Abstract
Introduction
Postgraduate medical trainees frequently work ≥ 24- hour shifts causing fatigue and adverse consequences such as motor vehicle incidents (MVIs). We aim to determine the incidence of MVIs during the commutes of trainees in British Columbia (BC) in the preceding year.
Methods
We completed a retrospective, cross-sectional survey of trainees regarding work hours, shifts, and MVIs in the previous year. MVIs included falling asleep while driving, sudden braking or swerving to avoid a collision, unintentionally running a red light or stop sign, or collisions.
Results
Of 273 respondents, over half (54.6%) reported ≥1 MVI, one in 14 were in a collision (7.0%), and two thirds (66.3%) reported that the safety of their commute had been impacted by fatigue in the past year. After adjustment for road exposure and shift-related factors, every ten km increase in commute length was associated with an increased risk of MVI (aOR=1.54;95%CI:1.15-2.12). Reported attentional failures, such as unintentionally running a red light and/or stop sign, increased for every ten hours on-call (aOR=1.44;95%CI:1.03-2.04) and for every additional past-midnight shift worked (aOR=1.13;95%CI:1.01-1.26).
Discussion
Trainees with longer and more frequent commutes had an increased risk of MVIs. Trainees who worked more hours on-call and more past-midnight shifts reported significantly more attentional failures while commuting. This study helps us understand factors affecting trainee commuter safety and supports calls for the provision of safe alternatives to commuting for postgraduate trainees.
Abstract
Introduction
Les résidents et moniteurs cliniques (fellows) en médecine travaillent souvent ≥ 24 heures d’affilée, ce qui entraîne de la fatigue et des conséquences néfastes comme les accidents de la route, parfois évités de justesse. Notre objectif était de déterminer la fréquence des accidents de la route et des incidents qui auraient pu entraîner un accident, survenus lors des déplacements des résidents ou moniteurs cliniques en Colombie-Britannique (C.-B.) au cours de l’année précédente.
Méthodes
Nous avons réalisé une enquête rétrospective transversale auprès des résidents. Les questions portaient sur les heures travaillées, les quarts de travail et les accidents ou les incidents pouvant entraîner un accident de la route, au cours de l’année précédente. Les incidents et accidents visés comprenaient la somnolence au volant, le freinage brusque ou l’embardée pour éviter une collision, le non-respect involontaire d’un feu rouge ou d’un panneau d’arrêt, et la collision.
Résultats
Pour l’année de référence, parmi les 273 répondants, plus de la moitié (54,6 %) ont signalé ≥1 accident, un répondant sur 14 a été impliqué dans une collision (7,0 %) et deux tiers (66,3 %) ont déclaré que la fatigue avait affecté la sécurité de leur déplacement. Après ajustement pour tenir compte de l’exposition à la route et des facteurs liés aux quarts de travail, chaque portion de 10 km qui s’ajoutait au trajet était associée à une augmentation du risque d’accident ou incident de la circulation (aOR=1.54;IC95%:1.15-2.12). Les baisses d’attention signalées, liées par exemple au franchissement involontaire d’un feu rouge ou d’un panneau d’arrêt, augmentaient pour chaque période de 10 heures de garde (aOR=1,44 ; 95 % IC:1,03-2,04) et pour chaque quart supplémentaire effectué après minuit (aOR=1,13 ; 95 % IC:1,01-1,26).
Discussion
Les stagiaires dont les trajets étaient plus longs et plus fréquents présentaient un risque plus élevé d’implication dans un accident ou incident de la route. Les stagiaires qui travaillaient plus d’heures de garde et plus de quarts de nuit ont signalé une fréquence considérablement plus élevée de pertes d’attention pendant les trajets. Cette étude nous aide à comprendre les facteurs qui affectent la sécurité des trajets domicile-travail des résidents et moniteurs cliniques et montre la pertinence des appels à la mise en place d’options sécuritaires pour les déplacements concernés.
Introduction
Canadian postgraduate medical trainees frequently work extended hours when compared to other professions. Strict regulations on maximum duty hours exist for pilots, truck drivers, and marine personnel due to the serious effects of sleep deprivation.1-3 However, the maximum number of hours a medical resident can work varies substantially, with some countries having strict national regulations, such as those in the European Union, while others only have recommendations provided by their national medical associations.4 In Canada, currently there are no standard national regulations on work hours as agreements are negotiated within each province.4 Currently the limit is between 24-26 hours of consecutive work in all provinces except Quebec, where the limit has been set to 16 hours.4 The Resident Doctors of British Columbia (RDBC) Collective Agreement states that if a resident works a shift of 24 hours or longer without four consecutive hours of rest, they shall be dismissed from duty no later than 10:00am unless there are “exigent circumstances, such as a patient emergency”.5 The “exigent circumstances” caveat is ambiguous and a typical resident work day starts well in advance of 10:00am the preceding day which often results in residents working more than 24 consecutive hours.
