Abstract
COVID-19 pandemic situation has affected millions of people with tens of thousands of deaths worldwide. Despite all efforts for finding drugs or vaccines, the key role for the survival of patients is still related to the immune system. Therefore, improving the efficacy and the functionality of the immune system of COVID-19 patients is very crucial. The potential new, non-invasive, FDA-approved biophysical technology that could be considered in this regard is tumor treating fields (TTFields) based on an alternating electric field has great biological effects. TTFields have significant effects in improving the functionality of dendritic cell, and cytotoxic T-cells, and these cells have a major role in defense against viral infection. Hence, applying TTFields could help COVID-19 patients against infection. Additionally, TTFields can reduce viral genomic replication, by reducing the expressions of some of the vital members of DNA replication complex genes from the minichromosome maintenance family (MCMs). These genes not only are involved in DNA replication but it has also been proven that they have a crucial role in viral replication. Also, TTFields suppress the formation of the network of tunneling nanotubes (TNTs) which is knows as filamentous (F)-actin-rich tubular structures. TNTs have a critical role in promoting the spread of viruses through improving viral entry and acting as a protective agent for viral components from immune cells and even pharmaceuticals. Moreover, TTFields enhance autophagy which leads to apoptosis of virally infected cells. Thus, it can be speculated that using TTFields may prove to be a promising approach as a subsidiary treatment of COVID-19.
Graphical abstract
Keywords: Bioelectricity, Biophysical treatment, COVID-19, TTFields, Immunity system
Introduction
Novel coronavirus disease (COVID-19) has affected millions of people and has caused thousands of deaths worldwide. This pandemic has caused unpresented health, economic, and even cultural crises around the world [1]. Furthermore, in addition to its direct consequences, this infection has adversely impacted daily practice of medicine by its interference in the medical system and introduced new challenges to public health [2–5]. SARS-CoV-2 is the human beta-coronavirus that caused COVID-19. CoVs are enveloped, positive-sense single-stranded RNA viruses from the family of the Coronaviridae. This family of viruses is mainly characterized by club-like spikes that project from their surface, an unusually large RNA genome, and a unique replication strategy [6–8]. The virus mainly targets the lower respiratory system, leading to acute respiratory distress syndrome (ARDS) which may lead to death. Generally, the functional cycle of this virus is like other viruses, which include the steps of entering the cell, replicating its genomic structure, and forming new viruses that attack other healthy cells by destroying the primary cell and aggravating the symptoms of the disease, and eventually, the patient cannot survive if the immune system cannot rescue its defense [9–11]. However, the main cause of COVID-19 disease severity is a strong inflammatory process called a cytokine storm, which ultimately leads to organ failure and patient death [12–15]. Steps of disease progression in COVID-19 include viral replication and mild symptoms in the early infection phase, adaptive immunity stimulation and predominance of respiratory symptoms in the pulmonary phase, and hyperinflammatory conditions such as ARDS in the hyper inflammation phase. Clinical manifestations include fever, non-productive cough, dyspnea, myalgia, fatigue, normal or decreased leukocyte counts, and radiographic evidence of pneumonia [16, 17]. Since, drug delivery in lung tissue has complications, there have been attempts that should be made to fight COVID-19 locally at the infected sites [18]. Also, recent studies focused on finding molecular therapies based on blocking the entrance of virus into healthy cells by blocking receptors at the site of virus binding (such as angiotensin receptor blockers (ARBs)) [19]. However, the key role in the survival of patients is still related to the systemic immune system. Hence, improving the efficacy of the immune system of COVID-19 infected patients is very critical in improving the outcome in the affected population [20]. Moreover, in spite of many efforts to identify chemical-based methods for the treatment of COVID-19 infection, there is no effort or even speculation about potential applications of biophysical means for the treatment of COVID-19. Furthermore, there are some similarities in the biological aspects of cancerous cells, and virally infected cells [21, 22]. For example, it has been proven that conversion of a healthy cell to a cancerous cell is initiated by alterations in the metabolic pathways. Interestingly, viruses can stimulate a metabolic pathway similar to that of tumor cells in their host tissues and even in the neighboring cells which lead to uncontrolled proliferation [23]. Also, the similarity between some cancer treatment methods and treatment of viruses has been reported [24]. Also, recent editorial investigators from the University of Pennsylvania have proposed performing FDG-PET-CT to detect and characterize systemic manifestations of COVID-19 infection in various organs in the body. FDG is avidly taken up by the inflammatory cells which can be readily visualized by this imaging modality. Since COVID-19 virus causes significant inflammation in the lungs, GI tract, lymph nodes, and cardiovascular structures, total body imaging by PET allows visualizing systemic manifestation of this very aggressive infection. Furthermore, FDG-PET imaging allows to detect cerebral complications of this disease which are relatively common and are a major cause of disability in this population. Also, FDG is heavily taken up by the venous clots which are known to develop in patients with this infection. In addition, PET imaging provides quantitative data and this allows monitoring the course of the disease and assessing response to standard and experimentation interventions. Therefore, performing FDG-PET-CT imaging will substantially enhance our ability to assess COVID-19 patients at various stages of this dangerous and potentially fatal disease. This will lead to optimal management of these patients [25]. Also, recently low-dose radiation therapy has been suggested for the treatment of COVID-19 [26].Thus, based on the success of biophysical treatment of cancer, we propose a biophysical subsidiary treatment method for COVID-19 [27–29]. We believe that biophysical approaches which are based on recently introduced technologies may allow treating COVID infections locally, particularly in the lungs [30–34].
Current coping strategies with COVID-19
We wish to indicate that of approximately 44 SARS-CoV-2 candidate vaccines that were in clinical trials (phase I–III) and additional 164 candidates have been in preclinical stages; currently, just 8 vaccines may achieve a certificate for using in human [35]. Currently, the Pfizer, Moderna, and Astro-Zeneca vaccines have been approved by the FDA and WHO. Additionally, in spite of promising results that have been reported following the administration of COVID-19 vaccines, allergic reactions to vaccines have been observed [36, 37]. Developing vaccine has been a time-consuming process and producing a large volume for immunizing a large population, has been very challenging [38, 39]. Also, mutation of SARS-COV-2 viruses is of concern about controlling this pandemic situation in the future [40, 41].
