Abstract
One of the most important developing cell types in any biological system is the gamete (sperm and egg). The transmission of phenotypes and optimally adapted physiology to subsequent generations is in large part controlled by gametogenesis. In contrast to genetics, the environment actively regulates epigenetics to impact the physiology and phenotype of cellular and biological systems. The integration of epigenetics and genetics is critical for all developmental biology systems at the cellular and organism level. The current review is focused on the role of epigenetics during gametogenesis for both the spermatogenesis system in the male and oogenesis system in the female. The developmental stages from the initial primordial germ cell through gametogenesis to the mature sperm and egg are presented. How environmental factors can influence the epigenetics of gametogenesis to impact the epigenetic transgenerational inheritance of phenotypic and physiological change in subsequent generations is reviewed.
Keywords: Gametogenesis, Spermatogenesis, Oogenesis, PGCs, Epigenetics, Transgenerational, Review
How environmental factors can influence the epigenetics of gametogenesis to impact the epigenetic transgenerational inheritance of phenotypic and physiological change in subsequent generations is reviewed.
Introduction
The germ line is an enduring link between all generations of a species. After the fertilization of the oocyte by the sperm, a totipotent zygote will give rise to all cell lineages of the organism, including the germ line itself. The primordial germ cells (PGCs) are the precursor pluripotent stem cells for the sperm and egg. They are established during the perigastrulation epiblast stage of the mammalian embryo. The PGCs specification is regulated by a unique and complex gene network induced by signals from extra-embryonic tissues [1]. In the gonads, these PGCs will differentiate into the male prospermatogonia or female oogonia in response to Sertoli or granulosa cell signaling. The prospermatogonia continue in the gametogenesis process and undergo spermatogenesis to develop into the mature sperm. The oogonia continue into the gametogenesis process and undergo oogenesis to develop into the mature oocyte. Therefore, gametogenesis can be seen as a crucial first step for the perpetuation of the mammalian life cycle [2].
The crucial aspect of gametogenesis is the production of genetically and epigenetically competent gametes, which are necessary for normal fertilization and the organism’s development. Epigenetics is defined as the factors and processes around DNA that require genome activity independent of DNA sequence, and are mitotically stable. The components include DNA methylation, histone modifications, and non-coding RNA chromatin structure that regulate gene activity independent of DNA sequence [3]. Maternal and paternal gametes display genomic imprinted differences due to DNA methylation and other epigenetic modifications established in the germ line during gametogenesis, but this is only a small component of the epigenome and its regulation of biology.
Interestingly, previous studies have shown that epigenetic modifications can occur during gametogenesis under the influence of environmental factors (stress, diet, pollutants, etc.), which can lead to phenotypical defects in the individuals exposed and in the subsequent generations through the germline. This non-genetic form of inheritance is termed epigenetic transgenerational inheritance and is mediated through epigenetic alterations (i.e. epimutations) in the sperm or egg.
The current review presents the molecular basis of germ cell development (i.e. gametogenesis), and also how the environment can induce stable epimutations and modified phenotypes through the transgenerational inheritance phenomenon.
Mammalian gametogenesis and primordial germ cell development
Primordial germ cell specification
The totipotent stem cells derived from the zygote are the product of fertilization of the oocyte by the sperm, which gives rise to all cell lineages of an organism, and the germline itself. Thus, the specification of primordial germ cells (PGCs) is a pivotal first step for the acquisition of the germline pluripotent cell and the continuation of the mammalian life cycle [1]. In metazoans, two different processes form the germline in the male and female, giving rise to sperm and oocytes. Caenorhabditis elegans and Drosophila melanogaster have been used to describe the mechanism for PGC specification in invertebrates, and Zebrafish and Xenopus in non-mammalian vertebrates [4–7]. At the onset of development, preformation of germ plasm segregates the germ and the soma. The germ plasm is comprised of RNA, proteins, and organelles that are grouped in a specific location within the oocytes, then allocated to a few cells in the germline of the developing embryo [8]. In this instance, the germline is always differentiated from somatic cells across generations. Alternatively, in mammals, the germline is induced within a population of pluripotent cells. The ectopic expression of germline genes in the soma can be tumorigenic [9], however, specification failure in the germline is a reproductive dead end. This specification process requires a precise orchestration to ensure a timely restriction from the soma. Somatic cells not allocated to the germline will undergo differentiation and perish, whereas the germline has the ability of establishing a new organism in the next generation [10]. The primordial germ cells are specified during early embryonic development. Bone morphogenic protein (BMP) signaling is indispensable for PGC specification, and targeted disruption of Bmp2, Bmp4, Bmp8b, or BMP signaling transducers Smad1, Smad4, Smad5 or Alk2, all demonstrate loss or reduced numbers of PGC [11–16].
The first phase of gametogenesis happens in early embryogenesis, during the formation and migration of PGCs into the gonadal ridge [17, 18]. Mouse models have been primarily used to study the mammalian germ cell development. In the early post-implantation embryo epiblast, PGCs specification is initiated. At mouse embryonic day E6.25 in some pluripotent epiblast cells, bone morphogenetic protein (BMP) and WNT signals from extra-embryonic tissues to induce the expression of a key regulator of PGC fate: the PR domain zinc-finger protein 1 (PRDM1, also known as BLIMP1) [2, 19]. Two other factors are upregulated next, PRDM14 and the transcription factor AP2γ (encoded by Tfap2c) [20, 21]. The germ cell fate is then induced by the transcription factor network formed by PRDM1, PRDM14, and AP2γ [22–24]. This tripartite network suppresses somatic gene expression such as Hoxa1, Hoxb1, Lim1, Evx1, Fgf8, and Snail genes, while initiating the germ cell transcriptional program but also setting off a genome-wide epigenetic reprogramming [13, 20, 22, 25–28]. Interestingly, Blimp1 and Prdm14 have distinct binding patterns relative to promoters, whereas Blimp1 is important for the repression of almost all genes usually downregulated in PGCs, as well as for the restoration of pluripotency and epigenetic reprogramming (Figure 1) [29]. The restoration of pluripotency and epigenetic reprogramming are regulated by Prdm14, independently from Blimp1, that defines a novel genetic pathway with strict specificity to the germ cell lineage [30]. In mice, the knockout (KO) of Blimp1, Prdm14, or Ap2γ result in PGCs specification defects highlighting the fact that these three factors are dominant coordinators of the transcriptional program for the establishment of the germ cell fate. In addition, the concomitant overexpression of these three factors in cells in vitro induces mouse germ cell formation in the absence of cytokines [22] shows again the importance of these three transcription factors. After embryonic day 7 (E7) in the mouse, the PGCs are then specified and express PGC-characteristic markers, such as stage-specific embryonic antigen 1 (SSEA1) or developmental pluripotency associated 3 (DPPA3 or STELLA) [31–34]. The expression of several pluripotent genes is also maintained in the PGCs such as Nanog, Oct4 and SRY (sex-determining region-Y) [35–38]. Sybirna and collaborators recently revealed a crucial role for PRDM14 in human germ cell fate, where a loss of function affects the efficiency of specification and results in an aberrant hPGCLC transcriptome. Moreover, their study showed that PRDM14 targets are not conserved between mouse and human, which highlights the evolutionary divergence in the molecular network for PGC specification [39].
Figure 1 .
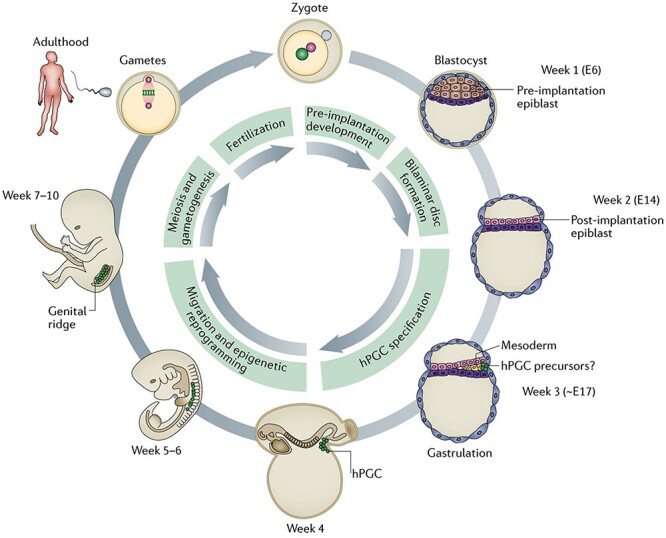
Human germline development. Just after fertilization, a zygote is formed. At week 1, the blastocyst develops and contains pluripotent epiblast cells, which will give rise to all lineages in the embryo, including the germ line. At week 2, the blastocyst implants into the uterine wall. The human primordial germ cells (hPGCs) are probably specified around the time of gastrulation around week 3. At week 4, the hPGCs are localized near the yolk sac wall close to the allantois. After that stage, the hPGCs migrate through the hindgut to the developing genital ridges. At this developmental stage, the migrating hPGCs go through a genome-wide epigenetic reprogramming, including global DNA demethylation, to erase imprints and other somatic epigenetic marks. During the fetus development and adult life, the germ line will undergo meiosis and gametogenesis to differentiate into sperm and eggs. At the same time, the genome is remethylated and acquires appropriate epigenetic signatures for the generation of a totipotent zygote upon fertilization (modified from [1]).
Although, most studies have been conducted in mice, recent findings in non-rodent mammals have highlighted the similarities and differences between species. In humans, the PGC formation occurs in the third week of gestation. In vitro studies of human PGCs have shown that these cells originate from mesodermal precursor cells, and BMP and WNT signaling pathways are also essential for specification [1, 40, 41]. In contrast to mice, human PGCs lack Sox2 expression. Therefore, the species differences between human and mice PGC transcriptional network may be explained by the differences in either pluripotency circuitry or embryonic origin [40].
Primordial germ cell migration
Just after their specification, between E7.5 and E10.5, while proliferating the PGCs migrate through the hindgut and genital ridge then into the developing gonads to differentiate into gametes [27, 42, 43]. Two germ cell–soma signaling pathways cKIT-STEEL and SDF-CXCR4 are required for the normal migration of PGCs. In mice, germ cells express c-KIT, whereas STEEL is expressed in the somatic cells lining the route to the gonad. The interaction between c-KIT and STEEL is fundamental for PGC proliferation, survival, and migration from the primitive streak to the genital ridge [44–48]. Sterility because of a lack of spermatogonial stem cells and thus differentiated germ cells has been observed in homozygous cKit and Steel mutant mice [46, 49–51]. The chemoattractant stromal cell-derived factor 1 (SDF-1) expressed at the genital ridges in the surrounding mesenchyme also facilitates the directional PGC migration. SDF-1 is detected by its receptor C-X-C chemokine receptor type 4 (CXCR4) expressed on the surface of PGCs [47]. A knockdown of the activity of CXCR4b and of the SDF-1a ligand has been shown to result in severe PGC migration defects such as very few PGCs reaching the genital ridge [52]. Alternatively, the migration of PGCs can be redirected toward sites of ectopically expressed SDF-1a [52–54]. This ectopic expression of SDF-1 can account for the development of some extra-gonadal cell tumors in humans [27].
During their migration, PGCs continue to proliferate and reach 500 cells in each fetal gonad at E10.5 in the mouse [55]. At this stage, the PGC differentiate into oogonia in females or gonocytes (i.e. prospermatogonia) in males. To form germline cysts, between E10.5 and E14.5, the fetal germ cells undergo five additional mitotic divisions with incomplete cytokinesis [56]. These cysts cluster together and will form germ cell nests in both female and male fetal gonads [55–57]. These germ cell nests will then resolve and generate the primary oocytes or prospermatogonia in the differentiated female and male gonads, respectively.
Primordial germ cells and epigenetics
DNA methylation
The first DNA methylation erasure period is incomplete and happens in the early embryo, leaving paternally and maternally imprinted genes intact and in all somatic lineages subsequently derived. The second DNA methylation erasure period is more comprehensive and occurs during the germline specification. The function of the DNA methylation erasure is to generate in the case of the embryo a totipotent stem cell population, and for PGCs a pluripotent stem cell population. However, despite these two epigenetic methylation erasure processes, epigenetic information can be passed down to the offspring, similar to imprinted genes, even though the mechanisms behind this process remain to be elucidated (Figure 2).
Figure 2 .
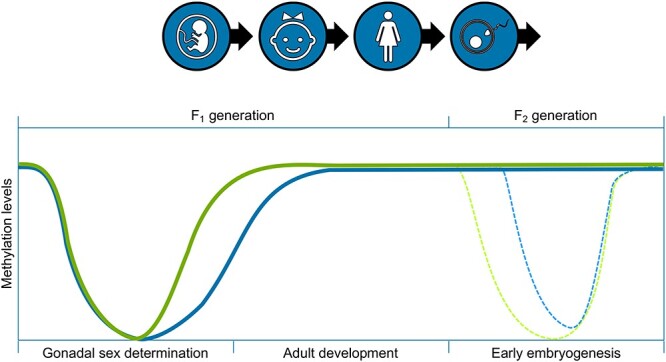
Epigenetic reprogramming (DNA methylation erasure) during primordial germ cell development at gonadal sex determination and following fertilization in the early embryo (modified from [283]).
Upon specification, during the rapid proliferation of PGCs, the first DNA methylation erasure happens and consists of a passive DNA methylation between E6.5 and E10.5 in the mouse, which results from repressing de novo DNA methyltransferases DNMT3a/b [58–62]. Still, the maintenance of DNA methyltransferase 1 (DNMT1) prevents the dilution of DNA methylation modifications on parentally imprinted regions and meiotic gene promoters [63]. Moreover, a loss of Dnmt1 in PGCs results in a premature meiotic entry in females and precocious differentiation in prospermatogonia in males, and causes infertility [63].
Further demethylation erasure takes place between E10.5 and E12.5 in the mouse, while the PGCs migrate to the genital ridge and begin sex determination. At this period, DNA methylation is at its lowest level due to enzymatic activity from TET1 and TET2 removing DNA methylation [64–66]. During this DNA demethylation erasure window, the maternally and paternally imprinted loci and resistant promoter regions are erased [65, 67]. Interestingly, several studies have demonstrated that a loss of TET1 and 2 in the germ cells does not impact infertility, and few loci showed altered epigenetic states [65, 68–70]. Despite the near complete DNA demethylation erasure process, some genome loci remain methylated in human and mouse PGCs and are referred as ‘escapees’ [58, 64, 71, 72]. In both species, these escapees have been shown to be associated with retrotransposable elements [58, 64, 71–73], subtelomeric regions [71] and pericentrometric satellite repeats [72] also display these escapees.
The PGCs extensive epigenetic reprogramming includes a genome-wide loss of approximately 90% of 5-methylcytosine (5mC) [58, 64, 65, 68, 71, 74–77]. Even though the underlying molecular mechanisms of this process have until recently remained unclear, a set of germline reprogramming responsive (GRR) genes is crucial for the correct progression of PGC development and gametogenesis. These genes show unique promoter sequence characteristics, with high levels of both 5mC and 5-hydroxymethylcytosine (5hmC). These genes are targets of TET1, the ten eleven translocation (TET) enzymes, which oxidize 5mCs and promote locus-specific reversal of DNA methylation [78]. The PRC1 is the canonical polycomb repressive complex PRC1, which promotes compact local chromatin structures and longer-range chromatin interactions [79]. The loss of DNA methylation combined with PRC1 repression is uniquely required for GRR gene activation. In this epigenetically poised state, TET1 is required to potentiate a full and efficient activation. TET1 seems to be especially important in female PGCs [68], since they start meiotic prophase soon after completion of epigenetic reprogramming, thus requiring the timely expression of these genes. A slight hypermethylation at GRR gene promoters in the mouse E14.5 Tet1−/− PGCs, Hill and collaborators also demonstrate that TET1 stimulates transcription of GRR genes via a DNA demethylation-independent mechanism [80, 81]. In addition, TET1 may also enhance transcription through regulation of the levels of 5mC and 5hmC at non-promoter cis-active elements, such as enhancers [79]. TET1 might also have a critical role in the subsequent removal of aberrant residual and/or de novo DNA methylation [79]. This suggests that global reprogramming events require efficient protection from de novo DNA methylation to stabilize the newly acquired epigenetic state after the removal of 5mC. PGC epigenetic reprogramming entails complex erasure of epigenetic information and suggests that to enable gametogenesis, a timely and efficient activation of GRR genes is required [79].
Usually, a loss of DNA methylation in somatic cells induces an ectopic expression of retrotransposons, an anarchic proliferation, and apoptosis [82]. However, PGCs develop normally despite this hypomethylated state. The hypothesis is that the chromatin reorganization could enhance the genome stability and ensure proper chromosome alignment and segregation during mitosis, as well as global transcriptional quiescence during this developmental period [25, 58, 64, 71, 74, 83]. Studies in different models have shown that this process seem to be conserved in multiple species. Experiments with human PGCs have found that these DNA demethylation events follow the same patterns as the ones found in the rodents [72, 73, 84].
Histone marks
In a murine model, before the DNA methylation erasure, the pre-migratory PGCs start a process of reprogramming that erases epigenetic marks. One of the central epigenetic changes in pre-migratory and early migratory mouse PGCs is the loss of H3K9me2. This event is followed by an accumulation of H3K27me3 signal [74, 83, 85]. Eguizabal and collaborators showed in early human gonadal PGCs similar chromatin changes in the human early developing germ line [86]. An erasure of genomic imprints and dynamic changes in chromatin modifications are observed in the mouse PGCs after their entry in the genital ridge [74]. After week 9 of gestation, and similarly to porcine PGCs, human PGCs lose H3K27me3 [86].
Spermatogenesis & spermiogenesis
Male fertility relies on the production by the testis of large numbers of normal spermatozoa. This process is known as spermatogenesis, which can be divided in three major steps: (i) mitosis with the multiplication of the spermatogonia, (ii) meiosis to reduce the number of chromosomes from diploid to haploid cells, which starts with type B spermatogonia into the prophase of the first meiotic division. The cells are then called primary spermatocytes that then divide to form secondary spermatocytes, which will divide and undergo meiosis to form the round spermatids, (iii) and finally, the spermiogenesis, which refers to the successful maturation of round spermatids into spermatozoa [87]. All of these steps are central in the spermatogenic process, and any defect during the spermatogenesis can result in the reduction or absence of sperm production, or production of abnormal sperm (Figure 3).
Figure 3 .
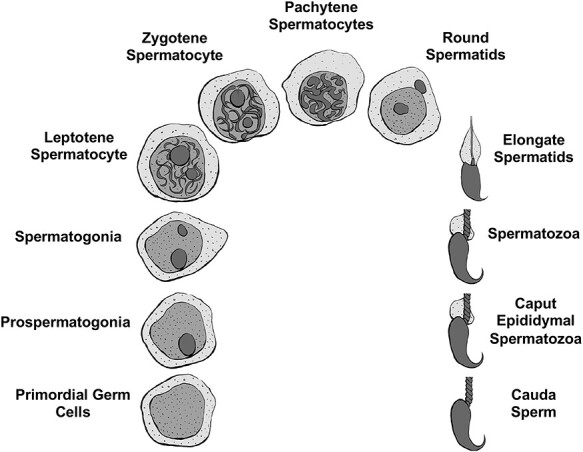
Gametogenesis and spermatogenic germ cell stages (modified from [162]).
