Abstract
Given high COVID-19 infection and mortality rates among racial minorities in the US and their higher rates of religiosity, it is important to examine how the intersection of race and religion influences perceptions of COVID-19 vaccinations. Data for this study come from online surveys conducted in twelve congregations between October and December 2020 (N = 1,609). Based on logistic regression analyses, this study demonstrates a severe disparity of 24 percentage points (95% confidence interval 0.14–0.33) in anticipated COVID-19 vaccine acceptance between African Americans and White Americans, even when controlling for trust in COVID-19 information from scientists and levels of worrying about COVID-19 as well as religiosity and demographic factors. Religiosity is negatively associated with COVID-19 vaccine acceptance across racial groups. The findings suggest that the intersection of race and religion should be considered when designing immunization programs, for instance by fostering collaborations and dialogue with faith leaders of racial minority congregations.
Keywords: COVID-19, Vaccine acceptance, Vaccine hesitancy, Racial minorities, Religion, Health disparities
1. Introduction
Given high COVID-19 infection and mortality rates among racial minorities in the US [1] and their higher rates of religious observance [2], it is important to examine how the intersection of race and religion influences perceptions of COVID-19 vaccinations. There has been public health concern about vaccine hesitancy among African American populations [3], about their lower COVID-19 vaccine acceptance rates in particular [4], and about inequitable vaccine access in general [5]. Since African Americans, and to a slightly lesser extent, Hispanics, have been particularly hard hit by the health and economic consequences of the COVID-19 pandemic [6], lower vaccination rates could potentially further worsen racial inequalities. Even though religious and non-religious people tend to base their vaccine decisions on similar risk-benefit calculations and very few religious doctrines oppose vaccinations altogether [7], [8], religiosity has sometimes been linked with negative attitudes and skepticism towards vaccinations [9], [10]. Moreover, the role of faith communities and faith leaders have been noted as important avenues for the understanding of attitudes towards vaccines [11]. The complexities of the intersection of race and religion need to be explored for targeted COVID-19 immunization programs. The present study investigates racial differences in COVID-19 vaccine attitudes among a sample of members of religious congregations from diverse faith traditions, and the extent to which these racial differences in anticipated COVID-19 vaccine acceptance and trust in information from scientists about COVID-19 intersect with religiosity.
2. Data and methods
Data for this study come from online surveys conducted in twelve congregations between October and December 2020 in Washington DC, Maryland, Virginia, and Texas (N=1,609). A diverse sample of 75 congregations from different faith traditions (Buddhist, Christian, Hindu, Jewish, and Muslim traditions) was invited to participate in an online survey of how their communities have been impacted by the COVID-19 pandemic, out of which 18 communities expressed interest in participating, and 12 finally committed to participate. These include four Catholic, three Jewish (one Orthodox and two Reformed), two African American Baptist, one Evangelical, one Mormon, and one Hindu community. Congregation leaders who expressed interest in participation received an online link to the survey which they sent to their community mailing lists as well as small groups (councils, boards, committees, etc.). Weekly reminders were sent for three weeks. Each community received $1000 for their participation in the study and a report of main findings. Although this sample of congregations is not meant to be statistically representative of either their denominations or localities, participants across communities tended to be those members who are highly involved in their communities. In the estimation of the leaders of these religious communities, the sample represents those members who are most active and regularly involved in their communities and is well suited to inform us of patterns of anticipated COVID-19 vaccine acceptance among highly religious populations.
The main outcome variable of anticipated COVID-19 vaccine acceptance was replicated from the Pew Research Center’s American Trends Panel and was worded as follows: “If a vaccine to prevent COVID-19 were available today, would you…” [12]. Respondents had four response options from “definitely get the vaccine”, “probably get the vaccine”, “probably not get the vaccine”, to “definitely not get the vaccine”. In a similar way to other studies [13], the two positive and negative options were each collapsed and a binary indicator for anticipated COVID-19 vaccine acceptance was created.