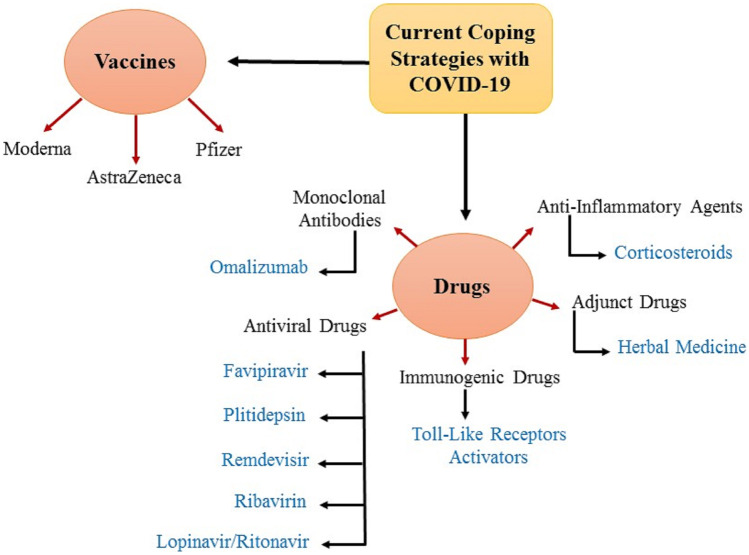
Drugs for COVID-19 can be categorized into five main groups. Antiviral drugs for COVID-19 include Ribavirin, Favipiravir, Remdevisir, Lopinavir/ritonavir (LPV/RTV), and Plitidepsin. This group mainly acts by interfering in viral replication, and is considered as anti-replicative drugs [16, 42, 43]. Remdevisir has attracted the most attention among antiviral drugs for COVID-19. The next group is anti-inflammatory agents, which is used for inhibiting cytokine storm and attenuating hyperinflammation [44]. The most important drugs in this category are corticosteroids [45, 46]. Another group is the drugs that activate special segments of the immune system against viruses, which are called immunogenic drugs, and play a key role in linking innate and adaptive immunity such as activators of toll-like receptors (TLR)[47, 48]. Other groups of drugs are monoclonal antibodies which are suitable candidates for immune therapy of COVID-19 like Omalizumab [49–51]. The last group of drugs against COVID-19 is adjunct drugs. They include stem cell treatments and herbal medicine [52]. Additionally, using combination of drugs like the combination of Lopinavir and ritonavir in combination with interferon β or using antibodies along with corticosteroids has also been suggested [53, 54]. A brief schematic of the most important current coping strategies with COVID-19 infection is illustrated in Fig. 1.
Fig. 1.
An overview of the most important current coping strategies with COVID-19
Similarities of treatment for cancer and COVID-19
In an interesting recent study for finding novel potential drugs by virtual screening of their molecular dynamics has shown that seven drugs can be promising candidates against COVID-19. These drugs are sapanisertib, ornidazole, napabucasin, lenalidomide, daniquidone, indoximod, and salicylamide. Among these, sapanisertib, napabucasin, lenalidomide, daniquidone, and indoximod are anticancer drugs. Also, except for indoximod which improves T cell function against cancer cells, the others have anti-replication effects [55]. Hence, it can be concluded that anticancer drugs based on anti-DNA or RNA are good candidates for coping with COVID-19. This can be related to the biology, and treatment strategies between cancerous cells and virally infected cells, as noted above. But, certainly one of the most important molecular mechanisms of similarity between cancer and viral infection is related to their genomic replication [21–23].
Generally, the scientific rationale and molecular mechanisms which link viral replication in virally infected cells and DNA replication in cancer cells are based on a family of proteins called the minichromosome maintenance (MCM) Family [56, 57]. MCM proteins were first recognized in the yeast Saccharomyces cerevisiae and identified to have an essential role in DNA replication in all eukaryotic cells. They exhibit helicase activity in replication initiation and play essential roles in limiting replication in each cell cycle. At least 10 homologs of them have been characterized in humans, among which the MCM2–7 complex contributes to the pre-replication complex formation and exhibits helicase activity [58]. Overexpression of MCMs are detected in various cancer cell lines, and clinically correlated to carcinogenesis. So, MCMs are candidate markers for cell proliferation, and increasing in their level are considered as biomarkers for various malignancies [59–61].
Interestingly, it has been proven that MCMs have a vital role in viral replication. Its roles were confirmed by depleting MCMs and assaying transient and long-term maintenance of the viral episomes. In fact, MCMs cooperate with LANA during the G1/S phase of the cell cycle to support viral DNA replication. Latency-associated nuclear antigen (LANA) is a viral gene that serves as the master regulator of latency. Also, this protein is a multifunctional nuclear protein that has an important role in inducing malignancies [62]. Furthermore, MCM proteins are associated with RNA polymerase II holoenzyme, which plays a key role in SARS-CoV-2 genome replication [63, 64]. Moreover, even though the MCM complex is thought to be a DNA replicative helicase, in research studying replication of the influenza virus RNA, it has been proved that MCM interacted with the PA subunit of the viral RNA-dependent RNA polymerase that is found to be involved in the replication genetically. This function is attributed to the MCM functions, and being a scaffold between the nascent RNA chains and the viral polymerase [65]. As mentioned before, several researchers proved that RNA-dependent RNA polymerase has a vital role in SARS-CoV-2 genome replication [66]. So, owing to similarities between the influenza virus, and the SARS-COV-2 virus, it seems that MCMs also have a key function in SARS-COV-2 viral replication [67, 68].
Also, another molecular mechanism that has a resemblance in virally infected cells and cancer cells is related to the function of the network of tunneling nanotubes. Network of tunneling nanotubes (TNTs) are well-known filamentous (F)-actin-rich tubular structures that have been connected to the cytoplasm of the adjacent and or distant cells to mediate efficient cell-to-cell communication. They are composed of long cytoplasmic bridges with a terrific ability to accomplish a diverse array a wide range of functions including maintenance of cellular physiology and cell survival up to promoting immune surveillance [69, 70]. Ironically, the crucial impact of TNTs in the progression of many types of cancer especially in their metastases process them has been well studied [71, 72].
Interestingly, the critical role of TNTs in promoting the spread of various pathogens including viruses either during the early or late phases of their lifecycle has widely been documented. Actually, TNTs facilitate viral entry and replication, especially for SARS-COV-2 viruses. Moreover, it has been reported that TNTs can be used by viruses for evading from host immunity and avoiding pharmaceutical targeting by using them to pass their genomes to naive cells. Also, apart from acting as a protective agent for viral components from the extracellular environment, employing TNTs for the propagation of viral infection is more energetically favorable than other possible pathways [73, 74]. Hence, the role of TNTs in transferring mRNAs, viral RNAs, and non-coding RNAs makes it a suitable target for finding new approaches against COVID-19 [70, 73, 75].
Moreover, one more molecular mechanism in which viral replication in the viral infected cell and cancer cells have similarities is the role of eukaryotic-translation-elongation-factor-1-alpha (eEF1A). eEF1A not only has a major role in the delivery of all aminoacyl-tRNAs to the ribosome, except for initiator and selenocysteine tRNAs but it has also several roles including the regulation of the actin cytoskeleton, controlling cell proliferation and cell death, and the cultivation of viral replication[76, 77]. Additionally, it has high expression in tumors. Hence, its high level may be considered as a tumor marker [78–80].
Furthermore, the role of eEF1A in replication of SARS-COV-1, respiratory syncytial virus (RSV), and other RNA virus replication and pathogenesis has been proved previously [81–85]. Also, the association between eEF1A and RNA polymerase II as a key factor in SARS-COV-2 viral replication makes it a suitable target for designing or repurposing drugs [86]. Ironically, Plitidepsin which is an anti-tumor drug and targets eEF1 has been repurposed for COVID-19 infection. Moreover, in vitro study has demonstrated that Plitidepsin has better potential than Remdevisir against SARS-CoV-2 by a factor of 27.5, with lower toxicity in cell culture [87–90].
