Abstract
Background
COVID-19 has introduced novel stressors into American adolescents’ lives. Studies have shown that adolescents adopt an array of coping mechanisms and social supports when contending with stress. It is unclear, though, which strategies are most effective in mitigating daily pandemic-related stress, as few micro-longitudinal studies have explored adolescents’ daily affect during COVID-19. Parental support may also be a critical component of adolescents’ pandemic-related coping, as adolescents’ peer networks have been limited by public health measures.
Methods
This longitudinal study examined links between stress, coping, parental support, and affect across 14 consecutive days and 6216 assessments from a national sample of adolescents (N=444; Mage=15.0; 60% female; 44% Black/African American, 39% White/Europen American, 9% Latinx, 6% Asian American, 2% Native American) during school closures and state-mandated stay-at-home orders between April 8 and April 21, 2021.
Results
Adolescents’ health and financial stress predicted increases in same-day (health stress’ effect size = .16; financial stress’ effect size = .11) and next-day negative affect (health stress’ effect size = .05; financial stress’ effect size = .08). Adolescents’ secondary control engagement coping predicted increases in same-day (effect size = .10) and next-day (effect size = .04) positive affect and moderated the link between health stress and negative affect. Parental social support predicted increases in same-day (effect size = .26) and next-day (effect size = .06) positive affect and decreases in same-day (effect size = .17) negative affect and moderated the link between financial stress and negative affect.
Limitations
Results are indicative of conditions at the immediate onset of COVID-19 and should be interpreted as such.
Conclusions
Findings provide information as to how health providers and parents can help adolescents mitigate the impact of COVID-19-related health and economic stressors on their psychological well-being. It remains critical to monitor the psychosocial impact of the pandemic on adolescents’ affect while continuing to identify personal and environmental protective factors for reducing harm and maximizing resilience.
Keywords: Stress, Coping, Parental support, Psychological well-being, COVID-19
1. Introduction
Stress during adolescence is a normative developmental phenomenon (Shankar and Park, 2016; Wang, M.-T., Degol, J. L., & Henry, D. A. 2020); however, during the COVID-19 pandemic, adolescents experienced circumstances that may have exacerbated these naturally occurring stressors, such as loss of education time, restricted access to peers, and disruption of daily routines (Fegert et al., 2020). Not only are these adolescents experiencing intensified versions of “typical” stressors, but they also have been impacted by pandemic-related concerns about infection, quarantine, and economic stability, all of which have been linked to feelings of ongoing, unavoidable stress (Brooks et al., 2020; Polizzi et al., 2020; Wang, M.-T., Scanlon, C. L., Hua, M., & Del Toro, J. 2021). As such, adolescents’ daily coping and the extent to which they receive social support from parents during this challenging time may have consequences for their psychological well-being (Cicchetti and Rogosch, 2002; Luthar and Brown, 2007).
Studies have shown that adolescents adopt a wide array of coping mechanisms when contending with stress (Compas et al., 2017; Skinner and Zimmer-Gembeck, 2007). For instance, some adolescents tend to use coping strategies that directly impact a situation; others may use strategies aimed at adapting to a challenging situation; still others may opt to avoid the stressor completely (Connor-Smith et al., 2000). While extant literature has supported the typology of these coping strategies, it is unclear which strategies are most effective in mitigating daily pandemic-related stress. Moreover, adolescents often rely on their social networks—including their parents—to provide support during times of crisis (Cook et al., 2016; Kolak et al., 2018; McMahon et al., 2020; Wang, M.-T. & Eccles, J. S. 2012). Parental social support in the time of COVID-19 may be a critical component of positive adolescent adjustment, as adolescents’ peer networks were limited by stay-at-home orders. Thus, it is imperative to understand adolescents’ daily experiences of pandemic-related stress and which coping strategies and supports buffer against the effect of stress on psychological well-being.
In this study, we used a daily-diary approach to examine the longitudinal links of COVID-related stress, coping strategies, and parental support with adolescents’ daily affect at the onset of a global pandemic. We also investigated the mitigating role of coping strategies and parental support in the link between stress and adolescents’ affect. The 14-day micro-longitudinal design along with a nationwide American sample provide a novel insight into real-time adolescent stress and adjustment during a pandemic.
1.1. Theoretical and empirical rationale
Drawing from the strength-based ecological framework of risk and resilience, we aim to understand the context of stress surrounding American adolescents during the COVID-19 pandemic and identify ways to promote psychological wellness (Cowen, 1994). According to Kirby and Fraser (1997), an individual's overall well-being is closely linked to their daily experiences of risk and protective factors. Risk factors refer to situations or circumstances that increase maladjustment, such as daily stress, a hostile parent-child relationship, or maladaptive coping. Risk factors present adolescents with adversities that impede their ability to fulfill needs, acquire competencies, and form relationships with others (Sandler, 2001), thereby raising the likelihood of maladaptive functioning (Cicchetti and Rogosch, 2002). Conversely, protective factors are internal or external resources (e.g., adaptive coping skills or social support, respectively) that not only lead to increased well-being but also buffer against the nefarious effects of risk factors. It is posited that these protective factors contribute to resilience—an individual's capacity to endure, persist, and triumph despite stressful circumstances (Corcoran and Nichols-Casebolt, 2004; Luthar and Brown, 2007).
2. Adolescent stress and psychosocial well-being
We focused on health and financial stressors since these stressors have been prominently featured in extant literature addressing COVID-19 (e.g., Polizzi et al. 2020) and adolescents are limited in their ability to directly change circumstances contributing to their pandemic-related health and financial worries.
2.1. Pandemic-related health stress
The potential for COVID-19 infection and death confronted adolescents with stressors related to their own and loved ones’ well-being. Polizzi et al. (2020) warned against impending health-related stressors during the nascent stages of the COVID-19 outbreak, cautioning that individuals may start worrying about their own and others’ risk of infection or death. In addition, news media were saturated with infection and mortality rates, and fear of interacting with COVID-19-infected individuals has been documented (Lin, 2020; Polizzi et al., 2020). Consequently, COVID-19’s pandemic nature likely exacerbated fear and worry that resulted in stigmatization and anxiety (Guan et al., 2020). Scholars have shown that pandemics are tied to helplessness and hopelessness (Polizzi et al., 2020) as well as to loneliness and social isolation (Loades et al., 2020), all of which are hallmark emotions associated with affective disorders. For adolescents, worry over losing a loved one and the actual loss of a loved one have been connected to significant mental health problems (Stikkelbroek et al., 2016). Hence, pandemic-related stress over the potential infection and death of loved ones may put adolescents at risk for affective maladjustment.
2.2. Pandemic-related financial stress
With more than 44.2 million Americans filing for unemployment during the first 2.5 months of the COVID-19 pandemic (Lambert, 2020) and the closing of schools abruptly challenging food security for many children dependent on government-subsidized meals (Van Lancker and Parolin, 2020), COVID-19 drastically increased financial stressors faced by adolescents and their families (Prime et al., 2020). Researchers have long understood that financial stress deleteriously depletes the cognitive, social, and emotional resources available for coping with other life stressors (Wadsworth, 2015). In adolescents, financial stress has been associated with a higher likelihood of poor mental health (Arbel et al., 2018; Schneider et al., 2015). For instance, Santiago and colleagues (2011) found that elevated financial stress was associated with increased anxiety, depression, and attention difficulties. Because Americans are generally unprepared for even a minor financial emergency (McGrath, 2016), many adolescents may have experienced heightened economic stress surrounding the potential for or actuality of their parents losing their job and the ability to obtain basic needs during COVID-19.
