Abstract
Despite the availability of a prophylactic vaccine, chronic hepatitis B (CHB) caused by the hepatitis B virus (HBV) is a major health problem affecting an estimated 292 million people globally. Current therapeutic goals are to achieve functional cure characterized by HBsAg seroclearance and the absence of HBV-DNA after treatment cessation. However, at present, functional cure is thought to be complicated due to the presence of covalently closed circular DNA (cccDNA) and integrated HBV-DNA. Even if the episomal cccDNA is silenced or eliminated, it remains unclear how important the high level of HBsAg that is expressed from integrated HBV DNA is for the pathology. To identify therapies that could bring about high rates of functional cure, in-depth knowledge of the virus’ biology is imperative to pinpoint mechanisms for novel therapeutic targets. The viral proteins and the episomal cccDNA are considered integral for the control and maintenance of the HBV life cycle and through direct interaction with the host proteome they help create the most optimal environment for the virus whilst avoiding immune detection. New HBV-host protein interactions are continuously being identified. Unfortunately, a compendium of the most recent information is lacking and an interactome is unavailable. This article provides a comprehensive review of the virus-host relationship from viral entry to release, as well as an interactome of cccDNA, HBc, and HBx.
Keywords: hepatitis B virus, interactome, viral-host life cycle, cccDNA, HBx, HBc
Introduction
Hepatitis B virus (HBV) is a member of the Hepadnaviridae family which is transmitted via bodily fluids as well as by vertical transmission (Davis et al., 1989; Schweitzer et al., 2015). The outcome of HBV infection is determined by multiple host and viral factors, and determines whether the infection will be acute, chronic, or occult (Fanning et al., 2019). Despite the availability of a prophylactic vaccine and potent antiviral treatments, chronic hepatitis B (CHB) infection affects 292 million individuals worldwide (Lazarus et al., 2018). The current standard of care is treatment with nucleos(t)ide analogs (NUCs) (i.e., lamivudine, adefovir, entecavir, telbivudine, and tenofovir), that inhibit the HBV polymerase reverse transcription (Liang et al., 2015). These therapies lead to suppression of viral replication, visible by a decrease in viral load, the normalization of serum alanine transaminase and improvement of liver histology (Bitton Alaluf and Shlomai, 2016). However, even prolonged treatment with NUCs rarely results (<10%) in functional cure of CHB and most often leads to virological relapse after treatment cessation (Liang et al., 2015; Kim, 2018).
Also pegylated interferon alpha (peg-IFNα) is approved for use in CHB patients although it is not the preferred therapy due to the occurrence of side effects. Furthermore, it is counter indicated for some patients such as those with liver cirrhosis (Saracco et al., 1994).
Untreated or off-treatment chronic patients are at risk to develop life threatening conditions such as fibrosis, cirrhosis, liver failure, and hepatocellular carcinoma (HCC). In 2015, 887,000 people died from HBV-related cirrhosis and liver cancer alone (WHO, 2017). The ultimate therapeutic goal in CHB is preventing these life-limiting outcomes and to achieve a functional cure characterized by the loss of surface antigen (HBsAg) and HBV-DNA in the blood off-treatment.
Hepatitis B virus functional cure will be achieved when the high viral load, the antigen burden and inadequate host immune responses are overcome and thus may need a broader therapeutic approach involving multiple targets, both viral and host. With regard to the latter, in-depth knowledge of the HBV life cycle is indispensable for identifying mechanisms, that are targetable with new therapeutics.
Part of the therapeutic approach may be to target the interface between viral proteins and cellular targets. The HBV viral proteins have pluripotent functions and our understanding of how they interact with host proteins is continuously evolving. The interactions of these viral factors with the host cell proteome are complex and helps to shape the cellular environment for the virus to replicate. In addition, cccDNA, the template of all viral mRNAs, behaves as a minichromosome and attracts a multitude of protein partners. However, all these reported interactions are scattered in literature, and currently there is no overview bringing together the interactome of HBV. This review aims to provide such an overview, from entry to viral release, it summarizes the known interactions between viral proteins and host proteins. Because cccDNA, HBc, and HBx have been described in many interactions, we focused the construction of an interactome network around these three entities.
