Abstract
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has unmasked mankind’s vulnerability to biological threats. Although higher age is a major risk factor for disease severity in COVID-19, several predisposing risk factors for mortality are related to low cardiorespiratory and metabolic fitness, including obesity, cardiovascular disease, diabetes, and hypertension. Reaching physical activity (PA) guideline goals contribute to protect against numerous immune and inflammatory disorders, in addition to multi-morbidities and mortality. Elevated levels of cardiorespiratory fitness, being non-obese, and regular PA improves immunological function, mitigating sustained low-grade systemic inflammation and age-related deterioration of the immune system, or immunosenescence. Regular PA and being non-obese also improve the antibody response to vaccination. In this review, we highlight potential physiological, cellular, and molecular mechanisms that are affected by regular PA, increase the host antiviral defense, and may determine the course and outcome of COVID-19. Not only are the immune system and regular PA in relation to COVID-19 discussed, but also the cardiovascular, respiratory, renal, and hormonal systems, as well as skeletal muscle, epigenetics, and mitochondrial function.
Keywords: virus, immunology, physical activity, exercise, health, COVID-19, SARS-CoV-2, obesity
1. Introduction
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), rapidly increased to pandemic magnitude during the first quarter of 2020 [1]. The severity of COVID-19 appears to be a net consequence of the combination of SARS-CoV-2 infection and the person’s cardiorespiratory and metabolic fitness, age, sex, and ethnicity [2,3,4,5,6]. Some individuals who become infected with SARS-CoV-2 present with mild or no symptoms of illness, whereas others become critically ill and dependent on intensive care with a poor prognosis [7].
The physiological and cellular factors that interact and determine an individual’s vulnerability to SARS-CoV-2 remain to be determined. Research has highlighted several predisposing risk factors for mortality in COVID-19, many of which are related to low cardiorespiratory and metabolic fitness, including obesity, cardiovascular disease (CVD), diabetes [2,4,8,9,10], and metabolic syndrome (MetS) [11]. It is reasonable to assume that a physically active lifestyle results in physiological and molecular stress-induced adaptations in all tissues affected by exercise, which may be protective following SARS-CoV-2 infection, in contrast to the sedentary lifestyle associated with obesity [12].
The objective of this narrative review is to highlight potential physiological, cellular, and molecular mechanisms affected by regular physical activity (PA) and exercise that may regulate antiviral defenses and determine the course and outcome of COVID-19. First, we aim to explain the deterioration of fitness due to physical inactivity and sedentariness. Second, the biology of SARS-CoV-2 is briefly reviewed. Finally, we aim to illuminate the physiological and cellular effects of exercise on fitness and the potential of exercise as a protective measure against severe complications induced by SARS-CoV-2 infection. In addition to the immune system, also the cardiovascular, respiratory, renal, and hormonal systems, as well as skeletal muscle, epigenetics, and mitochondrial function in relation to regular PA and antiviral defense is discussed in novel aspects.
2. Definitions
PA is defined as any bodily movement generated by the contraction of skeletal muscles that raises energy expenditure above resting metabolic rate [13]. Exercise is a subcategory of PA that is planned and structured, favoring physical fitness. The World Health Organization (WHO) recommends either 150–300 min of moderate-intensity (3–6 metabolic equivalents, 1 metabolic equivalent = 3.5 mL of O2 per kg of body weight per minute) or 75–150 min of vigorous-intensity (>6 metabolic equivalents) PA per week for adults [14]. To confer additional health benefits, 300 min of moderate-intensity or 150 min of vigorous-intensity PA per week is suggested. Being physically active entails fulfilling these guidelines and not fulfilling them is considered being physically inactive [15]. Sedentary behavior is defined as any waking behavior with an energy expenditure ≤ 1.5 metabolic equivalents while sitting or lying. Consequently, a person can be physically active and still be classified as sedentary.
3. Fitness and Health Status, Immunity, and Infection
A sedentary lifestyle with obesity or MetS increases the risk of severe disease due to viral infections [16,17]. In contrast, PA elicits protective effects against both bacterial and viral infections [18,19,20,21]. How this knowledge can be extrapolated to COVID-19 is yet to be determined. However, emerging data indicate that obesity, diabetes, and MetS are some of the major risk factors associated with COVID-19 severity and mortality [4,8,22,23,24]. Although obesity is closely associated with all features of MetS, including abdominal adiposity, hypertension, dyslipidemia, and insulin resistance [25,26], PA and fair cardiorespiratory fitness are significant factors that counteract MetS, even in obese individuals [27]. Risk factors linked to obesity are more or less treatable with exercise [28], and epidemiological research has clearly shown that regular PA decreases the risk of comorbidities and all-cause mortality [29,30]. Common to several of the aforementioned risk factors and comorbidities are sustained low-grade systemic inflammation, characterized by increased levels of proinflammatory cytokines and disturbed regulation of fibrinolysis [31]. In this context, PA and exercise, or the lack thereof, play an important role in wide-ranging effects on brain, cardiorespiratory, metabolic, endocrine, muscular, and immunological functions.
4. Deterioration of Fitness Status during a Short Period of Physical Inactivity
Lockdowns and restrictions have affected the majority of humanity during the COVID-19 pandemic. Protective measures aiming to slow the spread of COVID-19 have affected the possibilities for PA and exercise according to data retrieved from activity trackers and mobile phones from all over the world [32,33]. These temporary restrictions have negatively affected the already ongoing crises of physical inactivity and obesity frequently addressed during the COVID-19 pandemic [34,35,36]. Longitudinal studies have shown that, in some cohorts, COVID-19 lockdowns led to an increase in body weight, snacking, and the consumption of ultra-processed foods, whereas activity decreased [37].
Physical inactivity and sedentary time are associated with multiple chronic diseases and premature mortality and contribute to a major economic burden worldwide [38]. Physical inactivity has been indicated to be the cause of 9% of deaths worldwide [39]. Physical inactivity plays a role, independent of other factors, in lowering cardiovascular and muscular fitness and, thus, the age of onset of chronic disease, decreasing the quality of life and shortening the health span [40]. Total sitting time, independent of PA, is associated with a higher risk of several major chronic diseases and all-cause mortality [41]. Physical inactivity and sedentary time are also substantial predictors of hospitalization and have been described as the central driver of mortality risk in longitudinal studies [42]. In contrast, increased PA at any intensity, of any duration, and less time spent being sedentary are associated with a reduced risk of premature mortality [30]. In terms of PA, doing something is better than doing nothing [29,30]; although more is better, a small dose of PA corresponding to 75 min per week, below current recommendations, substantially reduces mortality [43].
Changes in PA patterns are quickly reflected in human physiology. This is exemplified by the effects of 2 weeks of a reduced step count, which deteriorated multiorgan insulin sensitivity and muscle mass, and increased central and liver adiposity and dyslipidemia [44,45]. In the short term, prolonged sitting time negatively impacts metabolic markers, which is attenuated by PA [46]. Notably, from the perspective of COVID-19, physical inactivity per se is associated with low-grade systemic inflammation [47], which is further exacerbated by obesity [48], abdominal obesity in particular [49]. Undoubtedly, this is a major concern given restrictions, general mobility, and PA during the COVID-19 pandemic.
Accordingly, physical inactivity and a sedentary lifestyle are linked to an increase in all-cause mortality, and just a few days of being sedentary is sufficient to induce negative effects on metabolism, cardiorespiratory fitness, and skeletal muscle fitness.
5. SARS-CoV-2 and COVID-19
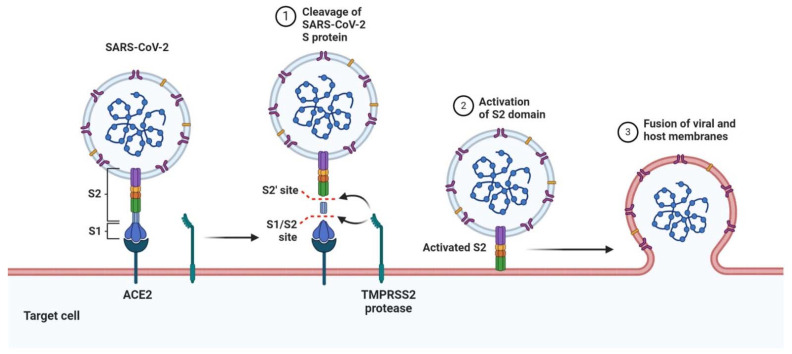
SARS-CoV-2 belongs to the Coronaviridae family within the order of Nidovirales. It transmits between humans mainly through droplets, but also via contact and/or aerosols [50]. The virus mainly targets the respiratory tract, but in some patients with severe illness, the virus disseminates to other organs, including the heart, liver, brain, kidneys [51], and intestine [52]. Infectious virions are equipped with a positive sense, single-stranded RNA genome that is unusually large compared to other RNA viruses. The genome encodes several non-structural and structural proteins, including the receptor-binding spike (S) protein, membrane (M) protein, envelope (E) protein, and a nucleocapsid (N) protein [53]. The cell and tissue tropism appear to be largely, but not entirely, dependent on the expression of the entry receptor angiotensin-converting enzyme 2 (ACE2), as well as cellular proteases, including TMPRSS2 [54]. Neutralizing antibodies mainly target the S protein, which contains a relatively high level of N-linked glycans compared to receptor-binding viral glycoproteins of other viruses [55]. These glycans partially protect the S protein from neutralizing antibodies. To interact with the ACE2 receptor, proteases, including TMPRSS2, cleave and activate the S protein, which undergoes a conformational change, resulting in exposure of the receptor-binding domain and facilitating a high-affinity interaction with ACE2 (Figure 1) [52,54,56,57].
Figure 1.
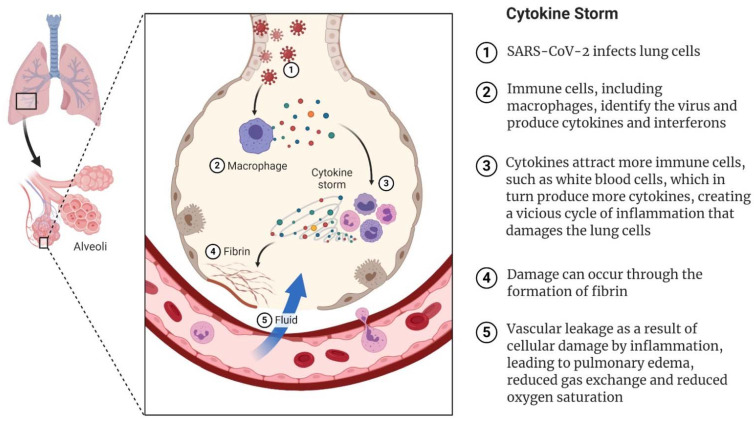
How SARS-CoV-2 can trigger the cytokine storm leading to severe COVID-19. The virus infects lung epithelial cells and is detected by resident macrophages, which trigger the production of interferons and cytokines. When more immune cells are attracted, more cytokines are produced, leading to a cytokine storm. Cell damage can occur via the formation of fibrin and weakened blood vessels, leading to fluid accumulation in the alveoli, respiratory failure, and general deterioration of organ function.
Recent studies suggest that heparan sulfate [58] and neuropilin 1 [59] are additional host factors that can be used for attachment and cell entry by SARS-CoV-2 in addition to ACE2 and TMPRSS2, which together contribute to and regulate SARS-CoV-2 infection and tissue-tropism. Infection also activates innate immunity, which consumes additional energy. After cell entry, SARS-CoV-2 downregulates the expression of ACE2 [60]. This contributes to reduced uptake of more virus, but also inflammation and blood flow, potentially leading to multiorgan failure due to the overactivation of angiotensin (Ang) II [61]. Of significant interest here is the consequence of the physiological-cellular Ang II-ACE-ACE2 interaction following SARS-CoV-2 infection from the perspective of exercise versus MetS.
COVID-19 mostly affects the respiratory system, although multiple extrapulmonary manifestations are common [62]. The initial infection of epithelial cells and the sequential pulmonary capillary endothelial cell infection prompt an influx of inflammatory cells, causing endothelialitis, alveolar wall thickening, and hyaline membrane formation, which are visualized at autopsy [63,64]. Interstitial infiltrates of leukocytes and edema create the typical ground-glass opacities seen on computer tomography. Ultimately, pneumonia vascular leakage and fluid accumulation lead to pulmonary edema, respiratory failure, hypoxia, and hypercapnia (Figure 2). Some critically ill patients develop fulminant acute respiratory distress syndrome (ARDS), septic shock, or multiorgan failure, and respiratory failure is the leading cause of death in patients with COVID-19 [65,66].
Figure 2.
Mechanism of SARS-CoV-2 viral entry. Receptor-binding spike (S) protein engages with the host ACE2 receptor. TMPRSS2 cleaves and activates the S protein, which undergoes a conformational change, facilitating interaction with the host ACE2, driving the fusion of viral and host membranes. Recent studies also suggest that the S protein interacts with cellular heparan sulfate adjacent to the ACE2-binding site (not depicted).
Pneumonia caused by SARS-CoV-2 is often accompanied by increased levels of C reactive protein (CRP), equivalent to those seen in bacterial pneumonia, and the secretion of hyaluronan, which affects oxygenation [67]. Some patients develop a hyperinflammatory syndrome and coagulopathy with a prothrombotic state. Thrombotic complications include both arterial and venous manifestations [62]. Critically ill patients have very high levels of inflammatory markers, such as CRP, erythrocyte sedimentation rate, fibrinogen, ferritin, interleukin (IL)-1, IL-6, and D-dimer. Leukocytosis is rarely seen, and lymphocytopenia is common. High levels of CRP and D-dimer and low lymphocyte counts are associated with poorer prognosis and death [68,69]. Disseminated intravasal coagulation (DIC) is a frequent occurrence [70]. However, COVID-19-associated hypercoagulopathy is dominated by thrombosis, whereas bleeding is the most prominent feature of DIC. The presence of endotheliopathy has been reported in COVID-19 and is likely associated with critical illness and death [62]. A subgroup of patients develops a cytokine storm syndrome, with unrestrained release of cytokines and devastating consequences for the host (Figure 2). Cytokine storm and hypercoagulopathy lead to destruction of the lungs, multiorgan failure, and thrombotic tendencies, with micro-thrombosis of the lungs further exacerbating lung tissue destruction. Immune-mediated lung injury (e.g., DIC and ARDS) is associated with adverse outcomes in patients with COVID-19 [63]. The hyperinflammatory response to the infection may be responsible for many of the commonly seen complications of the disease, such as lung damage, kidney failure, cardiovascular complications, neurological problems, and liver damage [71].
Redox regulators, mitochondrial factors, and non-coding RNAs are host factors affected by exercise and may dictate the outcome of SARS-CoV-2 infection [72]. PA and exercise induce several lines of stress, followed by adaptations if the exercise is repeated over time [28]. The adaptations are specific to the type, volume, and intensity of training and include physiological and cellular adaptations in many organs [73,74,75,76]. Some adaptive responses to stress following exercise include neuromuscular, respiratory, cardiovascular, hormonal, immunological, and cellular adaptations that improve or maintain factors that affect endurance, strength, and mobility, as well as health. In this context, the cellular and physiological mechanisms that determine the outcome of COVID-19, the effects of PA, and fitness state are of interest when examining differences in the impact of the virus in young vs. elderly, and in men vs. women as noted in epidemiological studies [4].
6. Effects of Physical Activity and Exercise on Human Biology in View of COVID-19
Epidemiological studies have shown that regular PA reduces the incidence of bacterial and viral infection across an individual’s lifespan and decreases the mortality and incidence of influenza and pneumonia [77,78]. Prospective studies have consistently shown that elevated levels of cardiorespiratory fitness and regular PA improve immunological function, confirming the association. Regarding COVID-19 and physical fitness, a few studies have shown protective effects of higher physical fitness (measured as cardiorespiratory fitness (VO2max), muscle strength, sport participation, walking pace or attending to PA guidelines). One study reported that maximal exercise capacity is independently and inversely associated with the likelihood of hospitalization due to COVID-19 [79]. Although more studies are warranted, cardiorespiratory fitness was argued to directly reflect the integrated function of multiple organ systems and an individual’s ability to tolerate cardiopulmonary stress. Another physiological rationale is the enhanced immune function with moderate PA. Another study showed that people over 50 years of age who engage in PA twice a week or more often have a lower risk of COVID-19 hospitalization, with the protective effect explained by muscular strength [80]. Others have found that regular sports participation, regardless of sex and age, positively affects the clinical outcome of hospitalized COVID-19 patients [81]. One study on self-reported walking pace, a simple measure of physical fitness, reported that slow walkers have almost twice the risk of severe and lethal COVID-19 compared to brisk walkers [5]. A prospective observational study in hospitalized patients with COVID-19 that assessed muscle strength on admission observed that the length of hospital stay was significantly shorter among patients in the highest tertile of strength [82]. Recently, a study investigating a cohort of 76,395 South Korean adults found that adults engaging in the recommended levels of PA had a decreased likelihood of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related death [83]. In the aforementioned study, the authors argue that enhanced immunosurveillance, delayed onset of immunosenescence and reduced systemic inflammation, all to be discussed here, as possible explanations as immunological effects decreasing the risk of infection and severity due to COVID-19.
6.1. Adipose Tissue, Obesity, MetS, and Endocrine Effects in Relation to COVID-19 and the Effects of Exercise
Several of the detrimental effects of aging and low-grade systemic inflammation (specifically immunosenescence and inflammaging discussed in Section 6.2) go hand-in-hand with the effects of obesity, MetS, and physical inactivity [21]. Although obesity and MetS are risk factors for cardiovascular mortality [84], they also lead to a decrease in immune function [85], similar to immunosenescence. Regarding COVID-19, MetS is associated with increased mortality in SARS-CoV [86,87] and MERS-CoV [88,89] infection. Obesity was also determined to be a risk factor for the 2009 H1N1 pandemic [90].