The unique and timely survey made it possible to ask detailed questions about attitudes regarding COVID-19. Two relevant variables are employed in the regression models: Firstly, responses to the statement “I trust the information about the virus from scientific experts” (on a 1–4 scale from “do not agree”, “agree a little”, “agree moderately”, to “agree completely”) were recoded into a binary indicator of trust in COVID-19 information from scientific experts (agreement vs disagreement). Secondly, a binary variable for worrying about COVID-19 was generated (coded one if respondents selected any of the following two statements “I regularly worry about becoming sick with COVID-19” and “I regularly worry that my family or friends will become sick with COVID-19”, zero otherwise). Levels of religiosity are measured on a four-point scale for an individual respondent’s frequency of prayer (“Outside of religious services, about how often do you spend time alone praying or meditating these days?”: “once a week or less”, “a few times a week”, “once a day”, “several times a day”; treated as continuous).
The main independent variable, race, is categorized into four groups: White (68% of respondents), African American (11%), Hispanic (11%), Asian Americans (6%) and Other (4%). Other covariates are gender (binary), continuous age, an age-squared term for non-linear trends of age, marital status (binary; differentiating those who are married or in a partnership with those who are divorced, never married, or widowed), household income (up to $50,000; $50,001–$100,000; $100,001–$150,000; more than $150,000; treated as continuous), educational attainment (binary, contrasting those with at least a college degree to those with less), self-rated physical health (“in general, how would you rate your physical health?”, 11-point scale from “poor” to “excellent”), political affiliation (“generally speaking, do you usually think of yourself as a Democrat, Republican, or Independent?”; collapsed into a binary indicator of Democrat vs Republican and Independent).
Anticipated COVID-19 vaccine acceptance is modelled in three nested logistic regression models. In model one, only the focal predictor variable of race (with White Americans as the reference group) is analyzed. In model two, trust in COVID-19 information from scientists, worrying about COVID-19, and religiosity are added as contextual factors. It is expected that trust in information from scientists is a strong predictor of anticipated COVID-19 vaccine acceptance and that it could explain a significant portion of the racial differences. Likewise, the extent of worrying about COVID-19 captures an assessment of the personal risk to, as well as overall nature of, the virus. In model 3, all mentioned covariates are included as control variables.
Having applied listwise deletion of missing cases, the resulting analytical sample is reduced by 33 per cent (N =1,070). The logistic regressions are calculated with robust standard errors (Huber-Sandwich estimator), but clustered standard errors at the congregation level are also presented as a robustness check. The confidence intervals and statistical significance tests refer to the 95% levels. The AIC, BIC, and Chi-squared (deviance) model-fit statistics are offered and predicted probabilities of anticipated COVID-19 vaccine acceptance across racial groups are visualized based on average marginal effects.
3. Results
The descriptive statistics of the sample for each variable are presented in Table 1 . 87% of whites, 56% of African Americans, 68% of Hispanics, 89% of Asian Americans and 82% of the other racial group express anticipated COVID-19 vaccine acceptance. There is very high trust of COVID-19 information from scientific experts across all races (82–90%). In terms of demographic attributes, most respondents tend to be female, have high household incomes, and are educated at a degree level or higher. The average age is around 58 years (range 18–96, mean 57.8, standard deviation 15.7).
Table 1.
