714003110 [DOI] [PubMed] [Google Scholar]
- 11.Ashdown-Franks G, Williams J, Vancampfort D, Firth J, Schuch F, Hubbard K, et al. Is it possible for people with severe mental illness to sit less and move more? A systematic review of interventions to increase physical activity or reduce sedentary behaviour. Schizophr Res. (2018) 202:3–16. 10.1016/j.schres.2018.06.058 [DOI] [PubMed] [Google Scholar]
- 12.Naslund JA, Whiteman KL, McHugo GJ, Aschbrenner KA, Marsch LA, Bartels SJ. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. (2017) 47:83–102. 10.1016/j.genhosppsych.2017.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Speyer H, Christian Brix Norgaard H, Birk M, Karlsen M, Storch Jakobsen A, Pedersen K, et al. The CHANGE trial: no superiority of lifestyle coaching plus care coordination plus treatment as usual compared to treatment as usual alone in reducing risk of cardiovascular disease in adults with schizophrenia spectrum disorders and abdominal obesity. World Psychiatry. (2016) 15:155–65. 10.1002/wps.20318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osborn D, Burton A, Hunter R, Marston L, Atkins L, Barnes T, et al. Clinical and cost-effectiveness of an intervention for reducing cholesterol and cardiovascular risk for people with severe mental illness in English primary care: a cluster randomised controlled trial. Lancet Psychiatry. (2018) 5:145–54. 10.1016/S2215-0366(18)30007-5 [DOI] [PubMed] [Google Scholar]
- 15.Holt RIG, Gossage-Worrall R, Hind D, Bradburn MJ, McCrone P, Morris T, et al. Structured lifestyle education for people with schizophrenia, schizoaffective disorder and first-episode psychosis (STEPWISE): randomised controlled trial. Br J Psychiatry. (2019) 214:63–73. 10.1192/bjp.2018.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vancampfort D, Firth J, Schuch FB, Rosenbaum S, Mugisha J, Hallgren M, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. (2017) 16:308–15. 10.1002/wps.20458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dipasquale S, Pariante CM, Dazzan P, Aguglia E, McGuire P, Mondelli V. The dietary pattern of patients with schizophrenia: a systematic review. J Psychiatr Res. (2013) 47:197–207. 10.1016/j.jpsychires.2012.10.005 [DOI] [PubMed] [Google Scholar]
- 18.Jackson JG, Diaz FJ, Lopez L, de Leon J. A combined analysis of worldwide studies demonstrates an association between bipolar disorder and tobacco smoking behaviors in adults. Bipolar Disord. (2015) 17:575–97. 10.1111/bdi.12319 [DOI] [PubMed] [Google Scholar]
- 19.Correll CU, Schooler NR. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr Dis Treat. (2020) 16:519–34. 10.2147/NDT.S225643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Storch Jakobsen A, Speyer H, Nørgaard HCB, Hjorthøj C, Krogh J, Mors O, et al. Associations between clinical and psychosocial factors and metabolic and cardiovascular risk factors in overweight patients with schizophrenia spectrum disorders – baseline and two-years findings from the CHANGE trial. Schizophr Res. (2018) 199:96–102. 10.1016/j.schres.2018.02.047 [DOI] [PubMed] [Google Scholar]
- 21.Wardig RE, Bachrach-Lindstrom M, Foldemo A, Lindstrom T, Hultsjo S. prerequisites for a healthy lifestyle-experiences of persons with psychosis. Issues Ment Health Nurs. (2013) 34:602–10. 10.3109/01612840.2013.790525 [DOI] [PubMed] [Google Scholar]
- 22.Bellass S, Lister J, Kitchen C, Kramer L, Alderson S, Doran T, et al. Living with diabetes alongside a severe mental illness: a qualitative exploration with people with severe mental illness, family members and healthcare staff. Diabet Med. (2021) 38:e14562. 10.1111/dme.14562 [DOI] [PubMed] [Google Scholar]
- 23.Citrome L, Holt RI, Walker DJ, Hoffmann VP. Weight gain and changes in metabolic variables following olanzapine treatment in schizophrenia and bipolar disorder. Clin Drug Investig. (2011) 31:455–82. 10.2165/11589060-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 24.De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. (2011) 8:114–26. 10.1038/nrendo.2011.156 [DOI] [PubMed] [Google Scholar]
- 25.Ohaeri JU, Akanji AO. Metabolic syndrome in severe mental disorders. Metab Syndr Relat Disord. (2011) 9:91–8. 10.1089/met.2010.0053 [DOI] [PubMed] [Google Scholar]
