Abstract
Background
The COVID-19 pandemic has seen a rapid increase in the use of telehealth to deliver services to autistic individuals and their families. Research into the provision of autism assessments via telehealth is limited and few studies have explored clinician perspectives of conducting diagnostic assessments for autism in this way. The objective of this study was to examine the acceptability of a new telehealth model from the perspective of key stakeholder groups in an Australian community-based sample i.e. clients undergoing assessment, parent/carers and expert clinicians.
Methods
Sixteen adult clients (Mage = 39.00, SDage = 14.39) and fifty-six parent/carers of children and adults (Mage = 44.09, SDage = 9.87) undergoing autism assessments completed an online survey about their experiences of assessments via telehealth. Of these, six clients and twelve parent/carers agreed to participate in follow up interviews. Seven clinicians were also interviewed.
Results
In this study, the majority of adults and parent/carers reported that they, or the person they cared for, felt comfortable interacting with the clinician, would be willing to undergo future assessments via telehealth and were not concerned that important information had been missed during the assessment. Although the clinicians were slightly less satisfied with tele-assessment process compared to face-to-face and relied on external sources of information more than they would during a face-to-face assessment, their overall confidence in their diagnostic decision making remained high.
Conclusion
Autism assessment via telehealth may be an acceptable alternative in some circumstances. However, a telehealth service should consider screening clients for suitability and adequately preparing clients for tele-assessments.
Keywords: Autism, Assessment, Diagnosis, Telehealth, Covid-19
1. Introduction
The COVID-19 pandemic is impacting the daily lives of most people around the world. The pandemic is also changing how support is provided to autistic individuals and their families. A recent survey conducted by the Simons Foundation Powering Autism Research for Knowledge (SPARK) on the impact of COVID-19 on American families with autistic children found that by mid-2020 35 % of 8000 families were receiving services and interventions via telehealth (SPARK, 2020). Telehealth is “the provision of health care remotely by means of a variety of telecommunication tools, including telephones, smartphones, and mobile wireless devices, with or without a video connection” (Dorsey & Topol, 2016, p. 154). In addition to providing a means of service delivery in crises such as the current pandemic, telehealth increases access to health care for people in specific circumstances such as for those with low mobility or residing in rural locations (Brown, 2013). Telehealth service provision can also reduce the cost of health care, support referral pathways, and facilitate faster access to expert services for autistic people (Daschle & Dorsey, 2015; Stainbrook et al., 2019). Options to increase provision of timely assessment services are critically important, as delayed diagnosis results in delays to early intervention. Early diagnosis also facilitates access to funding and support services for the family and reduces the frustration and stress that often accompanies long delays in accessing an accurate diagnosis (Rabba, Dissanayake, & Barbaro, 2019; Zwaigenbaum et al., 2015).
Aside from the practical advantages, there may be particular aspects of telehealth service provision that are beneficial for autistic people and their families. An assessment provided in the home may be less stressful for autistic children and adults who often struggle with changes to routine and sensory aspects of the environment (Boulter, Freeston, South, & Rodgers, 2014; Horder, Wilson, Mendez, & Murphy, 2014; Kerns et al., 2014). Many autistic people have an affinity for technology and screen-based devices (Hedges, Odom, Hume, & Sam, 2018; Kuo, Orsmond, Coster, & Cohn, 2014) and may find engaging in a telehealth environment less intimidating than an in-person interaction (Mazurek & Wenstrup, 2013). Autistic individuals have also been shown to view communication via the internet as aiding comprehension, reducing emotional, social and time pressures, and offering more control over communication compared to face to face interactions (Benford & Standen, 2009; Gillespie-Lynch, Kapp, Shane-Simpson, Smith, & Hutman, 2014).
Researchers have conducted studies to examine the feasibility, reliability, and validity of services such as diagnostic assessments, early intervention and therapy via telehealth for supporting autistic individuals. Sutherland, Trembath, and Roberts (2018) conducted a systematic review of telehealth provision for autism services for children and adults and found that outcomes were largely positive and equivalent to those achieved via face-to-face services. However, the majority of research has been focused on delivery of therapy rather than diagnostic assessments (Valentine et al., 2021). The use of telehealth for autism diagnoses has been investigated in three studies. Reese et al. (2013) found no significant difference in diagnostic accuracy or ratings on diagnostic tools between assessments delivered via telehealth and assessments delivered in-person in a sample of pre-school aged children previously diagnosed with either autism or a developmental delay. They also found no difference in parent satisfaction for assessments delivered in person compared to telehealth (Reese et al., 2013, 2015). Shutte et al. (2015) found that there was substantial agreement on diagnostic classification according to Module 4 of the Autism Diagnostic Observation Schedule (Lord, Rutter, DiLavore, & Risi, 2008) between assessments delivered in-person and assessments delivered via telehealth for adults. Participant satisfaction was also found to be high.
Studies to date have been conducted in research centres, limited to very young children (under 5 years old) or adults with previous diagnoses of autism. Acceptability and satisfaction in relation to telehealth assessments has focused on client or parent perspectives (Reese et al., 2013, 2015; Shutte et al., 2015). There is little known about expert clinicians’ experiences of administering an autism assessment via telehealth and developing a diagnostic formulation without any face-to-face contact with the person undergoing assessment.
Clinicians’ experiences of telehealth autism assessments are important when considering whether telehealth meets ethical standards of clinical practice, assessing the validity of the assessment process, and ensuring assessments can be administered effectively in community settings. Sufficient clinician knowledge, skills and confidence in using telehealth are necessary for telehealth assessments to be delivered according to professional standards (Australian Psychological Society, 2007). For telehealth autism assessments specifically, clinicians’ views on whether telehealth delivery provides them with sufficient opportunity to assess autistic symptomatology (for example, quality of joint attention), and whether telehealth allows adequate client-clinician engagement are likely to impact clinician confidence. Practical issues such as technology quality and availability of necessary resources for clinicians to conduct telehealth assessments are also indicators of feasibility.
