Abstract
K. pneumoniae (KPN) is one of the widest spread bacteria in which combined resistance to several antimicrobial groups is frequent. The most common β-lactamases found in K. pneumoniae are class A carbapenemases, both chromosomal-encoded (i.e., NMCA, IMI-1) and plasmid-encoded (i.e., GES-enzymes, IMI-2), VIM, IMP, NDM, OXA-48, and extended-spectrum β-lactamases (ESBLs) such as CTX-M enzymes. In the present study, a total of 68 carbapenem-resistant KPN were collected from twelve long-term care facilities (LTCFs) in the Northern Italian region. The whole-genome sequencing (WGS) of each KPN strain was determined using a MiSeq Illumina sequencing platform and analysed by a bacterial analysis pipeline (BAP) tool. The WGS analysis showed the prevalence of ST307, ST512, and ST37 as major lineages diffused among the twelve LTCFs. The other lineages found were: ST11, ST16, ST35, ST253, ST273, ST321, ST416, ST1519, ST2623, and ST3227. The blaKPC-2, blaKPC-3, blaKPC-9, blaSHV-11, blaSHV-28, blaCTX-M-15, blaOXA-1, blaOXA-9, blaOXA-23, qnrS1, qnrB19, qnrB66, aac(6′)-Ib-cr, and fosA were the resistance genes widespread in most LTCFs. In this study, we demonstrated the spreading of thirteen KPN lineages among the LTCFs. Additionally, KPC carbapenemases are the most widespread β-lactamase.
Keywords: Klebsiella pneumoniae, WGS, β-lactamases
1. Introduction
β-lactams are the most widely prescribed antibiotics, used to treat a wide range of bacterial infections worldwide [1]. Since their introduction in clinical practice, resistance to β-lactams has progressively increased. Gram-negative bacteria resistance to β-lactams involves several factors such as (i) active efflux modification, (ii) decreased outer membrane permeability, (iii) mutations altering PBPs expression or function, and (iv) β-lactamases production, which remains the main mechanism of resistance employed by bacteria [2,3]. β-lactamases are usually divided into four classes, considering the Ambler classification: class A (TEM, SHV, ESBLs, and KPC); class B (MBL, NDM, VIM, and IMP); class C (Amp-C); and class D (OXA). Particularly widespread are the extended spectrum β-lactamases (ESBLs), against which the antibiotic class of carbapenems maintains their activity. However, carbapenemases, β-lactamases capable of hydrolysing even carbapenems, have emerged since 1982 in the Serratia marcescens clinical isolate (SME-1 carbapenemase) [4]. To date, serine- and metallo-carbapenemases are widely spread, especially among Enterobacterales [5]. The data from the European Antimicrobial Resistance Surveillance Network (EARS-Net) displayed that carbapenemase-producing Enterobacterales (CPE) are responsible for the majority of human infections [6]. Among Enterobacterales, Klebsiella pneumoniae, one of the most widely spread bacteria, is listed by the World Health Organization (WHO) as one of the worrisome pathogens in which combined resistance to several antimicrobials (β-lactams, quinolones, and aminoglycosides) is very frequent [7,8]. K. pneumoniae represents an important reservoir for class A (KPC, SHV, GES, IMI, and NMCA), class B (i.e., VIM, IMP, and NDM), class D carbapenemases (OXA-48), and extended-spectrum β-lactamases (ESBLs) such as CTX-M variants [5,9]. Carbapenem-resistant K. pneumoniae is largely disseminated around the world [10,11,12,13,14]. One reason for the rapid dissemination of K. pneumoniae is the presence of antibiotic resistance genes in mobile genetic elements and the Inc-groups, which belong to plasmids IncF, IncFII(K1), IncR, IncX, IncX3, IncI2, and ColE1 [15,16,17,18,19]. However, carbapenem-resistant K. pneumoniae strains are not only confined to healthcare settings, but also to the community and among residents of LTCFs [20,21,22,23,24]. In Italy, the carbapenem-resistant Enterobacterales from LTCFs have been reported since 2010 in different endemic areas [25,26,27,28]. The aim of the present study was to investigate the dissemination of antibiotic resistance genes in K. pneumoniae isolated from rectal swabs of residents in the LTCFs of the Veneto Region (Northern Italy). The molecular analysis of the WGS of these strains was performed by next-generation sequencing (NGS).
2. Materials and Methods
2.1. Setting
Between July 2018 and June 2019, we conducted a point-prevalence survey among the residents of 27 LTCFs in the Veneto Region, Northern Italy. Participation was on a voluntary basis. The study-specific data were collected on a single day for each LTCF involved; in the LTCFs with a high number of beds, data collection was spread over two or more consecutive days. However, all the beds in one ward were surveyed on the same day. The surveys were not conducted simultaneously in all 27 LTCFs, but at different periods for each facility in accordance with the availability of both the local staff to collaborate with researchers in the collection of clinical data and study-specific biological samples, and of the reference microbiology laboratory to accept samples and perform analysis.
Only subjects housed in the facility for at least 48 h were asked for consent to participate. A total of 118 variables, such as hospitalization and surgery during the previous year, antibiotics within the last three months, and the presence of medical devices (i.e., urinary catheter; peripheral vascular catheter; central venous catheter; nasogastric tube; and percutaneous endoscopic gastrostomy) were collected from each enrolled participant. Additionally, the enteric carriage of ESBL and carbapenemase-producing Gram-negative bacteria was assessed collecting a rectal swab from every enrolled resident.
2.2. Strains Selection
The rectal swabs were collected and inoculated onto ChromID ESBL agar (bioMerieux, Marcy l’Etoile, France) with an Ertapenem disk (10 μg) and on Mac Conkey agar with a Meropenem disk (10 μg). The plates were incubated at 35 ± 2 °C under aerobic conditions for 24 h. The isolates were identified at the species level using an automated Vitek2 System (bioMerieux, Marcy l’Etoile, France). Resistance to carbapenems were interpreted according to the EUCAST criteria and confirmed with an immunochromatographic lateral flow assay Carba5 (NG Biotech, Guipry, France). A Vitek2 system (version 9.02, bioMérieux, Marcy l’Etoile, France) was used to confirm carbapenem resistance and to perform antimicrobial susceptibilities for other substances.
2.3. DNA Extraction and Whole-Genome Sequencing (WGS)
Total nucleic acid was extracted using a MagMAX Microbiome Ultra Nucleic Acid Isolation kit (Applied Biosystems and ThermoFisher Scientific, Monza, Italy). The DNA concentrations were measured using a Qubit fluorometer (ThermoFisher Scientific) to determine DNA input. The genomic libraries were prepared using a Swift 2S Turbo DNA Library kit (Swift Biosciences, Ann Arbor, MI, USA) and the WGS was performed on an Illumina MiSeq platform using v3 reagent kits generating 2 × 300 bp paired-end reads (Illumina, San Diego, CA, USA).