Extended shifts and resultant sleep deprivation have been shown to increase the incidence of medication and diagnostic errors, percutaneous injuries, and mental health problems.6-8 Multiple studies from the United States (US) found a positive association between extended shift duration, fatigue, and risk of motor vehicle incidents (MVI) s.9-12 Notably, motor vehicle collisions (MVCs) were found to be the 3rd leading cause of death for residents in the US.13 A US study found that interns had increased likelihood of reporting a MVC (OR=2.3) or near-miss (OR=5.9) after an extended versus non-extended shift.10 Further, each additional extended shift per month increased the risk of any MVC by 9.1% and increased the risk of a MVC while commuting from work by 16.2%.10 A study of Emergency Medicine residents found that 74% of collisions and 80% of near-misses followed night shifts.12 A Canadian study of Family Medicine residents found that rural residents were more likely to be involved in a collision while urban residents experienced more close calls.14 Rural residents also drove more than double the distance of their urban counterparts, suggesting an impact of road exposure on commuter safety.14 Evidently, these results have implications for the health and safety of residents, since extended work shifts are a hallmark of medical education and training. Furthermore, extended shifts may also put members of the public at risk during residents’ commute home from the hospital.
There is limited Canadian data examining the relationship of postgraduate trainee shift length, monthly work hours, and driving safety. This study aimed to retrospectively determine the occurrence of motor vehicle collisions and/or near misses during the commutes of postgraduate trainees practicing in BC in the preceding year and to study the association of MVIs with work-hours, shift type, and speciality.
Methods
Survey design
We developed the survey (Appendix A, Article 3) through an iterative design process. We ensured face validity by seeking input from resident groups during development. A draft survey was piloted during the Department of Emergency Medicine “Research in Progress” Rounds and feedback from faculty and residents was collected and considered during subsequent survey refinement.
Participants
Participants were invited to partake in the study if they were current postgraduate trainees in British Columbia, including residents and fellows, and had driven to work at least once in the preceding 12 months.
Recruitment and data collection
Recruitment for the survey occurred via two emails through the RDBC biweekly newsletter, the Rounds (Appendix A, Article 1) to current postgraduate medical trainees in BC. Individual emails were also sent to each residency department to invite their trainees to participate. The data collection period lasted from February 14, 2020 until April 6, 2020. Participation was incentivized by an opportunity to enter a raffle for gift cards upon completion of the survey which was separate and anonymous from the collection of individual survey results. Consent was included on the first page of the survey (Appendix A, Article 2). Study data was collected and managed using the UBC instance of the Research Electronic Data Capture (REDCap) application.15,16 REDCap is a secure, web-based software platform designed to support data capture for research studies.
Outcome measures
A motor vehicle incident (MVI) was defined as falling asleep while driving or stopped in traffic, sudden braking or swerving to avoid a collision, unintentionally running a red light or stop sign, or a motor vehicle collision. Relevant studies examining motor vehicle incidents in residents and interns included similar types of motor vehicle incidents and “near-misses.”10,11
The primary outcome was an MVI in the past 12 months. We examined each MVI component (i. falling asleep, ii. running stop light/sign, iii. sudden braking or swerving, and iv. collision) as secondary outcomes. We also examined MVIs in the past 30 days. We considered the following explanatory factors: road exposure (commute length, commutes per week), days worked by shift type (standard days worked in past 30 days, past-midnight shifts worked in past 30 days, and on-call shifts worked in past 30 days), hours worked by shift type (average hours worked per week, hours per on-call shift, hours per standard work day) and specialty (surgical or medical).
Statistical analysis
We computed descriptive statistics for all outcomes, explanatory factors, and demographics of survey respondents, including counts and proportions for categorical variables, and means and standard deviations for numeric variables. For each outcome, odds ratios (OR) were estimated using a separate logistic regression model per explanatory factor. Adjusted odds ratios (aOR) were then estimated by including all explanatory factors in a single logistic regression model. We also examined differences in explanatory factors by specialty. We computed averages with 95% confidence intervals and used t-tests to compare the average of each factor among trainees with surgical versus medical specialties. We considered p ≤ 0.05 to be statistically significant.
This research was approved by the University of British Columbia (UBC) Research Ethics Board (ID #H19-00982).
Results
Demographic data
Of 1755 active postgraduate trainees completing their training in BC, 273 (15.6%) returned complete surveys. The average age of respondents was 29.8 (± 3.5) years with 146 (53.5%) identifying as female, 124 (45.4%) as male, and 3 (1.1%) as another gender. Of the respondents, 216 (79.1%) were in a medical discipline, and 57 (20.9%) were in a surgical discipline, as defined by CaRMS.17 Respondent characteristics are presented in Table 1.
