Abstract
Background
Pressurized metered dose inhalers (pMDIs) and dry powder inhalers (DPIs) are commonly used drug-delivering devices for patients with chronic airway diseases. Appropriate peak inhalation flow rate (PIFR) and inhaler technique is essential for effective therapy. We aimed at optimizing inhalation therapy through the analysis of PIFRs in patients with chronic obstructive pulmonary disease (COPD) or asthma as well as the effect of technique training using In-Check DIAL® to help patients to achieve their optimal inspiratory flow rates.
Methods
The study continuously enrolled patients who were diagnosed as COPD or asthma from respiratory clinics. PIFRs were described and analyzed between the newly-diagnosed and follow-up patients, and the stable and acute exacerbation patients, respectively. Every participant was trained inhaler technique using In-Check DIAL®. PIFRs before and after training was compared by self-control analysis.
Results
Among a total of 209 patients, the average age was 56.9 years. For DPIs users, 10.8% patients had a PIFR < 30 L/min and 44.1% patients had a PIFR ≥ 60 L/min before technique training. After technique training, scarcely patient (1.5%) had a PIFR < 30 L/min, and 60.5% patients had a PIFR ≥ 60 L/min. The patient’s average PIFR increased by 5.6L/min after training. The increase in PIFR before and after training was significant (p < 0.001) for most patients, but no significant variation was found in patients with acute exacerbation (p = 0.822).
Conclusions
A considerable number of patients with COPD or asthma were not able to achieve the minimum or optimal PIFR for DPIs. Inhaler training can increase patients’ PIFRs and improve their ability to use DPIs.
Trail registration The study has registered in chictr.org.cn (ChiCTR1900024707) and been approved by the Ethics Committee of Zhongshan Hospital of Fudan University (B2019-142).
Keywords: Chronic obstructive pulmonary disease, Asthma, Dry powder inhalers, Peak inhalation flow rate, Technique training
Introduction
Chronic respiratory diseases, especially Chronic obstructive pulmonary disease (COPD) and asthma, are common diseases worldwide with leading mortality and morbidity. In China, the prevalence of COPD in patients over 40 years old was 8.2–13.7% [1, 2]. COPD has accounted for 1.6% of all hospital admissions and ranked as the fourth leading cause of death in urban areas and the third leading cause of death in rural areas worldwide [3]. COPD has been a heavy burden for China, with a direct medical cost of $72 to $3565 per capita per year accounting for 40% of the average family's total income [4]. In the recent epidemiological studies, the overall prevalence of asthma in China ranged from 1.2 to 5.8%, while 4.2% among adults [5, 6].
Inhalation therapies, including inhaled corticosteroid (ICS), long-acting β2 agonists (LABA) and long-acting muscarinic antagonists (LAMA), play an important role for the treatment and management of both COPD and asthma [7]. Inhalers typically used for inhalation therapy are sorted into three types based on their respective technical characteristics and particle properties: pressurized metered dose inhaler (pMDI), dry powder inhalers (DPIs), soft mist inhalers (SMI). pMDIs do not require the patients’ peak inhalation flow rate (PIFR) to reach a certain value, but drug delivery using pMDIs is highly dependent on the patient’s inhaler technique [8]. Failure to coordinate or synchronize actuation with inhalation leading to suboptimal lung deposition are commonplace reported in previous studies [9]. In comparison, DPIs are essentially breath-actuated and easier to use correctly than pMDIs, but demand patients to generate a sufficient inspiratory flow to release the powder and break up the powder packets into respirable particles (less than 5 μm in diameter) [10].
Recently, PIFR has been believed as a measure to assess patients' capacity to use DPIs [11]. DPIs approved for treatment of COPD and Asthma include the HandiHaler, Turbuhaler, Aerolizer, Accuhaler/Diskus, Breezhaler, Genuair/Pressair, etc. The recommended technique for patients when using DPIs is ‘a fast and hard inhalation’. Due to the difference in the internal resistance of devices, the level of resistance that the patient needs to overcome when using different DPIs varies. For example, using DPIs with high resistance like Turbuhaler and HandiHaler require more inspiratory effort than using those with low resistance like Breezhaler. Patients using DPIs need to achieve a minimum inhalation rate for the effective clinical response or ideally an optimal rate for the best response. Given previous studies, it is generally considered that PIFR less than 30 L/min is insufficient for the use of DPIs [12]. PIFR of at least 60L/min achieved by patients can bring about optimal drug delivery through DPIs [13]. Unlike DPIs, the technical essential for patients when using pMDI is ‘a slow and deep inhalation’, which requires that the patient's PIFR should be less than 90 L/min [14]. However, observational studies demonstrate that 19% of patients with stable COPD or asthma [15] and 32% to 47% of in-patients prior to discharge after recovering from exacerbation suffered a suboptimal PIFR (less than 60L/min) [16]. Moreover, the PIFRs of 12% of elder Turbuhaler users were even lower than the minimum effective rate (30 L/min) [17]. If patients' inspiratory flow rate does not match DPIs, the insufficient PIFR associating with the dose of inhaled drugs poorly deposited in lung will result in unsatisfied efficacy and potentially poor prognosis [18, 19]. Overall, PIFR is an important consideration for physicians to choose an appropriate inhaler for patients.
Appropriate technique for the usage of inhalers is quite important for the efficacy of inhalation therapy that improper technique is significantly associated with uncontrolled symptoms and increased exacerbation rate [20]. For patients using DPIs and pMDIs, the most critical and common technique errors are inappropriate inspiratory maneuver and poorly synchronized hand actuation with inhalation, respectively [21]. Several reports have revealed that up to 70%-80% of patients made at least 1 inhalation technique error when using DPIs, and 86%-87% of patients when using pMDIs [22, 23]. Especially, patients using Turbuhaler are most likely to make mistakes [24]. Therefore, enhancing patients’ inhaler technique through teaching and training may contribute to improving prognosis and decreasing medical expenditure.