Descriptive statistics and respondent characteristics by racial groups.
| White | African American | Hispanic | Asian American | Other | |
|---|---|---|---|---|---|
| Mean/Proportion | Mean/Proportion | Mean/Proportion | Mean/Proportion | Mean/Proportion | |
| Anticipated COVID-19 vaccine acceptance (binary) | 0.87 | 0.56 | 0.68 | 0.89 | 0.71 |
| Trust in COVID-19 information from scientists (binary) | 0.90 | 0.82 | 0.83 | 0.89 | 0.85 |
| Worrying about COVID-19 (binary) | 0.47 | 0.45 | 0.61 | 0.37 | 0.53 |
| Frequency of prayer a | |||||
| Once a week or less | 0.35 | 0.12 | 0.22 | 0.11 | 0.14 |
| A few times a week | 0.16 | 0.23 | 0.18 | 0.11 | 0.18 |
| Once a day | 0.23 | 0.25 | 0.34 | 0.38 | 0.25 |
| Several times a day | 0.26 | 0.41 | 0.27 | 0.39 | 0.43 |
| Age in years (range: 18–96) | 59.40 | 59.66 | 48.69 | 58.43 | 55.19 |
| Gender: Men (ref. Women) | 0.36 | 0.25 | 0.15 | 0.51 | 0.30 |
| Marital status: Married or in partnership (ref. Not married) | 0.78 | 0.50 | 0.72 | 0.76 | 0.80 |
| Household income a | |||||
| Up to $50,000 | 0.10 | 0.22 | 0.33 | 0.15 | 0.12 |
| $50,001–$100,000 | 0.19 | 0.36 | 0.36 | 0.23 | 0.35 |
| $100,001–$150,000 | 0.25 | 0.19 | 0.20 | 0.25 | 0.18 |
| More than $150,000 | 0.46 | 0.23 | 0.11 | 0.37 | 0.35 |
| Education: College degree or higher (ref. Less than a college degree) | 0.87 | 0.57 | 0.58 | 0.97 | 0.77 |
| Political party: Republican or Independent (ref. Democrat) | 0.51 | 0.14 | 0.44 | 0.42 | 0.61 |
| Self-rated physical health (0–10 scale) | 7.33 | 7.16 | 7.09 | 7.20 | 7.18 |
| Observations b | 966 | 156 | 158 | 89 | 57 |
a Treated as continuous in the logistic regressions b Sample statistics before listwise missing data deletion was applied. Remaining analytical sample after listwise deletion: N = 1,070
Note: Data come from 12 religious faith communities/congregations, based on an online survey that was conducted between October and December 2020 in the San Antonio and Washington, D.C., metropolitan areas.
The results of Model 1, as shown in Table 2, very strongly demonstrate that African Americans express the lowest level of anticipated COVID-19 vaccine acceptance: Compared to Whites, they have 0.19 times the odds (95% CI 0.12–0.29) of anticipated COVID-19 vaccine acceptance. While Hispanics also have lower anticipated COVID-19 vaccine acceptance (OR 0.38, 95%, CI 0.24–0.62), Asian Americans (OR 1.21, 95% CI 0.54–2.73) and other racial groups (OR 0.69, 95% CI 0.33–1.45) do not have a statistically significantly different level of anticipated COVID-19 vaccine acceptance than Whites.
Table 2.
Nested logistic regression models of anticipated COVID-19 vaccine acceptance among religious populations (N = 1,070).
