Abstract
Objective
To obtain evidence-based conclusions about the effect of acupuncture on pain relief in women undergoing oocyte retrieval, the results of randomized controlled trials (RCTs) that met the criteria were assessed on the Pain Assessment Scale and pregnancy indicators.
Search Methods
References were retrieved in MEDLINE, EMBASE, CNKI database, CBM database, VIP database, and Wanfang database from inception to June 26, 2021. Unpublished ongoing trials were searched in the Clinical Trials Registries. This review included RCTs that investigated the acupuncture analgesic effects during oocyte retrieval in women undergoing in vitro fertilization.
Results
Fourteen RCTs (2503 women in total) with six types of comparisons were finally included. The quality of concluding evidence was generally low or very low. Performance bias and outcome assessment bias was the main risk of bias of the included studies. Acupuncture combined with conscious sedation and analgesia (CSA) was associated with less intraoperative (SMD=−1.03; 95% CI: −1.71 to −0.36) and postoperative (SMD = −1.11; 95% CI: −1.51 to −0.71) pain compared to receive CSA alone in oocyte retrieval. Acupuncture with non-steroidal anti-inflammatory drugs (NSAIDs) was more effective than using NSAIDs alone for postoperative analgesia (MD = −1.76; 95% CI: −2.08 to −1.44).
Conclusion
Acupuncture complex analgesic therapy is more effective than utilizing CSA or NSAIDs alone. Furthermore, there is no significant consensus on whether there is an analgesic effect of applying acupuncture alone during oocyte retrievals, which needs further research. The overall results should be interpreted with caution due to the high risk of bias/low-GRADE scores among these studies.
Protocol and Registration
PROSPERO registration number: CRD42020170095.
Keywords: acupuncture, analgesia, oocyte retrieval, meta-analysis, systematic review
Introduction
Oocytes pick-up (OPU) through the vagina under ultrasound guidance is a frequently performed outpatient procedure during assisted reproductive technology (ART). Anesthesia is still integral in this procedure which relieved repeated pain and negative emotions in women undergoing in vitro fertilization (IVF). Among the standard methods of analgesia, the need for general anesthesia (GA) declines with less-invasive oocyte retrieval techniques, and paracervical block (PCB) cannot meet a woman’s anesthesia minimum needs.1 Thus, conscious sedation and analgesia (CSA) are the most common and acceptable anesthesia methods with a high degree of satisfaction.2 These pharmacological anesthetics provide immediate analgesia and are widely used in clinical practice. However, studies have found that anesthetic drugs penetrate the follicular fluid and negatively affect oocyte fertilization and embryo growth.3–5 There are definite needs to investigate non-pharmacological analgesia to reduce side effects and adverse events undergoing IVF.
Acupuncture has been widely used during long periods for analgesia.6,7 Prolonged clinical practice proved acupuncture compound analgesia therapy in OPU has the advantages of safety, high efficiency, fast recovery, and few side effects.8,9 Although previous systematic review10 demonstrated no evidence supporting acupuncture to be more optimal for pain relief during OPU than PCA with CSA, the updated Cochrane review supported acupuncture is appropriate to adjuvant analgesia OPU process. Various analgesic combinations are the current trend in OPU and are hotspots of peer attention. Therefore, acupuncture analgesia during OPU as non-pharmacological and desirable solutions needs to be evaluated comprehensively and systematically.
This review would include randomized controlled trials (RCTs) on acupuncture for pain relief during OPU to conduct a systematic review and meta-analysis of the relevant studies. It aimed to evaluate acupuncture for pain relief during OPU in an evidence-based perspective and provided recommendations for acupuncture clinical analgesia.
Materials and Methods
The review was registered at PROSPERO. All contents and report details were strictly referred to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).11
Search Strategy
Both English and Chinese publications of six databases, including PubMed, EMBASE, Chinese National Knowledge Infrastructure (CNKI), VIP Database, Chinese Biomedical Literature (CBM) Database, and Wan-Fang Database, were searched electronically from inception to June 26, 2021. The search strategy included the medical subject headings (MeSH) terms in combination with free words. It was adjusted according to different databases. The searched MeSH terms were as follows: Fertilization in Vitro; Sperm Injections, Intracytoplasmic; Ovarian Follicle; Oocyte Donation; Oocyte Retrieval; Analgesia; Acupuncture; Acupuncture Therapy; Electroacupuncture; Moxibustion; Acupuncture Analgesia; Transcutaneous Electric Nerve Stimulation; Acupressure. The unpublished ongoing trials were searched in clinical trial registries through the World Health Organization (WHO) International Clinical Trial Registry Platform, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov, Chinese Clinical Trial Register. Besides, retrieved RCTs of published reviews were manually searched. The exact search strategies were shown in Supplementary Enclosure.
Inclusion Criteria
RCTs that evaluated the efficacy of acupuncture analgesia for women undergoing transvaginal oocyte retrieval (as part of IVF) were included in the study. In a broad sense, acupuncture therapies included auricular acupuncture, electroacupuncture, manual acupuncture, transcutaneous electrical acupoint stimulation (TEAS). There was no restriction on intervention duration for acupuncture treatment, but it should be recorded in detail. Drug analgesia (such as sedatives, non-steroidal anti-inflammatory drugs, etc), invasive sham acupuncture (such as shallow sting), non-invasive placebo acupuncture, as well as treatment in the control group were accepted. Studies with different types of acupuncture in the control group were excluded.
Primary outcome indicators were subjective pain assessment scale such as the simplified McGill pain questionnaire (SF-MPQ),12 visual analog scale (VAS),13 and WHO pain rating scale. Both the VAS and WHO pain scores are simple self-rating scales. The VAS is a scale consisting of vertically oriented 10 cm lines on paper representing pain from mild to severe (0–10 or 0–100 points). WHO pain scores were likely to be a numerical rating scale from 0 to 12, representing pain levels from mild to severe. SF-MPQ includes present pain intensity (PPI), pain rating index (PRI), and VAS. The PRI consists of 11 sensory phrases and four affective phrases to describe pain. For all phrases describing pain, “0” indicates no pain, “1” indicates mild pain, “2” indicates moderate pain, and “3” indicates severe pain. A score from 0 to 5 was used to indicate the PPI from no pain to extreme pain.
Secondary outcome indicators were pregnancy-related (such as the number of oocytes retrieved, clinical pregnancy rate, high-quality embryo rate, etc.) and surgery-related indicators (such as adverse reactions, emotion evaluation, etc.).
Study Selection
Study selections and data management were made by two reviewers (RRW and LC). We first screened the titles and abstracts. Then the entire content was downloaded, and the decision to include the study was made. Finally, the disagreement between RRW and LC regarding the selection was resolved by LYL. The retrieved literature with detailed information of the selected studies was imported into Excel.
Quality Assessment
Two reviewers (RRW and LC) used the Cochrane Handbook of Systematic Reviews14 to assess the risk of bias for each included trial. The risk of bias for the assessment category consisted of seven items. Each item was classified into three levels: low risk, unclear risk, and high risk. We used the Grading of Recommended Assessment Development and Evaluation (GRADE; Grade Pro version 3.6.1)15 to assess the quality of the evidence, which was categorized as high, moderate, low, and very low. The GRADE grading reduced the limitations of each study from high quality if any of the following limitations were present: 1) design limitations; 2) inconsistent results; 3) evidence of indirectness; 4) imprecision 5) reporting bias.
