Abstract
Background
Anxiety and alcohol use disorders are common and disabling conditions that people typically endure for many years before accessing treatment. The link between anxiety and alcohol use is well-established, with these issues commonly emerging and/or escalating during emerging adulthood. This randomized controlled trial evaluated a psychologist-supported, web-based intervention, designed with and for emerging adults, that aims to promote adaptive coping strategies, and prevent anxiety and alcohol use from progressing to chronic, mutually-reinforcing disorders.
Methods
Between December 2017 and September 2018, 123 emerging adults (aged 17–24) reporting anxiety symptoms and hazardous alcohol use were randomized to receive the Inroads or control (assessment plus alcohol information) intervention. The Inroads program combined five web-based cognitive behavioral therapy modules with weekly psychologist support via email/phone. Primary outcomes were alcohol consumption, severity of alcohol-related consequences, and general anxiety symptoms, assessed at baseline, 2 and 6-months post-baseline. Secondary outcomes included hazardous alcohol use and social anxiety. Trial Registration: Prospectively registered in the Australian New Zealand Clinical Trials Registry, ACTRN12617001609347.
Findings
Alcohol consumption and associated consequences reduced in both groups, with the Inroads group reporting greater alcohol reductions by 6-month follow-up (mean difference -0.74, 95% CI: -1.47 to -0.01, d = 0.24). Relative to controls, hazardous alcohol use reduced among Inroads participants at both follow-ups (2-month mean difference -2.14, 95% CI: -4.06 to -0.22). Inroads participants also reported reduced symptoms of general (mean difference -3.06, 95% CI: -4.97 to -1.15, d = 0.88) and social anxiety (mean difference -3.21, 95% CI: -6.34 to -0.07, d = 0.32) at 2-month follow-up, with improvements in social anxiety sustained at 6-months.
Interpretation
The Inroads program demonstrated beneficial effects on alcohol consumption, hazardous alcohol use, and anxiety symptoms. The web-based format is aligned with youth treatment preferences and can be delivered at scale to achieve wide dissemination and reduce the significant burden associated with these chronic, mutually reinforcing conditions.
Funding
Australian Rotary Health, Australian National Health and Medical Research Council.
Keywords: Alcohol, Alcohol-related disorders, Anxiety, Social anxiety, Comorbidity, Early intervention, Cognitive behavioral therapy, CBT, Internet-delivered, Web-based, Digital, Youth, Young adult, Emerging adult
Research in context.
Evidence before this study
Emerging adulthood is a peak risk period for onset and escalation of anxiety and alcohol use disorders, which commonly co-occur and tend to exacerbate each other in a self-perpetuating cycle. People with co-occurring anxiety and alcohol use disorders typically experience greater symptom severity and poor response to standard treatment approaches, however recent evidence supports the efficacy of integrated treatments that explicitly target the inter-relationship between anxiety and alcohol use.
Added value of this study
This is the first randomized controlled trial to evaluate an integrated, web-based intervention for emerging adults that promotes cognitive behavioral coping skills to manage anxiety symptoms, hazardous alcohol use and the connections between them. The results provide evidence that the Inroads program combined with low intensity psychologist support achieved more sustained reductions in alcohol consumption, and greater immediate reductions in anxiety symptoms and hazardous alcohol use relative to the control condition.
Implications of all the available evidence
A psychologist supported, web-based intervention that simultaneously addresses anxiety symptoms and hazardous drinking was well-received by emerging adults and resulted in significant reductions in anxiety and hazardous alcohol use. Importantly, the web-based format of the Inroads program means it can be disseminated widely and sustainably to promote adaptive coping strategies during a high-risk developmental stage, and prevent anxiety and alcohol use from exacerbating one another and becoming further entrenched.
Alt-text: Unlabelled box
1. Introduction
Globally, anxiety and alcohol use disorders are among the most prevalent and debilitating mental disorders, affecting up to one in four and one in six people in their lifetime, respectively [1]. It is common for anxiety and alcohol use disorders to co-occur, and when they do, the presenting symptoms tend to be more severe and associated with greater functional impairment than either disorder alone [2]. Anxiety symptoms typically precede hazardous alcohol use [3], and the self-medication model proposes that people with anxiety are susceptible to alcohol use disorders because they consume alcohol in an attempt to reduce or cope with anxiety symptoms [4]. Once established, anxiety and alcohol use disorders tend to exacerbate each other in a self-perpetuating cycle, whereby reliance on alcohol to cope with anxiety leads to progressively more drinking, and increasing alcohol use can lead to psychosocial problems and alcohol withdrawal symptoms, which in turn exacerbate anxiety [2].
Co-occurrence between anxiety and alcohol use disorders can also interfere with treatment and recovery from either disorder. People with co-occurring anxiety and alcohol use disorders may be less willing to seek or engage with treatment [3], and standard single-disorder treatments are less effective for people with co-occurring anxiety and alcohol use [2,3]. Given the mutually reinforcing connections between anxiety and alcohol use, effective treatment may require an integrated approach that targets both disorders concurrently, as well as the inter-relationship between them. Emerging evidence from clinical trials supports this view, with results showing greater reduction in anxiety symptoms, alcohol use and/or functional impairment following integrated treatment compared to traditional single-disorder approaches [5,6].
Emerging adulthood is a key window of opportunity for intervention to prevent the significant burden associated with co-occurring anxiety and alcohol use disorders. The term “emerging adulthood” has been applied to describe the unique period from the late teens through the mid-20s, which is characterised by a range of significant personal and social role changes, including increased independence, new relationships, occupational and living arrangements [7]. For some young people, adjusting to these changes can be challenging, and this developmental stage is a key risk period for the development and escalation of both anxiety and alcohol use disorders [8]. In Australia, one in six emerging adults aged 16–24 years met diagnosis for an anxiety disorder in the 12 months prior [9], and nearly one in three consume alcohol at hazardous levels as defined by the Alcohol Use Disorders Identification Test (AUDIT) [10]. Anxiety disorders in youth are associated with increased risk of coping-motivated drinking [11], earlier first use of alcohol [12] and progression from first alcohol use to regular use, and from regular use to alcohol use disorder [13]. In view of this inter-relationship, there are clear advantages to intervening in youth to promote adaptive coping strategies and address the interconnection between anxiety and alcohol use, before these conditions become deeply intertwined in an exacerbating self-perpetuating cycle.
Despite the developmental connections identified between anxiety and alcohol use, and significant and chronic health, legal, social and financial consequences associated with early onset of these disorders [14], there are no existing youth-focussed interventions that target anxiety symptoms, hazardous alcohol use and the interconnections between them. Web-based delivery is an advantageous format for youth interventions, as it reduces common barriers to help-seeking such as fear of judgement or stigma, and difficulties accessing treatment at a convenient time or location [15]. Indeed, a scoping review found that young people prefer online over face-to-face treatments, and feel more empowered, confident, in control and less concerned about privacy when support is delivered via videoconferencing or web-based applications [15]. Furthermore, a randomized controlled trial (RCT) supported the benefits of a youth-focussed web-based intervention for co-occurring depression and harmful alcohol use, with clinically significant short-term improvements observed compared to an attention-control [16]. Systematic review suggests the limitations of web-based interventions in terms of engagement and retention can be ameliorated through the provision of psychologist support via phone, chat or email [17].
To address the need for an engaging, non-stigmatizing intervention that equips young people with effective strategies to address co-occurring anxiety and alcohol use, we report the first RCT of a co-designed, web-based intervention for emerging adults (aged 17–24 years). We hypothesised that Inroads program combined with psychologist support via phone/email would achieve greater reductions sustained over 6-months in alcohol use, alcohol-related harms and anxiety symptoms compared to an active control (alcohol information and guidelines).
