Abstract
Metformin is a widely used antidiabetic drug for cancer prevention and treatment. However, the overproduction of lactic acid and its inefficiency in cancer therapy limit its application. Here, we demonstrate the synergistic effects of the lactate/GPR81 blockade (3-hydroxy-butyrate, 3-OBA) and metformin on inhibiting cancer cells growth in vitro. Simultaneously, this combination could inhibit glycolysis and OXPHOS metabolism, as well as inhibiting tumor growth and reducing serum lactate levels in tumor-bearing mice. Interestingly, we observed that this combination could enhance the functions of Jurkat cells in vitro and CD8+ T cells in vivo. In addition, considering that 3-OBA could recover the inhibitory effects of metformin on PD-1 expression, we further determined the dual blockade effects of PD-1/PD-L1 and lactate/GPR81 on the antitumor activity of metformin. Our results suggested that this dual blockade strategy could remarkably enhance the anti-tumor effects of metformin, or even lead to tumor regression. In conclusion, our study has proposed a novel and robust strategy for a future application of metformin in cancer treatment.
Keywords: metformin, GPR81, lactate, cancer immunotherapy, PD-1/PD-L1 blockade
1. Introduction
Despite considerable efforts and investments in the development of new cancer drugs, only 5% of them were approved for clinical therapeutics [1]. The substantial costs and slow pace of new drug discovery and development have provoked the exploration of new uses for approved drugs that are outside the scope of their original medical indication [2]. Compared with developing new drugs from scratch, the repurposing of existing drugs might potentially lower overall development costs and shorten development timelines.
Among the repurposed drugs, metformin is a promising candidate for cancer therapy. As a first-line drug for type 2 diabetes, metformin showed promising preventive effects on cancer [3,4,5]. Diabetics receiving metformin had a lower incidence of cancer than other patients [6,7]. Moreover, it has been found that metformin can directly suppress tumor growth by the activation of AMP activated protein kinase (AMPK) pathway, cell cycle arrest, and metabolic disorder [8,9,10]. Additionally, through promoting the secretion of tumor necrosis factor-α (TNF-α) and interferon γ (IFN-γ), metformin could significantly boost the anti-tumor activity of CD8+ T cells to indirectly retard tumor progression [11]. However, only high doses of metformin could impede tumor growth [12]. Unfortunately, high doses of metformin can lead to lactic acidosis and elevate intra-tumoral lactate levels [13,14]. Therefore, the application of metformin is a double-edged sword in cancer therapy, and it is crucial to employ the anti-tumor effects of metformin while reducing the undesired side effects caused by lactate.
Lactate, as the metabolite from cancer cells, facilitates cancer progression and metastasis [15,16,17]. Considerable studies have shown that excessive lactic acid induces a decrease in pH of the tumor microenvironment, which restrains the mobility and the cytotoxic function of T cells and even leads to apoptosis [18,19]. Lactate transmits pro-tumor signals through its receptor G-Protein Coupled Receptor 81 (GPR81), which is overexpressed in various types of cancer cells. The knockout of GPR81 can lower the sensitivity of tumor cells toward lactate, which allows to suppress tumor proliferation and metastasis [15]. Additionally, the activation of GPR81 mediated by lactate can also increases the expression of PD-L1 in tumor cells, to reduce IFN-γ secretion and the cell viability of co-cultured Jurkat cells [20]. A putative GPR81 antagonist, 3-hydroxy-butyrate (3-OBA) can be used to block the lactate/GPR81 pathway and protect cells from glucose deprivation [21]. Therefore, its application together with metformin will bring the opportunity to enhance the anti-tumor effects and reduce the side effects of metformin on lactate production.
Here, to improve the anti-tumor effect of metformin and reduce lactic acidosis, we sought to investigate whether blocking the lactate/GPR81 pathway could enhance the anti-tumor effects of low concentrations of metformin. Furthermore, we investigated the influence of the PD-1/PD-L1 blockade on the overall therapeutic performance of the combinational therapy. The results of this study demonstrate new evidence of this therapeutic mechanism and provide an effective strategy for anti-tumor application of metformin.
2. Materials and Methods
2.1. Cell Culture and Reagents
Human colon cancer cell lines HT29 and RKO, murine colon cancer cell line CT26, and the human T-lymphoblastic Jurkat cell line were purchased from ATCC and conserved by our laboratory. All cells were cultured in Dulbecco’s Modified Eagle Medium (DMEM) (Gibco, Grand Island, NY, USA) with 10% fetal bovine serum (FBS) (Sigma-Aldrich, St. Louis, MO, USA), supplemented with 100 μg/mL streptomycin (Solarbio, Beijing, China) and 100 U/mL penicillin (Solarbio, Beijing, China). Cells were cultured at 37 °C in an incubator with 5% CO2. Metformin (purity > 97.0%, Sangon Biothech, Shanghai, China), and 3-OBA (Sigma-Aldrich, St. Louis, MO, USA) was purchased.
2.2. TIMER Analysis, RNA Isolation and Quantitative Real-Time Polymerase Chain Reaction (PCR)
The Diff Exp module in the TIMER website (https://cistrome.shinyapps.io/timer/, accessed on 27 September 2019) was used to analyze the expression of GPR81 between tumor and normal tissue. Total RNA was extracted using RNA Isolation Kits (Vazyme, Nanjing, China) and then reversely transcribed into cDNA using HiScript III 1st Strand cDNA Synthesis Kits (Vazyme, Nanjing, China) according to the manufacturer’s instructions. We obtained the primer sequences for the targets from PrimerBank (https://pga.mgh.harvard.edu/primerbank/, accessed on 20 November 2019 and 5 January 2021), and verified their specificity in Primer-BLAST (https://www.ncbi.nlm.nih.gov/tools/primer-blast/, accessed on 20 November 2019 and 5 January 2021). The primer sequences used in experiments were synthesized by Sangon Biothech (Shanghai, China) and are listed in Table S1. After mixing the cDNA with SYSB qPCR Master-Mix (Vazyme, Nanjing, China) and setting the condition of the PCR reaction as follows: predegeneration at 95 °C for 3 min, 40 cycles of denaturation at 95 °C for 10 s, and extension at 60 °C for 30 s; melt curves were obtained at 95 °C for 15 s, 60 °C for 60 s, and 95 °C for 15 s. cDNA expression was monitored in a LightCycler 96 system (Roche, Basel, Switzerland).
2.3. Cell Growth Assay
HT29, RKO and CT26 cells were seeded in 96-well plates with 8 × 103, 4 × 103 and 3 × 103 cells per well, respectively, for 24 h. Then cells were treated with different concentration of metformin (5 mM, 15 mM, and 45 mM) and 3-OBA (0.1 mM, 1 mM, 10 mM, 15 mM, and 20 mM) for 48 h. Next, 20 μL of Cell Counting Kit-8 (CCK-8) (Beyotime, Shanghai, China) was added into each well and incubated for 2 h at 37 °C. Absorbance at 450 nm was determined by the microplate reader (PerkinElmer, Waltham, MA, USA). To evaluate the combinational effect of metformin and 3-OBA, we used the King’s method to calculate the Q value [22]. The Q value of 5 mM metformin and 15 mM 3-OBA was more than 1.15 and was the largest. Thus, we finally selected the combination of 5 mM metformin and 15 mM 3-OBA, with their obvious synergistic effect, to perform the studies.
