Abstract
Background
Back pain is the most common cause of disability worldwide. While disability generally is associated with greater mortality, the association between back pain and mortality is unclear. Our objective was to examine whether back pain is associated with increased mortality risk and whether this association varies by age, sex, and back pain severity.
Methods
A systematic search of published literature was conducted using PubMed, Web of Science, and Embase databases from inception through March 2019. We included English-language prospective cohort studies evaluating the association of back pain with all-cause mortality with follow-up periods >5 years. Three reviewers independently screened studies, abstracted data, and appraised risk of bias using the Quality in Prognosis Studies (QUIPS) tool. A random-effects meta-analysis estimated combined odds ratios (OR) and 95% confidence intervals (CI), using the most adjusted model from each study. Potential effect modification by a priori hypothesized factors (age, sex, and back pain severity) was evaluated with meta-regression and stratified estimates.
Results
We identified eleven studies with 81,337 participants. Follow-up periods ranged from 5 to 23 years. The presence of any back pain, compared to none, was not associated with an increase in mortality (OR, 1.06; 95% CI, 0.97 to 1.16). However, back pain was associated with mortality in studies of women (OR, 1.22; 95% CI, 1.02 to 1.46) and among adults with more severe back pain (OR, 1.26; 95% CI, 1.14 to 1.40).
Conclusion
Back pain was associated with a modest increase in all-cause mortality among women and those with more severe back pain.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06732-6.
INTRODUCTION
Back pain affects at least 80% of individuals during their lifetime1, 2. The onset of back pain most commonly occurs in adolescence or early adulthood and can persist or re-occur across the life course2, 3. Globally, back pain is responsible for more years lived with disability than any other condition4, 5. Back-related disability is not distributed equally across the lifespan or across sex: Older adults are more likely to become disabled from back pain than young adults6, 7 and older women are more likely than older men to report “restricting back pain”8. Disability, especially late in life, is an important risk factor for mortality9, 10. Back pain also may be associated with an elevated risk of mortality, but results of individual studies have varied overall and by age and sex groups.
In studies of older adults that did not present sex-specific results, back pain has been associated with a modest increased risk of mortality11, 12 or no increased risk13, 14. In contrast, studies in younger and middle-aged men and women have not found an increased sex-specific mortality risk15–17. Other studies have found that back pain is associated with increased mortality in older women18–20, but not in older men19. Furthermore, three studies suggest severe back pain phenotypes, but not less severe, are associated with an elevated risk of mortality18–20. No prior review has quantitatively synthesized the results of multiple studies to clarify the direction and magnitude of the association between back pain and mortality, either overall or in these different subgroups.
Therefore, we performed a systematic review and meta-analysis focused on two questions: First, among adults, is back pain independently associated with increased risk of all-cause mortality? Second, do age, sex, and back pain severity modify the association between back pain and mortality? We hypothesized that compared to adults without back pain, those with back pain would have a moderately increased risk of all-cause mortality. Additionally, we hypothesized the relative increase in risk of mortality associated with back pain would be highest among older adults, women, and those with more severe back pain.
METHODS
We followed the PRISMA systematic review and meta-analysis guidelines21. Our study followed an a priori established protocol published in PROSPERO on January 3, 2018 (registration number CRD42018072151).
Search Strategy
We searched for English-language studies relevant to the research question using MeSH terms for back pain (low back pain, sciatica), related conditions (kyphosis, lordosis, scoliosis, spinal fracture, spinal stenosis), and death (mortality, death, survival rate) in PubMed (1966–), EMBASE (1980–), and ISI Web of Science (1965–) through March 2019 (eAppendix 1). We also reviewed the reference lists of potentially eligible studies to identify other relevant studies.
Study Selection
Prospective cohort studies were selected if they enrolled adults (age >18) with and without non-specific back pain defined by self-report or clinical examination, included follow-up periods of >5 years, and reported all-cause mortality outcomes. Three independent reviewers (E.J.R., I.R., and P.S.) screened titles, abstracts, and keywords for eligibility. The full text of all potentially eligible studies was obtained and reviewed by all three reviewers. Disagreements about eligibility were resolved by discussion and consensus among reviewers and a senior investigator (R.S.).
Quality Assessment
Individual study risk of bias was independently assessed by two reviewers (E.J.R. and I.R.) using the validated Quality in Prognosis Studies (QUIPS) tool22, 23. To mitigate against possible conflict of interest, one study20 was assessed by P.S. and I.R. instead. Each study was evaluated according to predefined criteria consisting of six domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and analysis. The risk of bias in each domain was rated as low, moderate, or high based on information presented in the article and overall judgment by two reviewers. Discrepancies in assessments were resolved by a joint re-evaluation with a senior epidemiologist (L.F.).
Data Extraction and Analysis
For each eligible article, data were extracted independently by three reviewers (E.J.R., I.R., and P.S.) using a standardized extraction form. These data included details on study characteristics (author, year, design, sample size), population (age, sex, race/ethnicity), back pain status (method of assessment [self-report, physical exam] and severity [frequency or duration of symptoms, interference with physical function]), and potentially confounding variables included in multivariable models. We extracted estimates of all-cause and cause-specific mortality outcomes for the least and most adjusted models, using the most adjusted estimate from each study as the primary outcome of interest. If not available in tables or text, authors were contacted to obtain missing information or counts of deaths were estimated from figures.
Meta-analysis of All-cause Mortality
The association of back pain with mortality was recorded as either a hazard ratio (HR), odds ratio (OR), relative risk (RR), or standardized mortality ratio (SMR). All study-level estimates of mortality risk were analyzed as if they were ORs when calculating combined estimates24–26. Estimates of mortality risk from the most severe back pain category were used. When only two categories of back pain were presented (any back pain, yes or no), having any back pain was considered the most severe category. We calculated and plotted ORs and their 95% confidence intervals (CI). If CIs were not available, they were calculated from p values.