2.4. Bioinformatic Analysis
Raw data from the paired-end sequencing were quality checked with the FastQC tool (v.0.11.6, BaseSpaceLabs, Illumina, San Diego, CA, USA) and assembled with Velvet (v.1.2.10, BaseSpaceLabs, Illumina, San Diego, CA, USA) [29]. Velvet is incorporated as an assembler in a multiple-tool workflow, the CGE Bacterial Analysis Pipeline (BAP) (BaseSpaceApps, Illumina, San Diego, CA, USA). The BAP application predicts the species of bacterial input genomes using a k-mer-based approach [30]. These acquired antimicrobial resistance genes were identified using a BLAST-based approach, where the nucleotide sequence of the input genome was compared to the genes in the ResFinder database [31]. Multilocus sequence typing (MLST) was performed also using a BLAST-based approach [32]. BLAST was used to search for plasmid replicons using the PlasmidFinder database [33]. Identified plasmids of the IncF, IncH1, IncH2, IncI1, IncN, or IncA/C type were subtyped by plasmid MLST [33]. KmerFinder, ResFinder, and PlasmidFinder databases were synchronized with databases from the Center for Genomic Epidemiology (http://www.genomicepidemiology.org/) on 2 June 2017. MLST and pMLST data were downloaded from pubmlst.org on 17 May 2017.
3. Results
In total, 1933 rectal swabs in 2890 residents were performed. Overall, of 159 K. pneumoniae (KPN), isolated on a selective medium, only 68 of them were selected for this study for their carbapenem resistance profile. As shown in Table 1, all strains were resistant to at least two different class of antibiotics. Indeed, they exhibited a high resistance profile to β-lactams/β-lactamase inhibitors (amoxicillin-clavulanic acid and piperacillin-tazobactam), oxyiminocephalosporins (cefotaxime and ceftazidime), carbapenems (meropenem and ertapenem), and ciprofloxacin. Of 68 KPN, 36 (52.9%) were resistant to trimethoprim-sulfamethoxazole, respectively. All strains, analysed by Vitek2 system, were susceptible to colistin.
Table 1.
Antimicrobial susceptibility of 68 K. pneumoniae isolated from rectal swabs.
| LTCFs | No. Isolates | ST | Resistance Profile |
|---|---|---|---|
| CDS_RO | 15 | 307, 2623 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP |
| POCS_VR | 2 | 16 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| 2 | 35 | AMX, TZP, CTX, CAZ, CIP, MEM, SXT | |
| 3 | 512 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP | |
| POVSG_VR | 2 | 512 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP |
| IPABMC_VI | 2 | 253, 1519 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| CAR_VI | 2 | 512, 1519 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| IPABRS_VI | 11 | 37 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| IPABRT_VI | 5 | 512 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| IPABSC_VI | 3 | 416 | AMX, TZP, CTX, CAZ, MEM, CIP, SXT |
| SSA_BL | 5 | 321 | AMX, TZP, CTX, CAZ, MEM, CIP, SXT |
| ISRAA_TV | 7 | 307 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| CRMC_VE | 5 | 11, 273 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
| SAF_VE | 4 | 307 | AMX, TZP, CTX, CAZ, ERT, MEM, CIP, SXT |
AMX, Amoxicillin-clavulanic acid; TZP, piperacillin-tazobactam; CTX, cefotaxime; CAZ, ceftazidime; ERT, ertapenem; MEM, meropenem; CIP, ciprofloxacin; SXT, trimethoprim-sulfamethoxazole. ST, sub type.
For legal aspects, we used only the acronym of the twelve LTCFs.
3.1. WGS of K. pneumoniae
Whole-genome sequencing was carried out on 68 KPN isolates, and bioinformatic analysis was performed with a BAP tool that gave information about genome size, MLST, plasmid replicons, pMLST, and antimicrobial resistance genes. The genome size of the 68 KPN ranged from 5.1 to 5.74 Mb.
3.2. K. pneumoniae MLST
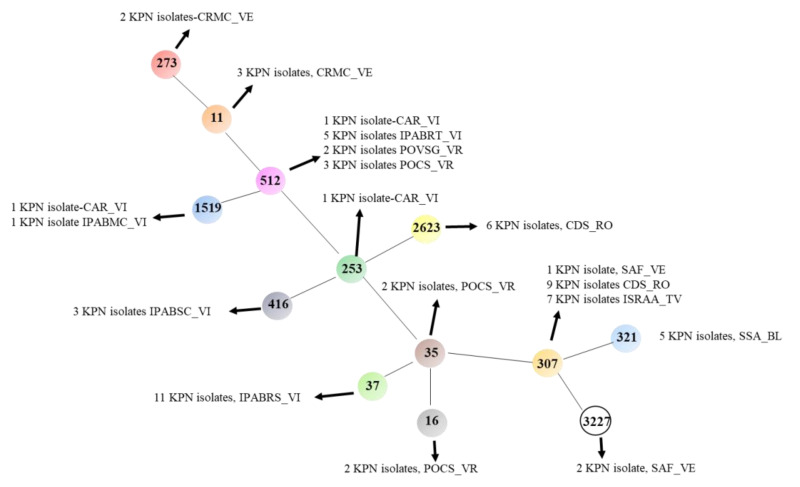
The MLST analysis showed the presence of thirteen KPN lineages: ST11, ST16, ST35, ST37, ST253, ST273, ST307, ST321, ST416, ST512, ST1519, ST2623, and ST3227. The most widespread STs were ST307 (17 isolates), ST512 (11 isolates), and ST37 (11 isolates). The ST307, ST512, and ST37 were identified in four, three, and one LTCFs, respectively. The remaining STs were endemic of only one LTCF (Figure 1, Table 2).
Figure 1.
Phylogenetic tree of K. pneumoniae strains selected for MLST. The minimum spanning tree was obtained using PHYLOViZ online software (http://www.phyloviz.net/). For legal aspects, we used only the acronym of the twelve LTCFs.
Table 2.
Genome analysis of K. pneumoniae isolated from residents of twelve LTCFs (Northern Italy).