In the current study, we aimed to investigate the PIFRs of patients with COPD or asthma, factors that affect PIFRs and the effect of inhaler technique training on optimizing patients’ PIFRs before inhalation therapy. Through this study, the optimized inhalation therapy based on PIFR should be guided both in selection of the most acceptable inhaler for patients and in training to improve inhaler technique.
Methods
Study design and recruitment
We conducted a prospective, self-control, single-center study at Respiratory Clinic in Zhongshan Hospital of Fudan University, Shanghai, China. All participants have signed an informed consent before being recruited. The study has registered in chictr.org.cn (ChiCTR1900024707) and been approved by the Ethics Committee of Zhongshan Hospital of Fudan University (B2019-142).
This study continuously enrolled patients who were diagnosed as COPD or asthma and prescribed inhalers attending Zhongshan Hospital of Fudan University from June 2020 to September 2020. Patients who were diagnosed with COPD or asthma were required to meet the diagnostic criteria defined by Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease(GOLD) 2019 Report [7] or Global Strategy for Asthma Management and Prevention (GINA 2019 update) [25] respectively, including medical history, symptoms and pulmonary function tests. For every patient enrolled in the study, a clear pulmonary function test result supporting the diagnosis was necessary (for COPD, FEV1/FVC < 0.7 post bronchodilator [7]; for asthma, an increase or decrease in FEV1 of > 12% and 200 ml from baseline, or a change in PEF of at least 20% [25]). Likewise, an exacerbation of asthma represents a change in symptoms and lung function from the patient's usual status in the light of GINA [25], and an exacerbation of COPD is defined as an acute worsening of respiratory symptoms that results in additional therapy in the light of GOLD report [7].
Exclusion criteria include the following: (1) the patient himself/herself did not participate in the consultation; (2) the patient was concomitant with interstitial lung disease, bronchiectasis, pulmonary embolism, and other lung diseases; (3) the patient suffered from cognitive impairment or not cooperating with the study due to poor mental state; (4) the patient did not agree to sign the informed consent.
Data collection
Demographic and clinical characteristics of participants with spirometry-diagnosed COPD or asthma were collected by researchers upon enrollment including gender, age, history of smoking, number of exacerbations in the past year, previous use of inhalation therapy, the severity and control of asthma, and GOLD severity classification (only for COPD patients). Meanwhile, participants were asked to fill out COPD Assessment Test (CAT) (only for patients with COPD) and modified Medical Research Council Dyspnea Scale (mMRC) (for all patients). The following data were also recorded: forced expiratory volume in 1 s (FEV1), FEV1/predicted FEV1 (FEV1%), forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC), peak expiratory flow (PEF), inspiratory capacity (IC), residual volume/total lung capacity (RV/TLC).
The researchers measured PIFR using In-Check® DIAL (Clement Clarke International, Harlow, UK and Alliance Tech Medical). Researches orally taught patients about inhaler techniques and the inhalation maneuver was trained by the device, and PIFR was measured again. All data collection was completed on the day of enrollment.
Peak inhalation flow rate measurement at different resistance
In the study, patients' PIFR was measured by In-Check DIAL®, which is designed to measure inspiratory flow and provides an adjustable dial with different sized openings to simulate resistances of various inhalers. It is accurate up to ± 10% or 10 L/min and is a low-range inspiratory flow metre (15–120 L/min) with options for resistance ranging from high to low. The In-Check DIAL® contains six levels of resistance groups for both pMDIs and DPIs classified as "pMDI"(at resistance of zero), “low” (simulating Breezhaler®), “medium low” (simulating Accuhaler®, Diskhaler®, Ellipta®), “medium” (simulating Spiromax®, GenuAir®, Clickhaler®, Turbohaler®), “medium high” (simulating Turbohaler®, Easyhaler®, Twisthaler®, NEXThaler®), and “high” (simulating Handihaler®, Easyhaler®M). PIFRs for pMDI devices were measured at no resistance and indicated as PIFR0. PIFRs at the resistance of corresponding levels simulating the prescribed DPI inhalers were measured before and after inhaler technique training, which were indicated as before-training PIFR (PIFRBT) and after-training PIFR (PIFRAT), respectively. Specifically, for DPI users, PIFRs at the resistance of prescribed devices were measured for 3 times and the best optimal one was recorded as PIFRBT. Then the patients were trained to use the inhaler (as described in Inhaler technique training by In-Check DIAL® below). After training, the best optimal value of 3 repeated measurements were recorded as PIFRAT..
All PIFR measurements are performed in a separate, private, and quiet consulting room on the day of enrollment. For patients with the exacerbation of asthma or COPD, their PIFRs were measured within 1–3 days of the onset of the exacerbation..
Inhaler technique training by In-Check DIAL®
The In-Check DIAL® can serve as a training device for inhalation muscles and contribute to improving patients’ skills to use inhalers. In this study, a total of 3 researchers participated in inhaler technique training. Before the beginning of the study, we had conducted uniform training and testing for these researchers on educational skills about usage of all types of inhalers and In-Check Dial®. Meanwhile, we had prepared standardized inhaler demonstration videos and manuals for patients. After patients were prescribed different inhalers, the researchers taught and trained their usage technique of respective inhalers. Researcher introduced the characteristics of the inhaler, demonstrated method of application and emphasized technical points to patients in the form of instructional videos and orally. Then patients were asked to train the inhaler technique using In-Check DIAL® with the resistance simulating the corresponding inhaler. Investigators were supposed to correct their technical errors during training until the patients used the inhaler correctly and reached an optimal PIFR as much as possible.
