Abstract
Acute lymphoblastic leukemia (ALL) is the most successful paradigm of how risk-adapted therapy and detailed understanding of the genetic alterations driving leukemogenesis and therapeutic response may dramatically improve treatment outcomes, with cure rates now exceeding 90% in children. However, ALL still represents a leading cause of cancer-related death in the young, and the outcome for older adolescents and young adults with ALL remains poor. In the past decade, next generation sequencing has enabled critical advances in our understanding of leukemogenesis. These include the identification of risk-associated ALL subtypes (e.g., those with rearrangements of MEF2D, DUX4, NUTM1, ZNF384 and BCL11B; the PAX5 P80R and IKZF1 N159Y mutations; and genomic phenocopies such as Ph-like ALL) and the genomic basis of disease evolution. These advances have been complemented by the development of novel therapeutic approaches, including those that are of mutation-specific, such as tyrosine kinase inhibitors, and those that are mutation-agnostic, including antibody and cellular immunotherapies, and protein degradation strategies such as proteolysis-targeting chimeras. Herein, we review the genetic taxonomy of ALL with a focus on clinical implications and the implementation of genomic diagnostic approaches.
Keywords: B-ALL, DUX4, IKZF1, PAX5, Ph-like, ZNF384, NUTM1, T-ALL, NOTCH1, BCL11B, transcriptome, genome
1. Introduction
Acute lymphoblastic leukemia (ALL) is the most frequent childhood tumor and despite cure rates now exceeding 90% in children, outcomes for older children and adults remain poor with cure rates below 40% in those over the age of 40 [1,2,3], despite pediatric-inspired chemotherapy regimens [4]. This discrepancy is in part attributable to the different prevalence of genetic alterations across age. ALL may be of B- (B-ALL) or T-lymphoid (T-ALL) lineage, and comprises over thirty distinct subtypes characterized by germline and somatic genetic alterations that converge on distinct gene expression profiles [5,6,7,8,9,10,11,12]. These subtypes are defined by disease-initiating recurrent chromosomal gains and losses (hyper- and hypodiploidy, and complex intrachromosomal amplification of chromosome 21); chromosomal rearrangements that deregulate oncogenes or encode chimeric fusion oncoproteins, importantly often including cryptic rearrangements not identifiable by conventional cytogenetic approaches, such as DUX4 and EPOR rearrangements; subtypes defined by single point mutations (e.g., PAX5 P80R or IKZF1 N159Y); subtypes defined by enhancer hijacking (e.g., BCL11B-rearrangements in T-ALL and lineage ambiguous leukemia) [5]; and subtypes that “phenocopy” established subtypes, with similar gene expression profile but different founding alterations (e.g., BCR-ABL1-like ALL and ETV6-RUNX1-like ALL) [7,13,14,15]. Secondary somatic DNA copy number alterations and sequence mutations are also important in leukemogenesis and treatment response, and their nature and prevalence vary according to the ALL subtype [6]. Multiple genes are associated with predisposition to ALL, including polymorphic variants in ARID5B, BAK1, CDKN2A, CDKN2B, CEBPE, ELK3, ERG, GATA3, IGF2BP1, IKZF1, IKZF3, LHPP, MYC, PTPRJ, TP63 and the BMI1-PIP4K2A locus or rare mutations in PAX5, TP53, IKZF1 and ETV6 [16]. Several are associated with ALL subtype, for example, variants in GATA3 have been associated with an increased risk of Philadelphia- like (Ph-like) ALL in patients of Hispanic ancestry [17], variants in TP63 and PTPRJ with ETV6-RUNX1 ALL [18] and in ERG with TCF3-PBX1 ALL and African American ancestry [19,20]. A variant in the deubiquitinase gene USP7 has been instead associated with risk of T-lineage ALL [19].
Accurate identification of the genetic abnormalities that drive ALL is important to risk stratify disease, and to guide the incorporation of molecular targeted therapeutic approaches to reduce the risk of relapse. This has been previously relied upon conventional karyotyping, fluorescence in situ hybridization (FISH) and targeted-molecular analyses. However, studies from this past decade have highlighted the importance of next generation sequencing (NGS) approaches to identify cryptic genetic rearrangements, structural DNA variation and gene expression signatures otherwise not identifiable that demand a revision of diagnostic approaches. This review describes the current genomic landscape of B- and T-ALL, highlighting their genetic characterization and diagnostic classification, clinical features, and therapeutic implications.
2. B-Cell Precursor Acute Lymphoblastic Leukemia
2.1. Previously Established Subtypes with Recurring Chromosomal Abnormalities
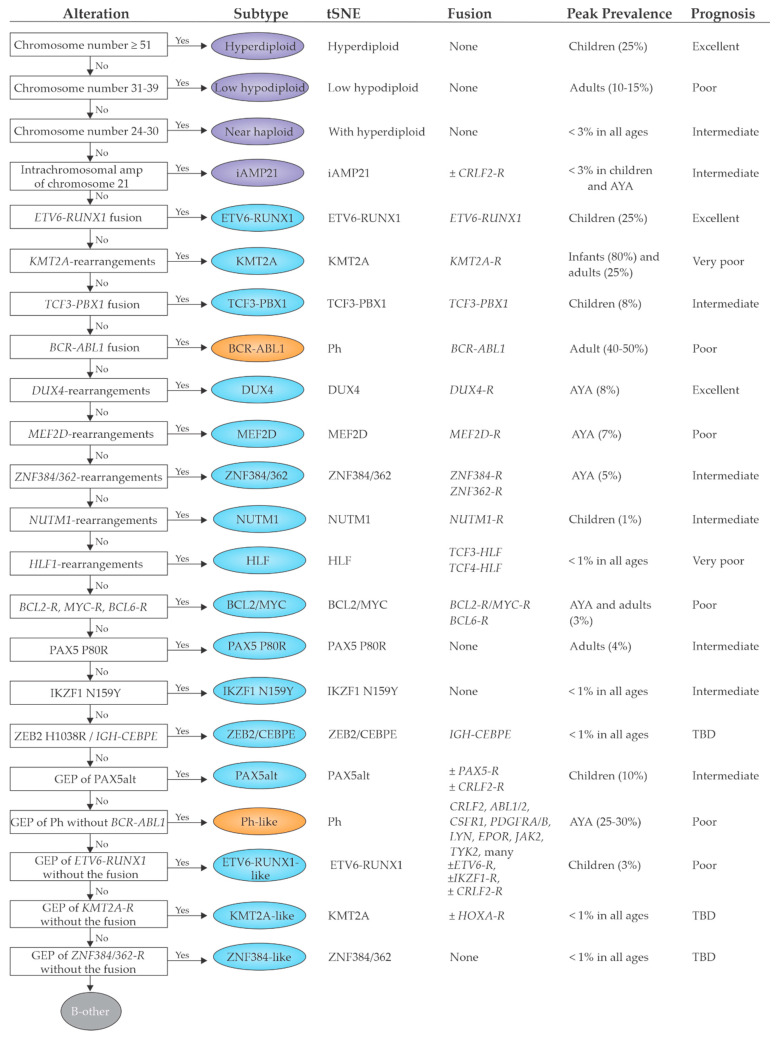
Prior the advent of NGS, classification of ALL has been relied on conventional karyotyping, FISH and targeted-molecular analyses for the identification of recurring chromosomal abnormalities including aneuploidy, chromosomal rearrangements and/or known gene fusions (Figure 1).
Figure 1.
This schematic algorithm for B-ALL subtyping was modified from the figure originally published in Paietta E. et al. Molecular Classification Improves Risk Assessment in Adult BCR-ABL1-negative B-ALL. Blood Prepublished Apr 25 2021; doi:10.1182/blood.2020010144 [83]. This figure describes each B-ALL subtype according to the specific genetic alterations and gene expression profile. Moreover, for each subtype peak prevalence and prognosis are shown. Subtypes are colored according to defining genetic alteration: gross chromosomal abnormalities (purple), transcription factor rearrangements (blue), other transcription factor alterations (blue), and kinase alterations (orange). Abbreviations: AYA, adolescent and young adult; tSNE, t-distributed stochastic neighbor embedding; TBD: to be defined; -R: rearranged.
2.1.1. Subtypes with Chromosomal Aneuploidy
Chromosomal aneuploidies [21], such as hyperdiploidy and hypodiploidy, are generally early initiating events acquired prenatally during fetal hematopoiesis and likely require secondary cooperating oncogenic insults to promote leukemia development [22].
High hyperdiploidy (modal number of 51–67 chromosomes, with nonrandom gains most commonly of chromosomes X, 4, 6, 10, 14, 17, 18, and 21) is present in 25–30% of ALL in children and is associated with young age (3–5 years) at diagnosis and favorable outcome [23,24]. Mutations of genes encoding mediators of Ras signaling (KRAS, NRAS, FLT3, PTPN11) and regulators of chromatin state (e.g., the histone 3 lysine 18 and 27 acetylase and transcriptional coregulator CREBBP, and the H3K36 methylase WHSC1) are frequent concomitant genetic events in high hyperdiploid ALL [23]. CREBBP mutations are enriched in the histone acetyl transferase domain and are selected during disease evolution [25]. As a potential mechanism for the generation of aneuploidy, hyperdiploid ALL blasts show a delay in early mitosis at prometaphase associated with defects in chromosome alignment, which lead to chromosome-segregation defects and nonmodal karyotypes [26]. Moreover, condensin complex activity is impaired, leading to chromosome hypocondensation, loss of centromere stiffness, and mislocalization of the chromosome passenger complex proteins Aurora B kinase (AURKB) and BIRC5 (survivin) in early mitosis [26]. Notwithstanding the favorable outcome of this subtype, condensin impairment suggests novel molecular targets (condensin-complex members, AURKB, or the spindle assembly checkpoint) for potential pharmacological intervention.
Hypodiploid ALL includes near haploid (24–31 chromosomes) and low hypodiploid (32–39 chromosomes) subtypes [27]. Near haploidy is present in ~2% of childhood ALL and is associated with Ras mutations (particularly NF1) and deletion/mutation of IKZF3. The gene expression profile and patterns of co-mutation (e.g., CREBBP and the Ras signaling pathway) are similar to high hyperdiploid ALL, suggesting a potential common origin of these two forms of leukemia. Low hypodiploidy instead is uncommon in children (~1%) but present in >10% of adults, and is characterized by deletion of IKZF2, RB1, CDKN2A/CDKN2B and near-universal mutations of TP53 mutations, which are inherited in approximately half of cases and indicate that low hypodiploid ALL is a manifestation of Li-Fraumeni syndrome [28]. Duplication of the aneuploid genome, resulting in clones with 50 to 78 chromosomes, is common, with duplicated subclones present in the majority of cases. Predominance of the duplicated clone, known as masked hypodiploidy, may be misdiagnosed as high hyperdiploidy [29]. However, these states may usually be distinguished as the duplicated hypodiploid genome typically exhibits diploid and tetraploid chromosomes; in contrast high hyperdiploidy is characterized by a mixture of triploid and some tetraploid chromosomes (e.g., chromosomes 21, X). Moreover, the pattern of chromosomal losses in hypodiploid ALL is not random and chromosome 21 is never lost indicating a central role in leukemic cell fitness [27]. Hypodiploid ALL is associated with unfavorable outcome, although this is mitigated by minimal residual disease (MRD) risk-stratified therapy in several studies [30]. Moreover, for patients who achieve MRD-negative status after induction, allogeneic transplantation has been shown to be not successful in improving overall survival [31,32]. Although MRD-oriented protocols, older adults and elderly patients with low hypodiploidy do fairly poor with higher five-year cumulative incidence of relapse compared to high hypodiploid cases [33], making them candidates for different treatment approaches (e.g., immunotherapy and targeted therapies). Among those, preclinical studies have shown that hypodiploid ALL cells are sensitive to Phosphoinositide 3-kinase (PI3K) and BCL2 Apoptosis Regulator (BCL2) inhibitors [27,34].
2.1.2. iAMP21
Intrachromosomal amplification of chromosome 21 (iAMP21) accounts for 1% of childhood ALL and is associated with older children (median age at diagnosis 9 years) and a low white cell count. Behind the formation of this chromosomal abnormality there is a characteristic mechanism of breakage–fusion–bridge cycles followed by chromothripsis and other complex structural rearrangements of chromosome 21 [35]. Two germline genomic alterations are associated with a markedly elevated risk of iAMP21. These are a germline Robertsonian translocation rob (15;21) and a germline ring chromosome 21 [36]. The presence of iAMP21 is associated with poor prognosis in most studies, although this has been improved with intensive treatment [37].
2.1.3. Subtypes with Recurrent Chromosomal Translocations and/or Gene Fusions
The t(12;21)(p13;q22) translocation with the ETV6-RUNX1 (TEL-AML1) fusion is the most common alteration in childhood B-ALL occurring in 20–25% of cases [38,39,40]. The ETV6-RUNX1 fusion is considered to be a leukemia-initiating alteration which arises in utero, as demonstrated by the identification in umbilical cord blood [39] and by the prenatal monoclonal origin in identical twins [41]. The typically prolonged latency from birth to clinically manifest leukemia indicates that ETV6-RUNX1 alone requires cooperating genetic events to induce leukemia, including deletion of the non-rearranged ETV6 allele, focal deletion of PAX5 and mutation of WHSC1 [39,42,43,44].
The t(1;19)(q23;p13) translocation encoding TCF3-PBX1 defines a subtype of 5–6% of pediatric B-ALL but only 1% of adult cases. This fusion is associated with a pre-B immunophenotype and expression of cytoplasmic immunoglobulin heavy chain and with higher peripheral blood white cell count at diagnosis [6,7,45]. Current intensive treatment has changed the historically high risk of TCF3-PBX1 childhood ALL that was in part ascribed to central nervous system (CNS) involvement and relapse in favorable and intermediate risk cases [46,47]. TCF3-PBX1 leukemic cells may be amenable to inhibition of pre-BCR signaling by dasatinib and ponatinib [48,49]. This approach may lead to compensatory upregulation of ROR1 expression, and thus, concomitant inhibition of ROR1 could enhance the sensitivity of dasatinib [50]. TCF3 and TCF4 are also rearranged to HLF, and define a rare subtype of ALL (<1%) associated with an extremely poor prognosis [3,7]. TCF3-PBX1 and TCF3-HLF ALL have distinct gene expression profiles and mutational landscapes [7,51]. TCF3-HLF ALL is associated with expression of stem cell and myeloid markers, alterations of PAX5 (deletions) and the Ras signaling pathway [7,51] and sensitivity to therapies inhibiting BCL2 and the pre-B cell receptor [52,53], immunologic therapies [54], and to Aurora A kinase inhibitors [55].
Rearrangements of the mixed-lineage leukemia 1 (MLL1) gene (now renamed Lysine [K]-specific methyl transferase 2A or KMT2A) on chromosome 11q23 to over 80 different partner genes define a subtype of leukemia with lymphoid and myeloid features and poor prognosis [12,56]. It occurs predominantly in infants (~80%), with a second peak of onset in adulthood where the most common partner of rearrangement is AFF1 [57]. It is typically associated with pro-B (CD10-) immunophenotype, and expression of myeloid markers. Irrespective of fusion partner or lineage phenotype this subtype shows a distinct gene expression signature with overexpression of HOX cluster genes and the HOX cofactor MEIS1 [58,59]. In infant KMT2A-rearranged ALL, the PI3K and Ras pathways are commonly altered [7,60,61]. KMT2A rearrangement is associated with altered chromatin patterning including H3K79 methylation, which has stimulated development of novel therapeutic approaches including inhibition of DOT1L [62], bromodomain, Menin, and the polycomb repressive complex [57,63,64]. The lineage plasticity characteristic of KMT2A-rearranged ALL is important in the context of immunotherapy, as this may facilitate loss of expression of CD19 and escape from CD19 Chimeric antigen receptor T cell (CAR-T) therapy [65].