| LTCFs | No. Isolates | Genome Size (bp) | MLST | Plasmid Replicons/pMLST | β-lactams Resistance Genes | Other Antibiotics Resistance Genes |
|---|---|---|---|---|---|---|
| SSA_BL | 5 | 5,736,085 | ST321 | IncFII(K), IncFIB(K), IncFIA(HI1), IncN/fii_k1 fia_19 |
blaVIM-1, blaSHV-99 |
aadA1, aph(3′)-XV, aacA4, fosA, mph(A), aac(6′)Ib-cr,oqxA, oqxB, qnrS1, sul1 dfrA14, catB2 |
| ISRAA_TV | 2 | 5,497,503 | ST307 | IncFIB(K), IncFII(K)/fii_k7 |
blaSHV-28, blaKPC-2, blaOXA-9, blaTEM-1A, blaCTX-M-15 |
fosA, dfrA14, qnrB66 |
| 2 | 5,164,710 | ST307 | IncFIB(K), IncFII(K)/fii_k7 | blaKPC-2, blaTEM-1A, blaOXA-9, blaCTX-M-15, blaSHV-28, blaOXA-1 | aac(6′)-Ib-cr, fosA, dfrA14, qnrB66, catB4 | |
| 2 | 5,578,258 | ST307 | IncFIB(K), IncFII(K)/fii_k7 | blaKPC-2, blaTEM-1A, blaOXA-9, blaCTX-M-15, blaSHV-28, blaOXA-1 | aac(6′)-Ib-cr, fosA, dfrA14, qnrB66, catB4, oqxA, oqxB | |
| 1 | 5,505,674 | ST307 | IncFIB(K), IncFII(K)/fii_k7 | blaKPC-2, blaTEM-1A, blaOXA-9, blaCTX-M-15, blaSHV-28, blaOXA-1 | aac(6′)-Ib-cr, fosA, dfrA14, catB4, oqxA, oqxB | |
| SAF_VE | 1 | 5,545,376 | ST307 | IncFIB(K), IncFII(K)/fii_k7 | blaKPC-2, blaTEM-1A, blaOXA-9, blaCTX-M-15, blaSHV-28, blaOXA-1 | aac(6′)-Ib-cr, fosA, dfrA14, qnrB66, catB4, oqxA, oqxB |
| 1 | 5,330,546 | ST3227 | IncFIB(pQil), IncFIB(K)/fii_k7 | blaKPC-9, blaTEM-1B, blaOXA-9, blaLEN-12, blaCTX-M-15, blaOXA-1 | aph(3′)-IIa, aac(6′)-Ib-cr, fosA, strA, strB, sul2, dfrA14, qnrB66, catB4 | |
| 1 | 5,545,568 | ST3227 | IncFIB(pQil), IncFII(K), IncFIB(K)/fii_k9 | blaOXA-9, blaTEM-1A, blaKPC-3, blaLEN-12, blaLEN-7, blaOXA-1 | aac(6′)-Ib-cr, aph(3′)-IIa, fosA, dfrA14, oqxB, qnrB66, catB4 | |
| 1 | 5,540,988 | ST307 | IncFII(K), IncFIB(K), IncR, IncL/M (pOXA-48)/fii_k5 | blaTEM-1A, blaSHV-11 | aph(3′)-Ia, fosA, qnrB19, oqxB | |
| CRMC_VE | 3 | 5,531,831 | ST11 | IncFII(pKPX1), ColpVC, Col(MG828)/fii_k7 | blaSHV-11, blaCTX-M-15, blaNDM-1 | aac(6′)-Ib-cr, fosA, oqxB, oqxA |
| 2 | 5,387,384 | ST273 | IncFII(K), IncFIB(K), Col(MG828)/fii_k7 | blaSHV-11, blaTEM-1B, blaOXA-1, blaCTX-M-15 | aac(3′)-IIa, aac(6′)-Ib-cr, strA, strB, fosA, sul2, dfrA14, oqxA, oqxB, catB4 | |
| CDS_RO | 3 | 5,424,562 | ST2623 | IncFII(K), IncFIB(K), IncFIA(HI1), ColRNAI/fii_k1 fia_10 |
blaCTX-M-15, blaSHV-1, blaTEM-1B, blaOXA-1 |
aac(6′)-Ib-cr, strA, strB, sul2 oqxA, oqxB, qnrB66, tet(D), catB4 |
| 3 | 5,666,417 | ST 2623 | IncFIB(pQil), IncFII(K), IncFIB(K), IncFIA(HI1), ColRNAI/fii_k1 fia_10 |
blaCTX-M-15, blaOXA-9, blaTEM-1B, blaOXA-1, blaKPC-3 | aac(6′)-Ib-cr, fosA, strA, strB, sul2, oqxA, oqxB, qnrB66, tet(D), catB4 | |
| 2 | 5,607,404 | ST307 | IncFIB(pQil), IncFII(K), IncFIA(HI1)/fii_k2 fia_19 |
blaTEM-1A, blaOXA-9, blaSHV-28, blaCTX-M-15, blaOXA-1, blaKPC-3 | aac(6′)-Ib-cr, strA, strB, fosA, sul2, oqxA, oqxB, qnrB66, catB4 | |
| 37 | 5,496,232 | ST307 | IncFIB(pQil), IncFII(K)/fii_k2 | blaCTX-M-15, blaTEM-1A, blaOXA-9, blaSHV-28, blaOXA-1, blaKPC-3 | aac(6′)-Ib-cr, fosA, sul2, oqxA, oqxB, qnrB66, catB4 | |
| 2 | 5,566,824 | ST307 | IncFIB(pQil), IncFII(K), IncFIA(HI1)/fii_k2 fia_19 |
blaCTX-M-15, blaTEM-1A, blaOXA-9, blaSHV-28, blaOXA-1, blaKPC-3 |
aac(6′)-Ib-cr, strA, strB, fosA, sul2, oqxA, oqxB qnrB66, catB4 |
|
| 2 | 5,634,072 | ST307 | IncFIB(pQil), IncFII(K), IncFIB(K)/fii_k2 | blaCTX-M-15, blaTEM-1A, blaOXA-9, blaSHV-28, blaOXA-1, blaKPC-3 | aac(6′)-Ib-cr, aac(3)-IIa, strA, strB, fosA, sul2, dfrA14, oqxA, oqxB, qnrB66, catB4 | |
| CAR_VI | 1 | 5,649,046 | ST512 | IncX3, IncFIB(K), IncFIB(pQil) IncFII(K)/fii_k2 | blaKPC-3, blaTEM-1A, blaOXA-9, blaSHV-11 | aadA2, aph(3′)-Ia, fosA, mph(A), sul1, dfrA12, oqxA, oqxB, catA1 |
| 1 | 5,487,176 | ST1519 | ColRNAI, IncFIB(pQil), IncFII(K)/fii_k2 |
blaKPC-3, blaOXA-9, blaSHV-11, blaTEM-1A | aadA2, aac(6′)-Ib-cr, fosA, sul1, oqxA, oqxB | |
| IPABMC_VI | 1 | 5,311,196 | ST1519 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K)/fii_k2 | blaSHV-11, blaKPC-3 | aac(6′)-Ib-cr, aadA2, fosA, mph(A), sul1, dfrA12, oqxB, catA1 |
| 1 | 5,651,358 | ST253 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K), IncN/ fii_k5/ST7 |
blaVIM-1, blaSHV-36 | aac(6′)-Ib-cr, aadA1, aacA4, fosA, sul1, dfrA14, qnrS1, catB2 | |
| IPABRS_VI | 2 | 5,167,604 | ST37 | ColRNAI, IncFII(K), IncFIB(K)/fii_k7 | blaCTX-M-15, blaSHV-11, blaOXA-1, blaTEM-1B | aac(6′)-Ib-cr, strA, strB, fosA, sul2, dfrA14, oqxA, oqxB, catB4 |
| 4 | 5,451,323 | ST37 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K), IncN/ fii_k7 |
blaSHV-11, blaOXA-1, blaKPC-2 | aac(6′)-Ib-cr, fosA, dfrA14, dfrA30, oqxB, oqxA, catB4 | |
| 3 | 5,424,901 | ST37 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K), IncN/ IncF: fii_k7 IncN: unknown |
blaSHV-11, blaOXA-1, blaKPC-2 |
aac(6′)-Ib-cr, fosA, dfrA30, dfrA14, oqxA, oqxB, catB4 | |