Table 1.
Demographic characteristics of respondents
| Count (%) or Mean (+/- SD) n = 273 (%) |
|
|---|---|
| Age (years) | 29.8 (+/- 3.5) |
| Gender | |
| Female | 146 (53.5) |
| Male | 124 (45.4) |
| Other | 3 (1.1) |
| Specialty Type | |
| Medical | 216 (79.1) |
| Family Medicine | 55 (20.1) |
| Psychiatry | 38 (13.9) |
| Emergency Medicine | 27 (9.9) |
| Pediatrics | 22 (8.1) |
| Internal Medicine | 18 (6.6) |
| Anesthesiology | 11 (4.0) |
| Diagnostic Radiology | 10 (3.7) |
| Radiation Oncology | 6 (2.2) |
| Dermatology | 5 (1.8) |
| Laboratory Medicine | 5 (1.8) |
| Neurology - Adult | 5 (1.8) |
| Other (<5 respondents) | 9 (3.3) |
| Surgical | 57 (20.9) |
| Obstetrics & Gynecology | 15 (5.5) |
| Orthopedic Surgery | 14 (5.1) |
| General Surgery | 9 (3.3) |
| Ophthalmology | 6 (2.2) |
| Other (<5 respondents) | 13 (4.8) |
| Postgraduate Year | |
| PGY1 | 69 (25.3) |
| PGY2 | 72 (26.4) |
| PGY3 | 45 (16.5) |
| PGY4 | 45 (16.5) |
| PGY5 + | 29 (10.6) |
| Fellow | 13 (4.8) |
Postgraduate trainees worked an average of 58.1 hours (±16.1; range:6-120) per week in the 30 days prior to completing the survey. Trainees worked an average of 10.3 (± 7.5) standard workdays (10.4 ± 5.4 hours) and 4.55(± 2.90) on-call shifts (18.6 ± 10.3 hours) in the previous 30 days. Trainees also reported an average of 1.21 (± 2.65) shifts where they were not on-call but were in the hospital past midnight. The average weekly work hours in the last 30 days reported by surgical trainees (74.4 ±17.9 hours) was significantly higher than for medical trainees (53.9 ±12.7 hours; p < 0.0001). Additionally, surgical trainees reported significantly more on-call shifts (6.77 ± 2.62 versus 3.97 ± 2.68; p < 0.0001) and significantly longer on-call shifts (23.5 ± 9.4 versus 17.3 ± 5.9 hours; p < 0.0001) than medical trainees, respectively (Table 2). There was no significant difference found in the number of standard workdays, length of standard workdays, or shifts past midnight between trainees in surgical and medical specialties.
Table 2.
Shift-related and road exposure factors by speciality
| All (n =273) |
Surgical (n = 57) | Medical (n =216) | ||
|---|---|---|---|---|
| Mean (SD) | P-value* | |||
| Shift-related | ||||
| Average hours worked per week | 58.1 (16.1) | 74.1 (17.9) | 53.9 (12.7) | <0.0001 |
| Standard days worked in past 30 days | 10.3 (7.5) | 11.0 (8.2) | 10.1 (7.3) | 0.4565 |
| Hours per standard work day | 10.4 (5.4) | 10.9 (2.1) | 10.3 (5.9) | 0.1988 |
| On-call shifts worked in past 30 days | 4.6 (2.9) | 6.8 (2.6) | 4.0 (2.7) | <0.0001 |
| Hours per on-call shift | 18.6 (10.3) | 23.5 (9.4) | 17.3 (10.2) | <0.0001 |
| Past-midnight shifts worked in past 30 days | 1.21 (2.7) | 1.1 (2.5) | 1.2 (2.7) | 0.6398 |
| Road exposure | ||||
| Length of commute (km) | 10.2 (9.7) | 7.7 (8.6) | 10.9 (9.8) | 0.0160 |
| Commutes per week | 5.6 (4.3) | 6.9 (5.1) | 5.2 (4.1) | 0.0250 |
| Weekly road exposure (km) | 64.3 (84.5) | 55.8 (75.5) | 66.6 (86.9) | 0.1899 |
t-test comparing average of explanatory factor among surgical versus medical trainees
Commute length
The average one way length of commute by trainees while driving was 10.2 (±9.7) km and they reported 5.58 (±4.33) commutes by vehicle per week. Trainees in medical specialties reported an average commute of 10.9 (±9.8) km which was significantly longer than surgical trainees (7.69 ± 8.59 km; p=0.0160). However, surgical trainees reported an average of 6.89 (±5.06) commutes per week which was significantly more than for medical trainees (5.23 ±4.06 commutes; p = 0.0250). Average weekly road exposure (commute length x trips per week) was 66 km for medical residents and 54 km for surgical residents (Table 2).
