Abstract
Objectives
This study tested the mediation effects of two facets of psychache – bearable and unbearable – in the relationship between exposure to suicide in the family and suicidal ideation in Portugal during the Covid‐19 pandemic.
Methods
Two hundred and forty‐four adults aged between 19 and 64 participated. Two groups were defined: one exposed to suicide in the family (n = 42) and a control group (n = 192).
Results
Path analysis using structural equation modelling tested a mediation model. Results demonstrated that unbearable psychache fully mediated the relationship between exposure to suicide and suicidal ideation, even when controlling for the mediation effects of depressive symptoms, the presence of a psychiatric diagnosis, and years of education.
Conclusions
These results suggest that rather than considering just the global experience of psychache in individuals exposed to suicide, researchers and clinicians should look to the presence of unbearable psychache given its contribution to suicidal ideation.
Practitioner points
Unbearable psychache fully mediated the relationship between exposure to suicide in the family and suicidal ideation
It is not the global experience of psychache that contributes to suicide ideation in individuals exposed to suicide in the family rather the presence of unbearable psychache
Keywords: exposure to family suicide, psychache, unbearable psychache, suicidal ideation, suicide survivors
Background
Worldwide, more than 800,000 people die by suicide annually (World Health Organization [WHO], 2019), and in Portugal, 1,061 suicides were recorded in 2017 (National Institute of Statistcis, 2017). Suicidal behaviours are particularly hard to predict (e.g., O’Connor & Nock, 2014; Overholser, Braden, & Dieter, 2012) and are multi‐causal in nature (Barzilay & Apter, 2014; Franklin et al., 2017). This suicide epidemiology calls out for empirical research as well as the design of prevention and intervention measures (e.g., Brás, Jesus, & Carmo, 2016).
Suicidal ideation can be understood as a set of thoughts, cognitions, and an outline of a plan to end one’s own life (Guerreiro, 2013; Klonsky, May, & Saffer, 2016). It can vary according to the degree of severity (Jacobs et al., 2010) from thoughts related to death and the uselessness of life (May, Overholser, Ridley, & Raymond, 2015), which is usually called passive ideation, to persistent thoughts about death, associated with an intense desire for self‐destruction and a suicide plan, which is referred to as active ideation (Sveticic & De Leo, 2012).
Several worldwide studies have attempted to understand suicidal behaviours, namely suicidal ideation, from a psychological perspective. Several psychological variables including psychache (psychache) (Shneidman, 1993) have been found to be systematically associated with suicidal ideation (e.g., Brown, Beck, Steer, & Grisham, 2000; Verrocchio et al., 2016), which has been revealed to be an important risk factor for effective suicide (e.g., Baca‐Garcia et al., 2011; Brezo et al., 2007), namely among those exposed to suicide (e.g., Campos, Holden, & Santos, 2017; Map le, Cerel, Sanford, Pearce, & Jordan, 2017).
Exposure to suicide and suicidal ideation
Shneidman (1972) estimated that, for each suicide, at least six individuals are affected, and Wrobleski’s (2002) estimation determined that each suicide leads to about 10 bereavements. Exposed individuals are directly or indirectly affected, and the impact depends on the relationship, degree of kinship, level of prior contact, and/or proximity and the age of the deceased (e.g., Berman, 2011; Mitchell, Kim, Progerson, & Mortimer‐Stephens, 2004). If suicide is seen as a way to escape the individual’s unbearable psychache (e.g., Verrocchio et al., 2016), it can also cause intense psychological suffering to those exposed (Jordan & McGann, 2017; Santos & Tavares, 2014). Beyond the psychological impact of the loss, strong evidence points to the fact that the complexity of the phenomenon (Jordan, 2001) and the associated stigma constitute a barrier to accepting the reality of the loss (e.g., Tal‐Young et al., 2012). Feelings usually associated with bereavement, such as sadness, loneliness, shock, and longing (Carqueja, 2017), are intensified in suicide survivors due to the added feelings of guilt, shame, and anger (Jordan, 2001; Kõlves et al., 2018; Sveen & Walby, 2008; Tal‐Young et al., 2012). These increase the risk of developing psychopathological symptoms like depressive symptoms (McMenamy, Jordan, & Mitchell, 2008) during the grieving process.
In fact, exposure to suicide is per se a suicide risk factor (Agerbo, Nordentoft, & Mortensen, 2002; De Leo & Heller, 2008; Hedstrom, Liu, & Nordvik, 2008; Rostila, Saarela, & Kawachi, 2013; Song, Kwon, & Kim, 2015; WHO, 2014). For example, research based on Danish national health records has shown a strong association between a family history of suicide and suicide risk (Agerbo et al., 2002). De Leo and Heller (2008) found that suicide exposure increases the risk of suicidal behaviour and death by suicide in Australian young people. Hedstrom et al., (2008) found that Swedish men exposed to a suicide in their family or at the workplace were more likely to die by suicide. Rostila et al., (2013) also found an increased risk of mortality by suicide among those who had experienced sibling suicide death. Song et al., (2015) found a significant correlation between suicidal ideation and exposure to suicide in close relationships (i.e., family, friends, and acquaintances), and their data also revealed that individuals losing a family member to suicide in their lifetime are 4.5 times more likely to experience suicide ideation.
A few studies in Portugal have looked into the suicide impact on exposed family members (e.g., Campos, Holden, et al., 2017; Campos, Holden, Spínola, Marques, & Santos, 2020; Santos, Campos, & Tavares, 2015b; Santos, Tavares, & Campos, 2015c). Santos et al., (2015b) revealed that family members exposed to suicide reported higher levels of distress and that 42% of those exposed experienced suicide ideation compared to just 5% in the community control group. Campos, Holden, et al., (2017) compared a sample of Portuguese people exposed to family suicide to a control group. Results showed that losing family members to suicide, the psychache construct assessed by the Psychache Scale, and their interaction made significant and unique contributions to explaining suicide risk variance. The potential mediating effect of psychache on the relationship between suicide exposure and suicidal ideation was not studied. More recently, Campos et al., (2020) compared the levels of suicide ideation and thwarted interpersonal needs between a control group and one made up of people with family suicide exposure and found significant differences between the Suicide Ideation Scale levels of the exposed group and the control group. The exposed group presented higher suicide risk levels, assessed by the suicide ideation indicator, even when controlling for levels of depressive symptoms and having a psychiatric diagnosis.