2.4. Cell Apoptosis Assay
HT29 cells were seeded in 24-well plates with 5 × 104 cells per well for 24 h. Then cells were treated with 15 mM 3-OBA, 5 mM metformin, and the combination. After 48 h, the cells were harvested and resuspended with Phosphate Buffered Saline (PBS) buffer. According to the manufacturers’ instructions of apoptosis assay kit (Beyotime, Shanghai, China), we added 195 μL Annexin V-FITC binding buffer, 5 μL Annexin V-fluorescein isothiocyanate (FITC), and 10 μL propidium iodide (PI) to 1 × 105 cells. Following a gentle vortex, the cells were incubated at room temperature for 20 min in the dark. Finally, flow cytometry was used to monitor fluorescence intensity.
2.5. Western Blot Analysis
After being treated with 15 mM 3-OBA, 5 mM metformin and the combination, HT29 cell were collected and lysed. The lysates were subjected to 8% polyacrylamide gels with SDS. Then the protein was transferred onto polyvinylidene fluoride membranes. The membranes were incubated by primary antibodies against β-actin (3700S, CST, 1:1000), GPR81 (A20321, ABclonal, 1:1000), mTOR (2983S, CST, 1:1000), and p-mTOR (5536S, CST, 1:1000), and recognized with secondary antibodies.
2.6. Glucose Uptake Assay
After HT29 and RKO cells were treated with 5 mM metformin and 15 mM 3-OBA for 48 h, the cells were incubated in glucose-free medium with 2 mM L-glutamine for 3 h. Then, 100 μM 2-Deoxy-2-[(7-nitro-2,1,3-benzoxadiazol-4-yl) amino]-D-glucose (2-NBDG) was added to the incubate for 30 min. Subsequently, the cells were collected and the fluorescence intensity was analyzed by flow cytometry.
2.7. Glycolysis and Mitochondrial Stress Test
HT29 and RKO cells were seeded into an XF24 culture microplate (Seahorse Bioscience, Billerica, MA, USA) at densities of 4 × 104 and 1 × 104 cells per well, respectively. After incubating overnight, cells were treated with 5 mM metformin, 15 mM 3-OBA, or the combination for 24 h. Then cells were rinsed twice with assay medium and placed in a non-CO2 incubator for 45 min. Meanwhile, glucose, oligomycin (OM), 2-deoxy glucose (2-DG), carbonyl cyanide-4 (trifluoromethoxy) phenylhydrazone (FCCP), and rotenone/antimycin A were diluted with the assay medium to specified concentrations. Finally, these reagents were loaded into the sensor cartridge and the plate was placed into Seahorse XFe24 Extracellular Flux Analyzers (Seahorse Bioscience, Billerica, USA) to monitor the extracellular acidification rate (ECAR) and the oxygen consumption rate (OCR).
2.8. Jurkat Cell Proliferation and Function Analysis
Under the stimulation of 1 μg/mL anti-human CD3 antibody (OKT3, eBioscience, San Diego, CA, USA) and 0.5 μg/mL anti-human CD28 antibody (CD28.2, eBioscience, San Diego, CA, USA), Jurkat cells were treated with 5 mM metformin, 15 mM 3-OBA, or the combination for 48 h. Alternatively, HT29 cells were treated with 5 mM metformin, 15 mM 3-OBA, or the combination for 48 h. Then culture supernatant was taken out separately to treat Jurkat cells for 48 h. A CCK8 kit was used to determine cell proliferation, or after pretreating cells with protein transport inhibitor for 4 h, cells were fixed and permeabilized for staining with P-phycoerythrin (PE) anti-human IFN-γ antibody (4S.B3, eBioscience, San Diego, CA, USA) and allophycocyanin (APC) anti-human IL-2 antibody (MQ1-17H12, eBioscience, San Diego, CA, USA). To distinguish the negative and positive cells, we used the matched isotype control or fluorescence minus one (FMO) control to define their boundaries.
2.9. Xenograft Tumor Growth
Animal experiments were approved by the Ethics Committee of Sun Yat-Sen University (SYSU-20200437) and performed complying to the national and institutional guidelines. Female BALB/c nude mice and female BALB/c mice (18–22 g) were purchased from Guangdong Medical Laboratory Animal Center. 1 × 107 HT29 and 2 × 105 CT26 cells were subcutaneously injected into the right flanks of BALB/c nude mice or the BALB/c mice, respectively. Tumor volumes were measured using a digital caliper every other day, and calculated as V (mm3) = 0.5 × length × width × height. When tumor volumes reached 40–80 mm3, mice were randomly divided into groups. Metformin (200 mg/kg), 3-OBA (75 mg/kg) and the combination of 3-OBA and metformin with the same dosage were intraperitoneally injected into mice every day. PD-1/PD-L1 blocking peptide C8 (2 mg/kg) [23] and the negative control normal saline were injected paratumorally every other day. Body weights were recorded every other day.
2.10. Serum Lactate Measurement
According to the manual of Lactate Assay Kit (Solarbio, Beijing, China), 100 µL of serum was sampled from mice and added into 1 mL of extracting solution I. After being centrifuged at 12,000× g at 4 °C for 10 min, 0.8 mL of the supernatant was then withdrawn. After 150 µL of extracting solution II was added, the samples were centrifuged at 12,000× g for 10 min. Then, the supernatant was harvested and measured.
2.11. Flow Cytometry
After treatment with metformin or 3-OBA, Jurkat cells were collected and stained with PE anti-human PD-1 antibody (MIH4, eBioscience, San Diego, CA, USA). The expression of PD-1 was evaluated using flow cytometry. Tumor tissues were removed from the mice, minced, and digested by collagenase IV (Invitrogen, Carlsbad, CA, USA) and Dnase I (Sigma-Aldrich, St. Louis, MO, USA) at 37 °C in a shaker for 40 min. Spleen and draining lymph nodes were ground and filtrated with a 70 μm filter. All samples were stained with FITC anti-mouse CD45 antibody (30-F11, eBioscience, San Diego, CA, USA), PerCP-eFluor 710 anti-mouse CD3 antibody (17A2, eBioscience, San Diego, CA, USA), Brilliant Violet 421 anti-mouse CD8 antibody (53–6.7, BioLegend, San Diego, CA, USA), and APC anti-mouse PD-1 antibody (RMP1-30, eBioscience, San Diego, CA, USA) for 30 min. After fixation and permeabilization, the cells were stained by PE anti-mouse IFN-γ antibody (XMG1.2, eBioscience, San Diego, CA, USA) for 30 min. The fluorescence intensity was analyzed by flow cytometry, and the matched isotype control was applied to distinguish the negative and positive cells.
2.12. Statistical Analysis
Results are presented as means ± standard deviation and were analyzed by a Student’s t-test or one-way analysis of variance (ANOVA). p < 0.05 was considered statistically significant.