Data Synthesis
Meta-analysis was performed by the Review Manager (version 5.3). I-square (I2) statistics and Cochran Q test assessed heterogeneity.16,17 I2 < 50% statistics or the P-value>0.01 was defined as low heterogeneity. When possible, we used a random-effects model for meta-analysis. For dichotomous variables, a risk ratio (RR) with a 95% Confidence Intervals (CIs) was used. Other binary data would be converted into an RR value. Continuous variables were analyzed by the Hedges’ g method and expressed as standardized mean difference (SMD) or mean difference (MD) with 95% CIs. We combined studies that had the same form of acupuncture intervention and the same controls. Due to the small number of included studies and limitations in study quality, we did not perform subgroup analysis and sensitivity analysis. The funnel plot did not apply to this study because of the small number of included literatures.18 For RCTs with multiple treatment arms, data of comparisons that met inclusion criteria were extracted as recommended by The Cochrane Handbook for Systematic Review of Interventions.14 For studies whose outcomes could not be combined, we performed a description for individual studies.
Results
Results of Searches
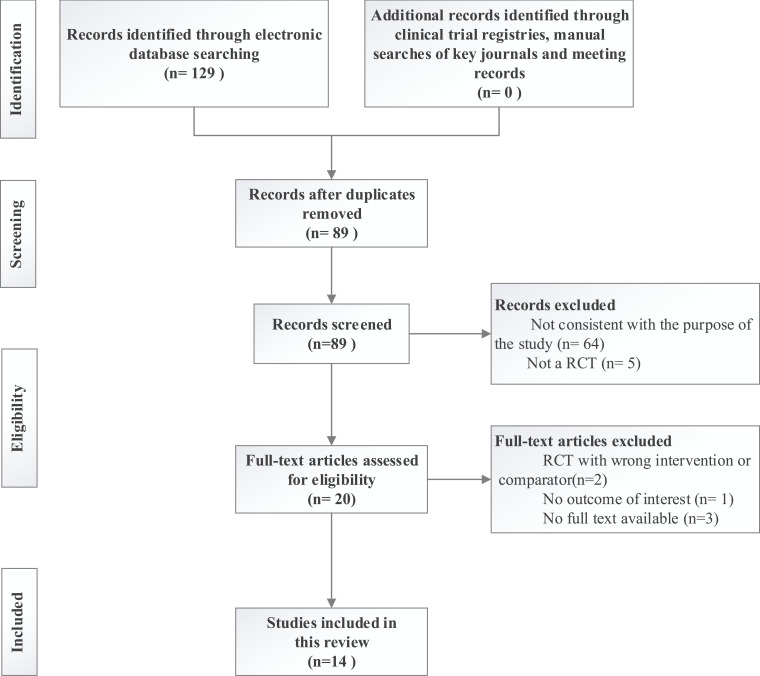
A total of 129 citations were retrieved. Forty duplicate studies were excluded. After screening titles and abstracts, a further 64 studies not consistent with the purpose and five with the wrong research type were excluded. Of the 20 identified trials, six studies did not meet the inclusion criteria (two19,20 with the wrong intervention or comparator, one21 without outcomes of interest, and three studies22–24 not available for full data) were excluded. Thus, 14 studies8,25–37 were included in the study. The PRISMA flowchart of the screening process is shown in Figure 1.
Figure 1.
Flow diagram of the screening process.
Table 1 shows the characteristic of RCTs included in the review. Overall, 2503 women were enrolled in this review, with sample sizes ranging from 60 to 409 for each study. Of the 14 included studies, 10 studies8,29–37 were conducted in mainland China. Five of the included studies29–32,35 were published master’s theses, and the remaining nine8,25–28,33,34,36,37 were journal articles. Five studies25–28,37 were published in English, and the other nine8,29–36 were published in Chinese. Five different acupuncture interventions were investigated: auricular point pressing,35 auricular electroacupuncture,28,34 electroacupuncture,8,25–27,29,31,33,36 TEAS,30,37 manual acupuncture.32
Table 1.
Characteristic of RCTs Included in the Review
| Study | Country | Multi/Single Center(s) | Sample Size, Randomized /Analyzed | Pain Measurement | Intervention/Contrrol | Time of Acupuncture Intervention |
|---|---|---|---|---|---|---|
| Stener-Victorin, et al (1999) | Sweden | Multi-center | 150/149 | VAS (0–100) | EA+PCB (lignocaine) Alfentanil+Atropine+PCB(lignocaine) |
EA: 30min before OPU till the end of the procedure |
| Humaidan, et al (2004) | Denmark | Single-center | 200/200 | VAS (0–100) | EA+PCB (lignocaine)+ Alfentanil Alfentanil+Benzodiazepine+PCB(lignocaine) |
EA: After the injection of propofol till the end of the procedure |
| Gejervall, et al (2005) | Sweden | Multi-center | 160/158 | VAS (0–100) | EA+PCB(lignocaine) Alfentanil+ Oral flunitrazepam+Rectal paracetamol+PCB(lignocaine) |
EA: 30–45 min before OPU till the end of the procedure |
| Sator-Katzenschlager, et al (2006) | Austria | Single-center | 94/94 | VAS (0–10) | Auricular EA+Metamizol+Remifentanil Auricular acupuncture+Metamizol+ Remifentanil Metamizol+ Remifentanil |
Auricular EA or auricular acupuncture: 30min before the procedure and last until 1 h after the procedure |
| Meng, et al (2008) | China | Single-center | 316/316 | Pain score of WHO (0–12); Pain rating of WHO | EA+ Dolantin Dolantin |
EA: 30-minute EA 1 day before OPU; EA 30min before OPU till the end of the procedure |
| Xu, et al (2008) | China | Single-center | 120/111 | VAS (0–100); Pain score of WHO (0–12); Pain rating of WHO | EA+Dolantin Dolantin |
EA: 30-minute EA 1 day before OPU; 30min before OPU till the end of the procedure |
| Kong, et al (2009) | China | Single-center | 60/60 | VAS (0–10); PRI (0–45); PPI (0–5) | TEAS+Dolantin Dolantin |
TEAS: 30min before OPU till the end of the procedure |
| Li, et al (2011) | China | Single-center | 409/409 | VAS (0–100) | EA+Dolantin Dolantin |
EA: 30min before OPU till the end of the procedure |
| Wang, et al (2011) | China | Single-center | 90/90 | VAS (0–10); PRI (0–45); PPI (0–5) | MA+Indometacin suppository Sham MA+Indometacin suppository Indometacin suppository |
MA: 15min before OPU till the end of the procedure |
| Chen, et al (2012) | China | Single-center | 134/134 | Pain score of WHO (0–12); Pain rating of WHO | EA+Dolantin Dolantin |
EA: 30min before OPU till the end of the procedure |
| Chen, et al (2015) | China | Single-center | 106/106 | VAS (0–10); Effective rate of analgesia | Auricular EA (Point group Auricular EA (Point group Pethidine |
Auricular EA: 10min before OPU till the end of the procedure |
| Fan, et al (2016) | China | Single-center | 90/90 | VAS (0–10); PRI (0–45); PPI (0–5) | Auricular point pressing+Indometacin suppository Sham auricular point pressing+Indometacin suppository Indometacin suppository |
Auricular point pressing: 20min before OPU, press the each auricular point for 30 seconds with even force |
| Yuan, et al (2017) | China | Single-center | 182/182 | Effective rate of analgesia | EA+propofol propofol |
EA: After the injection of propofol till the end of the procedure |
| Tian, et al (2020) | China | Multi-center | 392/390 | VAS (0–100); | TEAS Mock TEAS |
TEAS: 30min before OPU till the end of the procedure |
Abbreviations: VAS, visual analog scale; EA, electroacupuncture; PCB, paracervical block; OPU, oocyte pick-up; min, minute; MA, manual acupuncture; TEAS, transcutaneous electrical acupoint stimulation; WHO, World Health Organization; PRI, pain rating index; PPI, present pain intensity.
The included studies investigated populations of women undergoing IVF with a slight difference. Six studies25,26,27,31,33,34 recruited women undergoing IVF without other requirements. Thirteen studies8,25–36 included women with a mean age of under 35 years for females, and only one study37 included women with a mean age of over 35 years. Two studies29,37 specifically recruited women with previous IVF experience, while two studies30,35 required women undergoing the first-time IVF. Tian et al37 recruited women with five or fewer oocytes (diameter >10 mm) previously retrieved. See Table S1.
