Abstract
Introduction
The COVID-19 outbreak and the related lockdown measures have raised concerns regarding mental health, including alcohol misuse. Preliminary studies investigated alcohol consumption at the early stages of lockdown, but no longitudinal data regarding its evolution during and after the first lockdown are currently available.
Methods
We investigated changes in alcohol consumption among a convenience sample of 1,693 French-speaking Belgian adults using a 3-stage longitudinal online survey. All participants reported their consumption at different stages of lockdown: before lockdown onset (retrospectively, T0), at 2 different times during lockdown (T1 and T2), and after lockdown offset (T3). We also measured socio-demographic variables and the harmfulness of drinking patterns before lockdown.
Results
A mixed model with negative binomial distribution indicated that participants decreased their alcohol consumption after lockdown onset and returned to their initial alcohol consumption after lockdown offset. Younger individuals (18–30 years old) were more likely to decrease their consumption during the lockdown period (T1 and T2) than the periods preceding or following lockdown (T0 and T3), especially if they presented hazardous or problematic drinking patterns before lockdown. We only observed a rebound effect after lockdown offset among young moderate drinkers. All participants kept stable their alcohol consumption during lockdown (T1 and T2).
Conclusions
Lockdown onset and offset constitute key periods for alcohol consumption changes during the COVID-19 crisis, particularly in youth and in individuals with hazardous or problematic drinking patterns.
Keywords: COVID-19, Alcohol, Lockdown, Longitudinal study, Drinking patterns
Introduction
Confronted with the global outbreak of COVID-19, national authorities have imposed a large-scale lockdown in the first months of 2020 in many countries, drastically restricting mobility and social interactions. While these measures had a positive impact on the containment of the virus, the social isolation they triggered also led to distress and negatively affected mental health [1, 2]. Among these collateral damages, experts [3] raised the possibility of increased substance use during lockdown, especially regarding alcohol consumption.
Alcohol abuse constitutes a serious threat during sanitary crises, notably because it increases the likelihood of falls and violence towards cohabitants, and consequently, the number of hospital admissions [4]. Excessive alcohol consumption also undermines the immune system [5], making it less resistant to infectious agents, such as the COVID-19 [6], and hampers mental health, exacerbating depressive and anxiety symptoms [7]. It is therefore crucial to investigate how alcohol-related habits evolved during the lockdown period, notably to develop efficient intervention tools countering the potential emergence of alcohol use disorders during the present crisis and preventing such phenomenon in future ones.
Divergent predictions have emerged regarding the evolution of alcohol consumption during lockdown. A systematic review [8] identified two opposite scenarios, respectively predicting increased consumption (as a way of coping with psychological distress) or decreased consumption (resulting from reduced physical and/or financial availability of alcohol). Preliminary results suggest the coexistence of these opposite proposals, with an influence of age and pre-pandemic drinking patterns. Indeed, younger people appeared more likely to decrease consumption during lockdown [9, 10, 11] while individuals with higher stress levels [12, 13, 14, 15] and heavy drinking patterns [11, 16] increased their alcohol use.
However, these studies only examined alcohol consumption at the early stages of lockdown and did not offer any insight regarding its evolution during and after lockdown. The reduction of sanitary measures after lockdown offset (e.g., resurgence of physical social interactions, re-opening of bars and restaurants) might result in an immediate increase of alcohol consumption in the general population [17]. This could even lead to a rebound effect, namely to an increase in alcohol consumption post-lockdown compared to pre-lockdown, further increasing the risk of long-term alcohol-related consequences. Longitudinal data are thus required to investigate changes in alcohol consumption during but also after lockdown, and to specify the socio-demographical and clinical determinants of these changes.
The present study fills this gap by describing the evolution of alcohol consumption in a sample of French-speaking Belgians at the different stages of the lockdown: before lockdown onset (retrospectively, T0), at 2 different times during lockdown (T1 and T2), and after lockdown offset (T3). As Belgium has been particularly impacted by the pandemic [18] and endured a total lockdown with stringent measures during 7 weeks (March 18–May 3, 2020), it offers an ideal context to explore the evolution of alcohol consumption during and after lockdown in Western countries. In view of the available literature, we hypothesized (1) a globally reduced alcohol consumption (i.e., number of alcohol units per week) during the lockdown period, mostly in younger participants, with conversely an increased consumption in specific subgroups (e.g., heavy drinkers); (2) a potential rebound effect after lockdown offset, particularly in youth.
