Abstract
Rationale: The Global Burden of Disease program identified smoking and ambient and household air pollution as the main drivers of death and disability from chronic obstructive pulmonary disease (COPD).
Objectives: To estimate the attributable risk of chronic airflow obstruction (CAO), a quantifiable characteristic of COPD, due to several risk factors.
Methods: The Burden of Obstructive Lung Disease study is a cross-sectional study of adults, aged ≥40, in a globally distributed sample of 41 urban and rural sites. Based on data from 28,459 participants, we estimated the prevalence of CAO, defined as a postbronchodilator FEV1-to-FVC ratio less than the lower limit of normal, and the relative risks associated with different risk factors. Local relative risks were estimated using a Bayesian hierarchical model borrowing information from across sites. From these relative risks and the prevalence of risk factors, we estimated local population attributable risks.
Measurements and Main Results: The mean prevalence of CAO was 11.2% in men and 8.6% in women. The mean population attributable risk for smoking was 5.1% in men and 2.2% in women. The next most influential risk factors were poor education levels, working in a dusty job for ≥10 years, low body mass index, and a history of tuberculosis. The risk of CAO attributable to the different risk factors varied across sites.
Conclusions: Although smoking remains the most important risk factor for CAO, in some areas, poor education, low body mass index, and passive smoking are of greater importance. Dusty occupations and tuberculosis are important risk factors at some sites.
Keywords: chronic airflow obstruction, population-attributable risk, multinational study, Burden of Obstructive Lung Disease (BOLD) study
At a Glance Commentary.
Scientific Knowledge on the Subject
Many studies have assessed traditional risk factors for chronic airflow obstruction (CAO). In addition, the Global Burden of Disease program has estimated the disability-adjusted life-years lost due to chronic obstructive pulmonary disease and has quantified the risk factors that contribute to this. However, no attempt has been made to systematically assess the risk factors that contribute to the prevalence of CAO in different parts of the world using standardized methods for postbronchodilator lung function measures.
What This Study Adds to the Field
We provide local estimates of the excess prevalence due to several risk factors for each of 41 sites from around the world. This assessment is based on postbronchodilator lung function measures obtained using a standardized protocol across all sites. Tobacco smoking is still by far the most important risk factor for CAO, but there are very wide variations across sites in the attributable risk factors of CAO. The next most influential risk factor is poor education, which, along with low body mass index, is associated with deprivation. We also found that exposure to dusty jobs, tuberculosis, and passive smoking are important in some places. Tobacco control remains vital in the control of CAO, but the effects of social deprivation have been underestimated.
Chronic lung disease is one of the four chronic diseases prioritized by the United Nations (1). The Global Burden of Disease (GBD) program concluded that in 2010 it was the third most common cause of death, responsible for the ninth highest years of life lost globally (2), and the ninth most influential disease in reducing disability-adjusted life-years (3).
The importance of smoking is well recognized both as a risk factor for chronic airflow obstruction (CAO), an essential component of chronic obstructive pulmonary disease (COPD), and as a risk factor for mortality attributed to COPD (4). However, estimates of the proportion of disease caused by smoking have varied widely (5), and recognition that many people with CAO have no history of smoking has led to the search for other causes (6). Genetics, secondhand smoke, outdoor air pollution, indoor air pollution from biomass burning, diet, occupation, tuberculosis, and longstanding asthma have all been suggested as additional causes (6). The GBD program has provided comprehensive estimates of the burden of COPD, measured as disability-adjusted life-years lost, attributable to different risk factors, concluding that the most important ones, in order, were smoking, outdoor particulate pollution, household pollution, occupational exposure to particles, exposure to ozone, and secondhand tobacco smoke (7). However, for most low- and middle-income countries, these are based on indirect evidence.
We have previously identified the main modifiable risk factors for CAO in the BOLD (Burden of Obstructive Lung Disease) study (8), and here we have quantified the local prevalence of CAO that can be attributed to each of these main risk factors in each of 41 sites in 35 countries.
Methods
Study Population
The BOLD protocol has been published elsewhere (9). Representative samples of adults, aged ≥40, were identified from centers with populations of at least 150,000 people. Standardized questionnaires were translated into the local language, back-translated, and checked before being administered by trained fieldworkers. Questions were taken from standardized questionnaires, where these were available, and covered respiratory symptoms, smoking, and other risk factors, including age, sex, educational attainment, a history of tuberculosis, and a history of working in a dusty job. Height and weight were measured and spirometry was performed using an EasyOne spirometer (ndd Medizintechnik AG), before and after the administration of 200 μg salbutamol via a spacer (Clement Clarke International). All spirometry was checked centrally by one of the two pulmonary function reading centers. Tests used had to include at least three acceptable curves (no hesitation, complete blow, no artifact affecting the FEV1 or FVC), with the two best blows being within 200 ml of each other.
Outcome and Exposures
We defined CAO as a postbronchodilator FEV1/FVC ratio less than the lower limit of normal using the equations for European Americans in the third National Health and Nutrition Examination Survey (NHANES III) study (10). As potential exposures, we analyzed the modifiable risk factors for CAO identified in a preliminary analysis of only 14 of the BOLD sites (8), omitting self-reported medical conditions and reports of hospitalization with respiratory disease below the age of 10 as all these can be viewed as the consequences rather than the fundamental causes of CAO.
Statistical Analysis
By population-attributable risk (PAR), we mean the excess prevalence of CAO in the population that is attributable to a risk factor. We estimated the PAR for each of the following: body mass index (BMI) (underweight, normal weight, overweight, obese), doctor-diagnosed tuberculosis (ever/never), working in a dusty job (>10 yr, ≤10 yr), education (none to primary, secondary, more than secondary school), passive smoking (presence of somebody else smoking in the subject’s home in the last 2 wk), and pack-years of any smoking (never-smoker, 1–5 pack-years, 6–15 pack-years, 16–25 pack-years, >25 pack-years). We defined a pack-year as consumption of 20 cigarettes/d for a year. Equivalent values for other types of smoking products were taken from the Smoking Pack-Years Calculator (11).
PAR depends on the strength of the association between risk factor and outcome (relative risk), as well as the prevalence of the exposure to the risk factor and the prevalence of the outcome in the population of interest. For each of the 41 sites, we obtained a site-specific PAR (“local PAR”) by first estimating the population attributable fraction (PAF) using the model-based approach described by Miettinen (12), and then multiplying PAF by the prevalence of CAO to obtain PAR:
| (1.1) |
| (1.2) |
where is the proportion of cases exposed to the risk factor in the population under study, is the relative risk of CAO for the risk factor, and is the prevalence of CAO in the population. Where there was no exposed individual to a given risk factor in the sample, we have not calculated a value for PAR and it is effectively estimated to be zero.
For smoking and education, we estimated the PAR for each category, and we also estimated the overall PAR for the variable by combining PAR values across categories “c,” using the following formula (13):
| (1.3) |
where is the proportion of cases exposed to the ith level of the risk factor and is the RR for CAO for the ith category.
The RR of each risk factor was estimated by regressing the presence of CAO against age and all risk factors within each site using a log-binomial model, fitted separately for men and women. We investigated the heterogeneity of the RR estimates across sites using the I2 statistic (14). To increase the precision of the estimates of the site-specific RRs, and hence of site-specific PARs, we used a Bayesian hierarchical model where information on mean and variance of the RRs was borrowed across sites (15). This leads to more robust point and interval estimates, particularly for sites with smaller sample sizes, lower prevalence of CAO, or lower prevalence of exposure. The model assumes that the RRs vary across sites but that all site-specific RRs come from the same underlying distribution. In this model, we accounted for nonresponse, by adjusting for variables that affect the probability of selection in the survey (see online supplement) (16), and for a cluster and/or stratified sampling framework in some sites, by including an additional level of hierarchy in the model.
The uncertainty around the PAR estimate, which reflects not only the uncertainty in RR but also the uncertainty in Pd and Pe (see online supplement), is expressed by 95% credible intervals (95% CrIs), which represent the Bayesian equivalent to the frequentist 95% confidence intervals.
For each site, a total local PAR, representing the proportion of CAO at a single site explained by all risk factors considered, was derived by first estimating the total PAF using the formula proposed by Miettinen (12) and then multiplying the total PAF by the prevalence of CAO:
| (2.1) |
| (2.2) |
where k represents the risk factor and K the total number of risk factors for which PAR is estimated.
Results
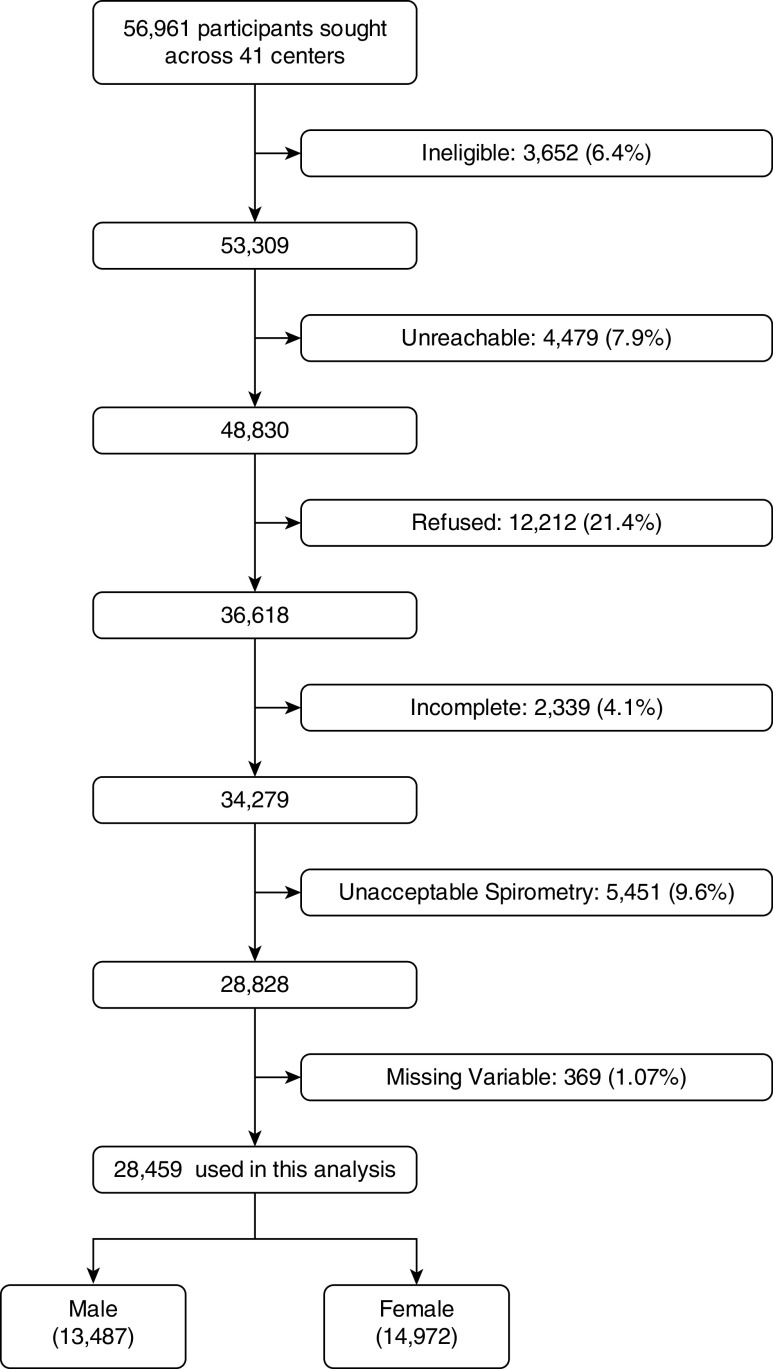
Of the 56,961 individuals invited to participate, 6.4% were ineligible and 7.9% could not be reached. A further 21.4% refused to take part and 4.1% did not complete the interviews. A further 10% had unacceptable spirometry. The 28,459 individuals included in the analyses thus represent 58.2% of the 48,830 people whom we were able to find and who were eligible for the study (Figure 1). The sampling strategy and response rates for each site are reported in Table E1 in the online supplement.