Endocrine and paracrine regulation
FSH
Many studies in the rat have defined the stages at which testosterone and follicle stimulating hormone (FSH) act during spermatogenesis. The general consensus, until the mid-1990s, was that FSH was paramount for the initiation of spermatogenesis, but its role in the adult was to maintain a normal quantitative germ cell production [88, 89]. However, the study of transgenic mice lacking FSH or its receptor (FSHR) showed that the males were fertile but with a reduced germ cell number [90–94]. Closer observations of these KO mice revealed a reduction in spermatogonia, spermatocytes, and spermatids numbers, which suggests that FSH increases the number of spermatogonia and facilitates their entry into meiosis [90–94]. However, studies on hpg. SCARKO (hypogonadal mice lacking gonadotrophins and intratesticular androgen crossed with mice lacking androgen receptors specifically on the Sertoli cells) or hpg. ARKO mice (hypogonadal mice lacking gonadotrophins and intratesticular androgen crossed with mice lacking androgen receptors ubiquitously) have shown that FSH does not induce round spermatid formation [95–98].
While a lack of FSH action has been shown to impact spermatogenesis, it is difficult to determine the role of this hormone on maintaining this process. This is explained by the fact that FSH or its receptor are missing from the start of reproductive development. During normal adult spermatogenesis, apoptosis is a sporadic event, occurring mainly among spermatogonia. Lack of FSH, before sexual maturity and during the first wave of spermatogenesis, which is accompanied by an outburst of focal apoptosis among germ cells, increases the level of cells dying which may impact the adult spermatogenesis [99]. Other studies in rats have suggested that FSH-treatment acts to increase spermatogonia and spermatocyte numbers but displays a limited or incomplete effect on spermatogenesis [100, 101]. While these findings mostly agree with the data with the FSHRKO mice, there are significant differences. In these two studies, it was proposed that FSH could promote the completion of meiosis in rats, which was not observed in the transgenic mice models [101, 102]. The mechanism of action of FSH remains unclear even though FSH can act indirectly through Sertoli cells to increase spermatogonial differentiation/proliferation, but also modify rates of germ cell apoptosis [103–107]. A further role for FSH in the testis might be maintenance of Sertoli cell water balance as an accumulation of fluid was observed in FSHRKO mice cells [108]. As a result, this can alter cell morphology and interactions between germ cells and Sertoli cells, thus could reduce normal spermatogenic efficiency.
Androgen
Androgen plays an essential role in development and maintenance of spermatogenesis, which has been emphasized by a study demonstrating that the precocious expression of androgen receptors (ARs) in Sertoli cells leads to premature spermatogenic cell development [109]. The role of androgens has been clearly demonstrated in any animal model in which androgen levels are reduced, such as through hypophysectomy, GnRH-treatment (agonist or antagonist), ethanedimethane sulfonate treatment (EDS) (which ablates Leydig cells), or in gonadotrophin-deficient mice. In all of these cases, significant loss of pachytene spermatocytes and round spermatids, especially at stages VII and VIII of spermatogenesis, can be reversed by a treatment with testosterone [98, 110–117]. Moreover, in mice lacking functional androgen receptors (tfm or ARKO), there is a significant loss of spermatocytes which are also unable to complete meiosis and form round spermatids [118–121]. Androgen maintains indirectly through the Sertoli cells meiosis, which appears to ensure the survival of pachytene spermatocytes and enable diplotene spermatocytes to enter meiotic division [121]. However, the role of androgens in spermiogenesis and spermiation remains unclear in regard to its role on the germ cell niche. Most testis cell types express androgen receptors, except the germ cells. Several studies have concluded that androgen action in the testis is only mediated through somatic cell populations [107, 122, 123].
Estrogen
The physiological role of estrogens in the adult testis has yet to be completely understood. However, some studies suggest that estrogen action is required in the neonate to enable a normal spermatogenesis in adulthood. Estrogen has multiple indirect effects through endocrine regulation and through other tissues on the testis, which makes the study of its action even more difficult. In the adult hpg mouse, estrogens stimulate spermatogenesis by actually stimulating the FSH release from the pituitary [124, 125]. Interestingly, exogenous estrogens inhibit spermatogenesis in normal adult animals by inhibiting LH secretion and intratesticular testosterone levels [126]. In some species, the aromatase activity present in the testis can convert androgens to estrogens, such as the horse testes, which produce large concentrations of estrogens [127, 128]. Several cell types in the testis, including the germ cells, express nuclear estrogen receptors (ERα and ERβ), and the membrane cell receptor GPR30 [129, 130]. In ArKO mice (lacking aromatase), the males are initially fertile, but spermatogenesis degenerates and an arrest is observed in the early stages of spermiogenesis and multinucleated cells in the tubular lumen appear [131]. Moreover, during neonatal period, estrogen-dependent ERα signaling is required for a normal adult spermatogenesis and fertility [132].
Spermiogenesis seems to be clearly affected by estrogens. In fact, after irradiation damage to the testis, estrogens are able to stimulate spermatogonial differentiation [133, 134], which is not correlated to intratesticular testosterone suppression [135]. Numerous studies have shown that estrogens are involved in the early development of spermatogenesis and are able to affect spermatogenesis. However, their role in the normal adult spermatogenesis still needs to be determined.
Activin
The majority of testicular cell types produce activins and activin-related proteins [136]. Even though they can act as hormones, they also behave as growth factors in regard to spermatogenesis. Sertoli cells and germ cells express activin receptors [136]. Culture of stem spermatogonia cells, spermatogonia and spermatocytes has shown that these cells are sensitive to activin [137–139]. Follistatin (FST) and follistatin-like 3 (FSTL3) are two activin-binding proteins that can act as antagonists to activin activity. However, overexpression of FST does not reduce local activin levels but causes infertility without clear effects on FSH levels [140]. In KO mice for FSLT3, an increase in germ cell numbers was observed which was correlated to the increase in Sertoli cell numbers [141]. These different findings suggest that activins have probably a regulatory role in maintaining spermatogenesis and ensuring normal Sertoli cell development and activity.
Spermatogonial formation and renewal
In the mammalian testis, once the primordial germ cells migrate there during fetal development, they associate themselves with the mesenchymal cells, which will later give rise to the Sertoli cells. At this point, the sex cords are formed. The primordial germ cells then differentiate into prospermatogonia and remain centrally positioned in the cords surrounded by immature Sertoli cells. After a period of proliferation, postnatal in the rodent and prenatal in the human, the prospermatogonia migrate to the basement membrane of the sex cords to divide and form type A spermatogonia (Figure 3). Depending on the species, differences have been reported. In the human, A pale, A dark, and B spermatogonia types have been identified [142]. In the rodent testis, multiple type A spermatogonia, intermediate and type B spermatogonia have been reported and their appearance in the testis is temporally controlled. In the rat, around postnatal day 4 or 5, spermatogonial proliferation begins with type B spermatogonia identified at P6. After a series of mitotic divisions, whose mechanisms are only starting to be understood, during puberty the type B spermatogonia develop the capacity to develop into the preleptotene stage of the meiotic process.
In the testis, the migration of primordial germ cells depends on their surface expression of c-kit protein, which is the receptor for stem cell factor (SCF), produced by the immature Sertoli cells. Mutations of the c-kit receptor will result in failure of spermatogenesis due to the absence of germ cells from the testis [143]. An upregulation of SCF mRNA on E5 has been and is concurrent with the beginning of spermatogonial division [144], which indicates an interaction between c-kit and SCF to mediate and modulate spermatogonial proliferation. Other essential growth factors in the fetus testis include transferring growth factor alpha (TGFα) [145] and neurotrophic factors [146].
SCF and c-kit have also been shown to regulate the adult testis survival of spermatogonia and spermatocytes [147]. Rat tubules cultures with FSH have been shown to influence germ cell apoptosis, affecting both mitotic and meiotic cell populations [106, 148]. GDNF and CSF1 signaling are important for spermatogonial stem cell renewal in the stem cell niche [149, 150]. Survival and developmental progression of spermatogonia depend upon expression of several genes, including the transcription factor ID4 [151] and the RNA binding protein NANOS2 [152]. Different sub-populations of spermatogonial stem cells express different genes, depending on whether that population is undergoing self-renewal, differentiation and progression, or replenishment of earlier stem cell stages [153, 154].
Spermatogenic stage germ cell development and epigenetics
Many studies have shown that the dynamics of epigenetic modifications and their regulatory networks are essential for normal spermatogenesis. Any perturbations of these epigenetic modifications is likely to cause degrees of infertility and these perturbations could result in phenotypic defects in subsequent generations [3, 155–157]. Two studies have shown that a high fat or low protein in male mice can alter the metabolic gene expression in the offspring mediated by small noncoding RNAs (sncRNAs) derived from transition ncRNAs [158, 159]. Abnormal DNA methylation is associated with altered histone modifications, dysregulation of ncRNA, abnormal protamination, and all of these contribute to male infertility. In the prospermatogonia, prepachytene piRNAs are necessary for silencing mobile elements through guiding the de novo DNA methylations of transposable elements in order to guarantee genome stability [160]. In late spermatocytes and round spermatids, the pachytene piRNAs could silence the retrotransposon sequences through degrading the 3′UTR of retrotransposon mRNAs or recruiting the DNMT3L to the retrotransposon locus [161]. Most studies on the different spermatogenesis stages have focused on one type of cells. In the field of infertility, histone modifications are mostly studied in the mature sperm. Our lab investigated the developmental alterations in DNA methylation during gametogenesis from PGCs to sperm. Rat fetal PGCs, prospermatogonia, spermatogonia, meiotic pachytene spermatocytes, haploid round spermatids, caput spermatozoa and mature cauda sperm were isolated and purified. Differential DNA methylation regions between each developmental stage involved were compared. The study identified a dynamic cascade of epigenetic changes during development, the most dramatic happening during the early developmental stages, which suggests complex alterations to regulate genome biology and gene expression during gametogenesis [162].
Epididymal maturation and epigenetics
Although spermatogenesis is complete with the formation of the spermatozoa following spermatogenesis, additional maturation of the sperm occurs in the epididymis [163–166]. The spermatozoa released into the seminiferous tubules collect in the rete testes and pass through the efferent ducts into the head of the epididymis called the caput epididymis. The spermatozoa in the caput epididymis go through a further maturation as it passes through the caput to the corpus epididymis and finally, to the cauda epididymis. The caput epididymis spermatozoa do not have the capacity to have motility [167, 168]. During the transit through the epididymis, the epididymal epithelial cells produce proteins that are acquired and modify the maturation of the sperm to then in the cauda epididymis gain the capacity to become motile following ejaculation from the vas deferens where sperm are collected following epididymal maturation and stored. Therefore, the caput spermatozoa undergo a final stage of maturation during epididymal transit to the cauda epididymis to mature and gain the capacity to develop motility. The cauda epididymal sperm are then stored in the vas deferens. The molecular level maturation remains to be fully elucidated, but some aspects of epididymal maturation are known [169, 170].
Epigenetic alterations during epididymal maturation of the sperm largely remain to be elucidated [171]. Although the sperm nuclei is transcriptionally silent due to the compaction of DNA with protamines in testicular spermatogenesis, protein and epididymal components like ncRNA can be passed to the sperm and localized in the head of the sperm in the acrosome vesicle [171]. The localization of epigenetic components like ncRNA in the sperm nuclei remains to be established, but has been speculated in previous literature [172, 173]. Therefore, the role of epididymal ncRNA for sperm epididymal maturation requires further research, but is potentially an important epigenetic aspect of sperm maturation to consider [174].
Recent studies have investigated the epigenetic alterations between the caput epididymal spermatozoa and the mature cauda epididymal sperm. Environmentally induced (DDT and vinclozolin) epigenetic alterations in sperm have been shown to alter differential DNA methylation regions (DMRs) between the caput and cauda epididymal stage sperm [175, 176]. In addition, analysis of histone retention sites in the caput spermatozoa versus cauda sperm have shown differential histone retention regions (DHRs) [177]. Therefore, during epididymal maturation of sperm, there are DNA methylation and histone retention alterations that occur and are a further epigenetic developmental aspect of gamete development.
Oogenesis
Oogenesis involves the production of female gametes called eggs, and begins with the differentiation of primordial germ cells into oogonia at the period of sex determination [178]. In mammals, oogonia proliferate mitotically during fetal life to form a pool of primary oocytes that arrest in the prophase stage of the first meiotic division and stay in this state of meiotic arrest until the female reaches adulthood [179]. In the developing embryo, the nests of arrested oogonia are surrounded by somatic pre-granulosa cells [180]. Interaction and communication between oogonia and the surrounding somatic cells are vital for normal follicle and oocyte development [181, 182]. The oogonia nests subsequently break down, many oogonia undergo programmed cell death, and the pre-granulosa cells migrate to surround each remaining arrested oocyte in a process termed primordial follicle assembly [183, 184] (Figure 4). A primordial follicle is composed of a single oocyte surrounded by a single layer of flattened pre-granulosa cells. Oocytes are maintained in primordial follicles until sexual maturity, at which point follicles begin to be recruited out of the pool of primordial follicles and undergo primordial to primary follicle transition [185, 186].
Figure 4 .
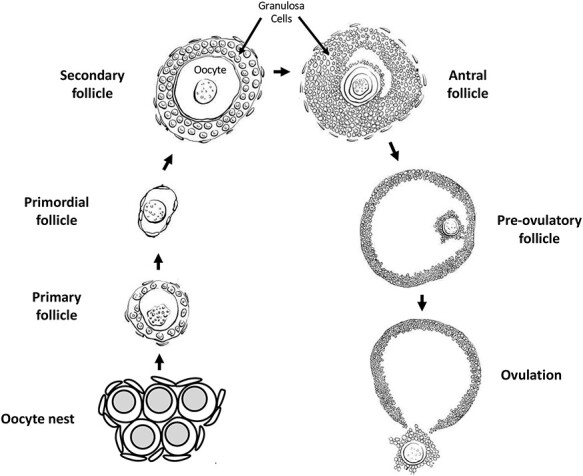
Oogenesis and ovarian follicle stages.
Once a primordial follicle undergoes transition and begins developing, the surrounding flattened pre-granulosa cells become cuboidal and begin proliferating, themselves surrounded by the ovarian stromal cells destined to become theca cells. The follicle is now termed a primary follicle [180]. Subsequent growth and development of the follicle into secondary and pre-antral follicle stages involves continued proliferation of the granulosa cells to form multiple layers, and the initial development of a theca cell layer around the granulosa cells. Follicles with multiple layers of granulosa cells gain sensitivity to follicle stimulating hormone (FSH) secreted by the pituitary, and thus are regulated to grow and develop in cyclic waves in coordination with the estrous cycle [187]. As the granulosa and theca cell layers proliferate a fluid-filled space or antrum forms in the follicle, eventually dividing the granulosa cells into cumulus granulosa surrounding the oocyte and mural granulosa around the inside periphery of the follicle [188]. Extensive cell–cell communication and growth factor signaling between the oocyte and somatic cells occurs at all stages of oogenesis [181, 182]. Most developing follicles do not reach the stage at which ovulation occurs. Rather, follicles at several stages undergo atresia and regress [189–191], (Figure 4).
A luteinizing hormone (LH) surge from the pituitary induces ovulation in late-stage pre-ovulatory follicles, as well as promoting the resumption of meiosis in the oocyte [192]. Meiosis progresses in ovulated oocytes through the production of the first polar body, and then arrests again in metaphase two of the second meiotic division until the time of fertilization. If fertilization occurs, then meiosis again resumes and progresses to completion with the production of the second polar body and the formation of the female pronucleus. Syngamy is the fusion of the male and female pronuclei in the newly formed zygote [193, 194]. Subsequently, the zygotic genome is activated in a carefully controlled manner to allow expression of needed genes in the newly formed individual, while suppressing expression of undesirable genes such as retrotransposons [195, 196].
Epigenetics during oogenesis and in oocytes
Information about the normal epigenetic changes that occur during oogenesis is limited. This is in part due to the difficulty of evaluating developing oocytes in ovaries, and the relatively small number of oocytes available for isolation and study compared to what can be done with male germ cells. Nonetheless, some knowledge of normal epigenomic development in female germ cells has been determined.
Primordial follicle assembly, primordial to primary follicle transition, and many subsequent stages of oogenesis have been shown to be regulated by small non-coding RNA expression, as detailed later in the non-coding RNAs section of Epigenetic Programming During Gametogenesis [197–200], (Figure 4). DNA methylation occurs at sites that are differentially imprinted between male and female gametes so that imprinted genes can be mono-allelically expressed in offspring. DNA methylation is gained gradually on imprinted genes in oocytes in developing follicles after the primary follicle stage, continuing through antral follicle stages of development [201, 202]. In the oocytes of antral stage follicles and later, H3K4Me3 histone methylation increases. This is important for normal function in mature oocytes, and is involved with establishing the DNA methylation pattern in mature oocytes [203–206].
Using in vitro xenogeneic reconstituted ovaries (xrOvaries) with mouse embryonic ovarian somatic cells, Yamashiro and collaborators studied if human primordial germ cell–like cells (hPGCLC) can undergo further development [207]. They observed around 80% of genome-wide 5mC levels in human-induced pluripotent stem cells (hiPSCs) and incipient mesoderm-like cells (iMeLCs) which decreased progressively to around 20% in hPGCLC-derived cells in culture day 77 cells, then dropped at around 13% in culture day 120 cells. Based on their data, the demethylation occurred throughout the genome. Moreover, the 5mC distribution profiles of the culture days 77 to 120 cells were comparable to those observed in the oogonia and gonocytes at weeks 7 to 10. However, they were different to those seen in the blastocysts [208] and naïve human embryonic stem cells (hESCs) [207, 209]. This study demonstrated that hPGCLC-derived cells demethylate their 5mCs similarly to that of oogonia and gonocytes but not early embryonic cells and their putative in vitro counterparts [207].
Epigenetic programming during gametogenesis
Epigenetics
Epigenetics refers to ‘the molecular factors and processes around the DNA that regulate genome activity independent of DNA sequence, and that are mitotically stable’ [3]. These molecular processes include DNA methylation, chromatin structure, histone modifications and retention, non-coding RNAs, and RNA methylation (Figure 5). The epigenome is the complex integration of epigenetic modifications. The first epigenome analysis mapped histone acetylation and methylation in yeast [210]. These epigenetic processes and factors are central for an organism to respond to its environment with changes in gene expression. Moreover, epigenetic mechanisms are required for a stem cell type to develop into a differentiated cell type, which make them an integral part of normal biology [3, 211, 212].