Methods
Study Design
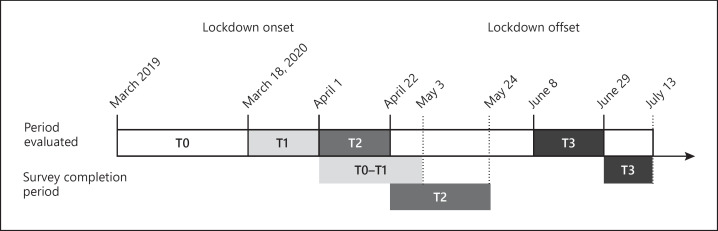
We adopted a 3-stage longitudinal design (Fig. 1) using Qualtrics Survey Software. We assessed alcohol-related variables before lockdown (T0) retrospectively at T1 and collected longitudinal measures of alcohol consumption during the 3 weeks preceding T1, T2, and T3. We disseminated the first stage (T1) of the survey through social media (Facebook and Twitter), University website, and national/regional press between April 1 and May 3, 2020, that is, 2–6 weeks after the onset of the strict lockdown (requirement to stay home; closure of bars, restaurants, and nonessential shops [alcohol remained available through home delivery services and in supermarkets]; prohibition of nonessential travels), which was identical across all Belgian regions. Participants who provided their e-mail address for the follow-up of the survey were contacted 3 weeks after their first participation for the second stage (T2). The third stage (T3) was completed between June 29 and July 13, 3–5 weeks after lockdown offset (i.e., re-opening of bars and restaurants; close contact allowed with 10 persons per week; recreational activities and travels allowed). Participants provided their written informed consent before starting the survey and were not compensated for their participation. This study complied with the ethical standards of the Helsinki Declaration of 1975, as revised in 2008, and the longitudinal design was approved by the Ethics Committee of the Psychological Sciences Research Institute (UCLouvain, Study Approval Number: Projet2020-44). The present results are part of a larger project exploring alcohol consumption changes during the COVID-19 crisis in the Belgian population [9].
Fig. 1.
Timeline of the procedure followed for the 3 stages of the survey assessing alcohol consumption at T0, T1, T2, and T3 measurement times.
Participants
The online survey focused on French-speaking Belgian adults, without further eligibility criteria as our target was the general population. A total of 2,007 participants fully responded to the 3 stages of the study. We excluded 314 participants (15.5%) of the sample who completed all the stages because their responses were incomplete (N = 178, 8.9%), aberrant (N = 17, 0.8%), or because participants were living outside Belgium (and were thus confronted to different lockdown conditions, N = 119, 5.9%). The final analyses included 1,693 participants (987 women) and all participants were aged 18 or older (age range: 18–90).
Measures
Socio-Demographic Variables
We assessed gender, age, and education (i.e., primary, secondary, and higher education). Participants were grouped in 3 age ranges: younger (18–30 years old), middle-aged (31–50 years old), and older (51+ years old). We chose these grouping ranges to have a similar sample size in each group, but also because age is known to strongly predict alcohol consumption. For example, young adults present higher levels of excessive consumption patterns, such as heavy drinking or binge drinking [19]. Moreover, these age-based groups appeared differentially impacted by lockdown conditions, with stronger reduction of social interactions and perturbation of usual lifestyle in youth [9, 10, 11].
Alcohol Use Disorder Identification Test
We used the alcohol use disorder identification test (AUDIT) [20] to assess the baseline (T0) harmfulness of alcohol use during the last 12 months before lockdown onset (explicitly excluding the lockdown period). The questionnaire comprised 10 items (score range: 0–40), higher scores reflecting higher intensity/harmfulness of alcohol use. We distinguished 3 groups of participants based on AUDIT scores [21]: moderate drinkers (AUDIT score <8), hazardous drinkers (AUDIT score between 8 and 15), and problematic drinkers (individuals at risk for alcohol use disorders; AUDIT score ≥16). The AUDIT showed good reliability in the current sample (Cronbach's α = 0.819).
