Abstract
The impact of obesity on clinical outcomes following joint replacement procedures is resounding. Therefore, multiple strategies to achieve a substantial weight loss before surgery are needed in obese patients. The aim of the study was to test the effect of a fiber-enriched high carbohydrate (FEHC) diet on the reduction in body weight and pain in elderly obese patients undergoing total hip arthroplasty (THA). Sixty-one candidates for THA were included in our study. Prior to the procedure, the participants have been randomly assigned to a 3-month diet intervention (FEHC diet or free diet). Anthropometric measures and food questionnaires were collected at the enrollment and after 3 months. The Oxford Hip Score (OHS), the Hip disability and Osteoarthritis Outcome Score (HOOS) and the Western Ontario McMaster Universities OA Index (WOMAC) were administered at baseline and before surgery. A statistically significant variation of weight was found in the FEHC diet group (−3.7 kg, −4.4–−2.5) compared to the control group (−0.2 kg; −1.4–1.7; p < 0.0001), as well as significant improvements in the OHS (p < 0.0001), the HOOS (p < 0.0001) and the WOMAC (p < 0.0001) questionnaires. According to the results of the study, the FEHC diet in obese patients undergoing THA might help weight loss and improve related anthropometric parameters as well as hip function and pain.
Keywords: fiber, diet, total hip arthroplasty, total hip replacement, obesity, elderly
1. Introduction
Obesity is one of the preventable causes of death and accounts for over 2.5 million deaths annually worldwide [1]. The prevalence of obesity is expected to progressively rise with an increasing trend in the younger population. It is expected to determine an inevitable increase in hip osteoarthritis (OA) and an exponential increase in total hip arthroplasty (THA) procedures [2]. Indeed, the higher mechanical load in weight-bearing joints negatively impact on joint homeostasis [3]. Metabolic disorders and potential systemic mediators related to obesity might also contribute to joint degeneration and favor the development of OA [4,5].
THA is now the third most commonly performed operation in Western countries [6]. It involves the surgical remodeling of the hip to restore congruity, relieve pain and improve joint function. The demand for THA has increased over the years due to the proven success of these procedures to ameliorate the quality of life of patients [7]. Several conditions and risk factors are responsible for this increase, among which the most important are mechanical factors, including higher body mass index (BMI), traumatic injuries, malformations, heavy physical stress at work and aging [6].
Patients with a higher BMI have an increased risk of peri-operative complications, prolonged duration of surgery, extended rehabilitation, and convalescence, as well as various short-term complications, especially infections and dislocations [8,9,10,11,12], and a shortened duration of the prosthesis. Moreover, in terms of efficacy, overweight and obese patients seem to benefit from arthroplasty as much as non-obese patients, despite a slower recovery and lower function-related scores [13,14,15,16,17].
Therefore, weight loss in patients undergoing THA is desirable not only before surgery, but especially in the postoperative period. However, weight loss and lifestyle change are an insurmountable obstacle in people with obesity and diabetes [18]. Several studies have underlined the beneficial effects of preoperative dietary interventions on weight loss, the reduced risk of post-operative infections and improved glycemic control before total joint arthroplasty [19,20,21]. Over time, several dietary approaches for weight loss in people with obesity have been proposed, each one characterized by different contents of macronutrients. Several studies have confirmed the central role of a high-fiber diet in weight loss. Undoubtedly, the most important and recognized is the Mediterranean diet, characterized by high consumption of fruit, vegetables, nuts, cereals and olive oil, as well as a moderate consumption of fish and poultry and a low consumption of sweets, red meat and dairy products [22].
However, very few studies investigated the role of specific diet administration in the preoperative stage on reducing body weight and pain in elderly obese patients undergoing THA. Based on the proven beneficial effect of a high daily consumption of dietary fiber, the aim of this study was to assess the efficacy of a fiber-enriched high carbohydrate (FEHC) diet on reducing body weight, pain and hip function in elderly obese patients undergoing THA.
2. Materials and Methods
2.1. Patients
A cross sectional study was conducted at the Department of Orthopaedic and Trauma Surgery of the Campus Bio-Medico University Hospital, Rome, Italy. Patients aged between 65–85 years old, with a BMI > 30 kg/m2 and affected by primary hip OA and scheduled for THA were included in the study between 2019 and 2020. Patients suffering from secondary hip OA, femur neck fracture and osteonecrosis of the femoral head were excluded. The study protocol has been approved by the Ethical Committee of Campus Bio-Medico University of Rome.