Motor vehicle incidents
Of the respondents, 149 (54.6%) reported at least one MVI on their commute in the preceding year, with 55 (20.1%) reporting at least one MVI in the preceding 30 days (Table 3). The most common MVI was “suddenly braking or swerving to avoid a crash” (44.3% of participants). Compared to medical trainees, surgical trainees had a significantly higher likelihood of reporting an MVI in the past 12 months (OR=1.89, CI:1.04-3.55; p = 0.0411) (Table 4). However, after controlling for road exposure and shift-related factors, the type of specialty (surgical vs. medical) was not significantly associated with MVIs in the past 12 months (Figure 1).
Table 3.
MVI by specialty type
| All (n = 273) |
Surgical (n = 57) |
Medical (n = 216) |
|
|---|---|---|---|
| Any motor vehicle incident | |||
| Past 12 months* | 149 (54.6%) | 38 (66.7%) | 111 (51.4%) |
| Past 30 days | 55 (20.1%) | 11 (19.3%) | 44 (20.4%) |
| Collision | |||
| Past 12 months | 19 (7.0%) | 7 (12.3%) | 12 (5.6%) |
| Past 30 days | 5 (1.8%) | 1 (1.8%) | 4 (1.9%) |
| Fell asleep | |||
| Past 12 months | 46 (16.8%) | 13 (22.8%) | 33 (15.3%) |
| Past 30 days | 9 (3.3%) | 0 | 9 (4.2%) |
| Ran stop light/sign | |||
| Past 12 months | 61 (22.3%) | 13 (22.8%) | 48 (22.2%) |
| Past 30 days | 8 (2.9%) | 1 (1.8%) | 7 (3.2%) |
| Sudden brake or swerve | |||
| Past 12 months | 121 (44.3%) | 29 (50.9%) | 92 (42.6%) |
| Past 30 days | 43 (15.8%) | 10 (17.5%) | 33 (15.3%) |
Significantly different unadjusted OR for MVI between surgical and medical; refer to Table 3 for OR and p-values
Table 4.
Adjusted and unadjusted odds ratios for all motor vehicle incidents, motor vehicle collisions, and unintentionally running a red light or stop sign.
| Unadjusted Odds Ratios (OR) | Adjusted Odds Ratios (aOR) | |||
|---|---|---|---|---|
| Past 12 months | Past 30 days | Past 12 months | Past 30 days | |
| All Motor Vehicle Incidents | ||||
| Length of commute (per 10 km) | 1.52 (1.16, 2.04) p = 0.0035 |
1.65 (1.25, 2.20) p = 0.0005 |
1.54 (1.15, 2.12) p = 0.0058 |
1.60 (1.18, 2.20) p = 0.0031 |
| Commutes per week | 1.09 (1.03, 1.15) p = 0.0049 |
1.15 (1.07, 1.24) p = 0.0001 |
1.06 (1.00, 1.13) p = 0.0601 |
1.13 (1.05, 1.23) p = 0.0015 |
| Surgical vs Medical Trainees | 1.89 (1.04, 3.55) p = 0.0411 |
0.93 (0.43, 1.90) p = 0.8576 |
1.99 (0.95, 4.28) p = 0.0730 |
0.56 (0.20, 1.44) p = 0.2426 |
| Motor Vehicle Collisions | ||||
| Average hours worked per week (per 10 hrs) | 1.40 (1.07, 1.84) p = 0.0128 |
1.04 (0.59, 1.73) p = 0.8785 |
1.34 (0.91, 2.05) p = 0.1554 |
1.02 (0.49, 2.09) p = 0.9493 |
| Hours per on-call shift (per 10 hours) | 1.69 (1.06, 2.77) p = 0.0306 |
0.72 (0.30, 1.68) p = 0.4375 |
1.59 (0.92, 2.80) p = 0.0968 |
0.50 (0.12, 1.68) p = 0.2939 |
| Unintentionally running a Red Light or Stop Sign | ||||
| Shifts Past-Midnight | 1.08 (0.98, 1.19) p = 0.1056 |
1.09 (0.84, 1.30) p = 0.4016 |
1.13 (1.01, 1.26) p = 0.0232 |
1.07 (0.82, 1.32) p = 0.5676 |
| Hours per on-call shift (per 10 hours) | 1.26 (0.95, 1.68) p = 0.1142 |
0.68 (0.34, 1.34) p = 0.2612 |
1.44 (1.03, 2.04) p = 0.0354 |
0.74 (0.28, 1.64) p = 0.4979 |
Figure 1.