2. Methods
2.1. Study design
The study was a parallel RCT conducted nationally across Australia. The target sample size (n = 122) was conservatively designed to have 80% power to detect a moderate effect size of 0.5 between conditions, assuming 35% attrition. Trial procedures, pre-specified outcomes and sample size calculations are detailed in the study protocol [18]. The study was prospectively registered with the Australian New Zealand Clinical Trials Registry (ACTRN12617001609347) and received approval from the University of New South Wales (HC17185) and University of Sydney (2018/877) Human Research Ethics Committees. The study adheres to the CONSORT guidelines [19] for reporting randomised trials.
2.2. Participants and recruitment
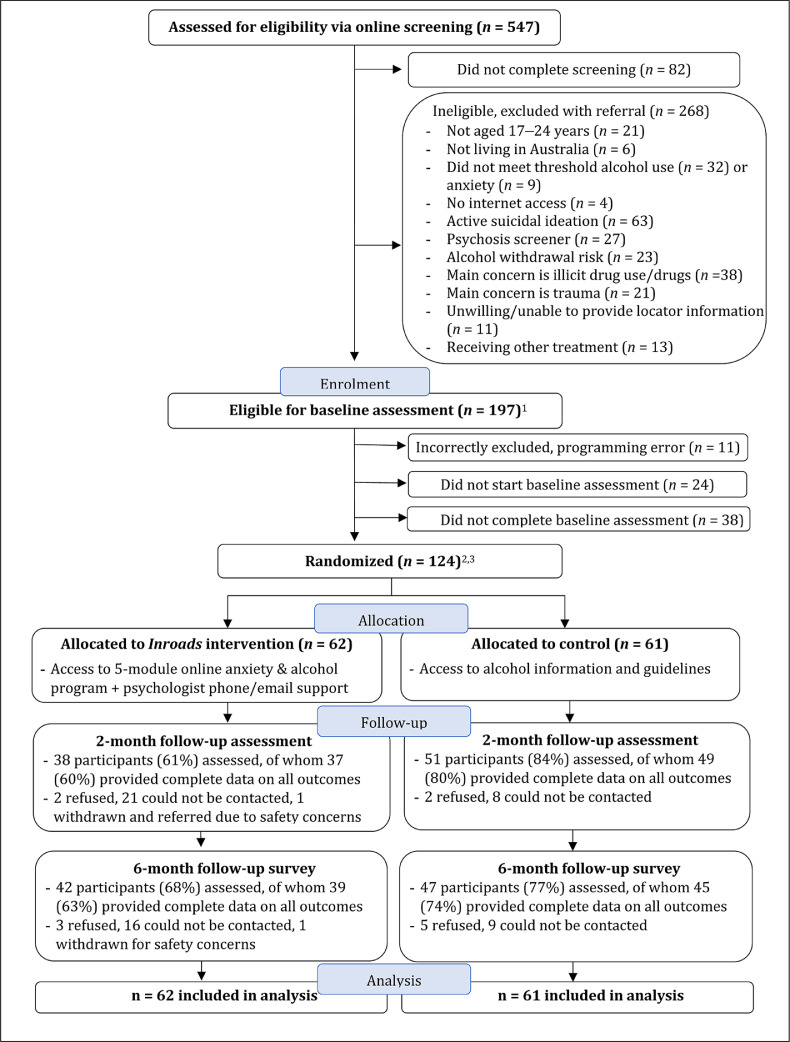
Participants were recruited to the study between 19th December 2017 and 11th September 2018 via a comprehensive, targeted strategy including media coverage, social media, distribution of flyers at educational institutions, and referral from youth services. Eligible participants were currently: (i) aged between 17 and 24 years and living in Australia, (ii) reporting hazardous levels of alcohol use, as indicated by a score of ≥ 8 on the AUDIT [20], and (iii) reporting at least mild anxiety symptoms, as indicated by a score ≥ 5 on the Generalized Anxiety Disorder Questionnaire (GAD-7) [21] or ≥ 6 on the Mini-Social Phobia Inventory (Mini-SPIN) [22]. Screening instruments (detailed in [18]) assessed the following exclusion criteria: (i) unable or unwilling to provide contact information, (ii) insufficient English literacy or no access to the Internet, (iii) daily use of cannabis, benzodiazepines, or weekly use of psychostimulants, (iv) self-reported primary concern related to trauma or substances other than alcohol, (v) at significant risk of complicated alcohol withdrawal, (vi) active suicidal ideation, (vii) active symptoms of psychosis, or (viii) currently accessing ongoing psychological treatment. These exclusion criteria reflected characteristics that would impede treatment engagement, or where more intensive or specialized support was indicated. Fig. 1 shows participant recruitment, flow through the trial, and retention at follow-up assessments.
Fig. 1.
CONSORT diagram showing participant flow through the study. 1Participants who were eligible for the study did not differ significantly on symptom severity at screening (AUDIT, GAD-7, Mini-SPIN) from those who did not complete screening, nor from those who were excluded (p values > .32), with the exception of GAD-7 scores, which were significantly higher among excluded participants than eligible participants (t(463) = 2.45, p = .01). 2Participants who were randomised to the study had significantly higher AUDIT scores at screening than participants who were eligible but did not proceed to treatment (t(195) = -3.23, p = .001). Mini-SPIN and GAD-7 symptom severity was not different between these two groups at the screening assessment (p values > .52). 3One ineligible participant was incorrectly randomized due to a programming error and was excluded from the study, leaving a final sample of n = 123.
2.3. Randomization and masking
Eligible participants were individually randomized on a 1:1 basis to the intervention group (Inroads program), or the control group (alcohol information and safe drinking guidelines). Randomization was programmed with the constraint that no more than 10 participants could be consecutively allocated into one condition to ensure balanced group sizes. To avoid potential for bias, participants were randomized via the trial website using a computer-generated randomization sequence, which was concealed from the research team. The research assistant (BL) responsible for calling participants about follow up assessments was blinded to group allocation. As participants played an active role in implementing the intervention strategies it was not possible to blind them to the intervention they were allocated to.
2.4. Outcomes
Primary outcomes: Primary alcohol outcomes were mean standard drinks (10g of alcohol) consumed per day over the past 28 days, assessed by a computerized Timeline Follow-Back procedure (TLFB)[23] and alcohol-related consequences, assessed by the Brief-Young Adult Alcohol Consequences Questionnaire (B-YAACQ; range 0–24)[24]. Anxiety symptoms were assessed by the GAD-7 (range 0–21), which is sensitive to symptoms across anxiety disorders and has been validated in emerging adults [21].
Secondary outcomes: Frequency of binge drinking (single episode consumption of ≥ 5 standard drinks) was derived from TLFB data, severity of hazardous alcohol use was assessed by the AUDIT total score range (0–40)[20], specific social anxiety symptoms were assessed by a composite of the Social Interaction Anxiety Scale and Social Phobia Scale–Short forms (SIAS+SPS; range 0–48)[25], and depression symptoms were assessed by the Depression and Anxiety Stress Scale (DASS-21; range 0–42)[26]. Functional impairment was captured by the global score on the Sheehan Disability Scale (range 0 “unimpaired” to 30 “highly impaired”)[27], and number of days lost or unproductive due to symptoms were examined separately as this indicator of impairment is not captured by the global score. The observed reliability (Cronbach's α) for all outcome variables is provided in Supplementary Table 1.