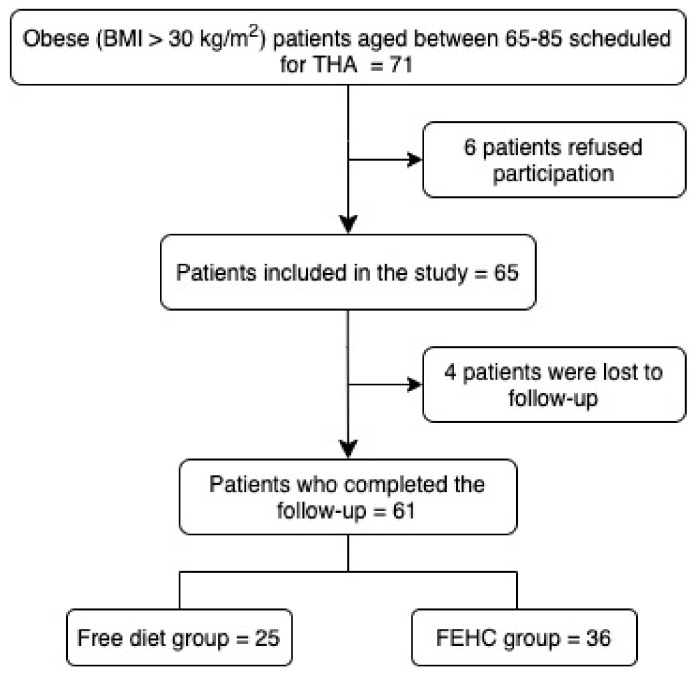
All patients were allocated in the following two groups using computer-generated random numbers (Microsoft Excel v. 16.48, Microsoft, Redmond, WA, USA) at the time of inclusion: (1) a free diet group and (2) an FEHC diet group. A total of 61 patients scheduled for THA were enrolled in the study, 36 in an FEHC group and 25 in the free diet group (Figure 1). Patients in the free diet group received general information about a healthy diet but not a specific diet, whereas individuals included in the FEHC diet group followed a specific diet for 3 months before surgery with controlled micronutrients and a restricted caloric content of 1700 kcal. The macronutrient composition was 72% from carbohydrates, 10% from vegetable proteins and 18% from fats. Complex carbohydrates (derived from whole grains, legumes, fruit, and vegetables) were 60% (255 g). Simple sugars (integrated with seasonal fresh fruit) were 12% of total carbohydrates (54 g). Daily fiber content was 40 g per 1000 kcal; animal products and or added sugars were not included.
Figure 1.
Patient inclusion flowchart.
2.2. Study Variables and Outcome Measurements
Age, gender, height, weight, and cholesterol level in a blood sample were annotated at the baseline on enrolment and at the follow-up visit after 3 months. BMI was calculated as weight (kg) divided by height squared (m2). Adherence to diet was investigated through a periodic monthly follow-up visit and a weekly telephone call.
Functional outcomes were assessed at the baseline after 3 months of dietary intervention with the Oxford Hip Score (OHS), the Hip disabilities and Osteoarthritis Outcome Score (HOOS) and the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index. OHS is a joint-specific patient-reported outcome measure tool to evaluate disability in patients undergoing THA (score range = 12–60) [23]. HOOS is a 40-item questionnaire to assess patient-relevant outcomes in five separate subscales (pain, symptoms, activity of daily living, sport and recreation function and hip related quality of life; score range = 0–100) [24]. The WOMAC Osteoarthritis Index is a self-administered questionnaire consisting of 24 items divided into the following 3 subscales: pain, stiffness, and physical function (score range = 0–96) [8]. In addition, the minimal clinically important difference (MCID) of the adopted scales was calculated using a distribution-based method [25].
2.3. Statistical Analysis
Statistical analyses were performed using Statistical Package for Social Science (SPSS) for Mac 26.0. Differences were considered significant at the p < 0.05 level. Data of continuous variables are presented as mean values ± standard deviation (SD). Median values with inter-quartile ranges were provided for non-normally distributed variables. Analysis of variance (ANOVA) for normally distributed variables was performed according to diet; otherwise, the nonparametric Mann–Whitney U H test was adopted. The two-tailed Fisher exact test was used for dichotomous variables. Eventually, body parameters and questionnaire scores were compared before and after the dietetic intervention by using the Wilcoxon signed-rank test.