Expansion of the adipose tissue (AT) mass during obesity is a key factor in increased systemic inflammation. The obese inflammatory state is characterized by elevated levels of TNF-α, IL-1β, IL-6, IL-17, IL-22, and CRP [91,92,93], which is also seen in physically inactive and sedentary individuals [47,49,94]. Reduced levels of anti-inflammatory and organ-protective adipokines (cytokines secreted by AT) are seen in obesity [95]. Pro-inflammatory Toll-like receptors (TLRs) are also overexpressed in obese subjects [96] as discussed in Section 6.2. Accumulation of AT, especially abdominal AT, leads to increased infiltration by pro-inflammatory M1-type macrophages, reducing the presence of anti-inflammatory M2 macrophages [91,92,97]. In turn, M1 macrophages release pro-inflammatory adipokines, including TNF-α, IL-1B, and IL-6. This shift towards M1 macrophages plays a central role in the systemic inflammation induced by obesity [98]. Some have called the baseline inflammatory obese state a barrier to the induction of a robust antiviral response, allowing for increased viral shedding and transmission [17]. Many argue that AT is a reservoir for extensive viral spread and increased shedding, not least of all due to the pro-inflammatory and immunocompromised state described below. This is also argued by Ryan and Caplice [99], as AT-resident cells are a proven target for multiple viruses: influenza A, SARS-CoV, adenovirus, and HIV target macrophages; SARS-CoV and HIV target lymphocytes; and H1N1, influenza A, and adenovirus target adipocytes.
Similar to other coronaviruses, SARS-CoV-2 activates the NACHT-, LRR-, and pyrin domain-containing 3 (NLRP3) inflammasome, increasing the production of pro-inflammatory cytokines [100,101,102,103]. As reviewed by Freeman and Swartz [104], NLRP3 has a known role in hyperinflammatory ARDS, severe MERS-COV, and SARS-CoV infection, and initial studies have indicated its involvement in severe COVID-19 [105]. Obesity, as well as aging, triggers activation of the NLRP3 inflammasome [106,107]. Thus, age-induced (inflammaging) and obesity-induced NLRP3 hyperactivity could predispose patients to the cytokine storm often seen in severe COVID-19 [106]. Thus, several NLRP3 inhibitors are in pre-clinical or clinical trials for the treatment of COVID-19, as summarized by van den Berg and te Velde [108]. Overall, obese individuals have been shown to be more susceptible to other infections, with more intense cytokine storms due to obesity-induced systemic inflammation [109].
In obese individuals, the antibody response to influenza vaccine is impaired [110]. Vaccinated obese adults have twice the risk of influenza compared to non-obese vaccinated adults [110]. Consequently, the primary means of preventing influenza, and speculatively COVID-19, could be weakened due to obesity. This is troublesome given the significant increase in obesity worldwide in the last few decades. An initial study showed that central obesity, as well as hypertension and dyslipidemia, is associated with lower antibody titers 1–4 weeks after the second inoculation with a COVID-19 mRNA vaccine [111]. Another study showed that higher BMI is associated with lower antibody titers in Italian health workers [112]. Furthermore, in obese individuals, the duration of influenza A virus shedding is prolonged [113], which could increase viral transmission. This has also been seen with SARS-CoV-2; obese patients require longer hospital stays and longer duration (6 days) to obtain a negative oropharyngeal or nasal swab [114].
Obesity and physical inactivity may both lead to endocrine abnormalities. Due to increased activity of the hypothalamic-pituitary-adrenal (HPA) axis, individuals with abdominal obesity have increased secretion of cortisol [115]. In addition to the adrenal cortex, cortisol production by adipocytes is also elevated in hyperinsulemic conditions [116]. Excess cortisol is, in turn, associated with increased abdominal adiposity and several cardiovascular sequelae, including, but not limited to, hypertonia, hyperglycemia, insulin resistance, dyslipidemia, and MetS [117]. Consequently, increased levels of cortisol induced by obesity and physical inactivity increase the risk of several comorbidities and risk factors for severe COVID-19 [4,24,118]. Contracting skeletal muscles release myokines that exert endocrine effects on abdominal adiposity, whereas other myokines have local paracrine effects in signaling pathways involved in fat oxidation [119]. Thus, physical inactivity leads to a metabolic decline, whereas regular PA allows for weight maintenance and/or the reduction of abdominal obesity and induction of an anti-inflammatory environment.
As ACE2 expression is a key factor for SARS-CoV-2 entry into host cells, it is reasonable to assume that low levels of ACE2 would protect against infection, viral amplification, and ultimately a lethal outcome in COVID-19. However, according to a recent model of viral dynamics and gene expression of ACE2 in rats and humans, there is a strong negative correlation between ACE2 and lethality [120]. This hypothesis agrees with research demonstrating that the ACE2 receptor is expressed at lower levels in men than in women, and decreases with age, inflammatory-related comorbidity, and with reduced testosterone and estrogen levels [121].
Regarding sex hormones, PA, and immunity, men with subnormal testosterone levels have higher concentrations of pro-inflammatory cytokines (IL-1β, IL-2, and TNFα) [122,123], which can be counteracted by testosterone supplementation [124]. In this regard, exercise has been shown to attenuate the age-related decline in testosterone in sedentary males [125,126]. Although exercise could diminish the age-related decline in testosterone, it seems to have no significant effect on basal levels in middle-aged men [127]. Testosterone is generally thought to be somewhat immunosuppressive, whereas estrogen is a natural enhancer of immunity [128,129]. In females, estrogen increases humoral immunity and has been shown to be antiviral, protecting against several viruses, including influenza A, HIV, Ebola, hepatitis C, and human cytomegalovirus [130]. This protection is due to several mechanisms, including increased viral-specific T cells (VSTs) in the lungs [131]. In postmenopausal females, exercise can increase estrogen levels, even in sedentary females. A small number of studies have examined the role of testosterone in COVID-19. In contrast to the immunosuppressive reputation of testosterone, some studies have found that low pre-infection levels of testosterone, or low levels of testosterone during infection, are related to worse COVID-19 outcomes [132,133]. However, these were preliminary studies and not rigorous randomized controlled trials. Notably, testosterone levels decrease during infection [134], making the association of lower levels and worse outcome a self-fulfilling prophecy. In addition, lower levels of testosterone often come with comorbid conditions and low metabolic fitness, including obesity, diabetes, and MetS [135]. Thus, testosterone possibly plays a role in driving ACE-2 and TMPRSS2 to increase viral entry [135], but no robust evidence yet shows that testosterone explains why men have a disproportionately high mortality rate in COVID-19.
6.2. The Immune System in Relation to COVID-19 and the Effects of Exercise
The host immunological response following infection with SARS-CoV-2 is crucial to the progression of COVID-19. An appropriate and well-regulated immune response with a balanced interaction between the innate and adaptive immune responses is key to controlling COVID-19 severity [136].
The immune system is influenced by PA and fitness status [78,91,119,137,138]. Age-associated deterioration of immune competency, immunosenescence, is a profound and multifaceted transformation that occurs gradually with age in humans [139,140,141,142,143,144,145,146,147], and is highly influenced by regular PA during one’s lifetime. With the vast majority of COVID-19 deaths occurring in the elderly and pathology data pointing to both immunosenescence and inflammaging/systemic inflammation as major risk factors for mortality [49,91,106,137,146,148,149,150,151], the effects of regular PA are of substantial interest.
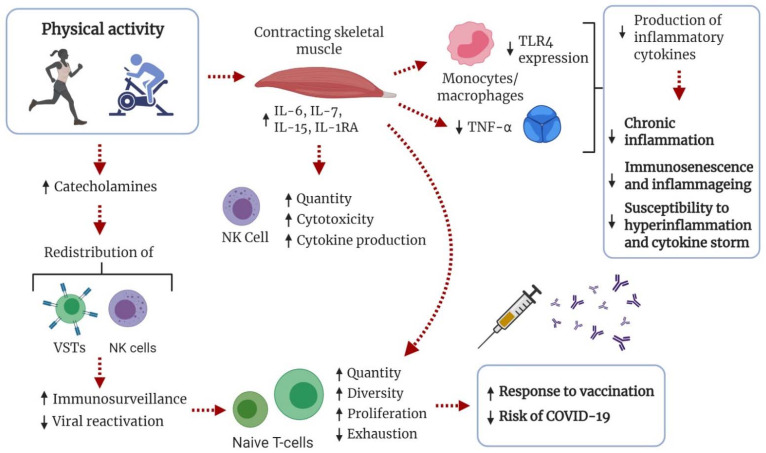
TLRs are vital components in the innate immune system and important for the detection of pathogens and antiviral responses [152]. With advancing age, the TLR function is dysregulated, resulting in inappropriate TLR signaling and cytokine production [143,153]. Downregulated expression of TLRs on monocytes and macrophages, with reduced production of pro-inflammatory cytokines has been suggested as an anti-inflammatory effect of exercise [91,150,154,155]. In contrast, low metabolic fitness, such as obesity with insulin resistance or MetS, can increase the expression of TLR4 [156]. Exercise-induced alterations in TLR signaling, such as reduced TLR4 signaling [157], could attenuate the detrimental effects of low-grade systemic inflammation, improving general health and resiliency. Subsequently, this may attenuate the hyperactivation of monocyte-derived macrophages contributing to the cytokine storm and hyperinflammation in COVID-19 (Figure 3).
Figure 3.
Schematic of immunological adaptations influenced by physical activity (PA) that could increase tolerance to COVID-19. In response to increased levels of catecholamines, viral-specific T cells (VSTs) and natural killer (NK) cells are redistributed in tissues. Immunosurveillance is increased and viral reactivation decreased, preventing T-cell senescence and increasing the number and diversity of naïve T cells. This is known to increase the response to influenza vaccination and decrease the risk of infection. During exercise, skeletal muscle releases myokines with anti-inflammatory effects. Importantly, production of tumor necrosis factor alpha (TNF-α) is inhibited. Regular PA can lead to downregulated expression of Toll-like receptors (TLRs) on monocytes and macrophages, leading to reduced production of pro-inflammatory cytokines.
The SARS-CoV-2 S protein interacts with TLRs, especially TLR4 [158,159], leading to inflammatory responses. Therefore, in obese patients with increased expression of TLR4, the AT, which is already inflamed, makes a favorable environment for SARS-CoV-2-TLR4 interaction, exacerbating the pro-inflammatory cytokine production and increasing the severity of COVID-19 [160]. Treatment with TLR4 antagonists has been used successfully during other viral infections. As summarized elsewhere [161], TLR4 antagonists consistently reduce chemokine and cytokine production, mitigating disease symptoms. Excess activation of TLR4 plays a role in the pathogenesis of viral diseases. Several authors have suggested clinical trials to test TLR4 antagonists in the treatment of severe COVID-19 [162]. However, although no clinical trial data yet support its use, controlling the conditions related to an adverse outcome in COVID-19, such as being physically active, non-obese, and metabolically healthy, is essential.
Exercise and PA lead to an immunostimulatory catecholamine-mediated redistribution of NK cells and VSTs [78,146,149,163]. This increases immune surveillance and apoptosis of senescent T cells, and reduces reactivation of cytomegalovirus, Epstein-Barr virus, and varicella zoster virus. Consequently, the accumulation of senescent T cells is prevented, whereas the count and diversity of naïve T cells is maintained. Animal and human data support the notion that regular moderate-intensity PA improves viral defense effectiveness and decreases morbidity and mortality in viral infections and respiratory illnesses [21,78]. Importantly, increased PA has been shown to improve the immunological response to influenza vaccination [164,165]. Both acute and chronic exposure to exercise seem to enhance the immunological response to vaccination [166], but the optimal exercise regimen, dose-response relationships, and clinical importance are yet to be fully elucidated. Increased PA is also associated with better control of latent viral infections [167] and a reduced risk of pneumonia [18] and infectious disease mortality [19]. Emerging data show that the severity of the COVID-19 cytokine storm and its complications is associated with lymphopenia, with lower counts of and exhausted VSTs, CD4+ and CD8+ T cells, and NK cells [168,169,170]. High-intensity exercise has also been shown to enhance the effector profile of CD8+ T cells in mice [171] and obese humans [172]. Accordingly, the anti-immunosenescent effects of regular PA could be an important measure for maintaining resiliency against COVID-19 and other viral infections with advancing age (Figure 3).
In the context of leukocytes, physically active older adults have been shown to have increased telomerase activity and longer leukocyte telomere length compared to physically inactive peers [173,174]. This context is associated with better survival from sepsis and lower severity of ARDS [175]. Recently, shorter leukocyte telomere length was found to be associated with a higher risk of adverse COVID-19 outcomes, independent of other major risk factors, including chronological age [176,177]. As reviewed by Garatachea [178], habitual PA, especially aerobic exercise, as well as good cardiorespiratory fitness, is associated with longer leukocyte telomere length.
PA has anti-inflammatory effects important for attenuating not only inflammaging, but also general systemic inflammation as seen in the physically inactive and obese populations. Cytokines released by contracting skeletal muscles (“myokines”) have local and pleiotropic anti-inflammatory, immune-regulatory, and health-promoting effects [179]. With exercise bouts of sufficient load, IL-6 is exponentially released with exercise duration [180]. With increased levels of IL-6, there is a multiple-fold increase in circulating levels of anti-inflammatory cytokines IL-10 and IL-1ra). Importantly, exercise-induced release of IL-6 inhibits the production of the pro-inflammatory cytokine TNF-α [91,181], a master regulator of inflammatory cytokine production [182] highly involved in the COVID-19 cytokine storm (Figure 3). Although IL-6 is traditionally known as a pro-inflammatory cytokine vital in the initiation of the acute immunological response, research now supports IL-6 as a multifaceted cytokine capable of eliciting both pro- and anti-inflammatory effects depending on the context [183]. In addition, IL-7 [184] and IL-15 [185], which are both lymphocyte proliferative factors [186], are released during exercise, supporting the function and proliferation of immune cells, mainly naïve T cells. IL-15 is also essential for maintaining memory CD8+ T cells [187] and NK-cell activation, production, and cytotoxicity [188], making it an important factor in the stimulation of immune responses to infections. These transient exercise-induced changes lead to improved protection against sustained low-grade systemic inflammation and pro-inflammatory cytokines [180,181]. It is also important to mention that these anti-inflammatory effects are seen in both young and elderly people, and are even more evident in pathological conditions, such as obesity, CVD, and type II diabetes [47,180,189].
In summary, the connection between physical inactivity, obesity, and MetS with diminished viral defense is evident, creating an immunological case for increasing PA and reducing obesity and MetS in society [21]. Compared to an unfit, obese, and physically inactive individual, a fit, lean, and physically active individual has improved immune function and viral defenses. In the elderly, the anti-immunosenescent and anti-inflammatory effects of PA are of particular interest for increasing resiliency against COVID-19 and its cytokine storm.
6.3. The Cardiovascular System in Relation to COVID-19 and the Effects of Exercise
In addition to the hyperinflammatory state and coagulopathy, the pathophysiological features of the cardiovascular system observed in COVID-19 patients include detrimental effects on the heart and vascular compartment [190]. Regarding cardiac health, exercise training and endurance training, in particular, generate anatomical, functional [191], and metabolic [192] effects on the cardiovascular system that promote overall health and physical endurance.
Importantly, PA mitigates several of the cardiovascular and metabolic risk factors associated with COVID-19 severity, not the least of which is MetS [193]. In short, the therapeutic effects of PA improve coagulation and fibrinolytic homeostasis, endothelial function, and blood pressure regulation, increases blood volume and cardiac ejection fraction, and reduces myocardial oxygen demand and platelet aggregation [28]. This could decrease some of the major cardiovascular complications caused by COVID-19, including myocarditis, cardiogenic shock, and thromboembolism. Due to cellular adaptation to temporary exercise-induced stress, training has been proposed as a preconditioning strategy for cardioprotection against myocardial damage by ischemia/reperfusion [194,195].
Vascular immunopathology, coagulopathy, and thrombosis are well-recognized features of lung abnormalities in COVID-19 that correlate with mortality risk. An imbalance between the activators and inhibitors of the coagulation and fibrinolytic system is commonly seen in obesity, and an increased level of obesity positively correlates with COVID-19 severity and mortality [196]. Therefore, the disturbed hemostatic balance in overweight individuals, with increased coagulation and impaired fibrinolysis, prior to SARS-CoV-2-infection may increase the risk of severe COVID-19. Thus, regular exercise is a natural approach to either prevent or reduce inflammation, and preserve or restore hemostasis. Studies indicate a positive effect of exercise on the regulation of both coagulation and fibrinolysis [197]. This is strengthened by the fact that regular PA reduces all-cause and cardiovascular mortality [198] independent of the intensity of PA [199]. Additional adaptive responses to exercise are indicated by decreased red blood cell aggregation in obese men [200] and improved systolic blood pressure in men and women with pulmonary hypertension.
Due to the vascular adaptation to PA and exercise, the renin-angiotensin system (RAS), which includes ACE2, is of particular interest in the outcome of SARS-CoV-2 infection. ACE2 cleaves Ang II into Ang(1-7) [201]. The RAS is a complex endocrine system that plays an important function in controlling metabolic and cardiovascular homeostasis. In individuals with low fitness and/or cardiometabolic disease, there is an imbalance between the RAS axes, which have been described in depth by others [202]. In short, exercise shifts the balance of the RAS towards the protective ACE2/Ang(1-7)/proto-oncogene, G protein–coupled receptor (MAS) axis in relation to the ACE/Ang II/Angtiotension II receptor type I (AT1R) axis. The latter axis is often hyperactivated in individuals with diabetes, obesity, hypertension, and/or sustained low-grade systemic inflammation [203]. Similarly, increased Ang II is associated with vasculopathy and coagulopathy syndromes in COVID-19 patients [204]. In contrast, activation of the ACE2/Ang(1-7)/MAS axis is anti-inflammatory and vasodilatory, and has several protective effects on the cardiovascular and renal systems, such as anti-thrombolytic functions.
Manipulation of the RAS, balancing it towards the protective arm, is considered a potential therapy for COVID-19 [205]. Accordingly, it strengthens the significance of PA and exercise in improving fitness and the clinical outcome of COVID-19. This has also been argued by others [206,207], suggesting that higher levels of cardiorespiratory fitness may confer innate immune protection against COVID-19 by attenuating the cytokine storm by modulating the RAS and ACE2 activity. As reviewed by Magalhaes, et al. [208], the protective arm of the RAS plays a central role in COVID-19. Antihypertensive ACE inhibitors have successfully been used in the treatment of severe COVID-19 [205,209], and multiple clinical trials suggesting that Ang(1-7) can be used to treat COVID-19 are ongoing (see https://clinicaltrials.gov/ct2/show/NCT04332666, accessed on 5 June 2021, https://www.clinicaltrials.gov/ct2/show/NCT04401423, accessed on 5 June 2021 and https://clinicaltrials.gov/ct2/show/NCT04375124, accessed on 5 June 2021). Notably, ACE inhibitors act by modulating the RAS similar to the response to PA and exercise.
