Abstract
Objective
During the COVID-19 pandemic, visits for diabetes care were abruptly canceled without predefined procedures to re-engage patients. This study was designed to determine how outreach influences patients to maintain diabetes care and identify factors that might impact the intervention’s efficacy.
Methods
A diabetes nursing team attempted outreach for patients who had a canceled appointment for diabetes between March 16, 2020, and June 19, 2020. Outreach status was defined as reached, message left, or no contact. Outcomes were defined as follows: (1) booking and (2) keeping a follow-up appointment.
Results
Seven hundred eighty-seven patients were included (384 [49%] were reached, 152 (19%) were left a message, and 251 (32%) had no contact). Reached patients were more likely to book [odds ratio (OR) = 2.43, P < .001] and keep an appointment (OR = 2.39, P < .001) than no-contact patients. Leaving a message did not increase the odds of booking (OR = 1.05, P = .84) or keeping (OR = 1.17, P = .568) an appointment compared with no contact. Older age was a significant predictor of booking an appointment (OR = 1.014 for each year of age, P = .037). Patients on insulin were more likely to keep their appointment (OR = 1.70, P = .008). Patients with a higher hemoglobin A1C level were less likely to keep their appointment (OR = 0.87 for each 1.0% increase in the hemoglobin A1C level, P = .011).
Conclusion
These findings suggest that to optimize re-engagement during care disruption, 1-way communication is no better than no contact and that 2-way communication increases the likelihood that patients will maintain access to care. In addition, although higher-risk patients (eg, patients with older age or those on insulin) may be more incentivized to stay engaged, targeted outreach is needed for those with chronically poor glycemic control.
Key words: diabetes, re-engagement, care disruption, COVID-19
Abbreviations: HbA1C, hemoglobin A1C; OR, odds ratio; PWD, people with diabetes
Introduction
Across the globe, the COVID-19 pandemic has caused sustained disruptions in access to usual care, and this has had a significant impact on people with diabetes (PWD).1, 2, 3, 4 On January 20, 2020, the first case of COVID-19 in the United States was diagnosed in Washington state, and by March 2, 2020, the SARS-CoV-2 virus was identified in Massachusetts. A pandemic was declared on March 11, 2020, by the World Health Organization, and the United States entered a national emergency on March 13, 2020.5 This rapid succession of events led public health officials to advise people to stay at home for mild illness to limit the workload of hospitals and save medical resources for moderate-to-severe illness. This resulted in a 25% to 88% decrease in emergency room visits,6, 7, 8 up to 72% canceled elective surgeries,9 , 10 and reduced routine care visits.11, 12, 13 Although the decrease in emergency room visits may have partially been due to fewer opportunities for injuries and trauma during the lockdown, it was also thought to have been due to patients delaying care.3 , 6, 7, 8
PWD have been uniquely impacted by the pandemic, with many groups publishing a 2-3-fold increased risk of severe disease and mortality due to COVID-19, compared with people without diabetes.1 Early recognition of this risk has led to more confinement of PWD and decreased engagement with chronic care management. Moreover, as a result of population-level lockdown orders, patients have had less access to healthy foods, reduced options for exercise, missed appointments, and interrupted access to medications.2, 3, 4 Considering the decades of evidence showing the importance of patient engagement in achieving and maintaining disease control,14, 15, 16, 17, 18 clinicians have become concerned about a negative impact on outcomes, especially given the lack of applicable guidance for health care providers and systems to maintain patient engagement during the pandemic.
Previous natural disasters and pandemics resulted in the same patterns of care disruption and lack of guidance to keep patients engaged throughout. Hurricanes Katrina (2005), Sandy (2012), and Maria (2017) led to clinics being closed for extended periods of time, leading to lack of access to medications, decreased rates of routine health screenings, and worsening of disease.19, 20, 21 During a 2003 SARS outbreak in Toronto, Nasef et al22 described a disorganized and inconsistent approach to patient care due to lack of advanced pandemic planning. These past disasters, both weather- and pandemic-related, demonstrate that the public’s attention focuses on the acute event and away from their health, which can take many months to re-engage.20
Despite calls for future disaster planning,2 , 6 , 9 , 11 , 19 , 21 , 22 the optimal methodology to maintain patient engagement in diabetes care during crises remains unknown. In the days before the lockdown in Massachusetts, the Brigham and Women’s Hospital Diabetes Program developed and implemented a standardized method of outreach to re-engage patients whose upcoming visits to the clinic had been canceled. This study employed a natural experiment to determine how communication between patients and providers influences patients’ re-engagement and explored factors that may impact the intervention’s efficacy.