Interactions During the Early Phases of HBV Infection
The HBV particle consists of an incomplete 3.2 kb double-stranded (ds)DNA genome [relaxed circular DNA (RC-DNA)] packaged together with the viral polymerase in an icosahedral capsid assembled by HBV core (HBc) proteins (Summers et al., 1975). This nucleocapsid is enveloped by a lipid membrane studded with three forms of HBV surface antigen protein (collectively referred to as HBsAg) to compose the virus or Dane particle [reviewed by Bruss (2004)].
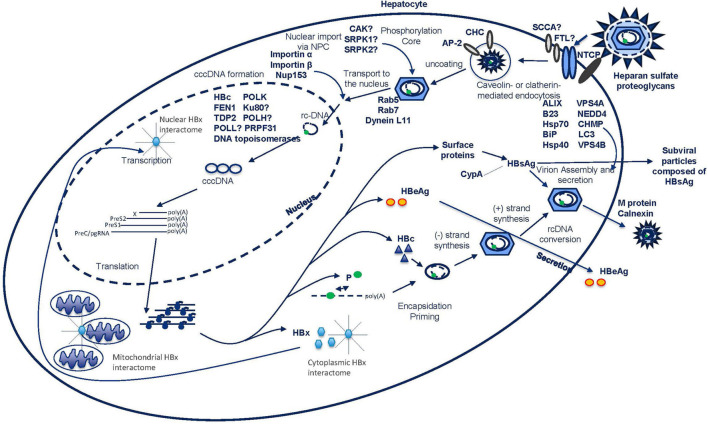
The life cycle of HBV begins upon its interaction with heparan sulfate proteoglycans (HSPGs) and subsequent binding to the sodium taurocholate co-transporting polypeptide (NTCP) receptor on the surface of the hepatocyte (Watashi et al., 2014; Yan et al., 2014; Figure 1). The interaction between virus and cell induces conformational changes of the membrane embedded myristoylated N-terminal preS1-domain of the viral large surface protein (L-HBsAg) leading to exposure of the receptor binding site for the NTCP receptor, which enables binding of the virus and entrance into the cell (Schulze et al., 2007, 2010; Yan et al., 2012, 2013, 2014; Nkongolo et al., 2014; Watashi et al., 2014). Recently, a crucial role in mediating HBV-NTCP internalization of epidermal growth factor receptor (EGFR) was published (Iwamoto et al., 2019). Besides the NTCP receptor, squamous cell carcinoma antigen 1 (SCCA1) and ferritin light chain (FTL) have also been identified as HBV co-receptors (Figure 1). Triple complexes of preS1, FTL, and SCCA1 were observed and overexpression assays with these proteins showed increased infection rates both in vitro and in vivo (Hao et al., 2012). The prevention of entry has been of interest as an antiviral target to circumvent viral spread by blocking de novo infection. In recent years molecules such as Myrcludex B (also known as bulevirtide), ezetimibe, cyclosporin derivates (CsA), and monoclonal antibodies against HBsAg epitopes were identified to interfere with this process (Gripon et al., 2005; Lucifora et al., 2013; Shimura et al., 2017).
FIGURE 1.
HBV life cycle from viral entry to release.
The virus enters the cell by inducing endocytosis via caveolin-mediated endocytosis or via clathrin-mediated pathways (Macovei et al., 2010; Umetsu et al., 2018; Figure 1). In differentiated HepaRG cells, HBV infection has shown to be dependent on caveolin-mediated endocytosis. However, in Umetsu et al. (2018), the formation of a complex between the L-HBsAg, the clathrin heavy chain (CHC) and the clathrin adaptor protein-2 (AP-2) was described, suggesting an alternative endocytosis pathway (Figure 1). Indeed, inhibition of the clathrin-mediated pathway by silibinin and chlorpromazine has been reported to impair HBV uptake (Huang et al., 2012). Further work will be needed to understand the relative importance of these two pathways. After endocytosis, subsequent movement of the virus through the endocytic pathway is regulated by Rab proteins. These are guanosine triphosphatases (GTPases) that occupy specific endocytic compartments and direct endocytic vesicles to different cellular compartments. Silencing of Rab5 or Rab7, in contrast with Rab9 and Rab11, resulted in the inhibition of the early stages of HBV infection implying that the transport of virus to late endosomes is important for a successful infection (Macovei et al., 2013; Figure 1).