In Australia, strict social distancing guidelines were put in place in late March 2020 as a result of the COVID-19 pandemic (Australian Government Department of Health, 2020), which led to the cessation of most face-to-face autism assessment services across the country at that time. In order to continue offering services for the duration of the pandemic, Autism Spectrum Australia’s specialist assessment service developed a novel telehealth model of service delivery. This assessment service is a tertiary referral service conducting assessments for children (from 18 months), adolescents and adults. Telehealth assessments were offered as an option to all referred clients and their families from March 2020 onwards. This afforded a unique opportunity to examine acceptability of diagnostic assessments provided via telehealth in a community based setting across a broad age range. The objective of this study, therefore, was to examine the acceptability of autism assessments via telehealth from the perspectives of all key stakeholder groups, i.e., adults undergoing assessment, their family members and expert clinicians involved in the delivery of autism assessments.
2. Method
2.1. Participants
Participants for this study were recruited from a tertiary referral autism assessment service based in Sydney, Australia. A total of 163 tele-assessments was conducted between March and October 2020. Adult participants and parents/carers of children and adults who underwent telehealth assessment for autism between March 2020 and October 2020 were recruited via email approximately two weeks after the assessment date. Clinicians were also invited to participate in an interview via email three months after commencement of telehealth assessments. Participants were 16 adults aged between 21 and 76 years (62.5 % F, M = 39 yrs, SD = 14.39) and 56 parent/carers between 26 and 69 years of age (91 % F, M =44.09 yrs, SD = 9.87). Parent/carers reported on assessments for their child, or person they cared for, who was aged between 2 and 60 years of age (33 % F, M = 13.08 yrs, SD = 11.32) (see Table 1 for demographics). Seven clinicians were also recruited into the study via email invitation. All clinicians were employed as diagnosticians with Aspect’s specialist assessment team (duration of service ranging from 1 year to 8.5 years, M = 4.5 years). Clinicians were all registered psychologists and six of the seven clinicians had Masters level training in either educational/developmental psychology (1), neuropsychology (1) or clinical psychology (4). All clinicians had received formal training on autism assessment tools including the Autism Diagnostic Observation schedule – 2nd Edition (ADOS-2) (Lord, Luyster, Gotham, & Guthrie, 2012) and the Autism Diagnostic Interview-Revised (ADI-R) (Le Couteur, Lord, & Rutter, 2003).
Table 1.
Adult and parent/carer demographics.
| Adult participants (n = 16) | Parent/carer participants (n = 56) | |
|---|---|---|
| Age (Mean, SD) | 39 (14.39) | 44.09 (9.87) |
| Age of person assessed (Mean, SD) | n/a | 13.08 (11.32) |
| Gender | 10 F; 6 M | 51 F; 5 M |
| Gender of child assessed | n/a | 19 F; 36 M |
| Ethnicity n (%) | ||
| Aboriginal | 1 (6 %) | 5 (9 %) |
| Caucasian | 13 (82 %) | 45 (80 %) |
| Asian | 1 (6 %) | 4 (6 %) |
| European | 1 (2 %) | |
| Hispanic | 1 (2 %) | |
| Middle Eastern | 1 (6 %) | 2 (4 %) |
| Highest level of education n(%) | ||
| Completed primary school | 2 (4 %) | |
| Completed Year 10 (School Certificate or equivalent) | 3 (18 %) | 7 (13 %) |
| Completed Year 12 (High School Certificate or equivalent) | 2 (13 %) | 6 (11 %) |
| Trade / apprenticeship | 2 (4 %) | |
| Certificate or diploma | 2 (13 %) | 18 (32 %) |
| Undergraduate studies at university | 4 (25 %) | 8 (14 %) |
| Postgraduate studies at university | 5 (31 %) | 13 (22 %) |
2.2. Design and procedure
Ethics approval for this study was provided by Griffith University Research Office (HREC number 2020/692). The telehealth assessments were conducted over one day by one of the seven clinicians and consisted of the same four components as an in-person assessment i.e. review of background information prior to assessment, clinical observational assessment of the child/adult, structured interview conducted with parent/carer or other informant and feedback session. The structured interview (ADI-R) and feedback session were identical to an in-person assessment with the exception of being delivered via telehealth rather than face-to-face. However, the clinical observational assessment which during an in-person assessment is the appropriate ADOS module, could not be delivered in a standardised way via telehealth. Instead, five clinical observational protocols were developed with activities based on ADOS activities. Those activities that required engaging in play with the clinician in Modules 1, 2 and 3 were modified so that parents could be coached to administer the activities as the clinician observed for the relevant behaviours. Parents were provided with a list of toys required for the activities prior to the assessment day. Activities that were conversational in nature were undertaken by the clinician via telehealth.
Clients who expressed an interest in participating in the study were provided with a link to an online questionnaire via email and gave informed consent prior to completing the questionnaire. The questionnaire took approximately 10 min to complete and was hosted by SurveyMonkey between March and October 2020. At the end of the questionnaire, clients were given the option to provide their contact details if they wished (via a separate online form) to be invited to participate in a follow-up interview. Six adult clients and 17 parents and carers agreed to be interviewed. All seven clinicians who conducted autism assessments were also interviewed. The 2nd author conducted the semi-structured interviews, which lasted between 20−30 min and were held between March and September 2020. The interviews were conducted via Zoom or phone according to the preferences of the participant. Interviews were audio-recorded.
2.3. Measures
Two questionnaires were used (one for adult participants and one for parent/carer participants). The information gathered from each questionnaire was identical, with only minor wording changes to suit the respondent’s profile, i.e. adult self-report versus parent/carer report. Questionnaires included demographic and diagnostic information, level of experience with using video-conferencing technology, any technical difficulties experienced during the assessment and items from a Satisfaction Survey used in two previous studies of autism assessment by telehealth (Reese et al., 2013; Shutte et al., 2015). Participants responded to three statements on a 5-point Likert scale from strongly agree to strongly disagree in relation to level of comfort interacting with the clinician, being able to say and do things online as they would in person and willingness to have an assessment via telehealth in the future.
The semi-structured interviews for adults and parent/carers consisted of open-ended questions about the positive and negative aspects of the assessment experience (see supplementary materials). They were asked to describe their experience, including what they thought had worked well and what had not worked well. They were also asked whether they would recommend a telehealth assessment and to elaborate on reasons as to why or why not. Clinicians were asked to compare telehealth delivery to standard in-person assessment in terms of ease of administration and interpretation for each component of the assessment (clinical observation, developmental interview with parent/carers, diagnostic formulation, provision of feedback of assessment results). Clinicians also rated their confidence (on a scale from 1 to 100) in conducting assessments via telehealth and face-to-face.