Weekly Alcohol Consumption
We assessed alcohol consumption through an adaptation of the timeline follow-back method [22]. We measured the frequency and quantity of alcohol consumption (i.e., number of units consumed each day, from Monday to Sunday and 1 unit corresponding to 10 g of ethanol in Belgium) during a typical week related to each period described above (T0, T1, T2, and T3). We computed a “units per week score” at each stage of the survey, by summing daily consumptions.
Statistical Analyses
We used R [23] to perform descriptive statistics on socio-demographic and alcohol-related variables. We used a negative binomial model using the glmmTMB R package [24] to address overdispersed distribution (online suppl. Fig. 1; for all online suppl. material, see www.karger.com/doi/10.1159/000518218) due to a large number of zero-count observations regarding the number of alcohol units per week (20.98% of the observations) [25]. The model was fitted to test for the effects of time (T0, T1, T2, and T3), AUDIT (moderate, hazardous, and problematic drinkers) and age (younger, middle-aged, and older), as well as their interaction terms, on the number of alcohol units consumed per week. Gender (0 = male, 1 = female) was included as a covariate and participant was included as random effect to account for repeated measures. Planned orthogonal contrasts were computed according to our hypotheses for AUDIT group (contrast 1: moderate vs. hazardous and problematic; contrast 2: hazardous vs. problematic), age range (contrast 1: younger vs. middle-aged and older; contrast 2: middle-aged vs. older), and for time (contrast 1: T1 and T2 vs. T0 and T3; contrast 2: T0 vs. T3; contrast 3: T1 vs. T2). We plotted interaction effects using ggplot2 R package [26] and included 95% confidence limits for the subgroup means without assuming normality using Hmisc R package [27].
Results
Descriptive Statistics of the Final Sample
A total of 8,489 adult participants (5,220 women) fully responded to the online survey at T1, 3,338 kept responding at T2 and 2007 responded from T1 to T3. The 1,693 participants included in the final sample (19.9% of the initial convenience sample) did not differ from those who dropped out from the survey or were excluded (N = 6,796) in terms of alcohol units consumed per week at T0 (t [2,832.832] = 1.642, p = 0.101) or T1 (t [8,487] = 1.376, p = 0.169). The final sample was however older (t [2,358.552] = 15.286, p < 0.001) and contained a higher percentage of women (χ2 [28,488] = 14.890, p = 0.001) and individuals with higher education (χ2 [28,488] = 25.302, p < 0.001) than the original one.
Mean age of the final sample was 41.52 years old (standard deviation = 16.32). The sample comprised 987 women (58.3%). Most participants had completed higher education (82%, N = 1,395), 17% completed secondary education (N = 280), and 1% completed primary education (N = 18). Mean AUDIT score for the whole sample was 6.29 (standard deviation = 5.40), under the cut-off score for hazardous drinking (AUDIT > 7 [21]). Only 146 of them (8.6% of the final sample) did not consume alcohol during the last year, compared to 23.5% of nondrinkers in the general population in Belgium (WHO, 2018).
Global Changes in Alcohol Consumption
From T0 to T1, 38.9% of the sample (N = 658) decreased their consumption, 32.2% (N = 545) did not change their consumption (i.e., consumed the same number of units per week), and 28.9% (N = 490) reported increased consumption. From T1 to T2, 30.1% (N = 509) decreased their consumption, 37.4% (N = 634) did not change their consumption, and 32.5% (N = 550) reported increased consumption. From T2 to T3, 48.2% (N = 816) increased their consumption, 27.5% (N = 466) decreased their consumption, and 24.3% (N = 411) did not change their consumption. From T0 to T3, 41.6% (N = 705) increased their consumption, 34.9% (N = 591) decreased their consumption, and 23.4% (N = 397) did not change their consumption (Table 1).
Table 1.