Subsequently, another area that has things in common between virology and cancer biology is autophagy. Autophagy or self-eating is an evolutionarily conserved degradative process in which cytoplasmic components located in eukaryotic cells which are captured for subsequent degradation through lysosomal hydrolases. Also, it is crucial to maintain homeostasis and avoiding from nutritional, metabolic, and infection-mediated stresses [91]. Moreover, its role in diseases progression especially cancers in different stages of them has been discussed previously [92, 93]. Also, autophagy plays important role in viral replication and coordinates adaptive immunity by delivering virus-derived antigens for presentation to T lymphocytes [94]. Moreover, in some viruses, they evolved anti-autophagy strategies to hide from host immunity and cultivate viral replication [95]. Hence, it can be speculated that autophagy could be a suitable therapeutic target for COVID-19. Ironically, it has been reported that based on the settled cross-talk between autophagy and apoptosis, increasing autophagy can lead to apoptosis of virally infected cells and disrupts the viral replication cycle [96].
Furthermore, sensitivity and function of T cells and dendritic cells have great importance in cancer treatment, and overcoming viral infection (like SARS-COV-2) [97–99]. So, the rational for proposing indoximod for COVID-19 treatment may also indicate some similarity between cancer treatment drugs and antiviral agents against SARS-COV-2 viruses [100, 101].
Hence, it seems that treatments of COVID-19 and cancer have several similarities. Therefore, if we can find a suitable physical treatment for cancer that can interfere with MCM and TNT functions for avoiding from SARS-COV-2 viruses’ replication, and improve the T cells and dendritic cells (DC cells), also increased autophagy, it could also have great potential for application as a subsidiary treatment for COVID-19 infection. Fortunately, the technology that can fulfill these qualifications is available and named as the fourth modality against cancer; this technology is tumor treating fields (TTFields) [102].
Tumor treating fields, its benefits, and COVID-19
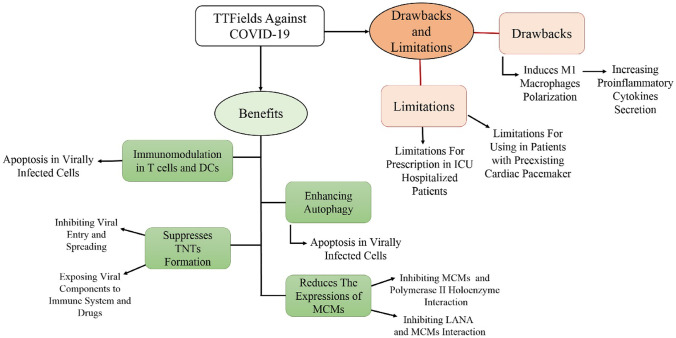
Tumor treating fields (TTFields) technology is a non-invasive treatment technology based on the alternate electrical field and the biophysical phenomenon of dielectrophoresis. Its therapeutic effects are based on preventing mitosis by disturbing genomic polymerization, as well as disruption of the mitosis spindle, and creation of a heterogeneous electric field in the cell, resulting in dysfunction in cancer cells [103–105]. Briefly, TTFields has several mechanisms of beneficial action in cancers including being anti-mitotic, inhibiting DNA repair (through reducing MCMs expression), immunomodulation, increasing cell membrane permeability, hindering migration and metastases (through reduction in signaling including nuclear factor (NF)-κB-, mitogen-activated protein kinase (MAPK)-, and phosphatidylinositol 3-kinase (PI3K)/Akt-dependent), attenuating TNT formation, and enhancing autophagy (Fig. 2b) [106–108]. Also, it can be applied through different arrays of electrodes on the head, chest, and abdomen for several types of cancer (Fig. 2a). Owing to the great ability in cancer treatment and its flexibility for administration in different cancers, it has been nominated as the fourth modality in cancer treatment [102, 109–114].
Fig. 2.
a Possibility for applying TTFields for several types of cancers by using different arrays of electrodes on the head, chest, and abdomen. b Mechanisms for being advantageous in applying TTFields against cancer
Moreover, it was confirmed that TTFields not only attenuate the rejoining of radiation-induced DNA double-strand breaks (DSBs) but they also induce DNA DSBs. The mechanism of this phenomenon is shown that TTFields reducing in the expressions of MCMs include MCM6 and MCM10 and the Fanconi’s Anemia pathway genes [115]. As mentioned above, MCMs were introduced as replication licensing factors, which are proved that play an essential role in viral genomic replication in vivo as well as in vitro [62, 63, 65, 66, 116]. So, it seems that TTFields can reduce SARS-COV-2 viral genome replication, which is very important for stopping the pathogenesis process of viruses.
Furthermore, it has been reported that TTFields can suppress the formation of TNTs drastically, and as far as mentioned above, TNTs can facilitate SARS-COV-2 viral entry, and evading them from the immune system and pharmaceutical targeting [73, 108]. Hence, it can be speculated that TTFields not only can reduce SARS-COV-2 viral entry, and replication, but it can also enhance the efficiency of the immune system and antiviral pharmaceuticals against them.
Additionally, as far as mentioned above, TTFields enhances autophagy, and increasing autophagy in SARS-COV-2 virally infected cells can lead to apoptosis in them[96, 106, 107, 117]. Hence, it can be supposed that TTFields can induce apoptosis in SARS-COV-2 virally infected cells subsequently disrupt the viral replication cycle.
Also, this heterogeneous electric field can disrupt the enzymatic function of the cell during the synthesis of genomic material, and even induce apoptosis in the abnormal cell [105, 118]. Moreover, the most important regions that can be invaded and damaged by COVID-19 infection are located in the chest and abdomen. Also, considering the presence of different electrode arrays for covering this area (Fig. 2a), it can be assumed that TTFields may be beneficial for preventing from multi-organ damages related to COVID-19 infection. Another advantage of this treatment is that it does not harm healthy cells; therefore, it is FDA-approved [104]. Also, the safety of using TTFields for glioblastoma patients in the COVID-19 pandemic situation has been proved by experts [119]. Moreover, another key advantage of TTFields is improving the function of the immune system and inducing immunogenicity, which improves the function of dendritic cells as an antigen-presenting cell and increases the sensitivity and function of cytotoxic-T cells [102, 120–122]. Additionally, it has been suggested that one of the key problems of the immune system in COVID-19 is the loss of bridging between innate and adaptive immunity [123]. Interestingly, both of these cells play an important role in the treatment of COVID-19 viral infection also, bridging between the innate and adaptive immune system. Another important point is that this technology can be used as a monotherapy or combinational therapy with other therapies such as Remdevisir [124–128]. This technology has now reached phase II of clinical trials for lung cancer [113]; using this technology is very simple and only requires putting its electrodes on the chest wall of the patient and selecting the suitable frequency. Therefore, TTFields can reduce the degree of SARS-COV-2 viral replication and as such can improve the efficiency by activating immune cells like dendritic cells and cytotoxic T cells.