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Race: African American (ref. White) | 0.19*** | 0.19*** | 0.19*** |
| (0.12–0.29) | (0.11–0.31) | (0.11–0.33) | |
| Race: Hispanic (ref. White) | 0.38*** | 0.35*** | 0.58+ |
| (0.24–0.62) | (0.20–0.62) | (0.32–1.08) | |
| Race: Asian American (ref. White) | 1.21 | 1.45 | 1.24 |
| (0.54–2.73) | (0.60–3.53) | (0.47–3.32) | |
| Race: Other (ref. White) | 0.48+ | 0.59 | 0.69 |
| (0.20–1.15) | (0.28–1.25) | (0.33–1.45) | |
| Trust in COVID-19 information from scientists (binary) | 7.59*** | 6.97*** | |
| (4.83–11.93) | (4.26–11.42) | ||
| Worrying about COVID-19 (binary) | 1.42+ | 1.59* | |
| (0.99–2.03) | (1.08–2.35) | ||
| Frequency of prayer (1–4 scale) | 0.79** | 0.83* | |
| (0.68–0.93) | (0.70–0.98) | ||
| Gender: Men (ref. Women) | 2.64*** | ||
| (1.71–4.08) | |||
| Age in years (continuous) | 0.93 | ||
| (0.85–1.02) | |||
| Age squared (interaction term) | 1.00* | ||
| (1.00–1.00) | |||
| Marital status: Married or in partnership (ref. Not married) | 1.25 | ||
| (0.80–1.95) | |||
| Household income (1–4 scale) | 1.24* | ||
| (1.02–1.50) | |||
| Education: College degree or higher (ref. Less than a college degree) | 1.53+ | ||
| (0.97–2.42) | |||
| Self-rated physical health (0–10 scale) | 1.06 | ||
| (0.97–1.17) | |||
| Political party: Republican or Independent (ref. Democrat) | 0.54** | ||
| (0.35–0.82) | |||
| Observations | 1,070 | 1,070 | 1,070 |
| AIC | 940 | 833 | 790 |
| BIC | 965 | 873 | 880 |
| Chi-squared (deviance) | 930 | 817 | 754 |
Exponentiated coefficients of the nested logistic regressions (models 1–3) that represent the odds ratios of COVID-19 vaccine acceptance. Statistical significance at the 95% level: *** p < 0.001, ** p < 0.01, * p < 0.05, + p < 0.1 and 95% confidence intervals of the odds ratios are shown in parentheses. Robust standard errors have been employed for the calculation of the statistics.
Age, age squared, the frequency of prayer (originally ordinal), household income (originally ordinal) and self-rated physical health are treated as continuous variables. All other variables are employed as factors using binary/dummy codings.
Model 2 explores variables that are associated with the racial differences in anticipated COVID-19 vaccine acceptance. Results show that trust in COVID-19 information from scientific experts (OR 7.59, 95% CI 4.83–11.93) and the frequency of prayer (OR 0.79, 95% CI 0.68–0.93) very strongly correspond with COVID-19 vaccine attitudes. Crucially, in Model 2 and Model 3, which add important contextual control variables, the stark racial differences in vaccine attitudes remain statistically significant and are not explained: In both models, the odds ratio of anticipated COVID-19 vaccine acceptance for African Americans remain unchanged at 0.19 (95% CI 0.11–0.33, p < 0.001), but in Model 3, Hispanics no longer have a statistically significant difference compared with Whites (OR 0.58, 95% CI 0.32–1.08). This suggests that demographics and socio-economic factors can explain the lack of anticipated COVID-19 vaccine acceptance among Hispanics, but not among African Americans. Worrying about the detrimental health effects of COVID-19 was insignificant (p < 0.1) in Model 2, but significant in the full model with 1.54 times (95% CI 1.05–2.26) the odds of anticipated COVID-19 vaccine acceptance (p < 0.05).