Number of alcohol units consumed per week in the whole sample and in moderate, hazardous, and problematic drinkers at T0, T1, T2, and T3, according to their age: mean (SD)
| T0 | T1 | T2 | T3 | |
|---|---|---|---|---|
| Whole sample (N = 1,693) | 8.42 (10.50) | 6.90 (10.08) | 6.91 (10.20) | 8.37 (10.90) |
| Younger (N = 560) | 8.28 (10.05) | 3.88 (5.73) | 3.88 (6.12) | 7.34 (8.44) |
| Middle-aged (N = 607) | 7.84 (8.63) | 7.94 (10.06) | 7.78 (10.07) | 8.37 (9.26) |
| Older (N = 526) | 9.26 (12.69) | 8.90 (12.68) | 9.13 (12.76) | 9.48 (14.33) |
| Moderate drinkers (N = 1,166) | 4.23 (4.76) | 4.35 (5.73) | 4.45 (5.88) | 4.97 (5.94) |
| Younger (N = 334) | 2.97 (3.33) | 2.46 (3.82) | 2.57 (4.66) | 3.97 (5.28) |
| Middle-aged (N = 419) | 4.36 (4.31) | 5.09 (5.90) | 4.96 (5.93) | 5.13 (5.42) |
| Older (N = 413) | 5.11 (5.83) | 5.14 (6.45) | 5.45 (6.35) | 5.61 (6.79) |
| Hazardous drinkers (N = 404) | 14.00 (8.68) | 10.40 (10.03) | 10.17 (10.24) | 13.41 (12.57) |
| Younger (N = 170) | 12.95 (7.58) | 5.16 (5.40) | 4.88 (5.27) | 10.26 (6.72) |
| Middle-aged (N = 153) | 12.73 (6.36) | 11.96 (8.78) | 11.59 (8.39) | 13.03 (8.30) |
| Older (N = 81) | 18.60 (12.42) | 18.43 (13.05) | 18.58 (14.18) | 20.72 (22.22) |
| Problematic drinkers (N = 123) | 29.89 (18.17) | 19.50 (22.38) | 19.53 (22.66) | 24.11 (18.54) |
| Younger (N = 56) | 25.79 (15.23) | 8.46 (10.79) | 8.65 (11.29) | 18.52 (13.91) |
| Middle-aged (N = 35) | 28.06 (15.47) | 24.57 (23.94) | 24.81 (24.48) | 26.77 (16.87) |
| Older (N = 32) | 39.06 (22.47) | 33.25 (26.32) | 32.78 (26.65) | 31.00 (24.18) |
SD, standard deviation.
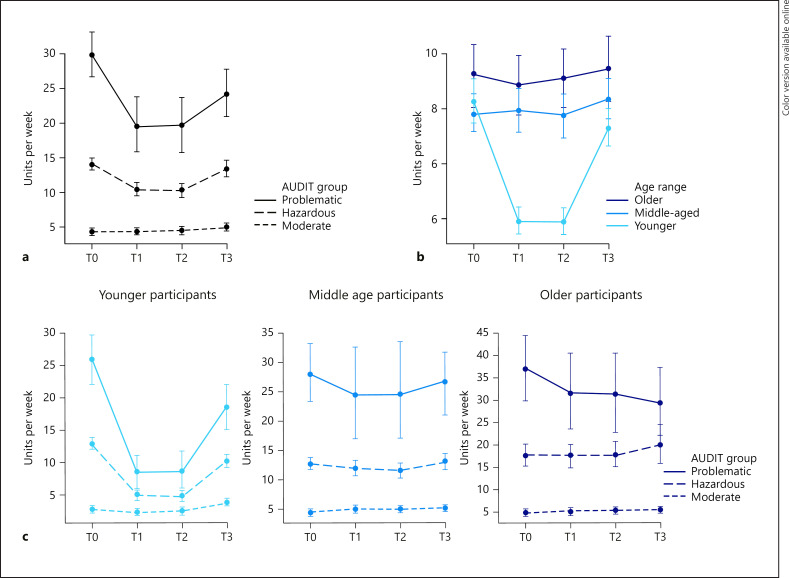
Negative Binomial Model
Independently of measurement times, the model1 indicated that alcohol consumption in drinkers was predicted by drinking patterns, with higher consumption among hazardous and problematic drinkers than moderate drinkers (z = 24.40, SE = 0.020, p < 0.001), and among problematic compared to hazardous drinkers (z = 5.27, SE = 0.049, p < 0.001; Fig. 2a). This result was expected since our groups of drinkers were based on AUDIT scores, which included a measure of weekly alcohol consumption at T0. Age also predicted alcohol consumption, with higher consumption among middle-aged and older participants compared to younger participants (z = 8.96, SE = 0.023, p < 0.001; Fig. 2b).