2.3. Coping and adolescent affect
The Responses to Stress Model identifies coping as a buffer in the relation between stress and adjustment while also distinguishing between engagement/approach coping and disengagement/avoidance coping (Connor-Smith et al., 2000). On the one hand, engagement coping is composed of primary and secondary control coping. Primary control engagement coping involves altering a stressor or one's response to a stressor by using strategies such as problem solving, emotional expression, and emotion regulation. Secondary control engagement coping encompasses adapting to a stressor through acceptance, cognitive restructuring, positive thinking, or distraction. On the other hand, disengagement coping encompasses behavioral, affective, and cognitive avoidance.
Compas et al. (2017) concluded that both primary and secondary control engagement coping were associated with adaptive psychological well-being, including heightened positive affect and lowered negative affect. Both types of coping have been linked to better psychological functioning in the context of poverty-related and traumatic stress (Wadsworth et al., 2011). Conversely, adolescents using disengagement strategies (e.g., avoidance, denial, and wishful thinking) as a means of coping with stress have a higher risk of experiencing emotional maladjustment (Compas et al., 2017). Yet, it is noteworthy that certain types of coping strategies may operate differentially on adolescents’ affect pending the duration and intensity of stress. For instance, Jensen et al. (2013) found that although problem solving (i.e., primary control engagement coping) was often the go-to coping strategy for many adolescents, distraction (i.e., secondary control engagement coping) and avoidance (i.e., disengagement coping) were the most widely used adolescent coping strategies when faced with life-threatening situations. Since the context of stress surrounding the novel coronavirus has been ongoing and unavoidable, coping via disengagement strategies (e.g., situation avoidance) may not be possible. Conversely, acceptance, distraction, cognitive restructuring, and/or optimistic thinking (i.e., secondary control engagement coping) may provide immediate relief from intense stressors (Sheppes and Gross, 2011).
2.4. Parental support and adolescent affect
Parental support has been identified as one of the most effective protective factors during uncontrollably high periods of stress (Rodriguez-Llanes et al., 2013). Since adolescents were likely spending more time at home due to stay-at-home orders, the role of parental social support may be especially critical for their children's psychological well-being during the pandemic (Pfefferbaum et al., 2014). Indeed, family cohesion and parental emotional support have been connected to positive affect throughout adolescence, and secure parent-child relationships have been found to buffer against the effects of stress during challenging times (Cook et al., 2016; Kolak et al., 2018; McMahon et al., 2020). Prosocial relationships with parents have also been linked to resilience in the face of adversity (Luthar, 2006), and researchers have established that parental social support has a direct positive effect on adolescents’ affect, especially following exposure to mass trauma (Dimitry, 2012; Kronenberg et al., 2010).
2.5. The current study
Despite the psychological consequences associated with pandemic-related public health measures (Brooks et al., 2020), most studies examining the impact of pandemics have focused on medical personnel or other adults. Even fewer longitudinal studies have examined the effect of pandemic-related stress on adolescents’ daily affect, leaving much to be learned about adolescents’ daily responses to stress during pandemics. To capture adolescents’ daily stress, coping, parental support, and affect at the onset of the pandemic, we examined a nationwide sample using daily-diary approaches across 14 days. Our study was uniquely situated in the context of a burgeoning pandemic and can provide an intensive view into adolescents’ everyday experiences and behaviors as they unfold in real time. Moreover, the daily-diary approach minimized systematic recall bias and examined within-person processes and variability in these processes over time (Bolger et al., 2003).
In this study, we investigated (a) same- and next-day links between pandemic-related health and financial stress and adolescents’ affect, (b) same- and next-day links between coping strategies and parental support and adolescents’ affect, and (c) the moderating effect of coping strategies and parental support on the link between adolescents’ stress and their affect. We hypothesized that higher levels of health and financial stress would be positively correlated with negative affect. Moreover, we expected that secondary control engagement coping and parental support would link to increased positive affect and decreased negative affect. Finally, we anticipated that the link between stress and affect would vary by adolescents’ secondary control engagement coping or parental support, though we refrained from specific hypotheses regarding the strength and pattern of moderation effects due to a limited literature base.
3. Methods
3.1. Participants
This study used data from an ongoing nationwide longitudinal study examining school experiences, family functioning, and adolescent well-being in the United States. The original study recruited a national sample of adolescents by using a representative, random sampling method. When COVID-19 was declared a national emergency in the United States in March 2020, the original longitudinal study was leveraged by inviting a subsample of adolescent participants to participate in a 14-day daily-diary study focusing on adolescents’ stress and adjustment during the pandemic. As a condition of participation, participants’ state governments had to have issued stay-at-home orders that mandated schools and nonessential businesses to close. Approximately 79% of the qualified participants from the original study agreed to participate in the daily-diary study. The final sample included 444 adolescents aged 13–18 from 38 states (Mage = 15.0; 40% male; 44% Black/African American, 39% White/Europen American, 9% Latinx, 6% Asian American, 2% Native American; 62% with incomes below 130% of the poverty level). This subsample differed by sociodemographic characteristics from the original sample in only one way: It had more participants from the Northeast and South regions (vs. West and Midwest) as compared to the original study sample (see Table 1 ). The higher number of participants from the Northeast and South regions was attributed to the fact that more states in these regions implemented stay-at-home orders during the study.
Table 1.
Adolescent participants’ demographic characteristics (N = 444).
| Characteristics | % |
|---|---|
| Age/Grade | |
| Age 13-14 | 37.8 |
| Age 15-16 | 36.3 |
| Age 17-18 | 25.9 |
| Sex | |
| Female | 60.0 |
| Male | 40.0 |
| Race | |
| Black or African American | 44.4 |
| White or European American | 39.2 |
| Latinx | 08.6 |
| Asian American | 06.3 |
| Native American | 01.5 |
| Parent's highest education | |
| High school/GED or less | 24.8 |
| Some college or more | 75.2 |
| Parent lost job due to COVID-19 | 14.0 |
| Household income below 130 percent of the national poverty level | 62.2 |
| U.S. Region | |
| Northeast | 55.1 |
| Midwest | 07.7 |
| South | 20.3 |
| West | 16.9 |
3.2. Procedures
At the time of data collection, all schools and nonessential businesses within the participants’ home states were closed to facilitate social distancing. All consented adolescents and their parents first completed baseline measures and provided demographic information. All adolescents then completed daily-diary assessments between 5:00 pm and 12:00 am using their cellphones, tablets, or computers across 14 consecutive days from April 8 to April 21, 2021. Participants received two to four reminders to complete the daily diary via email or text message each day. Parents received $20 for completing the baseline survey, and adolescents received $40 for completing the baseline survey and daily-diary entries. All materials and procedures were approved by the authors’ university institutional review board.