Adverse Events were determined by (i) spontaneous reports to the study psychologists or research team, (ii) open feedback questions probing about negative aspects of the program and (iii) deterioration in anxiety, alcohol use or overall functional impairment according to the widely used reliable change index. Full details regarding the definition and assessment of adverse events are provided in the Supplementary Material.
2.5. Procedure
Prospective participants were referred to the study website (inroads.org.au) to review information about the study procedures prior to consent. Participants were informed that should they be allocated to the control group, they could enroll in the Inroads program, if they wished, following completion of the 6-month follow-up assessment. Consenting participants completed online eligibility screening, and those meeting inclusion criteria were invited to complete an online baseline assessment of sociodemographic characteristics, primary and secondary outcomes. Ineligible participants were provided with a list of referral options. To allow some flexibility in the rate of program completion, assessments were administered at 2-months post-baseline (primary end point), and again at 6-months post-baseline. For participants in the Inroads group, the 2-month assessment included feedback questions about the program. All participants received automatic email prompts to complete assessments. If participants did not complete the follow-up assessments within 3 days, standardized email and SMS reminders were sent, and reminder calls were made by a Research Assistant (BL) who was blind to group allocation. Participants were reimbursed with a $30 gift voucher for each follow-up assessment, and participants who completed both assessments were entered into a draw to win an Apple iPhone.
2.6. Interventions
Inroads anxiety and alcohol use intervention: A detailed description of the Inroads program is provided in the trial protocol [18]. Inroads is a youth-focused, web-based cognitive behavioural therapy (CBT) program for emerging adults (aged 17–24 years), to concurrently address transdiagnostic anxiety, hazardous alcohol use and the connections between them. The program draws on components from tested integrated treatments for adults with social anxiety and alcohol use disorder [28] and youth alcohol use and depression control [16]. Participants are guided through five sequential modules, with access to each module opened at a rate of one per week. The five modules focus on: (1) understanding patterns and motives for alcohol use, psychoeducation about cognitive, physiological and behavioral aspects of anxiety, and the inter-relationship between anxiety and drinking; (2) introduction to cognitive therapy and application to anxious thoughts; (3) CBT strategies for sticking to drinking limits and cognitive therapy targeting positive alcohol expectancies i.e. “drinking thinking”; (4) the link between avoidance and anxiety, gradually facing fears through behavioral experiments; (5) social support, longer-term goal-setting and relapse prevention. The program was co-developed with the target age group and in consultation with youth service providers; this development process is described in full elsewhere [29]. To optimize participant retention, the program incorporated interactive and engaging features such as quizzes, videos, and case vignettes, and participants were encouraged to progress through the modules via automated email notifications. Support was provided by a clinical psychologist via a weekly email providing feedback and personalized suggestions aligned to module content. In addition, telephone/text chat sessions (30 minutes) were offered following Modules 1 and 4; these focused on motivational enhancement, developing a shared problem formulation, troubleshooting, and tailoring behavioral experiments and cognitive therapy exercises. Participants could request additional psychologist support via phone/email if required due to distress or difficulty understanding or applying the program content.
Assessment plus alcohol information (control): Following baselines assessment, participants in the control group received an online information pamphlet outlining the effects of alcohol and risks of overuse, the Australian National Health and Medical Research Council's recommended guidelines for safe alcohol consumption, and a list of links to national telephone helplines and alcohol information websites. Participants were advised to read the information carefully and reflect on how it may apply to their circumstances. The information pamphlet was available for immediate download and was also emailed to participants.
2.7. Statistical analysis
All analyses were conducted on an intention to treat basis using Stata version 14.0. Normality assumptions were examined, and sensitivity analyses with transformed data conducted in cases when normality assumptions were violated. Primary analyses were multi-level mixed effects analysis, a rigorous method for modelling change over time that uses all available data and accommodates missing responses using maximum likelihood estimation. Models used baseline measurements as the reference point to estimate participant-specific starting points and change over time. Intervention was dummy-coded (Control = 0, Inroads = 1), and group by time interactions were examined to assess between-group differences in outcomes over time. Preliminary models estimated the most appropriate model and covariance structure was determined with reference to model fit statistics (restricted log likelihood, Akaike Information Criterion and Bayesian Information Criterion). Linear and quadratic effects were tested, however categorical coding for time was preferential for all variables. Final models incorporated estimation of a random intercept and slope and utilized an auto-regressive error structure for within-person repeated observations over time. Between and within-group effect sizes (Cohen's d) were calculated from the model estimated beta coefficients.
2.8. Role of the funding source
The funding source had no role in the design or execution of this study, nor its analyses, interpretation or decision to submit results.
3. Results
3.1. Participant characteristics
Fig. 1 illustrates the flow of participants through the study phases (enrolment, allocation and follow-up) according to CONSORT 2010 guidelines [19]. Online screening was conducted with 547 participants, of whom 82 did not complete screening, and 268 were referred because they did not meet the eligibility criteria. The final sample comprised 123 participants recruited between 19th December 2017 and 11th September 2018, who were 67% female, with a mean age of 21.6 (sd = 2.2). The majority reported moderate to severe anxiety symptoms at baseline, with 72% reporting anxiety in the moderate or severe category of the GAD-7 and 81% meeting Mini-SPIN criteria for a possible social anxiety disorder diagnosis. The sample also reported high levels of alcohol use, with a mean past-month consumption of 104 standard drinks, and 60% of the sample reporting AUDIT total scores indicative of alcohol dependence. As shown in Fig. 1, full baseline data were available for all participants, and 96 participants (78%) provided data for at least one of the two follow-up assessments. In response to an honesty screener [30], 98% of participants reported that their survey responses were truthful. Table 1 reports descriptive characteristics for the sample by group. The two groups were well-matched at baseline on outcome measures (Table 2), with the exception of the Sheehan Disability Scale score, which was significantly higher in the control group (t(118) = 3.10, p = .002). These baseline differences were accommodated within the analyses, which modelled change over time from participant-specific starting points estimated using baseline measurements.
Table 1.
Baseline demographic and clinical characteristics by study group.