Methods
This study was derived from an administrative program to address the increase in cancelations during the initial period of the COVID-19 pandemic. The study was approved by the institutional review board. To prepare for the expected high rates of cancelation during transition to virtual clinics, the diabetes program launched a patient-tracking initiative that temporarily redeployed ambulatory nurses to perform remote outreach. Between March 16, 2020, and June 19, 2020, ie, 14 weeks, an administrative report (physician online reporting) was run daily to capture all canceled and scheduled appointments with the physician, nurse practitioner, or registered nurse in the diabetes clinic. Patients who canceled and had not been seen at the clinic within the last month were placed in the patient tracker system, a sharable workbook, for proactive outreach by a diabetes nursing team. Outreach was conducted via telephone and online patient portal messaging for those who had access; interpreter services were used per standard practice for those who did not speak English. Documentation of outreach messages and calls was standardized using a predesigned note template that addressed acute problems, medication, supply access, and encouragement to schedule a follow-up visit (Supplementary Material). After the intervention period, a chart review was performed to record 2 outcomes: (1) whether the patient booked an appointment and (2) whether the patient kept the appointment before the end of October 2020, 4 months after the end of the intervention.
Statistical Analysis
Baseline descriptive statistics are presented as frequency (percentage) for categorical variables and mean (SD) for continuous variables. Outreach status for scheduling an appointment was defined as reached (2-way communication between the clinician and patient), message left (1-way communication by the provider), or no contact (no communication between the provider and patient). Engagement outcomes were defined as follows: (1) booking a follow-up appointment with the endocrinology department and (2) keeping an appointment by the end of October 2020. Multivariable logistic regression models were used to determine the association (using odds ratios [ORs] with 95% CIs) between booking or keeping an appointment and the outreach status, with adjustment for baseline covariates. Patients with nonpandemic-related cancelations were excluded from the analysis. We defined these cancelations using the following criteria: (1) canceled prior to the year 2020, (2) canceled because of transferring care to elsewhere, (3) provider rescheduled the clinic visit to a different date, or (4) there was a notation by the staff that the appointment was made erroneously. The statistical analyses were performed using Stata, version 15.0.
Results
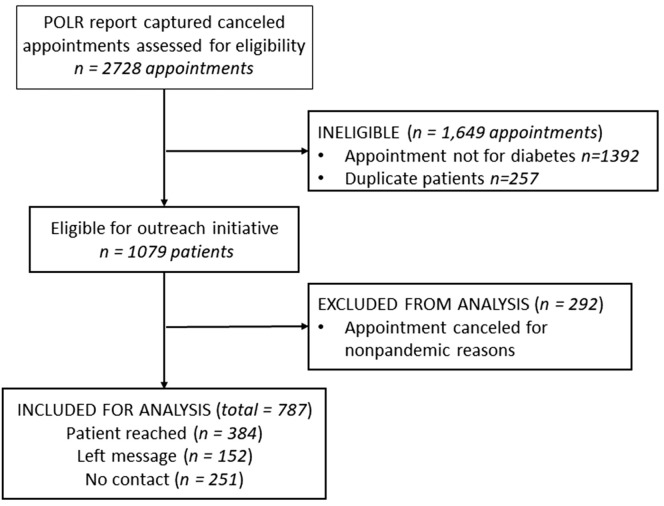
A total of 2728 patients were identified as having a canceled appointment between March 16, 2020, and June 19, 2020. Of these, 1392 were excluded because the appointment was not for diabetes, 257 were excluded because of duplicate entries, and 292 were excluded because the appointment was canceled for nonpandemic-related reasons. The remaining 787 patients were considered as having canceled appointments for diabetes due to the pandemic and were included in this analysis (Fig. 1 ).
Fig. 1.
Strengthening the Reporting of Observational Studies in Epidemiology flowchart for inclusion. Physician online reporting reports captured 2728 canceled appointments between March 16, 2020, and June 19, 2020, ie, 14 weeks. Of these, 1941 patients were excluded, and the remaining 787 patients were included in the analysis of the outreach initiative. Outreach status was defined as reached (2-way communication between the clinician and patient via telephone or an electronic health record portal message), message left (1-way communication, eg, voicemail), or no contact. POLR = physician online reporting.