4. Measures
4.1. Daily affect
Adolescents’ positive and negative affect were measured daily using the Positive and Negative Affect Scale for Children (PANAS-C), a well-validated psychological scale (Laurent et al., 1999). We assessed positive affect with four items (e.g., grateful, energetic, happy, hopeful) and negative affect with six items (e.g., sad, anxious, depressed). Adolescents reported their mood during the past 24 h on a 5-point scale from 1 (not at all) to 5 (extremely). Items were averaged together to form daily composite scores of positive affect (RC = .82) and negative affect (RC = .87).
4.2. Daily stress
We assessed daily stress using a modified version of the Multicultural Events Schedule for Adolescents (Gonzales et al., 2001). Adolescents were asked how stressful they found these occurring events and rated the stressfulness of health and financial stressors over the past 24 h on a 4-point scale ranging from 1 (not at all) to 4 (a lot). Items regarding health stressors (six items; e.g., being infected by coronavirus disease; your family members being infected by coronavirus disease) and financial stressors (three items; e.g., not having enough food to eat; not having money to buy basic necessities) were averaged together to form daily composite scores (health stress: RC = .91; financial stress: RC = .76).
4.3. Daily coping
We measured adolescents’ daily coping using an abbreviated version of the Response to Stress Questionnaire (Connor-Smith et al., 2000). Adolescents were asked whether they did these things (i.e., different strategies) to make themselves feel good or help themselves to deal with some concern or worries. Engagement coping was assessed by 10 items measuring primary (e.g., “I tried some possible ways to solve the problem/concern”) and secondary (e.g., “I looked at the bright side of the problem”; “I keep my mind off the problem by exercising, listening to music, etc.”) control coping responses. Disengagement coping was measured by three items (e.g., “I avoided thinking about the problem/concern”). Adolescents rated each item on a 4-point scale ranging from 1 (not at all) to 4 (a lot). Due to the skewed nature of daily coping, the items were recoded into binary indicators (0 = no, 1 = yes) and summed together to form daily composite scores of primary control coping (RC = .87), secondary control coping (RC = .77), and disengagement coping (RC = .68). Confirmatory factor analyses were conducted to verify that these three coping constructs were related but distinct constructs.
4.4. Daily parental support
We measured the extent to which adolescents positively interacted with parents and received social support from them each day with items from the Network of Relationship Inventory (e.g., “I felt socially supported by my parent”; “I did something fun or relaxing with my parent”; Furman and Buhrmester, 2009). The items had a 5-point response scale ranging from 1 (not at all) to 5 (a lot; RC = .79).
4.5. Covariates
Due to their associations with adolescents’ stress, coping, and affect, we accounted for several sociodemographic and pandemic-specific covariates. We included the numerical day of reporting (1–14) and weekend (0 = weekday, 1 = weekend) as time-level covariates. Six child-level covariates were collected from child reports or parent reports: (a) adolescents’ age, (b) sex, (c) race, (d) federal poverty level as a proxy of socioeconomic status (e.g., household incomes below 130 percent of the poverty level), (e) adolescents’ emotion regulation, and (f) whether parents experienced job loss during the COVID-19 pandemic.
As our participants lived across the United States, we included pandemic-related covariates regarding the type of community (i.e., urban, suburban, and rural) and localized severity of COVID-19 (i.e., publicly available infection cases for each participant's specific county) to contextualize our results within COVID-19. Finally, we included adolescents’ average levels of positive and negative affect in early March of 2020 (i.e., before the pandemic). The inclusion of pre-pandemic affective outcomes allowed us to capture the change in adolescents’ affect possibly due to the pandemic.
4.6. Analytic plan
This study examined how adolescents’ stress, coping, and parental support predicted their affect using longitudinal multilevel modeling in Mplus with daily observations (Level 1) nested within participants (Level 2). The outcomes of interest were same- and next-day affect at Level 1. Level 1 key predictors included stress, coping, and parental support. At Level 2, we explained the variation in adolescents’ average level of affect over time by including child-level covariates. All Level 1 predictors were group mean centered at the individual level. The main effects of stress, coping, and parental support on affect were tested first, and interactions between stress-coping and stress-parental support were tested sequentially. The intraclass correlation (days within person) indicated that approximately 70% of the outcome variance was at the person level (positive affect: 66%; negative affect: 69%), whereas ~30% was at the daily level (positive affect: 34%; negative affect: 31%), thus justifying the use of a multilevel modeling approach.
4.7. Missing data
The amount of missing data at both the daily and person levels was low. Of the possible 6,216 daily assessments (14 days, 444 adolescents), there were only 7.4% missing data at the daily level (n = 462 missing daily assessments) due to missing or partially completed daily diaries. There were also varying levels of missing data at the child level: 100% of adolescents and parents completed the baseline and demographic surveys; 66% of adolescents did not miss any daily-diary entries; 22% missed 1 or 2 daily entries; and 6% missed 3,4 daily entries. On average, adolescents completed 13 out of 14 daily-diary entries. Little's missing completely at random test suggested that the data were missing completely at random, χ 2 (14) = 9.51, p = ns. An examination of missing data patterns indicated that adolescents with complete data did not differ from those with missing data on key constructs or demographic characteristics. To retain all adolescents in the analyses, we accounted for missing data through full-information maximum likelihood estimation.
5. Results
5.1. Descriptive statistics
Over the 14 days of daily data collection, 423 adolescents (95.3% of the participants) reported health stress on more than one day, and 3876 days (62% of the total days) included adolescent reports of health stress. In addition, 377 adolescents (85% of the participants) reported financial stress on more than one day, and 3,098 days (50% of the total days) included reports of financial stress. Table 2 presents means, standard deviations, and correlations among all study constructs.
Table 2.
Descriptive statistics (means, standard deviations, and zero-order bivariate correlations) for all study constructs.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Mean (S.D.) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Within-Person Variables | ||||||||||||
| 1 | Negative affect | 1 | 1.60 (0.78) | |||||||||
| 2 | Positive affect | -.20 | 1 | 3.18 (1.10) | ||||||||
| 3 | Health stress | .36 | .14 | 1 | 1.68 (0.79) | |||||||
| 4 | Financial stress | .33 | .07 | .54 | 1 | 1.56 (0.74) | ||||||
| 5 | Primary control coping | .15 | .22 | .28 | .23 | 1 | 1.50 (1.63) | |||||
| 6 | Secondary control coping | .07 | .29 | .26 | .19 | .53 | 1 | 2.04 (1.52) | ||||
| 7 | Disengagement coping | .16 | .13 | .27 | .19 | .41 | .44 | 1 | 0.91 (0.87) | |||
| 8 | Parental support | -.19 | .59 | .17 | .11 | .21 | .24 | .08 | 1 | 3.65 (1.31) | ||
| 9 | Day | -.04 | -.02 | -.08 | -.07 | -.05 | -.09 | -.07 | -.03 | 1 | 6.50 (4.03) | |
| 10 | Weekend | -.04 | .05 | -.02 | -.02 | -.02 | -.03 | -.02 | .01 | .03 | 1 | 0.28 (0.45) |
| Between-Person Variables | ||||||||||||
| 1 | White vs. Black | 1 | 0.33 (0.47) | |||||||||
| 2 | Other race vs. Black | -.38 | 1 | 0.23 (0.42) | ||||||||
| 3 | Girls vs. Boys | .04 | -.05 | 1 | 0.60 (0.49) | |||||||
| 4 | Age | .21 | -.05 | .15 | 1 | 9.04 (1.55) | ||||||
| 5 | SES (middle-high income vs low-income) | .34 | .05 | .02 | .20 | 1 | 0.38 (0.49) | |||||
| 6 | Emotion regulation | .06 | -.01 | .02 | .07 | .17 | 1 | 2.26 (0.76) | ||||
| 7 | Lost job due to COVID-19 | -.09 | -.05 | -.11 | -.09 | -.14 | -.04 | 1 | 0.14 (0.35) | |||
| 8 | Suburban vs. urban residents | .14 | -.01 | -.05 | .18 | .35 | .01 | .05 | 1 | 0.29 (0.45) | ||
| 9 | Rural vs. urban residents | -.16 | -.06 | -.04 | -.23 | -.11 | .05 | -.04 | -.23 | 1 | 0.11 (0.32) | |
| 10 | COVID infection cases | .33 | -.07 | .05 | .28 | .12 | -.06 | -.08 | -.02 | .50 | 1 | 32688.65 (29475.39) |
Note: Bolded values indicate p-values less than .05; non-bolded values indicate p-values .05 and greater.