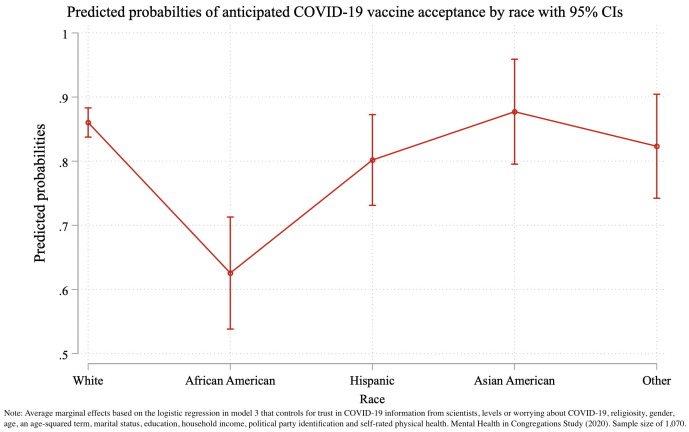
In terms of control variables, men are more likely than women to endorse the COVID-19 vaccine (OR 2.64, 95% CI 1.71–4.08). Higher levels of income are associated with higher anticipated COVID-19 vaccine acceptance (OR 1.24, 95% CI 1.02–1.50). Education is not statistically significant when jointly controlling for income, but it was significant on its own (not shown). Marital status and self-rated physical health are not significant predictors of anticipated COVID-19 vaccine acceptance. Political affiliation, however, is significant and the combined group of Republicans or Independents has 0.54 (95% CI 0.32–0.82) times the odds of anticipated COVID-19 acceptance than Democrats. While anticipated vaccine acceptance is highest among the older and oldest respondents, the significant age-squared term indicates that there is an inverse association among the youngest respondents aged 18–35 who also express more acceptance than respondents in their 40s. As visualized in Fig. 1 , when simultaneously controlling for all these variables, African Americans still have a 24 percentage point (95% CI 14–33) lower predicted probability of anticipated COVID-19 vaccine acceptance than White Americans.
Fig. 1.
Predicted probabilities of anticipated COVID-19 vaccine acceptance by race with 95% CIs.
The lower AIC, BIC, and Chi-squared model-fit statistics suggests improvements as more variables are controlled for. Although the confidence intervals widen when employing congregation-level clustered standard errors as seen in (see Supplementary Material), the direction of the results remain largely the same.
4. Discussion
Racial minorities such as African Americans and Hispanics are disproportionately impacted by the COVID-19 pandemic in the US, but also exhibit significantly higher levels of vaccine hesitancy. The present study of US congregation members set out to examine the extent to which the intersection of race and religiosity influences anticipated COVID-19 vaccine acceptance as well as trust in scientific information about COVID-19. Consistent with general population data, we find that African Americans who report relatively high levels of religiosity are more likely to exhibit much lower rates of anticipated COVID-19 vaccine acceptance than White Americans or Asian Americans [14], [15]. Similarly, levels of anticipated COVID-19 vaccine acceptance of religious Hispanics are also lower than the ones of religious Whites, but this difference can be attributed to demographic and socio-economic factors.
The results show that lower levels of trust in scientific information about the virus as well as higher levels of religiosity in these communities are associated with lower levels of anticipated COVID-19 vaccine acceptance. Yet in our sample, although African Americans and Hispanics have relatively lower levels of trust in information about the virus from scientists, the vast majority in their communities do trust such scientific information. Indeed, the level of trust among Whites and Asian Americans in this religious sample is even higher than the levels of trust (77–79%) in healthcare providers and officials that were reported in another study [16]. Consistent with other research, socioeconomic conditions and political partisanship (with Republicans and Independents having much more vaccine hesitancy than Democrats) especially are related to anticipated COVID-19 vaccine acceptance in our sample [17], [18], but none of these factors can explain away the notably low levels of anticipated COVID-19 acceptance for African Americans.
While both science skepticism and religiosity contribute to racial disparities in vaccine acceptance, they do not fully explain these differences. For African Americans in particular, researchers have argued that mistrust of the medical community is less due to the trauma of historical atrocities such as Tuskegee and more due to everyday racism and racialized care in healthcare institutions [3]. Significant proportions of African Americans and Hispanics have also expressed concerns about the safety and effectiveness of the COVID-19 vaccine [19]. Given the strong association between a higher frequency of prayer and lower vaccine acceptance, future research should assess whether this relates to religiously-motivated skepticism of vaccines, social networks and ecological factors within congregations as communities [20], or whether other aspects such as concerns about side-effects of long-term health effects are at play that are not that different from the general population [21]. It is important to bear in mind that despite these racial differences in COVID-19 attitudes, racial groups themselves are not homogenous and that simplifications and biased media representations can be counter-productive for building trust in vaccines [22]. Indeed, the overall levels of anticipated COVID-19 vaccine acceptance are high in these data, suggesting that the discourse on religiosity and its intersection with race should not automatically be framed negatively. Furthermore, the role of religiosity in shaping COVID-19 vaccine attitudes also matters in a general sense and for other population groups such as medical students [10].