The frequency of patients with BCR-ABL1 (Philadelphia chromosome) arising from the t(9;22)(q34;q11) translocation increases with age with 2–5% in childhood, 6% in adolescents and young adults (AYA), and more than 25% in adults [66,67]. Although historically considered a high-risk subtype, the incorporation of tyrosine kinase inhibitors (TKIs) into the standard treatment regimen for BCR-ABL1-positive ALL significantly improved clinical outcomes [68,69,70]. Secondary cooperative mutations are IKZF1, PAX5 and CDKN2A/B deletions [42,69,71,72]. IKZF1 alterations (most commonly deletions) have been associated with unfavorable outcome irrespective of TKI exposure [68,73], especially when co-occurring with (CDKN2A or CDKN2B, PAX5, or both: IKZF1plus) [68,69].
2.2. Emerging B-ALL Subtypes Defined by Genome Sequencing Studies
NGS approaches, particularly whole transcriptome sequencing (WTS), have enabled several research groups the identification of a large number of novel genetic alterations. These include cryptic rearrangements not identifiable by conventional approaches; novel subtypes that “phenocopy” established subtypes sharing similar gene expression profile but having different founding alterations; and subtypes defined by a single point mutation.
2.2.1. DUX4, MEF2D, ZNF384 and NUTM1 Gene Fusions
Translocation of DUX4 to the immunoglobulin heavy chain locus (IGH) is a cytogenetically cryptic alteration occurring in 5–10% of B-ALL and resulting in overexpression of a 3′ truncated DUX4 protein [7,13,74,75,76,77]. DUX4 is located within the D4Z4 subtelomeric repeat element on chromosome 4q/10q and encodes a double homeobox transcription factor that activates expression of large number of genes in early developing embryos, but it is thereafter silenced in most somatic cells [78]. Aberrant DUX4 expression is associated with facioscapulohumeral dystrophy (FSHD) [79], while DUX4 rearrangements have been also identified in Ewing-like sarcoma [80] and rhabdomyosarcoma [81]. In B-ALL, truncated DUX4 protein binds to an intragenic region of ERG resulting in transcriptional deregulation, and commonly, expression of a C-terminal ERG protein fragment, and/or ERG deletion. This subtype has a very distinctive gene expression profile and immunophenotype (CD2 and CD371 positive), common deletions of IKZF1 (40%) and despite this, excellent outcome [76,77,82,83]. Accurate identification of all cases of DUX4-rearranged ALL requires direct identification of rearrangement (e.g., by WTS), or alternatively, gene expression-based clustering or high DUX4 expression. The detection of strong CD371 cell surface expression by flow cytometry is a promising surrogate marker for this subtype [84]. Although ERG deletion is common in, and largely restricted to DUX4-rearranged ALL, these deletions are secondary events, commonly subclonal, and not present in all cases. Thus, the use of ERG deletion as a surrogate for identification of DUX4-rearranged ALL is suboptimal and should be avoided.
MEF2D (myocyte enhancer factor 2D) rearrangements occur in ~4% of childhood and 10% adult B-ALL cases. This subtype shows a distinct immunophenotype with low/absent expression of CD10, and positivity for CD38 and cytoplasmic µ chain, and distinct expression profiles [7,85,86,87,88]. MEF2D is the 5′ partner in all described fusions, whereas B-cell CLL/lymphoma (BCL) 9 and heterogeneous nuclear ribonucleoprotein U-like 1 (HNRNPUL1) are the two most recurrent 3′ partners. The rearrangements result in enhanced MEF2D transcriptional activity, increased HDAC9 expression and sensitivity to histone deacetylase inhibitors, such as panobinostat [85]. MEF2D has also been implicated in a core transcription factor regulatory circuit involving SREBF1 that regulates pre-BCR and lipid metabolism, that are therapeutic vulnerabilities [89]. Sensitivity to staurosporine and venetoclax has been also described [90]. MEF2D-rearranged ALL shows high levels of minimal residual disease and is considered to be an unfavorable subtype because of its poor event-free survival rates [82,83].
ZNF384-, or less commonly, ZNF362-rearranged acute leukemia is a biologically and clinically distinct leukemic subtype present in ~6% of childhood, 7.3% of adult, and 15% of AYA B-ALL, and in 48% of B/myeloid mixed phenotype acute leukemia (MPAL) [7,13,91,92,93]. These cases show a characteristic immunophenotype with weak CD10 and aberrant expression of the myeloid markers, CD13, and/or CD33 [92,94]. Expression of myeloperoxidase (MPO) is often the only feature distinguishing cases diagnosed as B-ALL (MPO−) or B/myeloid MPAL (MPO+). Different fusion partners, usually transcription factor (e.g., TAF15 and TCF3) or chromatin modifiers (e.g., CREBBP, EP300, SMARCA2, and ARID1B) have been identified for ZNF384, with EP300 being the most common. In all rearrangements the zinc-finger domains of the C2H2-type zinc-finger transcription factors ZNF384/ZNF362 are retained [7,13,91,92,95]. The same cooperating genetic alterations and transcriptional profile is observed in ZNF384-rearranged B-ALL and MPAL, and both exhibit lineage plasticity during disease progression (e.g., with shift in immunophenotype from lymphoid to myeloid from diagnosis to relapse). ZNF384 rearrangements are acquired in a subset of hematopoietic stem cells and prime leukemia cells for lineage plasticity [92]. A report of ZNF384-rearranged ALL in twins implicated a fetal hematopoietic progenitor as the cell of origin confirming that these rearrangements are founder alterations [96]. Prognosis varies by fusion partner: the EP300-ZNF384 fusion is associated with favorable outcome while the TCF3-ZNF384 fusion is frequently associated with late relapses and a poor prognosis [92,93]. However, overexpression of FLT3, characteristic of this subtype, makes this leukemia amenable to FLT3 inhibition [97].
NUTM1 (nuclear protein in testis midline carcinoma family 1) rearrangements (<2% of childhood B-ALL and mostly infant without KMT2A-rearrangements) [7,13,88,98,99,100] are characterized by fusion of NUTM1 to different partners, including transcription factors and epigenetic regulators (e.g., ACIN1, AFF1, ATAD5, BRD9, CHD4, CUX1, IKZF1, RUNX1, SLC12A6, and ZNF618), that drive aberrant NUTM1 expression [7,13]. In all fusions, the NUT domain is retained, and this is hypothesized to lead to global changes in chromatin acetylation [101] and to sensitivity to histone deacetylase inhibitors or bromodomain inhibitors in case of fusions with BRD9. NUTM1 rearrangements confer an excellent prognosis to current therapeutic approaches [82,83,98]. Since not all NUTM1 fusions are detectable by karyotyping either break-apart FISH or, preferably, WTS are the best approaches for diagnosis. In addition, the finding that both RNA expression of the 3′ exons and protein expression are highly specific for this subtype may help in diagnosis.
2.2.2. Subtypes That Phenocopy Established Subtypes
Ph-Like ALL
Ph-like or BCR-ABL1-like ALL is characterized by a gene expression signature similar to that of Ph-positive ALL but lacking the pathognomonic BCR-ABL1 oncoprotein of Ph+ ALL [15,66,102,103,104,105,106,107,108,109,110]. Its incidence ranges from ~10–15% in children to ~20% in older adults, with a peak (25–30%) in the AYA ALL population. Similar to patients with Ph+ ALL, patients with Ph-like ALL often exhibit adverse clinical features and poor outcome and frequently harbor alterations of IKZF1 or other B-lymphoid transcription factor genes. Over 60 heterogenous genetic alterations in kinases and cytokine receptors drive constitutively active kinase or cytokine receptor signaling, many of which have been shown to be druggable with a variety of kinase inhibitors. The most commonly mutated pathways are the ABL and JAK-STAT pathways with multiple rearrangements and lesions that converge on downstream ABL/JAK-STAT signaling. Founder alterations may be grouped into three broad types: (i) JAK/STAT alterations including: mutations activating cytokine receptors (e.g., CRLF2 and IL7R); enhancer hijacking gene rearrangements deregulating cytokine receptor expression (e.g., IGH-CRLF2 and P2RY8–CRLF2) [111,112,113,114]; gene fusions and/or mutations activating kinases (e.g., JAK1, JAK2, JAK3, TYK2); and rearrangements hijacking and truncating cytokine receptor expression (e.g., cryptic EPOR rearrangements) [115]; (ii) fusions involving ABL-class genes (ABL1, ABL2, CSF1R, LYN, PDGFRA, PDGFRB); and (iii) less common fusions (FLT3, FGFR1, NTRK3, PTK2B) [109] whose number is growing with increasing sequencing studies of different cohorts. Among these, alterations of CRLF2 are present in approximately half of Ph-like ALL in AYAs and adults. CRLF2 is located in the pseudoautosomal region of the sex chromosomes (PAR1) at Xp22.3/Yp11.3, and its alterations include: (1) a cryptic rearrangement that juxtaposes CRLF2 to the IGH locus; (2) a focal deletion in the pseudoautosomal region of the sex chromosomes resulting in P2Y receptor family member 8 (P2RY8)-CRLF2 fusion that positions CRLF2 under the control of the P2RY8 promoter; and less frequently by (3) an activating CRLF2 point mutation, F232C. PAR1 deletions, as a surrogate for rearrangement of CRLF2, have been incorporated into the criteria for “IKZF1plus”, a designation based on DNA copy number profiling, commonly by single nucleotide polymorphism (SNP) or multiplex ligation-dependent probe amplification (MLPA) arrays. In some studies, IKZF1plus has been associated with a higher risk of relapse defined by co-occurrence of the IKZF1 deletion with deletion of CDKN2A, CDKN2B, PAX5, and/or PAR1 region in the absence of ERG deletion [116]. Notably, however, the IKZF1plus designation typically does not consider cases with IGH-CRLF2 due to the inability of these platforms to detect this alteration.
The heterogeneous genomic landscape and often cytogenetically cryptic alterations identified in Ph-like ALL may make diagnosis of this entity and its driver alterations challenging, but several tractable diagnostic approaches are available, depending on technical capability of a laboratory, and the desired clinical/diagnostic endpoint (e.g., identification of the gene expression profile of Ph-like ALL c.f. identification of the most common driver kinase alterations). Comprehensive clinical NGS, including WTS, is the best approach to identify Ph-like ALL patients with targetable kinase alterations, as it enables analysis of gene expression, fusions, aneuploidy and sequence mutations. Selective/capture-based sequencing approaches (e.g., Archer FusionPlex, and FoundationOne Heme) also identify the majority of kinase-deregulating rearrangements in Ph-like ALL. If genomic approaches are not available, a more targeted screening approach using routine diagnostics, including flow cytometry (especially for CRLF2, for which positivity on flow cytometry is strongly correlated with rearrangement) and FISH for the most common kinase targets of rearrangement, is still effective for swift identification of Ph-like ALL [104]. The identification of specific genetic lesions is important for guiding targeted therapeutic intervention as a proportion of kinase-activating alterations in Ph-like ALL can, at least based on in vitro and preclinical models, be targeted by FDA-approved TKIs: JAK-STAT signaling (JAK inhibition); ABL-class fusions (ABL inhibitor); FLT3 and NTRK3 fusions (FLT3 and NTRK3 inhibitor) [104]. Several recent studies have described the efficacy of ABL1 and NTRK inhibitors in the treatment of Ph-like ALL cases with rearrangement of these genes [117,118]. Combinatorial use of kinase inhibitors against multiple signaling has shown synergism in patient-derived xenograft (PDX) models of CRLF2/JAK mutant (JAK and PI3K/mTOR inhibitors), ABL/PDGFR mutant (dasatinib and PI3K/mTOR inhibitor) and EPOR-rearranged (ponatinib and ruxolitinib) [119]. Moreover, recently dual JAK/GSPT1-degrading proteolysis-targeting chimeras PROTACs have been developed and showed efficacy in Ph-like B-ALL kinase-driven PDX models which were otherwise unresponsive to type I JAK inhibitors [120]. Lastly, the use of immunotherapeutic agents, such as blinatumomab, inotuzumab, and CAR-T cells (including those targeting CRLF2 [121], represents a promising alternative approach for this subtype which is irrespective of a specific genetic alteration or response to prior chemotherapies [104]).
ETV6-RUNX1-Like ALL
ETV6-RUNX1-like ALL is characterized by a gene expression profile and immunophenotype (CD27 positive, CD44 low to negative) similar to ETV6-RUNX1 ALL, but lacking the ETV6-RUNX1 fusion [122] and favorable prognosis [7,13,75,122,123]. These cases harbor alternate gene fusions or copy number alterations in ETS family transcription factors (ETV6, ERG, FLI1), IKZF1 or TCF3. ETV6-RUNX1-like ALL develops in children harboring germline ETV6 mutations with subsequent somatic alterations of the second ETV6 allele, consistent with the notion that biallelic alteration of ETV6 is central in leukemogenesis [124]. It is more common children (~3%) and confers an unfavorable prognosis in children due to high levels of MRD and worst event-free survival rates [82].
2.2.3. Subtypes Defined by a Single Point Mutation
PAX5 P80R and PAX5alt
The PAX5 P80R subtype (~3% of B-ALL cases) is characterized by the presence of a hot spot mutation at amino acid 80 in the DNA binding domain of the paired box DNA-binding transcription factor PAX5 [7,13,125,126]. B-ALL cases with PAX5 P80R show a distinct gene expression profile with the majority of cases having either hemizygous or homozygous mutation, caused by deletion of the wild-type PAX5 allele or copy-neutral loss of heterozygosity. In a subset of cases, in addition to PAX5 P80R there is a second frameshift, nonsense or deleterious missense PAX5 mutation. Thus, biallelic PAX5 alterations—with mutation of one allele and loss of activity of the second allele—are a hallmark of this subtype [7,125]. In support of the role of biallelic alteration of PAX5 in the pathogenesis of this subtype, knock-in mouse models of germline Pax5 mutations have shown that heterozygous Pax5P80R/+ knock-in mice develop transplantable B-ALL, with genetic inactivation of the wildtype Pax5 allele [7]. In contrast, Pax5G183S/+ knock in mice (modeling the germline PAX5 G183S mutation observed in familial ALL) show a low penetrance of ALL [127], supporting its role as a haploinsufficient tumor suppressor. Additional important cooperating lesions include CDKN2A loss and signaling pathway mutations, most commonly in Ras signaling genes or in the JAK/STAT pathway [7,125].
PAX5alt comprises about 7% cases with diverse PAX5 alterations, including rearrangements, sequence mutations and focal intragenic amplifications [7]. Over 20 different partner genes have been identified with PAX5-ETV6 being the most common. Children in this subtype are more commonly classified as high risk rather than standard risk (according to National Cancer Institute (NCI) criteria). In addition to PAX5 alterations, recurrent genetic lesions observed in these cases include copy number losses affecting cell-cycle regulation genes such as CDKN2A, RB1 and BTG1, B-cell development genes, transcriptional regulators and/or epigenetic modifiers (for example, KDM6A, KMT2A and ATRX) [7]. Both PAX5 P80R and PAX5alt subtypes are associated with intermediate to favorable prognosis [7,82,83,126].
IKZF1 N159Y
IKZF1 encodes the transcription factor IKAROS, which is a member of the family of zinc finger DNA-binding proteins required for lymphoid lineage ontogeny and homeostasis [128,129]. The most common type of IKZF1 alteration is a focal deletion occurring in 15% of ALL cases and in >50% of high risk ALL [42,72,103]. Deletions result in loss-of-function or in the dominant negative IK6 isoform and are associated with poor outcome [73,103]. In addition to deletions, missense, frameshift and nonsense mutations have been also described in pediatric high-risk B-ALL patients. Among those the missense p.Asn159Tyr mutation defines a subtype (<1% of B-ALL) with a distinct gene expression profile characterized by upregulation of genes with roles in oncogenesis (the IKZF1-interacting gene YAP1), chromatin remodeling (SALL1), and signaling (ARHGEF28) that are not deregulated in other subgroups of IKZF1-altered ALL [7,74]. In contrast to PAX5 P80R ALL, the nonmutated wild-type allele of the mutated transcription factor (here IKZF1) is retained [72]. As for most other missense mutations observed in IKZF1 zinc fingers, IKZF1 N159Y induces misregulation of IKZF1 transcriptional activation, in part through distinctive nuclear mislocalization and enhanced intercellular adhesion [130].