Fig. 2.
Number of alcohol units consumed per week at T0, T1, T2, and T3 according to AUDIT scores (a), age-group (b) and their interaction (c). AUDIT, alcohol use disorder identification test.
Regarding measurement times, the first planned contrast indicated that alcohol consumption significantly decreased during lockdown (T1 and T2) compared to before and after lockdown (T0 and T3; z = 16.20, SE = 0.008, p < 0.001). Interactions revealed that this effect was driven by younger participants with hazardous and problematic drinking patterns (z = −7.41, SE = 0.004, p < 0.001; Fig. 2c). This effect was explained by a stronger decrease of consumption during lockdown in younger than middle-aged and older participants (z = −18.57, SE = 0.006, p < 0.001; Fig. 2b), and in hazardous and problematic than moderate drinkers (z = 8.00, SE = 0.005, p < 0.001; Fig. 2a).
The second contrast comparing T0 and T3 indicated the absence of a general rebound effect, as participants' alcohol consumption level, as a whole, did not differ during these measurement times (p > 0.050). Interactions indicated that younger participants more strongly decreased their alcohol consumption after lockdown offset compared to before lockdown onset than middle-aged and older participants (z = −3.03, SE = 0.007, p = 0.002; Fig. 2b). In the same vein, problematic drinkers showed a stronger decrease in their consumption between T0 and T3 than hazardous drinkers (z = 2.71, SE = 0.014, p = 0.007; Fig. 2a). Results also revealed a slight increase of alcohol consumption between T0 and T3 in moderate drinkers, which was not reported in hazardous and problematic drinkers (z = 6.41, SE = 0.007, p < 0.001, Fig. 2a), showing the presence of a rebound effect in this subgroup. This effect was specific to younger moderate drinkers, while the opposite pattern was found among younger hazardous and problematic drinkers who rather showed lower consumption at T3 than T0 (z = −4.33, SE = 0.005, p < 0.001; Fig. 2c). The third contrast comparing T1 and T2 showed that alcohol consumption did not vary during the different stages of lockdown in any subgroup of participants (all p values >0.050).
Discussion
Alcohol consumption during COVID-19-related lockdown has raised concerns among researchers and clinicians. We conducted a longitudinal study measuring alcohol consumption during and after lockdown in a large sample of adults, while considering 2 major risk factors described in previous studies, namely, age and pre-lockdown consumption patterns [10, 11, 12].
Our results firstly showed the major effects of age and pre-lockdown drinking patterns on alcohol consumption during the current health crisis. Independently of the stages of the survey, older and middle-aged participants showed higher consumption than younger ones. As expected, problematic drinkers reported the highest consumption at each measurement time, followed by hazardous and moderate drinkers. These findings confirmed the need to consider these 2 factors to fully understand consumption's variations.
Regarding our first hypothesis, we observed a general pattern of decreased consumption during lockdown in the whole sample, in comparison with the period preceding or following lockdown. Surprisingly, both hazardous and problematic drinkers decreased their consumption during lockdown, by almost 4 and 10 units per week, respectively. Moderate drinkers did not show such changes after lockdown onset, probably due to their already low pre-lockdown consumption. These findings go against previous results [11, 16] suggesting that pre-pandemic heavy drinking may constitute a risk factor for increasing consumption during lockdown. Such conflicting results might be explained by differences in alcohol-related culture and norms across samples, but also by differences with previous studies in terms of drinking severity assessment (e.g., amount of alcohol units per week rather than AUDIT [16]) or sample size (e.g., only 132 participants presenting harmful/hazardous drinking patterns [11]). Our findings also showed that this pattern actually concerned younger participants with hazardous and problematic drinking patterns, who decreased their consumption following lockdown onset and then re-augmented it after lockdown offset. The former finding is in line with most previous studies showing that younger individuals were more likely to reduce their consumption during lockdown [9, 10, 11]. The latter may be attributable to the re-emergence of drinking contexts at lockdown offset (e.g., re-opening of bars/restaurants, return to normal social interactions), known to be associated with high consumption in youth.