Our primary analysis was a random-effects model, using the approach by DerSimonian and Laird to calculate the summary OR and 95% CI.27 A secondary analysis was also done using a fixed-effect model.27 We quantified the heterogeneity of ORs of individual studies using the I2 statistic.28 We considered I2 values less than 0.25 as low, 0.25–0.75 as moderate, and over 0.75 as high28. The possibility of publication bias was assessed through visual inspection of a funnel plot. Our funnel plot graphed the effect size (log odds ratio) of each study on the horizontal axis and the standard error, which reflects the sample size, on the vertical axis.
Meta-regression and Stratified Analyses
Potential effect modification by a priori hypothesized factors (age, sex, and back pain severity) was evaluated with meta-regression and stratified estimates. First, we performed a meta-regression by mean study age. Stratified estimates for older and younger adults were also generated by combining studies where the mean study age was 65 and older or under 65, respectively. Second, we performed a meta-regression evaluating the risk of mortality by the proportion of female study participants. Sex-stratified estimates of mortality were also generated for studies of men only, women only, or those including both men and women. Third, we performed stratified analyses by back pain severity subgroups characterized as “severe,” “moderate,” or “mild/unspecified.” Studies that used an exposure with three or more levels and a clear severe category were classified as “severe.” From the remaining studies, we characterized studies with three levels but no clear severe category as “moderate” and those with only two levels as “mild/unspecified.” In a sensitivity analysis of the “severe” group, we combined studies initially characterized as “severe” or “moderate.”
All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Search Results
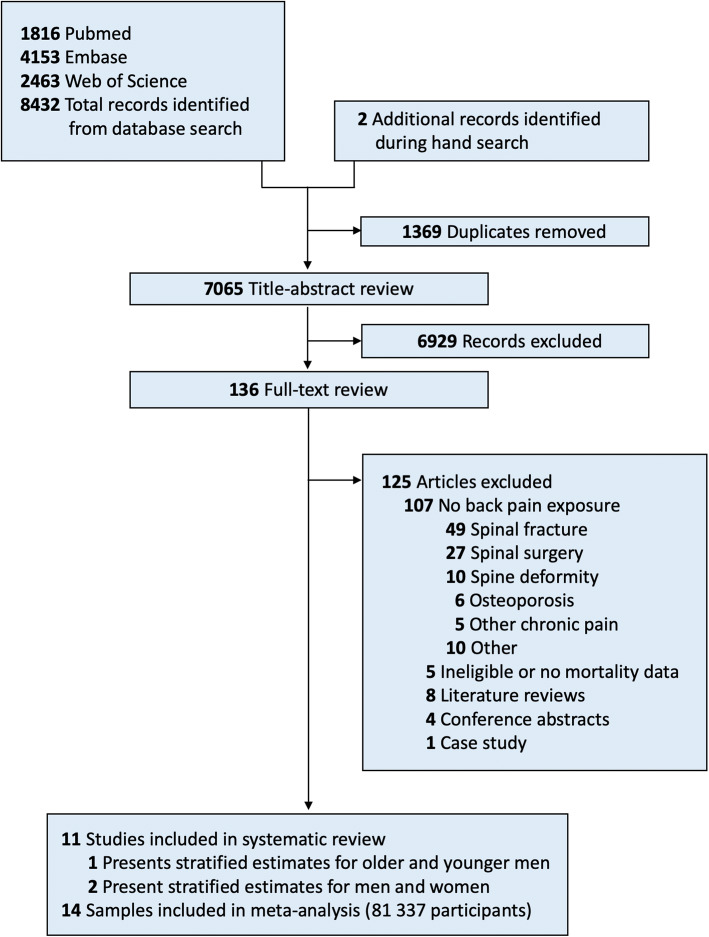
Of 7065 unique publications identified through our initial search, we excluded all but 136 based on title and abstract review (Fig. 1). A list of all excluded full-text articles and reason for exclusion is shown in eAppendix 6. Most of the excluded studies evaluated the association of back-related conditions (e.g., spinal fractures) with mortality, but did not include information on the association of back pain symptoms with mortality. Eleven studies published between 1988 and 2019, with 81,337 participants, met our inclusion criteria (Table 1). Roughly half of the included studies recruited participants from Scandinavian countries (n=5), followed by the UK (n=3), and Australia, Israel, and the USA (n=1 each). In the single study that reported the race of participants, all were white20. The prevalence of any back pain (i.e., without regard to severity or frequency) ranged from 23.6 to 76%. The longest follow-up periods lasted 20 to 23 years13, 15, 19 and half of studies followed participants for periods of 10 to 14 years11, 14, 16, 17, 20, 29. All studies ascertained all-cause mortality from death registries or death certificates, with five studies (seven samples) also reporting cause-specific mortality.
Figure 1.
PRISMA flow diagram.
Table 1.