Despite all advantages mentioned before, applying TTFields against COVID-19 infection may be faced with drawbacks and limitations. The first consideration that should be noted is that TTFields have a novel immunoregulatory effect on macrophages by stimulation changing M2 macrophages to the M1 [129–131]. Also, as far as mentioned in the literature, M1 macrophage is responsible for increasing pro-inflammatory cytokines like IL-1β, IL-12, TNF-α, and nitric oxide synthase (iNOS) which may help to cytokine storm [132–134]. Thus, targeting macrophages is suggested as a therapeutic option for COVID-19 infection [135]. Hence, using anti-inflammatory pharmaceuticals along with applying TTFields can be a solution for this challenge [136–138]. However, the role of macrophages in COVID-19 is a controversial area [139, 140].
However, the most important limitation is related to the limitations for prescribing TTFields against COVID-19 in patients who need to be hospitalized in intensive care units (ICU), or critical care units (CCU). Also, considering the demand for accurately controlling and monitoring of vital characteristics of patients in critical condition especially for intubated patients, which is needed to connect so many critical care monitoring types of equipment to the patient’s body [141, 142]. Therefore, it is possible that there is not enough space on the body of patients especially on the chest area for putting TTFields electrodes. Also, the possible electrical interference between TTFields and critical care devices is a great obstacle for applying TTFields in patients in critical conditions. Hence, it seems that TTFields just can be used for COVID-19 patients before critical condition. However, more studies are needed for coordinating applying TTFields with guidelines related to the management of COVID-19 patients during hospital admission in a non-intensive care setting [143]. So, it seems that TTFields can be considered as a suitable subsidiary treatment for COVID-19 patients before hospitalization in ICU, especially in patients with comorbidities who are associated with a higher risk of mortality [144–147]. Additionally, there are some limitations for applying TTFields in patients with a pre-existing cardiac pacemaker [148].
As such using the tumor treatment field could be proposed as an appropriate subsidiary treatment of COVID-19 especially for patients before reaching to critical stages of diseases, especially those with comorbidities. Also, the potential mechanism for the benefits, drawbacks, and limitations of using TTFields technology for coping with COVID-19 infection is shown in Fig. 3.
Fig. 3.
Potential mechanism for the benefits, drawbacks, and limitations of using TTFields technology for coping with COVID-19 infection
The optimal instrument for using this technology is Novo TTFields -100L and the frequency range that could be administrated between 150 and 200 kHz with the voltage 1–2 V/cm. The period for exposing the patient to TTFields is 12 h a day. The system has also a portable device that can be operated from a standard wall socket or a portable battery pack [103, 113]. In a clinical trial, one could select a control group with conventional treatment, and an experimental group with combination of both conventional treatment and exposure to TTFields, respectively. Moreover, it should be noted that before applying this system in a clinical trial, it should be evaluated in the in vitro and in vivo studies.
Conclusion
Since the future course of the COVID-19 pandemic is uncertain at this time, exploring new treatment options for viral infections is very timely and well justified. Biophysics modalities have shown promising results in challenging domains like cancers. Therefore, applying biophysical interventions like TTFields should be considered in the future. So, owing to the critical role of the immune system in COVID-19 patients, and the role of TTFields in improving the functionality of dendritic cells, and cytotoxic T cells, and the major role of these cells for defense against viral infection, it can be concluded that applying TTFields can help COVID-19 patients against this disease. Moreover, TTFields can reduce viral genomic replication by decreasing the expression of MCMs. Also, TTFields suppress the formation of the TNTs which plays a major role in promoting the spread of viruses through improving viral entry and acting as a protective agent for viral components from immune cells and even pharmaceuticals. Moreover, TTFields lead to apoptosis in SARS-COV-2 virally infected cells through increasing autophagy in them. However, TTFields can induce macrophage polarization to the M1 type. So, the administration of anti-inflammatory drugs along with TTFields is necessary to avoid hyperinflammation. It is far-fetched that this technology is able to use in patients admitted to the ICU. Subsequently, it should be noted that this technology is non-invasive, safe, and convenient. Thus, it could be considered as an appropriate subsidiary treatment for COVID-19 patients especially before reaching critical stages of diseases, particularly those with comorbidities.
Acknowledgements
The authors are very appreciative of Mrs. Azadeh Shamsnejad for her critical efforts in the English language editing of the manuscript.
Author contribution
The major roles of professors including Carolina Scagnolari, Jafar Ai, and Nima Rezaei were supervising in searching, also editing the manuscript. The major roles of other co-authors were searching, reviewing articles, and extracting the gist of each article for preparing the manuscript. Also, Dr.Mohammad Hasan Shoormeij helped us in improving our manuscript from the clinical aspects, also in designing new figures.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval
Not applicable.
Consent to participate
The authors declare that they have completely consent to participation.
Consent for publication
The authors declare that they have completely consent to publication.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ahmad Reza Farmani, Email: ahmadrezafarmani66@gmail.com.
Forough Mahdavinezhad, Email: mahdaviforough@gmail.com.
Carolina Scagnolari, Email: carolina.scagnolari@uniroma1.it.
Mahsa Kouhestani, Email: mahsa.bah.k@gmail.com.
Sadegh Mohammadi, Email: s.mohammadi.ippi@gmail.com.
Jafar Ai, Email: jafar_ai@tums.ac.ir.
Mohammad Hasan Shoormeij, Email: mhshoormeij@gmail.com.
Nima Rezaei, Email: rezaei_nima@tums.ac.ir.
