Myopia is the most common cause of visual impairment worldwide,1 and younger age at onset may progress to high myopia.2 As a result of coronavirus disease 2019 (COVID-19) causing an unprecedented global pandemic, most nations have imposed various strict containment measures on citizens, including limited outdoor activities and school closures, to prevent spread of the virus that causes COVID-19. These COVID-19 quarantines have led to billions of students simultaneously experiencing life-altering challenges, which may influence the incidence or worsening of myopia, or both, among schoolchildren.3 Establishing a COVID-19 intervention model in a clinical study is highly valuable for uncovering the crucial risk factors of myopia development.
Herein, we conducted a large-scale intervention study of myopia development with 12-month follow-up among schoolchildren in 1305 elementary and high schools in 11 districts of Wenzhou City, Zhejiang Province, China. The goal of the current study was to assess the impact of COVID-19 quarantine on myopia progression and incidence. All schoolchildren were invited to complete a self-administered questionnaire regarding demographic information. Certified technicians were trained to determine visual acuity (VA) and autorefraction testing by using the GoldEye RM-9000 (Shenzhen Aist Industrial Co., Ltd). Myopia was identified as an uncorrected visual acuity of less than 20/25 and a spherical equivalent refraction (SER) of –0.5 diopter (D) or less.4 High myopia was defined as an SER of –6.0 D or less. Because analysis for right and left eyes yielded a satisfactory correlation (Pearson correlation coefficient, 0.954), SER data from the right eye were used arbitrarily for assessing myopia development. The present study was approved by the ethics committee of the Wenzhou Medical University Affiliated Eye Hospital. Participant completion of the questionnaire was considered informed consent. All research adhered to the tenets of the Declaration of Helsinki. We performed examination at 3 time points: June 2019, December 2019, and June 2020, which provide large-scale and valuable intervention data for 6 months before and after the COVID-19 pandemic. The detailed methods are available at: https://github.com/mayunlong89/MIES_project.
A total of 1 060 925 students 7 to 18 years of age were recruited at baseline (June 2019; Fig S1, available at www.aaojournal.org). After stringent sample filtering, 1 001 749 students (550 756 male students and 450 993 female students) were included in the current study (Fig S1). Two follow-up examinations were conducted, in December 2019 involving 813 755 students (81.2%) and in June 2020 involving 768 492 students (76.7%). During August 2020, we resurveyed 12 013 students who were selected randomly from all grades to collect students’ outdoor activity time and online course time during the normal period and the COVID-19 quarantine and other 15 basic characteristics.
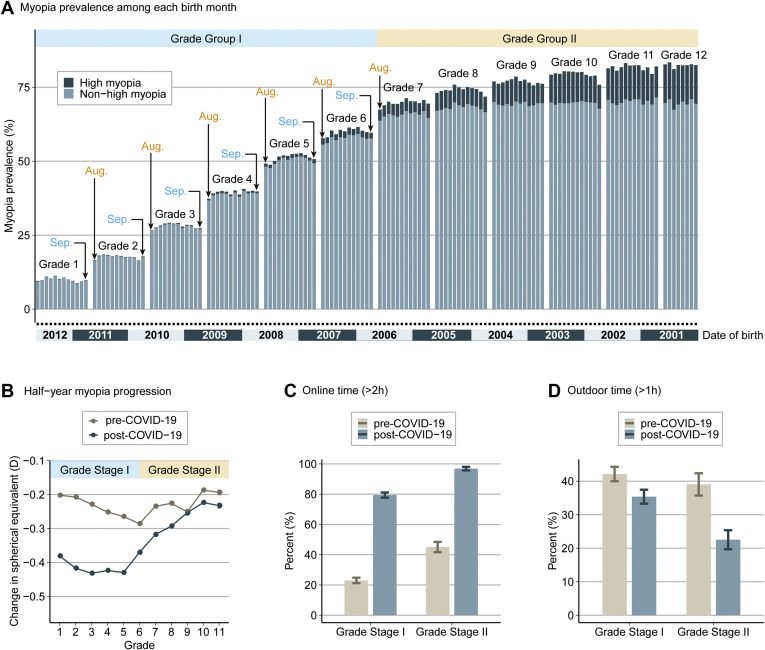
Overall myopia prevalence increased from 52.89% (95% confidence interval [CI], 52.79%–52.99%) in June 2019 to 53.9% (95% CI, 53.79%–54.01%) in December 2019 and 59.35% (95% CI, 59.24%–59.46%) in June 2020, which was consistent with the results of a recent study.5 The high myopia prevalence increased from 4.11% (95% CI, 4.07%–4.15%) in June 2019 to 4.24% (95% CI, 4.2%–4.29%) in December 2019 and 4.99% (95% CI, 4.94%–5.04%) in June 2020 (Table S1, available at www.aaojournal.org). Notably, the prevalence of myopia increased in a stepwise manner by grade, without being affected by the students’ birth months (Fig 1A). A mean increase in myopia prevalence of 8.54% during grades 1 through 6 was observed, compared with 4.32% in grades 7 through 12. The prevalence of high myopia increased from a mean of 4.46% (95% CI, 4.32%–4.6%) during grade 7 to a mean of 13.25% (95% CI, 12.95%–13.55%) during grade 12. The overall 1-year incidence rate of myopia was 22.66% (95% CI, 22.52%–22.80%) and that of high myopia was 1.8% (95% CI, 1.77%–1.83%). Multivariate Cox regression analyses also showed that grade was statistically significantly associated with myopia (hazard ratio [HR], 1.1; 95% CI, 1.08–1.13; P < 0.001) and high myopia (HR, 1.4; 95% CI, 1.35–1.46; P < 0.001), whereas age and birth month showed nonsignificant