| Control (n = 61) | Inroads (n = 62) | |
|---|---|---|
| Age (years),M(SD) | 21.19 (2.2) | 21.94 (2.2) |
| Sex,n(%) | ||
| Male | 17 (27.8%) | 22 (35.5%) |
| Female | 43 (70.5%) | 40 (64.5%) |
| Transgender or Non-binary Gender | 1 (1.6%) | 0 (0%) |
| Sexual orientation,n(%) | ||
| Heterosexual | 43 (70.5%) | 47 (75.8%) |
| Gay/ Homosexual | 4 (6.6%) | 5 (8.1%) |
| Bisexual | 13 (21.3%) | 9 (14.5%) |
| Other | 1 (1.6%) | 1 (1.6%) |
| Highest education obtained,n(%) | ||
| Primary School Qualification | 3 (4.9%) | 4 (6.5%) |
| Secondary School Qualification | 31 (50.8%) | 22 (35.5%) |
| Trade Certificate or Apprenticeship | 2 (3.3%) | 2 (3.2%) |
| Other Tertiary Diploma or Certificate | 7 (11.5%) | 9 (14.5%) |
| Bachelor's degree or Higher | 18 (29.5%) | 25 (40.3%) |
| Country of Birthn(%) | ||
| Australia | 49 (80.3%) | 52 (83.8%) |
| Other | 12 (19.7%) | 10 (16.1%) |
| Residence,n(%) | ||
| Major city | 54 (88.5%) | 55 (88.7%) |
| Regional or Remote | 7 (11.5%) | 7 (11.3%) |
| Employment status,n(%) | ||
| Employed Full Time | 20 (32.8%) | 29 (46.8%) |
| Employed Part-time/Casual | 19 (31.2%) | 14 (22.6%) |
| Full-time Student | 16 (26.2%) | 14 (22.6%) |
| Unemployed | 6 (9.8%) | 5 (8.1%) |
| Age at first drink (years),M(SD) | 14.69 (1.5) | 14.85 (2.1) |
| Total drinks past month,M(SD) | 108.27 (99.2) | 99.60 (85.4) |
| Total drinking days past month,M(SD) | 14.49 (7.7) | 14.15 (8.1) |
| Hazardous alcohol use severity (AUDIT category1;%) | ||
| Medium level | 11 (18.0%) | 17 (27.4%) |
| High level | 15 (24.6%) | 6 (9.7%) |
| Probable dependence | 35 (57.4%) | 39 (62.9%) |
| Baseline cannabis use,n(%) | ||
| Never | 22 (36.1%) | 23 (37.1%) |
| Less than monthly | 28 (45.9%) | 23 (37.1%) |
| Monthly | 6 (9.8%) | 8 (12.9%) |
| Weekly | 5 (8.2%) | 8 (12.9%) |
| Use of other illicit drugs,n(%) | ||
| Never | 32 (52.5%) | 25 (40.3%) |
| Less than monthly | 21 (34.4%) | 28 (45.2%) |
| Monthly | 8 (13.1%) | 9 (14.5%) |
| Primary concern (self-reported),n(%) | ||
| Anxious, on edge or unable to control worry | 33 (54.1%) | 26 (41.9%) |
| Fear or embarrassment, being center of attention | 8 (13.1%) | 6 (9.7%) |
| Feeling sad or depressed | 12 (19.7%) | 13 (21.0%) |
| Problems or concerns about alcohol use | 8 (13.1%) | 17 (27.4%) |
| GAD-7 severity category,n(%) | ||
| Minimal | 0 (0%) | 1 (1.6%) |
| Mild | 15 (24.6%) | 18 (29%) |
| Moderate | 23 (37.7%) | 23 (37.1%) |
| Severe | 23 (37.7%) | 20 (32.3%) |
1For descriptive purposes, AUDIT hazardous alcohol use total scores are grouped here according to categories of increasing alcohol risk from medium level (scores 8–15), high level (scores 16–19), to indication for alcohol dependence (scores of 20 and above)19.
Note: In line with the CONSORT 2010 guidelines, no test of significance of baseline differences between intervention groups were conducted for the covariates; however, the data were examined to identify any large differences between groups at baseline.
Table 2.
Primary and secondary outcomes by group (Inroads and control) at 2-month and 6-month follow-up assessments.
| Baseline |
2 months |
6 months |
||
|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||
| Primary outcomes | ||||
| 1. Average drinks per day, past month (TLFB) | ||||
| Control | 3.61 (3.31) | 2.14 (1.36) | 2.45 (1.88) | |
| Inroads | 3.32 (2.85) | 1.51 (1.14) | 1.53 (1.12) | |
| 2. Alcohol-related consequences (b-YAACQ) | ||||
| Control | 15.77 (4.59) | 13.20 (6.34) | 11.32 (6.45) | |
| Inroads | 14.21 (4.42) | 9.38 (6.43) | 7.19 (4.88) | |
| 3. Anxiety (GAD-7) | ||||
| Control | 12.84 (4.39) | 10.39 (5.42) | 9.23 (5.13) | |
| Inroads | 12.19 (4.09) | 6.84 (4.44) | 7.33 (4.52) | |
| Secondary outcomes | ||||
| 1. Hazardous alcohol use (AUDIT total) | ||||
| Control | 21.62 (6.39) | 18.84 (6.95) | 17.23 (6.22) | |
| Inroads | 21.02 (5.76) | 15.50 (5.64) | 14.26 (5.99) | |
| 2. Binge drinking frequency, past month (TLFB) | ||||
| Control | 8.17 (7.02) | 5.37 (4.87) | 6.83 (6.29) | |
| Inroads | 8.631 (7.08) | 3.87 (3.49) | 3.77 (3.31) | |
| 3. Social anxiety symptoms (SPS+SIAS) | ||||
| Control | 20.08 (9.19) | 19.08 (9.60) | 18.21 (10.16) | |
| Inroads | 17.81 (10.58) | 12.74 (8.82) | 11.59 (7.81) | |
| 4. Depression symptoms (DASS-21) | ||||
| Control | 16.39 (8.33) | 14.47 (8.38) | 14.29 (9.34) | |
| Inroads | 16.13 (8.47) | 11.16 (8.64) | 10.48 (8.69) | |
| 5. Functional impairment (SDS) | ||||
| Overall impairment score | ||||
| Control | 14.43 (6.72) | 9.76 (7.03) | 9.46 (7.21) | |
| Inroads | 11.49 (6.61) | 7.78 (7.27) | 4.62 (4.08) | |
| Days lost due to symptoms | ||||
| Control | 0.84 (1.21) | 0.62 (1.07) | 0.94 (1.42) | |
| Inroads | 0.63 (1.33) | 0.65 (1.53) | 0.15 (0.67) | |
| Unproductive days due to symptoms | ||||
| Control | 2.33 (2.01) | 1.68 (1.68) | 1.81 (1.88) | |
| Inroads | 2.10 (1.89) | 1.19 (1.93) | 0.49 (0.82) | |
M = Mean, SD = Standard deviation, b-YAACQ = Brief Young Adult Alcohol Consequences Questionnaire, TLFB = Timeline Follow Back, GAD-7 = Generalized Anxiety Disorder-7 questionnaire, AUDIT = Alcohol Use Disorders Identification Test, SIAS = Social Interaction Anxiety, SPS = Social Phobia Scale, DASS = Depression Anxiety Stress Scales, SDS = Sheehan Disability Scale.
3.2. Primary outcomes
Mixed model results for primary outcomes and corresponding effect sizes are reported in Table 3.
Table 3.
Mixed models for repeated measures fitted to primary outcomes with time period and intervention group.
| Baseline to 2-month follow-up |
Baseline to 6-month follow-up |
|||||
|---|---|---|---|---|---|---|
| Primary Outcomes |
b [95% CI] |
Cohen's d | p-value |
b [95% CI] |
Cohen's d | p-value |
| 1. Average drinks per day (TLFB) | ||||||
| Time effect (Control) | −1.14 [−1.64 to −0.65] | 0.33 | <0.001 | −0.80 [−1.31 to −0.29] | 0.23 | .002 |
| Time effect (Inroads) | −1.45 [−2.01 to −0.88] | 0.47 | <0.001 | −1.54 [−2.08 to −1.01] | 0.49 | <0.001 |
| Group x Time Interaction | −0.30 [−1.05 to 0.43] | 0.10 | .425 | −0.74 [−1.47 to −0.01] | 0.24 | .049 |
| 2. Alcohol-related consequences (b-YAACQ) | ||||||
| Time effect (Control) | −2.44 [−4.00 to −0.88] | 0.54 | .002 | −4.30 [−5.96 to −2.65] | 0.95 | <0.001 |
| Time effect (Inroads) | −4.57 [−6.32 to −2.84] | 1.02 | <0.001 | −6.60 [−8.35 to −4.85] | 1.47 | <0.001 |
| Group x Time Interaction | −2.14 [−4.47 to 0.19] | 0.48 | .073 | −2.29 [−4.71 to 0.11] | 0.51 | .062 |
| 3. Anxiety (GAD-7) | ||||||
| Time effect (Control) | −2.47 [−3.74 to −1.19] | 0.72 | <0.001 | −3.64 [−5.16 to −2.13] | 1.05 | <0.001 |
| Time effect (Inroads) | −5.56 [−6.97 to −4.14] | 1.60 | <0.001 | −4.96 [−6.53 to −3.38] | 1.43 | <0.001 |
| Group x Time Interaction | −3.06 [ −4.97 to −1.15] | 0.88 | .002 | −1.31 [−3.49 to 0.87] | 0.38 | .238 |
Alcohol use. Average daily alcohol consumption decreased significantly in both groups from baseline to 2-month follow-up. There was weak evidence of a group by time interaction at 6-month follow-up, indicating a rebound in alcohol use among participants in the control group, while participants in the Inroads group maintained lower levels of daily alcohol consumption by 6-month follow up (b= −0.74, 95% CI = [−1.47, −0.01], d = 0.24). Negative consequences related to alcohol consumption also decreased significantly in both groups from baseline to 2-month follow-up, and this was sustained at 6-month follow-up with no evidence of greater benefit in the Inroads group compared to control.