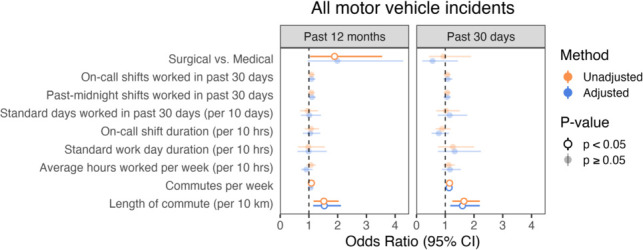
Odds ratios for occurrence of MVIs by explanatory factors
Number and length of commutes
After adjusting for road exposure and shift-related factors, trainees with longer commutes were more likely to report an MVI in the past 12 months (aOR=1.54 per 10 km;95%,CI:1.15-2.12;p = 0.0058) and in the past 30 days (aOR=1.60 per 10 km;95%CI:1.18-2.20; p = 0.0031). Having more commutes per week also increased the odds of reporting an MVI in the past 30 days (aOR=1.13 per trip;95%CI:1.05-1.23; p = 0.0015) (Table 4). Other explanatory factors were not associated with MVIs (Figure 1).
Secondary outcomes
Nineteen trainees (7.0%) reported 22 motor vehicle collisions in the past year. Trainees were more likely to report a collision for every additional ten hours worked per week (OR=1.40,95%CI:1.07-1.84; p = 0.0128) and for every additional ten hours of being on-call (OR=1.69,95%CI:1.06-2.77;p = 0.0306), however these associations were not significant after adjustment for explanatory factors (Table 4). After adjustment, the odds of reporting unintentionally running a red light or stop sign significantly increased (aOR=1.44;95%CI:103-2.04;p = 0.0354) for every ten additional hours spent on-call and for every additional past-midnight shift worked in the preceding 30 days (aOR=1.13;CI:1.01-1.26;p = 0.0232) (Table 4).
Trainee safety
Notably 181 respondents (66.3%) reported feeling that the safety of their commute had been impacted by fatigue in the last 12 months. One third of respondents (31.5%) detailed their experience commuting in the open-ended response portion of the survey (Table 5). Many cited methods employed to mitigate fatigue, which would have impaired their ability to commute safely, including sleeping in a call room or vehicle prior to driving home, or using loud music or open windows to stay awake. A few trainees noted living close to the hospital in order to avoid driving. Others used alternate modes of transportation including transit, biking, or walking. Multiple trainees suggested a need for program support and reimbursement for taxi fare or ride share programs in the event that they are too fatigued to drive home safely.
Table 5.
Select trainee quotes from the open-ended responses
| General comments regarding danger of driving home after work 24 hour shifts |
|---|
|
“It is not unusual, while driving home post call, to suddenly realize I am not properly focused on driving or that I am failing to notice things that I usually would (pedestrians, cyclist). The whole concept of 24 hour call is outdated, dangerous and needs to be reconsidered.”
“During my residency, driving home after a 24 hour call shift with minimal sleep was VERY dangerous. I would equate it as equal to or worse than driving impaired - no focus, no attention, auto pilot, trying as fast as possible to get home to go to sleep. There were times where I could not keep my eyes open while driving.” |
| Methods employed to avoid driving home after an on-call shift |
|
“I had one incident of falling asleep while driving and thankfully woke without harming myself or anyone else. Following this I chose to sleep at the hospital to avoid further incidents.”
“I feel myself nearly falling asleep post call when driving back [from the hospital]. I have to roll down the windows and blast music to stay awake” “My safety has not been impacted during residency because I fell asleep while driving on the highway in medical school (woke up drifting lanes, didn't crash), and now I always nap at the hospital or get a ride home.” |
| Seeking out other means of transportation |
| “I actually bike or bus only because on rotations where I drove I had so many issues eg falling asleep at red lights. I also pay a premium to live close to the hospital in order to make walking and biking possible.” |
| Program support and reimbursement |
|
“To say it [residency] is the most stressful time of life is an understatement, and the lack of help while on call, and to and from call is disheartening.”
