Abstract
Background
Faced with possible shortages due to COVID-19, many states updated or rapidly developed crisis standards of care (CSCs) and other pandemic preparedness plans (PPPs) for rationing resources, particularly ventilators.
Research Question
How have US states incorporated the controversial standard of rationing by age and/or life-years into their pandemic preparedness plans?
Study Design and Methods
This was an investigator-initiated, textual analysis conducted from April to June 2020, querying online resources and in-state contacts to identify PPPs published by each of the 50 states and for Washington, DC. Analysis included the most recent versions of CSC documents and official state PPPs containing triage guidance as of June 2020. Plans were categorized as rationing by (A) short-term survival (≤ 1 year), (B) 1 to 5 expected life-years, (C) total life-years, (D) “fair innings,” that is, specific age cutoffs, or (O) other. The primary measure was any use of age and/or life-years. Plans were further categorized on the basis of whether age/life-years was a primary consideration.
Results
Thirty-five states promulgated PPPs addressing the rationing of critical care resources. Seven states considered short-term prognosis, seven considered whether a patient had 1 to 5 expected life-years, 13 rationed by total life-years, and one used the fair innings principle. Seven states provided only general ethical considerations. Seventeen of the 21 plans considering age/life-years made it a primary consideration. Several plans borrowed heavily from a few common sources, although use of terminology was inconsistent. Many documents were modified in light of controversy.
Interpretation
Guidance with respect to rationing by age and/or life-years varied widely. More than one-half of PPPs, many following a few common models, included age/life-years as an explicit rationing criterion; the majority of these made it a primary consideration. Terminology was often vague, and many plans evolved in response to pushback. These findings have ethical implications for the care of older adults and other vulnerable populations during a pandemic.
Key Words: age, bioethics, COVID-19, crisis standards of care, critical care medicine, discrimination, medical ethics, rationing, resource allocation, triage
Abbreviations: CSC, crisis standards of care; DHHS, Department of Health and Human Services; OCR, Office for Civil Rights; PPP, pandemic preparedness plan; SOFA, Sequential Organ Failure Assessment
Take-home Points.
Study Question: How was age incorporated into US crisis standards of care and other state-level pandemic preparedness plans as a criterion for rationing access to intensive care during the 2020 wave of the COVID-19 pandemic?
Results: Of the 35 states that had promulgated formal pandemic preparedness plans during this time, 17 made age or the idea of maximizing the total number of life-years expected to be saved a primary rationing consideration. Seven considered only the chances for short-term survival regardless of age. Many states modified their plans in mid-course in response to allegations that their plans discriminated against disabled and older citizens.
Interpretation: There is ongoing disagreement about whether and how age ought to be incorporated into plans for rationing access to intensive care resources during a health crisis.
In 2009, at the height of the H1N1 influenza pandemic, the Institute of Medicine convened a committee to develop guidance for state and local public health officials. The committee defined “crisis standards of care” as the optimal “level of health and medical care capable of being delivered during a catastrophic event” (Institute of Medicine,1 p. 2). The committee’s report began the process of establishing which core elements should constitute crisis standards of care (CSC) documents and how they should be implemented. However, even before this report’s publication, states had been creating their own CSCs, and other types of pandemic preparedness plans (PPPs), in the form of triage guidelines to be implemented when a state-wide emergency was declared.2
Although to our knowledge only one US state PPP has been activated during the COVID-19 pandemic,3 the implementation of these plans has the potential to affect millions of people, and the extent to which guidelines may have been adopted by individual hospitals during the pandemic is not known. The rapid endorsement of protocols, with minimal public input in some cases, has raised ethical questions, and investigation of their various approaches to rationing is warranted.
For several decades, there have been warring philosophies among those studying resource allocation. Whereas some scholars hold that saving the most lives should be the ultimate goal of triage, other ethicists have focused on saving the most years of human life, a priority that takes many forms in the rationing literature.4 Whereas other studies have analyzed CSCs, with some focusing on the basic structure of plans, their foundational ethical values, and their concordance with Institute of Medicine guidance,2 , 5, 6, 7 our study provides a comprehensive look at every state PPP available at the time of our investigation, with a unique and detailed focus on the ethically controversial issue of how age and life-years are incorporated into triage schemes.
Methods
We began our analysis by coming to a consensus on the common definitions of three key phrases in the rationing literature. Life-years are calculated on the basis of a person’s remaining life expectancy.8 , 9 The life-cycles argument categorizes people on the basis of age brackets, giving priority to the young over the old.10 , 11 The fair innings principle establishes a single age cutoff beyond which one can be said to have had one’s “fair share” of life. In a crisis, those who have gotten their fair innings are excluded from, or at the very least deprioritized for, scarce resources.9 , 10 , 12
With these definitions in mind, we set out to clarify not simply whether these terms were used, but how these concepts were operationalized by state PPPs. Between April and June 2020, two members of our group (E. S. and K. Y. J.) conducted a Google search of publicly available online documents to identify CSCs or other PPPs. Initially, search terms included state names and “Crisis Standards of Care.” If that search did not yield obvious results (within the first 10 search results), alternative search terms included the state name and “rationing protocols,” “triage guidelines,” or “resource allocation.” Alternative types of PPPs were searched for by inputting a state name, followed by “Pandemic Influenza Plan” or “Emergency Operations Plan.” If necessary, state Department of Health or Office of the Governor websites were searched for COVID-19 rationing plans. Several key collections of CSCs were also queried to ensure no documents were missed.13, 14, 15
When no plan meeting the inclusion criteria was identified, the contact person for a state medical society or hospital association, the administrative contact in the state’s governor’s office, or an in-state ethicist known to the team was contacted directly via phone or email to inquire whether a state plan existed or was being drafted.