- 26.Morrison P, Meehan T, Stomski NJ. living with antipsychotic medication side-effects: the experience of australian mental health consumers. Int J Ment Health Nurs. (2015) 24:253–61. 10.1111/inm.12110 [DOI] [PubMed] [Google Scholar]
- 27.Shiers D, Bradshaw T, Campion J. Health inequalities and psychosis: time for action. Br J Psychiatry. (2015) 207:471–3. 10.1192/bjp.bp.114.152595 [DOI] [PubMed] [Google Scholar]
- 28.Vick B, Jones K, Mitra S. Poverty and severe psychiatric disorder in the U.S.: evidence from the medical expenditure panel survey. J Ment Health Policy Econ. (2012) 15:83–96. [PubMed] [Google Scholar]
- 29.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. (2010) 1186:125–45. 10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]
- 30.Grigoroglou C, Munford L, Webb RT, Kapur N, Ashcroft DM, Kontopantelis E. Prevalence of mental illness in primary care and its association with deprivation and social fragmentation at the small-area level in England. Psychol Med. (2020) 50:293–302. 10.1017/S0033291719000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nielsen L, Riddle M, King JW, Team NIHSoBCI, Aklin WM, Chen W, et al. The NIH science of behavior change program: transforming the science through a focus on mechanisms of change. Behav Res Ther. (2018) 101:3–11. 10.1016/j.brat.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. (2008) 337:a1655. 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Czajkowski SM, Powell LH, Adler N, Naar-King S, Reynolds KD, Hunter CM, et al. From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. (2015) 34:971–82. 10.1037/hea0000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larsen KR, Michie S, Hekler EB, Gibson B, Spruijt-Metz D, Ahern D, et al. Behavior change interventions: the potential of ontologies for advancing science and practice. J Behav Med. (2017) 40:6–22. 10.1007/s10865-016-9768-0 [DOI] [PubMed] [Google Scholar]
- 36.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. (2013) 46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 37.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Safety Health Care. (2005) 14:26–33. 10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keyworth C, Epton T, Goldthorpe J, Calam R, Armitage CJ. Acceptability, reliability, and validity of a brief measure of capabilities, opportunities, and motivations (“COM-B”). Br J Health Psychol. (2020) 25:474–501. 10.1111/bjhp.12417 [DOI] [PubMed] [Google Scholar]
- 39.Connell LE, Carey RN, de Bruin M, Rothman AJ, Johnston M, Kelly MP, et al. Links between behavior change techniques and mechanisms of action: an expert consensus study. Ann Behav Med. (2019) 53:708–20. 10.1093/abm/kay082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carey RN, Connell LE, Johnston M, Rothman AJ, de Bruin M, Kelly MP, et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med. (2019) 53:693–707. 10.31234/osf.io/x5372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnston M, Carey RN, Bohlen LEC, Johnston DW, Rothman AJ, Bruin Md, et al. Development of an online tool for linking behavior change techniques and mechanisms of action based on triangulation of findings from literature synthesis and expert consensus. Transl Behav Med. (2020) 41:1049–65. 10.1093/tbm/ibaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hagger MS, Moyers S, McAnally K, McKinley LE. Known knowns and known unknowns on behavior change interventions and mechanisms of action. Health Psychol Rev. (2020) 14:199–212. 10.1080/17437199.2020.1719184 [DOI] [PubMed] [Google Scholar]
- 43.Johnson BT, Scott-Sheldon LA, Carey MP. Meta-synthesis of health behavior change meta-analyses. Am J Public Health. (2010) 100:2193–8. 10.2105/AJPH.2008.155200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Michie S, Johnston M. Theories and techniques of behaviour change: developing a cumulative science of behaviour change. Health Psychol Rev. (2012) 6:1–6. 10.1080/17437199.2012.65496426616119 [DOI] [Google Scholar]
- 45.DIAMONDS . Improving Diabetes Self-Managment for People With Severe Mental Illness. (2020). Available from: https://www.york.ac.uk/healthsciences/research/mental-health/projects/diamonds/ (accessed August 02, 2021).