Psychache and suicidal ideation
Psychological models of suicide consider the simultaneous effect of psychological variables in predicting suicidal behaviours (e.g., Barzilay & Apter, 2014). Within these models, Shneidman (1993, 1998) has posited that psychache is a necessary condition for suicidal behaviours, regardless of the presence or absence of other risk variables such as depression. Suicide occurs when psychache exceeds an individual’s threshold of tolerance. It is caused by unfulfilled basic psychological needs (e.g., security, feelings of belonging, accomplishment, and autonomy) which lead to an acute and extremely painful affective state associated with feelings of guilt, anguish, loneliness, fear, helplessness, shame, humiliation, anger, and despair (Orbach, Mikulincer, Sirota, & Gilboa‐Schechtman, 2003). In certain cases, psychache can be so intense and unbearable that it leads the individual to try to escape from it, considering death as the only solution.
Empirical research of suicidal risk within a psychological framework demonstrates a robust relationship between psychache and suicidal behaviours (e.g., Campos et al., 2016; DeLisle & Holden, 2004) and, more specifically, between psychache and suicidal ideation (e.g., Brown et al., 2000; DeLisle & Holden, 2009; Ducasse et al., 2018; Troister & Holden, 2012). Two meta‐analyses have corroborated this relationship (Ducasse et al., 2018; Verricchio et al., 2016).
In a four‐year longitudinal study of undergraduates (Montemarano, Troister, Lambert, & Holden, 2018), psychache was found to mediate the relationship between other risk factors, such as depression, hopelessness, and suicidal ideation. A two‐year longitudinal study (Troister & Holden, 2012) of undergraduates with significant suicidal ideation demonstrated that psychache was statistically related to suicidal ideation, and changes in psychache were associated with changes in suicidal ideation, even when depression and hopelessness were controlled. Troister, D’Agata, and Holden (2015) also found that psychache in a sample of university students was a better long‐term predictor of suicide risk than depression or hopelessness. Psychache and suicidal ideation have been found to vary in the same direction (DeLisle & Holden, 2004, 2009), with psychache being the only variable that statistically predicted suicidal ideation, after controlling for the effect of other clinical variables.
According to Shneidman (1993, 1998), when psychache becomes unbearable, individuals may be motivated to attempt suicide. If psychache is not a constant experience, if there are different levels of pain (Shneidman, 1998), it seems plausible to think that unbearable psychache is that most closely related to suicide risk. Using the Psychache Scale (Holden, Mehta, Cunningham, & McLeod, 2001), Pachkowski, May, Tsai, and Klonsky (2019) recently reported that, when psychache severity is divided into two levels, bearable and unbearable, the latter is a significant predictor of suicidal behaviours. Campos and Holden (2020), however, found unbearable psychache to be no more robust than bearable psychache in statistically predicting suicide attempts.
Aim of the study
Given that suicidal ideation is an important indicator of suicide risk (e.g., Baca‐Garcia et al., 2011), is more prevalent in people exposed to suicide (e.g., Campos, Holden, et al., 2017; Santos, Campos, & Tavares, 2015a), and that empirical research also demonstrates a relationship between psychache and suicidal behaviours, namely suicidal ideation (e.g., Verrocchio et al., 2016), the present study tested the mediation effect of psychache on the relationship between family suicide exposure and suicidal ideation as an indicator of suicide risk in a sample of a Portuguese adults. In other words, we have tested if exposure to suicide in the family leads to the experience of psychache, which, in turn, augments the probability of presenting suicide ideation, an important proxy for effective suicide. Testing this model may contribute to enhance knowledge about why exposure to suicide may augment suicide risk. We also tested a competing moderation model. Exposure to suicide can not only leads directly to psychache, which in turn leads to suicidal ideation, but psychache can also moderate/potentiate the relationship between exposure to suicide in the family and suicidal ideation, clarifying under which circumstances exposure leads to suicide ideation. Bearable and unbearable psychache were defined as different dimensions of psychache as proposed by Pachkowski et al., (2019) and were measured using the Psychache Scale (Holden et al., 2001) and according to Shneidman’s (1993) perspective. Sociodemographic variables previously reported to be related to suicide ideation, such as sex, age, marital, and unemployed status, years of education, and the presence of a psychiatric diagnosis (Overholser et al., 2012) were controlled. Depressive symptoms were added as a mediating covariate. The literature has shown the importance of depressive symptoms for suicide risk (Arria et al., 2009; Brown et al., 2000) as well as a robust relationship between suicide exposure and depression (Cerel et al., 2016). Unbearable psychache was predicted to fully mediate the relationship between family suicide exposure and suicidal ideation.
Method
Participants and procedure
Of a total 247 adult Portuguese respondents, three were excluded as they reported residing outside of the country. The remaining inclusion criteria were ages between 18 and 65 and having a minimum of six years of formal education. The actual ages ranged from 19 to 64 (M = 35.34; SD = 12.05), and the sample was mostly female (n = 196; 80.3%). Mean years of education was 13.91 (SD = 2.58) and varied from 6 to 19 years. Ninety participants (36.9%) were either married or living together.
Participants answered a Google research protocol published online for 24 days in April/May 2020, during the first lockdown in Portugal due to the Covid‐19 pandemic. The protocol link was distributed through social networks. An informed consent form appeared on the first page, where participants were informed of the study objectives and the anonymous and voluntary nature of their participation. Participates were said: ‘We would like to ask for your collaboration to participate in a research on several psychological variables and thoughts about death and risk behaviours. Given the current situation in the country, we would also ask you to answer a few questions regarding the impact of the coronavirus pandemic’. Participants indicated their consent by clicking ‘continue’ and then received a brief sociodemographic and clinical questionnaire, followed by several instruments. All participants were provided with telephone numbers of available mental health services.
Measures
Sociodemographic and clinical form. The following sociodemographic and clinical data were gathered: age, gender, district, years of education, profession, employment and marital status, and whether they had a psychiatric diagnosis.