ZEB2 H1038R and IGH-CEBPE
In unsupervised clustering of leukemic cell gene expression, cases with the H1038R mutation in ZEB2 phenocopy the translocation t(14;14)(q11;q32) [13], which results in IGH-CEBPE fusion, suggesting a common activated pathway of leukemogenesis and defining a rare B-ALL subtype (<1%). This is associated with NRAS sequence mutations (>50% of cases), upregulation of LMO1 and downregulation of SMAD1 and BMP2 [10]. However, neither the IGH or ZEB2 mutations are unique to this group, nor do they explain all cases in this distinct gene expression and experimental validation is required to demonstrate their role as leukemogenic drivers. B-ALL with ZEB2 mutation is associated with poor event-free survival and high relapse [131].
2.3. Prognostic Implications
The frequent and wide use of genomics to profile the landscape of ALL has allowed a tailored refinement of risk in association with standard criteria, such as MRD levels [82] (Figure 1). In childhood B-ALL, ETV6-RUNX1, high-hyperdiploid, and DUX4-rearranged B-ALL are categorized as favorable due the highest overall survival rates and the lowest relapse rates, despite elevated early MRD in DUX4-rearranged cases. BCR-ABL1, BCR-ABL1-like, ETV6-RUNX1-like, KMT2A-rearranged, and MEF2D-rearranged ALL show high levels of MRD and the worst event-free survival rates and thus are categorized to be unfavorable subtypes. The remaining subtypes including TCF3-PBX1, PAX5alt, iAMP21, hypodiploid, ZNF384-rearranged, NUTM1-rearranged, and PAX5 P80R ALL have intermediate risk [81]. These prognostic groups have been mostly confirmed in a historic, non-MRD risk adapted trial (UKALLXII/ECOG-ACRIN E2993, NCT00002514) in adolescents and adult B-ALL cases [83] according to the following risk assignment: standard risk genotypes: DUX4-rearranged, ETV6-RUNX1/-like, TCF3-PBX1, PAX5 P80R, high-hyperdiploid; high-risk genotypes: Ph-like, KMT2A-AFF1, low-hypodiploid/near-haploid, BCL2/MYC-rearranged; and intermediate-risk genotypes: PAX5alt, ZNF384/-like, and MEF2D-rearranged.
3. T-Cell Acute Lymphoblastic Leukemia (T-ALL)
3.1. Genomic Overview of T-ALL
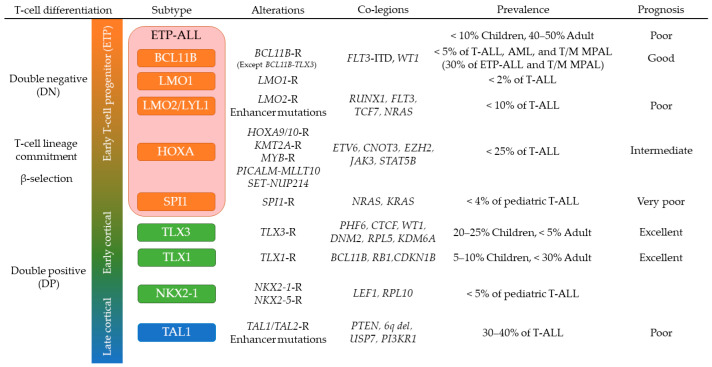
T-ALL leukemic cells express a subset of T-cell makers (CD3, cyCD3, CD2, CD5, CD7, CD8) and arises from immature T-cell progenitors [132,133]. Pediatric T-ALL accounts for 10–15% of newly diagnosed pediatric ALL and is characterized by higher incidence in boys, high initial white blood cell counts, mediastinal mass, CNS infiltration, and slightly worse prognosis compared to B-ALL [134]. The majority of T-ALL cases may be subclassified into subtypes according to the aberrant expression and dysregulated pathways of transcription factors and oncogenes induced by leukemia-initiating alterations involving basic helix–loop–helix (bHLH) factors (TAL1, TAL2, LYL1), homeobox genes (TLX1 (HOX11), TLX3 (HOX11L2), NKX2-1, NKX2-5, HOXA), LMO1, LMO2, MYB, BCL11B and SPI1 (Figure 2) [5,135,136]. These subtypes are defined with expression profiles by WTS or microarray, however, almost half of these leukemia-initiating alterations in T-ALL show intergenic breakpoints that can be missed by WTS but rescued by whole genome sequencing (WGS) [135,136]. Epigenomic analyses have also identified novel leukemia-initiating alterations in non-coding regions [5,137,138].
Figure 2.
T-cell differentiation and T-ALL subtyping. This schema describes differentiation stages of each T-ALL subtype according to the specific genetic alterations leading to aberrant expression of rearranged or mutated genes. Prevalence and prognosis of each subtype are shown. Subtypes are colored according to corresponding normal T-cell differentiation stage: early T-cell precursor (ETP, red and orange), early stages of cortical thymocytes maturation (green), and late stages of cortical thymocytes maturation (blue). Abbreviations: T-ALL: T-cell acute lymphoblastic leukemia; T/M MPAL: T/myeloid mixed phenotype acute leukemia; -R: rearranged.
NOTCH1 activating mutations and deletion of CDKN2A/CDKN2B loci (9p21) are found in over 70% of T-ALL cases and considered as secondary but core events in leukemogenesis [135,136,139]. Concurrent somatic mutations and copy number alterations are frequently observed in T-ALL leading to dysregulation of several cellular pathways, including JAK-STAT signaling (IL7R, JAK1, JAK3, DNM2), Ras signaling (NRAS, KRAS, and NF1), PI3K-AKT signaling (PTEN, AKT1, PIK3CA PIK3CD), epigenetic regulation (PHF6, SUZ12, EZH2, KDM6A), transcription factors and regulators (ETV6, GATA3, RUNX1, LEF1, WT1, BCL11B), and translation regulators (CNOT3, RPL5, RPL10) [135,136,140,141]. Accumulation of these aberrant expression and dysregulated pathways disrupt the normal T-cell differentiation, proliferation, and survival, and results in T-ALL with unique gene expression signatures reflecting the point of differentiation arrest during T-cell development [133,140]. In addition to expression profiles, DNA methylation signatures are also associated with immunophenotypic profiles and normal T-cell development differentiation stage [142,143].
3.2. T-ALL in Early Stages of Cortical Thymocyte Maturation
T-ALL with CD1a+, CD4+, and CD8+ immunophenotype includes several subgroups, such as rearrangements of TLX1, TLX3, NKX2-1, reflecting a differentiation arrest in early stages of cortical thymocyte maturation and confers a relatively favorable prognosis [144,145]. These subgroups almost commonly harbor NOTCH1 and CDKN2A alterations. Dysregulated expression of HOX transcription factor genes is mostly induced by chromosomal translocations and inversions that juxtapose these genes to enhancers in the TCR and BCL11B regulatory regions [135,146]. Importantly, BCL11B rearrangements (BCL11B-TLX3) in this subgroup are mechanistically distinct from those identified in BCL11B-rearranged lineage ambiguous leukemias, in that in the BCL11B-TLX3 leukemia, the BCL11B enhancer is used for aberrant expression of TLX3 at the cost of the loss of expression of BCL11B, leading to complete difference in expression profiles [5,146,147]. Instead, TLX3 rearranged T-ALL (including BCL11B-TLX3) shares gene expression signatures, DNA methylation profiles, somatic mutations (BCL11B, WT1, PHF6, DNM2), and downstream targets (JAK-STAT, epigenetic regulators) with TLX1 rearranged T-ALL [135,136,142,143,145]. Some of overlapping genomic features with TLX1/TLX3 rearranged T-ALL, including NUP214-ABL1 (TKIs) and JAK-STAT pathway (ruxolitinib, a JAK-STAT inhibitor), can be targetable and have been incorporated into ongoing clinical trials [148].
3.3. TAL1-Driven T-ALL with Late Stages of Cortical Thymocyte Maturation
Deregulation of the TAL1 oncogene is a feature of T-ALL that typically exhibits a late cortical thymocyte immunophenotype (CD4+, CD8+, CD3+) and comprises approximately 40% of T-ALL [135,136]. This T-ALL subtype includes TAL1 and TAL2 rearranged cases and is further classified into two subgroups by expression profiles whose one expresses PTCRA (pre-TCR) suggesting LCK activation that correlated with dasatinib sensitivity [136,145,149]. During normal T-cell differentiation, TAL1 expression is transcriptionally silenced along with T-cell lineage commitment to proceed appropriate TCR rearrangements and differentiation [133]. TAL1 overexpression is induced by several mechanisms: (1) chromosomal translocations with TCRA/D; (2) sub-microscopic interstitial deletion (STIL-TAL1); (3) disruption of insulated neighborhoods by losing CTCF binding sites [150]; and (4) somatic indels in a noncoding intergenic regulatory element upstream of TAL1 to generate aberrant MYB binding site (MuTE) [137]. The latter two mechanisms have benefited of NGS technologies for their identification. Dysregulated TAL1 expression inhibits the function of E-protein dimers by forming TAL1-E-protein heterodimer [151]. Furthermore, TAL1 forms the central node of the core regulatory circuit to coordinately regulate downstream target genes with several hematopoietic transcription factors including GATA3, RUNX1, MYB, and the ETS family genes, which is active in normal hematopoietic stem cell (HSC) and progenitor cells [152,153], and RUNX1 inhibition is reported to impair the growth of T-ALL but not normal hematopoietic cells [154]. However, although TAL1 functions as a master transcription factor related to T-cell differentiation and leukemogenesis of T-ALL, only 30% of transgenic mice develop T-ALL after a latent period, indicating that additional abnormalities are required for leukemogenesis [155]. Expression of Lmo2 accelerates the onset of leukemia in Tal1 transgenic mice, and LMO1/LMO2 are commonly expressed in human TAL1-driven T-ALL [156,157]. Other cooperative genes and noncoding RNAs in TAL1-driven T-ALL include ARID5B, ARIEL, and MYC, driving aberrant expression of TAL1 [158,159]. In addition, PI3K-AKT pathway genes including PTEN are frequently mutated in this subgroup [135,136], which associates with glucocorticoid resistance and can be reversed by the inhibition of this pathway [160]. Several cell cycle regulators including CDK6 and CCND3 are regulated by TAL1 complex [152] and may be potential targets of therapeutic intervention [161].
3.4. Early T-Cell Precursor (ETP) ALL and Mixed Phenotype Acute Leukemia
ETP-ALL is often referred to as a subtype of T-ALL as it exhibits an immunophenotype analogous to the earliest stages of T-cell development (cytoplasmic CD3+, CD7+; CD8−, CD1a−, CD5weak), and with expression of myeloid and/or stem-cell markers [144,162]. However, the genomic alterations and gene expression profile of ETP-ALL are more similar to a hematopoietic stem cell than a T cell precursor, suggesting that ETP-ALL could be included in a subgroup of immature acute leukemias of ambiguous lineage (ALAL), originating from a hematopoietic progenitor at a maturational stage prior to initiation of a definitive program of T cell differentiation. Consistent with this, recent studies have defined a subgroup of BCL11B-deregulated ALAL, that includes one third of ETP-ALL and T/myeloid mixed phenotype acute leukemia (T/M MPAL) cases with a very distinct expression profile [5]. BCL11B-deregulated ALAL is characterized by structural variations of the region containing BCL11B at 14q32 including translocations and high-copy amplification generating a distal neo-enhancer, that each leads to aberrant expression of BCL11B, in the case of the rearrangements by hijacking super-enhancers active in CD34+ hematopoietic stem and progenitor cell (HSPCs) [5,147]. FLT3 activating mutations were found in 80% of BCL11B-deregulated ALAL, and concurrent expression of BCL11B and FLT3-ITD on HSPC exhibited synergistic effects on activating T-cell directed differentiation to express cytoplasmic CD3 while blocking myeloid differentiation [5]. Other genomic features of ETP-ALL include a subgroup of aberrant expression of PU.1 (SPI1 fusions), HOXA genes (rearrangements of HOXA genes, KMT2A rearrangements, PICALM-MLLT10, SET-NUP214) and mutations of multiple cellular pathways (Ras signaling, JAK-STAT signaling, and epigenetic regulators) and transcription factors related to T-cell development [135,136,163]. Especially, T-ALL with SPI1 fusions represents unique expression profiles with high relapse rate [5,136]. Again, several of these genomic mutations were shared with T/M MPAL, including biallelic WT1 alterations, mutations of hematopoietic transcription factors (ETV6, RUNX1, CEBPA) and activating mutations of signaling pathways (JAK-STAT, FLT3, Ras) [92,163], supporting that they are similar entities in the spectrum of immature leukemias and both might have sensitivity to FLT3 and/or JAK inhibition [164].
3.5. NOTCH1 Activating Mutations in T-ALL
NOTCH1 encodes a highly conserved ligand-dependent transcription factor. The NOTCH1 signaling pathway plays an important role in the commitment of T-cell lineage specification and for further T-cell development [133,165]. In T-ALL, NOTCH1 activating mutations are found in more than 70% of cases and is considered an oncogene involved in leukemogenesis [135,136]. Aberrant activation of NOTCH1 pathway in T-ALL is mostly induced by (1) ligand-independent activation (somatic mutations, indels and large deletions that disrupt the negative regulatory region), or (2) impairment of the proteasomal degradation of intracellular domain of NOTCH1 (truncation of the PEST domain, NOTCH1 mutations in 3′ untranslated region, and FBXW7 mutations) [166,167,168,169,170,171]. These two types of NOTCH1 activating mutations have synergistic effects and more than 20% of T-ALL cases harbor both types of alterations [166]. However, most NOTCH1 activating mutations found in human T-ALL are considered as a weak tumor initiator event. Co-existence of both types of NOTCH1 mutations in hematopoietic progenitors tends to induce a transient preleukemic CD4+/CD8+ double positive cells and takes 10 to 15 weeks to fully transform into T-ALL, suggesting that they are alone incompletely leukemogenic [172,173,174]. In addition, more than 40% of T-ALL cases harbor subclonal NOTCH1 activating mutations and their heterogeneity at diagnosis was reported by several studies [135,136,175]. Furthermore, NOTCH1 activating mutations are considered to be acquired as a late secondary event in leukemogenesis [139,175,176].
A key target of NOTCH1 is the MYC oncogene that shares several overlapping target genes with NOTCH1 to promote cell proliferation and dysregulate anabolic pathways in T-ALL [174,177,178]. NOTCH1 controls T-cell-specific distal enhancer of MYC (“NMe”), resulting in the NOTCH1-MYC regulatory circuit [174,177,178]. In addition, pre-TCR signaling also correlates with NOTCH signaling, leading to LCK signaling and robust cell growth at DN3 stage in the T-cell development, which can be targetable by dasatinib [149,179].
Due to the high prevalence and importance of NOTCH1 activating mutations in T-ALL, targeted therapy on NOTCH1 pathway has been a major interest. This includes γ-secretase inhibitors (GSIs), ADAM inhibitors, SERCA inhibitors, and monoclonal antibodies [180]. Among them, GSIs, that block the activation process of NOTCH receptors by inhibiting proteolytic cleavage, have been tested in preclinical and Phase 1 studies [181,182]. However, the usage of GSIs in T-ALL is still in a developing phase due to gastrointestinal toxicity and insufficient antitumor responses that mostly induce transient growth arrest rather than cell death [183,184]. To overcome these problems, combination with other agents have been explored including glucocorticoids that showed synergistic effects by reversing glucocorticoid resistance [185]. Inhibition of mTORC1 signaling and PKCδ signaling are also promising combination strategies to restore GSIs sensitivity in resistant cells [186,187].