Statistical analysis
Descriptive statistics were used to characterize the demographic and clinical characteristics of patients and the distribution of PIFR in all patients and subgroups (continuous variables including value of PIFR0, PIFRBT and PIFRAT are described as mean ± standard deviation, while categorical variables including the number of patients whose PIFR was less than 30L/min, 30 L/min to 60L/min or greater than 60L/min were described as frequency and percentage). We divided all patients to 2 subgroups in 2 different ways, namely the newly-diagnosed group/follow-up group (ND group/FU group), and the stable group/acute exacerbation group (stable group/AE group). The values of PIFR0, PIFRBT and PIFRAT between subgroups were compared using Mann–Whitney U test or independent-sample t test. The comparison of self-control group (PIFRBT vs. PIFRAT) was performed by paired-samples t test (for the value of PIFR) or McNemar's test (for the categorical variables of PIFR). Due to the range limitation of In-Check Dial®, the PIFR0 we measured did not obey the normal distribution. Considering the related variables analyzed include categorical variables such as sex, the correlation of PIFR0 with lung function index, CAT score and mMRC score were estimated using Spearman rank correlation analysis to ensure the consistency of the results The general significance level was set to 0.05. All statistical analyses were conducted using IBM SPSS Statistics V.22 (IBM Corporation, Armonk, NY, USA).
Results
Demographic characteristics of participants
A total of 209 patients who met all inclusion criteria and with no exclusion items were continuously enrolled at the period of patient recruitment in the study, and none of the invited patients refused to participate. The demographic characteristics of the participants were presented in Table 1 (the patients with both asthma and COPD were categorized into COPD). Among all participants, there were 126 males (60.3%). The average age of all participants was 56.9 ± 17.6(mean ± SD) years, and 93 patients (45.6%) had a history of smoking.
Table 1.
Demographic characteristics of participants
| Asthma (n = 93) | COPD (n = 116) | Total (n = 209) | |
|---|---|---|---|
| Sex, male (%) | 37 (39.8) | 89 (76.7) | 126 (60.3) |
| Age (years) | 44.9 ± 15.4 | 66.6 ± 12.7 | 56.9 ± 17.6 |
| Smoking status (%) | |||
| Yes (including current and former smokers) | 19 (21.1) | 74 (64.9) | 93 (45.6) |
| Current | 14 (15.5) | 27 (23.7) | 41 (20.1) |
| Former | 5 (5.6) | 47 (41.2) | 52 (25.5) |
| Never | 66 (73.3) | 38 (33.3) | 104 (51.0) |
| Secondhand | 5 (5.6) | 2 (1.8) | 7 (3.4) |
Data are shown as means ± standard deviation or number (%) patients
COPD, chronic obstructive pulmonary disease
Clinical characteristics of participants
The clinical characteristics of all participants including 93 patients with asthma and 116 patients with COPD are shown in Table 2. Among all patients, 77 patients were newly diagnosed as COPD or asthma who were prescribed inhalation therapy for the first time (ND group), 132 patients were followed up (FU group); 34 patients with the exacerbation of COPD or asthma and 174 patients with stable COPD or asthma.
Table 2.
Clinical characteristics of participants
| Asthma (n = 93) | COPD (n = 116) | Total (n = 209) | |
|---|---|---|---|
| Stable /AE status | |||
| AE (%) | 10 (10.8) | 24 (20.9) | 34 (16.3) |
| Stable (%) | 83 (89.2) | 91 (79.1) | 174 (83.7) |
| Newly diagnosed/follow-up patients | |||
| Newly-diagnosed (%) | 41 (44.1) | 36 (31.0) | 77 (36.8) |
| Follow-up (%) | 52 (55.9) | 80 (69.0) | 132 (63.2) |
| Number of acute exacerbations in the past year | |||
| 0 (%) | 75 (80.6) | 82 (70.7) | 157 (75.1) |
| 1 (%) | 10 (10.8) | 18 (15.5) | 28 (13.4) |
| 2 (%) | 3 (3.2) | 7 (6.0) | 10 (4.8) |
| ≥ 3 (%) | 5 (5.4) | 9 (7.8) | 14 (6.7) |
| Pulmonary function | |||
| FEV1 (L), mean ± SD | 2.3 ± 0.8 | 1.4 ± 0.6 | 1.8 ± 0.8 |
| FEV1, %predicted, mean ± SD | 81.5 ± 21.4 | 51.7 ± 22.0 | 65.5 ± 26.3 |
| FEV1/FVC, mean ± SD | 74.4 ± 10.9 | 55.7 ± 11.6 | 64.3 ± 14.6 |
| PEF (L), mean ± SD | 5.9 ± 1.9 | 4.0 ± 1.8 | 4.9 ± 2.1 |
| IC (L), mean ± SD | 2.3 ± 0.6 | 2.0 ± 0.7 | 2.1 ± 0.7 |
| RV/TLC, mean ± SD | 43.1 ± 9.0 | 51.0 ± 9.8 | 47.3 ± 10.2 |
| GOLD | |||
| I (%) | / | 12 (14.5) | / |
| II (%) | / | 23 (27.7) | / |
| III (%) | / | 36 (43.4) | / |
| IV (%) | / | 12 (14.5) | / |
| Severity of asthma | |||
| Mild and moderate asthma (%) | 86 (92.5) | / | / |
| Severe asthma (%) | 7 (7.5) | / | / |
| Control of asthma | |||
| Well and partly controlled (%) | 83 (89.2) | / | / |
| Uncontrolled (%) | 10 (10.8) | / | / |
| CAT, mean ± SD | / | 10.5 ± 6.5 | / |
| mMRC, mean ± SD | 0.4 ± 0.7 | 1.2 ± 1.0 | 0.8 ± 0.9 |
Data are shown as means ± standard deviation or number (%) patients
COPD, chronic obstructive pulmonary disease; AE, acute exacerbation; FEV1, forced expiratory volume in 1 s; FEV1%, FEV1/predicted FEV1; FEV1/FVC, forced expiratory volume in 1 s/forced vital capacity; PEF, peak expiratory flow; IC, inspiratory capacity; RV/TLC, residual volume/total lung capacity; GOLD, Global initiative for Chronic Obstructive Lung Disease; CAT, COPD Assessment Test; mMRC, Medical Research Council Dyspnea Scale
Measurements of PIFRs
Table 3 showed the distribution of PIFR in all patients and patients with different clinical conditions. The PIFR in Table 3 includes PIFR0 of all patients, but PIFRBT and PIFRAT only for patients using DPIs. 61 participants (28.9%) have used 2 or more inhalers. The average PIFR0 of all patients was 101.7 ± 24.7L/min, among which the average PIFR0 was 103.0 ± 24.6L/min for patients with asthma and 100.7 ± 24.9L/min for patients with COPD, respectively (p = 0.445, U = 5705.0). The average PIFR0 was 94.2 ± 28.2 L/min for ND group and 106.1 ± 21.4L/min for FU group, respectively (p < 0.001, U = 6522.0); the average PIFR0 was 96.9 ± 26.3L/min for AE group and 102.9 ± 24.3L/min for stable group, respectively (p = 0.143, U = 2517.5).