Psychache Scale (Holden et al., 2001) is a 13‐item scale assessing the concept of psychache (Shneidman, 1993). The first nine items rated the frequency of psychache, using a 5‐point Likert scale from 1 – ‘Never’ to 5 – ‘Always’ (e.g., ‘I seem to ache inside’; ‘Psychologically, I feel terrible’; ‘My pain makes me want to scream’). The remaining four items measured the intensity of psychache with four questions ranging from 1 – ‘Strongly disagree’ to 5 – ‘Strongly agree’ and assessed the intensity of psychache (e.g., ‘I can’t take my pain anymore’; ‘My pain is making me fall apart’). Total scores varied from 13 to 65, with higher results indicating greater levels of psychache. The original version of the scale presented an alpha coefficient of.92. The Psychache scale can differentiate individuals at‐risk for suicide from those not at risk, even when controlling for variables such as depression and hopelessness (e.g., DeLisle & Holden, 2004). Pachkowski et al., (2019) differentiated two subscales, a 3‐item one evaluating unbearable psychache (e.g., ‘I can’t take my pain anymore’; ‘Because of my pain, my situation is impossible’; ‘My pain is making me fall apart’) versus a 10‐item tool assessing a more moderate or bearable form of pain (e.g., ‘I seem to ache inside’). The original Portuguese version (Campos, Holden, & Gomes, 2018) reported an alpha coefficient of.95, while that of the current study was .96. The alpha coefficient for the unbearable psychache scale was.93, and for the bearable psychache was .95. The mean overall psychache score was 24.08 (SD = 10.72).
Center for Epidemiologic Studies Depression Scale (CES‐D; Radloff, 1977) is a 20‐item measure assessing the frequency of depressive symptoms in the week prior to the assessment (Radloff, 1977). Items (e.g., ‘I felt depressed’) are answered on a 4‐point Likert scale ranging from zero referring to ‘Never or very rarely – less than 1 day’ to three ‘Very frequently or always – 5‐7 days’. The total score ranged from 0 to 60, with higher results indicating a greater level of depressive symptoms. Radloff (1977) reported alpha coefficient values of .85 and .90 for community and clinical samples, respectively. The Portuguese version (Gonçalves & Fagulha, 2004) reported internal consistency alpha coefficient values ranging from .85 to .92 across various samples, while that of the current study was .91, and the mean score was 21.62 (SD = 11.36). For the Portuguese version, 48.7% of the participants score equal or above the cut‐off point of 21 is suggested by Gonçalves and Fagulha (2004).
Suicide Ideation Scale (SIS; Luxton, Rudd, Reger, & Gahm, 2011) is a 10‐item measure evaluating suicidal ideation in the previous week. Items (e.g., ‘I have been thinking of ways to kill myself’; ‘I have come close to taking my own life’) were scored on 5‐point Likert scale ranging from 1 – ‘Never or none of the time’ to 5 – ‘Always or many times’. Scores varied from 10 to 50, with higher values representing higher levels of suicidal ideation. The original version of the scale (Luxton et al., 2011) presented an alpha reliability coefficient of .91 in a clinical sample. The Portuguese version used herein (Campos, Holden, & Lambert, 2019) had an alpha coefficient of .86 in a community sample. It should be noted that, in the Portuguese version, the evaluation period is two weeks prior to the evaluation. In the current study, the alpha coefficient was .94, and the mean score was 11.91 (SD = 4.86).
Exposure to suicide assessment
To assess family suicide exposure, participants were asked if any family member had died of suicide, and if so, information was requested about which family member, when, what suicide method was used, and the degree of impact (using a 1 – ‘minimal impact’ to 5 – ‘high impact’ scale; Campos, Holden, et al., 2017).
Data analysis
Sixty‐five participants indicated that a family member had died by suicide; however, 10 were eliminated for not specifying the date of the event. Ten of the remaining 55 respondents reported a suicide date prior to the participants’ birth, so they were considered non‐exposed. Furthermore, three participants reported minimal impact and were also considered non‐exposed. Thus, we identified two groups: a suicide exposure group (n = 42) and a control (n = 192). Fourteen of the 42 exposed participants reported being the grandchildren of the deceased, six were children, one was a godfather, nine were nephews of the deceased, one was a sibling, two were great‐grandchildren, sixteen were cousins, and two had another kind of kinship. Eight exposed individuals (19%) reported two or more family suicides. Hanging was the most frequent method (48% of cases), followed by intoxication (24%) using medication, drug or poison, and drowning accounted for 12.0% of the cases. Mean time since the suicide was 16.74 years (SD = 11.34).
Table 1 presents the descriptive results as a function of group membership (suicide exposure versus control) for the sociodemographic variables of age, gender, years of education, employment, and marital status and whether participants had a psychiatric diagnosis. Descriptive statistics by group for suicidal ideation, the two dimensions of psychache, and depressive symptoms are also displayed. For all variables, the exposed and control groups were compared using t or χ 2 tests.
Table 1.
Descriptive and inferential statistics for control (n = 192) and suicide exposed (n = 42) groups
| Variables | n | % | Mean (SD) | n | % | Mean (SD) | t/χ2 |
|---|---|---|---|---|---|---|---|
| Sociodemographic variables | Control group | Exposed group | |||||
| Age in years | 35.26 (11.99) | 36.31 (12.82) | .51 | ||||
| Years of education | 14.03 (2.53) | 13.56 (2.85) | |||||
| Unemployment | |||||||
| Employed | 157 | 81.8 | 28 | 66.7 | 4.75* | ||
| Unemployed | 35 | 18.2 | 14 | 33.3 | |||
| Gender | |||||||
| Male | 35 | 18.2 | 9 | 21.4 | .23 | ||
| Female | 157 | 81.8 | 33 | 78.6 | |||
| Marital status | |||||||
| Not married | 120 | 62.5 | 27 | 64.3 | .047 | ||
| Married or living together | 72 | 37.5 | 15 | 35.7 | |||
| Having had a psychiatric diagnosis | |||||||
| No | 171 | 89.1 | 37 | 88.1 | .033 | ||
| Yes | 21 | 10.9 | 5 | 11.9 | |||
| Study variables | |||||||
| Suicidal ideation | 11.46 (3.75) | 13.95 (8.17) | 3.02** d = .39 a | ||||
| Bearable psychache | 18.44 (8.26) | 21.57 (10.22) | 2.13* d = .34 a | ||||
| Unbearable psychache | 4.72 (2.28) | 5.86 (3.38) | 2.07* d = .40 a | ||||
| Depressive symptoms | 20.92 (10.84) | 24.86 (13.14) | 2.05* d = .33 a | ||||
Cohen’s d. *p < .05, **p < .01.