4. Implications for Diagnosis
The revolution in genomic characterization of ALL has created important opportunities and challenges for the clinical implementation of sequencing-based approaches for diagnosis and management of ALL (Table 1). This is particularly true for B-ALL, where many of the recently identified subtypes are associated with prognosis (even in the context of MRD-based risk-adapted therapy) [82,83] and where molecular characterization is needed to identify patients suitable for targeted therapy (an exemplar being Ph-like ALL). This is currently less compelling for T-ALL where identification of founding lesions driving T-ALL subtypes are of biological and mechanistic interest but are not typically used to risk stratify or guide therapy, exceptions possibly being kinase inhibition for JAK-STAT alterations and ABL1 rearrangements, identification of alterations in Ras, PTEN, NOTCH1 and/or FBXW7 that have been found to be associated with outcome in some studies [188], and LCK dependence for dasatinib therapy [149]. The challenge is clinical implementation of appropriately comprehensive diagnostic approaches to identify all key genomic features. Despite the mutationally sparse genome of ALL, there is striking diversity of the nature of underlying driver alterations, including sequence mutations, DNA copy number alterations, and structural variations, many of which may involve the non-coding genome. Accurate subtyping is also challenged by the inability of conventional cytogenetic and targeted molecular approaches to identify several types of driver (e.g., DUX4-rearrangement) and the importance of identifying phenocopies (e.g., ETV6-RUNX1-like, and Ph-like ALL). Thus, moving forward, optimal clinical diagnostics require genomic approaches. The choice of approach in part rests on how clinical information will be used. If comprehensive subtyping and identification of all potentially clinically relevant genomic alterations is desirable, a combination of DNA and RNA-based technologies is required. For example, the combination of WGS and WTS enables the identification of sequence mutations, DNA copy number alterations, aneuploidy and structural variants (from WGS) together with identification of fusion chimeras, mutant allele expression, and gene expression profiling (from WTS). The use of one or both approaches is becoming increasingly widely used, and at St Jude Children’s Research Hospital, three platform sequencing (WGS, WTS and exome sequencing) is clinical standard of care, informs clinical decision making in ALL [148], and retrieves more actionable clinical information than any single platform alone [189]. WGS is offered using a paired non-tumor sample to aid identification of somatic variants and provides the opportunity to return clinically relevant germline findings. Moreover, this comprehensive approach enables a more streamlined workflow [190,191,192], provided the demands of analysis and interpretation can be met.
Table 1.
Clinical implementation of high-throughput sequencing.
| Platform | Capability | Cost | Detectable Subtypes |
Difficult Subtypes |
|---|---|---|---|---|
| WTS (RNAseq) |
Fusion chimeras Gene expression profiling Mutant allele expression Alternative splicing analysis (BCR/TCR rearrangements) (Sequence mutations) (Copy number analysis) |
Moderate | B-ALL ETV6-RUNX1; KMT2A; TCF3-PBX1; BCR-ABL1; DUX4; MEF2D; ZNF384/362 NUTM1; HLF; BCL2/MYC; PAX5alt; ZEB2/CEBPE; -like subtypes |
B-ALL Aneuploidies |
| T-ALL HOXA (KMT2A-R, PICALM-MLLT10, SET-NUP214); SPI1; NKX2-1; TAL1 (STIL-TAL1) |
T-ALL BCL11B; TLX1/3; LMO1/2; HOXA (others); TAL1 (others); T-other |
|||
| WGS | Sequence mutations Structural variants Copy number analysis (BCR/TCR rearrangements) (GWAS) |
High | B-ALL Aneuploidies; ETV6-RUNX1; KMT2A; TCF3-PBX1; BCR-ABL1; DUX4; MEF2D; ZNF384/362; NUTM1; HLF; BCL2/MYC; PAX5 P80R; IKZF1 N159Y; ZEB2/CEBPE; Sequence and structural alterations in Ph-like ALL |
B-ALL -like subtypes; Part of PAX5alt |
| T-ALL BCL11B; TLX1/3; LMO1/2; HOXA; SPI1; NKX2-1; TAL1 |
T-ALL T-other |
|||
| WES | Sequence mutations (coding) Structural variants (coding) Copy number analysis |
Moderate | B-ALL (Aneuploidies) PAX5 P80R IKZF1 N159Y Sequence mutations in Ph-like ALL (e.g., JAK1/2/3, Ras) |
Most of other B-ALL and T-ALL subtypes |
| Targeted sequencing (DNA and/or RNA) |
Fusion chimeras (targeted) Gene expression (targeted) Sequence mutations (targeted) Structural variants (targeted) (Copy number analysis) |
Low | Targeted alterations | Non-targeted alterations |
The parenthesis in “Capability” indicates analyses in development. Abbreviations: WTS: whole transcriptome sequencing; BCR: B-cell receptor; TCR: T-cell receptor; WGS: whole genome sequencing; GWAS: genome wide association study; WES: whole exome sequencing; -R: rearranged.
However, WGS is not yet widely used clinically, and many clinicians and providers seek alternative approaches to identify clinically relevant alterations. These fall into three main categories: single platform sequencing, sub-genomic sequencing, and targeted detection of genomic alterations. In the first category, single platform WTS provides near comprehensive characterization of clinically relevant alterations in ALL, particularly B-ALL: gene expression-based profiling to identify subgroups and phenocopies; fusion transcripts; and interrogation of specific sequence mutations (e.g., JAKs, PAX5 and IKZF1) [7,193]. Moreover, several methods are available that utilize expression and mutant allele fraction to robustly identify large scale chromosomal copy number changes, thus providing a surrogate for conventional cytogenetic identification of aneuploidy [7,194]. WTS as a single platform has limitations—it is challenging to identify all sequence variations although analytic platforms are improving, it cannot identify focal DNA copy number alterations that may impact targetable pathways (e.g., SH2B3 deletions in JAK-STAT-driven Ph-like ALL) and does not identify rearrangements that may deregulate oncogenes without resulting in a RNA chimera—for example rearrangements of oncogenes in T-ALL such as TLX3 and those involving TCR, where breakpoints are frequently intergenic [135], the diverse rearrangements in BCL11B-rearranged ALAL [5], or non-coding sequence mutations that drive oncogenes such as TAL1 and LMO1/2 [137,138].
Several platforms are available for targeted DNA and/or RNA sequencing, often using capture-based approaches. These including Foundation Medicine [195] and the FusionPlex ALL Kit (Invitae, previously ArcherDx). These have the advantage of being somewhat simpler to access or implement in routine diagnostic laboratories, and the ability to detect the majority of chimeric fusion events in B-ALL. Similar reservations to WTS apply regarding the limited ability of these platforms to detect intergenic rearrangements in ALL; moreover, these platforms either have limited (Foundation) or no (Archer) capability to detect DNA copy number alterations, particularly those that are single copy, and may have difficulty resolving complex rearrangements (e.g., truncating rearrangements of EPOR in Ph-like ALL) [115]. Capture based DNA sequencing for sequence mutations is widely used in hematological malignancies, but is not well suited to diagnosis of ALL due to the lack of detection of rearrangements and structural variations. As described above, the MLPA platform is widely used by several groups to identify focal DNA copy number alterations and the “IKZF1plus” composite genotype, but this platform is not an adequate surrogate for sensitive detection of several key subtypes: e.g., ERG deletion in DUX4-rearranged ALL (only ~50% of cases have clonal ERG deletion), and PAR1 deletion in CRLF2-rearranged ALL (IGH-CRLF2 is usually not accompanied by PAR1 deletion).
In the absence of sequencing-based approaches, several subtypes and drivers may be identified by flow cytometry, immunophenotypic and targeted molecular approaches. Flow cytometry may be used to detect CRLF2 rearrangements, that result in cell surface expression of CRLF2, as well as markers associated with distinct subtypes (e.g., CD371 in DUX4-rearranged ALL). FISH may be used to detect rearrangement of the most commonly rearranged genes in Ph-like ALL for which targeted therapies are currently available (e.g., ABL-family kinase genes, CRLF2, NTRK3) with caveats—for example, the focal insertions of EPOR into IGH and similar enhancer regions are not robustly detected by FISH due to the small size of the EPOR insertion. Specific subtype-defining rearrangements may be detected by conventional molecular approaches such as RT-PCR. Thus, these composite approaches may be suitable to detect many actionable alterations in ALL, but do not provide a pathway to comprehensive identification of all driver lesions of prognostic significance.
5. Conclusions
Large-scale integrative genome-wide sequencing studies have profoundly transformed the molecular taxonomy of ALL, resulting in the identification of new entities with prognostic and therapeutic significance. There are over 30 different B/T-ALL subtypes defined by distinct constellations of somatic and/or germline genetic alterations that converge on distinct gene expression patterns. The identification of these dysregulated pathways is crucial for clinical management of ALL patients and most importantly for guiding therapeutic intervention. The best example is provided by the constitutively active kinases in Ph-like which are druggable by a variety of single or combinatorial TKIs. Although the enormous clinical and genetic progress of the past decade, much work remains, as most studies have lacked NGS and have not validated the mechanisms by which fusions/mutations cooperate in leukemogenesis, and not fully defined potential for targeting. Due to the heterogeneity of genetic lesions, optimal clinical diagnosis of ALL requires genomic and/or transcriptomic sequencing in order to identify fusions, aneuploidy and sequence mutations required for disease stratification. The use of such approaches is becoming increasingly widespread. Recently, new immunotherapeutic agents (e.g., developed antibodies and CAR-T cells) have been efficacious in a proportion of patients, but failed in others. Thus, efforts should be focused in the future on defining subtype specific vulnerabilities to improve treatment strategy and outcome.
Acknowledgments
The authors thank collaborators that have contributed patient samples, data, intellectual and technical expertise to the work described in this study, particularly the St. Jude Children’s Research Hospital—Washington University Pediatric Cancer Genome Project, Children’s Oncology Group Therapeutically Applicable Research to Generate Effective Treatments (TARGET) project (https://ocg.cancer.gov/programs/target/projects/acute-lymphoblastic-leukemia, accessed on 19 August 2021), the Eastern Cooperative Oncology Group—American College of Radiology Imaging Network (ECOG-ACRIN), The Alliance—Cancer and Leukemia Group B, and MD Anderson Cancer Center.
Author Contributions
Writing—original draft preparation, I.I., S.K. and C.G.M.; writing—review and editing, I.I., S.K. and C.G.M.; visualization, I.I. and S.K.; supervision, I.I. and C.G.M. All authors have read and agreed to the published version of the manuscript.
Funding
Work conducted by the authors described in this review was supported by the National Institutes of Health, including an NCI Outstanding Investigator Award R35 CA197697 (to C.G.M.), NCI Cancer Center Support Grant (CA021765) an St. Baldrick’s Foundation Robert J. Arceci Innovation Award (to C.G.M.) and the Henry Schueler 41&9 Foundation (to C.G.M.); a Garwood Postdoctoral Fellowship of the Hematological Malignancies Program of the St Jude Children’s Research Hospital Comprehensive Cancer Center (to S.K.); and the American Lebanese Syrian Associated Charities of St. Jude Children’s Research Hospital.
Conflicts of Interest
I.I. has received honoraria from Amgen and Mission Bio; S.K. declares no conflict of interest.; C.G.M. has received research funding from Loxo Oncology (relevant to the use of TRK inhibition in Ph-like ALL), AbbVie (venetoclax in ALL) and Pfizer; honoraria from Amgen and Illumina. These funders had no role in the writing of this manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tran T.H., Hunger S.P. The genomic landscape of pediatric acute lymphoblastic leukemia and precision medicine opportunities. Semin. Cancer Biol. 2020 doi: 10.1016/j.semcancer.2020.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Pui C.-H. Precision medicine in acute lymphoblastic leukemia. Front. Med. 2020;14:689–700. doi: 10.1007/s11684-020-0759-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inaba H., Mullighan C.G. Pediatric acute lymphoblastic leukemia. Haematologica. 2020;105:2524. doi: 10.3324/haematol.2020.247031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stock W., Luger S.M., Advani A.S., Yin J., Harvey R.C., Mullighan C.G., Willman C.L., Fulton N., Laumann K.M., Malnassy G., et al. A pediatric regimen for older adolescents and young adults with acute lymphoblastic leukemia: Results of CALGB 10403. Blood. 2019;133:1548–1559. doi: 10.1182/blood-2018-10-881961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montefiori L.E., Bendig S., Gu Z., Chen X., Polonen P., Ma X., Murison A., Zeng A., Garcia-Prat L., Dickerson K., et al. Enhancer hijacking drives oncogenic BCL11B expression in lineage ambiguous stem cell leukemia. Cancer Discov. 2021 doi: 10.1158/2159-8290.CD-21-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iacobucci I., Mullighan C.G. Genetic Basis of Acute Lymphoblastic Leukemia. J. Clin. Oncol. 2017;35:975–983. doi: 10.1200/JCO.2016.70.7836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gu Z., Churchman M.L., Roberts K.G., Moore I., Zhou X., Nakitandwe J., Hagiwara K., Pelletier S., Gingras S., Berns H., et al. PAX5-driven subtypes of B-progenitor acute lymphoblastic leukemia. Nat. Genet. 2019;51:296–307. doi: 10.1038/s41588-018-0315-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pui C.-H., Nichols K.E., Yang J.J. Somatic and germline genomics in paediatric acute lymphoblastic leukaemia. Nat. Rev. Clin. Oncol. 2018;16:227–240. doi: 10.1038/s41571-018-0136-6. [DOI] [PubMed] [Google Scholar]
- 9.Schwab C., Harrison C.J. Advances in B-cell Precursor Acute Lymphoblastic Leukemia Genomics. HemaSphere. 2018;2:e53. doi: 10.1097/HS9.0000000000000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li J., Dai Y., Wu L., Zhang M., Ouyang W., Huang J., Chen S. Emerging molecular subtypes and therapeutic targets in B-cell precursor acute lymphoblastic leukemia. Front. Med. 2021;15:347–371. doi: 10.1007/s11684-020-0821-6. [DOI] [PubMed] [Google Scholar]