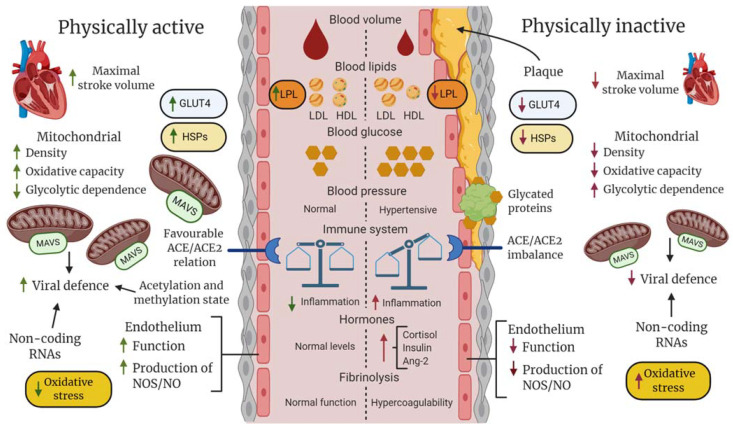
Collectively, exercise has a positive effect on the hemostatic balance and blood pressure, which may prevent high frictional resistance and shear stress on the vascular wall, coagulopathy, and thrombosis, reducing the risk of severe COVID-19. Furthermore, a well-regulated RAS and activated ACE2/Ang(1-7)/MAS axis induced by PA and exercise could be a significant factor in decreasing COVID-19 severity. These adaptations are summarized in Figure 4.
Figure 4.
Hypothetical description of differences between fit (physically active and non-obese) and unfit (physically inactive and obese) individuals in regard to general vascular, blood, and cellular components that could collectively determine clinical outcome following SARS-CoV-2 infection. At the systemic level, regular physical activity (PA), such as exercise training, promotes hormonal homeostasis and improves maximal stroke and blood volume, enhancing blood perfusion and oxygen saturation of tissues. In an unfit state with hypertension, an imbalance between the innate and adaptive immune systems, increased platelet aggregation, dyslipidemia, and abnormally high glucose levels increase the risk of lipid deposition, protein glycation and clot formation, inflammatory responses in the vascular wall, and atherosclerosis, which decrease blood perfusion and oxygen saturation, potentially leading to an infarct in the worst-case scenario. At the cellular level, the temporary metabolic and mechanical stress induced during PA results in improved stress-defense (e.g., heat shock proteins [HSPs], antioxidants), improved mitochondrial capacity in aerobic adenosine triphosphate production and antiviral response (mitochondrial antiviral signaling protein [MAVS]), enhanced uptake and utilization of glucose and fatty acids via increased expression of glucose transporter type 4 (GLUT-4) and lipoprotein lipase (LPL), and improved endothelial functions, including the balance between ACE/ACE2, nitric oxide (NO) production, and endothelin release. Regular PA may also produce a favorable balance between epigenetic factors that facilitate the expression of genes encoding proteins that enhance general cellular functions and activate proteins and non-coding genes that inhibit amplification of SARS-CoV-2.
6.4. The Respiratory System in Relation to COVID-19 and the Effects of Exercise
From a pulmonary perspective, PA can increase the strength and endurance of the respiratory muscles [210]. Although it does not directly improve pulmonary function, it can make them more efficient and reduce the work of breathing. Concerning lung tissue damage and ARDS, PA can increase the diffusing capacity of the pulmonary alveoli. Endurance training is especially effective in this manner [211]. Highly fit, older adults have an increased diffusion capacity compared to less fit, age-matched peers [212]. In mice, aerobic exercise has been shown to attenuate acute lung injury by modulating the inflammatory and reactice oxygen species (ROS) balance [213,214,215].
Obesity also plays a role in respiratory dysfunction. It is associated with low lung volume and low respiratory muscle strength [216]. Being obese impairs respiratory mechanisms by increasing airway resistance and gas exchange [216]. Furthermore, obstructive sleep apnea (OSA) is more common in obese than normal-weight adults. However, obesity can also entail obesity hypoventilation syndrome (OHS), and some individuals suffer from both conditions. In OHS, obese individuals experience hypoventilation-induced hypoxia and hypercapnia regardless of the time of day, whereas OSA causes hypoventilation only during sleep [217]. Pre-existing OSA or OHS seriously limit respiratory function and, once affected by COVID-19, there is a minimum spare capacity. Accordingly, more mechanical ventilation is required in obese patients hospitalized with COVID-19 [218]. Abdominal adiposity can also obstruct the prone positioning necessary to avoid intubation in critically ill COVID-19 patients. Others have reported that abdominal adiposity and high intramuscular fat deposition are independent risk factors for critical care illness, mechanical ventilation, and death [219,220]. Therefore, regular exercise and being non-obese could improve respiratory resilience in COVID-19 due to the higher tolerance for pulmonary stress.
6.5. The Kidneys and Gastrointestinal System in Relation to COVID-19 and the Effects of Exercise
Reduced renal function is a risk factor for COVID-19 mortality [4]. Acute kidney injury (AKI) and chronic kidney disease (CKD) were evaluated in a recent meta-analysis, and both demonstrated a strong association with disease severity and mortality in COVID-19 compared to patients without CKD or AKI [221]. CKD and AKI are strongly interrelated with diabetes [222], and fasting blood glucose is an independent predictor of COVID-19 mortality in patients without a previous diabetes diagnosis [223]. Furthermore, ACE2 is highly expressed in the kidneys [224], offering a high possibility for SARS-CoV-2 infiltration and subsequent down-regulation of ACE2 by SARS-CoV-2. Thus, reduced expression of ACE2 in the kidneys, which reduces the ACE/ACE2 ratio, has been suggested as a possible cause of local vasoconstriction and inflammation, necrosis, and kidney damage in COVID-19 patients [225,226].
PA prevents many of the risk factors associated with the development of CKD, such as diabetic hypertension [227]. Some of the effects attributed to this include the preservation or improvement of insulin sensitivity, glucose tolerance, vascular endothelial function, hormonal balance, and altered adipocytokine profiles, which are all achievable through PA.
Although the direct effect of PA and exercise on the kidneys and renal function in humans remains unclear, PA prevents and reduces many of the aforementioned risk factors [227]. In this regard, the gene encoding protein Klotho is an attractive factor suggested as an anti-aging protein in the hallmark study by Kuro-o et al. [228]. Klotho is crucial for the performance of fibroblast growth factor (FGF) and involved in a multitude of regulatory roles, the metabolism of fatty acids and glucose, and anti-inflammatory and anti-oxidative actions [229]. In this context, Klotho supports and preserves blood vessel and kidney functions [230]. Klotho is abundantly expressed in the kidneys and brain, and modestly expressed in skeletal muscle [228]. The secreted, circulating form of Klotho (S-Klotho) is decreased with age, CKD, and CVD [231]. Interestingly, a 10- to 13-year prospective cohort of middle-aged males without any underlying disease demonstrated that low S-Klotho at baseline predicts an increased risk of developing high fasting plasma glucose (FPG) [232]. High FPG is a pre-diabetic state that also increases the risk of developing hypertension and kidney disease [233] and of death from COVID-19 [223].
A cohort study of master sprint athletes showed that they had better renal function, lower degree of inflammation, and higher Klotho levels than healthy but untrained age-matched peers [234]. This is in agreement with other studies that found higher S-Klotho levels in athletes compared to healthy controls [235] and an increased level with moderate-intensity exercise training [236]. Interestingly, a positive relationship has been shown between the S-Klotho level and the fat oxidation capacity at rest, as well as during exercise [237]. In rats, endurance training results in increased Klotho levels in the brain and kidneys, accompanied by an increased life span and attenuation of excessive ROS production [238]. In mice, the protein level of Klotho is acutely decreased in the skeletal muscle following one bout of exhaustive exercise, accompanied by a marked increase within 24 h compared to baseline [239]. The acute decrease in Klotho in the skeletal muscle may contribute to the increase in S-Klotho seen in studies of humans, which indicate a role of S-Klotho as a health-preserving myokine in the prevention of severe COVID-19. Furthermore, a marked acute increase in S-Klotho by exercise observed in endurance runners, but not in sprinters [240], suggests that the increase in S-Klotho could be dependent on aerobic fitness level and composition. A release of Klotho into the bloodstream from the skeletal muscle, despite relatively low expression per mass, could potentially account for a significant amount of S-Klotho, particularly as an effect of exercise training, because the muscle mass comprises approximately 30–40% of the total body mass. Consequently, muscle-derived Klotho may represent a novel myokine that may help explain some of the health and anti-aging effects of PA via anti-inflammatory, anti-oxidative effects and the preservation of vessel functions, which ultimately protect against severe COVID-19. Klotho is a promising candidate for predicting health status and as a biomarker for evaluating rehabilitation progress post-COVID-19.
Collectively, it is generally accepted that PA prevents the development of hypertension [28], insulin resistance [46,241], endothelial dysfunction [28], and systemic inflammation [91,150,151]. The regulatory factors underlying increased Klotho levels and improved ACE2/ACE ratio in the kidneys in relation to lifestyle factors, such as exercise, are yet to be discovered.
Gastrointestinal (GI) symptoms, such as diarrhea, nausea, and abdominal pain, are commonly seen in COVID-19 patients [242]. The high expression of ACE in the GI tract [243] may partly explain the vulnerability of the GI tract to SARS-CoV-2. Research on effects of PA and exercise on the GI tract is limited. However, regular PA seems to improve the microbiota composition and homeostasis of the immune system [244]. Intestinal dysbiosis and a leaky gut may contribute to the systemic inflammation generally seen in MetS. Clinical observations demonstrate that many COVID-19 patients have severe GI symptoms and detectable SARS-CoV-2 RNA in their stool, along with microbiome dysbiosis and inflammatory indicators [245]. A clinical study including patients with type 2 diabetes showed that 6 months of exercise, combined with caloric restriction, improved the intestinal microbiota composition and gut barrier function and reduced intestinal mycetes overgrowth and systemic inflammation [246]. Furthermore, a growing body of evidence indicates that obesity, MetS, intestinal dysbiosis, and asthma are closely associated. Interestingly, improved asthma control, lung function, and airway hyperresponsiveness are often seen after bariatric surgery, which also goes along with an improved gut microbial ecosystem and glycemic control [247]. Therefore, evidence indicates a close immunological link between the GI and respiratory tracts. At this point, a gut–lung axis has been proposed that affects the outcome of microbial infections and the progression of several diseases [248].
Whether exercise improves the mucosal dysbiosis in the lungs and intestines, thus preventing the development of severe COVID-19, remains to be elucidated. However, maintaining gut barrier function and controlling systemic inflammation by being metabolically healthy is advisable.
6.6. Skeletal Muscle in Relation to COVID-19 and the Effects of Exercise
The regular use of the skeletal muscles via PA and exercise training has fundamental effects at several physiological levels, including an acute increase in the utilization of fatty acids and glucose, followed by muscle adaptations that enhance the uptake of these energy components during exercise [249]. These adaptations to training are important for handling the challenge of the acute increase in blood glucose and lipids following a meal, preventing sustained vascular stress by these factors and, ultimately, CVD (Figure 4). The role of acute exercise and adaptation to training in relation to glucose and fat metabolism and the prevention of CVD and type 2 diabetes are reviewed in depth elsewhere [250,251,252].
Contrasting physiological, cellular, and molecular adaptations are developed through a lifestyle with or without regular PA. Regular PA, particularly recurrent exercise training, results in an improved capacity within the energy systems to meet the increased demand for adenosine triphosphate (ATP) during PA [253]. Exercise training also results in adaptations related to other challenges, such as mechanical, heat, and hormonal stress, increased levels of ROS [254], decreased blood and muscular pH and oxygen, the accumulation of metabolites, and changes in ion homeostasis.
Both endurance and resistance workouts [255] are accompanied by an acute increase in BP. Extremely high systolic and diastolic BP can occur during weightlifting, exemplified by a group mean value of 320/250 mmHg (highest 480/350 mmHg) during leg press with heavy resistance [256]. With this in mind, regular exercise has been shown to reduce the BP at rest in hypertensive subjects [257,258]. Furthermore, PA and exercise training improve hemodynamics and prevent vascular damage. Exercise-induced exposure to hydrostatic pressure and shear stress leads to adaptations that may prevent pro-inflammatory responses and vasculopathy following infection with SARS-CoV-2. These include increased expression of endothelial nitric oxide synthase (eNOS), which promotes vasodilatation via NO, increased capillarity, enhanced autonomic tone, and production of the vasoconstrictor endothelin-1 [259]. All of these may prevent pro-inflammatory responses and vasculopathy following infection with SARS-CoV-2. In obese rats, endurance training has been shown to modulate the cardiac RAS pathways, enhancing the ACE2 pathway over the ACE pathway [260]. Hypertensive rats subjected to endurance training have reduced blood pressure, decreased levels of the Ang II receptor AT1R, and increased levels of the Ang-(1-7) receptor MAS in brain tissue, with a parallel decrease in the production of ROS [261].
A potential adaptive response in humans to exercise training, such as reduced cell signaling in the Ang II pathway and increased activity of the ACE2-Ang-(1-7)-MAS pathway, may also enhance cellular energy metabolism in addition to increased defenses against ROS. In addition to the negative effects on the vascular system of the hyperactivated RAS, Ang II has been shown to suppress the phosphorylation of AMP-activated protein kinase (AMPK) in rat skeletal muscle [262]. This is an important finding, as AMPK is a central regulator of adaptation to exercise training, such as improved insulin sensitivity and glucose uptake [263]. As hyperglycemia is a risk factor for CVD and severe COVID-19 [223], the metabolic functions of the skeletal muscle are of major importance for health. Maintaining muscle mass and function with PA is crucial to sustaining insulin sensitivity and glucose disposal and protecting against comorbidities [264]. Dysfunctional skeletal muscle, as seen with chronic inactivity, aging, and tissue damage, is a precipitating cause in conditions such as type II diabetes, CVD, and cancer.
6.7. Epigenetics in Relation to COVID-19 and the Effects of Exercise
Epigenetic factors are modulated by exercise [265] and may play a protective role in the physiological and cellular responses to viral infection. Epigenetics includes factors that regulate gene expression through histone methylation and acetylation, DNA/RNA methylation, chromatin remodeling, and non-coding RNAs [266]. Recently, a role of microRNAs (miRNAs) was suggested in the regulation of translation processes involved in SARS-CoV-2 infection and its disease, COVID-19, by either blocking or degrading mRNA with subsequent knockdown or suppression of specifically related genes [267,268]. MiRNAs are non-coding RNAs that play a role in the regulation of gene expression, binding to target gene mRNAs and inducing mRNA degradation to inhibit protein synthesis [269]. A potential role of miRNA in lung diseases is exemplified by elevated levels of several sequences found in the plasma of patients with chronic obstructive pulmonary disease (COPD) [270] and may play a role in COVID-19. Interestingly, recent research identified 42 potential human antiviral miRNAs predicted to target SARS-CoV-2 [271]. Among these, circulatory miR-125a has been shown to increase in response to high-intensity exercise [272], as well as miR-23b in skeletal muscle following aerobic exercise, but without any concordant increases in plasma vesicular miR-23b [273,274,275,276]. The role of exercise-induced miRNAs in the obstruction of viral gene expression is an exciting field of research for the future. The miRNA signature in the cardiorespiratory system, skeletal muscle, kidneys, brain, blood vessels, and blood plasma may all respond to exercise and correlate with fitness status; thus, they may have a protective role in the defense against detrimental effects of SARS-CoV-2.
It could be hypothesized that the protective feature of regular PA and exercise training involves inhibition of host cell gene expression that would otherwise be “highjacked” by SARS-CoV-2 in the development of COVID-19. Exercise has been shown to induce significant epigenetic changes, regarding both the acetylation and methylation of histones [277,278]. Histone acetylation and methylation are reversible regulatory processes that facilitate and obstruct, respectively, gene expression [279]. However, epigenetic research in exercise biology is at an early stage and skewed heavily towards muscle function research. Nonetheless, in the context of vulnerable groups at higher risk of developing COVID-19, hypermethylation of DNA in the muscle has been observed with aging [280] and reversed in type 2 diabetes with training [280]. Increased histone acetylation in skeletal muscle has been shown following resistance training [281], as well as an increased frequency of genome-wide hypomethylation, which was preserved over a detraining period and further enhanced in response to re-training [282]. Changes in host-derived long non-coding RNAs (lncRNAs) were recently identified in the lung tissues of patients with COVID-19 [283]. LncRNAs have been suggested to play an important role in the regulation of immune responses and comorbidities [284]. Interestingly, lncRNAs have been shown to be differentially expressed in skeletal muscle between different training protocols [285]. However, the specific roles of lncRNAs in the host response to SARS-CoV-2, or in exercise biology, remain to be investigated.
Collectively, PA and exercise result in epigenetic changes (Figure 4) together with increased expression of genes linked to enhanced muscle functions [286,287,288,289]. Whether changes in the epigenetic signature seen in human skeletal muscle following training correspond to similar changes in the cardiovascular-respiratory system is yet to be determined, although this has been emphasized [290,291,292,293]. Although speculative, the aforementioned epigenetic changes could potentially be involved in increasing resiliency towards viral infection, including SARS-CoV-2 infection.
6.8. Mitochondrial Health in Relation to COVID-19 and the Effects of Exercise
The mitochondrion is the aerobic powerhouse that generates essential ATP in all cells that contain this organelle. Beyond the synthesis of ATP, the mitochondrion produces cofactors, lipids, and cell signaling factors and plays a role in steroid metabolism, calcium homeostasis, and apoptosis [294]. Furthermore, a vital role of the mitochondrion in antiviral defense has been discovered in recent years [295].