The mean (SD) age of the patients included was 61.7 (14.2) years; of all the patients, 53.7% were women, 67.3% were White, and 89% spoke English. Type 2 diabetes was present in 85% of the population, the baseline hemoglobin A1C (HbA1C) level was 7.96% (1.81) (63 mmol/mol), 65% were on insulin, and the baseline glomerular filtration rate was 74.2 mL/min (24.9) (Table ). Of the 787 patients, 384 (49%) were reached, 152 (19%) were left a message, and 251 (32%) had no contact (Table). The no-contact cohort was used as a reference group for the statistical analysis and comparison.
Table.
Patient Population Characteristics by Outreach Status
| Variable | Total N = 787 (100%) |
Patient reached n = 384 (48.8%) |
Left message n = 152 (19.3%) |
No contact n = 251 (31.9%) |
P value among groups |
|---|---|---|---|---|---|
| Age, y, (mean ± SD) | 61.7 ± 14.2 | 61.5 ± 13.8 | 59.4 ± 14.2 | 63.3 ± 14.5 | .025a |
| Female, n (%) | 423 (53.7%) | 211 (54.9%) | 72 (47.4%) | 140 (55.8%) | .209b |
| Race, n (%) | .163b | ||||
| Asian | 39 (5.0%) | 20 (5.2%) | 11 (7.2%) | 8 (3.2%) | |
| Black | 110 (14.0%) | 46 (11.9%) | 21 (13.8%) | 43 (17.1%) | |
| Hispanic | 34 (4.3%) | 14 (3.6%) | 5 (3.3%) | 15 (5.9%) | |
| White | 530 (67.3%) | 269 (70.05%) | 94 (61.8%) | 167 (66.5%) | |
| Other | 43 (5.5%) | 21 (5.5%) | 12 (7.9%) | 10 (3.9%) | |
| Unknown | 31 (4.0%) | 14 (3.6%) | 9 (5.9%) | 8 (3.2%) | |
| Insurance, n (%)d | .477b | ||||
| Commercial | 411 (53.0%) | 201 (52.6%) | 82 (55.0%) | 128 (52.0%) | |
| Medicaid | 82 (11.6%) | 34 (8.9%) | 17 (11.4%) | 31 (12.6%) | |
| Medicare | 279 (36.0%) | 146 (38.2%) | 49 (32.9) | 84 (34.2%) | |
| Self-pay/other | 5 (0.6%) | 1 (0.3%) | 1 (0.7%) | 3 (1.2%) | |
| Type 2 diabetes | 665 (84.5%) | 314 (81.7%) | 126 (82.9%) | 225 (89.6%) | .035b |
| Type 1 diabetes | 93 (11.8%) | 53 (13.8%) | 21 (13.8%) | 19 (7.6%) | |
| Insulin use, n (%) | 508 (64.5%) | 263 (68.5%) | 95 (62.5%) | 150 (59.7%) | .067b |
| Baseline HbA1C %, mmol/mol, (mean ± SD) | 7.96 ±1.81 (63 ± 17.63) | 7.83 ±1.72 (62 ± 16.65) | 8.26 ±1.78 (67 ± 17.30) | 7.97 ±1.94 (64 ± 19.05) | .056a |
| Baseline GFR, mL/min, (mean ± SD) | 74.2 ± 24.9 | 74.1 ± 25.01 | 77.27 ± 25.9 | 72.59 ± 23.97 | .225a |
| Deceased, n (%) | 9 (1.1%) | 4 (1.0) | 0 (0.0%) | 5 (2.0%) | .215c |
Abbreviations: GFR = glomerular filtration rate; HbA1C = hemoglobin A1C.
Patients who canceled a diabetes appointment between March 16, 2020, and June 19, 2020, because of the pandemic were provided outreach by a diabetes nursing team. The outreach status was defined as reached (2-way communication between the clinician and patient via telephone or an electronic health record portal message), message left (1-way communication, eg, voicemail), or no contact.
P values indicate differences among the groups based on analysis of variance.
P values indicate differences among the groups based on the chi-square test.
P values indicate differences among the groups based on the Fisher exact test.