The precise location and timing of nucleocapsid release from the envelope remains unclear, but this process is required prior to nuclear entry. Transport of the nucleocapsid to the nucleus is facilitated by the microtubule network and the dynein L11 motor proteins through a direct interaction with the capsid (Osseman et al., 2018; Figure 1). In the nucleocapsid “uncoating” process, phosphorylation of the C-terminus of HBc destabilizes the capsid and allows the binding of importins α and β (Kann et al., 1999; Barrasa et al., 2001; Nguyen et al., 2008). Although a direct interaction has not been established, a number of kinases including core associated kinase (CAK), SR protein-specific kinase 1 (SRPK1) and SR protein-specific kinase 2 (SRPK2), have been reported to be involved in this phosphorylation process (Kau and Ting, 1998; Daub et al., 2002; Figure 1).
Once the nucleocapsid arrives at the nuclear pore complex (NPC), it can pass the complex as an intact particle (Pante and Kann, 2002; Fay and Pante, 2015). Interestingly, HBV seems to utilize a unique way of triaging immature from mature capsids at the level of the NPC as only mature capsids disassemble. In this process, importin β and Nup153 play a role via direct interaction with the capsid (Schmitz et al., 2010; Figure 1). Once through the NPC, the capsid is deposited in the nuclear basket where only mature capsids can pass. In the nucleus, the final uncoating, where capsid structures and viral DNA separate, takes place in an importin α and β-dependent manner (Gallucci and Kann, 2017).
The cccDNA Minichromosome
Once inside the nucleus, the RC-DNA is converted into cccDNA (Summers et al., 1975; Tuttleman et al., 1986; Wu et al., 1990; Lieberman, 2016). Early research using duck hepatitis B virus (DHBV) showed that the cccDNA was in fact organized as a minichromosome similar to host chromatin and SV40 (Newbold et al., 1995). Further DHBV studies showed that in vitro between 1 and 56 copies cccDNA reside in the nuclei of infected cells (Kock et al., 2010). These copy numbers were slightly lower (1–17 copies/cell) in in vivo studies in ducks. Further it was determined that the half-life of DHBV cccDNA is between 35 and 57 days (Addison et al., 2002; Zhang et al., 2003) although shorter half-lives have described (Tuttleman et al., 1986; Wu et al., 1990; Newbold et al., 1995). In vitro kinetic studies were also done using HBV, cccDNA formation is an early life cycle event (Tuttleman et al., 1986) and it was shown that the cccDNA pool grows over the course of 3 days after which a stable pool is reached (5–12 copies/cell) with a half-life of about 40 days (Ko et al., 2014). Similar findings were done using woodchuck HBV (Dandri et al., 2000). Patient samples of HBV infected individuals showed that cccDNA copy numbers were much lower in vivo ranging from 0.01 to 9 copies/cell but at the same time had a much longer half-life of months to a year (Werle-Lapostolle et al., 2004; Bourne et al., 2007; Boyd et al., 2016; Huang et al., 2021). Interestingly, the size and half-life of the cccDNA pool in patients has been suggested to depend on the antigen status (Lythgoe et al., 2021) as much more cccDNA has been shown in HBeAg positive patients while only 0.002 copies/cell were observed in patients that showed HBsAg seroclearance (Werle-Lapostolle et al., 2004).
The cccDNA genome is transcribed to different viral RNAs coding for HBx (0.7-kb RNA), three forms of HBsAg (2.4-kb RNA encoding the large and 2.1-kb RNA encoding the middle and small HBsAg), pre-core protein or HBeAg (3.5-kb RNA) and the core and polymerase protein (pre-genomic RNA or pgRNA, 3.5-kb). This pgRNA also becomes incorporated in the nucleocapsid thereby providing the template for the viral polymerase to produce RC-DNA.