Figure 1.
Flow diagram showing recruitment to the study.
Just over half of the sample (52.6%) was female. The mean age was 55 years in men and 54 years in women, the youngest population being in Mysore (India) (48 in men; 46 in women) and the oldest being in Lisbon (Portugal) (64 in men; 63 in women) (Tables 1 and 2). On average 59% of men and 22% of women had ever smoked, and 25% of men and 7% of women had smoked more than 20 pack-years; 31% of men and 14% of women had worked in dusty jobs for >10 years; 29% of men and 36% of women had had no more than primary school; and 3% of men and 2% of women reported a history of tuberculosis.
Table 1.
Characteristics of Study Population and Prevalence of Risk Factors in 41 Sites (Men)
| Smoking (%) |
Education (%) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site | Sample Size | Age (Mean yr) | BMI (Mean) | Underweight (%) | Never-Smokers | 1–5 Pack-Years | 6–15 Pack-Years | 16–25 Pack-Years | 25+ Pack-Years | Passive Smoking (%) | None to Primary School | Secondary School | More than Secondary School | History of TB (%) | Dusty Job >10 yr (%) |
| Albania (Tirana) | 467 | 56.40 | 27.81 | 0.21 | 37.04 | 0.86 | 7.92 | 8.57 | 45.61 | 22.91 | 13.06 | 46.68 | 40.26 | 1.07 | 55.89 |
| Algeria (Annaba) | 442 | 53.34 | 25.74 | 3.85 | 23.53 | 7.01 | 16.29 | 16.52 | 36.65 | 5.88 | 32.13 | 36.88 | 31 | 3.39 | 42.08 |
| Australia (Sydney) | 251 | 58.33 | 28.02 | 0.40 | 39.44 | 15.94 | 12.35 | 11.55 | 20.72 | 10.76 | 2.39 | 31.47 | 66.14 | 1.20 | 26.69 |
| Austria (Salzburg) | 685 | 57.87 | 26.68 | 0.58 | 35.62 | 10.80 | 12.99 | 13.72 | 26.86 | 19.27 | 8.47 | 65.26 | 26.28 | 2.48 | 23.36 |
| Benin (Sèmè-Kpodji) | 237 | 53.22 | 24.61 | 4.22 | 95.78 | 1.27 | 1.69 | 0.84 | 0.42 | 0 | 68.78 | 25.32 | 5.91 | 0.84 | 31.65 |
| Cameroon (Limbe) | 171 | 52.42 | 25.20 | 1.75 | 63.16 | 9.94 | 15.20 | 5.85 | 5.85 | 2.92 | 53.22 | 34.50 | 12.28 | 0.58 | 50.29 |
| Canada (Vancouver) | 343 | 54.43 | 27.07 | 0.58 | 34.11 | 19.83 | 12.83 | 9.91 | 23.32 | 6.71 | 2.04 | 18.08 | 79.88 | 3.21 | 16.33 |
| China (Guangzhou) | 236 | 54.03 | 23.30 | 5.08 | 18.64 | 6.36 | 14.83 | 21.61 | 38.56 | 18.64 | 20.76 | 63.14 | 16.10 | 4.66 | 30.93 |
| England (London) | 323 | 57.92 | 27.55 | 0.31 | 28.17 | 12.38 | 16.72 | 11.76 | 30.96 | 15.17 | 5.88 | 40.25 | 53.87 | 2.17 | 21.05 |
| Estonia (Tartu) | 307 | 59.97 | 28.32 | 0.98 | 36.16 | 11.07 | 15.64 | 12.70 | 24.43 | 10.42 | 2.93 | 44.95 | 52.12 | 7.82 | 23.78 |
| Germany (Hannover) | 349 | 58.56 | 27.71 | 0.57 | 26.93 | 12.89 | 16.05 | 14.04 | 30.09 | 15.19 | 1.43 | 63.32 | 35.24 | 3.15 | 20.06 |
| Iceland (Reykjavik) | 403 | 55.90 | 28.30 | 0.50 | 29.28 | 19.60 | 11.17 | 16.87 | 23.08 | 16.38 | 7.20 | 14.64 | 78.16 | 3.97 | 24.32 |
| India (Kashmir) | 411 | 51.62 | 21.80 | 10.22 | 23.60 | 2.19 | 7.06 | 1.70 | 65.45 | 61.80 | 73.24 | 22.87 | 3.89 | 0.24 | 0.73 |
| India (Mumbai) | 275 | 51.44 | 23.45 | 8.36 | 84.36 | 2.91 | 6.18 | 4 | 2.55 | 0.36 | 11.27 | 51.27 | 37.45 | 0.36 | 8.36 |
| India (Mysore) | 256 | 47.96 | 24.61 | 2.73 | 77.73 | 3.13 | 11.33 | 4.30 | 3.52 | 0 | 12.89 | 42.58 | 44.53 | 0 | 3.52 |
| India (Pune) | 501 | 53.38 | 22.20 | 16.37 | 79.04 | 14.37 | 4.39 | 1.60 | 0.60 | 10.58 | 42.51 | 47.31 | 10.18 | 1.20 | 10.58 |
| Jamaica | 243 | 56.94 | 24.04 | 9.05 | 35.80 | 8.23 | 11.93 | 12.76 | 31.28 | 12.76 | 27.57 | 61.32 | 11.11 | 0.41 | 54.32 |
| Kyrgyztan (Chui) | 270 | 52.95 | 26.22 | 1.11 | 22.59 | 12.96 | 13.33 | 14.44 | 36.67 | 1.85 | 1.11 | 52.59 | 46.30 | 1.48 | 32.96 |
| Kyrgyztan (Naryn) | 315 | 52.83 | 25.19 | 2.22 | 39.37 | 12.70 | 17.14 | 10.79 | 20 | 0.32 | 4.76 | 40 | 55.24 | 0.32 | 6.67 |
| Malawi (Blantyre) | 160 | 53.73 | 22.98 | 10.63 | 69.38 | 15 | 10 | 3.13 | 2.50 | 3.13 | 47.50 | 46.88 | 5.63 | 4.38 | 18.75 |
| Malawi (Chikwawa) | 221 | 54.91 | 20.89 | 19.46 | 51.58 | 20.81 | 20.81 | 3.62 | 3.17 | 1.36 | 88.24 | 11.31 | 0.45 | 4.07 | 20.36 |
| Malaysia (Penang) | 340 | 54.98 | 25.78 | 2.94 | 50.29 | 5.88 | 13.53 | 8.53 | 21.76 | 16.47 | 32.06 | 61.47 | 6.47 | 0 | 35.88 |
| Morocco (Fes) | 354 | 56.51 | 25.85 | 1.98 | 40.68 | 10.73 | 12.99 | 9.89 | 25.71 | 7.91 | 65.25 | 23.16 | 11.58 | 1.13 | 53.67 |
| Netherlands (Maastricht) | 297 | 57.54 | 27.43 | 0 | 25.93 | 15.49 | 15.15 | 14.81 | 28.62 | 21.89 | 12.12 | 27.61 | 60.27 | 0.67 | 18.86 |
| Nigeria (Ile-Ife) | 345 | 56.17 | 23.83 | 5.22 | 76.52 | 15.36 | 5.22 | 1.45 | 1.45 | 1.74 | 34.78 | 39.13 | 26.09 | 0.87 | 25.80 |
| Norway (Bergen) | 323 | 58.94 | 26.86 | 0.62 | 29.10 | 9.91 | 20.43 | 18.89 | 21.67 | 24.46 | 5.57 | 54.18 | 40.25 | 0.62 | 35.91 |
| Pakistan (Karachi) | 268 | 54.29 | 25.09 | 8.58 | 51.49 | 10.07 | 11.94 | 7.46 | 19.03 | 9.33 | 44.40 | 38.06 | 17.54 | 0.37 | 34.70 |
| Philippines (Manila) | 378 | 52.16 | 24.37 | 8.73 | 16.14 | 15.87 | 21.69 | 16.14 | 30.16 | 39.68 | 7.67 | 71.43 | 20.90 | 10.58 | 40.21 |
| Philippines (Nampicuan-Talugtug) | 356 | 53.79 | 21.35 | 20.51 | 23.03 | 5.90 | 13.76 | 20.51 | 36.80 | 36.52 | 16.29 | 69.94 | 13.76 | 5.06 | 25.28 |
| Poland (Krakow) | 265 | 55.26 | 27.43 | 0 | 20.75 | 6.04 | 15.09 | 16.98 | 41.13 | 40.75 | 34.72 | 52.08 | 13.21 | 3.77 | 57.36 |
| Portugal (Lisbon) | 331 | 63.98 | 27.97 | 0 | 38.37 | 10.27 | 6.65 | 8.76 | 35.95 | 11.18 | 44.41 | 31.12 | 24.47 | 5.74 | 45.62 |
| Saudi Arabia (Riyadh) | 371 | 50.66 | 29.59 | 0.81 | 51.75 | 5.12 | 9.97 | 9.70 | 23.45 | 3.23 | 20.75 | 44.47 | 34.77 | 2.70 | 19.41 |
| South Africa (Uitsig and Ravensmead) | 311 | 53.56 | 24.64 | 11.25 | 15.76 | 14.47 | 30.87 | 19.61 | 19.29 | 47.59 | 40.51 | 50.80 | 8.68 | 19.61 | 38.26 |
| Sri Lanka | 457 | 54.15 | 23.17 | 13.35 | 51.42 | 18.16 | 17.29 | 6.56 | 6.56 | 5.03 | 30.85 | 66.74 | 2.41 | 1.09 | 43.54 |
| Sudan (Gezeira) | 298 | 55.44 | 23.94 | 8.72 | 52.68 | 16.44 | 15.44 | 7.38 | 8.05 | 6.71 | 64.43 | 27.52 | 8.05 | 0.34 | 27.18 |
| Sudan (Khartoum) | 306 | 55.74 | 25.17 | 5.88 | 61.44 | 8.82 | 14.05 | 6.86 | 8.82 | 4.25 | 55.56 | 29.74 | 14.71 | 0.65 | 21.90 |
| Sweden (Uppsala) | 283 | 58.45 | 27.22 | 0 | 31.45 | 18.73 | 19.08 | 12.37 | 18.37 | 6.71 | 13.78 | 37.81 | 48.41 | 0.71 | 27.56 |
| Trinidad and Tobago | 435 | 55.46 | 26.98 | 2.30 | 48.97 | 7.36 | 11.03 | 10.80 | 21.84 | 17.47 | 37.47 | 39.77 | 22.76 | 0 | 40.23 |
| Tunisia (Sousse) | 309 | 53.33 | 26.94 | 1.62 | 20.06 | 1.29 | 8.41 | 18.12 | 52.10 | 20.39 | 35.92 | 47.25 | 16.83 | 0 | 51.78 |
| Turkey (Adana) | 389 | 53.80 | 27.66 | 0.77 | 19.02 | 7.97 | 11.05 | 14.14 | 47.81 | 44.99 | 72.75 | 22.11 | 5.14 | 2.83 | 49.10 |
| United States (Lexington, Kentucky) | 205 | 57.20 | 30.29 | 0 | 20.98 | 13.17 | 6.83 | 4.88 | 54.15 | 28.78 | 2.44 | 50.73 | 46.83 | 1.46 | 51.71 |
Definition of abbreviations: BMI = body mass index; TB = tuberculosis.