Missing data from 10 individuals.
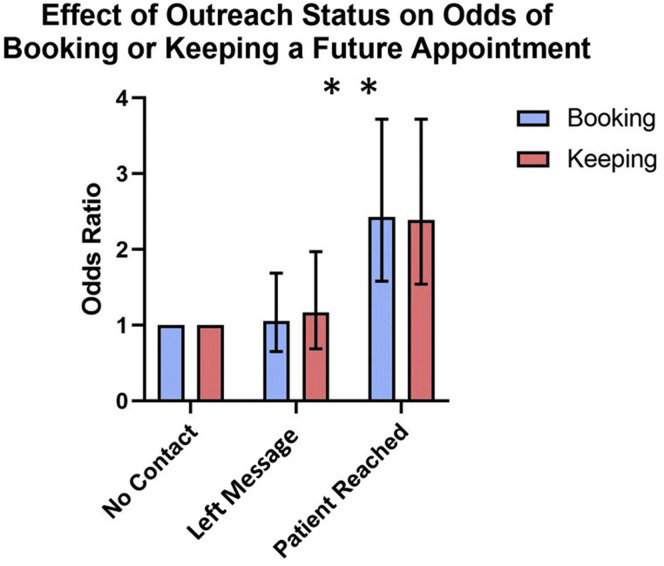
Overall, of the 787 patients who received the outreach intervention, 648 (82%) patients subsequently booked a visit. There was no significant difference in booking an appointment between those who were not contacted (76%) and those who were left a message (77%) (OR = 1.05, 95% CI [0.65-1.69], P = .84). In contrast, of the patients who were reached, 89% booked an appointment (OR = 2.43, 95% CI [1.58-3.72], P < .001] (Fig. 2 ). In a univariate analysis, older patients were found to be more likely to book an appointment (OR = 1.014, 95% CI [1.001-1.026] for each year of age, age range 18-99 years, P = .037). Portal messaging was the only other significant predictor of booking an appointment, with 86% of patients who received a portal message booking an appointment compared with 80% of those who did not (OR = 1.50, 95% CI [1.01-2.23], P = .045). Booking an appointment was significantly associated neither with receiving a telephone voicemail message nor with the patient’s sex, race or ethnicity, language spoken (English vs non-English), type of diabetes, insulin use, or the HbA1C level.
Fig. 2.
Odds of booking or keeping a future appointment based on outreach status. A diabetes nursing team attempted outreach for 787 patients after a canceled appointment for diabetes during 14 weeks of the COVID-19 pandemic. Outreach status (x-axis) was defined as reached (2-way communication between the clinician and patient via telephone or an electronic health record portal message), message left (1-way communication, eg, voicemail), or no contact. Outcomes were defined as booking an appointment and keeping the appointment after the outreach initiative and before October 31, 2020. Reached patients were significantly more likely to book (odds ratio = 2.43, 95% CI [1.58-3.72], P < .001) and keep (odds ratio = 2.39, 95% CI [1.54-3.72], P < .001) an appointment than no contact patients.
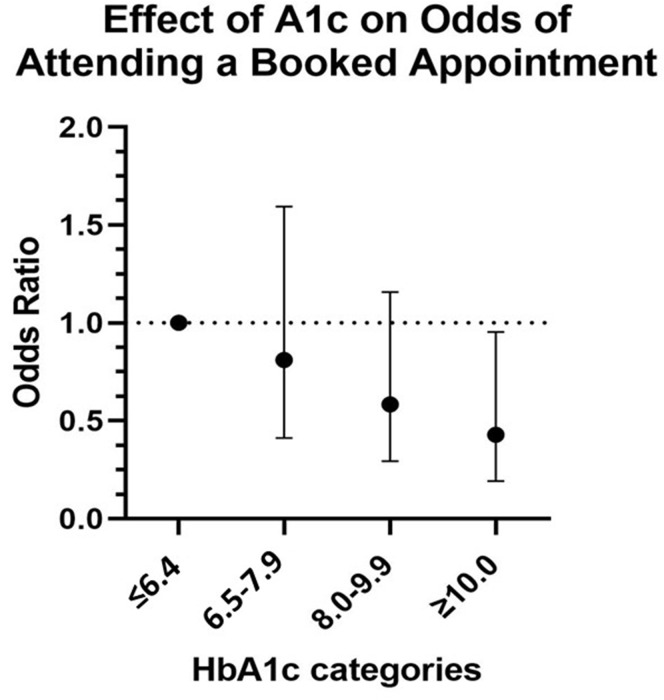
Of the 648 patients who booked an appointment, 519 (80%) patients kept their appointment. Similar to the booking outcome, there was no significant difference in keeping an appointment between those who were not contacted (72%) and those who were left a message (75%) (OR = 1.17, 95% CI [0.69-1.97], P = .568), whereas 86% of patients who were reached kept their appointment (OR = 2.39, 95% CI [1.54-3.72], P < .001). In a univariate analysis, patients on insulin were found to be more likely to keep their appointment (OR = 1.70, 95% CI [1.15-2.52], P = .008), whereas patients with a higher HbA1C level were less likely to keep their appointment (OR = 0.87, 95% CI [0.79-0.97] for each 1.0% increase in the HbA1C level, HbA1C range 4.7%-16.0% (28-151 mmol/mol), P = .011) (Fig. 3 ).