Host Factors Involved in cccDNA Formation
Little is known about the host factors involved in the formation of the cccDNA. The L-HBsAg is not directly involved in cccDNA formation, but is part of a negative feedback mechanism in which high levels of surface protein shut down nuclear shuttling of mature nucleocapsids and direct the cell to produce virions instead (Summers et al., 1990). HBc is suggested to be present during the cccDNA formation process (Kock et al., 2010; Schreiner and Nassal, 2017) which is further evidenced by the fact that capsid modifiers inhibit cccDNA formation (Berke et al., 2017).
Several host factors have been reported to interact with HBV cccDNA during its formation and have quite diverse roles. The Flap endonuclease 1 (FEN1), an endonuclease that plays a role in DNA replication and repair, was shown to interact with RC-DNA in the nucleus and additionally could promote cccDNA formation in vitro (Kitamura et al., 2018; Figure 1). The discovery of a protein partner involved in DNA damage repair is coherent with the previous finding that this machinery is exploited by viruses to their own benefit (Schreiner and Nassal, 2017). Ku80, a component of non-homologous end joining DNA repair pathway, was essential for synthesis of cccDNA from dsDNA, but not from RC-DNA (Guo et al., 2012; Figure 1). In these processes, HBx could be an adaptor to link cccDNA formation with DNA damage response pathways, under the assumption that HBx is already present in the cell when cccDNA is being formed (Hodgson et al., 2012; Guo et al., 2014; Murphy et al., 2016; Niu C. et al., 2017). The link with the host DNA damage and repair machinery does not end with this interaction, the tyrosyl-DNA-phosphodiesterase (TDP2) also plays a partial role in cccDNA formation by releasing the viral transcriptase from the RC-DNA (Koniger et al., 2014; Cui et al., 2015; Figure 1). The host DNA polymerases K (POLK), H (POLH), and L (POLL) have all been reported to have a positive impact on cccDNA formation, however, the exact mechanism(s) is (are) not yet clear (Qi et al., 2016; Figure 1). In addition to DNA polymerases, knockout experiments showed the importance of cellular DNA ligase 1 and 2 in cccDNA formation (Long et al., 2017). Recently, it was shown that the plus-strand and the minus-strand require different cellular proteins. The plus-strand repair required proliferating cell nuclear antigen (PCNA), replication factor C (RFC) complex, DNA polymerase delta (POLδ), flap endonuclease 1 (FEN1), and DNA ligase 1 (LIG1) while the repair of the minus-strand only required FEN1 and LIG1 (Wei and Ploss, 2020). Also cellular DNA topoisomerases are required for cccDNA formation and amplification (Sheraz et al., 2019). Finally, pre-mRNA processing factor 31 (PRPF31) was identified as a cccDNA-associating factor involved in cccDNA formation (Kinoshita et al., 2017; Figure 1).
The Interactome of the cccDNA
Similar to a cellular chromosome, the cccDNA is bound to histones to form a minichromosome. These host-derived histones (H2A, H2B, H3, and H4) provide, together with the viral HBc, the stable scaffold for the cccDNA to be supercoiled (Newbold et al., 1995; Chong et al., 2017). That being said, the role of HBc in both cccDNA formation and maintenance is still under investigation. For example, despite their involvement in several processes regarding cccDNA formation, maintenance and transcription, capsid modifying compounds do not eliminate the cccDNA pool (Berke et al., 2017) nor is HBc essential for transcription (Zhang et al., 2014).
On the cccDNA of Duck hepatitis B virus (DHBV), nucleosomes are non-randomly positioned, suggesting that, like host cellular chromatin, positioning of the nucleosomes and histone modifications of the cccDNA may regulate cccDNA transcription (Bock et al., 1994; Pollicino et al., 2006). Methylation, acetylation, phosphorylation or other posttranslational modifications (PTMs) of these cccDNA-bound histone tails can fine tune the gene expression by altering the chromatin structure (Tropberger et al., 2015). This change in structure can wind the chromatin more tightly to prevent access of transcription factors and repress gene transcription. On the other hand, histone modifications can also result in increased DNA accessibility, transcription factor binding and therefore promoting gene activation (Li et al., 2007; Voss and Hager, 2014). In addition, the minichromosome attracts several other partners, many of which are transcription factors that further determine whether the cccDNA is transcriptionally active or inactive (Table 1).