Anxiety. Participants in both groups reported significant reductions in their anxiety symptoms, and a significant group by time interaction indicated greater reduction at 2-month follow up for participants in the Inroads group (b= −3.06, 95% CI = [−4.97, −1.15], d = 0.88). The control group showed a pattern of continued anxiety reduction, and by 6-month follow up, had achieved comparable reductions to the Inroads group, with no evidence of between-group differences.
3.3. Secondary outcomes
Table 4 reports mixed model results for the secondary outcomes.
Table 4.
Mixed model for repeated measures fitted to secondary outcomes with time period and treatment groups.
| Baseline to 2-month follow-up |
Baseline to 6-month follow-up |
|||||
| Secondary Outcomes |
b [95% CI] |
Cohen's d | p-value |
b [95% CI] |
Cohen's d | p-value |
| 1. Hazardous alcohol use (AUDIT total) | ||||||
| Time effect (Control) | −2.49 [−3.77 to −1.20] | 0.41 | <0.001 | −4.02 [−5.57 to −2.49] | 0.66 | <0.001 |
| Time effect (Inroads) | −4.63 [−6.05 to −3.20] | 0.76 | <0.001 | −6.31 [−7.93 to −4.69] | 1.04 | <0.001 |
| Group x Time Interaction | −2.14 [−4.06 to −0.22] | 0.35 | .029 | −2.29 [−4.51 to −0.05] | 0.38 | .045 |
| 2. Binge drinking per month (TLFB) | ||||||
| Time effect (Control) | −2.28 [−3.53 to −1.03] | 0.32 | .001 | −0.75 [−2.07 to 0.56] | 0.11 | .261 |
| Time effect (Inroads) | −3.70 [−5.11 to −2.29] | 0.53 | <0.001 | −4.05 [−5.45 to −2.65] | 0.58 | <0.001 |
| Group x Time Interaction | −1.42 [−3.30 to 0.46] | 0.20 | .138 | −3.30 [−5.21 to −1.38] | 0.47 | .001 |
| 3. Social Anxiety symptoms (SPS+SIAS) | ||||||
| Time effect (Control) | −1.38 [−3.46 to 0.71] | 0.14 | .196 | −2.21 [−4.69 to 0.26] | 0.22 | .080 |
| Time effect (Inroads) | −4.71 [−7.04 to −2.38] | 0.48 | <0.001 | −5.92 [−8.52 to −3.33] | 0.59 | <0.001 |
| Group x Time Interaction | −3.21 [−6.34 to −0.07] | 0.32 | .045 | −3.71 [−7.29 to −0.12] | 0.37 | .043 |
| 4. Depression symptoms (DASS) | ||||||
| Time effect (Control) | −4.82 [−7.35 to −2.29] | 0.50 | <0.001 | −6.82 [−9.43 to −4.21] | 0.71 | <0.001 |
| Time effect (Inroads) | −8.78 [−11.58 to −5.97] | 0.91 | <0.001 | −9.14 [−11.87 to −6.42] | 0.96 | <0.001 |
| Group x Time Interaction | −3.79 [−7.58 to −0.02] | 0.39 | .049 | −2.32 [−6.09 to 1.46] | 0.24 | .229 |
| 5. Functional impairment (SDS) | ||||||
| Time effect (Control) | −5.33 [−7.24 to −3.41] | 0.79 | <0.001 | −4.99 [−7.35 to −3.13] | 0.75 | <0.001 |
| Time effect (Inroads) | −3.46 [−5.60 to −1.31] | 0.52 | .002 | −6.72 [−8.96 to −4.47] | 1.01 | <0.001 |
| Group x Time Interaction | 1.87 [−1.00 to 4.75] | 0.28 | .202 | −1.48 [−4.55 to 1.61] | 0.22 | .348 |
Hazardous alcohol use. AUDIT hazardous alcohol use scores reduced from baseline to 2-month follow up in both groups, with further reductions by 6-month follow up. A significant group by time interaction indicated that participants in the Inroads group reported greater reduction than control in hazardous alcohol use at 2-month (b= −2.14, 95% CI = [−4.06, −0.22], d = 0.35) and 6-month follow up (b= −2.29, 95% CI = [−4.51, −0.05], d = 0.38). Frequency of binge-drinking also reduced in both groups from baseline to 2-month follow-up, however there was evidence of a relapse to baseline levels in the control group by 6-month follow-up. In contrast, participants in the Inroads group reported sustained reductions in binge-drinking, with significant benefits evident compared to control at 6-month follow-up (b= −3.30, 95% CI = [−5.21, −1.38], d = 0.47).
Social anxiety symptoms. Participants in the Inroads group reported a significant reduction in social anxiety symptoms that was sustained at 6-month follow up. Participants in the control group did not significantly improve. A significant group by time interaction indicated benefits of the Inroads program compared to control at 2-month (b= −3.21, 95% CI = [−6.34, −0.07], d = 0.32) and 6-month (b= −3.71, 95% CI = [−7.29, −0.12], d = 0.37) follow-up.
Depression and Functional Impairment. A reduction in depression symptoms was evident at 2-month follow-up for both groups, with weak evidence to suggest greater reductions for participants in the Inroads group (b= −3.79, 95% CI = [−7.58, −0.02], d = 0.39). Continued reductions in depression symptoms were observed, with the control group achieving comparable gains to the Inroads group by 6-month follow-up. Reductions in functional impairment were also observed for both groups, with no evidence of a group by time interaction at either timepoint. However, at 6-month follow-up the Inroads and control groups reported a greater reduction in the number of days lost due to their symptoms (β=0.58 [CI: 0.03 to 1.12], p=.038; d = 0.31) and the number of unproductive days due to their symptoms (β=0.94 [CI: 0.14 to 1.75], p=.022; d = 0.46).
3.4. Clinical relevance
To explore the clinical relevance of the intervention effects, we calculated the proportion of participants in each group who reported symptoms indicative of clinical anxiety or alcohol use disorder at each follow-up (see Table 5). Non-parametric tests indicated that at 2-month follow-up, there were significantly fewer participants in the Inroads group with a probable diagnoses of general anxiety disorder (39.5% vs 68.6%, χ2(1) = 7.52, p < .01) and social anxiety disorder (52.6% vs 74.5%, χ2(1) = 4.59, p = .03). At 6-month follow-up, there were fewer participants in the Inroads group who were exceeding the Australian alcohol guidelines (72.3% vs 48.8%, χ2(1) = 5.13, p = .02). No other group comparisons met statistical significance (p values ranged from 0.05 to 0.27).