Our second hypothesis regarding a general rebound effect was not confirmed, as average consumption in our whole sample went back to pre-lockdown levels after lockdown offset, but without exceeding them. Moreover, while we observed a globally increased consumption after lockdown offset, problematic drinkers did not reach their pre-lockdown consumption (T0: ∼30 U/week, T3: ∼24 U/week), unlike hazardous drinkers (T0 and T3: ∼14 U/week). As such, the lockdown period might have been protective for problematic drinkers, as their consumption after lockdown offset re-augmented, but without getting back to their pre-lockdown consumption. Conversely, moderate drinkers showed a slight rebound effect at lockdown offset (increase by <1 U/week compared to pre-lockdown and lockdown periods). The interaction between drinking patterns and age revealed that post-lockdown consumption was higher than before lockdown in younger moderate drinkers, expressing a slight rebound effect in this subgroup.
Finally, our findings showed that the whole sample kept their alcohol consumption quite stable throughout lockdown (T1 and T2). The stability of the consumption pattern during lockdown is supported across ages and previous alcohol consumption patterns, as no subgroup showed a significant difference between T1 and T2.
The present findings have key implications at theoretical and clinical levels. First, this longitudinal study provides new insights on changes in alcohol consumption during the COVID-19 lockdown period in a large sample of individuals. Beyond the short-term effect of lockdown onset on drinking behaviours explored in previous studies, our findings offer a first global overview of consumption before, during, and after the first lockdown. We identified the lockdown offset as a key period regarding consumption changes, particularly in youth. The potential for increased alcohol consumption or rebound effects in some subgroups (e.g., college students or individuals diagnosed with alcohol use disorder) should be further investigated in future studies with more representative samples, particularly in view of the repeated alternation between lockdown and less restrictive periods throughout the persisting crisis. Second, our findings surprisingly showed that lockdown had a protective effect on the general population, as most of our sample decreased their alcohol consumption after lockdown onset, but also kept it stable throughout the lockdown period. This was particularly true for participants with hazardous or problematic drinking patterns before lockdown, thus reinforcing the protective effect of lockdown on the more vulnerable individuals regarding alcohol consumption. Such result might be explained by the drastic reduction of social activities and meetings (e.g., reduction of social contact, closure of bars and restaurants), but also by the awareness of the population regarding the consequences related to acute drug consumption during a sanitary crisis (e.g., injuries, domestic violence, and hospitalizations). Identifying subgroups that decreased their consumption at key stages of the current sanitary crisis might help to promote the positive effects of temporary abstinence (or alcohol use reduction) on their well-being and mental health [28]. Finally, at-risk subgroups who increased consumption after lockdown offset (e.g., younger individuals) might benefit from the development of prevention and intervention programs, to lower the risk of developing alcohol-related disorder [29] and its related health consequences (including an increased vulnerability towards COVID-19 infection [6]).
This study bares some limitations. Firstly, the evaluation of alcohol consumption at each measurement time focused on subjective self-reported measures, which might have limited the accuracy of participants' responses [30]. Secondly, the results regarding alcohol consumption before lockdown onset (T0) were recorded retrospectively, which was unavoidable but might have led to evaluation biases. Moreover, as all longitudinal studies involving the repeated use of similar evaluation tools at various time points, our findings were at risk of leading to a “regression towards the mean” phenomenon that might partly explain the decrease in reported consumption at T3. It should also be underlined that our final sample was composed of <20% of the initial convenience sample (with a higher percentage of women, elderly, and highly educated individuals), and included less nondrinkers than the general Belgian population (8.6% compared to 23.5%; WHO, 2018). Our sample can thus not be considered as representative of the whole Belgian population. Finally, these results are specifically related to the impact of the first lockdown period on alcohol consumption, and might not be indicative of the further evolution of such consumption throughout the still ongoing worldwide health crisis.