Fig. 3.
Effect of HbA1C on the odds of attending a booked appointment after the outreach intervention. Outreach was attempted for 787 patients who canceled an appointment for diabetes during the COVID-19 pandemic. Outcome was defined as booking and keeping an appointment after the outreach initiative. Patients with a higher HbA1C level were less likely to keep their appointment (odds ratio = 0.87 for each 1.0% increase in the HbA1C level, P for trend = .01). HbA1C is reported in quartiles of ≤6.4% (≤46 mmol/mol), 6.5% to 7.9% (48-63 mmol/mol), 8% to 9.9% (64-85 mmol/mol), and ≥10% (≥86 mmol/mol). HbA1C = hemoglobin A1C.
Discussion
Patient engagement and activation have been defined as the capability and willingness to participate in care. It has also been recognized that this relationship between providers and patients is shaped by the environment in which care is being delivered.23 , 24 During the SARS-CoV-2 pandemic, a major disruption of usual, in-person care took place worldwide, forcing both clinical programs and patients to disengage from routine care management. This natural experiment implemented a patient outreach initiative conducted during the pandemic at a single institution. We compared the impact of the outreach status on patient re-engagement while identifying other factors that might impact the intervention’s efficacy and found that patients who were left a message were no more likely to book or keep an appointment than patients who received no contact (Fig. 2). We also found that those with worse glycemic control and younger people were less likely to maintain care.
The primary result suggests that leaving a message is as ineffective as no contact perhaps because it does not sufficiently activate the patient. In support of this concept, the patients who were reached, ie, those who had an interaction with a clinician from the care team, were significantly more likely to book and keep their future appointment (Fig. 2). This suggests that 2-way communication with a patient is important for re-engagement after a significant care disruption. We also found that portal messaging had a significant impact on booking rates, whereas telephone contact did not, which might have been because the patient was able to request an appointment on the online portal where they were communicating with their provider.
The other factors that clearly influenced re-engagement included age, baseline HbA1C level, and insulin use. Older patients were more likely to book an appointment, with the likelihood increasing with each year of age. Patients on insulin were more likely to keep their appointment, perhaps to maintain prescriptions and dosing adjustments. In contrast, patients with a higher baseline HbA1C level were less likely to keep their appointment, with a linear reduction in likelihood with higher HbA1C level quartile ranges (Fig. 3). Several studies have reported male sex, younger age, not being on insulin, more complications, and poor control as being risk factors for patients becoming lost to follow-up in diabetes care.16 , 18 , 25 , 26 Importantly, the additional patient characteristics that were more frequent in the no-contact group than in the reached group included Black race (17.1% vs 11.9 %, respectively), Hispanic ethnicity (5.9% vs 3.6%, respectively), and Medicaid health insurance (12.6% vs 8.9%, respectively). Although not statistically significant, these differences are indicators that certain patient groups, namely ethnic minority groups and those with a lower socioeconomic status, are less likely to access bidirectional communication with clinic staff. For example, a small group of patients did not have a working telephone.