- 11.Mullighan C.G. How advanced are we in targeting novel subtypes of ALL? Best Pract. Res. Clin. Haematol. 2019;32:101095. doi: 10.1016/j.beha.2019.101095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kimura S., Mullighan C.G. Molecular markers in ALL: Clinical implications. Best Pract. Res. Clin. Haematol. 2020;33:101193. doi: 10.1016/j.beha.2020.101193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li J.-F., Dai Y.-T., Lilljebjörn H., Shen S.-H., Cui B.-W., Bai L., Liu Y.-F., Qian M.-X., Kubota Y., Kiyoi H., et al. Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1223 cases. Proc. Natl. Acad. Sci. USA. 2018;115:E11711–E11720. doi: 10.1073/pnas.1814397115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts K.G., Morin R.D., Zhang J., Hirst M., Zhao Y., Su X., Chen S.-C., Payne-Turner D., Churchman M.L., Harvey R., et al. Genetic Alterations Activating Kinase and Cytokine Receptor Signaling in High-Risk Acute Lymphoblastic Leukemia. Cancer Cell. 2012;22:153–166. doi: 10.1016/j.ccr.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberts K.G., Li Y., Payne-Turner D., Harvey R., Yang Y.-L., Pei D., McCastlain K., Ding L., Lu C., Song G., et al. Targetable Kinase-Activating Lesions in Ph-like Acute Lymphoblastic Leukemia. N. Engl. J. Med. 2014;371:1005–1015. doi: 10.1056/NEJMoa1403088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klco J.M., Mullighan C.G. Advances in germline predisposition to acute leukaemias and myeloid neoplasms. Nat. Rev. Cancer. 2020;21:122–137. doi: 10.1038/s41568-020-00315-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perez-Andreu V., Roberts K.G., Harvey R., Yang W., Cheng C., Pei D., Xu H., Gastier-Foster J., Lim J.Y.-S., Chen I.-M., et al. Inherited GATA3 variants are associated with Ph-like childhood acute lymphoblastic leukemia and risk of relapse. Nat. Genet. 2013;45:1494–1498. doi: 10.1038/ng.2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellinghaus E., Stanulla M., Richter G., Kronnie G.T., Cario G., Cazzaniga G., Horstmann M., Grümayer R.P., Cavé H., Trka J., et al. Identification of germline susceptibility loci in ETV6-RUNX1-rearranged childhood acute lymphoblastic leukemia. Leukemia. 2011;26:902–909. doi: 10.1038/leu.2011.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qian M., Zhao X., Devidas M., Yang W., Gocho Y., Smith C., Gastier-Foster J.M., Li Y., Xu H., Zhang S., et al. Genome-Wide Association Study of Susceptibility Loci for T-Cell Acute Lymphoblastic Leukemia in Children. J. Natl. Cancer Inst. 2019;111:1350–1357. doi: 10.1093/jnci/djz043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qian M., Xu H., Perez-Andreu V., Roberts K.G., Zhang H., Yang W., Zhang S., Zhao X., Smith C., Devidas M., et al. Novel susceptibility variants at the ERG locus for childhood acute lymphoblastic leukemia in Hispanics. Blood. 2019;133:724–729. doi: 10.1182/blood-2018-07-862946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Molina O., Abad M.A., Solé F., Menéndez P. Aneuploidy in Cancer: Lessons from Acute Lymphoblastic Leukemia. Trends Cancer. 2020;7:37–47. doi: 10.1016/j.trecan.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 22.Greaves M. A causal mechanism for childhood acute lymphoblastic leukaemia. Nat. Rev. Cancer. 2018;18:471–484. doi: 10.1038/s41568-018-0015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paulsson K., Lilljebjörn H., Biloglav A., Olsson L., Rissler M., Castor A., Barbany G., Fogelstrand L., Nordgren A., Sjögren H., et al. The genomic landscape of high hyperdiploid childhood acute lymphoblastic leukemia. Nat. Genet. 2015;47:672–676. doi: 10.1038/ng.3301. [DOI] [PubMed] [Google Scholar]
- 24.Paulsson K., Johansson B. High hyperdiploid childhood acute lymphoblastic leukemia. Genes Chromosom. Cancer. 2009;48:637–660. doi: 10.1002/gcc.20671. [DOI] [PubMed] [Google Scholar]
- 25.Mullighan C.G., Zhang J., Kasper L.H., Lerach S., Payne-Turner D., Phillips L.A., Heatley S., Holmfeldt L., Collins-Underwood J.R., Ma J., et al. CREBBP mutations in relapsed acute lymphoblastic leukaemia. Nature. 2011;471:235–239. doi: 10.1038/nature09727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Molina O., Vinyoles M., Granada I., Roca-Ho H., Gutierrez-Agüera F., Valledor L., López C.M.L., Rodríguez-González P., Trincado J.L., Tirados-Menéndez S., et al. Impaired Condensin Complex and Aurora B kinase underlie mitotic and chromosomal defects in hyperdiploid B-cell ALL. Blood. 2020;136:313–327. doi: 10.1182/blood.2019002538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmfeldt L., Wei L., Diaz-Flores E., Walsh M., Zhang J., Ding L., Payne-Turner D., Churchman M., Hagström-Andersson A., Chen S.-C., et al. The genomic landscape of hypodiploid acute lymphoblastic leukemia. Nat. Genet. 2013;45:242–252. doi: 10.1038/ng.2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Comeaux E.Q., Mullighan C.G. TP53Mutations in Hypodiploid Acute Lymphoblastic Leukemia. Cold Spring Harb. Perspect. Med. 2016;7:a026286. doi: 10.1101/cshperspect.a026286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carroll A.J., Shago M., Mikhail F.M., Raimondi S.C., Hirsch B.A., Loh M.L., Raetz E.A., Borowitz M.J., Wood B.L., Maloney K.W., et al. Masked hypodiploidy: Hypodiploid acute lymphoblastic leukemia (ALL) mimicking hyperdiploid ALL in children: A report from the Children’s Oncology Group. Cancer Genet. 2019;238:62–68. doi: 10.1016/j.cancergen.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mullighan C.G., Jeha S., Pei D., Payne-Turner D., Coustan-Smith E., Roberts K.G., Waanders E., Choi J.K., Ma X., Raimondi S.C., et al. Outcome of children with hypodiploid ALL treated with risk-directed therapy based on MRD levels. Blood. 2015;126:2896–2899. doi: 10.1182/blood-2015-09-671131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pui C.-H., Rebora P., Schrappe M., Attarbaschi A., Baruchel A., Basso G., Cavé H., Elitzur S., Koh K., Liu H.-C., et al. Outcome of Children with Hypodiploid Acute Lymphoblastic Leukemia: A Retrospective Multinational Study. J. Clin. Oncol. 2019;37:770–779. doi: 10.1200/JCO.18.00822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McNeer J.L., Devidas M., Dai Y., Carroll A.J., Heerema N.A., Gastier-Foster J.M., Kahwash S., Borowitz M.J., Wood B.L., Larsen E., et al. Hematopoietic Stem-Cell Transplantation Does Not Improve the Poor Outcome of Children with Hypodiploid Acute Lymphoblastic Leukemia: A Report From Children’s Oncology Group. J. Clin. Oncol. 2019;37:780–789. doi: 10.1200/JCO.18.00884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ribera J., Granada I., Morgades M., Vives S., Genescà E., González C., Nomdedeu J., Escoda L., Montesinos P., Mercadal S., et al. The poor prognosis of low hypodiploidy in adults with B-cell precursor acute lymphoblastic leukaemia is restricted to older adults and elderly patients. Br. J. Haematol. 2019;186:263–268. doi: 10.1111/bjh.15887. [DOI] [PubMed] [Google Scholar]
- 34.Diaz-Flores E., Comeaux E.Q., Kim K.L., Melnik E.M., Beckman K., Davis K.L., Wu K., Akutagawa J., Bridges O., Marino R., et al. Bcl-2 Is a Therapeutic Target for Hypodiploid B-Lineage Acute Lymphoblastic Leukemia. Cancer Res. 2019;79:2339–2351. doi: 10.1158/0008-5472.CAN-18-0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harrison C.J. Blood Spotlight on iAMP21 acute lymphoblastic leukemia (ALL), a high-risk pediatric disease. Blood. 2015;125:1383–1386. doi: 10.1182/blood-2014-08-569228. [DOI] [PubMed] [Google Scholar]
- 36.Harrison C.J., Schwab C. Constitutional abnormalities of chromosome 21 predispose to iAMP21-acute lymphoblastic leukaemia. Eur. J. Med. Genet. 2016;59:162–165. doi: 10.1016/j.ejmg.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Moorman A.V., Robinson H., Schwab C., Richards S.M., Hancock J., Mitchell C.D., Goulden N., Vora A., Harrison C. Risk-Directed Treatment Intensification Significantly Reduces the Risk of Relapse among Children and Adolescents with Acute Lymphoblastic Leukemia and Intrachromosomal Amplification of Chromosome 21: A Comparison of the MRC ALL97/99 and UKALL2003 Trials. J. Clin. Oncol. 2013;31:3389–3396. doi: 10.1200/JCO.2013.48.9377. [DOI] [PubMed] [Google Scholar]
- 38.Golub T., McLean T., Stegmaier K., Ritz J., Sallan S., Neuberg D., Gilliland D.G. TEL-AML1: The most common gene rearrangement in childhood ALL. Blood. 1995;86:2377. [Google Scholar]
- 39.Sundaresh A., Williams O. Mechanism of ETV6-RUNX1 Leukemia. Adv. Exp. Med. Biol. 2017;962:201–216. doi: 10.1007/978-981-10-3233-2_13. [DOI] [PubMed] [Google Scholar]
- 40.Shurtleff S.A., Buijs A., Behm F.G., Rubnitz J., Raimondi S.C., Hancock M.L., Chan G.C.F., Pui C.H., Grosveld G., Downing J.R. TEL/AML1 fusion resulting from a cryptic t(12;21) is the most common genetic lesion in pediatric ALL and defines a subgroup of patients with an excellent prognosis. Leukemia. 1995;9:1985–1989. [PubMed] [Google Scholar]
- 41.Ford A.M., Greaves M. ETV6-RUNX1 + Acute Lymphoblastic Leukaemia in Identical Twins. Adv. Exp. Med. Biol. 2017;962:217–228. doi: 10.1007/978-981-10-3233-2_14. [DOI] [PubMed] [Google Scholar]
- 42.Mullighan C., Goorha S., Radtke I., Miller C.B., Coustan-Smith E., Dalton J.D., Girtman K., Mathew S., Ma J., Pounds S., et al. Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature. 2007;446:758–764. doi: 10.1038/nature05690. [DOI] [PubMed] [Google Scholar]
- 43.Kuiper R.P., Schoenmakers E.F.P.M., Van Reijmersdal S.V., Hehir-Kwa J.Y., Van Kessel A.G., van Leeuwen F.N., Hoogerbrugge P.M. High-resolution genomic profiling of childhood ALL reveals novel recurrent genetic lesions affecting pathways involved in lymphocyte differentiation and cell cycle progression. Leukemia. 2007;21:1258–1266. doi: 10.1038/sj.leu.2404691. [DOI] [PubMed] [Google Scholar]
- 44.Papaemmanuil E., Rapado I., Li Y., Potter N.E., Wedge D., Tubio J., Alexandrov L.B., Van Loo P., Cooke S.L., Marshall J., et al. RAG-mediated recombination is the predominant driver of oncogenic rearrangement in ETV6-RUNX1 acute lymphoblastic leukemia. Nat. Genet. 2014;46:116–125. doi: 10.1038/ng.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burmeister T., Gökbuget N., Schwartz S., Fischer L., Hubert D., Sindram A., Hoelzer D., Thiel E. Clinical features and prognostic implications of TCF3-PBX1 and ETV6-RUNX1 in adult acute lymphoblastic leukemia. Haematologica. 2009;95:241–246. doi: 10.3324/haematol.2009.011346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jeha S., Pei D., Choi J., Cheng C., Sandlund J.T., Coustan-Smith E., Campana D., Inaba H., Rubnitz J.E., Ribeiro R.C., et al. Improved CNS Control of Childhood Acute Lymphoblastic Leukemia without Cranial Irradiation: St Jude Total Therapy Study 16. J. Clin. Oncol. 2019;37:3377–3391. doi: 10.1200/JCO.19.01692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pui C.-H., Tang J.-Y., Yang J.J., Chen S.-J., Chen Z. International Collaboration to Save Children with Acute Lymphoblastic Leukemia. J. Glob. Oncol. 2019;5:1–2. doi: 10.1200/JGO.19.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Buchner M., Müschen M. Targeting the B-cell receptor signaling pathway in B lymphoid malignancies. Curr. Opin. Hematol. 2014;21:341–349. doi: 10.1097/MOH.0000000000000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van der Veer A., van der Velden V.H., Willemse M.E., Hoogeveen P.G., Petricoin E.F., Beverloo H.B., Escherich G., Horstmann M.A., Pieters R., den Boer M.L. Interference with pre-B-cell receptor signaling offers a therapeutic option for TCF3-rearranged childhood acute lymphoblastic leukemia. Blood Cancer J. 2014;4:e181. doi: 10.1038/bcj.2014.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bicocca V., Chang B., Masouleh B.K., Muschen M., Loriaux M.M., Druker B.J., Tyner J.W. Crosstalk between ROR1 and the Pre-B Cell Receptor Promotes Survival of t(1;19) Acute Lymphoblastic Leukemia. Cancer Cell. 2012;22:656–667. doi: 10.1016/j.ccr.2012.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fischer U., Forster M., Rinaldi A., Risch T., Sungalee S., Warnatz H.-J., Bornhauser B., Gombert M., Kratsch C., Stütz A.M., et al. Genomics and drug profiling of fatal TCF3-HLF−positive acute lymphoblastic leukemia identifies recurrent mutation patterns and therapeutic options. Nat. Genet. 2015;47:1020–1029. doi: 10.1038/ng.3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Frismantas V., Dobay M.P., Rinaldi A., Tchinda J., Dunn S.H., Kunz J., Richter-Pechanska P., Marovca B., Pail O., Jenni S., et al. Ex vivo drug response profiling detects recurrent sensitivity patterns in drug-resistant acute lymphoblastic leukemia. Blood. 2017;129:e26–e37. doi: 10.1182/blood-2016-09-738070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Glover J.M., Loriaux M., Tyner J., Druker B., Chang B.H. In vitro sensitivity to dasatinib in lymphoblasts from a patient with t(17;19)(q22;p13) gene rearrangement pre-B acute lymphoblastic leukemia. Pediatr. Blood Cancer. 2011;59:576–579. doi: 10.1002/pbc.23383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mouttet B., Vinti L., Ancliff P., Bodmer N., Brethon B., Cario G., Chen-Santel C., Elitzur S., Hazar V., Kunz J., et al. Durable remissions in TCF3-HLF positive acute lymphoblastic leukemia with blinatumomab and stem cell transplantation. Haematologica. 2019;104:e244–e247. doi: 10.3324/haematol.2018.210104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leonard J., Wolf J.S., Degnin M., Eide C.A., LaTocha D., Lenz K., Wilmot B., Mullighan C.G., Loh M., Hunger S.P., et al. Aurora A kinase as a target for therapy in TCF3-HLF rearranged acute lymphoblastic leukemia. Haematologica. 2021 doi: 10.3324/haematol.2021.278692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.El Chaer F., Keng M., Ballen K.K. MLL-Rearranged Acute Lymphoblastic Leukemia. Curr. Hematol. Malig. Rep. 2020;15:83–89. doi: 10.1007/s11899-020-00582-5. [DOI] [PubMed] [Google Scholar]
- 57.Winters A.C., Bernt K.M. MLL-Rearranged Leukemias—An Update on Science and Clinical Approaches. Front. Pediatr. 2017;5:4. doi: 10.3389/fped.2017.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Armstrong S.A., Staunton J.E., Silverman L.B., Pieters R., Boer M.D., Minden M.D., Sallan S.E., Lander E.S., Golub T.R., Korsmeyer S.J. MLL translocations specify a distinct gene expression profile that distinguishes a unique leukemia. Nat. Genet. 2001;30:41–47. doi: 10.1038/ng765. [DOI] [PubMed] [Google Scholar]