3. Results
3.1. The Anti-Tumor Efficacy of Metformin and 3-OBA on Colorectal Cancer Cells
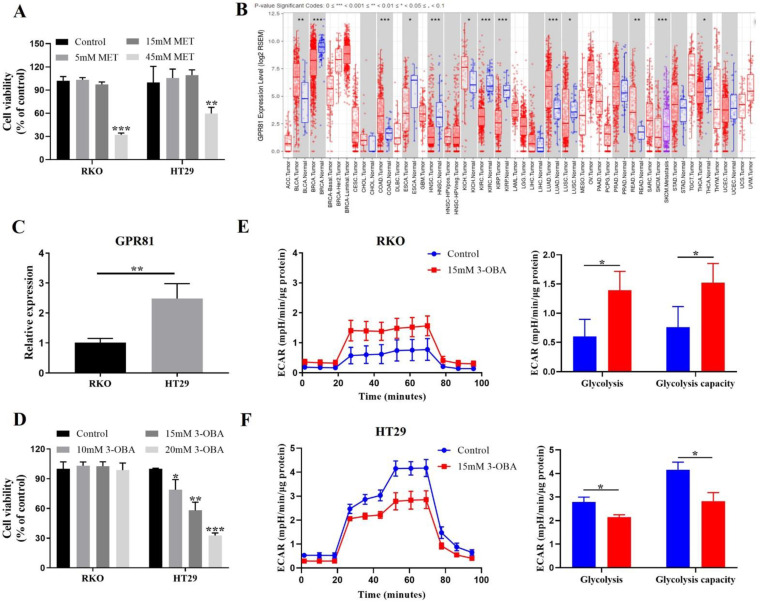
The cell growth assay showed that 45 mM metformin could significantly inhibit the proliferation of human colon cancer cell lines, HT29, and RKO cells, but 5 mM and 15 mM metformin could not (Figure 1A). As reported elsewhere, the effective in vitro concentration of metformin was very high, usually between 10 and 40 mM [13,14]. Thus, we selected 5 mM metformin to perform the studies. Considering that metformin may result in lactic acidosis to promote cancer progression, we performed a glycolysis-stress test to monitor glycolysis. As shown in Supplementary Figure S1A,B, metformin elevated glycolysis, suggesting that metformin can indeed promote the lactic acid production of cancer cells.
Figure 1.
Effects of metformin and 3-OBA on cell proliferation and metabolism. (A) RKO and HT29 cells were treated with various concentrations of metformin (5 mM, 15 mM, 45 mM) for 48 h. Cell viability was measured by CCK-8 assay. (B) GPR81 expression of a wide variety of cancers in TIMER. (C) Relative mRNA expression of GPR81 in RKO and HT29 cells. (D) RKO and HT29 cells were treated with different concentrations of 3-OBA (10 mM, 15 mM, 20 mM) for 48 h. Cell viability was measured by CCK-8 assay. (E,F) Extracellular acidification rate (ECAR) of RKO (E) or HT29 (F) cells pretreated with 15 mM 3-OBA was detected in the presence of glucose, oligomycin (OM), and 2-deoxy glucose (2-DG). Representative histograms of at least three independent experiments are shown. * p < 0.05, ** p < 0.01, *** p < 0.001.
Since excessive lactate could weaken the anti-proliferation activity of metformin, it is important to interrupt lactate/GPR81 signaling. Firstly, we exploited TIMER [24], a web server, to analyze the expression of GPR81 in multiple cancers. It was found that GPR81 was highly expressed in colorectal cancer compared with normal tissue (Figure 1B). The results of quantitative real-time PCR (Figure 1C) and western blot (Supplementary Figure S1C) showed that GPR81 expression was significantly higher in HT29 cells than in RKO cells. 3-OBA could inhibit the proliferation of HT29 cells, but not RKO cells (Figure 1D; Supplementary Figure S1D,E). Recently, it has been revealed that silencing GPR81 could suppress the expression of lactate transporters and monocarboxylate transporters (MCTs) [15]. Similarly, 3-OBA could inhibit MCT1 and MCT4 expression in HT29 cells with high GPR81 expression levels, but not in RKO cells with low expression of GPR81 (Supplementary Figure S1F,G). These data illustrate that GPR81 may be associated with glycolysis. We monitored glycolysis, and discovered that 3-OBA inhibited the glycolysis of HT29 cells (Figure 1F), while improving that of RKO cells (Figure 1E). Therefore, 3-OBA has an inhibitory effect in the proliferation and glycolysis of colorectal cancer cells with high GPR81 expression, suggesting that 3-OBA can reduce the lactate levels and enhance the anti-tumor effects of metformin.
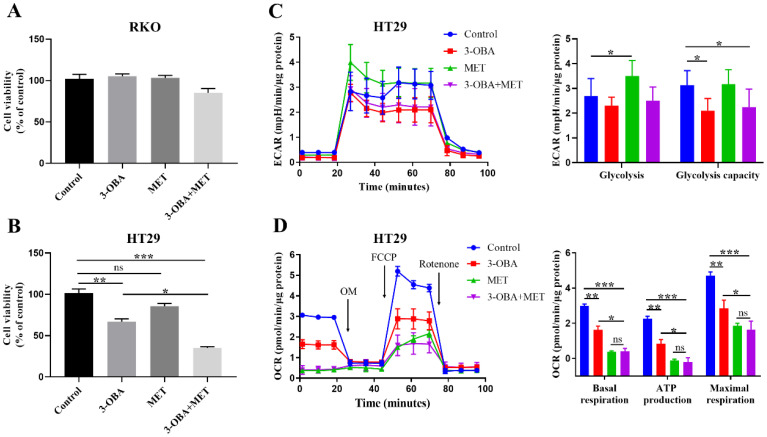
3.2. The Synergistic Effects of Metformin and 3-OBA on Cell Growth and Lactate Metabolism
Next, we determined whether the anti-tumor effect of metformin was elevated by the combination through a lactate/GPR81 pathway blockade. The results showed that the combination of 3-OBA and metformin had no effects on the proliferation of RKO cells (Figure 2A), but inhibited the proliferation of HT29 cells more significantly than metformin or 3-OBA alone (Figure 2B). As shown in Supplementary Figure S2A, the combination had no effect on cell apoptosis. Similar anti-proliferation effect was shown in the murine colon cancer cell line CT26 (Supplementary Figure S2B). The results of ECAR showed that glycolysis in HT29 cells was blocked by 3-OBA and the combination (Figure 2C). The reduction of lactate production would in turn promote oxidative phosphorylation (OXPHOS), we thus used a mito-stress test to measure OXPHOS. Surprisingly, 3-OBA and the combination also inhibited OXPHOS in addition to inhibiting glycolysis (Figure 2D). Therefore, when combined with 3-OBA, the anti-proliferation effect of metformin was enhanced and lactate metabolism was suppressed.
Figure 2.
The combination of 3-OBA and metformin inhibits the cell proliferation and lactate metabolism of HT29. (A,B) RKO (A) or HT29 (B) cells were treated with 15 mM 3-OBA, 5 mM metformin, and the combination, then cell viability was determined by CCK-8 assay. (C,D) Extracellular acidification rate (ECAR) (C) or oxygen consumption rate (OCR) (D) of HT29 cells pretreated with 15 mM 3-OBA, 5 mM metformin, and the combination. The OCR were detected in the presence of oligomycin (OM), carbonyl cyanide-4 (trifluoromethoxy), phenylhydrazone (FCCP), and rotenone. Representative histograms of at least three independent experiments were shown. * p < 0.05, ** p < 0.01, *** p < 0.001; ns represents no significant difference.