The quality and quantity of the mitochondrial mass within each cell are significant for the rate of ATP synthesis, substrate flexibility, stress responses, homeostasis, the cellular metabolic rate, health, and survival. Therefore, the mitochondrial capacity may be a crucial factor in organs infected by SARS-CoV-2. Related to risk factors associated with COVID-19, a reduction in PA results in reduced mitochondrial oxidative capacity and insulin signaling in human skeletal muscle [296]. Furthermore, hyperglycemia and overproduction of ROS by the mitochondria have been suggested to be a major trigger of the inflammation and vascular damage seen in type 2 diabetes [297]. Sustained low-grade systemic inflammation, which is commonly observed in individuals at high risk of COVID-19 [298], is associated with increased mitochondrial ROS production in the endothelium, as well as vascular dysfunction [299]. Therefore, pro-inflammatory cytokines and ROS likely produce a vicious cycle in COVID-19 patients [300]. In contrast to reduced PA, increased PA via endurance training has been shown to improve mitochondrial function and the lipid oxidation capacity in both lean and obese subjects [301], and to enhance the insulin sensitivity and glucose uptake [302]. It has been hypothesized [303], and now shown [304], that SARS-CoV-2 manipulates the mitochondrial metabolism. Findings from COVID-19 patients suggest that mitochondrial dysfunction drives a systemic immune response in COVID-19 pathogenesis. As suggested by Ajaz et al. [304] and others [305,306], maintenance of mitochondrial health and function is essential for an adequate innate immune system response to counteract the modulation by SARS-CoV-2
Mitochondrial biogenesis, the process that increases the mitochondrion density and aerobic oxidation capacity following exercise, is not restricted only to the skeletal muscle. This is exemplified by enhanced mitochondrial respiratory capacity, redox balance, abundance of manganese superoxide dismutase (MnSOD), and NO bioavailability in the arteries of mice following training [307]. Furthermore, exercise training in rats has been shown to increase the activity of antioxidative enzymes in several tissues, including the brain, liver, lungs, and muscle [308]. This would be expected to decrease the pro-oxidative tone of the intracellular milieu, favoring a more reduced and physiologically advantageous environment for carrying out normal cellular processes. In addition, the level of heat shock protein 70 (HSP70) has been shown to be upregulated in the lungs of rats after exercise training, which attenuates heat-induced acute pulmonary edema, inflammation, and ischemic and oxidative damage in the lungs [309]. Acute thermal stress measured during exercise, with a temperature of 38–40 °C in the core [310] and skeletal muscle and brain, is likely to be another factor that stimulates the expression of HSPs in many organs [311]. Related to the panorama of risk factors for COVID-19, an imbalance between extracellular HSP70 (eHSP70) and intracellular HSP70 (iHSP70) which is counteracted by exercise, has been proposed to play a role in type 2 diabetes, with eHSP being more pro-inflammatory and iHSP70 more anti-inflammatory and associated with better insulin sensitivity [312] (Figure 4). Individuals with chronic disease that is inflammatory in nature (obesity, type 2 diabetes, CVD) have a disturbed and suppressed anti-inflammatory heat shock response. Therefore, NF-kB and NLRP3 inflammasomes are activated, leading to a massive cytokine storm, predisposing these patients to severe COVID-19, as also discussed by Heck, et al. [313].
We could further speculate that a difference in vulnerability to COVID-19 between fit and unfit individuals is related to differences at the level of and interconnections between inflammatory exposure, cytoprotection, and mitochondrial capacity. In line with this speculation, the mitochondrial dysfunction generally seen with aging and in comorbidities related to metabolic syndrome and low-grade systemic inflammation has been highlighted in relation to the poor prognosis of COVID-19 [314]. It can also be speculated that regular exercise produces some anti-viral mechanism in host cells that inhibits the replication machinery of the invading SARS-CoV-2 and, thus, the pathogenesis of COVID-19. Here, the effect of exercise training on the mitochondrial antiviral-signaling protein (MAVS) and regulating factors is interesting, but not yet explored. As reviewed by Refolo et al. [295], the MAVS signalosome can rapidly induce the expression of hundreds of genes with antiviral properties in response to infection with an RNA virus. This is further discussed by Burtscher, Millet and Burtscher [306], who argued for mitochondrial integrity and, thus, enhanced MAVS. However, increased fatty acid metabolism could support viral replication in obese individuals. Several studies have demonstrated that intracellular lipid droplets interact with RNA viruses and can support their replication and the production of inflammatory mediators [315,316]. Therefore, increased mitochondrial function and lipid metabolism via regular PA and being non-obese may be other factors that affect the outcome of COVID-19 between fit and unfit individuals [305]. In addition, increased mitochondrial density (i.e., increased number and size of mitochondria) in all tissues affected by an increased metabolic rate because of exercise training may increase the density of MAVS, which enhances the anti-viral response following infection by SARS-CoV-2 (Figure 4). Lastly, enhanced mitochondrial function has been shown in blood platelets with exercise, in stroke patients [317], and in patients with heart failure [318], along with improved aerobic capacity. Thus, improved mitochondrial function in platelets after PA and exercise may reduce thrombogenesis and the risk of coagulopathy following SARS-CoV-2 infection.
7. Conclusions
The COVID-19 pandemic has unmasked mankind’s vulnerability to biological threats. Old age and obesity with one or more comorbidities are clearly defined risk factors for developing severe COVID-19. These risk factors are all associated with a sedentary lifestyle and low cardiorespiratory fitness. However, PA, such as exercise, generates cellular and physiological responses that support health and mobility and prevent comorbidities and mortality. Research on the effects of viral infections at the level of cellular and physiological mechanisms in relation to physical fitness is clearly lacking. Hopefully, these potential links will be explored in the future in light of the COVID-19 pandemic. Efforts must be made against the pandemic of obesity and physical inactivity to increase the average cardiorespiratory, metabolic, and immunological fitness of the population, thus increasing host antiviral defenses and the pandemic resistance of mankind. A decreased response to vaccination and prolonged virus shedding in obese individuals must also be stressed and further investigated in controlled studies. Research on exercise regimens, including modality, duration, and intensity, as well for increasing immunological fitness and the immunological response to vaccination, will benefit our society in future pandemics. The prevention and treatment of obesity and low physical fitness will likely improve mankind’s resilience against a global viral challenge, so aptly illustrated by the current COVID-19 pandemic.
Acknowledgments
All figures were made using BioRender.com. Figure 1: Adapted from “Cytokine storm” (2021), retrieved from https://app.biorender.com/biorender-templates, accessed on 10 June 2021. Figure 2: Adapted from “Mechanism of SARS-CoV-2 Viral Entry” (2021), retrieved from https://app.biorender.com/biorender-templates, accessed on 10 June 2021.
Author Contributions
J.J. and M.S. conceptualized the paper, performed the literature review, and wrote the first draft of the manuscript. I.C., M.F. and N.A. wrote sections of the manuscript. All authors contributed substantially and intellectually to the paper. J.J. and M.S. made the figures. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. [(accessed on 31 March 2020)]. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Wu C., Chen X., Cai Y., Xia J.A., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D., Inglesby P., et al. OpenSAFELY: Factors associated with COVID-19 death in 17 million patients. Nature. 2020;584:430. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yates T., Razieh C., Zaccardi F., Rowlands A.V., Seidu S., Davies M.J., Khunti K. Obesity, walking pace and risk of severe COVID-19 and mortality: Analysis of UK Biobank. Int. J. Obes. 2021;45:1155–1159. doi: 10.1038/s41366-021-00771-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerrigan D.J., Brawner C.A., Ehrman J.K., Keteyian S. Cardiorespiratory Fitness Attenuates the Impact of Risk Factors Associated with COVID-19 Hospitalization. Mayo Clin. Proc. 2021;96:822–823. doi: 10.1016/j.mayocp.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 8.Zhu L., She Z.-G., Cheng X., Qin J.-J., Zhang X.-J., Cai J., Lei F., Wang H., Xie J., Wang W., et al. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020;31:1068–1077. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tchang B.G., Askin G., Sahagun A., Hwang J., Huang H., Mendelsohn Curanaj F.A., Seley J.J., Safford M.M., Alonso L.C., Aronne L.J., et al. The independent risk of obesity and diabetes and their interaction in COVID-19: A retrospective cohort study. Obesity. 2021;29:971–975. doi: 10.1002/oby.23172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tavakol Z., Ghannadi S., Tabesh M.R., Halabchi F., Noormohammadpour P., Akbarpour S., Alizadeh Z., Nezhad M.H., Reyhan S.K. Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study. J. Public Health. 2021:1–9. doi: 10.1007/s10389-020-01468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie J., Zu Y., Alkhatib A., Pham T.T., Gill F., Jang A., Radosta S., Chaaya G., Myers L., Zifodya J.S., et al. Metabolic Syndrome and COVID-19 Mortality Among Adult Black Patients in New Orleans. Diabetes Care. 2020;44:188–193. doi: 10.2337/dc20-1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Radak Z., Torma F., Berkes I., Goto S., Mimura T., Posa A., Balogh L., Boldogh I., Suzuki K., Higuchi M., et al. Exercise effects on physiological function during aging. Free Radic Biol. Med. 2019;132:33–41. doi: 10.1016/j.freeradbiomed.2018.10.444. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . Global Recommendations on Physical Activity for Health. World Health Organization; Geneva, Switzerland: 2010. [PubMed] [Google Scholar]
- 14.Bull F.C., Al-Ansari S.S., Biddle S., Borodulin K., Buman M.P., Cardon G., Carty C., Chaput J.-P., Chastin S., Chou R., et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latimer-Cheung A.E., Chastin S.F.M., Altenburg T.M., Chinapaw M.J.M., Altenburg T.M., et al. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith M., Honce R., Schultz-Cherry S. Metabolic Syndrome and Viral Pathogenesis: Lessons from Influenza and Coronaviruses. J. Virol. 2020;94:e00665-20. doi: 10.1128/JVI.00665-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Honce R., Schultz-Cherry S. Impact of obesity on influenza A virus pathogenesis, immune response, and evolution. Front. Immunol. 2019;10:1071. doi: 10.3389/fimmu.2019.01071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baik I., Curhan G.C., Rimm E.B., Bendich A., Willett W.C., Fawzi W.W. A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women. Arch. Intern. Med. 2000;160:3082–3088. doi: 10.1001/archinte.160.20.3082. [DOI] [PubMed] [Google Scholar]
- 19.Hamer M., O’Donovan G., Stamatakis E. Lifestyle risk factors, obesity and infectious disease mortality in the general population: Linkage study of 97,844 adults from England and Scotland. Prev. Med. 2019;123:65–70. doi: 10.1016/j.ypmed.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Paulsen J., Askim Å., Mohus R.M., Mehl A., Dewan A., Solligård E., Damås J.K., Åsvold B.O. Associations of obesity and lifestyle with the risk and mortality of bloodstream infection in a general population: A 15-year follow-up of 64,027 individuals in the HUNT Study. Int. J. Epidemiol. 2017;46:1573–1581. doi: 10.1093/ije/dyx091. [DOI] [PubMed] [Google Scholar]
- 21.Nieman D.C. Coronavirus Disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society. J. Sport Health Sci. 2020;9:293–301. doi: 10.1016/j.jshs.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samuels J.D. Obesity Phenotype is a Predictor of COVID-19 Disease Susceptibility. Obesity. 2020;28:1368. doi: 10.1002/oby.22866. [DOI] [PubMed] [Google Scholar]
- 23.Zheng K.I., Gao F., Wang X.B., Sun Q.F., Pan K.H., Wang T.Y., Ma H.L., Liu W.Y., George J., Zheng M.H. Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism. 2020;108:154244. doi: 10.1016/j.metabol.2020.154244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kass D.A., Duggal P., Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 2020;395:1544–1545. doi: 10.1016/S0140-6736(20)31024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beltran-Sanchez H., Harhay M.O., Harhay M.M., McElligott S. Prevalence and trends of metabolic syndrome in the adult U.S. population, 1999–2010. J. Am. Coll. Cardiol. 2013;62:697–703. doi: 10.1016/j.jacc.2013.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee M.-K., Han K., Kim M.K., Koh E.S., Kim E.S., Nam G.E., Kwon H.-S. Changes in metabolic syndrome and its components and the risk of type 2 diabetes: A nationwide cohort study. Sci. Rep. 2020;10:2313. doi: 10.1038/s41598-020-59203-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ortega F.B., Cadenas-Sanchez C., Migueles J.H., Labayen I., Ruiz J.R., Sui X., Blair S.N., Martinez-Vizcaino V., Lavie C.J. Role of Physical Activity and Fitness in the Characterization and Prognosis of the Metabolically Healthy Obesity Phenotype: A Systematic Review and Meta-analysis. Prog. Cardiovasc. Dis. 2018;61:190–205. doi: 10.1016/j.pcad.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Pedersen B.K., Saltin B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports. 2015;25((Suppl. S3)):1–72. doi: 10.1111/sms.12581. [DOI] [PubMed] [Google Scholar]
- 29.Ekelund U., Steene-Johannessen J., Brown W.J., Fagerland M.W., Owen N., Powell K.E., Bauman A., Lee I.M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–1310. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 30.Ekelund U., Tarp J., Steene-Johannessen J., Hansen B.H., Jefferis B., Fagerland M.W., Whincup P., Diaz K.M., Hooker S.P., Chernofsky A., et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trost S., Pratley R., Sobel B. Impaired fibrinolysis and risk for cardiovascular disease in the metabolic syndrome and type 2 diabetes. Curr. Diab. Rep. 2006;6:47–54. doi: 10.1007/s11892-006-0052-5. [DOI] [PubMed] [Google Scholar]
- 32.Fitbit The Impact of Coronavirus on Global Activity. [(accessed on 5 April 2020)]. Available online: https://blog.fitbit.com/covid-19-global-activity/
- 33.Apple Mobility Trends Reports. [(accessed on 14 May 2020)]. Available online: https://www.apple.com/covid19/mobility.