Table 5.
Number and proportion of participants screening positively for clinically significant anxiety and alcohol use symptoms at baseline, 2-month and 6-month follow-up.
| Baseline | 2 months | 6 months | ||
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| 1. Probable alcohol use dependence (AUDIT) | ||||
| Control | 35 (57.4%) | 22 (43.1%) | 15 (31.9%) | |
| Inroads | 39 (62.9%) | 10 (26.3%) | 9 (21.4%) | |
| 2. Alcohol use above recommended guidelines (>10 standard drinks/week) | ||||
| Control | 48 (78.7%) | 33 (66.0%) | 34 (72.3%) | |
| Inroads | 43 (69.4%) | 20 (54.1%) | 20 (48.8%) | |
| 3. Probable anxiety disorder (GAD-7) | ||||
| Control | 55 (90.2%) | 35 (68.6%) | 29 (61.7%) | |
| Inroads | 56 (90.3%) | 15 (39.5%) | 18 (42.9%) | |
| 4. Probable social anxiety disorder (SIAS-6) | ||||
| Control | 50 (82.0%) | 38 (74.5%) | 32 (68.1%) | |
| Inroads | 42 (67.7%) | 20 (52.6%) | 20 (47.6%) | |
Note. Probable alcohol dependence was defined according to the recommended cut-off of >20 on the AUDIT19. Alcohol use above recommended guidelines was defined according the Australian National Health and Medical Research Council's guidelines of < 10 standard drinks per week. Probable anxiety disorder spanning generalised anxiety, panic disorder and social anxiety disorder was defined by a score of >8 on the GAD-731. Probable social anxiety diagnosis was defined by a score of >7 on the SIAS-624.
3.5. Treatment fidelity and feedback
Over one-third (39%) of the sample allocated to the Inroads group completed (defined as actively interacting with > 85% of content) all five program modules, 51% completed at least three modules and 77% completed at least one module. Supplementary analyses among the Inroads participants indicated a dose effect, with symptom change from baseline to follow-up on all primary and secondary outcomes increasing with completion of more online modules (see Supplementary Table 6). Forty-four (71%) of the Inroads participants also completed the Module 1 call (n = 42) or text chat (n = 2) session with the study psychologist, and 29 participants (47%) completed both Module 1 and 4 calls. Psychologist support beyond the standard two phone calls and weekly emails was required for four participants due to personal crises, deterioration of symptoms, or safety concerns. Feedback from participants in the Inroads group at 2-month follow-up indicated the majority found the program useful or very/extremely useful (92%), of good/very good quality (97%), and would recommend it to others (92%).
External support for anxiety or alcohol use from a counsellor or psychologist was reported at 2-month follow-up by 16 participants (32%) in the control group, and 10 participants (27%) in the Inroads group. To determine whether external support may have confounded the intervention effects, primary analyses were repeated with this variable included as a covariate; however, no significant effect was observed on change over time for any primary or secondary outcome (all p values > 0.02).
3.6. Adverse events
Deterioration of symptoms were reported at 2-month follow-up by one participant in the Inroads group, and at 6-month follow-up by four participants in the control group. Spontaneous reporting to the study psychologists was only relevant for participants in the Inroads group. Of these, six reported adverse events (relapse or symptom deterioration) during or subsequent to the program. Five of these participants explicitly attributed the adverse event to circumstances external to the program. There were no reports of serious adverse events. See supplementary material for full details.
3.7. Sensitivity analyses
Non-normal distribution of the residuals was observed on the GAD-7, average drinks per day, frequency of binge-drinking, and DASS depression symptoms. For these variables, the best normality transformation was identified, and analyses were conducted using transformed data (see Supplementary Tables 2 and 3). In all cases, there was no substantive difference in results for analyses using transformed data, and thus results from raw data models are reported for ease of interpretation.
Attrition rates were significantly lower in the Inroads group at 2-month follow-up (χ2=7.66, p=.006), but not at 6-month follow-up (χ2=1.33, p=.249). Participants that were lost to follow-up were not significantly different at baseline from those assessed at 2 and/or 6-month assessment on any sociodemographic or outcome variable, with the exception of the truthfulness question. Participants who reported they were answering truthfully were more likely to provide follow-up data (p=.048). To explore the robustness of our results to the impact of data attrition, analyses were repeated with models that incorporated this variable; results were consistent with the principal analyses (see Supplementary Tables 4 and 5).
4. Discussion
This study tested a novel, web-based intervention to address co-occurring anxiety symptoms and hazardous alcohol use among emerging adults. The results demonstrated that the Inroads program was well-received and resulted in significantly greater improvements on some primary and secondary outcomes. For alcohol consumption and severity of alcohol-related consequences, both groups demonstrated significant improvements immediately post-intervention (2-months post-baseline), with significant benefits of the Inroads program compared to control only emerging at the 6-month follow-up for alcohol use. Secondary alcohol outcomes indicated additional benefits for participants in the Inroads group relative to control, with significantly greater reductions in binge-drinking episodes at 6-month follow-up, and consistently lower levels of hazardous drinking (as indicated by the AUDIT) at both 2-month and 6-month assessment. Greater improvements in general anxiety and social anxiety symptoms were also observed in the Inroads group compared to control at 2-months follow-up, but this between-group difference was only sustained at 6-month follow-up in the case of social anxiety. There was also weak evidence of reduced depression symptoms in the Inroads group immediately post-delivery. Overall functional impairment did not differ significantly between groups, although there was evidence that participants in the Inroads group reported fewer unproductive days and days lost due to their symptoms.
We hypothesised that providing participants with strategies to concurrently manage their alcohol and anxiety use would achieve greater reduction in alcohol consumption and related consequences. Contrary to expectations, the difference between the Inroads and control groups on self-reported alcohol-related consequences did not reach statistical significance; however, between-group differences in average drinks per day were observed at the 6-month follow-up. In general, between-group effect sizes were smaller than the moderate size of effect used as a basis for our power calculations, suggesting that a larger sample may have been required to detect significant differences between groups. The smaller than expected between-group effect sizes for alcohol outcomes reflect that on average, trial participants were able to make substantial reductions in their level of alcohol consumption, whether allocated to receive the Inroads program or alcohol information and safe drinking guidelines. To put this into context, at baseline participants in the Inroads and control group drank an average of 3.3 and 3.6 standard drinks per day, respectively, by 2-months post-baseline this had reduced in both groups to 1.5 and 2.1 standard drinks. The finding of significant alcohol use reductions in control groups is not unusual, and a number of systematic reviews have identified that simply asking questions about alcohol use can result in short-term changes in drinking behavior [31]. However, the Inroads program appears to offer benefits over and above providing alcohol assessment and health information in terms of participants’ capacity to sustain these changes in the longer term. At 6-month follow-up, a rebound in average drinks per day was observed in the control group, whereas the Inroads group sustained a mean reduction of 1.5 standard drinks per day. Benefits of the Inroads program over the control intervention were most evident and consistent on indices of problematic alcohol use as measured by the AUDIT, which captures hazardous patterns of drinking linked to alcohol dependence and considerable physical and psychological harms. Further supporting the clinical relevance of the benefits associated with the program, post-hoc analyses indicated that significantly fewer participants in the Inroads group were drinking in excess of Australian recommended guidelines at 6-month follow-up. While benefits of the Inroads program emerged over the longer-term for some alcohol outcomes, the impact on anxiety symptoms was most evident immediately post-delivery. At 2-month follow-up, the proportion of Inroads participants screening positive for an anxiety disorder (encompassing general anxiety, social anxiety and panic disorder) had reduced from 90% to 43%, and from 68% to 48% for social anxiety disorder, rates that were significantly lower than those observed in the control group. While participants in the Inroads group demonstrated a large immediate reduction in general anxiety symptoms; the control group showed a pattern of more gradual anxiety reduction, and by 6-month follow up there was no evidence of between-group differences. The reduction in anxiety symptoms in the control group over the longer-term may correspond to participants’ alcohol reduction: as noted, anxiety and alcohol symptoms tend to fuel each other in a self-perpetuating cycle. Prolonged alcohol use is associated with biological and neuroadaptations that increase anxiety symptoms, particularly during periods of sobriety or withdrawal, and hence reductions in alcohol consumption are likely to alleviate anxious arousal [32]. In contrast, the between-group differences in social anxiety symptoms were sustained over the longer term, with Inroads participants reporting greater symptom reductions at both the 2-month and 6-month assessment. This finding aligns with previous trial results for adults with co-occurring social anxiety and alcohol use disorders, which showed significant social anxiety symptom reduction when anxiety symptoms were addressed in an integrated treatment package, compared to when alcohol use reduction was the sole focus of treatment [5]. The divergent findings for different types of anxiety presentations holds important implications for management; while targeting alcohol use may be sufficient to ameliorate general levels of arousal and stress, other presentations such as social anxiety are likely to require anxiety management strategies to explicitly target the underlying cognitions and avoidance behaviors [28].