Quality of Studies
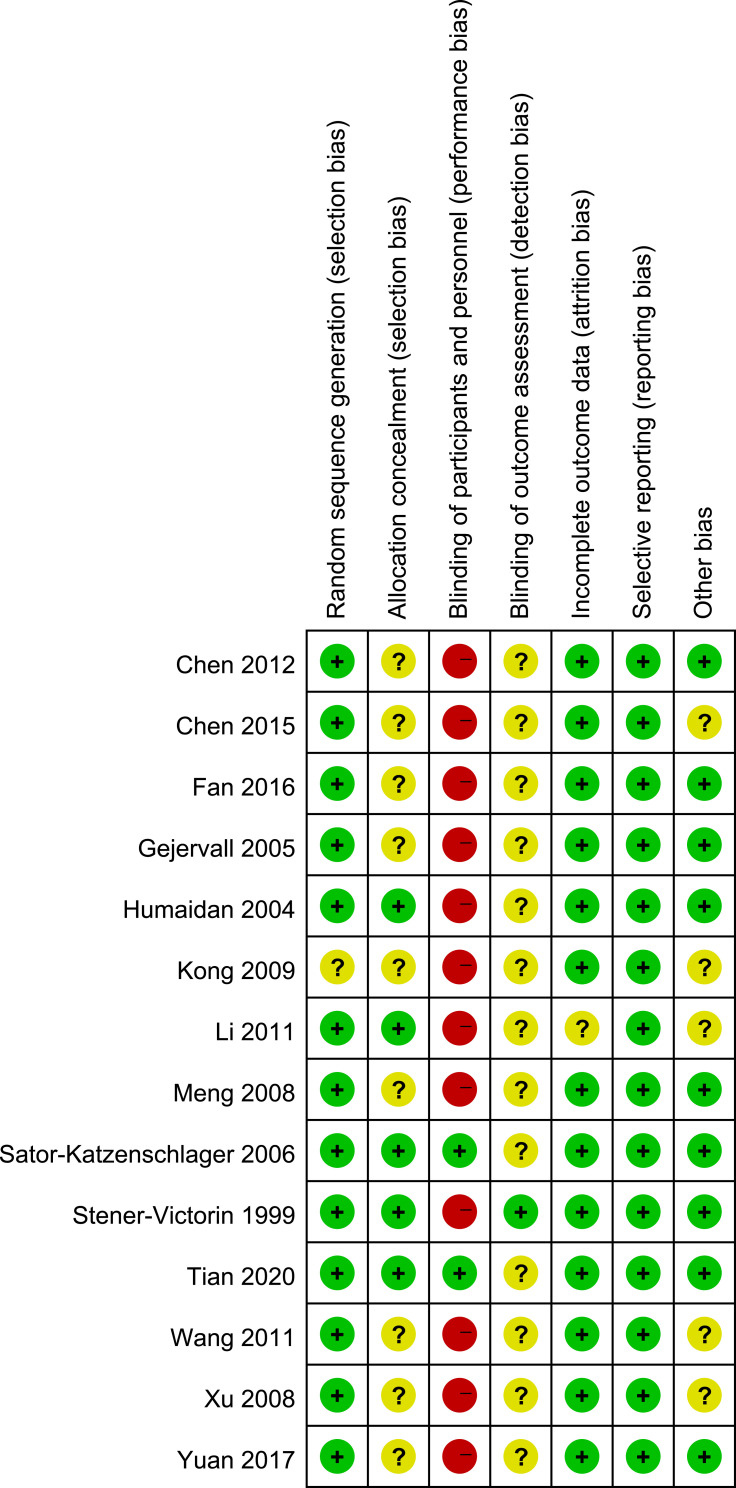
Figure 2 and Figure S1 demonstrated the risk of bias of the included studies. Only one study,30 which mentioned random methods, did not apply random sequence generation. Five studies25,26,28,31,37 applied allocation concealment. Only two studies28,37 applied the blinding of participants. Details of missing data were not reported in all included studies except for one study32 that had selective reporting bias due to the suspected incomplete report. Five studies29–32,34 remained other unclear bias. We assessed evidence to be generally of low or very low quality based on GRADE, owing to the high risk of bias and high heterogeneity. Self-rating scales as a primary indicator for evaluating pain were not high-quality evidence. The summary findings of various six interventions were conducted (see Table 2).
Figure 2.
Review authors’ judgments about each risk of bias item for each included study.
Table 2.
Quality of Evidence Based on GRADE
| Outcome Indicators (No. of Comparisons) | Result Summary | ||||
|---|---|---|---|---|---|
| No. of Participants | Effect Measurement (95% CI) |
Quality of Evidence | |||
| Intervention Group | Control Group | Relative Effect | Absolute Effect | ||
| Electroacupuncture with PCB versus PCB with CSA | |||||
| Intraoperative pain measured by VAS (3 comparisons of 3 RCTs) | 253 | 254 | _ | SMD 0.74 (0.42 to 1.06) |
⊕⊕○○ Low a, b |
| Postoperative pain measured by VAS (3 comparisons of 3 RCTs) |
253 | 254 | _ | SMD 0.30 (0.12 to 0.47) |
⊕⊕○○ Low a, b |
| Number of oocytes retrieved (1 comparison of 1 RCT) |
78 | 80 | _ | MD 2.00 (−0.04 to 4.04) |
⊕⊕○○ Low a, c |
| Adverse reactions (1 comparison of 1 RCT) |
_ | _ | Not estimate | _ | ⊕⊕○○ Low a, c |
| Acupuncture stimulation with CSA versus CSA | |||||
| Intraoperative pain measured by VAS (3 comparisons of 2 RCTs) |
212 | 210 | _ | SMD −1.03 (−1.71 to −0.36) |
⊕⊕○○ Low a, b |
| Intraoperative pain measured by WHO pain scores (3 comparisons of 3 RCTs) |
272 | 289 | _ | MD −1.21 (−2.18, −0.25) |
⊕⊕○○ Low a, b |
| Postoperative pain measured by simple numeral self-rating scale (2 comparisons of 2 RCTs) | 89 | 82 | _ | SMD −1.11 (−1.51 to −0.71) |
⊕⊕○○ Low a, e |
| Present pain intensity one hour after OPU (1 comparison of 1 RCT) |
30 | 30 | _ | MD −1.43 (−2.00 to −0.86) |
⊕⊕○○ Low a, e |
| Present pain intensity directly after OPU (1 comparison of 1 RCT) |
30 | 30 | _ | MD −0.94 (−1.24, −0.64) |
⊕⊕○○ Low a, e |
| Pain rating index directly after OPU (1 comparison of 1 RCT) |
30 | 30 | _ | MD −1.03 (−1.70, −0.36) |
⊕⊕○○ Low a, e |
| Pain rating index one hour after OPU (1 comparison of 1 RCT) |
30 | 30 | _ | MD −0.78 (−0.89 to −0.67) |
⊕⊕○○ Low a, e |
| Effective rates of pain intensity (4 comparisons of 4 RCTs) |
359 | 366 | OR 2.20 (0.82 to 5.87) | _ | ⊕○○○ Very Low a, b, d |
| Number of oocytes retrieved (4 comparisons of 3 RCTs) |
242 | 240 | _ | SMD 0.15 (−1.28 to 1.58) |
⊕⊕○○ Low a, c |
| Clinical pregnancy rate (3 comparisons of 3 RCTs) |
_ | _ | _ | Not estimate | ⊕⊕○○ Low a, c |
| High-quality embryo rate (1 comparison of 1 RCT) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Fertilization rate (2 comparisons of 2 RCTs) |
_ | _ | NOT estimate | _ | ⊕○○○ Very Low a, c, e |
| Abortion rate (2 comparisons of 2RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Content of β-endorphin in serum (1 comparison of 1 RCT) |
_ | _ | _ | Not estimate | ⊕○○○ Very Low a, c, e |
| Adverse reactions (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕⊕○○ Low a, c |
| Emotion evaluations (1 comparison of 1 RCT) |
_ | _ | _ | Not estimate | ⊕○○○ Very Low a, c, e |
| Acupuncture stimulation versus sham acupuncture stimulation | |||||
| Postoperative pain measured by simple numeral self-rating scale (1 comparison of 1 RCT) | 196 | 194 | _ | MD 3.82 (3.49 to 4.16) |
⊕⊕⊕○ Moderate a |
| Content of β-endorphin in serum (1 comparison of 1 RCT) |
_ | _ | _ | Not estimate | ⊕⊕○○ Low a, c |
| Acupuncture stimulation with NASIDs versus sham acupuncture stimulation with NASIDs | |||||
| Postoperative pain measured by simple numeral self-rating scale (2 comparisons of 2 RCTs) | 60 | 60 | _ | MD −1.76 (−2.08 to −1.44) |
⊕⊕○○ Low a, e |
| Present pain intensity directly after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −0.79 (−0.99 to −0.59) |
⊕⊕○○ Low a, e |
| Present pain intensity one hour after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −0.49 (−0.65 to −0.34) |
⊕⊕○○ Low a, e |
| Pain rating index directly after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −4.31 (−4.80 to −3.82) |
⊕⊕○○ Low a, e |
| Pain rating index one hour after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −1.05 (−1.27 to −0.82) |
⊕⊕○○ Low a, e |
| Number of oocytes retrieved (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −1.75 (−3.53 to 0.04) |