Since racial minorities are more likely to trust leaders of their own communities than either scientific experts or the government, more dialogue and collaboration is needed between medical and religious communities to communicate reliable information about the safety and efficacy of the vaccine. Exemplary efforts include academic-community partnerships [23], stakeholder engagement to increase public awareness [24], and initiatives by religious communities to distribute vaccines among high-risk populations [25]. The WHO’s Tailoring Immunization Programs have been effectively used in a Charedi Jewish community for identifying barriers to and enablers of vaccination [21]. With the expansion of such efforts at building trust, understanding and collaboration in religious settings with a focus on racial minorities, there is a chance to make the ongoing pandemic less detrimental to racial minority communities and to prevent further exacerbation of health inequities.
Confidence in the findings of this study is gained by the fact that the presented odds ratios and distributions of the demographic characteristics closely mirror those of US general population analyses [13], [14]: Women have lower levels of vaccine acceptance than men; education and especially postgraduate education are linked with more vaccine acceptance, and there is an U-shaped association with vaccine acceptance across age.
This study is limited in that it is not based on a nationally representative sample. Also, data were only collected during a single period (October-December 2020) just before COVID-19 vaccines became available, and vaccination attitudes are evolving over time [26]. Further, the religious and racial context in the US is unique and the findings of this study are unlikely to be transferrable to other countries. Nonetheless, given that the disproportionate burden of disease of COVID-19 on racial and religious minorities is a global phenomenon — for instance, members of a Charedi Jewish community in the UK had more than five times the estimated SARS-CoV-2 seroprevalence than the overall population [27] — country-specific studies can gradually increase the evidence-base on vaccination attitudes.
Funding sources
Data collection for this study was funded by a grant from the John Templeton Foundation (#61107).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We are very grateful for Professor Jason Schnittker’s feedback of an earlier version of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.09.005.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
The following are the Supplementary data to this article:
References
- 1.Tai D.B.G., Shah A., Doubeni C.A., Sia I.G., Wieland M.L. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pew Research Center. Racial and ethnic composition; 2021.
- 3.Bajaj S.S., Stanford F.C. Beyond Tuskegee - Vaccine Distrust and Everyday Racism. N Engl J Med. 2021;384(5):e12. doi: 10.1056/NEJMpv2035827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bunch L. A Tale of Two Crises: Addressing Covid-19 Vaccine Hesitancy as Promoting Racial Justice. HEC Forum. 2021 doi: 10.1007/s10730-021-09440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burgos R.M., Badowski M.E., Drwiega E., Ghassemi S., Griffith N., Herald F., et al. The race to a COVID-19 vaccine: Opportunities and challenges in development and distribution. Drugs Context. 2021;10:1–10. doi: 10.7573/dic.2020-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tirupathi R., Muradova V., Shekhar R., Salim S.A., Al-Tawfiq J.A., Palabindala V. COVID-19 disparity among racial and ethnic minorities in the US: A cross sectional analysis. Travel Med Infect Dis. 2020;38:101904. doi: 10.1016/j.tmaid.2020.101904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kasstan B. “If a rabbi did say ‘you have to vaccinate’, we wouldn't”: Unveiling the secular logics of religious exemption and opposition to vaccination. Soc Sci Med. 2021;280:114052. doi: 10.1016/j.socscimed.2021.114052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grabenstein J.D. What the World's religions teach, applied to vaccines and immune globulins. Vaccine. 2013;31(16):2011–2023. doi: 10.1016/j.vaccine.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Rutjens B.T., Sutton R.M., van der Lee R. Not all skepticism is equal: Exploring the ideological antecedents of science acceptance and rejection. Pers Soc Psychol B. 2018;44(3):384–405. doi: 10.1177/0146167217741314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia L.L., Yap J.F.C. The role of religiosity in COVID-19 vaccine hesitancy. J Public Health-Uk. 2021 doi: 10.1093/pubmed/fdab192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruijs W.L., Hautvast J.L., Kerrar S., van der Velden K., Hulscher M.E. The role of religious leaders in promoting acceptance of vaccination within a minority group: a qualitative study. Bmc Public Health. 2013;13:511. doi: 10.1186/1471-2458-13-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pew Research Center. Survey question wording and topline; 2020.