The immediate and sustained reductions in social anxiety symptoms for participants in the Inroads group provide a potential explanation for these participants’ improved capacity to maintain changes in the drinking behavior at 6-month follow-up compared to control. While a rebound in average number of alcoholic drinks per day and frequency of binge-drinking was observed in the control group, participants in the Inroads group maintained reductions over the longer term. The improved capacity to sustain changes to alcohol use behavior beyond the initial 2-month period may be attributable, at least in part, to the development of effective anxiety management strategies, and thus a decreased reliance on alcohol as a means of coping with anxiety symptoms. Control participants, on the other hand, may have found it difficult to sustain alcohol reductions beyond the initial months (when motivation is at its highest), as they were confronted by social settings and other situations that triggered anxiety and coping-motivated drinking. This hypothesis is suggested by the self-medication model of anxiety and alcohol use [4] and will be tested in subsequent analyses of the mediators and mechanisms of change underlying the current intervention effects.
The current findings are interpreted within the context of several limitations. Participant retention is a challenge for all longitudinal research. Data attrition in the current study was at the lower end of rates reported in a meta-review of web-based alcohol interventions [33], with 72% of participants providing data at 2-month and 6-month follow up, and 78% providing data for at least one follow-up assessment. At 2-month follow-up, higher attrition was observed in the Inroads group compared to control, which may relate to digital fatigue as Inroads participation involved more frequent interaction with the program website. The potential impact of data attrition was examined in sensitivity analyses and all analyses accounted for missing responses using maximum likelihood estimation. Less than half of the participants allocated to the Inroads program completed all five program modules, reflecting the high rates of treatment non-completion that are also observed in the face-to-face drug and alcohol treatment literature [34]. The web-based format of the Inroads program circumvents many of the common barriers to help-seeking, reaching youth who may be unwilling to attend face-to-face treatment. This is a key strength, but it will be important for future research to explore the possibility that web-based recruitment and delivery attracts samples with differing characteristics [35], such as lower levels of motivation or commitment to treatment, that may in turn impact upon program completion rates.
Secondly, the control condition was not matched to the Inroads program in terms of length of intervention content or access to therapist support. Given the known benefits of comprehensive alcohol assessment and information provision [31,36], we considered this study design an appropriate first step to ascertain the incremental benefit of providing integrated intervention for both anxiety and alcohol use. However, from this design we cannot draw firm conclusions about which components of the Inroads program (i.e., module content, psychologist support sessions, or participant implementation of cognitive behavioral strategies) were responsible for the observed symptom reductions post program delivery. Our dose-response analyses suggest that engagement with the module content was important for achieving change, with greater symptom reductions on all outcomes observed as number of completed modules increased. To build upon the current findings, forthcoming secondary analyses will examine the specific therapeutic components that mediate the intervention effects observed in the current study.
Finally, the trial design necessitated a number of exclusion criteria. Participants were excluded if they were engaging in daily use of cannabis, benzodiazepines, or weekly use of psychostimulants. There is a high degree of co-occurrence between alcohol and other substance use, indeed in the current sample, 22% were reporting daily or monthly cannabis use at baseline. It is therefore important for future research to examine whether the skills gained through the Inroads program may generalize to other substances, and to explore adaptation of integrated programs to assist youth managing anxiety symptoms in the context of problematic use across multiple substances. Participants were also excluded if they were experiencing active suicidal ideation, symptoms of psychosis, or at risk of complicated alcohol withdrawal. These exclusion criteria were implemented due to safety concerns and reflect a limitation of web-based interventions more generally: they are unlikely to provide sufficiently intensive and individualized care to accommodate more severe and complex presentations. Other limitations of web-based interventions include potential privacy and data security risks, and restrictions on access for people with some disabilities or low literacy levels.
Despite these limitations, web-based delivery of mental health interventions has significant potential, given this format aligns with youth preferences, reduces the perceived stigma associated with treatment-seeking [15], and is readily scalable. Emerging adults commonly report using alcohol to reduce or cope with anxiety, and once this maladaptive pattern of coping is established, anxiety and hazardous alcohol use tend to fuel each other in a vicious cycle that increases impairment and interferes with recovery. The results of this trial provide initial evidence to support the benefits of an integrated, web-based intervention for anxiety and alcohol use, which demonstrated reductions in anxiety symptoms, alcohol consumption and hazardous alcohol use relative to control. By combining engaging, interactive web-based content with low intensity psychologist support via phone or email, the Inroads program can be disseminated sustainably and widely, including to youth living in areas where there is limited or no access to mental health services. Importantly, the Inroads program provides the opportunity to intervene during a high-risk developmental stage when symptoms are emerging, to promote adaptive coping strategies and prevent anxiety and alcohol use from becoming deeply intertwined disorders that exacerbate one another in a self-perpetuating cycle.
Declaration of Competing Interest
None
Acknowledgments
Data sharing statement
The data presented in this study are not publicly available due to ethics approval requirements.
Acknowledgment
The authors would like to acknowledge the contribution of Nurul Praharso who assisted with delivery of psychologist support sessions, and Rachel Visontay, Julia Boyle and Damien Bellemore who provide research assistance support. We are extremely grateful to all the participants who took part in this study.
Funding
The research was supported by funding from an Australian Rotary Health mental health research grant and salary support from the National Health and Medical Research Council (GNT1132853; Centre of Research Excellence in the Prevention and Early Intervention in Mental Illness and Substance Use).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.101048.
