Abstract
Background: Nipple discomfort inhibits breastfeeding goals, particularly between 0 and 8 weeks postpartum (PP), and yet the specific dermatologic entities that contribute to nipple soreness have not been clearly delineated. Moreover, there remains a lack of evidence-based guidelines for nipple symptoms and skin diseases.
Methods: A survey was distributed to 6–8-week PP women, 18–50 years of age, with an intent to exclusively or partially breastfeed (“at the breast” or “pump”). The study aimed to characterize nipple skin symptoms (pain and itching) and lesions (eczema, redness, cuts, or wounds) and any association between these nipple problems and past dermatologic history, breastfeeding outcomes, and the ability to meet her breastfeeding goals.
Results: Findings paralleled Centers for Disease Control and Prevention (CDC) statistics with a 25% decline in breastfeeding rates between birth, 86.3% (189), and 6–8 weeks PP, 64.5% (145). By 6–8 weeks PP, exclusive “formula” and “exclusive feeding at the breast” showed the largest increase (+16.4%) and decrease (−22.9%), respectively. Although no significant difference was found in comparison of nipple problems to feeding methods or skin history, women who reported pumping or PP redness/eczema had higher odds ratios of a change in feeding practice, history of eczema, and sensitive skin. Strong pumping intentions were also associated with the highest risk of unmet breastfeeding goals.
Conclusion: Regardless of feeding method, product, or provider use, PP nipple problems predominantly arose between 1 and 3 weeks PP. Clinical Trial Registration number 201901737.
Keywords: nipple dermatitis, nipple pain, postpartum, breastfeeding, pumping, lactation
Introduction
The stated intention to breastfeed is one of the strongest predictors of breastfeeding initiation, but the dynamic nature of breastfeeding is often affected by socioenvironmental factors and the experience itself.1 Nipple pain and skin abnormalities are a major prohibitive factor for achieving breastfeeding goals, particularly within the 1–8 week postpartum (PP) period.2–5 Previous studies have identified the prevalence of self-reported nipple symptoms (pain and itch) in PP women to be as high as 79% and self-reported nipple damage at 58%.6 Anecdotal evidence and self-reported data suggest several factors contributing to nipple soreness such as poor latch, low milk supply, flat or inverted nipples, mechanical stressors, infection, or exacerbations of inflammatory conditions (psoriasis or eczema).7,8 However, studies have not used discrete dermatologic entities to categorize the problem, thus also potentially limiting the ability to establish proper therapies. Topical products and medical devices (breast pumps, shells, or shields) are available over the counter (OTC), but they can inhibit the maternal-infant interaction and may even exacerbate pain.8–11 Second, there remains no clear, evidence-based guidelines regarding particular skin diseases of the nipple and their most effective treatment regimens, likely due to a lack and variability of data in current literature.
Although the majority of studies focus on infections of the nipple or breast tissue, the more prevalent complaints from breastfeeding include nipple dermatitis, fissures, pain, and itching.12,13 Comparisons between lanolin and other nipple products (all-purpose nipple ointment, warm/cold compresses, air drying, peppermint water, analgesics, and breast shields) have demonstrated equal effectiveness in reducing nipple pain and healing time, improving satisfaction and duration of breastfeeding.14–16 In a larger study by Dennis et al. in 2014 (656 PP women), no product superiority was observed when comparing glycerin pads, shells, lanolin, expressed milk, or ointment in treatment of nipple discomfort.13 Despite evaluating 656 women in a trial of five products (glycerin pads, shells, lanolin, expressed milk, or ointment), Dennis et al. reported insufficient evidence to conclude which product was superior in treating nipple discomfort. Rather, they noted all therapies “mild-to-moderately” reduced symptoms, and all women reported a general reduction in pain 7–10 days PP regardless of product used.13 A similar study was conducted by Morland-Schultz and Hill reporting no difference between topicals and commented on the dire need for early breastfeeding education, particularly anticipatory guidance regarding nipple pain.17 In contrast, Gungor et al. identified olive oil as the preferred PP nipple treatment when compared to lanolin.18