5.2. Stress, coping, parental support, and adolescent affect
5.2.1. Same-Day Effect on Negative Affect
Health and financial stress were related to more same-day negative affect (health stress: B = .17, SE = .03, p < .001, 95% CI [.11, .23], effect size (ES) = .16; financial stress: B = .12, SE = .04, p < .001, 95% CI [.05, .19], ES = .11), while parental support was related to less same-day negative affect (B = -.09, SE = .02, p < .001, 95% CI [-.12, -.07], ES = -.17; Model 2, Table 3 ).
Table 3.
Multilevel model predicting adolescents’ same-day and next-day negative affect over a 14-day period.
| Same-Day Negative Affect | Next-Day Negative Affect | |||||
|---|---|---|---|---|---|---|
| Within-Person Effects | Baseline | Main Effect | Moderators | Baseline | Main Effect | Moderators |
| Day | -.01 (.00)** | .00 (.01) | .00 (.01) | -.01 (.00)** | .00 (.00) | .00 (.00) |
| Weekend | -.06 (.01)*** | -.05 (.01)*** | -.05 (.01)*** | -.08 (.02)*** | -.06 (.01)*** | -.06 (.01)*** |
| Health stress | .18 (.03)*** | .17 (.03)*** | .06 (.03)* | .06 (.02)* | ||
| Financial stress | .13 (.04)** | .12 (.04)** | .08 (.03)** | .08 (.03)** | ||
| Primary control coping | .01 (.01) | .01 (.01) | .00 (.01) | .00 (.01) | ||
| Secondary control coping | -.01 (.01) | -.01 (.01) | -.01 (.01) | -.01 (.01) | ||
| Disengagement coping | .02 (.02) | .01 (.01) | -.03 (.02) | -.03 (.02) | ||
| Parent support | -.09 (.02)*** | -.09 (.02)*** | -.01 (.01) | -.01 (.01) | ||
| Health stress × Secondary control | .05 (.02)* | .03 (.01)* | ||||
| Financial stress × Parent support | .06 (.03)* | .01 (.04) | ||||
| Between-Person Effects | ||||||
| White vs. Black | -.04 (.06) | -.04 (.06) | -.04 (.06) | -.01 (.08) | -.02 (.08) | -.02 (.08) |
| Other vs. Black | .05 (.06) | .05 (.06) | .05 (.06) | .04 (.08) | .03 (.08) | .03 (.08) |
| Girls vs. Boys | -.07 (.05) | -.07 (.06) | -.07 (.06) | -.10 (.06) | -.09 (.06) | -.09 (.06) |
| Age | .04 (.02)* | .04 (.02)* | .04 (.02)* | .04 (.03)+ | .05 (.02)* | .05 (.02)* |
| Socioeconomic status | .02 (.06) | .02 (.06) | .02 (.06) | .01 (.08) | .01 (.08) | .01 (.08) |
| Adolescent emotion regulation | -.15 (.03)*** | -.15 (.03)*** | -.15 (.03)*** | -.16 (.04)*** | -.16 (.04)*** | -.16 (.04)*** |
| Parent lost job vs. not | -.08 (.06) | -.08 (.06) | -.07 (.06) | -.08 (.08) | -.09 (.08) | -.09 (.08) |
| Pre-COVID-19 negative affect | .60 (.05)*** | .60 (.05)*** | .60 (.05)*** | .71 (.08)*** | .71 (.07)*** | .71 (.07)*** |
| Suburban vs. urban residents | -.12 (.06)* | -.12 (.06)* | -.12 (.06)* | -.19 (.07)** | -.20 (.07)** | -.20 (.07)** |
| Rural/town vs. urban residents | -.18 (.07)* | -.18 (.07)* | -.18 (.07)* | -.18 (.10) | -.16 (.10) | -.17 (.10) |
| COVID-19 infection cases | .03 (.06) | .03 (.06) | .03 (.06) | .06 (.08) | .08 (.08) | .08 (.08) |
| Fit indices | ||||||
| LL | -15621.96 | -15347.95 | -15336.09 | -12283.02 | -11754.15 | -11747.31 |
| AIC | 31616.82 | 31200.46 | 31187.32 | 24894.45 | 23857.61 | 23856.68 |
| BIC | 32042.95 | 31666.28 | 31666.46 | 25241.49 | 24241.28 | 24253.14 |
Note: * p < .05, ** p < .01, *** p < .001.