Figure 5 .

Epigenetic mechanisms and processes (marks) (modified from [330]).
DNA methylation and histone modifications
De novo DNA methylation in males restarts in prospermatogonia at E14.5 in mice and is fully established at birth [213, 214]. In both female and male germlines, the factors responsible for mediating DNA methylation DNMT3A or 3B and DNMT3L at imprinted loci were identified [215–217]. In the gametes, the sequence identity and the characteristics of imprinted regions are now well characterized; however, the mechanisms targeting the de novo methyltransferases to imprinted regions remain to be further investigated [218]. In oocytes, the establishment of DNA methylation at imprinted or retrotransposon-rich sites occurs gradually in growing follicles subsequent to the primary follicle stage (reviewed in [201, 202]).
During meiosis of the gametogenesis process, germ cells stop their progress at the prophase stage to allow parental genomes to exchange genetic information through meiosis recombination [219]. At this stage, chromosomes pair in a homologous manner, and large pieces of the chromosomes can be exchanged through crossover events [219, 220]. These crossover events are necessary to maintain euploidy in gametes. An absence of crossover events has been linked to infertility and aneuploidy in the offspring [221, 222]. These meiotic crossover events happen at genomic hotspots and are enriched in regions outside of promoters that bear histone H3K4me3 peaks and established by Prdm9 [223–228]. Mutations in enzymes involved in histone posttranslational modifications observed in meiosis have been shown to have an impact (decrease or increase) on the DNA double-strand break activity, which suggests a role for histone modifications in the initiation and/or repair activity [229–232]. In oocytes, H3K4Me3 histone methylation increases from the antral follicle stage onward, and is important for meiotic recombination, oocyte maturation, oocyte transcriptional activity, and for the establishment of a normal DNA methylation pattern in mature oocytes [203–206, 233, 234].
Chromatin structure & histones
The chromatin reorganization during meiosis is largely transient. The most extensive modifications in chromatin state, structure, or composition occurs after male and female meiosis [220]. In the sperm, the vast majority of histones are replaced with sperm-specific nuclear proteins called protamines [235]. This process is facilitated by different steps: hyperacetylation of histones in round spermatids believed to weaken the interactions between histones and DNA, this will enable the eviction and replacement of histones by testes-specific histone variants, then by transition proteins to end with protamines [236–238]. Because of their endonuclease-inaccessible toroid structure, protamines manage to package the sperm DNA into a tenfold more compact structure than the heterochromatin found in somatic nuclei [239, 240]. The retained histones in the sperm were believed to be remnants of incomplete histone-to-protamine replacement, but recent studies have demonstrated that these retained histones are present at key developmental gene promoters/enhancers in mature sperm. These retained histones bear both active or repressive histone modification [241, 242].
This programmatic retention and evolutionary conservation of histone localization suggests that epigenetic information can be passed through the paternal lineage. Moreover, alteration in histone levels, or chromatin regulators involved in spermatogenesis leads to developmental defects, which can be passed on to the subsequent generation [243, 244]. Altogether, these studies imply that retained histones serve as molecular carriers of epigenetic memory; however, the mechanisms are yet to be elucidated.
Non-coding RNAs
DNA is not the only means to transmit the information between generations. Non-coding RNAs (ncRNAs) are regulatory elements of gene expression and chromatin structure [245]. The differential susceptibility to these non-coding RNAs contributes to tissue-specific gene expression. Early on, ncRNAs are important in the germline development, but they are also crucial players in posttranscriptional gene control during spermatogenesis and oogenesis. Different classes of ncRNAs exist, but this section will focus on microRNAs (miRNAs), Piwi interacting RNAs (piRNAs), and long non-coding RNAs (lncRNAs) and their role in the PGCs and the gametes.
miRNAs
During the PGC specification, some miRNAs are selectively expressed such as miR-10b, −18a, −93, −106b, −126-3p, −127, −181a, −181b, and − 301. All of them have important functions in these cells such as differentiation, migration, and apoptosis in PGCs in mice [246]. For instance, Medeiros and collaborators have shown that in mice a deficiency in miR-290-295 cluster result in an abnormal germ cell with defect in the PGC migration [247]. In the female, an upregulation of miR-29b has been shown to induce PGC development by targeting DNA methyltransferases Dnmt3a and Dnmt3b [248]. In the zebrafish, miR-202-5p has been identified as a potential germ plasma-specific biomarker due to its potential role in the germ cell development [249]. Other microRNAs have been linked to PGC migration in the zebrafish as well, such as miR-430, which regulates sdf1a and cxcr7 mRNAs key transcripts regulating migration [250].
In the early stages of spermatogenesis, different miRNAs have been described in mammals as being crucial for germ cell self-renewal and differentiation. miR-34c has been identified as promoting mouse spermatogonial stem cell (SSCs) differentiation by targeting Nanos2 [251]. Moreover, this miRNA has another role in the later stage of spermatogenesis where miR-34c is involved in apoptotic events of spermatocytes and round spermatids [252], and also in the NOTCH signaling, which is important in the control of germ cell differentiation [253]. A list of miRNAs involved in cell cycle regulation have been identified such as miR-293, 291a-5p, 290-5p and 294 [254]. Other miRNAs are involved in later stages of spermatogenesis. The Let-7 miR family is involved in the mouse spermatogonial differentiation, especially in the maturation of undifferentiated spermatogonia to A1 spermatogonia by suppressing Lin28 [255]. In contrast, some miRNAs such as miR-146 play a crucial role in keeping spermatogonia in an undifferentiated state in the mouse [256]. Other miRNAs play a role in the regulation of meiotic and postmeiotic events in the later stages of spermatogenesis such as the miR-449 cluster. During murine spermatogenesis, the upregulation of miR-449 cluster is crucial for the initiation of meiosis [257]. These miRNAs by targeting BCL2 and AFT1 are involved in germ cell apoptosis [258].
piRNAs
Another class of sncRNAs, piRNAs have been discovered in the germline. Their role is to safeguard the germline genome from retrotransposons and protect the genomic stability [259, 260]. These piRNAs are believed to be involved in pathway components of DNA methylation remodeling during early PGC specification in mammals [209]. Moreover, a loss of Piwi function in mice or zebrafish results in a decrease of germ cells by apoptosis, this underlying its role in germ cell maintenance [261].
lncRNAs
The role of long non-coding RNAs in PGC specification has not been described. Some researchers suggest their possible roles in controlling transcription factors such as BLIMP1/PRDM1 or DAZL [262, 263]. In fact, more than 300 binding sites of BLIMP1/PRDM1 in the murine PGCs are associated with non-coding genes whose functions in PGCs specification are still unknown [23, 262]. The lncRNA-Tcam1 and lncRNA-HSVIII have a crucial role in pachytene spermatocytes, which implies their potential participation in the transcriptional regulation of spermatocyte-specific gene expression [264]. LncRNAs have been linked to functions related to post-transcriptional control during spermatogenesis, such as tubulin cofactor A (TBCA), which has the ability to interact with tubulin during the microtubule rearrangement process [265]. However, most studies have been conducted in rats, so not much is known about lncRNAs in the human. In human spermatogenesis, male infertility has been associated with NLC1-C through the control of miRNA expression via RNA-binding proteins [266].
ncRNAs in oocytes
Most of the studies have focused on miRNAs in oogenesis and ovary function using conditional KO mice models to evaluate their involvement in the ovary. By using this approach, a clear role has been outlined for miRNAs in folliculogenesis, oocyte maturation, and ovulation. Other miRNAs are also involved in the assembly of primordial follicles, the transition from primordial to primary follicles, follicular growth, oocyte maturation, ovulation, and the formation of the corpus luteum in mammals [198, 199, 267–269]. After a conditional knockout of Dicer1 from follicular granulosa cells in mammals, abnormal oocyte maturation, disrupted follicular development and ovulation, increased follicular atresia, and infertility were reported [270–272]. Other studies have demonstrated miRNAs involvement in granulosa cells proliferation, survival, terminal differentiation, steroidogenesis, and cumulus expansion [200, 273–281]. The overexpression of miR-143 in murine 15.5 dpc ovaries has been shown to repress the formation of primordial follicles by stopping the proliferation of pre-granulosa cells. An increased number of primordial follicles were observed in transfected 18.5 dpc ovaries with miR-376a (reviewed by Grossman and Shalgi [197]).
Environmental toxicant exposures resulting in epigenetic changes in gametes
In addition to epigenetic changes being a part of the normal developmental process for gametes, it is also possible that exposure to environmental factors will induce abnormal epigenetic changes to the germ cell epigenome [282, 283]. Such changes may be heritable and affect the phenotype of subsequent generations [156, 284]. Exposure of male mice to the endocrine disruptor bisphenol A (BPA) induces changes to DNA methylation in the fetal germ cells of their developing offspring [285]. Primordial germ cells are also induced to alter DNA methylation in response to hypoglycemic conditions in the uterus [286] or from exposure to the agricultural fungicide vinclozolin [287]. Exposure to a wide variety of environmental factors can lead to DNA methylation changes in spermatozoa and mature sperm [288]. In rodents, direct exposure to arsenic [289], the fungal toxin zearalenone [290], the plastics compounds bisphenol A (i.e. BPA) [291] and phthalates [292], the agricultural fungicide vinclozolin [293], the pesticide dichlorodiphenyltrichloroethane (DDT) [294], and the herbicides glyphosate [295] and atrazine [296], all induce sperm DNA methylation changes. In humans, studies have shown that environmental factors such as exposure to phthalates [297], alcohol [298], flame retardants [299, 300], chemotherapy treatment [301], obesity [302], and exercise [303] are correlated to sperm DNA methylation changes (Figure 6). In one fish species, exposure to BPA resulted in changes to oocyte DNA methylation in the next generation [304], (Table 1).
Figure 6 .
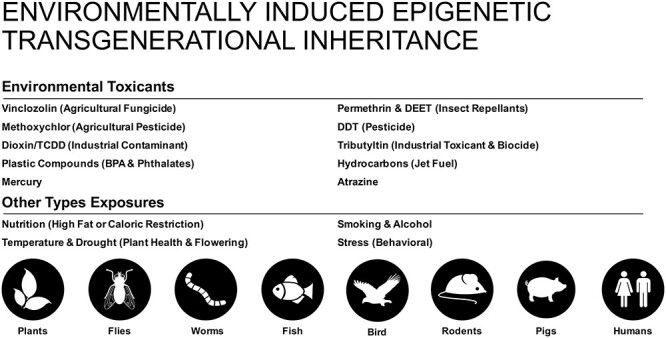
Environmentally induced epigenetic transgenerational inheritance. Various exposures and species investigated (modified from [156]).
Table 1.
Environmental exposures resulting in epigenetic changes in gametes.
| Environmental exposure | Epigenetic change | Cell type | Reference |
|---|---|---|---|
| BPA | DNA methylation | Fetal germ cells | Zhang et al. (2012) [285] |
| Uterine hypoglycemia | DNA methylation | PGCs | Ren et al. (2018) [286] |
| Arsenic | DNA methylation | Sperm | Nohara et al. (2019) [289] |
| Zearalenone | DNA methylation | Sperm | Gao et al. (2019) [290] |
| BPA | DNA methylation | Sperm | Rahman et al. (2020) [291] |
| Phthalates | DNA methylation | Sperm | Prados et al. (2015) [292] |
| Vinclozolin | DNA methylation | Sperm | Beck et al. (2017) [293] |
| DDT | DNA methylation | Sperm | Skinner et al. (2018) [294] |
| Glyphosate | DNA methylation | Sperm | Kubsad et al. (2019) [295] |
| Atrazine | DNA methylation | Sperm | McBirney et al. (2017) [296] |
| BPA | DNA methylation | Fish oocyte | Zhu et al. (2020) [304] |
| Phthalates | DNA methylation | Human sperm | Wu et al. (2017) [297] |
| Alcohol | DNA methylation | Human sperm | Ouko et al. (2009) [298] |
| Flame retardants | DNA methylation | Human sperm | Soubry et al. (2017), Greeson et al. (2020) [299, 300] |
| Chemotherapy | DNA methylation | Human sperm | Shnorhavorian et al. (2017) [301] |
| Obesity | DNA methylation | Human sperm | Soubry et al. (2016) [302] |
| Exercise | DNA methylation | Human sperm | Denham et al. (2015) [303] |
| BPA | Histone acetylation | Fish sperm | Lombo et al. (2019) [305] |
| BPA | histone methylation | Fish oocyte | Zhu et al. (2020) [304] |
| Carbendazim and chlorothalonil | Histone H3K9me3 | Sperm | Li et al. (2018) [306] |
| Zearalenone | Histone H3K27 methylation | Sperm | Gao et al. (2019) [290] |
| Chlordecone | Histone H3K4Me3 | Developing testes | Gely-Pernot et al. (2018) [307] |
| Chlordecone | Histone H3K4Me3 | Oocytes | Legoff et al. (2019) [308] |
| Restraint stress | Histone acetylation, methylation, phosphorylation | Oocytes | Wu et al. (2015) [309] |
| Cigarette smoke | Histone retention | Human sperm | Hamad et al. (2014) [313] |
| Smoke | Histone retention | Human sperm | Lettieri et al. (2020) [314] |
| Caloric restriction in utero | Histone retention and DNA methylation | Sperm | Radford et al. (2014) [315] |
| DDT | DNA methylation, non-coding RNA expression, and histone retention | Sperm | Skinner et al. (2018) [294] |
| Vinclozolin | DNA methylation, non-coding RNA expression, and histone retention | Sperm | Ben Maamar et al. (2018) [316] |
| Vinclozolin | miRNA | PGCs | Brieno-Enriquez et al. (2015) [317] |
| Early life trauma | miRNA and lncRNA | Sperm | Dickson et al. (2018), Gapp et al. (2014, 2020) [318–320] |
| Early life stress | miRNA | Human sperm | Dickson et al. (2018) [318] |
| Smoking | miRNA | Human sperm | Marczylo et al. (2012) [321] |
| Obesity | miRNA | Human sperm | Lopez et al. (2018), Donkin et al. (2015) [322, 323] |
| Bariatric surgery | miRNA | Human sperm | Donkin et al. (2015) [323] |
Epigenetic changes to histones in germ cells can occur after exposure to environmental factors. For example, zebrafish exposed to BPA showed decreased sperm histone acetylation, as well as impaired primordial germ cell migration, although these findings were not associated with decreased fertility [305]. BPA exposure in a minnow species resulted in changes in oocyte histone methylation in the offspring [304]. Pubertal exposure of mice to the fungicides carbendazim and chlorothalonil caused changes in H3K9me3 levels in sperm [306]. Pubertal exposure to the fungal toxin zearalenone altered mouse histone H3K27 methylation [290]. In mice, exposure to the pesticide chlordecone resulted in altered levels of H3K4Me3 in developing testes [307]. Exposure to chlordecone in mice also resulted in changes in H3K4me3 and H4ac in mature oocytes [308]. Even exposure to chronic restraint stress can alter histone acetylation, methylation and phosphorylation in germinal vesicle-stage oocytes [309].
Another way in which environmental factors can alter histones in sperm is to affect which histones are retained as male germ cells develop. As male germ cells undergo spermiogenesis, most of the histones associated with the DNA are replaced by protamines [236, 310]. Protamines help condense and package DNA into the small sperm head. However, some histones are retained, and they are often located near developmental regulatory genes that are expressed early in embryonic development [311]. Exposure to environmental toxicants has been shown to alter retention of histones in sperm [312]. Men exposed to either cigarette smoke [313] or the smoke of surrounding fires [314] have been shown to have an altered ratio of histones to protamines in sperm. In utero exposure to caloric restriction in mice has also been shown to alter histone retention in sperm [315]. In transgenerational studies in rats, it was found that exposure of gestating female F0 generation rats to either DDT or vinclozolin resulted in changes in histone retention in the subsequent transgenerational F3 generation, but interestingly not in the intervening F1 and F2 generations [294, 312, 316]. However, F1, F2 and F3 exposure-lineage generations all showed changes in DNA methylation and non-coding RNA expression (Table 1).
The expression of non-coding RNA (ncRNA) in germ cells is another epigenetic factor that can be responsive to environmental factors. Mice exposed to vinclozolin in utero exhibited changes in micro-RNAs in their primordial germ cells [317]. Rats exposed to either vinclozolin or DDT in utero have been shown to have altered levels of piwi-interacting RNAs (piRNAs) and small tRNA fragments in sperm upon reaching adulthood [294, 316]. Traumatic stress can also be an environmental factor that causes epigenetic changes in sperm. In mouse models of early life trauma, changes in miRNAs and long non-coding RNAs were seen in sperm from exposed males [318–320]. Interestingly, the behavioral and metabolic alterations seen in the resulting offspring were recapitulated by injection of sperm RNAs from traumatized males into fertilized wild-type oocytes [319]. In humans, changes in miRNA expression in sperm have been seen after exposure to early life stress [318], smoking [321], obesity [322, 323], and bariatric surgery [323] (Table 1).
Epigenetic transgenerational inheritance
Exposure to environmental factors, such as toxicants, can induce epigenetic changes in germ cells that can affect the subsequent generations. These epimutation changes are brought to the next generation at fertilization and have the possibility of altering gene expression and phenotype in the developing embryo. Since the germ cell epimutations can affect the earliest stem cells formed in the embryo, then any subsequent cell type in the embryo and adult animal may have epimutations and changes in gene expression that could affect their phenotype [156].
Epigenetic transgenerational inheritance is defined as germline-mediated inheritance of epigenetic information between generations in the absence of continued direct environmental influences that leads to phenotypic variation [3]. When a male or a non-pregnant female is exposed to an environmental factor that can induce epigenetic change, then epimutations can arise in that individual (the F0 generation), and that individual’s germ cells. The germ cells that contribute to forming the next F1 generation were directly exposed to the environmental factor, so epigenetic and phenotypic changes seen in the F1 generation are an example of direct multigenerational exposure, but not transgenerational inheritance [324], (Figure 7). If these F1 generation animals pass on epigenetic and phenotypic changes to the unexposed F2 generation, then this is an example of epigenetic transgenerational inheritance. Similarly, if a pregnant female is exposed to an environmental factor such as a toxicant, the developing F1 generation embryo is directly exposed, and the germ cells in that embryo that go on to form the F2 generation are also directly exposed. Epigenetic and phenotypic changes would have to be seen in subsequent F3 generation or later generations for this to be an example of epigenetic transgenerational inheritance (Figure 7, Table 2) [156, 157, 324].
Figure 7 .