Table 3.
Distribution of PIFR
| Patients using 2 or more inhalers (%) | Patients using 2 or more DPIs (%) | PIFR0, L/min | PIFRBT, L/min | PIFRAT, L/min | |
|---|---|---|---|---|---|
| All patients | 61 (28.9) | 27 (12.9) | 118.0 (90.0,120.0) | 55.4 ± 21.1 | 61.0 ± 18.8 |
| Asthma/COPD group | |||||
| Asthma group | 14 (15.1) | 5 (5.4) | 120.0 (90.0,120.0) | 56.6 ± 20.6 | 62.9 ± 17.4 |
| COPD group | 47 (40.2) | 22 (18.8) | 115.0 (85.0,120.0) | 54.7 ± 21.5 | 60.0 ± 17.8 |
| P value (MD, 95%CI) | / | / | 0.445 | 0.541 (MD = 1.9, 95% CI [−4.3, 8.1]) | 0.278 ((MD = 3.2, 95% CI [−2.6, 8.9]) |
| ND/FU group | |||||
| ND group | 10 (13.0) | 5 (6.4) | 105.0 (70.0, 120.0) | 47.8 ± 18.0 | 55.9 ± 16.1 |
| FU group | 51 (38.3) | 22 (16.6) | 120.0 (95.0, 120.0) | 60.0 ± 21.6 | 64.0 ± 17.9 |
| p value | / | / | 0.000 | 0.000 (MD = 12.1, 95%CI [6.2,18,1]) | 0.002 (MD = 8.9, 95%CI [3.3,14.5]) |
| AE/stable group | |||||
| AE group | 19 (54.3) | 8 (22.9) | 120.0 (90.0, 120.0) | 51.3 ± 18.5 | 51.8 ± 11.4 |
| Stable group | 42 (24.1) | 19 (10.9) | 110.0 (77.5, 120.0) | 56.5 ± 21.5 | 63.3 ± 17.9 |
| p value | / | / | 0.143 | 0.192 (MD = 5.2, 95% CI [−2.6,13.0]) | 0.000 (MD = 13.0, 95% CI [−5.9, 20.1]) |
Patients using 2 or more inhalers/DPIs are shown as number (%) patients. Data are shown as means ± standard deviation or median (25% quartile, 75%quartile). The PIFR data in Table 3 includes PIFR0 of all patients, and PIFRBT and PIFRAT only for patients using DPIs
CI, confidence interval; COPD, chronic obstructive pulmonary disease; AE, acute exacerbation; ND, newly-diagnosed; FU, follow-up; PIFR0, peak inhalation flow rate measured at resistant of “pMDI”; PIFRBT, peak inhalation flow rate measured before-training; PIFRAT, peak inhalation flow rate measured after training; MD, mean difference
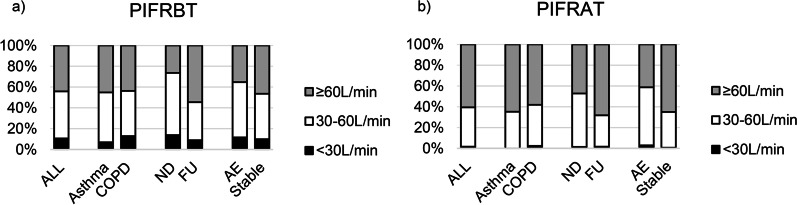
27 participants (12.9%) have used 2 or more DPIs. As shown in Fig. 1, 21 patients (10.8%) had a PIFRBT less than 30 L/min, and 86 patients (44.1%) had a PIFRBT greater than or equal to 60 L/min before technique training. 13.9%/26.4% newly-diagnosed patients had a PIFRBT < 30 L/min/ ≥ 60 L/min; as contrasted, 8.9%/54.5% follow-up patients had a PIFRBT < 30 L/min/ ≥ 60 L/min. Relatively, scarcely patient (only 3 patients, 1.5%) had a PIFRAT less than 30 L/min, and a rather high 118 patients (60.5%) had a PIFRAT greater than or equal to 60 L/min after technique training. The group of AE contained a total of 34 patients, consisting of 10 patients with asthma and 24 with COPD. We did not find a significant difference in PIFRBT (p = 0.350, 95% CI [−5.7.22.4]) or in PIFRAT (p = 0.784, 95% CI [−7.0, 11.7]) between the patients with asthma exacerbation and COPD exacerbation. Additionally, PIFRAT of the AE group was significantly lower than that of the stable group (p < 0.001, MD = 13.0, 95% CI [−5.9, 20.1]). Even after training, 58.8% of AE patients still failed to achieve optimal PIFR.