- 59.Yeoh E.-J., Ross M.E., Shurtleff S.A., Williams W., Patel D., Mahfouz R., Behm F.G., Raimondi S.C., Relling M.V., Patel A., et al. Classification, subtype discovery, and prediction of outcome in pediatric acute lymphoblastic leukemia by gene expression profiling. Cancer Cell. 2002;1:133–143. doi: 10.1016/S1535-6108(02)00032-6. [DOI] [PubMed] [Google Scholar]
- 60.Andersson A.K., Ma J., Wang J., Chen X., Gedman A.L., Dang J., Nakitandwe J., Holmfeldt L., Parker M., Easton J., et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat. Genet. 2015;47:330–337. doi: 10.1038/ng.3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Valentine M.C., Linabery A., Chasnoff S., Hughes A.E.O., Mallaney C., Sanchez N., Giacalone J., Heerema N.A., Hilden J.M., Spector L., et al. Excess congenital non-synonymous variation in leukemia-associated genes in MLL−infant leukemia: A Children’s Oncology Group report. Leukemia. 2013;28:1235–1241. doi: 10.1038/leu.2013.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Perner F., Gadrey J.Y., Xiong Y., Hatton C., Eschle B.K., Weiss A., Stauffer F., Gaul C., Tiedt R., Perry J.A., et al. Novel inhibitors of the histone methyltransferase DOT1L show potent antileukemic activity in patient-derived xenografts. Blood. 2020;136:1983–1988. doi: 10.1182/blood.2020006113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen C.-W., Koche R., Sinha A.U., Deshpande A.J., Zhu N., Eng R., Doench J., Xu H., Chu S.H., Qi J., et al. DOT1L inhibits SIRT1-mediated epigenetic silencing to maintain leukemic gene expression in MLL-rearranged leukemia. Nat. Med. 2015;21:335–343. doi: 10.1038/nm.3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Klossowski S., Miao H., Kempinska K., Wu T., Purohit T., Kim E., Linhares B.M., Chen D., Jih G., Perkey E., et al. Menin inhibitor MI-3454 induces remission in MLL1-rearranged and NPM1-mutated models of leukemia. J. Clin. Investig. 2019;130:981–997. doi: 10.1172/JCI129126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liao W., Kohler M.E., Fry T., Ernst P. Does lineage plasticity enable escape from CAR-T cell therapy? Lessons from MLL-r leukemia. Exp. Hematol. 2021;100:1–11. doi: 10.1016/j.exphem.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roberts K.G., Gu Z., Payne-Turner D., McCastlain K., Harvey R., Chen I.-M., Pei D., Iacobucci I., Valentine M., Pounds S.B., et al. High Frequency and Poor Outcome of Philadelphia Chromosome–Like Acute Lymphoblastic Leukemia in Adults. J. Clin. Oncol. 2017;35:394–401. doi: 10.1200/JCO.2016.69.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bernt K., Hunger S.P.M. Current Concepts in Pediatric Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia. Front. Oncol. 2014;4:54. doi: 10.3389/fonc.2014.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Slayton W.B., Schultz K.R., Kairalla J.A., Devidas M., Mi X., Pulsipher M.A., Chang B.H., Mullighan C., Iacobucci I., Silverman L.B., et al. Dasatinib Plus Intensive Chemotherapy in Children, Adolescents, and Young Adults with Philadelphia Chromosome–Positive Acute Lymphoblastic Leukemia: Results of Children’s Oncology Group Trial AALL0622. J. Clin. Oncol. 2018;36:2306–2314. doi: 10.1200/JCO.2017.76.7228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Foà R., Bassan R., Vitale A., Elia L., Piciocchi A., Puzzolo M.-C., Canichella M., Viero P., Ferrara F., Lunghi M., et al. Dasatinib–Blinatumomab for Ph-Positive Acute Lymphoblastic Leukemia in Adults. N. Engl. J. Med. 2020;383:1613–1623. doi: 10.1056/NEJMoa2016272. [DOI] [PubMed] [Google Scholar]
- 70.Foà R., Vitale A., Vignetti M., Meloni G., Guarini A., De Propris M.S., Elia L., Paoloni F., Fazi P., Cimino G., et al. Dasatinib as first-line treatment for adult patients with Philadelphia chromosome–positive acute lymphoblastic leukemia. Blood. 2011;118:6521–6528. doi: 10.1182/blood-2011-05-351403. [DOI] [PubMed] [Google Scholar]
- 71.Mullighan C., Miller C.B., Radtke I., Phillips L.A., Dalton J.T., Ma J., White D., Hughes T., Le Beau M.M., Pui C.-H., et al. BCR–ABL1 lymphoblastic leukaemia is characterized by the deletion of Ikaros. Nature. 2008;453:110–114. doi: 10.1038/nature06866. [DOI] [PubMed] [Google Scholar]
- 72.Iacobucci I., Storlazzi C.T., Cilloni D., Lonetti A., Ottaviani E., Soverini S., Astolfi A., Chiaretti S., Vitale A., Messa F., et al. Identification and molecular characterization of recurrent genomic deletions on 7p12 in the IKZF1 gene in a large cohort of BCR-ABL1–positive acute lymphoblastic leukemia patients: On behalf of Gruppo Italiano Malattie Ematologiche dell’Adulto Acute Leukemia Working Party (GIMEMA AL WP) Blood. 2009;114:2159–2167. doi: 10.1182/blood-2008-08-173963. [DOI] [PubMed] [Google Scholar]
- 73.Martinelli G., Iacobucci I., Storlazzi C.T., Vignetti M., Paoloni F., Cilloni D., Soverini S., Vitale A., Chiaretti S., Cimino G., et al. IKZF1 (Ikaros) Deletions in BCR-ABL1–Positive Acute Lymphoblastic Leukemia Are Associated with Short Disease-Free Survival and High Rate of Cumulative Incidence of Relapse: A GIMEMA AL WP Report. J. Clin. Oncol. 2009;27:5202–5207. doi: 10.1200/JCO.2008.21.6408. [DOI] [PubMed] [Google Scholar]
- 74.Liu Y.-F., Wang B.-Y., Zhang W.-N., Huang J.-Y., Li B.-S., Zhang M., Jiang L., Li J.-F., Wang M.-J., Dai Y.-J., et al. Genomic Profiling of Adult and Pediatric B-cell Acute Lymphoblastic Leukemia. EBioMedicine. 2016;8:173–183. doi: 10.1016/j.ebiom.2016.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lilljebjörn H., Henningsson R., Wittsten A.H., Olsson L., Orsmark-Pietras C., Von Palffy S., Askmyr M., Rissler M., Schrappe M., Cario M.S.G., et al. Identification of ETV6-RUNX1-like and DUX4-rearranged subtypes in paediatric B-cell precursor acute lymphoblastic leukaemia. Nat. Commun. 2016;7:11790. doi: 10.1038/ncomms11790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yasuda T., Tsuzuki S., Kawazu M., Hayakawa F., Kojima S., Ueno T., Imoto N., Kohsaka S., Kunita A., Doi K., et al. Recurrent DUX4 fusions in B cell acute lymphoblastic leukemia of adolescents and young adults. Nat. Genet. 2016;48:569–574. doi: 10.1038/ng.3535. [DOI] [PubMed] [Google Scholar]
- 77.Zhang J., McCastlain K., Yoshihara H., Xu B., Chang Y., Churchman M.L., Wu G., Li Y., Wei L., Iacobucci I., et al. Deregulation of DUX4 and ERG in acute lymphoblastic leukemia. Nat. Genet. 2016;48:1481–1489. doi: 10.1038/ng.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dib C., Zakharova V., Popova E., Kiseleva E., Chernyak B., Lipinski M., Vassetzky Y.S. DUX4 Pathological Expression: Causes and Consequences in Cancer. Trends Cancer. 2019;5:268–271. doi: 10.1016/j.trecan.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 79.Himeda C.L., Jones P.L. The Genetics and Epigenetics of Facioscapulohumeral Muscular Dystrophy. Annu. Rev. Genom. Hum. Genet. 2019;20:265–291. doi: 10.1146/annurev-genom-083118-014933. [DOI] [PubMed] [Google Scholar]
- 80.Miettinen M., Felisiak-Golabek A., Contreras A.L., Glod J., Kaplan R.N., Killian J.K., Lasota J. New fusion sarcomas: Histopathology and clinical significance of selected entities. Hum. Pathol. 2019;86:57–65. doi: 10.1016/j.humpath.2018.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sirvent N., Trassard M., Ebran N., Attias R., Pedeutour F. Fusion of EWSR1 with the DUX4 facioscapulohumeral muscular dystrophy region resulting from t(4;22)(q35;q12) in a case of embryonal rhabdomyosarcoma. Cancer Genet. Cytogenet. 2009;195:12–18. doi: 10.1016/j.cancergencyto.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 82.Jeha S., Choi J., Roberts K.G., Pei D., Coustan-Smith E., Inaba H., Rubnitz J.E., Ribeiro R.C., Gruber T.A., Raimondi S.C., et al. Clinical Significance of Novel Subtypes of Acute Lymphoblastic Leukemia in the Context of Minimal Residual Disease–Directed Therapy. Blood Cancer Discov. 2021;2:326–337. doi: 10.1158/2643-3230.BCD-20-0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Paietta E., Roberts K.G., Wang V., Gu Z., Buck G., Pei D., Cheng C., Levine R.L., Abdel-Wahab O., Cheng Z., et al. Molecular Classification Improves Risk Assessment in Adult BCR-ABL1-negative B-ALL. Blood. 2021 doi: 10.1182/blood.2020010144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schinnerl D., Mejstrikova E., Schumich A., Zaliova M., Fortschegger K., Nebral K., Attarbaschi A., Fiser K., Kauer M.O., Popitsch N., et al. CD371 cell surface expression: A unique feature of DUX4-rearranged acute lymphoblastic leukemia. Haematologica. 2019;104:e352–e355. doi: 10.3324/haematol.2018.214353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gu Z., Churchman M., Roberts K., Li Y., Liu Y., Harvey R.C., McCastlain K., Reshmi S.C., Payne-Turner D., Iacobucci I., et al. Genomic analyses identify recurrent MEF2D fusions in acute lymphoblastic leukaemia. Nat. Commun. 2016;7:13331. doi: 10.1038/ncomms13331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Suzuki K., Okuno Y., Kawashima N., Muramatsu H., Okuno T., Wang X., Kataoka S., Sekiya Y., Hamada M., Murakami N., et al. MEF2D-BCL9 Fusion Gene Is Associated With High-Risk Acute B-Cell Precursor Lymphoblastic Leukemia in Adolescents. J. Clin. Oncol. 2016;34:3451–3459. doi: 10.1200/JCO.2016.66.5547. [DOI] [PubMed] [Google Scholar]
- 87.Ohki K., Kiyokawa N., Saito Y., Hirabayashi S., Nakabayashi K., Ichikawa H., Momozawa Y., Okamura K., Yoshimi A., Ogata-Kawata H., et al. Clinical and molecular characteristics of MEF2D fusion-positive B-cell precursor acute lymphoblastic leukemia in childhood, including a novel translocation resulting in MEF2D-HNRNPH1 gene fusion. Haematologica. 2018;104:128–137. doi: 10.3324/haematol.2017.186320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ueno H., Yoshida K., Shiozawa Y., Nannya Y., Iijima-Yamashita Y., Kiyokawa N., Shiraishi Y., Chiba K., Tanaka H., Isobe T., et al. Landscape of driver mutations and their clinical impacts in pediatric B-cell precursor acute lymphoblastic leukemia. Blood Adv. 2020;4:5165–5173. doi: 10.1182/bloodadvances.2019001307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tsuzuki S., Yasuda T., Kojima S., Kawazu M., Akahane K., Inukai T., Imaizumi M., Morishita T., Miyamura K., Ueno T., et al. Targeting MEF2D-fusion Oncogenic Transcriptional Circuitries in B-cell Precursor Acute Lymphoblastic Leukemia. Blood Cancer Discov. 2020;1:82–95. doi: 10.1158/2643-3230.BCD-19-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tange N., Hayakawa F., Yasuda T., Odaira K., Yamamoto H., Hirano D., Sakai T., Terakura S., Tsuzuki S., Kiyoi H. Staurosporine and venetoclax induce the caspase-dependent proteolysis of MEF2D-fusion proteins and apoptosis in MEF2D-fusion (+) ALL cells. Biomed. Pharmacother. 2020;128:110330. doi: 10.1016/j.biopha.2020.110330. [DOI] [PubMed] [Google Scholar]
- 91.Zaliova M., Stuchly J., Winkowska L., Musilova A., Fiser K., Slamova M., Starkova J., Vaskova M., Hrusak O., Sramkova L., et al. Genomic landscape of pediatric B-other acute lymphoblastic leukemia in a consecutive European cohort. Haematologica. 2019;104:1396–1406. doi: 10.3324/haematol.2018.204974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Alexander T.B., Gu Z., Iacobucci I., Dickerson K., Choi J.K., Xu B., Payne-Turner D., Yoshihara H., Loh M.L., Horan J., et al. The genetic basis and cell of origin of mixed phenotype acute leukaemia. Nature. 2018;562:373–379. doi: 10.1038/s41586-018-0436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hirabayashi S., Butler E.R., Ohki K., Kiyokawa N., Bergmann A.K., Möricke A., Boer J.M., Cavé H., Cazzaniga G., Yeoh A.E.J., et al. Clinical characteristics and outcomes of B-ALL with ZNF384 rearrangements: A retrospective analysis by the Ponte di Legno Childhood ALL Working Group. Leukemia. 2021:1–6. doi: 10.1038/s41375-021-01199-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hirabayashi S., Ohki K., Nakabayashi K., Ichikawa H., Momozawa Y., Okamura K., Yaguchi A., Terada K., Saito Y., Yoshimi A., et al. ZNF384-related fusion genes define a subgroup of childhood B-cell precursor acute lymphoblastic leukemia with a characteristic immunotype. Haematologica. 2016;102:118–129. doi: 10.3324/haematol.2016.151035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Janet N.B., Kulkarni U., Arun A.K., Bensega B., Devasia A.J., Korula A., Abraham A., George B., Mathews V., Balasubramanian P. Systematic application of fluorescence in situ hybridization and immunophenotype profile for the identification of ZNF384 gene rearrangements in B cell acute lymphoblastic leukemia. Int. J. Lab. Hematol. 2021;43:658–663. doi: 10.1111/ijlh.13580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bueno C., Tejedor J.R., Bashford-Rogers R., González-Silva L., Valdés-Mas R., Agraz-Doblás A., de la Guardia R.D., Ribera J., Zamora L., Bilhou-Nabera C., et al. Natural history and cell of origin of TCF3-ZNF384 and PTPN11 mutations in monozygotic twins with concordant BCP-ALL. Blood. 2019;134:900–905. doi: 10.1182/blood.2019000893. [DOI] [PubMed] [Google Scholar]
- 97.Griffith M., Griffith O.L., Krysiak K., Skidmore Z., Christopher M.J., Klco J., Ramu A., Lamprecht T.L., Wagner A.H., Campbell K., et al. Comprehensive genomic analysis reveals FLT3 activation and a therapeutic strategy for a patient with relapsed adult B-lymphoblastic leukemia. Exp. Hematol. 2016;44:603–613. doi: 10.1016/j.exphem.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boer J.M., Valsecchi M.G., Hormann F.M., Antic Z., Zaliova M., Schwab C., Cazzaniga G., Arfeuille C., Cave H., Attarbaschi A., et al. Favorable outcome of NUTM1-rearranged infant and pediatric B cell precursor acute lymphoblastic leukemia in a collaborative international study. Leukemia. 2021:1–5. doi: 10.1038/s41375-021-01333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hormann F.M., Hoogkamer A.Q., Beverloo H.B., Boeree A., Dingjan I., Wattel M.M., Stam R.W., Escherich G., Pieters R., Boer M.L.D., et al. NUTM1 is a recurrent fusion gene partner in B-cell precursor acute lymphoblastic leukemia associated with increased expression of genes on chromosome band 10p12.31-12.2. Haematologica. 2019;104:e455–e459. doi: 10.3324/haematol.2018.206961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.McEvoy C.R., Fox S.B., Prall O.W.J. Emerging entities in NUTM1-rearranged neoplasms. Genes Chromosom. Cancer. 2020;59:375–385. doi: 10.1002/gcc.22838. [DOI] [PubMed] [Google Scholar]
- 101.French C.A. NUT Carcinoma: Clinicopathologic features, pathogenesis, and treatment. Pathol. Int. 2018;68:583–595. doi: 10.1111/pin.12727. [DOI] [PubMed] [Google Scholar]