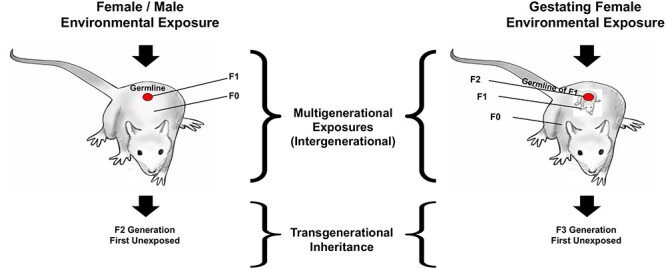
Environmentally induced transgenerational epigenetic inheritance. Schematic of multigenerational versus transgenerational environmental exposures (modified from [324]).
Table 2.
Environmental exposures promoting epigenetic transgenerational inheritance.
| Environmental exposure | Epigenetic change | Cell type | Reference |
|---|---|---|---|
| Several toxicants (review) | DNA methylation | Sperm | Nilsson et al. (2018) [156] |
| DDT | DNA methylation | Sperm | Ben Maamar et al. (2019) [176] |
| DDT | DNA methylation, non-coding RNA, and histone retention | Sperm | Skinner et al. (2018) [294] |
| Vinclozolin | DNA methylation, non-coding RNA expression, and histone retention | Sperm | Ben Maamar et al. (2018) [316] |
| Vinclozolin | DNA methylation | Sperm | Anway et al. (2005) [157] |
| DDT or vinclozolin | Histone retention | Sperm | Ben Maamar et al. (2020) [177] |
| Glyphosate | DNA methylation | Sperm | Kubsad et al. (2019) [295] |
| Atrazine | DNA methylation | Sperm | McBirney et al. (2017) [296] |
| Methoxychlor | DNA methylation | Sperm | Manikkam et al. (2014) [331] |
| Glyphosate | DNA methylation and histone retention | Sperm | Ben Maamar et al. (2020) [332] |
| Dioxin | DNA methylation | Sperm | Manikkam et al. (2012) [333] |
| BPA | DNA methylation | Sperm | Rahman et al. (2020) [291] |
| Phthalates | DNA methylation | Sperm | Prados et al. (2015) [292] |
| Jet fuel | DNA methylation | Sperm | Manikkam et al. (2012) [334] |
| Vinclozolin | tRNA halves | Sperm | Schuster et al. (2016) [335] |
| Methylmercury | DNA methylation | Fish sperm | Carvan et al. (2017) [326] |
| Nutrition change | Gene promoter methylation | Pig liver | Braunschweig et al. (2012) [336] |
| Famine | DNA methylation | Human blood cells | Jiang et al. (2020) [337] |
| Genetic manipulation | Histone modifications | Drosophila embryos | Xia et al. (2016) [338] |
| Genetic manipulation | Histone modifications | Caenorhabditis elegans larvae | Kelly et al. (2014) [339] |
| Vinclozolin | tRNA halves | Sperm | Schuster et al. (2016) [335] |
Epimutations have been reported in transgenerational generation gametes after ancestral exposure to a wide variety of environmental stressors including toxicants [156] and psychological stress [325]. This phenomenon has been observed in several organisms including fish [326] and rodents [157] (reviewed in [156]) (Table 2). Epimutations have been reported in transgenerational F3 generation rat sperm after ancestral exposure to several toxicants [156]. One question that occurs is at what stage of germ cell development do these sperm epimutations arise, or are they continuously present? Two recent studies have addressed this question. The first examined differences in DNA methylation compared to controls after ancestral exposure to DDT [176]. The number of differential DNA methylation regions (DMRs) was determined for the spermatogenic stages of primordial germ cells, prospermatogonia, spermatogonia, pachytene spermatocytes, round spermatids, caput epididymal spermatozoa, and cauda epididymal sperm. It was found that, of the 265 DMRs present in cauda epididymal sperm, 26% arose in the prospermatogonia stage, 25% in spermatogonia, 18% in pachytene spermatocytes, 5% in round spermatids, 12% in caput epididymal spermatozoa, and 14% only arose in cauda epididymal sperm (Figure 3). Similar observations were made with ancestral vinclozolin exposure [327]. This shows that transgenerational changes in DNA methylation arise throughout gametogenesis.
Similarly, another study examined transgenerational differences in histone retention in sperm from rats ancestrally exposed to DDT or vinclozolin [177]. In mature sperm nuclei, most histone proteins are replaced by protamines to facilitate packaging the DNA into the small sperm head [328]. However, some histones are retained, sometimes near genes that are important to early embryo development [243, 329]. In this study [177], the sites of differential histone retention (DHR) were determined for the spermatogenic stages of round spermatids, caput epididymal spermatozoa, and cauda epididymal sperm. It was found that, of those DHRs that were present in cauda epididymal sperm, about 50% were present in round spermatids, very few arose in caput epididymal spermatozoa, and 40–50% arose at the cauda epididymal sperm stage. Again, this shows that an environmentally induced cascade of histone retention changes occurs during different stages of spermatogenic development.
Recently, two studies investigated the integration of DMR, ncRNA, and DHR by overlapping the different genomic sites between the different epimutations. Rats were ancestrally exposed to DDT or vinclozolin and the F1, F2, and F3 generations sperm epimutations examined. The chromosomal locations of the DMR, ncRNA, and DHR epimutations were distinct with few overlapping, but present in the same regions with similar genomic features such as CpG deserts. Comparing the F1, F2, and F3 generations provided insights into the integration of the different epimutations and the direct exposure versus transgenerational impacts of exposures. Interestingly, the effects observed in the F3 generation were different than those observed in the direct exposure F1 and F2 generations. Direct exposure impacted the ncRNA in the F1 generation, but to a much lesser extent in the F2 and F3 generations. DMR were predominant in the F1, F2, and F3 generations, whereas the DHRs were observed primarily in the F3 generation. Observations suggest a potential role for ncRNA-directed DNA methylation and DNA methylation-directed histone retention in the environmentally induced epigenetic transgenerational inheritance of altered gametogenesis [294, 316].
Conclusions and future research
Normal fertilization and early embryonic development require the integration of genetic and epigenetic processes in the gametes. Few developmental or physiological processes will not require the integration of these two distinct molecular mechanisms. Understanding the underlying processes and mechanisms in vivo will help us better understand the gametogenesis and formation of the sperm and egg, as well as pathologies such as idiopathic infertility. The past few decades have advanced our knowledge of primordial germ cell and gamete development. This has provided insights into the molecular mechanism involved in related disorders, such as infertility and birth defects. These findings are also promising in the field of reproductive therapies.
Although a genetic focus can identify the genes involved in a developmental process such as gametogenesis, an understanding of the epigenetics is required to clarify how the gene expression is controlled and environmental factors regulate the developmental process. The DNA methylation, histone modifications, ncRNA, and chromatin structure are the epigenetic mechanisms required to regulate the gene expression. Therefore, no development or biological process can be understood without the integration of epigenetics and genetics. This is the case for normal developmental processes like spermatogenesis and oogenesis, as well as abnormal processes involved in pathology. The ability of environmental factors such as nutrition, toxicants, or stress to impact developmental processes like gametogenesis involves alterations in the epigenetics to then impact the basic genetics and gene expression. Since the gametogenesis process produces the gametes, sperm and eggs, alterations in gametogenesis impact the future generations physiology, phenotype, and gametes. This non-genetic form of inheritance termed epigenetic transgenerational inheritance requires manipulation during gametogenesis to obtain epigenetically modified sperm and eggs. Therefore, the current review provides the basic information on the gametogenesis process, epigenetic regulation of the developmental process, and impacts on epigenetic transgenerational inheritance. As the information on epigenetic regulation of gametogenesis is a new area of research, future research is needed to expand our understanding of the integration of epigenetics and genetics in gametogenesis.
The future research suggested includes the following, Table 3. A need to examine all the gametogenesis stages from PGCs to gametes to understand the integration and transition between the different stages of development. A need to integrate all the epigenetic processes and gene expression for a more complete understanding of the epigenetic regulation of gametogenesis. Emphasis on genome-wide analysis and system biology approaches in the study of gametogenesis to fully understand the developmental process and associated pathology. A need for a generational context, to incorporate the environmentally induced epigenetic transgenerational inheritance of gametogenesis alterations into our understanding of gamete development. Without these more complete systems biology approaches, the progress of research and impacts will be diminished.
Table 3.
Future research in gametogenesis.
| 1) | Examine all stages PGCs to gametes for epigenetic and genetic transitions. |
|---|---|
| 2) | Examine and investigate all the epigenetic processes (DNA methylation, histones, ncRNA, and chromatin structure) for the epigenetic regulation of gametogenesis. |
| 3) | Use systems biology and genome-wide analyses to integrate the epigenetics and genetics of the gametogenesis process. |
| 4) | Incorporate environmentally induced epigenetic transgenerational inheritance into our research and understanding of generational impacts of altering gamete epigenetics. |
Acknowledgements
We thank Dr. Jennifer L.M. Thorson for critical review of the manuscript. We thank Dr. Stephanie King for the drawings of the stages of spermatogenesis and oogenesis. We acknowledge Ms. Amanda Quilty for assistance in editing the manuscript, and Ms. Heather Johnson for assistance in preparation of the manuscript.
Conflict of interest: The authors declare no conflict of interest.
Grant support: This study was supported by John Templeton Foundation (50183 and 61174) (https://templeton.org/) grants to M.K.S. and NIH (ES012974) (https://www.nih.gov/) grant to M.K.S. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Millissia Ben Maamar, Center for Reproductive Biology, School of Biological Sciences, Washington State University, Pullman, WA, USA.
Eric E Nilsson, Center for Reproductive Biology, School of Biological Sciences, Washington State University, Pullman, WA, USA.
Michael K Skinner, Center for Reproductive Biology, School of Biological Sciences, Washington State University, Pullman, WA, USA.
Abbreviations
Primordial germ cells (PGCs)
Bone morphogenetic protein (BMP).
Knock-out (KO).
Stromal cell-derived factor 1 (SDF-1).
Chemokine receptor type 4 (CXCR4).
5-methylcytosine (5mC).
Germline reprogramming responsive (GRR).
Ten eleven translocation (TET).
Follicle stimulating hormone (FSH).
Androgen receptors (ARs).
Ethanedimethane sulfonate treatment (EDS).
Follistatin (FST).
Follistatin-like 3 (FSTL3).
Stem cell factor (SCF).
Luteinizing hormone (LH).
Non-coding RNAs (ncRNAs).
MicroRNAs (miRNAs).
Piwi interacting RNAs (piRNAs).
Long non-coding RNAs (lncRNAs).
Tubulin cofactor A (TBCA).
Bisphenol A (BPA).
Differential DNA methylation regions (DMRs).
Differential histone retention sites (DHRs).
Author Contributions
MBM—Writing and editing manuscript.
EN—Writing and editing manuscript.
MKS—Funding acquisition, writing and editing manuscript.
References
- 1.Tang WW, Kobayashi T, Irie N, Dietmann S, Surani MA. Specification and epigenetic programming of the human germ line. Nat Rev Genet 2016; 17:585–600. [DOI] [PubMed] [Google Scholar]
- 2.Ohinata Y, Ohta H, Shigeta M, Yamanaka K, Wakayama T, Saitou M. A signaling principle for the specification of the germ cell lineage in mice. Cell 2009; 137:571–584. [DOI] [PubMed] [Google Scholar]
- 3.Skinner MK. Environmental epigenetic transgenerational inheritance and somatic epigenetic mitotic stability. Epigenetics 2011; 6:838–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seydoux G, Dunn MA. Transcriptionally repressed germ cells lack a subpopulation of phosphorylated RNA polymerase II in early embryos of Caenorhabditis elegans and Drosophila melanogaster. Development 1997; 124:2191–2201. [DOI] [PubMed] [Google Scholar]
- 5.Boswell RE, Mahowald AP. Tudor, a gene required for assembly of the germ plasm in Drosophila melanogaster. Cell 1985; 43:97–104. [DOI] [PubMed] [Google Scholar]
- 6.Capowski EE, Martin P, Garvin C, Strome S. Identification of grandchildless loci whose products are required for normal germ-line development in the nematode Caenorhabditis elegans. Genetics 1991; 129:1061–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christerson LB, McKearin DM. Orb is required for anteroposterior and dorsoventral patterning during drosophila oogenesis. Genes Dev 1994; 8:614–628. [DOI] [PubMed] [Google Scholar]
- 8.Matova N, Cooley L. Comparative aspects of animal oogenesis. Dev Biol 2001; 231:291–320. [DOI] [PubMed] [Google Scholar]
- 9.Simpson AJ, Caballero OL, Jungbluth A, Chen YT, Old LJ. Cancer/testis antigens, gametogenesis and cancer. Nat Rev Cancer 2005; 5:615–625. [DOI] [PubMed] [Google Scholar]
- 10.Leitch HG, Smith A. The mammalian germline as a pluripotency cycle. Development 2013; 140:2495–2501. [DOI] [PubMed] [Google Scholar]
- 11.Lawson KA, Dunn NR, Roelen BA, Zeinstra LM, Davis AM, Wright CV, Korving JP, Hogan BL. Bmp4 is required for the generation of primordial germ cells in the mouse embryo. Genes Dev 1999; 13:424–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saitou M, Barton SC, Surani MA. A molecular programme for the specification of germ cell fate in mice. Nature 2002; 418:293–300. [DOI] [PubMed] [Google Scholar]
- 13.Saitou M, Yamaji M. Primordial germ cells in mice. Cold Spring Harb Perspect Biol 2012; 4:a008375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tremblay KD, Dunn NR, Robertson EJ. Mouse embryos lacking Smad1 signals display defects in extra-embryonic tissues and germ cell formation. Development 2001; 128:3609–3621. [DOI] [PubMed] [Google Scholar]
- 15.Ying Y, Liu XM, Marble A, Lawson KA, Zhao GQ. Requirement of bmp 8b for the generation of primordial germ cells in the mouse. Mol Endocrinol 2000; 14:1053–1063. [DOI] [PubMed] [Google Scholar]
- 16.Ying Y, Zhao GQ. Cooperation of endoderm-derived BMP2 and extraembryonic ectoderm-derived BMP4 in primordial germ cell generation in the mouse. Dev Biol 2001; 232:484–492. [DOI] [PubMed] [Google Scholar]
- 17.Saffman EE, Lasko P. Germline development in vertebrates and invertebrates. Cell Mol Life Sci 1999; 55:1141–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomperts M, Garcia-Castro M, Wylie C, Heasman J. Interactions between primordial germ cells play a role in their migration in mouse embryos. Development 1994; 120:135–141. [DOI] [PubMed] [Google Scholar]
- 19.Ohinata Y, Payer B, O'Carroll D, Ancelin K, Ono Y, Sano M, Barton SC, Obukhanych T, Nussenzweig M, Tarakhovsky A, Saitou M, Surani MA. Blimp1 is a critical determinant of the germ cell lineage in mice. Nature 2005; 436:207–213. [DOI] [PubMed] [Google Scholar]
- 20.Yamaji M, Seki Y, Kurimoto K, Yabuta Y, Yuasa M, Shigeta M, Yamanaka K, Ohinata Y, Saitou M. Critical function of Prdm14 for the establishment of the germ cell lineage in mice. Nat Genet 2008; 40:1016–1022. [DOI] [PubMed] [Google Scholar]
- 21.Weber S, Eckert D, Nettersheim D, Gillis AJ, Schafer S, Kuckenberg P, Ehlermann J, Werling U, Biermann K, Looijenga LH, Schorle H. Critical function of AP-2 gamma/TCFAP2C in mouse embryonic germ cell maintenance. Biol Reprod 2010; 82:214–223. [DOI] [PubMed] [Google Scholar]
- 22.Magnusdottir E, Dietmann S, Murakami K, Gunesdogan U, Tang F, Bao S, Diamanti E, Lao K, Gottgens B, Azim Surani M. A tripartite transcription factor network regulates primordial germ cell specification in mice. Nat Cell Biol 2013; 15:905–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magnusdottir E, Surani MA. How to make a primordial germ cell. Development 2014; 141:245–252. [DOI] [PubMed] [Google Scholar]
- 24.Nakaki F, Hayashi K, Ohta H, Kurimoto K, Yabuta Y, Saitou M. Induction of mouse germ-cell fate by transcription factors in vitro. Nature 2013; 501:222–226. [DOI] [PubMed] [Google Scholar]
- 25.Ancelin K, Lange UC, Hajkova P, Schneider R, Bannister AJ, Kouzarides T, Surani MA. Blimp1 associates with Prmt5 and directs histone arginine methylation in mouse germ cells. Nat Cell Biol 2006; 8:623–630. [DOI] [PubMed] [Google Scholar]
- 26.Hayashi K, de Sousa Lopes SM, Surani MA. Germ cell specification in mice. Science 2007; 316:394–396. [DOI] [PubMed] [Google Scholar]
- 27.Richardson BE, Lehmann R. Mechanisms guiding primordial germ cell migration: Strategies from different organisms. Nat Rev Mol Cell Biol 2010; 11:37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vincent SD, Dunn NR, Sciammas R, Shapiro-Shalef M, Davis MM, Calame K, Bikoff EK, Robertson EJ. The zinc finger transcriptional repressor Blimp1/Prdm1 is dispensable for early axis formation but is required for specification of primordial germ cells in the mouse. Development 2005; 132:1315–1325. [DOI] [PubMed] [Google Scholar]