Longitudinal Cohort Studies Evaluating the Association of Back Pain and All-Cause Mortality
| Author, year (country) | No of participants by sex | Mean age | Reference (%) and exposure(s) (%) | Follow-up (years) | Potential confounders in: A: Least adjusted model B: Most adjusted model (if available) |
All-cause mortality estimatea (95% CI) |
|---|---|---|---|---|---|---|
|
Astrand et al.,15 1988 (Sweden) |
391 men | 50 |
No back pain (68) Back pain on self-report (25) Back abnormality on exam (16) |
22 | A: Crude |
Back pain A: RR=1.02 (0.75 to 1.39) Back abnormality A: RR=1.23 (0.89 to 1.71) |
|
Penttinen et al.,16 1994 (Finland) |
1860 men | 40b |
No back pain (32) Back pain (68) |
13 |
A: Crude B: Age, smoking, BMI, and social status |
Back pain A: RR=1.27 (0.82 to 1.97) B: NR |
| 1788 men | 58b |
No back pain (33) Back pain (67) |
13 |
A: Crude B: Age, smoking, BMI, and social status |
Back pain A: RR=0.84 (0.68 to 1.03) B: NR |
|
|
Heliovaara et al.,17 1995 (Finland) |
3322 men | 55b |
No previous back pain (23) 1-5 back pain episodes (22) >5 back pain episodes (55) |
12–14 | A: Age |
1-5 episodes A: RR=1.0 (0.8 to 1.2) >5 episodes A: RR=0.9 (0.7 to 1.0) |
| 3895 women | 55b |
No previous back pain (26) 1-5 back pain episodes (20) >5 back pain episodes (54) |
12–14 | A: Age |
1-5 episodes A: RR=0.9 (0.7 to 1.2) >5 episodes A: RR=1.0 (0.8 to 1.2) |
|
|
Kareholt et al.,13 1998 (Sweden) |
923 men 931 women |
65b |
No pain (NR) Mild back/hip pain (NR) Severe back/hip pain (NR) |
23 | A: Age and sex |
Mild back/hip pain A: HR=0.89 (0.77 to 1.03) Severe back/hip pain A: HR=1.04 (0.88 to 1.23) |
|
Jacobs et al.,29 2005 (Israel) |
249 men | 70 |
No back pain (69) Chronic back pain (31) |
12 | A: Physical activity, self-rated health, hypertension, diabetes mellitus, ischemic heart disease, neoplasm, and smoking status |
Chronic back pain A: HR=0.41 (0.25 to 0.68) |
|
Zhu et al.,18 2007 (Australia) |
1484 women | 75 |
Infrequent back pain (51) Frequent back pain (28) Daily back pain (22) |
5 |
A: Age B: Age, BMI, smoking history, analgesia use, diabetes, cardiovascular disease, hypercholesterolemia, and hypertension |
Frequent back pain A: HR=1.27 (0.70 to 2.32) B: HR=1.21 (0.66 to 2.22) Daily back pain A: HR=2.03 (1.14 to 3.60) B: HR=1.85 (1.00 to 3.43) |
|
Torrance et al.,14 2010 (UK) |
1464 menc 1631 womenc |
58 |
No chronic pain (55) Chronic back pain (45) |
10 | A: Age, sex, education, and housing |
Chronic back pain A: HR=1.08 (0.92 to 1.27) |
|
Jordan et al.,11 2010 (UK) |
22 281 men 27 232 women |
66 |
No back pain (81) Back pain (19) |
10 | A: Age and sex standardized |
Back pain A: SMR=1.17 (1.12 to 1.22) |
|
Docking et al.,19 2015 (UK) |
411 men | 83b |
No back pain (79) Non-disabling back pain (18) Disabling back pain (3) |
20 |
A: Crude B: Age, residence, social class, marital status, arthritis/rheumatism, use of medication, previous use of general anesthetic, chest pain, shortness of breath, and fall history |
Non-disabling back pain A: HR=1.0 (0.8 to 1.3) B: HR=0.9 (0.7 to 1.2) Disabling back pain A: HR=1.4 (0.8 to 2.6) B: HR=1.0 (0.5 to 1.9) |
| 763 women | 83b |
No back pain (67) Non-disabling back pain (26) Disabling back pain (7) |
20 |
A: Crude B: Age, residence, social class, marital status, arthritis/rheumatism, use of medication, previous use of general anesthetic, chest pain, shortness of breath, and fall history |
Non-disabling back pain A: HR=1.0 (0.8 to 1.1) B: HR=0.9 (0.8 to 1.1) Disabling back pain A: HR=1.5 (1.2 to 2.0) B: HR=1.4 (1.1 to 1.9) |
|
|
Fernandez et al.,12 2017 (Denmark) |
1741 men 2650 women |
78 |
No spinal pain (65) Spinal pain (35) |
9.2 |
A: Crude B: Depression |
Spinal pain A: HR=1.13 (1.06 to 1.21) B: HR=1.03 (0.96 to 1.11) |
|
Roseen et al.,20 2019 (USA) |
8321 women | 72 |
No back pain (24) Non-persistent back pain (23) Infrequent persistent back pain (44) Frequent persistent back pain (9) |
14.1 |
A: Age B: Age, education, marital status, living alone, recruitment site, obesity, excellent general health, current smoker, prevalent vertebral fracture, arthritis, hip pain, fall history, hospitalizations, hypertension, previous stroke, diabetes, history of breast cancer, previous breast surgery, and anxiety medication use |
Non-persistent A: HR=1.05 (0.96 to 1.14) B: HR=1.01 (0.93 to 1.10) Infrequent persistent A: HR=1.04 (0.97 to 1.12) B: HR=0.98 (0.91 to 1.05) Frequent persistent A: HR=1.46 (1.32 to 1.61) B: HR=1.24 (1.11 to 1.39) |
CI, confidence interval; NR, not reported; OR, odds ratio; HR, hazard ratio; SMR, standardized mortality ratio; BMI, body mass index
aEstimate of effect size are presented as using HR, OR, or SMR
bMean age was estimated for meta-regression in the following studies: Mean age for Penttinen and Kareholt was estimated using age range; Mean estimate for Jordan was an average of mean age for back pain and control group; Mean age for sex-specific estimates in Heliovaara and Docking was based on the overall mean age of sample
cThe number of men and women for Torrance is based on the proportion of women in the entire sample of 5853 participants (52.7% female) applied to 3095 individuals with either chronic low back pain or no chronic pain
Two studies presented sex-stratified results17, 19 and one included separate estimates for younger and older men (age 30–49 and 50–66, respectively)16. This resulted in 14 samples derived from 11 studies: six samples of men only, four of women only, and four of both men and women (proportion female ranged from 50 to 65%). The mean age ranged from 40 to 83 years and was 65 or higher in seven studies. Five studies (six samples) included only two levels of back pain and were characterized as “mild/unspecified” back pain11, 12, 14, 16, 29. Three studies (four samples) had multiple levels of pain but the most severe level did not clearly represent severe pain, i.e., back abnormality on physical exam, history of five or more previous episodes of back pain with no requirement of current pain, or current severe back or hip pain without information on duration13, 15, 17. We characterized these phenotypes as “moderate” back pain. We identified three studies (four samples) that had multi-level exposures and a clear “severe” category, i.e., disabling back pain, daily back pain, and frequent back pain persisting over a 2-year period18–20.