- 102.Boer M.L.D., van Slegtenhorst M., De Menezes R.X., Cheok M., Buijs-Gladdines J.G., Peters S.T., Van Zutven L.J., Beverloo H.B., Van der Spek P.J., Escherich G., et al. A subtype of childhood acute lymphoblastic leukaemia with poor treatment outcome: A genome-wide classification study. Lancet Oncol. 2009;10:125–134. doi: 10.1016/S1470-2045(08)70339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mullighan C., Su X., Zhang J., Radtke I., Phillips L.A., Miller C.B., Ma J., Liu W., Cheng C., Schulman B.A., et al. Deletion of IKZF1and Prognosis in Acute Lymphoblastic Leukemia. N. Engl. J. Med. 2009;360:470–480. doi: 10.1056/NEJMoa0808253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Iacobucci I., Roberts K. Genetic Alterations and Therapeutic Targeting of Philadelphia-Like Acute Lymphoblastic Leukemia. Genes. 2021;12:687. doi: 10.3390/genes12050687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Roberts K.G., Reshmi S.C., Harvey R., Chen I.-M., Patel K., Stonerock E., Jenkins H., Dai Y., Valentine M., Gu Z., et al. Genomic and outcome analyses of Ph-like ALL in NCI standard-risk patients: A report from the Children’s Oncology Group. Blood. 2018;132:815–824. doi: 10.1182/blood-2018-04-841676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Reshmi S.C., Harvey R.C., Roberts K.G., Stonerock E., Smith A., Jenkins H., Chen I.-M., Valentine M., Liu Y., Li Y., et al. Targetable kinase gene fusions in high-risk B-ALL: A study from the Children’s Oncology Group. Blood. 2017;129:3352–3361. doi: 10.1182/blood-2016-12-758979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tasian S.K., Hurtz C., Wertheim G.B., Bailey N., Lim M., Harvey R., Chen I.-M., Willman C.L., Astles R., Zebrowski A., et al. High incidence of Philadelphia chromosome-like acute lymphoblastic leukemia in older adults with B-ALL. Leukemia. 2016;31:981–984. doi: 10.1038/leu.2016.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jain N., Roberts K.G., Jabbour E., Patel K., Eterovic A.K., Chen K., Zweidler-McKay P., Lu X., Fawcett G., Wang S.A., et al. Ph-like acute lymphoblastic leukemia: A high-risk subtype in adults. Blood. 2017;129:572–581. doi: 10.1182/blood-2016-07-726588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Roberts K.G. The biology of Philadelphia chromosome-like ALL. Best Pract. Res. Clin. Haematol. 2017;30:212–221. doi: 10.1016/j.beha.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 110.Chiaretti S., Messina M., Foà R. BCR/ABL1-like acute lymphoblastic leukemia: How to diagnose and treat? Cancer. 2018;125:194–204. doi: 10.1002/cncr.31848. [DOI] [PubMed] [Google Scholar]
- 111.Mullighan C.G., Collins-Underwood J.R., Phillips L.A., Loudin M.G., Liu W., Zhang J., Ma J., Coustan-Smith E., Harvey R.C., Willman C.L., et al. Rearrangement of CRLF2 in B-progenitor–and Down syndrome–associated acute lymphoblastic leukemia. Nat. Genet. 2009;41:1243–1246. doi: 10.1038/ng.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yoda A., Yoda Y., Chiaretti S., Bar-Natan M., Mani K., Rodig S.J., West N., Xiao Y., Brown J.R., Mitsiades C., et al. Functional screening identifies CRLF2 in precursor B-cell acute lymphoblastic leukemia. Proc. Natl. Acad. Sci. USA. 2009;107:252–257. doi: 10.1073/pnas.0911726107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Russell L.J., Jones L., Enshaei A., Tonin S., Ryan S.L., Eswaran J., Nakjang S., Papaemmanuil E., Tubio J.M.C., Fielding A.K., et al. Characterisation of the genomic landscape ofCRLF2-rearranged acute lymphoblastic leukemia. Genes Chromosom. Cancer. 2017;56:363–372. doi: 10.1002/gcc.22439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hertzberg L., Vendramini E., Ganmore I., Cazzaniga G., Schmitz M., Chalker J., Shiloh R., Iacobucci I., Shochat C., Zeligson S., et al. Down syndrome acute lymphoblastic leukemia, a highly heterogeneous disease in which aberrant expression of CRLF2 is associated with mutated JAK2: A report from the International BFM Study Group. Blood. 2010;115:1006–1017. doi: 10.1182/blood-2009-08-235408. [DOI] [PubMed] [Google Scholar]
- 115.Iacobucci I., Li Y., Roberts K.G., Dobson S.M., Kim J.C., Payne-Turner D., Harvey R.C., Valentine M., McCastlain K., Easton J., et al. Truncating Erythropoietin Receptor Rearrangements in Acute Lymphoblastic Leukemia. Cancer Cell. 2016;29:186–200. doi: 10.1016/j.ccell.2015.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Stanulla M., Dagdan E., Zaliova M., Möricke A., Palmi C., Cazzaniga G., Eckert C., Kronnie G.T., Bourquin J.-P., Bornhauser B., et al. IKZF1plus Defines a New Minimal Residual Disease–Dependent Very-Poor Prognostic Profile in Pediatric B-Cell Precursor Acute Lymphoblastic Leukemia. J. Clin. Oncol. 2018;36:1240–1249. doi: 10.1200/JCO.2017.74.3617. [DOI] [PubMed] [Google Scholar]
- 117.Tanasi I., Ba I., Sirvent N., Braun T., Cuccuini W., Ballerini P., Duployez N., Tanguy-Schmidt A., Tamburini J., Maury S., et al. Efficacy of tyrosine kinase inhibitors in Ph-like acute lymphoblastic leukemia harboring ABL-class rearrangements. Blood. 2019;134:1351–1355. doi: 10.1182/blood.2019001244. [DOI] [PubMed] [Google Scholar]
- 118.Schewe D.M., Lenk L., Vogiatzi F., Winterberg D., Rademacher A.V., Buchmann S., Henry D., Bergmann A.K., Cario G., Cox M.C. Larotrectinib in TRK fusion–positive pediatric B-cell acute lymphoblastic leukemia. Blood Adv. 2019;3:3499–3502. doi: 10.1182/bloodadvances.2019000700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Niswander L.M., Loftus J.P., Lainey E., Caye-Eude A., Pondrom M., Hottman D.A., Iacobucci I., Mullighan C.G., Jain N., Konopleva M., et al. Therapeutic potential of ruxolitinib and ponatinib in patients with EPOR-rearranged Philadelphia chromosome-like acute lymphoblastic leukemia. Haematologica. 2021 doi: 10.3324/haematol.2021.278697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chang Y., Min J., Jarusiewicz J., Actis M., Bradford S.Y.-C., Mayasundari A., Yang L., Chepyala D., Alcock L.J., Roberts K.G., et al. Degradation of Janus kinases in CRLF2-rearranged acute lymphoblastic leukemia. Blood. 2021 doi: 10.1182/blood.2020006846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Qin H., Cho M., Haso W., Zhang L., Tasian S.K., Oo H.Z., Negri G.L., Lin Y., Zou J., Mallon B.S., et al. Eradication of B-ALL using chimeric antigen receptor–expressing T cells targeting the TSLPR oncoprotein. Blood. 2015;126:629–639. doi: 10.1182/blood-2014-11-612903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zaliova M., Kotrová M., Bresolin S., Stuchly J., Stary J., Hrusak O., Kronnie G.T., Trka J., Zuna J., Vaskova M. ETV6/RUNX1-like acute lymphoblastic leukemia: A novel B-cell precursor leukemia subtype associated with the CD27/CD44 immunophenotype. Genes Chromosom. Cancer. 2017;56:608–616. doi: 10.1002/gcc.22464. [DOI] [PubMed] [Google Scholar]
- 123.Zaliova M., Moorman A.V., Cazzaniga G., Stanulla M., Harvey R.C., Roberts K.G., Heatley S.L., Loh M.L., Konopleva M., Chen I.-M., et al. Characterization of leukemias with ETV6-ABL1 fusion. Haematologica. 2016;101:1082–1093. doi: 10.3324/haematol.2016.144345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nishii R., Baskin-Doerfler R., Yang W., Oak N., Zhao X., Yang W., Hoshitsuki K., Bloom M., Verbist K.C., Burns M.A., et al. Molecular basis of ETV6-mediated predisposition to childhood acute lymphoblastic leukemia. Blood. 2021;137:364–373. doi: 10.1182/blood.2020006164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bastian L., Schroeder M.P., Eckert C., Schlee C., Tanchez J.O., Kämpf S., Wagner D.L., Schulze V., Isaakidis K., Lázaro-Navarro J., et al. PAX5 biallelic genomic alterations define a novel subgroup of B-cell precursor acute lymphoblastic leukemia. Leukemia. 2019;33:1895–1909. doi: 10.1038/s41375-019-0430-z. [DOI] [PubMed] [Google Scholar]
- 126.Passet M., Boissel N., Sigaux F., Saillard C., Bargetzi M., Ba I., Thomas X., Graux C., Chalandon Y., Leguay T., et al. PAX5 P80R mutation identifies a novel subtype of B-cell precursor acute lymphoblastic leukemia with favorable outcome. Blood. 2019;133:280–284. doi: 10.1182/blood-2018-10-882142. [DOI] [PubMed] [Google Scholar]
- 127.Shah S., Schrader K., Waanders E., Timms A.E., Vijai J., Miething C., Wechsler J., Yang J., Hayes J., Klein R., et al. A recurrent germline PAX5 mutation confers susceptibility to pre-B cell acute lymphoblastic leukemia. Nat. Genet. 2013;45:1226–1231. doi: 10.1038/ng.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Vairy S., Tran T.H. IKZF1 alterations in acute lymphoblastic leukemia: The good, the bad and the ugly. Blood Rev. 2020;44:100677. doi: 10.1016/j.blre.2020.100677. [DOI] [PubMed] [Google Scholar]
- 129.Churchman M.L., Mullighan C.G. Ikaros: Exploiting and targeting the hematopoietic stem cell niche in B-progenitor acute lymphoblastic leukemia. Exp. Hematol. 2016;46:1–8. doi: 10.1016/j.exphem.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Churchman M.L., Low J., Qu C., Paietta E.M., Kasper L.H., Chang Y., Payne-Turner D., Althoff M.J., Song G., Chen S.-C., et al. Efficacy of Retinoids in IKZF1-Mutated BCR-ABL1 Acute Lymphoblastic Leukemia. Cancer Cell. 2015;28:343–356. doi: 10.1016/j.ccell.2015.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zaliova M., Potuckova E., Lukes J., Winkowska L., Starkova J., Janotova I., Sramkova L., Stary J., Zuna J., Stanulla M., et al. Frequency and prognostic impact of ZEB2 H1038 and Q1072 mutations in childhood B-other acute lymphoblastic leukemia. Haematologica. 2020;106:886–890. doi: 10.3324/haematol.2020.249094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Aifantis I., Raetz E.A., Buonamici S. Molecular pathogenesis of T-cell leukaemia and lymphoma. Nat. Rev. Immunol. 2008;8:380–390. doi: 10.1038/nri2304. [DOI] [PubMed] [Google Scholar]
- 133.Yui M., Rothenberg E. Developmental gene networks: A triathlon on the course to T cell identity. Nat. Rev. Immunol. 2014;14:529–545. doi: 10.1038/nri3702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Teachey D.T., Pui C.-H. Comparative features and outcomes between paediatric T-cell and B-cell acute lymphoblastic leukaemia. Lancet Oncol. 2019;20:e142–e154. doi: 10.1016/S1470-2045(19)30031-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Liu Y., Easton J., Shao Y., Maciaszek J., Wang Z., Wilkinson M.R., McCastlain K., Edmonson M., Pounds S.B., Shi L., et al. The genomic landscape of pediatric and young adult T-lineage acute lymphoblastic leukemia. Nat. Genet. 2017;49:1211–1218. doi: 10.1038/ng.3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Seki M., Kimura S., Isobe T., Yoshida K., Ueno H., Nakajima-Takagi Y., Wang C., Lin L., Kon A., Suzuki H., et al. Recurrent SPI1 (PU.1) fusions in high-risk pediatric T cell acute lymphoblastic leukemia. Nat. Genet. 2017;49:1274–1281. doi: 10.1038/ng.3900. [DOI] [PubMed] [Google Scholar]
- 137.Mansour M., Abraham B., Anders L., Berezovskaya A., Gutierrez A., Durbin A., Etchin J., Lawton L., Sallan S.E., Silverman L.B., et al. An oncogenic super-enhancer formed through somatic mutation of a noncoding intergenic element. Science. 2014;346:1373–1377. doi: 10.1126/science.1259037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hu S., Qian M., Zhang H., Guo Y., Yang J., Zhao X., He H., Lu J., Pan J., Chang M., et al. Whole-genome noncoding sequence analysis in T-cell acute lymphoblastic leukemia identifies oncogene enhancer mutations. Blood. 2017;129:3264–3268. doi: 10.1182/blood-2017-03-771162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Mansour M.R., Duke V., Foroni L., Patel B., Allen C., Ancliff P.J., Gale R.E., Linch D.C. Notch-1 Mutations Are Secondary Events in Some Patients with T-Cell Acute Lymphoblastic Leukemia. Clin. Cancer Res. 2007;13:6964–6969. doi: 10.1158/1078-0432.CCR-07-1474. [DOI] [PubMed] [Google Scholar]
- 140.Gianni F., Belver L., Ferrando A. The Genetics and Mechanisms of T-Cell Acute Lymphoblastic Leukemia. Cold Spring Harb. Perspect. Med. 2019;10:a035246. doi: 10.1101/cshperspect.a035246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Belver L., Ferrando L.B.A. The genetics and mechanisms of T cell acute lymphoblastic leukaemia. Nat. Rev. Cancer. 2016;16:494–507. doi: 10.1038/nrc.2016.63. [DOI] [PubMed] [Google Scholar]
- 142.Kimura S., Seki M., Kawai T., Goto H., Yoshida K., Isobe T., Sekiguchi M., Watanabe K., Kubota Y., Nannya Y., et al. DNA methylation-based classification reveals difference between pediatric T-cell acute lymphoblastic leukemia and normal thymocytes. Leukemia. 2019;34:1163–1168. doi: 10.1038/s41375-019-0626-2. [DOI] [PubMed] [Google Scholar]
- 143.Roels J., Thénoz M., Szarzyńska B., Landfors M., De Coninck S., Demoen L., Provez L., Kuchmiy A., Strubbe S., Reunes L., et al. Aging of Preleukemic Thymocytes Drives CpG Island Hypermethylation in T-cell Acute Lymphoblastic Leukemia. Blood Cancer Discov. 2020;1:274–289. doi: 10.1158/2643-3230.BCD-20-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ferrando A.A., Neuberg D.S., Staunton J., Loh M.L., Huard C., Raimondi S.C., Behm F.G., Pui C.-H., Downing J.R., Gilliland D., et al. Gene expression signatures define novel oncogenic pathways in T cell acute lymphoblastic leukemia. Cancer Cell. 2002;1:75–87. doi: 10.1016/S1535-6108(02)00018-1. [DOI] [PubMed] [Google Scholar]
- 145.Soulier J., Clappier E., Cayuela J.-M., Regnault A., García-Peydró M., Dombret H., Baruchel A., Toribio M.L., Sigaux F. HOXA genes are included in genetic and biologic networks defining human acute T-cell leukemia (T-ALL) Blood. 2005;106:274–286. doi: 10.1182/blood-2004-10-3900. [DOI] [PubMed] [Google Scholar]
- 146.Dadi S., Le Noir S., Bornet D.P., Lhermitte L., Zacarias-Cabeza J., Bergeron J., Villarèse P., Vachez E., Dik W.A., Millien C., et al. TLX Homeodomain Oncogenes Mediate T Cell Maturation Arrest in T-ALL via Interaction with ETS1 and Suppression of TCRα Gene Expression. Cancer Cell. 2012;21:563–576. doi: 10.1016/j.ccr.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 147.Di Giacomo D., La Starza R., Gorello P., Pellanera F., Atak Z.K., De Keersmaecker K., Pierini V., Harrison C.J., Arniani S., Moretti M., et al. 14q32 rearrangements deregulating BCL11B mark a distinct subgroup of T and myeloid immature acute leukemia. Blood. 2021 doi: 10.1182/blood.2020010510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Inaba H., Azzato E.M., Mullighan C.G. Integration of Next-Generation Sequencing to Treat Acute Lymphoblastic Leukemia with Targetable Lesions: The St. Jude Children’s Research Hospital Approach. Front. Pediatr. 2017;5:258. doi: 10.3389/fped.2017.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gocho Y., Liu J., Hu J., Yang W., Dharia N.V., Zhang J., Shi H., Du G., John A., Lin T.-N., et al. Network-based systems pharmacology reveals heterogeneity in LCK and BCL2 signaling and therapeutic sensitivity of T-cell acute lymphoblastic leukemia. Nat. Rev. Cancer. 2021;2:1–16. doi: 10.1038/s43018-020-00167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hnisz D., Weintraub A.S., Day D.S., Valton A.-L., Bak R., Li C., Goldmann J., Lajoie B.R., Fan Z.P., Sigova A.A., et al. Activation of proto-oncogenes by disruption of chromosome neighborhoods. Science. 2016;351:1454–1458. doi: 10.1126/science.aad9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Park S.T., Sun X.-H. The Tal1 Oncoprotein Inhibits E47-mediated Transcription. J. Biol. Chem. 1998;273:7030–7037. doi: 10.1074/jbc.273.12.7030. [DOI] [PubMed] [Google Scholar]