3. Results
The mean age of the study population was 73 ± 6 years, and 36 (59%) were female. Additionally, 36 subjects were randomized to the FEHC diet, while 25 participants received the control free diet. The main characteristics of the population are shown in Table 1; specifically, the patients who followed the FEHC diet had significantly higher scores in the HOOS questionnaire at both baseline and follow-up times, and lower scores in the WOMAC questionnaire at follow-up as compared with the controls. The variations in body parameters and questionnaire scores from baseline to follow-up according to the FEHC diet are depicted in Table 2, while the improvement in body parameters and questionnaire scores according to the FEHC diet are described in Table 3.
Table 1.
Characteristics of the study population according to FEHC diet.
| FEHC Diet (n = 36) Mean (SD) or Median (IQR) or n (%) |
Free Diet (n = 25) Mean (SD) or Median (IQR) or n (%) |
p | |
|---|---|---|---|
| Age (years) | 74 (7) | 72 (6) | 0.146 |
| Gender (female) | 23 (64) | 13 (52) | 0.431 |
| Weight at baseline (kg) | 89.3 (80.0–100.2) | 91.5(84.0–95.6) | 0.889 |
| Weight at follow-up (kg) | 86.8 (74.5–95.5) | 89.0 (82.6–96.2) | 0.205 |
| BMI at baseline (kg/m2) | 33.4 (31.8–37.5) | 32.3 (30.9–34.3) | 0.070 |
| BMI at follow-up (kg/m2) | 31.7 (30.1–35.1) | 32.0 (30.8–33.8) | 0.832 |
| Total cholesterol at baseline (mg/dL) | 198 (40) | 202 (31) | 0.721 |
| Total cholesterol at follow-up (mg/dL) | 180 (28) | 203 (34) | 0.006 |
| OHS questionnaire baseline | 31 (27–44) | 37 (34–46) | 0.108 |
| OHS questionnaire follow-up | 38 (30–46) | 34 (29–41) | 0.199 |
| HOOS questionnaire baseline | 65 (53–88) | 32 (24–39) | <0.0001 |
| HOOS questionnaire follow-up | 65 (54–91) | 29 (23–31) | <0.0001 |
| WOMAC questionnaire baseline | 0.38 (0.32–0.47) | 0.39 (0.33–0.47) | 0.826 |
| WOMAC questionnaire follow-up | 0.37 (0.29–0.43) | 0.43 (0.37–0.49) | 0.005 |
Table 2.
Variation in anthropometric parameters and questionnaire scores from baseline (T0) to follow-up (T1) according to FEHC diet.
| FEHC Diet (n = 36) | Free Diet (n = 25) | p | |
|---|---|---|---|
| Weight (kg) | −3.7 (−4.4–−2.5) | −0.2 (−1.4–1.7) | <0.0001 |
| BMI (kg/m2) | −1.5 (−2.0–−0.8) | 0.1 (−0.7–1.2) | <0.0001 |
| Total cholesterol (mg/dL) | 18 (7–33) | −9 (−12–−2) | <0.0001 |
| OHS questionnaire | 3 (2–7) | −4 (−10–0) | <0.0001 |
| HOOS questionnaire | 1 (−1–2) | −3 (−4–−2) | <0.0001 |
| WOMAC questionnaire | −0.05 (−0.05–−0.02) | 0.03 (0.02–0.05) | <0.0001 |
Table 3.
Improvement in body parameters and questionnaire scores according to FEHC diet.