Appendix. Supplementary materials
References
- 1.Kessler R.C., Aguilar-Gaxiola S., Alonso J. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith J.P., Randall C.L. Anxiety and alcohol use disorders: comorbidity and treatment considerations. Alcohol Res. 2012;34(4):414–431. [PMC free article] [PubMed] [Google Scholar]
- 3.Smith J.P., Book S.W. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment. Addict Behav. 2010;35(1):42–45. doi: 10.1016/j.addbeh.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khantzian E.J. The self-medication hypothesis revisited: the dually diagnosed patient. Prim Psychiatry. 2003;10(9):47–54. [Google Scholar]
- 5.Stapinski L., Sannibale C., Subotic S. Aust N Z J Psychiatry. 2021. Randomised controlled trial of integrated CBT and motivational interviewing for comorbid social anxiety and alcohol use disorders. ;55(2):207–220. [DOI] [PubMed] [Google Scholar]
- 6.Kushner M.G., Maurer E.W., Thuras P. Hybrid cognitive behavioral therapy versus relaxation training for co-occurring anxiety and alcohol disorder: a randomized clinical trial. J Consult Clin Psychol. 2013;81(3):429. doi: 10.1037/a0031301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnett J.J. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 8.Elkins I.J., King S.M., McGue M., Iacono W.G. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: prospective links from adolescence to young adulthood. J Abnorm Psychol. 2006;115(1):26–39. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- 9.Australian bureau of statistics A. National survey of mental health and wellbeing: summary of results. (Catalogue No 43260)2007.
- 10.O'Brien H., Callinan S., Livingston M., Doyle J.S., Dietze P.M. Population patterns in Alcohol Use Disorders Identification Test (AUDIT) scores in the Australian population. Aust N Z J Public Health. 2020;44(6):462–467. doi: 10.1111/1753-6405.13043. 2007–2016. [DOI] [PubMed] [Google Scholar]
- 11.Stapinski L.A., Edwards A.C., Hickman M. Drinking to cope: a latent class analysis of coping motives for alcohol use in a large cohort of adolescents. Prev Sci. 2016;17(5):584–594. doi: 10.1007/s11121-016-0652-5. [DOI] [PubMed] [Google Scholar]
- 12.Birrell L., Newton N.C., Teesson M., Tonks Z., Slade T. Anxiety disorders and first alcohol use in the general population. Findings from a nationally representative sample. J Anxiety Disord. 2015;31:108–113. doi: 10.1016/j.janxdis.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Conway K.P., Swendsen J., Husky M.M., He J.P., Merikangas K.R. Association of lifetime mental disorders and subsequent alcohol and illicit drug use: results from the national comorbidity survey–adolescent supplement. J Am Acad Child Adolesc Psychiatry. 2016;55(4):280–288. doi: 10.1016/j.jaac.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 14.Hall W.D., Patton G., Stockings E. Why young people's substance use matters for global health. Lancet Psychiatry. 2016;3(3):265–279. doi: 10.1016/S2215-0366(16)00013-4. [DOI] [PubMed] [Google Scholar]
- 15.Boydell K., Hodgins M., Pignatiello A., Teshima J., Edwards H., Willis D. Using technology to deliver mental health services to children and youth: a scoping review. J Can Acad Child Adolesc Psychiatry. 2014;23(2):87–99. [PMC free article] [PubMed] [Google Scholar]
- 16.Deady M., Mills K.L., Teesson M., Kay-Lambkin F. An online intervention for Co-occurring depression and problematic alcohol use in young people: primary outcomes from a randomized controlled trial. J Med Internet Res. 2016;18(3):e71. doi: 10.2196/jmir.5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions — A systematic review. Internet Interv. 2014;1(4):205–215. [Google Scholar]
- 18.L.A. Stapinski, K. Prior, N.C. Newton, et al. Protocol for the inroads study: a randomized controlled trial of an internet-delivered, cognitive behavioral therapy–based early intervention to reduce anxiety and hazardous alcohol use among young people. 2019; 8(4): e12370. [DOI] [PMC free article] [PubMed]
- 19.Moher D., Hopewell S., Schulz K.F. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63(8):e1–e37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Babor T., Higgins-Biddle J., Saunders J., Monteiro M. 2nd ed. World Health Organization; Geneva: 2001. The alcohol use disorders identification test, guidelines for use in primary care. [Google Scholar]
- 21.Byrd-Bredbenner C., Eck K., Quick V. Psychometric properties of the generalized anxiety disorder-7 and generalized anxiety disorder-mini in United States university students. Front Psychol. 2020;11:2512. doi: 10.3389/fpsyg.2020.550533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connor K.M., Kobak K.A., Churchill L.E., Katzelnick D., Davidson J.R. Mini-SPIN: a brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14(2):137–140. doi: 10.1002/da.1055. [DOI] [PubMed] [Google Scholar]
- 23.Rueger S.Y., Trela C.J., Palmeri M., King A.C. Self-administered web-based timeline followback procedure for drinking and smoking behaviors in young adults. J Stud Alcohol Drugs. 2012;73(5):829–833. doi: 10.15288/jsad.2012.73.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kahler C.W., Hustad J., Barnett N.P., Strong D.R., Borsari B. Validation of the 30-day version of the brief young adult alcohol consequences questionnaire for use in longitudinal studies. J Stud Alcohol Drugs. 2008;69(4):611–615. doi: 10.15288/jsad.2008.69.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peters L., Sunderland M., Andrews G., Rapee R.M., Mattick R.P. Development of a short form Social Interaction Anxiety (SIAS) and Social Phobia Scale (SPS) using nonparametric item response theory: the SIAS-6 and the SPS-6. Psychol Assess. 2012;24(1):66–76. doi: 10.1037/a0024544. [DOI] [PubMed] [Google Scholar]
- 26.Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 27.Sheehan D. Charles Scribner and Sons; New York: 1983. The sheehan disability scales. the anxiety disease and how to overcome it. [Google Scholar]
- 28.Stapinski L.A., Rapee R.M., Sannibale C., Teesson M., Haber P., Baillie A.J. The clinical and theoretical basis for integrated cognitive behavioral treatment of comorbid social anxiety and alcohol use disorders. Cogn Behav Pract. 2015;22(4):504–521. [Google Scholar]
- 29.L.A. Stapinski, K. Prior, E. Kelly, et al. 2021 Co-design of the inroads program: an internet-delivered cognitive-behavioral intervention for young adults with co-occurring anxiety and alcohol use problems. Manuscript in preparation: *Equally credited authors.
- 30.Wiederman M.W. The truth must be in here somewhere: examining the gender discrepancy in self-reported lifetime number of sex partners. J Sex Res. 1997;34(4):375–386. [Google Scholar]
- 31.Miles L.M., Rodrigues A.M., Sniehotta F.F., French D.P. Asking questions changes health-related behavior: an updated systematic review and meta-analysis. J Clin Epidemiol. 2020;123:59–68. doi: 10.1016/j.jclinepi.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anker J.J., Kushner M.G. Co-occurring alcohol use disorder and anxiety: bridging psychiatric, psychological, and neurobiological perspectives. Alcohol Res. 2019;40(1) doi: 10.35946/arcr.v40.1.03. arcr.v40.1.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hadjistavropoulos H.D., Mehta S., Wilhelms A., Keough M.T., Sundström C. A systematic review of internet-delivered cognitive behavior therapy for alcohol misuse: study characteristics, program content and outcomes. Cogn Behav Ther. 2020;49(4):327–346. doi: 10.1080/16506073.2019.1663258. [DOI] [PubMed] [Google Scholar]
- 34.Woodward A.M., Raskin I.E., Blacklow B. A profile of the substance abuse treatment industry: organization, costs, and treatment completion. Subst Use Misuse. 2008;43(5):647–679. doi: 10.1080/10826080601096640. [DOI] [PubMed] [Google Scholar]
- 35.Moseson H., Kumar S., Juusola J.L. Comparison of study samples recruited with virtual versus traditional recruitment methods. Contemp Clin Trials Commun. 2020;19 doi: 10.1016/j.conctc.2020.100590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCambridge J., Kypri K. Can simply answering research questions change behavior? Systematic review and meta analyses of brief alcohol intervention trials. PLoS ONE. 2011;6(10):e23748. doi: 10.1371/journal.pone.0023748. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.