- 29.Gunesdogan U, Magnusdottir E, Surani MA. Primordial germ cell specification: A context-dependent cellular differentiation event [corrected]. Philos Trans R Soc Lond B Biol Sci 2014; 369:20130543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kurimoto K, Yabuta Y, Ohinata Y, Shigeta M, Yamanaka K, Saitou M. Complex genome-wide transcription dynamics orchestrated by Blimp1 for the specification of the germ cell lineage in mice. Genes Dev 2008; 22:1617–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fox N, Damjanov I, Martinez-Hernandez A, Knowles BB, Solter D. Immunohistochemical localization of the early embryonic antigen (SSEA-1) in postimplantation mouse embryos and fetal and adult tissues. Dev Biol 1981; 83:391–398. [DOI] [PubMed] [Google Scholar]
- 32.Ginsburg M, Snow MH, McLaren A. Primordial germ cells in the mouse embryo during gastrulation. Development 1990; 110:521–528. [DOI] [PubMed] [Google Scholar]
- 33.Sato M, Kimura T, Kurokawa K, Fujita Y, Abe K, Masuhara M, Yasunaga T, Ryo A, Yamamoto M, Nakano T. Identification of PGC7, a new gene expressed specifically in preimplantation embryos and germ cells. Mech Dev 2002; 113:91–94. [DOI] [PubMed] [Google Scholar]
- 34.Tam PP, Zhou SX. The allocation of epiblast cells to ectodermal and germ-line lineages is influenced by the position of the cells in the gastrulating mouse embryo. Dev Biol 1996; 178:124–132. [DOI] [PubMed] [Google Scholar]
- 35.Chambers I, Silva J, Colby D, Nichols J, Nijmeijer B, Robertson M, Vrana J, Jones K, Grotewold L, Smith A. Nanog safeguards pluripotency and mediates germline development. Nature 2007; 450:1230–1234. [DOI] [PubMed] [Google Scholar]
- 36.Avilion AA, Nicolis SK, Pevny LH, Perez L, Vivian N, Lovell-Badge R. Multipotent cell lineages in early mouse development depend on SOX2 function. Genes Dev 2003; 17:126–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scholer HR, Ruppert S, Suzuki N, Chowdhury K, Gruss P. New type of POU domain in germ line-specific protein Oct-4. Nature 1990; 344:435–439. [DOI] [PubMed] [Google Scholar]
- 38.Yamaguchi S, Kimura H, Tada M, Nakatsuji N, Tada T. Nanog expression in mouse germ cell development. Gene Expr Patterns 2005; 5:639–646. [DOI] [PubMed] [Google Scholar]
- 39.Sybirna A, Tang WWC, Pierson Smela M, Dietmann S, Gruhn WH, Brosh R, Surani MA. A critical role of PRDM14 in human primordial germ cell fate revealed by inducible degrons. Nat Commun 2020; 11:1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Irie N, Weinberger L, Tang WW, Kobayashi T, Viukov S, Manor YS, Dietmann S, Hanna JH, Surani MA. SOX17 is a critical specifier of human primordial germ cell fate. Cell 2015; 160:253–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kojima Y, Sasaki K, Yokobayashi S, Sakai Y, Nakamura T, Yabuta Y, Nakaki F, Nagaoka S, Woltjen K, Hotta A, Yamamoto T, Saitou M. Evolutionarily distinctive transcriptional and signaling programs drive human germ cell lineage specification from pluripotent stem cells. Cell Stem Cell 2017; 21:517–532 e515. [DOI] [PubMed] [Google Scholar]
- 42.Anderson R, Copeland TK, Scholer H, Heasman J, Wylie C. The onset of germ cell migration in the mouse embryo. Mech Dev 2000; 91:61–68. [DOI] [PubMed] [Google Scholar]
- 43.Molyneaux KA, Stallock J, Schaible K, Wylie C. Time-lapse analysis of living mouse germ cell migration. Dev Biol 2001; 240:488–498. [DOI] [PubMed] [Google Scholar]
- 44.Ewen K, Baker M, Wilhelm D, Aitken RJ, Koopman P. Global survey of protein expression during gonadal sex determination in mice. Mol Cell Proteomics 2009; 8:2624–2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gu Y, Runyan C, Shoemaker A, Surani A, Wylie C. Steel factor controls primordial germ cell survival and motility from the time of their specification in the allantois, and provides a continuous niche throughout their migration. Development 2009; 136:1295–1303. [DOI] [PubMed] [Google Scholar]
- 46.Ohta H, Tohda A, Nishimune Y. Proliferation and differentiation of spermatogonial stem cells in the w/wv mutant mouse testis. Biol Reprod 2003; 69:1815–1821. [DOI] [PubMed] [Google Scholar]
- 47.Raz E. Guidance of primordial germ cell migration. Curr Opin Cell Biol 2004; 16:169–173. [DOI] [PubMed] [Google Scholar]
- 48.Runyan C, Schaible K, Molyneaux K, Wang Z, Levin L, Wylie C. Steel factor controls midline cell death of primordial germ cells and is essential for their normal proliferation and migration. Development 2006; 133:4861–4869. [DOI] [PubMed] [Google Scholar]
- 49.Blume-Jensen P, Jiang G, Hyman R, Lee KF, O'Gorman S, Hunter T. Kit/stem cell factor receptor-induced activation of phosphatidylinositol 3′-kinase is essential for male fertility. Nat Genet 2000; 24:157–162. [DOI] [PubMed] [Google Scholar]
- 50.Chabot B, Stephenson DA, Chapman VM, Besmer P, Bernstein A. The proto-oncogene c-kit encoding a transmembrane tyrosine kinase receptor maps to the mouse W locus. Nature 1988; 335:88–89. [DOI] [PubMed] [Google Scholar]
- 51.Reith AD, Rottapel R, Giddens E, Brady C, Forrester L, Bernstein A. W mutant mice with mild or severe developmental defects contain distinct point mutations in the kinase domain of the c-kit receptor. Genes Dev 1990; 4:390–400. [DOI] [PubMed] [Google Scholar]
- 52.Doitsidou M, Reichman-Fried M, Stebler J, Koprunner M, Dorries J, Meyer D, Esguerra CV, Leung T, Raz E. Guidance of primordial germ cell migration by the chemokine SDF-1. Cell 2002; 111:647–659. [DOI] [PubMed] [Google Scholar]
- 53.Ara T, Nakamura Y, Egawa T, Sugiyama T, Abe K, Kishimoto T, Matsui Y, Nagasawa T. Impaired colonization of the gonads by primordial germ cells in mice lacking a chemokine, stromal cell-derived factor-1 (SDF-1). Proc Natl Acad Sci U S A 2003; 100:5319–5323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Molyneaux KA, Zinszner H, Kunwar PS, Schaible K, Stebler J, Sunshine MJ, O'Brien W, Raz E, Littman D, Wylie C, Lehmann R. The chemokine SDF1/CXCL12 and its receptor CXCR4 regulate mouse germ cell migration and survival. Development 2003; 130:4279–4286. [DOI] [PubMed] [Google Scholar]
- 55.Pepling ME, Spradling AC. Female mouse germ cells form synchronously dividing cysts. Development 1998; 125:3323–3328. [DOI] [PubMed] [Google Scholar]
- 56.Lei L, Spradling AC. Mouse primordial germ cells produce cysts that partially fragment prior to meiosis. Development 2013; 140:2075–2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mork L, Maatouk DM, McMahon JA, Guo JJ, Zhang P, McMahon AP, Capel B. Temporal differences in granulosa cell specification in the ovary reflect distinct follicle fates in mice. Biol Reprod 2012; 86:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seisenberger S, Andrews S, Krueger F, Arand J, Walter J, Santos F, Popp C, Thienpont B, Dean W, Reik W. The dynamics of genome-wide DNA methylation reprogramming in mouse primordial germ cells. Mol Cell 2012; 48:849–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kagiwada S, Kurimoto K, Hirota T, Yamaji M, Saitou M. Replication-coupled passive DNA demethylation for the erasure of genome imprints in mice. EMBO J 2013; 32:340–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kurimoto K, Yamaji M, Seki Y, Saitou M. Specification of the germ cell lineage in mice: A process orchestrated by the PR-domain proteins, Blimp1 and Prdm14. Cell Cycle 2008; 7:3514–3518. [DOI] [PubMed] [Google Scholar]
- 61.Seki Y, Yamaji M, Yabuta Y, Sano M, Shigeta M, Matsui Y, Saga Y, Tachibana M, Shinkai Y, Saitou M. Cellular dynamics associated with the genome-wide epigenetic reprogramming in migrating primordial germ cells in mice. Development 2007; 134:2627–2638. [DOI] [PubMed] [Google Scholar]
- 62.Shirane K, Kurimoto K, Yabuta Y, Yamaji M, Satoh J, Ito S, Watanabe A, Hayashi K, Saitou M, Sasaki H. Global landscape and regulatory principles of DNA methylation reprogramming for germ cell specification by mouse pluripotent stem cells. Dev Cell 2016; 39:87–103. [DOI] [PubMed] [Google Scholar]
- 63.Hargan-Calvopina J, Taylor S, Cook H, Hu Z, Lee SA, Yen MR, Chiang YS, Chen PY, Clark AT. Stage-specific demethylation in primordial germ cells safeguards against precocious differentiation. Dev Cell 2016; 39:75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hackett JA, Sengupta R, Zylicz JJ, Murakami K, Lee C, Down TA, Surani MA. Germline DNA demethylation dynamics and imprint erasure through 5-hydroxymethylcytosine. Science 2013; 339:448–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yamaguchi S, Shen L, Liu Y, Sendler D, Zhang Y. Role of Tet1 in erasure of genomic imprinting. Nature 2013; 504:460–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vincent JJ, Huang Y, Chen PY, Feng S, Calvopina JH, Nee K, Lee SA, Le T, Yoon AJ, Faull K, Fan G, Rao A et al. Stage-specific roles for tet1 and tet2 in DNA demethylation in primordial germ cells. Cell Stem Cell 2013; 12:470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kobayashi H, Sakurai T, Miura F, Imai M, Mochiduki K, Yanagisawa E, Sakashita A, Wakai T, Suzuki Y, Ito T, Matsui Y, Kono T. High-resolution DNA methylome analysis of primordial germ cells identifies gender-specific reprogramming in mice. Genome Res 2013; 23:616–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yamaguchi S, Hong K, Liu R, Shen L, Inoue A, Diep D, Zhang K, Zhang Y. Tet1 controls meiosis by regulating meiotic gene expression. Nature 2012; 492:443–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dawlaty MM, Breiling A, Le T, Raddatz G, Barrasa MI, Cheng AW, Gao Q, Powell BE, Li Z, Xu M, Faull KF, Lyko F et al. Combined deficiency of Tet1 and Tet2 causes epigenetic abnormalities but is compatible with postnatal development. Dev Cell 2013; 24:310–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Popp C, Dean W, Feng S, Cokus SJ, Andrews S, Pellegrini M, Jacobsen SE, Reik W. Genome-wide erasure of DNA methylation in mouse primordial germ cells is affected by AID deficiency. Nature 2010; 463:1101–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guibert S, Forne T, Weber M. Global profiling of DNA methylation erasure in mouse primordial germ cells. Genome Res 2012; 22:633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang WW, Dietmann S, Irie N, Leitch HG, Floros VI, Bradshaw CR, Hackett JA, Chinnery PF, Surani MA. A unique gene regulatory network resets the human germline epigenome for development. Cell 2015; 161:1453–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Guo F, Yan L, Guo H, Li L, Hu B, Zhao Y, Yong J, Hu Y, Wang X, Wei Y, Wang W, Li R et al. The transcriptome and DNA Methylome landscapes of human primordial germ cells. Cell 2015; 161:1437–1452. [DOI] [PubMed] [Google Scholar]
- 74.Hajkova P, Ancelin K, Waldmann T, Lacoste N, Lange UC, Cesari F, Lee C, Almouzni G, Schneider R, Surani MA. Chromatin dynamics during epigenetic reprogramming in the mouse germ line. Nature 2008; 452:877–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hajkova P, Erhardt S, Lane N, Haaf T, El-Maarri O, Reik W, Walter J, Surani MA. Epigenetic reprogramming in mouse primordial germ cells. Mech Dev 2002; 117:15–23. [DOI] [PubMed] [Google Scholar]
- 76.Hill PW, Amouroux R, Hajkova P. DNA demethylation, Tet proteins and 5-hydroxymethylcytosine in epigenetic reprogramming: An emerging complex story. Genomics 2014; 104:324–333. [DOI] [PubMed] [Google Scholar]
- 77.Lee J, Inoue K, Ono R, Ogonuki N, Kohda T, Kaneko-Ishino T, Ogura A, Ishino F. Erasing genomic imprinting memory in mouse clone embryos produced from day 11.5 primordial germ cells. Development 2002; 129:1807–1817. [DOI] [PubMed] [Google Scholar]
- 78.Surani MA, Hajkova P. Epigenetic reprogramming of mouse germ cells toward totipotency. Cold Spring Harb Symp Quant Biol 2010; 75:211–218. [DOI] [PubMed] [Google Scholar]
- 79.Hill PWS, Leitch HG, Requena CE, Sun Z, Amouroux R, Roman-Trufero M, Borkowska M, Terragni J, Vaisvila R, Linnett S, Bagci H, Dharmalingham G et al. Epigenetic reprogramming enables the transition from primordial germ cell to gonocyte. Nature 2018; 555:392–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Williams K, Christensen J, Pedersen MT, Johansen JV, Cloos PA, Rappsilber J, Helin K. TET1 and hydroxymethylcytosine in transcription and DNA methylation fidelity. Nature 2011; 473:343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vella P, Scelfo A, Jammula S, Chiacchiera F, Williams K, Cuomo A, Roberto A, Christensen J, Bonaldi T, Helin K, Pasini D. Tet proteins connect the O-linked N-acetylglucosamine transferase Ogt to chromatin in embryonic stem cells. Mol Cell 2013; 49:645–656. [DOI] [PubMed] [Google Scholar]
- 82.Smith ZD, Meissner A. DNA methylation: Roles in mammalian development. Nat Rev Genet 2013; 14:204–220. [DOI] [PubMed] [Google Scholar]
- 83.Seki Y, Hayashi K, Itoh K, Mizugaki M, Saitou M, Matsui Y. Extensive and orderly reprogramming of genome-wide chromatin modifications associated with specification and early development of germ cells in mice. Dev Biol 2005; 278:440–458. [DOI] [PubMed] [Google Scholar]
- 84.Gkountela S, Zhang KX, Shafiq TA, Liao WW, Hargan-Calvopina J, Chen PY, Clark AT. DNA demethylation dynamics in the human prenatal germline. Cell 2015; 161:1425–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kurimoto K, Yabuta Y, Hayashi K, Ohta H, Kiyonari H, Mitani T, Moritoki Y, Kohri K, Kimura H, Yamamoto T, Katou Y, Shirahige K et al. Quantitative dynamics of chromatin Remodeling during germ cell specification from mouse embryonic stem cells. Cell Stem Cell 2015; 16:517–532. [DOI] [PubMed] [Google Scholar]
- 86.Eguizabal C, Herrera L, De Onate L, Montserrat N, Hajkova P, Izpisua Belmonte JC. Characterization of the epigenetic changes during human gonadal primordial germ cells reprogramming. Stem Cells 2016; 34:2418–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.de Kretser DM, Loveland KL, Meinhardt A, Simorangkir D, Wreford N. Spermatogenesis. Hum Reprod 1998; 13:1–8. [DOI] [PubMed] [Google Scholar]
- 88.Griswold MD. Action of FSH on mammalial Sertoli cells. In: Russell L.D. GMD (ed.) The Sertoli Cell. Clearwater, FL: Cache River Press; 1993: 493–508. [Google Scholar]
- 89.Zirkin BR, Awoniyi C, Griswold MD, Russell LD, Sharpe R. Is FSH required for adult spermatogenesis? J Androl 1994; 15:273–276. [PubMed] [Google Scholar]
- 90.Abel MH, Baker PJ, Charlton HM, Monteiro A, Verhoeven G, De Gendt K, Guillou F, O'Shaughnessy PJ. Spermatogenesis and sertoli cell activity in mice lacking sertoli cell receptors for follicle-stimulating hormone and androgen. Endocrinology 2008; 149:3279–3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kumar TR, Wang Y, Lu N, Matzuk MM. Follicle stimulating hormone is required for ovarian follicle maturation but not male fertility. Nat Genet 1997; 15:201–204. [DOI] [PubMed] [Google Scholar]
- 92.Abel MH, Wootton AN, Wilkins V, Huhtaniemi I, Knight PG, Charlton HM. The effect of a null mutation in the follicle-stimulating hormone receptor gene on mouse reproduction. Endocrinology 2000; 141:1795–1803. [DOI] [PubMed] [Google Scholar]
- 93.Dierich A, Sairam MR, Monaco L, Fimia GM, Gansmuller A, LeMeur M, Sassone-Corsi P. Impairing follicle-stimulating hormone (FSH) signaling in vivo: Targeted disruption of the FSH receptor leads to aberrant gametogenesis and hormonal imbalance. Proc Natl Acad Sci U S A 1998; 95:13612–13617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wreford NG, Rajendra Kumar T, Matzuk MM, de Kretser DM. Analysis of the testicular phenotype of the follicle-stimulating hormone beta-subunit knockout and the activin type II receptor knockout mice by stereological analysis. Endocrinology 2001; 142:2916–2920. [DOI] [PubMed] [Google Scholar]
- 95.O'Shaughnessy PJ, Monteiro A, Verhoeven G, De Gendt K, Abel MH. Effect of FSH on testicular morphology and spermatogenesis in gonadotrophin-deficient hypogonadal mice lacking androgen receptors. Reproduction 2010; 139:177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Singh J, Handelsman DJ. The effects of recombinant FSH on testosterone-induced spermatogenesis in gonadotrophin-deficient (hpg) mice. J Androl 1996; 17:382–393. [PubMed] [Google Scholar]
- 97.Baines H, Nwagwu MO, Hastie GR, Wiles RA, Mayhew TM, Ebling FJ. Effects of estradiol and FSH on maturation of the testis in the hypogonadal (hpg) mouse. Reprod Biol Endocrinol 2008; 6:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Haywood M, Spaliviero J, Jimemez M, King NJ, Handelsman DJ, Allan CM. Sertoli and germ cell development in hypogonadal (hpg) mice expressing transgenic follicle-stimulating hormone alone or in combination with testosterone. Endocrinology 2003; 144:509–517. [DOI] [PubMed] [Google Scholar]
- 99.Rodriguez I, Ody C, Araki K, Garcia I, Vassalli P. An early and massive wave of germinal cell apoptosis is required for the development of functional spermatogenesis. EMBO J 1997; 16:2262–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.McLachlan RI, Wreford NG, de Kretser DM, Robertson DM. The effects of recombinant follicle-stimulating hormone on the restoration of spermatogenesis in the gonadotropin-releasing hormone-immunized adult rat. Endocrinology 1995; 136:4035–4043. [DOI] [PubMed] [Google Scholar]
- 101.Russell LD, Corbin TJ, Borg KE, De Franca LR, Grasso P, Bartke A. Recombinant human follicle-stimulating hormone is capable of exerting a biological effect in the adult hypophysectomized rat by reducing the numbers of degenerating germ cells. Endocrinology 1993; 133:2062–2070. [DOI] [PubMed] [Google Scholar]
- 102.Sun YT, Wreford NG, Robertson DM, de Kretser DM. Quantitative cytological studies of spermatogenesis in intact and hypophysectomized rats: Identification of androgen-dependent stages. Endocrinology 1990; 127:1215–1223. [DOI] [PubMed] [Google Scholar]
- 103.Ruwanpura SM, McLachlan RI, Stanton PG, Loveland KL, Meachem SJ. Pathways involved in testicular germ cell apoptosis in immature rats after FSH suppression. J Endocrinol 2008; 197:35–43. [DOI] [PubMed] [Google Scholar]