Table 2.
Characteristics of Study Population and Prevalence of Risk Factors in 41 Sites (Women)
| Smoking (%) |
Education (%) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site | Sample Size | Age (Mean yr) | BMI (Mean) | Underweight (%) | Never-Smokers | 1–5 Pack-Years | 6–15 Pack-Years | 16–25 Pack-Years | 25+ Pack-Years | Passive Smoking (%) | None to Primary School | Secondary School | More than Secondary School | History of TB (%) | Dusty Job >10 yr (%) |
| Albania (Tirana) | 472 | 52.79 | 28.28 | 0.64 | 88.56 | 1.69 | 4.24 | 3.60 | 1.91 | 45.55 | 12.08 | 48.73 | 39.19 | 0.42 | 48.09 |
| Algeria (Annaba) | 448 | 51.65 | 30.84 | 0.22 | 99.33 | 0.22 | 0.22 | 0 | 0.22 | 17.19 | 50 | 38.62 | 11.38 | 1.12 | 5.36 |
| Australia (Sydney) | 265 | 58.93 | 27.92 | 0.38 | 52.08 | 13.21 | 11.70 | 8.30 | 14.72 | 11.70 | 3.77 | 39.25 | 56.98 | 0.38 | 12.08 |
| Austria (Salzburg) | 573 | 57.41 | 26.12 | 1.57 | 55.67 | 8.55 | 13.96 | 8.73 | 13.09 | 25.48 | 13.96 | 63.53 | 22.51 | 2.97 | 13.61 |
| Benin (Sèmè-Kpodji) | 308 | 50.50 | 28.07 | 3.25 | 100 | 0 | 0 | 0 | 0 | 0.32 | 84.09 | 14.61 | 1.30 | 0.32 | 13.96 |
| Cameroon (Limbe) | 116 | 51.95 | 28.75 | 2.59 | 99.14 | 0.86 | 0 | 0 | 0 | 1.72 | 63.79 | 30.17 | 6.03 | 1.72 | 62.07 |
| Canada (Vancouver) | 483 | 57.20 | 26.45 | 1.04 | 49.69 | 13.46 | 12.42 | 8.70 | 15.73 | 5.38 | 2.48 | 24.22 | 73.29 | 3.11 | 9.73 |
| China (Guangzhou) | 236 | 54.22 | 23.38 | 5.51 | 93.64 | 1.69 | 1.69 | 0.42 | 2.54 | 28.81 | 37.71 | 53.81 | 8.47 | 2.12 | 27.54 |
| England (London) | 354 | 58.39 | 26.69 | 1.13 | 42.94 | 12.15 | 14.41 | 9.89 | 20.62 | 17.51 | 5.37 | 38.98 | 55.65 | 2.82 | 6.78 |
| Estonia (Tartu) | 305 | 61.72 | 28.62 | 1.31 | 68.52 | 11.15 | 10.49 | 6.89 | 2.95 | 18.36 | 3.28 | 43.61 | 53.11 | 7.21 | 15.74 |
| Germany (Hannover) | 334 | 57.64 | 26.84 | 0.90 | 50 | 9.28 | 11.98 | 10.48 | 18.26 | 22.16 | 1.80 | 73.65 | 24.55 | 4.19 | 8.08 |
| Iceland (Reykjavik) | 354 | 57.03 | 27.53 | 0.28 | 38.70 | 16.38 | 16.95 | 11.86 | 16.10 | 17.51 | 10.45 | 43.79 | 45.76 | 5.65 | 5.93 |
| India (Kashmir) | 341 | 51.13 | 23.18 | 10.26 | 70.97 | 1.76 | 1.76 | 0.29 | 25.22 | 68.62 | 91.79 | 6.74 | 1.47 | 0.59 | 0 |
| India (Mumbai) | 165 | 50.41 | 24.43 | 7.27 | 100 | 0 | 0 | 0 | 0 | 2.42 | 37.58 | 47.27 | 15.15 | 1.82 | 1.21 |
| India (Mysore) | 345 | 45.91 | 24.77 | 5.51 | 98.55 | 0.58 | 0.29 | 0.58 | 0 | 0 | 25.22 | 51.01 | 23.77 | 0 | 1.16 |
| India (Pune) | 341 | 51.06 | 21.82 | 22.29 | 99.71 | 0 | 0 | 0 | 0.29 | 12.02 | 78.89 | 19.35 | 1.76 | 0.29 | 2.64 |
| Jamaica | 335 | 55.13 | 30.05 | 2.99 | 81.49 | 6.87 | 5.37 | 3.28 | 2.99 | 17.91 | 19.70 | 65.37 | 14.93 | 0.90 | 17.91 |
| Kyrgyzstan (Chui) | 588 | 52.96 | 29.55 | 1.02 | 92.35 | 3.40 | 1.70 | 1.87 | 0.68 | 9.69 | 3.57 | 57.48 | 38.95 | 1.19 | 16.33 |
| Kyrgyzstan (Naryn) | 505 | 53.66 | 28.11 | 1.58 | 97.43 | 2.18 | 0 | 0 | 0.40 | 4.75 | 5.74 | 37.62 | 56.63 | 0.99 | 1.19 |
| Malawi (Blantyre) | 241 | 51.27 | 26.42 | 3.73 | 97.51 | 1.24 | 0.83 | 0.41 | 0 | 2.90 | 66.80 | 29.88 | 3.32 | 6.22 | 11.62 |
| Malawi (Chikwawa) | 211 | 52.69 | 22.68 | 12.32 | 88.63 | 5.21 | 3.79 | 0.47 | 1.90 | 5.21 | 93.84 | 5.69 | 0.4 | 3.79 | 2.84 |
| Malaysia (Penang) | 323 | 54.06 | 26.34 | 2.17 | 100 | 0 | 0 | 0 | 0 | 35.29 | 38.70 | 53.56 | 7.74 | 0 | 12.38 |
| Morocco (Fes) | 414 | 53.93 | 29.62 | 1.21 | 99.03 | 0 | 0.24 | 0.24 | 0.48 | 18.84 | 84.30 | 12.56 | 3.14 | 2.17 | 13.04 |
| Netherlands (Maastricht) | 289 | 57.54 | 27.46 | 1.04 | 39.79 | 10.73 | 14.88 | 11.76 | 22.84 | 17.99 | 13.84 | 36.33 | 49.83 | 2.08 | 4.84 |
| Nigeria (Ile-Ife) | 538 | 54.84 | 26.32 | 5.02 | 96.28 | 2.97 | 0.56 | 0.19 | 0 | 1.67 | 56.69 | 27.14 | 16.17 | 0.19 | 12.08 |
| Norway (Bergen) | 334 | 60.56 | 26.25 | 1.20 | 42.22 | 8.38 | 22.46 | 13.17 | 13.77 | 18.56 | 9.28 | 57.19 | 33.53 | 0 | 18.56 |
| Pakistan (Karachi) | 339 | 49.38 | 27.55 | 3.83 | 92.04 | 2.06 | 0.88 | 1.18 | 3.83 | 15.34 | 67.55 | 20.06 | 12.39 | 0.59 | 9.14 |
| Philippines (Manila) | 515 | 52.48 | 25.30 | 5.24 | 68.93 | 16.12 | 8.54 | 3.11 | 3.30 | 55.15 | 12.23 | 63.50 | 24.27 | 5.24 | 19.03 |
| Philippines (Nampicuan-Talugtug) | 366 | 54.33 | 21.74 | 21.58 | 69.95 | 9.56 | 11.75 | 5.74 | 3.01 | 55.74 | 15.30 | 71.04 | 13.66 | 2.19 | 13.66 |
| Poland (Krakow) | 257 | 55.92 | 28.03 | 1.56 | 55.64 | 10.12 | 14.40 | 10.51 | 9.34 | 38.91 | 41.25 | 44.36 | 14.40 | 1.56 | 22.96 |
| Portugal (Lisbon) | 379 | 62.80 | 28.44 | 0.26 | 78.10 | 5.80 | 5.54 | 1.58 | 8.97 | 19.79 | 49.87 | 33.25 | 16.89 | 3.69 | 39.31 |
| Saudi Arabia (Riyadh) | 325 | 49.95 | 33.14 | 0.31 | 97.85 | 0 | 0.62 | 0.31 | 1.23 | 7.69 | 54.77 | 30.77 | 14.46 | 0.92 | 1.23 |
| South Africa (Uitsig and Ravensmead) | 529 | 54.47 | 29.79 | 5.48 | 42.16 | 11.91 | 25.14 | 9.64 | 11.15 | 50.85 | 47.26 | 46.69 | 6.05 | 12.48 | 22.87 |
| Sri Lanka | 566 | 53.41 | 25.05 | 7.07 | 99.82 | 0 | 0 | 0.18 | 0 | 11.31 | 24.56 | 72.44 | 3 | 0.53 | 12.01 |
| Sudan (Gezeira) | 277 | 52.27 | 28.86 | 0.72 | 98.56 | 1.08 | 0.36 | 0 | 0 | 17.69 | 66.79 | 27.08 | 6.14 | 0.72 | 7.58 |
| Sudan (Khartoum) | 210 | 51.51 | 28.32 | 7.62 | 97.14 | 1.43 | 0.95 | 0.48 | 0 | 11.90 | 57.62 | 30.95 | 11.43 | 1.43 | 5.71 |
| Sweden (Uppsala) | 264 | 58.35 | 26.79 | 0 | 47.35 | 13.26 | 15.53 | 10.98 | 12.88 | 5.30 | 12.12 | 37.12 | 50.76 | 1.52 | 9.47 |
| Trinidad and Tobago | 656 | 53.26 | 30.20 | 2.44 | 87.96 | 3.20 | 3.51 | 2.44 | 2.90 | 26.22 | 39.18 | 41.01 | 19.82 | 0 | 10.52 |
| Tunisia (Sousse) | 352 | 52.71 | 31.26 | 0.85 | 90.91 | 1.70 | 3.98 | 1.14 | 2.27 | 51.14 | 65.06 | 29.55 | 5.40 | 0 | 25.57 |
| Turkey (Adana) | 417 | 53.47 | 31.45 | 0.48 | 69.54 | 9.59 | 8.63 | 5.76 | 6.47 | 63.07 | 84.41 | 13.67 | 1.92 | 2.16 | 29.26 |
| United States (Lexington, Kentucky) | 302 | 56.18 | 31.11 | 0.33 | 45.70 | 7.95 | 7.28 | 8.28 | 30.79 | 32.12 | 2.98 | 48.68 | 48.34 | 1.99 | 16.23 |
Definition of abbreviations: BMI = body mass index; TB = tuberculosis.
The mean prevalence of CAO was 11.2% in men and 8.6% in women, but ranged from 3.5% in Riyadh (Saudi Arabia) to 23.2% in Uitsig and Ravensmead (South Africa) in men, and from 2% in Sousse (Tunisia) to 19.4% in Salzburg (Austria) in women (Table 3).
Table 3.