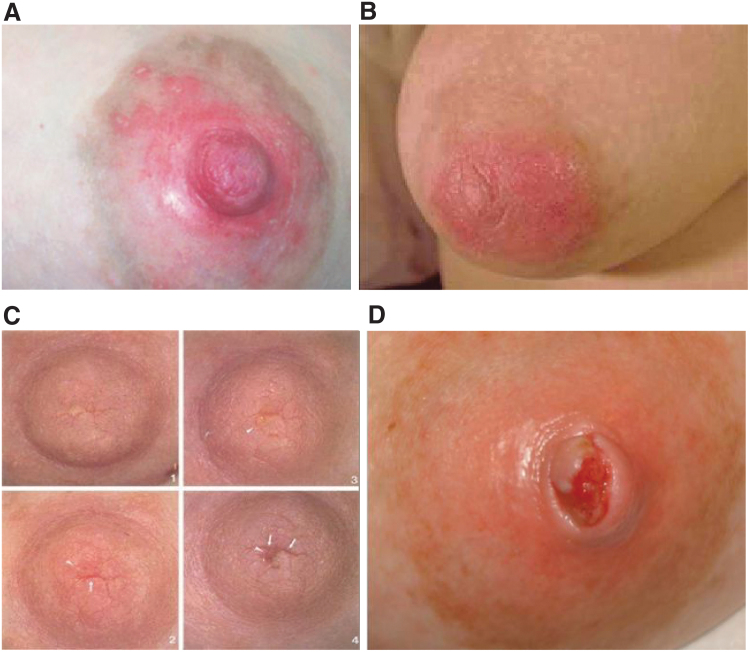
The purpose of this study was to characterize the incidence and risk factors for nipple symptoms (pain and itch) in 6–8 week PP women, and to characterize the incidence of self-reported skin entities (redness, eczema, cuts, and open wounds). It also aimed to evaluate any relationship between nipple skin symptoms/lesions (Fig. 1), dermatologic skin history, and breastfeeding outcomes. As secondary outcome measures, we sought to clarify which products are commonly utilized and which health care providers are primarily caring for this patient population.
FIG. 1.
Nipple skin lesions. (A) Redness. (B) Eczema (atopic dermatitis). (C) Cuts (fissures); five white arrows point to individual cuts/fissures. (D) Open wounds.
Methods
A review of literature was performed using the key phrases “nipple dermatitis,” “nipple pain,” “nipple itching,” “nipple soreness,” “breastfeeding,” “formula feeding,” “breast pumping,” and “nipple treatments” on the following databases: PubMed, CINAHL, and ClinicalKey. This search could not identify literature addressing maternal skin history, such as atopic dermatitis, psoriasis, or other chronic cutaneous disorders, in the context of breastfeeding difficulties.
A single-site cross-sectional study was performed using a 13-question, paper survey developed by the University of Iowa Hospitals and Clinics (UIHC) Departments of Dermatology, and Obstetrics and Gynecology. The project was reviewed and accepted by the UIHC Institutional Review Board (ID: 201901726).
The survey was distributed to our population of interest: 6–8 week PP mothers, 18–50 years of age, with expressed intention to exclusively or partially breastfeed. The study excluded non-English-speaking patients, females younger than 18 years or older than 50 years, and respondents outside the 6–8 week PP window. It also excluded patients unable to independently complete the questionnaire. In a 4-month recruitment period, the study aimed to survey 200 eligible participants, a goal achieved with 220 respondents.
Upon survey dissemination, consent was implied and participants were instructed to leave questions blank, which they did not wish to answer. Accordingly, patients were not excluded for lack of survey completion. All surveys remained anonymous and no chart review was performed for this study. Accordingly, no names, medical record numbers, or other identifiers were collected. Survey responses were documented in a secure database (REDCap). The REDCap platform is managed by the Institute for Clinical and Translational Science at the University of Iowa and access is limited to IRB-approved research team members.
Statistical analysis was performed using the latest software of SAS (9.4, University of Iowa Institute for Clinical and Translational Science) with a significance level set at p < 0.05. Demographic and survey data, compiled in the REDCap database, included both continuous and categorical variables. Fisher's exact test and Cohen's kappa coefficient were used to determine significance and measure of agreement, respectively, among pairs of categorical variables. Stratified variables were listed as a percentage with corresponding “n” number. In regard to feeding methods, the term “breastfeeding” corresponded to feeding “at the breast.” Subjects were asked about all types of feeding, including (1) exclusive breastfeeding, (2) breastfeeding with pumping and bottle feeding of expressed breast milk, (3) breastfeeding and/or pumping with formula supplementation, and (4) exclusive formula. “Intended” practices (breastfeeding, pumping, and/or formula) represented day 0, while “current” practices represented 6–8 weeks PP. For data analysis, we also defined “change” in feeding practices as any deviation at 6–8 weeks from intended (day 0) method. Odds ratios (OR) with a 95% confidence interval were applied to categorical values with a binomial distribution. We also defined “nipple symptoms” as nipple pain or itching, as well as “nipple skin lesions” as redness, eczema (atopic dermatitis), cuts (fissures), or open wounds of the nipple.