Our findings suggest that the COVID-19 pandemic created a period of heightened risk for patients already known to be at risk of disengaging from their diabetes care. It is well established that strong care engagement is vital for reaching goals and optimizing control.18 Patients who attend regular appointments are more likely to meet clinical targets, whereas patients who skip appointments are less likely to gain control and are more at risk of becoming lost to follow-up.14, 15, 16, 17 What follows is a vicious cycle of worsening glycemic control, continued disengagement, and, ultimately, poor outcomes. The period of care disruption during the COVID-19 pandemic allowed patients to fall into common patterns of disengagement. Although published guidelines mainly addressed inpatient care, chronic or routine care was overlooked, potentially creating a massive burden on the medical field for years to come.7 , 12 The findings of this study stress the importance of targeted outreach to patients who have known risk factors for disengagement during a major care disruption.
The consequences of disengagement without re-engagement for PWD extend far beyond the impact of poor glycemic control. The pandemic-induced moderate-to-severe psychologic effects included fear, anxiety, stress, and panic, as reported by surveyed patients and providers,3 , 4 , 27 which likely contributed to disengagement at a time when patients required targeted behavioral health treatment. Clinicians reported an increased incidence of diabetic ketoacidosis with a more severe presentation, emergent hypoglycemic episodes, and a missed or delayed diagnosis of acute-onset type 1 diabetes because of delayed care.3 , 6 Given that PWD are at higher risk of developing and dying from cancer, delayed cancer screenings might have an impact that will probably materialize in the next decade.11 It is also likely that PWD will be significantly impacted by backlogs in surgeries, particularly for foot or lower limb, cardiovascular, and musculoskeletal conditions.9
Although the current literature28 stresses on the importance of sustaining patient engagement, there is lack of guidance on how to achieve this goal during and after a dramatic care disruption such as a pandemic. Our results suggest that 2-way communication is important for patient re-engagement after an appointment cancelation. Not only does a response from the patient confirm that outreach was received, the action of participating in the communication might be a catalyst for the next action, which is booking another appointment. This action might serve as a reminder or a motivator to re-engage in care. Studies over the past 2 decades have found that a meaningful interpersonal exchange between a provider and patient can lead to patient activation, which increases the likelihood of the patient maintaining care and practicing self-management behaviors.25 , 29 , 30 When there is no communication between the provider and patient, the patient does not have the opportunity to be engaged or activated in their care and, thus, would be less likely to re-engage. The findings from this study suggest that targeted outreach for those at risk is necessary during disruptions to maintain continuity of care.
The reasons why certain patient groups are at higher risk of disengagement are likely complex and multidimensional; thus, identifying a single approach to maintaining engagement is difficult. As for the best practice, interpreters for those who do not speak English are important, as used in this study as part of standard care, but a more culturally aligned approach might be required to optimize re-engagement. For example, a large body of data from mostly observational studies generally supports the use of community health workers among some groups with chronic disease. In a recent single-center randomized clinical trial, a community health worker intervention reduced 30-day hospital readmissions of adult general medicine inpatients with at least 2 chronic conditions by nearly 50%, and intervention participants were also less likely to miss clinic appointments. Because hospitalizations often lead to disruptions in care, these results might be generalizable to other types of disruption.31
However, this initiative was time consuming for the clinical team, and the addition of complexity to the basic administrative functions of a clinic is often unwelcome. Therefore, the procedure outlined here might not be a sustainable approach for many practices. Future studies should investigate more sustainable approaches, such as culturally acceptable, patient-tailored short message service text messaging using a chat bot or a member of the clinical or administrative team. These findings can guide a priori planning, which will be vital for keeping patients and providers safe while also maintaining routine care throughout in future pandemics and outbreaks.
Because of the observational design of this study, there are several limitations. The designation of appointments being canceled because of the pandemic can be interpreted as subjective by researchers. Some cancelations, especially early in the intervention, were labeled with reasons that were clearly not pandemic-related; for example, the visit was rescheduled to another date or the appointment was booked erroneously. However, there were other appointments for which the reason had to be assumed because the specific cause was not listed. The number of cancelations due to the pandemic could have been inflated because of this.
Because this was not a randomized or protocol-led study, the outreach team might have had biases regarding who they attempted to contact on the list because we did not mandate a specific order of contact on the shared work list. This may have resulted in the patient population not being as random as assumed. Additionally, we did not examine whether different nurses had a differential impact on booking or keeping appointments. We do not know whether the nurse was known to the patient or whether patients interacting with someone known to them was more effective than them interacting with someone not known to them. Additionally, we do not know whether the administrative staff would have been as successful as the nursing team members.