2.4. Data analysis
Quantitative analyses of survey and interview responses were conducted in relation to client experience with technology, technical aspects of the assessment, client satisfaction ratings and clinician confidence ratings.
Interview recordings were transcribed with filler words such as “um” removed to aid readability. The interview transcripts were thematically analysed using the six-step process outlined by Braun and Clarke (2013). The research team aimed to present the experiences of participants in a more realist and descriptive way, hence only the semantic coding technique was implemented. Additionally, sub-themes and themes were identified through an inductive approach (bottom up).
To start the thematic analysis, the 2nd author, who conducted the interviews, read the transcripts to re-familiarise with the data. Once transcripts were read, relevant pieces of interview data were coded by the 2nd author to answer the objective of the study. Coding was completed via NVivo 12 software. Once the coding of all transcripts was completed, the 2nd author identified patterns of codes to generate an initial set of sub-themes and themes. The 1st and 2nd authors first reviewed the themes and sub-themes, then resolved any discrepancies and decided on a final set of themes and sub-themes.
3. Results
3.1. Client satisfaction
Client participants responded to three Likert style questions relating to their, or their child’s, comfort interacting with the clinician, ability to convey important information during the assessment and willingness to have future assessments conducted online (Table 2 ). Approximately one-third of participants felt that there were important things that they, or their child, were unable to do or say online that they would have been able to do or say in person (27.2 % of parent/carers; 37.5 % of adults). The majority of participants reported that they, or their child, felt comfortable interacting with the clinician (79.6 % of parent/carers; 81.3 % of adults) and that they would be willing to undergo future assessments online (67.8 % of parent/carers; 62.6 % of adults).
Table 2.
Satisfaction ratings for adults and parent/carers.
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
|---|---|---|---|---|---|
| I (or the person I care for) felt comfortable interacting with the clinician online | |||||
| Parent/carer clients | 19 (35.2 %) | 24 (44.4 %) | 6 (11.1 %) | 2 (3.7 %) | 3 (5.6 %) |
| Adult clients | 6 (37.5 %) | 7 (43.8 %) | 3 (18.8 %) | 0 | 0 |
| There were important things that I (or the person I care for) was unable to do or say online that I/he/she would have been able to do or say in person | |||||
| Parent/carer clients | 0 | 15 (27.2 %) | 23 (41.8 %) | 10 (18.2 %) | 7 (12.8 %) |
| Adult clients | 0 | 6 (37.5 %) | 2 (12.5 %) | 5(31.3 %) | 3 (18.8 %) |
| If I (or the person I care for) had to have assessments in the future I would be willing to (have him/her) do the assessment online | |||||
| Parent/carer clients | 19 (33.9 %) | 19 (33.9 %) | 10 (17.9 %) | 6 (10.7 %) | 2 (3.6 %) |
| Adult clients | 1 (6.3 %) | 9 (56.3 %) | 4 (25 %) | 1 (6.3 %) | 1 (6.3 %) |
Client participants also responded to four Likert style questions relating to the quality and clarity of the video and audio, and how experienced they were with various technology (see Table 3 ). All but two client participants reported that the quality and clarity of the audio and video were acceptable during tele-assessment. All but one client participant reported that they were experienced or very experienced using technology such as computers, smartphones and apps, with the majority (90 %) reporting that they were also familiar with videoconferencing apps.
Table 3.
Technology experiences for adults and parent/carers.
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |
|---|---|---|---|---|---|
| The quality and clarity of the video (picture) was acceptable | |||||
| Parent/carer clients | 31 (55.4 %) | 24 (42.9 %) | 0 | 1 (1.7 %) | 0 |
| Adult clients | 6 (37.5 %) | 9 (56.3 %) | 0 | 1 (6.3 %) | 0 |
| The quality and clarity of the audio (sound) was acceptable | |||||
| Parent/carer clients | 33 (59.0 %) | 21 (37.6 %) | 1 (1.7 %) | 1 (1.7 %) | 0 |
| Adult clients | 7 (43.8 %) | 7 (43.8 %) | 1 (6.3 %) | 1 (6 %) | 0 |
| Very experienced | Somewhat experienced | Not experienced at all | |
|---|---|---|---|
| How experienced are you in using computers, smart phones, and apps? | |||
| Parent/carer clients | 32 (57.2 %) | 23 (41.1 %) | 1 (1.7 %) |
| Adult clients | 10 (62.5 %) | 6 (37.5 %) | 0 |
| How experienced are you with videoconferencing technology such as Zoom, Skype or Facetime? | |||
| Parent/carer clients | 19 (33.9 %) | 32 (57.2 %) | 5 (8.9 %) |
| Adult clients | 9 (56.3 %) | 5 (31.3 %) | 1 (12.5 %) |
Approximately one third of client participants (n = 22, 30.6 %) reported experiencing some level of technical difficulty during the assessment including poor internet connection and lags in audio and/or video. Nine participants (12.5 %) reported that the technical difficulties impacted the assessment to some extent.
3.2. Clinician confidence
During interviews, clinicians were asked to rate their confidence in delivering telehealth assessments compared to face-to-face assessments (see Table 4 for confidence ratings). All clinicians expressed feeling equally confident about their administration of the interview component. Overall, clinicians reported feeling somewhat less confident in conducting the observational component of the assessment. There was more variability in clinician confidence ratings for the observational component of the assessment –some felt less confident assessing younger children via telehealth.
Table 4.