⊕○○○ Very Low a, c, e |
| High-quality embryo rate (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Fertilization rate (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Content of β-endorphin in serum (1 comparison of 1 RCT) |
_ | _ | _ | Not estimate | ⊕○○○ Very Low a, c, e |
| Adverse reactions (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Acupuncture stimulation with NASIDs versus NASIDs | |||||
| Postoperative pain measured by simple numeral self-rating scale (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −1.96 (−2.32 to 1.69) |
⊕⊕○○ Low a, e |
| Present pain intensity directly after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −0.94 (−1.18 to −0.71) |
⊕⊕○○ Low a, e |
| Present pain intensity one hour after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −0.32 (−0.47 to −0.17) |
⊕⊕○○ Low a, e |
| Pain rating index directly after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −4.15 (−4.74 to −3.56) |
⊕⊕○○ Low a, e |
| Pain rating index one hour after OPU (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −1.17 (−1.40 to −0.94) |
⊕⊕○○ Low a, e |
| Number of oocytes retrieved (2 comparisons of 2 RCTs) |
60 | 60 | _ | MD −0.83 (−2.66 to 1.00) |
⊕○○○ Very Low a, c, e |
| High-quality embryo rate (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Fertilization rate (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Content of β-endorphin in serum (1 comparison of 1 RCT) |
_ | _ | _ | Not estimate | ⊕○○○ Very Low a, c, e |
| Adverse reactions (2 comparisons of 2 RCTs) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
| Acupuncture stimulation versus CSA | |||||
| Postoperative pain measured by simple numeral self-rating scale (2 comparisons of 1 RCT) | _ | _ | _ | Not estimate | ⊕⊕○○ Low a, e |
| Effective rates of pain intensity (2 comparisons of 1 RCT) |
_ | _ | Not estimate | _ | ⊕⊕○○ Low a, e |
| Number of oocytes retrieved (2 comparisons of 1 RCT) |
_ | _ | _ | Not estimate | ⊕⊕○○ Low a, e |
| Adverse reactions (2 comparisons of 1 RCT) |
_ | _ | Not estimate | _ | ⊕○○○ Very Low a, c, e |
Notes:aDownload one level for serious risk of bias: included studies did not conduct the blinding method, and unclear risk of bias in one or two domains. bDowngraded one level for serious inconsistent: interventions of included studies inconsistent, or the outcome indicators exist statistical heterogeneous. cDowngraded one level for serious indirectness: this outcome index cannot directly represent the analgesic effect of acupuncture. dDowngraded one level for serious imprecision: some studies still judging the curative effect by indirect indexes such as pain grading and scoring. eDowngraded one level for serious imprecision: very small sample size.
Primary Outcomes
Various criteria were used to evaluate analgesic effectiveness: pain scores and rating of WHO were used in three studies;8,29,33 SF-MPQ were used in three studies;30,32,35 eight studies25–29,31,34,35 also used VAS to evaluate pain intensity; two studies34,36 conducted effective rate of analgesia (see Table 1). Eight studies25–28,30,32,35,37 recorded pain scores at multiple time points (see Table S2). We evaluated intraoperative and postoperative pain separately. The varied comparisons were as follows:
Electroacupuncture with PCB versus CSA with PCB;
Acupuncture stimulation (electroacupuncture) with CSA versus CSA;
Acupuncture stimulation versus CSA;
Acupuncture stimulation versus sham acupuncture stimulation;
Acupuncture stimulation with NASIDs versus sham acupuncture stimulation with NASIDs;
Acupuncture stimulation with NASIDs versus NASIDs.
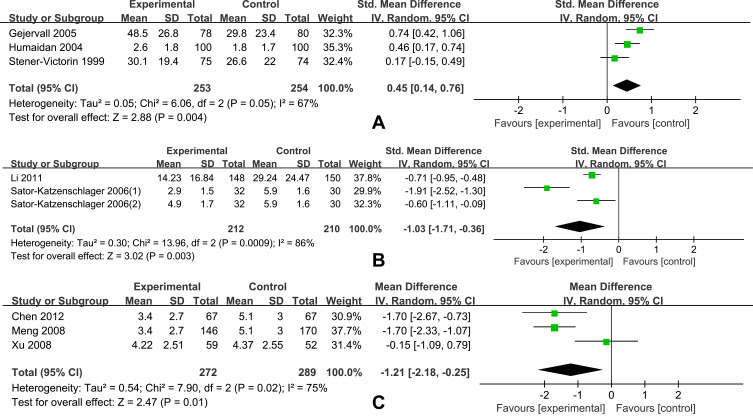
Simple Self-Rating Scale
Scores were pooled according to different scales (WHO pain rating scale or VAS). Meta-analysis showed that the analgesic intervention of PCB with CSA had a significant reduction in pain intensity than electroacupuncture with PCB during OPU (SMD=0.45, 95% CI: 0.14 to 0.76, Figure 3A). Three comparisons showed less intraoperative pain during OPU with acupuncture stimulation with CSA compared to CSA alone, with VAS scores of −1.03 (SMD=−1.03, 95% CI: −1.71 to −0.36, Figure 3B). Electroacupuncture with CSA showed better analgesia than CSA alone evaluated by WHO pain scores of −1.21 (MD=−1.21, 95% CI: −2.18 to −0.25, Figure 3C).
Figure 3.
Forest plot for intraoperative pain of random effect model evaluated by simple self-rating scales. (A) Forest plot for intraoperative pain of random effect model evaluated by VAS (Electroacupuncture with PCB versus PCB with CSA). (B) Forest plot for intraoperative pain of random effect model evaluated by VAS (Acupuncture stimulation with CSA versus CSA). (C) Forest plot for intraoperative pain of random effect model evaluated by WHO pain rating scale (Electroacupuncture with CSA versus CSA).