- 104.Ruwanpura SM, McLachlan RI, Stanton PG, Meachem SJ. Follicle-stimulating hormone affects spermatogonial survival by regulating the intrinsic apoptotic pathway in adult rats. Biol Reprod 2008; 78:705–713. [DOI] [PubMed] [Google Scholar]
- 105.Simorangkir DR, Ramaswamy S, Marshall GR, Pohl CR, Plant TM. A selective monotropic elevation of FSH, but not that of LH, amplifies the proliferation and differentiation of spermatogonia in the adult rhesus monkey (Macaca mulatta). Hum Reprod 2009; 24:1584–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Henriksen K, Kangasniemi M, Parvinen M, Kaipia A, Hakovirta H. In vitro, follicle-stimulating hormone prevents apoptosis and stimulates deoxyribonucleic acid synthesis in the rat seminiferous epithelium in a stage-specific fashion. Endocrinology 1996; 137:2141–2149. [DOI] [PubMed] [Google Scholar]
- 107.Skinner MK. Cell-cell interactions in the testis. Endocr Rev 1991; 12:45–77. [DOI] [PubMed] [Google Scholar]
- 108.Grover A, Sairam MR, Smith CE, Hermo L. Structural and functional modifications of sertoli cells in the testis of adult follicle-stimulating hormone receptor knockout mice. Biol Reprod 2004; 71:117–129. [DOI] [PubMed] [Google Scholar]
- 109.Hazra R, Corcoran L, Robson M, McTavish KJ, Upton D, Handelsman DJ, Allan CM. Temporal role of Sertoli cell androgen receptor expression in spermatogenic development. Mol Endocrinol 2013; 27:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pakarainen T, Zhang FP, Makela S, Poutanen M, Huhtaniemi I. Testosterone replacement therapy induces spermatogenesis and partially restores fertility in luteinizing hormone receptor knockout mice. Endocrinology 2005; 146:596–606. [DOI] [PubMed] [Google Scholar]
- 111.Cameron DF, Muffly KE, Nazian SJ. Reduced testosterone during puberty results in a midspermiogenic lesion. Proc Soc Exp Biol Med 1993; 202:457–464. [DOI] [PubMed] [Google Scholar]
- 112.Huang HF, Marshall GR, Rosenberg R, Nieschlag E. Restoration of spermatogenesis by high levels of testosterone in hypophysectomized rats after long-term regression. Acta Endocrinol 1987; 116:433–444. [DOI] [PubMed] [Google Scholar]
- 113.Sun YT, Irby DC, Robertson DM, de Kretser DM. The effects of exogenously administered testosterone on spermatogenesis in intact and hypophysectomized rats. Endocrinology 1989; 125:1000–1010. [DOI] [PubMed] [Google Scholar]
- 114.Awoniyi CA, Sprando RL, Santulli R, Chandrashekar V, Ewing LL, Zirkin BR. Restoration of spermatogenesis by exogenously administered testosterone in rats made azoospermic by hypophysectomy or withdrawal of luteinizing hormone alone. Endocrinology 1990; 127:177–184. [DOI] [PubMed] [Google Scholar]
- 115.Sharpe RM, Fraser HM, Ratnasooriya WD. Assessment of the role of Leydig cell products other than testosterone in spermatogenesis and fertility in adult rats. Int J Androl 1988; 11:507–523. [DOI] [PubMed] [Google Scholar]
- 116.O’Donnell L, Meachem SJ, Stanton PG, RI ML. CHAPTER 21- Endocrine Regulation of Spermatogenesis. In: Knobil and Neill's Physiology of Reproduction (Third Edition), Academic Press, Cambridge, MA, vol. 1. 2006: 1017–1069. [Google Scholar]
- 117.Russell LD, Clermont Y. Degeneration of germ cells in normal, hypophysectomized and hormone treated hypophysectomized rats. Anat Rec 1977; 187:347–366. [DOI] [PubMed] [Google Scholar]
- 118.O'Shaughnessy PJ, Monteiro A, Abel M. Testicular development in mice lacking receptors for follicle stimulating hormone and androgen. PLoS One 2012; 7:e35136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lyon MF, Hawkes SG. X-linked gene for testicular feminization in the mouse. Nature 1970; 227:1217–1219. [DOI] [PubMed] [Google Scholar]
- 120.Johnston H, Baker PJ, Abel M, Charlton HM, Jackson G, Fleming L, Kumar TR, O'Shaughnessy PJ. Regulation of Sertoli cell number and activity by follicle-stimulating hormone and androgen during postnatal development in the mouse. Endocrinology 2004; 145:318–329. [DOI] [PubMed] [Google Scholar]
- 121.De Gendt K, Swinnen JV, Saunders PT, Schoonjans L, Dewerchin M, Devos A, Tan K, Atanassova N, Claessens F, Lecureuil C, Heyns W, Carmeliet P et al. A Sertoli cell-selective knockout of the androgen receptor causes spermatogenic arrest in meiosis. Proc Natl Acad Sci U S A 2004; 101:1327–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lyon MF, Glenister PH, Lamoreux ML. Normal spermatozoa from androgen-resistant germ cells of chimaeric mice and the role of androgen in spermatogenesis. Nature 1975; 258:620–622. [DOI] [PubMed] [Google Scholar]
- 123.Johnston DS, Russell LD, Friel PJ, Griswold MD. Murine germ cells do not require functional androgen receptors to complete spermatogenesis following spermatogonial stem cell transplantation. Endocrinology 2001; 142:2405–2408. [DOI] [PubMed] [Google Scholar]
- 124.Allan CM, Couse JF, Simanainen U, Spaliviero J, Jimenez M, Rodriguez K, Korach KS, Handelsman DJ. Estradiol induction of spermatogenesis is mediated via an estrogen receptor-{alpha} mechanism involving neuroendocrine activation of follicle-stimulating hormone secretion. Endocrinology 2010; 151:2800–2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ebling FJ, Brooks AN, Cronin AS, Ford H, Kerr JB. Estrogenic induction of spermatogenesis in the hypogonadal mouse. Endocrinology 2000; 141:2861–2869. [DOI] [PubMed] [Google Scholar]
- 126.Hunt DM, Saksena SK, Chang MC. Effects of estradiol-17 beta on reproduction in adult male rats. Arch Androl 1979; 2:129–133. [DOI] [PubMed] [Google Scholar]
- 127.Zondek B. Mass excretion of Œstrogenic hormone in the urine of the stallion. Nature 1934; 133:209–210. [Google Scholar]
- 128.Dorrington JH, Fritz IB, Armstrong DT. Control of testicular estrogen synthesis. Biol Reprod 1978; 18:55–64. [DOI] [PubMed] [Google Scholar]
- 129.Carreau S, Bouraima-Lelong H, Delalande C. Estrogen, a female hormone involved in spermatogenesis. Adv Med Sci 2012; 57:31–36. [DOI] [PubMed] [Google Scholar]
- 130.Chimento A, Sirianni R, Delalande C, Silandre D, Bois C, Ando S, Maggiolini M, Carreau S, Pezzi V. 17 beta-estradiol activates rapid signaling pathways involved in rat pachytene spermatocytes apoptosis through GPR30 and ER alpha. Mol Cell Endocrinol 2010; 320:136–144. [DOI] [PubMed] [Google Scholar]
- 131.Robertson KM, O'Donnell L, Jones ME, Meachem SJ, Boon WC, Fisher CR, Graves KH, McLachlan RI, Simpson ER. Impairment of spermatogenesis in mice lacking a functional aromatase (cyp 19) gene. Proc Natl Acad Sci U S A 1999; 96:7986–7991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sinkevicius KW, Laine M, Lotan TL, Woloszyn K, Richburg JH, Greene GL. Estrogen-dependent and -independent estrogen receptor-alpha signaling separately regulate male fertility. Endocrinology 2009; 150:2898–2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Cacciola G, Chioccarelli T, Fasano S, Pierantoni R, Cobellis G. Estrogens and spermiogenesis: New insights from type 1 cannabinoid receptor knockout mice. Int J Endocrinol 2013; 2013:501350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shetty G, Weng CC, Bolden-Tiller OU, Huhtaniemi I, Handelsman DJ, Meistrich ML. Effects of medroxyprogesterone and estradiol on the recovery of spermatogenesis in irradiated rats. Endocrinology 2004; 145:4461–4469. [DOI] [PubMed] [Google Scholar]
- 135.Porter KL, Shetty G, Shuttlesworth GA, Weng CC, Huhtaniemi I, Pakarinen P, Meistrich ML. Estrogen enhances recovery from radiation-induced spermatogonial arrest in rat testes. J Androl 2009; 30:440–451. [DOI] [PubMed] [Google Scholar]
- 136.Hedger MP, Winnall WR. Regulation of activin and inhibin in the adult testis and the evidence for functional roles in spermatogenesis and immunoregulation. Mol Cell Endocrinol 2012; 359:30–42. [DOI] [PubMed] [Google Scholar]
- 137.Hakovirta H, Kaipia A, Soder O, Parvinen M. Effects of activin-a, inhibin-a, and transforming growth factor-beta 1 on stage-specific deoxyribonucleic acid synthesis during rat seminiferous epithelial cycle. Endocrinology 1993; 133:1664–1668. [DOI] [PubMed] [Google Scholar]
- 138.Mather JP, Attie KM, Woodruff TK, Rice GC, Phillips DM. Activin stimulates spermatogonial proliferation in germ-Sertoli cell cocultures from immature rat testis. Endocrinology 1990; 127:3206–3214. [DOI] [PubMed] [Google Scholar]
- 139.Nagano M, Ryu BY, Brinster CJ, Avarbock MR, Brinster RL. Maintenance of mouse male germ line stem cells in vitro. Biol Reprod 2003; 68:2207–2214. [DOI] [PubMed] [Google Scholar]
- 140.Guo Q, Kumar TR, Woodruff T, Hadsell LA, DeMayo FJ, Matzuk MM. Overexpression of mouse follistatin causes reproductive defects in transgenic mice. Mol Endocrinol 1998; 12:96–106. [DOI] [PubMed] [Google Scholar]
- 141.Oldknow KJ, Seebacher J, Goswami T, Villen J, Pitsillides AA, O'Shaughnessy PJ, Gygi SP, Schneyer AL, Mukherjee A. Follistatin-like 3 (FSTL3) mediated silencing of transforming growth factor beta (TGFbeta) signaling is essential for testicular aging and regulating testis size. Endocrinology 2013; 154:1310–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Heller CH, Clermont Y. Kinetics of the germinal epithelium in man. Recent Prog Horm Res 1964; 20:545–575. [PubMed] [Google Scholar]
- 143.Reith DA, Bernstein A. Molecular biology of the W and Steel loci. Genome Anal 1991; 3:105–133. [Google Scholar]
- 144.Munsie M, Schlatt S, deKretser DM, Loveland KL. Expression of stem cell factor in the postnatal rat testis. Mol Reprod Dev 1997; 47:19–25. [DOI] [PubMed] [Google Scholar]
- 145.Cupp AS, Skinner MK. Expression, action, and regulation of transforming growth factor alpha and epidermal growth factor receptor during embryonic and perinatal rat testis development. J Androl 2001; 22:1019–1029. [DOI] [PubMed] [Google Scholar]
- 146.Cupp AS, Tessarollo L, Skinner MK. Testis developmental phenotypes in neurotropin receptor trkA and trkC null mutations: Role in formation of seminiferous cords and germ cell survival. Biol Reprod 2002; 66:1838–1845. [DOI] [PubMed] [Google Scholar]
- 147.Packer AI, Besmer P, Bachvarova RF. Kit ligand mediates survival of type a spermatogonia and dividing spermatocytes in postnatal mouse testes. Mol Reprod Dev 1995; 42:303–310. [DOI] [PubMed] [Google Scholar]
- 148.Shetty J, Marathe GK, Dighe RR. Specific immunoneutralization of FSH leads to apoptotic cell death of the pachytene spermatocytes and spermatogonial cells in the rat. Endocrinology 1996; 137:2179–2182. [DOI] [PubMed] [Google Scholar]
- 149.Oatley JM, Avarbock MR, Brinster RL. Glial cell line-derived neurotrophic factor regulation of genes essential for self-renewal of mouse spermatogonial stem cells is dependent on Src family kinase signaling. J Biol Chem 2007; 282:25842–25851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Oatley JM, Oatley MJ, Avarbock MR, Tobias JW, Brinster RL. Colony stimulating factor 1 is an extrinsic stimulator of mouse spermatogonial stem cell self-renewal. Development 2009; 136:1191–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Oatley MJ, Kaucher AV, Racicot KE, Oatley JM. Inhibitor of DNA binding 4 is expressed selectively by single spermatogonia in the male germline and regulates the self-renewal of spermatogonial stem cells in mice. Biol Reprod 2011; 85:347–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ciccarelli M, Giassetti MI, Miao D, Oatley MJ, Robbins C, Lopez-Biladeau B, Waqas MS, Tibary A, Whitelaw B, Lillico S, Park CH, Park KE et al. Donor-derived spermatogenesis following stem cell transplantation in sterile NANOS2 knockout males. Proc Natl Acad Sci U S A 2020; 117:24195–24204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hermann BP, Cheng K, Singh A, Roa-De La Cruz L, Mutoji KN, Chen IC, Gildersleeve H, Lehle JD, Mayo M, Westernstroer B, Law NC, Oatley MJ et al. The mammalian spermatogenesis single-cell transcriptome, from Spermatogonial stem cells to spermatids. Cell Rep 2018; 25:1650–1667 e1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Griswold MD, Oatley JM. Concise review: Defining characteristics of mammalian spermatogenic stem cells. Stem Cells 2013; 31:8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Leslie M. EPIGENETICS. Sperm RNA fragments modify offspring metabolism. Science 2016; 351:13. [DOI] [PubMed] [Google Scholar]
- 156.Nilsson E, Sadler-Riggleman I, Skinner MK. Environmentally induced epigenetic transgenerational inheritance of disease. Environmental Epigenetics 2018; 4:1, dvy016–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Anway MD, Cupp AS, Uzumcu M, Skinner MK. Epigenetic transgenerational actions of endocrine disruptors and male fertility. Science 2005; 308:1466–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Sharma U, Conine CC, Shea JM, Boskovic A, Derr AG, Bing XY, Belleannee C, Kucukural A, Serra RW, Sun F, Song L, Carone BR et al. Biogenesis and function of tRNA fragments during sperm maturation and fertilization in mammals. Science 2016; 351:391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Chen Q, Yan M, Cao Z, Li X, Zhang Y, Shi J, Feng GH, Peng H, Zhang X, Zhang Y, Qian J, Duan E et al. Sperm tsRNAs contribute to intergenerational inheritance of an acquired metabolic disorder. Science 2016; 351:397–400. [DOI] [PubMed] [Google Scholar]
- 160.Aravin AA, Sachidanandam R, Bourc'his D, Schaefer C, Pezic D, Toth KF, Bestor T, Hannon GJ. A piRNA pathway primed by individual transposons is linked to de novo DNA methylation in mice. Mol Cell 2008; 31:785–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Stalker L, Russell SJ, Co C, Foster RA, LaMarre J. PIWIL1 is expressed in the canine testis, increases with sexual maturity, and binds small RNAs. Biol Reprod 2016; 94:17. [DOI] [PubMed] [Google Scholar]
- 162.Ben Maamar M, Beck D, Nilsson E, McCarrey JR, Skinner MK. Developmental alterations in DNA methylation during gametogenesis from primordial germ cells to sperm. Dev Biol 2021; Second revision submitted and publication pending. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Vreeburg JT, Holland MK, Cornwall GA, Rankin TL, Orgebin-Crist MC. Secretion of epididymal proteins and their interactions with spermatozoa. Bull Assoc Anat (Nancy) 1991; 75:171–173. [PubMed] [Google Scholar]
- 164.Cornwall GA. Role of posttranslational protein modifications in epididymal sperm maturation and extracellular quality control. Adv Exp Med Biol 2014; 759:159–180. [DOI] [PubMed] [Google Scholar]
- 165.Austin CR. Observations on the penetration of the sperm in the mammalian egg. Aust J Sci Res B 1951; 4:581–596. [DOI] [PubMed] [Google Scholar]
- 166.Chang MC. Fertilizing capacity of spermatozoa deposited into the fallopian tubes. Nature 1951; 168:697–698. [DOI] [PubMed] [Google Scholar]
- 167.Young LG, Hinton BT, Gould KG. Surface changes in chimpanzee sperm during epididymal transit. Biol Reprod 1985; 32:399–412. [DOI] [PubMed] [Google Scholar]
- 168.Han Y, Haines CJ, Feng HL. Role(s) of the serine/threonine protein phosphatase 1 on mammalian sperm motility. Arch Androl 2007; 53:169–177. [DOI] [PubMed] [Google Scholar]
- 169.James ER, Carrell DT, Aston KI, Jenkins TG, Yeste M, Salas-Huetos A. The role of the epididymis and the contribution of Epididymosomes to mammalian reproduction. Int J Mol Sci 2020; 21:5377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sullivan R, Legare C, Lamontagne-Proulx J, Breton S, Soulet D. Revisiting structure/functions of the human epididymis. Andrology 2019; 7:748–757. [DOI] [PubMed] [Google Scholar]
- 171.Sharma A. Transgenerational epigenetics: Integrating soma to germline communication with gametic inheritance. Mech Ageing Dev 2017; 163:15–22. [DOI] [PubMed] [Google Scholar]
- 172.Conine CC, Sun F, Song L, Rivera-Perez JA, Rando OJ. MicroRNAs absent in caput sperm are required for normal embryonic development. Dev Cell 2019; 50:7–8. [DOI] [PubMed] [Google Scholar]
- 173.Chu C, Zhang YL, Yu L, Sharma S, Fei ZL, Drevet JR. Epididymal small non-coding RNA studies: Progress over the past decade. Andrology 2019; 7:681–689. [DOI] [PubMed] [Google Scholar]
- 174.Sharma U. Paternal contributions to offspring health: Role of sperm small RNAs in intergenerational transmission of epigenetic information. Front Cell Dev Biol 2019; 7:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Scott IM, Rubinstein GM, Poole FL 2nd, Lipscomb GL, Schut GJ, Williams-Rhaesa AM, Stevenson DM, Amador-Noguez D, Kelly RM, Adams MWW. The thermophilic biomass-degrading bacterium Caldicellulosiruptor bescii utilizes two enzymes to oxidize glyceraldehyde 3-phosphate during glycolysis. J Biol Chem 2019; 294:9995–10005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ben Maamar M, Nilsson E, Sadler-Riggleman I, Beck D, McCarrey JR, Skinner MK. Developmental origins of transgenerational sperm DNA methylation epimutations following ancestral DDT exposure. Dev Biol 2019; 445:280–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Ben Maamar M, Beck D, Nilsson E, McCarrey JR, Skinner MK. Developmental origins of transgenerational sperm histone retention following ancestral exposures. Dev Biol 2020; 465:31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Sanchez F, Smitz J. Molecular control of oogenesis. Biochim Biophys Acta 1822; 2012:1896–1912. [DOI] [PubMed] [Google Scholar]
- 179.Mehlmann LM. Stops and starts in mammalian oocytes: Recent advances in understanding the regulation of meiotic arrest and oocyte maturation. Reproduction 2005; 130:791–799. [DOI] [PubMed] [Google Scholar]
- 180.Rajah R, Glaser EM, Hirshfield AN. The changing architecture of the neonatal rat ovary during histogenesis. Dev Dyn 1992; 194:177–192. [DOI] [PubMed] [Google Scholar]