References
- 1.Hanaei S, Rezaei N. COVID-19: developing from an outbreak to a pandemic. Arch Med Res. 2020;51(6):582. doi: 10.1016/j.arcmed.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Azzi Y, et al. Covid-19 and solid organ transplantation: a review article. Transplantation. 2021;105(1):37–55. doi: 10.1097/TP.0000000000003523. [DOI] [PubMed] [Google Scholar]
- 3.Barba M, et al. Cancer patients and coronavirus disease 2019: evidence in context. J Transl Med. 2020;18(1):315. doi: 10.1186/s12967-020-02483-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Shamsi HO, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25(6):e936–e945. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong YP, Khong TY, Tan GC. The effects of COVID-19 on placenta and pregnancy: what do we know so far? Diagnostics. 2021;11(1):94. doi: 10.3390/diagnostics11010094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison AG, Lin T, Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunology. 2020;41(12):1100–1115. doi: 10.1016/j.it.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin Y, et al. Virology epidemiology pathogenesis and control of COVID-19. Viruses. 2020;12(4):372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexandrova R, et al. The virus that shook the world: questions and answers about SARS-CoV-2 and COVID-19. Biotechnol Biotechnol Equip. 2021;35(1):74–102. doi: 10.1080/13102818.2020.1847683. [DOI] [Google Scholar]
- 9.Shereen MA, et al. COVID-19 infection: origin transmission and characteristics of human coronaviruses. J Adv Res. 2020;24:91. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saghazadeh A, Rezaei N. Immune-epidemiological parameters of the novel coronavirus–a perspective. Expert Rev Clin Immunol. 2020;16(5):465–470. doi: 10.1080/1744666X.2020.1750954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McIntosh K, Hirsch MS, Bloom AJ. Coronavirus disease 2019 (COVID-19): Epidemiology virology and prevention. Lancet Infect Dis. 2020;1:2019–2020. [Google Scholar]
- 12.Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93(1):250–256. doi: 10.1002/jmv.26232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karmakar D, et al. Road map to understanding SARS-CoV-2 clinico-immunopathology and COVID-19 disease severity. Pathogens. 2021;10(1):5. doi: 10.3390/pathogens10010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodrigues TS, et al. Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients. J Exp Med. 2021;218(3):e20201707. [DOI] [PMC free article] [PubMed]
- 15.Chowdhury MA, et al. Immune response in COVID-19: a review. J Infect Public Health. 2020;13(11):1619–1629. doi: 10.1016/j.jiph.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsang HF, et al. An update on COVID-19 pandemic: the epidemiology pathogenesis prevention and treatment strategies. Expert Rev Anti Infect Ther. 2021;19(7):877–888. doi: 10.1080/14787210.2021.1863146. [DOI] [PubMed] [Google Scholar]
- 17.Li X, et al. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Momtazmanesh S, et al. All together to fight COVID-19. Am J Trop Med Hyg. 2020;102(6):1181–1183. doi: 10.4269/ajtmh.20-0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang T, et al. Coronavirus membrane fusion mechanism offers as a potential target for antiviral development. Antiviral Res. 2020;178:104792. [DOI] [PMC free article] [PubMed]
- 20.Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID-19: Friend or foe?. Life Sci. 2020;256:117900. [DOI] [PMC free article] [PubMed]
- 21.Wang XG, et al. Treating cancer as an infectious disease—viral antigens as novel targets for treatment and potential prevention of tumors of viral etiology. PLoS One. 2007;2(10):e1114. [DOI] [PMC free article] [PubMed]
- 22.Benharroch D, Osyntsov L. Infectious diseases are analogous with cancer Hypothesis and implications. J Cancer. 2012;3:117. doi: 10.7150/jca.3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magalhaes I, et al. The metabolic profile of tumour and virally infected cells shapes their microenvironment counteracting T cell immunity. Front Immunol. 2019;10:2309. doi: 10.3389/fimmu.2019.02309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paiardini M, et al. HIV and cancer immunotherapy: similar challenges and converging approaches. Front Immunol. 2020;11:519. doi: 10.3389/fimmu.2020.00519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alavi A, Werner TJ, Gholamrezanezhad A. The critical role of FDG-PET/CT imaging in assessing systemic manifestations of COVID-19 infection. Eur J Nucl Med Mol Imaging. 2021;48:956–962. doi: 10.1007/s00259-020-05148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Venkatesulu BP, et al. Low-dose radiation therapy for COVID-19: promises and pitfalls. JNCI Cancer Spectr. 2021;5(1):pkaa103. [DOI] [PMC free article] [PubMed]
- 27.Pokorný J, et al. Biophysical insights into cancer transformation and treatment. Sci World J. 2013;2013:195028. [DOI] [PMC free article] [PubMed]
- 28.Huang X, et al. Biophysical signal transduction in cancer cells: understanding its role in cancer pathogenesis and treatment. Biochim Biophys Acta Rev Cancer. 2020;1874(2):188402. [DOI] [PubMed]
- 29.Veerasubramanian PK, et al. Biophysical and epigenetic regulation of cancer stemness invasiveness and immune action. Curr Tissue Microenviron Rep. 2020;1(4):277–300. doi: 10.1007/s43152-020-00021-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohamed K, et al. Borderless collaboration is needed for COVID-19—a disease that knows no borders. Infect Control Hosp Epidemiol. 2020;41(10):1245–1246. doi: 10.1017/ice.2020.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parupudi A, et al. Biophysical characterization of influenza a virions. J Virol Methods. 2017;247:91–98. doi: 10.1016/j.jviromet.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Qasim MZ, et al. The potential applications of picotechnology in biomedical and environmental sciences. Environ Sci Pollut Res. 2020;27(1):133–142. doi: 10.1007/s11356-019-06554-4. [DOI] [PubMed] [Google Scholar]
- 33.Prathyusha K, et al. Pico technology: Instruments used and Applications in pharmaceutical field. Research Journal of Pharmaceutical Dosage Forms and Technology. 2018;10(1):34.
- 34.Rabiee N, et al. COVID-19 and picotechnology: potential opportunities. Med Hypotheses. 2020;144:109917. [DOI] [PMC free article] [PubMed]
- 35.Tumban E. Lead SARS-CoV-2 candidate vaccines: expectations from phase III trials and recommendations post-vaccine approval. Viruses. 2021;13(1):54. doi: 10.3390/v13010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rawat K, Kumari P, Saha L. COVID-19 vaccine: A recent update in pipeline vaccines, their design and development strategies. Eur J Pharmacol. 2020;892:173751. [DOI] [PMC free article] [PubMed]
- 37.de Vrieze J. Pfizer's vaccine raises allergy concerns. Sci. 2021;371(6524):10–11. doi: 10.1126/science.371.6524.10. [DOI] [PubMed] [Google Scholar]
- 38.Paltiel AD, et al. Clinical outcomes of a COVID-19 vaccine: implementation over efficacy: study examines how definitions and thresholds of vaccine efficacy coupled with different levels of implementation effectiveness and background epidemic severity translate into outcomes. Health Aff. 2021;40(1):42–52. doi: 10.1377/hlthaff.2020.02054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weintraub RL, et al. COVID-19 vaccine to vaccination: why leaders must invest in delivery strategies now: analysis describe lessons learned from past pandemics and vaccine campaigns about the path to successful vaccine delivery for COVID-19. Health Aff. 2021;40(1):33–41. doi: 10.1377/hlthaff.2020.01523. [DOI] [PubMed] [Google Scholar]
- 40.Dawood AA. Mutated COVID-19 may foretell a great risk for mankind in the future. New Microbes New Infect. 2020;35:100673. [DOI] [PMC free article] [PubMed]
- 41.Grubaugh ND, Hanage WP, Rasmussen AL. Making sense of mutation: what D614G means for the COVID-19 pandemic remains unclear. Cell. 2020;182(4):794–795. doi: 10.1016/j.cell.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.C&EN Global Enterprise. Plitidepsin could fight COVID-19. 2021;99(4):5–5.