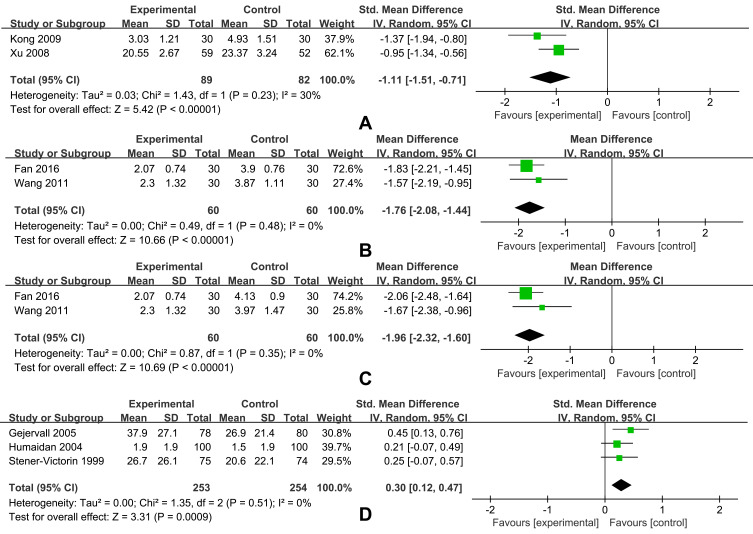
It was significantly lower postoperative pain of the acupuncture stimulation with CSA than CSA (SMD=−1.11, 95% CI: −1.51 to −0.71, Figure 4A). There was a significantly higher analgesic effect in the acupuncture stimulation with NSAIDs than sham acupuncture stimulation with NSAIDs (MD=−1.76, 95% CI: −2.08 to −1.44, Figure 4B). Investigators37 found that TEAS was associated with less pain when compared with mock TEAS (MD=−5.80, 95% CI: −6.10 to −5.55). Better analgesia effects were found in acupuncture stimulation with NSAIDs than NSAIDs (MD=−1.96, 95% CI: −2.32 to −1.60, Figure 4C). Chen et al study34 recorded that auricular electroacupuncture of two acupoint schemes was lower of postoperative VAS scores compared with CSA (P<0.05). An absolutely opposite result was that electroacupuncture with PCB showed the worse analgesic effect of PCB with CSA (SMD=0.30; 95% CI: 0.12 to 0.47, Figure 4D).
Figure 4.
Forest plot for postoperative pain measured by simple self-rating scales. (A) Forest plot for postoperative pain of random effect model evaluated by VAS (Acupuncture stimulation with CSA versus CSA). (B) Forest plot for postoperative pain of random effect model evaluated by VAS (Acupuncture stimulation with NSAIDs versus sham acupuncture stimulation with NSAIDs). (C) Forest plot for postoperative pain of random effect model evaluated by VAS (Acupuncture stimulation with NSAIDs versus NSAIDs). (D) Forest plot for postoperative pain of random effect model evaluated by VAS (Electroacupuncture with PCB versus PCB with CSA).
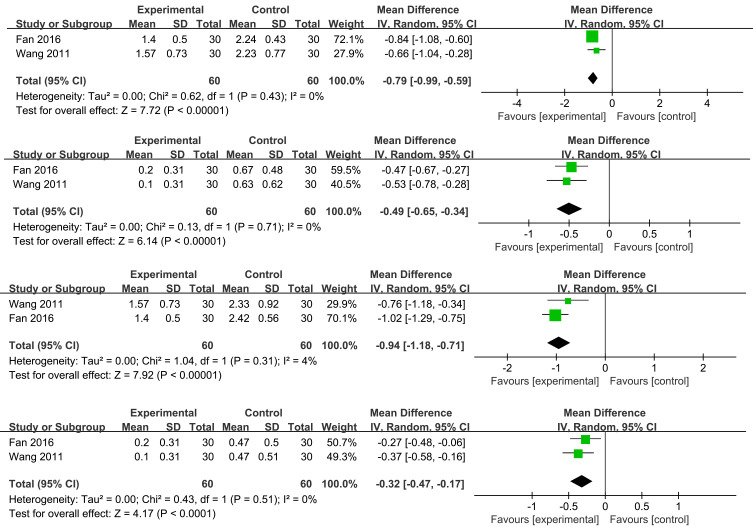
Present Pain Intensity and Pain Rating Index
There were significantly lower PPI scores of acupuncture stimulation with NSAIDs with high heterogeneity than sham acupuncture stimulation with NSAIDs under random models of whether directly after OPU (MD=−0.79, 95% CI: −0.99 to −0.59, Figure 5A) or one hour later (MD=−0.49, 95% CI: −0.65 to −0.34, Figure 5B). Acupuncture stimulation with NSAIDs also demonstrated lower PPI than NSAIDs whether directly (MD=−0.94, 95% CI: −1.18 to −0.71, Figure 5C) or one hour after OPU (MD=−0.32, 95% CI: −0.47 to −0.17, Figure 5D). One study30 showed that participants undergoing TEAS with CSA had lower PPI scores than CSA alone, whether directly (MD=−1.43, 95% CI: −2.00 to −0.86) or one hour after OPU (MD=−0.94, 95% CI: −1.24 to −0.64).
Figure 5.
Forest plot for pain of random effect model evaluated by PPI. (A) Forest plot for pain directly after oocyte retrieval of random effect model evaluated by PPI (Acupuncture stimulation with NASIDs versus sham acupuncture stimulation with NASIDs). (B) Forest plot for pain one hour after oocyte retrieval of random effect model evaluated by PPI (Acupuncture stimulation with NASIDs versus sham acupuncture stimulation with NASIDs). (C) Forest plot for pain directly after oocyte retrieval of random effect model evaluated by PPI (Acupuncture stimulation with NASIDs versus NASIDs). (D) Forest plot for pain one hour after oocyte retrieval of random effect model evaluated by PPI (Acupuncture stimulation with NASIDs versus NASIDs).
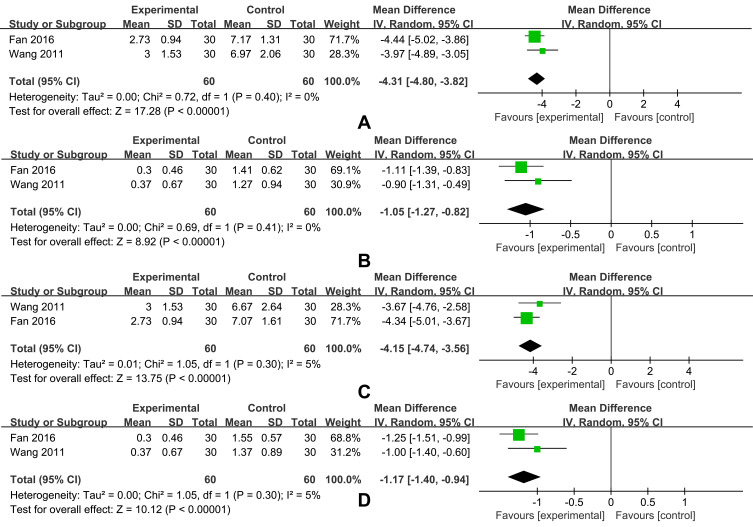
Significantly lower PRI scores were observed in groups treated with acupuncture with NSAIDs versus sham acupuncture with NSAIDs under random models of whether directly after OPU (MD=−4.31, 95% CI: −4.80 to −3.82, Figure 6A) or one hour later (MD=−1.05, 95% CI: −1.27 to −0.82, Figure 6B). NSAIDs was associated with a higher PRI than acupuncture with NSAIDs directly (MD=−4.15, 95% CI: −4.74 to −3.56, Figure 6C) or one hour after OPU (MD=−1.17, 95% CI: −1.40 to −0.94, Figure 6D). CSA was associated with higher PRI scores than TEAS combined with CSA calculated in Kong’s study30 whether directly (MD=−1.03, 95% CI: −1.70 to −0.36) or one hour after OPU (MD=−0.56, 95% CI: −0.93 to −0.19).
Figure 6.