- 46.Huber M, Knottnerus JA, Green L, Horst Hvd, Jadad AR, Kromhout D, et al. How should we define health? BMJ. (2011) 343:d4163. 10.1136/bmj.d4163 [DOI] [PubMed] [Google Scholar]
- 47.Peeples M, Tomky D, Mulcahy K, Peyrot M, Siminerio L. Evolution of the American Association of Diabetes Educators' diabetes education outcomes project. Diabetes Educ. (2007) 33:794–817. 10.1177/0145721707307615 [DOI] [PubMed] [Google Scholar]
- 48.American Association of Diabetes Educators . An effective model of diabetes care and education: revising the AADE7 Self-Care Behaviors((R)). Diabetes Educ. (2020) 46:139–60. 10.1177/0145721719894903 [DOI] [PubMed] [Google Scholar]
- 49.Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. (2020) 9:17. 10.1186/s13643-020-1274-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Coventry PA, Meader N, Melton H, Temple M, Dale H, Wright K, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLoS Med. (2020) 17:e1003262. 10.1371/journal.pmed.1003262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.OECD Country Classifications ,. (2018). Available from: http://www.oecd.org/tad/xcred/country-classification.htm (accessed August 02, 2021).
- 52.Covidence, Systematic Review Software Melbourne, Australia . Available from: www.covidence.org (accessed August 02, 2021).
- 53.National Institute for Health and Care Excellence . Methods for the Development of NICE Public Health Guidance. 3rd ed (2012). Available from: http://nice.org.uk/process/pmg4 (accessed August 02, 2021). [PubMed] [Google Scholar]
- 54.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arbour-Nicitopoulos KP, Duncan MJ, Remington G, Cairney J, Faulkner GE. The utility of the health action process approach model for predicting physical activity intentions and behavior in schizophrenia. Front Psychiatry. (2017) 8:135. 10.3389/fpsyt.2017.00135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ashton M, Rigby A, Galletly C. what do 1000 smokers with mental illness say about their tobacco use? Aust N Z J Psychiatry. (2013) 47:631–6. 10.1177/0004867413482008 [DOI] [PubMed] [Google Scholar]
- 57.Berti L, Bonfioli E, Chioffi L, Morgante S, Mazzi MA, Burti L. Lifestyles of patients with functional psychosis compared to those of a sample of the regional general population: findings from a study in a community mental health service of the Veneto region, Italy. Community Ment Health J. (2018) 54:1050–6. 10.1007/s10597-017-0223-7 [DOI] [PubMed] [Google Scholar]
- 58.Bezyak JL, Berven NL, Chan F. stages of change and physical activity among individuals with severe mental illness. Rehabil Psychol. (2011) 56:182–90. 10.1037/a0024207 [DOI] [PubMed] [Google Scholar]
- 59.Campion G, Francis V, Preston A, Wallis A. Health behaviour and motivation to change. Ment Health Nurs. (2005) 25:12–5. [Google Scholar]
- 60.Dickerson F, Bennett M, Dixon L, Burke E, Vaughan C, Delahanty J, et al. smoking cessation in persons with serious mental illnesses: the experience of successful quitters. Psychiatr Rehabil J. (2011) 34:311–6. 10.2975/34.4.2011.311.316 [DOI] [PubMed] [Google Scholar]
- 61.Faulkner G, Taylor A, Munro S, Selby P, Gee C. the acceptability of physical activity programming within a smoking cessation service for individuals with severe mental illness. Patient Educ Couns. (2007) 66:123–6. 10.1016/j.pec.2006.11.003 [DOI] [PubMed] [Google Scholar]
- 62.Filia SL, Baker AL, Richmond R, Castle DJ, Kay-Lambkin FJ, Sakrouge R, et al. Health behaviour risk factors for coronary heart disease (CHD) in smokers with a psychotic disorder: baseline results. Ment Health Subst Use. (2011) 4:158–71. 10.1080/17523281.2011.555088 [DOI] [Google Scholar]