- 34.Jakobsson J., Malm C., Furberg M., Ekelund U., Svensson M. Physical Activity during the Coronavirus (COVID-19) Pandemic: Prevention of a Decline in Metabolic and Immunological Functions. Front. Sports Act. Living. 2020;2:57. doi: 10.3389/fspor.2020.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Narici M., De Vito G., Franchi M., Paoli A., Moro T., Marcolin G., Grassi B., Baldassarre G., Zuccarelli L., Biolo G., et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur. J. Sport Sci. 2020;21:614–635. doi: 10.1080/17461391.2020.1761076. [DOI] [PubMed] [Google Scholar]
- 36.Honce R., Schultz-Cherry S. A tale of two pandemics: Obesity and COVID-19. J. Travel Med. 2020;27:taaa097. doi: 10.1093/jtm/taaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhutani S., vanDellen M.R., Cooper J.A. Longitudinal Weight Gain and Related Risk Behaviors during the COVID-19 Pandemic in Adults in the US. Nutrients. 2021;13:671. doi: 10.3390/nu13020671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ding D., Lawson K.D., Kolbe-Alexander T.L., Finkelstein E.A., Katzmarzyk P.T., van Mechelen W., Pratt M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet. 2016;388:1311–1324. doi: 10.1016/S0140-6736(16)30383-X. [DOI] [PubMed] [Google Scholar]
- 39.Lee I.M., Shiroma E.J., Lobelo F., Puska P., Blair S.N., Katzmarzyk P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Booth F.W., Roberts C.K., Thyfault J.P., Ruegsegger G.N., Toedebusch R.G. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol. Rev. 2017;97:1351–1402. doi: 10.1152/physrev.00019.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patterson R., McNamara E., Tainio M., de Sa T.H., Smith A.D., Sharp S.J., Edwards P., Woodcock J., Brage S., Wijndaele K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pulsford R.M., Stamatakis E., Britton A.R., Brunner E.J., Hillsdon M. Associations of sitting behaviours with all-cause mortality over a 16-year follow-up: The Whitehall II study. Int. J. Epidemiol. 2015;44:1909–1916. doi: 10.1093/ije/dyv191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hupin D., Roche F., Gremeaux V., Chatard J.C., Oriol M., Gaspoz J.M., Barthélémy J.C., Edouard P. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥ 60 years: A systematic review and meta-analysis. Br. J. Sports Med. 2015;49:1262–1267. doi: 10.1136/bjsports-2014-094306. [DOI] [PubMed] [Google Scholar]
- 44.Thyfault J.P., Krogh-Madsen R. Metabolic disruptions induced by reduced ambulatory activity in free-living humans. J. Appl. Physiol. 2011;111:1218–1224. doi: 10.1152/japplphysiol.00478.2011. [DOI] [PubMed] [Google Scholar]
- 45.Bowden Davies K.A., Sprung V.S., Norman J.A., Thompson A., Mitchell K.L., Halford J.C.G., Harrold J.A., Wilding J.P.H., Kemp G.J., Cuthbertson D.J. Short-term decreased physical activity with increased sedentary behaviour causes metabolic derangements and altered body composition: Effects in individuals with and without a first-degree relative with type 2 diabetes. Diabetologia. 2018;61:1282–1294. doi: 10.1007/s00125-018-4603-5. [DOI] [PubMed] [Google Scholar]
- 46.Loh R., Stamatakis E., Folkerts D., Allgrove J.E., Moir H.J. Effects of Interrupting Prolonged Sitting with Physical Activity Breaks on Blood Glucose, Insulin and Triacylglycerol Measures: A Systematic Review and Meta-analysis. Sports Med. 2020;50:295–330. doi: 10.1007/s40279-019-01183-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Suzuki K. Chronic Inflammation as an Immunological Abnormality and Effectiveness of Exercise. Biomolecules. 2019;9:223. doi: 10.3390/biom9060223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Handschin C., Spiegelman B.M. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454:463–469. doi: 10.1038/nature07206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ertek S., Cicero A. Impact of physical activity on inflammation: Effects on cardiovascular disease risk and other inflammatory conditions. Arch. Med. Sci. AMS. 2012;8:794–804. doi: 10.5114/aoms.2012.31614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leung N.H.L. Transmissibility and transmission of respiratory viruses. Nat. Rev. Microbiol. 2021:1–18. doi: 10.1038/s41579-021-00535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Puelles V.G., Lütgehetmann M., Lindenmeyer M.T., Sperhake J.P., Wong M.N., Allweiss L., Chilla S., Heinemann A., Wanner N., Liu S., et al. Multiorgan and Renal Tropism of SARS-CoV-2. N. Engl. J. Med. 2020;383:590–592. doi: 10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lamers M.M., Beumer J., van der Vaart J., Knoops K., Puschhof J., Breugem T.I., Ravelli R.B.G., Paul van Schayck J., Mykytyn A.Z., Duimel H.Q., et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369:50–54. doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yadav R., Chaudhary J.K., Jain N., Chaudhary P.K., Khanra S., Dhamija P., Sharma A., Kumar A., Handu S. Role of Structural and Non-Structural Proteins and Therapeutic Targets of SARS-CoV-2 for COVID-19. Cells. 2021;10:821. doi: 10.3390/cells10040821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A., et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e278. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Watanabe Y., Allen J.D., Wrapp D., McLellan J.S., Crispin M. Site-specific glycan analysis of the SARS-CoV-2 spike. Science. 2020;369:330–333. doi: 10.1126/science.abb9983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ziegler C.G.K., Allon S.J., Nyquist S.K., Mbano I.M., Miao V.N., Tzouanas C.N., Cao Y., Yousif A.S., Bals J., Hauser B.M., et al. SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues. Cell. 2020;181:1016–1035.e1019. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lukassen S., Chua R.L., Trefzer T., Kahn N.C., Schneider M.A., Muley T., Winter H., Meister M., Veith C., Boots A.W., et al. SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 2020;39:e105114. doi: 10.15252/embj.2020105114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Clausen T.M., Sandoval D.R., Spliid C.B., Pihl J., Perrett H.R., Painter C.D., Narayanan A., Majowicz S.A., Kwong E.M., McVicar R.N., et al. SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Cell. 2020;183:1043–1057.e1015. doi: 10.1016/j.cell.2020.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cantuti-Castelvetri L., Ojha R., Pedro L.D., Djannatian M., Franz J., Kuivanen S., van der Meer F., Kallio K., Kaya T., Anastasina M., et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Banu N., Panikar S.S., Leal L.R., Leal A.R. Protective role of ACE2 and its downregulation in SARS-CoV-2 infection leading to Macrophage Activation Syndrome: Therapeutic implications. Life Sci. 2020;256:117905. doi: 10.1016/j.lfs.2020.117905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S., Bikdeli B., Ahluwalia N., Ausiello J.C., Wan E.Y., et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 63.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cummings M.J., Baldwin M.R., Abrams D., Jacobson S.D., Meyer B.J., Balough E.M., Aaron J.G., Claassen J., Rabbani L.E., Hastie J., et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Phua J., Weng L., Ling L., Egi M., Lim C.M., Divatia J.V., Shrestha B.R., Arabi Y.M., Ng J., Gomersall C.D., et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hellman U., Karlsson M.G., Engström-Laurent A., Cajander S., Dorofte L., Ahlm C., Laurent C., Blomberg A. Presence of hyaluronan in lung alveoli in severe Covid-19: An opening for new treatment options? J. Biol. Chem. 2020;295:15418–15422. doi: 10.1074/jbc.AC120.015967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X., Liu L., Shan H., Lei C.-L., Hui D.S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-19 and Multiorgan Response. Curr. Probl. Cardiol. 2020;45:100618. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nemes R., Koltai E., Taylor A.W., Suzuki K., Gyori F., Radak Z. Reactive Oxygen and Nitrogen Species Regulate Key Metabolic, Anabolic, and Catabolic Pathways in Skeletal Muscle. Antioxidants. 2018;7:85. doi: 10.3390/antiox7070085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hawley J.A., Hargreaves M., Joyner M.J., Zierath J.R. Integrative Biology of Exercise. Cell. 2014;159:738–749. doi: 10.1016/j.cell.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 74.Giudice J., Taylor J.M. Muscle as a paracrine and endocrine organ. Curr. Opin. Pharmacol. 2017;34:49–55. doi: 10.1016/j.coph.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Booth F.W., Thomason D.B. Molecular and cellular adaptation of muscle in response to exercise: Perspectives of various models. Physiol. Rev. 1991;71:541–585. doi: 10.1152/physrev.1991.71.2.541. [DOI] [PubMed] [Google Scholar]
- 76.Malm C., Jakobsson J., Isaksson A. Physical Activity and Sports—Real Health Benefits: A Review with Insight into the Public Health of Sweden. Sports. 2019;7:127. doi: 10.3390/sports7050127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Campbell J.P., Turner J.E. Debunking the Myth of Exercise-Induced Immune Suppression: Redefining the Impact of Exercise on Immunological Health Across the Lifespan. Front. Immunol. 2018;9:648. doi: 10.3389/fimmu.2018.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nieman D.C., Wentz L.M. The compelling link between physical activity and the body’s defense system. J. Sport Health Sci. 2019;8:201–217. doi: 10.1016/j.jshs.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brawner C.A., Ehrman J.K., Bole S., Kerrigan D.J., Parikh S.S., Lewis B.K., Gindi R.M., Keteyian C., Abdul-Nour K., Keteyian S.J. Maximal Exercise Capacity is Inversely Related to Hospitalization Secondary to Coronavirus Disease 2019. Mayo Clin. Proc. 2020 doi: 10.1016/j.mayocp.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Maltagliati S., Sieber S., Sarrazin P., Cullati S., Chalabaev A., Millet G.P., Boisgontier M.P., Cheval B. Muscle Strength Explains the Protective Effect of Physical Activity against COVID-19 Hospitalization among Adults aged 50 Years and Older. medRxiv. 2021 doi: 10.1101/2021.02.25.21252451. [DOI] [PubMed] [Google Scholar]
- 81.Halabchi F., Mazaheri R., Sabeti K., Yunesian M., Alizadeh Z., Ahmadinejad Z., Aghili S.M., Tavakol Z. Regular Sports Participation as a Potential Predictor of Better Clinical Outcome in Adult Patients with COVID-19: A Large Cross-Sectional Study. J. Phys. Act. Health. 2020;18:8–12. doi: 10.1123/jpah.2020-0392. [DOI] [PubMed] [Google Scholar]
- 82.Gil S., Filho W.J., Shinjo S.K., Ferriolli E., Busse A.L., Avelino-Silva T.J., Longobardi I., de Oliveira G.N., Swinton P., Gualano B., et al. Muscle Strength and Muscle Mass as Predictors of Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Prospective Observational Study. medRxiv. 2021 doi: 10.1101/2021.03.30.21254578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lee S.W., Lee J., Moon S.Y., Jin H.Y., Yang J.M., Ogino S., Song M., Hong S.H., Abou Ghayda R., Kronbichler A., et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: A nationwide cohort study. Br. J. Sports Med. 2021 doi: 10.1136/bjsports-2021-104203. [DOI] [PubMed] [Google Scholar]
- 84.Mottillo S., Filion K.B., Genest J., Joseph L., Pilote L., Poirier P., Rinfret S., Schiffrin E.L., Eisenberg M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010;56:1113–1132. doi: 10.1016/j.jacc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 85.Milner J.J., Beck M.A. The impact of obesity on the immune response to infection. Proc. Nutr. Soc. 2012;71:298–306. doi: 10.1017/S0029665112000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yang J.K., Feng Y., Yuan M.Y., Yuan S.Y., Fu H.J., Wu B.Y., Sun G.Z., Yang G.R., Zhang X.L., Wang L., et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006;23:623–628. doi: 10.1111/j.1464-5491.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- 87.Booth C.M., Matukas L.M., Tomlinson G.A., Rachlis A.R., Rose D.B., Dwosh H.A., Walmsley S.L., Mazzulli T., Avendano M., Derkach P., et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 88.Badawi A., Ryoo S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): A systematic review and meta-analysis. Int. J. Infect. Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Matsuyama R., Nishiura H., Kutsuna S., Hayakawa K., Ohmagari N. Clinical determinants of the severity of Middle East respiratory syndrome (MERS): A systematic review and meta-analysis. BMC Public Health. 2016;16:1203. doi: 10.1186/s12889-016-3881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Van Kerkhove M.D., Vandemaele K.A.H., Shinde V., Jaramillo-Gutierrez G., Koukounari A., Donnelly C.A., Carlino L.O., Owen R., Paterson B., Pelletier L., et al. Risk Factors for Severe Outcomes following 2009 Influenza A (H1N1) Infection: A Global Pooled Analysis. PLoS Med. 2011;8:e1001053. doi: 10.1371/journal.pmed.1001053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gleeson M., Bishop N.C., Stensel D.J., Lindley M.R., Mastana S.S., Nimmo M.A. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 2011;11:607–615. doi: 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- 92.Gregor M.F., Hotamisligil G.S. Inflammatory Mechanisms in Obesity. Annu. Rev. Immunol. 2011;29:415–445. doi: 10.1146/annurev-immunol-031210-101322. [DOI] [PubMed] [Google Scholar]
- 93.Marseglia L., Manti S., D’Angelo G., Nicotera A., Parisi E., Di Rosa G., Gitto E., Arrigo T. Oxidative stress in obesity: A critical component in human diseases. Int. J. Mol. Sci. 2014;16:378–400. doi: 10.3390/ijms16010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Walsh N.P., Gleeson M., Shephard R.J., Gleeson M., Woods J.A., Bishop N., Fleshner M., Green C., Pedersen B.K., Hoffman-Goete L. Position statement part one: Immune function and exercise. Exerc. Immunol. Rev. 2011;17:6–63. [PubMed] [Google Scholar]
- 95.Nigro E., Scudiero O., Monaco M.L., Palmieri A., Mazzarella G., Costagliola C., Bianco A., Daniele A. New insight into adiponectin role in obesity and obesity-related diseases. Biomed. Res. Int. 2014;2014:658913. doi: 10.1155/2014/658913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ahmad R., Al-Mass A., Atizado V., Al-Hubail A., Al-Ghimlas F., Al-Arouj M., Bennakhi A., Dermime S., Behbehani K. Elevated expression of the toll like receptors 2 and 4 in obese individuals: Its significance for obesity-induced inflammation. J. Inflamm. 2012;9:48. doi: 10.1186/1476-9255-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guzik T.J., Skiba D.S., Touyz R.M., Harrison D.G. The role of infiltrating immune cells in dysfunctional adipose tissue. Cardiovasc. Res. 2017;113:1009–1023. doi: 10.1093/cvr/cvx108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chawla A., Nguyen K.D., Goh Y.P.S. Macrophage-mediated inflammation in metabolic disease. Nat. Rev. Immunol. 2011;11:738–749. doi: 10.1038/nri3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ryan P.M., Caplice N.M. Is Adipose Tissue a Reservoir for Viral Spread, Immune Activation, and Cytokine Amplification in Coronavirus Disease 2019? Obesity. 2020;28:1191–1194. doi: 10.1002/oby.22843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shah A. Novel Coronavirus-Induced NLRP3 Inflammasome Activation: A Potential Drug Target in the Treatment of COVID-19. Front. Immunol. 2020;11:1021. doi: 10.3389/fimmu.2020.01021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nieto-Torres J.L., Verdiá-Báguena C., Jimenez-Guardeño J.M., Regla-Nava J.A., Castaño-Rodriguez C., Fernandez-Delgado R., Torres J., Aguilella V.M., Enjuanes L. Severe acute respiratory syndrome coronavirus E protein transports calcium ions and activates the NLRP3 inflammasome. Virology. 2015;485:330–339. doi: 10.1016/j.virol.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fung S.Y., Yuen K.S., Ye Z.W., Chan C.P., Jin D.Y. A tug-of-war between severe acute respiratory syndrome coronavirus 2 and host antiviral defence: Lessons from other pathogenic viruses. Emerg. Microbes Infect. 2020;9:558–570. doi: 10.1080/22221751.2020.1736644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shi C.-S., Nabar N.R., Huang N.-N., Kehrl J.H. SARS-Coronavirus Open Reading Frame-8b triggers intracellular stress pathways and activates NLRP3 inflammasomes. Cell Death Discov. 2019;5:101. doi: 10.1038/s41420-019-0181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Freeman T.L., Swartz T.H. Targeting the NLRP3 inflammasome in severe COVID-19. Front. Immunol. 2020;11:1518. doi: 10.3389/fimmu.2020.01518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Paul O., Tao J.Q., Litzky L., Feldman M., Montone K., Rajapakse C., Bermudez C., Chatterjee S. Vascular Inflammation in Lungs of Patients with Fatal Coronavirus Disease 2019 (COVID-19) Infection: Possible role for the NLRP3 inflammasome. medRxiv. 2021 doi: 10.1101/2021.03.19.21253815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging. 2020;12:9959. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kanneganti T.-D., Dixit V.D. Immunological complications of obesity. Nat. Immunol. 2012;13:707–712. doi: 10.1038/ni.2343. [DOI] [PubMed] [Google Scholar]
- 108.van den Berg D.F., te Velde A.A. Severe COVID-19: NLRP3 Inflammasome Dysregulated. Front. Immunol. 2020;11:1580. doi: 10.3389/fimmu.2020.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ramos Muniz M.G., Palfreeman M., Setzu N., Sanchez M.A., Saenz Portillo P., Garza K.M., Gosselink K.L., Spencer C.T. Obesity Exacerbates the Cytokine Storm Elicited by Francisella tularensis Infection of Females and Is Associated with Increased Mortality. BioMed Res. Int. 2018;2018:3412732. doi: 10.1155/2018/3412732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Green W.D., Beck M.A. Obesity Impairs the Adaptive Immune Response to Influenza Virus. Ann. Am. Thorac. Soc. 2017;14:S406–S409. doi: 10.1513/AnnalsATS.201706-447AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Watanabe M., Balena A., Tuccinardi D., Tozzi R., Risi R., Masi D., Caputi A., Rossetti R., Spoltore M.E., Filippi V., et al. Central obesity, smoking habit, and hypertension are associated with lower antibody titres in response to COVID-19 mRNA vaccine. Diabetes Metab. Res. Rev. 2021 doi: 10.1002/dmrr.3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Pellini R., Venuti A., Pimpinelli F., Abril E., Blandino G., Campo F., Conti L., De Virgilio A., De Marco F., Di Domenico E.G., et al. Obesity may hamper sars-cov-2 vaccine immunogenicity. medRxiv. 2021 doi: 10.1101/2021.02.24.21251664. [DOI] [Google Scholar]