| 2 | 5,444,858 | ST37 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K), IncN/ IncF: fii_k7 |
blaSHV-11, blaOXA-1, blaKPC-2 |
aac(6′)-Ib-cr, fosA, dfrA30, dfrA14, oqxA, oqxB, catB4 | |
| IPABRT_VI | 5 | 5,406,932 | ST512 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K)/fii_k2 |
blaLEN-12, blaTEM-1A, blaKPC-3, blaOXA-9 |
aac(6′)-Ib-cr, aadA1, fosA, sul1, dfrA1, oqxB, tet(D) |
| IPABSC_VI | 1 | 5,634,812 | ST416 | IncFII(K), IncFIA(HI1), ColRNAI, IncN, IncFIB(K)/ IncF: fii_k4, fia_18 IncN: ST7 |
blaVIM-1, blaSHV-14 | aadA1, aph(3′)-XV, aacA4, fosA, sul1, dfrA14, oqxA, oqxB, qnrS1, catB2 |
| 2 | 5,477,368 | ST416 | IncFII(K), IncFIB(Mar), ColRNAI, IncN, IncFIB(K)/ IncF: fii_k5 IncN: ST7 |
blaVIM-1, blaOKP-B-3 | aadA1, aph(3′)-XV, aacA4, aac(6′)-Ib-cr, fosA, sul1, qnrS1, catB2, oqxB, oqxA | |
| POVSG_VR | 1 | 5,346,528 | ST512 | ColRNAI, IncFIB(K)/fii_k2 | blaLEN-7, blaOXA-9, blaTEM-1A | aph(3′)-IIa, aadA2, aac(6′)-Ib-cr, fosA, sul1 |
| 1 | 5,101,877 | ST512 | ColRNAI, IncFIB(pQil), IncFII(K), IncFIB(K)/fii_k2 |
blaKPC-9, blaOXA-9, blaTEM-1A |
aph(3′)-IIa, aadA2, aac(6′)-Ib-cr, fosA, sul1 | |
| POCS_VR | 1 | 5,548,552 | ST512 | IncFIB(pQil), IncFII(K), IncFIB(K), ColRNAI, IncX3/ fii_k2 |
blaOXA-9, blaSHV-11, blaTEM-1A, blaKPC-3 |
aadA2, aac(6′)-Ib-cr, mph(A), sul1, dfrA12, oqxB, oqxA, catA1 |
| 2 | 5,589,508 | ST512 | IncFII(K), IncFIA(HI1), ColRNAI, IncFIB(K), Col(MG828), FIA(pBK30683)/fii_k12 fia_10 |
blaOXA-23, blaLEN-12, blaCTX-M-15, blaOXA-1 |
aac(3)-IIa, aac(6′)-Ib-cr, aadA1, fosA, sul1, dfrA1, oqxB, qnrB6, tet(D), tet(B), catB4, catA1 | |
| 2 | 5,604,773 | ST16 | IncFIB(pQil), IncFII(K), IncFIB(K), IncX4/fii_k2 |
blaKPC-3, blaCTX-M-15, blaTEM-1B, blaSHV-1, blaOXA-1 |
strA, aac(6′)-Ib-cr, strB, fosA, sul2, dfrA14, oqxB, oqxA, qnrB66, tet(A), catB4 | |
| 2 | 5,589,102 | ST35 | IncFIB(pQil), IncFII(K), IncFIB(K)/fii_k2 |
blaTEM-1A, blaOXA-9, blaKPC-3, blaSHV-33 |
fosA, oqxB, oqxA |
For legal aspects, we only used the acronym of the twelve LTCFs.
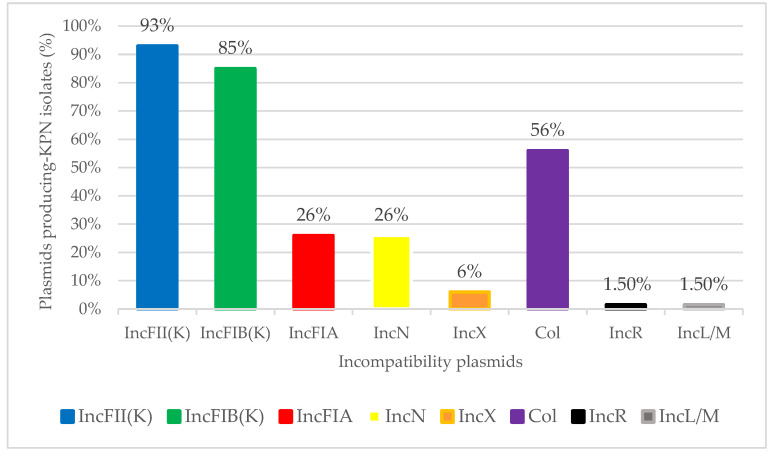
3.3. Plasmids Replicons and pMLST
Incompatibility plasmids IncFII(K), IncFIB(K), IncFIA(HI1), IncN, IncF, IncFIB (pQil), IncL/M, IncX3, IncX4, Col (MG828), ColpVC, and ColRNAI were detected in all KPN analysed (Figure 2). Overall, IncF was the predominant plasmid found in 100% of the KPN, followed by Col (38 out of 68 KPN), IncN (18 out of 68 KPN), IncX (4 out of 68 KPN), IncR (1 out of 68 KPN), and IncL/M (1 out of 68 KPN) type plasmids. Among IncF plasmids, the predominant was IncFII(K) (found in 63 out of 68 KPN), followed by IncFIB(K) (found in 52 out of 68 KPN), and IncFIA (found in 18 out of 68 KPN). Regarding pMLST, the major plasmid lineage was fiik7 (25 KPN isolates), followed by fiik1 (11 isolates), fia19 (9 isolates), fia10 (8 isolates), fiik5 (4 isolates), fiik2 (2 isolates), fiik4 (1 isolate), fiik9 (1 isolate), and fia18 (1 isolate). In most KPNs, the simultaneous presence of more than one plasmid was found.
Figure 2.
Distribution of incompatibility plasmids found in 68 K. pneumoniae isolated from residents of twelve LTCFs (Northern Italy).
3.4. β-Lactam Resistance Genes
The β-lactam resistance genes were found in all KPNs with a moderate variability among the LTCFs (Table 2). The prototype genes blaTEM-1A/blaTEM-1B were found in 65% of KPN isolates, whereas the blaSHV variants (blaSHV-1, blaSHV-11, blaSHV-14, blaSHV-28, blaSHV-33, blaSHV-36, and blaSHV-99) were found in 76% of KPN strains (52 out of 68) isolated in the twelve LTCFs with a prevalence of blaSHV-11 (31% of isolates), followed by blaSHV-28 (25% of isolates) (Table 3). blaKPC-2 and blaKPC-3 were found in 47 out of 68 isolates (69%) collected in 9 to 12 LTCFs. blaKPC-2 was retrieved in 17 isolates belonging to ST37 and ST307, whereas blaKPC-3 was found in 30 KPNs belonging to seven different ST lineages (Table 3). blaKPC-9 was found in two KPN isolates (ST512 and ST3227 lineages) collected from two different LTCFs. The OXA variants were the predominant β-lactamase found in 93% of KPNs (63 out of 68 isolates). In detail, OXA-1, OXA-9, and OXA-1/OXA-9 associations were found in 20, 13, and 20 KPN isolates, respectively. blaOXA-23 was identified in two ST512 isolated from two residents of the same LTCF. The blaLEN-7 and blaLEN-12 genes were found in 11 KPN isolates (ST512 and ST3227 lineages) in four of the LTCFs. blaCTX-M-15 was found in 35 out of 68 KPNs, belonging to eight different lineages (Table 3). The metallo-β-lactamases, VIM-1 and NDM-1, were detected in nine and three KPN isolates, respectively. The three NDM-1-producing KPNs were identified only in one LTCF. The blaOXA-23 gene was found in two ST512 isolates in combination with blaCTX-M-15, blaOXA-1, and blaLEN-12.