Fig. 1.
Percentage of different PIFRBT and PIFRAT. Figure is percent stacked column charts of the PIFR distribution for patients using DPIs before and after technique training. a There were 21 (10.8%) patients with a PIFRBT < 30L/min and 86 (44.1%) patients with a PIFRBT ≥ 60L/min among all patients. The population and proportions of patients with a PIFRBT < 30L/min in ND/FU group were 10 (13.9%)/11(8.9%). The population and proportions of patients with a PIFRBT ≥ 60L/min in ND/FU group were 19 (26.4%)/67 (54.5%). b There were 3 (1.5%) patients with a PIFRAT < 30L/min and 118 (60.5%) patients with a PIFRAT ≥ 60L/min among all patients. COPD, chronic obstructive pulmonary disease; AE, acute exacerbation; ND, newly-diagnosed; FU, follow-up; PIFRBT, peak inhalation flow rate measured before-training; PIFRAT, peak inhalation flow rate measured after training
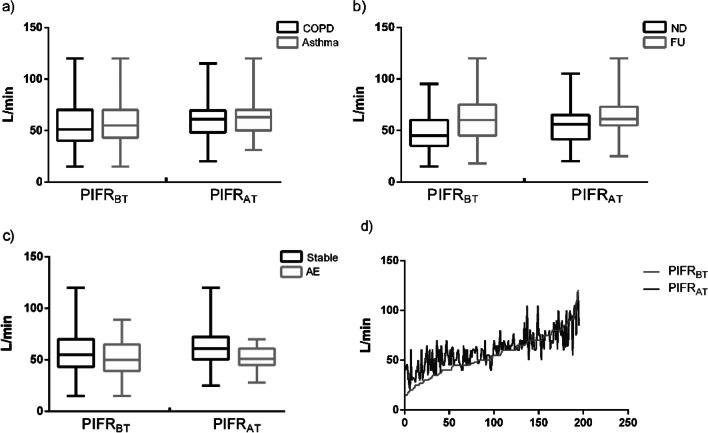
Optimal PIFRs rates improved after technique training
In a total of 209 subjects, 166 (79.4%) subjects were using DPIs. Figure 2 showed the distribution and training-associated changes of PIFRs in patients of different clinical conditions using DPIs. The average PIFRBT and PIFRAT in all patients was 55.4 ± 21.1 L/min and 61.0 ± 18.8 L/min respectively (see Table 3) (p < 0.001, MD = 5.2, 95% CI [3.8, 7.4]). The similar increased PIFRs after training were found in patients with both COPD and asthma, new-diagnosed and follow-up patients (p all < 0.001, COPD group: MD = 5.3, 95% CI [3.0, 7.6]; Asthma group: MD = 6.3, 95% CI [3.2, 9.3]; ND group: MD = 8.2, 95% CI [5.8, 10.5]; FU group: MD = 4.1, 95% CI [1.6, 6.67]). However, the patients' PIFRAT showed a significant improvement over PIFRBT in Stable group but there was no significant difference between PIFRAT and PIFRBT in AE group (Stable group: p < 0.001, MD = 6.8, 95% CI [4.8, 8.8]; AE group: p = 0.822, MD = 0.5, 95% CI [−3.8 ,4.7]). Meanwhile, McNemar's test demonstrated that the percentages of patients reaching minimum PIFR (30 L/min) and optimal PIFR (60 L/min) after technique training were both significantly improved (p < 0.001, χ2 = 16.1, 25.3). Furthermore, the similar improvement in the percentages of patients reaching minimum PIFR and optimal PIFR after training were found in patients with both COPD and asthma, new-diagnosed and follow-up patients (p all < 0.005, except for p value of improvement in minimum PIFR achieving by patients with asthma was 0.063). It should be noted that the significant improvement in PIFRs after training was not found in AE group, either in asthma exacerbators (p = 0.250, χ2 = 1.3) or COPD exacerbators (p = 0.625, χ2 = 0.3).
Fig. 2.
Distribution and variation trend of PIFR in COPD/Asthma group, ND/FU group, AE/Stable group and all patients. Figure describes the distribution and changes of PIFRBT and PIFRAT for patients using DPIs in COPD/Asthma group, ND/FU group, AE/Stable group and all patients. a is a box diagram showing the improvement from PIFRBT to PIFRAT in COPD/Asthma group. b is a box diagram showing the improvement from PIFRBT to PIFRAT in ND/FU group. c is a box diagram showing the improvement from PIFRBT to PIFRAT in AE/Stable group. d is a line chart for PIFRBT and PIFRAT in all patients, which the two values corresponding to each abscissa value are PIFRBT and PIFRAT of the same patient. When the patient's PIFR was relatively low, training increases the PIFR value more obviously. COPD, chronic obstructive pulmonary disease; AE, acute exacerbation; ND, newly-diagnosed; FU, follow-up; PIFRBT, peak inhalation flow rate measured before-training; PIFRAT, peak inhalation flow rate measured after training
In our study, 13(16.3%) of the patients who used pMDIs (N = 80) had a PIFR greater than 90 L/min before training, among them 7 (46.2%) were COPD patients and 6 (53.8%) were asthmatic patients. Most of them 12 (92.3%) had stable diseases. Compared with subjects with PIFR less than 90L/min, they had similar lung function (FEV1%: 59.7 ± 30.7 vs 58.8 ± 27.2, p = 0.925, 95% CI [−20.1, 18.3]) and symptoms (mMRC: 0.8 ± 1.2 vs 1.2 ± 1.0, p = 0.225, 95% CI [−0.3, 1.1]). Although training has improved the patients’ inhaler technique of pMDI to some extent, but it was not statistically significant (p = 0.065, χ2 = 3.3). It is worth noting that there were still 7.5% subjects using pMDIs with a PIFR greater than 90L/min after training.