Prevalence of CAO by Site and Sex
| Men |
Women |
|||
|---|---|---|---|---|
| Site | Sample Size | CAO [n (%)] | Sample Size | CAO [n (%)] |
| Albania (Tirana) | 467 | 60 (12.85) | 472 | 20 (4.24) |
| Algeria (Annaba) | 442 | 41 (9.28) | 448 | 20 (4.46) |
| Australia (Sydney) | 251 | 19 (7.57) | 265 | 35 (13.21) |
| Austria (Salzburg) | 685 | 88 (12.85) | 573 | 111 (19.37) |
| Benin (Sèmè-Kpodji) | 237 | 18 (7.59) | 308 | 24 (7.79) |
| Cameroon (Limbe) | 171 | 9 (5.26) | 116 | 4 (3.45) |
| Canada (Vancouver) | 343 | 44 (12.83) | 483 | 58 (12.01) |
| China (Guangzhou) | 236 | 22 (9.32) | 236 | 15 (6.36) |
| England (London) | 323 | 52 (16.10) | 354 | 56 (15.82) |
| Estonia (Tartu) | 307 | 27 (8.79) | 305 | 16 (5.25) |
| Germany (Hannover) | 349 | 35 (10.03) | 334 | 26 (7.78) |
| Iceland (Reykjavik) | 403 | 36 (8.93) | 354 | 47 (13.28) |
| India (Kashmir) | 411 | 71 (17.27) | 341 | 53 (15.54) |
| India (Mumbai) | 275 | 17 (6.18) | 165 | 13 (7.88) |
| India (Mysore) | 256 | 29 (11.33) | 345 | 19 (5.51) |
| India (Pune) | 501 | 29 (5.79) | 341 | 23 (6.74) |
| Jamaica | 243 | 25 (10.29) | 335 | 25 (7.46) |
| Kyrgyzstan (Chui) | 270 | 39 (14.44) | 588 | 47 (7.99) |
| Kyrgyzstan (Naryn) | 315 | 36 (11.43) | 505 | 25 (4.95) |
| Malawi (Blantyre) | 160 | 11 (6.88) | 241 | 22 (9.13) |
| Malawi (Chikwawa) | 221 | 40 (18.10) | 211 | 20 (9.48) |
| Malaysia (Penang) | 340 | 15 (4.41) | 323 | 11 (3.41) |
| Morocco (Fes) | 354 | 42 (11.86) | 414 | 31 (7.49) |
| Netherlands (Maastricht) | 297 | 57 (19.19) | 289 | 50 (17.30) |
| Nigeria (Ile-Ife) | 345 | 26 (7.54) | 538 | 36 (6.69) |
| Norway (Bergen) | 323 | 48 (14.86) | 334 | 34 (10.18) |
| Pakistan (Karachi) | 268 | 39 (14.55) | 339 | 22 (6.49) |
| Philippines (Manila) | 378 | 49 (12.96) | 515 | 27 (5.24) |
| Philippines (Nampicuan-Talugtug) | 356 | 58 (16.29) | 366 | 45 (12.30) |
| Poland (Krakow) | 265 | 40 (15.09) | 257 | 31 (12.06) |
| Portugal (Lisbon) | 331 | 46 (13.90) | 379 | 36 (9.50) |
| Saudi Arabia (Riyadh) | 371 | 13 (3.50) | 325 | 9 (2.77) |
| South Africa (Uitsig and Ravensmead) | 311 | 73 (23.47) | 529 | 86 (16.26) |
| Sri Lanka | 457 | 54 (11.82) | 566 | 22 (3.89) |
| Sudan (Gezeira) | 298 | 17 (5.70) | 277 | 15 (5.42) |
| Sudan (Khartoum) | 306 | 32 (10.46) | 210 | 21 (10.00) |
| Sweden (Uppsala) | 283 | 29 (10.25) | 264 | 22 (8.33) |
| Trinidad and Tobago | 435 | 28 (6.44) | 656 | 44 (6.71) |
| Tunisia (Sousse) | 309 | 26 (8.41) | 352 | 7 (1.99) |
| Turkey (Adana) | 389 | 77 (19.79) | 417 | 38 (9.11) |
| United States (Lexington, Kentucky) | 205 | 28 (13.66) | 302 | 49 (16.23) |
Definition of abbreviation: CAO = chronic airflow obstruction.
After mutual adjustment, the RRs for the several risk factors were mostly consistent across sites, as shown by the I2 values in Figure 2. Smoking more than 25 pack-years, compared with never smoking, was associated with an RR of 3.1 (95% CrI, 2.6–3.8) in women and 3.4 (95% CrI, 2.8–4.1) in men, with significant variation across the sites only for men. Other risk factors with statistically significant results were passive smoking, having secondary school or less, being underweight compared with normal weight, having a history of tuberculosis, and having worked >10 years in a dusty job.
Figure 2.
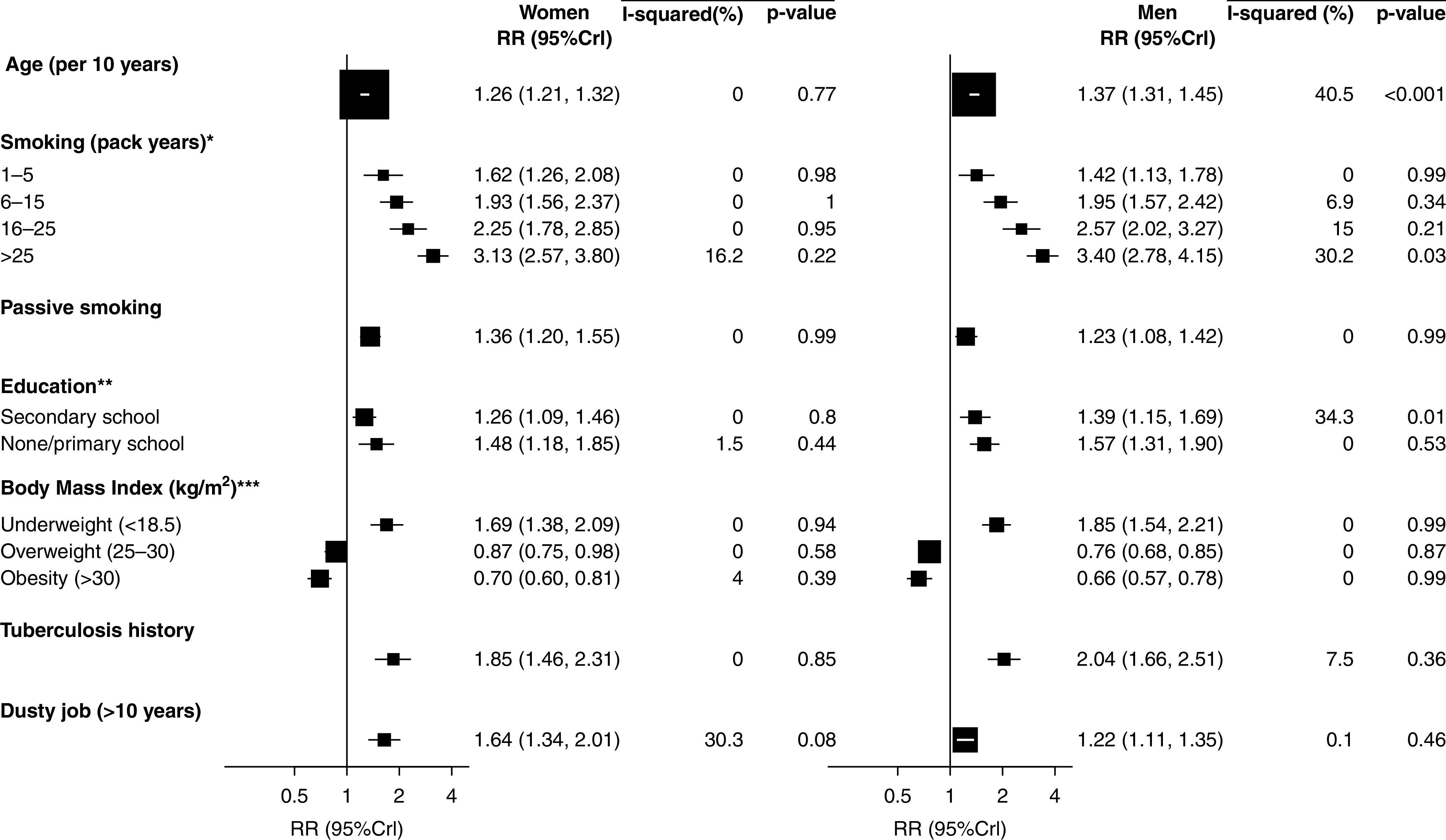
Sex-specific relative risk for chronic airflow obstruction among 28,459 adults aged 40–89 years, and their variation across sites. The P value relates to the significance of the I-squared value. Square sizes reflect the amount of statistical information (i.e., inversely proportional to the variance of the log RR), together with the 95% credible intervals (horizontal lines) representing the Bayesian equivalent to the frequentist 95% confidence intervals. 95% CrI = 95% credible interval; RR = relative risk mutually adjusted for all risk factors shown here. *Reference: never-smoker; **reference: more than secondary school; ***reference: normal weight (18.5–24.9 kg/m2).
The mean and range of the local PARs are given in Table 4. The local values of PAR for each risk factor associated with CAO are shown in Figure 3A (men) and Figure 3B (women), with detailed results in Table E2A (men) and Table E2B (women). On average, 5.2% of men and 2.2% of women aged ≥40 have CAO attributable to smoking, but in Uitsig and Ravensmead (South Africa), this figure is 11.7% for men, and in Lexington, Kentucky (United States), it is 9.5% for women. On average, 2.3% of men and 1.4% of women in the same age group have CAO attributable to poor education (defined as having secondary school or less), rising to 6.2% for men in Uitsig and Ravensmead (South Africa) and 4.3% for women in Kashmir (India). Lesser amounts of disease are attributable to long-term occupation in dusty jobs (men: 0.65%; women: 0.29%), being underweight (men: 0.43%; women: 0.30%), and having a history of tuberculosis (men: 0.36%; women: 0.26%), although in Uitsig and Ravensmead (South Africa) 3.8% of men and 2.1% of women had CAO attributable to tuberculosis.
Table 4.
Mean and Range of PAR for CAO across Study Sites by Risk Factor and Sex
| PAR by Risk Factor* | Men [Mean (Min–Max)] | Women [Mean (Min–Max)] |
|---|---|---|
| Smoking | 5.07 (0.53–11.7) | 2.11 (0–9.46) |
| Poor education† | 2.33 (0.65–6.25) | 1.37 (0.34–4.32) |
| Passive smoking | 0.31 (0–1.64) | 0.48 (0–2.18) |
| History of tuberculosis | 0.36 (0–3.77) | 0.26 (0–2.05) |
| Working in a dusty job >10 yr | 0.65 (0.02–1.6) | 0.29 (0–0.9) |
| Underweight | 0.43 (0–3) | 0.30 (0–1.52) |
| Total PAR, unadjusted‡ | 9.15 (2.6–27.79) | 4.81 (0.92–15.77) |
| Total PAR, adjusted§ | 7.24 (2.21–18.17) | 4.14 (0.94–11.21) |
| Total prevalence, % | 11.2 | 8.6 |
| Prevalence explained, % | 64.6 | 48.1 |
Definition of abbreviations: CAO = chronic airflow obstruction; PAR = population attributable risk.
PAR represents the percentage of the total population (aged ≥40 yr) with CAO attributable to the specified risk factor.
Poor education, defined as having secondary school or less.
The total unadjusted PAR is the sum of all estimates across all causes. It is slightly different from the sum of the figures reported above because it is computed from the individual sites and there is some rounding effect.
The total adjusted PAR is obtained using Equations 2.1 and 2.2 in the methods section and is slightly less than the unadjusted PAR.
Figure 3.