Table 3.
Distribution of β-lactamases among K. pneumoniae isolated from residents of 12 LTCFs (Northern Italy).
| β-lactamases | Classes | Isolates No. (%) | ST |
|---|---|---|---|
| TEM-1 | A | 44 (65) | 16, 35, 37, 273, 307, 512, 1519, 2623, 3227 |
| KPC-2 | A | 17 (25) | 37, 307 |
| KPC-3 | A | 30 (44) | 16, 35, 307, 512, 1519, 2623, 3227 |
| KPC-9 | A | 2 (3) | 512, 3227 |
| SHV-1 | A | 5 (7) | 16, 2623 |
| SHV-11 | A | 21 (31) | 11, 37, 273, 307, 512, 1519 |
| SHV-14 | A | 1 (1.5) | 416 |
| SHV-28 | A | 17 (25) | 307 |
| SHV-33 | A | 2 (3) | 35 |
| SHV-36 | A | 1 (1.5) | 253 |
| SHV-99 | A | 5 (7) | 321 |
| CTX-M-15 | A | 35 (51) | 11, 16, 37, 273, 307, 512, 2623, 3227 |
| LEN-7 | A | 2 (3) | 512, 3227 |
| LEN-12 | A | 9 (13) | 512, 3227 |
| OKP-B3 | A | 2 (3) | 416 |
| VIM-1 | B | 9 (13) | 253, 321, 416 |
| NDM-1 | B | 3 (4.5) | 11 |
| OXA-1 | D | 40 (59) | 16, 37, 273, 307, 512, 2623, 3227 |
| OXA-9 | D | 33 (48) | 35, 307, 512, 1519, 2623, 3227 |
| OXA-23 | D | 2 (3) | 512 |
3.5. Fluoroquinolone Resistance Genes
Plasmid-mediated resistance to fluoroquinolones was identified in all KPNs. Different plasmid-mediated mechanisms were implicated in quinolone resistance: (i) aac(6′)Ib-cr in 100% of KPNs, (ii) qnr elements in 58% of KPNs, and (iii) oqxAB multidrug efflux pump was detected in 53 KPN isolates disseminated in ten LTCFs. Among the qnr elements, the major qnr found were qnrB66 (in 26 out of 68 KPNs), followed by qnrS1 (9 out of 68 KPNs), qnrB6 (one isolate), and qnrB19 (one isolate).
3.6. Other Antimicrobial Resistance Genes
Several molecular mechanisms of sulfamethoxazole/trimethoprim resistance have been described in the literature; however, the most common mechanism is the acquisition of dihydrofolate reductase dfr. Indeed, 54 out of 68 strains that were analyzed showed the presence of dfrA12, dfrA14, and dfrA30. In detail, 4 KPNs showed dfrA12, 39 KPNs showed dfrA14, and 11 KPNs presented both dfrA14 and dfrA30. Resistance to aminoglycosides was mediated by aadA1, aadA2, aph(3′)-XV, aacA4, aph(3′)-Ia, and aph(3′)-IIa, and by the bi-functional gene aac(6′)Ib-cr, which confers resistance to both fluoroquinolones and aminoglycosides. Other antibiotic resistance genes detected in KPN were the following: mphA (macrolide resistance) detected in 8 KPNs; sul1 and sul2 (sulfonamide resistance) detected in 22 and 20 KPNs, respectively; catA1, catB2, and catB4 (chloramphenicol resistance) detected in 50 KPNs; strA and strB (streptomycin resistance) detected in 23 KPNs; tet(A), tet(B), and tet(D) (tetracycline resistance) detected in 13 KPNs; and fosA gene (fosfomycin resistance) detected in 61 KPNs.
4. Discussion
Carbapenem-resistant K. pneumoniae is designated by the Centres for Disease Control and Prevention (CDC) as one of the microorganisms that poses an urgent threat to public health worldwide. K. pneumoniae can spread rapidly in healthcare settings, and it is responsible for numerous human infections such as urinary, respiratory, and bloodstream infections [34,35]. In Italy, an epidemic spread of K. pneumoniae ST258, as a major contributor of carbapenem-resistant Enterobacterales, has been observed since 2010 [36,37]. In parallel, even though most infections still occur in nosocomial settings, K. pneumoniae emerged as a cause of severe community-acquired infections. The present study investigated the genome of carbapenem-resistant KPN in twelve LTCFs in a Northern Italy region. Among the 68 carbapenem-resistant KPNs, the most widespread clones were represented by ST307 and ST512. In ISRAA_TV LTCF, the ST307 was the unique lineage found, and it harbors the same plasmids but different resistance genes. K. pneumoniae ST307 has been reported from many countries, and it has been responsible for several global nosocomial [38,39] and long-term care center outbreaks [40,41]. Whole-genome sequencing performed by Wyres et al. on 95 K. pneumoniae ST307 revealed the presence of FIB-like plasmids harbouring the blaCTX-M-15 gene adjacent to the ISECp1 element such as the other ST307 isolated in different geographical areas [38,42]. The ST307 harbouring blaCTX-M-15 in association with aac(6′)-Ib-cr and qnrB6 genes, as well as in our strains, was also described in an Italian regional survey (Sicily, Southern Italy) [27].
In the present study, K. pneumoniae ST512, found in four LTCFs, harboured KPC-3 and KPC-9, CTX-M-15, SHV-11, OXA-9, OXA-23, and LEN-12 β-lactamases. The carbapenem-resistant K. pneumoniae ST512 has been considered the predominant lineage in isolates, causing severe bloodstream infections in a Northern Italian hospital [43]. For a long time, Italy has been an endemic country for K. pneumoniae ST258/ST512 lineages [36,37,43,44,45], but recently, other STs emerged [46]. The K. pneumoniae ST37 was the third most spread lineage (11 isolates) but it was detected only in one LTCF (IPABRS_VI). A determination of the correlation between this evidence and the presence of specific risk factors in the reference population is underway. The ST37 has been described in several papers as an ertapenem-resistant K. pneumoniae with a modified outer membrane permeability [47,48].
A wide variety of plasmids were found in each whole KPN genome. The IncF plasmids were predominant in the KPN analysed in this study. This plasmid family is widely diffused in clinically relevant Enterobacterales, especially IncFII(K), which is considered a virulent plasmid because of its ability to co-exist with other plasmids in a single cell [49,50]. Most of these plasmids are conjugative and this facilitates the dissemination of resistance genes among different strains and species. This is the case of IncFIA(pBK30683 plasmid found in ST512 (POCS_VR LTCF), co-harbouring blaOXA-23, blaOXA-1, blaCTX-M-15, and blaLEN-12. The OXA-23 class D carbapenemase is normally produced by A. baumannii, and it is very rare in K. pneumoniae [51,52]. However, pBK30683 is a plasmid of 139,941 bp that seems to originate from the cointegration of pBK30661 (belonging to IncFIA family plasmids) with a 68 Kb genetic element, harbouring a complete set of genes for plasmid replication, stability, and conjugation [53]. This could explain the “jump” of blaOXA-23 from one species to another.