“I strongly believe there should be an option for a taxi paid for by our program in cases of fatigue.” |
Discussion
Two thirds of respondents (66.3%) reported that the safety of their commute had been impacted by fatigue in the past year, over half (54.6%) were involved in at least one MVI, and 19 were in a collision (7.0%). The risk of MVIs was higher in residents with a higher number of commutes or longer commutes. These findings are similar to a previous Canadian study comparing road safety in urban versus rural PGY2 Family Medicine residents, in which 141 residents responded, 76 (54%) reported a close call and 31 (22%) reported a collision in the preceding 22 months.14
We determined that trainees who worked more past-midnight shifts and/or more hours on-call per week were more likely to report unintentionally running a red light or stop sign in the last year. Multiple trainees in our study shared their concerns regarding driving home after working in excess of 24 consecutive hours. Existing literature supports the claim that longer work hours, and the resultant sleep deprivation, are associated with a higher incidence of medication and diagnostic errors, percutaneous injuries, and MVIs in medical trainees.6,7,10
Attentional errors in interns occur at more than double the rate at night, particularly in interns who work extended shifts.19 Following the implementation of a 16-h consecutive work hour restriction for first-year residents in the United States in 2011, the mean risk of motor vehicle collisions decreased by 24% and the percutaneous injury risk decreased by more than 40%.18 While we were unable to demonstrate an association between past-midnight shifts, hours on-call, and all MVIs, the significant association with running a red light or stop sign suggests that working past-midnight and spending more hours on-call puts trainees at increased risk of attentional failures while commuting and likely translates into a higher risk of more serious MVIs over time.
We found that the number and length of commutes was associated with increased risk of MVIs. This association was observed previously in Canadian rural Family Medicine residents who drove significantly more than their urban counterparts and had a higher incidence of motor vehicle crashes.14 As this illustrates, there are a variety of factors that determine the number and length of a trainee’s commute, and in turn their risk of an MVI. These factors may include how far a trainee lives from their site, the requirement of trainees to cover multiple clinical sites and travel to academic sessions, as well as the need to make multiple commutes between home and work for personal, family, or professional reasons. These findings are at odds with many existing policies for reimbursement for commuting alternatives (ie. taxis, ride-shares) which are based on the type of shift worked, but do not consider factors associated with commute length and/or frequency.
Under the current RDBC Collective Agreement, residents may be reimbursed for “taxi fare from home to the hospital and return” when scheduled to be “on-call.”5 Considering that longer and more frequent commutes are associated with increased risk of MVI irrespective of the type of shift, and that over two-thirds of trainees reported feeling that fatigue had impacted the safety of their commute in the last year, our findings suggest a need for broader inclusion criteria to reimburse residents for safe transport alternatives outside of just “on-call” shifts. In response to the studies conducted in the United States, the implementation of education programs, coping strategies, and the creation of schedules sensitive to circadian cycles have been proposed.12 In our study, numerous trainees suggested reimbursement for taxi fares as an option to combat driving while fatigued. Some residency programs have adopted such policies to offer round-trip taxicab vouchers to residents on request, such as the University of Michigan Department of Surgery.10
An important strength of this study is that it included trainees in all specialties and at all levels of training, whereas many other studies examined residents within a particular specialty or interns only. As such, we captured variable call and work-hour requirements. However, the generalizability of our results is limited due to the low survey response rate (15.6%), the lack of uniform response rate across specialities, and the lack of identification of rural vs. urban trainees. Another limitation of this dataset is that it is self-reported and may be subject to recall and/or reporting bias. This survey may have been subject to sampling bias, especially if trainees who had an MVI were more likely to participate. We attempted to limit the risk of recall bias by placing a time-restriction of the last 12 months for reporting MVIs, which likely excluded some incidents. Furthermore, we opted to have trainees report their work hours for the last 30 days and to assume that this would reflect their work hours in the last 12 months. However, we recognize that trainees experience a wide variety of work hours and shift requirements based on the specialty through which they rotate. Lastly, we focused on MVIs by car, however many trainees commute by other means which were not captured.
Conclusion
The majority of medical trainees feel unsafe during their commute and MVIs are commonly reported. MVIs are associated with greater commute lengths and more frequent commutes. Trainees who worked more hours on-call and more past-midnight shifts increasingly reported attentional failures, such as running a red light or stop sign. These findings support calls for provision of safe alternatives to commuting for postgraduate trainees.
Acknowledgments
Acknowledgements: Thank you to University of British Columbia’s Department of Emergency Medicine NERD curriculum educators and colleagues (specifically Drs. Frank Scheuermeyer, Ben Huang, and Riley Golby) and those in attendance at Research in Progress Rounds for their contributions to our survey. Trainees, thank you for sharing your experiences.
Appendix A.
Article 1: Survey advertisement
Dear postgraduate trainees,
We are a research team at UBC performing a study on post-shift commuter safety in postgraduate trainees practicing in British Columbia. Participating in our survey allows us to study postgraduate trainee commuter safety, which can help impact policy development to make work safer.
Everyone who participates in this survey, even those who withdraw, will be allowed to enter a draw for one of five gift cards valued at $100 to either Mountain Equipment Co-op or Starbucks. In order to enter the draw, participants must submit their email address, and this will be saved separately from answers in the survey to maintain anonymity.