| FEHC Diet (n = 36) n (%) |
Free Diet (n = 25) n (%) |
p | |
|---|---|---|---|
| Weight loss | 35 (97) | 14 (56) | <0.0001 |
| BMI loss | 35 (97) | 14 (56) | <0.0001 |
| Reduced total cholesterol | 32 (89) | 5 (20) | <0.0001 |
| OHS questionnaire | 31 (86) | 6 (24) | <0.0001 |
| HOOS questionnaire | 24 (67) | 3 (12) | <0.0001 |
| WOMAC questionnaire | 18 (50) | 1 (4) | <0.0001 |
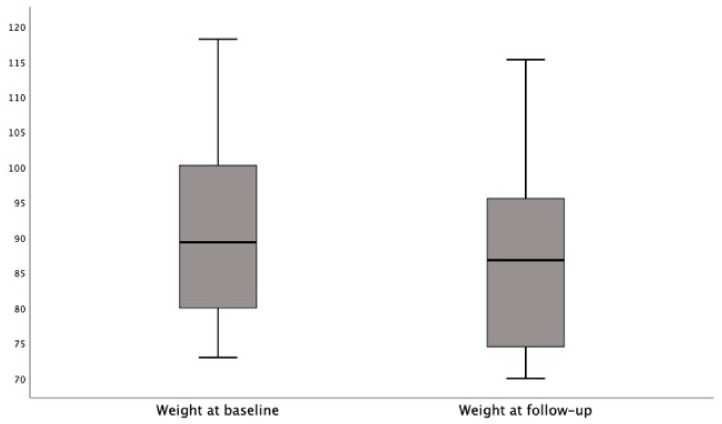
The Wilcoxon signed-rank test indicated that the follow-up weight medians were significantly lower than the baseline medians in the participants on the FEHC diet (Z = −5.1; p < 0.0001. Figure 2); conversely, the weight medians did not differ from baseline to follow-up in the participants on the free diet (Z = −0.3; p = 777).
Figure 2.
The follow-up weight medians were significantly lower than the baseline medians in participants on FEHC diet.
The Wilcoxon signed-rank test indicated that the follow-up BMI medians were significantly lower than the baseline medians in the participants on the FEHC diet (Z = −5.2; p < 0.0001); conversely, the weight medians did not differ from baseline to follow-up in the participants on the free diet (Z = 0.6; p = 954). The Wilcoxon signed-rank test indicated that the follow-up OHS scores (median 38) were significantly higher than the baseline scores (median: 31) in the participants on the FEHC diet (Z = 4.2; p <0.0001); conversely, the follow-up OHS scores (median: 34) were significantly lower than the baseline scores (median: 37) in the participants on the free diet (Z = −3.0; p = 0.002).
The Wilcoxon signed-rank test indicated that the follow-up HOOS scores were significantly higher than the baseline scores in the participants on the FEHC diet (Z = 2.1; p = 0.033); conversely, the follow-up HOOS scores were significantly lower than the baseline scores in the participants on the free diet (Z = −3.6; p < 0.0001).
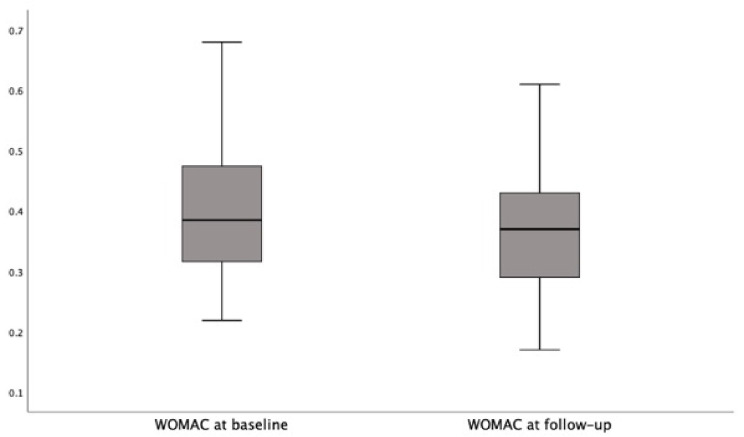
The Wilcoxon signed-rank test indicated that the follow-up WOMAC scores (median: 0.37) were significantly lower than the baseline scores (median: 0.38) in the participants on the FEHC diet (Z = −5.1; p < 0.0001. Figure 3); conversely, the follow-up WOMAC scores (median 0.43) were significantly higher than the baseline scores (median: 0.39) in the participants on the free diet (Z = 4.2; p < 0.0001).
Figure 3.
The follow-up WOMAC scores in participants on FEHC diet.
Additionally, MCID calculation documented a small effect (Table 4).
Table 4.