Class A, B, and D β-lactamases were identified in all the KPN strains. The major carbapenemases were the KPC variants (KPC-2, KPC-3, and KPC-9), VIM-1, NDM-1 metallo-β-lactamases, and OXA-23. KPC-9 is a KPC-3 variant with a V239A substitution. CTX-M-15 is the most common ESBL in K. pneumoniae. In our strains, CTX-M-15 was identified in eight different ST lineages (11, 16, 37, 273, 307, 512, 2623, and 3227). The blaCTX-M-15 gene is often flanked by a sequence insertion (IS) such as ISEcp1, which facilitates its mobility. The β-lactamases LEN and OKP-B are chromosomally encoded and are frequently found in K. pneumoniae as well as the oxacillinases (OXA-1 and OXA-9).
5. Conclusions
This study found that the LTCFs represent an important incubator for class A, B, and D carbapenemases, ESBLs, and other antibiotic resistance genes, reflecting the local hospital trends. In many cases, the total dependence of residents on nurse care for their daily living activities exposes them to both the selection and horizontal transmission of antibiotic-resistant organisms. It is important for LTCFs to develop effective control measures to prevent outbreaks of antibiotic-resistant strains.
Acknowledgments
The authors thanks Giuseppe Cornaglia for having strongly supported this study with his scientific enthusiasm. Thanks to the LTCF Veneto working group, composed of Giorgia Be, Nicola Salerno, Lorenza Lambertenghi, Ilaria Coledan (Infectious Disease Section, Department of Diagnostic and Public Health, University of Verona, Italy) for the collection of biological samples.
Author Contributions
Conceptualization, A.P. and M.P.; methodology, A.M.A., A.P., S.C., L.M., A.B. and L.N.; investigation, A.P., S.C. and A.M.A.; data curation, M.P., G.L.C. and A.M.A.; writing—original draft preparation, M.P. and A.M.A.; writing—review and editing, M.P., A.P., G.L.C. and A.M.A.; visualization, E.T.; supervision, M.P., G.A. and E.T.; project administration, A.P., G.L.C. and A.M.A.; funding acquisition, A.M.A., G.A. and M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Regione Veneto, DGR 1656; 17/10/2017 and University of L’Aquila internal funds.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bush K., Bradford P.A. β-Lactams and β-lactamase inhibitors: An overview. Cold Spring Harb. Perspect. Med. 2016;6:a025247. doi: 10.1101/cshperspect.a025247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.King D.T., Sobhanifar S., Strynadka N. The mechanisms of resistance to β-lactam antibiotics. In: Gotte M., Berghuis A., editors. Handbook of Antimicrobial Resistance. Springer; New York, NY, USA: 2014. pp. 1–22. [Google Scholar]
- 3.Bush K., Bradford P.A. Epidemiology of β-Lactamase-Producing Pathogens. Clin. Microbiol. Rev. 2020;33:e00047-19. doi: 10.1128/CMR.00047-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naas T., Vandel L., Sougakoff W., Livermore D.M., Nordmann P. Cloning and sequence analysis of the gene for a carbapenem-hydrolyzing class A beta-lactamase, Sme-1, from Serratia marcescens S6. Antimicrob. Agents Chemother. 1994;38:1262–1270. doi: 10.1128/AAC.38.6.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bush K. Past and Present Perspectives on β-Lactamases. Antimicrob. Agents Chemother. 2018;62:e01076-18. doi: 10.1128/AAC.01076-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Centre for Disease Prevention and Control . Antimicrobial Resistance in the EU/EEA (EARS-Net)-Annual Epidemiological Report 2019. ECDC; Stockholm, Sweden: 2020. [Google Scholar]
- 7.World Health Organization Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. 2017. [(accessed on 25 February 2017)]. Available online: https://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf.
- 8.David S., Reuter S., Harris S.R., Glasner C., Feltwell T., Argimon S., Abudahab K., Goater R., Giani T., Errico G., et al. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat. Microbiol. 2019;4:1919–1929. doi: 10.1038/s41564-019-0492-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Queenan A.M., Bush K. Carbapenemases: The versatile β-Lactamases. Clin. Microbiol. Rev. 2007;20:440–458. doi: 10.1128/CMR.00001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madni O., Amoako D.G., Abia A.L.K., Rout J., Essack S.Y. Genomic investigation of carbapenem-resistant Klebsiella pneumoniae colonization in an intensive care unit in South Africa. Genes. 2021;12:951. doi: 10.3390/genes12070951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhan Q., Xu Y., Wang B., Yu J., Shen X., Liu L., Cao X., Guo Y., Yu F. Distribution of fluoroquinolone resistance determinants in carbapenem-resistant Klebsiella pneumoniae clinical isolates associated with bloodstream infections in China. BMC Microbiol. 2021;21:164. doi: 10.1186/s12866-021-02238-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed M.A.E.E., Yang Y., Yang Y., Yan B., Chen G., Hassan R.M., Zhong L.L., Chen Y., Roberts A.P., Wu Y., et al. Emergence of iypervirulent carbapenem-resistant Klebsiella pneumoniae coharboring a bla(NDM-1)-carrying virulent plasmid and a blaKPC-2)-carrying plasmid in an Egyptian Hospital. mSphere. 2021;6:e00088-21. doi: 10.1128/mSphere.00088-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barbarini D., Russello G., Brovarone F., Capatti C., Colla R., Perilli M., Moro M.L., Carretto E. Evaluation of carbapenem-resistant Enterobacteriaceae in an Italian setting: Report from the trench. Infect. Genet. Evol. 2015;30:8–14. doi: 10.1016/j.meegid.2014.11.025. [DOI] [PubMed] [Google Scholar]
- 14.Brescini L., Morroni G., Valeriani C., Castelletti S., Mingoia M., Simoni S., Masucci A., Montalti R., Vivarelli M., Giacometti A., et al. Clinical and epidemiological characteristics of KPC-producing Klebsiella pneumoniae from bloodstream infections in a tertiary referral center in Italy. BMC Infect. Dis. 2019;19:611. doi: 10.1186/s12879-019-4268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin J., Phan H.T.T., Findlay J., Stoesser N., Pankhurst L., Navickaite I., De Maio N., Eyre D.W., Toogood G., Orsi N.M., et al. Covert dissemination of carbapenemase-producing Klebsiella pneumoniae (KPC) in a successfully controlled outbreak: Long- and short-read whole-genome sequencing demonstrate multiple genetic modes of transmission. J. Antimicrob. Chemother. 2017;72:3025–3034. doi: 10.1093/jac/dkx264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naas T., Cuzon G., Villegas M.V., Lartigue M.F., Quinn J.P., Nordmann P. Genetic structures at the origin of acquisition of the β-lactamase blaKPC gene. Antimicrob. Agents. Chemother. 