- 152.Sanda T., Lawton L.N., Barrasa M.I., Fan Z.P., Kohlhammer H., Gutierrez A., Ma W., Tatarek J., Ahn Y., Kelliher M.A., et al. Core Transcriptional Regulatory Circuit Controlled by the TAL1 Complex in Human T Cell Acute Lymphoblastic Leukemia. Cancer Cell. 2012;22:209–221. doi: 10.1016/j.ccr.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Nottingham W.T., Jarratt A., Burgess M., Speck C.L., Cheng J.F., Prabhakar S., Rubin E.M., Li P.S., Sloane-Stanley J., Kong A.S.J., et al. Runx1-mediated hematopoietic stem-cell emergence is controlled by a Gata/Ets/SCL-regulated enhancer. Blood. 2007;110:4188–4197. doi: 10.1182/blood-2007-07-100883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Choi A., Illendula A., Pulikkan J.A., Roderick J.E., Tesell J., Yu J., Hermance N., Zhu L.J., Castilla L.H., Bushweller J.H., et al. RUNX1 is required for oncogenic Myb and Myc enhancer activity in T-cell acute lymphoblastic leukemia. Blood. 2017;130:1722–1733. doi: 10.1182/blood-2017-03-775536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.O’Neil J., Shank J., Cusson N., Murre C., Kelliher M. TAL1/SCL induces leukemia by inhibiting the transcriptional activity of E47/HEB. Cancer Cell. 2004;5:587–596. doi: 10.1016/j.ccr.2004.05.023. [DOI] [PubMed] [Google Scholar]
- 156.Draheim K.M., Hermance N., Yang Y., Arous E., Calvo J., Kelliher M.A. A DNA-binding mutant of TAL1 cooperates with LMO2 to cause T cell leukemia in mice. Oncogene. 2010;30:1252–1260. doi: 10.1038/onc.2010.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ferrando A.A., Look A.T. Gene expression profiling in T-cell acute lymphoblastic leukemia. Semin. Hematol. 2003;40:274–280. doi: 10.1016/S0037-1963(03)00195-1. [DOI] [PubMed] [Google Scholar]
- 158.Leong W.Z., Tan S.H., Ngoc P.C.T., Amanda S., Yam A.W.Y., Liau W.-S., Gong Z., Lawton L.N., Tenen D.G., Sanda T. ARID5B as a critical downstream target of the TAL1 complex that activates the oncogenic transcriptional program and promotes T-cell leukemogenesis. Genes Dev. 2017;31:2343–2360. doi: 10.1101/gad.302646.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tan S.H., Leong W.Z., Ngoc P.C.T., Tan T.K., Bertulfo F.C., Lim M.C., An O., Li Z., Yeoh A.E.J., Fullwood M.J., et al. The enhancer RNA ARIEL activates the oncogenic transcriptional program in T-cell acute lymphoblastic leukemia. Blood. 2019;134:239–251. doi: 10.1182/blood.2018874503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Piovan E., Yu J., Tosello V., Herranz D., Ambesi-Impiombato A., Da Silva A.C., Sanchez-Martin M., Perez-Garcia A., Rigo I., Castillo M., et al. Direct Reversal of Glucocorticoid Resistance by AKT Inhibition in Acute Lymphoblastic Leukemia. Cancer Cell. 2013;24:766–776. doi: 10.1016/j.ccr.2013.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jena N., Sheng J., Hu J.K., Li W., Zhou W., Lee G., Tsichlis N., Pathak A., Brown N., Deshpande A., et al. CDK6-mediated repression of CD25 is required for induction and maintenance of Notch1-induced T-cell acute lymphoblastic leukemia. Leukemia. 2015;30:1033–1043. doi: 10.1038/leu.2015.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Coustan-Smith E., Mullighan C., Onciu M., Behm F.G., Raimondi S.C., Pei D., Cheng C., Su X., Rubnitz J., Basso G., et al. Early T-cell precursor leukaemia: A subtype of very high-risk acute lymphoblastic leukaemia. Lancet Oncol. 2009;10:147–156. doi: 10.1016/S1470-2045(08)70314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhang J., Ding L., Holmfeldt L., Wu G., Heatley S., Payne-Turner D., Easton J., Chen X., Wang J., Rusch M., et al. The genetic basis of early T-cell precursor acute lymphoblastic leukaemia. Nature. 2012;481:157–163. doi: 10.1038/nature10725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Maude S.L., Dolai S., Delgado-Martin C., Vincent T., Robbins A., Selvanathan A., Ryan T., Hall J., Wood A.C., Tasian S.K., et al. Efficacy of JAK/STAT pathway inhibition in murine xenograft models of early T-cell precursor (ETP) acute lymphoblastic leukemia. Blood. 2015;125:1759–1767. doi: 10.1182/blood-2014-06-580480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.McCarter A.C., Wang Q., Chiang M. Notch in Leukemia. Adv. Exp. Med. Biol. 2018;1066:355–394. doi: 10.1007/978-3-319-89512-3_18. [DOI] [PubMed] [Google Scholar]
- 166.Weng A., Ferrando A.A., Lee W., Iv J.P.M., Silverman L.B., Sanchez-Irizarry C., Blacklow S.C., Look A.T., Aster J.C. Activating Mutations of NOTCH1 in Human T Cell Acute Lymphoblastic Leukemia. Science. 2004;306:269–271. doi: 10.1126/science.1102160. [DOI] [PubMed] [Google Scholar]
- 167.Sulis M.L., Williams O., Palomero T., Tosello V., Pallikuppam S., Real P.J., Barnes K., Zuurbier L., Meijerink J.P., Ferrando A.A. NOTCH1 extracellular juxtamembrane expansion mutations in T-ALL. Blood. 2008;112:733–740. doi: 10.1182/blood-2007-12-130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Haydu J.E., De Keersmaecker K., Duff M.K., Paietta E., Racevskis J., Wiernik P.H., Rowe J.M., Ferrando A. An activating intragenic deletion in NOTCH1 in human T-ALL. Blood. 2012;119:5211–5214. doi: 10.1182/blood-2011-10-388504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Thompson B.J., Buonamici S., Sulis M.L., Palomero T., Vilimas T., Basso G., Ferrando A., Aifantis I. The SCFFBW7 ubiquitin ligase complex as a tumor suppressor in T cell leukemia. J. Exp. Med. 2007;204:1825–1835. doi: 10.1084/jem.20070872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.O’Neil J., Grim J., Strack P., Rao S., Tibbitts D., Winter C., Hardwick J., Welcker M., Meijerink J., Pieters R., et al. FBW7 mutations in leukemic cells mediate NOTCH pathway activation and resistance to γ-secretase inhibitors. J. Exp. Med. 2007;204:1813–1824. doi: 10.1084/jem.20070876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Suarez-Puente X., Beà S., Valdés-Mas R., Villamor N., Gutiérrez-Abril J., Martin-Subero J.I., Munar M., Rubio-Perez C., Jares P., Aymerich M., et al. Non-coding recurrent mutations in chronic lymphocytic leukaemia. Nature. 2015;526:519–524. doi: 10.1038/nature14666. [DOI] [PubMed] [Google Scholar]
- 172.Chiang M., Xu L., Shestova O., Histen G., L’Heureux S., Romany C., Childs M.E., Gimotty P.A., Aster J.C., Pear W.S. Leukemia-associated NOTCH1 alleles are weak tumor initiators but accelerate K-ras–initiated leukemia. J. Clin. Investig. 2008;118:3181–3194. doi: 10.1172/JCI35090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wendorff A.A., Quinn S.A., Rashkovan M., Madubata C.J., Ambesi-Impiombato A., Litzow M.R., Tallman M.S., Paietta E., Paganin M., Basso G., et al. Phf6 Loss Enhances HSC Self-Renewal Driving Tumor Initiation and Leukemia Stem Cell Activity in T-ALL. Cancer Discov. 2018;9:436–451. doi: 10.1158/2159-8290.CD-18-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Herranz D., Ambesi-Impiombato A., Palomero T., Schnell S.A., Belver L., Wendorff A.A., Xu L., Castillo-Martin M., Llobet-Navás D., Cordon-Cardo C., et al. A NOTCH1-driven MYC enhancer promotes T cell development, transformation and acute lymphoblastic leukemia. Nat. Med. 2014;20:1130–1137. doi: 10.1038/nm.3665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Albertí-Servera L., Demeyer S., Govaerts I., Swings T., De Bie J., Gielen O., Brociner M., Michaux L., Maertens J., Uyttebroeck A., et al. Single-cell DNA amplicon sequencing reveals clonal heterogeneity and evolution in T-cell acute lymphoblastic leukemia. Blood. 2021;137:801–811. doi: 10.1182/blood.2020006996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.De Bie J., Demeyer S., Alberti-Servera L., Geerdens E., Segers H., Broux M., De Keersmaecker K., Michaux L., Vandenberghe P., Voet T., et al. Single-cell sequencing reveals the origin and the order of mutation acquisition in T-cell acute lymphoblastic leukemia. Leukemia. 2018;32:1358–1369. doi: 10.1038/s41375-018-0127-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yashiro-Ohtani Y., Wang H., Zang C., Arnett K.L., Bailis W., Ho Y., Knoechel B., Lanauze C., Louis L., Forsyth K., et al. Long-range enhancer activity determinesMycsensitivity to Notch inhibitors in T cell leukemia. Proc. Natl. Acad. Sci. USA. 2014;111:E4946–E4953. doi: 10.1073/pnas.1407079111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Sanchez-Martin M., Ferrando A. The NOTCH1-MYC highway toward T-cell acute lymphoblastic leukemia. Blood. 2017;129:1124–1133. doi: 10.1182/blood-2016-09-692582. [DOI] [PubMed] [Google Scholar]
- 179.Reizis B. Direct induction of T lymphocyte-specific gene expression by the mammalian Notch signaling pathway. Genes Dev. 2002;16:295–300. doi: 10.1101/gad.960702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zheng R., Li M., Wang S., Liu Y. Advances of target therapy on NOTCH1 signaling pathway in T-cell acute lymphoblastic leukemia. Exp. Hematol. Oncol. 2020;9:31. doi: 10.1186/s40164-020-00187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Papayannidis C., De Angelo D.J., Stock W., Huang B., Shaik M.N., Cesari R., Zheng X., Reynolds J.M., English P.A., Ozeck M., et al. A Phase 1 study of the novel gamma-secretase inhibitor PF-03084014 in patients with T-cell acute lymphoblastic leukemia and T-cell lymphoblastic lymphoma. Blood Cancer J. 2015;5:e350. doi: 10.1038/bcj.2015.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Gavai A.V., Quesnelle C.A., Norris D.J., Han W.-C., Gill P.S., Shan W., Balog A., Chen K., Tebben A.J., Rampulla R., et al. Discovery of Clinical Candidate BMS-906024: A Potent Pan-Notch Inhibitor for the Treatment of Leukemia and Solid Tumors. ACS Med. Chem. Lett. 2015;6:523–527. doi: 10.1021/acsmedchemlett.5b00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Sanchez-Martin M., Ambesi-Impiombato A., Qin Y., Herranz D., Bansal M., Girardi T., Paietta E., Tallman M.S., Rowe J.M., De Keersmaecker K., et al. Synergistic antileukemic therapies inNOTCH1-induced T-ALL. Proc. Natl. Acad. Sci. USA. 2017;114:2006–2011. doi: 10.1073/pnas.1611831114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Wei P., Walls M., Qiu M., Ding R., Denlinger R.H., Wong A., Tsaparikos K., Jani J.P., Hosea N.A., Sands M., et al. Evaluation of Selective γ-Secretase Inhibitor PF-03084014 for Its Antitumor Efficacy and Gastrointestinal Safety to Guide Optimal Clinical Trial Design. Mol. Cancer Ther. 2010;9:1618–1628. doi: 10.1158/1535-7163.MCT-10-0034. [DOI] [PubMed] [Google Scholar]
- 185.Real P., Tosello V., Palomero T., Castillo M., Hernando E., De Stanchina E., Sulis M.L., Barnes K., Sawai C., Homminga I., et al. γ-secretase inhibitors reverse glucocorticoid resistance in T cell acute lymphoblastic leukemia. Nat. Med. 2008;15:50–58. doi: 10.1038/nm.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Cullion K., Draheim K.M., Hermance N., Tammam J., Sharma V.M., Ware C., Nikov G., Krishnamoorthy V., Majumder P.K., Kelliher M.A. Targeting the Notch1 and mTOR pathways in a mouse T-ALL model. Blood. 2009;113:6172–6181. doi: 10.1182/blood-2008-02-136762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Franciosa G., Smits J.G.A., Minuzzo S., Martinez-Val A., Indraccolo S., Olsen J.V. Proteomics of resistance to Notch1 inhibition in acute lymphoblastic leukemia reveals targetable kinase signatures. Nat. Commun. 2021;12:2507. doi: 10.1038/s41467-021-22787-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Trinquand A., Tanguy-Schmidt A., Ben Abdelali R., Lambert J., Beldjord K., Lengliné E., De Gunzburg N., Bornet D.P., Lhermitte L., Mossafa H., et al. Toward a NOTCH1/FBXW7/RAS/PTEN–Based Oncogenetic Risk Classification of Adult T-Cell Acute Lymphoblastic Leukemia: A Group for Research in Adult Acute Lymphoblastic Leukemia Study. J. Clin. Oncol. 2013;31:4333–4342. doi: 10.1200/JCO.2012.48.5292. [DOI] [PubMed] [Google Scholar]
- 189.Newman S., Nakitandwe J., Kesserwan C.A., Azzato E.M., Wheeler D.A., Rusch M., Shurtleff S., Hedges D.J., Hamilton K.V., Foy S.G., et al. Genomes for Kids: The scope of pathogenic mutations in pediatric cancer revealed by comprehensive DNA and RNA sequencing. Cancer Discov. 2021 doi: 10.1158/2159-8290.CD-20-1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jobanputra V., Wrzeszczynski K.O., Buttner R., Caldas C., Cuppen E., Grimmond S., Haferlach T., Mullighan C., Schuh A., Elemento O. Clinical interpretation of whole-genome and whole-transcriptome sequencing for precision oncology. Semin. Cancer Biol. 2021 doi: 10.1016/j.semcancer.2021.07.003. [DOI] [PubMed] [Google Scholar]
- 191.Rosenquist R., Cuppen E., Buettner R., Caldas C., Dreau H., Elemento O., Frederix G., Grimmond S., Haferlach T., Jobanputra V., et al. Clinical utility of whole-genome sequencing in precision oncology. Semin. Cancer Biol. 2021 doi: 10.1016/j.semcancer.2021.06.018. [DOI] [PubMed] [Google Scholar]
- 192.Meggendorfer M., Jobanputra V., Wrzeszczynski K.O., Roepman P., de Bruijn E., Cuppen E., Buttner R., Caldas C., Grimmond S., Mullighan C.G., et al. Analytical demands to use whole-genome sequencing in precision oncology. Semin. Cancer Biol. 2021 doi: 10.1016/j.semcancer.2021.06.009. [DOI] [PubMed] [Google Scholar]
- 193.Walter W., Shahswar R., Stengel A., Meggendorfer M., Kern W., Haferlach T., Haferlach C. Clinical application of whole transcriptome sequencing for the classification of patients with acute lymphoblastic leukemia. BMC Cancer. 2021;21:1–11. doi: 10.1186/s12885-021-08635-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Flensburg C., Oshlack A., Majewski I.J. Detecting copy number alterations in RNA-Seq using SuperFreq. Bioinformatics. 2021 doi: 10.1093/bioinformatics/btab440. [DOI] [PubMed] [Google Scholar]
- 195.He J., Abdel-Wahab O., Nahas M.K., Wang K., Rampal R.K., Intlekofer A., Patel J., Krivstov A., Frampton G., Young L.E., et al. Integrated genomic DNA/RNA profiling of hematologic malignancies in the clinical setting. Blood. 2016;127:3004–3014. doi: 10.1182/blood-2015-08-664649. [DOI] [PMC free article] [PubMed] [Google Scholar]