Clinician confidence ratings of interview and observational components of tele-assessment.
| Interview component |
Observational component |
|||
|---|---|---|---|---|
| Face-to-face | Telehealth | Face-to-face | Telehealth | |
| Clinician 1 | 95 % | 95 % | 95 % | 95 % |
| Clinician 2 | 100 % | 100 % | 100 % | 65 % (younger children) to 100 % (adults) |
| Clinician 3 | 98 % | 98 % | 100 % | 98 % |
| Clinician 4 | 90 % | 90 % | 80 % | 80 % |
| Clinician 5 | 90 % | 90 % | 90 % | 65 % |
| Clinician 6 | 100 % | 100 % | 95 % | 80 % (younger children) to 95 % (adults) |
| Clinician 7 | 100 % | 100 % | 100 % | 90 % (younger children) to 95 % (adults) |
3.3. Thematic analysis results
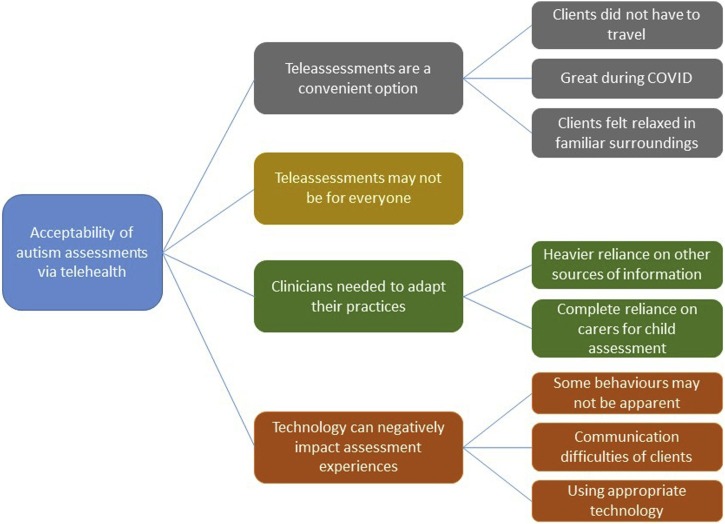
To investigate the acceptability of autism assessments via telehealth, adults undergoing assessment, family members and expert clinicians involved in the delivery of autism assessments, were interviewed about their telehealth experiences. We identified four themes and associated sub-themes (see Fig. 1 ).
Fig. 1.
Acceptability of autism assessments.
3.3.1. Tele-assessments are a convenient option
All three stakeholder groups considered tele-assessments to be a convenient option. The convenience of being assessed in the comfort of the clients’ own homes was especially relevant during the COVID-19 pandemic.
“I think given the circumstances, I think that's as good as it really gets, I suppose. Especially during the COVID-19 times, it's quite handy to be able to do the assessment over the video call.” (Adult #1)
“Because it's very convenient as we're kind of stuck at home and not encouraged to go out at the moment. So this is a very good solution for us.” (Adult #5)
“I think I would recommend telehealth assessments during a COVID-19 situation, definitely. It's better to have the assessment by telehealth rather than not have it. (Carer #8)
The opportunity to have an assessment within a familiar environment meant clients felt comfortable and relaxed at home.
“For me personally, I think it was good to be able to do this from the comfort of my own home. It made me a little bit more relaxed, and not over anxious or sort of, you know, thinking too much about how the day was going to progress so it was, yeah, it was in my familiar surroundings. So that was a really good thing for me personally.” (Adult #6)
“It is a lot more relaxed when the children are in their own environment. I think that's a plus.”(Carer #7)
“If they're more used to online, or they feel more comfortable online, because it's less threatening for them, it's less anxiety-provoking for them. And so, I think it fits them better” (Clinician #3)
In addition to enabling assessments to be conducted during the pandemic, the clinicians thought the ability of tele-assessments to support regional participants or participants who need to travel long distances was advantageous.
“I think particularly for regional families, families that are not close to a centre. It's so easy. And that's the feedback that I got from a lot of the families that we did telehealth, it just so happened that they were from regional areas. And at the end of the assessment all of them said this is preferable. Not having to travel. Most of them would usually stay overnight. The child is usually very dysregulated when they turn up to the centre and they've been in the car for two, three hours, so that can often be a problem. So this is a real advantage that you get to kind of see, see them when they're more regulated.” (Clinician #1)
“I think what I really see as a big positive is the ability to reach families that would otherwise not be able to come to the clinic and get an assessment. They could be waiting for months and months and months, might require travel at some cost that not everybody can afford, so the child or client goes without. I think that's probably the biggest plus I see, is the outreach ability, I think.” (Clinician #2)
3.3.2. Technology can negatively impact assessment experiences
Although clients, carers and clinicians shared mostly positive technology experiences, they also described some instances where technology negatively impacted on their assessment experience. All three stakeholder groups expressed concerns that some important aspects of client behaviour may not be as apparent to the clinician in a telehealth assessment. There was a perception from clients and carers that subtle behavioural characteristics that might be important for clinicians to observe may not have been apparent when their view was limited to what could be seen on the screen.
“I guess it might be a little bit limiting, you know, as you can only see what's on the screen. So you're not sort of, not from my perspective, but from the person observing me, they can't see the whole picture. So they can't see my body language or anything like that, that might sort of, help in the assessment.” (Adult #6)
“Some of his mannerisms, when he gets under distress, he does tend to…stand up and, turn around and do a little circle. So it's not really that noticeable. But he does do that occasionally and under that circumstance that wouldn't have been noticed.” (Carer #3)
“I think in a different environment, he might've engaged differently…I think there would be a lot more distractions.” (Carer #12)
Similarly, clinicians described some challenges with the administration of assessment items via telehealth and not being able to accurately make judgements about behaviours of interest. Clinicians found that verbal and/or conversation skills were the easiest skills to assess, whereas all clinicians found that eye contact was the most difficult behaviour to observe via videoconferencing.
“I think the hardest thing was the eye contact because I guess the client is not really engaging in eye contact at all. They're looking at you on the screen, not in the camera. So that was challenging.” (Clinician #1)
“Eye contact is a bit harder to guage, depending on the camera. Because, sometimes the child is actually looking at the screen, but the camera is elsewhere on the computer.” (Clinician #5)
“Joint attention was quite difficult. It was something I had to ask the parents about a little bit when it came to that.” (Clinician #4)
Some adult clients reported difficulties associated with communicating via telehealth, which impacted their assessment experience. The communication difficulties were largely related to reading other people’s body language and turn-taking, not being able to use compensatory strategies they had developed, and feeling self-conscious about viewing themselves or their own behaviour on the screen.