Conclusions
The evolution of alcohol consumption throughout the COVID-19 lockdown period highly varied according to age and pre-pandemic drinking patterns. In our study, younger individuals decreased their alcohol consumption after lockdown onset, especially those with high AUDIT scores. The lockdown offset in turn led to increased alcohol consumption among all participants (especially younger ones) compared to lockdown levels. It only led to a rebound effect among younger moderate drinkers, who might constitute an at-risk population regarding consumption at the end of lockdown periods.
Statement of Ethics
Participants provided their written informed consent before starting the survey. This study complied with the ethical standards of the World Medical Association Declaration of Helsinki (as revised in 2008). In view of the need to acquire data as soon as the beginning of COVID-19-related lockdown, which was unforeseeable, and of the fact that ethical approval cannot be obtained after the start of a study, this study is exempt from Ethical Committee approval regarding the first data acquisition periods, but (1) the study strictly followed the guidelines of the Ethical Committee of the Psychological Sciences Research Institute (UCLouvain, Belgium); (2) the longitudinal part of the study has been approved by the Ethical Committee of the Psychological Sciences Research Institute (UCLouvain, Belgium, Study Approval Number: Projet2020-44).
Conflict of Interest Statement
The authors report no conflict of interest.
Funding Sources
Pierre Maurage (Senior Research Associate), Zoé Bollen, and Coralie Creupelandt (Junior Research Associates) are funded by the Belgian Fund for Scientific Research (F.R.S.-FNRS, Brussels, Belgium). Sullivan Fontesse and Alice Laniepce are supported by the French Community of Belgium with a grant (ARC Grant No. 16/20-071). These funding sources did not exert any influence or censorship on the present work.
Author Contributions
Zoé Bollen contributed to conceptualization, methodology, formal analysis, investigation, project administration, visualization, and writing − original draft. Arthur Pabst contributed to conceptualization, methodology, formal analysis, investigation, project administration, visualization, and writing − review and editing. Coralie Creupelandt contributed to conceptualization, methodology, formal analysis, investigation, project administration, visualization, and writing − review & editing. Sullivan Fontesse contributed to conceptualization, methodology, investigation, visualization, project administration. Alice Laniepce contributed to conceptualization, methodology, project administration, visualization, and writing − review and editing. Pierre Maurage contributed to conceptualization, methodology, investigation, project administration, visualization, and writing − review and editing and supervision.
Data Availability Statement
All data related to this study are available upon request to the authors.
References
- 1.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395((10227)):912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020 Aug;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. 2020 May;5((5)):e259. doi: 10.1016/S2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010 Nov;376((9752)):1558–65. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- 5.Molina PE, Happel KI, Zhang P, Kolls JK, Nelson S. Focus on: alcohol and the immune system. Alcohol Res Health. 2010;33((1–2)):97–108. [PMC free article] [PubMed] [Google Scholar]
- 6.Testino G. Are patients with alcohol use disorders at increased risk for COVID-19 infection? Alcohol Alcohol. 2020 Jun 25;55((4)):344–6. doi: 10.1093/alcalc/agaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anker JJ, Kushner MG. Co-occurring alcohol use disorder and anxiety: bridging the psychiatric, psychological, and neurobiological perspectives. Alcohol Res. 2019 Dec 30;40((1)):arcr.v40.1.03. doi: 10.35946/arcr.v40.1.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rehm J, Kilian C, Ferreira-Borges C, Jernigan D, Monteiro M, Parry CDH, et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. 2020 May;39((4)):301–4. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bollen Z, Pabst A, Creupelandt C, Fontesse S, Lannoy S, Pinon N, et al. Prior drinking motives predict alcohol consumption during the COVID-19 lockdown: a cross-sectional online survey among Belgian college students. Addict Behav. 2021;115:106772. doi: 10.1016/j.addbeh.2020.106772. [DOI] [PubMed] [Google Scholar]