TABLE 1.
List of known protein-cccDNA interactions associated with increased or decreased transcriptional regulation.
| cccDNA minichromosome partner | Process | References |
| Associated with Enhanced Replication – Verified Interactions | ||
| HBx | Required for replication and transcription. | Belloni et al., 2009 |
| HBc | HBc binds to the CpG islands of HBV cccDNA. | Guo et al., 2011 |
| CBP | HBx interacts and cooperates with CBP to modify chromatin dynamics and enhances CREB activity. | Pollicino et al., 2006; Belloni et al., 2009 |
| P300 | HBx increases amount of P300 recruited to promotors. | Belloni et al., 2009 |
| PCAF | Recruited to the cccDNA after HBx binding to the minichromosome. | Belloni et al., 2009 |
| LSD1/KDM1A | Recruited in an HBx-dependent manner, induces HBV replication and HBV transcription involves the demethylation of histone 3 lysine 9 (H3K9). | Alarcon et al., 2016 |
| CREB/CREB1 | Essential for HBV replication. It binds to the cAMP response elements (CREs) located at the X and preS2 promoters. Interaction with cccDNA dependent on CRTC1. | Tacke et al., 2005; Kim B.K. et al., 2008; Tang et al., 2014) |
| STAT1 | Binds to cccDNA, binding impaired upon IFN treatment. | Belloni et al., 2012 |
| STAT2 | Binds to cccDNA, binding impaired upon IFN treatment. | Belloni et al., 2012 |
| STAT3 | May bind to enhancer I (ENI) and increase function. | Quarleri, 2014 |
| Set1A/SETD1A | Recruited via a HBx-dependent manner, stimulates an active cccDNA epigenetic state by methylating histone 3 lysine 4 (H3K4) in viral HBV promoters. | Alarcon et al., 2016 |
| CRTC1 | Recruited to the preS2/S promotor for the activation of replication. Interaction with cccDNA dependent on CREB/CREB1. | Tang et al., 2014 |
| KLF15 | Activates S and HBc promotors and enhances replication when overexpressed. | Zhou et al., 2011 |
| SIRT1 | SIRT1 interacts with HBx and promotes the recruitment of HBx and other transcriptional factors to the cccDNA (specifically to the precore promoter), promoting the activation of HBV transcription (Deng et al., 2017). However, after IFNα treatment, SIRT1 is recruited to the cccDNA to repress transcription. | Belloni et al., 2012 |
| RFX1 | Binds the enhancer region upon doxorubicin treatment to promote replication. | Wang et al., 2018 |
| RXRα | RXRα recruitment to the cccDNA in parallel with P300 recruitment | Zhang Y. et al., 2017 |
| SP1 | Several binding sites, depending on the site, the activity of SP1 is enhancing or inhibitory. | Quasdorff and Protzer, 2010 |
| TBP | Binds the TATA box. | Quasdorff and Protzer, 2010 |
| NRF1 | Binds to the HBx promotor and positively regulates HBx transcription | Quasdorff and Protzer, 2010 |
| C/EBP | Binds enhancer II (EnhII) and the HBc promotor. Low concentrations have a positive effect on replication while high concentrations evoke inhibition. Potentially also a repressor role. | Pei and Shih, 1990; Quasdorff and Protzer, 2010 |
| PPAR | Increases transcription from several promotors. | Quasdorff and Protzer, 2010 |
| FXR/NR1H4 | Can bind EnhII and HBc regions to have a stimulating effect on transcription. | Quasdorff and Protzer, 2010 |
| AP1 | Binding to HBc promotor and shown to work in synergy with SIRT and HBx. | Quasdorff and Protzer, 2010; Ren et al., 2014 |
| HNF1/HNF1A | Binding sites on the preS promotor. HNF1/HNF1A synergistically works with Oct1 and LRH-1/NR5A2 to enhance replication. | Zhou and Yen, 1991; Cai et al., 2003 |
| LRH-1 (NR5A2)/hB1F | Transactivator of the EnhII and HBc regions. Synergy with HNF1/HNF1A. | Cai et al., 2003; Quasdorff and Protzer, 2010 |
| HNF3 | Several binding sites identified, binding seems to be associated with a stimulating effect. | Cai et al., 2003; Quasdorff and Protzer, 2010 |
| HNF4/HNF4A | Stimulation of transcription from several promotors. | Cai et al., 2003; Quasdorff and Protzer, 2010 |
| HLF | Stimulatory effect on the HBc regulatory region. | Ishida et al., 2000 |