The survey will take approximately 10 minutes to complete and can be found at the link below. Consent documentation is contained in the survey itself.
Thank you for your participation,
Dr. Louise Cassidy
Emergency Medicine PGY3 - University of British Columbia
louise.cassidy@alumni.ubc.ca
Dr. Jeff Brubacher
Director of Vancouver Coastal Health Research Institute
Emergency Medicine, Vancouver General Hospital
Emma Croft
MSI2
University of British Columbia Medical School
Article 2: Consent Form
Commuter safety in postgraduate medical trainees in British Columbia
Ethics ID H19-00982
Lead author: Dr. Louise Cassidy
Co-author: Emma Croft
Principal Investigator: Dr. Jeff Brubacher
Hello,
If you are a postgraduate trainee practicing in British Columbia and have driven to work at least once in the last 12 months, you are invited to take part in this online survey. This survey is collecting data for a research project studying commuter safety in postgraduate trainees practicing in British Columbia. Participating in this study allows us to study postgraduate trainee commuter safety, which can help impact policy development to make work safer.
What is the aim of the study?
The aim of the study is to determine the incidence of postgraduate trainees in British Columia who have experienced unsafe driving incidents while commuting.
Why is this study important?
Medical trainees are routinely scheduled to work shifts of an extended duration during their residency training.
Research completed in the United States suggests that interns who work more extended length shifts per month had an increased risk of a crash while commuting home from work.
No Canadian data currently exists on this topic.
What are the potential benefits of completing this study?
Upon completion of the survey you will have the option to enter a draw for one of five gift cards, valued at $100.
In order to enter the draw you will need to enter your email. Your email will be stored separately from your survey responses and once the winners of the draw are announced, the list of emails will be destroyed.
What are the questions about?
There are some questions regarding demographics, work hours, and the average number of shifts worked at a certain length per month.
Other questions involve quantifying the type of unsafe driving incidents that have occurred in the last 12 months of medical training.
There are some sections that have an additional area for free text response. These are voluntary and you may opt to not write anything.
How long will it take?
Approximately 10 minutes.
What happens if I would like to leave the survey?
Participation in the survey is completely voluntary and you may leave at any time.
Is my personal information safe?
We do not collect any personal information except your email address if you would like to participate in the draw.
Your email address will be stored separately and unlinked from your survey responses.
Once the study is complete, data may be made publicly available, and after that time participants will not be able to withdraw their data.
Given some of the information that will be collected is personal, we will mitigate the risk of exposing sensitive information by anonymizing data collection and de-identifying data in it’s presentation.
Please note that completing this survey indicates that you have read and understand this consent form and you agree to participate. If you have any questions about this study, please don’t hesitate to contact the primary author, Louise Cassidy, at louise.cassidy@alumni.ubc.ca
If you have any concerns or complaints about your rights as a research participant and/or your experiences while participating in this study, contact the Research Participant Complaint Line in the UBC Office of Research Ethics at 604-822-8598 or if long distance e-mail RSIL@ors.ubc.ca or call toll free 1-877-822-8598.
Thank you in advance for you participation.
Article 3: Survey
Commuter safety in postgraduate medical trainees in British Columbia
Ethics ID H19-00982
Lead author: Dr. Louise Cassidy
Co-author: Emma Croft
Principal Investigator: Dr. Jeff Brubacher
Research Aims:
To determine in current postgraduate trainees in British Columbia
what is the incidence of trainees that have experienced an unsafe driving incident on their commute home from work
to study the association of driving incidents and hours of work
Are you a postgraduate medical trainee in British Columbia?
No = Not eligible to complete the survey
Yes = Eligible to complete the survey
Have you driven to work at least once in the past 12 months?
No = Not eligible to complete the survey
Yes = Eligible to complete the survey
1. Post-graduate training year: PGY1, PGY2, PGY3, PGY4, PGY5, PGY6, PGY7, fellow, other: specify _____
2. Specialty drop-down menu:
3. Age:
4. What gender do you identify with: Female, Male, Other.
5. On average, how many km is your commute to/from work one-way?
6. In the last 30 days of your medical training:
How many hours did you work in an average week?
How many commutes to and from work did you make in an average week?
How many hours was your standard work day? How many standard workdays did you work in the last 30 days?
How many hours were your “on-call” shifts? How many times were you “on-call” in the last 30 days?
How many times were you not “on-call”, but were in the hospital past midnight? (ie. evening shifts, night shifts, night float, evening call, long days)?
7. Please answer the following questions regarding unsafe driving incidents in your last 12 months of medical training:
(A) Have the following driving incidents occurred on your commute in the last 12 months of your medical training? (YES or NO)
Fallen asleep while driving or stopped in traffic (Y/N)
Sudden braking or swerving by you or another driver was required to avoid a crash (Y/N)
Unintentionally running a red light and/or stop sign (Y/N)
-
Motor vehicle collision (Y/N)
- If YES, How many times did this occur in the last 12 months?