To investigate the mechanism of glycolysis suppression, we used a 2-NBDG fluorescent probe to detect whether glucose uptake, as the first step of glucose metabolism, was affected. It was observed that glucose uptake was not impacted by 3-OBA, but was significantly increased in the combinational treatment (Supplementary Figure S2C). This observation indicates that the glycolysis inhibiting effects of the combined treatment was not due to glucose uptake. Then, we investigates the expression of metabolic enzymes related to glycolysis. The results showed that metformin down-regulated the expression of hexokinase 2 (HK2), but it was up-regulated by the combination. All three treatments could elevate the expression of aldose 1-epimerase (GALM). Among these enzymes, the expressions of phosphoglycerate mutase 1 (PGAM1), phosphoglycerate mutase 2 (PGAM2), and alpha-enolase (ENO1), located on the upstream of lactate production and OXPHOS, were significantly decreased by treatment with the combination, which might result in glycolysis inhibition and reduced lactate production (Supplementary Figure S2D,E), and might lead to the increase of glucose uptake. The mammalian targets of rapamycin (mTOR) and GPR81 play a vital role in cell metabolism [25,26]. Thus, we detected their protein levels and found that the combined treatment could significantly reduce the expression of GPR81 and mTOR phosphorylation (Supplementary Figure S2F), which may collectively result in the significant inhibition of cell proliferation and metabolism.
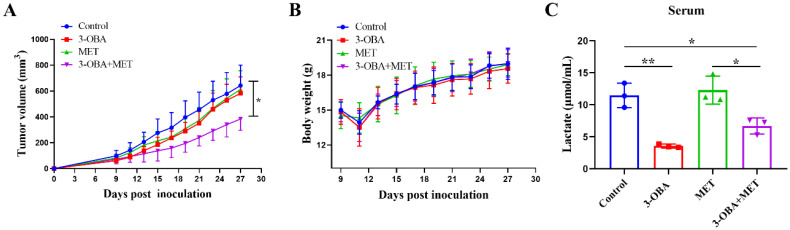
3.3. 3-OBA Could Enhance the Anti-Tumor Effects of Metformin
In the human colon cancer HT29 cell bearing tumor model, the tumor volume was significantly reduced with the combinational treatment of 3-OBA and metformin (Figure 3A). There was no significant difference in body weight between the groups (Figure 3B). High levels of lactate in serum were associated with poor prognosis and reduced overall survival of various cancers [27,28]. We evaluated the serum lactate levels in tumor-bearing mice. The results showed that 3-OBA and the combinational treatment reduced lactic acid levels in serum (Figure 3C).
Figure 3.
The combination of 3-OBA and metformin inhibits HT29 tumor cell growth in vivo. BALB/c nude mice (n = 6) were intraperitoneal injected with 75 mg/kg of 3-OBA, 200 mg/kg of metformin, and the combination, (A) tumor volumes and (B) body weights were measured every other day. (C) Lactate concentration in serum after different treatments. * p < 0.05, ** p < 0.01.
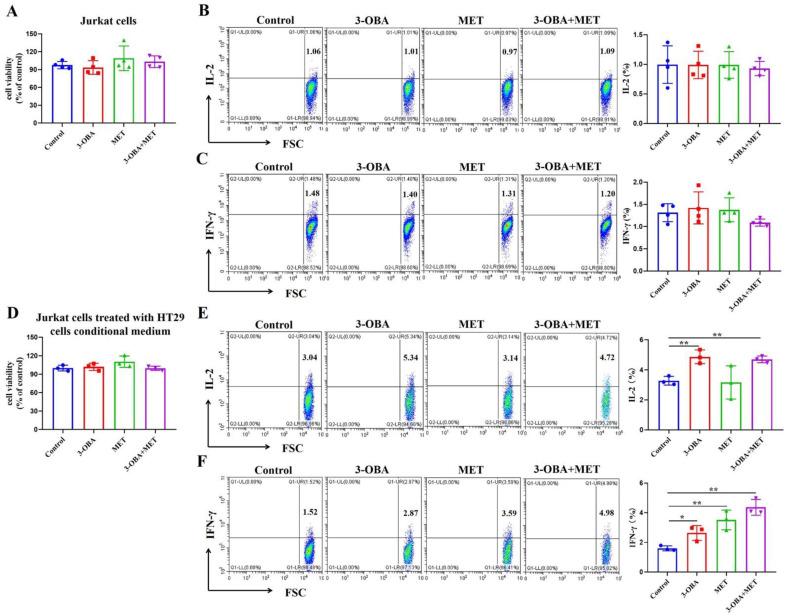
3.4. T Cell Function Could Be Elevated by Metformin and 3-OBA
Since the combinational treatment of 3-OBA and metformin affected the proliferation of tumor cells, we next explored whether the combination might also inhibit T cells, a class of tumor-killing cells. Jurkat cells were treated with the combination, and we found that proliferation (Figure 4A) and the ability to secrete IL-2 and IFN-γ (Figure 4B,C) were unchanged. To investigate whether low glycolysis-mediated lactate level reduction after the combination treatment could promote T cell growth or enhance T cell cytotoxicity, the conditional medium from HT29 cells treated by 3-OBA, metformin, or their combination, was subsequently used to treat Jurkat cells. Although there was no significant difference in the proliferation of Jurkat cells between each group (Figure 4D), the secretion of IL-2 was promoted by the 3-OBA group and the combination group (Figure 4E). Furthermore, all three treatment groups improved the levels of IFN-γ in Jurkat cells, and the secretion of IFN-γ in the combination group was slightly higher than that in the metformin group (Figure 4F). These results suggest that the combination could promote the anti-tumor activity of T cells.
Figure 4.
Effects of the combination of 3-OBA and metformin in the proliferation and functions of Jurkat cells. After treatment with 15 mM 3-OBA, 5 mM metformin, or the combination, (A) cell viability and (B,C) the secretions of IL-2 (B) or IFN-γ (C) by Jurkat cells were measured. After treatment with the conditional medium from HT29 cells treated by 3-OBA, metformin, or their combination, (D) cell viability and (E,F) the secretions of IL-2 (E) or IFN-γ (F) by Jurkat cells were monitored. Representative histograms of at least three independent experiments were shown. * p< 0.05, ** p < 0.01.
The expression of the immune checkpoints (such as PD-1) in T cells is associated with their cytotoxic function [29,30]. Flow cytometry results showed that metformin down-regulated PD-1 expression of Jurkat cells, while 3-OBA up-regulated its expression. And there was no significant difference in PD-1 expression between the combination and the control (Supplementary Figure S3A). Thus, metformin alone may reduce patients’ response to PD-1-blockade-based immunotherapy, which could be overcome in combination with 3-OBA.
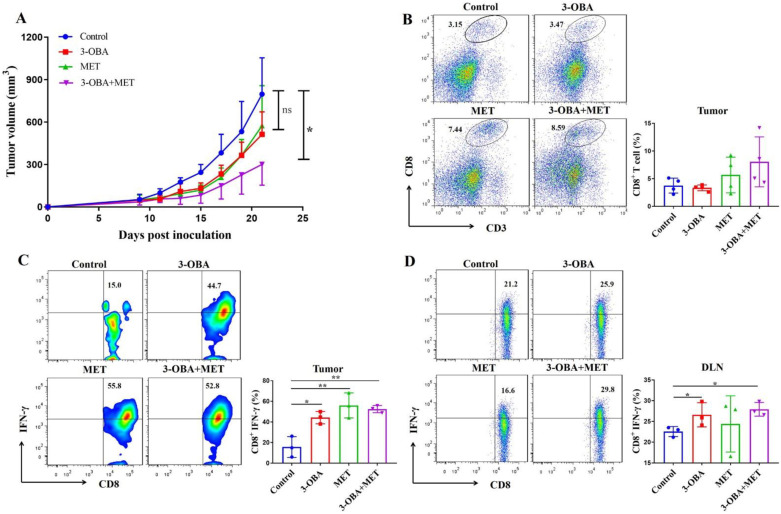
3.5. The Combination of Metformin and 3-OBA Could Activate T Cell in Vivo
As shown in Figure 5A, the combination treatment significantly inhibited tumor growth in CT26-bearing mice, but metformin or 3-OBA alone did not. Although there was no statistical difference compared with the control group, the percentage of CD8+ T cells after combinational treatment did increase (Figure 5B). We found that the IFN-γ levels of intra-tumoral CD8+ T cells in all three treatment groups were significantly increased compared with the control group (Figure 5C). Metformin increased the IFN-γ production of CD8+ T cells in the spleen, but no significant difference was found in other groups (Supplementary Figure S3B). In the draining lymph nodes, 3-OBA alone and the combination significantly elevated the IFN-γ proportion of CD8+ T cells, but metformin did not (Figure 5D). Considering that the function of CD8+ T cells in the draining lymph node usually reflects the antitumor immune response inside the tumor, although there was no significant difference in the infiltration of the CD8+ T cells, our results indicate that metformin combined with 3-OBA could elevate CD8+ T cell functions and thus enhance anti-tumor efficacy.