- 63.Gorczynski P, Vancampfort D, Patel H. Evaluating correlations between physical activity, psychological mediators of physical activity, and negative symptoms in individuals living with psychosis and diabetes. Psychiatr Rehabil J. (2018) 41:153–6. 10.1037/prj0000298 [DOI] [PubMed] [Google Scholar]
- 64.Kelly DL, Raley HG, Lo S, Wright K, Liu F, McMahon RP, et al. perception of smoking risks and motivation to quit among nontreatment-seeking smokers with and without schizophrenia. Schizophr Bull. (2012) 38:543–51. 10.1093/schbul/sbq124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Klingaman EA, Viverito KM, Medoff DR, Hoffmann RM, Goldberg RW. Strategies, barriers, and motivation for weight loss among veterans living with schizophrenia. Psychiatr Rehabil J. (2014) 37:270–6. 10.1037/prj0000084 [DOI] [PubMed] [Google Scholar]
- 66.Kreyenbuhl J, Leith J, Medoff DR, Fang L, Dickerson FB, Brown CH, et al. a comparison of adherence to hypoglycemic medications between type 2 diabetes patients with and without serious mental illness. Psychiatry Res. (2011) 188:109–14. 10.1016/j.psychres.2011.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Matthews E, Cowman M, Brannigan M, Sloan D, Ward PB, Denieffe S. Examining the barriers to physical activity between active and inactive people with severe mental illness in Ireland. Mental Health Phys Act. (2018) 15:139–44. 10.1016/j.mhpa.2018.10.003 [DOI] [Google Scholar]
- 68.Mishu MP, Peckham EJ, Heron PN, Tew GA, Stubbs B, Gilbody S. Factors associated with regular physical activity participation among people with severe mental ill health. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:887–95. 10.1007/s00127-018-1639-2 [DOI] [PubMed] [Google Scholar]
- 69.Mulligan K, McBain H, Lamontagne-Godwin F, Chapman J, Flood C, Haddad M, et al. barriers to effective diabetes management - a survey of people with severe mental illness. BMC Psychiatry. (2018) 18:165. 10.1186/s12888-018-1744-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Muralidharan A, Klingaman EA, Molinari V, Goldberg RW. Perceived barriers to physical activity in older and younger veterans with serious mental illness. Psychiatr Rehabil J. (2018) 41:67–71. 10.1037/prj0000245 [DOI] [PubMed] [Google Scholar]
- 71.Ogawa M, Miyamoto Y, Kawakami N. factors associated with glycemic control and diabetes self-care among outpatients with schizophrenia and type 2 diabetes. Arch Psychiatr Nurs. (2011) 25:63–73. 10.1016/j.apnu.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 72.Peckham E, Bradshaw TJ, Brabyn S, Knowles S, Gilbody S. exploring why people with smi smoke and why they may want to quit: baseline data from the scimitar rct. J Psychiatr Ment Health Nurs. (2016) 23:282–9. 10.1111/jpm.12241 [DOI] [PubMed] [Google Scholar]
- 73.Prochaska JJ, Reyes RS, Schroeder SA, Daniels AS, Doederlein A, Bergeson B. an online survey of tobacco use, intentions to quit, and cessation strategies among people living with bipolar disorder. Bipolar Disord. (2011) 13:466–73. 10.1111/j.1399-5618.2011.00944.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Romain AJ, Abdel-Baki A. using the transtheoretical model to predict physical activity level of overweight adults with serious mental illness. Psychiatry Res. (2017) 258:476–80. 10.1016/j.psychres.2017.08.093 [DOI] [PubMed] [Google Scholar]