We encouraged the nursing team to use both the internet-based portal and telephone outreach methods because the objective of the program was to try to reach the patient by whatever means necessary; however, this meant that the 2 variables could not be separated. Portal messaging was a significant predictor of booking an appointment, but that variable was a mix of the use of the portal alone and the use of the portal and telephone. It is impossible, based on these data, to determine the sole impact of outreach via the portal versus that via telephone.
In addition, it can be speculated that portal access might help identify patients who are more capable of navigating the challenges of virtual care and, thus, were more engaged by our standards. Additionally, although portal access might indicate that the patient can navigate these challenges, these data cannot be used to indicate which factor is more significant, access to the portal or the messaging outreach itself.
Finally, we were only able to report associations between the intervention and its outcome. We did not report causation, ie, the fact whether outreach caused the patients to book and keep their appointment.
Conclusions
In this observational study, we found that in a method designed to optimize engagement during a care disruption, 1-way communication was not better than no contact, and 2-way communication increased the likelihood of patient re-engagement. In addition, patients with a higher baseline HbA1C level were less likely to keep their appointments, whereas patients on insulin were more likely to re-engage. We concluded that although more complex patients (eg, patients with older age or those on insulin) might be more incentivized to remain engaged, patient-tailored, targeted outreach might be needed for those with chronically poor glycemic control, especially those who are unable to be contacted, because this group has a greater prevalence of highest-risk ethnic and socioeconomic groups. With the increasing use of telemedicine and mobile health tools, it is of great importance to redefine and support effective patient engagement. More research in this area is needed to confirm the best practice for programs to adopt in order to maintain continuity of care during major care disruptions with the goal of avoiding a larger health crisis of worsening chronic disease.
Acknowledgment
We acknowledge the tireless work of the BWH Diabetes Program nursing team (Charles K. McKitrick, MSN, RN, CDE; Colleen M. Smith, NP; Marina Donahue, NP; Kristen M. Fowler, NP; and Kayla L. Del Valle, NP) who provided reassurance and support to their patients during this pandemic. This study was presented at the American Diabetes Association 81st Scientific Sessions (2021) as a poster (849-P).
Disclosure
The authors have no multiplicity of interest to disclose.
Supplementary Materials
References
- 1.Li B., Yang J., Zhao F., et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beran D., Perone S.A., Perolini M.C., et al. Beyond the virus: ensuring continuity of care for people with diabetes during COVID-19. Prim Care Diabetes. 2021;15(1):16–17. doi: 10.1016/j.pcd.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elbarbary N.S., Santos T.J., Beaufort C., Agwu J.C., Calliari L.E., Scaramuzza A.E. COVID-19 outbreak and pediatric diabetes: perceptions of health care professionals worldwide. Pediatr Diabetes. 2020;21(7):1083–1092. doi: 10.1111/pedi.13084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joensen L.E., Madsen K.P., Holm L., et al. Diabetes and COVID-19: psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark—what characterizes people with high levels of COVID-19-related worries? Diabetes Med. 2020;37(7):1146–1154. doi: 10.1111/dme.14319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Archived: who timeline - covid-19. https://www.who.int/news/item/27-04-2020-who-timeline---covid-19 Accessed March 19, 2021.