Results
Among 220 survey respondents, 219 met inclusion criteria for statistical analysis. Upon survey distribution (6–8 weeks PP), the average age of mothers and infants was 30.0 years and 48.4 ± 5.5 days, respectively. The majority of women, 84.5% (185), identified as “white, non-Hispanic” for their race and ethnicity and had previously breastfed one or more infants, 46.6% (102). Review of dermatologic medical history identified a predominance of environmental allergies, 27.4% (60), asthma, 12.8% (28), and eczema 9.6% (21) (Table 1). Evaluation of feeding intentions (day 0) versus current practices (6–8 weeks PP) determined a majority, 52.5% (115), and minority, 5.0% (11), reported intent to exclusively “breastfeed” and “formula” feed, respectively. Feeding practices at 6–8 weeks, however, largely incorporated pumping and formula: 36.4% (80) reported “breastfeeding with pumping” and 21.4% (47) exclusive formula. By weighted Kappa analysis (SAS 9.4), the interrater reliability among responders of planned versus current feeding practices was 0.2442, 95% confidence interval (CI 0.1407–0.3437), SE 0.0518, correlating to a “fair” degree of consistency (Table 1). Among respondents who changed their intended versus current method at 6–8 weeks, “exclusive breastfeeding” showed the greatest reduction in frequency, −22.9%, while “exclusive formula feeding” showed a net +16.5% increase (Table 2). Findings also showed none of the women, 5.0% (11), who intended to exclusively formula feed deviated from this plan by 6–8 weeks PP. By Fisher's method (SAS 9.4), statistically significant differences were identified when comparing intended versus change in method (p = 0.0003) as well as current versus change in method (p < 0.0001).
Table 1.
Demographics of Survey Participants
| Characteristics | % (n) |
|---|---|
| Mean age (30.0 years) | 100.0% (219) |
| Race/ethnicity | |
| American Indian/Alaskan | 0.9% (2) |
| Asian | 5.4% (12) |
| Black | 5.9% (13) |
| Hispanic/Latino | 9.1% (20) |
| White/Caucasian | 84.5% (185) |
| Multiple Races | 5.02% (11) |
| Declined | 0.4% (1) |
| Dermatologic medical history | |
| Mastitis | 7.3% (16) |
| Eczema | 9.6% (21) |
| Asthma | 12.8% (28) |
| Rhinitis | 8.7% (19) |
| Allergies | 27.4% (60) |
| Skin allergies (lanolin/soaps/lotions/fragrances) | 2.7% (6) |
| First baby | 36.5% (80) |
| First breastfed baby | 46.6% (102) |
| Infant age at time of survey (48.4 ± 5.5 days) | 100.0% (219) |
Table 2.
Feeding Intentions and Current Practices
| Feeding practice | Intention % (n) | Current % (n) | % Change (n) |
|---|---|---|---|
| Exclusive breastfeeding | 52.5% (115) | 29.6% (65) | −22.9% (−50) |
| Breastfeeding with pumping | 33.8% (74) | 36.4% (80) | +2.6% (+6) |
| Breastfeeding and/or pumping with formula | 8.7% (19) | 12.7% (28) | +4.0% (+9) |
| Exclusive formula | 5.0% (11) | 21.4% (47) | +16.4% (+36) |
To further evaluate breastfeeding outcomes, we examined possible associations between feeding plan, nipple problems, and dermatologic history (eczema or allergies) (Fisher's exact, SAS 9.4). No significant difference was identified in comparison of intended (p = 0.1039) or current (p = 0.7485) breastfeeding method to self-reported nipple skin lesions (cuts/open wounds and redness/eczema) experienced between 0 and 8 weeks PP (Fig. 1). Similarly, no significant difference was determined among women who changed their feeding method and reported nipple skin lesions (p = 0.9753). Comparison of formula use, history of eczema (p = 0.1520), or allergies (p = 0.5383) to nipple skin lesions also revealed no significance difference. Although 36.1% (79) of total participants (219) reported a history of “environmental” allergies, only 2.7% (6) identified skin sensitivities to lanolin, lotions, soaps, or fragrances.