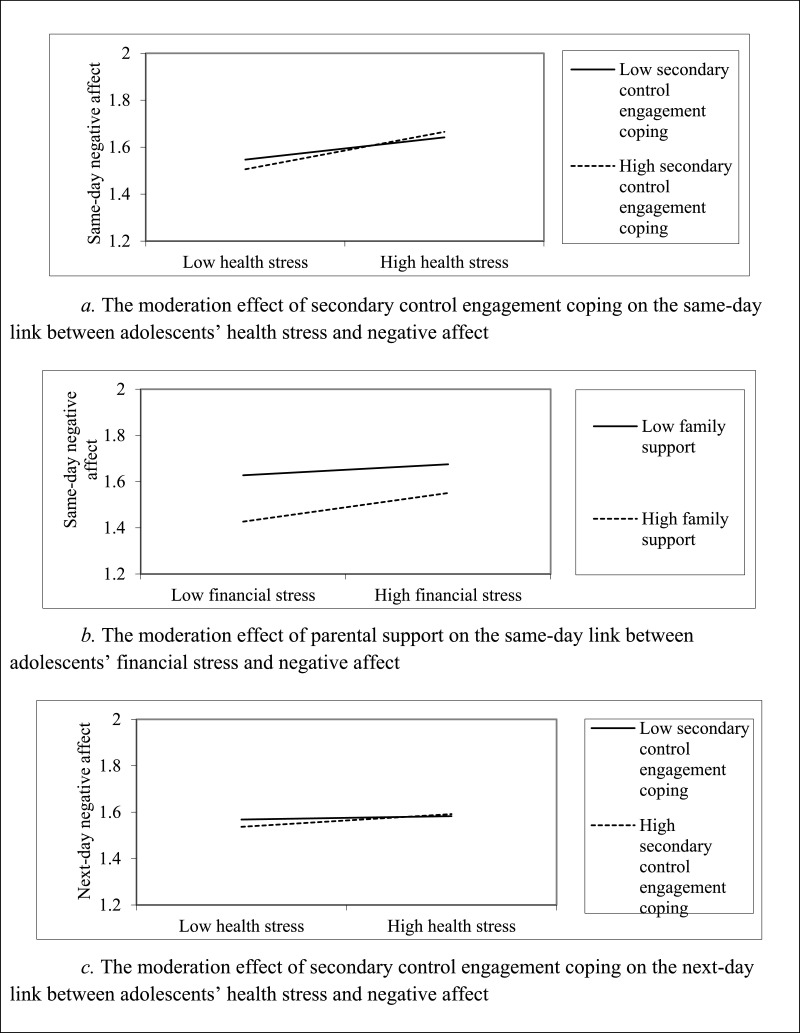
As shown in Model 3, Table 3, two significant interaction effects emerged for same-day negative affect: The association between stress and negative affect varied based on secondary control engagement coping (B = .05, SE = .02, p < .05, 95% CI [.01, .10], ES = .05) and parental support (B = .06, SE = .03, p < .05, 95% CI [.01, .12], ES = .05). We plotted the interaction at high (Mean + 1 SD) and low (Mean - 1 SD) levels of each variable. Secondary control engagement coping moderated the link between health stress and negative affect (see Fig. 1 a): On days when health stress was low and secondary control engagement coping was high, adolescents experienced less negative affect (B = .13, t = .28). In contrast, adolescents experienced higher negative affect (B = .22, t = .42) when they had high health stress and high secondary control engagement coping. Moreover, parental support buffered against the effect of financial stress on negative affect, regardless of adolescents’ stress level (see Fig. 1b; low parental support: B = .18, t = .29; high parental support: B = .07, t = .45).
Fig. 1.
Moderation effects (a). The moderation effect of secondary control engagement coping on the same-day link between adolescents’ health stress and negative affect (b). The moderation effect of parental support on the same-day link between adolescents’ financial stress and negative affect (c). The moderation effect of secondary control engagement coping on the next-day link between adolescents’ health stress and negative affect.
5.2.2. Next-day effect on negative affect
In Table 3, health and financial stress predicted more next-day negative affect (health stress: B = .06, SE = .02, p < .05, 95% CI [.01, .08], ES = .05; economic stress: B = .08, SE = .03, p < .01, 95% CI [.02, .12], ES = .08). Further, one significant interaction effect emerged for next-day negative affect (B = .03, SE = .01, p < .05, 95% CI [.01, .05], ES = .04). In Fig. 1c, secondary control engagement coping moderated the positive link between health stress and negative affect. On days when health stress was low and secondary control engagement coping was high, adolescents experienced less negative affect the following day (B = .02, t = .03). Adolescents with high health stress and high secondary control engagement coping experienced more negative affect the following day (B = .07, t = .10).
5.2.3. Same-day effect on positive affect
As shown in Table 4 , health and financial stress were not related to same-day positive affect (health stress: B = .02, SE = .04, p = ns, 95% CI [-.05, .09]; financial stress: B = -.02, SE = .03, p = ns, 95% CI [-.09, .05]) while secondary control engagement coping and parental support were related to heightened same-day positive affect (secondary control engagement coping: B = .07, SE = .02, p < .001, 95% CI [.04, .10], ES = .10; parental support: B = .23, SE = .02, p < .001, 95% CI [.20, .27], ES = .26). No significant interaction effect emerged for same-day positive affect (B = -.02, SE = .03, p = ns, 95% CI [-.08, .04]; B = .01, SE = .04, p = ns, 95% CI [-.07, .10]).
Table 4.
Multilevel model predicting adolescents’ same-day and next-day positive affect over a 14-day period.
| Same-Day Positive Affect | Next-Day Positive Affect | |||||
|---|---|---|---|---|---|---|
| Within-Person Effects | Baseline | Main Effect | Moderators | Baseline | Main Effect | Moderators |
| Day | -.01 (.00)* | .00 (.00) | .00 (.00) | -.01 (.00)* | -.01 (.00)* | -.01 (.00)* |
| Weekend | .12 (.02)*** | .12 (.02)*** | .12 (.02)*** | .12 (.02)*** | .12 (.02)*** | .12 (.02)*** |
| Health stress | .02 (.04) | -.02 (.04) | -.01 (.03) | -.01 (.03) | ||
| Financial stress | -.02 (.04) | -.02 (.04) | .00 (.03) | .00 (.03) | ||
| Primary control coping | -.01 (.01) | -.01 (.01) | -.01 (.01) | -.01 (.01) | ||
| Secondary control coping | .07 (.02)*** | .07 (.02)*** | .03 (.01)* | .03 (.01)* | ||
| Disengagement coping | -.03 (.02)+ | -.03 (.02)+ | .00 (.00) | .00 (.00) | ||
| Parent support | .23 (.02)*** | .23 (.02)*** | .04 (.01)** | .04 (.01)** | ||
| Health stress × Secondary control | -.02 (.03) | -.01 (.02) | ||||
| Financial stress × Parent support | .01 (.04) | .01 (.03) | ||||
| Between-Person Effects | ||||||
| White vs. Black | -.10 (.10) | -.10 (.10) | -.10 (.10) | -.11 (.10) | -.11 (.10) | -.10 (.10) |
| Other vs. Black | -.24 (.11)* | -.23 (.11)* | -.23 (.11)* | -.24 (.11)* | -.24 (.11)* | -.24 (.11)* |
| Girls vs. Boys | -.06 (.08) | -.06 (.08) | -.06 (.08) | -.06 (.08) | -.06 (.08) | -.06 (.08) |
| Age | -.03 (.03) | -.03 (.03) | -.03 (.03) | -.03 (.03) | -.03 (.03) | -.03 (.03) |
| Socioeconomic status | .02 (.09) | .02 (.09) | .02 (.09) | .03 (.08) | .02 (.08) | .02 (.08) |
| Adolescent emotion regulation | .09 (.05) | .09 (.05) | .09 (.05) | .09 (.05) | .09 (.05) | .09 (.05) |
| Parent lost job vs. not | .02 (.11) | .02 (.11) | .02 (.11) | .01 (.10) | .01 (.10) | .01 (.10) |
| Pre-COVID-19 positive affect | .80 (.05)*** | .80 (.05)*** | .80 (.05)*** | .80 (.05)*** | .81 (.05)*** | .81 (.05)*** |
| Suburban vs. urban residents | .04 (.08) | .04 (.08) | .04 (.08) | .04 (.08) | .05 (.08) | .05 (.08) |
| Rural/town vs. urban residents | .16 (.15) | .16 (.15) | .16 (.15) | .16 (.15) | .15 (.15) | .15 (.15) |
| COVID-19 infection cases | -.27 (.11)* | -.27 (.11)* | -.27 (.11)* | -.27 (.10)** | -.28 (.11)** | -.28 (.11)** |
| Fit indices | ||||||
| LL | -7066.60 | -6822.75 | -6822.35 | -7829.11 | -7565.01 | -7564.90 |
| AIC | 14377.15 | 13901.49 | 13904.70 | 15976.87 | 15457.18 | 15976.88 |
| BIC | 14716.73 | 14280.81 | 14297.32 | 16363.06 | 15874.57 | 16363.06 |
Note: * p < .05, ** p < .01, *** p < .001.