2008;52:1257–1263. doi: 10.1128/AAC.01451-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia-Fernandez S., Villa L., Carta C., Venditti C., Giordano A., Venditti M., Mancini C., Carattoli A. Klebsiella pneumoniae ST258 producing KPC-3 identified in Italy carries novel plasmids and OmpK36/OmpK35 porin variants. Antimicrob. Agents. Chemother. 2012;56:2143–2145. doi: 10.1128/AAC.05308-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen L., Chavda K.D., Melano R.G., Jacobs M.R., Levi M.H., Bonomo R.A., Kreiswirth B.N. Complete sequence of a bla(KPC-2)-harboring IncFII(K1) plasmid from a Klebsiella pneumoniae sequence type 258 strain, Antimicrob. Agents. Chemother. 2013; 57, 1542–1545. Agents. Chemother. 2013;57:1542–1545. doi: 10.1128/AAC.02332-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cerdeira L.T., Cunha M.P.V., Francisco G.R., Bueno M.F.C., Araujo B.F., Ribas R.M., Gontijo-Filho P.P., Knöbl T., de Oliveira Garcia D., Lincopan N. IncX3 plasmid harboring a non-Tn4401 genetic element (NTEKPC) in a hospital-associated clone of KPC-2-producing Klebsiella pneumoniae ST340/CG258. Diagn. Microbiol. Infect. Dis. 2017;89:164–167. doi: 10.1016/j.diagmicrobio.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Endimiani A., Depasquale J.M., Forero S., Perez F., Hujer A.M., Roberts-Pollack D., Fiorella P.D., Pickens N., Kitchel B., Casiano-Colón A.E., et al. Emergence of blaKPC-containing Klebsiella pneumoniae in a long-term acute care hospital: A new challenge to our healthcare system. J. Antimicrob. Chemother. 2009;64:1102–1110. doi: 10.1093/jac/dkp327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ben-David D., Masarwa S., Navon-Venezia S., Mishali H., Fridental I., Rubinovitch B., Smollan G., Carmeli Y., Schwaber M.J., Israel PACF CRKP (Post-Acute-Care Facility Carbapenem-Resistant Klebsiella pneumoniae) Working Group Carbapenem-resistant Klebsiella pneumonia in post-acute-care facilities in Israel. Infect. Control Hosp. Epidemiol. 2011;32:845–853. doi: 10.1086/661279. [DOI] [PubMed] [Google Scholar]
- 22.Giani T., Antonelli A., Caltagirone M., Mauri C., Nicchi J., Arena F., Nucleo E., Bracco S., Pantosti A., AMCLI-CoSA survey participants et al. Evolving β-lactamase epidemiology in Enterobacteriaceae from Italian nationwide surveillance, October 2013: KPC-carbapenemase spreading among outpatients. Euro. Surveill. 2017;22:30583. doi: 10.2807/1560-7917.ES.2017.22.31.30583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen H.Y., Jean S.S., Lee Y.L., Lu M.C., Ko W.C., Liu P.Y., Hsueh P.R. Carbapenem-Resistant Enterobacterales in Long-Term Care Facilities: A Global and Narrative Review. Front. Cell Infect. Microbiol. 2021;11:601968. doi: 10.3389/fcimb.2021.601968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lapp Z., Crawford R., Miles-Jay A., Pirani A., Trick W.E., Weinstein R.A., Hayden M.K., Snitkin E.S., Lin M.Y. Regional spread of blaNDM-1-containing Klebsiella pneumoniae ST147 in post-acute care facilities. Clin. Infect. Dis. 2021:ciab457. doi: 10.1093/cid/ciab457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ambretti S., Bassetti M., Clerici P., Petrosillo N., Tumietto F., Viale P., Rossolini G.M. Screening for carriage of carbapenem-resistant Enterobacteriaceae in settings of high endemicity: A position paper from an Italian working group on CRE infections. Antimicrob. Resist. Infect. Control. 2019;8:136. doi: 10.1186/s13756-019-0591-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arena F., Vannetti F., Di Pilato V., Fabbri L., Colavecchio O.L., Giani T., Marraccini C., Pupillo R., Macchi C., Converti F., et al. Diversity of the epidemiology of carbapenemase-producing Enterobacteriaceae in long-term acute care rehabilitation settings from an area of hyperendemicity, and evaluation of an intervention bundle. J. Hosp. Infect. 2018;100:29–34. doi: 10.1016/j.jhin.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 27.Bonura C., Giuffre M., Aleo A., Fasciana T., Di Bernardo F., Stampone T., Giammanco A., Palma D.M., Mammina C., MDR-GN Working Group An update of the evolving epidemic of blaKPC carrying Klebsiella pneumoniae in Sicily, Italy, 2014: Emergence of multiple non-ST258 clones. PLoS ONE. 2015;10:e0132936. doi: 10.1371/journal.pone.0132936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arena F., Di Pilato V., Vannetti F., Fabbri L., Antonelli A., Coppi M., Pupillo R., Macchi C., Rossolini G.M. Population structure of KPC carbapenemase-producing Klebsiella pneumoniae in a long-term acute-care rehabilitation facility: Identification of a new lineage of clonal group 101, associated with local hyperendemicity. Microb. Genom. 2020;6:e000308. doi: 10.1099/mgen.0.000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zerbino D.R. Using the Velvet de novo assembler for short-read sequencing technologies. Curr. Protoc. Bioinformatics. 2010;11:11.5.1–11.5.12. doi: 10.1002/0471250953.bi1105s31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Larsen M.V., Cosentino S., Lukjancenko O., Saputra D., Rasmussen S., Hasman H., Sicheritz-Pontén T., Aarestrup F.M., Ussery D.W., Lund O. Benchmarking of methods for genomic taxonomy. J. Clin. Microbiol. 2014;52:1529–1539. doi: 10.1128/JCM.02981-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zankari E., Hasman H., Cosentino S., Vestergaard M., Rasmussen S., Lund O., Aarestrup F.M., Larsen M.V. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 2012;67:2640–2644. doi: 10.1093/jac/dks261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Larsen M.V., Cosentino S., Rasmussen S., Friis C., Hasman H., Marvig R.L., Jelsbak L., Sicheritz-Pontén T., Ussery D.W., Aarestrup F.M., et al. Multilocus sequence typing of total-genome-sequenced bacteria. J. Clin. Microbiol. 2012;50:1355–1361. doi: 10.1128/JCM.06094-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carattoli A., Zankari E., García-Fernández A., Voldby Larsen M., Lund O., Villa L., Møller Aarestrup F., Hasman H. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob. Agents. Chemother. 2014;58:3895–3903. doi: 10.1128/AAC.02412-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang Y., Yang Y., Chen G., Lin M., Chen Y., He R., Galvão K.N., El-Gawad El-Sayed Ahmed M.A., Roberts A.P., Wu Y., et al. Molecular characterization of carbapenem-resistant and virulent plasmids in Klebsiella pneumoniae from patients with bloodstream infections in China. Emerg. Microbes. Infect. 2021;10:700–709. doi: 10.1080/22221751.2021.1906163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magi G., Tontarelli F., Caucci S., Sante L.D., Brenciani A., Morroni G., Giovanetti E., Menzo S., Mingoia M. High prevalence of carbapenem-resistant Klebsiella pneumoniae ST307 recovered from fecal samples in an Italian hospital. Future Microbiol. 2021;16:703–711. doi: 10.2217/fmb-2020-0246. [DOI] [PubMed] [Google Scholar]