Methodological Quality
The most frequent potential biases identified were in the domains of prognostic factor measurement and study confounding (Table 2). None of the studies used validated instruments to measure back-related pain or function, e.g., Brief Pain Inventory and Roland Morris Disability Questionnaire. Most studies did not provide a rationale for the covariables included in statistical models as confounders; none used causal graphs (e.g., directed acyclic graphs) to illustrate assumptions of potential causal relationships. Two studies reported only unadjusted models15, 16. Among the seven studies reporting adjusted models, common covariates were age11, 14, 18–20, smoking18, 20, 29, socioeconomic status14, 19, 20, sex11, 14, 30, cardiovascular disease18–20, 29, and body mass index18, 20. Other sources of bias included inadequate study participation13, 15 where assessors deemed that study participants may not have represented the source population, and no reporting of sex-specific analyses11, 12. All studies but one were rated low risk of bias due to study attrition, primarily due to the use of death registries or certificates to ascertain mortality.
Table 2.
| Author | Domains assessed for risk of bias | Analysis | Comments | ||||
|---|---|---|---|---|---|---|---|
| Study participation | Study attrition | Prognostic factor measurement | Outcome measurement | Study confounding | |||
|
Astrand et al.,15 1988 |
Moderate | Low | Low | Low | High | High | Inadequate sampling of source population. Report only crude results. No report of sample size of exposed and unexposed group that died and use of life-table analysis. |
|
Penttinen et al.,16 1994 |
Moderate | Low | High | Low | Low | Moderate | Unclear description of the study population. Back pain was only measured for one year before. No report of back pain question. Results analyzed using regression. |
|
Heliovaara et al.,17 1995 |
Low | Low | Moderate | Low | Low | Low | Self-report of back pain. |
|
Kareholt et al.,13 1998 |
High | Low | High | Low | Moderate | Moderate | Inadequate study participation. No explicit inclusion or exclusion criteria. High prognostic factor bias due to self-report and exposure consisting of both back pain and hip pain. |
|
Jacobs et al.,29 2005 |
Low | Low | High | Low | Moderate | Moderate | High risk of misclassification resulting from yes vs. no for frequent back pain. Probable mediator variables (e.g., physical activity) adjusted for in models. No reporting on women or crude data. |
|
Zhu et al.,18 2007 |
Low | Low | Moderate | Low | Low | Low | Self-report of back pain. |
|
Torrance et al.,14 2010 |
Low | Low | Moderate | Low | Low | Low | Postal survey questionnaire more focused on generalized pain with only one question on back pain. |
|
Jordan et al.,11 2010 |
Low | Moderate | Moderate | Low | Low | Low | Undisclosed loss to follow up. Potential misclassification bias of back pain exposure (cases needed to have a new diagnosis to be eligible, rather than persistent back pain). |
|
Docking et al.,19 2015 |
Low | Low | Moderate | Low | Moderate | Low | Self-report of back pain. Probable moderator variables adjusted for in models. |
|
Fernandez et al.,12 2017 |
Low | Low | Moderate | Low | Moderate | Low | Self-report of back pain. Age not explicitly considered a confounder. |
|
Roseen et al.,20 2019 |
Moderate | Low | Moderate | Low | Low | Low | No report on survey non-response. Self-report of back pain |
Descriptive Assessment of Individual Studies
Of eleven studies (fourteen samples), about half (5 studies, 6 samples) observed a modest increase in mortality (Table 1).
Of four studies that did not stratify estimates by sex, only one observed an increase in mortality risk11. All four studies that included older women found a modest increase in mortality11, 18–20. One of these reported an increase in mortality among older women (HR=1.5; 95%CI, 1.2–1.9) but not older men (HR=1.0; 95%CI, 0.5–1.9)19. In three of these studies, back pain exposure was categorized into three or four groups, e.g., none/infrequent, frequent back pain, and daily back pain. One study, which evaluated multiple back pain phenotypes, found that “any” back pain was not associated with mortality but other phenotypes were, e.g., frequent back pain, back pain that limits daily activities, and difficulty lifting a 10-pound object due to back pain20. Of six studies (seven samples) including only men, all found no association between back pain and mortality13–17. One study found that back pain in older Israeli men was associated with lower mortality risk (HR=0.41; 95%CI, 0.25–0.68).29 Most of these studies categorized back pain as present or absent.
Cause-specific mortality findings are summarized in eAppendix 2. The results for cardiovascular mortality were mixed; in two studies, back pain was associated with an increased risk of cardiovascular mortality in younger men16 and older women20. However, four other studies that included middle-aged men16, 17, women17, or both men and women12, 14 found no elevated risk of cardiovascular mortality. The two studies that assessed pulmonary deaths observed an increased risk of pulmonary-related death14, 20. Among the two studies assessing cancer deaths, an increased risk of cancer deaths was observed in older women20 but not in middle-aged adults14.