associations with myopia and high myopia (Fig S2A–D, available at www.aaojournal.org). To reduce the influence of a large sample size, we performed a permutation analysis of downsampling 1000 times by randomly selecting 10% students from total samples with retaining the proportion of students in each grade. We found the significant associations of grade with myopia and high myopia to be very stable, whereas age and birth month remained nonsignificant (Fig S2C–H). Together, our results reveal that increasing grade of education burden has important effects on myopia development rather than age, which could be categorized into 2 grade stages: grade stage I (grades 1–6), representing a myopia sensitive stage, and grade stage II (grades 7–12), representing a high myopia sensitive stage.
Figure 1.
Graphs showing the prevalence of myopia and high myopia and the influence of coronavirus disease 2019 (COVID-19) quarantine on myopia progression. A, Prevalence of myopia and high myopia divided by schoolchildren birth month among all grades at baseline. Each grade was divided into 12 bars according to birth month, ranging from September through August of the next year according to Chinese enrollment policy. B, Differences of grade-specific half-year myopia progression between the period before and after the COVID-19 quarantine. C, Differences in schoolchildren’s online time between the period before and after the COVID-19 quarantine categorized by grade stages I and II. D, Differences in schoolchildren’s outdoor activity time between the period before and after the COVID-19 quarantine categorized by grade stages I and II. To reduce the effects of age increasing during the COVID-19 quarantine, we divided the students of each grade into 2 independent sets (before COVID-19 quarantine vs. after COVID-19 quarantine) according to student birth months: the set before the COVID-19 quarantine includes students from September 1 through February 28 of the next year, and the set after the COVID-19 quarantine includes students from March 1 through August 31 (see Fig S2I). D = diopter.
We performed comparison analyses to assess the influence of COVID-19 on myopia progression of 6 months between the period before and after the COVID-19 quarantine. The students in each grade were divided into 2 independent groups according to their birth months to keep the matched age distribution between samples from before and after the COVID-19 quarantine (Fig S2I). We found that 6-month myopia progression among all schoolchildren increased by approximate 1.5 times from –0.23 D before the COVID-19 quarantine to –0.343 D after the COVID-19 quarantine (P < 0.001), and myopia progression speed of students from grade stage I was faster than that of students from grade stage II after the COVID-19 quarantine (Fig 1B). Furthermore, we found that the half-year incidence rate of myopia increased from 8.5% before the COVID-19 quarantine to 13.62% after the COVID-19 quarantine (P < 0.001). Stratified by educational level, educational system, and region of habitation, students showed a remarkably higher risk of myopia developing after the COVID-19 quarantine than before the COVD-19 quarantine (P <0.001). During the COVID-19 quarantine, 2 widely reported behavioral changes of students’ online time (>2 hours; i.e., increased 3.14 times in grade stage I and 2.07 times in grade stage II) and outdoor activity times (>1 hour; i.e., decreased 1.14 times in grade stage I and 1.71 times in grade stage II; Fig 1C, D) have been observed. Furthermore, by using multivariate regression analyses, we found that students’ online time was significantly positively associated with increased myopia incidence (HR, 1.14; 95% CI, 1.07–1.22; P = 3.39 × 10–5) and progression (spherical equivalent [SE]; β = 0.0188; P = 0.022), whereas outdoor activity time was significantly negatively associated with increased myopia incidence (HR, 0.91; 95% CI, 0.85–0.97; P = 0.021) and progression (SE; β = –0.0189; P = 0.039). These results partially may explain why half-year myopia progression substantially increased during the COVID-19 lockdown, which is consistent with previous reports.3 , 5 , 6 Together, our findings consistently suggest that the COVID-19 quarantine was a risk factor for the progression and incidence of myopia.