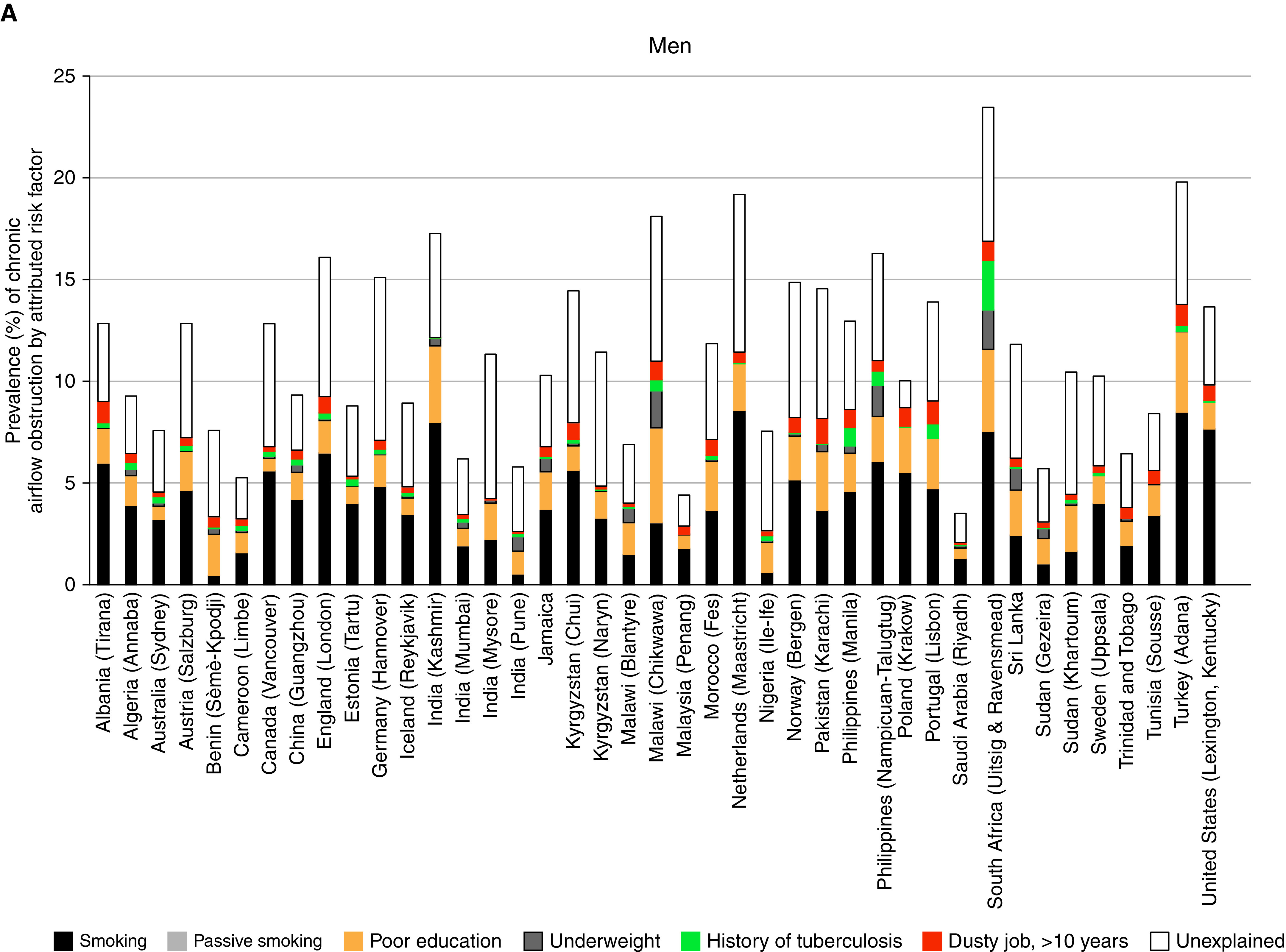
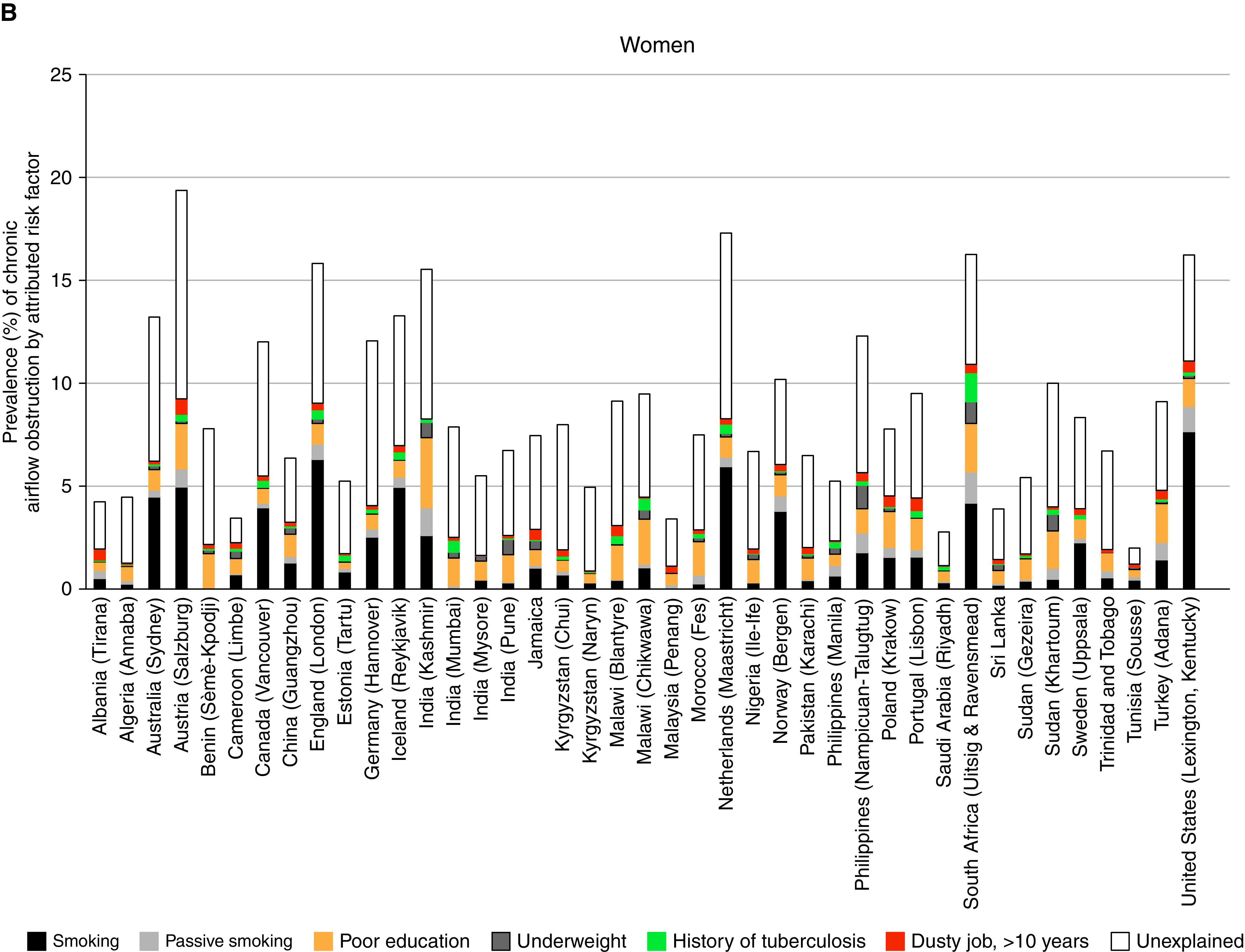
Population-attributable risk (i.e., prevalence of chronic airflow obstruction attributable to different risk factors) by site for (A) men and (B) women.
All variables together explained on average 64.6% of CAO in men and 48.1% in women; more than 75% of CAO was explained for men in Tirana (Albania), Guangzhou (China), Adana (Turkey), Kashmir (India), and Uitsig and Ravensmead (South Africa), whereas for women, more than 75% of CAO was explained only in Limbe (Cameroon) (Table 4 and Figures 3A and 3B).
Discussion
In this large study, the mean prevalence of CAO in adults aged ≥40 years was 11.2% in men and 8.6% in women. The mean prevalence of CAO attributable to smoking was 5.2% in men and 2.2% in women. The next most influential risk factor was poor education, followed by low BMI, passive smoking, working in a dusty job for >10 years, and a history of tuberculosis, but the contributions of different risk factors varied markedly from place to place. This is the first attempt to provide estimates of local attributable risks for CAO from direct observation of postbronchodilator lung function on a multinational scale within a standardized framework.
Because the RRs associated with each of the risk factors are similar in all sites, variation in PAR across sites is mostly determined by the prevalence of the risk factor. Tobacco consumption was the most influential risk factor, although there are many sites where it was not, particularly among women. The high prevalence of CAO attributable to tobacco in Kashmir is due to the high prevalence of hookah smoking in older people of both sexes in this area. As in a previous analysis (8), we confirm a smaller, but still significant, RR associated with passive smoking, and >1% of women are estimated to have CAO attributable to secondhand smoke in Adana (Turkey), Salzburg (Austria), Kashmir (India) Lexington, Kentucky (United States), and Uitsig and Ravensmead (South Africa).
The risk factor with the highest PAR after tobacco was poor education. This is one of several markers of social position associated with COPD. In an earlier analysis involving a subset of BOLD sites, a lower prevalence of CAO was associated with a higher asset score based on household assets. This effect was largely independent of education and other variables, suggesting that education accounts for only part of the effects of deprivation (17, 18). Because the asset score was measured only in some sites, we could not include it in this analysis.
CAO was associated with being underweight, as previously shown in a subset of the BOLD sites (19). We have presented the risk here in comparison with the normal weight group (18.5 < BMI < 25), although in fact the risk continues to decline in the overweight and obese groups. The association is consistent, is independent of other risk factors, such as smoking, and has been shown in nonsmokers (20). Although a low BMI could be the result of the illness causing CAO (reverse causation), prospective analysis of FEV1 decline in clinical trials has shown a slower decline in those with a higher BMI (21) and obstruction has been shown to develop in people with a low body mass for reasons unconnected to airway disease, such as anorexia nervosa (22). We suggest that this association is at least partly causal, possibly linked to an inadequate diet, potentially including a poor diet in early life or during gestation and other factors affecting BMI from childhood. We estimate that >1% of men have CAO attributable to being underweight in Sri Lanka, Nampicuan-Talugtug (Philippines), Chikwawa (Malawi), and Uitsig and Ravensmead (South Africa).
We confirmed that there is a consistent association between working in a dusty job for >10 years and CAO. However, we have found the PAR to be much lower than would be implied by some earlier estimates (23), the highest prevalence of CAO attributable to >10 years in a dusty job being 1.6% (95% CrI, 0.4–3.6) in men from Karachi (Pakistan) and 0.9% (95% CrI, 0.25–1.76) in women from Salzburg (Austria). Our questionnaire uses a very simple question and the definition of a dusty job could be expected to vary considerably both from person to person and from place to place, and any random error in the answers to this question would reduce the estimated RR. However, this question is the same as that used in other studies, including some reporting the much higher estimates that are often quoted (24, 25). In addition, there is very little heterogeneity between places in the association (RR) between a positive answer to this question and the probability of CAO, but there are wide variations in the PAR ranging up to 0.9% of women in Salzburg (Austria) with CAO attributable to working in a dusty job and to 1.6% among men in Karachi (Pakistan). Where previous studies have been undertaken preferentially in populations where the exposure is more prevalent, as might be expected in studies focused on occupational risks, this will have given an inflated estimate of the average contribution of occupation. Our figures might also be lower because we have not included exposure to gases and fumes and because we asked about dust exposure lasting at least 10 years, so excluding short-term effects. Nevertheless, we are not the first to suggest that the effects of occupation on airflow obstruction reported in the literature may have been exaggerated (26).