Meta-analysis
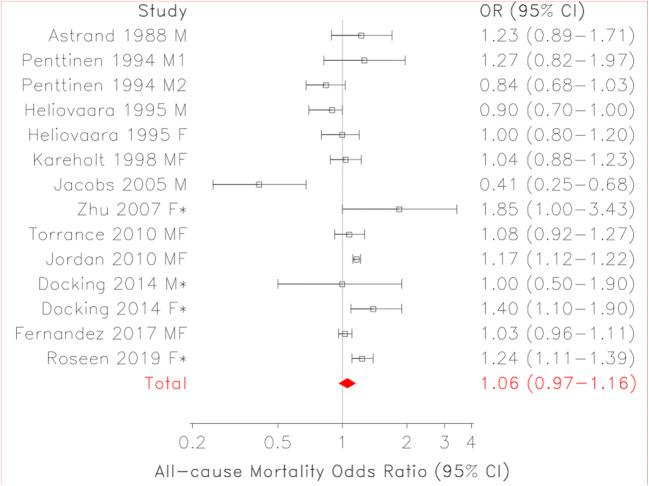
The presence of any back pain, compared to none was not associated with an increase in mortality in our random-effects analysis (OR=1.06; 95%CI, 0.97–1.16; df=13; I2=78%) (Table 2, Fig. 2). The fixed-effect analysis resulted in a somewhat larger risk of mortality (OR=1.10; 95%CI, 1.07–1.14). A high I2 value and shift in the effect estimate from fixed to random effects model suggest the presence of significant heterogeneity in our overall combined estimate. A hole on the left side of our funnel plot and an outlier29 on the same side are shown in eAppendix 3.
Figure 2.
Forest plot of studies evaluating back pain and all-cause mortality. Footnote: M, male; F, female; M1, men ages 30–49; M2, men ages 50–66; *Frequent/disabling back pain phenotype; CI, confidence interval.
In meta-regression by mean study age, each 1-year increase in mean study age did not result in an increase in the risk of mortality associated with back pain (log odds per year=0.004; df=13; p=0.30; eAppendix 4). However, the risk of mortality associated with back pain appeared higher among studies with a mean age of 65 or older (OR=1.11; 95%CI, 0.99–1.24; df=7; I2=78%) than studies where the mean age was under 65 (OR=0.98; 95%CI, 0.89–1.10; df=5; I2=45%) (Table 3). The risk of mortality associated with back pain was increased in samples with a greater proportion of female participants (meta-regression, increase in log odds per 1% increase in proportion female=0.0028; df=13; p=0.0006; eAppendix 5). Sex-stratified analyses showed that back pain was associated with elevated mortality risk in studies of women (OR=1.22; 95%CI, 1.02–1.46; df=3; I2=57%) but not of men (OR=0.90; 95%CI, 0.73–1.12; df=5; I2=68%). Lastly, compared to persons with no back pain, “severe” back pain was associated with increased mortality risk (OR=1.26; 95%CI, 1.14–1.40; df=3; I2=19%), but back pain characterized as “moderate” or “mild/unspecified” severity was not (OR=0.99; 95%CI, 0.89–1.10; df=3; I2=36%; and OR=1.00; 95%CI, 0.87–1.15; df=5; I2=85%; respectively). A sensitivity analysis that included studies initially characterized as “moderate” found this attenuated the relationship between “severe” back pain and mortality (OR=1.12; 95%CI, 0.97–1.28; df=7; I2=71%).
Table 3.
Combined Estimates of the Association of Back Pain with Mortality, Overall, and Stratified by Age, Sex, and Severity of Back Pain
| No. of participants | No. of samples | Combined estimate OR (95% CI) | Heterogeneity I2 | |
|---|---|---|---|---|
| All-cause mortality | ||||
| Overall | 81,337 | 14 | 1.06 (0.97, 1.16) | 0.78 |
| Mean study age | ||||
| <65 | 14,351 | 6 | 0.98 (0.89, 1.10) | 0.45 |
| >65 | 66,986 | 8 | 1.11 (0.99, 1.24) | 0.78 |
| Sex | ||||
| Male | 8021 | 6 | 0.90 (0.73, 1.12) | 0.68 |
| Female | 14,463 | 4 | 1.22 (1.02, 1.46) | 0.57 |
| Mixed | 58,853 | 4 | 1.09 (1.00, 1.19) | 0.69 |
| Back pain severity | ||||
| Mild/unspecified | 60,896 | 6 | 1.00 (0.87, 1.15) | 0.85 |
| Moderate | 9462 | 4 | 0.99 (0.89, 1.10) | 0.36 |
| Severe | 10,979 | 4 | 1.26 (1.14, 1.40) | 0.19 |
| Sensitivity analysisa | 20,441 | 8 | 1.12 (0.97, 1.28) | 0.71 |
aSensitivity analysis combines eight samples with multi-level back pain exposures
DISCUSSION
In this meta-analysis of 11 studies with 81,337 middle-aged and older adults, back pain was not associated with an increase in all-cause mortality compared to adults without back pain. Age did not appear to modify the association between back pain and mortality. We found no association in men with any back pain or among adults with non-severe back pain. However, back pain was associated with mortality in studies of women and among adults with more severe back pain.
No prior systematic review, to our knowledge, has reported on the association of back pain with mortality. Overall, we observed high levels of heterogeneity and a non-significant association of back pain with mortality. A previous systematic review found that non-specific chronic pain was associated with a small but not statistically significant risk of mortality31. They also found high levels of heterogeneity in their overall estimate and hypothesized that heterogeneity may be explained by pain phenotype or other subgroups (e.g., age, sex)31. A recent study on acute musculoskeletal pain (<1-month pain duration in various sites) found no association with all-cause mortality, suggesting that chronicity of musculoskeletal pain may drive results32. Other studies have reported an increased risk of mortality with other chronic disabling musculoskeletal conditions, e.g., osteoarthritis33, 34.
Our findings suggest age does not modify the association of back pain and mortality. This was unexpected as the impact of back pain on disability increases with age6, 7, 35, especially among women8. This observation may support our findings that pain phenotype is important. For example, only older adults with back pain that interferes with daily life may be at risk of increased mortality36. The mortality risk associated with more severe back pain may be higher among older adults than younger adults. Our meta-regression approach used mean study age. Without patient-level data on age, meta-regression results are necessarily limited and should only be viewed as hypothesis-generating for future research and not as definitive.
Our finding of elevated mortality among women with back pain, but not among men, indicates the long-term consequences of back pain may differ by sex. Docking et al. speculate their observation of increased mortality risk in older women with back pain, but not older men, may be related to undiagnosed osteoporotic fractures19. Indeed, both clinically diagnosed and silent vertebral fractures are associated with an increased risk of mortality in older women.37 However, two studies in our review found that adjusting for prevalent vertebral fractures did not account for the association between back pain and mortality11, 20.