- 13.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Callaghan T, Moghtaderi A, Lueck JA, Hotez PJ, Strych U, Dor A, et al. Correlates and disparities of COVID-19 vaccine hesitancy. Available at SSRN 3667971; 2020. [DOI] [PMC free article] [PubMed]
- 15.Razai MS, Osama T, McKechnie DG, Majeed A. Covid-19 vaccine hesitancy among ethnic minority groups. Brit Med J Publ Group; 2021. [DOI] [PubMed]
- 16.Shafiq M, Elharake JA, Malik AA, McFadden SM, Aguolu OG, Omer SB. COVID-19 Sources of Information, Knowledge, and Preventive Behaviors Among the US Adult Population. J Public Health Manage Pract 2021;27:278–84. [DOI] [PubMed]
- 17.Allcott H., Boxell L., Conway J., Gentzkow M., Thaler M., Yang D. Polarization and public health: Partisan differences in social distancing during the coronavirus pandemic. J Public Econ. 2020;191:104254. doi: 10.1016/j.jpubeco.2020.104254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodman S.W., Pepinsky T.B. Partisanship, health behavior, and policy attitudes in the early stages of the COVID-19 pandemic. SSRN Electron J. 2020 doi: 10.1371/journal.pone.0249596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Covid Collaborative. Coronavirus Vaccine Hesitancy in Black and Latinx Communities; 2021.
- 20.Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the US: A social-ecological perspective. Soc Sci Med. 2021;270:113684. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Letley L., Rew V., Ahmed R., Habersaat K.B., Paterson P., Chantler T., et al. Tailoring immunisation programmes: using behavioural insights to identify barriers and enablers to childhood immunisations in a Jewish community in London. UK Vaccine. 2018;36(31):4687–4692. doi: 10.1016/j.vaccine.2018.06.028. [DOI] [PubMed] [Google Scholar]
- 22.Kasstan B. Vaccines and vitriol: an anthropological commentary on vaccine hesitancy, decision-making and interventionism among religious minorities. Anthropol Med. 2020;1–9 doi: 10.1080/13648470.2020.1825618. [DOI] [PubMed] [Google Scholar]
- 23.Williams J.T.B., Miller A., O'Leary S.T. Sacred or secular? Exploring religious Coloradans’ questions about vaccines. Vaccine. 2020;38(45):6971–6974. doi: 10.1016/j.vaccine.2020.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fletcher F.E., Allen S., Vickers S.M., Beavers T., Hamlin C.M., Young-Foster D., et al. COVID-19's Impact on the African American Community: a stakeholder engagement approach to increase public awareness through virtual town halls. Health Equity. 2020;4(1):320–325. doi: 10.1089/heq.2020.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacInnis A. Black Churches Step in to Help Distribute COVID-19 Vaccines. Christianity Today. 2021 [Google Scholar]
- 26.Fridman A., Gershon R., Gneezy A., Capraro V. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE. 2021;16(4):e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaskell K.M., Johnson M., Gould V., Hunt A., Stone N.RH., Waites W., et al. SARS-CoV-2 seroprevalence in a strictly-Orthodox Jewish community in the UK: A retrospective cohort study. Lancet Regional Health-Europe. 2021;6:100127. doi: 10.1016/j.lanepe.2021.100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.