- 113.Maier H.E., Lopez R., Sanchez N., Ng S., Gresh L., Ojeda S., Burger-Calderon R., Kuan G., Harris E., Balmaseda A., et al. Obesity Increases the Duration of Influenza A Virus Shedding in Adults. J. Infect. Dis. 2018;218:1378–1382. doi: 10.1093/infdis/jiy370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Moriconi D., Masi S., Rebelos E., Virdis A., Manca M.L., De Marco S., Taddei S., Nannipieri M. Obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding. Obes. Res. Clin. Pract. 2020;14:205–209. doi: 10.1016/j.orcp.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Björntorp P. Endocrine abnormalities of obesity. Metabolism. 1995;44:21–23. doi: 10.1016/0026-0495(95)90315-1. [DOI] [PubMed] [Google Scholar]
- 116.Anderson A.J., Andrew R., Homer N.Z.M., Hughes K.A., Boyle L.D., Nixon M., Karpe F., Stimson R.H., Walker B.R. Effects of Obesity and Insulin on Tissue-Specific Recycling between Cortisol and Cortisone in Men. J. Clin. Endocrinol. Metab. 2020;106:e1206–e1220. doi: 10.1210/clinem/dgaa896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Whitworth J.A., Williamson P.M., Mangos G., Kelly J.J. Cardiovascular consequences of cortisol excess. Vasc. Health Risk Manag. 2005;1:291–299. doi: 10.2147/vhrm.2005.1.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang A., Leng Y., Zhang Y., Wu K., Ji Y., Lei S., Xia Z. Meta-Analysis of coagulation parameters associated with disease severity and poor prognosis of COVID-19. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pedersen B.K. The diseasome of physical inactivity—And the role of myokines in muscle--fat cross talk. J. Physiol. 2009;587:5559–5568. doi: 10.1113/jphysiol.2009.179515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bastolla U. Mathematical model of SARS-Cov-2 propagation versus ACE2 fits COVID-19 lethality across age and sex and predicts that of SARS, supporting possible therapy. Front. Mol. Biosci. 2020;8:706122. doi: 10.3389/fmolb.2021.706122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chen J., Jiang Q., Xia X., Liu K., Yu Z., Tao W., Gong W., Han J.J. Individual variation of the SARS-CoV-2 receptor ACE2 gene expression and regulation. Aging Cell. 2020;19:e13168. doi: 10.1111/acel.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kalinchenko S.Y., Tishova Y.A., Mskhalaya G.J., Gooren L.J.G., Giltay E.J., Saad F. Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: The double-blinded placebo-controlled Moscow study. Clin. Endocrinol. 2010;73:602–612. doi: 10.1111/j.1365-2265.2010.03845.x. [DOI] [PubMed] [Google Scholar]
- 123.Klein S.L., Flanagan K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016;16:626–638. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 124.Malkin C.J., Pugh P.J., Jones R.D., Kapoor D., Channer K.S., Jones T.H. The effect of testosterone replacement on endogenous inflammatory cytokines and lipid profiles in hypogonadal men. J. Clin. Endocrinol. Metab. 2004;89:3313–3318. doi: 10.1210/jc.2003-031069. [DOI] [PubMed] [Google Scholar]
- 125.Hayes L.D., Herbert P., Sculthorpe N.F., Grace F.M. Exercise training improves free testosterone in lifelong sedentary aging men. Endocr. Connect. 2017;6:306–310. doi: 10.1530/EC-17-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ari Z., Kutlu N., Uyanik B.S., Taneli F., Buyukyazi G., Tavli T. Serum testosterone, growth hormone, and insulin-like growth factor-1 levels, mental reaction time, and maximal aerobic exercise in sedentary and long-term physically trained elderly males. Int. J. Neurosci. 2004;114:623–637. doi: 10.1080/00207450490430499. [DOI] [PubMed] [Google Scholar]
- 127.Hawkins V.N., Foster-Schubert K., Chubak J., Sorensen B., Ulrich C.M., Stancyzk F.Z., Plymate S., Stanford J., White E., Potter J.D., et al. Effect of exercise on serum sex hormones in men: A 12-month randomized clinical trial. Med. Sci. Sports Exerc. 2008;40:223–233. doi: 10.1249/mss.0b013e31815bbba9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cutolo M., Sulli A., Capellino S., Villaggio B., Montagna P., Seriolo B., Straub R.H. Sex hormones influence on the immune system: Basic and clinical aspects in autoimmunity. Lupus. 2004;13:635–638. doi: 10.1191/0961203304lu1094oa. [DOI] [PubMed] [Google Scholar]
- 129.Foo Y.Z., Nakagawa S., Rhodes G., Simmons L.W. The effects of sex hormones on immune function: A meta-analysis. Biol. Rev. Camb. Philos. Soc. 2017;92:551–571. doi: 10.1111/brv.12243. [DOI] [PubMed] [Google Scholar]
- 130.Peretz J., Pekosz A., Lane A.P., Klein S.L. Estrogenic compounds reduce influenza A virus replication in primary human nasal epithelial cells derived from female, but not male, donors. Am. J. Physiol. Lung Cell Mol. Physiol. 2016;310:L415–L425. doi: 10.1152/ajplung.00398.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Robinson D.P., Hall O.J., Nilles T.L., Bream J.H., Klein S.L. 17β-estradiol protects females against influenza by recruiting neutrophils and increasing virus-specific CD8 T cell responses in the lungs. J. Virol. 2014;88:4711–4720. doi: 10.1128/JVI.02081-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Çayan S., Uğuz M., Saylam B., Akbay E. Effect of serum total testosterone and its relationship with other laboratory parameters on the prognosis of coronavirus disease 2019 (COVID-19) in SARS-CoV-2 infected male patients: A cohort study. Aging Male. 2020;23:1493–1503. doi: 10.1080/13685538.2020.1807930. [DOI] [PubMed] [Google Scholar]
- 133.Rastrelli G., Di Stasi V., Inglese F., Beccaria M., Garuti M., Di Costanzo D., Spreafico F., Greco G.F., Cervi G., Pecoriello A., et al. Low testosterone levels predict clinical adverse outcomes in SARS-CoV-2 pneumonia patients. Andrology. 2021;9:88–98. doi: 10.1111/andr.12821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Trumble B.C., Blackwell A.D., Stieglitz J., Thompson M.E., Suarez I.M., Kaplan H., Gurven M. Associations between male testosterone and immune function in a pathogenically stressed forager-horticultural population. Am. J. Phys. Anthropol. 2016;161:494–505. doi: 10.1002/ajpa.23054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Auerbach J.M., Khera M. Testosterone’s Role in COVID-19. J. Sex. Med. 2021;18:843–848. doi: 10.1016/j.jsxm.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Blanco-Melo D., Nilsson-Payant B.E., Liu W.-C., Uhl S., Hoagland D., Møller R., Jordan T.X., Oishi K., Panis M., Sachs D., et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell. 2020;181:1036–1045.e1039. doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nieman D.C., Pence B.D. Exercise immunology: Future directions. J. Sport Health Sci. 2020;9:432–445. doi: 10.1016/j.jshs.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Fernández-Lázaro D., González-Bernal J.J., Sánchez-Serrano N., Navascués L.J., Ascaso-del-Río A., Mielgo-Ayuso J. Physical Exercise as a Multimodal Tool for COVID-19: Could It Be Used as a Preventive Strategy? Int. J. Environ. Res. Public Health. 2020;17:8496. doi: 10.3390/ijerph17228496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Goronzy J.J., Weyand C.M. Understanding immunosenescence to improve responses to vaccines. Nat. Immunol. 2013;14:428–436. doi: 10.1038/ni.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Weng N.P. Aging of the immune system: How much can the adaptive immune system adapt? Immunity. 2006;24:495–499. doi: 10.1016/j.immuni.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Goronzy J.J., Weyand C.M. Immune aging and autoimmunity. Cell. Mol. Life Sci. 2012;69:1615–1623. doi: 10.1007/s00018-012-0970-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Goronzy J.J., Weyand C.M. Aging, autoimmunity and arthritis: T-cell senescence and contraction of T-cell repertoire diversity—catalysts of autoimmunity and chronic inflammation. Arthritis Res. Ther. 2003;5:225–234. doi: 10.1186/ar974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Oh S.-J., Lee J.K., Shin O.S. Aging and the Immune System: The Impact of Immunosenescence on Viral Infection, Immunity and Vaccine Immunogenicity. Immune Netw. 2019;19:e37. doi: 10.4110/in.2019.19.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cavanagh M.M., Weyand C.M., Goronzy J.J. Chronic inflammation and aging: DNA damage tips the balance. Curr. Opin. Immunol. 2012;24:488–493. doi: 10.1016/j.coi.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shaw A.C., Joshi S., Greenwood H., Panda A., Lord J.M. Aging of the innate immune system. Curr. Opin. Immunol. 2010;22:507–513. doi: 10.1016/j.coi.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Duggal N.A., Niemiro G., Harridge S.D.R., Simpson R.J., Lord J.M. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat. Rev. Immunol. 2019;19:563–572. doi: 10.1038/s41577-019-0177-9. [DOI] [PubMed] [Google Scholar]
- 147.Franceschi C., Campisi J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J. Gerontol. Ser. A. 2014;69:S4–S9. doi: 10.1093/gerona/glu057. [DOI] [PubMed] [Google Scholar]
- 148.Turner J.E. Is immunosenescence influenced by our lifetime “dose” of exercise? Biogerontology. 2016;17:581–602. doi: 10.1007/s10522-016-9642-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Turner J.E., Brum P.C. Does Regular Exercise Counter T Cell Immunosenescence Reducing the Risk of Developing Cancer and Promoting Successful Treatment of Malignancies? Oxid. Med. Cell. Longev. 2017;2017:4234765. doi: 10.1155/2017/4234765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Collao N., Rada I., Francaux M., Deldicque L., Zbinden-Foncea H. Anti-Inflammatory Effect of Exercise Mediated by Toll-Like Receptor Regulation in Innate Immune Cells—A Review. Int. Rev. Immunol. 2020;39:39–52. doi: 10.1080/08830185.2019.1682569. [DOI] [PubMed] [Google Scholar]
- 151.da Luz Scheffer D., Latini A. Exercise-induced immune system response: Anti-inflammatory status on peripheral and central organs. Biochim. Et Biophys. Acta Mol. Basis Dis. 2020;1866:165823. doi: 10.1016/j.bbadis.2020.165823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kawai T., Akira S. Antiviral signaling through pattern recognition receptors. J. Biochem. 2007;141:137–145. doi: 10.1093/jb/mvm032. [DOI] [PubMed] [Google Scholar]
- 153.Shaw A.C., Panda A., Joshi S.R., Qian F., Allore H.G., Montgomery R.R. Dysregulation of human Toll-like receptor function in aging. Ageing Res. Rev. 2011;10:346–353. doi: 10.1016/j.arr.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Gleeson M., McFarlin B., Flynn M. Exercise and Toll-like receptors. Exerc. Immunol. Rev. 2006;12:34–53. [PubMed] [Google Scholar]
- 155.Jialal I., Kaur H., Devaraj S. Toll-like receptor status in obesity and metabolic syndrome: A translational perspective. J. Clin. Endocrinol. Metab. 2014;99:39–48. doi: 10.1210/jc.2013-3092. [DOI] [PubMed] [Google Scholar]
- 156.Rogero M.M., Calder P.C. Obesity, Inflammation, Toll-Like Receptor 4 and Fatty Acids. Nutrients. 2018;10:432. doi: 10.3390/nu10040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Flynn M.G., McFarlin B.K. Toll-like receptor 4: Link to the anti-inflammatory effects of exercise? Exerc. Sport Sci. Rev. 2006;34:176–181. doi: 10.1249/01.jes.0000240027.22749.14. [DOI] [PubMed] [Google Scholar]
- 158.Choudhury A., Mukherjee S. In silico studies on the comparative characterization of the interactions of SARS-CoV-2 spike glycoprotein with ACE-2 receptor homologs and human TLRs. J. Med. Virol. 2020;92:2105–2113. doi: 10.1002/jmv.25987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zhao Y., Kuang M., Li J., Zhu L., Jia Z., Guo X., Hu Y., Kong J., Yin H., Wang X., et al. SARS-CoV-2 spike protein interacts with and activates TLR41. Cell Res. 2021:1–3. doi: 10.1038/s41422-021-00495-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Brandão S.C.S., Ramos J.O.X., Dompieri L.T., Godoi E., Figueiredo J.L., Sarinho E.S.C., Chelvanambi S., Aikawa M. Is Toll-like receptor 4 involved in the severity of COVID-19 pathology in patients with cardiometabolic comorbidities? Cytokine Growth Factor Rev. 2020 doi: 10.1016/j.cytogfr.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Olejnik J., Hume A.J., Mühlberger E. Toll-like receptor 4 in acute viral infection: Too much of a good thing. PLoS Pathog. 2018;14:e1007390. doi: 10.1371/journal.ppat.1007390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Aboudounya M.M., Heads R.J. COVID-19 and Toll-Like Receptor 4 (TLR4): SARS-CoV-2 May Bind and Activate TLR4 to Increase ACE2 Expression, Facilitating Entry and Causing Hyperinflammation. Mediat. Inflamm. 2021;2021:8874339. doi: 10.1155/2021/8874339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Nieman D.C., Nehlsen-Cannarella S.L., Markoff P.A., Balk-Lamberton A.J., Yang H., Chritton D.B., Lee J.W., Arabatzis K. The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections. Int. J. Sports Med. 1990;11:467–473. doi: 10.1055/s-2007-1024839. [DOI] [PubMed] [Google Scholar]
- 164.Kohut M.L., Arntson B.A., Lee W., Rozeboom K., Yoon K.J., Cunnick J.E., McElhaney J. Moderate exercise improves antibody response to influenza immunization in older adults. Vaccine. 2004;22:2298–2306. doi: 10.1016/j.vaccine.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 165.Woods J.A., Keylock K.T., Lowder T., Vieira V.J., Zelkovich W., Dumich S., Colantuano K., Lyons K., Leifheit K., Cook M., et al. Cardiovascular exercise training extends influenza vaccine seroprotection in sedentary older adults: The immune function intervention trial. J. Am. Geriatr. Soc. 2009;57:2183–2191. doi: 10.1111/j.1532-5415.2009.02563.x. [DOI] [PubMed] [Google Scholar]
- 166.Pascoe A.R., Fiatarone Singh M.A., Edwards K.M. The effects of exercise on vaccination responses: A review of chronic and acute exercise interventions in humans. Brain. Behav. Immun. 2014;39:33–41. doi: 10.1016/j.bbi.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 167.Simpson R.J., Hussain M., Baker F., Bigley A.B., Peek M.K., Stowe R.P. Cardiorespiratory fitness is associated with better control of latent herpesvirus infections in a large ethnically diverse community sample: Evidence from the Texas City Stress and Health Study. Brain. Behav. Immun. 2017;66:e35. doi: 10.1016/j.bbi.2017.07.128. [DOI] [Google Scholar]
- 168.Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.-Q., Wang Q., Miao H. Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal. Transduct. Target. Ther. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zheng M., Gao Y., Wang G., Song G., Liu S., Sun D., Xu Y., Tian Z. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell. Mol. Immunol. 2020;17:533–535. doi: 10.1038/s41423-020-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Liu J., Li S., Liu J., Liang B., Wang X., Wang H., Li W., Tong Q., Yi J., Zhao L., et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020;55:102763. doi: 10.1016/j.ebiom.2020.102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Rundqvist H., Veliça P., Barbieri L., Gameiro P.A., Bargiela D., Gojkovic M., Mijwel S., Reitzner S.M., Wulliman D., Ahlstedt E., et al. Cytotoxic T-cells mediate exercise-induced reductions in tumor growth. Elife. 2020;9:e59996. doi: 10.7554/eLife.59996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Dorneles G.P., da Silva I.M., Santos M.A., Elsner V.R., Fonseca S.G., Peres A., Romão P.R.T. Immunoregulation induced by autologous serum collected after acute exercise in obese men: A randomized cross-over trial. Sci. Rep. 2020;10:21735. doi: 10.1038/s41598-020-78750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Simões H.G., Rosa T.S., Sousa C.V., Aguiar S.d.S., Motta-Santos D., Degens H., Korhonen M.T., Campbell C.S.G. Does Longer Leukocyte Telomere Length and Higher Physical Fitness Protect Master Athletes From Consequences of Coronavirus (SARS-CoV-2) Infection? Front. Sports Act. Living. 2020;2:87. doi: 10.3389/fspor.2020.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sjögren P., Fisher R., Kallings L., Svenson U., Roos G., Hellénius M.L. Stand up for health--avoiding sedentary behaviour might lengthen your telomeres: Secondary outcomes from a physical activity RCT in older people. Br. J. Sports Med. 2014;48:1407–1409. doi: 10.1136/bjsports-2013-093342. [DOI] [PubMed] [Google Scholar]
- 175.Liu S., Wang C., Green G., Zhuo H., Liu K.D., Kangelaris K.N., Gomez A., Jauregui A., Vessel K., Ke S. Peripheral blood leukocyte telomere length is associated with survival of sepsis patients. Eur. Respir. J. 2020;55:1901044. doi: 10.1183/13993003.01044-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang Q., Codd V., Raisi-Estabragh Z., Musicha C., Bountziouka V., Kaptoge S., Allara E., Angelantonio E.D., Butterworth A.S., Wood A.M., et al. Older biological age is associated with adverse COVID-19 outcomes: A cohort study in UK Biobank. medRxiv. 2021 doi: 10.1101/2021.03.20.21254010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sanchez-Vazquez R., Guío-Carrión A., Zapatero-Gaviria A., Martínez P., Blasco M.A. Shorter telomere lengths in patients with severe COVID-19 disease. Aging. 2021;13:1–15. doi: 10.18632/aging.202463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Garatachea N., Pareja-Galeano H., Sanchis-Gomar F., Santos-Lozano A., Fiuza-Luces C., Morán M., Emanuele E., Joyner M.J., Lucia A. Exercise Attenuates the Major Hallmarks of Aging. Rejuvenation Res. 2015;18:57–89. doi: 10.1089/rej.2014.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Severinsen M.C.K., Pedersen B.K. Muscle-Organ Crosstalk: The Emerging Roles of Myokines. Endocr. Rev. 2020;41:594–609. doi: 10.1210/endrev/bnaa016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Leal L.G., Lopes M.A., Batista M.L., Jr. Physical Exercise-Induced Myokines and Muscle-Adipose Tissue Crosstalk: A Review of Current Knowledge and the Implications for Health and Metabolic Diseases. Front. Physiol. 2018;9:1307. doi: 10.3389/fphys.2018.01307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Petersen A.M., Pedersen B.K. The anti-inflammatory effect of exercise. J. Appl. Physiol. 2005;98:1154–1162. doi: 10.1152/japplphysiol.00164.2004. [DOI] [PubMed] [Google Scholar]