I also find it hard, like reading, I guess, those body cues and language, to be able to know sort of when I should step in and answer the question or if I should pause. I find that a little bit harder online.” (Adult #3)
“I have a habit of talking over people anyway, but when you're face-to-face, you've got that bit of time delay…you could sort of take turns a little bit better…That's probably why I've found it a little bit more difficult. I wasn't sure when I was ready to respond or when I should be responding when the next question sort of finished. That was the only thing, but that's only because it's online.” (Adult #6)
“So I've learnt ways to like, if I lean against something or if I'm holding a pen or like diverting their attention to something I'm doing in the environment. So they're not noticing that I'm not looking at them, whereas online, I can't do those things. So it's very obvious that I'm not looking at the person online. And so I was already quite uncomfortable with that.” (Adult #2)
“I became very aware I can see myself. Like, right now, half of my screen is out, I can get this feedback, I can see myself doing the actions. I become very conscious of the actions I'm doing, which I'm not sure helps the assessment.” (Adult #4)
The use of inappropriate technology such as using phones rather than computer/laptop/iPad negatively impacted the assessment experience of clients and clinicians.
“I've had people use their phones rather than a computer. And it's tough. I'm tiny on the screen…I don't think it's really very good if the only access they have is a phone…But it's not, for me, not being able to see what's happening. It's more that the client isn't really seeing you.. So maybe they're not referring back to you.” (Clinician #2)
“I've had one adult face-to-face assessment…for someone who was overseas, and this was the first case where they actually didn't have the Zoom set up through like a laptop or iPad. They only had their mobile…So the major component of the assessment was the observation, but that was done through a mobile phone which is just really not a great quality observation. That was quite challenging.” (Clinician #4)
“I had one parent trying to do it on a phone, that just doesn't work. The screen is so tiny, the child can't see. They have to have an iPad or a computer because if they're a significantly hyperactive child, it doesn't work because they're not going to stay in the one spot in front of the phone. I think, first, they need to have appropriate technology, doing it on a phone is not appropriate for [behavioural observations]. The child, especially if they need to view pictures and things on the screen, it's way too small.” (Clinician #6)
Using appropriate technology in an optimal manner was also very important, for example, even when clients used laptops/computers/iPads, issues with camera angles sometimes prevented clinicians from making accurate observations.
“It's just harder to sometimes see everything that's going on. You may miss little bits and pieces, the camera is in a fixed location and the child's moving around. Obviously depending on how far away they are from the screen, the audio might not be as strong. There's those sort of factors.” (Clinician #4)
“I guess the other challenge is more about what you're able to see through the camera, so if there were ways that we could set up or have things that made it clearer in terms of seeing the room that they were in.” (Clinician #5)
3.3.3. Clinicians needed to adapt their practices
In order to assess clients via telehealth, clinicians needed to adapt their usual assessment practices. The assessments conducted for younger children were perceived to be more difficult because they required more involvement from parents and parental coaching was needed.
“Adults were definitely the easiest and then followed by older children with good language…I think it's the age of the client as well as the tasks being able to be pretty much entirely done over telehealth.” (Clinician #2)
“For older children and adults, I actually found it pretty similar to what we would do in face-to-face, so there wasn't a lot of modifications or variations around that.” (Clinician #5)
For child assessments, clinicians talked about relying less on their own observations and needing to be more reliant on supplementary sources of information from clients’ parents, teachers, and doctors in order to reach a diagnostic conclusion.
“I think the only thing that's hard diagnostically when you're looking at the autism criteria is…the non-verbal category. I found myself being more reliant on the parent information and information from other sources to kind of get a read on that. Everything else generally I found diagnostically I could gather.” (Clinician #1)
“I think I spoke a little bit earlier about with the younger children, if they were not particularly easy diagnostically, that over telehealth I felt like I could rely on my own observations a bit less than I would rely on my own observations if I had them face-to-face. I'd say, I think I could see that it could be a bit of a difficulty with some of those cases. I don't think I would have the same concerns with older children or adults.” (Clinician #2)
“Probably the only thing is in those cases where I feel slightly less confident in my observations, then I have to rely on other information, maybe a little bit more than I would ordinarily.” (Clinician #7)
For child assessments, clinicians identified the importance of the level of preparation of parents/carers prior to the tele-assessment, as assessments tended to flow better when parents/carers were well prepared and organized.
“I don't think this is a typical experience because the parents were extremely prepared and proactive. But for them it was quite easy. She had organized each of the sections into tubs. All I would have to say is, we're going to move to section now and she would be like, ok, no problem and then we'd get that stuff out. And I had both parents too, so that was really helpful. She was super organized. Yeah. So for me, I found that to be really helpful, but I can imagine that if I didn't have a client that was as proactive that it would be problematic.” (Clinician #1)
“I had a family that was completely unprepared. We managed to get through it, it was absolutely fine. Diagnostically, no problem. It was just, they weren't very organized. Actually, I've done two now I think… It was still just more difficult.” (Clinician #2)
Clinicians reported that the parents’ abilities to be coached and understand instructions impacted the quality of child tele-assessments and the degree of difficulty in conducting the assessments.
“I think one of the challenges was having to remind parents not to coach the child…. sometimes parents would do things like directing the child more than you would like in an observational assessment.” (Clinician #4)
“[some] parents didn't really listen to your instruction and would go a few steps ahead or would point when you asked them not to point…some parents listen brilliantly. I'd only give short instructions at a time. Others, they're those parents that have a tendency to take over. You get that in face-to-face as well though. But I guess you can control for more of the clinician-led activities when you're in face-to-face. Whereas, sometimes the parents went a little bit rogue.” (Clinician #6)
3.3.4. Tele-assessments may not be for everyone
Based on clinician feedback, it seems that tele-assessments are most suitable for youth and adult clients.
“I think it's great for adults, and the older teenagers who won't get out of bed or the ones who are more anxious. So, I think it helps them.” (Clinician #3)
Clinicians identified certain client types of clients for whom tele-assessments may not be suitable, including younger children with mild symptoms, children with ADHD and those with moderate or severe challenging behaviours.