Clinical factors that effect PIFRs
As shown in Table 4, Spearman test demonstrated that PIFR0 was not significantly relative to sex, BMI (body mass index), FEV1%, FEV1/FVC, RV/TLC and CAT score, but was weakly relative to FEV1, PEF, IC, and mMRC score. Among them, PIFR0 was positively correlated with FEV1, PEF, and IC (p values are 0.013, 0.008, 0.001, and r values are 0.199, 0.218, and 0.284, respectively). On the contrary, PIFR0 showed a negative correlation with mMRC score (p = 0.005, r = -0.200).
Table 4.
Relativity between PIFR0 and clinical indicators
| Clinical indicators | p value | R (95% CI) |
|---|---|---|
| Sex | 0.061 | −0.130 (−0.261, 0.016) |
| BMI | 0.312 | 0.071 (−0.076, 0.248) |
| FEV1 | 0.013* | 0.199 (0.072, 0.351) |
| FEV1, %predicted | 0.900 | −0.010 (−0.172, 0.149) |
| FEV1/FVC | 0.948 | 0.005 (−0.149, 0.169) |
| PEF | 0.008* | 0.218 (0.097, 0.356) |
| IC | 0.001* | 0.284 (0.097, 0.422) |
| RV/TLC | 0.255 | −0.098 (−0.296, 0.084) |
| CAT | 0.632 | −0.047 (−0.230, 0.162) |
| mMRC | 0.005* | −0.200 (−0.346, −0.044) |
Except for FEV1 (%predicted), which is the percentage of predicted value, the other pulmonary function parameters are absolute values
r, Spearman rank correlation coefficient; BMI, body mass index; FEV1, forced expiratory volume in 1 s; FEV1%, FEV1/predicted FEV1; FEV1/FVC, forced expiratory volume in 1 s/forced vital capacity; PEF, peak expiratory flow; IC, inspiratory capacity; RV/TLC, residual volume/total lung capacity; CAT, COPD Assessment Test; mMRC, Medical Research Council Dyspnea Scale.
*p value < 0.05
Discussion
Different inhalers have different requirements for the patient's inspiratory flow rate and technique [26]. Although the types of inhalers available to doctors and patients are increasing day by day, there are still many patients whose PIFR does not match the requirements of the inhaler or the inhaler technique is not qualified, resulting in suboptimal efficacy of inhalation therapy [27, 28]. In this prospective, self-control, single-center study, the number of patients with very severe COPD (GOLD IV, defined as FEV1% < 30%) is relatively small (12 patients, 14.5%) since the patients we enrolled were all outpatients. Though after training, 39.5% of patients were not yet able to achieve the optimal PIFR (60L/min), which showed that there were still quite a few patients with a suboptimal inspiratory flow rate even in patients with mild, moderate or severe COPD (GOLD I–III).
In this study, in addition to routine instructional video and oral guidance by physicians, we additionally emphasized the application of In-Check DIAL® in technique training. Our study has shown that 10.8% of patients using DPI could not achieve the minimum PIFR (30L/min) and 55.9% of patients could not achieve the optimal PIFR (60L/min) before technical training. After training, almost no patients had a PIFR less than 30L/min, and the number of patients who did not reach the optimal flow rate was significantly reduced, which revealed that technique training helped to significantly increased both the value of PIFR and the proportion of patients that reached the minimum and optimal flow rate. Our attempt to train patients with In-Check DIAL® truly contributed to improving PIFR of patients with COPD or asthma. Moreover, the improvement of PIFR in COPD patients before and after training was more significant than that of asthmatic patients. Therefore, we considered that COPD patients need more training, probably because asthma patients were younger and stronger in learning ability than COPD patients.
We have investigated the distribution of PIFRs in patients with different clinical conditions in this study. By comparing PIFR (including PIFR0, PIFRAT and PIFRBT) in new-diagnosed (indicating no effective treatment had ever be used) vs. follow-up patients and patients in exacerbation vs. stable stage, we found that PIFR of ND/FU group or AE/Stable group showed a significant difference. It meant that compared with follow-up patients, newly-diagnosed patients who were given inhalation therapy for the first time benefited more from inhaler technique training in improving the ability of using DPIs; and compared with AE patients, patients in the stable phase benefited more in improving PIFR.
From the distribution of PIFRAT and PIFRBT, it is not difficult to find that among all the groups before teaching, ND group had the largest proportion of PIFRBT less than 30 L/min (13.9%) and the smallest proportion of PIFRBT greater than or equal to 60 L/min (26.4%), but FU group had the largest proportion of PIFRBT greater than or equal to 60 L/min (54.5%). These data suggest that newly diagnosed patients should strengthen knowledge education and inhaler technique training, and pMDIs may be prescribed for some patients with suboptimal PIFR (DPIs can be prescribed after improvement).
Among all the groups after teaching, AE group had the least proportion of PIFRAT greater than or equal to 60 L/min (41.2%), which is significantly lower than that of the stable group (68.3%). In the AE group, the improvement in PIFR before and after training (P > 0.050) did not reach statistical significance, indicating that many AE patients had poor inhalation ability and the benefits of training for AE patients were limited. It can be found that when the influence of technical factors on PIFR is excluded, AE patients had a higher suboptimal rate and a worse ability to use DPIs than stable patients, but physicians kept giving DPIs to them (AE patients used 1.00 DPIs per capita). Previous researches have shown similar conclusions that acute exacerbations were associated with decrease in PIFR [27, 29]. For example, Palen et al. found that 50% of patients with an exacerbation of asthma or COPD were unable to generate optimal PIFR using Turbuhaler (compared with 5% of those without AE) [30]. All these data have proved that more AE patients were suitable to be prescribed SMIs or pMDIs rather than DPIs.