- 182.Parameswaran N., Patial S. Tumor necrosis factor-α signaling in macrophages. Crit. Rev. Eukaryot. Gene Expr. 2010;20:87–103. doi: 10.1615/CritRevEukarGeneExpr.v20.i2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cox A.A., Sagot Y., Hedou G., Grek C., Wilkes T., Vinik A.I., Ghatnekar G. Low-Dose Pulsatile Interleukin-6 As a Treatment Option for Diabetic Peripheral Neuropathy. Front. Endocrinol. 2017;8:89. doi: 10.3389/fendo.2017.00089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Haugen F., Norheim F., Lian H., Wensaas A.J., Dueland S., Berg O., Funderud A., Skålhegg B.S., Raastad T., Drevon C.A. IL-7 is expressed and secreted by human skeletal muscle cells. Am. J. Physiol.-Cell Physiol. 2010;298:C807–C816. doi: 10.1152/ajpcell.00094.2009. [DOI] [PubMed] [Google Scholar]
- 185.Rinnov A., Yfanti C., Nielsen S., Akerström T.C., Peijs L., Zankari A., Fischer C.P., Pedersen B.K. Endurance training enhances skeletal muscle interleukin-15 in human male subjects. Endocrine. 2014;45:271–278. doi: 10.1007/s12020-013-9969-z. [DOI] [PubMed] [Google Scholar]
- 186.Wallace D.L., Bérard M., Soares M.V., Oldham J., Cook J.E., Akbar A.N., Tough D.F., Beverley P.C. Prolonged exposure of naïve CD8+ T cells to interleukin-7 or interleukin-15 stimulates proliferation without differentiation or loss of telomere length. Immunology. 2006;119:243–253. doi: 10.1111/j.1365-2567.2006.02429.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Perera P.-Y., Lichy J.H., Waldmann T.A., Perera L.P. The role of interleukin-15 in inflammation and immune responses to infection: Implications for its therapeutic use. Microbes Infect. 2012;14:247–261. doi: 10.1016/j.micinf.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Al-Attar A., Presnell S.R., Clasey J.L., Long D.E., Walton R.G., Sexton M., Starr M.E., Kern P.A., Peterson C.A., Lutz C.T. Human Body Composition and Immunity: Visceral Adipose Tissue Produces IL-15 and Muscle Strength Inversely Correlates with NK Cell Function in Elderly Humans. Front. Immunol. 2018;9:440. doi: 10.3389/fimmu.2018.00440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kwon J.H., Moon K.M., Min K.-W. Exercise-Induced Myokines can Explain the Importance of Physical Activity in the Elderly: An Overview. Healthcare. 2020;8:378. doi: 10.3390/healthcare8040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mahenthiran A.K., Mahenthiran A.K., Mahenthiran J. Cardiovascular system and COVID-19: Manifestations and therapeutics. Rev. Cardiovasc. Med. 2020;21:399–409. doi: 10.31083/j.rcm.2020.03.124. [DOI] [PubMed] [Google Scholar]
- 191.Wilson M.G., Ellison G.M., Cable N.T. Basic science behind the cardiovascular benefits of exercise. Br. J. Sports Med. 2016;50:93–99. doi: 10.1136/bjsports-2014-306596rep. [DOI] [PubMed] [Google Scholar]
- 192.Kolwicz S.C., Jr. An “Exercise” in Cardiac Metabolism. Front. Cardiovasc. Med. 2018;5:66. doi: 10.3389/fcvm.2018.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Stefan N., Birkenfeld A.L., Schulze M.B., Ludwig D.S. Obesity and impaired metabolic health in patients with COVID-19. Nat. Rev. Endocrinol. 2020;16:341–342. doi: 10.1038/s41574-020-0364-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Borges J.P., da Silva Verdoorn K. Cardiac Ischemia/Reperfusion Injury: The Beneficial Effects of Exercise. Adv. Exp. Med. Biol. 2017;999:155–179. doi: 10.1007/978-981-10-4307-9_10. [DOI] [PubMed] [Google Scholar]
- 195.Penna C., Alloatti G., Crisafulli A. Mechanisms Involved in Cardioprotection Induced by Physical Exercise. Antioxid Redox Signal. 2020;32:1115–1134. doi: 10.1089/ars.2019.8009. [DOI] [PubMed] [Google Scholar]
- 196.Pranata R., Lim M.A., Yonas E., Vania R., Lukito A.A., Siswanto B.B., Meyer M. Body mass index and outcome in patients with COVID-19: A dose-response meta-analysis. Diabetes Metab. 2020;47:101178. doi: 10.1016/j.diabet.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Paton C.M., Brandauer J., Weiss E.P., Brown M.D., Ivey F.M., Roth S.M., Hagberg J.M. Hemostatic response to postprandial lipemia before and after exercise training. J. Appl. Physiol. 2006;101:316–321. doi: 10.1152/japplphysiol.01363.2005. [DOI] [PubMed] [Google Scholar]
- 198.Schnohr P., O’Keefe J.H., Lange P., Jensen G.B., Marott J.L. Impact of persistence and non-persistence in leisure time physical activity on coronary heart disease and all-cause mortality: The Copenhagen City Heart Study. Eur. J. Prev. Cardiol. 2017;24:1615–1623. doi: 10.1177/2047487317721021. [DOI] [PubMed] [Google Scholar]
- 199.Fan M., Yu C., Guo Y., Bian Z., Li X., Yang L., Chen Y., Li M., Li X., Chen J., et al. Effect of total, domain-specific, and intensity-specific physical activity on all-cause and cardiovascular mortality among hypertensive adults in China. J. Hypertens. 2018;36:793–800. doi: 10.1097/HJH.0000000000001601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Kim S.W., Jung W.S., Park W., Park H.Y. Twelve Weeks of Combined Resistance and Aerobic Exercise Improves Cardiometabolic Biomarkers and Enhances Red Blood Cell Hemorheological Function in Obese Older Men: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health. 2019;16:5020. doi: 10.3390/ijerph16245020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Warner F.J., Smith A.I., Hooper N.M., Turner A.J. Angiotensin-converting enzyme-2: A molecular and cellular perspective. Cell. Mol. Life Sci. 2004;61:2704–2713. doi: 10.1007/s00018-004-4240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Frantz E., Dalla C., Prodel E., Braz I.D., Giori I.G., Bargut T., Cristina L., Magliano D., Angelo C., Nobrega A., et al. Modulation of the renin–angiotensin system in white adipose tissue and skeletal muscle: Focus on exercise training. Clin. Sci. 2018;132:1487–1507. doi: 10.1042/CS20180276. [DOI] [PubMed] [Google Scholar]
- 203.Evangelista F.S. Physical Exercise and the Renin Angiotensin System: Prospects in the COVID-19. Front. Physiol. 2020;11:1282. doi: 10.3389/fphys.2020.561403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Labò N., Ohnuki H., Tosato G. Vasculopathy and Coagulopathy Associated with SARS-CoV-2 Infection. Cells. 2020;9:1583. doi: 10.3390/cells9071583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhang P., Zhu L., Cai J., Lei F., Qin J.J., Xie J., Liu Y.M., Zhao Y.C., Huang X., Lin L., et al. Association of Inpatient Use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers with Mortality Among Patients with Hypertension Hospitalized with COVID-19. Circ. Res. 2020;126:1671–1681. doi: 10.1161/CIRCRESAHA.120.317134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Zbinden-Foncea H., Francaux M., Deldicque L., Hawley J.A. Does high cardiorespiratory fitness confer some protection against pro-inflammatory responses after infection by SARS-CoV-2? Obesity. 2020;28:1378–1381. doi: 10.1002/oby.22849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Motta-Santos D., Santos R.A.S., Santos S.H.S. Angiotensin-(1-7) and Obesity: Role in Cardiorespiratory Fitness and COVID-19 Implications. Obesity. 2020;28:1786. doi: 10.1002/oby.22949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Magalhaes G.S., Rodrigues-Machado M.D.G., Motta-Santos D., Campagnole-Santos M.J., Santos R.A.S. Activation of Ang-(1-7)/Mas Receptor Is a Possible Strategy to Treat Coronavirus (SARS-CoV-2) Infection. Front. Physiol. 2020;11:730. doi: 10.3389/fphys.2020.00730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Lo K.B., Bhargav R., Salacup G., Pelayo J., Albano J., McCullough P.A., Rangaswami J. Angiotensin converting enzyme inhibitors and angiotensin II receptor blockers and outcomes in patients with COVID-19: A systematic review and meta-analysis. Expert Rev. Cardiovasc. Ther. 2020;18:919–930. doi: 10.1080/14779072.2020.1826308. [DOI] [PubMed] [Google Scholar]
- 210.McKenzie D.C. Respiratory physiology: Adaptations to high-level exercise. Br. J. Sports Med. 2012;46:381. doi: 10.1136/bjsports-2011-090824. [DOI] [PubMed] [Google Scholar]
- 211.Tedjasaputra V., Bouwsema M.M., Stickland M.K. Effect of aerobic fitness on capillary blood volume and diffusing membrane capacity responses to exercise. J. Physiol. 2016;594:4359–4370. doi: 10.1113/JP272037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Coffman K.E., Carlson A.R., Miller A.D., Johnson B.D., Taylor B.J. The effect of aging and cardiorespiratory fitness on the lung diffusing capacity response to exercise in healthy humans. J. Appl. Physiol. 2017;122:1425–1434. doi: 10.1152/japplphysiol.00694.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Reis Goncalves C.T., Reis Goncalves C.G., de Almeida F.M., Lopes F.D., dos Santos Durao A.C., dos Santos F.A., da Silva L.F., Marcourakis T., Castro-Faria-Neto H.C., Vieira R.P., et al. Protective effects of aerobic exercise on acute lung injury induced by LPS in mice. Crit. Care. 2012;16:R199. doi: 10.1186/cc11807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Shi Y., Liu T., Nieman D.C., Cui Y., Li F., Yang L., Shi H., Chen P. Aerobic Exercise Attenuates Acute Lung Injury through NET Inhibition. Front. Immunol. 2020;11:409. doi: 10.3389/fimmu.2020.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Toledo A.C., Magalhaes R.M., Hizume D.C., Vieira R.P., Biselli P.J.C., Moriya H.T., Mauad T., Lopes F.D.T.Q.S., Martins M.A. Aerobic exercise attenuates pulmonary injury induced by exposure to cigarette smoke. Eur. Respir. J. 2012;39:254. doi: 10.1183/09031936.00003411. [DOI] [PubMed] [Google Scholar]
- 216.Murugan A.T., Sharma G. Obesity and respiratory diseases. Chron. Respir. Dis. 2008;5:233–242. doi: 10.1177/1479972308096978. [DOI] [PubMed] [Google Scholar]
- 217.Liu C., Chen M.-S., Yu H. The relationship between obstructive sleep apnea and obesity hypoventilation syndrome: A systematic review and meta-analysis. Oncotarget. 2017;8:93168–93178. doi: 10.18632/oncotarget.21450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., Labreuche J., Mathieu D., Pattou F., Jourdain M. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity. 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yang Y., Ding L., Zou X., Shen Y., Hu D., Hu X., Li Z., Kamel I.R. Visceral Adiposity and High Intramuscular Fat Deposition Independently Predict Critical Illness in Patients with Sars-COV-2. Obesity. 2020;28:2040–2048. doi: 10.1002/oby.22971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Petersen A., Bressem K., Albrecht J., Thieß H.M., Vahldiek J., Hamm B., Makowski M.R., Niehues A., Niehues S.M., Adams L.C. The role of visceral adiposity in the severity of COVID-19: Highlights from a unicenter cross-sectional pilot study in Germany. Metabolism. 2020;110:154317. doi: 10.1016/j.metabol.2020.154317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Wang B., Luo Q., Zhang W., Yu S., Cheng X., Wang L., Chen X., Chen Y. The Involvement of Chronic Kidney Disease and Acute Kidney Injury in Disease Severity and Mortality in Patients with COVID-19: A Meta-Analysis. Kidney Blood Press. Res. 2021;46:17–30. doi: 10.1159/000512211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Hapca S., Siddiqui M.K., Kwan R.S.Y., Lim M., Matthew S., Doney A.S.F., Pearson E.R., Palmer C.N.A., Bell S. The Relationship between AKI and CKD in Patients with Type 2 Diabetes: An Observational Cohort Study. J. Am. Soc. Nephrol. 2021;32:138. doi: 10.1681/ASN.2020030323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Wang S., Ma P., Zhang S., Song S., Wang Z., Ma Y., Xu J., Wu F., Duan L., Yin Z., et al. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: A multi-centre retrospective study. Diabetologia. 2020;63:2102–2111. doi: 10.1007/s00125-020-05209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hikmet F., Méar L., Edvinsson Å., Micke P., Uhlén M., Lindskog C. The protein expression profile of ACE2 in human tissues. Mol. Syst. Biol. 2020;16:e9610. doi: 10.15252/msb.20209610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Armaly Z., Kinaneh S., Skorecki K. Renal Manifestations of Covid-19: Physiology and Pathophysiology. J. Clin. Med. 2021;10:1216. doi: 10.3390/jcm10061216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Costa L.B., Perez L.G., Palmeira V.A., Macedo E.C.T., Ribeiro V.T., Lanza K., Simões E.S.A.C. Insights on SARS-CoV-2 Molecular Interactions With the Renin-Angiotensin System. Front. Cell Dev. Biol. 2020;8:559841. doi: 10.3389/fcell.2020.559841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Stump C.S. Physical Activity in the Prevention of Chronic Kidney Disease. Cardiorenal Med. 2011;1:164–173. doi: 10.1159/000329929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Kuro-o M., Matsumura Y., Aizawa H., Kawaguchi H., Suga T., Utsugi T., Ohyama Y., Kurabayashi M., Kaname T., Kume E., et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390:45–51. doi: 10.1038/36285. [DOI] [PubMed] [Google Scholar]
- 229.Kuro O.M. The Klotho proteins in health and disease. Nat. Rev. Nephrol. 2019;15:27–44. doi: 10.1038/s41581-018-0078-3. [DOI] [PubMed] [Google Scholar]
- 230.Buchanan S., Combet E., Stenvinkel P., Shiels P.G. Klotho, Aging, and the Failing Kidney. Front. Endocrinol. 2020;11:560. doi: 10.3389/fendo.2020.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Saar-Kovrov V., Donners M.M.P.C., van der Vorst E.P.C. Shedding of Klotho: Functional Implications in Chronic Kidney Disease and Associated Vascular Disease. Front. Cardiovasc. Med. 2021;7:407. doi: 10.3389/fcvm.2020.617842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Nakanishi K., Nishida M., Taneike M., Yamamoto R., Moriyama T., Yamauchi-Takihara K. Serum Klotho Levels Contribute to the Prevention of Disease Progression. Int. J. Gen. Med. 2021;14:229–236. doi: 10.2147/IJGM.S291437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Mancusi C., Izzo R., di Gioia G., Losi M.A., Barbato E., Morisco C. Insulin Resistance the Hinge Between Hypertension and Type 2 Diabetes. High. Blood Press. Cardiovasc. Prev. 2020;27:515–526. doi: 10.1007/s40292-020-00408-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Rosa T.D.S., Corrêa H.L., Barbosa L.P., Santos P.A.D., Leite P.L.A., Aguiar S.S., Deus L.A., Maciel L.A., Neves R.V.P., Simoes H.G. Age-related Decline in Renal Function is Attenuated in Master Athletes. Int. J. Sports Med. 2021 doi: 10.1055/a-1332-1594. [DOI] [PubMed] [Google Scholar]
- 235.Mostafidi E., Moeen A., Nasri H., Ghorbani Hagjo A., Ardalan M. Serum Klotho Levels in Trained Athletes. Nephrourol. Mon. 2016;8:e30245. doi: 10.5812/numonthly.30245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Middelbeek R.J.W., Motiani P., Brandt N., Nigro P., Zheng J., Virtanen K.A., Kalliokoski K.K., Hannukainen J.C., Goodyear L.J. Exercise intensity regulates cytokine and klotho responses in men. Nutr. Diabetes. 2021;11:5. doi: 10.1038/s41387-020-00144-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Amaro-Gahete F.J., De-la O.A., Jurado-Fasoli L., Ruiz J.R., Castillo M.J. Association of basal metabolic rate and fuel oxidation in basal conditions and during exercise, with plasma S-klotho: The FIT-AGEING study. Aging. 2019;11:5319–5333. doi: 10.18632/aging.102100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Ji N., Luan J., Hu F., Zhao Y., Lv B., Wang W., Xia M., Zhao X., Lao K. Aerobic exercise-stimulated Klotho upregulation extends life span by attenuating the excess production of reactive oxygen species in the brain and kidney. Exp. Ther. Med. 2018;16:3511–3517. doi: 10.3892/etm.2018.6597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Rao Z., Zheng L., Huang H., Feng Y., Shi R. α-Klotho Expression in Mouse Tissues Following Acute Exhaustive Exercise. Front. Physiol. 2019;10:1498. doi: 10.3389/fphys.2019.01498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Matsubara T., Miyaki A., Akazawa N., Choi Y., Ra S.G., Tanahashi K., Kumagai H., Oikawa S., Maeda S. Aerobic exercise training increases plasma Klotho levels and reduces arterial stiffness in postmenopausal women. Am. J. Physiol. Heart Circ. Physiol. 2014;306:H348–H355. doi: 10.1152/ajpheart.00429.2013. [DOI] [PubMed] [Google Scholar]
- 241.Conn V.S., Koopman R.J., Ruppar T.M., Phillips L.J., Mehr D.R., Hafdahl A.R. Insulin Sensitivity Following Exercise Interventions: Systematic Review and Meta-Analysis of Outcomes Among Healthy Adults. J. Prim. Care Community Health. 2014;5:211–222. doi: 10.1177/2150131913520328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Alberca G.G.F., Solis-Castro R.L., Solis-Castro M.E., Alberca R.W. Coronavirus disease-2019 and the intestinal tract: An overview. World J. Gastroenterol. 2021;27:1255–1266. doi: 10.3748/wjg.v27.i13.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Harmer D., Gilbert M., Borman R., Clark K.L. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532:107–110. doi: 10.1016/S0014-5793(02)03640-2. [DOI] [PubMed] [Google Scholar]
- 244.Cook M.D., Allen J.M., Pence B.D., Wallig M.A., Gaskins H.R., White B.A., Woods J.A. Exercise and gut immune function: Evidence of alterations in colon immune cell homeostasis and microbiome characteristics with exercise training. Immunol. Cell Biol. 2016;94:158–163. doi: 10.1038/icb.2015.108. [DOI] [PubMed] [Google Scholar]
- 245.Guo M., Tao W., Flavell R.A., Zhu S. Potential intestinal infection and faecal–oral transmission of SARS-CoV-2. Nat. Rev. Gastroenterol. Hepatol. 2021;18:269–283. doi: 10.1038/s41575-021-00416-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Pasini E., Corsetti G., Assanelli D., Testa C., Romano C., Dioguardi F.S., Aquilani R. Effects of chronic exercise on gut microbiota and intestinal barrier in human with type 2 diabetes. Minerva Med. 2019;110:3–11. doi: 10.23736/S0026-4806.18.05589-1. [DOI] [PubMed] [Google Scholar]
- 247.Kim Y.J., Womble J.T., Gunsch C.K., Ingram J.L. The Gut/Lung Microbiome Axis in Obesity, Asthma, and Bariatric Surgery: A Literature Review. Obesity. 2021;29:636–644. doi: 10.1002/oby.23107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.He Y., Wen Q., Yao F., Xu D., Huang Y., Wang J. Gut-lung axis: The microbial contributions and clinical implications. Crit. Rev. Microbiol. 2017;43:81–95. doi: 10.1080/1040841X.2016.1176988. [DOI] [PubMed] [Google Scholar]
- 249.Holloszy J.O., Coyle E.F. Adaptations of skeletal muscle to endurance exercise and their metabolic consequences. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1984;56:831–838. doi: 10.1152/jappl.1984.56.4.831. [DOI] [PubMed] [Google Scholar]