- 181.El-Hayek S, Clarke HJ. Control of oocyte growth and development by intercellular communication within the follicular niche. Results Probl Cell Differ 2016; 58:191–224. [DOI] [PubMed] [Google Scholar]
- 182.Buccione R, Schroeder AC, Eppig JJ. Interactions between somatic cells and germ cells throughout mammalian oogenesis. Biol Reprod 1990; 43:543–547. [DOI] [PubMed] [Google Scholar]
- 183.Kezele P, Nilsson E, Skinner MK. Cell-cell interactions in primordial follicle assembly and development. Front Biosci 2002; 7:d1990–d1996. [DOI] [PubMed] [Google Scholar]
- 184.Grive KJ. Pathways coordinating oocyte attrition and abundance during mammalian ovarian reserve establishment. Mol Reprod Dev 2020; 87:843–856. [DOI] [PubMed] [Google Scholar]
- 185.Chen Y, Yang W, Shi X, Zhang C, Song G, Huang D. The factors and pathways regulating the activation of mammalian primordial follicles in vivo. Front Cell Dev Biol 2020; 8:575706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Skinner MK. Regulation of primordial follicle assembly and development. Hum Reprod Update 2005; 11:461–471. [DOI] [PubMed] [Google Scholar]
- 187.Gougeon A. Human ovarian follicular development: From activation of resting follicles to preovulatory maturation. Ann Endocrinol (Paris) 2010; 71:132–143. [DOI] [PubMed] [Google Scholar]
- 188.Rodgers RJ, Irving-Rodgers HF. Formation of the ovarian follicular antrum and follicular fluid. Biol Reprod 2010; 82:1021–1029. [DOI] [PubMed] [Google Scholar]
- 189.Son WY, Das M, Shalom-Paz E, Holzer H. Mechanisms of follicle selection and development. Minerva Ginecol 2011; 63:89–102. [PubMed] [Google Scholar]
- 190.Craig J, Orisaka M, Wang H, Orisaka S, Thompson W, Zhu C, Kotsuji F, Tsang BK. Gonadotropin and intra-ovarian signals regulating follicle development and atresia: The delicate balance between life and death. Front Biosci 2007; 12:3628–3639. [DOI] [PubMed] [Google Scholar]
- 191.Marcozzi S, Rossi V, Salustri A, De Felici M, Klinger FG. Programmed cell death in the human ovary. Minerva Ginecol 2018; 70:549–560. [DOI] [PubMed] [Google Scholar]
- 192.Sen A, Caiazza F. Oocyte maturation: A story of arrest and release. Front Biosci (Schol Ed) 2013; 5:451–477. [DOI] [PubMed] [Google Scholar]
- 193.Georgadaki K, Khoury N, Spandidos DA, Zoumpourlis V. The molecular basis of fertilization (review). Int J Mol Med 2016; 38:979–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Bhakta HH, Refai FH, Avella MA. The molecular mechanisms mediating mammalian fertilization. Development 2019; 146:dev176966. [DOI] [PubMed] [Google Scholar]
- 195.Svoboda P. Mammalian zygotic genome activation. Semin Cell Dev Biol 2018; 84:118–126. [DOI] [PubMed] [Google Scholar]
- 196.Schulz KN, Harrison MM. Mechanisms regulating zygotic genome activation. Nat Rev Genet 2019; 20:221–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Grossman H, Shalgi R. A role of MicroRNAs in cell differentiation during gonad development. Results Probl Cell Differ 2016; 58:309–336. [DOI] [PubMed] [Google Scholar]
- 198.Liang Y, Ridzon D, Wong L, Chen C. Characterization of microRNA expression profiles in normal human tissues. BMC Genomics 2007; 8:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Ro S, Song R, Park C, Zheng H, Sanders KM, Yan W. Cloning and expression profiling of small RNAs expressed in the mouse ovary. RNA 2007; 13:2366–2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Yao G, Liang M, Liang N, Yin M, Lu M, Lian J, Wang Y, Sun F. MicroRNA-224 is involved in the regulation of mouse cumulus expansion by targeting Ptx3. Mol Cell Endocrinol 2014; 382:244–253. [DOI] [PubMed] [Google Scholar]
- 201.Tomizawa S, Nowacka-Woszuk J, Kelsey G. DNA methylation establishment during oocyte growth: Mechanisms and significance. Int J Dev Biol 2012; 56:867–875. [DOI] [PubMed] [Google Scholar]
- 202.Sendzikaite G, Kelsey G. The role and mechanisms of DNA methylation in the oocyte. Essays Biochem 2019; 63:691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Sha QQ, Zhang J, Fan HY. Function and regulation of histone H3 Lysine-4 methylation during oocyte meiosis and maternal-to-zygotic transition. Front Cell Dev Biol 2020; 8:597498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Yu C, Fan X, Sha QQ, Wang HH, Li BT, Dai XX, Shen L, Liu J, Wang L, Liu K, Tang F, Fan HY. CFP1 regulates histone H3K4 Trimethylation and developmental potential in mouse oocytes. Cell Rep 2017; 20:1161–1172. [DOI] [PubMed] [Google Scholar]
- 205.Sha QQ, Dai XX, Jiang JC, Yu C, Jiang Y, Liu J, Ou XH, Zhang SY, Fan HY. CFP1 coordinates histone H3 lysine-4 trimethylation and meiotic cell cycle progression in mouse oocytes. Nat Commun 2018; 9:3477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Andreu-Vieyra CV, Chen R, Agno JE, Glaser S, Anastassiadis K, Stewart AF, Matzuk MM. MLL2 is required in oocytes for bulk histone 3 lysine 4 trimethylation and transcriptional silencing. PLoS Biol 2010; 8:e1000453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Yamashiro C, Sasaki K, Yabuta Y, Kojima Y, Nakamura T, Okamoto I, Yokobayashi S, Murase Y, Ishikura Y, Shirane K, Sasaki H, Yamamoto T et al. Generation of human oogonia from induced pluripotent stem cells in vitro. Science 2018; 362:356–360. [DOI] [PubMed] [Google Scholar]
- 208.Okae H, Chiba H, Hiura H, Hamada H, Sato A, Utsunomiya T, Kikuchi H, Yoshida H, Tanaka A, Suyama M, Arima T. Genome-wide analysis of DNA methylation dynamics during early human development. PLoS Genet 2014; 10:e1004868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.von Meyenn F, Berrens RV, Andrews S, Santos F, Collier AJ, Krueger F, Osorno R, Dean W, Rugg-Gunn PJ, Reik W. Comparative principles of DNA methylation reprogramming during human and mouse in vitro primordial germ cell specification. Dev Cell 2016; 39:104–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Pokholok DK, Harbison CT, Levine S, Cole M, Hannett NM, Lee TI, Bell GW, Walker K, Rolfe PA, Herbolsheimer E, Zeitlinger J, Lewitter F et al. Genome-wide map of nucleosome acetylation and methylation in yeast. Cell 2005; 122:517–527. [DOI] [PubMed] [Google Scholar]
- 211.Boland MJ, Nazor KL, Loring JF. Epigenetic regulation of pluripotency and differentiation. Circ Res 2014; 115:311–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Avgustinova A, Benitah SA. Epigenetic control of adult stem cell function. Nat Rev Mol Cell Biol 2016; 17:643–658. [DOI] [PubMed] [Google Scholar]
- 213.Kato Y, Kaneda M, Hata K, Kumaki K, Hisano M, Kohara Y, Okano M, Li E, Nozaki M, Sasaki H. Role of the Dnmt3 family in de novo methylation of imprinted and repetitive sequences during male germ cell development in the mouse. Hum Mol Genet 2007; 16:2272–2280. [DOI] [PubMed] [Google Scholar]
- 214.Li JY, Lees-Murdock DJ, Xu GL, Walsh CP. Timing of establishment of paternal methylation imprints in the mouse. Genomics 2004; 84:952–960. [DOI] [PubMed] [Google Scholar]
- 215.Bestor TH, Bourc'his D. Transposon silencing and imprint establishment in mammalian germ cells. Cold Spring Harb Symp Quant Biol 2004; 69:381–387. [DOI] [PubMed] [Google Scholar]
- 216.Bourc'his D, Xu GL, Lin CS, Bollman B, Bestor TH. Dnmt3L and the establishment of maternal genomic imprints. Science 2001; 294:2536–2539. [DOI] [PubMed] [Google Scholar]
- 217.Kaneda M, Okano M, Hata K, Sado T, Tsujimoto N, Li E, Sasaki H. Essential role for de novo DNA methyltransferase Dnmt3a in paternal and maternal imprinting. Nature 2004; 429:900–903. [DOI] [PubMed] [Google Scholar]
- 218.Smallwood SA, Tomizawa S, Krueger F, Ruf N, Carli N, Segonds-Pichon A, Sato S, Hata K, Andrews SR, Kelsey G. Dynamic CpG island methylation landscape in oocytes and preimplantation embryos. Nat Genet 2011; 43:811–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Marston AL, Amon A. Meiosis: Cell-cycle controls shuffle and deal. Nat Rev Mol Cell Biol 2004; 5:983–997. [DOI] [PubMed] [Google Scholar]
- 220.Kota SK, Feil R. Epigenetic transitions in germ cell development and meiosis. Dev Cell 2010; 19:675–686. [DOI] [PubMed] [Google Scholar]
- 221.Baudat F, Manova K, Yuen JP, Jasin M, Keeney S. Chromosome synapsis defects and sexually dimorphic meiotic progression in mice lacking Spo11. Mol Cell 2000; 6:989–998. [DOI] [PubMed] [Google Scholar]
- 222.Zelazowski MJ, Sandoval M, Paniker L, Hamilton HM, Han J, Gribbell MA, Kang R, Cole F. Age-dependent alterations in meiotic recombination cause chromosome segregation errors in spermatocytes. Cell 2017; 171:601–614 e613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Baudat F, Buard J, Grey C, Fledel-Alon A, Ober C, Przeworski M, Coop G, de Massy B. PRDM9 is a major determinant of meiotic recombination hotspots in humans and mice. Science 2010; 327:836–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hayashi K, Yoshida K, Matsui Y. A histone H3 methyltransferase controls epigenetic events required for meiotic prophase. Nature 2005; 438:374–378. [DOI] [PubMed] [Google Scholar]
- 225.Jeffreys AJ, Kauppi L, Neumann R. Intensely punctate meiotic recombination in the class II region of the major histocompatibility complex. Nat Genet 2001; 29:217–222. [DOI] [PubMed] [Google Scholar]
- 226.McVean GA, Myers SR, Hunt S, Deloukas P, Bentley DR, Donnelly P. The fine-scale structure of recombination rate variation in the human genome. Science 2004; 304:581–584. [DOI] [PubMed] [Google Scholar]
- 227.Myers S, Bottolo L, Freeman C, McVean G, Donnelly P. A fine-scale map of recombination rates and hotspots across the human genome. Science 2005; 310:321–324. [DOI] [PubMed] [Google Scholar]
- 228.Parvanov ED, Petkov PM, Paigen K. Prdm9 controls activation of mammalian recombination hotspots. Science 2010; 327:835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gong F, Miller KM. Mammalian DNA repair: HATs and HDACs make their mark through histone acetylation. Mutat Res 2013; 750:23–30. [DOI] [PubMed] [Google Scholar]
- 230.Hirota K, Mizuno K, Shibata T, Ohta K. Distinct chromatin modulators regulate the formation of accessible and repressive chromatin at the fission yeast recombination hotspot ade6-M26. Mol Biol Cell 2008; 19:1162–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Sollier J, Lin W, Soustelle C, Suhre K, Nicolas A, Geli V, de La Roche Saint-Andre C. Set1 is required for meiotic S-phase onset, double-strand break formation and middle gene expression. EMBO J 2004; 23:1957–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yamashita K, Shinohara M, Shinohara A. Rad6-Bre1-mediated histone H2B ubiquitylation modulates the formation of double-strand breaks during meiosis. Proc Natl Acad Sci U S A 2004; 101:11380–11385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Hanna CW, Taudt A, Huang J, Gahurova L, Kranz A, Andrews S, Dean W, Stewart AF, Colome-Tatche M, Kelsey G. MLL2 conveys transcription-independent H3K4 trimethylation in oocytes. Nat Struct Mol Biol 2018; 25:73–82. [DOI] [PubMed] [Google Scholar]
- 234.Stewart KR, Veselovska L, Kim J, Huang J, Saadeh H, Tomizawa S, Smallwood SA, Chen T, Kelsey G. Dynamic changes in histone modifications precede de novo DNA methylation in oocytes. Genes Dev 2015; 29:2449–2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Rando OJ. Intergenerational transfer of epigenetic information in sperm. Cold Spring Harb Perspect Med 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Bao J, Bedford MT. Epigenetic regulation of the histone-to-protamine transition during spermiogenesis. Reproduction 2016; 151:R55–R70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Barral S, Morozumi Y, Tanaka H, Montellier E, Govin J, de Dieuleveult M, Charbonnier G, Coute Y, Puthier D, Buchou T, Boussouar F, Urahama T et al. Histone variant H2A.L.2 guides transition protein-dependent protamine assembly in male germ cells. Mol Cell 2017; 66:89–101 e108. [DOI] [PubMed] [Google Scholar]
- 238.Hoghoughi N, Barral S, Vargas A, Rousseaux S, Khochbin S. Histone variants: Essential actors in male genome programming. J Biochem 2018; 163:97–103. [DOI] [PubMed] [Google Scholar]
- 239.Furrer R. Physical characteristics of mouse sperm nuclei. Biophys J 1976; 16:811–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Hud NV, Allen MJ, Downing KH, Lee J, Balhorn R. Identification of the elemental packing unit of DNA in mammalian sperm cells by atomic force microscopy. Biochem Biophys Res Commun 1993; 193:1347–1354. [DOI] [PubMed] [Google Scholar]
- 241.Brykczynska U, Hisano M, Erkek S, Ramos L, Oakeley EJ, Roloff TC, Beisel C, Schubeler D, Stadler MB, Peters AH. Repressive and active histone methylation mark distinct promoters in human and mouse spermatozoa. Nat Struct Mol Biol 2010; 17:679–687. [DOI] [PubMed] [Google Scholar]
- 242.Hammoud SS, Nix DA, Zhang H, Purwar J, Carrell DT, Cairns BR. Distinctive chromatin in human sperm packages genes for embryo development. Nature 2009; 460:473–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Ihara M, Meyer-Ficca ML, Leu NA, Rao S, Li F, Gregory BD, Zalenskaya IA, Schultz RM, Meyer RG. Paternal poly (ADP-ribose) metabolism modulates retention of inheritable sperm histones and early embryonic gene expression. PLoS Genet 2014; 10:e1004317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Siklenka K, Erkek S, Godmann M, Lambrot R, McGraw S, Lafleur C, Cohen T, Xia J, Suderman M, Hallett M, Trasler J, Peters AH et al. Disruption of histone methylation in developing sperm impairs offspring health transgenerationally. Science 2015, 2001-2014; 350:aab2006. [DOI] [PubMed] [Google Scholar]
- 245.Larriba E, del Mazo J. Role of non-coding RNAs in the transgenerational epigenetic transmission of the effects of Reprotoxicants. Int J Mol Sci 2016; 17:452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Bhin J, Jeong HS, Kim JS, Shin JO, Hong KS, Jung HS, Kim C, Hwang D, Kim KS. PGC-enriched miRNAs control germ cell development. Mol Cells 2015; 38:895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Medeiros LA, Dennis LM, Gill ME, Houbaviy H, Markoulaki S, Fu D, White AC, Kirak O, Sharp PA, Page DC, Jaenisch R. Mir-290-295 deficiency in mice results in partially penetrant embryonic lethality and germ cell defects. Proc Natl Acad Sci U S A 2011; 108:14163–14168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Takada S, Berezikov E, Choi YL, Yamashita Y, Mano H. Potential role of miR-29b in modulation of Dnmt3a and Dnmt3b expression in primordial germ cells of female mouse embryos. RNA 2009; 15:1507–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Zhang J, Liu W, Jin Y, Jia P, Jia K, Yi M. MiR-202-5p is a novel germ plasm-specific microRNA in zebrafish. Sci Rep 2017; 7:7055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Staton AA, Knaut H, Giraldez AJ. miRNA regulation of Sdf1 chemokine signaling provides genetic robustness to germ cell migration. Nat Genet 2011; 43:204–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Yu M, Mu H, Niu Z, Chu Z, Zhu H, Hua J. miR-34c enhances mouse spermatogonial stem cells differentiation by targeting Nanos2. J Cell Biochem 2014; 115:232–242. [DOI] [PubMed] [Google Scholar]
- 252.Liang X, Zhou D, Wei C, Luo H, Liu J, Fu R, Cui S. MicroRNA-34c enhances murine male germ cell apoptosis through targeting ATF1. PLoS One 2012; 7:e33861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Bouhallier F, Allioli N, Lavial F, Chalmel F, Perrard MH, Durand P, Samarut J, Pain B, Rouault JP. Role of miR-34c microRNA in the late steps of spermatogenesis. RNA 2010; 16:720–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.McIver SC, Stanger SJ, Santarelli DM, Roman SD, Nixon B, McLaughlin EA. A unique combination of male germ cell miRNAs coordinates gonocyte differentiation. PLoS One 2012; 7:e35553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Tong MH, Mitchell D, Evanoff R, Griswold MD. Expression of Mirlet7 family microRNAs in response to retinoic acid-induced spermatogonial differentiation in mice. Biol Reprod 2011; 85:189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Huszar JM, Payne CJ. MicroRNA 146 (Mir146) modulates spermatogonial differentiation by retinoic acid in mice. Biol Reprod 2013; 88:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Bao J, Li D, Wang L, Wu J, Hu Y, Wang Z, Chen Y, Cao X, Jiang C, Yan W, Xu C. MicroRNA-449 and microRNA-34b/c function redundantly in murine testes by targeting E2F transcription factor-retinoblastoma protein (E2F-pRb) pathway. J Biol Chem 2012; 287:21686–21698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Chen X, Li X, Guo J, Zhang P, Zeng W. The roles of microRNAs in regulation of mammalian spermatogenesis. J Anim Sci Biotechnol 2017; 8:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Weick EM, Miska EA. piRNAs: From biogenesis to function. Development 2014; 141:3458–3471. [DOI] [PubMed] [Google Scholar]
- 260.Ku HY, Lin H. PIWI proteins and their interactors in piRNA biogenesis, germline development and gene expression. Natl Sci Rev 2014; 1:205–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Houwing S, Kamminga LM, Berezikov E, Cronembold D, Girard A, van den Elst H, Filippov DV, Blaser H, Raz E, Moens CB, Plasterk RH, Hannon GJ et al. A role for Piwi and piRNAs in germ cell maintenance and transposon silencing in zebrafish. Cell 2007; 129:69–82. [DOI] [PubMed] [Google Scholar]
- 262.Taylor DH, Chu ET, Spektor R, Soloway PD. Long non-coding RNA regulation of reproduction and development. Mol Reprod Dev 2015; 82:932–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Zhang C, Gao L, Xu EY. LncRNA, a new component of expanding RNA-protein regulatory network important for animal sperm development. Semin Cell Dev Biol 2016; 59:110–117. [DOI] [PubMed] [Google Scholar]