Figure 5.
The combination of 3-OBA and metformin could suppress CT26 tumor cell growth and active CD8+ T cells. BALB/c mice (n = 6) were treated with 75 mg/kg of 3-OBA, 200 mg/kg of metformin, and the combination every day. (A) Tumor volumes. (B) The ratio of intra-tumoral CD8+ T cells. (C) The proportion of IFN-γ+ CD8+ T cells in tumors (D) and in the draining lymph nodes. * p < 0.05, ** p < 0.01. ns denotes no significant difference.
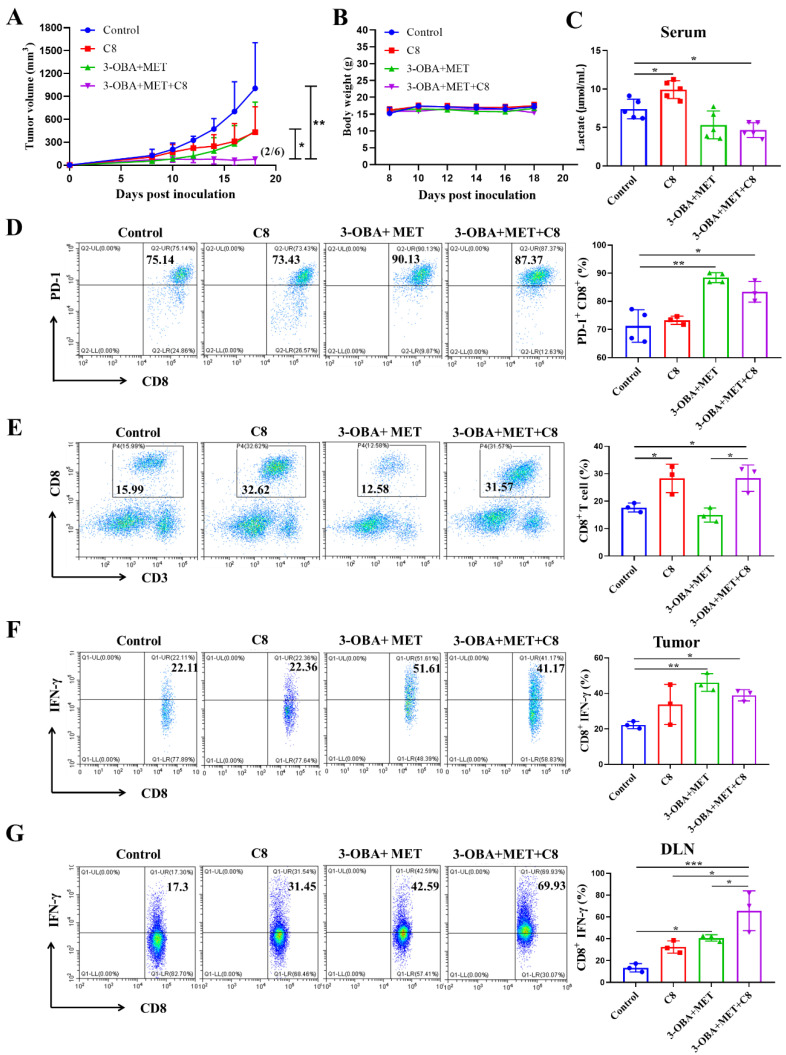
3.6. PD-1 Blockade Could Further Improve the Antitumor Efficacy of Metformin/3-OBA Combination Treatment
To further enhance the antitumor effects, combined with PD-1 blockade may be an appropriate choice. The combination of 3-OBA and metformin was found to reduce the production of lactic acid, and recovered the inhibitory effect of metformin on PD-1 expression. This evidence indicated that the antitumor effects of metformin would be further enhanced by a PD-1 blockade. Here, cyclic peptide C8 was used as a PD-1/PD-L1 inhibitor, as developed by our group previously [23]. In CT26 mouse models, the antitumor effect of C8 combined with metformin and 3-OBA was significantly greater than that of the metformin and 3-OBA combination group and the C8 alone group (Figure 6A). All treatments had no influence on the body weight of the mice, ensuring their safety profiles (Figure 6B). As shown in Figure 6C, serum lactate was increased after C8 treatment, but lower than the control after treatment with the combination of C8, metformin, and 3-OBA. Interestingly, it was observed that the combination of 3-OBA and metformin dramatically up-regulated the expression of PD-1 in intra-tumoral CD8+ T cells in vivo, which provided a theoretical basis for the combination PD-1 blockade. Although C8 alone could not affect PD-1 expression, it could be upregulated when combined with 3-OBA and metformin (Figure 6D).
Figure 6.
C8 could enhance the anti-tumor effects of the combination of 3-OBA and metformin in vivo. (A) Tumor volumes after different treatments. In the combination treatment of 75 mg/kg 3-OBA, 200 mg/kg metformin, and 2 mg/kg C8, tumors of two mice regressed (n = 6). (B) Body weights. (C) Serum lactate in mice. The effects of the combination of 3-OBA, metformin, and C8 on (D) PD-1 expression of CD8+ T cells, (E) intra-tumoral CD8+ T cell proportions, (F) the ratio of IFN-γ+ CD8+ T cells in tumors, (G) and in the draining lymph nodes. (n = 3) * p < 0.05, ** p < 0.01, *** p < 0.001.
We next determined whether combining the PD-1 blockade was more effective at improving the cytotoxic effect of T cells. It was found that after combination with C8, the proportion of CD8+ T cells in tumor tissue was observably elevated compared with the combination of 3-OBA and metformin (Figure 6E). Meanwhile, the addition of C8 significantly elevated the ratio of CD8+ IFN-γ+ T cells in tumor compared with the control (Figure 6F). These results revealed that the combination of metformin, 3-OBA, and C8 could fully exert the proliferation capacity and cytotoxic activity of CD8+ T cells against cancer. Although C8 combined with metformin and 3-OBA did not increase the proportion of CD8+ IFN-γ+ T cells in the spleen (Supplementary Figure S3C), its ratio in the lymph nodes was significantly increased compared to the C8 group and the combination group of metformin and 3-OBA (Figure 6G). Therefore, the dual blockade of lactate/GPR81 and the PD-1/PD-L1 pathway augments the function of CD8+ T cells and prominently enhances the anti-tumor efficacy of metformin.