Bootstrapping (with 1,000 samples constructing bias‐corrected confidence intervals) evaluated significance levels. A path analysis model was tested using AMOS software (version 21) to verify whether psychache (bearable and unbearable) and depressive symptoms mediated the relationship between the exogenous variable (exposed or control group) as well as the endogenous variable, suicidal ideation. Demographic variables significantly correlated with suicidal ideation or that differentiated groups were included as exogenous covariates. A hierarchical multiple regression analysis also tested if the two dimensions of psychache moderated the relationship between group membership and suicidal ideation. For this regression analysis, any sociodemographic or clinical variable that correlated significantly with suicidal ideation or that differentiated groups was entered in the first step of both regressions. Group membership was entered in step two. Unbearable and bearable psychache were entered in step three, and the interaction terms between group membership and the two psychache dimensions were entered in the fourth and the final step. Variables were standardized before calculating the interaction product term.
Results
Table 1 shows that unemployment was the only sociodemographic variable that differentiated groups, with a higher percentage of unemployed individuals in the exposed group. Groups did differ significantly on bearable and unbearable psychache, depressive symptoms, and suicidal ideation. Years of education (r(217) = −.14, p < .05), having a psychiatric diagnosis (r(234) = .34, p < .01), depressive symptoms (r(234) = .57, p < .01), group (r(234) = .20, p < .01), bearable psychache (r(234) = .58, p < .01), and unbearable psychache (r(234) = .63, p < .01) correlated significantly with suicidal ideation. In the exposed group, time since suicide did not correlate significantly with suicidal ideation (r(42) = .00, ns). Given that unemployment differentiated groups and that years of education and psychiatric diagnosis correlated with suicidal ideation, these variables were introduced in the following analyses as covariates.
In the direct model (see Figure 1a), group presented a significant direct effect on suicidal ideation (β = .189, SE = .075, p < .05, CI 95% [0.038, 0.334]); yet, the mediation model (Figure 1b) did not reveal a direct, significant effect of group on suicidal ideation. The direct effect of group on unbearable psychache was significant (β = .164, SE = .067, p < .01, CI 95% [0.033, 0.297]), as was that of unbearable psychache on suicidal ideation (β = .377, SE = .143, p < .01, CI 95% [0.107, 0.646]). The direct effect of group on depressive symptoms was also significant (β = .141, SE = .064, p < .05, CI 95% [0.025, 0.279]), as was that of depressive symptoms on suicidal ideation (β = .227, SE = .093, p < .05 CI 95% [0.046, 0.405]). It is worth pointing out that bearable psychache did not significantly relate to suicidal ideation. Finally, a significant, indirect effect of group on suicidal ideation was also identified (β = .105, SE = .040, p < .01, CI 95% [0.026, 0.190]). These results suggest that unbearable psychache variable fully mediates the relationship between group and suicidal ideation.
Figure 1.
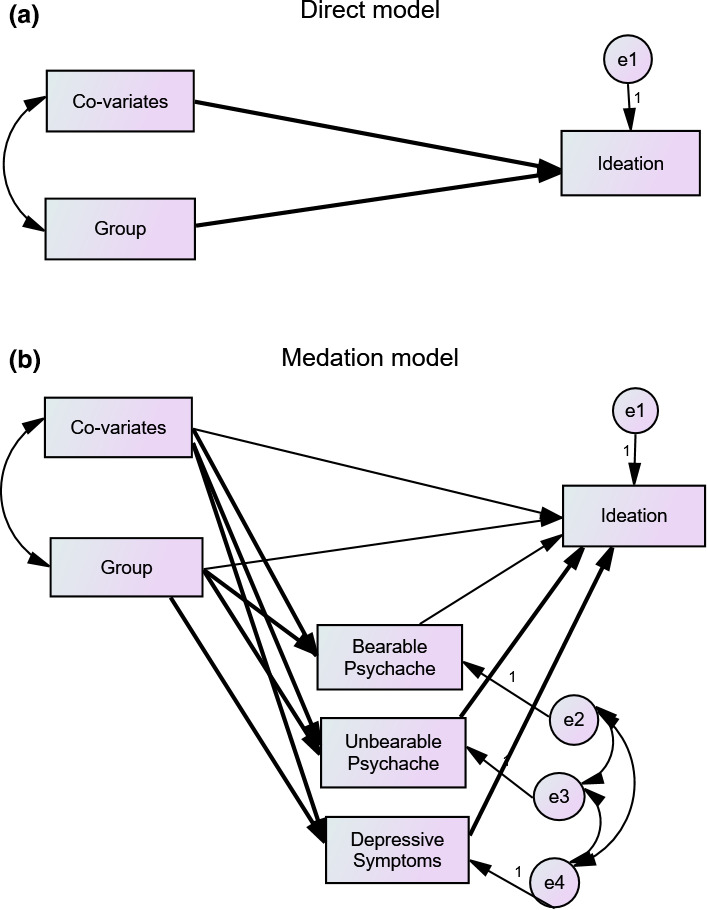
Graphical representation of the tested model. Note: Significant paths are highlighted.
The hierarchical multiple regression analysis revealed that bearable psychache and unbearable psychache did not moderate the relationship between exposure to suicide and suicidal ideation.
Discussion
The present study tested the mediation effects of bearable and unbearable psychache in the relationship between family suicide exposure and suicidal ideation in a sample of Portuguese community adults. A competing moderation model was also tested.
Results suggested that individuals exposed to suicide reported higher levels of suicidal ideation than those without a family history of suicide. These results are consistent with the literature (e.g., Almeida et al., 2012; Campos et al., 2020; Crosby & Sacks, 2002; Kuramoto et al., 2010; Qin, Agerbo, & Mortensen, 2002; Qin, Agerbo, & Mortensen, 2003; Song et al., 2015) which shows that individuals exposed to suicide often exhibit a higher risk of suicide than the general population, namely when suicidal ideation is considered as an indicator of suicide risk. In the present study, the two groups also differed regarding the levels of bearable and unbearable psychache. These findings are consistent with the previous ones revealing a strong relationship between family suicide exposure and psychache (e.g., Campos, Holden, et al., 2017). These results also echoed those in the literature regarding a relationship between psychache and suicidal ideation (e.g., Ducasse et al., 2018).
Years of education, psychiatric diagnose, and depressive symptoms were also found to correlate with suicidal ideation. These results align with the previous studies suggesting that psychiatric diagnosis is a strong predictor of suicidal behaviours and suicide (e.g., Arria et al., 2009; Borges, Angst, Nock, Ruscio, & Kessler, 2008; Cavanagh, Carson, Sharpe, & Lawrie, 2003; Conner, Duberstein, Conwell, Seidlitz, & Caine, 2001) and that a significant percentage of individuals with suicidal ideation simultaneously present psychopathology, in particular, depressive symptoms (Khan, Mahmud, Mehtab, Zaman, & Prince, 2008; McMenamy et al., 2008; Overholser et al., 2012). Results also echoed those of Almasi et al., (2009) that found that low educational levels are related to suicidal ideation. This lack of education may be associated with inadequate or insufficient levels of psychological health literacy, which may, in turn, lead the individual to adopt more risky behaviours (Zhang, Tao, Wu, Tao, & Fang, 2016).