| FTF | Stimulatory effect on EnhII. | Ishida et al., 2000 |
| Parvulin 14 | Recruited to cccDNA in the presence of HBx to promote transcriptional activation. | Saeed et al., 2018 |
| Parvulin 17 | Recruited to cccDNA in the presence of HBx to promote transcriptional activation. | Saeed et al., 2018 |
| Activation-induced cytidine deaminase (AID) | Interaction enhances cccDNA transcription. | Qiao et al., 2016 |
| P19 | Interaction enhances cccDNA transcription. | Qiao et al., 2016 |
| Associated with enhanced Replication – Potential Interactions | ||
| CRTC2 | Enhances HBV transcription and replication by inducing PGC1α expression. | Tian et al., 2014 |
| PGC1α | Induction of HBV transcription, potentially via FOXO1. | Quasdorff and Protzer, 2010; Tian et al., 2014 |
| NF1 | Three binding sites on HBV genome. | Ori et al., 1994; Quasdorff and Protzer, 2010 |
| Oct1 | Oct-1 and HNF-1 sites are necessary for liver-specific transcription of the preS1 promoter. | Zhou and Yen, 1991 |
| EFC | Binding site identified in central HBc promotor. | Quarleri, 2014 |
| Associated with supressed Replication – Verified Interactions | ||
| HDAC1 | Correlated with decline in replication. | Belloni et al., 2009; Levrero et al., 2009 |
| Actively recruited to the cccDNA under IFNα-treatment to repress transcription. | Belloni et al., 2012 | |
| YY1 | Part of the transcriptional repressor complex PRC2. Actively recruited to the cccDNA under IFNα treatment to repress transcription. | Belloni et al., 2012 |
| SETDB1 | Repressing histone deacetylase. | Riviere et al., 2015; Alarcon et al., 2016 |
| EZH2 | Repression of cccDNA. | Salerno et al., 2020 |
| HP1/CBX1 | HP1/CBX1 proteins are recruited to the cccDNA through interaction with H3K9me3 and contribute to transcriptional repression. | Riviere et al., 2015 |
| Spindlin 1/SPIN1 | Inhibition of transcription from the cccDNA via epigenetic modulation. | Ducroux et al., 2014 |
| APOBEC3G | May contribute to cccDNA editing. Antiviral effect through DNA and RNA packaging. | Nguyen et al., 2007; Luo et al., 2016 |
| SP1 | Several binding sites, depending on the site the activity of SP1 is enhancing or inhibitory. | Quasdorff and Protzer, 2010 |
| TR4 | Repressing function by inhibition of HNF4A mediated transactivation. Binds the HBc promotor. | Quasdorff and Protzer, 2010 |
| HNF1/HNF1A | Binding site identified on EnhII. Binding associated with a decline in replication by induction of NF-κB/NFKB1. | Cai et al., 2003; Dai X. et al., 2014; Lin et al., 2017 |
| HNF6 | Inhibits gene expression and replication. | Hao et al., 2015 |
| COUP-TF/NH2F1 | Overexpression of COUP-TF/NH2F1 led to a decrease in replication via binding on NRRE in the enhancer and HBc regions. | Yu and Mertz, 2003 |
| PRMT5 | PRMT5-mediated histone H4 dimethyl Arg3 (H4R3me2) repressed cccDNA transcription. PRMT5-H4R3me2 interacted with HBc and the Brg1-based hSWI/SNF chromatin remodeler, which accounted for the reduced binding of RNA polymerase II to cccDNA. | Zhang W. et al., 2017 |
| E4BP4/NFIL3 | Associated with suppression of EnhII. | Ishida et al., 2000 |
| NREBP | Inhibits core promotor activity by binding the NRE. Binding is inhibited by HBx. | Lee et al., 2019 |
| ZHX2 | Restriction factor that regulates HBV promoter activities and cccDNA modifications. | Xu et al., 2018 |
| Associated with supressed Replication – Potential Interactions | ||
| Prox1 | Interacts with LRH-1/NR5A2 and downregulates LRH-1/NR5A2 mediated activation. | Quasdorff and Protzer, 2010 |
| APOBEC3A | Upregulation by IFNα and lymphotoxin-β receptor resulted in cytidine deamination, | Lucifora et al., 2014 |
| apurinic/apyrimidinic site formation and finally cccDNA degradation. | ||
| APOBEC3B | Upregulation by IFNα and lymphotoxin-β receptor resulted in cytidine deamination, | Lucifora et al., 2014 |
| apurinic/apyrimidinic site formation and finally cccDNA degradation. | ||