4. Discussion
Drug repurposing is a promising strategy to discover ‘new’ anti-tumor agents from existing ones with full medical specification [31]. Metformin, a commonly prescribed drug for type 2 diabetes, has a proven therapeutic effect in cancer prevention and the reduction of cancer morbidity and mortality [32,33,34]. However, the effective dose of metformin on cancer therapy is often too high, thus inducing the accumulation of lactate and presenting a risk of lactic acidosis [12]. Here, we confirmed that low concentrations of metformin had no anti-proliferative effect on tumor cells, but elevated glycolysis levels to produce excessive lactate. The results of metabolomic analysis showed that metformin could elevate lactate levels [35]. A recent study demonstrated that excessive lactate could lower anti-tumor efficacy of chemotherapeutic agents such as doxorubicin and paclitaxel [36]. Therefore, the production of plethoric lactate may be a key factor to trigger the low anti-tumor efficacy of metformin. GPR81 is a receptor of lactate and mediates the signal transduction of extracellular lactate [15]. Thus, whether blocking lactate/GPR81 pathway can increase the anti-tumor efficacy of metformin should be determined.
Our results showed that 3-OBA, a GPR81 antagonist, remarkably enhanced the anti-tumor effects of metformin. Moreover, the combination of 3-OBA and metformin was able to lower glycolysis levels and reduce serum lactate levels. Serum lactate is an important prognostic biomarker for cancer patients [37,38], thus its reduction represents a remarkable anti-tumor effect of the combination. For maintaining the physiological functions of tumor cells, metabolic plasticity would shift from glycolysis to OXPHOS [39]. Moreover, metabolic rewiring between glycolysis and OXPHOS is a crucial factor to drive drug resistance [40]. Intriguingly, the combination did not increase the levels of OXPHOS, but decreased them. These results showed that the combination might reduce the chance of chemoresistance.
Finding the tumor inhibitory effects governed by the combination of lactate/GPR81 pathway blockade and metformin, we hypothesized whether it might also impair T cells. We found that the combination could significantly enhance IFN-γ secretion of CD8+ T cells in tumors and the draining lymph nodes. Similarly, a recent study has also demonstrated that the IFN-γ secretion of Jurkat cells increased after co-culturing with GPR81-expression cancer cells, as compared to the cells without GPR81 expression [41]. However, the number of intra-tumoral CD8+ T cells remained the same. To further enhance the anti-tumor activity of T cells, we combined PD-1/PD-L1 blockade therapy together with the lactate/GPR81 pathway blockade and metformin. Thrillingly, we observed that the additional adoption of PD-1/PD-L1 blockade therapy inhibited tumor growth even more significantly and induced tumor regression, albeit while noting that it also increased the quantity of intra-tumoral CD8+ T cells. Furthermore, it was found that the proportion of IFN-γ+ CD8+ T cells in the draining lymph nodes was elevated remarkably.
Although the combinational application of metformin and a PD-1/PD-L1 blockade has been reported for cancer therapy, it did not promote the objective response rate (ORR), nor offer a survival benefit [42,43,44]. Metformin indeed suppresses PD-1 and PD-L1 expression [45,46,47], which lowers patients’ response to PD-1/PD-L1 blockade therapy [48]. Therefore, metformin in combination with the PD-1/PD-L1 blockade therapy is inadequate to cause a permanent impairment of tumor cells. In this study, it was interesting to find that when combined with 3-OBA, PD-1 expression was restored to a level even higher than that of the control. In addition, a recent study has illustrated that after treatment with an immune checkpoint inhibitor, the mice bearing glycolysis-low tumors survived longer and had lower metastasis rates than mice with highly glycolytic tumors [49]. These data showed that the increase of PD-1 expression and the decrease of glycolysis induced by blocking the lactate/GPR81 pathway could enhance the combinational anti-tumor effects of metformin and the PD-1/PD-L1 blockade.
In the present study, a combinational therapy of 3-OBA and metformin demonstrated a significant anti-tumor effect on the HT29 cell line and a PD-1-responsive CT26 tumor model. However, whether the combination can improve the response to the treatment of PD-1/PD-L1 blockade in clinical settings remains uncertain. For expanding the population benefit from PD-1/PD-L1 blocking therapy, the issue is worthy of further interrogation and investigation. Besides, the combinational treatment could slow down the tumor growth and provide more time for patients to receive treatment, further surgery or even radiation therapy is still warranted.
In conclusion, lactate/GPR81 pathway blockade and metformin synergistically inhibited colorectal cancer cell growth and activated CD8+ T cells. In addition, the combination simultaneously decreased glycolysis and OXPHOS, which might result from the down-regulation of glycolytic enzymes, mTOR phosphorylation, and GPR81 levels, but not glucose uptake. And it also significantly reduced serum lactate levels. In addition, the therapeutic effect was further improved in combination with a PD-1/PD-L1 blockade via significantly increasing the number of CD8+ T cells in the tumors and elevating the secretion of IFN-γ in the lymph nodes. In summary, our study provided a potential strategy for improving the cancer-therapeutic effect of metformin. Moreover, it may offer an effective method to raise patients’ response to the treatment of PD-1/PD-L1 blockade.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/biom11091373/s1, Figure S1: Effect of metformin or 3-OBA on colorectal cancer cells, Figure S2: Mechanism of the combination of 3-OBA and metformin mediated metabolism inhibition, Figure S3: The combinational effects on PD-1 expression and IFN-γ secretion, Table S1: Primer sequences used for quantitative real-time PCR.
Author Contributions
Conceptualization, S.C. and Y.G.; methodology, S.C.; software, R.S.; validation, X.J. and Y.G.; formal analysis, S.C., X.Z. and Y.G.; investigation, S.C., X.Z., X.Y., W.L., S.L., Z.H., C.L. and N.S.; data curation, S.C. and Y.G.; writing—original draft preparation, S.C.; writing—review and editing, X.Z., G.C., J.L. and Y.G.; visualization, S.C.; supervision, X.Z. and Y.G.; project administration, X.S. and Y.G.; funding acquisition, X.S. and Y.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (Nos. U20A20369, 81822043, 81901687), the Key Incubation Fund of SYSU (19ykzd29), the Shenzhen Science and Technology Program (KQTD20190929173853397) and the “Pearl River Talent Plan” Innovation and Entrepreneurship Team Project of Guangdong Province (2019ZT08Y464).