If NO, stop. If YES, then:
(B) Have the following driving incidents occurred on your commute in the last 30 days of your medical training? If NO, stop. If YES,
-
(e)
Fallen asleep while driving or stopped in traffic (Y/N)
-
(f)
Sudden braking or swerving by you or another driver was required to avoid a crash (Y/N)
-
(g)
Unintentionally running a red light and/or stop sign (Y/N)
-
(h)
Motor vehicle collision (Y/N)
(C) Did it occur?
After a standard work day? (Y/N)
After an “on-call” shift? (Y/N)
After a shift were you were NOT “on-call”, but were in hospital past midnight? (ie. evening shifts, night shifts, night float, evening call?) (Y/N)
8. In the last 12 months of residency, have you felt your safety has been impacted by fatigue on your commute?
- Yes
- No
9. Free text box if you would like to share your experience
Footnotes
Conflicts of Interest: The authors have no competing interests to declare.
Funding: This research study was awarded the Resident Doctors of British Columbia Innovation Fund for Scholarly Pursuits, valued at $2500, in March 2019.
References
- 1.Canadian aviation regulations: aeronautics act, SOR2018-269, s.14; 1996September10. Available from: https://laws.justice.gc.ca/eng/regulations/SOR-96-433/page-134.html. [Accessed on Mar 2,2020].
- 2.Commercial vehicle drivers hours of service regulations, SOR2005-313. 2005October25. Available from: https://laws-lois.justice.gc.ca/eng/regulations/SOR-2005-313/index.html. [Accessed on Mar 2,2020].
- 3.Marine personnel regulations, SOR2007-115. 2007May31 Available from: https://laws-lois.justice.gc.ca/eng/regulations/sor-2007-115/page-44.html#h-731414. [Accessed on Mar 2,2020].
- 4.Pattani R, Wu PE, Dhalla IA. Resident duty hours in Canada: past, present and future. CMAJ. 2014;186(10):761-5. 10.1503/cmaj.131053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Resident Doctors of BC collective agreement. 2019April1. Available from: https://residentdoctorsbc.ca/bargaining-benefits/collective-agreement/. [Accessed on Jun 5, 2020].
- 6.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838-48. 10.1056/NEJMoa041406 [DOI] [PubMed] [Google Scholar]
- 7.Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296(9):1055-62. 10.1001/jama.296.9.1055 [DOI] [PubMed] [Google Scholar]
- 8.Ogawa R, Seo E, Maeno T, Ito M, Sanuki M, Maeno T. The relationship between long working hours and depression among first-year residents in japan. BMC Med Educ. 2018;18(1):50. 10.1186/s12909-018-1171-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marcus CL, Loughlin GM. Effect of sleep deprivation on driving safety in housestaff. Sleep. 1996;19(10):763-6. 10.1093/sleep/19.10.763 [DOI] [PubMed] [Google Scholar]
- 10.Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125-34. 10.1056/nejmoa041401 [DOI] [PubMed] [Google Scholar]
- 11.West CP, Tan AD, Shanafelt TD. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87(12):1138-44. 10.1016/j.mayocp.2012.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steele MT, Ma OJ, Watson WA, Thomas HA Jr, Muelleman RL. The occupational risk of motor vehicle collisions for emergency medicine residents. Acad Emerg Med. 1999;6(10):1050-3. 10.1111/j.1553-2712.1999.tb01191.x [DOI] [PubMed] [Google Scholar]
- 13.Yaghmour NA, Brigham TP, Richter T, et al. Causes of death of residents in ACGME-accredited programs 2000 through 2014: Implications for the learning environment. Acad Med. 2017;92(7):976-83. 10.1097/acm.0000000000001736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janke F, Dobbs B, McKay R, Linsdell M, Babenko O. Family medicine residents' risk of adverse motor vehicle events: A comparison between rural and urban placements. Can Med Educ J. 2013;4(2):e28-40. [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CaRMS. Surgical and Non-Surgical Disciplines; 2019April12 Available from: https://www.carms.ca/wp-content/uploads/2019/04/disciplines_en.pdf. [Accessed on May 25, 2020].
- 18.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829-37. 10.1056/nejmoa041404 [DOI] [PubMed] [Google Scholar]
- 19.Weaver MD, Landrigan CP, Sullivan JP, et al. The association between resident physician work-hour regulations and physician safety and health. Am J Med. 2020;133(7):e343-54. 10.1016/j.amjmed.2019.12.053 [DOI] [PMC free article] [PubMed] [Google Scholar]