| SIRT 3 | Mediates cccDNA transcription. Repression lifted by HBx. | Ren et al., 2018 |
Verified interactions are those protein-protein interactions that were identified using proteomics methods such as pull downs or yeast-2-hybrid. Potential interactions are those which have been shown using methods that strongly suggest an interaction (e.g., co-localization) but were not verified using pull-down methods.
As previously mentioned, HBx and HBc proteins are bound to cccDNA. HBc has been described to modulate transcription from the cccDNA. Zlotnick et al. showed that the presence of HBc on a CpG island in the cccDNA can be linked to increased cccDNA activity, while methylation of the CpG island correlated with decreased cccDNA activity (Zlotnick et al., 2015). In addition, the presence of HBc appears to have a role in the maintenance of the structure of the cccDNA (Bock et al., 2001). Together these data suggest that HBc contributes to the epigenetic regulation of the cccDNA, which in turn contributes to its longevity.
Modalities Acting on cccDNA
A role in viral rebound made cccDNA a target for new antiviral drug development. Success of such tactics relies on complete inhibition of cccDNA throughout the lifespan of the hepatocyte. A first approach is to target the formation of cccDNA, although it can be questioned how much benefit CHB patients will have of such a therapy in the event the cccDNA does not become reduced. Several molecules reported to act through this mechanism have been described in literature. However, to date, these molecules have either been stopped at pre-clinical stage or did not progress far in clinical trials (Cai et al., 2012; Liu et al., 2016). The only assets which encompass this capacity and are still under clinical investigation are the entry inhibitor bulevirtide and capsid assembly modulators. The latter are small molecules that accelerate capsid formation but turned out to have a dual mode of action in preventing cccDNA formation when added in vitro at early stages of infection (Berke et al., 2017; Vandenbossche et al., 2019). Secondly, a number of molecules have been described that silence the cccDNA, either by inhibiting cccDNA transcription [e.g., Tamibarotene (Nkongolo et al., 2019)] or by diminishing HBV RNA levels post-transcription (e.g., RNA destabilizers such as RG7834 (Mueller et al., 2019); RNA interference). Tamibarotene never made it to clinical trials for HBV, while RG7834 was stopped in Phase I. Transcriptional control of cccDNA expression may also be achieved by interfering with the function of HBx, HBc or an interaction partner. An example is the interference between HBx and DNA damage-binding protein 1 (DDB1). HBx was found to hijack DDB1 which in turn recruits the ubiquitylation machinery to send Structural Maintenance of Chromosomes protein 5/6(SMC5/6), a transcriptional repressor of cccDNA, to the proteasome for degradation. Two molecules, pevonedistat, a NEDD8-activating enzyme inhibitor, and nitazoxanide, a thiazolide anti-infective agent, have been shown to restore SMC5/6 levels and suppress viral transcription (Decorsiere et al., 2016; Sekiba et al., 2019a,b). Recently, epigenetic modifiers that specifically target viral factors involved in the regulation of cccDNA expression have been described and are currently being evaluated. Several selective inhibitors (e.g., C646) for histone acetyltransferase like CBP and P300 have been used to study the inhibitory effect on HBV transcription (Tropberger et al., 2015). The prodrug GS-5801 has also been shown to inhibit transcription from cccDNA by blocking the activity of lysine demethylase 5 (KDM5) (Gilmore et al., 2017). Although these observations show that silencing of HBV transcription is possible, the main throwback of most of these targets is the lack of desired selectivity for cccDNA and their potential to impact cellular processes.