Range of scores and minimal clinically important differences (MCIDs) of adopted scales.
| Range of Score | MCID | |
|---|---|---|
| OHS questionnaire | 12–60 | 0.12 |
| HOOS questionnaire | 0–100 | 0.45 |
| WOMAC questionnaire | 0–96 | 0.10 |
4. Discussion
In this study, we found a close correlation (p < 0.001) between the use of the FEHC diet and the improvement of anthropometric parameters. The FEHC diet, in three months of administration, produced a significant reduction in body weight and BMI compared to the free diet group. The FEHC diet led to an improvement in OHS (p < 0.0001), HOOS (p < 0.0001) and WOMAC (p < 0.0001) scores even before undergoing THA, suggesting the efficacy of weight loss in the optimization of hip symptoms and motility. Nevertheless, dietary intervention in our population had only small effects considering the MCID results. However, it is possible that the short follow up might contribute to these data.
Obesity and OA are two interconnected healthcare problems affecting a large proportion of the adult population worldwide. The increasing weight of the population will lead to nearly 1.3 billion and 573 million adults being overweight and obese by 2030, respectively. Moreover, OA increases as the population ages, representing a leading cause of chronic pain and disability among older people [26].
Considering the high impact of obesity on the complication rate and outcomes, weight loss is warmly encouraged before THA, as a decrease in body weight > 10% is associated with improved pain and functional scores [27]. In some cases where rapid and consistent weight loss is desirable, bariatric surgery has been employed to optimize morbidly obese patients before THA. However, a meta-analysis from Smith et al. [28] reported that preoperative bariatric surgery did not improve the risk of infection, deep venous thrombosis, pulmonary embolism, and revision surgery. Therefore, the role of bariatric surgery for managing obesity before THA surgery remains controversial.
Obesity leads to low-grade systemic inflammation, and weight reduction can reduce adipose tissue and restore normal secretion patterns [29,30].
The reduction in pain may be associated with a reduction in weight (an important risk factor for OA in the lower joints for increasing the biomechanical stress) and a modification of the inflammation parameters that seem to increase hip OA [2].
Several studies have found a clear relationship between weight loss in obese adults and pain reduction. In the guidelines from the American College of Rheumatology [31] and European League Against Rheumatism [32], weight loss and physical exercise are recommended in overweight or obese patients with OA.
Lui et al. investigated the effect of non-surgical, non-pharmacological weight loss interventions in patients who are obese prior to THA. The authors concluded that there is insufficient evidence to support the recommendation that patients who are obese lose weight (≥5%) within the year prior to THA [19].
In a systematic review, Seward et al. investigated preoperative nonsurgical weight loss interventions before THA and knee arthroplasty. The conclusion of this study is that the available evidence indicates that short-term, nonsurgical, preoperative weight loss interventions before THA can produce statistically significant weight loss and a decreased BMI that may help some patients with severe obesity achieve a BMI below the standard 40 kg/m2 cut-off for surgery. However, it remains unknown if the amount of weight loss from these interventions is clinically significant and sufficient to improve outcomes after THA [20].
The role of fiber in the regulation of body weight has already been discussed in the literature. Dietary fiber is defined as an enzymatically undegradable and non-absorbable component of the diet. Fibers can be mainly divided into the two different types: soluble and insoluble. The difference is essentially in the capacity of the fiber itself to dissolve in water; indeed, most vegetables contain both types with different proportions [33].
Experimental studies have shown how a diet rich in fiber reduces the absorption of free fatty acids by using them as energy in the fermentation process of the fibers in the intestine. In addition, dietary fibers have the ability to retain water; this leads to a lowering of the energy/weight ratio of the ingested food, stimulating the sense of satiety despite a reduced energy intake and, thus, reducing voluntary food intake [34,35].
Many physiological mechanisms of the action of dietary fiber in weight loss have been studied. Fiber appears to reduce food intake through the increased effort and time it takes to chew it [36]. In a study by Birketvedt et al., the addition of dietary fiber in a low-calorie diet significantly improved weight loss, with the placebo group presenting a 5.8 kg weight reduction compared to an 8.0 kg weight reduction in the group with fiber supplementation [37]. Studies of postmenopausal women have also shown that the introduction of a higher fiber content within a very low-fat diet increases weight loss [38]. In a study by Te Morenga et al., a diet rich in fiber was demonstrated to reduce hunger and increase patient compliance compared to a protein-rich diet. Moreover, besides having a statistically significant effect on body weight or comparable to the latter, it has shown an important association with a reduction in blood pressure [39]. A key aspect of a higher fiber diet is also linked to a reduction in cholesterol levels. In a study published in the Journal Of The American College Of Nutrition [40], a diet rich in fiber was shown to reduce low-density lipoprotein (LDL) cholesterol levels not only in dyslipidemic patients, but also in normolipidemic subjects. These aspects have also been correlated with the risk of coronary events: in a study by Anderson et al., a clear inversely proportional relationship was demonstrated between the amount of soluble fiber introduced with the diet and the incidence of coronary events [41].