Forest plot for pain of random effect model evaluated by PRI. (A) Forest plot for pain directly after oocyte retrieval of random effect model evaluated by PRI (Acupuncture stimulation with NSAIDs versus sham acupuncture stimulation with NSAIDs). (B) Forest plot for pain one hour after oocyte retrieval of random effect model evaluated by PRI (Acupuncture stimulation with NSAIDs versus sham acupuncture stimulation with NSAIDs). (C) Forest plot for pain directly after oocyte retrieval of random effect model evaluated by PRI (Acupuncture stimulation with NSAIDs versus NSAIDs). (D) Forest plot for pain one hour after oocyte retrieval of random effect model evaluated by PRI (Acupuncture stimulation with NSAIDs versus NSAIDs.
Effective Rates of Pain Intensity
In two studies,34,36 effective analgesia was defined as patients having no pain or mild pain during OPU. According to WHO rating, one study29 defined grade I, II, III as the corresponding intervention; otherwise, the analgesic efficacy is invalid (grade IV). Of two studies,8,33 the analgesic effect graded excellent or good were defined as the corresponding intervention otherwise invalid (grade poor). There was no significant difference in the effective rate in reducing oocyte retrieval pain of acupuncture with CSA than CSA alone (RR=1.02, 95% CI: 1.00 to 1.04, Figure S2). This finding was supported by another study,35 CSA was only associated with more pain during oocyte retrieval than auricular electroacupuncture of two different acupoint selection schemes (auricular electroacupuncture group: 35/36, 97.2%; versus CSA group: 33/34, 97.05%).
Secondary Outcomes
The Number of Oocytes Retrieved
A total of seven studies27,28,30–32,34,35 reported the number of oocytes retrieved that there was no significant difference observed in any comparisons. Meta-analysis showed no significant difference of the number of oocytes retrieved in acupuncture stimulation with NSAIDs group with either sham acupuncture with NSAIDs group (MD=−1.75, 95% CI: −3.53 to −0.04, Figure S3a) or NSAIDs (MD=−0.83, 95% CI: −2.66 to 1.00, Figure S3b). Measurement of acupuncture with CSA (MD=0.15, 95% CI: −1.28 to 1.58, Figure S3c) did not show advantages over CSA in the number of oocytes retrieved. Electroacupuncture with PCB showed no significant difference in the number of oocytes retrieved with CSA and PCB (P=0.06) in Gejervall et al study.27
Other Pregnancy Outcomes
We have documented and described pregnancy outcomes as follows: clinical pregnancy rates, quality embryo rates, fertilization rates, and abortion rates due to high heterogeneity. Five studies30–32,35,36 reported the clinical pregnancy rate after the intervention, but there was no difference between the intervention and control groups (P>0.05). Three studies30,32,35 reported the high-quality embryo rate after the intervention, but there was no difference between the intervention group and control groups (P>0.05). Four studies30,32,35,36 reported the fertilization rate after the intervention. Yuan’s study36 reported the fertilization rate per woman, and there was no significant difference between the acupuncture group and the control group (P>0.05). There was no significant difference in the total fertilization rate of the other three studies30,32,35 between the acupuncture group and the control group (P>0.05). Two studies31,36 reported the abortion rate after the intervention, but there was no difference between the intervention and control groups (P>0.05) (see Tables S3-S6).
Operation Related Indexes
Adverse Reactions
Six studies8,28,29,33,35,36 discussed the types of adverse reactions after surgery and the corresponding number of patients. The adverse reactions of OPU mainly included nausea, vomiting, and dizziness (see Table S7).
Emotion Changes
Four studies25–27,29 evaluated the emotional changes of participants at different time points. The results are uncertain because of different measurement standards. For preoperative emotions, one study25 demonstrated women in the acupuncture group were more stressed (P<0.05), a different result was found in another two studies26,27 that there was no difference between their groups (P>0.05). Two studies showed that there was no difference in an intraoperative emotional state.27,29
Follow-Up Assessment
Only Humaidan et al26 followed up with abdominal pain 24 hours after leaving the clinic, once every six hours. Also, the pain of the observation group and the control group decreased 30 minutes after leaving the clinic, and there was no significant difference between the two groups (P>0.05).
Operation Duration
The operation duration was recorded in six studies.27,28,32,34–36 There was no significant difference between the experimental and control groups (see Table S8). Yuan et al36 found that the time spent in the electroacupuncture combined with propofol group was shorter than propofol alone. EA combined with PCB treatment in Gejervall et al study27 took longer than premedication and alfentanil. Fan35 and Wang32 conducted correlation analysis and found that there was no correlation between operation time and postoperative PRI, VAS, and PPI in the acupuncture group and the control group (P>0.05). Humaidan et al26 found that the outpatient time and cost of each OPU in the acupuncture group were significantly lower than those in the control group (P<0.001). Gejervall et al27 made an economic comparison between acupuncture and non-acupuncture, and found no significant difference in cost between the two groups (P = 0.718).
β-Endorphin in Serum
Three studies30,35,37 reported postoperative β-endorphin in serum. The intervention group of Fan’s study35 and Tian et al study37 was significantly higher than the control group (P<0.05), and there was no difference in Kong’s study30 between the intervention group and the control group (P>0.05). See Table S9.
Discussion
General Discussion of Main Results
This review included 14 studies and investigated the analgesic effects of acupuncture in women during OPU through meta-analysis. Although previous reviews have examined several aspects of acupuncture analgesia,2,10,38 only one of these studies10 examined the analgesic effect of acupuncture-based during OPU limitedly. Other studies utilized acupuncture as an adjunctive therapy exploring analgesia for OPU.2,38 Compared to previous studies, we updated relevant studies to dates8,29–37 and selected more specific analytical measures.10 Finally, we included 14 studies with varied quality of individual studies separately. The overall sample size varies widely between studies, ranging from 60 to 409, and only two studies28,37 reported blinded methods, which resulted in higher bias and heterogeneity.
Our findings were consistent with the previous studies2 that acupuncture combined with active analgesia showed better effects than single-strand analgesia. Acupuncture with CSA was more effective than CSA in intraoperative8,28,29,31,33 and postoperative29,30 analgesia. Meanwhile, acupuncture with NSAIDs was more effective than sham acupuncture stimulation with NSAIDs (or NSAIDs alone).32,35 Regarding PPI and PRI scores at postoperative or one hour postoperatively, the acupuncture group (with or without the combination of other analgesic methods) in all three studies30,32,35 showed better analgesia than the control group. Besides, our findings suggested there was no significant analgesic advantage comparing electroacupuncture with PCB versus CSA with PCB, that there were no obvious analgesic advantages of the two interventions. In Stener-Victorin et al study,25 the analgesic effect of acupuncture combined with PCB was inferior to the analgesic effect of the combination of PCB and CSA. Noteworthy, participants in control groups in Gejervall et al study27 and Humaidan et al study26 received sedative pre-administration consisting of 0.5 mg of oral flurazepam and 1 g of rectal paracetamol, or 10 mg of benzodiazepines before intravenous injection of fentanyl and PCB. We cannot readily distinguish between anxiolytic, sedative, and analgesic effects because the preoperative medication might interfere to some extent with the ability to report pain experience.
In only one study, acupuncture was used as an independent analgesic. Tian et al conducted a large-sample study that proved that TEAS was more effective than mock TEAS.37 The number of oocytes retrieved and the related need for repeat aspirations directly affected the demand for analgesics. In this study, acupuncture could be independent and enough to relieve pain, possibly due to the small number of eggs taken in the two groups (mean <3). Discomfort and pain during or after oocyte retrieval due to the several aspirations performed to obtain more oocytes. When more oocytes are retrieved, the ability of acupuncture to meet analgesia requires further exploration.