According to the study by Duarte et al., lung function measurements demonstrated a significant lower FEV1, total lung capacity (TLC), inspiratory capacity (IC) and a significant greater RV/TLC in the suboptimal PIFR group compared to the optimal PIFR group [31]. By contrast, Ghosh et al. demonstrated that the only factor found to be consistently associated with a lower PIFR was female gender, but there was a lack of consistent correlation between PIFR and FEV1 or FEV1% predicted or FVC or CAT score [26, 32]. In fact, the factors affecting PIFR are still controversial. In this study, we found a weak positive correlation between PIFR of outpatients with FEV1, PEF and IC (r = 0.199, 0.218, and 0.284), and a weak negative correlation with mMRC score (r = -0.200). However, our attempt to construct a qualified prediction model for PIFR based on these factors was a failure. At this stage, it is still necessary to measure PIFR by In-Check DIAL® to guide inhaler choice.
In addition, a slow and deep inhalation is required when using pMDIs, and a PIFR greater than 90L/min is considered too fast. Some studies have proven the necessity to educate patients regarding correct pMDI technique [33, 34]. Our results showed that training reduced the PIFR value of patients, but it was not statistically significant, which implied that technique training had potential impact for patients to use pMDIs correctly in the aspect of optimal PIFR.
Conclusions
In general, a considerable number of outpatients with COPD or asthma were not able to achieve the optimal PIFRs for using DPIs. Inhaler education including training using In-Check DIAL® played an important role in improving patients’ PIFRs and we recommend that all patients who are prescribed inhalers should have their abilities evaluated and techniques trained. PIFR was associated with patients’ FEV1, PEF, IC and mMRC, but the correlation was not strong enough to indicate optimal PIFR to use specific DPIs. Besides, patients with AECOPD or asthma attack generally had suboptimal PIFRs and should be prescribed DPIs with caution.
Acknowledgements
This study was supported by the National Natural Science Foundation of China under Grant (No.81970035) and National Innovative Research Team of High-level Local Universities in Shanghai.
Abbreviations
- COPD
Chronic obstructive pulmonary disease
- AE
Acute exacerbation
- BMI
Body mass index
- FEV1
Forced expiratory volume in 1 s
- FEV1%
FEV1/predicted FEV1
- FEV1/FVC
Forced expiratory volume in 1 s/forced vital capacity
- PEF
Peak expiratory flow
- IC
Inspiratory capacity
- RV/TLC
Residual volume/total lung capacity
- CAT
COPD Assessment Test
- mMRC
Medical Research Council Dyspnea Scale
- ND
Newly-diagnosed
- FU
Follow-up
- PIFR0
Peak inhalation flow rate measured at resistant of “pMDI”
- PIFRBT
Peak inhalation flow rate measured before-training
- PIFRAT
Peak inhalation flow rate measured after training
Authors' contributions
JH, CD, NX, JZ, ML, XY and JZ contributed substantially to the study design, acquisition of data and data analysis. JH, XY and JZ took part in drafting the article or revising it critically for important intellectual content. JH analyzed and interpreted the data, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China under Grant (No.81970035).
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to policy requirements but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study has been approved by the Ethics Committee of Zhongshan Hospital of Fudan University (B2019-142) and is registered in the Chinese Clinical Trial Registry (No. ChiCTR1900024707). All methods were carried out in accordance with the principles in the Declaration of Helsinki. Written informed consent was obtained from the patients or their relatives.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
The authors Jian-lan Hua and Xiao-fen Ye contributed to the manuscript equally.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. doi: 10.1016/S0140-6736(18)30841-9. [DOI] [PubMed] [Google Scholar]
- 2.Zhong N, Wang C, Yao W, Chen P, Kang J, Huang S, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–760. doi: 10.1164/rccm.200612-1749OC. [DOI] [PubMed] [Google Scholar]
- 3.Fang X, Wang X, Bai C. COPD in China: the burden and importance of proper management. Chest. 2011;139(4):920–929. doi: 10.1378/chest.10-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu B, Wang Y, Ming J, Chen W, Zhang L. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis. 2018;13:1353–1364. doi: 10.2147/COPD.S161555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet. 2019;394(10196):407–418. doi: 10.1016/S0140-6736(19)31147-X. [DOI] [PubMed] [Google Scholar]
- 6.Brusselle GG, Ko FW-S. Prevalence and burden of asthma in China: time to act. The Lancet. 2019;394(10196):364–6. [DOI] [PubMed]
- 7.Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Lung Disease 2019 Report. https://goldcopd.org/gold-reports/. [DOI] [PubMed]
- 8.Newman SP. Principles of metered-dose inhaler design. Respir Care. 2005;50(9):1177–1190. [PubMed] [Google Scholar]
- 9.Crompton GK. Problems patients have using pressurized aerosol inhalers. Eur J Respir Dis Suppl. 1982;119:101–104. [PubMed] [Google Scholar]
- 10.Atkins PJ. Dry powder inhalers: an overview. Respiratory care. 2005;50(10):1304–12; discussion 12. [PubMed]
- 11.Newman SP. Drug delivery to the lungs from dry powder inhalers. Curr Opin Pulm Med. 2003;9(Suppl 1):S17–20. doi: 10.1097/00063198-200304001-00005. [DOI] [PubMed] [Google Scholar]