This study has some limitations. The first limitation was related to randomization, and this produced a selection bias in the enrollment of the patients that was clear in the significant difference in the HOOS score. Additionally, no data regarding the sub-score of the adopted scales were recorded; thus, only the total final scores were shown. Ultimately, we cannot determine the adherence to the diet; however, this is issue is common in most studies on diet. Even though the baseline and follow-up weights indicated that the high-fiber diet does not produce any significant weight loss as compared to the free diet, the intra-group variation was significant; this might reflect an insufficient sample size. Thus, further, larger studies are needed to support our hypotheses.
5. Conclusions
The present study has shown that the administration of an FEHC diet may promote an improvement of body weight and BMI in obese elderly patients with hip OA scheduled for THA. Indeed, the patients who followed an FEHC diet for three months lost weight and improved their clinical scores before surgery. Indeed, losing weight is crucial in order to avoid surgical complications as well as boost the postoperative recovery. Therefore, a dietary approach based on an FEHC diet for obese elderly patients may be successful to lose weight and improve clinical outcomes in this specific subset of patients. Although, after three months of the diet, the follow up BMI and weight did not differ significantly in the two groups; there was an improvement in cholesterol and on the WOMAC questionnaire that investigates symptoms such as pain, stiffness, and functional autonomy.
Author Contributions
Conceptualization, F.C., C.B. and N.N.; methodology, A.L.; supervision, G.V., R.P. and N.N.; validation, F.C., F.R. and G.V.; visualization, G.V.; writing—original draft, F.C., F.R. and L.A.; writing—review and editing, F.C., A.L., M.E.C., F.R., L.A., G.V., C.B. and G.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Campus Bio-Medico University of Rome (protocol code 42/18 PAR ComEt CBM, 19/06/2018).
Informed Consent Statement
Every patient signed an informed consent before inclusion.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lupoli R., Lembo E., Saldalamacchia G., Avola C.K., Angrisani L., Capaldo B. Bariatric surgery and long-term nutritional issues. World J. Diabetes. 2017;8:464–474. doi: 10.4239/wjd.v8.i11.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gandhi R., Wasserstein D., Razak F., Davey J.R., Mahomed N.N. BMI independently predicts younger age at hip and knee replacement. Obesity. 2010;18:2362–2366. doi: 10.1038/oby.2010.72. [DOI] [PubMed] [Google Scholar]
- 3.Inacio M.C., Kritz-Silverstein D., Paxton E.W., Fithian D.C. Do patients lose weight after joint arthroplasty surgery? A systematic review. Clin. Orthop. Relat Res. 2013;471:291–298. doi: 10.1007/s11999-012-2537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kluzek S., Newton J.L., Arden N.K. Is osteoarthritis a metabolic disorder? Br. Med. Bull. 2015;115:111–121. doi: 10.1093/bmb/ldv028. [DOI] [PubMed] [Google Scholar]
- 5.Cannata F., Vadala G., Ambrosio L., Napoli N., Papalia R., Denaro V., Pozzilli P. Osteoarthritis and type 2 diabetes: From pathogenetic factors to therapeutic intervention. Diabetes Metab. Res. Rev. 2020;36:e3254. doi: 10.1002/dmrr.3254. [DOI] [PubMed] [Google Scholar]
- 6.Harris E.C., Coggon D. HIP osteoarthritis and work. Best Pract. Res. Clin. Rheumatol. 2015;29:462–482. doi: 10.1016/j.berh.2015.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robinson P.D., McEwan J., Adukia V., Prabhakar M. Osteoarthritis and arthroplasty of the hip and knee. Br. J. Hosp. Med. 2018;79:C54–C59. doi: 10.12968/hmed.2018.79.4.C54. [DOI] [PubMed] [Google Scholar]