We also sought to determine possible associations between nipple complaints and change in feeding practices, history of eczema, or sensitive skin (Table 3). Nipple complaints were again characterized as nipple lesions (cuts/open wounds and redness/eczema) or nipple symptoms (pain or itching) arising in between 0 and 8 weeks PP (Fig. 1). Irrespective of breastfeeding method, nipple complaints predominantly occurred between 1 and 3 weeks PP. Among women who reported nipple pain with breastfeeding (53.2%) and pumping (38.3%), the latter method had a higher OR, 2.00, 95% CI (1.09–3.67), of change in PP feeding practices. Pain with breastfeeding had a greater association with a history of skin allergies (sensitive skin), although did not achieve statistical significance, OR 1.39 (0.74–2.62). In comparison of nipple itching with pumping (14.2%) and breastfeeding (21.0%), the former had a greater association to all categories: change in feeding practice (OR 2.46 [1.00–6.04]), history of eczema (OR 3.66 [1.23–10.89]), and sensitive skin (OR 0.72 [0.27–1.92]). Categories were also compared to nipple skin lesions, including 10.2% (22) who reported PP cuts/wounds and 14.4% (31) who reported redness/eczema, irrespective of breastfeeding method (Fig. 1). Development of redness/eczema had a higher risk association with both change in feeding method, 1.08 (0.50–2.31), and history of eczema, 2.70 (0.96–7.61), while cuts/wounds were more associated with skin sensitivity, 1.59 (0.63–4.01) (Table 3).
Table 3.
Associations Between Nipple Symptoms, Dermatologic History, and Change in Feeding Practice
| Symptoms | % (n) | Change in feeding practice (OR) | History of eczema (OR) | History of skin allergies—“sensitive skin” (OR) |
|---|---|---|---|---|
| Nipple pain with | ||||
| Breastfeeding | 53.2% (101) | 1.14 (0.64–2.02) | 0.87 (0.34–2.19) | 1.39 (0.74–2.62) |
| Pumping | 38.3% (70) | 2.00 (1.09–3.67) | 1.03 (0.38–2.80) | 0.97 (0.50–1.87) |
| Nipple itching with | ||||
| Breastfeeding | 21.0% (39) | 2.00 (0.98–4.11) | 1.01 (0.31–3.22) | 0.66 (0.29–1.50) |
| Pumping | 14.2% (25) | 2.46 (1.00–6.04) | 3.66 (1.23–10.89) | 0.72 (0.27–1.92) |
| Nipple lesions | ||||
| Cuts/wounds | 10.2% (22) | 0.94 (0.39–2.29) | 0.92 (0.20–4.22) | 1.59 (0.63–4.01) |
| Redness/eczema | 14.4% (31) | 1.08 (0.50–2.31) | 2.70 (0.96–7.61) | 0.74 (0.30–1.82) |
“Breastfeeding” refers to feeding “at the breast.”
OR, odds ratios.
To further elucidate determinants of breastfeeding success, survey measures (categorical variables) were compared in relationship to women who did and did not meet their breastfeeding goals. Regardless of intended plan versus outcome, 7.3% (16) women stated their breastfeeding goals had not been met at 6–8 weeks due to nipple problems. Comparison of demographic variables or feeding plan to breastfeeding goals revealed no significant difference. Nipple symptoms (pain or itching) by method (breastfeeding or pumping) revealed one significant association to impaired goals. Nipple pain with pumping was reported in 38.5% (67) women, of which 16.4% (11) reported unmet goals with a significance of p = 0.0138, OR 1.31 (1.33–12.11). Few women, 7.9% (3) and 8.0% (2), reported impaired goals with nipple itching while breastfeeding and pumping, respectively. Comparisons to self-reported nipple skin symptoms (cuts/wound and redness/eczema) were statistically significant (p = 0.0003) with a higher prevalence, 31.8% (7), of unfulfilled goals among women with cuts/wound. Evaluation of products (nipple shields, lanolin; n = 148, p = 0.0256) and provider use (MD and non-MD; n = 154, p = 0.0018) also revealed statistically significant differences. A higher prevalence of unmet goals was identified in women using both nipple shields and lanolin, 20.8% (5), as well as those seeking care from both MD and non-MD providers, 38.5% (5).
Among all participants (n = 219), the most commonly used products included, lanolin 62.1% (136), gel pads 25.6% (56), and nipple shields 16.0% (35). Survey results regarding health care providers utilized in this population were more variable. In the mother-baby-unit, 46.2% (101) of women sought care from lactation consultants and 37.0% (81) from nurses. Although women received care from OB and pediatric physicians, no women were evaluated by internal medicine or dermatology specialists.