The limitations of this study should be noted. The study participants were schoolchildren and did not include adults at universities and middle-aged or quinquagenarian individuals; hence, our findings are limited to a younger population. We also did not collect information on parental myopia among more than 1 million students, which is an important risk factor for myopia in schoolchildren. It should be noted that noncycloplegic SER results were used for defining myopia. Although this parameter is less accurate than cycloplegic refraction, it is useful and effective for screening and monitoring myopia in a large-scale population. It is important to remember that the identified associations of risk factors with myopia development do not equal causation. Further related studies need to be performed to determine causation. Furthermore, students’ online time and outdoor activity time changes during the COVID-19 quarantine were based on self-report; thus, these measurements may be affected by recall bias. In view of the ongoing COVID-19 spread worldwide, more studies are warranted to explore the influence of COVID-19 on myopia progression in schoolchildren based on more different ethnicities.
The present study provides valuable intervention data to assess the impact of COVID-19 quarantine-related lifestyle changes on myopia development among schoolchildren. We found an interesting COVID-19–induced influence of myopia developing among children and adolescents, indicating that different intervention strategies should be applied to control myopia among elementary and high school students.
Footnotes
Disclosure(s): All authors have completed and submitted the ICMJE disclosures form.
The author(s) have no proprietary or commercial interest in any materials discussed in this article.
Supported by the National Natural Science Foundation of China (grant no.: U20A20364); the Key Program of National Natural Science Foundation of China (grant no.: 81830027 [J.Q.]); the National Natural Science Foundation of China (grant no.: 61871294); the Zhejiang Provincial Natural Science Foundation of China (grant no.: LR19C060001); the Scientific Research Foundation for Talents of Wenzhou Medical University (grant no.: QTJ18023 [J.S.]); and the Key Research and Development Program of Zhejiang Province (grant no.: 2020C03036 [L.X.]).
HUMAN SUBJECTS: Human subjects were included in this study. The human ethics committees at Wenzhou Medical University Affiliated Eye Hospital approved the study. Completion of the questionnaire by all participants was considered informed consent. All research adhered to the tenets of the Declaration of Helsinki.
No animal subjects were included in this study.
Author Contributions:
Conception and design: Zhou, W.-Q.Li, F.Lu, Su, Qu
Analysis and interpretation: Xu, Ma, Yuan, Y.Zhang, G.Zhang, Tu, X.Lu, J.Li, Xiong, Chen, Liu, Xue, Zhou, W.-Q.Li, Wu, Bao, Chen, F.Lu, Su, Qu
Data collection: Xu, Ma, Yuan, Y.Zhang, Wang, G.Zhang, Tu, J.Li, Xiong, Chen, Liu, Xue, Bao, Chen, F.Lu, Su, Qu
Obtained funding: Study was performed as part of regular employment duties at Wenzhou Medical University. No additional funding was provided.
Overall responsibility: Xu, Ma, Yuan, Wang, X.Lu, J.Li, Wu, F.Lu, Su, Qu
Supplementary Data
References
- 1.Holden B.A., Fricke T.R., Wilson D.A. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Gwiazda J., Hyman L., Dong L.M. Factors associated with high myopia after 7 years of follow-up in the Correction of Myopia Evaluation Trial (COMET) cohort. Ophthalmic Epidemiol. 2007;14(4):230–237. doi: 10.1080/01658100701486459. [DOI] [PubMed] [Google Scholar]
- 3.Wong C.W., Tsai A., Jonas J.B. Digital screen time during the COVID-19 pandemic: risk for a further myopia boom? Am J Ophthalmol. 2020;223:333–337. doi: 10.1016/j.ajo.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flitcroft D.I., He M., Jonas J.B. IMI-defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. 2019;60(3):M20–M30. doi: 10.1167/iovs.18-25957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J., Li Y., Musch D.C. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139(3):293–300. doi: 10.1001/jamaophthalmol.2020.6239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiang M., Zhang Z., Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63(4):531–532. doi: 10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.