We found that the highest risk of mortality associated with back pain was observed in studies that included only women17–20 and those with “severe” back pain18–20. However, three samples were included in both sub-analyses18–20, making it difficult to disentangle the relative impact of more severe back pain and female sex. Furthermore, only one study of men included a back pain category that captured “severe” back pain. Additional prospective studies of men are necessary to clarify this association.
The clinical implications of our study hinge on understanding the mechanisms by which more severe back pain may be associated with earlier mortality. Given that patients with back pain may have difficulty performing daily living activites38, we propose disability as a credible mediator9, 39. Three studies in our review support this causal model12, 19, 20, one of which performed causal mediation analyses suggesting half of the observed increase in mortality risk could be attributed to limitations in activities of daily living20. This observation is further supported by a recent study which found limitations in function related to pain (i.e., symptoms preventing walking a quarter of a mile) mediated the majority of a modest association of “concerning” chronic pain, compared to no pain, with mortality40. Reduced physical activity may lead to weight gain and development or worsening of chronic conditions, such as cardiovascular disease, which can further increase mortality risk18, 41, 42. Back pain has also been linked with poor balance and falls, which can result in fragility fractures43, 44. Mortality attributed to falls is on the rise in the USA45, and managing back-related pain and function may be important for preventing falls among older Americans35, 46.
Additional pathways between back pain and mortality are relatively unexplored. There is likely a bidirectional relationship between back pain and psychological factors; i.e., adults with anxiety/depression may be more likely to develop and report more severe or persistent back pain or vice versa35, 47. Patients who exhibit poor pain coping strategies (e.g., low pain self-efficacy, catastrophizing) may avoid physical activity, plausibly increasing their mortality risk via inactivity. Researchers have also identified an association between back pain and suicide48–50. Psychological factors were addressed in only one study in our review12. The complex relationship among back pain, mental health conditions, and mortality is an important area of future study.
We found little information on the impact of back pain treatment on the observed mortality risk in adults with back pain. Opioids, which are commonly prescribed for back pain, can carry the risk of dependence, addiction, overdose, and death51–54. In addition to overdose deaths, opioid use for non-cancer pain is associated with increased cardiovascular mortality in middle-aged and older adults55. This may be particularly relevant for studies gathering data in the last two decades when opioid use markedly increased for musculoskeletal pain56. Other pain medications commonly used to manage chronic back pain may also impact mortality risk. For example, long-term use of NSAIDs is associated with cardiovascular events and mortality57–59. Not seeking care, or not engaging in appropriate self-care, may also lead to disability or a generally worse health state, which may contribute to earlier mortality. Clinical practice guidelines from the American College of Physicians recommend non-pharmacologic approaches (e.g., acupuncture, chiropractic care, physical therapy) as safe and effective first-line treatment for acute and chronic low back pain60. However, little is known about whether the use of these or other therapies for managing back pain affects mortality.
Important limitations of this systematic review and meta-analysis include the variability in the measurement of back pain and the lack of a uniform approach to identifying levels of back pain, i.e., phenotyping. For our overall estimate of mortality risk, we combined studies that included a wide range of back pain exposures. Patients with mild or non-disabling back pain were included in this analysis, likely biasing findings toward the null. We tried to address this limitation by obtaining a combined estimate for studies that clearly included a severe back pain phenotype (e.g., frequent or disabling chronic back pain). Confounders included in multivariable models differed across studies, and residual confounding remains a plausible explanation for our findings. Variation in back pain measurement and adjustment for confounders likely contributed to the high level of heterogeneity observed in our combined estimate. Heterogeneity was reduced somewhat in stratified analyses, mainly when combining the four samples using a severe back pain phenotype.
Additionally, no study included in this review was specifically designed to examine the association of back pain with mortality a priori. A hole observed in our funnel plot provides further support of potential publication bias, which may bias results away from the null. However, an outlier on the left side of our funnel plot was observed as well, which would tend to pull these results in the opposite direction, i.e., toward the null. Lastly, incomplete data on some demographic groups (e.g., racial or ethnic minorities, low-income adults) may limit generalizability to understudied populations.
CONCLUSION
Back pain was associated with a modest increase in the risk of all-cause mortality among women and those with more severe back pain. This study raises the question of whether better management of back-related pain and disability, over time, may extend life.
Supplementary Information
(DOCX 44 kb)
Additional Contributions
We thank David Felson, MD, MPH, Tuhina Neogi, MD, PhD, and others at the Boston University Clinical Epidemiology Research and Training Unit for reviewing this manuscript. The search strategy was performed with the assistance of David Flynn MS, a research librarian at the Boston University School of Medicine. Additional thanks to Nicola Torrance, PhD, for providing additional data for this review.
Author Contribution
Drs. Roseen, Rajendran, LaValley, and Saper had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Roseen, Rajendran, Stein, Fredman, Fink, LaValley, and Saper
Acquisition, analysis, or interpretation of data: Roseen, Rajendran, Stein, Fredman, and LaValley
Drafting of the manuscript: Roseen, Rajendran, and Stein
Critical revision of the manuscript for important intellectual content: Roseen, Rajendran, Stein, Fredman, Fink, LaValley, and Saper
Statistical analysis: Roseen and LaValley
Obtained funding: n/a
Administrative, technical, or material support: Roseen and Rajendran
Study supervision: Roseen, Rajendran, Saper
Funding
Dr. Roseen’s work on this manuscript was supported by awards from the National Center for Complementary and Integrative Health (NCCIH, F32-AT009272, K23-AT010487).