- 6.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369 doi: 10.1136/bmj.m1401. m1401. https://doi.org/10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 8.Mantica G., Riccardi N., Terrone C., Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020;183(June):40–41. doi: 10.1016/j.puhe.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVIDSurg Collaborative Elective surgery cancelations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M. Elective surgery in the time of COVID-19. Am J Surg. 2020;219(6):900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maringe C., Spicer J., Morris M., et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen-See S. Disruption of cancer care in Canada during COVID-19. Lancet Oncol. 2020;21(8):e374. doi: 10.1016/S1470-2045(20)30397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loeb A.E., Rao S.S., Ficke J.R., Morris C.D., Riley L.H., Levin A.S. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pantalone K.M., Misra-Hebert A.D., Hobbs T.M., et al. The probability of a1c goal attainment in patients with uncontrolled type 2 diabetes in a large integrated delivery system: a prediction model. Diabetes Care. 2020;43(8):1910–1919. doi: 10.2337/dc19-0968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Archibald L.K., Gill G.V. Diabetic clinic defaulters—who are they and why do they default? Pract Diabetes Int. 1992;9(1):13–14. [Google Scholar]
- 16.Griffin S.J. Lost to follow-up: the problem of defaulters from diabetes clinics. Diabetes Med. 1998;15(suppl 3):S14–S24. doi: 10.1002/(sici)1096-9136(1998110)15:3+<s14::aid-dia725>3.3.co;2-9. [DOI] [PubMed] [Google Scholar]
- 17.Jacobson A.M., Adler A.G., Derby L., Anderson B.J., Wolfsdorf J.I. Clinic attendance and glycemic control: study of contrasting groups of patients with IDDM. Diabetes Care. 1991;14(7):599–601. doi: 10.2337/diacare.14.7.599. [DOI] [PubMed] [Google Scholar]
- 18.Tino S., Wekesa C., Kamacooko O., et al. Predictors of loss to follow up among patients with type 2 diabetes mellitus attending a private not for profit urban diabetes clinic in Uganda—a descriptive retrospective study. BMC Health Serv Res. 2019;19(1):598. doi: 10.1186/s12913-019-4415-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fonseca V.A., Smith H., Kuhadiya N., et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632–1638. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ekperi L., Thomas E., LeBlanc T.T., et al. The impact of Hurricane Sandy on HIV testing rates: an interrupted time series analysis, January 1, 2011‒December 31, 2013. PLoS Curr. 2018;10(Sep 13) doi: 10.1371/currents.dis.ea09f9573dc292951b7eb0cf9f395003. ecurrents.dis.ea09f9573dc292951b7eb0cf9f395003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiménez-Mangual B.C., Cuevas-Acevedo D.M., Quiles-Alves N., Rodríguez-Nazario I., Melin K.R. Description of patients medications needs and the community pharmacist’s role in Puerto Rico following a natural disaster. J Prim Care Community Health. 2019;10(Jan-Dec) doi: 10.1177/2150132719842701. 215013271984270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nasef N., O’Brien K., Wylie L., Unger S. Lessons from SARS: a retrospective study of outpatient care during an infectious disease outbreak. BMC Pediatr. 2010;10(1):1–6. doi: 10.1186/1471-2431-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hibbard J., Greene J. What the evidence showes about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff. 2013;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 24.Higgins T., Larson E., Schnall R. Unraveling the meaning of patient engagement: a concept analysis. Patient Educ Couns. 2017;100(1):30–36. doi: 10.1016/j.pec.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 25.Lee R., Samsudin M., Thirumoorthy T., Low L., Kwan Y. Factors affecting follow-up non-attendance in patients with type 2 diabetes mellitus and hypertension: a systematic review. Singapore Med J. 2019;60(5):216–223. doi: 10.11622/smedj.2019042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chew B.H., Lee P.Y., Shariff-Ghazali S., Cheong A.T., Ismail M., Taher S.W. Predictive factors of follow-up non-attendance and mortality among adults with type 2 diabetes mellitus—an analysis of the Malaysian diabetes registry 2009. Curr Diabetes Rev. 2015;11(2):122–131. doi: 10.2174/1573399811666150115105206. [DOI] [PubMed] [Google Scholar]
- 27.Wang C., Pan R., Wan X., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lyles C.R., Nelson E.C., Frampton S., Dykes P.C., Cemballi A.G., Sarkar U. Using electronic health record portals to improve patient engagement: research priorities and best practices. Ann Intern Med. 2020;172(11Suppl):S123–S129. doi: 10.7326/M19-0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Almutairi N., Hosseinzadeh H., Gopaldasani V. The effectiveness of patient activation intervention on type 2 diabetes mellitus glycemic control and self-management behaviors: a systematic review of RCTs. Prim Care Diabetes. 2020;14(1):12–20. doi: 10.1016/j.pcd.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 30.Riedl D., Schüßler G. The influence of doctor-patient communication on health outcomes: a systematic review. Z Psychosom Med Psychother. 2017;63(2):131–150. doi: 10.13109/zptm.2017.63.2.131. [DOI] [PubMed] [Google Scholar]
- 31.Carter J., Hassan S., Walton A., Yu L., Donelan K., Thorndike A.N. Effect of community health workers on 30-day hospital readmissions in an accountable care organization population: a randomized clinical trial. JAMA Netw Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.10936. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.