- 75.Roosenschoon BJ, Kamperman AM, Deen ML, Weeghel JV, Mulder CL. Determinants of clinical, functional and personal recovery for people with schizophrenia and other severe mental illnesses: a cross-sectional analysis. PLoS ONE. (2019) 14:e0222378. 10.1371/journal.pone.0222378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shor R, Shalev A. barriers to involvement in physical activities of persons with mental illness. Health Promot Internation. (2016) 31:116–23. 10.1093/heapro/dau078 [DOI] [PubMed] [Google Scholar]
- 77.Spivak S, Cullen BA, Eaton W, Nugent KL, Rodriguez K, Mojtabai R. Delays in seeking general medical services and measurable abnormalities among individuals with serious mental illness. Psychiatr Serv. (2018) 69:479–82. 10.1176/appi.ps.201700327 [DOI] [PubMed] [Google Scholar]
- 78.Twyford J, Lusher J. Determinants of exercise intention and behaviour among individuals diagnosed with schizophrenia. J Ment Health. (2016) 25:303–9. 10.3109/09638237.2015.1124399 [DOI] [PubMed] [Google Scholar]
- 79.Vancampfort D, De Hert M, Vansteenkiste M, De Herdt A, Scheewe TW, Soundy A, et al. the importance of self-determined motivation towards physical activity in patients with schizophrenia. Psychiatry Res. (2013) 210:812–8. 10.1016/j.psychres.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 80.Vancampfort D, De Hert M, Broderick J, Lederman O, Firth J, Rosenbaum S, et al. Is autonomous motivation the key to maintaining an active lifestyle in first-episode psychosis? Early Interv Psychiatry. (2018) 12:821–7. 10.1111/eip.12373 [DOI] [PubMed] [Google Scholar]
- 81.Vermeulen J, Schirmbeck F, Blankers M, van Tricht M, van den Brink W, de Haan L, et al. Smoking, symptoms, and quality of life in patients with psychosis, siblings, and healthy controls: a prospective, longitudinal cohort study. Lancet Psychiatry. (2019) 6:25–34. 10.1016/S2215-0366(18)30424-3 [DOI] [PubMed] [Google Scholar]
- 82.Zechner MR, Gill KJ. predictors of physical activity in persons with mental illness: testing a social cognitive model. Psychiatr Rehabil J. (2016) 39:321–7. 10.1037/prj0000191 [DOI] [PubMed] [Google Scholar]
- 83.Bandura A. Toward a psychology of human agency. Perspect Psychol Sci. (2006) 1:164–80. 10.1111/j.1745-6916.2006.00011.x [DOI] [PubMed] [Google Scholar]
- 84.Godin G, Shephard RJ. A simple method to assess exercise behaviour in the community. Can J Appl Sport Sci. (1985) 10:141–6. [PubMed] [Google Scholar]
- 85.Azjen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behaviour. J Appl Soc Psychol. (2002) 32:665–83. 10.1111/j.1559-1816.2002.tb00236.x [DOI] [Google Scholar]
- 86.Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ. (2015) 350:g7714. 10.1136/bmj.g7714 [DOI] [PubMed] [Google Scholar]
- 87.Lawrence D, Kisely S. Inequalities in healthcare provision for people with severe mental illness. J Psychopharmacol. (2010) 24(4 Suppl.):61–8. 10.1177/1359786810382058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Howlett N, Schulz J, Trivedi D, Troop N, Chater A. A prospective study exploring the construct and predictive validity of the COM-B model for physical activity. J Health Psychol. (2019) 24:1378–91. 10.1177/1359105317739098 [DOI] [PubMed] [Google Scholar]
- 89.Vancampfort D, Knapen J, Probst M, Scheewe T, Remans S, De Hert M. a systematic review of correlates of physical activity in patients with schizophrenia. Acta Psychiatr Scand. (2012) 125:352–62. 10.1111/j.1600-0447.2011.01814.x [DOI] [PubMed] [Google Scholar]
- 90.Vancampfort D, Correll CU, Probst M, Sienaert P, Wyckaert S, De Herdt A, et al. a review of physical activity correlates in patients with bipolar disorder. J Affect Disord. (2013) 145:285–91. 10.1016/j.jad.2012.07.020 [DOI] [PubMed] [Google Scholar]
- 91.Chau AKC, Zhu C, So SH-W. Loneliness and the psychosis continuum: a meta-analysis on positive psychotic experiences and a meta-analysis on negative psychotic experiences. Int Rev Psychiatry. (2019) 31:471–90. 10.1080/09540261.2019.1636005 [DOI] [PubMed] [Google Scholar]
- 92.Catty J, Lissouba P, White S, Becker T, Drake RE, Fioritti A, et al. Predictors of employment for people with severe mental illness: results of an international six-centre randomised controlled trial. Br J Psychiatry. (2008) 192:224–31. 10.1192/bjp.bp.107.041475 [DOI] [PubMed] [Google Scholar]
- 93.Alvarez-Jimenez M, Gleeson J, Henry L, Harrigan S, Harris M, Killackey E, et al. Road to full recovery: longitudinal relationship between symptomatic remission and psychosocial recovery in first-episode psychosis over 7.5 years. Psychol Med. (2012) 42:595. 10.1017/S0033291711001504 [DOI] [PubMed] [Google Scholar]
- 94.Kuipers E, Garety P, Fowler D, Freeman D, Dunn G, Bebbington P. Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms. Schizophr Bull. (2006) 32(Suppl. 1):S24–31. 10.1093/schbul/sbl014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Szatkowski L, McNeill A. Diverging trends in smoking behaviors according to mental health status. Nicotine Tobacco Res. (2014) 17:356–60. 10.1093/ntr/ntu173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Szatkowski L, McNeill A. The delivery of smoking cessation interventions to primary care patients with mental health problems. Addiction. (2013) 108:1487–94. 10.1111/add.12163 [DOI] [PubMed] [Google Scholar]
- 97.Addington J, el-Guebaly N, Addington D, Hodgins D. Readiness to stop smoking in schizophrenia. Can J Psychiatry. (1997) 42:49–52. 10.1177/070674379704200107 [DOI] [PubMed] [Google Scholar]
- 98.Gilbody S, Peckham E, Bailey D, Arundel C, Heron P, Crosland S, et al. Smoking cessation for people with severe mental illness (SCIMITAR+): a pragmatic randomised controlled trial. Lancet Psychiatry. (2019) 6:379–90. 10.1016/S2215-0366(19)30047-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Conley RR, Ascher-Svanum H, Zhu B, Faries DE, Kinon BJ. The burden of depressive symptoms in the long-term treatment of patients with schizophrenia. Schizophr Res. (2007) 90:186–97. 10.1016/j.schres.2006.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. (2016) 46:2869–81. 10.1017/S0033291716001732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Trainor K, Leavey G. barriers and facilitators to smoking cessation among people with severe mental illness: a critical appraisal of qualitative studies. Nicotine Tob Res. (2017) 19:14–23. 10.1093/ntr/ntw183 [DOI] [PubMed] [Google Scholar]
- 102.Barre LK, Ferron JC, Davis KE, Whitley R. healthy eating in persons with serious mental illnesses: understanding and barriers. Psychiatr Rehabil J. (2011) 34:304–10. 10.2975/34.4.2011.304.310 [DOI] [PubMed] [Google Scholar]
- 103.Bradizza CM, Stasiewicz PR. Qualitative analysis of high-risk drug and alcohol use situations among severely mentally ill substance abusers. Addict Behav. (2003) 28:157–69. 10.1016/S0306-4603(01)00272-6 [DOI] [PubMed] [Google Scholar]
- 104.Horii T, Momo K, Yasu T, Kabeya Y, Atsuda K. Determination of factors affecting medication adherence in type 2 diabetes mellitus patients using a nationwide claim-based database in Japan. PLoS ONE. (2019) 14:e0223431. 10.1371/journal.pone.0223431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kontopantelis E, Olier I, Planner C, Reeves D, Ashcroft DM, Gask L, et al. Primary care consultation rates among people with and without severe mental illness: a UK cohort study using the Clinical Practice Research Datalink. BMJ Open. (2015) 5:e008650. 10.1136/bmjopen-2015-008650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Minchin M, Roland M, Richardson J, Rowark S, Guthrie B. Quality of care in the United Kingdom after removal of financial incentives. N Engl J Med. (2018) 379:948–57. 10.1056/NEJMsa1801495 [DOI] [PubMed] [Google Scholar]