An association between tuberculosis and CAO has been known for many years in addition to any association with reduced lung volumes (27), and in our study the RR was very consistent across sites. Our definition of tuberculosis is based on a self-reported history. It seems unlikely that people would not know if they had been treated for tuberculosis, although there might be reluctance in some communities to admit to the diagnosis. In many sites there was no mention of tuberculosis by any of the participants, but in sites with a high burden of tuberculosis, CAO attributable to tuberculosis was a substantial problem. In Uitsig and Ravensmead (South Africa), 4% of men and 2.05% of women aged ≥40 have CAO attributable to tuberculosis.
The GBD program is the most comprehensive attempt to estimate attributable risks for COPD as they relate to mortality and disability-adjusted life-years lost (7). Both the GBD analysis and the current analysis agree that the most important risk factor is tobacco smoking, but the GBD analysis places particulate air pollution and indoor pollution as the next most important factors. We were not able to find any association between CAO and burning solid fuels in previous BOLD analyses (28). Three large Chinese cohorts that have recorded both lung function and cooking fuel use have also failed to show any such association (29–31). The main evidence for the contrary view comes from small studies that are more prone to the play of chance and that demonstrate a strong publication bias (32). The evidence from BOLD does not support the view that indoor air pollution causes a substantial amount of CAO. We do not have individual data on personal exposure to outdoor air pollution in this study and did not investigate this further in this analysis.
To present findings that are intuitively accessible, we have reported results with reference to the prevalence of CAO. We have defined this by the lower limit of normal using NHANES III equations for European Americans (10). The use of a single standard for all population groups is reasonable for the FEV1/FVC ratio, although this is not true for the FEV1 and the FVC on their own. Kiefer and colleagues showed that whereas >10% of the variance in the FEV1 or FVC was explained by ethnicity in the NHANES III study (33), this was <1% for the FEV1/FVC ratio. We have selected the fifth centile as the definition of “normal.” This is an arbitrary cutoff to define CAO, and although it does determine the nominal prevalence of “CAO,” it does not affect the estimate of PAR (34).
The sites in BOLD were selected to represent all the regions defined by the GBD except for Latin America and the high-income countries of Asia Pacific. We also failed to find a site in Oceania. Within this plan, the sites were self-selecting as they had to have local teams able and willing to take on the project. The stipulation that the sampled population had to have a size of at least 150,000 individuals prevented very small and unrepresentative populations from being selected, but the sites themselves are not strictly representative of the regions. The very consistent RR estimates across sites suggest that these could be used to estimate local PAR for other areas, if local estimates of the prevalence of risk factors and CAO are known.
Exposure to all the risk factors were assessed by self-report, as in most other similar studies. Differences in reporting across sites do not appear to have affected the RRs, which appear to be very consistent across sites. Differences in reporting will, however, have had more influence on the estimated prevalence of the risk factors, which could have affected the estimates of attributable risk.
Attributable risks can sum to more than 1 (35). All estimates of attributable risk make a strong assumption that the estimated associations are entirely causal. Some parts of these associations, however, are either confounded or the product of reverse causation. Mutual adjustment of the RRs used in the current analysis reduces the problem of confounding, but does not eliminate it, and does not address the issue of reverse causation. We estimated risk from cross-sectional rather than longitudinal data. In a chronic irreversible condition, this is likely to lead to less bias than with some other conditions, but differences in mortality in different risk groups may still bias the RR estimates. Other risks of bias include the “healthy worker” (36) and even a “healthy smoker” (37) effect that can lead people with poorer health to avoid certain risky exposures possibly including, in this case, dusty jobs and smoking. We are unable to address this limitation further in a cross-sectional study. With all these limitations, the risk factors considered in this analysis account for, on average, 64.6% of CAO in men and 48.1% in women. The measurement of some of the risk factors was very crude; with better measurements, we would expect to explain more of the condition, and addition of other unmeasured risks such as a more specific estimate of wealth might also have accounted for more.
Conclusions
There is substantial variation in the prevalence of CAO, and the single most important risk factor globally remains tobacco smoking, followed by measures that we interpret as indicators of deprivation, such as poor education and low BMI. Passive smoking is also an important risk factor. Of the more specific risk factors, >10 years in a dusty job is associated with CAO, but the risk attributable to this exposure in the BOLD sites is less than some previous reports have suggested. Dusty jobs need further investigation to identify the main contributing occupations and exposures and how these can be remediated. Tuberculosis is also an important risk factor in areas where this disease is still common. More needs to be done to understand the link between poor education and the prevalence of CAO. Local estimates of PARs are important for prioritizing public health programs, and these results should contribute to this process.
Footnotes
Supported by Wellcome Trust grant 085790/Z/08/Z for the BOLD (Burden of Obstructive Lung Disease) study. The initial BOLD program was funded in part by unrestricted educational grants to the Operations Center in Portland, Oregon, from Altana, Aventis, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Merck, Novartis, Pfizer, Schering-Plough, Sepracor, and the University of Kentucky (Lexington, Kentucky). A full list of local funders can be found at https://www.boldstudy.org.
Author Contributions: P.B. and A.S.B. were engaged in the initial design of the study; J.P., C.M., M.B. and F.G.E. analyzed the data; P.B., J.P., C.M. and A.F.S.A. drafted the initial manuscript; all authors contributed to its development and approved the final version.
Originally Published in Press as DOI: 10.1164/rccm.202005-1990OC on November 10, 2020
A complete list of BOLD Collaborative Research Group members may be found before the beginning of the References.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
Contributor Information
Collaborators: Hasan Hafizi, Anila Aliko, Donika Bardhi, Holta Tafa, Natasha Thanasi, Arian Mezini, Alma Teferici, Dafina Todri, Jolanda Nikolla, Rezarta Kazasi, Hamid Hacene Cherkaski, Amira Bengrait, Tabarek Haddad, Ibtissem Zgaoula, Maamar Ghit, Abdelhamid Roubhia, Soumaya Boudra, Feryal Atoui, Randa Yakoubi, Rachid Benali, Abdelghani Bencheikh, Nadia Ait-Khaled, Christine Jenkins, Guy Marks, Tessa Bird, Paola Espinel, Kate Hardaker, Brett Toelle, Michael Studnicka, Torkil Dawes, Bernd Lamprecht, Lea Schirhofer, Akramul Islam, Syed Masud Ahmed, Shayla Islam, Qazi Shafayetul Islam, Mesbah-Ul Haque, Tridib Roy Chowdhury, Sukantha Kumar Chatterjee, Dulal Mia, Shyamal Chandra Das, Mizanur Rahman, Nazrul Islam, Shahaz Uddin, Nurul Islam, Luiza Khatun, Monira Parvin, Abdul Awal Khan, Maidul Islam, Herve Lawin, Arsene Kpangon, Karl Kpossou, Gildas Agodokpessi, Paul Ayelo, Benjamin Fayomi, Bertrand Mbatchou, Atongno Humphrey Ashu, Wan C. Tan, Wen Wang, NanShan Zhong, Shengming Liu, Jiachun Lu, Pixin Ran, Dali Wang, Jin-ping Zheng, Yumin Zhou, Rain Jõgi, Hendrik Laja, Katrin Ulst, Vappu Zobel, Toomas-Julius Lill, Ayola Akim Adegnika, Tobias Welte, Isabelle Bodemann, Henning Geldmacher, Alexandra Schweda-Linow, Thorarinn Gislason, Bryndis Benedikdtsdottir, Kristin Jörundsdottir, Lovisa Gudmundsdottir, Sigrun Gudmundsdottir, Gunnar Gudmundsson, Mahesh Rao, Parvaiz A. Koul, Sajjad Malik, Nissar A. Hakim, Umar Hafiz Khan, Rohini Chowgule, Vasant Shetye, Jonelle Raphael, Rosel Almeda, Mahesh Tawde, Rafiq Tadvi, Sunil Katkar, Milind Kadam, Rupesh Dhanawade, Umesh Ghurup, Sanjay Juvekar, Siddhi Hirve, Somnath Sambhudas, Bharat Chaidhary, Meera Tambe, Savita Pingale, Arati Umap, Archana Umap, Nitin Shelar, Sampada Devchakke, Sharda Chaudhary, Suvarna Bondre, Savita Walke, Ashleshsa Gawhane, Anil Sapkal, Rupali Argade, Vijay Gaikwad, Sundeep Salvi, Bill Brashier, Jyoti Londhe, Sapna Madas, Althea Aquart-Stewart, Akosua Francia Aikman, Talant M. Sooronbaev, Bermet M. Estebesova, Meerim Akmatalieva, Saadat Usenbaeva, Jypara Kydyrova, Eliza Bostonova, Ulan Sheraliev, Nuridin Marajapov, Nurgul Toktogulova, Berik Emilov, Toktogul Azilova, Gulnara Beishekeeva, Nasyikat Dononbaeva, Aijamal Tabyshova, Kevin Mortimer, Wezzie Nyapigoti, Ernest Mwangoka, Mayamiko Kambwili, Martha Chipeta, Gloria Banda, Suzgo Mkandawire, Justice Banda, Li-Cher Loh, Abdul Rashid, Siti Sholehah, Mohamed C. Benjelloun, Chakib Nejjari, Mohamed Elbiaze, Karima El Rhazi, E. F. M. Wouters, G. J. Wesseling, Daniel Obaseki, Gregory Erhabor, Olayemi Awopeju, Olufemi Adewole, Amund Gulsvik, Tina Endresen, Lene Svendsen, Asaad A. Nafees, Luisito F. Idolor, Teresita S. de Guia, Norberto A. Francisco, Camilo C. Roa, Fernando G. Ayuyao, Cecil Z. Tady, Daniel T. Tan, Sylvia Banal-Yang, Vincent M. Balanag, Jr., Maria Teresita N. Reyes, Renato. B. Dantes, Renato B. Dantes, Lourdes Amarillo, Lakan U. Berratio, Lenora C. Fernandez, Norberto A. Francisco, Gerard S. Garcia, Teresita S. de Guia, Luisito F. Idolor, Sullian S. Naval, Thessa Reyes, Camilo C. Roa, Jr., Ma. Flordeliza Sanchez, Leander P. Simpao, Ewa Nizankowska-Mogilnicka, Jakub Frey, Rafal Harat, Filip Mejza, Pawel Nastalek, Andrzej Pajak, Wojciech Skucha, Andrzej Szczeklik, Magda Twardowska, Cristina Bárbara, Fátima Rodrigues, Hermínia Dias, João Cardoso, João Almeida, Maria João Matos, Paula Simão, Moutinho Santos, Reis Ferreira, M. Al Ghobain, H. Alorainy, E. El-Hamad, M. Al Hajjaj, A. Hashi, R. Dela, R. Fanuncio, E. Doloriel, I. Marciano, L. Safia, Eric Bateman, Anamika Jithoo, Desiree Adams, Edward Barnes, Jasper Freeman, Anton Hayes, Sipho Hlengwa, Christine Johannisen, Mariana Koopman, Innocentia Louw, Ina Ludick, Alta Olckers, Johanna Ryck, Janita Storbeck, Kirthi Gunasekera, Rajitha Wickremasinghe, Asma Elsony, Hana A. Elsadig, Nada Bakery Osman, Bandar Salah Noory, Monjda Awad Mohamed, Hasab Alrasoul Akasha Ahmed Osman, Namarig Moham ed Elhassan, Abdel Mu‘is El Zain, Marwa Mohamed Mohamaden, Suhaiba Khalifa, Mahmoud Elhadi, Mohand Hassan, Dalia Abdelmonam, Christer Janson, Inga Sif Olafsdottir, Katarina Nisser, Ulrike Spetz-Nyström, Gunilla Hägg, Gun-Marie Lund, Terence Seemungal, Fallon Lutchmansingh, Liane Conyette, Imed Harrabi, Myriam Denguezli, Zouhair Tabka, Hager Daldoul, Zaki Boukheroufa, Firas Chouikha, Wahbi Belhaj Khalifa, Ali Kocabaş, Attila Hancioglu, Ismail Hanta, Sedat Kuleci, Ahmet Sinan Turkyilmaz, Sema Umut, Turgay Unalan, Peter G. J. Burney, Anamika Jithoo, Louisa Gnatiuc, Hadia Azar, Jaymini Patel, Caron Amor, James Potts, Michael Tumilty, Fiona McLean, Risha Dudhaiya, A. Sonia Buist, Mary Ann McBurnie, William M. Vollmer, Suzanne Gillespie, Sean Sullivan, Todd A. Lee, Kevin B. Weiss, Robert L. Jensen, Robert Crapo, Paul Enright, David M. Mannino, John Cain, Rebecca Copeland, Dana Hazen, and Jennifer Methvin