- 8.Haverkamp D., Klinkenbijl M.N., Somford M.P., Albers G.H., van der Vis H.M. Obesity in total hip arthroplasty—does it really matter? A meta-analysis. Acta Orthop. 2011;82:417–422. doi: 10.3109/17453674.2011.588859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huddleston J.I., Wang Y., Uquillas C., Herndon J.H., Maloney W.J. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin. Orthop. Relat Res. 2012;470:490–496. doi: 10.1007/s11999-011-1967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y., Morshed S., Joseph T., Bozic K., Ries M.D. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin. Orthop. Relat Res. 2006;453:142–146. doi: 10.1097/01.blo.0000238874.09390.a1. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy J.W., Young D., Meek D.R.M., Patil S.R. Obesity is associated with higher complication rates in revision total hip arthroplasty. J. Orthop. 2018;15:70–72. doi: 10.1016/j.jor.2018.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Namba R.S., Paxton L., Fithian D.C., Stone M.L. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J. Arthroplast. 2005;20:46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 13.Davis A.M., Wood A.M., Keenan A.C., Brenkel I.J., Ballantyne J.A. Does body mass index affect clinical outcome post-operatively and at five years after primary unilateral total hip replacement performed for osteoarthritis? A multivariate analysis of prospective data. J. Bone Joint Surg. Br. 2011;93:1178–1182. doi: 10.1302/0301-620X.93B9.26873. [DOI] [PubMed] [Google Scholar]
- 14.Jackson M.P., Sexton S.A., Yeung E., Walter W.L., Walter W.K., Zicat B.A. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J. Bone Joint Surg. Br. 2009;91:1296–1300. doi: 10.1302/0301-620X.91B10.22544. [DOI] [PubMed] [Google Scholar]
- 15.Jones C.A., Cox V., Jhangri G.S., Suarez-Almazor M.E. Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthr. Cartil. 2012;20:511–518. doi: 10.1016/j.joca.2012.02.637. [DOI] [PubMed] [Google Scholar]
- 16.Lubbeke A., Stern R., Garavaglia G., Zurcher L., Hoffmeyer P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327–334. doi: 10.1002/art.22542. [DOI] [PubMed] [Google Scholar]
- 17.McCalden R.W., Charron K.D., MacDonald S.J., Bourne R.B., Naudie D.D. Does morbid obesity affect the outcome of total hip replacement? An analysis of 3290 THRs. J. Bone Joint Surg. Br. 2011;93:321–325. doi: 10.1302/0301-620X.93B3.25876. [DOI] [PubMed] [Google Scholar]
- 18.Cannata F., Vadala G., Russo F., Papalia R., Napoli N., Pozzilli P. Beneficial Effects of Physical Activity in Diabetic Patients. J. Funct. Morphol. Kinesiol. 2020;5:70. doi: 10.3390/jfmk5030070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lui M., Jones C.A., Westby M.D. Effect of non-surgical, non-pharmacological weight loss interventions in patients who are obese prior to hip and knee arthroplasty surgery: A rapid review. Syst. Rev. 2015;4:121. doi: 10.1186/s13643-015-0107-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seward M.W., Briggs L.G., Bain P.A., Chen A.F. Preoperative Nonsurgical Weight Loss Interventions Before Total Hip and Knee Arthroplasty: A Systematic Review. J. Arthroplast. 2021 doi: 10.1016/j.arth.2021.06.021. [DOI] [PubMed] [Google Scholar]
- 21.Drost J.M., Cook C.B., Spangehl M.J., Probst N.E., Mi L., Trentman T.L. A Plant-Based Dietary Intervention for Preoperative Glucose Optimization in Diabetic Patients Undergoing Total Joint Arthroplasty. Am. J. Lifestyle Med. 2019:1559827619879073. doi: 10.1177/1559827619879073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trichopoulou A., Martinez-Gonzalez M.A., Tong T.Y., Forouhi N.G., Khandelwal S., Prabhakaran D., Mozaffarian D., de Lorgeril M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014;12:112. doi: 10.1186/1741-7015-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wylde V., Learmonth I.D., Cavendish V.J. The Oxford hip score: The patient’s perspective. Health Qual. Life Outcomes. 2005;3:66. doi: 10.1186/1477-7525-3-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nilsdotter A.K., Lohmander L.S., Klassbo M., Roos E.M. Hip disability and osteoarthritis outcome score (HOOS)—Validity and responsiveness in total hip replacement. BMC Musculoskelet. Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wyrwich K.W., Bullinger M., Aaronson N., Hays R.D., Patrick D.L., Symonds T. Estimating clinically significant differences in quality of life outcomes. Qual. Life Res. 2005;14:285–295. doi: 10.1007/s11136-004-0705-2. [DOI] [PubMed] [Google Scholar]
- 26.Reyes C., Leyland K.M., Peat G., Cooper C., Arden N.K., Prieto-Alhambra D. Association Between Overweight and Obesity and Risk of Clinically Diagnosed Knee, Hip, and Hand Osteoarthritis: A Population-Based Cohort Study. Arthritis Rheumatol. 2016;68:1869–1875. doi: 10.1002/art.39707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NICE Joint Replacement (Primary): Hip, Knee and Shoulder. [(accessed on 28 May 2021)]. Available online: www.nice.org.uk/guidance/ng157.