- 43.Guisado-Vasco P, et al. Plitidepsin for the management of a cancer patient infected with SARS-CoV-2 while receiving chemotherapy. Ann Oncol. 2021. [DOI] [PMC free article] [PubMed]
- 44.Shende P, Khanolkar B, Gaud RS. Drug repurposing: new strategies for addressing COVID-19 outbreak. Expert Rev Anti Infect Ther. 2021;19(6):689–706. doi: 10.1080/14787210.2021.1851195. [DOI] [PubMed] [Google Scholar]
- 45.Cusinato J, et al. Repurposing drugs for the management of COVID-19. Expert Opin Ther Pat. 2021;31(4):295–307. doi: 10.1080/13543776.2021.1861248. [DOI] [PubMed] [Google Scholar]
- 46.van Paassen J, et al. Corticosteroid use in COVID-19 patients: a systematic review and meta-analysis on clinical outcomes. Crit Care. 2020;24(1):696. doi: 10.1186/s13054-020-03400-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Florindo HF, et al. Immune-mediated approaches against COVID-19. Nat Nanotechnol. 2020;15(8):630–645. doi: 10.1038/s41565-020-0732-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.El-Zayat SR, Sibaii H, Mannaa FA. Toll-like receptors activation signaling and targeting: an overview. Bull Natl Res Cent. 2019;43(1):187. doi: 10.1186/s42269-019-0227-2. [DOI] [Google Scholar]
- 49.Jahanshahlu L, Rezaei N. Monoclonal antibody as a potential anti-COVID-19. Biomed Pharmacother. 2020;129:110337. [DOI] [PMC free article] [PubMed]
- 50.Abdelmaksoud A, Goldust M, Vestita M. Omalizumab and COVID19 treatment: could it help?. Dermatol Ther. 2020. [DOI] [PMC free article] [PubMed]
- 51.Farmani AR, et al. Anti-IgE monoclonal antibodies as potential treatment in COVID-19. Immunopharmacol Immunotoxicol. 2021;43(3):259–264. doi: 10.1080/08923973.2021.1925906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Silveira D, et al. COVID-19: is there evidence for the use of herbal medicines as adjuvant symptomatic therapy? Front Pharmacol. 2020;11:1479. doi: 10.3389/fphar.2020.581840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bhagat S, et al. Novel corona virus (COVID-19) pandemic: current status and possible strategies for detection and treatment of the disease. Expert Rev Anti Infect Ther. 2020;1–24. [DOI] [PubMed]
- 54.Saghazadeh A, Rezaei N. Towards treatment planning of COVID-19: Rationale and hypothesis for the use of multiple immunosuppressive agents: Anti-antibodies, immunoglobulins, and corticosteroids. Int Immunopharmacol. 2020;84:106560. [DOI] [PMC free article] [PubMed]
- 55.Chowdhury KH, et al. Drug repurposing approach against novel coronavirus disease (COVID-19) through virtual screening targeting SARS-CoV-2 main protease. Biology. 2021;10(1):2. doi: 10.3390/biology10010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Forsburg SL. Eukaryotic MCM proteins: beyond replication initiation. Microbiol Mol Biol Rev. 2004;68(1):109–131. doi: 10.1128/MMBR.68.1.109-131.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Das M, et al. MCM paradox: abundance of eukaryotic replicative helicases and genomic integrity. Mol Biol Int. 2014;2014:574850. [DOI] [PMC free article] [PubMed]
- 58.Liu Z, et al. MCM family in HCC: MCM6 indicates adverse tumor features and poor outcomes and promotes S/G2 cell cycle progression. BMC Cancer. 2018;18(1):200. doi: 10.1186/s12885-018-4056-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu S, et al. MCMs in cancer: prognostic potential and mechanisms. Anal Cell Pathol. 2020;2020:3750294. doi: 10.1155/2020/3750294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Das M, et al. over expression of minichromosome maintenance genes is clinically correlated to cervical carcinogenesis. PloS One. 2013;8(7):e69607. [DOI] [PMC free article] [PubMed]
- 61.Hua C, et al. Minichromosome Maintenance (MCM) Family as potential diagnostic and prognostic tumor markers for human gliomas. BMC Cancer. 2014;14(1):526. doi: 10.1186/1471-2407-14-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dabral P, et al. Minichromosome maintenance proteins cooperate with LANA during the G1/S phase of the cell cycle to support viral DNA replication. J Virol. 2019;93(7):e02256–e2318. doi: 10.1128/JVI.02256-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yankulov K, et al. MCM proteins are associated with RNA polymerase II holoenzyme. Mol Cell Biol. 1999;19(9):6154–6163. doi: 10.1128/MCB.19.9.6154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhu W, et al. RNA-dependent RNA polymerase as a target for COVID-19 drug discovery. SLAS Discov. 2020;25(10):1141–1151. doi: 10.1177/2472555220942123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kawaguchi A, Nagata K. De novo replication of the influenza virus RNA genome is regulated by DNA replicative helicase MCM. EMBO J. 2007;26(21):4566–4575. doi: 10.1038/sj.emboj.7601881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen J, et al. Structural basis for helicase-polymerase coupling in the SARS-CoV-2 replication-transcription complex. Cell. 2020;182(6):1560–1573. doi: 10.1016/j.cell.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang Q, et al. Structural basis for RNA replication by the SARS-CoV-2 polymerase. Cell. 2020;182(2):417–428. doi: 10.1016/j.cell.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Friedman N, et al. Transcriptomic profiling of human corona virus (HCoV)-229E -infected human cells and genomic mutational analysis of HCoV-229E and SARS-CoV-2. BioRxiv. 2020; 2020.08.17.253682.
- 69.Cordero Cervantes D, Zurzolo C. Peering into tunneling nanotubes—the path forward. EMBO J. 2021;40(8):e105789. [DOI] [PMC free article] [PubMed]
- 70.Han X, Wang X. Opportunities and challenges in tunneling nanotubes research: how far from clinical application? Int J Mol Sci. 2021;22(5):2306. doi: 10.3390/ijms22052306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sahu P, Jena SR, Samanta L. Tunneling nanotubes: a versatile target for cancer therapy. Curr Cancer Drug Targets. 2018;18(6):514–521. doi: 10.2174/1568009618666171129222637. [DOI] [PubMed] [Google Scholar]
- 72.Hanna SJ, et al. Tunneling nanotubes a novel mode of tumor cell–macrophage communication in tumor cell invasion. J Cell Sci. 2019;132(3):jcs223321. [DOI] [PMC free article] [PubMed]
- 73.Tiwari V, et al. Role of tunneling nanotubes in viral infection neurodegenerative disease and cancer. Front Immunol. 2021;12:2256. doi: 10.3389/fimmu.2021.680891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kumar A, et al. Influenza virus exploits tunneling nanotubes for cell-to-cell spread. Sci Rep. 2017;7(1):40360. doi: 10.1038/srep40360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Haimovich G, Dasgupta S, Gerst JE. RNA transfer through tunneling nanotubes. Biochem Soc Trans. 2020;49(1):145–160. doi: 10.1042/BST20200113. [DOI] [PubMed] [Google Scholar]