Plans were included in our analysis if they (1) were promulgated by one of the 50 US states and Washington, DC and (2) were either official, government CSC protocols that had been published in their final forms, or were other types of state-endorsed PPPs, such as pandemic influenza plans or emergency operations plans, that included specific triage guidance. Only the most recent version of each plan (as of June 2020) was included. Draft PPPs were not analyzed, nor were state-specific rationing plans that were not actually endorsed by the state-wide government (such as plans found that were independently produced by state medical societies). Instead, states with these guidelines were listed as having no plan, although precise notes were included in our database (e-Table 1).
The PPP documents fitting our inclusion criteria were then systematically reviewed and summarized on the basis of their fundamental triage schemes, including use of Sequential Organ Failure Assessment (SOFA) or other scores,16 longevity considerations, and tiebreaker criteria. Moreover, special attention was paid to the use of key terminology, including “life-years,” “life-cycles/stages,” and “fair innings.” Guidelines were then independently categorized by the two primary reviewers, based on the extent to which age/life-years was operationalized in each plan, as outlined (Table 1 ). Category A plans were those that considered only individuals’ likelihood of survival in the short term when triaging them for critical care resources. Category B plans considered a person’s next 1 to 5 expected life-years. Category C plans accounted for a person’s total anticipated number of life-years. Category D plans used the “fair innings” principle, creating specific age cutoffs for resources. Finally, category O plans did not provide specific guidance but, rather, general ethical frameworks for hospitals to follow. Any state protocol that considered age/life-years to some extent (ie, those falling into category B, C, or D) was further stratified on the basis of whether age/life-years was a primary consideration in the plan. Age/life-years was only considered a secondary consideration for a plan if it was included in tiebreaker criteria or explicitly designated as less than a primary consideration in multitiered triage schemes (eg, see Colorado in e-Table 1).
Table 1.
State Pandemic Preparedness Plan Categories Based on Use of Age/Life-Years
| Category | Definition |
|---|---|
| A. Short-term survival | Triage is based on expected effectiveness of treatment (ie, ≤ 1-y prognosis from admission). Many of these guidelines focus on SOFA score |
| B. One to five expected life-years | Triage is based on expected survival/prognosis beyond 1 y and up to 5 y from admission. Many of these guidelines exclude patients with conditions expected to impact their remaining life-years, such as NYHA class III HF, ALS, etc. |
| C. Total life-years | Triage considers the principle of life cycles (comparing individuals on the basis of age bracket), calculates individuals’ total expected life-years (based on age or prognosis in the long term), or prioritizes children over adults as a general rule |
| D. Fair innings | Triage involves any kind of age cutoff (the practical effect of the fair innings principle). Often these cutoffs are found in ICU exclusion criteria |
| O. Other | PPPs do not offer specific triage guidance, but instead provide general guiding ethical principles, or examples of several frameworks without a clear priority in endorsement |
ALS = amyotrophic lateral sclerosis; HF = heart failure; NYHA = New York Heart Association; PPP = pandemic preparedness plan; SOFA = Sequential Organ Failure Assessment.
When a plan seemed to fall into more than one triage category, often based on its primary vs secondary considerations, it was categorized according to the broadest set of considerations stipulated in the document (eg, given a category C designation, if both B and C applied). If a document did not mandate a detailed triage algorithm, but rather provided example strategies it endorsed, the plan was categorized according to what its authors deemed was permissible. If a plan merely mentioned an ethical principle (eg, fair innings), but then did not go on to employ that principle in its triage guidelines, the principle was not considered in the categorization of the plan; in every case, we paid attention to the implementation of triage criteria rather than the words used to describe them. When, as occurred in two or three instances, there was a disagreement concerning categorization, based on how two of the authors interpreted a plan’s text, three of our group members discussed the appropriate categorization and came to a consensus for each state.
During the categorization process for state PPPs, the authors noted any information obtained within the documents on the origin of their guidelines, as well as their reception by patient advocates. A subanalysis was performed for plans using the term “life-years” to determine the underlying meaning of the phrase in each case.
Results
PPPs by State
A triage or emergency protocol of some type was identified for every state and Washington, DC (Table 2 and e-Table 1). Sixteen guidelines had to be excluded from our analysis because they did not meet inclusion criteria (only existing in draft form, etc.).
Table 2.
State Pandemic Preparedness Plan Categorizationa
| Category | Stateb |
|---|---|
| A. Short-term survival | AL, CA, DE, IA, LA, NM, TN |
| B. One to 5 expected life-years | AK, IN, KS, MN, RI, UT, VT |
| C. Total life-years | AZ, CO, MA, MI, MO, MT, NC, NJ, NY, OK, OR, PA, WA |
| D. Fair innings | KY |
| O. Other | CT, IL, MS, NV, OH, VA, WY |
| No plan meeting inclusion criteria | EOP/PIP without triage guide (GA, ID, ME, NE, ND, SD) Not state-endorsed (AR, FL, SC, TX, WV, DC) CSC drafts (HI, MD, NH, WI) |
CSC = crisis standards of care; EOP = emergency operations plan; PIP = pandemic influenza plan.
If a state used age/life-years as a primary consideration for triage, its two-letter abbreviation is in boldface. (For plan details and links to documents, see e-Table 1 in the online article.)
Official two-letter US state name abbreviations are used for brevity.