“I would say some of the kids that were quite hyperactive made it difficult because they wouldn't stay in front of the camera or they'd go other places and you had to try and move around with them.” (Clinician #5)
“I had another child and trying to get him to sit in front of the computer, it ended up taking us an hour and 45 min and it's usually 45 min. Whereas, in the clinic that's easier to control. You can have some toys there and give them a break and then use visual schedules.” (Clinician #6)
Similarly, some carers thought that an online setting was not the best option for assessing their children.
“[Son] has moderate to severe difficulties in both areas of development relating to autism so for telehealth, it presented a bit of a challenge because he wasn't really engaging with the screen. We found the same with his therapy, while his occupational therapist and speech were conducting telehealth sessions, we had very limited engagement with the therapist over the screen. So it made it very difficult.” (Carer #10)
4. Discussion
By integrating feedback from three key stakeholder groups who had participated in a novel telehealth assessment model developed in response to COVID-19 restrictions, this study aimed to examine the acceptability of telehealth assessments for children and adults from the perspectives of both clients and clinicians in a community-based sample. In this study, the majority of adults and parent/carers reported that they, or the person they cared for, felt comfortable interacting with the clinician, would be willing to undergo future assessments via telehealth and were not concerned that important information had been missed during the assessment. Many participants appreciated the comfort and convenience of having an assessment in the home setting. These findings are consistent with previous research involving preschool-aged children and adults (Reese et al., 2013; Shutte et al., 2015; Stainbrook et al., 2019) and provide further evidence of the general acceptability of telehealth assessments from a client perspective across a broad age range.
Although the overall feedback from clients was positive, a number of factors were identified that impacted on client satisfaction with the process. Adult clients were concerned about communication difficulties in the online environment, particularly using and reading body language and feeling self-conscious about seeing themselves on-screen. For both adult clients and parents/carers, concerns were raised in relation to clinicians possibly missing subtle aspects of behaviour that may not be as apparent via a screen. A number of practical concerns were also raised i.e. parents having difficulty supporting their child to complete assessment activities and technical difficulties that impacted the smooth running of the assessment. These findings are consistent with telehealth research conducted with the general population. For example, in terms of communication difficulties, some users of videoconferencing systems are self-conscious about their image and can be distracted by seeing their own video (de Vasconcelos Filho, Inkpen, & Czerwinski, 2009). Health professionals have identified non-verbal communication skills such as using empathetic gestures as an important interpersonal skill in telehealth delivery (Henry, Ames, Block, & Vozenilek, 2018). Technology difficulties such as internet problems have also been reported by clinicians as a drawback to tele-assessments (Kemp et al., 2021; Sutherland, Hodge, Chan, & Silove, 2021).
At the time of writing, to the authors’ knowledge, this is the first study to examine the acceptability of autism assessments via telehealth from the perspective of clinicians. Clinicians (as well as clients) thought tele-assessments were a convenient option for clients. Clinicians also reported that telehealth allowed regional participants or participants who need to travel long distances to be assessed. Even prior to the pandemic, telehealth services improved access to healthcare for people living in rural and remote areas of Australia (Bradford, Caffery, & Smith, 2016). Clinicians were expert diagnosticians with significant face-to-face assessment experience. They felt that they needed to adapt their practices for tele-assessments, including less reliance on their own observations and heavier reliance on supplementary sources of information and parents for child assessments. Research has consistently shown that adaptations of clinical practices are required to support clients or patients via telehealth (Malandraki, Arkenberg, Mitchell, & Malandraki, 2021; Waller et al., 2021), and assessments for some conditions such as chronic pain require additional involvement from the clients or patients (e.g., Perez, Niburski, Stoopler, & Ingelmo, 2021). A number of specific challenges related to telehealth delivery for autism assessments were identified by clinicians, including administration difficulties with eye contact being most challenging to assess. Assessments of younger children were more challenging in general than those involving older children or adults.
Despite these challenges and modifications to clinical practice, most clinicians still reported a high degree of confidence in conducting telehealth assessments. A recent survey of Australian healthcare professionals on how they adapted to telehealth during the pandemic showed that confidence to use telehealth increased with practice (Taylor et al., 2021). Prior to the COVID-19 pandemic, telehealth assessments for autism were largely viewed as an option for families living in regional and remote locations only, allowing them access to expert clinicians and reducing the cost of health care and additional travel for these families (Reese et al., 2015). However, our findings indicate that telehealth assessments may provide an acceptable option in other circumstances, including those that lead to restrictions on in-person assessment due to public health concerns.
Not only are telehealth assessments useful during a pandemic due to public health concerns, providing adult clients and families with the option of telehealth or some form of blended model for autism assessment post-pandemic is likely to improve accessibility. Lewis (2017) explored the barriers to formal autism diagnosis in adults and identified high cost (including cost of appointment and travel) and lack of access to autism specialists as two of the main barriers. Cost has also been identified as a major barrier to autism diagnosis in other studies (e.g., Huang, Arnold, Foley, & Trollor, 2021). The limited accessibility of adult assessment can lead to adults self-diagnosing, a prevalent yet controversial phenomenon in online autistic communities (Sarrett, 2016). Offering clients autism assessments via telehealth can reduce the cost of assessments and improve access to autism specialists living in different places. These findings have a number of implications for clinical practice in the delivery of telehealth autism assessments. When considering telehealth as an alternative to face-to-face assessments, a screening process that includes a pre-assessment interview or discussion about the assessment process and technology requirements should be undertaken. This would enable clients and parents/carers to make informed choices on the assessment delivery mode that best suits them. For example, our sample mentioned difficulties with using mobile phones which suggests that telehealth assessments may be best conducted using computers or laptops rather than mobile telephones. In addition, as technical difficulties also impacted assessments for some clients in this study, familiarity with the technology to be used may also be an important consideration. Both clinician and parent/carer clients noted the importance of parent preparation and involvement. It is important that parents are made aware of the assessment process and their role in it so that they are willing and able to provide the support needed to assist the clinician in the administration aspects of the assessment. Supporting documentation in writing for clients and parents/carers about what to expect and what is required for telehealth autism assessments is important, with documentation in easy-read language and other formats. Supporting documentation could include instructions on how to set-up videoconferencing cameras with a diagram. Rapport building could also be enhanced during a pre-assessment interview or discussion by providing an opportunity for the assessing clinician to meet briefly in an online environment with the person to be assessed or their family members outside of the formal assessment environment.
Concerns related to the observation of behaviours relevant to an autism assessment were expressed by all key stakeholder groups. To enhance the assessment of behaviours that are more challenging to assess via telehealth (for example, eye contact and joint attention), supplementary background information could be requested by clinicians prior to telehealth assessment sessions. This could be in the form of naturalistic videos of social behaviours. Alternatively, parent/carers could be primed to closely observe their children in the lead up to the assessment by providing information prior to assessment about behaviours of concern. During observational assessments of younger children, it would be helpful for clinicians to take time to provide adequate instruction to parents/carers when assessing younger children, and for clinicians to explain to parents/carers the purpose of each activity to improve their understanding. As in face-to-face autism assessments, it is important for clinicians to ask parents/carers of children how typical their child’s behaviour was in the assessment, however, the feedback from clinicians in this sample would suggest that this is even more important in telehealth assessments.
This study has a number of limitations. A small sample size was utilised, and this applies to the adult and clinician participant groups in particular, therefore the quantitative results should be interpreted with caution. Participants were recruited from a tertiary assessment service with clinicians who specialise in the diagnosis of autism and so findings may not generalise to other community-based teams. Clients paid a fee for autism assessments and so the sample could overly represent clients from a high socio-economic background. Data was not collected from clients or parents/carers who declined a telehealth assessment and opted to wait for a face-to-face assessment to be conducted and so it is unknown what factors influenced their decision or their demographic characteristics. These limitations mean that the results of the current study may not generalise to the broader population.
Further research on the acceptability of telehealth autism assessments could involve a more diverse sample with clients and clinicians recruited from a range of services in the community. Collecting data on the co-occurring conditions of clients would inform the acceptability of telehealth autism assessments for clients who present with complex presentations such as severe mental illness or complex trauma. Finally, further research to develop evidence based assessment tools that are suitable for telehealth assessments is needed to ensure reliability of diagnostic decisions made via telehealth.
CRediT authorship contribution statement
Vicki Gibbs: Conceptualization, Methodology, Formal analysis, Writing - original draft. Ru Ying Cai: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft. Fiona Aldridge: Methodology, Writing - review & editing. Michelle Wong: Conceptualization, Methodology, Writing - review & editing.
Declaration of Competing Interest
Authors VG, RYC and FA are currently employed by the organisation that provided the telehealth assessment service. Author MW has no competing or potential conflicts of interest.
No. of reviews completed is 2
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.rasd.2021.101859.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Australian Government Department of Health . 2020. COVID-19 national health plan – Primary care package – MBS telehealth services and increased practice incentive payments.https://www.health.gov.au/resources/publications/COVID-19-national-health-plan-primary-care-package-mbs-telehealth-services-and-increased-practice-incentive-payments April 3, Retrieved from. [Google Scholar]
- Australian Psychological Society . 2007. Code of ethics. Melbourne, Vic. [Google Scholar]
- Benford P., Standen P. The internet: a comfortable communication medium for people with Asperger syndrome (AS) and high functioning autism (HFA)? Journal of Assistive Technologies. 2009;3(2):44–53. doi: 10.1108/17549450200900015. [DOI] [Google Scholar]
- Boulter C., Freeston M., South M., Rodgers J. Intolerance of uncertainty as a framework for understanding anxiety in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2014;44(6):1391–1402. doi: 10.1007/s10803-013-2001-x. [DOI] [PubMed] [Google Scholar]
- Bradford N., Caffery L., Smith A. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural and Remote Health. 2016;16(3808) doi: 10.22605/RRH3808. [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. Sage; London: 2013. Successful qualitative research: A practical guide for beginners. [Google Scholar]
- Brown E.M. The Ontario Telehealth Network: A case report. Telehealth and e-Health. 2013;19(5):373–376. doi: 10.1089/tmj.2012.0299. [DOI] [PubMed] [Google Scholar]
- Daschle T., Dorsey E.R. The return of the house call. Annals of Internal Medicine. 2015;162(8):587–588. doi: 10.7326/M14-2769. [DOI] [PubMed] [Google Scholar]
- de Vasconcelos Filho J.E., Inkpen K., Czerwinski M. Image, appearance and vanity in the use of media spaces and videoconference systems. International ACM conference on Supporting group work (group 2009) 2009 https://www.microsoft.com/en-us/research/wp-content/uploads/2016/02/Image_Appearance_Group2009.pdf Retrieved from. [Google Scholar]
- Dorsey E.R., Topol E.J. State of telehealth. The New England Journal of Medicine. 2016;375:154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- Gillespie-Lynch K., Kapp S.K., Shane-Simpson C., Smith D.S., Hutman T. Intersections between the autism spectrum and the internet: Perceived benefits and preferred functions of computer-mediated communication. Intellectual and Developmental Disabilities. 2014;52(6):456–469. doi: 10.1352/1934-9556-52.6.456. [DOI] [PubMed] [Google Scholar]
- Hedges S.H., Odom S.L., Hume K., Sam A. Technology use as a support tool by secondary students with autism. Autism. 2018;22(1):70–79. doi: 10.1177/1362361317717976. [DOI] [PubMed] [Google Scholar]
- Henry B.W., Ames L.J., Block D.E., Vozenilek J.A. Experienced practitioners’ views on interpersonal skills in telehealth delivery. The Internet Journal of Allied Health Sciences and Practice. 2018;16(2) [Google Scholar]
- Horder J., Wilson C.E., Mendez M.A., Murphy D.G. Autistic traits and abnormal sensory experiences in adults. Journal of Autism and Developmental Disorders. 2014;44(6):1461–1469. doi: 10.1007/s10803-013-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Arnold S.R.C., Foley K., Trollor J.N. Choose your own adventure: Pathways to adulthood autism diagnosis in Australia. Journal of Autism and Developmental Disorders. 2021 doi: 10.1007/s10803-021-05169-4. [DOI] [PubMed] [Google Scholar]
- Kemp M.T., Liesman D.R., Williams A.M., Brown C.S., Iancu A.M., Wakam G.K., et al. Surgery provider perceptions on telehealth visits during the COVID-19 pandemic: Room for improvement. Journal of Surgical Research. 2021;260:300–306. doi: 10.1016/j.jss.2020.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns C.M., Kendall P.C., Berry L., Souders M.C., Franklin M.E., Schultz R.T., et al. Traditional and atypical presentations of anxiety in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2014;44(11):2851–2861. doi: 10.1007/s10803-014-2141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo M.H., Orsmond G.I., Coster W.J., Cohn E.S. Media use among adolescents with autism spectrum disorder. Autism. 2014;18(8):914–923. doi: 10.1177/1362361313497832. [DOI] [PubMed] [Google Scholar]
- Le Couteur A., Lord C., Rutter M. Western Psychological Services; Los Angeles, CA: 2003. Autism diagnostic interview-revised. [Google Scholar]
- Lewis L.F. A mixed methods study of barriers to formal diagnosis of autism Spectrum disorder in adults. Journal of Autism and Developmental Disorders. 2017;47(8):2410–2424. doi: 10.1007/s10803-017-3168-3. [DOI] [PubMed] [Google Scholar]
- Lord C., Luyster R.J., Gotham K., Guthrie W. Western Psychological Services; Torrance, CA: 2012. Autism diagnostic observation schedule, second edition (ADOS-2) manual. [DOI] [Google Scholar]
- Lord C., Rutter M., DiLavore P., Risi S. Western Psychological Services; Los Angeles: 2008. Autism diagnostic observation schedule: ADOS manual. [Google Scholar]
- Malandraki G.A., Arkenberg R.H., Mitchell S.S., Malandraki J.B. Telehealth for dysphagia across the life span: Using contemporary evidence and expertise to guide clinical practice during and after COVID-19. American Journal of Speech-Language Pathology. 2021;30(2):532–550. doi: 10.1044/2020_AJSLP-20-00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek M.O., Wenstrup C. Television, video game and social media use among children with ASD and typically developing siblings. Journal of Autism and Developmental Disorders. 2013;43(6):1258–1271. doi: 10.1007/s10803-012-1659-9. [DOI] [PubMed] [Google Scholar]
- Perez J., Niburski K., Stoopler M., Ingelmo P. Telehealth and chronic pain management from rapid adaptation to long-term implementation in pain medicine: A narrative review. PAIN Reports. 2021;6(1):e912. doi: 10.1097/PR9.0000000000000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabba A.S., Dissanayake C., Barbaro J. Parents’ experiences of an early autism diagnosis: Insights into their needs. Research in Autism Spectrum Disorders. 2019;66 doi: 10.1016/j.rasd.2019.101415. [DOI] [Google Scholar]
- Reese R.M., Jamison R., Wendland M., Fleming K., Braun M.J., Schuttler J.O., et al. Evaluating interactive videoconferencing for assessing symptoms of autism. Telehealth and e-Health. 2013;19(9):671–677. doi: 10.1089/tmj.2012.0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reese R.M., Jamison R., Braun M.J., Wendland M., Black W., Hadorn M., et al. Brief Report: Use of Interactive Television in Identifying Autism in Young Children: Methodology and Preliminary Data. Journal of Autism and Developmental Disorders. 2015;45(5):1474–1482. doi: 10.1007/s10803-014-2269-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarrett J.C. Biocertification and neurodiversity: The role and implications of self-diagnosis in autistic communities. Neuroethics. 2016;9:23–26. doi: 10.1007/s12152-016-9247-x. [DOI] [Google Scholar]
- Shutte J.L., McCue M.P., Parmanto B., McGonigle J., Handen B., Lewis A., et al. Usability and reliability of a remotely administered adult autism assessment, the autism diagnostic observation schedule (ADOS) module 4. Telehealth and e-Health. 2015;21(3):176–184. doi: 10.1089/tmj.2014.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons Foundation Powering Autism Research for Knowledge . 2020. Impact of COVID-19 on families and children with autism.https://d2dxtcm9g2oro2.cloudfront.net/wp-content/uploads/2020/04/03195500/spark-COVID-19-survey-results.pdf Retrieved from. [Google Scholar]
- Stainbrook J., Weitlauf A., Juárez A., Taylor J., Hine J., Broderick N., et al. Measuring the service system impact of a novel telediagnostic service program for young children with autism spectrum disorder. Autism: the International Journal of Research and Practice. 2019;23(4):1051–1056. doi: 10.1177/1362361318787797. [DOI] [PubMed] [Google Scholar]
- Sutherland R., Trembath D., Roberts J. Telehealth and autism: A systematic search and review of the literature. International Journal of Speech-Language Pathology. 2018;20(3):324–336. doi: 10.1080/17549507.2018.1465123. [DOI] [PubMed] [Google Scholar]
- Sutherland R., Hodge A., Chan E., Silove N. Clinician experiences using standardised language assessments via telehealth. International Journal of Speech-Language Pathology. 2021 doi: 10.1080/17549507.2021.1903079. [DOI] [PubMed] [Google Scholar]
- Taylor A., Caffery L.J., Gesesew H.A., King A., Bassal A., Ford K., et al. How Australian health care services adapted to telehealth during the COVID-19 pandemic: A survey of telehealth professionals. Frontiers in Public Health. 2021;9 doi: 10.3389/fpubh.2021.648009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine A., Hall S., Young E., Brown B., Groom M., Hollis C., et al. Implementation of telehealth services to assess, monitor, and treat neurodevelopmental disorders: Systematic review. Journal of Medical Internet Research. 2021;23(1):e22619. doi: 10.2196/22619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller G., Pugh M., Mulkens S., Moore E., Mountford V.A., Carter J., et al. Cognitive-behavioral therapy in the time of coronavirus: Clinician tips for working with eating disorders via telehealth when face-to-face meetings are not possible. International Journal of Eating Disorders. 2021;53(7):1132–1141. doi: 10.1002/eat.23289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwaigenbaum L., Bauman M.L., Stone W.L., Yirmiya N., Estes A., Hansen R.L., et al. Early identification of autism spectrum disorder: recommendations for practice and research. Pediatrics. 2015;136(Supplement 1):S10–S40. doi: 10.1542/peds.2014-3667C. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.