Declarations
Disclaimer
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of NCCIH.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentations
This work was presented, in part, at the National Institutes of Health 13th Annual Pain Consortium Symposium (June 1, 2018) in Bethesda, MD; the Society for Epidemiologic Research Annual Meeting (June 20, 2019) in Minneapolis, MN; and the International Forum for Back and Neck Pain Research in Primary Care (July 5, 2019) in Quebec City, Quebec, Canada.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Eric J. Roseen, Email: Eric.Roseen@bmc.org.
Iniya Rajendran, Email: IR1@bu.edu.
Peter Stein, Email: Stein.PJ@gmail.com.
Lisa Fredman, Email: LFredman@bu.edu.
Howard A. Fink, Email: Howard.Fink@va.gov.
Michael P. LaValley, Email: MLava@bu.edu.
Robert B. Saper, Email: Robert.Saper@bmc.org.
References
- 1.Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. The Lancet. 2012;379(9814):482–491. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 2.Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 3.Dunn KM, Hestbaek L, Cassidy JD. Low back pain across the life course. Best Pract Res Clin Rheumatol. 2013;27(5):591–600. doi: 10.1016/j.berh.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 4.G. B. D. Disease Injury, Incidence Prevalence, Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-1602. [DOI] [PMC free article] [PubMed]
- 5.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. The Lancet. 2018;391(10137):2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 6.Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154(12):2649–2657. doi: 10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Iorio A, Abate M, Guralnik JM, et al. From chronic low back pain to disability, a multifactorial mediated pathway: the InCHIANTI study. Spine (Phila Pa 1976). 2007;32(26):E809–815. doi: 10.1097/BRS.0b013e31815cd422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill TM. Epidemiology of restricting back pain in community-living older persons. J Am Geriatr Soc. 2011;59(4):610–614. doi: 10.1111/j.1532-5415.2011.03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper R, Strand BH, Hardy R, Patel KV, Kuh D. Physical capability in mid-life and survival over 13 years of follow-up: British birth cohort study. BMJ. 2014;348:g2219. doi: 10.1136/bmj.g2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu LW, Chen WL, Peng TC, et al. All-cause mortality risk in elderly individuals with disabilities: a retrospective observational study. BMJ Open. 2016;6(9):e011164. doi: 10.1136/bmjopen-2016-011164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jordan KP, Croft P. Mortality and cancer in patients with new musculoskeletal episodes: a cohort study. British Journal of General Practice. 2010;60(572). [DOI] [PMC free article] [PubMed]
- 12.Fernandez M, Boyle E, Hartvigsen J, et al. Is this back pain killing me? All-cause and cardiovascular-specific mortality in older Danish twins with spinal pain. Eur J Pain. 2017;21(5):938–948. doi: 10.1002/ejp.996. [DOI] [PubMed] [Google Scholar]
- 13.Kareholt I, Brattberg G. Pain and mortality risk among elderly persons in Sweden. Pain. 1998;77(3):271–278. doi: 10.1016/S0304-3959(98)00103-1. [DOI] [PubMed] [Google Scholar]
- 14.Torrance N, Elliott AM, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380–386. doi: 10.1016/j.ejpain.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 15.Astrand NE, Isacsson SO. Back pain, back abnormalities, and competing medical, psychological, and social factors as predictors of sick leave, early retirement, unemployment, labour turnover and mortality: A 22 year follow up of male employees in a Swedish pulp and paper company. British Journal of Industrial Medicine. 1988;45(6):387–395. doi: 10.1136/oem.45.6.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Penttinen J. Back pain and risk of fatal ischaemic heart disease: 13 year follow up of Finnish farmers. BMJ. 1994;309(6964):1267–1268. doi: 10.1136/bmj.309.6964.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heliovaara M, Makela M, Aromaa A, Impivaara O, Knekt P, Reunanen A. Low back pain and subsequent cardiovascular mortality. Spine (Phila Pa 1976). 1995;20(19):2109–2111. doi: 10.1097/00007632-199510000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Zhu K, Devine A, Dick IM, Prince RL. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine (Phila Pa 1976). 2007;32(18):2012–2018. doi: 10.1097/BRS.0b013e318133fb82. [DOI] [PubMed] [Google Scholar]
- 19.Docking RE, Fleming J, Brayne C, et al. The relationship between back pain and mortality in older adults varies with disability and gender: results from the Cambridge City over-75s Cohort (CC75C) study. Eur J Pain. 2015;19(4):466–472. doi: 10.1002/ejp.568. [DOI] [PubMed] [Google Scholar]
- 20.Roseen EJ, LaValley MP, Li S, et al. Association of Back Pain with All-Cause and Cause-Specific Mortality Among Older Women: a Cohort Study. J Gen Intern Med. 2019;34(1):90–97. doi: 10.1007/s11606-018-4680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144(6):427–437. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- 23.Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 24.Johnson WD, Semaan S, Hedges LV, Ramirez G, Mullen PD, Sogolow E. A protocol for the analytical aspects of a systematic review of HIV prevention research. J Acquir Immune Defic Syndr. 2002;30(Suppl 1):S62–72. doi: 10.1097/00042560-200207011-00007. [DOI] [PubMed] [Google Scholar]
- 25.Borenstein M. Effect sizes for continuous data. In: Cooper H HL, Valentine JC,, ed. The Handbook of Research Synthesis and Meta-analysis. New York, NY: Russell Sage Foundation; 2009:221-235.