Our results suggest that unbearable psychache is a significant mediating variable that helps to explain the relationship between suicide exposure and ideation, even when controlling for the mediation effect of depressive symptoms. The main goal of the study was to test whether the relationship of exposure to suicide in the family to suicide ideation could be explained, at least partially, by an unbearable experience of suffering and pain. This mediation effect may be explained by the psychological vulnerability and internal suffering experienced by individuals with family suicide exposure (Shneidman, 1993) which may then lead to the perception of unbearable psychache, thus contributing to suicidal ideation. However, our results suggest that it is the experience of unbearable psychache rather than a global experience of psychache that mediates the relationship between family suicide exposure and suicidal ideation. But, besides bereavement, other components of exposure to suicide in the family may contribute to suicide‐related outcomes. The relationship between history of exposure to suicide in the family and suicidal ideation may be explained by other variables, such as a genetic loading for suicide or modelling of suicidal escape behaviour in the family.
It must be said, however, that the fact of the data were collected during the pandemic, and a lockdown in Portugal may have had a considerable impact on the levels of suffering and psychache of the participants. In fact, in the present sample, 48.7% of participants presented a result equal to or above the cut‐off point for the Portuguese version of the CES‐D. Previous research shows that the impact of the pandemic on mental health was very strong (National Institute of Health Ricardo Jorge, 2020), and we can speculate that it may increase the experience of unbearable psychache and thus increase the risk of suicide in individuals who have been exposed to suicide in the family. Also comparing the current sample with a pre‐pandemic sample used in a previous study (Campos et al., 2019), the current sample presents significantly higher levels of psychache and suicidal ideation. The pandemic has increased the experience of fear and loneliness and called for adaptive strategies of coping. For someone who is experiencing unbearable levels of psychache and has to cope with the challenges of a pandemic, including the isolation and loneliness and way too much time to ruminate, the situation may become very hard to handle. The pandemic can increase the salience and intensity of psychological pain and then increase suicidal ideation and risk for suicide. A person who is experiencing increased levels of psychache and is also someone who is self‐critical and who feels helpless and hopeless may have higher risk related to suicidal thoughts and urges.
Results also demonstrated that unbearable psychache does not moderate the relationship of exposure to suicide in the family to suicidal ideation, which suggests that despite unbearable psychache explains why exposure may lead to suicidal ideation (exposure leads to unbearable psychache which in turns leads to suicidal ideation). It does not potentiate the effect of exposure to suicide in the family on suicidal ideation.
Limitations and conclusions
The present study has some limitations. First, a major limitation is the cross‐sectional study design that prevents making any causal inferences. Additionally, we have relied just on self‐report measures that are susceptible to several response bias (Dowling, Bolt, Deng, & Li, 2016). Future studies should consider using other data collection methods, such as interviews, and opt for longitudinal designs. The convenience, low risk sample constitutes another limitation, which should be addressed in the future. In addition to the small sample size, the disparity between the number of female and male participants is an issue, as is the online data collection. Online assessments raise a series of questions including self‐selection and lack of generalizability (Hauser, Paolacci, & Chandler, 2018). Future research should collect data in person and differentiate between survivor subgroups (e.g., friends, co‐workers, and family members). It should also be noted that these data were collected in the midst of a national state of emergency and public lockdown due to the Covid‐19 pandemic, whose mental health effects may have been profound. Social and physical distancing, fear, economic crisis, unemployment, uncertainty, and doubt are known triggers of severe psychological distress. Data collection during this period may have influenced the results in ways that are difficult to assess.
Results, however, suggest the need to implement adequate postvention strategies in the population. As argued by Shneidman (1996), ‘postvention aims primarily at mollifying the psychological sequelae of a suicidal death in the survivor‐victim’ (Andriessen, 2009). In fact, postvention also means prevention (Andriessen, 2009). The increased risk of suicide in suicide survivors demands the elaboration of prevention measures. The present study suggests that exposed individuals experiencing unbearable psychache will benefit the most from psychological interventions designed to facilitate the bereaving process, especially if the family suicide is associated with clinically significant suffering (Carqueja, 2017; Jordan & McMenamy, 2004). An elaboration of experiences of unbearable psychache might encourage individuals to consider alternatives to suicide and to develop more adaptive coping strategies to psychological suffering. It is also recommended that preventive initiatives be carried out within the general population to demystify suicide and combat the stigma associated with it.
Author contributions
Rui C. Campos, PhD (Conceptualization; Formal analysis; Supervision; Writing – original draft; Writing – review & editing) Alexandra Medina Pereira (Conceptualization; Data curation; Formal analysis; Writing – original draft).
Conflict of interest
All authors declare no conflict of interest.
Data availability statement
Data is available on request.
Acknowledgement
We wish to think all participants on this study.
References
- Agerbo, E. , Nordentoft, M. , & Mortensen, P. B. (2002). Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case‐control study. BMJ, 325, 74. 10.1136/bmj.325.7355.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almasi, K. , Belso, N. , Kapur, N. , Webb, R. , Cooper, J. , Hadley, S. , … Appleby, L. (2009). Risk factors for suicide in Hungary: a case‐control study. BMC Psychiatry, 9(1). 10.1186/1471-244x-9-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida, O. P. , Draper, B. , Snowdon, J. , Lautenschlager, N. T. , Pirkis, J. , Byrne, G. , … Pfaff, J. J. (2012). Factors associated with suicidal thoughts in a large community study of older adults. British Journal of Psychiatry, 201, 466–472. 10.1192/bjp.bp.112.110130 [DOI] [PubMed] [Google Scholar]
- Andriessen, K. (2009). Can postvention be prevention? Crisis, 30(1), 43–47. 10.1027/0227-5910.30.1.43 [DOI] [PubMed] [Google Scholar]
- Arria, A. M. , O’Grady, K. E. , Caldeira, K. M. , Vincent, K. B. , Wilcox, H. C. , & Wish, E. W. (2009). Suicide ideation among college students: A multivariate analysis. Archives of Suicide Research, 13, 230–246. 10.1080/13811110903044351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baca‐Garcia, E. , Perez‐Rodriguez, M. M. , Oquendo, M. A. , Keyes, K. M. , Hasin, D. S. , Grant, B. F. , & Blanco, C. (2011). Estimating risk for suicide attempt: Are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. Journal of Affective Disorders, 134, 327–332. 10.1016/j.jad.2011.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzilay, S. , & Apter, A. (2014). Psychological models of suicide. Archives of Suicide Research, 18, 295–312. 10.1080/13811118.2013.824825 [DOI] [PubMed] [Google Scholar]
- Berman, A. L. (2011). Estimating the population of survivors of suicide: Seeking an evidence base. Suicide and Life‐Threatening Behavior, 41(1), 110–116. 10.1111/j.1943-278x.2010.00009.x [DOI] [PubMed] [Google Scholar]
- Borges, G. , Angst, J. , Nock, M. K. , Ruscio, A. M. , & Kessler, R. C. (2008). Risk factors for the incidence and persistence of suicide‐related outcomes: A 10‐year follow‐up study using the National Comorbidity Surveys. Journal of Affective Disorders, 105, 25–33. 10.1016/j.jad.2007.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brás, M. , Jesus, S. , & Carmo, C. (2016). Fatores psicológicos de risco e protetores associados à ideação suicida em adolescentes. Psicologia, Saúde & Doenças, 17, 132–149. 10.15309/16psd170203 [DOI] [Google Scholar]
- Brezo, J. , Paris, J. , Tremblay, R. , Vitaro, F. , Hébert, M. , & Turecki, G. (2007). Identifying correlates of suicide attempts in suicidal ideators: A population‐based study. Psychological Medicine, 37, 1551–1562. 10.1017/S0033291707000803 [DOI] [PubMed] [Google Scholar]
- Brown, G. K. , Beck, A. T. , Steer, R. A. , & Grisham, J. R. (2000). Risk factors for suicide in psychiatric outpatients: A 20‐year prospective study. Journal of Consulting and Clinical Psychology, 68, 371–377. 10.1037/0022-006x.68.3.371 [DOI] [PubMed] [Google Scholar]
- Campos, R. C. , & Holden, R. R. (2020). Psychological pain and previous suicide attempts in young adults: Results with the Portuguese version of the Psychache Scale. Journal of Clinical Psychology, 76, 1965–1971. 10.1002/jclp.22973 [DOI] [PubMed] [Google Scholar]
- Campos, R. C. , Holden, R. R. , & Gomes, M. (2018). Assessing psychache as a suicide risk variable: Data with the Portuguese version of the psychache scale. Death Studies, 43, 527–533. 10.1080/07481187.2018.1493002 [DOI] [PubMed] [Google Scholar]
- Campos, R. C. , Holden, R. R. , & Lambert, C. E. (2019). Avoidance of psychological pain and suicidal ideation in community samples: Replication across two countries and two languages. Journal of Clinical Psychology, 75, 2160–2168. 10.1002/jclp.22837 [DOI] [PubMed] [Google Scholar]
- Campos, R. , Holden, R. , Laranjeira, P. , Troister, T. , Oliveira, A. , Costa, F. , … Fresca, N. (2016). Self‐report depressive symptoms do not directly predict suicidality in nonclinical individuals: Contributions toward a more psychosocial approach to suicide risk. Death Studies, 40, 335–349. 10.1080/07481187.2016.1150920 [DOI] [PubMed] [Google Scholar]
- Campos, R. C. , Holden, R. R. , & Santos, S. (2017). Exposure to suicide in the family: Suicide risk and psychache in individuals who have lost a family member by suicide. Journal of Clinical Psychology, 74, 407–417. 10.1002/jclp.22518 [DOI] [PubMed] [Google Scholar]
- Campos, R. C. , Holden, R. R. , Spínola, J. , Marques, D. , & Santos, S. (2020). Exposure to suicide in the family: Suicidal ideation and unmet interpersonal needs in young adults who have lost a family member by suicide. The Journal of Nervous and Mental Disease, 208, 201–207. 10.1097/nmd.0000000000001106 [DOI] [PubMed] [Google Scholar]
- Carqueja, E. (2017). Luto: Um Processo Dinâmico. In: Salazar H. (Coord.), (Ed.), Intervenção psicológica em cuidados paliativos (pp. 57–87). Lisboa: Pactor. [Google Scholar]
- Cavanagh, J. T. O. , Carson, A. J. , Sharpe, M. , & Lawrie, S. M. (2003). Psychological autopsy studies of suicide: A systematic review. Psychological Medicine, 33, 395–405. 10.1017/s0033291702006943 [DOI] [PubMed] [Google Scholar]
- Cerel, J. , Maple, M. , van de Venne, J. , Moore, M. , Flaherty, C. , & Brown, M. (2016). Exposure to suicide in the community: Prevalence and correlates in one U.S. state. Public Health Reports, 131(1), 100–107. 10.1177/003335491613100116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner, K. R. , Duberstein, P. R. , Conwell, Y. , Seidlitz, L. , & Caine, E. D. (2001). Psychological vulnerability to completed suicide: A review of empirical studies. Suicide and Life‐Threatening Behavior, 31(4), 367–385. 10.1521/suli.31.4.367.22048 [DOI] [PubMed] [Google Scholar]
- Crosby, A. E. , & Sacks, J. J. (2002). Exposure to suicide: Incidence and association with suicidal ideation and behavior: United States, 1994. Suicide and Life‐Threatening Behavior, 32(3), 321–328. 10.1521/suli.32.3.321.22170 [DOI] [PubMed] [Google Scholar]
- De Leo, D. , & Heller, T. (2008). Social modeling in the transmission of suicidality. Crisis: the Journal of Crisis's Intervention and Suicide. Prevention, 29(1), 11–19. 10.1027/0227-5910.29.1.11 [DOI] [PubMed] [Google Scholar]
- DeLisle, M. , & Holden, R. R. (2004). Depression, hopelessness, and psychache as increasingly specific predictors of suicidal manifestations. Canadian Clinical Psychologist, 15, 7–10. [Google Scholar]
- DeLisle, M. M. , & Holden, R. R. (2009). Differentiating between depression, hopelessness, and psychache in university undergraduates. Measurement and Evaluation in Counseling and Development, 42(1), 46–63. 10.1177/0748175609333562 [DOI] [Google Scholar]
- Dowling, N. M. , Bolt, D. M. , Deng, S. , & Li, C. (2016). Measurement and control of bias in patient reported outcomes using multidimensional item response theory. BMC Medical Research Methodology, 16, 1–18. 10.1186/s12874-016-0161-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducasse, D. , Holden, R. R. , Boyer, L. , Artéro, S. , Calati, R. , Guillaume, S. , … Olié, E. (2018). Psychological pain in suicidality: A meta‐analysis. Journal of Clinical Psychiatry, 79. 10.4088/JCP.16r10732 [DOI] [PubMed] [Google Scholar]
- Franklin, J. C. , Ribeiro, J. D. , Fox, K. R. , Bentley, K. H. , Kleiman, E. M. , Huang, X. , … Nock, M. K. (2017). Risk factors for suicidal thoughts and behaviors: A meta‐analysis of 50 years of research. Psychological Bulletin, 145, 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Gonçalves, B. , & Fagulha, T. (2004). The Portuguese version of the Center for Epidemiologic Studies Depression Scale (CES‐D). European Journal of Psychological Assessment, 20, 339–348. 10.1027/1015-5759.20.4.339 [DOI] [Google Scholar]
- Guerreiro, D. (2013). Glossário. In: Santos J. C. (Relator), Carvalho A., Peixoto B., Saraiva C. B., Sampaio D., Amaro F., Santos J. C., Santos J. H., & Santos N. (eds), Plano nacional de prevenção do suicídio 2013‐2017. Lisoba: Direção‐Geral da Saúde. [Google Scholar]
- Hauser, D. , Paolacci, G. , & Chandler, J. (2018). Common concerns with MTurk as a participant pool: Evidence and solutions. In Kardes F., Herr P., & Schwarz N. (Eds), Handbook in research methods in consumer psychology.England, UK: Routledge. [Google Scholar]
- Hedstrom, P. , Liu, K.‐Y. , & Nordvik, M. K. (2008). Interaction domains and suicide: A population‐based panel study of suicides in Stockholm, 1991–1999. Social Forces, 87, 713–740. 10.1353/sof.0.0130 [DOI] [Google Scholar]
- Holden, R. R. , Mehta, K. , Cunningham, E. J. , & McLeod, L. D. (2001). Development and preliminary validation of a scale of psychache. Canadian Journal of Behavioural Science, 33, 224–232. 10.1037/h0087144 [DOI] [Google Scholar]
- Jacobs, D. , Baldessarini, R. , Conwell, Y. , Fawcett, J. , Horton, L. , Meltzer, H. , … Simon, R. I. (2010). Practice guidelines for the assessment and treatment of patients with suicidal behaviors. APA Practice Guidelines.
- Jordan, J. R. (2001). Is suicide bereavement different? A reassessment of the literature. Suicide and Life‐Threatening Behaviour, 31(1), 91–102. 10.1521/suli.31.1.91.21310 [DOI] [PubMed] [Google Scholar]
- Jordan, J. R. , & McGann, V. (2017). Clinical work with suicide loss survivors: Implications of the U.S. Postvention guidelines. Death Studies, 41, 659–672. 10.1080/07481187.2017.1335553 [DOI] [PubMed] [Google Scholar]
- Jordan, J. R. , & McMenamy, J. (2004). Interventions for suicide survivors: A review of the literature. Suicide and life‐threatening Behavior, 34(4), 337–349. [DOI] [PubMed] [Google Scholar]
- Khan, M. M. , Mahmud, S. , Karim, M. S. , Zaman, M. , & Prince, M. (2008). Case–control study of suicide in Karachi, Pakistan. British Journal of Psychiatry, 193(05), 402–405. 10.1192/bjp.bp.107.042069 [DOI] [PubMed] [Google Scholar]
- Klonsky, E. D. , May, A. M. , & Saffer, B. Y. (2016). Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology, 12(1), 307–330. 10.1146/annurev-clinpsy-021815-093204 [DOI] [PubMed] [Google Scholar]
- Kõlves, K. , Zhao, Q. , Ross, V. , Hawgood, J. , Spence, S. H. , & de Leo, D. (2018). Suicide and other sudden death bereavement of immediate family members: An analysis of grief reactions six‐months after death. Journal of Affective Disorders, 243, 96–102. 10.1016/j.jad.2018.09.018 [DOI] [PubMed] [Google Scholar]
- Kuramoto, S. J. , Stuart, E. A. , Runenson, B. , Lichtenstein, P. L. , Långström, N. , & Wilcox, H. C. (2010). Maternal or paternal suicide and offspring’s psychiatric and suicide‐attempt hospitalization risk. Pediatrics, 126, 1026–1032. 10.1542/peds.2010-0974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luxton, D. D. , Rudd, D. , Reger, M. A. , & Gahm, G. A. (2011). A psychometric study of the suicide ideation scale. Archives of Suicide Research, 15, 250–258. 10.1080/13811118.2011.589720 [DOI] [PubMed] [Google Scholar]
- Maple, M. , Cerel, J. , Sanford, R. , Pearce, T. , & Jordan, J. (2017). Is exposure to suicide beyond kin associated with risk for suicidal behavior? A systematic review of the evidence. Suicide and Life‐Threatening Behavior, 47, 461–474. 10.1111/sltb.12308 [DOI] [PubMed] [Google Scholar]
- May, C. N. , Overholser, J. C. , Ridley, J. , & Raymond, D. (2015). Passive suicidal ideation: A clinically relevant risk factor for suicide in treatment‐seeking veterans. Illness, Crisis & Loss, 23, 261–277. 10.1177/1054137315585422 [DOI] [Google Scholar]
- McMenamy, J. M. , Jordan, J. R. , & Mitchell, A. M. (2008). What do suicide survivors tell us they need? Results of a pilot study. Suicide and Life‐Threatening Behavior, 38, 375–389. 10.1521/suli.2008.38.4.375 [DOI] [PubMed] [Google Scholar]
- Mitchell, A. M. , Kim, Y. , Prigerson, H. G. , & Mortimer‐Stephens, M. K. (2004). Complicated grief in survivors of suicide. Crisis, 25, 12–18. 10.1027/0227-5910.25.1.12 [DOI] [PubMed] [Google Scholar]