Institutional Review Board Statement
Animal experiments were approved by the Ethics Committee of Sun Yat-Sen University (SYSU-20200437) and performed complying to the national and institutional guidelines.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gupta S.C., Sung B., Prasad S., Webb L.J., Aggarwal B.B. Cancer drug discovery by repurposing: Teaching new tricks to old dogs. Trends Pharmacol. Sci. 2013;34:508–517. doi: 10.1016/j.tips.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Nosengo N. Can you teach old drugs new tricks? Nature. 2016;534:314–316. doi: 10.1038/534314a. [DOI] [PubMed] [Google Scholar]
- 3.Zhou J., Massey S., Story D., Li L. Metformin: An Old Drug with New Applications. Int. J. Mol. Sci. 2018;19:2863. doi: 10.3390/ijms19102863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heckman-Stoddard B., DeCensi A., Sahasrabuddhe V.V., Ford L.G. Repurposing metformin for the prevention of cancer and cancer recurrence. Diabetologia. 2017;60:1639–1647. doi: 10.1007/s00125-017-4372-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kheirandish M., Mahboobi H., Yazdanparast M., Kamal W., Kamal M.A. Anti-cancer Effects of Metformin: Recent Evidences for its Role in Prevention and Treatment of Cancer. Curr. Drug Metab. 2018;19:793–797. doi: 10.2174/1389200219666180416161846. [DOI] [PubMed] [Google Scholar]
- 6.Wu D., Hu D., Chen H., Shi G., Fetahu I., Wu F., Rabidou K., Fang R., Tan L., Xu S., et al. Glucose-regulated phosphorylation of TET2 by AMPK reveals a pathway linking diabetes to cancer. Nat. Cell Biol. 2018;559:637–641. doi: 10.1038/s41586-018-0350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatoum D., McGowan E.M. Recent Advances in the Use of Metformin: Can Treating Diabetes Prevent Breast Cancer? BioMed Res. Int. 2015;2015:548436. doi: 10.1155/2015/548436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dowling R., Zakikhani M., Fantus I.G., Pollak M., Sonenberg N. Metformin Inhibits Mammalian Target of Rapamycin–Dependent Translation Initiation in Breast Cancer Cells. Cancer Res. 2007;67:10804–10812. doi: 10.1158/0008-5472.CAN-07-2310. [DOI] [PubMed] [Google Scholar]
- 9.Skinner H.D., Crane C.H., Garrett C.R., Eng C., Chang G.J., Skibber J.M., Rodriguez-Bigas M.A., Kelly P., Sandulache V.C., Delclos M.E., et al. Metformin use and improved response to therapy in rectal cancer. Cancer Med. 2013;2:99–107. doi: 10.1002/cam4.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ota S., Horigome K., Ishii T., Nakai M., Hayashi K., Kawamura T., Kishino A., Taiji M., Kimura T. Metformin suppresses glucose-6-phosphatase expression by a complex I inhibition and AMPK activation-independent mechanism. Biochem. Biophys. Res. Commun. 2009;388:311–316. doi: 10.1016/j.bbrc.2009.07.164. [DOI] [PubMed] [Google Scholar]
- 11.Eikawa S., Nishida M., Mizukami S., Yamazaki C., Nakayama E., Udono H. Immune-mediated antitumor effect by type 2 diabetes drug, metformin. Proc. Natl. Acad. Sci. USA. 2015;112:1809–1814. doi: 10.1073/pnas.1417636112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duque J.E., López C., Cruz N. Antitumor mechanisms of metformin: Signaling, metabolism, immunity and beyond. Univ. Sci. 2010;15:122–129. doi: 10.11144/javeriana.SC15-2.amom. [DOI] [Google Scholar]
- 13.Ugwueze C.V., Ogamba O.J., Young E.E., Onyenekwe B.M., Ezeokpo B.C. Metformin: A possible option in cancer chemotherapy. Anal. Cell. Pathol. 2020;2020:7180923. doi: 10.1155/2020/7180923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sena P., Mancini S., Benincasa M., Mariani F., Palumbo C., Roncucci L. Metformin induces apoptosis and alters cellular responses to oxidative stress in ht29 colon cancer cells: Preliminary findings. Int. J. Mol. Sci. 2018;19:1478. doi: 10.3390/ijms19051478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roland C.L., Arumugam T., Deng D., Liu S.H., Philip B., Gomez S., Burns W.R., Ramachandran V., Wang H., Cruz-Monserrate Z., et al. Cell Surface Lactate Receptor GPR81 Is Crucial for Cancer Cell Survival. Cancer Res. 2014;74:5301–5310. doi: 10.1158/0008-5472.CAN-14-0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhup S., Dadhich R.K., Porporato P.E., Sonveaux P. Multiple Biological Activities of Lactic Acid in Cancer: Influences on Tumor Growth, Angiogenesis and Metastasis. Curr. Pharm. Des. 2012;18:1319–1330. doi: 10.2174/138161212799504902. [DOI] [PubMed] [Google Scholar]
- 17.Ippolito L., Morandi A., Giannoni E., Chiarugi P. Lactate: A Metabolic Driver in the Tumour Landscape. Trends Biochem. Sci. 2019;44:153–166. doi: 10.1016/j.tibs.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 18.Fischer K., Hoffmann P., Völkl S., Meidenbauer N., Ammer J., Edinger M., Gottfried E., Schwarz S., Rothe G., Hoves S., et al. Inhibitory effect of tumor cell–derived lactic acid on human T cells. Blood. 2007;109:3812–3819. doi: 10.1182/blood-2006-07-035972. [DOI] [PubMed] [Google Scholar]
- 19.Haas R., Smith J., Rocher-Ros V., Nadkarni S., Montero-Melendez T., D’Acquisto F., Bland E.J., Bombardieri M., Pitzalis C., Perretti M., et al. Lactate Regulates Metabolic and Pro-inflammatory Circuits in Control of T Cell Migration and Effector Functions. PLoS Biol. 2015;13:e1002202. doi: 10.1371/journal.pbio.1002202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng J., Yang H., Zhang Y., Wei H., Zhu Z., Zhu B., Yang M., Cao W., Wang L., Wu Z. Tumor cell-derived lactate induces TAZ-dependent upregulation of PD-L1 through GPR81 in human lung cancer cells. Oncogene. 2017;36:5829–5839. doi: 10.1038/onc.2017.188. [DOI] [PubMed] [Google Scholar]
- 21.Shen Z., Jiang L., Yuan Y., Deng T., Zheng Y.-R., Zhao Y.-Y., Li W.-L., Wu J.-Y., Gao J.-Q., Hu W.-W., et al. Inhibition of G Protein-Coupled Receptor 81 (GPR81) Protects Against Ischemic Brain Injury. CNS Neurosci. Ther. 2014;21:271–279. doi: 10.1111/cns.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Z., Zhang R., Hao C., Pei X., Li J., Wang L. GANT61 and Valproic Acid Synergistically Inhibited Multiple Myeloma Cell Proliferation via Hedgehog Signaling Pathway. Med. Sci. Monit. 2020;26:e920541-1–e920541-9. doi: 10.12659/MSM.920541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhai W., Zhou X., Zhai M., Li W., Ran Y., Sun Y., Du J., Zhao W., Xing L., Qi Y., et al. Blocking of the PD-1/PD-L1 interaction by a novel cyclic peptide inhibitor for cancer immunotherapy. Sci. China Life Sci. 2020;64:548–562. doi: 10.1007/s11427-020-1740-8. [DOI] [PubMed] [Google Scholar]