Overall, 35 published, state-endorsed PPPs were identified, dating from 2007 through 2020. Seven fell into category A (short-term survival), seven into category B (1-5 expected life-years), 13 into category C (total life-years), one was considered category D (fair innings), and seven were labeled category O (other) (Table 2). All protocols were official CSCs, and most were written in 2020. Eleven plans (Connecticut, Indiana, Iowa, Kansas, Louisiana, Michigan, Mississippi, New Mexico, New York, Oregon, and Virginia) predated the pandemic, having been written from 2007 to 2019 (e-Table 1). Of the 21 states considering age/life-years to some extent in their plans (the sum of categories B, C, and D), 17 states used it as a primary consideration and four as a secondary one (Table 2).
Use of Age/Life-Years
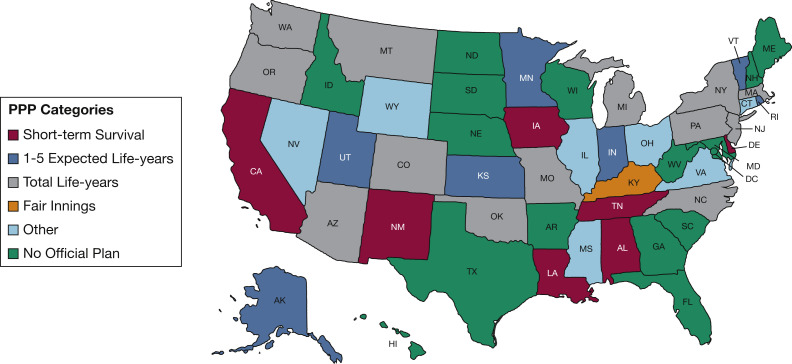
Figure 1 displays the categorizations listed in Table 2. Ultimately, we found that category A plans based on short-term survival were seen mainly in southern states, with the exception of Iowa and Delaware. Essentially, all of these plans advocated for triage based on a patient’s SOFA score, in an effort to represent their likelihood of survival to discharge (e-Table 1).
Figure 1.
State PPP use of age/life-years. PPP = pandemic preparedness plan.
Category B protocols, or those considering whether a patient was expected to have 1 to 5 life-years remaining postadmission, showed no specific geographic predisposition. These plans either specified chronic conditions that could limit 5-year survival as exclusion criteria, or included these comorbid conditions in triage scores so as to deprioritize these patients (e-Table 1).
Category C plans, or those using total life-years concepts, were similarly scattered. Many of these plans were based on one prototype from the University of Pittsburgh (as described below), which used a combination of SOFA score, comorbidities, and life-cycles considerations, giving priority to younger age groups over older (e-Table 1).
Only Kentucky fell into category D, using the fair innings principle. Although other states mentioned the term “fair innings” in the text of their guidelines, only Kentucky operationalized the use of a strict age cutoff, suggesting it would be permissible to exclude all patients over the age of 85 (e-Table 1).
Finally, category O/Other included plans scattered around the country. Typically, these plans were short documents that provided nonspecific triage guidance, such as general ethical principles and example frameworks, without endorsing one scheme over another. Almost one-half of these plans predated the pandemic (e-Table 1).
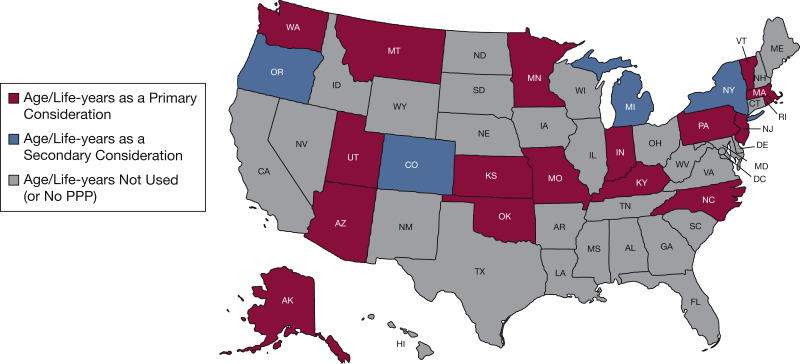
Emphasis on Age/Life-Years
States considering age/life-years in any way (categories B, C, and D) were then stratified on the basis of whether age or life-years was a primary consideration in their guidelines (Fig 2 ). Of the 21 state plans in this subanalysis, 17 plans made age/life-years a primary consideration, typically by factoring life-years maximization in some way into their exclusion criteria or primary triage score. In contrast, four state CSCs used age/life-years solely in the event that primary considerations, such as SOFA score/clinical status, led to ties in scoring (e-Table 1).
Figure 2.
State PPP emphasis on age/life-years as a primary or secondary consideration. PPP = pandemic preparedness plan.
Origin of Plans
Just as PPP content varied, so did protocol approval processes. Many states were found to have at least general triage protocols for health care resources before the COVID-19 pandemic, some of which represented years of public and committee input that was incorporated into the latest version of guidelines.17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36 Other states established expert committees to develop de novo guidelines only in 2020.37, 38, 39, 40, 41, 42 Still others chose to model their plans on preexisting guidelines.43, 44, 45, 46, 47, 48, 49, 50, 51 Three plans (by New York, Minnesota, and the University of Pittsburgh) were particularly influential on the PPPs endorsed by states (see “Notes” in e-Table 1).
The 2015 New York Ventilator Allocation Guidelines included triage based on SOFA score, exclusion criteria to reflect “immediate or near-immediate mortality” despite therapy (New York State Department of Health, New York State Task Force on Life and the Law,30 p. 14), and use of a measured “fair innings” approach to prioritize children over adults in case of ties (New York State Department of Health, New York State Task Force on Life and the Law,30 p. 105). These guidelines influenced a variety of rationing plans, including the Vermont CSC ventilator allocation scheme,51 and served as a prototype for category A PPPs in their primary focus on SOFA score and the short-term survival of patients.
Minnesota’s 2020 Patient Care Strategies for Scarce Resource Situations were based on consideration of SOFA score, duration of benefit (1- to 2-year prognosis), duration of need, and response to mechanical ventilation.27 These guidelines were copied into the Alaska CSC,43 and the Montana and Vermont plans were heavily influenced by them.46 , 51 The Montana CSC serves as an example for rationing guidelines considering 1- to 5-year expected survival.
Finally, the University of Pittsburgh Model Policy (the Model), which was finalized in the spring of 2020, was the most influential plan found. White and colleagues focused on “saving lives” and “saving life-years” (White et al,52 p. 6). To do so, they based their triage scheme on a patient’s SOFA score plus their expected survival beyond their acute illness. Life-cycles considerations were used to prioritize the younger over the older in case of ties.52 These guidelines ultimately served as a prototype for the total life-years category and went on to be fully adopted by the state of Pennsylvania.48 Subsequently, Massachusetts, Oklahoma, North Carolina, and New Jersey incorporated the Model into their plans,44 , 45 , 49 , 50 while the Arizona, Missouri, and Montana PPPs also highlighted the Model’s key principles.18 , 45 , 46 Despite widespread adoption, the University of Pittsburgh Model, as well as many of the plans it influenced, evolved significantly over a few months as a result of pushback from the community.
Operationalization of Terms
We categorized state plans according to whether the actual triage protocols were best described as operationalizing the concepts of life-years, fair innings, and so on, rather than whether the terms themselves were included in guidelines. This standard became necessary as there was little correlation found between the terms used and the actual triage schemes proposed (e-Table 1). As an example, Figure 3 offers a breakdown of the meaning of life-years maximization in the nine PPPs (mainly part of the Pittsburgh cohort) that used the term “life-years” in their guidelines. Ultimately, five of the plans (Colorado, Massachusetts, Missouri, Pennsylvania, and New Jersey) ended up only going so far as to consider 1- to 5-year survival,20 , 42 , 45 , 48 , 50 while two (Montana and North Carolina) used 10-year prognosis as a proxy for life-years maximization.46 , 49 New York, meanwhile, spoke of prioritizing children over adults (a life-cycles consideration),30 and Michigan proposed that age, quality-adjusted life-years (QALYs), or disability-adjusted life-years (DALYs) be used as a secondary consideration, invoking both the fair innings principle and the goal of life-years maximization for justification.32
Figure 3.
A comparison of operational definitions of life-years from nine state PPPs: what would it mean to maximize “life-years”? PPP = pandemic preparedness plan.
Critical Reception
Definitions were often changed in response to community feedback. During the spring of 2020, it became clear that there was a debate between PPP working groups and a loose coalition of ethicists and disability and elder rights advocates, with some of the latter parties writing letters to state leaders and even having cases opened with the Department of Health and Human Services Office for Civil Rights (OCR).53, 54, 55, 56 As an example, Disability Rights Pennsylvania wrote a letter to Governor Wolf of Pennsylvania53 and filed a complaint against the state with the OCR, stating that an early draft of Pennsylvania’s guidelines discriminated against those with preexisting disabilities by factoring in their expected life-years rather than their “individualized assessment of immediate-term survivability” (Darr,54 p. 5). The draft protocol that Disability Rights Pennsylvania rejected57 was based on the version of the University of Pittsburgh Model then being promoted by its originators, which considered a patient’s SOFA score as well as any “major comorbid conditions with substantial impact on long-term survival,” providing examples of illnesses expected to impact 10-year prognosis (White et al,58 p. 6). As a result of the complaint, Pennsylvania modified its guidelines to explicitly consider only survival up to 5 years postadmission in its primary triage criteria. In addition, the state added a nondiscrimination statement and removed any mention of specific comorbidities.48 Ultimately, the OCR resolved its complaint against Pennsylvania,59 , 60 and several states followed suit in modifying their plans,56 although the concept of maximizing life-years remained widespread.
Discussion
Most Plans Considered Age/Life-Years as an Explicit Triage Criterion
Rationing health care by age and its various congeners has been controversial for decades.8 , 11 , 61, 62, 63, 64, 65, 66 Our primary objective was to determine to what extent age/life-years was considered in state PPPs that were ready to be used during the COVID-19 pandemic. Our protocol categorized plans considering short-term projected survival up to 1 year as rationing based on treatment effectiveness rather than age. Plans invoking prognosis for 1 to 5 expected life-years (based on comorbid conditions) or explicitly invoking total life-years/related concepts or fair innings were categorized as rationing by age/life-years. We found that 60% of plans (21 of 35) invoked rationing by age/life-years; moreover, for 81% of these plans (17 of 21), age and/or life-years were primary considerations (Figs 1 and 2).
Several Plans Had a Few Common Origins
Several state plans were found to be heavily influenced by a few preexisting frameworks, in particular the widely circulated Pittsburgh Model Policy.52 This finding is unsurprising, given that the majority of plans identified were written or updated in 2020, as the pandemic began to worsen. Despite an efficient drafting process, many of these plans required adaptation over time due to public criticism or federal investigations (e-Table 1).
Imprecise Language Abounded
Vague and imprecise language about age and rationing was used throughout many plans. In particular, the term “life-years,” a central concept that was adapted into several PPPs based on the University of Pittsburgh Model, was operationalized in four different ways in the nine plans that used it. As states attempted to navigate their own PPP approval processes, their plans’ varying use of terms created (and continues to create) opportunities for confusion in the implementation and regulation of triage schemes, confounding the already fraught act of prognosis estimation (Fig 3).
Pushback Has Been Significant
Finally, pushback against rationing by age/life-years has been significant, and civil rights complaints were filed in several states by marginalized groups such as the elderly and disabled (who often have fewer expected life-years).54, 55, 56 Even though some changes have been made to plans (with Arizona resolving a complaint with the OCR as recently as May 25, 2021),56 the debate rages on, with the OCR opposing any use of a patient’s “long-term life expectancy” in allocation decisions.67 All of this suggests that a more comprehensive and inclusive vetting process is needed to avoid policy mistakes and the unjust exclusion of certain groups.
Strengths and Limitations
We categorized plans to reflect the practical use of age and life-years in PPP guidelines, with a focus on the specifics of triage schemes. We believe this is a key strength of this study, given there was little correspondence between the actual meaning of triage algorithms and the terms used in protocols. Our method for tracking down protocols was rigorous, and we believe we have identified more plans than any previously published study; however, we cannot be sure that we have included all official PPPs active during the time of this analysis. In addition, we did not examine health care system or hospital-based protocols, nor did we include state-wide guidelines that were not government-endorsed. Finally, we did not examine actual practice and cannot comment on how plans would directly affect patient care.
Interpretation
In summary, we found that most rationing plans invoke the language of life-years or related concepts to incorporate longevity considerations, but triage by age cutoffs is uncommon. Imprecise use of language abounds, making analysis challenging. The use of certain terms, which might be taken as endorsement of particular ethical principles, ought not be equated with the meaning behind triage algorithms. Although several plans were widely circulated, ethical consensus is still lacking on the use of age/life-years to allocate critical care resources in the United States, as evidenced by the OCR complaints filed. Although OCR intervention has resulted in some changes to published PPPs, many retain the language of “life-years” or “life-cycles” and consider survival beyond the acute period of illness. Although only one of these plans has been invoked, plans that appear to be discriminatory, even if never used, can affect patient and public trust. Ultimately, both the vague endorsement of these principles, and the inclusion of life-years in the majority of available rationing guidelines in the United States, leave room for confusion, undue subjectivity, and perhaps even age- or disability-based discrimination in the implementation of guidelines. Such confusion or discrimination might worsen existing inequities in resource distribution should another COVID-19 surge (or another pandemic) lead to the deployment of these plans.
Acknowledgments
Author contributions: E. S. and D. P. S. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. E. S., K. Y. J., MK. G., B. P., and D. P. S. contributed substantially to the study design, data analysis and interpretation, and writing of the manuscript.
Financial/nonfinancial disclosures: None declared.
Additional information: The e-Table can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Supplementary Data
References
- 1.Institute of Medicine, Board on Health Sciences Policy, Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations . National Academies Press; Washington, DC: 2009. Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report. [PubMed] [Google Scholar]
- 2.Romney D., Fox H., Carlson S., Bachmann D., O’Mathuna D., Kman N. Allocation of scarce resources in a pandemic: a systematic review of US state crisis standards of care documents. Disaster Med Public Health Prep. 2020;14(5):677–683. doi: 10.1017/dmp.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brennan T. AZDHS activates crisis standards of care as COVID-19 surge leads to worries at Arizona hospitals. FOX 10 Phoenix. June 29, 2020 https://www.fox10phoenix.com/news/azdhs-activates-crisis-standards-of-care-as-covid-19-surge-leads-to-worries-at-arizona-hospitals Accessed December 6, 2020. [Google Scholar]
- 4.Gaurke M.K., Prusak B., Jeong K.Y., Scire E.M., Sulmasy D.P. Life-years and rationing in the COVID-19 pandemic: a critical analysis. Hastings Cent Rep. 2021;51(5):18–29. doi: 10.1002/hast.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cleveland Manchanda E.C., Sanky C., Appel J.M. Crisis standards of care in the USA: a systematic review and implications for equity amidst COVID-19. J Racial Ethn Health Disparities. 2021;8:824–836. doi: 10.1007/s40615-020-00840-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Margus C., Sarin R.R., Molloy M., Ciottone G.R. Crisis standards of care implementation at the state level in the United States. Prehosp Disaster Med. 2020;35(6):599–603. doi: 10.1017/S1049023X20001089. [DOI] [PubMed] [Google Scholar]
- 7.Piscitello G.M., Kapania E.M., Miller W.D., Rojas J.C., Siegler M., Parker W.F. Variation in ventilator allocation guidelines by US state during the coronavirus disease 2019 pandemic: a systematic review. JAMA Netw Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colvin-Adams M., Valapour M., Hertz M., et al. Lung and heart allocation in the United States. Am J Transplant. 2012;12(12):3213–3234. doi: 10.1111/j.1600-6143.2012.04258.x. [DOI] [PubMed] [Google Scholar]
- 9.White D.B., Katz M.H., Luce J.M., Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009;150(2):132–138. doi: 10.7326/0003-4819-150-2-200901200-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emanuel E.J., Wertheimer A. Who should get influenza vaccine when not all can? Science. 2006;312(5775):854–855. doi: 10.1126/science.1125347. [DOI] [PubMed] [Google Scholar]
- 11.Harris J. Routledge; London: 1985. The Value of Life: An Introduction to Medical Ethics. [Google Scholar]
- 12.Williams A. Intergenerational equity: an exploration of the “fair innings” argument. Health Econ. 1997;6(2):117–132. doi: 10.1002/(sici)1099-1050(199703)6:2<117::aid-hec256>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 13.Catholic Health Association of the United States State and state agency plans and guidelines. https://www.chausa.org/newsroom/coronavirus-resources/ethics/state-policies-for-covid-19 Updated April 6, 2020. Accessed December 26, 2020.
- 14.US Department of Health & Human Services ASPR Technical Resources, Assistance Center, and Information Exchange (TRACIE). State level crisis standards of care. April 9, 2020. https://files.asprtracie.hhs.gov/documents/4-9-20-state-level-csc-plans-guidance-policy.pdf Accessed October 28, 2020.
- 15.UNC Center for Bioethics State, national, and international organization guidelines. https://bioethics.unc.edu/state-national-and-international-organization-guidelines/ Updated August 4, 2020. Accessed October 31, 2020.
- 16.Vincent J.L., Moreno R., Takala J., et al. Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 17.Alabama Crisis Standards of Care Guidelines Work Group Alabama crisis standards of care guidelines: managing modified care protocols and the allocation of scarce medical resources during a healthcare emergency. February 28, 2020. https://www.adph.org/CEPSecure/assets/alabamacscguidelines2020.pdf Accessed December 28, 2020.
- 18.Arizona Department of Health Services COVID-19 addendum: allocation of scarce resources in acute care facilities recommended for approval by State Disaster Medical Advisory Committee (SDMAC). June 12, 2020. https://www.bannerhealth.com/-/media/files/project/bh/locations/banner-lassen/covid-19-addendum.ashx Accessed October 6, 2021.
- 19.California Department of Public Health California SARS-CoV-2 pandemic crisis care guidelines. June 2020. https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/COVID-19/California%20SARS-CoV-2%20Crisis%20Care%20Guidelines%20-June%208%202020.pdf Accessed December 28, 2020.
- 20.Colorado Subject Matter Experts Advisory Panel for the Governor’s Expert Emergency Epidemic Response Committee Crisis standards of care guidelines for hospitals for the COVID-19 pandemic. Version 2.0. April 26, 2020. https://georgetown.box.com/s/b38v3yok3lkoc7bze3mjwgik1deha7lw Accessed October 6, 2021.
- 21.Connecticut Department of Public Health, Standards of Care Workgroup Standards of care: providing health care during a prolonged public health emergency. October 2010. https://portal.ct.gov/-/media/Departments-and-Agencies/DPH/dph/legal/StandardsofCarefinalpdf.pdf Accessed December 29, 2020.
- 22.Illinois Department of Public Health Guidelines on emergency preparedness for hospitals during COVID-19. June 2020. https://www.dph.illinois.gov/sites/default/files/Guidelines%20on%20Emergency%20Preparedness.pdf Accessed December 29, 2020.
- 23.Indiana State Department of Health Crisis Standards of Care Community Advisory Group Crisis standards of patient care guidance with an emphasis on pandemic influenza: triage and ventilator allocation guidelines. April 2014. https://emeraldcoasthcc.org/sites/emeraldcoasthcc.site/files/indiana-crisis-standards-of-care-2014.pdf Accessed December 29, 2020.
- 24.Iowa Department of Public Health An ethical framework for use during a pandemic: report of the Iowa Department of Public Health Ethics Committee. September 2007. http://publications.iowa.gov/17889/1/panflu_ehtical_guidelines_manual.pdf Accessed December 29, 2020.
- 25.Kansas Department of Health and Environment Guidelines for the use of modified health care protocols in acute care hospitals during public health emergencies. Second revision. September 2013. https://www.kdheks.gov/cphp/download/Crisis_Protocols.pdf Accessed December 29, 2020.
- 26.Louisiana Department of Health, Emergency Support Function 8 Health & Medical Section State hospital crisis standard of care guidelines in disasters. Version 4.0. February 2019. https://bloximages.newyork1.vip.townnews.com/nola.com/content/tncms/assets/v3/editorial/3/03/30339376-84a4-11ea-a8d4-0f02d2e4e840/5ea0528be9f00.pdf.pdf Accessed December 29, 2020.
- 27.Minnesota Department of Health, Minnesota Health Care Preparedness Program Patient care strategies for scarce resource situations. Version 6.0. May 2020. https://www.health.state.mn.us/communities/ep/surge/crisis/standards.pdf Accessed December 28, 2020.
- 28.Mississippi State Department of Health Office of Emergency Planning and Response. Crisis standards of care. February 21, 2017. https://msdh.ms.gov/msdhsite/_static/resources/7221.pdf Accessed December 30, 2020.
- 29.New Mexico Department of Health, Epidemiology and Response Division New Mexico crisis standards of care plan. June 2018. https://www.nmhealth.org/publication/view/plan/4877/ Accessed December 30, 2020.
- 30.New York State Department of Health New York State Task Force on Life and the Law. Ventilator allocation guidelines. November 2015. https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf Accessed December 28, 2020.
- 31.Oregon Health Authority, Public Health Division Oregon crisis care guidance. June 2018. https://georgetown.box.com/s/whqonvb8tin88op6ksvx0c5phtuv3k2w Accessed December 28, 2020.
- 32.State of Michigan, Department of Community Health, Office of Public Health Preparedness Guidelines for ethical allocation of scarce medical resources and services during public health emergencies in Michigan. Version 2.0. November 2012. https://georgetown.box.com/s/90q5f4c2emi92niz37ql6wl85ntasnfb Accessed October 6, 2021.