- 250.Bird S.R., Hawley J.A. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc. Med. 2016;2:e000143. doi: 10.1136/bmjsem-2016-000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Gemmink A., Schrauwen P., Hesselink M.K.C. Exercising your fat (metabolism) into shape: A muscle-centred view. Diabetologia. 2020;63:1453–1463. doi: 10.1007/s00125-020-05170-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Hargreaves M., Spriet L.L. Exercise Metabolism: Fuels for the Fire. Cold Spring Harb. Perspect. Med. 2018;8:a029744. doi: 10.1101/cshperspect.a029744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Coyle E.F. Physical activity as a metabolic stressor. Am. J. Clin. Nutr. 2000;72:512s–520s. doi: 10.1093/ajcn/72.2.512S. [DOI] [PubMed] [Google Scholar]
- 254.Ji L.L., Yeo D., Kang C., Zhang T. The role of mitochondria in redox signaling of muscle homeostasis. J. Sport Health Sci. 2020;9:386–393. doi: 10.1016/j.jshs.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Phillips S.A., Das E., Wang J., Pritchard K., Gutterman D.D. Resistance and aerobic exercise protects against acute endothelial impairment induced by a single exposure to hypertension during exertion. J. Appl. Physiol. 2011;110:1013–1020. doi: 10.1152/japplphysiol.00438.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.MacDougall J.D., Tuxen D., Sale D.G., Moroz J.R., Sutton J.R. Arterial blood pressure response to heavy resistance exercise. J. Appl. Physiol. 1985;58:785–790. doi: 10.1152/jappl.1985.58.3.785. [DOI] [PubMed] [Google Scholar]
- 257.Kazeminia M., Daneshkhah A., Jalali R., Vaisi-Raygani A., Salari N., Mohammadi M. The Effect of Exercise on the Older Adult’s Blood Pressure Suffering Hypertension: Systematic Review and Meta-Analysis on Clinical Trial Studies. Int. J. Hypertens. 2020;2020:2786120. doi: 10.1155/2020/2786120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Oliver-Martínez P.A., Ramos-Campo D.J., Martínez-Aranda L.M., Martínez-Rodríguez A., Rubio-Arias J. Chronic effects and optimal dosage of strength training on SBP and DBP: A systematic review with meta-analysis. J. Hypertens. 2020;38:1909–1918. doi: 10.1097/HJH.0000000000002459. [DOI] [PubMed] [Google Scholar]
- 259.Green D.J., Hopman M.T., Padilla J., Laughlin M.H., Thijssen D.H. Vascular Adaptation to Exercise in Humans: Role of Hemodynamic Stimuli. Physiol. Rev. 2017;97:495–528. doi: 10.1152/physrev.00014.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Barretti D.L., Magalhães Fde C., Fernandes T., do Carmo E.C., Rosa K.T., Irigoyen M.C., Negrão C.E., Oliveira E.M. Effects of aerobic exercise training on cardiac renin-angiotensin system in an obese Zucker rat strain. PLoS ONE. 2012;7:e46114. doi: 10.1371/journal.pone.0046114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Ren C.Z., Yang Y.H., Sun J.C., Wu Z.T., Zhang R.W., Shen D., Wang Y.K. Exercise Training Improves the Altered Renin-Angiotensin System in the Rostral Ventrolateral Medulla of Hypertensive Rats. Oxid. Med. Cell. Longev. 2016;2016:7413963. doi: 10.1155/2016/7413963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Shinshi Y., Higashiura K., Yoshida D., Togashi N., Yoshida H., Miyazaki Y., Ura N., Shimamoto K. Angiotensin II inhibits glucose uptake of skeletal muscle via the adenosine monophosphate-activated protein kinase pathway. J. Am. Soc. Hypertens. 2007;1:251–255. doi: 10.1016/j.jash.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 263.Richter E.A., Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol. Rev. 2013;93:993–1017. doi: 10.1152/physrev.00038.2012. [DOI] [PubMed] [Google Scholar]
- 264.Drake J.C., Wilson R.J., Yan Z. Molecular mechanisms for mitochondrial adaptation to exercise training in skeletal muscle. FASEB J. 2016;30:13–22. doi: 10.1096/fj.15-276337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Hall E.C.R., Murgatroyd C., Stebbings G.K., Cunniffe B., Harle L., Salter M., Ramadass A., Westra J.W., Hunter E., Akoulitchev A., et al. The Prospective Study of Epigenetic Regulatory Profiles in Sport and Exercise Monitored Through Chromosome Conformation Signatures. Genes. 2020;11:905. doi: 10.3390/genes11080905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Bird A. Perceptions of epigenetics. Nature. 2007;447:396–398. doi: 10.1038/nature05913. [DOI] [PubMed] [Google Scholar]
- 267.Khan M.A., Sany M.R.U., Islam M.S., Islam A. Epigenetic Regulator miRNA Pattern Differences among SARS-CoV, SARS-CoV-2, and SARS-CoV-2 World-Wide Isolates Delineated the Mystery Behind the Epic Pathogenicity and Distinct Clinical Characteristics of Pandemic COVID-19. Front. Genet. 2020;11:765. doi: 10.3389/fgene.2020.00765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Mitash N., Donovan J.E., Swiatecka-Urban A. The Role of MicroRNA in the Airway Surface Liquid Homeostasis. Int. J. Mol. Sci. 2020;21:3848. doi: 10.3390/ijms21113848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.He L., Hannon G.J. MicroRNAs: Small RNAs with a big role in gene regulation. Nat. Rev. Genet. 2004;5:522–531. doi: 10.1038/nrg1379. [DOI] [PubMed] [Google Scholar]
- 270.Donaldson A., Natanek S.A., Lewis A., Man W.D., Hopkinson N.S., Polkey M.I., Kemp P.R. Increased skeletal muscle-specific microRNA in the blood of patients with COPD. Thorax. 2013;68:1140–1149. doi: 10.1136/thoraxjnl-2012-203129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Sardar R., Satish D., Birla S., Gupta D. Integrative analyses of SARS-CoV-2 genomes from different geographical locations reveal unique features potentially consequential to host-virus interaction, pathogenesis and clues for novel therapies. Heliyon. 2020;6:e04658. doi: 10.1016/j.heliyon.2020.e04658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Schmitz B., Breulmann F.L., Jubran B., Rolfes F., Thorwesten L., Krüger M., Klose A., Schnittler H.J., Brand S.M. A three-step approach identifies novel shear stress-sensitive endothelial microRNAs involved in vasculoprotective effects of high-intensity interval training (HIIT) Oncotarget. 2019;10:3625–3640. doi: 10.18632/oncotarget.26944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Camera D.M., Ong J.N., Coffey V.G., Hawley J.A. Selective Modulation of MicroRNA Expression with Protein Ingestion Following Concurrent Resistance and Endurance Exercise in Human Skeletal Muscle. Front. Physiol. 2016;7:87. doi: 10.3389/fphys.2016.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.D’Souza R.F., Markworth J.F., Aasen K.M.M., Zeng N., Cameron-Smith D., Mitchell C.J. Acute resistance exercise modulates microRNA expression profiles: Combined tissue and circulatory targeted analyses. PLoS ONE. 2017;12:e0181594. doi: 10.1371/journal.pone.0181594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.D’Souza R.F., Woodhead J.S.T., Zeng N., Blenkiron C., Merry T.L., Cameron-Smith D., Mitchell C.J. Circulatory exosomal miRNA following intense exercise is unrelated to muscle and plasma miRNA abundances. Am. J. Physiol. Endocrinol. Metab. 2018;315:E723–E733. doi: 10.1152/ajpendo.00138.2018. [DOI] [PubMed] [Google Scholar]
- 276.Silver J.L., Alexander S.E., Dillon H.T., Lamon S., Wadley G.D. Extracellular vesicular miRNA expression is not a proxy for skeletal muscle miRNA expression in males and females following acute, moderate intensity exercise. Physiol. Rep. 2020;8:e14520. doi: 10.14814/phy2.14520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.McGee S.L., Hargreaves M. Histone modifications and exercise adaptations. J. Appl. Physiol. 2011;110:258–263. doi: 10.1152/japplphysiol.00979.2010. [DOI] [PubMed] [Google Scholar]
- 278.Tian H., Liu S., Ren J., Lee J.K.W., Wang R., Chen P. Role of Histone Deacetylases in Skeletal Muscle Physiology and Systemic Energy Homeostasis: Implications for Metabolic Diseases and Therapy. Front. Physiol. 2020;11:949. doi: 10.3389/fphys.2020.00949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Javaid N., Choi S. Acetylation- and Methylation-Related Epigenetic Proteins in the Context of Their Targets. Genes. 2017;8:196. doi: 10.3390/genes8080196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Turner D.C., Gorski P.P., Maasar M.F., Seaborne R.A., Baumert P., Brown A.D., Kitchen M.O., Erskine R.M., Dos-Remedios I., Voisin S., et al. DNA methylation across the genome in aged human skeletal muscle tissue and muscle-derived cells: The role of HOX genes and physical activity. Sci. Rep. 2020;10:15360. doi: 10.1038/s41598-020-72730-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Lim C., Shimizu J., Kawano F., Kim H.J., Kim C.K. Adaptive responses of histone modifications to resistance exercise in human skeletal muscle. PLoS ONE. 2020;15:e0231321. doi: 10.1371/journal.pone.0231321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Seaborne R.A., Strauss J., Cocks M., Shepherd S., O’Brien T.D., van Someren K.A., Bell P.G., Murgatroyd C., Morton J.P., Stewart C.E., et al. Human Skeletal Muscle Possesses an Epigenetic Memory of Hypertrophy. Sci. Rep. 2018;8:1898. doi: 10.1038/s41598-018-20287-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Vishnubalaji R., Shaath H., Alajez N.M. Protein Coding and Long Noncoding RNA (lncRNA) Transcriptional Landscape in SARS-CoV-2 Infected Bronchial Epithelial Cells Highlight a Role for Interferon and Inflammatory Response. Genes. 2020;11:760. doi: 10.3390/genes11070760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Fernandes J.C.R., Acuña S.M., Aoki J.I., Floeter-Winter L.M., Muxel S.M. Long Non-Coding RNAs in the Regulation of Gene Expression: Physiology and Disease. Noncoding RNA. 2019;5:17. doi: 10.3390/ncrna5010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Bonilauri B., Dallagiovanna B. Long Non-coding RNAs Are Differentially Expressed after Different Exercise Training Programs. Front. Physiol. 2020;11:567614. doi: 10.3389/fphys.2020.567614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Hargreaves M. Exercise and Gene Expression. Prog. Mol. Biol. Transl. Sci. 2015;135:457–469. doi: 10.1016/bs.pmbts.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 287.Howlett K.F., McGee S.L. Epigenetic regulation of skeletal muscle metabolism. Clin. Sci. 2016;130:1051–1063. doi: 10.1042/CS20160115. [DOI] [PubMed] [Google Scholar]
- 288.Jacques M., Hiam D., Craig J., Barrès R., Eynon N., Voisin S. Epigenetic changes in healthy human skeletal muscle following exercise- a systematic review. Epigenetics. 2019;14:633–648. doi: 10.1080/15592294.2019.1614416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Widmann M., Nieß A.M., Munz B. Physical Exercise and Epigenetic Modifications in Skeletal Muscle. Sports Med. 2019;49:509–523. doi: 10.1007/s40279-019-01070-4. [DOI] [PubMed] [Google Scholar]
- 290.Soplinska A., Zareba L., Wicik Z., Eyileten C., Jakubik D., Siller-Matula J.M., De Rosa S., Malek L.A., Postula M. MicroRNAs as Biomarkers of Systemic Changes in Response to Endurance Exercise-A Comprehensive Review. Diagnostics. 2020;10:813. doi: 10.3390/diagnostics10100813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Seaborne R.A., Sharples A.P. The Interplay Between Exercise Metabolism, Epigenetics, and Skeletal Muscle Remodeling. Exerc. Sport Sci. Rev. 2020;48:188–200. doi: 10.1249/JES.0000000000000227. [DOI] [PubMed] [Google Scholar]
- 292.Ferrari L., Vicenzi M., Tarantini L., Barretta F., Sironi S., Baccarelli A.A., Guazzi M., Bollati V. Effects of Physical Exercise on Endothelial Function and DNA Methylation. Int. J. Environ. Res. Public Health. 2019;16:2530. doi: 10.3390/ijerph16142530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Evans W.S., Sapp R.M., Kim K.I., Heilman J.M., Hagberg J., Prior S.J. Effects of Exercise Training on the Paracrine Function of Circulating Angiogenic Cells. Int. J. Sports Med. 2020 doi: 10.1055/a-1273-8390. [DOI] [PubMed] [Google Scholar]
- 294.Friedman J.R., Nunnari J. Mitochondrial form and function. Nature. 2014;505:335–343. doi: 10.1038/nature12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Refolo G., Vescovo T., Piacentini M., Fimia G.M., Ciccosanti F. Mitochondrial Interactome: A Focus on Antiviral Signaling Pathways. Front. Cell Dev. Biol. 2020;8:8. doi: 10.3389/fcell.2020.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Bilet L., Phielix E., van de Weijer T., Gemmink A., Bosma M., Moonen-Kornips E., Jorgensen J.A., Schaart G., Zhang D., Meijer K., et al. One-leg inactivity induces a reduction in mitochondrial oxidative capacity, intramyocellular lipid accumulation and reduced insulin signalling upon lipid infusion: A human study with unilateral limb suspension. Diabetologia. 2020;63:1211–1222. doi: 10.1007/s00125-020-05128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 298.Mauvais-Jarvis F. Aging, Male Sex, Obesity, and Metabolic Inflammation Create the Perfect Storm for COVID-19. Diabetes. 2020;69:1857–1863. doi: 10.2337/dbi19-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Trott D.W., Fadel P.J. Inflammation as a mediator of arterial ageing. Exp. Physiol. 2019;104:1455–1471. doi: 10.1113/EP087499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Zhang J., Tecson K.M., McCullough P.A. Endothelial dysfunction contributes to COVID-19-associated vascular inflammation and coagulopathy. Rev. Cardiovasc. Med. 2020;21:315–319. doi: 10.31083/j.rcm.2020.03.126. [DOI] [PubMed] [Google Scholar]
- 301.Devries M.C., Samjoo I.A., Hamadeh M.J., McCready C., Raha S., Watt M.J., Steinberg G.R., Tarnopolsky M.A. Endurance training modulates intramyocellular lipid compartmentalization and morphology in skeletal muscle of lean and obese women. J. Clin. Endocrinol. Metab. 2013;98:4852–4862. doi: 10.1210/jc.2013-2044. [DOI] [PubMed] [Google Scholar]
- 302.Meex R.C., Schrauwen-Hinderling V.B., Moonen-Kornips E., Schaart G., Mensink M., Phielix E., van de Weijer T., Sels J.P., Schrauwen P., Hesselink M.K. Restoration of muscle mitochondrial function and metabolic flexibility in type 2 diabetes by exercise training is paralleled by increased myocellular fat storage and improved insulin sensitivity. Diabetes. 2010;59:572–579. doi: 10.2337/db09-1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Singh K.K., Chaubey G., Chen J.Y., Suravajhala P. Decoding SARS-CoV-2 hijacking of host mitochondria in COVID-19 pathogenesis. Am. J. Physiol.-Cell Physiol. 2020;319:C258–C267. doi: 10.1152/ajpcell.00224.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Ajaz S., McPhail M.J., Singh K.K., Mujib S., Trovato F.M., Napoli S., Agarwal K. Mitochondrial metabolic manipulation by SARS-CoV-2 in peripheral blood mononuclear cells of patients with COVID-19. Am. J. Physiol.-Cell Physiol. 2021;320:C57–C65. doi: 10.1152/ajpcell.00426.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Burtscher J., Cappellano G., Omori A., Koshiba T., Millet G.P. Mitochondria: In the Cross Fire of SARS-CoV-2 and Immunity. iScience. 2020;23:101631. doi: 10.1016/j.isci.2020.101631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Burtscher J., Millet G.P., Burtscher M. Low cardiorespiratory and mitochondrial fitness as risk factors in viral infections: Implications for COVID-19. Br. J. Sports Med. 2020 doi: 10.1136/bjsports-2020-103572. [DOI] [PubMed] [Google Scholar]
- 307.Park S.Y., Rossman M.J., Gifford J.R., Bharath L.P., Bauersachs J., Richardson R.S., Abel E.D., Symons J.D., Riehle C. Exercise training improves vascular mitochondrial function. Am. J. Physiol. Heart Circ. Physiol. 2016;310:H821–H829. doi: 10.1152/ajpheart.00751.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Somani S.M., Husain K. Exercise training alters kinetics of antioxidant enzymes in rat tissues. Biochem. Mol. Biol. Int. 1996;38:587–595. [PubMed] [Google Scholar]
- 309.Chang C.H., Kao C.H., Chio C.C., Lin C.H., Lin M.T., Chang C.P. Attenuating heatstroke-induced acute lung inflammation, edema, and injury in rats by exercise preconditioning. J. Trauma. Acute Care Surg. 2013;74:1052–1059. doi: 10.1097/TA.0b013e31827a3618. [DOI] [PubMed] [Google Scholar]
- 310.Trangmar S.J., Chiesa S.T., Kalsi K.K., Secher N.H., González-Alonso J. Whole body hyperthermia, but not skin hyperthermia, accelerates brain and locomotor limb circulatory strain and impairs exercise capacity in humans. Physiol. Rep. 2017;5:e13108. doi: 10.14814/phy2.13108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Henstridge D.C., Febbraio M.A., Hargreaves M. Heat shock proteins and exercise adaptations. Our knowledge thus far and the road still ahead. J. Appl. Physiol. 2016;120:683–691. doi: 10.1152/japplphysiol.00811.2015. [DOI] [PubMed] [Google Scholar]
- 312.Krause M., Heck T.G., Bittencourt A., Scomazzon S.P., Newsholme P., Curi R., Homem de Bittencourt P.I., Jr. The chaperone balance hypothesis: The importance of the extracellular to intracellular HSP70 ratio to inflammation-driven type 2 diabetes, the effect of exercise, and the implications for clinical management. Mediat. Inflamm. 2015;2015:249205. doi: 10.1155/2015/249205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Heck T.G., Ludwig M.S., Frizzo M.N., Rasia-Filho A.A., Homem de Bittencourt P.I. Suppressed anti-inflammatory heat shock response in high-risk COVID-19 patients: Lessons from basic research (inclusive bats), light on conceivable therapies. Clin. Sci. 2020;134:1991–2017. doi: 10.1042/CS20200596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Moreno Fernández-Ayala D.J., Navas P., Lόpez-Lluch G. Age-related mitochondrial dysfunction as a key factor in COVID-19 disease. Exp. Gerontol. 2020;142:111147. doi: 10.1016/j.exger.2020.111147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.da Silva Gomes Dias S., Soares V.C., Ferreira A.C., Sacramento C.Q., Fintelman-Rodrigues N., Temerozo J.R., Teixeira L., Barreto E., Mattos M., de Freitas C.S., et al. Lipid droplets fuel SARS-CoV-2 replication and production of inflammatory mediators. bioRxiv. 2020 doi: 10.1101/2020.08.22.262733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Silvas J.A., Jureka A.S., Nicolini A.M., Chvatal S.A., Basler C.F. Inhibitors of VPS34 and lipid metabolism suppress SARS-CoV-2 replication. bioRxiv Prepr. Serv. Biol. 2020 doi: 10.1101/2020.07.18.210211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Hsu C.C., Tsai H.H., Fu T.C., Wang J.S. Exercise Training Enhances Platelet Mitochondrial Bioenergetics in Stroke Patients: A Randomized Controlled Trial. J. Clin. Med. 2019;8:2186. doi: 10.3390/jcm8122186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Chou C.H., Fu T.C., Tsai H.H., Hsu C.C., Wang C.H., Wang J.S. High-intensity interval training enhances mitochondrial bioenergetics of platelets in patients with heart failure. Int. J. Cardiol. 2019;274:214. doi: 10.1016/j.ijcard.2018.07.104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.