- 264.Anguera MC, Ma W, Clift D, Namekawa S, Kelleher RJ 3rd, Lee JT. Tsx produces a long noncoding RNA and has general functions in the germline, stem cells, and brain. PLoS Genet 2011; 7:e1002248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Nolasco S, Bellido J, Goncalves J, Tavares A, Zabala JC, Soares H. The expression of tubulin cofactor a (TBCA) is regulated by a noncoding antisense Tbca RNA during testis maturation. PLoS One 2012; 7:e42536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Lu M, Tian H, Cao YX, He X, Chen L, Song X, Ping P, Huang H, Sun F. Downregulation of miR-320a/383-sponge-like long non-coding RNA NLC1-C (narcolepsy candidate-region 1 genes) is associated with male infertility and promotes testicular embryonal carcinoma cell proliferation. Cell Death Dis 2015; 6:e1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Li M, Liu Y, Wang T, Guan J, Luo Z, Chen H, Wang X, Chen L, Ma J, Mu Z, Jiang AA, Zhu L et al. Repertoire of porcine microRNAs in adult ovary and testis by deep sequencing. Int J Biol Sci 2011; 7:1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Ling YH, Ren CH, Guo XF, Xu LN, Huang YF, Luo JC, Zhang YH, Zhang XR, Zhang ZJ. Identification and characterization of microRNAs in the ovaries of multiple and uniparous goats (Capra hircus) during follicular phase. BMC Genomics 2014; 15:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Hossain MM, Ghanem N, Hoelker M, Rings F, Phatsara C, Tholen E, Schellander K, Tesfaye D. Identification and characterization of miRNAs expressed in the bovine ovary. BMC Genomics 2009; 10:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Hong X, Luense LJ, McGinnis LK, Nothnick WB, Christenson LK. Dicer1 is essential for female fertility and normal development of the female reproductive system. Endocrinology 2008; 149:6207–6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Nagaraja AK, Andreu-Vieyra C, Franco HL, Ma L, Chen R, Han DY, Zhu H, Agno JE, Gunaratne PH, DeMayo FJ, Matzuk MM. Deletion of dicer in somatic cells of the female reproductive tract causes sterility. Mol Endocrinol 2008; 22:2336–2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Gonzalez G, Behringer RR. Dicer is required for female reproductive tract development and fertility in the mouse. Mol Reprod Dev 2009; 76:678–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Cui N, Hao G, Zhao Z, Wang F, Cao J, Yang A. MicroRNA-224 regulates self-renewal of mouse spermatogonial stem cells via targeting DMRT1. J Cell Mol Med 2016; 20:1503–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Yan G, Zhang L, Fang T, Zhang Q, Wu S, Jiang Y, Sun H, Hu Y. MicroRNA-145 suppresses mouse granulosa cell proliferation by targeting activin receptor IB. FEBS Lett 2012; 586:3263–3270. [DOI] [PubMed] [Google Scholar]
- 275.Dai A, Sun H, Fang T, Zhang Q, Wu S, Jiang Y, Ding L, Yan G, Hu Y. MicroRNA-133b stimulates ovarian estradiol synthesis by targeting Foxl2. FEBS Lett 2013; 587:2474–2482. [DOI] [PubMed] [Google Scholar]
- 276.Zhang Q, Sun H, Jiang Y, Ding L, Wu S, Fang T, Yan G, Hu Y. MicroRNA-181a suppresses mouse granulosa cell proliferation by targeting activin receptor IIA. PLoS One 2013; 8:e59667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Carletti MZ, Fiedler SD, Christenson LK. MicroRNA 21 blocks apoptosis in mouse periovulatory granulosa cells. Biol Reprod 2010; 83:286–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Lin F, Li R, Pan ZX, Zhou B, Yu DB, Wang XG, Ma XS, Han J, Shen M, Liu HL. miR-26b promotes granulosa cell apoptosis by targeting ATM during follicular atresia in porcine ovary. PLoS One 2012; 7:e38640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Yang X, Zhou Y, Peng S, Wu L, Lin HY, Wang S, Wang H. Differentially expressed plasma microRNAs in premature ovarian failure patients and the potential regulatory function of mir-23a in granulosa cell apoptosis. Reproduction 2012; 144:235–244. [DOI] [PubMed] [Google Scholar]
- 280.Kitahara Y, Nakamura K, Kogure K, Minegishi T. Role of microRNA-136-3p on the expression of luteinizing hormone-human chorionic gonadotropin receptor mRNA in rat ovaries. Biol Reprod 2013; 89:114. [DOI] [PubMed] [Google Scholar]
- 281.Yin M, Lu M, Yao G, Tian H, Lian J, Liu L, Liang M, Wang Y, Sun F. Transactivation of microRNA-383 by steroidogenic factor-1 promotes estradiol release from mouse ovarian granulosa cells by targeting RBMS1. Mol Endocrinol 2012; 26:1129–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Cescon M, Chianese R, Tavares RS. Environmental impact on male (in)fertility via epigenetic route. J Clin Med 2020; 9:2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Jirtle RL, Skinner MK. Environmental epigenomics and disease susceptibility. Nat Rev Genet 2007; 8:253–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Xavier MJ, Roman SD, Aitken RJ, Nixon B. Transgenerational inheritance: How impacts to the epigenetic and genetic information of parents affect offspring health. Hum Reprod Update 2019; 25:518–540. [DOI] [PubMed] [Google Scholar]
- 285.Zhang XF, Zhang LJ, Feng YN, Chen B, Feng YM, Liang GJ, Li L, Shen W. Bisphenol a exposure modifies DNA methylation of imprint genes in mouse fetal germ cells. Mol Biol Rep 2012; 39:8621–8628. [DOI] [PubMed] [Google Scholar]
- 286.Ren J, Cheng Y, Ming ZH, Dong XY, Zhou YZ, Ding GL, Pang HY, Rahman TU, Akbar R, Huang HF, Sheng JZ. Intrauterine hyperglycemia exposure results in intergenerational inheritance via DNA methylation reprogramming on F1 PGCs. Epigenetics Chromatin 2018; 11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Skinner M, Guerrero-Bosagna C, Haque MM, Nilsson E, Bhandari R, McCarrey J. Environmentally induced transgenerational epigenetic reprogramming of primordial germ cells and subsequent germline. PLoS One 2013; 8:1–15 e66318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Jawaid A, Jehle KL, Mansuy IM. Impact of parental exposure on offspring health in humans. Trends Genet 2020; 37:373–388. [DOI] [PubMed] [Google Scholar]
- 289.Nohara K, Suzuki T, Okamura K. Gestational arsenic exposure and paternal intergenerational epigenetic inheritance. Toxicol Appl Pharmacol 2020; 409:115319. [DOI] [PubMed] [Google Scholar]
- 290.Gao Y, Zhao Y, Zhang H, Zhang P, Liu J, Feng Y, Men Y, Li L, Shen W, Sun Z, Min L. Pubertal exposure to low doses of zearalenone disrupting spermatogenesis through ERalpha related genetic and epigenetic pathways. Toxicol Lett 2019; 315:31–38. [DOI] [PubMed] [Google Scholar]
- 291.Rahman MS, Pang WK, Ryu DY, Park YJ, Pang MG. Multigenerational and transgenerational impact of paternal bisphenol a exposure on male fertility in a mouse model. Hum Reprod 2020; 35:1740–1752. [DOI] [PubMed] [Google Scholar]
- 292.Prados J, Stenz L, Somm E, Stouder C, Dayer A, Paoloni-Giacobino A. Prenatal exposure to DEHP affects spermatogenesis and sperm DNA methylation in a strain-dependent manner. PLoS One 2015; 10:e0132136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Beck D, Sadler-Riggleman I, Skinner MK. Generational comparisons (F1 versus F3) of vinclozolin induced epigenetic transgesnerational inheritance of sperm differential DNA methylation regions (epimutations) using MeDIP-Seq. Environmental Epigenetics 2017; 3:1, dvx016–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Skinner MK, Ben Maamar M, Sadler-Riggleman I, Beck D, Nilsson E, McBirney M, Klukovich R, Xie Y, Tang C, Yan W. Alterations in sperm DNA methylation, non-coding RNA and histone retention associate with DDT-induced epigenetic transgenerational inheritance of disease. Epigenetics Chromatin 2018; 11:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Kubsad D, Nilsson EE, King SE, Sadler-Riggleman I, Beck D, Skinner MK. Assessment of glyphosate induced epigenetic transgenerational inheritance of pathologies and sperm Epimutations: Generational toxicology. Sci Rep 2019; 9:6372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.McBirney M, King SE, Pappalardo M, Houser E, Unkefer M, Nilsson E, Sadler-Riggleman I, Beck D, Winchester P, Skinner MK. Atrazine induced epigenetic transgenerational inheritance of disease, lean phenotype and sperm Epimutation pathology biomarkers. PLoS One 2017; 12:1–37 e0184306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Wu H, Estill MS, Shershebnev A, Suvorov A, Krawetz SA, Whitcomb BW, Dinnie H, Rahil T, Sites CK, Pilsner JR. Preconception urinary phthalate concentrations and sperm DNA methylation profiles among men undergoing IVF treatment: A cross-sectional study. Hum Reprod 2017; 32:2159–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Ouko LA, Shantikumar K, Knezovich J, Haycock P, Schnugh DJ, Ramsay M. Effect of alcohol consumption on CpG methylation in the differentially methylated regions of H19 and IG-DMR in male gametes: Implications for fetal alcohol spectrum disorders. Alcohol Clin Exp Res 2009; 33:1615–1627. [DOI] [PubMed] [Google Scholar]
- 299.Soubry A, Hoyo C, Butt CM, Fieuws S, Price TM, Murphy SK, Stapleton HM. Human exposure to flame-retardants is associated with aberrant DNA methylation at imprinted genes in sperm. Environ Epigenet 2017; 3:dvx003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Greeson KW, Fowler KL, Estave PM, Kate Thompson S, Wagner C, Clayton Edenfield R, Symosko KM, Steves AN, Marder EM, Terrell ML, Barton H, Koval M et al. Detrimental effects of flame retardant, PBB153, exposure on sperm and future generations. Sci Rep 2020; 10:8567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Shnorhavorian M, Schwartz SM, Stansfeld B, Sadler-Riggleman I, Beck D, Skinner MK. Differential DNA methylation regions in adult human sperm following adolescent chemotherapy: Potential for epigenetic inheritance. PLoS One 2017; 12:1–18 e0170085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Soubry A, Guo L, Huang Z, Hoyo C, Romanus S, Price T, Murphy SK. Obesity-related DNA methylation at imprinted genes in human sperm: Results from the TIEGER study. Clin Epigenetics 2016; 8:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Denham J, O'Brien BJ, Harvey JT, Charchar FJ. Genome-wide sperm DNA methylation changes after 3 months of exercise training in humans. Epigenomics 2015; 7:717–731. [DOI] [PubMed] [Google Scholar]
- 304.Zhu L, Liu Y, Xue X, Yuan C, Wang Z. BPA's transgenerational disturbance to transcription of ovarian steroidogenic genes in rare minnow Gobiocypris rarus via DNA and histone methylation. Sci Total Environ 2020; 762:143055. [DOI] [PubMed] [Google Scholar]
- 305.Lombo M, Getino-Alvarez L, Depince A, Labbe C, Herraez MP. Embryonic exposure to bisphenol a impairs primordial germ cell migration without jeopardizing male breeding capacity. Biomolecules 2019; 9:307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Li H, Zhang P, Zhao Y, Zhang H. Low doses of carbendazim and chlorothalonil synergized to impair mouse spermatogenesis through epigenetic pathways. Ecotoxicol Environ Saf 2020; 188:109908. [DOI] [PubMed] [Google Scholar]
- 307.Gely-Pernot A, Hao C, Legoff L, Multigner L, D'Cruz SC, Kervarrec C, Jegou B, Tevosian S, Smagulova F. Gestational exposure to chlordecone promotes transgenerational changes in the murine reproductive system of males. Sci Rep 2018; 8:10274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Legoff L, Dali O, D'Cruz SC, Suglia A, Gely-Pernot A, Hemery C, Kernanec PY, Demmouche A, Kervarrec C, Tevosian S, Multigner L, Smagulova F. Ovarian dysfunction following prenatal exposure to an insecticide, chlordecone, associates with altered epigenetic features. Epigenetics Chromatin 2019; 12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Wu XF, Yuan HJ, Li H, Gong S, Lin J, Miao YL, Wang TY, Tan JH. Restraint stress on female mice diminishes the developmental potential of oocytes: Roles of chromatin configuration and histone modification in germinal vesicle stage oocytes. Biol Reprod 2015; 92:13. [DOI] [PubMed] [Google Scholar]
- 310.Torres-Flores U, Hernandez-Hernandez A. The interplay between replacement and retention of histones in the sperm genome. Front Genet 2020; 11:780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Oikawa M, Simeone A, Hormanseder E, Teperek M, Gaggioli V, O'Doherty A, Falk E, Sporniak M, D'Santos C, Franklin VNR, Kishore K, Bradshaw CR et al. Epigenetic homogeneity in histone methylation underlies sperm programming for embryonic transcription. Nat Commun 2020; 11:3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Ben Maamar M, Sadler-Riggleman I, Beck D, Skinner MK. Epigenetic transgenerational inheritance of altered sperm histone retention Sites. Sci Rep 2018; 5308:5301–5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Hamad MF, Shelko N, Kartarius S, Montenarh M, Hammadeh ME. Impact of cigarette smoking on histone (H2B) to protamine ratio in human spermatozoa and its relation to sperm parameters. Andrology 2014; 2:666–677. [DOI] [PubMed] [Google Scholar]
- 314.Lettieri G, D'Agostino G, Mele E, Cardito C, Esposito R, Cimmino A, Giarra A, Trifuoggi M, Raimondo S, Notari T, Febbraio F, Montano L et al. Discovery of the involvement in DNA oxidative damage of human sperm nuclear basic proteins of healthy Young Men living in polluted areas. Int J Mol Sci 2020; 21:4198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Radford EJ, Ito M, Shi H, Corish JA, Yamazawa K, Isganaitis E, Seisenberger S, Hore TA, Reik W, Erkek S, Peters A, Patti ME et al. In utero effects. In utero undernourishment perturbs the adult sperm methylome and intergenerational metabolism. Science 2014; 345:1255903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Ben Maamar M, Sadler-Riggleman I, Beck D, McBirney M, Nilsson E, Klukovich R, Xie Y, Tang C, Yan W, Skinner MK. Alterations in sperm DNA methylation, non-coding RNA expression, and histone retention mediate vinclozolin-induced epigenetic transgenerational inheritance of disease. Environmental Epigenetics 2018; 4:1, dvy010–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Brieno-Enriquez MA, Garcia-Lopez J, Cardenas DB, Guibert S, Cleroux E, Ded L, Hourcade Jde D, Peknicova J, Weber M, Del Mazo J. Exposure to endocrine disruptor induces transgenerational epigenetic deregulation of microRNAs in primordial germ cells. PLoS One 2015; 10:e0124296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Dickson DA, Paulus JK, Mensah V, Lem J, Saavedra-Rodriguez L, Gentry A, Pagidas K, Feig LA. Reduced levels of miRNAs 449 and 34 in sperm of mice and men exposed to early life stress. Transl Psychiatry 2018; 8:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Gapp K, Jawaid A, Sarkies P, Bohacek J, Pelczar P, Prados J, Farinelli L, Miska E, Mansuy IM. Implication of sperm RNAs in transgenerational inheritance of the effects of early trauma in mice. Nat Neurosci 2014; 17:667–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Gapp K, van Steenwyk G, Germain PL, Matsushima W, Rudolph KLM, Manuella F, Roszkowski M, Vernaz G, Ghosh T, Pelczar P, Mansuy IM, Miska EA. Alterations in sperm long RNA contribute to the epigenetic inheritance of the effects of postnatal trauma. Mol Psychiatry 2020; 25:2162–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Marczylo EL, Amoako AA, Konje JC, Gant TW, Marczylo TH. Smoking induces differential miRNA expression in human spermatozoa: A potential transgenerational epigenetic concern? Epigenetics 2012; 7:432–439. [DOI] [PubMed] [Google Scholar]
- 322.Lopez P, Castro A, Florez M, Miranda K, Aranda P, Sanchez-Gonzalez C, Llopis J. Arredondo M. miR-155 and miR-122 expression of spermatozoa in obese subjects. Front Genet 2018; 9:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Donkin I, Versteyhe S, Ingerslev LR, Qian K, Mechta M, Nordkap L, Mortensen B, Appel EV, Jorgensen N, Kristiansen VB, Hansen T, Workman CT et al. Obesity and bariatric surgery drive epigenetic variation of spermatozoa in humans. Cell Metab 201523:369–78. [DOI] [PubMed] [Google Scholar]
- 324.Skinner MK. What is an epigenetic transgenerational phenotype? F3 or F2. Reprod Toxicol 2008; 25:2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Rodgers AB, Morgan CP, Leu NA, Bale TL. Transgenerational epigenetic programming via sperm microRNA recapitulates effects of paternal stress. Proc Natl Acad Sci U S A 2015; 112:13699–13704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Carvan MJr, Kalluvila TA, Klingler RH, Larson JK, Pickens M, Mora-Zamorano FX, Connaughton VP, Sadler-Riggleman I, Beck D, Skinner MK. Mercury-induced epigenetic transgenerational inheritance of abnormal neurobehavior is correlated with sperm epimutations in zebrafish. PLoS One 2017; 12:1–26 e0176155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Skinner MK, Nilsson E, Sadler-Riggleman I, Beck D, JR MC. Transgenerational sperm DNA methylation Epimutation developmental origins following ancestral Vinclozolin exposure. Epigenetics 2019; 14:721–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Oliva R, Dixon GH. Vertebrate protamine genes and the histone-to-protamine replacement reaction. Prog Nucleic Acid Res Mol Biol 1991; 40:25–94. [DOI] [PubMed] [Google Scholar]
- 329.Hammoud SS, Nix DA, Hammoud AO, Gibson M, Cairns BR, Carrell DT. Genome-wide analysis identifies changes in histone retention and epigenetic modifications at developmental and imprinted gene loci in the sperm of infertile men. Hum Reprod 2011; 26:2558–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Skinner MK. A new kind of inheritance. Sci Am 2014; 311:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]