Pain Assessments and Management
Pain is a highly subjective and complex physiological and psychological activity, so subjective perception is the primary standard for evaluation.39,40 In surgical pain assessment, pain sensation should be reassessed several times depending on the type of procedure, adequacy of initial pain relief, side effects, presence of complications, and clinical status changes.40 The SMDs in pain on the simple self-rating scale (both VAS and WHO pain rating) between different acupuncture compound methods showed a clinical improvement in this review.8,28,29,31,33 Most of the studies used a one-dimensional scale pain assessment tool with fewer time points for pain assessment, and the percentage of pain reduction was not calculated. Therefore, data consolidation was complex, making it difficult to provide high-quality, evidence-based evidence. Threshold assessment may be an additional valuable tool based on individual variability,41 while biochemical markers that can be used to measure pain under stress, such as β-endorphin in serum and urinary CRF-LI concentrations, are also valuable. Still, only one study mentioned intraoperative threshold assessment,29 while three studies30,35,37 reported postoperative β-endorphin in serum.
Advantages of Acupuncture for Analgesia
Acupuncture is an appropriate option for women to avoid pharmacological anesthesia, including GA, PCB, CSA, which mainly produces postoperative adverse effects and potential effects on oocytes or embryos. Regional anesthesia has minimal effect on oocytes due to limited absorption in the circulation.42 Conversely, GA found in the follicular fluid may imply potential harms.43 Although the need for GA or non-invasive transvaginal OPU was decreased, the side effects of local anesthesia such as spinal headache, back pain, urinary retention, and significant nerve damage, and the inability to significantly meet the minimum requirements for analgesia have limited the potential use of local anesthesia. Propofol conscious sedation becomes a clear choice for OPU with rapid onset and recovery, adequate pain control, and no toxic side effects on the embryo and oocyte. Four studies8,29,33,36 included in this review indicated acupuncture combined with dolantin or propofol analgesia decreased adverse effects compared to using dolantin or propofol alone.
Over the years, acupuncture has become more widely recognized as having definitive efficacy in treating acute or chronic pain.44,45 This conventional therapy achieves pain intensity during OPU by suppressing the endogenous opioid system, increasing endogenous opioid peptide release, reducing inflammation, and improving uterine blood flow changes.6,46,47 In this review, Fan35 and Tian et al37 found significantly higher β-endorphin in the acupuncture group than the control groups (P<0.05). We also discovered that acupuncture is a safe analgesic approach since there were no differences between groups about the number of oocytes retrieved27,28,30–32,34,35 or clinical pregnancy30–32,35,36 after the procedure.
Limitations
The review included a small number of studies with relatively low-quality evidence. Comparison of previous studies across trials was made difficult because acupuncture analgesia is often combined with other analgesic methods and by the lack of standard pain assessments. Indicators regarding the assessment, management of pain were not included in the study for discussion.
Conclusions
Acupuncture compound pharmacological anesthesia, which is more effective than a single form of pain relief, is worth promoting and safe. The quality of evidence regarding acupuncture alone as an analgesic is inadequate, and it is questionable whether minimal analgesia can be achieved. More high-quality trials need to be conducted to explore the analgesia of acupuncture for OPU in the future. The reduction in scores with the self-rated pain scales indicates a limitation in the improvement of symptoms. There should be more consensus and dimensionality in the assessment of pain. Individualized treatment and satisfaction assessment should also be considered in the management of pain.
Funding Statement
This work was funded by the National Natural Science Foundation of China (grant number 81973966); Sichuan Provincial Science and Technology Department Project (grant number 2020JDJQ0051); Clinical Research Center for Acupuncture and Moxibustion in Sichuan Province.
Abbreviations
OPU, oocytes pick-up; ART, assisted reproductive technology; IVF, in vitro fertilization; GA, general anesthesia; PCB, paracervical block; CSA, conscious sedation and analgesia; RCTs, randomized controlled trials; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses; TEAS, transcutaneous electrical acupoint stimulation; SF-MPQ, simplified McGill pain questionnaire; VAS, visual analog scale; WHO, World Health Organization; ORs, odds ratios; SMD, standardized mean difference; MD, mean difference; CIs, confidence Intervals; GRADE, Grading of Recommended Assessment Development and Evaluation; NSAIDs, non-steroidal anti-inflammatory drugs; PPI, present pain intensity; PRI, pain rating index; NRS, numerical rating scale.
Data Sharing Statement
All the data was shown in the article.
Ethics Approval
Not applicable.
Consent for Publication
Written informed consent for publication was obtained from all participants.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kwan I, Wang R, Pearce E, Bhattacharya S. Pain relief for women undergoing oocyte retrieval for assisted reproduction. Cochrane Database Syst Rev. 2018;7(1):5. doi: 10.1186/s13643-018-0693-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hammarberg K, Wikland M, Nilsson L, Enk L. Patients’ experience of transvaginal follicle aspiration under local anesthesia. Ann N Y Acad Sci. 1988;541:134–137. doi: 10.1111/j.1749-6632.1988.tb22249.x [DOI] [PubMed] [Google Scholar]
- 3.Beck R, Brizzi A, Cinnella G, Raimondo P, Kuczkowski KM. Anesthesia and analgesia for women undergoing oocyte retrieval. Pick Up Oocyte Manage. 2020. [Google Scholar]
- 4.Soussis I, Boyd O, Paraschos T, et al. Follicular fluid levels of midazolam, fentanyl, and alfentanil during transvaginal oocyte retrieval. Fertil Steril. 1995;64(5):1003–1007. doi: 10.1016/S0015-0282(16)57919-9 [DOI] [PubMed] [Google Scholar]
- 5.Wikland M, Evers H, Jakobsson AH, Sandqvist U, Sjoblom P. The concentration of lidocaine in follicular fluid when used for paracervical block in a human IVF-ET programme. Hum Reprod. 1990;5(8):920–923. doi: 10.1093/oxfordjournals.humrep.a137220 [DOI] [PubMed] [Google Scholar]
- 6.Qiao L, Guo M, Qian J, Xu B, Gu C, Yang Y. Research advances on acupuncture analgesia. Am J Chin Med. 2020;48(2):245–258. doi: 10.1142/S0192415X20500135 [DOI] [PubMed] [Google Scholar]
- 7.Chen T, Zhang WW, Chu YX, Wang YQ. Acupuncture for pain management: molecular mechanisms of action. Am J Chin Med. 2020;48(4):793–811. doi: 10.1142/S0192415X20500408 [DOI] [PubMed] [Google Scholar]
- 8.Meng P, Wang LL, Xu B, Sun HX. [Application of acupuncture compound anesthesia in transvaginal ultrasound-guided oocyte retrieval]. Zhongguo Zhen Jiu. 2008;28(6):451–455. Chinese. [PubMed] [Google Scholar]
- 9.Xiang A, Cheng K, Shen X, Xu P, Liu S. The immediate analgesic effect of acupuncture for pain: a systematic review and meta-Analysis. Evid Based Complement Alternat Med. 2017;2017:3837194. doi: 10.1155/2017/3837194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stener-Victorin E. The pain-relieving effect of electroacupuncture and conventional medical analgesic methods during oocyte retrieval: a systematic review of randomized controlled trials. Hum Reprod. 2005;20(2):339–349. DOI: 10.1093/humrep/deh595 [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 12.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. doi: 10.1016/0304-3959(75)90044-5 [DOI] [PubMed] [Google Scholar]
- 13.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med. 1988;18(4):1007–1019. doi: 10.1017/S0033291700009934 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Green SCochrane Handbook for Systematic Reviews of Interventions. Version 5.0.1 [updated September 2008]. The Cochrane Collaboration; 2008. Available from: http://www.cochrane-handbook.org. Accessed March30, 2018..