5.2.4. Next-day effect on positive affect
Next-day positive affect was positively predicted by secondary control engagement coping and parental support (secondary control engagement coping: B = .03, SE = .01, p < .05, 95% CI [.01, .05], ES = .04; parental support: B = .04, SE = .01, p < .01, 95% CI [.02, .07], ES = .06), but it was not significantly predicted by health or financial stress (see Table 4; health stress: B = .00, SE = .03, p = ns, 95% CI [-.03, .04]; financial stress: B = -.01, SE = .03, p = ns, 95% CI [-.07, .04]). No significant interaction effect emerged for next-day positive affect (B = .00, SE = .03, p = ns, 95% CI [-.06, .06]).
6. Discussion
Amidst COVID-19's stay-at-home orders and mandated school closures, American adolescents were thrust into developmentally challenging circumstances (Wang et al., in press). In this study, we identified how pandemic-related stressors, potential coping mechanisms, and parental support link to adolescents’ daily positive and negative affect. Using a daily-diary approach with a nationwide American sample, we found that adolescents’ health and financial stress predicted same- and next-day increases in negative affect. Furthermore, adolescents’ secondary control engagement coping not only predicted same- and next-day increases in positive affect, but it also moderated the link between health stress and negative affect. Parental support predicted increases in adolescents’ same- and next-day positive affect and decreases in same-day negative affect. Parental support also moderated the link between financial stress and negative affect.
6.1. Pandemic-related stress and adolescent affect
Pervasive health and financial stress were linked to same- and next-day increases in adolescents’ negative affect. These results were unsurprising, as the presence of both health-related and financial stressors creates a context of unavoidable and unpredictable pandemic-related stress. With the United States leading the world in COVID-19 infection and death rates, adolescents were faced with the very real possibility of losing a loved one, an occurrence that has been linked to significant mental health deficits (Stikkelbroek et al., 2016). Moreover, the contagion of pandemics often requires public health measures that necessarily impact the national economy. Indeed, millions of Americans lost their jobs during the COVID-19 pandemic (Lambert, 2020). Hence, the health and financial stressors associated with the pandemic are inextricably intertwined, salient risk factors that threaten adolescents’ daily affect.
6.2. Coping and adolescent affect
In alignment with literature supporting the benefits of engagement coping on adolescent functioning (Compas et al., 2017), secondary control engagement coping—such as positive thinking, cognitive restructuring, acceptance, and distraction—was linked to same- and next-day increases in positive affect, indicating both immediate and sustained benefits. In addition, neither primary control engagement coping strategies (e.g., problem solving, emotional expression and regulation) nor disengagement coping strategies (e.g., denial, avoidance, and wishful thinking) predicted adolescents’ positive or negative affect in this study.
Why, then, were secondary control engagement coping strategies effective while other coping strategies were not? Primary control engagement coping strategies depend on an individual's ability to control certain aspects of or responses to a given stressor, whereas disengagement responses assume that the stressor and its associated stress are avoidable (Compas et al., 2017; Connor-Smith et al., 2000). However, in the context of a pandemic, health and financial stressors are, in large part, out of adolescents’ control and unavoidable. Thus, coping mechanisms reliant on primary control or disengagement may be less likely to evoke positive affect than those that emphasize adaptation and accommodation. Indeed, perceived controllability over stressors has been found to positively influence adolescents’ likelihood of using adaptive coping strategies (Zimmer-Gembeck et al., 2016). In light of this information, parents and practitioners who work with adolescents contending with pandemic-related stress may encourage the use of secondary control engagement coping strategies—such as distraction (e.g., exercising, reading, helping others) and optimistic thinking—so as to promote positive affect among adolescents.
Furthermore, the buffering role of secondary control engagement coping in pandemic-related health stress was stronger when that stress was low; yet, as health stress increased, this buffering effect diminished. There may be differences in short- and long-term coping regarding both type and efficacy (Jensen et al., 2013; Sheppes and Gross, 2011). For example, secondary control engagement coping has been found to not only be the preferred (Jensen et al., 2013) but also the most efficacious coping mechanisms for handling short-term periods of intense stress (Sheppes and Gross, 2011). It follows, then, that as stress levels fluctuate throughout the course of the pandemic, certain coping skills may become more or less effective.
In alignment with an underlying assumption of the Responses to Stress Model, effective coping occurs when the positive impact of coping or protective factors outweighs the negative impact of the stressor, thereby illustrating that responses to stress and the efficacy of coping necessarily oscillate based on context. Although secondary control engagement coping strategies were effective for adolescents managing low levels of COVID-19-related health stress, it may be the case that solely using secondary control engagement coping strategies is no longer sufficient to counter the negative effects of elevated stress on well-being. Moreover, exogenous contextual variables and temporal shifts in health-related stressors may have affected the efficacy of secondary control engagement coping (Sandler, 2001). As COVID-19 continues to affect American families, it will be important to monitor the types and intensity of stressors, adolescents’ use of coping mechanisms, and the efficacy of those coping mechanisms in promoting positive developmental outcomes.
6.3. Parental support and adolescent psychological well-being
Parental support predicted adolescents’ increased positive affect within and across days and was related to lower same-day negative affect. Parental support has contributed to adolescents’ resilience, especially when that support comes during traumatic or developmentally challenging times (Bradley, 2007; Kolak et al., 2018). Consistent with the documented literature on poverty and psychological well-being (Santiago et al., 2017; Schneider et al., 2015; Wadsworth, 2015), we also found that parental support buffered against the same-day effect of financial stress on adolescents’ negative affect, and this buffering effect existed regardless of adolescents’ level of stress. The efficacy of parental support is highly dependent on context (Jensen et al., 2013; Wadsworth, 2015). As a result, the degree to which adolescents have perceived control over a given stressor may be an important determinate of efficacy (Zacher and Rudolph, 2020; Zimmer-Gembeck et al., 2016): Although adolescents can engage in direct and preventative measures to protect their own health during a pandemic (e.g., social distancing), they may have little, if any, control over the financial circumstances of their family. Ergo, when a family experiences financial stress, adolescents may need their parents’ assistance to navigate it.
6.4. Limitations and future directions
Although our daily-diary assessment provides a longitudinal perspective on adolescents’ daily experiences, the 14-day assessment period was limited to the immediate onset of the pandemic. Future work should examine the extent to which these patterns hold throughout and after the pandemic, especially considering that disaster-related psychosocial impairments may lead to long-term negative developmental cascades (Masten, 2021). Researchers should also consider using within-day experience sampling so as to better understand the daily dynamics among stress, coping, and adjustment. In doing so, we can provide further credence to the causal relations suggested, but not proven, by our results. In addition, future studies should investigate adolescents’ coping strategies and parental support as mediators in addition to moderators. For instance, some adolescents may be more likely to adopt disengagement coping strategies when confronted with stress, which in turn may lead to more negative affect. Finally, though racially and socioeconomically diverse, our nationwide sample had more adolescent participants from certain regions than others (e.g., the Midwest). This study should be replicated with geographically different samples to enhance the generalizability of the key findings.