BOLD (Burden of Obstructive Lung Disease) Collaborative Research Group members: Albania: Hasan Hafizi (principal investigator [PI]), Anila Aliko, Donika Bardhi, Holta Tafa, Natasha Thanasi, Arian Mezini, Alma Teferici, Dafina Todri, Jolanda Nikolla, and Rezarta Kazasi (Tirana University Hospital Shefqet Ndroqi, Albania); Algeria: Hamid Hacene Cherkaski (PI), Amira Bengrait, Tabarek Haddad, Ibtissem Zgaoula, Maamar Ghit, Abdelhamid Roubhia, Soumaya Boudra, Feryal Atoui, Randa Yakoubi, Rachid Benali, Abdelghani Bencheikh, and Nadia Ait-Khaled (Faculté de Médecine Annaba, Service de Epidémiologie et Médecine Préventive, El Hadjar, Algeria); Australia: Christine Jenkins (PI), Guy Marks (PI), Tessa Bird, Paola Espinel, Kate Hardaker, and Brett Toelle (Woolcock Institute of Medical Research, Sydney, Australia); Austria: Michael Studnicka (PI), Torkil Dawes, Bernd Lamprecht, and Lea Schirhofer (Department of Pulmonary Medicine, Paracelsus Medical University, Salzburg, Austria); Bangladesh: Akramul Islam (PI), Syed Masud Ahmed (Co-PI), Shayla Islam, Qazi Shafayetul Islam, Mesbah-Ul-Haque, Tridib Roy Chowdhury, Sukantha Kumar Chatterjee, Dulal Mia, Shyamal Chandra Das, Mizanur Rahman, Nazrul Islam, Shahaz Uddin, Nurul Islam, Luiza Khatun, Monira Parvin, Abdul Awal Khan, and Maidul Islam (James P. Grant School of Public Health, BRAC [Building Resources Across Communities] University, Institute of Global Health, Dhaka, Bangladesh); Benin: Herve Lawin (PI), Arsene Kpangon, Karl Kpossou, Gildas Agodokpessi, Paul Ayelo, and Benjamin Fayomi (Unit of Teaching and Research in Occupational and Environmental Health, University of Abomey Calavi, Cotonou, Benin); Cameroon: Bertrand Mbatchou (PI) and Atongno Humphrey Ashu (Douala General Hospital, Douala, Cameroon); Canada: Wan C. Tan (PI) and Wen Wang (iCapture Center for Cardiovascular and Pulmonary Research, University of British Columbia, Vancouver, BC, Canada); China: NanShan Zhong (PI), Shengming Liu, Jiachun Lu, Pixin Ran, Dali Wang, Jin-ping Zheng, and Yumin Zhou (Guangzhou Institute of Respiratory Health, First Affiliated Hospital of Guangzhou Medical College, Guangzhou, China); Estonia: Rain Jõgi (PI), Hendrik Laja, Katrin Ulst, Vappu Zobel, and Toomas-Julius Lill (Lung Clinic, Tartu University Hospital, Tartu, Estonia); Gabon: Ayola Akim Adegnika (PI) (Centre de Recherches Medicale de Lambarene, Lambarene, Gabon); Germany: Tobias Welte (PI), Isabelle Bodemann, Henning Geldmacher, and Alexandra Schweda-Linow (Department of Pneumology, Hannover Medical School and German Center of Lung Research, Hannover, Germany); Iceland: Thorarinn Gislason (PI), Bryndis Benedikdtsdottir, Kristin Jörundsdottir, Lovisa Gudmundsdottir, Sigrun Gudmundsdottir, and Gunnar Gudmundsson (Department of Allergy, Respiratory Medicine, and Sleep, Landspitali University Hospital, Reykjavik, Iceland); India: Mahesh Rao (PI) (JSS Medical College, Mysuru, India); Parvaiz A. Koul (PI), Sajjad Malik, Nissar A. Hakim, and Umar Hafiz Khan (Sher-i-Kashmir Institute of Medical Sciences, Srinagar, J&K, India); Rohini Chowgule (PI), Vasant Shetye, Jonelle Raphael, Rosel Almeda, Mahesh Tawde, Rafiq Tadvi, Sunil Katkar, Milind Kadam, Rupesh Dhanawade, and Umesh Ghurup (Indian Institute of Environmental Medicine, Mumbai, India); Sanjay Juvekar (PI), Siddhi Hirve, Somnath Sambhudas, Bharat Chaidhary, Meera Tambe, Savita Pingale, Arati Umap, Archana Umap, Nitin Shelar, Sampada Devchakke, Sharda Chaudhary, Suvarna Bondre, Savita Walke, Ashleshsa Gawhane, Anil Sapkal, Rupali Argade, and Vijay Gaikwad (Vadu Health and Demographic Surveillance System, King Edward Memorial Hospital Research Centre Pune, Pune India); Sundeep Salvi (PI), Bill Brashier, Jyoti Londhe, and Sapna Madas (Chest Research Foundation, Pune India); Jamaica: Althea Aquart-Stewart (PI) and Akosua Francia Aikman (University of the West Indies, Kingston, Jamaica); Kyrgyzstan: Talant M. Sooronbaev (PI), Bermet M. Estebesova, Meerim Akmatalieva, Saadat Usenbaeva, Jypara Kydyrova, Eliza Bostonova, Ulan Sheraliev, Nuridin Marajapov, Nurgul Toktogulova, Berik Emilov, Toktogul Azilova, Gulnara Beishekeeva, Nasyikat Dononbaeva, and AijamalTabyshova (Pulmonology and Allergology Department, National Centre of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan); Malawi: Kevin Mortimer (PI), Wezzie Nyapigoti, Ernest Mwangoka, Mayamiko Kambwili, Martha Chipeta, Gloria Banda, Suzgo Mkandawire, and Justice Banda (the Malawi Liverpool Wellcome Trust, Blantyre, Malawi); Malaysia: Li-Cher Loh (PI), Abdul Rashid, and Siti Sholehah (Royal College of Surgeons in Ireland and University College Dublin Malaysia Campus); Morocco: Mohamed C. Benjelloun (PI), Chakib Nejjari, Mohamed Elbiaze, and Karima El Rhazi (Laboratoire d’épidémiologie, Recherche Clinique et Santé Communautaire, Fès, Morroco); Netherlands: E. F. M. Wouters and G. J. Wesseling (Maastricht University Medical Center, Maastricht, the Netherlands); Nigeria: Daniel Obaseki (PI), Gregory Erhabor, Olayemi Awopeju, and Olufemi Adewole (Obafemi Awolowo University, Ile-Ife, Nigeria); Norway: Amund Gulsvik (PI), Tina Endresen, and Lene Svendsen (Department of Thoracic Medicine, Institute of Medicine, University of Bergen, Bergen, Norway); Pakistan: Asaad A. Nafees (PI), Muhammad Irfan, Zafar Fatmi, Aysha Zahidie, Natasha Shaukat, and Meesha Iqbal (Aga Khan University, Karachi, Pakistan); Philippines: Luisito F. Idolor (PI), Teresita S. de Guia, Norberto A. Francisco, Camilo C. Roa, Fernando G. Ayuyao, Cecil Z. Tady, Daniel T. Tan, Sylvia Banal-Yang, Vincent M. Balanag, Jr., Maria Teresita N. Reyes, and Renato. B. Dantes (Lung Centre of the Philippines, Philippine General Hospital, Nampicuan and Talugtug, the Philippines); Renato B. Dantes (PI), Lourdes Amarillo, Lakan U. Berratio, Lenora C. Fernandez, Norberto A. Francisco, Gerard S. Garcia, Teresita S. de Guia, Luisito F. Idolor, Sullian S. Naval, Thessa Reyes, Camilo C. Roa, Jr., Ma. Flordeliza Sanchez, and Leander P. Simpao (Philippine College of Chest Physicians, Manila, the Philippines); Poland: Ewa Nizankowska-Mogilnicka (PI), Jakub Frey, Rafal Harat, Filip Mejza, Pawel Nastalek, Andrzej Pajak, Wojciech Skucha, Andrzej Szczeklik, and Magda Twardowska, (Division of Pulmonary Diseases, Department of Medicine, Jagiellonian University School of Medicine, Krakow, Poland); Portugal: Cristina Bárbara (PI), Fátima Rodrigues, Hermínia Dias, João Cardoso, João Almeida, Maria João Matos, Paula Simão, Moutinho Santos, and Reis Ferreira (the Portuguese Society of Pneumology, Lisbon, Portugal); Saudi Arabia: M. Al Ghobain (PI), H. Alorainy (PI), E. El-Hamad, M. Al Hajjaj, A. Hashi, R. Dela, R. Fanuncio, E. Doloriel, I. Marciano, and L. Safia (Saudi Thoracic Society, Riyadh, Saudi Arabia); South Africa: Eric Bateman (PI), Anamika Jithoo (PI), Desiree Adams, Edward Barnes, Jasper Freeman, Anton Hayes, Sipho Hlengwa, Christine Johannisen, Mariana Koopman, Innocentia Louw, Ina Ludick, Alta Olckers, Johanna Ryck, and Janita Storbeck, (University of Cape Town Lung Institute, Cape Town, South Africa); Sri Lanka: Kirthi Gunasekera (PI) and Rajitha Wickremasinghe (Medical Research Institute, Central Chest Clinic, Colombo, Sri Lanka); Sudan: Asma Elsony (PI), Hana A. Elsadig, Nada Bakery Osman, Bandar Salah Noory, Monjda Awad Mohamed, Hasab Alrasoul Akasha Ahmed Osman, Namarig Moham ed Elhassan, Abdel Mu‘is El Zain, Marwa Mohamed Mohamaden, Suhaiba Khalifa, Mahmoud Elhadi, Mohand Hassan, and Dalia Abdelmonam (the Epidemiological Laboratory, Khartoum, Sudan); Sweden: Christer Janson (PI), Inga Sif Olafsdottir, Katarina Nisser, Ulrike Spetz-Nyström, Gunilla Hägg, and Gun-Marie Lund (Department of Medical Sciences: Respiratory Medicine and Allergology, Uppsala University, Uppsala, Sweden); Trinidad and Tobago: Terence Seemungal (PI), Fallon Lutchmansingh, and Liane Conyette (University of the West Indies, St. Augustine, Trinidad and Tobago); Tunisia: Imed Harrabi (PI), Myriam Denguezli, Zouhair Tabka, Hager Daldoul, Zaki Boukheroufa, Firas Chouikha, and Wahbi Belhaj Khalifa (University Hospital Farhat Hached, Faculté de Médecine, Sousse, Tunisia); Turkey: Ali Kocabaş (PI), Attila Hancioglu, Ismail Hanta, Sedat Kuleci, Ahmet Sinan Turkyilmaz, Sema Umut, and Turgay Unalan (Department of Chest Diseases, Cukurova University School of Medicine, Adana, Turkey); UK: Peter G. J. Burney (PI), Anamika Jithoo, Louisa Gnatiuc, Hadia Azar, Jaymini Patel, Caron Amor, James Potts, Michael Tumilty, Fiona McLean, and Risha Dudhaiya (National Heart and Lung Institute, Imperial College London, London, UK); United States: A. Sonia Buist (PI) (Oregon Health & Science University, Portland, Oregon); Mary Ann McBurnie, William M. Vollmer, and Suzanne Gillespie (Kaiser Permanente Center for Health Research, Portland, Oregon); Sean Sullivan (University of Washington, Seattle, Washington); Todd A. Lee and Kevin B. Weiss (Northwestern University, Chicago, Illinois); Robert L. Jensen and Robert Crapo (Latter Day Saints