- 10.Callinan S, Smit K, Mojica-Perez Y, D'Aquino S, Moore D, Kuntsche E. Shifts in alcohol consumption during the COVID-19 pandemic: early indications from Australia. Addiction. 2021;116((6)):1381–88. doi: 10.1111/add.15275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chodkiewicz J, Talarowska M, Miniszewska J, Nawrocka N, Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health. 2020 Jun 29;17((13)):4677. doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koopmann A, Georgiadou E, Kiefer F, Hillemacher T. Did the general population in Germany drink more alcohol during the COVID-19 pandemic lockdown? Alcohol Alcohol. 2020 Oct 20;55((6)):698–9. doi: 10.1093/alcalc/agaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. 2020 Nov;110:106527. doi: 10.1016/j.addbeh.2020.106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oksanen A, Savolainen I, Savela N, Oksa R. Psychological stressors predicting increased drinking during the COVID-19 crisis: a Longitudinal National Survey Study of workers in Finland. Alcohol Alcohol. 2021;56((3)):299–306. doi: 10.1093/alcalc/agaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tran TD, Hammarberg K, Kirkman M, Nguyen HTM, Fisher J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J Affect Disord. 2020 Dec 1;277:810–3. doi: 10.1016/j.jad.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neill E, Meyer D, Toh WL, Rheenen TE, Phillipou A, Tan EJ, et al. Alcohol use in Australia during the early days of the COVID-19 pandemic: initial results from the COLLATE project. Psychiatry Clin Neurosci. 2020 Oct;74((10)):542–9. doi: 10.1111/pcn.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mallet J, Dubertret C, Le Strat Y. Addictions in the COVID-19 era: current evidence, future perspectives a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2020 Aug 12;106:110070. doi: 10.1016/j.pnpbp.2020.110070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Available from: https://www.statista.com/statistics/1104709/coronavirus-deaths-worldwide-per-million-inhabitants/
- 19.Lannoy S, Billieux J, Dormal V, Maurage P. Behavioral and cerebral impairments associated with binge drinking in youth: a critical review. Psychol Belg. 2019 Mar 29;59((1)):116–55. doi: 10.5334/pb.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88((6)):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 21.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test (AUDIT) manual: guidelines for use in primary care. Department of Mental Health and Substance Dependence, WHO; 2001. pp. p. 4–32. [Google Scholar]
- 22.Sobell LC, Sobell MB. Measuring alcohol consumption. Totowa, NJ: Humana Press; 1992. Timeline follow-back; pp. p. 41–72. [Google Scholar]
- 23.R Core Team . R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. Available from: https://www.R-project.org/ [Google Scholar]
- 24.Brooks ME, Kristensen K, van Benthem KJ, Magnusson A, Berg CW, Nielsen A, et al. glmmTMB balances speed and flexibility among packages for zero-inflated generalized linear mixed modeling. R J. 2017;9((2)):378–400. Available from: https://journal.r-project.org/archive/2017/RJ-2017-066/index. http://dx.doi.org/10.32614/rj-2017-066. [Google Scholar]
- 25.Warton DI. Many zeros does not mean zero inflation: comparing the goodness-of-fit of parametric models to multivariate abundance data. Environmetrics. 2005;16:275–89. [Google Scholar]
- 26.Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer-Verlag; 2016. ISBN 978–3–319–24277–4. Available from: https://ggplot2.tidyverse.org. [Google Scholar]
- 27.Harrell FE, With Contributions from Charles Dupont and Many Others “Hmisc: harrell miscellaneous.” R package version 4.0-1. 2020 [Google Scholar]
- 28.de Visser RO, Nicholls J. Temporary abstinence during dry January: predictors of success; impact on well-being and self-efficacy. Psychol Health. 2020 Nov;35((11)):1293–305. doi: 10.1080/08870446.2020.1743840. [DOI] [PubMed] [Google Scholar]
- 29.The Lancet Gastroenterology Hepatology Drinking alone: COVID-19, lockdown, and alcohol-related harm. Lancet Gastroenterol Hepatol. 2020 Jul;5((7)):625. doi: 10.1016/S2468-1253(20)30159-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Del Boca FK, Darkes J, McRee B. Self-report assessments of psychoactive substance use and dependence. In: Sher KJ, editor. The Oxford handbook of substance use and substance use disorders. Oxford University Press; 2016. pp. p.430–65. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data related to this study are available upon request to the authors.