6.5. Implications and conclusion
At the onset of COVID-19, adolescents faced a host of novel or amplified stressors that impacted their psychological well-being. While our findings showed strong connections between daily stressors and negative affect, we were also able to determine several factors—namely, secondary control engagement coping and parental social support—that helped youth mitigate the impact of health and financial stress on negative affect while also supporting youth's positive emotional experience in the midst of a global crisis. Practitioners working to support youth during times of heightened health or financial stress may want to encourage the use of secondary control engagement coping strategies among youth (e.g., distraction, cognitive restructuring) and remind parents of how important it is for youth to feel their social and emotional support during times of adversity. Moreover, researchers should continue to pursue lines of inquiry that allow for a better understanding of how adolescents’ stressors, coping responses, and affective states may have shifted throughout the course of the pandemic. In particular, future studies should pursue questions pertaining to post-COVID psychological well-being and adjustment of adolescents to determine which individual, family, or school factors may mitigate the long-term psychosocial effects related to a multi-systemic disaster.
Americans have not encountered a health crisis this pervasive or economically devastating since the Spanish flu pandemic of 1918, and COVID-19 placed adolescents into unprecedented developmentally challenging circumstances. Our study's micro-longitudinal design and critically timed data collection periods allowed us to show that American adolescents’ pandemic-related health and financial stress were closely tied to their daily affect, even in the nascent stages of the pandemic. Although much is left to learn about coping and support as the pandemic continues, our study provides the first steps toward understanding how we may mitigate the impact of COVID-19-related health and economic stressors on adolescents’ psychological well-being. Considering the prolonged, pervasive, and contentious nature of the COVID-19 crisis in the United States, it is critical to monitor the psychosocial impact of the pandemic on adolescents while continuing to identify personal and environmental protective factors for maximizing resilience.
CRediT authorship contribution statement
Ming-Te Wang: Conceptualization, Writing – original draft, Writing – review & editing. Juan Del Toro: Formal analysis, Data curation, Writing – review & editing. Christina L. Scanlon: Resources, Writing – original draft. Jacqueline D. Schall: Data curation, Resources, Writing – review & editing. Angela L. Zhang: Data curation, Resources, Writing – review & editing. Allison M. Belmont: Data curation, Resources, Writing – review & editing. Sarah E. Voltin: Data curation, Writing – review & editing. Keri A. Plevniak: Data curation, Writing – review & editing.
Declaration of Competing Interest
All other authors declare that they have no conflicts of interest.
Acknowledgments
Acknowledgments
None.
Role of Funding
None.
References
- Arbel R., Perrone L., Margolin G. Adolescents’ daily worries and risky behaviors: The buffering role of support seeking. J. Clin. Child Adolesc. Psychol. 2018;47(6):900–911. doi: 10.1080/15374416.2016.1169536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger N., Davis A., Rafaeli E. Diary methods: capturing life as it is lived. Annu. Rev. Psychol. 2003;54(1):579–616. doi: 10.1146/annurev.psych.54.101601.145030. [DOI] [PubMed] [Google Scholar]
- Bradley R.A. Parenting in the breach: how parents help children cope with developmentally challenging circumstances. Parenting. 2007;7(2):99–148. doi: 10.1080/15295190701306896. [DOI] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet N. Am. Ed. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D., Rogosch F.A. A developmental psychopathology perspective on adolescence. J. Consult. Clin. Psychol. 2002;70(1):6–20. doi: 10.1037/0022-006X.70.1.6. [DOI] [PubMed] [Google Scholar]
- Compas B.E., Jaser S.S., Bettis A.H., Watson K.H., Gruhn M.A., Dunbar J.P., Williams E., Thigpen J.C. Coping, emotion regulation, and psychopathology in childhood and adolescence: a meta-analysis and narrative review. Psychol. Bull. 2017;143(9):939–991. doi: 10.1037/bul0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor-Smith J.K., Compas B.E., Wadsworth M.E., Thomsen A.H., Saltzman H. Responses to stress in adolescence: measurement of coping and involuntary stress responses. J. Consult. Clin. Psychol. 2000;68(6):976–992. doi: 10.1037/0022-006X.68.6.976. [DOI] [PubMed] [Google Scholar]
- Cook S.H., Heinze J.E., Miller A.L., Zimmerman M.A. Transitions in friendship attachment during adolescence are associated with developmental trajectories of depression through adulthood. J. Adolesc. Health. 2016;58(3):260–266. doi: 10.1016/j.jadohealth.2015.10.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran J., Nichols-Casebolt A. Risk and resilience ecological framework for assessment and goal formulation. Child Adolesc. Soc. Work J. 2004;21(3):211–235. doi: 10.1023/B:CASW.0000028453.79719.65. [DOI] [Google Scholar]
- Cowen E.L. The enhancement of psychological wellness: Challenges and opportunities. Am. J. Community Psychol. 1994;22(2):149–179. doi: 10.1007/BF02506861. [DOI] [PubMed] [Google Scholar]
- Dimitry L. A systematic review on the mental health of children and adolescents in areas of armed conflict in the Middle East. Child Care Health Dev. 2012;38(2):153–161. doi: 10.1111/j.1365-2214.2011.01246.x. [DOI] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14(1):20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furman W., Buhrmester D. Methods and measures: the network of relationships inventory: behavioral systems version. Int. J.Behav. Dev. 2009;33(5):470–478. doi: 10.1177/0165025409342634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales N.A., Tein J.Y., Sandler I.N., Friedman R.J. On the limits of coping: interaction between stress and coping for inner-city adolescents a test of the stress-buffering effects of coping in a multiethnic sample of urban adolescents. J. Adolesc. Res. 2001;16:372–395. In LIMITS OF COPING. Issue 4. [Google Scholar]; doi:10.1177/0743558401164005.