- 12.Nielsen KG, Auk IL, Bojsen K, Ifversen M, Klug B, Bisgaard H. Clinical effect of Diskus dry-powder inhaler at low and high inspiratory flow-rates in asthmatic children. Eur Respir J. 1998;11(2):350–354. doi: 10.1183/09031936.98.11020350. [DOI] [PubMed] [Google Scholar]
- 13.Engel T, Heinig JH, Madsen F, Nikander K. Peak inspiratory flow and inspiratory vital capacity of patients with asthma measured with and without a new dry-powder inhaler device (Turbuhaler) Eur Respir J. 1990;3(9):1037–1041. [PubMed] [Google Scholar]
- 14.Pauwels R, Newman S, Borgström L. Airway deposition and airway effects of antiasthma drugs delivered from metered-dose inhalers. Eur Respir J. 1997;10(9):2127–2138. doi: 10.1183/09031936.97.10092127. [DOI] [PubMed] [Google Scholar]
- 15.Kawamatawong T, Khiawwan S, Pornsuriyasak P. Peak inspiratory flow rate measurement by using In-Check DIAL® for the different inhaler devices in elderly with obstructive airway diseases. J Asthma Allergy. 2017;10:17–21. doi: 10.2147/JAA.S127580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahler DA. Peak inspiratory flow rate as a criterion for dry powder inhaler use in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2017;14(7):1103–1107. doi: 10.1513/AnnalsATS.201702-156PS. [DOI] [PubMed] [Google Scholar]
- 17.Janssens W, VandenBrande P, Hardeman E, De Langhe E, Philps T, Troosters T, et al. Inspiratory flow rates at different levels of resistance in elderly COPD patients. Eur Respir J. 2008;31(1):78–83. doi: 10.1183/09031936.00024807. [DOI] [PubMed] [Google Scholar]
- 18.Mahler DA, Waterman LA, Ward J, Gifford AH. Comparison of dry powder versus nebulized beta-agonist in patients with COPD who have suboptimal peak inspiratory flow rate. J Aerosol Med Pulm Drug Deliv. 2014;27(2):103–109. doi: 10.1089/jamp.2013.1038. [DOI] [PubMed] [Google Scholar]
- 19.Al-Showair RA, Tarsin WY, Assi KH, Pearson SB, Chrystyn H. Can all patients with COPD use the correct inhalation flow with all inhalers and does training help? Respir Med. 2007;101(11):2395–2401. doi: 10.1016/j.rmed.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 20.Usmani OS, Lavorini F, Marshall J, Dunlop WCN, Heron L, Farrington E, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10. doi: 10.1186/s12931-017-0710-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Molimard M, Raherison C, Lignot S, Balestra A, Lamarque S, Chartier A, et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49(2). [DOI] [PubMed]
- 22.Price DB, Román-Rodríguez M, McQueen RB, Bosnic-Anticevich S, Carter V, Gruffydd-Jones K, et al. Inhaler errors in the CRITIKAL Study: type, frequency, and association with asthma outcomes. J Allergy Clin Immunol Pract. 2017;5(4):1071–81.e9. doi: 10.1016/j.jaip.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Cho-Reyes S, Celli BR, Dembek C, Yeh K, Navaie M. Inhalation technique errors with metered-dose inhalers among patients with obstructive lung diseases: a systematic review and meta-analysis of U.S. studies. Chronic Obstr Pulm Dis. 2019;6(3):267–80. [DOI] [PMC free article] [PubMed]
- 24.Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Global Strategy for Asthma Management and Prevention (2019 update). https://ginasthma.org/gina-reports/.
- 26.Ghosh S, Ohar JA, Drummond MB. Peak inspiratory flow rate in chronic obstructive pulmonary disease: implications for dry powder inhalers. J Aerosol Med Pulm Drug Deliv. 2017;30(6):381–387. doi: 10.1089/jamp.2017.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loh CH, Peters SP, Lovings TM, Ohar JA. Suboptimal inspiratory flow rates are associated with chronic obstructive pulmonary disease and all-cause readmissions. Ann Am Thorac Soc. 2017;14(8):1305–1311. doi: 10.1513/AnnalsATS.201611-903OC. [DOI] [PubMed] [Google Scholar]
- 28.Sharma G, Mahler DA, Mayorga VM, Deering KL, Harshaw O, Ganapathy V. Prevalence of low peak inspiratory flow rate at discharge in patients hospitalized for COPD exacerbation. Chronic Obstr Pulm Dis. 2017;4(3):217–224. doi: 10.15326/jcopdf.4.3.2017.0183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Broeders ME, Molema J, Hop WC, Vermue NA, Folgering HT. The course of inhalation profiles during an exacerbation of obstructive lung disease. Respir Med. 2004;98(12):1173–1179. doi: 10.1016/j.rmed.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 30.van der Palen J. Peak inspiratory flow through diskus and turbuhaler, measured by means of a peak inspiratory flow meter (In-Check DIAL) Respir Med. 2003;97(3):285–289. doi: 10.1053/rmed.2003.1289. [DOI] [PubMed] [Google Scholar]
- 31.Duarte AG, Tung L, Zhang W, Hsu ES, Kuo YF, Sharma G. Spirometry measurement of peak inspiratory flow identifies suboptimal use of dry powder inhalers in ambulatory patients with COPD. Chronic Obstr Pulm Dis. 2019;6(3):246–255. doi: 10.15326/jcopdf.6.3.2018.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghosh S, Pleasants RA, Ohar JA, Donohue JF, Drummond MB. Prevalence and factors associated with suboptimal peak inspiratory flow rates in COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:585–595. doi: 10.2147/COPD.S195438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Worafi YM. Evaluation of inhaler technique among patients with asthma and COPD in Yemen. Journal of Taibah University Medical Sciences. 2018;13(5):488–490. doi: 10.1016/j.jtumed.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elgendy MO, Hassan AH, Saeed H, Abdelrahim ME, Eldin RS. Asthmatic children and MDI verbal inhalation technique counseling. Pulmonary Pharmacol Therap. 2020;61:101900. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to policy requirements but are available from the corresponding author on reasonable request.