- 15.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Böhning D, Lerdsuwansri R, Holling H. Some general points on the measure of heterogeneity in meta-analysis. Metrika. 2017;80(6–8):685–695. doi: 10.1007/s00184-017-0622-3 [DOI] [Google Scholar]
- 17.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 19.Humaidan P. Pain relief during oocyte retrieval - exploring the role of different frequencies of electroacupuncture. Reprod Biomed Online. 2006;13(1):120–125. doi: 10.1016/S1472-6483(10)62025-1 [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y. Application of transcutaneous electrical nerve stimulation in postoperative analgesia. Smart Healthcare. 2021;7(5):85–86,89. [Google Scholar]
- 21.Zhang J, Wang X, Lü R. Analgesic effect of acupuncture at hegu (LI 4) on transvaginal oocyte retrieval with ultrasonography. J Tradit Chin Med. 2013;33(3):294–297. doi: 10.1016/S0254-6272(13)60167-3 [DOI] [PubMed] [Google Scholar]
- 22.Zhang XY. The Clinical Study of Transcutaneous Electrical Acupoint Stimulation Analgesia During Oocyte Retrieval Operation in vitro Fertilization-Embryo Transfer (IVF-ET). Shandong University of TCM; 2014. [Google Scholar]
- 23.Ding W, Huang JA randomized controlled study on the analgesic effect of electroacupuncture at different auricular points on in vitro fertilization-embryo transfer egg retrieval. Proceedings of the 2015 Annual Meeting of the Chinese Society of Acupuncture and Moxibustion. Shanghai. [Google Scholar]
- 24.Cui SL, Li JY, Yu CY, et al. The role of electroacupuncture in in vitro fertilization for oocyte retrieval. Proceedings of the 2017 World Congress of Acupuncture and Moxibustion and the 2017 Annual Meeting of the Chinese Society of Acupuncture and Moxibustion. Beijing. [Google Scholar]
- 25.Stener-Victorin E, Waldenstrom U, Nilsson L, Wikland M, Janson PO. A prospective randomized study of electroacupuncture versus alfentanil as anaesthesia during oocyte aspiration in in-vitro fertilization. Hum Reprod. 1999;14(10):2480–2484. doi: 10.1093/humrep/14.10.2480 [DOI] [PubMed] [Google Scholar]
- 26.Humaidan P, Stener-Victorin E. Pain relief during oocyte retrieval with a new short duration electroacupuncture technique - an alternative to conventional analgesic methods. Hum Reprod. 2004;19(6):1367–1372. doi: 10.1093/humrep/deh229 [DOI] [PubMed] [Google Scholar]
- 27.Gejervall AL, Stener-Victorin E, Moller A, Janson PO, Werner C, Bergh C. Electroacupuncture versus conventional analgesia: a comparison of pain levels during oocyte aspiration and patients’ experiences of well-being after surgery. Hum Reprod. 2005;20(3):728–735. doi: 10.1093/humrep/deh665 [DOI] [PubMed] [Google Scholar]
- 28.Sator-Katzenschlager SM, Wolfler MM, Kozek-Langenecker SA, et al. Auricular electroacupuncture as an additional perioperative analgesic method during oocyte aspiration in IVF treatment. Hum Reprod. 2006;21(8):2114–2120. doi: 10.1093/humrep/del110 [DOI] [PubMed] [Google Scholar]
- 29.Xu JY. Clinical Observation on Efficacy of Analgesia for Electroacupuncture Interventional Therapy on Patients with Multiple Oocyte Aspiration Process of in vitro Fertilization and Embryo Transfer Training. Nanjing University of TCM; 2008. [Google Scholar]
- 30.Kong W. Application of Acupuncture Compound Anesthesia in Oocyte Retrieval Operation Undergoing in vitro Fertilization-Embryo Transfer. Shandong University of TCM; 2008. [Google Scholar]
- 31.Li N. A Clinical Study of Acupuncture Treatment in IVF-ET. Universuty of Lanzhou; 2011. [Google Scholar]
- 32.Wang XH. Application of Acupuncture Anethesia in IVF-ET Transvaginal Ultrasound-Guided Oocyte Retrieval. Shandong University of TCM; 2011. [Google Scholar]
- 33.Chen QQ, Wei QL, Zhang XH. [Effects of eletroacupuncture on supplementary analgesia and improvement of adverse reactions induced by dolant in oocyte retrieval]. Zhongguo Zhen Jiu. 2012;32(12):1113–1116. Chinese. [PubMed] [Google Scholar]
- 34.Chen H, Wang YP, Xing JQ, et al. [Application of electroacupuncture at auricular points for analgesia in IVF-ET]. Jiangsu Med. 2015;41(23):2863–2865. Chinese. [Google Scholar]
- 35.Fan K. Application of Auricular Analgesic Therapy in IVF-ET Transvaginal Ultrasound-Guided Oocyte Retrieval. Shandong University of TCM; 2016. Chinese. [Google Scholar]
- 36.Yuan H, Zhang LS, Wang N. [Evaluation of analgesic effect of acupuncture combined with electroacupuncture in IVF-ET]. J External Ther TCM. 2017;26(3):38–39. Chinese. [Google Scholar]
- 37.Tian L, Feng X, Zhang R, et al. Pain relief during oocyte retrieval by transcutaneous electrical acupoint stimulation: a single-blinded, randomized, controlled multicenter trial. Evid Based Complement Alternat Med. 2020;2020:3285648. doi: 10.1155/2020/3285648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheong YC, Dix S, Hung Y, Ng E, WL Ledger, Farquhar C. Acupuncture and assisted reproductive technology. Cochrane Db Syst Rev. 2013;7. doi: 10.1002/14651858.CD006920.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–1093. doi: 10.1016/j.jpainsymman.2010.08.016 [DOI] [PubMed] [Google Scholar]
- 40.Gordon DB. Acute pain assessment tools: let us move beyond simple pain ratings. Curr Opin Anaesthesiol. 2015;28(5):565–569. doi: 10.1097/ACO.0000000000000225 [DOI] [PubMed] [Google Scholar]
- 41.Lund I, Lundeberg T. Aspects of pain, its assessment and evaluation from an acupuncture perspective. Acupunct Med. 2006;24(3):109–117. doi: 10.1136/aim.24.3.109 [DOI] [PubMed] [Google Scholar]
- 42.Kogosowski A, Lessing JB, Amit A, Rudick V, Peyser MR, David MP. Epidural block: a preferred method of anesthesia for ultrasonically guided oocyte retrieval. Fertil Steril. 1987;47(1):166–168. doi: 10.1016/S0015-0282(16)49954-1 [DOI] [PubMed] [Google Scholar]
- 43.Guasch E, Gómez R, Brogly N, Gilsanz F. Anesthesia and analgesia for transvaginal oocyte retrieval. Should we recommend or avoid any anesthetic drug or technique? Curr Opin Anaesthesiol. 2019;32(3):285–290. doi: 10.1097/ACO.0000000000000715 [DOI] [PubMed] [Google Scholar]
- 44.Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for Chronic Pain: update of an individual patient data meta-analysis. J Pain. 2018;19(5):455–474. doi: 10.1016/j.jpain.2017.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jan AL, Aldridge ES, Rogers IR, Visser EJ, Bulsara MK, Niemtzow RC. Does acupuncture have a role in providing analgesia in the emergency setting? a systematic review and meta-analysis. Emerg Med Australas. 2017;29(5):490–498. doi: 10.1111/1742-6723.12832 [DOI] [PubMed] [Google Scholar]
- 46.Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26(1):17–22. doi: 10.1016/S0166-2236(02)00006-1 [DOI] [PubMed] [Google Scholar]
- 47.Erthal V, da Silva MD, Cidral-Filho FJ, Santos AR, Nohama P. ST36 laser acupuncture reduces pain-related behavior in rats: involvement of the opioidergic and serotonergic systems. Lasers Med Sci. 2013;28(5):1345–1351. doi: 10.1007/s10103-012-1260-7 [DOI] [PubMed] [Google Scholar]