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D.S.C., Du B., Li L., Zen G., Yuen K.-Y., Chen R., Tang C., Wang T., Chen P., Xiang J., Zhong N. Clinical characteristics of coronavirus disease 2019 in China. J. Emerg. Med. 2020;58(4):711–712. doi: 10.1016/j.jemermed.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen T.K., Ellestad A., Dyb G. Children and adolescents’ self-reported coping strategies during the Southeast Asian Tsunami. Br. J. Clin. Psychol. 2013;52(1):92–106. doi: 10.1111/bjc.12003. [DOI] [PubMed] [Google Scholar]
- Kirby L., Fraser M., Fraser M. Risk and Resilience in Childhood: an Ecological Perspective. NASW; 1997. Risk and resilience in childhood; pp. 10–33. [DOI] [Google Scholar]
- Kolak A.M., Van Wade C.L., Ross L.T. Family unpredictability and psychological distress in early adulthood: the role of family closeness and coping mechanisms. J. Child Fam. Stud. 2018;27(12):3842–3852. doi: 10.1007/s10826-018-1211-4. [DOI] [Google Scholar]
- Kronenberg M.E., Hansel T.C., Brennan A.M., Osofsky H.J., Osofsky J.D., Lawrason B. Children of Katrina: lessons learned about postdisaster symptoms and recovery patterns. Child Dev. 2010;81(4):1241–1259. doi: 10.1111/j.1467-8624.2010.01465.x. [DOI] [PubMed] [Google Scholar]
- Lambert L. Fortune; 2020. 45.7 Million Have Filed for Unemployment During the Pandemic — Greater Than the Combined Population of 23 States. June. [Google Scholar]
- Laurent J., Catanzaro S.J., Rudolph K.D., Joiner T.E., Potter K.I., Lambert S., Osborne L., Gathright T. A measure of positive and negative affect for children: scale development and preliminary validation. Psychol. Assess. 1999;11(3) doi: 10.1037/1040-3590.11.3.326. [DOI] [Google Scholar]
- Lin C.Y. Social health and behavior. Soc. Health Behav. 2020;3(1):1–2. doi: 10.4103/SHB.SHB. [DOI] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S.S., Cicchetti D., Cohen D.J. Vol. 3. John Wiley and Sons Ltd; 2006. Resilience in development: A synthesis of research across five decades; pp. 739–795. (Developmental Psychopathology: Risk, disorder, and Adapation). (2nd ed. [DOI] [Google Scholar]
- Luthar S.S., Brown P.J. Maximizing resilience through diverse levels of inquiry: Prevailing paradigms, possibilities, and priorities for the future. Dev. Psychopathol. 2007;19(3):931–955. doi: 10.1017/S0954579407000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten A.S. Resilience of children in disasters: a multisystem perspective. Int. J. Psychol. 2021;56(1):1–11. doi: 10.1002/ijop.12737. [DOI] [PubMed] [Google Scholar]
- McGrath M. Forbes; 2016, January. 63% of Americans Don't Have Enough Savings to Cover A $500 Emergency. https://www.forbes.com/sites/maggiemcgrath/2016/01/06/63-of-americans-dont-have-enough-savings-to-cover-a-500-emergency/#674be58b4e0d. [Google Scholar]
- McMahon G., Creaven A.M., Gallagher S. Stressful life events and adolescent well-being: the role of parent and peer relationships. Stress Health. 2020:1–12. doi: 10.1002/smi.2923. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B., Noffsinger M.A., Wind L.H., Allen J.R. Children's coping in the context of disasters and terrorism. J. Loss Trauma. 2014;19(1):78–97. doi: 10.1080/15325024.2013.791797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polizzi C., Lynn S.J., Perry A. Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clin. Neuropsychiatry. 2020;17(2):59–62. doi: 10.36131/CN20200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020 doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Llanes J.M., Vos F., Guha-Sapir D. Measuring psychological resilience to disasters: are evidence-based indicators an achievable goal? Environ, Health A Glob. Access Sci. Source. 2013;12(1):1–10. doi: 10.1186/1476-069X-12-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler I. Quality and ecology of adversity as common mechanisms of risk and resilience. Am. J. Community. Psychol. 2001;29(1):19–61. doi: 10.1023/A:1005237110505. [DOI] [PubMed] [Google Scholar]
- Santiago, C., Wadsworth, M., & Stump, J. (2011). Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effect on psychological syndromes among divers low-income families. Journal of Economic Psychology, 32(2), 218-230. doi:10.1016/j.joep.2009.10.008.
- Santiago C.D.C., Brewer S.K., Fuller A.K., Torres S.A., Papadakis J.L., Ros A.M. Stress, coping, and mood among latino adolescents: a daily diary study. J. Res. Adolesc. 2017;27(3):566–580. doi: 10.1111/jora.12294. [DOI] [PubMed] [Google Scholar]
- Schneider W., Waldfogel J., Brooks-Gunn J. The great recession and behavior problems in 9-year-old children. Dev. Psychol. 2015;51(11):1615–1629. doi: 10.1037/dev0000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar N.L., Park C.L. Effects of stress on students’ physical and mental health and academic success. Int. J. Sch. Educ. Psychol. 2016;4(1):5–9. doi: 10.1080/21683603.2016.1130532. [DOI] [Google Scholar]
- Sheppes G., Gross J.J. Is Timing everything? Temporal considerations in emotion regulation. Pers. Soc. Psychol. Rev. 2011;15(4):319–331. doi: 10.1177/1088868310395778. [DOI] [PubMed] [Google Scholar]
- Skinner E.A., Zimmer-Gembeck M.J. The development of coping. Annu. Rev. Psychol. 2007;58:119–144. doi: 10.1146/annurev.psych.58.110405.085705. [DOI] [PubMed] [Google Scholar]
- Stikkelbroek Y., Bodden D.H.M., Reitz E., Vollebergh W.A.M., Van Baar A.L. Mental health of adolescents before and after the death of a parent or sibling. Eur. Child Adolesc. Psychiatry. 2016;25(1):49–59. doi: 10.1007/s00787-015-0695-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Lancker W., Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Health. 2020;5(5):e243–e244. doi: 10.1016/S2468-2667(20)30084-0. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth M.E. Development of maladaptive coping: a functional adaptation to chronic, uncontrollable stress. Child Dev. Perspect. 2015;9(2):96–100. doi: 10.1111/cdep.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth M.E., Raviv T., Santiago C.D., Etter E.M. Testing the adaptation to poverty-related stress model: predicting psychopathology symptoms in families facing economic hardship. J. Clin. Child Adolesc. Psychol. 2011;40(4):646–657. doi: 10.1080/15374416.2011.581622. [DOI] [PubMed] [Google Scholar]
- Wang, M.-T., Henry, D. A. Scanlon, C. L, Del Toro, J., Voltin, S. (in press). Adolescent psychosocial adjustment during COVID-19: An intensive longitudinal study. Journal of Clinical Child and Adolescent Psychology. [DOI] [PubMed]
- Wang, M.-T. & Eccles, J. S. (2012). Social support matters: Longitudinal effects of social support on three dimensions of school engagement from middle to high school. Child Development, 83, 877-895. [DOI] [PubMed]
- Wang, M.-T., Degol, J. L., & Henry, D. A. (2020). An integrative development-in-sociocultural-context model for children’s engagement in learning. American Psychologist, 74, 1086-1102. [DOI] [PubMed]
- Wang, M.-T., Scanlon, C. L., Hua, M., & Del Toro, J. (2021). Safely social: Promoting and sustaining adolescent engagement in social distancing during the COVID-19 pandemic. Journal of Adolescent Health, 68, 1059-1066. [DOI] [PubMed]
- Zacher H., Rudolph C.W. Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. Am. Psychol. 2020 doi: 10.1037/amp0000702. [DOI] [PubMed] [Google Scholar]
- Zimmer-Gembeck M.J., Van Petegem S., Skinner E.A. Emotion, controllability and orientation towards stress as correlates of children's coping with interpersonal stress. Motiv. Emot. 2016;40(1):178–191. doi: 10.1007/s11031-015-9520-z. [DOI] [Google Scholar]