Hospital, Salt Lake City, Utah); Paul Enright (University of Arizona, Tucson, Arizona); David M. Mannino (PI), John Cain, Rebecca Copeland, Dana Hazen, and Jennifer Methvin (University of Kentucky, Lexington, Kentucky). Additional local support for BOLD clinical sites was provided by: Boehringer Ingelheim China (GuangZhou, China); Turkish Thoracic Society, Boehringer-Ingelheim, and Pfizer (Adana, Turkey); Altana, AstraZeneca, Boehringer-Ingelheim, GlaxoSmithKline, Merck Sharpe & Dohme, Novartis, Salzburger Gebietskrankenkasse and Salzburg Local Government (Salzburg, Austria); Research for International Tobacco Control, the International Development Research Centre, the South African Medical Research Council, the South African Thoracic Society GlaxoSmithKline Pulmonary Research Fellowship, and the University of Cape Town Lung Institute (Cape Town, South Africa); and Landspítali-University Hospital-Scientific Fund, GlaxoSmithKline Iceland, and AstraZeneca Iceland (Reykjavik, Iceland); GlaxoSmithKline Pharmaceuticals, Polpharma, Ivax Pharma Poland, AstraZeneca Pharma Poland, ZF Altana Pharma, Pliva Kraków, Adamed, Novartis Poland, Linde Gaz Polska, Lek Polska, Tarchomińskie Zakłady Farmaceutyczne Polfa, Starostwo Proszowice, Skanska, Zasada, Agencja Mienia Wojskowego w Krakowie, Telekomunikacja Polska, Biernacki, Biogran, Amplus Bucki, Skrzydlewski, Sotwin, and Agroplon (Cracow, Poland); Boehringer-Ingelheim, and Pfizer Germany (Hannover, Germany); the Norwegian Ministry of Health’s Foundation for Clinical Research, and Haukeland University Hospital’s Medical Research Foundation for Thoracic Medicine (Bergen, Norway); AstraZeneca, Boehringer-Ingelheim, Pfizer, and GlaxoSmithKline (Vancouver, Canada); Marty Driesler Cancer Project (Lexington, Kentucky); Altana, Boehringer Ingelheim (Phil), GlaxoSmithKline, Pfizer, Philippine College of Chest Physicians, Philippine College of Physicians, and United Laboratories (Phil) (Manila, Philippines); Air Liquide Healthcare P/L, AstraZeneca P/L, Boehringer Ingelheim P/L, GlaxoSmithKline Australia P/L, Pfizer Australia P/L (Sydney, Australia), Department of Health Policy Research Programme, Clement Clarke International (London, UK); Boehringer Ingelheim and Pfizer (Lisbon, Portugal), Swedish Heart and Lung Foundation, The Swedish Association against Heart and Lung Diseases, Glaxo Smith Kline (Uppsala, Sweden), Seed Money Grant (PF20/0512), Aga Khan University, and Chiesi Pakistan (Pvt.) Limited (Karachi, Pakistan).
References
- 1.United Nations General Assembly. New York: United Nations: 2012. Resolution adopted by the general assembly on 19 September 2011 66/2. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. [Google Scholar]
- 2. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet . 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet . 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 4. Doll R, Peto R. Mortality in relation to smoking: 20 years’ observations on male British doctors. BMJ . 1976;2:1525–1536. doi: 10.1136/bmj.2.6051.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wilson D, Adams R, Appleton S, Ruffin R. Difficulties identifying and targeting COPD and population-attributable risk of smoking for COPD: a population study. Chest . 2005;128:2035–2042. doi: 10.1378/chest.128.4.2035. [DOI] [PubMed] [Google Scholar]
- 6. Eisner MD, Anthonisen N, Coultas D, Kuenzli N, Perez-Padilla R, Postma D, et al. Committee on Nonsmoking COPD, Environmental and Occupational Health Assembly. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med . 2010;182:693–718. doi: 10.1164/rccm.200811-1757ST. [DOI] [PubMed] [Google Scholar]
- 7. GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med . 2017;5:691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hooper R, Burney P, Vollmer WM, McBurnie MA, Gislason T, Tan WC, et al. Risk factors for COPD spirometrically defined from the lower limit of normal in the BOLD project. Eur Respir J . 2012;39:1343–1353. doi: 10.1183/09031936.00002711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buist AS, Vollmer WM, Sullivan SD, Weiss KB, Lee TA, Menezes AM, et al. The Burden of Obstructive Lung Disease Initiative (BOLD): rationale and design. COPD . 2005;2:277–283. [PubMed] [Google Scholar]
- 10. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med . 1999;159:179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 11.Masters N, Tutt C.Smoking pack year calculator. 2007. http://smokingpackyears.com/
- 12. Miettinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol . 1974;99:325–332. doi: 10.1093/oxfordjournals.aje.a121617. [DOI] [PubMed] [Google Scholar]
- 13. Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health . 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ . 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. Cambridge: Cambridge University Press; 2006. Multilevel linear models: varying slopes, non-nested models, and other complexities. [Google Scholar]
- 16. Gelman A. Struggles with survey weighting and regression modeling. Stat Sci . 2007;22:153–164. [Google Scholar]
- 17. Townend J, Minelli C, Mortimer K, Obaseki DO, Al Ghobain M, Cherkaski H, et al. The association between chronic airflow obstruction and poverty in 12 sites of the multinational BOLD study. Eur Respir J . 2017;49:1601880. doi: 10.1183/13993003.01880-2016. [DOI] [PubMed] [Google Scholar]
- 18. Atassi M, Kava ACF, Nejjari C, Benjelloun MC, El Biaze M, El Kinany K, et al. Association between chronic airflow obstruction and socio-economic position in Morocco: BOLD results. Int J Tuberc Lung Dis . 2020;24:202–206. doi: 10.5588/ijtld.19.0170. [DOI] [PubMed] [Google Scholar]
- 19. Vanfleteren LEGW, Lamprecht B, Studnicka M, Kaiser B, Gnatiuc L, Burney P, et al. Body mass index and chronic airflow limitation in a worldwide population-based study. Chron Respir Dis . 2016;13:90–101. doi: 10.1177/1479972315626012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lamprecht B, McBurnie M, Vollmer W, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest . 2011;139:752–763. doi: 10.1378/chest.10-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sun Y, Milne S, Jaw JE, Yang CX, Xu F, Li X, et al. BMI is associated with FEV 1 decline in chronic obstructive pulmonary disease: a meta-analysis of clinical trials. Respir Res . 2019;20:236. doi: 10.1186/s12931-019-1209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Coxson HO, Chan IH, Mayo JR, Hlynsky J, Nakano Y, Birmingham CL. Early emphysema in patients with anorexia nervosa. Am J Respir Crit Care Med . 2004;170:748–752. doi: 10.1164/rccm.200405-651OC. [DOI] [PubMed] [Google Scholar]
- 23. Blanc PD. Occupation and COPD: a brief review. J Asthma . 2012;49:2–4. doi: 10.3109/02770903.2011.611957. [DOI] [PubMed] [Google Scholar]
- 24. Blanc PD, Eisner MD, Balmes JR, Trupin L, Yelin EH, Katz PP. Exposure to vapors, gas, dust, or fumes: assessment by a single survey item compared to a detailed exposure battery and a job exposure matrix. Am J Ind Med . 2005;48:110–117. doi: 10.1002/ajim.20187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blanc PD, Annesi-Maesano I, Balmes JR, Cummings KJ, Fishwick D, Miedinger D, et al. The occupational burden of nonmalignant respiratory diseases: an official American Thoracic Society and European Respiratory Society statement. Am J Respir Crit Care Med . 2019;199:1312–1334. doi: 10.1164/rccm.201904-0717ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cullinan P. Occupation and chronic obstructive pulmonary disease (COPD) Br Med Bull . 2012;104:143–161. doi: 10.1093/bmb/lds028. [DOI] [PubMed] [Google Scholar]
- 27. Allwood BW, Myer L, Bateman ED. A systematic review of the association between pulmonary tuberculosis and the development of chronic airflow obstruction in adults. Respiration . 2013;86:76–85. doi: 10.1159/000350917. [DOI] [PubMed] [Google Scholar]
- 28. Amaral AFS, Patel J, Kato BS, Obaseki DO, Lawin H, Tan WC, et al. BOLD Collaborative Research Group. Airflow obstruction and use of solid fuels for cooking or heating: BOLD results. Am J Respir Crit Care Med . 2018;197:595–610. doi: 10.1164/rccm.201701-0205OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Smith M, Li L, Augustyn M, Kurmi O, Chen J, Collins R, et al. China Kadoorie Biobank collaborative group. Prevalence and correlates of airflow obstruction in ∼317,000 never-smokers in China. Eur Respir J . 2014;44:66–77. doi: 10.1183/09031936.00152413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fang L, Gao P, Bao H, Tang X, Wang B, Feng Y, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med . 2018;6:421–430. doi: 10.1016/S2213-2600(18)30103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, et al. China Pulmonary Health Study Group. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet . 2018;391:1706–1717. doi: 10.1016/S0140-6736(18)30841-9. [DOI] [PubMed] [Google Scholar]
- 32. Smith KR, Bruce N, Balakrishnan K, Adair-Rohani H, Balmes J, Chafe Z, et al. HAP CRA Risk Expert Group. Millions dead: how do we know and what does it mean? Methods used in the comparative risk assessment of household air pollution. Annu Rev Public Health . 2014;35:185–206. doi: 10.1146/annurev-publhealth-032013-182356. [DOI] [PubMed] [Google Scholar]
- 33. Kiefer EM, Hankinson JL, Barr RG. Similar relation of age and height to lung function among Whites, African Americans, and Hispanics. Am J Epidemiol . 2011;173:376–387. doi: 10.1093/aje/kwq417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Burney P, Minelli C. Using reference values to define disease based on the lower limit of normal biased the population attributable fraction, but not the population excess risk: the example of chronic airflow obstruction. J Clin Epidemiol . 2018;93:76–78. doi: 10.1016/j.jclinepi.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 35. Rowe AK, Powell KE, Flanders WD. Why population attributable fractions can sum to more than one. Am J Prev Med . 2004;26:243–249. doi: 10.1016/j.amepre.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 36. Fox AJ, Collier PF. Low mortality rates in industrial cohort studies due to selection for work and survival in the industry. Br J Prev Soc Med . 1976;30:225–230. doi: 10.1136/jech.30.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Becklake MR, Lalloo U. The ‘healthy smoker’: a phenomenon of health selection? Respiration . 1990;57:137–144. doi: 10.1159/000195837. [DOI] [PubMed] [Google Scholar]