- 33.State of Nevada, Department of Health and Human Services, Division of Public and Behavioral Health, Governor Sisolak’s Medical Advisory Team for the COVID-19 Response Crisis standards of care: crisis level guidance for COVID-19. April 2, 2020. https://nvhealthresponse.nv.gov/wp-content/uploads/2020/04/NV_DHHS_DPBH_CSCRecommendations_COVID-19_040220_ADA.pdf Accessed December 30, 2020.
- 34.Tennessee Altered Standards of Care Workgroup Guidance for the ethical allocation of scarce resources during a community-wide public health emergency as declared by the governor of Tennessee. Version 1.6. July 2016. https://www.tn.gov/content/dam/tn/health/documents/cedep/ep/Guidance_for_the_Ethical_Allocation_of_Scarce_Resources.pdf Updated June 10, 2020. Accessed December 30, 2020.
- 35.Troutman Sanders LLP (developed for the Virginia Department of Health) Critical resource shortages planning guide. September 2009. https://www.vdh.virginia.gov/content/uploads/sites/10/2019/01/VA-Critical-Resource-Shortages-Planning-Guide.pdf Accessed December 30, 2020.
- 36.Utah Hospital Association, Crisis Standards of Care Workgroup Utah crisis standards of care guidelines: COVID-19 annex. April 2020. https://georgetown.box.com/s/sm33r1aphmacjlhv1dd87y9mgxmo1xjx Accessed December 30, 2020.
- 37.Delaware Health and Social Services, Division of Public Health, Emergency Medical Services and Preparedness Section Crisis standards of care concept of operations. April 2020. https://www.centerforpublicrep.org/wp-content/uploads/2020/05/DE-CSC-ConOps-FInal-4-29-20.pdf Accessed December 28, 2020.
- 38.Kentucky Department for Public Health Crisis standards of care: guidance for the ethical allocation of scarce resources during a community-wide public health emergency. March 31, 2020. https://www.kyha.com/assets/docs/COVID19/Update/CrisisStandardsofCareFinal.pdf Accessed December 28, 2020.
- 39.Rhode Island Department of Health Crisis standards of care guidelines. April 27, 2020. https://health.ri.gov/publications/guidelines/crisis-standards-of-care.pdf Accessed December 28, 2020.
- 40.Ohio Department of Developmental Disabilities, Ohio Department of Health, and Ohio Department of Medicaid Guidance: COVID-19 standards of care for vulnerable populations. June 29, 2020. https://dodd.ohio.gov/wps/portal/gov/dodd/about-us/communication/news/news-guidance-covid-19-standards-of-care Accessed December 30, 2020.
- 41.Washington State Department of Health, Disaster Medical Advisory Committee Scarce resource management & crisis standards of care. March 2020. https://georgetown.box.com/s/ityh85u7vdwpf8l61o42j4564yovt5bm Accessed October 6, 2021.
- 42.Wyoming Department of Health, Public Health Division State Health Officer’s statewide instructions to health care providers and hospital ethics committee members. May 11, 2020. https://health.wyo.gov/wp-content/uploads/2020/05/SHOInstructionsCOVID19_May122020.pdf Accessed December 30, 2020.
- 43.Alaska Department of Health and Social Services, Division of Public Health, Rural and Community Health Systems Section Patient care strategies for scarce resource situations [adapted from Minnesota guidelines]. Version 1.0. March 2020. http://dhss.alaska.gov/dph/Epi/id/SiteAssets/Pages/HumanCoV/SOA_DHSS_CrisisStandardsOfCare.pdf Accessed December 28, 2020.
- 44.Commonwealth of Massachusetts, Executive Office of Health and Human Services, Department of Public Health, Crisis Standards of Care Advisory Working Group Crisis standards of care planning guidance for the COVID-19 pandemic. April 7, 2020. https://georgetown.box.com/s/tl6p5t8gb3vuazc8mdnbvoiyyovfg4q4 Revised April 20, 2020. Accessed December 28, 2020.
- 45.Missouri Hospital Association A framework for managing the 2020 COVID-19 pandemic response and implementing crisis standards of care. April 20, 2020. https://georgetown.box.com/s/zi2wp61iomzln83ej16b53muzfkmpk74r Accessed October 6, 2021.
- 46.Montana Department of Public Health and Human Services Scarce resource management & crisis care guidance. 2020. https://georgetown.box.com/s/fqv7uy9qtr71or5d58j5s3b6ne0urjni Accessed December 30, 2020.
- 47.Oklahoma State Department of Health Hospital crisis standards of care resource reference cards. April 7, 2020. https://www.ok.gov/health2/documents/Hospital%20Crisis%20Standards%20of%20Care.pdf Accessed December 28, 2020.
- 48.Pennsylvania Department of Health and the Hospital & Healthsystem Association of Pennsylvania Interim Pennsylvania crisis standards of care for pandemic guidelines. Version 2. https://www.health.pa.gov/topics/Documents/Diseases%20and%20Conditions/COVID-19%20Interim%20Crisis%20Standards%20of%20Care.pdf April 10, 2020. Accessed December 30, 2020.
- 49.Scarce Critical Care Resource Allocation Advisory Group North Carolina protocol for allocating scarce inpatient critical care resources in a pandemic. April 6, 2020. https://www.ncha.org/wp-content/uploads/2020/04/North-Carolina-Protocol-for-Allocating-Scarce-Inpatient-Critical-Care-Resources-in-a-Pandemic_FINAL-4-6-2020541-1.pdf Accessed December 28, 2020.
- 50.State of New Jersey Department of Health Allocation of critical care resources during a public health emergency (adapted from the University of Pittsburgh model policy). April 11, 2020. https://nj.gov/health/legal/covid19/FinalAllocationPolicy4.11.20v2%20.pdf Accessed December 28, 2020.