- 24.Li T., Fan J., Wang B., Traugh N., Chen Q., Liu J.S., Li B., Liu X.S. TIMER: A Web Server for Comprehensive Analysis of Tumor-Infiltrating Immune Cells. Cancer Res. 2017;77:e108–e110. doi: 10.1158/0008-5472.CAN-17-0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tadakawa M., Takeda T., Li B., Tsuiji K., Yaegashi N. The anti-diabetic drug metformin inhibits vascular endothelial growth factor expression via the mammalian target of rapamycin complex 1/hypoxia-inducible factor-1α signaling pathway in ELT-3 cells. Mol. Cell. Endocrinol. 2015;399:1–8. doi: 10.1016/j.mce.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 26.Liu C., Wu J., Zhu J., Kuei C., Yu J., Shelton J., Sutton S.W., Li X., Yun S.J., Mirzadegan T., et al. Lactate Inhibits Lipolysis in Fat Cells through Activation of an Orphan G-protein-coupled Receptor, GPR81. J. Biol. Chem. 2009;284:2811–2822. doi: 10.1074/jbc.M806409200. [DOI] [PubMed] [Google Scholar]
- 27.Branco M., Linhares P., Carvalho B., Santos P., Costa B., Vaz R. Serum lactate levels are associated with glioma malignancy grade. Clin. Neurol. Neurosurg. 2019;186:105546. doi: 10.1016/j.clineuro.2019.105546. [DOI] [PubMed] [Google Scholar]
- 28.Shih C.-C., Lee T.-S., Tsuang F.-Y., Lin P.-L., Cheng Y.-J., Cheng H.-L., Wu C.-Y. Pretreatment serum lactate level as a prognostic biomarker in patients undergoing supratentorial primary brain tumor resection. Oncotarget. 2017;8:63715–63723. doi: 10.18632/oncotarget.18891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen L. Co-inhibitory molecules of the B7–CD28 family in the control of T-cell immunity. Nat. Rev. Immunol. 2004;4:336–347. doi: 10.1038/nri1349. [DOI] [PubMed] [Google Scholar]
- 30.Sharpe A.H., Freeman G.J. The B7–CD28 superfamily. Nat. Rev. Immunol. 2002;2:116–126. doi: 10.1038/nri727. [DOI] [PubMed] [Google Scholar]
- 31.Ashburn T.T., Thor K.B. Drug repositioning: Identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 2004;3:673–683. doi: 10.1038/nrd1468. [DOI] [PubMed] [Google Scholar]
- 32.Noto H., Goto A., Tsujimoto T., Noda M. Cancer Risk in Diabetic Patients Treated with Metformin: A Systematic Review and Meta-analysis. PLoS ONE. 2012;7:e33411. doi: 10.1371/journal.pone.0033411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morales D.R., Morris A.D. Metformin in Cancer Treatment and Prevention. Annu. Rev. Med. 2015;66:17–29. doi: 10.1146/annurev-med-062613-093128. [DOI] [PubMed] [Google Scholar]
- 34.Najafi M., Cheki M., Rezapoor S., Geraily G., Motevaseli E., Carnovale C., Clementi E., Shirazi A. Metformin: Prevention of genomic instability and cancer: A review. Mutat. Res. Toxicol. Environ. Mutagen. 2018;827:1–8. doi: 10.1016/j.mrgentox.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Zhang J., Hang C., Jiang T., Yi S., Shao W., Li W., Lin D. Nuclear Magnetic Resonance-Based Metabolomic Analysis of the Anticancer Effect of Metformin Treatment on Cholangiocarcinoma Cells. Front. Oncol. 2020;10:570516. doi: 10.3389/fonc.2020.570516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh S.V., Chaube B., Mayengbam S.S., Singh A., Malvi P., Mohammad N., Deb A., Bhat M.K. Metformin induced lactic acidosis impaired response of cancer cells towards paclitaxel and doxorubicin: Role of monocarboxylate transporter. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2020;1867:166011. doi: 10.1016/j.bbadis.2020.166011. [DOI] [PubMed] [Google Scholar]
- 37.Wei Y., Xu H., Dai J., Peng J., Wang W., Xia L., Zhou F. Prognostic Significance of Serum Lactic Acid, Lactate Dehydrogenase, and Albumin Levels in Patients with Metastatic Colorectal Cancer. BioMed Res. Int. 2018;2018:1804086. doi: 10.1155/2018/1804086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bharadwaj S., Venkatraghavan L., Mariappan R., Ebinu J., Meng Y., Khan O., Tung T., Reyhani S., Bernstein M., Zadeh G. Serum lactate as a potential biomarker of non-glial brain tumors. J. Clin. Neurosci. 2015;22:1625–1627. doi: 10.1016/j.jocn.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 39.Duan K., Liu Z.-J., Hu S.-Q., Huo H.-Y., Xu Z.-R., Ruan J.-F., Sun Y., Dai L.-P., Yan C.-B., Xiong W., et al. Lactic acid induces lactate transport and glycolysis/OXPHOS interconversion in glioblastoma. Biochem. Biophys. Res. Commun. 2018;503:888–894. doi: 10.1016/j.bbrc.2018.06.092. [DOI] [PubMed] [Google Scholar]
- 40.Ma L., Zong X. Metabolic Symbiosis in Chemoresistance: Refocusing the Role of Aerobic Glycolysis. Front. Oncol. 2020;10:5. doi: 10.3389/fonc.2020.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xie Q., Zhu Z., He Y., Zhang Z., Zhang Y., Wang Y., Luo J., Peng T., Cheng F., Gao J., et al. A lactate-induced Snail/STAT3 pathway drives GPR81 expression in lung cancer cells. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2019;1866:165576. doi: 10.1016/j.bbadis.2019.165576. [DOI] [PubMed] [Google Scholar]
- 42.Wang D.Y., McQuade J.L., Rai R.R., Park J., Zhao S., Ye F., Beckermann K.E., Rubinstein S.M., Johnpulle R., Long G., et al. The Impact of Nonsteroidal Anti-Inflammatory Drugs, Beta Blockers, and Metformin on the Efficacy of Anti-PD-1 Therapy in Advanced Melanoma. Oncologist. 2019;25:e602–e605. doi: 10.1634/theoncologist.2019-0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Afzal M.Z., Mercado R.R., Shirai K. Efficacy of metformin in combination with immune checkpoint inhibitors (anti-PD-1/anti-CTLA-4) in metastatic malignant melanoma. J. Immunother. Cancer. 2018;6:64. doi: 10.1186/s40425-018-0375-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scharping N., Menk A.V., Whetstone R.D., Zeng X., Delgoffe G.M. Efficacy of PD-1 Blockade Is Potentiated by Metformin-Induced Reduction of Tumor Hypoxia. Cancer Immunol. Res. 2016;5:9–16. doi: 10.1158/2326-6066.CIR-16-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cha J.-H., Yang W.-H., Xia W., Wei Y., Chan L.-C., Lim S.-O., Li C.-W., Kim T., Chang S.-S., Lee H.-H., et al. Metformin Promotes Antitumor Immunity via Endoplasmic-Reticulum-Associated Degradation of PD-L1. Mol. Cell. 2018;71:606–620.e7. doi: 10.1016/j.molcel.2018.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xue J., Li L., Li N., Li F., Qin X., Li T., Liu M. Metformin suppresses cancer cell growth in endometrial carcinoma by inhibiting PD-L1. Eur. J. Pharmacol. 2019;859:172541. doi: 10.1016/j.ejphar.2019.172541. [DOI] [PubMed] [Google Scholar]
- 47.Zhang Z., Li F., Tian Y., Cao L., Gao Q., Zhang C., Zhang K., Shen C., Ping Y., Maimela N.R., et al. Metformin Enhances the Antitumor Activity of CD8+ T Lymphocytes via the AMPK–miR-107–Eomes–PD-1 Pathway. J. Immunol. 2020;204:2575–2588. doi: 10.4049/jimmunol.1901213. [DOI] [PubMed] [Google Scholar]
- 48.Shergold A.L., Millar R., Nibbs R.J. Understanding and overcoming the resistance of cancer to PD-1/PD-L1 blockade. Pharmacol. Res. 2019;145:104258. doi: 10.1016/j.phrs.2019.104258. [DOI] [PubMed] [Google Scholar]
- 49.Zappasodi R., Serganova I., Cohen I.J., Maeda M., Shindo M., Senbabaoglu Y., Watson M.J., Leftin A., Maniyar R., Verma S., et al. CTLA-4 blockade drives loss of Treg stability in glycolysis-low tumours. Nature. 2021;591:652–658. doi: 10.1038/s41586-021-03326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.