Discussion
Nipple pain is common in the early PP period and a common contributing factor to premature cessation of breastfeeding, particularly as traumatized nipples can become exquisitely tender as reported by several women in survey study by Williamson et al.19 In evaluation of 219 PP women, our survey data parallel the 2018 Centers for Disease Control statistics with a majority, 86.3% (189), reporting intent to exclusively feed at the breast with or without pumping, and a 25% decline in breastfeeding rates, 64.5% (145), as early as 6 weeks PP. Trends among breastfeeding patterns also demonstrated a decrease in women “breastfeeding exclusively,” 52.5% (115) to 29.6% (65), with a predominant increase in formula use followed by pumping (Table 2). Many a times, the reality of unmet expectations contributes to difficulties during this time, and this study provides data that could inform potential nursing mothers about these challenges. Pain during breastfeeding has been linked to new-onset depression, anxiety, and mastitis, all of which contribute to formula supplementation or lack of breastfeeding with subsequent infants.6,20–22 Additional risk factors reported for nipple pain include cesarean sections, Raynaud's syndrome causing vasospasm of the nipple, various medications, breast cancers, and autoimmune diseases.23–29
Analysis of breastfeeding cessation, intended plan versus method at 6–8 weeks, showed a significant decline in feeding at the breast by 6–8 weeks regardless of the presence or absence of nipple skin problems or dermatologic skin history. Notable differences were, however, identified in comparison of nipple problems by feeding method and skin history. Women who reported pumping or PP redness/eczema had higher OR of a change in feeding practice (0 to 6–8 weeks PP), history of eczema, and sensitive skin (Table 3). In contrast, women with cuts/wounds had a higher prevalence of unmet breastfeeding goals. Interestingly, the contribution of nipple itching, redness, wounds, and/or dermatitis to cessation or change in breastfeed method was not identified in previous literature, although a few studies showed a decline in breastfeeding secondary to “nipple cracks” and the broader category of “nipple soreness.”30–32 The majority of research otherwise focuses on “nipple pain” as a primary cause of breastfeeding difficulties. Our findings suggest that antenatal review of the dermatologic history may identify individuals at increased risk for nipple problems during lactation, and that anticipatory guidance surrounding nipple wound care is an important lever to prevent cessation of breastfeeding.
Because our study supports a correlation between changes in nipple skin and breastfeeding practices, management of breastfeeding women should include skin health and symptom management. Common practices for nipple comfort include natural or OTC products that have little, if any, rigorous scientific support and may even be dangerous. Natural therapies include warm compresses and moist heat. Women are also encouraged to continue breastfeeding to relieve milk supply and breast engorgement, as well as alternate breastfeeding positions and ensure a proper latch.13,33 The most commonly recommended OTC products include glycerin pads, peppermint water, and lanolin- and dexpanthenol-containing creams.9,14,34,35 Study findings corroborate previous literature, in which lanolin and nipple shields were most commonly utilized by survey respondents; however, a significant difference was also shown in comparison of nipple product(s) and respondents' abilities to meet their breastfeeding goals. Some women are also counseled on the common occurrence of nipple tenderness, and that nipple skin will simply “adjust” within 1–2 weeks of breastfeeding.
While many different interventions for nipple pain are available, it is unclear which are most effective.13 In addition, controversies remain in regard to their safety profile of OTC products. Peppermint oil may present safety hazards for young nursing infants, and while temporarily providing a “cooling” effect, can also have a drying effect on skin that leads to weakening of the skin barrier, making the delicate nipple skin even more subject to irritation. Furthermore, if peppermint is applied to the nipple, it should be cleansed before next feeding to avoid inadvertent ingestion by the infant. Likewise, the prevalence of hypersensitivity reactions to lanolin is gradually increasing so avoidance of potential allergens such as lanolin is recommended.36,37
These products stand in contrast to standard therapies recommended by dermatologists for itching, eczema (atopic dermatitis), wounds, or burns on skin surfaces, which include topical anti-inflammatory corticosteroids, topical calcineurin inhibitors, phototherapy, and/or oral antihistamines.38–40 For skin with barrier compromise, less is more when it comes to washing the skin and avoiding soap is de rigueur. Instead, frequent application of bland emollients is recommended along with use of moisture retentive dressings when the skin is open with cuts, abrasions, or ulcers. Blisters heal better when unbroken and maintaining a moist wound healing environment benefits all skin, including nipples.41–43
Because previous studies, corroborated by our data, identify a predominance of nipple pain, itching, or skin changes in the first (1–3) weeks of breastfeeding, it suggests anticipatory guidance and early intervention may optimize breastfeeding outcomes.2,4,13 On average, mothers and infants undergo 36 health care visits with their health care providers in the first year, most involving their general practitioners.2 Our data demonstrate that the majority, 70.3% (154), received prenatal/postnatal breastfeeding counseling, particularly from nursing staff or lactation consultants in the mother-baby unit. Despite the prevalence of nipple pain/itching or skin lesions, only 6.0% (13) sought care from a licensed physician, and 0% respondents were seen by a dermatologist or internists. Although primary care providers should be well equipped in assessing and addressing breastfeeding problems, an obvious gap exists as studies demonstrate incorrect advice or treatment failure is another major cause of breastfeeding cessation.44–46
In addition to establishing evidence-based guidelines for antenatal or PP nipple care, a greater understanding of nipple skin conditions is imperative as malignancies of the breast can easily be mistaken for benign conditions. To enhance current practices, we propose improved education and earlier intervention of breastfeeding complications due to skin changes. Furthermore, an integrated approach between specialists should be considered, such as pediatricians, obstetricians, and dermatologists. For example, Naimer et al. identified a benefit in use of dermoscopy in identification of microscopic/macroscopic nipple skin issues.46
Strengths of this study include the large sample size of women surveyed within the 6–8-week PP window. In future work, we plan to address the weaknesses of this study by expanding our survey population to multiple sites, including community-based facilities, larger metropolitan areas, and regions with added diversity. Our survey could be expanded to include additional personal history, such as previous breastfeeding difficulties and utilized products, history of C-section(s), complications in birth, or skin conditions, and social demographics such as working status. Additional reasons for ceasing breastfeeding may also be queried; for example, working mothers may choose formula over breastfeeding due to time constraints. A similar survey design, but prospective analysis, could be pursued to identify prenatal breastfeeding intent with follow-up at either or both 1 and 8 weeks PP. These historical variables would help to identify potential confounding variables. Finally, we hope to further categorize breast pathology in PP women using accurate dermatologic terms that will give precision to the clinical analysis of these entities, thereby opening up further avenues for treatment.
Conclusion
Treatment options and provider guidelines for nipple discomfort and skin issues arising in breastfeeding PP women remain limited. To enhance understanding, key factors contributing to nipple trauma must first be established, hence the creation of this survey study. Findings suggest nipple pain, itching, and skin trauma most commonly arise in the first (1–3) weeks PP, despite receiving breastfeeding guidance from one or more lactation consultants. Over 1/4th of women with intent to breastfeed had to forgo feeding at the breast, and supplement with formula or a pump. The survey also revealed OTC products, including lanolin cream and nipple shields, as mainstay treatment for nipple complaints. Although the study design cannot define a correlation between types of nipple trauma and most effective treatments, these data will add to the existing body of knowledge on management practices for nursing mothers, which may ultimately aid women in meeting their personal breastfeeding goal and improve overall breastfeeding rates. The value of the information gathered in this study is revealing a potential relationship between underlying dermatoses (eczema), sensitive skin, and incidence of nipple problems.
Disclosure Statement
No competing financial interests exist.
Funding Information
This study was supported, in part, by the University of Iowa Institute for Clinical and Translational Science (UI CTS), which is granted with Clinical and Translational Science Award funds from the National Institutes of Health (UL1TR002537).
References
- 1.Stuebe AM, Bonuck K. What predicts intent to breastfeed exclusively? Breastfeeding knowledge, attitudes, and beliefs in a diverse urban population. Breastfeed Med 2011;6:413–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mccallum SM, Rowe HJ, Gurrin L, et al. . Unsettled infant behaviour and health service use: A cross-sectional community survey in Melbourne, Australia. J Paediatr Child Health 2011;47:818–823 [DOI] [PubMed] [Google Scholar]
- 3.Wagner EA, Chantry CJ, Dewey KG, et al. . Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics 2013;132:865–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mccann MF, Baydar N, Williams RL. Breastfeeding attitudes and reported problems in a national sample of WIC participants. J Hum Lact 2007;23:314–324 [DOI] [PubMed] [Google Scholar]
- 5.Righard L, Alade MO. Sucking technique and its effect on success of breastfeeding. Birth 1992;19:185–189 [DOI] [PubMed] [Google Scholar]
- 6.Buck ML, Amir LH, Cullinane M, et al. . Nipple pain, damage, and vasospasm in the first 8 weeks postpartum. Breastfeed Med 2014;9:56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Odom EC, Li R, Scanlon KS, et al. . Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131:e726– e732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kent J, Ashton E, Hardwick C, et al. . Nipple pain in breastfeeding mothers: incidence, causes and treatments. Int J Environ Res Public Health 2015;12:12247–12263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mcclellan HL, Hepworth AR, Garbin CP, et al. . Nipple Pain during Breastfeeding with or without Visible Trauma. J Hum Lact 2012;28:511–521 [DOI] [PubMed] [Google Scholar]
- 10.Amir LH, Dennerstein L, Garland SM, et al. . Psychological aspects of nipple pain in lactating women. J Psychosom Obstet Gynaecol 1996;17:53–58 [DOI] [PubMed] [Google Scholar]
- 11.McKechnie AC, Eglash A. Nipple shields: A review of the literature. Breastfeed Med 2010;5:309–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lv X, Feng R, Zhai J. A combination of mupirocin and acidic fibroblast growth factor for nipple fissure and nipple pain in breastfeeding women: Protocol for a randomised, double-blind, controlled trial. BMJ Open 2019;9:e025526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dennis C-L, Jackson K, Watson J.. Interventions for treating painful nipples among breastfeeding women. Cochrane Database Syst Rev 2014:CD007366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melli MS, Rashidi MR, Delazar A, et al. . Effect of peppermint water on prevention of nipple cracks in lactating primiparous women: A randomized controlled trial. Int Breastfeed J 2007;2:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dennis CL, Schottle N, Hodnett E, et al. . An all-purpose nipple ointment versus lanolin in treating painful damaged nipples in breastfeeding women: A randomized controlled trial. Breastfeed Med 2012;7:473–479 [DOI] [PubMed] [Google Scholar]
- 16.Jackson KT, Dennis CL. Lanolin for the treatment of nipple pain in breastfeeding women: A randomized controlled trial. Matern Child Nutr 2017;13:e12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morland-Schultz K, Hill PD. Prevention of and therapies for nipple pain: A systematic review. J Obstet Gynecol Neonatal Nurs 2005;34:428–437 [DOI] [PubMed] [Google Scholar]
- 18.Gungor ANC, Oguz S, Vurur G, et al. . Comparison of olive oil and lanolin in the prevention of sore nipples in nursing mothers. Breastfeed Med 2013;8:334–335 [DOI] [PubMed] [Google Scholar]
- 19.Williamson I, Leeming D, Lyttle S, et al. . ‘It should be the most natural thing in the world’: Exploring first-time mothers breastfeeding difficulties in the UK using audio-diaries and interviews. Matern Child Nutr 2011;8:434–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li R, Fein SB, Chen J, et al. . Why mothers stop breastfeeding: Mothers self-reported reasons for stopping during the first year. Pediatrics 2008;122(Supplement 2):S69–S76 [DOI] [PubMed] [Google Scholar]
- 21.Scott JA, Landers MCG, Hughes RM, et al. . Psychosocial factors associated with the abandonment of breastfeeding prior to hospital discharge. J Hum Lact 2001;17:24–30 [DOI] [PubMed] [Google Scholar]
- 22.Watkins S, Meltzer-Brody S, Zolnoun D, et al. . Early breastfeeding experiences and postpartum depression. Obstet Gynecol 2011;118(2, Part 1):214–221 [DOI] [PubMed] [Google Scholar]