- 51.Vermont Department of Health Vermont crisis standards of care plan. Version 1.1. May 18, 2020. https://www.healthvermont.gov/sites/default/files/documents/pdf/Vermont%20CSC%20Plan%2005.18.2020.pdf Accessed December 30, 2020.
- 52.White D.B., Katz M., Luce J., Lo B. Allocation of scarce critical care resources during a public health emergency: executive summary. University of Pittsburgh Department of Critical Care Medicine. April 15, 2020. https://ccm.pitt.edu/sites/default/files/UnivPittsburgh_ModelHospitalResourcePolicy_2020_04_15.pdf Accessed December 30, 2020.
- 53.Radecic P.J., Darr K., Garman J., Disability Rights Pennsylvania A letter to Governor Wolf regarding medical rationing in Pennsylvania. March 27, 2020. https://www.disabilityrightspa.org/newsroom/a-letter-to-governor-wolf-regarding-medical-rationing-in-pennsylvania/ Accessed January 1, 2021.
- 54.Darr K. Re: Complaint of Disability Rights Pennsylvania concerning Pennsylvania’s interim crisis standards of care for pandemic guidelines. April 3, 2020. https://www.disabilityrightspa.org/wp-content/uploads/2020/04/s04.03.2020-DRP-OCR-Complaint-with-Exhibit-A-1.pdf Accessed January 9, 2021.
- 55.Williams L., Hyten A.S., Center C., Costanzo C., Mathis J., Crane S. RE: Complaint of disability discrimination filed by the Disability Rights Center of Kansas, the Topeka Independent Living Center, and Tessa Goupil. March 27, 2020. https://www.centerforpublicrep.org/wp-content/uploads/2020/03/Kansas-OCR-complaint-3.27.20-final.pdf Accessed January 1, 2021.
- 56.The Arc. HHS-OCR Complaints Re COVID-19 Medical Discrimination. March 23, 2020. https://thearc.org/resource/hhs-ocr-complaint-of-disability-rights-washington-self-advocates-in-leadership-the-arc-of-the-united-states-and-ivanova-smith/ Accessed January 1, 2021.
- 57.Pennsylvania Department of Health and the Hospital & Healthsystem Association of Pennsylvania Interim Pennsylvania crisis standards of care for pandemic guidelines. Version 1. March 22, 2020. https://int.nyt.com/data/documenthelper/6850-pennsylvania-triage-guidelines/02cb4c58460e57ea9f05/optimized/full.pdf Accessed January 9, 2021.
- 58.White D.B., Katz M.H., Luce J.M., Lo B. Allocation of scarce critical care resources during a public health emergency. University of Pittsburgh Department of Critical Care Medicine. March 26, 2020. https://georgetown.box.com/s/5hd9kx5q15kaywtjdjipt8ixh15nhby0 Accessed February 4, 2021.
- 59.Disability Rights Pennsylvania Civil rights complaint filed by Disability Rights Pennsylvania resulted in progress on Pennsylvania’s medical rationing guidelines. April 16, 2020. https://www.disabilityrightspa.org/newsroom/civil-rights-complaint-filed-by-disability-rights-pennsylvania-resulted-in-progress-on-pennsylvanias-medical-rationing-guidelines/ Accessed January 1, 2021.
- 60.HHS.gov OCR Resolves civil rights complaint against Pennsylvania after it revises its pandemic health care triaging policies to protect against disability discrimination. April 16, 2020. https://www.hhs.gov/about/news/2020/04/16/ocr-resolves-civil-rights-complaint-against-pennsylvania-after-it-revises-its-pandemic-health-care.html Accessed January 9, 2021.
- 61.Harris J. QALYfying the value of life. J Med Ethics. 1987;13(3):117–123. doi: 10.1136/jme.13.3.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roberts J.P. American Society of Transplant Surgeons letter to the OPTN Kidney Transplant Committee. December 18, 2008. https://asts.org/docs/default-source/optn-unos/proposed-kidney-allocation-concepts---asts-response-december-18-2008.pdf?sfvrsn=6 Accessed January 9, 2020.
- 63.Pandemic Influenza Ethics Initiative Work Group of the Veterans Health Administration’s National Center for Ethics in Health Care Meeting the challenge of pandemic influenza: ethical guidance for leaders and health care professionals in the Veterans Health Administration. July 2010. https://www.ethics.va.gov/docs/policy/meeting_the_challenge_of_pan_flu_ethical_guidance_vha_2010_web_posting_2013.pdf Accessed January 9, 2021.
- 64.Reese P.P., Caplan A.L., Bloom R.D., Abt P.L., Karlawish J.H. How should we use age to ration health care? Lessons from the case of kidney transplantation. J Am Geriatr Soc. 2010;58(10):1980–1986. doi: 10.1111/j.1532-5415.2010.03031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Organ Procurement and Transplantation Network Concepts for kidney allocation. February 16, 2011. http://media1.s-nbcnews.com/i/MSNBC/Sections/NEWS/z_Personal/AJohnson/110301_KidneyConceptDocument.pdf Accessed January 9, 2021.
- 66.Harris J. Why kill the cabin boy? Camb Q Healthc Ethics. 2021;30(1):4–9. doi: 10.1017/S0963180120000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.HHS.gov OCR provides technical assistance to ensure crisis standards of care protect against age and disability discrimination. January 14, 2021. https://www.hhs.gov/about/news/2021/01/14/ocr-provides-technical-assistance-ensure-crisis-standards-of-care-protect-against-age-disability-discrimination.html Accessed February 4, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.