- 28.Smith T.O., Aboelmagd T., Hing C.B., MacGregor A. Does bariatric surgery prior to total hip or knee arthroplasty reduce post-operative complications and improve clinical outcomes for obese patients? Systematic review and meta-analysis. Bone Joint J. 2016;98-B:1160–1166. doi: 10.1302/0301-620X.98B9.38024. [DOI] [PubMed] [Google Scholar]
- 29.Hauner H. Secretory factors from human adipose tissue and their functional role. Proc. Nutr. Soc. 2005;64:163–169. doi: 10.1079/PNS2005428. [DOI] [PubMed] [Google Scholar]
- 30.Thomas S., Browne H., Mobasheri A., Rayman M.P. What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology. 2018;57:iv61–iv74. doi: 10.1093/rheumatology/key011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hochberg M.C., Altman R.D., April K.T., Benkhalti M., Guyatt G., McGowan J., Towheed T., Welch V., Wells G., Tugwell P., et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64:465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 32.Fernandes L., Hagen K.B., Bijlsma J.W., Andreassen O., Christensen P., Conaghan P.G., Doherty M., Geenen R., Hammond A., Kjeken I., et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann. Rheum. Dis. 2013;72:1125–1135. doi: 10.1136/annrheumdis-2012-202745. [DOI] [PubMed] [Google Scholar]
- 33.Slavin J. Fiber and prebiotics: Mechanisms and health benefits. Nutrients. 2013;5:1417–1435. doi: 10.3390/nu5041417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howarth N.C., Saltzman E., Roberts S.B. Dietary fiber and weight regulation. Nutr. Rev. 2001;59:129–139. doi: 10.1111/j.1753-4887.2001.tb07001.x. [DOI] [PubMed] [Google Scholar]
- 35.Slavin J.L. Dietary fiber and body weight. Nutrition. 2005;21:411–418. doi: 10.1016/j.nut.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 36.Clark M.J., Slavin J.L. The effect of fiber on satiety and food intake: A systematic review. J. Am. Coll. Nutr. 2013;32:200–211. doi: 10.1080/07315724.2013.791194. [DOI] [PubMed] [Google Scholar]
- 37.Birketvedt G.S., Aaseth J., Florholmen J.R., Ryttig K. Long-term effect of fibre supplement and reduced energy intake on body weight and blood lipids in overweight subjects. Acta Med. (Hradec Kralove) 2000;43:129–132. doi: 10.14712/18059694.2019.126. [DOI] [PubMed] [Google Scholar]
- 38.Mueller-Cunningham W.M., Quintana R., Kasim-Karakas S.E. An ad libitum, very low-fat diet results in weight loss and changes in nutrient intakes in postmenopausal women. J. Am. Diet. Assoc. 2003;103:1600–1606. doi: 10.1016/j.jada.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 39.Te Morenga L.A., Levers M.T., Williams S.M., Brown R.C., Mann J. Comparison of high protein and high fiber weight-loss diets in women with risk factors for the metabolic syndrome: A randomized trial. Nutr. J. 2011;10:40. doi: 10.1186/1475-2891-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ullrich I.H. Evaluation of a high-fiber diet in hyperlipidemia: A review. J. Am. Coll. Nutr. 1987;6:19–25. doi: 10.1080/07315724.1987.10720161. [DOI] [PubMed] [Google Scholar]
- 41.Surampudi P., Enkhmaa B., Anuurad E., Berglund L. Lipid Lowering with Soluble Dietary Fiber. Curr. Atheroscler. Rep. 2016;18:75. doi: 10.1007/s11883-016-0624-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.