- 107.Hassan S, Ross J, Marston L, Burton A, Osborn D, Walters K. Exploring how health behaviours are supported and changed in people with severe mental illness: a qualitative study of a cardiovascular risk reducing intervention in Primary Care in England. Br J Health Psychol. (2020) 25:428–51. 10.1111/bjhp.12415 [DOI] [PubMed] [Google Scholar]
- 108.Leas L, McCabe M. Health behaviors among individuals with schizophrenia and depression. J Health Psychol. (2007) 12:563–79. 10.1177/1359105307078162 [DOI] [PubMed] [Google Scholar]
- 109.Bassilios B, Judd F, Pattison P, Nicholas A, Moeller-Saxone K. Predictors of exercise in individuals with schizophrenia: a test of the transtheoretical model of behavior change. Clin Schizophr Relat Psychoses. (2015) 8:173–82, 82A. 10.3371/CSRP.BAJU.030113 [DOI] [PubMed] [Google Scholar]
- 110.Farholm A, Sorensen M. Motivation for physical activity and exercise in severe mental illness: a systematic review of intervention studies. Int J Ment Health Nurs. (2016) 25:194–205. 10.1111/inm.12214 [DOI] [PubMed] [Google Scholar]
- 111.Michie S, Thomas J, Johnston M, Aonghusa PM, Shawe-Taylor J, Kelly MP, et al. The human behaviour-change project: harnessing the power of artificial intelligence and machine learning for evidence synthesis and interpretation. Implement Sci. (2017) 12:121. 10.1186/s13012-017-0641-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Michie S, Johnston M, Rothman AJ, de Bruin M, Kelly MP, Carey RN, et al. Developing an evidence-based online method of linking behaviour change techniques and theoretical mechanisms of action: a multiple methods study. Health Serv Deliv Res. (2021) 9:1–167. 10.3310/hsdr09010 [DOI] [PubMed] [Google Scholar]
- 113.Michie S, West R, Finnerty AN, Norris E, Wright AJ, Marques MM, et al. Representation of behaviour change interventions and their evaluation: development of the upper level of the behaviour change intervention ontology. Wellcome Open Res. (2020) 5:123. 10.12688/wellcomeopenres.15902.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Marques MM, Carey RN, Norris E, Evans F, Finnerty AN, Hastings J, et al. Delivering behaviour change interventions: development of a mode of delivery ontology. Wellcome Open Res. (2020) 5:125. 10.12688/wellcomeopenres.15906.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bacchetti P, Deeks SG, McCune JM. Breaking free of sample size dogma to perform innovative translational research. Sci Transl Med. (2011) 3:87ps24. 10.1126/scitranslmed.3001628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Michie S, West R, Campbell R, Brown J, Gainforth H. ABC of Behaviour Change Theories. Sutton: Silverback Publishing; (2014). [Google Scholar]
- 117.The Human Behaviour Change Project . The Theory & Techniques Tool. (2019). Available from: https://theoryandtechniquetool.humanbehaviourchange.org/ (accessed August 02, 2021).
- 118.Coventry P, Bower P, Blakemore A, Baker E, Hann M, Li J, et al. Satisfaction with a digitally-enabled telephone health coaching intervention for people with non-diabetic hyperglycaemia. npj Dig Med. (2019) 2:5. 10.1038/s41746-019-0080-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.