- 76.Mateyak MK, Kinzy TG. eEF1A: thinking outside the ribosome. J Biol Chem. 2010;285(28):21209–21213. doi: 10.1074/jbc.R110.113795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abbas W, Kumar A, Herbein G. The eEF1A proteins: at the crossroads of oncogenesis apoptosis and viral infections. Front Oncol. 2015;5:75. doi: 10.3389/fonc.2015.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen S-L, et al. eEF1A1 overexpression enhances tumor progression and indicates poor prognosis in hepatocellular carcinoma. Transl Oncol. 2018;11(1):125–131. doi: 10.1016/j.tranon.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lin C-Y, et al. Contradictory mRNA and protein misexpression of EEF1A1 in ductal breast carcinoma due to cell cycle regulation and cellular stress. Sci Rep. 2018;8(1):13904. doi: 10.1038/s41598-018-32272-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Joung EK, et al. Expression of EEF1A1 is associated with prognosis of patients with colon adenocarcinoma. J Clin Med. 2019;8(11):1903. doi: 10.3390/jcm8111903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhou B, et al. The nucleocapsid protein of severe acute respiratory syndrome coronavirus inhibits cell cytokinesis and proliferation by interacting with translation elongation factor 1α. J Virol. 2008;82(14):6962–6971. doi: 10.1128/JVI.00133-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang X, et al. EF1A interacting with nucleocapsid protein of transmissible gastroenteritis coronavirus and plays a role in virus replication. Vet Microbiol. 2014;172(3):443–448. doi: 10.1016/j.vetmic.2014.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wei T, et al. The eukaryotic elongation factor 1A is critical for genome replication of the paramyxovirus respiratory syncytial virus. PloS One. 2014;9(12):e114447. [DOI] [PMC free article] [PubMed]
- 84.Snape N, et al. The eukaryotic translation elongation factor 1A regulation of actin stress fibers is important for infectious RSV production. Virol J. 2018;15(1):182. doi: 10.1186/s12985-018-1091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li D, et al. The unexpected roles of eukaryotic translation elongation factors in RNA virus replication and pathogenesis. Microbiol Mol Biol Rev. 2013;77(2):253–266. doi: 10.1128/MMBR.00059-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vera M, et al. The translation elongation factor eEF1A1 couples transcription to translation during heat shock response. Elife. 2014;3:e03164. [DOI] [PMC free article] [PubMed]
- 87.White KM, et al. Plitidepsin has potent preclinical efficacy against SARS-CoV-2 by targeting the host protein eEF1A. Science. 2021;371(6532):926–931. doi: 10.1126/science.abf4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rodon J, et al. Identification of Plitidepsin as potent inhibitor of SARS-CoV-2-induced cytopathic effect after a drug repurposing screen. Front Pharmacol. 2021;12:278. doi: 10.3389/fphar.2021.646676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Papapanou M, et al. Plitidepsin: Mechanisms and clinical profile of a promising antiviral agent against COVID-19. J Pers Med. 2021;11(7):668. doi: 10.3390/jpm11070668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Martinez MA. Plitidepsin: a repurposed drug for the treatment of COVID-19. Antimicrob Agents Chemother. 2021;65(4):e00200–e221. doi: 10.1128/AAC.00200-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Khandia R, et al. A comprehensive review of autophagy and its various roles in infectious non-infectious and lifestyle diseases: current knowledge and prospects for disease prevention novel drug design and therapy. Cells. 2019;8(7):674. doi: 10.3390/cells8070674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mulcahy Levy JM, Thorburn A. Autophagy in cancer: moving from understanding mechanism to improving therapy responses in patients. Cell Death Differ. 2020;27(3):843–857. doi: 10.1038/s41418-019-0474-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Suares A, Medina MV, Coso O. Autophagy in viral development and progression of cancer. Front Oncol. 2021;11:147. doi: 10.3389/fonc.2021.603224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Choi Y, Bowman JW, Jung JU. Autophagy during viral infection — a double-edged sword. Nat Rev Microbiol. 2018;16(6):341–354. doi: 10.1038/s41579-018-0003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mao J, et al. Autophagy and viral infection. In: Cui J, et al., editors. Autophagy regulation of innate immunity. Singapore: Springer Singapore; 2019. pp. 55–78. [Google Scholar]
- 96.Shojaei S, et al. Autophagy and SARS-CoV-2 infection: a possible smart targeting of the autophagy pathway. Virulence. 2020;11(1):805–810. doi: 10.1080/21505594.2020.1780088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Palucka K, et al. Dendritic cells and immunity against cancer. J Intern Med. 2011;269(1):64–73. doi: 10.1111/j.1365-2796.2010.02317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Katz SG, Rabinovich PM. T cell reprogramming against cancer. Methods Mol Biol. 2020;2097:3–44. doi: 10.1007/978-1-0716-0203-4_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nagorsen D, et al. Natural T cell immunity against cancer. Clin Cancer Res. 2003;9(12):4296–4303. [PubMed] [Google Scholar]
- 100.Chen Z, Wherry EJ. T cell responses in patients with COVID-19. Nat Rev Immunol. 2020;20(9):529–536. doi: 10.1038/s41577-020-0402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Taefehshokr N, et al. Covid-19: perspectives on innate immune evasion. Front Immunol. 2020;11:2549. doi: 10.3389/fimmu.2020.580641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mun EJ, et al. Tumor-treating fields: a fourth modality in cancer treatment. Clin Cancer Res. 2018;24(2):266–275. doi: 10.1158/1078-0432.CCR-17-1117. [DOI] [PubMed] [Google Scholar]
- 103.Benson L. Tumor treating field’s technology: alternating electric field therapy for the treatment of solid tumors. Semin Oncol Nurs. 2018;34(2):137–150. doi: 10.1016/j.soncn.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 104.Davies AM, Weinberg U, Palti Y. Tumor treating fields: a new frontier in cancer therapy. Ann N Y Acad Sci. 2013;1291(1):86–95. doi: 10.1111/nyas.12112. [DOI] [PubMed] [Google Scholar]
- 105.Wong ET. Alternating electric fields therapy in oncology: a practical guide to clinical applications of tumor treating fields. Cham: Springer; 2016. [Google Scholar]
- 106.Rominiyi O, et al. Tumour treating field’s therapy for glioblastoma: current advances and future directions. Br J Cancer. 2021;124(4):697–709. doi: 10.1038/s41416-020-01136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Karanam NK, Story MD. An overview of potential novel mechanisms of action underlying tumor treating fields-induced cancer cell death and their clinical implications. Int J Radiat Biol. 2021;97(8):1044–1054. doi: 10.1080/09553002.2020.1837984. [DOI] [PubMed] [Google Scholar]
- 108.Sarkari A, Zhai E, Lou E. Tumor-treating fields (TTFields) suppress tunneling nanotube formation in malignant mesothelioma. Int J Radiat Oncol Biol Phys. 2019;105(1):E662. doi: 10.1016/j.ijrobp.2019.06.1058. [DOI] [Google Scholar]
- 109.Giladi M, et al. Mitotic disruption and reduced clonogenicity of pancreatic cancer cells in vitro and in vivo by tumor treating fields. Pancreatology. 2014;14(1):54–63. doi: 10.1016/j.pan.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 110.Grosu A, et al. Phase II HEPANOVA trial of tumor treating fields concomitant with sorafenib for advanced hepatocellular carcinoma. J Clin Oncol. 2019;37(4).
- 111.Michelhaugh SK, et al. Patient-derived metastatic renal carcinoma cells are highly sensitive to in vitro Tumor Treating Fields (TTFields). AACR Annual Meeting 2021; April 10–15, 2021 and May 17–21, 2021; Philadelphia, PA. Philadelphia:AACR; 2021.