- Montemarano, V. , Troister, T. , Lambert, C. E. , & Holden, R. R. (2018). A four‐year longitudinal study examining psychache and suicide ideation in elevated‐risk undergraduates: A test of Shneidman’s model of suicidal behavior. Journal of Clinical Psychology, 74, 1820–1832. 10.1002/jclp.22639 [DOI] [PubMed] [Google Scholar]
- National Institute of Health Ricardo Jorge (2020). Saúde mental em tempos de pandemia. Lisbon, Portugal: INSA. [Google Scholar]
- National Institute of Statistcis (2017). Causas de morte 2017. Lisboa, Portugal: INE. [Google Scholar]
- O’Connor, R. C. , & Nock, M. K. (2014). The psychology of suicidal behavior. The Lancet Psychiatry, 1, 73–85. 10.1016/S2215-0366(14)70222-6 [DOI] [PubMed] [Google Scholar]
- Orbach, I. , Mikulincer, M. , Sirota, P. , & Gilboa‐Schechtman, E. (2003). Mental pain: A multidimensional operationalization and definition. Suicide and Life‐Threatening Behavior, 33, 219–230. 10.1521/suli.33.3.219.23219 [DOI] [PubMed] [Google Scholar]
- Overholser, J. C. , Braden, A. , & Dieter, L. (2012). Understanding suicide risk: Identification of high‐risk groups during high‐risk times. Journal of Clinical Psychology, 68, 334–348. 10.1002/jclp.20859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachkowski, M. C. , May, A. M. , Tsai, M. , & Klonsky, E. D. (2019). A brief measure of unbearable psychache. Suicide and Life‐Threatening Behavior, 49, 1721–1734. 10.1111/sltb.12556 [DOI] [PubMed] [Google Scholar]
- Qin, P. , Agerbo, E. , & Mortensen, P. B. (2003). Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: A national register–based study of all suicides in Denmark, 1981–1997. American Journal of Psychiatry, 160, 765–772. 10.1176/appi.ajp.160.4.765 [DOI] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES‐D scale: A self‐report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rostila, M. , Saarela, J. , & Kawachi, I. (2013). Suicide following the death of a sibling: a nationwide follow‐up study from Sweden. British Medical Journal Open, 3, e002618. 10.1136/bmjopen-2013-002618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos, S. , Campos, R. C. , & Tavares, S. (2015a). O impacto do suicídio nos familiares: Evidências atuais. Evidências, 1, 16–23. [Google Scholar]
- Santos, S. , Campos, R. C. , & Tavares, S. (2015b). Suicidal ideation and distress in family members bereaved by suicide in Portugal. Death Studies, 39, 332–341. 10.1080/07481187.2014.946626 [DOI] [PubMed] [Google Scholar]
- Santos, S. , & Tavares, S. (2014). Sobreviventes. In Saraiva C. B., Peixoto B. & Sampaio D. (Eds.), Suicídio e comportamentos autolesivos – dos conceitos à prática clínica (pp. 445–453). Lisboa, Portugal: Lidel. [Google Scholar]
- Santos, S. , Tavares, S. , & Campos, R. C. (2015c). Distress in Portuguese family members bereaved by suicide: An exploratory study. Journal of Loss and Trauma, 20, 267–280. 10.1080/15325024.2014.934618 [DOI] [Google Scholar]
- Shneidman, E. (1972). Foreward. In Cain A. C. (Ed.), Survivors of suicide (pp. ix–xi). Springfield, IL: Charles C. Thomas. [Google Scholar]
- Shneidman, E. (1993). Suicide as psychache: A clinical approach to self‐destructive behavior. Lanham: Rowman & Littlefield Publishers Inc. [Google Scholar]
- Shneidman, E. (1996). The suicidal mind: Final thoughts and reflections. Oxford, UK: Oxford University Press. [Google Scholar]
- Shneidman, E. S. (1998). Further reflections on suicide and psychache . Suicide and Life‐Threatening Behavior, 28, 245–250. [PubMed] [Google Scholar]
- Song, I. H. , Kwon, S. W. , & Kim, J. E. (2015). Association between suicidal ideation and exposure to suicide in social relationships among family, friend, and acquaintance survivors in South Korea. Suicide and Life‐Threatening Behavior, 45, 376–390. 10.1111/sltb.12158 [DOI] [PubMed] [Google Scholar]
- Sveen, C. A. , & Walby, F. A. (2008). Suicide survivors’ mental health and grief reactions: A systematic review of controlled studies. Suicide and Life‐Threatening Behavior, 38(1), 13–29. 10.1521/suli.2008.38.1.13 [DOI] [PubMed] [Google Scholar]
- Sveticic, J. , & De Leo, D. (2012). The hypothesis of a continuum in suicidality: a discussion on its validity and practical implications. Mental Illness, 4, 73–78. 10.4081/mi.2012.e15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tal‐Young, I. , Iglewicz, A. , Glorioso, D. , Lanouette, N. , Seay, K. , Ilapakurti, M. , & Zisook, S. (2012). Suicide bereavement and complicated grief. Dialogues in Clinical Neuroscience, 14, 177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troister, T. , D'Agata, M. T. , & Holden, R. R. (2015). Suicide risk screening: Comparing the Beck Depression Inventory‐II, Beck Hopelessness Scale, and Psychache Scale in undergraduates. Psychological Assessment, 27, 1500–1506. 10.1037/pas0000126 [DOI] [PubMed] [Google Scholar]
- Troister, T. , & Holden, R. R. (2012). A two‐year prospective study of psychache and its relationship to suicidality among high‐risk undergraduates. Journal of Clinical Psychology, 68, 1019–1027. 10.1002/jclp.21869 [DOI] [PubMed] [Google Scholar]
- Verrocchio, M. C. , Carrozzino, D. , Marchetti, D. , Andreasson, K. , Fulcheri, M. , & Bech, P. (2016). Mental pain and suicide: a systematic review of the literature. Frontiers in Psychiatry, 7, 108. 10.3389/fpsyt.2016.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO] (2014). Preventing suicide: A global imperative. Retrieved from: https://www.who.int/mental_health/suicide‐prevention/exe_summary_english.pdf [Google Scholar]
- World Health Organization [WHO] (2019). Suicide. Geneva, Switzerland: WHO. Retrieved from: https://www.who.int/en/news‐room/fact‐sheets/detail/suicide [Google Scholar]
- Wrobleski, A. (2002). Suicide Survivors: A guide for those left behind. Minneapolis, MN: SAVE. [Google Scholar]
- Zhang, S. , Tao, F. , Wu, X. , Tao, S. , & Fang, J. (2016). Low health literacy and psychological symptoms potentially increase the risks of non‐suicidal self‐injury in Chinese middle school students. BMC Psychiatry, 16(1). 10.1186/s12888-016-1035-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available on request.