- 26.Rothman EF, McNaughton Reyes L, Johnson RM, LaValley M. Does the alcohol make them do it? Dating violence perpetration and drinking among youth. Epidemiol Rev. 2012;34:103–119. doi: 10.1093/epirev/mxr027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobs JM, Hammerman-Rosenberg R, Stessman J. Longevity and chronic back pain in older people. J Am Geriatr Soc. 2005;53(9):1636–1637. doi: 10.1111/j.1532-5415.2005.53487_5.x. [DOI] [PubMed] [Google Scholar]
- 30.Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PLoS One. 2017;12(6):e0178621. doi: 10.1371/journal.pone.0178621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith D, Wilkie R, Uthman O, Jordan JL, McBeth J. Chronic pain and mortality: a systematic review. PLoS One. 2014;9(6):e99048. doi: 10.1371/journal.pone.0099048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asberg AN, Hagen K, Stovner LJ, Heuch I, Zwart JA, Winsvold BS. Do incident musculoskeletal complaints influence mortality? The Nord-Trondelag Health study. PLoS One. 2018;13(9):e0203925. [DOI] [PMC free article] [PubMed]
- 33.Hochberg MC. Mortality in osteoarthritis. Clin Exp Rheumatol. 2008;26(5 Suppl 51):S120–124. [PubMed] [Google Scholar]
- 34.Wilkie R, Parmar SS, Blagojevic-Bucknall M, et al. Reasons why osteoarthritis predicts mortality: path analysis within a Cox proportional hazards model. RMD Open. 2019;5(2):e001048. doi: 10.1136/rmdopen-2019-001048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiner DK, Marcum Z, Rodriguez E. Deconstructing Chronic Low Back Pain in Older Adults: Summary Recommendations. Pain Med. 2016;17(12):2238–2246. doi: 10.1093/pm/pnw267. [DOI] [PubMed] [Google Scholar]
- 36.Smith D, Wilkie R, Croft P, McBeth J. Pain and Mortality in Older Adults: The Influence of Pain Phenotype. Arthritis Care Res (Hoboken). 2018;70(2):236–243. doi: 10.1002/acr.23268. [DOI] [PubMed] [Google Scholar]
- 37.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159(11):1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 38.Weiner DK, Haggerty CL, Kritchevsky SB, et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the Health ABC Cohort and implications for the future. Pain Med. 2003;4(4):311–320. doi: 10.1111/j.1526-4637.2003.03042.x. [DOI] [PubMed] [Google Scholar]
- 39.Feeny D, Huguet N, McFarland BH, Kaplan MS, Orpana H, Eckstrom E. Hearing, mobility, and pain predict mortality: a longitudinal population-based study. J Clin Epidemiol. 2012;65(7):764–777. doi: 10.1016/j.jclinepi.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith D, Wilkie R, Croft P, Parmar S, McBeth J. Pain and mortality: mechanisms for a relationship. Pain. 2018;159(6):1112–1118. doi: 10.1097/j.pain.0000000000001193. [DOI] [PubMed] [Google Scholar]
- 41.Oliveira CB, Maher CG, Franco MR, et al. Co-occurrence of Chronic Musculoskeletal Pain and Cardiovascular Diseases: A Systematic Review with Meta-analysis. Pain Med. 2020;21(6):1106–1121. doi: 10.1093/pm/pnz217. [DOI] [PubMed] [Google Scholar]
- 42.Tesarz J, Eich W, Baumeister D, Kohlmann T, D’Agostino R, Schuster AK. Widespread pain is a risk factor for cardiovascular mortality: results from the Framingham Heart Study. Eur Heart J. 2019;40(20):1609–1617. doi: 10.1093/eurheartj/ehz111. [DOI] [PubMed] [Google Scholar]
- 43.Makris UE, Paul TM, Holt NE, et al. The Relationship Among Neuromuscular Impairments, Chronic Back Pain, and Mobility in Older Adults. PM R. 2016;8(8):738–747. doi: 10.1016/j.pmrj.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leveille SG, Jones RN, Kiely DK, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302(20):2214–2221. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hartholt KA, Lee R, Burns ER, van Beeck EF. Mortality From Falls Among US Adults Aged 75 Years or Older, 2000-2016. JAMA. 2019;321(21):2131–2133. doi: 10.1001/jama.2019.4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu-Ambrose T, Davis JC, Best JR, et al. Effect of a Home-Based Exercise Program on Subsequent Falls Among Community-Dwelling High-Risk Older Adults After a Fall: A Randomized Clinical Trial. JAMA. 2019;321(21):2092–2100. doi: 10.1001/jama.2019.5795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Trivedi MH. The link between depression and physical symptoms. Prim Care Companion J Clin Psychiatry. 2004;6(Suppl 1):12–16. [PMC free article] [PubMed] [Google Scholar]
- 48.Penttinen J. Back pain and risk of suicide among Finnish farmers. Am J Public Health. 1995;85(10):1452–1453. doi: 10.2105/AJPH.85.10.1452-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ilgen MA, Kleinberg F, Ignacio RV, et al. Noncancer pain conditions and risk of suicide. JAMA Psychiatry. 2013;70(7):692–697. doi: 10.1001/jamapsychiatry.2013.908. [DOI] [PubMed] [Google Scholar]
- 50.Bohnert ASB, Ilgen MA. Understanding Links among Opioid Use, Overdose, and Suicide. N Engl J Med. 2019;380(1):71–79. doi: 10.1056/NEJMra1802148. [DOI] [PubMed] [Google Scholar]
- 51.Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 52.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 53.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–691. doi: 10.1001/archinternmed.2011.117. [DOI] [PubMed] [Google Scholar]
- 54.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.7326/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of Long-Acting Opioids and Mortality in Patients With Chronic Noncancer Pain. JAMA. 2016;315(22):2415–2423. doi: 10.1001/jama.2016.7789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stokes A, Berry KM, Hempstead K, Lundberg DJ, Neogi T. Trends in Prescription Analgesic Use Among Adults With Musculoskeletal Conditions in the United States, 1999-2016. JAMA Netw Open. 2019;2(12):e1917228. doi: 10.1001/jamanetworkopen.2019.17228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Trelle S, Reichenbach S, Wandel S, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ. 2011;342:c7086. doi: 10.1136/bmj.c7086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011;8(9):e1001098. doi: 10.1371/journal.pmed.1001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Antman EM, Bennett JS, Daugherty A, et al. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115(12):1634–1642. doi: 10.1161/CIRCULATIONAHA.106.181424. [DOI] [PubMed] [Google Scholar]
- 60.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Clinical Guidelines Committee of the American College of P. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 44 kb)