- 112.Swanson KD, Lok E, Wong ET. An overview of alternating electric fields therapy (NovoTTF Therapy) for the treatment of malignant glioma. Curr Neurol Neurosci Rep. 2016;16(1):8. doi: 10.1007/s11910-015-0606-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pless M, et al. A phase I/II trial of Tumor treating fields (TTFields) therapy in combination with pemetrexed for advanced non-small cell lung cancer. Lung Cancer. 2013;81(3):445–450. doi: 10.1016/j.lungcan.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 114.Vergote I, et al. Tumor treating fields in combination with paclitaxel in recurrent ovarian carcinoma: Results of the INNOVATE pilot study. Gynecol Oncol. 2018;150(3):471–477. doi: 10.1016/j.ygyno.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 115.Karanam NK, et al. Tumor treating fields cause replication stress and interfere with DNA replication fork maintenance: implications for cancer therapy. Transl Res. 2020;217:33–46. doi: 10.1016/j.trsl.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 116.Nash K, Chen W, Muzyczka N. Complete in vitro reconstitution of adeno-associated virus DNA replication requires the minichromosome maintenance complex proteins. J Virol. 2008;82(3):1458–1464. doi: 10.1128/JVI.01968-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kim EH, et al. Tumor-treating fields induce autophagy by blocking the Akt2/miR29b axis in glioblastoma cells. Oncogene. 2019;38(39):6630–6646. doi: 10.1038/s41388-019-0882-7. [DOI] [PubMed] [Google Scholar]
- 118.Silginer M, et al. Biological activity of tumor-treating fields in preclinical glioma models. Cell Death Dis. 2017;8(4):e2753–e2753. doi: 10.1038/cddis.2017.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gatson NTN, et al. Tumor treating fields for glioblastoma therapy during the COVID-19 Pandemic. Front Oncol. 2021;11:1494. doi: 10.3389/fonc.2021.679702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Voloshin T, et al. Abstract 6662: effects of tumor treating fields (TTFields) on dendritic cells functionality. Cancer Res. 2020;80(16):6662. doi: 10.1158/1538-7445.AM2020-6662. [DOI] [Google Scholar]
- 121.Voloshin T, et al. Tumor-treating fields (TTFields) induce immunogenic cell death resulting in enhanced antitumor efficacy when combined with anti-PD-1 therapy. Cancer Immunol Immunother. 2020;69(7):1191–1204. doi: 10.1007/s00262-020-02534-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Weinberg U, et al. Immunomodulatory effects of tumor treating fields (TTFields) on lung cancer models. Ann Oncol. 2019;30:ii2–ii3.
- 123.Rao VUS, et al. COVID-19: Loss of bridging between innate and adaptive immunity?. Med Hypotheses. 2020;144:109861. [DOI] [PMC free article] [PubMed]
- 124.Zhou R, et al. Acute SARS-CoV-2 infection impairs dendritic cell and t cell responses. Immunity. 2020;53(4):864–877. doi: 10.1016/j.immuni.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Borges RC, Hohmann MS, Borghi SM. Dendritic cells in COVID-19 immunopathogenesis: insights for a possible role in determining disease outcome. Int Rev Immunol. 2020;40(1–2):108–125. doi: 10.1080/08830185.2020.1844195. [DOI] [PubMed] [Google Scholar]
- 126.Campana P, et al. Dendritic cells and SARS-CoV-2 infection: still an unclarified connection. Cells. 2020;9(9):2046. doi: 10.3390/cells9092046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rosendahl Huber S, et al. T cell responses to viral infections–opportunities for peptide vaccination. Front Immunol. 2014;5:171. doi: 10.3389/fimmu.2014.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bieber K, Autenrieth SE. Dendritic cell development in infection. Mol Immunol. 2020;121:111–117. doi: 10.1016/j.molimm.2020.02.015. [DOI] [PubMed] [Google Scholar]
- 129.Wong ET, Timmons J, Swanson KD. Tumor treating fields exert cellular and immunologic effects. AACR Annual Meeting 2018; April 14–18, 2018; Chicago, IL. Philadelphia:AACR; 2018.
- 130.Brant B, et al. A novel immunoregulatory role of tumor treating fields (TTFields) on macrophage polarization. AACR Annual Meeting 2021; April 10–15, 2021 and May 17–21, 2021; Philadelphia, PA. Philadelphia:AACR; 2021.
- 131.Park J-I, et al. Tumor-treating fields induce RAW264. 7 macrophage activation via NK-κB/MAPK signaling pathways. Technol Cancer Res Treat. 2019;18:1533033819868225. [DOI] [PMC free article] [PubMed]
- 132.Kosyreva A, et al. The role of macrophages in the pathogenesis of SARS-CoV-2-associated acute respiratory distress syndrome. Front Immunol. 2021;12:1667. doi: 10.3389/fimmu.2021.682871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sapra L, et al. Phytotherapy for treatment of cytokine storm in COVID-19. Front Biosci. 2021;26(5):51–75. doi: 10.52586/4924. [DOI] [PubMed] [Google Scholar]
- 134.Ombrello MJ, Schulert GS. COVID-19 and cytokine storm syndrome: are there lessons from macrophage activation syndrome? Transl Res. 2021;232:1–12. doi: 10.1016/j.trsl.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gracia-Hernandez M, Sotomayor EM, Villagra A. Targeting macrophages as a therapeutic option in coronavirus disease 2019. Front Pharmacol. 2020;11:1659. doi: 10.3389/fphar.2020.577571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yang L, et al. The signal pathways and treatment of cytokine storm in COVID-19. Signal Transduct Target Ther. 2021;6(1):255. doi: 10.1038/s41392-021-00679-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rowaiye AB, et al. Attenuating the effects of novel COVID-19 (SARS-CoV-2) infection-induced cytokine storm and the implications. J Inflamm Res. 2021;14:1487. doi: 10.2147/JIR.S301784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lariccia V, et al. Challenges and opportunities from targeting inflammatory responses to SARS-CoV-2 infection: a narrative review. J Clin Med. 2020;9(12):4021. doi: 10.3390/jcm9124021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Meidaninikjeh S, et al. Monocytes and macrophages in COVID-19: Friends and foes. Life Sci. 2021;269:119010. [DOI] [PMC free article] [PubMed]
- 140.Lang FM, et al. GM-CSF-based treatments in COVID-19: reconciling opposing therapeutic approaches. Nat Rev Immunol. 2020;20:507–514. doi: 10.1038/s41577-020-0357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hajjar LA, et al. Intensive care management of patients with COVID-19: a practical approach. Ann Intensive Care. 2021;11(1):36. doi: 10.1186/s13613-021-00820-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Poston JT, Patel BK, Davis AM. Management of critically ill adults with COVID-19. JAMA. 2020;323(18):1839–1841. doi: 10.1001/jama.2020.4914. [DOI] [PubMed] [Google Scholar]
- 143.Nielsen Jeschke K, et al. Guideline for the management of COVID-19 patients during hospital admission in a non-intensive care setting. Eur Clin Respir J. 2020;7(1):1761677. doi: 10.1080/20018525.2020.1761677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Biswas M, et al. Association of sex age and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis. Intervirology. 2020;64(1):36–47. doi: 10.1159/000512592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gold MS, et al. COVID-19 and comorbidities: a systematic review and meta-analysis. Postgrad Med. 2020;132(8):749–755. doi: 10.1080/00325481.2020.1786964. [DOI] [PubMed] [Google Scholar]
- 146.Ejaz H, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. 2020;13(12):1833–1839. doi: 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Elezkurtaj S, et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep. 2021;11(1):4263. doi: 10.1038/s41598-021-82862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.McClelland S, III, et al. Tumor treating field’s utilization in a glioblastoma patient with a preexisting cardiac pacemaker: the first reported case. World Neurosurg. 2018;119:58–60. doi: 10.1016/j.wneu.2018.07.162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.