- 36.Giani T., Pini B., Arena F., Conte V., Bracco S., Migliavacca R., AMCLI-CRE Survey Participants. Pantosti A., Pagani L., Luzzaro F., et al. Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: Results of the first countrywide survey, 15 May to 30 June 2011. Euro. Surveill. 2013;18:20489. doi: 10.2807/ese.18.22.20489-en. [DOI] [PubMed] [Google Scholar]
- 37.Conte V., Monaco M., Giani T., D’Ancona F., Moro M.L., Arena F., D’Andrea M.M., Rossolini G.M., Pantosti A., AR-ISS Study Group on Carbapenemase-Producing K. pneumonia Molecular epidemiology of KPC-producing Klebsiella pneumoniae from invasive infections in Italy: Increasing diversity with predominance of the ST512 clade II sublineage. J. Antimicrob. Chemother. 2016;71:3386–3391. doi: 10.1093/jac/dkw337. [DOI] [PubMed] [Google Scholar]
- 38.Peirano G., Chen L., Kreiswirth B.N., Pitout J.D.D. Emerging Antimicrobial-Resistant High-Risk Klebsiella pneumoniae Clones ST307 and ST147. Antimicrob. Agents. Chemother. 2020;64:e01148-20. doi: 10.1128/AAC.01148-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baek E.H., Kim S.E., Kim S., Lee S., Cho O.H., In Hong S., Shin J.H., Hwang I. Successful control of an extended-spectrum β-lactamase-producing Klebsiella pneumoniae ST307 outbreak in a neonatal intensive care unit. BMC Infect. Dis. 2020;20:166. doi: 10.1186/s12879-020-4889-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boonstra M.B., Spijkerman D.C.M., Voor In ‘t Holt A.F., van der Laan R.J., Bode L.G.M., van Vianen W., Klaassen C.H.W., Vos M.C., Severin J.A. An outbreak of ST307 extended-spectrum beta-lactamase (ESBL)-producing Klebsiella pneumoniae in a rehabilitation center: An unusual source and route of transmission. Infect. Control. Hosp. Epidemiol. 2020;41:31–36. doi: 10.1017/ice.2019.304. [DOI] [PubMed] [Google Scholar]
- 41.Giufre M., Accogli M., Ricchizzi E., Barbanti F., Farina C., Fazii P., Mattei R., Sarti M., Barozzi A., Buttazzi R., et al. Multidrug-resistant infections in long-term care facilities: Extended-spectrum beta-lactamase-producing Enterobacteriaceae and hypervirulent antibiotic resistant Clostridium difficile. Diagn. Microbiol. Infect. Dis. 2018;91:275–281. doi: 10.1016/j.diagmicrobio.2018.02.018. [DOI] [PubMed] [Google Scholar]
- 42.Wyres K.L., Hawkey J., Hetland M.A.K., Fostervold A., Wick R.R., Judd L.M., Hamidian M., Howden B.P., Lohr I.H., Holt K.E. Emergence and rapid global dissemination of CTX-M-15-associated Klebsiella pneumoniae strain ST307. J. Antimicrob. Chemother. 2019;74:577–581. doi: 10.1093/jac/dky492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piccirilli A., Perilli M., Piccirilli V., Segatore B., Amicosante G., Maccacaro L., Bazaj A., Naso L., Lo Cascio G., Cornaglia G. Molecular characterization of carbapenem-resistant Klebsiella pneumoniae ST14 and ST512 causing bloodstream infections in ICU and surgery wards of a tertiary university hospital of Verona (northern Italy): Co-production of KPC-3, OXA-48, and CTX-M-15 β-lactamases. Diagn. Microbiol. Infect. Dis. 2020;96:114968. doi: 10.1016/j.diagmicrobio.2019.114968. [DOI] [PubMed] [Google Scholar]
- 44.Perilli M., Bottoni C., Pontieri E., Segatore B., Celenza G., Setacci D., Bellio P., Strom R., Amicosante G. Emergence of blaKPC-3-Tn4401a in Klebsiella pneumoniae ST512 in the municipal wastewater treatment plant and in the university hospital of a town in central Italy. J. Glob. Antimicrob. Resist. 2013;1:217–220. doi: 10.1016/j.jgar.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 45.Perilli M., Bottoni C., Grimaldi A., Segatore B., Celenza G., Mariani M., Bellio P., Frascaria P., Amicosante G. Carbapenem-resistant Klebsiella pneumoniae harbouring blaKPC-3 and blaVIM-2 from central Italy. Diagn. Microbiol. Infect. Dis. 2013;75:218–221. doi: 10.1016/j.diagmicrobio.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 46.Geraci D.M., Bonura C., Giuffrè M., Saporito L., Graziano G., Aleo A., Fasciana T., Di Bernardo F., Stampone T., Palma D.M., et al. Is the monoclonal spread of the ST258, KPC-3-producing clone being replaced in southern Italy by the dissemination of multiple clones of carbapenem-nonsusceptible, KPC-3-producing Klebsiella pneumoniae? Clin. Microbiol. Infect. 2015;21:e15–e17. doi: 10.1016/j.cmi.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 47.Garcìa-Fernandez A., Miriagou V., Papagiannitsis C.C., Giordano A., Venditti M., Mancini C., Carattoli A. An ertapenem-resistant extended-spectrum-β-lactamase-producing Klebsiella pneumoniae clone carries a novel OmpK36 porin variant. Antimicrob. Agents. Chemother. 2010;54:4178–4184. doi: 10.1128/AAC.01301-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Orsi G.B., Bencardino A., Vena A., Carattoli A., Venditti C., Falcone M., Giordano A., Venditti M. Patient risk factors for outer membrane permeability and KPC-producing carbapenem-resistant Klebsiella pneumoniae isolation: Results of a double case-control study. Infection. 2013;41:61–67. doi: 10.1007/s15010-012-0354-2. [DOI] [PubMed] [Google Scholar]
- 49.Oliveira É.M., Beltrão E.M.B., Scavuzzi A.M.L., Barros J.F., Lopes A.C.S. High plasmid variability, and the presence of IncFIB, IncQ, IncA/C, IncHI1B, and IncL/M in clinical isolates of Klebsiella pneumoniae with blaKPC and blaNDM from patients at a public hospital in Brazil. Rev. Soc. Bras. Med. Trop. 2020;53:e20200397. doi: 10.1590/0037-8682-0397-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Villa L., García-Fernández A., Fortini D., Carattoli A. Replicon sequence typing of IncF plasmids carrying virulence and resistance determinants. J. Antimicrob. Chemother. 2010;65:2518–2529. doi: 10.1093/jac/dkq347. [DOI] [PubMed] [Google Scholar]
- 51.Ramirez M.S., Bonomo R.A., Tolmasky M.E. Carbapenemases: Transforming Acinetobacter baumannii into a yet more dangerous menace. Biomolecules. 2020;10:720. doi: 10.3390/biom10050720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arabacı Ç., Dal T., Başyiğit T., Genişel N., Durmaz R. Investigation of carbapenemase and mcr-1 genes in carbapenem-resistant Klebsiella pneumoniae isolates. J. Infect. Dev. Ctries. 2019;13:504–509. doi: 10.3855/jidc.11048. [DOI] [PubMed] [Google Scholar]
- 53.Chen L., Chavda K.D., Melano R.G., Hong T., Rojtman A.D., Jacobs M.R., Bonomo R.A., Kreiswirth B.N. Molecular survey of the dissemination of two blaKPC-harboring IncFIA plasmids in New Jersey and New York hospitals. Antimicrob. Agents. Chemother. 2014;58:2289–2294. doi: 10.1128/AAC.02749-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable.