Abstract
Objective:
In selected children with drug-resistant epilepsy, epilepsy surgery is the most effective treatment option, but unfortunately remains highly underutilized. One of the critical obstacles to pursuing surgical therapy is parents/caregivers’ decision against surgery or to delay the surgery until no other treatment option exists. Understanding caregiver decision-making around epilepsy surgery can improve patient/caregiver experience and satisfaction while facilitating appropriate decision-making that optimizes clinical outcomes. The current review systematically explores the existing evidence on caregiver experience and the decision-making process toward epilepsy surgery.
Methods:
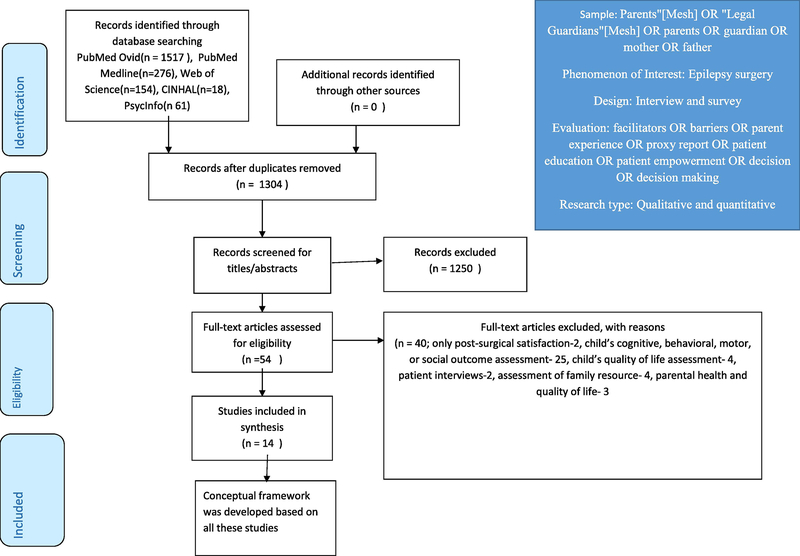
The study was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic literature review. Databases (PubMed Ovid, PubMed Medline, Web of Science, CINHAL, PsycInfo) were systematically searched in February 2021 using a defined search strategy and inclusion/exclusion criteria. Total 1304 articles were screened for titles and abstracts, and 54 full-text articles were retrieved for further assessment. We included 14 articles with critical quality assessment using two different tools for qualitative and questionnaire-based studies. A qualitative content analysis was performed to characterize caregiver experience, perception, and decision-making toward favorable or unfavorable opinions of epilepsy surgery.
Results:
Four concepts generated from the analysis may act as enablers or barriers to decisionmaking around epilepsy surgery: 1. Access to knowledge and information, 2. Communication and coordination issues, 3. Caregiver’s emotional state, and 4. Socioeconomic effects. Subsequently, we provided a narrative synthesis of practice recommendations and a conceptual framework to adopt multi-pronged interventions to overcome identified diverse barriers to effective caregiver decision-making.
Conclusion:
Multiple influences impact how caregivers decide about epilepsy surgery for their children, with no single factor identified as the primary driver for or against surgery. However, limited research has explored these influences. Future studies should focus on quantitatively examining factors to identify significant variables most likely to influence caregiver decision-making, ultimately overcoming barriers that limit utilization of epilepsy surgery as a treatment tool.
Keywords: Parent, guardian, choice, selection, option, recommendation
Epilepsy is the most common chronic neurologic disorder of childhood.1 Approximately one-third of children and youth with epilepsy have drug-resistant epilepsy (DRE), associated with neurocognitive and psychological decline, poor quality of life, increased risk of premature death, and higher societal economic burden.2 In selected children with DRE, epilepsy surgery has proven to be the most effective treatment option.3,4 Despite high-quality evidence, epilepsy surgery is one of the most underutilized evidence-based treatment interventions in modern medicine.5
Underutilization of epilepsy surgery has been comprehensively analyzed, recognizing a wide range of barriers to surgery, including patients’ and physicians’ perceptions of epilepsy surgery.6,7 However, decision-making for children can be more complex as parents and caregivers acting as proxy decision-makers and health care navigators for their children.8 Thus, one of the most critical obstacles in pediatric epilepsy surgery may be parents’/caregivers decisions not to pursue presurgical evaluation or surgical therapy for their children, in part related to fear and misconceptions about surgical risks and their unrealistic expectations regarding the efficacy of additional nonsurgical treatments.9–14 Caregiver experience and decision-making are based on many variables, including existing knowledge and perceptions about epilepsy surgery and interactions with healthcare providers (HCPs), the healthcare system, other family members, and the community. Diverse experiences and encounters may enable or act as barriers to the decision-making process toward the pursuit of epilepsy surgery. Caregivers balance the risks and benefits of surgery within the context of their emotional responses to the disease and treatment options while considering the future needs of their children (i.e., medical, emotional, and cognitive). Investigation of other pediatric conditions requiring surgical therapy (e.g., cleft lip and palate) showed that parental treatment choice is crucial in the decision to undergo surgery. 15 For pediatric epilepsy surgery, approximately 75% of the treatment choice is influenced by parents without a substantial contribution from their children.16 Thus, to increase the utilization of epilepsy surgery in children, it is vital to understand how caregivers perceive surgical treatment, focusing on the variables that most influence the decision-making process.
Beyond improved utilization, studying the caregiver experience and decision-making process will guide HCPs in counseling guardians appropriately around surgical treatment. Understanding caregiver perspectives allows more effective communication about surgical therapy between caregivers and HCPs. No previous systematic reviews have investigated caregiver perceptions and decision-making toward epilepsy surgery. Herein, we aim to synthesize the following research questions from primary resources (qualitative and quantitative studies): What are caregiver perceptions and experiences regarding epilepsy surgery? How do caregivers make decisions regarding epilepsy surgery for their children? What are potential barriers and facilitators for caregiver decision-making toward the pursuit of epilepsy surgery?
Finally, we conceptualize an integrative framework (summarizing the primary studies’ findings) that would help develop interventions to improve uptake of epilepsy surgery.
2. MATERIALS AND METHODS
2. 1. Search strategy
This review was undertaken in line with PRISMA standards.17 The inclusion and exclusion criteria can be found in Table 1. Studies were not excluded with date range limits. The search comprised three main stages. First, potentially eligible studies known to the authors were identified. References of these studies were hand-searched to identify other relevant articles. We utilized these articles to guide us in constructing the search and concept terms. Finally, a systematic search of Psych Info, PubMed (Medline and Ovid), Web of Science, and CINAHL was performed in February 2021 and conducted based on the three main concept terms identified in the stages above: 1. Epilepsy surgery OR (“Epilepsy/surgery”[Mesh]) OR ((“Epilepsy”[Mesh]) AND “Surgical Procedures, Operative”[Mesh]) 2. “Parents”[Mesh] OR “Legal Guardians”[Mesh] OR parents OR guardian OR mother OR father, and 3. (facilitators) OR (barriers)) OR (parent experience) OR (proxy report) OR (patient education) OR (patient empowerment)) OR (decision making). Hand searches were performed on references in these articles to identify any further relevant resources.
Table 1.
Inclusion and exclusion criteria.
| Factor | Inclusion criteria | Exclusion criteria |
|---|---|---|
|
| ||
| Purpose | Focusing on caregivers (parents/guardians) attitudes, opinions, views, behavior, and perceptions of epilepsy surgery; any study that provides insight into caregivers’ perceptions or behaviors toward epilepsy surgery. Studies must focus primarily on epilepsy surgery. Epilepsy surgery is defined as both potentially curative and resective surgeries, but exclude neuromodulation procedures such as vagal nerve stimulation | (1) Studies that were not fully published peer-reviewed studies (conference proceeding or gray literature) (2) Review articles or editorials (3) Studies that were not published in the English language (4) Duplicate publications (5) Studies assessing children’s perspectives about epilepsy surgery only (6) Studies assessing healthcare professionals’ perspectives about epilepsy surgery only (7) Studies that included patients with epilepsy but results related to epilepsy surgery could not be extracted separately |
| Sample | Caregivers of children and adolescents with epilepsy (with or without drug-resistant epilepsy). No restrictions on nationality | (8) Studies only assessing caregiver satisfaction after surgery without any insight about pre-surgery decision-making |
| Data collection | Primary research studies that collect data from >1 caregiver Qualitative or quantitative data collection methods, i.e., survey, questionnaire, interview, observations | |
| Data analysis | Qualitative or quantitative methods | |
| Journal article | English and peer-reviewed | |
2.2. Study selection
Two reviewers (DS and MH) independently reviewed all the titles and abstracts to determine the articles’ relevance to answering the research questions. The papers were labeled ‘included,’ ‘excluded,’ or ‘uncertain’ based on the inclusion and exclusion criteria. Both reviewers had to label ‘excluded’ to screen out articles at this stage. Subsequently, both reviewers read full texts of all ‘included’ and ‘uncertain’ articles to determine eligibility. Reviewers reached a consensus for study inclusion at this time.
2.3. Data Collection
The following data were extracted from each study: author(s), year of publication, sample size and characteristics, methodological considerations, and findings. Inconsistencies in extracted data were resolved through consensus.
2.4. Data analysis
The analysis comprised four main stages:
The study quality appraisals were conducted using two different tools.18,19 For qualitative studies, Consolidated criteria for reporting qualitative research( COREQ), a multi-item checklist, was used to inform personal characteristics of the interviewer, relationship with participants, participant selection, data collection, data analysis, and reporting. On the other hand, for questionnaire-based studies(survey), a 9-item specific critical appraisal tool was used to report research question and study design; validity and reliability; format; piloting; sampling; distribution, administration, and response; coding and analysis; results; and conclusions and discussion.20
We adopted an integrated design to mitigate the methodological differences between qualitative and quantitative studies as findings from these studies confirmed and extended each other by answering our research questions and addressing the same aspects of the targeted phenomenon.21,22 As questionnaire-based studies were highly heterogeneous, we couldn’t perform meta-analyses of these studies. So, we converted quantitative findings to qualitative data to combine with results from the primary qualitative studies.23 We undertook a content analytic approach with an open coding process consisting of reading through the data several times and grouping caregiver experience, perception, and decision-making to either favorable or unfavorable toward epilepsy surgery.24 A formal metasynthetic approach was taken with reading and rereading each study, line-by-line coding, grouping the codes by categorizing them into a hierarchical tree structure, and finally generating analytical themes.25 This was a cyclical process, as the authors amended the categories until consensus.
The authors next performed a narrative synthesis of practice recommendations from the primary studies. As in the previous stage, this was an iterative process, and a conceptual framework was developed and refined until consensus was reached between the authors.
Lastly, a write-up of the review was performed.
3. RESULTS
3.1. Literature review
The full text of 54 articles was assessed for eligibility, and 14 were included in the review (Figure 1 and Table 2). The 40 excluded articles had a primary assessment of the following parameters: satisfaction after surgery; child’s cognitive, behavioral, motor, or social outcome; child’s quality of life; patient status; family resource; parental health and quality of life.
Figure 1.
Flow of identification and selection process.
Table 2.
Studies included in this review.
| Author (year) | Method | Sample | Settings |
|---|---|---|---|
|
| |||
| Sassower (2001) | Telephone questionnaire and chart review | Twenty-seven parents of sixteen children with intractable epilepsy (prior to surgery) were telephone interviewed following a structured format of 24 questions, posed to both parents during single, 20-minute sessions | All Children’s Hospital, in St. Petersburg Florida |
| Swarztrauber (2003) | Qualitative analysis | Focus group interview (lasted 90 minutes) of 4 parents of adolescents (12–18 years old with ≥2 seizures/year) and with intractable epilepsy clinically relevant medication side effects or functional decline in the past year | UCLA, Los Angeles, California |
| Erba (2013) | Questionnaire-based study think and what the doctors can do | 138 parents (≥21 years old, a minimum of 5th grade education/reading skills, and to be free of any obvious or suspected cognitive impairment) of pediatric patients with epilepsy to understand acceptance of epilepsy surgery among parents | 6 pediatric epilepsy centers located in Lombardy, Northern Italy |
| Engelhart (2013) | Questionnaire-based study | 111 participants (55 only parents and 53 parents and children) evaluate their decision to proceed with epilepsy surgery (if they would opt again for surgery), at least one year after the operation | Dutch Collaborative Epilepsy Surgery Program |
| Baca(2015) | Qualitative (thematic) analysis | 37 interviews of parents of children who previously had resective epilepsy surgery | University of California Los Angeles |
| Heath (2016) | Qualitative (inductive thematic) analysis approach. | Individual semi-structured interviews (face-to-face, telephone, Skype) were conducted with 9 parents (purposive sampling) of children who had undergone pediatric epilepsy | Surgeries were done UK Specialist Children’s Hospital which hosts one of four national centers in England, commissioned to provide a Children’s Epilepsy Surgery Service (CESS) |
| Pieters (2016) | Qualitative (thematic) analysis | Individual semi-structured interviews with 37 parents of children who had previously undergone epilepsy surgery | The study and surgeries (2006–2011) were performed at UCLA |
| Ozanne (2016) | A qualitative content analysis | Seven to eighteen years after hemispherotomy, parents of 21 operated children were interviewed about the family life situation, expectations before surgery, and support and information before and after surgery | Population-based study from Sweden; parents of all patients who had undergone hemispherotomy in Sweden from 1995–2007 were invited to participate |
| Shen (2018) | An online questionnaire | 58 caregivers of children with pediatric epilepsy surgery | Surgeries were carried out in 6 countries with the majority performed in the United States at 30 different epilepsy centers. Some caregivers were approached and recruited during their children’s clinic visits at Lucile Packard Children’s Hospital and asked to go online to complete the survey |
| Ozanne (2018) | Qualitative analysis (combination of inductive and deductive qualitative content analysis) | Semi structured telephone interviews of the parents of 12 children to understand family situation before and after callosotomy | The Swedish National Epilepsy Surgery Register |
| Bach (2020) | Questionnaire-based study | 42 parents of children with epilepsy (irrespective of undergoing epilepsy surgery) were evaluated with the questionnaire consisting of four sections with 31 questions, including open-ended and closed-ended questions, and Likert scales to understand decision-making and experiences in epilepsy surgery | 13 epilepsy associations and patient organizations from Germany, Switzerland, and Austria, and three clinics from Berlin distributed the questionnaires and information sheets via their websites, magazines, mailing lists and/or newsletters, by letter, or in person |
| O’Brien (2020) | Qualitative analysis (constant comparison approach) | Semi-structured interviews were conducted with 9 parents and their children aged between 7 and 17 years old, who had undergone epilepsy surgery within the previous six months to three years, to understand family experiences throughout the surgery journey | Individuals were recruited from two hospitals in a joint children’s epilepsy surgery service (CESS), UK |
| Nguyen (2020) | Questionnaire-based study | 46 caregivers impression of epilepsy surgery in patients with tuberous sclerosis complex | Participants were recruited both online (Tuberous Sclerosis Alliance’s website, newsletter, and Facebook page) and in-person at Stanford Children’s Health |
| Sylvén (2020) | Thematic analysis | 107 Parents of the children and young people who underwent surgery completed surveys on two occasions, one just before their child underwent epilepsy surgery and another two years after the surgical intervention | Parents of children who children and youth (≤19 years) who underwent epilepsy surgery from 1995 to 2014 at Sahlgrenska University Hospital in Gothenburg, Sweden |
3.2. Study characteristics
Studies were published between 2001 and 2020. Overall, seven studies collected quantitative data and seven qualitative data. All qualitative studies collected retrospective parental perspectives with children who had previously undergone epilepsy surgery. Questionnaire-based studies involved heterogeneous samples, including parents of children with well-controlled epilepsy and parents who had refused surgery as a treatment option. All included studies fulfilled most quality appraisal conditions, and all data were used equally in the analysis. (Table 3A and 3B)
Table 3A.
Comprehensiveness of Reporting in Included Studies.
| Item | Studies Reporting Each Item |
|---|---|
|
| |
| Personal characteristics | |
| ○ Interviewer/facilitator identified | 1,3,4,6,7 |
| ○ Occupation of the interview of facilitator | 1,2,3,4,6, 7 |
| ○ Experience or training in qualitative research | |
| Relationship with participants | |
| ○ Relationship established before study commencement | 1,2,3,4,5 |
| Participant selection | |
| ○ Selection strategy (e.g., snowball, purposive, convenience, comprehensive) | 1,2,3,4,5,6,7 |
| ○ Method of approach or recruitment | 1,2,3,4,5 |
| ○ Sample size | 1,2,3,4,5,6,7 |
| ○ Number and/or reasons for nonparticipation | 4,5,6,7 |
| ○ Venue of data collection | 4 |
| ○ Presence of nonparticipants (e.g., clinical staff) | 4 |
| ○ Description of the sample | 1,3,4,5,6, 7 |
| Data collection | |
| ○ Questions, prompts or topic guide | 1,2,3,4,5,6,7 |
| ○ Repeat interviews/observations | |
| ○ Audio/visual recording | 1,2,3,4,5,6,7 |
| ○ Field notes | 2,4 |
| ○ Duration of data collection (interview or focus group) | 1,2,3,4 |
| ○ Translation and interpretation | 1,3 |
| ○ Protocol for data preparation and transcription | 1,2,3,4, 5 |
| ○ Data (or theoretical) saturation | 1,3,4 |
| Data analysis | |
| ○ Researcher/expert triangulation (multiple researchers involved in coding and analysis) | 1,2,3,5,6,7 |
| ○ Translation (specifies language in which analysis was done) | 1,3 |
| ○ Derivation of themes or findings (e.g., inductive, constant comparison) | 1,2,3,4,6,7 |
| ○ Use of software (e.g., NVivo, HyperRESEARCH, Atlas.ti) | 4 |
| ○ Member checking (participant feedback on findings) | |
| Reporting | |
| ○ Participant quotations or raw data provided (picture, diary entries) | 1,2,3,4,5,6,7 |
| ○ Range and depth of insight into participant perspectives (thick description provided) | 1,2,3,4,5,6,7 |
Baca (2015)
- Heath (2016)
- Pieters (2016)
- O’Brien (2020)
- Swartztrauber (2003)
- Ozanne (2016)
- Ozanne(2018).
Table 3B.
Critical Appraisal for questionnaire based studies.
| Study | Research question and study design | Validity and reliability | Format | Piloting | Sampling | Distribution, administration and response | Coding and analysis | Results | Conclusions and discussion |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Sassower (2001) | * | * | *** | * | * | *** | ** | ** | ** |
| Erba (2013) | *** | ** | *** | *** | ** | ** | *** | *** | *** |
| Engelhart (2013) | ** | * | ? | * | *** | * | ** | *** | *** |
| Shen (2018) | * | * | *** | * | * | * | ** | ** | *** |
| Sylv’en (2020) | * | * | *** | * | *** | *** | ** | ** | *** |
| Nguyen (2020) | ** | * | *** | ** | * | ** | ** | ** | *** |
| Bach (2020) | * | * | ** | * | * | * | ** | ** | *** |
- Strong
- Moderate
- Weak
- Unable to determine.
Research question and study design: Was a questionnaire the most appropriate method?
Validity and reliability: Have claims for validity been made, and are they justified? (Is there evidence that the instrument measures what it sets out to measure?) Have claims for reliability been made, and are they justified? (Is there evidence that the questionnaire provides stable responses over time and between researchers?)
Format: Are example questions provided? Did the questions make sense, and could the participants in the sample understand them? Were any questions ambiguous or overly complicated?
Piloting: Are details given about the piloting undertaken? Was the questionnaire adequately piloted in terms of the method and means of administration, on people who were representative of the study population?
Sampling: Was the sampling frame for the definitive study sufficiently large and representative?
Distribution, administration and response: Was the method of distribution and administration reported? Were the response rates reported, including details of participants who were unsuitable for the research or refused to take part? Have any potential response biases been discussed?
Coding and analysis: What sort of analysis was carried out and was this appropriate?
Results: Were all relevant data reported? Are quantitative results definitive (significant), and are relevant non-significant results also reported? Have qualitative results been adequately interpreted (e.g. using an explicit theoretical framework), and have any quotes been properly justified and contextualized?
Conclusions and discussion: Have the researchers drawn an appropriate link between the data and their conclusions? Have the findings been placed within the wider body of knowledge in the field (e.g. via a comprehensive literature review), and are any recommendations justified?
From the content analysis (qualitative metasynthesis), four key concepts (1. Access to knowledge and information, 2. Communication and coordination issues, 3. Caregiver’s emotional state, and 4. Socioeconomic effects) were identified to explain caregiver experience and decision-making for deferring or accepting epilepsy surgery.
3.3. Barriers to caregiver decision making/Factors for deferring epilepsy surgery
3.3.1. Access to knowledge and information
Many parents were unsatisfied with the information about epilepsy surgery provided in primary and secondary care settings.26 They struggled to navigate the healthcare system and learn about epilepsy and its various treatment options, including epilepsy surgery. 27,28 Many caregivers required extensive searches (i.e. websites) to find necessary information. Some were skeptical about the efficacy of surgery given negative experiences from previous treatment failure with AEDs.28,29 Surgery was primarily considered a last resort treatment option that would only be considered following the exhaustion of all other options27,29,30 In contrast, after referral to a tertiary center experienced in epilepsy surgery, parents received a large amount of information about surgical therapy, but some felt a lack of individualized options prevented them move forward with the pursuit of epilepsy surgery.27, 31
3.3.2. Communication and coordination issues
As with the knowledge gap, significant communication challenges existed between caregivers and HCPs. During initial encounters with HCPs after diagnosis of epilepsy, some caregivers developed a negative perception about surgery as HCPs in the primary and secondary settings portrayed reservations and insecurities regarding epilepsy surgery.32Additionally, caregivers felt more negativity toward surgery if it was not discussed as a potential treatment option from the outset. 29 The presurgical referral process was perceived by caregivers as slow and arduous. 27,30,31 Some needed to initiate contact with the epilepsy center themselves and struggled with finding the ‘right doctor.26,28,30 Option of epilepsy surgery was not given to some caregivers, leading to their inability to participate in an informed discussion.29 During post-surgical care, caregivers felt ill-informed about the difficulty of the rehabilitation process and the absence of psychosocial counseling.33 Some caregivers were frustrated about the poor quality of life associated with intellectual impairment, autism, weakness, or muscle spasms after surgery despite the child being seizure-free.33
3.3.3. Caregiver’s emotional state
At the beginning of the epilepsy surgery discussion, caregivers felt frustrated as pharmacotherapy did not improve seizure frequency. They also had difficulties finding physicians that they could build a trusting relationship.27,30 Caregivers felt overwhelmed with the responsibility of deciding on epilepsy surgery for their children and wanted their children to be old enough to participate in the decision, fearing they couldn’t communicate adequately to understand their children’s wish.28,30,32 Caregivers were willing to tolerate a great deal of dysfunction before considering surgery.28 They continued to hope unrealistically that their child might “outgrow” their seizures.30 Despite experiencing urgency and feeling vulnerable with continuing seizures and other comorbidities, caregivers felt ambiguous about surgery due to uncertainty about the outcome. 27,32 They worried about the surgical procedure and the potential for failure to achieve seizure freedom. 9,34 They were also concerned about negative changes in their child’s character or behavior (62%) and decline in their child’s independence and memory or concentration abilities (60% and 52%, respectively) after surgery.16 Half (50%) were afraid that their child would die from surgical complications.16 Throughout the process, caregivers felt lonely and without direction, particularly outside of clinical appointments.27,35
3.3.4. Socioeconomic effects
Caregiver decision-making about epilepsy surgery may also be dependent on the location of service. Erba et al. showed that caregivers of children followed in the three centers outside Milan had a sevenfold higher probability of rejecting epilepsy surgery as a possible treatment for their child’s epilepsy.36 Although the cause of this remarkable discrepancy is unknown, caregivers identified poor social support (community and healthcare system) as one of the barriers to epilepsy surgery. Caregivers felt directionless and wasted valuable time navigating the healthcare and insurance systems.27,30 Family conflicts- if there is no consensus about epilepsy surgery among caregivers- acted as an additional barrier to decision making.29 Parents, in particular, felt additional social pressure to manage the grief and concern of the child’s grandparents.32
3.4. Facilitators to caregiver decision making/factors for choosing epilepsy surgery
3.4.1. Access to knowledge and information
Some caregivers with prior knowledge of epilepsy surgery developed a good understanding of the process required to select candidates for surgery.27,28 Epilepsy surgery-specific information(risks, benefits, alternatives) provided by HCPs improved caregivers’ favorable impression toward epilepsy surgery, particularly in parents of prepubescent patients.36 Many caregivers independently searched the internet for information and videos.29 However, one study suggested that information coming from HCPs rather than information websites, internet forums, and patient organizations might be more helpful in forming favorable decisions about epilepsy surgery.16 Many caregivers became ‘epilepsy experts’ as they learned about the language physicians use to communicate about the disease and treatment options among themselves and searched to find the ‘right doctor’ to take care of their child.27 Increasing knowledge empowered caregivers to participate more fully in the decision-making process.29 In one study, parents and grandparents were more willing to consider surgery after seeing images of the child’s brain that helped them understand the severity of the child’s disorder.32
Caregivers felt much better about surgery-and in general, did not prevent them from proceeding with surgery- after being well-informed about unlikely but possible complications of surgery such as hemorrhage, hemiparesis, loss of speech, or even the risk of death.26,32A preoperative phone survey among parents of children with DRE showed that most parents would accept behavioral deterioration to gain seizure remission and would consider surgery if behavioral improvement occurs following surgery without complete seizure freedom.37 Majority of the parents also were willing to consider surgery to reduce seizures despite the risk of visual field defects, short-term memory deficits, and speech problems.37 Caregivers had more trust about epilepsy surgery when they understood the actual and balanced risk-benefit calculation despite the lack of any guarantees of success following surgery.16,26 Caregivers who decided for surgery more often received detailed, comprehensive information about all surgical treatment options involving the child in an age-appropriate way.
3.4.2. Communication and coordination issues
In two studies, HCPs considered some children as poor candidates for surgery based on the low likelihood of seizure-freedom and risks of neurologic deficit after surgery without properly communicating these factors to the caregivers. 31,38 However, caregivers- in certain situations- may consider surgery despite lower possibilities of seizure reduction or associated risk of neurologic deficit following the surgery.31,38 Although neurologists’ attitude toward epilepsy surgery, experience with surgical options, and ability to effectively discuss the risks and benefits of surgery significantly affected parents’ decision-making, some parents were persistent in looking for surgical options despite receiving negative opinions about surgery in the beginning. 30,38 They valued a good medical consultation and a consistent recommendation.16 Caregivers’ perception of their provider—including their view of the provider’s experience level, the provider’s ability to discuss risks and benefits understandably, and the provider’s ability to provoke trust—influenced the caregivers’ decisions about surgery significantly.38
After receiving the presurgical referral and navigating the complex process, caregivers generally felt relief under the care of a multidisciplinary team that they trusted to care for their child and transformed the view of epilepsy surgery as a necessary and valuable option.27,30 Caregivers described several facilitators during this navigation process: (1) pediatrician, nurse, epilepsy care coordinator or navigator, or social worker that championed and advocated for them and helped them navigate their journey (2) multidisciplinary epilepsy team, and (3) other similar families willing to share experience about epilepsy surgery.27
3.4.3. Caregiver’s emotional state
Caregivers were more willing to pursue surgery when they felt they had limited other choices to improve their child’s quality of life and worried about the side effects of medications, nights of interrupted sleep, and the possibility of seizures in potentially hazardous situations.26–29,33,35,38 Caregivers were also concerned that the path toward independence might be difficult for their children as they remained dependent on their parents for adherence to AEDs. 3 Increasing awareness about the severity of epilepsy and its impact on the child’s future life was agonizing for many parents. 30,34 Some caregivers believed that the surgical option might become unavailable once the child transitioned to adult services.29Some were fearful that the child would otherwise die or experience complications due to the seizures without surgery.26 They hoped for an expected reduction of seizures (even if seizure freedom was not possible) and reduced medication after surgery.16,26,35,38 The majority of caregivers also expected improved memory and concentration, greater independence, better school performance, and behavior in their children following surgery.16,35 Gradually, most caregivers felt that epilepsy surgery would be the best and right decision for their child, with the perceived need for surgery outweighing the possible risks and adverse effects.29 Some caregivers also recognized the potential to forego good outcomes if surgery was not pursued.34 Occasionally, caregivers perceived epilepsy surgery as a ‘low-risk operation’ from the outset and were highly receptive to surgical therapy, primarily trusting their physician’s opinion the most about epilepsy surgery. 36 Some felt a sense of duty to be “strong” and “brave” for their children, wishing to protect them from their feelings of anxiety.29 Many felt relieved as they could trust the recommendation of epilepsy surgery if it came from a multidisciplinary epilepsy surgery team meeting.29 Caregivers had greater confidence in surgery after consultation with several specialists, particularly in epilepsy centers.36 A small subset of caregivers were willing to pursue a second and even third surgery to improve seizure burden.38
3.4.4. Socioeconomic effects
Caregivers with higher education were more favorable to surgical options36 and were more favorable to surgery if the children were classified as more intelligent and less resistant to surgery.16 Many caregivers endorsed support from physicians at the local hospitals and the university hospitals/epilepsy centers (physicians, nurses, social workers, psychologists, rehabilitation specialists) as key to moving forward for surgery.26 Some reported that discussing treatment options with family members was helpful in the decision-making.29 Support from the community was also beneficial, particularly obtaining personal assistance and receiving help in taking care of the child and other siblings in nonclinical settings (daycare, school, etc.) when caregivers were not readily available.26
4. Discussion and practice recommendation:
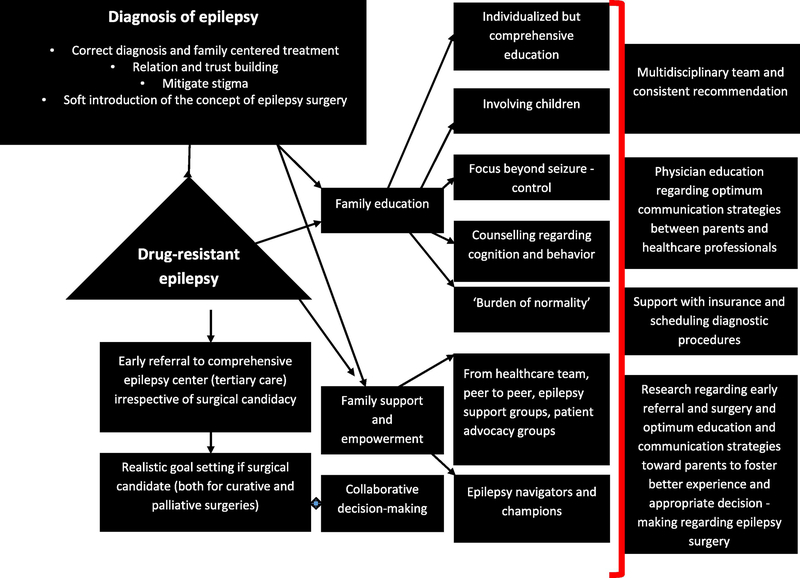
This systematic review provides the meta-synthesis of qualitative and quantitative studies on the caregiver decision-making process toward epilepsy surgery. Previously, Dewar et al. performed a systematic review regarding common conceptual themes shaping perceptions of epilepsy surgery among patients and physicians.6 An explanatory framework in that paper illustrated a triad of fear of surgery, ignorance of treatment options, and tolerance of symptoms leading to refusal of surgery.6 In our review, caregivers perceived a wide range of enablers and barriers to epilepsy surgery related to children, families, providers, health systems, or the community. Despite the lack of studies to assess the efficacy of interventions to overcome barriers, experts recommend multi-pronged strategies to improve surgical utilization.39(Table 4, Figure 2 ). Some of these suggested strategies are primarily applicable in comprehensive epilepsy centers, such as providing a multidisciplinary team of experts and dedicated epilepsy navigators. Still, some interventions are broadly appropriate, including prompt diagnosis and referral of patients of DRE, caregiver education, and shared decision-making process. In addition, many of these informational and relational strategies may indirectly improve parental emotional competencies and attitudes toward epilepsy surgery
Table 4.
Suggestions for clinical practice.
| Early interventions to improve caregiver experience of epilepsy surgery |
| • Early diagnosis and appropriate treatment of drug-resistant epilepsy |
| • Provision of information on the range of treatments-including epilepsy surgery (soft introduction)- from the outset, with the understanding that not all options may be viable or necessary for their child |
| • Early referral to comprehensive epilepsy centers (tertiary care) even when neurologists feel complete seizure-freedom is unlikely following surgery or the child is not a surgical candidate |
| • Caregiver-specific education to mitigate stigma |
| • Better patient–physician communication and strategies to improve caregiver’s trust in the healthcare system |
| Family education, support, and empowerment |
| • Consideration of parental and family well-being and living condition (family-centered care) |
| • Providing support and education for the family throughout the whole journey of epilepsy surgery (from the onset of epilepsy and for an extended duration after surgery) |
| • Presenting adequate information regarding epilepsy surgery, including information in a variety of formats (e.g., patient-directed literature, booklets, photographs, educational videos, patient and family testimonial video clips. URLs of relevant websites) to convey the idea that epilepsy surgery is not an ‘experimental’ option. A ‘frequently asked questions’ information sheet and written up case studies may be beneficial |
| • Discussing epilepsy surgery as a disease-improving intervention in selected patients with epileptic encephalopathy |
| • Steering caregivers to reputable digital and analog resources about epilepsy surgery |
| • Facilitating caregivers’ access to third sector agencies, community resources, online parent support groups, peer-to-peer support, and patient advocacy organizations |
| • Teaching caregivers to navigate insurance policies and the medical system |
| • Providing information about epilepsy surgery many times without jargon in cases when the physician recommends but the parent refuses surgical consideration |
| Shared decision-making |
| • Collaborative and informed decision-making (providing objective data covering indications, modalities of patient selection, expected outcome, and a realistic assessment of the risks) |
| • Consultation and consistent recommendation for surgery, including its impact on learning, development, and psychosocial outcome |
| • Discussion of caregiver expectations regarding neurodevelopmental and behavioral outcome and also the uncertainty and possible limitations of prediction of outcomes following surgery |
| • Counselling regarding ‘the burden of normality’ experienced by children and their families following epilepsy surgery |
| • Balanced discussion of potential positive and negative effects- beyond seizure outcome-following surgery that may be experienced by the patient |
| • Involving children (depending developmental context, such as biological, emotional, and cognitive variables) in the decision-making with age appropriate information |
| Strategies for the healthcare system |
| • Training to advance healthcare professionals’ communication skills, shared decision-making competency, and motivational interview techniques |
| • Developing a specialist multidisciplinary team (including social worker and rehabilitation) that can be involved with the child’s care as early as possible and follow the families for several years after surgery |
| • Providing universal neuropsychological assessment prior to surgery to understand potential impact of surgery beyond seizures |
| • Developing the role of patient navigators to counsel caregivers and help schedule diagnostic studies and appointments |
| • Fostering research that assesses the association of caregiver’s positive experience and favorable decision toward surgery |
Figure 2.
Integrated conceptual framework for potential caregiver-directed interventions for epilepsy surgery.
Early interventions to improve caregiver experience of epilepsy surgery
HCPs should focus on early diagnosis and appropriate family-centered treatment of epilepsy and DRE in primary and secondary care settings. Children with DRE should be promptly referred to comprehensive epilepsy centers, irrespective of the potential of epilepsy surgery. Early referral may allow a shorter duration of epilepsy before surgical treatment, which is associated with a higher seizure-freedom rate and better family satisfaction.40 Communication strategies to mitigate the stigma associated with epilepsy and improve caregivers’ trust in the healthcare system can be beneficial.
Family education, support, and empowerment
Although preferred formats and contents of family-directed education are unknown, caregiver education, support, and empowerment should be a continuous process starting with the diagnosis of epilepsy. A randomized controlled study among adult patients waiting for epilepsy surgery showed decreased anxiety and depression after receiving detailed information.41 These patients watched video interviews of patients already undergone surgery for epilepsy and received detailed information about diagnostic tests. Analog (i.e., easily understandable, appropriate length print materials with fact sheets, booklets; large visual aids in the examination and waiting rooms with treatment options for DRE) and digital (e-books, downloadable apps with or without interactive contents, URLs of relevant websites, patient and family testimonial videos, webinars, podcasts) tools can improve knowledge and reduce anxiety among caregivers.39 Despite increasing use and preference of digital technologies, a combination of multiple modalities with structured (compared to ad hoc instruction), patient- and health literacy-specific, and culturally appropriate(special considerations for racial, ethnic, language, and economically disadvantaged groups) strategies can provide incremental benefit, especially if verification of caregivers’ understanding is possible.42, 43 Patient-specific strategies also include showing children’s neuroimaging pictures to the caregivers, as well as using three-dimensional teaching tools, such as rubber brain models and virtual reality tools((when freely available) to provide caregivers more insights into the underlying brain anatomy, pathology, surgical procedure to improve knowledge and reduce anxieties.44 Besides providing direct information, HCPs also can steer caregivers to reputable online forums and peer-to-peer support programs to allow them to receive support and evidence-based information. Caregiver decision-making is not affected by the knowledge acquired only during the office and hospital visits, but information received between clinic visits- via telephone, email, patient portals tied to electronic health records- may significantly affect caregiver perception and thus decision-making toward surgery.45
Shared decision-making
Collaborative decision-making among HCPs and caregivers - taking into account family goals, preferences, values, and worries (strengths- and needs-based approach)- should be prioritized as recommended by The Institute of Medicine to improve healthcare quality. 46Several decisional-aid studies showed that parents exposed to treatment options(alternatives, risks, and benefits) had more knowledge, less decisional conflict, and more engagement while making a treatment choice in diverse settings, without increasing the visit duration.47,48 HCPs may introduce the concept of surgical therapy early in medical treatment and can actively seek parental views by listing all relevant treatment options-including surgery- for DRE. Although some parents may prefer one straightforward recommendation rather than options, the option-listing may temper medical authority and allow caregivers’ voices to be heard.49 In option-listing, HCPs should be mindful about discussing alternatives in balanced ways as immediate risk of surgery may need to be contrasted with long-term consequences of uncontrolled epilepsy(marginal risk-benefit analysis).50
Parents and physicians should also involve the children in the shared decision-making considering children’s evolving developmental context (e.g., biological, cognitive, and psychosocial variables).8 The lived experiences of the children can contribute significantly and meaningfully to enhance health decisions.51 Proxy decision-making without children’s involvement- primarily if due to power imbalances between children and parents- can cause strained family dynamics in the future as children develop more retrospective awareness of their situation with age and struggle to establish a different identity after surgery.8 Although determining the extent that children should be involved in the decision making is difficult, making the children feel safe and secure, building a trusting relationship, providing age-appropriate information(using graphics) in a relaxed setting over sufficient time, and giving children opportunity to express their views and concerns can be valuable in the decision-making process.52 It is also necessary for clinicians to have appropriate skills to engage children in the decision making.52
Strategies for the healthcare system
The involvement of a specialist multidisciplinary team (including social workers and rehabilitation experts) with the child’s care as early as possible can be beneficial, especially if that team can follow the families for several years after surgery. Similarly, dedicated patient navigators can significantly improve caregiver’s experience by coordinating care, providing social support, and facilitating communication between families and physicians. Physician-specific training to improve communication skills can be helpful to improve the epilepsy care experience. Finally, more research(possibly involving quality improvement initiatives and implementation science framework) is needed to pursue innovative solutions to improve caregivers’ experience and promote systemic uptake of evidence-based practices into the real world.53
Strengths and limitations:
This review provides the first synthesis of empirical studies on the caregiver decision-making process toward epilepsy surgery. The evidence from this systematic review highlights that while significant work has been conducted in a limited number of studies to explore caregiver experience and decision-making, this topic has been largely neglected to formulate specific practice recommendations. We synthesized an integrated framework that may facilitate interventions to promote effective caregiver decision-making for epilepsy surgery. However, there are several limitations in this review. Despite searching multiple databases following a deliberately inclusive search strategy, the possibility cannot be entirely excluded that relevant papers have been missed. The exclusion of non-English language studies may have resulted in publication bias. The included studies have limitations as several primary studies in the review are survey-based with a limited range of questions regarding caregiver experiences. These studies provided a less nuanced understanding of both experience and decision-making processes compared to detailed qualitative studies. The instrument used in these questionnaire-based studies mostly lacked reliability and validity. The survey administration, distribution, and response rate may also produce selection bias related to the participants’ literacy, surgical outcome, ethnicity, culture, and racial background. Most qualitative and survey-based studies were based on retrospective accounts of parents following surgery (sometimes after many years of surgery) and subjected to recall bias and likely affected by the post-surgery clinical outcomes. Additionally, many of the studies looked at parents and HCPs separately during the decision process, but the HCPs highly influence parents’ decision-making, and the dynamic interplay between them in decision-making is under-explored. Another limitation is that some relevant factors in decision-making are yet to be comprehensively evaluated. For example, no studies explored the potential impact of the caregiver’s financial situation contributing to the decision-making toward epilepsy surgery, such as fear of excessive debt following surgery, inability to cover upfront costs and inability to lose income for lost time at work during lengthy diagnostic workup and post-operative recovery.
Qualitative studies had small samples (as expected), but data saturation was not documented in most studies. In some studies, patients were not drawn from a large sample. Few studies had bias due to the provision of large cash incentives. Some studies focused on the experiences of parents over a long duration before and after surgery. Thus the parents may have forgotten some positive and negative aspects of the experience regarding surgery. Most studies included parents of children who underwent surgery (most had positive outcomes following surgery) to understand their experience and decision-making process. However, limited information is available to understand the caregiver experience of those who were not referred for surgery, declined referral to the epilepsy center, or declined surgery. Most qualitative studies recruited participants from one center; their experiences may have limited transferability to other healthcare organizations. Additionally, the diagnostic and therapeutic categories of children included in the research samples vary significantly from one homogenous group (diagnosis: patients with tuberous sclerosis or surgery: hemispherectomy/callosotomy) vs. a highly heterogeneous group comprising different etiologies surgical therapies. This made the comparison across studies impossible as caregiver experience and decision-making would be different with the existing neurologic condition of the child and curative vs. palliative epilepsy surgery. Finally, possible differences in parental experiences based on race or ethnic minority have not been studied.
5. Conclusion:
The purpose of understanding caregiver decision-making for epilepsy surgery is to improve the experience and satisfaction while facilitating appropriate decision-making that optimizes the clinical outcome of the child. Multiple influences impact how caregivers make decisions regarding surgery, with no single factor identified as the primary driver favoring or opposing surgery. Future studies should quantitatively examine many of these factors to identify significant variables that are most likely to influence caregiver decision-making. Additionally, we have limited understanding of how caregiver perception about epilepsy surgery changes over time (as previous studies had cross-sectional and/or retrospective designs). Future studies should follow a longitudinal prospective approach by conducting interviews before surgery to understand the decision-making process and at a specified time points after surgery (both short and long follow-up) to explore the evolution of pre-and post-surgical caregiver experience and its relation with quality of life in both children and caregivers. Future research is also needed to determine if caregiver attitudes toward surgery mediate the timing of presurgical referral and ultimate surgery and how physician-caregiver communication impacts caregiver perceptions and decision-making for surgery.
Acknowledgment:
The authors thank clinical services librarian Ms. Lindsay Ellis Blake, MLIS, AHIP (University of Arkansas for Medical Sciences), for her immense help with the search strategies.
Funding: Debopam Samanta is supported by the Translational Research Institute (TRI), grant UL1 TR003107 through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Megan Hoyt is supported by the ACRI/ABI Nursing and Allied Health Grant.
Footnotes
Disclosures:
The authors declare no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Friedman MJ, Sharieff GQ. Seizures in children. Pediatric Clinics. 2006;53(2):257–277. [DOI] [PubMed] [Google Scholar]
- 2.Engel J What can we do for people with drug-resistant epilepsy?: The 2016 wartenberg lecture. Neurology. 2016;87(23):2483–2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dwivedi R, Ramanujam B, Chandra PS, et al. Surgery for drug-resistant epilepsy in children. N Engl J Med. 2017;377(17):1639–1647. [DOI] [PubMed] [Google Scholar]
- 4.Sharp GB, Samanta D, Willis E. Options for pharmacoresistant epilepsy in children: When medications don’t work. Pediatr Ann. 2015;44(2):e43–e48. [DOI] [PubMed] [Google Scholar]
- 5.Samanta D, Ostendorf AP, Willis E, et al. Underutilization of epilepsy surgery: Part I: A scoping review of barriers. Epilepsy & Behavior. 2021:107837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dewar SR, Pieters HC. Perceptions of epilepsy surgery: A systematic review and an explanatory model of decision-making. Epilepsy Behav. 2015;44:171–178. [DOI] [PubMed] [Google Scholar]
- 7.Samanta D, Hoyt ML, Perry MS. Healthcare professionals’ knowledge, attitude, and perception of epilepsy surgery: A systematic review. Epilepsy & Behavior. 2021;122:108199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boland L, Graham ID, Légaré F, et al. Barriers and facilitators of pediatric shared decision-making: A systematic review. Implementation Science. 2019;14(1):1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vakharia VN, Duncan JS, Witt J, Elger CE, Staba R, Engel J Jr. Getting the best outcomes from epilepsy surgery. Ann Neurol. 2018;83(4):676–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hrazdil C, Roberts JI, Wiebe S, et al. Patient perceptions and barriers to epilepsy surgery: Evaluation in a large health region. Epilepsy Behav. 2013;28(1):52–65. doi: S1525–5050(13)00152–2 [pii]. [DOI] [PubMed] [Google Scholar]
- 11.Ladino LD, Benjumea-Cuartas V, Diaz-Marin DM, et al. Patients’ perceptions of and attitudes towards epilepsy surgery: Mistaken concepts in colombia. Rev Neurol. 2018;67(1):6–14. doi: rn2018015 [pii]. [PubMed] [Google Scholar]
- 12.Prus N, Grant AC. Patient beliefs about epilepsy and brain surgery in a multicultural urban population. Epilepsy & Behavior. 2010;17(1):46–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson CT, Noble E, Mani R, Lawler K, Pollard JR. Epilepsy surgery: Factors that affect patient decision-making in choosing or deferring a procedure. Epilepsy research and treatment. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi H, Pargeon K, Bausell R, Wong JB, Mendiratta A, Bakken S. Temporal lobe epilepsy surgery: What do patients want to know? Epilepsy & Behavior. 2011;22(3):479–482. [DOI] [PubMed] [Google Scholar]
- 15.Nelson PA, Caress A, Glenny A, Kirk SA. ‘Doing the” right” thing’: How parents experience and manage decision-making for children’s ‘Normalising’surgeries. Soc Sci Med. 2012;74(5):796–804. [DOI] [PubMed] [Google Scholar]
- 16.Bach Q, Thomale UW, Müller S. Parents’ and children’s decision-making and experiences in pediatric epilepsy surgery. Epilepsy Behav. 2020;107:107078. doi: S1525–5050(20)30257–2 [pii]. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International journal for quality in health care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 19.Bowling A Constructing and evaluating questionnaires for health services research. research methods in health: investigating health and health services. 1997. [Google Scholar]
- 20.Crombie IK, Harvey BJ. The pocket guide to critical appraisal: A handbook for health care professionals. Canadian Medical Association.Journal. 1997;157(4):448. [Google Scholar]
- 21.Tashakkori A, Teddlie C, Teddlie CB. Mixed methodology: Combining qualitative and quantitative approaches. Vol 46. sage; 1998. [Google Scholar]
- 22.Teddlie C Sage handbook of mixed methods in social & behavioral research. Sage; 2016. [Google Scholar]
- 23.Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Research in the schools: a nationally refereed journal sponsored by the Mid-South Educational Research Association and the University of Alabama. 2006;13(1):29. [PMC free article] [PubMed] [Google Scholar]
- 24.Hsieh H, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 25.Lachal J, Revah-Levy A, Orri M, Moro MR. Metasynthesis: An original method to synthesize qualitative literature in psychiatry. Frontiers in psychiatry. 2017;8:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozanne A, Verdinelli C, Olsson I, Edelvik A, H Graneheim U, Malmgren K. Callosotomy in children - parental experiences reported at long-term follow-up. Epilepsy Behav. 2018;86:91–97. doi: S1525–5050(18)30041–6 [pii]. [DOI] [PubMed] [Google Scholar]
- 27.Pieters HC, Iwaki T, Vickrey BG, Mathern GW, Baca CB. “It was five years of hell”: Parental experiences of navigating and processing the slow and arduous time to pediatric resective epilepsy surgery. Epilepsy Behav. 2016;62:276–284. doi: S1525–5050(16)30263–3 [pii]. [DOI] [PubMed] [Google Scholar]
- 28.Swarztrauber K, Dewar S, Engel J Jr. Patient attitudes about treatments for intractable epilepsy. Epilepsy & Behavior. 2003;4(1):19–25. [DOI] [PubMed] [Google Scholar]
- 29.Heath G, Abdin S, Begum R, Kearney S. Putting children forward for epilepsy surgery: A qualitative study of UK parents’ and health professionals’ decision-making experiences. Epilepsy Behav. 2016;61:185–191. doi: S1525–5050(16)30138-X [pii]. [DOI] [PubMed] [Google Scholar]
- 30.Baca CB, Pieters HC, Iwaki TJ, Mathern GW, Vickrey BG. “A journey around the world”: Parent narratives of the journey to pediatric resective epilepsy surgery and beyond. Epilepsia. 2015;56(6):822–832. doi: 10.1111/epi.12988 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shen A, Quaid KT, Porter BE. Delay in pediatric epilepsy surgery: A caregiver’s perspective. Epilepsy Behav. 2018;78:175–178. doi: S1525–5050(17)30707–2 [pii]. [DOI] [PubMed] [Google Scholar]
- 32.Ozanne A, Verdinelli C, Olsson I, H Graneheim U, Malmgren K. Parental experiences before and long-term after their children’s hemispherotomy - A population-based qualitative study. Epilepsy Behav. 2016;60:11–16. doi: S1525–5050(16)30039–7 [pii]. [DOI] [PubMed] [Google Scholar]
- 33.Engelhart MC, van Schooneveld MM, Jennekens-Schinkel A, van Nieuwenhuizen O. ‘With the benefit of hindsight’: Would you opt again for epilepsy surgery performed in childhood? European Journal of Paediatric Neurology. 2013;17(5):462–470. [DOI] [PubMed] [Google Scholar]
- 34.O’Brien J, Gray V, Woolfall K. Child and parent experiences of childhood epilepsy surgery and adjustment to life following surgery: A qualitative study. Seizure. 2020;83:83–88. doi: S1059–1311(20)30317–4 [pii]. [DOI] [PubMed] [Google Scholar]
- 35.Sylvén I, Olsson I, Hallböök T, Rydenhag B, Reilly C. ‘In the best case seizure-free’–Parental hopes and worries before and satisfaction after their child’s epilepsy surgery. Epilepsy & Behavior. 2020;110:107153. [DOI] [PubMed] [Google Scholar]
- 36.Erba G, Messina P, Pupillo E, Beghi E, OPTEFF Pediatric Group. Acceptance of epilepsy surgery in the pediatric age - what the parents think and what the doctors can do. Epilepsy Behav. 2013;29(1):112–120. doi: S1525–5050(13)00277–1 [pii]. [DOI] [PubMed] [Google Scholar]
- 37.Sassower KC, Rollinson DC, Duchowny M. Outcome of corpus callosotomy and other pediatric epilepsy surgery: Parental perceptions. Epileptic disorders. 2002;3(4):197–202. [PubMed] [Google Scholar]
- 38.Nguyen T, Porter BE. Caregivers’ impression of epilepsy surgery in patients with tuberous sclerosis complex. Epilepsy & Behavior. 2020;111:107331. [DOI] [PubMed] [Google Scholar]
- 39.Samanta D, Singh R, Gedela S, Scott Perry M, Arya R. Underutilization of epilepsy surgery: Part II: Strategies to overcome barriers. Epilepsy & Behavior. 2021:107853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bjellvi J, Olsson I, Malmgren K, Ramsay KW. Epilepsy duration and seizure outcome in epilepsy surgery: A systematic review and meta-analysis. Neurology. 2019;93(2):e159–e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andrewes D, Camp K, Kilpatrick C, Cook M. The assessment and treatment of concerns and anxiety in patients undergoing presurgical monitoring for epilepsy. Epilepsia. 1999;40(11):1535–1542. [DOI] [PubMed] [Google Scholar]
- 42.Shlobin NA, Clark JR, Hoffman SC, Hopkins BS, Kesavabhotla K, Dahdaleh NS. Patient education in neurosurgery: Part 2 of a systematic review. World Neurosurg. 2021;147:190–201.e1. doi: S1878–8750(20)32561–4 [pii]. [DOI] [PubMed] [Google Scholar]
- 43.Knapp C, Sberna-Hinojosa M, Baron-Lee J, Curtis C, Huang I. Does decisional conflict differ across race and ethnicity groups? A study of parents whose children have a life-threatening illness. J Palliat Med. 2014;17(5):559–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.House PM, Pelzl S, Furrer S, et al. Use of the mixed reality tool “VSI patient education” for more comprehensible and imaginable patient educations before epilepsy surgery and stereotactic implantation of DBS or stereo-EEG electrodes. Epilepsy Res. 2020;159:106247. [DOI] [PubMed] [Google Scholar]
- 45.Fiks AG, Localio AR, Alessandrini EA, Asch DA, Guevara JP. Shared decision-making in pediatrics: A national perspective. Pediatrics. 2010;126(2):306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baker A Crossing the quality chasm: A new health system for the 21st century. Vol 323. British Medical Journal Publishing Group; 2001. [Google Scholar]
- 47.Boland L, Kryworuchko J, Saarimaki A, Lawson ML. Parental decision making involvement and decisional conflict: A descriptive study. BMC pediatrics. 2017;17(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brinkman WB, Majcher JH, Poling LM, et al. Shared decision-making to improve attentiondeficit hyperactivity disorder care. Patient Educ Couns. 2013;93(1):95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Toerien M, Shaw R, Reuber M. Initiating decision‐making in neurology consultations:’recommending’versus ‘option‐listing’and the implications for medical authority. Sociol Health Illn. 2013;35(6):873–890. [DOI] [PubMed] [Google Scholar]
- 50.Edwards JC, Sobel RS, Bonilha L. Marginal decision-making in the treatment of refractory epilepsy. J Med Econ. 2018;21(5):438–442. doi: 10.1080/13696998.2017.1412975 [doi]. [DOI] [PubMed] [Google Scholar]
- 51.Eklund PG, Sivberg B. Adolescents’ lived experience of epilepsy. Journal of Neuroscience Nursing. 2003;35(1):40–50. [DOI] [PubMed] [Google Scholar]
- 52.Adams RC, Levy SE. Shared decision-making and children with disabilities: Pathways to consensus. Pediatrics. 2017;139(6). [DOI] [PubMed] [Google Scholar]
- 53.Samanta DLS. Implementation science to improve quality of neurological care. Pediatric Neurology. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]