- 23.Shamsa A, Bai J, Raviraj P, et al. . Mode of delivery and its associated maternal and neonatal outcomes. Open J Obstet Gynecol 2013;03:307–312 [Google Scholar]
- 24.Kearney MH, Cronenwett LR, Reinhardt R. Cesarean delivery and breastfeeding outcomes. Birth 1990;17:97–103 [DOI] [PubMed] [Google Scholar]
- 25.Zanardo V, Pigozzo A, Wainer G, et al. . Early lactation failure and formula adoption after elective caesarean delivery: Cohort study. Arch Dis Child Fetal Neonatal Ed 2013;98:F37–F41 [DOI] [PubMed] [Google Scholar]
- 26.Suzuki S, Hirohata S, Uriu K, et al. . Cesarean delivery as a factor promoting exclusive breastfeeding in Japan. J Matern Fetal Neonatal Med 2013;26:1762–1763 [DOI] [PubMed] [Google Scholar]
- 27.Wu M, Chason R, Wong M. Raynaud's phenomenon of the nipple. Obstet Gynecol 2012;119(Part 2):447–449 [DOI] [PubMed] [Google Scholar]
- 28.Mcguinness N, Cording V. Raynaud's phenomenon of the nipple associated with labetalol use. J Hum Lact 2012;29:17–19 [DOI] [PubMed] [Google Scholar]
- 29.Lawlor-Smith LS, Lawlor-Smith CL. Raynauds phenomenon of the nipple: A preventable cause of breastfeeding failure? Med J Aust 1997;166:448–448 [DOI] [PubMed] [Google Scholar]
- 30.Branger B.Description of 101 cases of nipple cracks and risk factors via case–control study in eight units of a perinatal network. Arch Pediatr 2020;27:45–50 [DOI] [PubMed] [Google Scholar]
- 31.Gianni ML, Bettinelli ME, Manfra P, et al. . Breastfeeding difficulties and risk for early breastfeeding cessation. Nutrients 2019;11:2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sun K, Chen M, Yin Y, et al. . Why Chinese mothers stop breastfeeding: Mothers' self-reported reasons for stopping during the first six months. J Child Health Care 2017;21:353–363 [DOI] [PubMed] [Google Scholar]
- 33.Menking-Hoggatt C. The effect of early skin-to-skin contact on breastfeeding duration and exclusivity: A mixed methods study (West Virginia University Dissertation). Graduate Theses, Dissertations, and Problem Reports. 6216. 2017; 10.33915/etd.6216 [DOI] [Google Scholar]
- 34.Shanazi M, Khalili AF, Kamalifard M, et al. . Comparison of the effects of lanolin, peppermint, and dexpanthenol creams on treatment of traumatic nipples in breastfeeding mothers. J Caring Sci 2015;4:297–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cable B, Stewart M, Davis J. Nipple wound care: A new approach to an old problem. J Hum Lact 1997;13:313–318 [DOI] [PubMed] [Google Scholar]
- 36.Contact Dermatitis. Prevalence of contact allergy to lanolin is increasing. Available at https://www.practiceupdate.com/content/prevalence-of-contact-allergy-to-lanolin-is-increasing/58729 (accessed August1, 2020)
- 37.Schelz Z, Molnar J, Hohmann J. Antimicrobial and antiplasmid activities of essential oils. Fitoterapia 2006;77:279–285 [DOI] [PubMed] [Google Scholar]
- 38.Sher L, Chang J, Patel I, et al. . Relieving the pruritus of atopic dermatitis: A meta-analysis. Acta Derm Venereol 2012;92:455–461 [DOI] [PubMed] [Google Scholar]
- 39.Majoie IL, Oldhoff JM, Weelden HV, et al. . Narrowband ultraviolet B and medium-dose ultraviolet A1 are equally effective in the treatment of moderate to severe atopic dermatitis. J Am Acad Dermatol 2009;60:77–84 [DOI] [PubMed] [Google Scholar]
- 40.He A, Feldman SR, Fleischer AB. An assessment of the use of antihistamines in the management of atopic dermatitis. J Am Acad Dermatol 2018;79:92–96 [DOI] [PubMed] [Google Scholar]
- 41.Wiktor A.Treatment of minor thermal burns. December 19, 2019. Available at https://www.uptodate.com/contents/treatment-of-minor-thermal-burns (accessed August1, 2020)
- 42.Baxter CR.Management of burn wounds. Dermatol Clin 1993;11:709–714 [PubMed] [Google Scholar]
- 43.Hartford CE.Care of outpatient burns. In: Herndon D, eds. Total Burn Care. Philadelphia: WB Saunders, 1996, p. 71. [Google Scholar]
- 44.Montalto SA, Borg H, Buttigieg-Said M, et al. . Incorrect advice: The most significant negative determinant on breastfeeding in Malta. Midwifery 2010;26:e6–e13 [DOI] [PubMed] [Google Scholar]
- 45.Hauck YL, Graham-Smith C, Mcinerney J, et al. . Western Australian women's perceptions of conflicting advice around breast feeding. Midwifery 2011;27:e156–e162 [DOI] [PubMed] [Google Scholar]
- 46.Naimer SA, Silverman WF. “Seeing is believing”: Dermatoscope facilitated breast examination of the breastfeeding woman with nipple pain. Breastfeed Med 2016;11:356–360 [DOI] [PubMed] [Google Scholar]