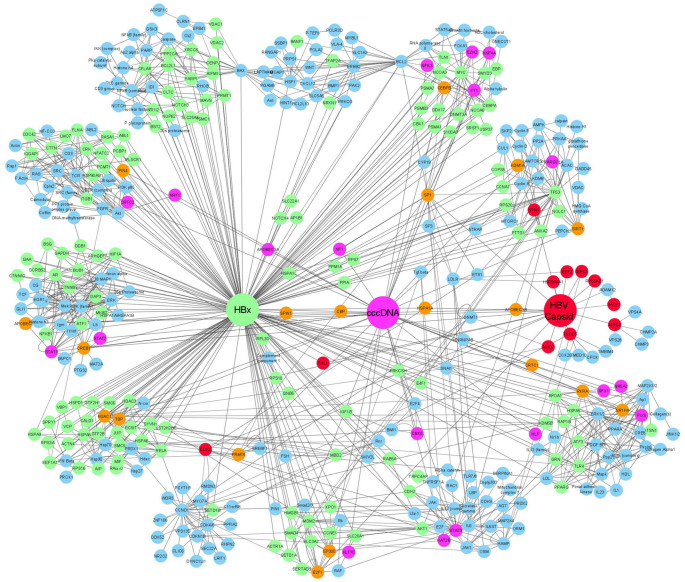
Complete elimination of cccDNA by compromising the stability or the half-life of the molecule is often dubbed the “Holy Grail” of HBV research. Many molecules have been described that phenotypically reduce the quantity or transcription level of cccDNA. Recently, a small molecule, ccc_R08, with an unknown mode of action was shown to decrease the pool of cccDNA together with a decrease in viral transcripts and viral antigens in primary human hepatocytes (PHH) and in an HBV minicircle mouse model (Wang et al., 2019). In most instances, information on the exact mechanism of such molecules is lacking implying a need to conduct target deconvolution studies to identify the respective interaction partner or process. We created a cccDNA network map, not only to visualize the currently known cccDNA interacting proteins but also to be put alongside such exercises (Figure 2).
FIGURE 2.
Gene association network showing the relationship between HBx, HBc, and HBV cccDNA interacting proteins. In the network, proteins which only interact with HBx are indicated in green, proteins which only interact with cccDNA are shown in pink, and proteins that only interact with HBc are shown in red. Proteins that were shown to interact with more than two of the founding nodes (cccDNA, HBc, and HBx) are depicted in orange. proteins that were extrapolated to connect to one or more interacting proteins are shown in blue.
The HBx Interactome
The interactome of HBx extends beyond its interaction with the cccDNA and associated proteins. Besides nuclear interaction partners, HBx also interacts with various proteins in the cytoplasm, the endoplasmic reticulum (ER) and the mitochondria (Henkler et al., 2001; Huh and Siddiqui, 2002; Belloni et al., 2009; Li et al., 2017; Figure 1). This may explain why this small viral protein (17-kDa) is not only involved in HBV replication, but is also shown to contribute to the development of HCC and interfere with cell cycle regulation, glucose metabolism, oxidative stress, calcium signaling, apoptosis and DNA repair (Luber et al., 1993; Waris et al., 2001; Bouchard et al., 2006; Benhenda et al., 2009; Table 2). The pivotal nature of HBx is demonstrated by Table 2 in which more than 250 HBx interaction partners are summarized. However, it does need to be mentioned that some of these interactions may be very weak or very brief and their relevance may be limited.
TABLE 2.
HBx interacting proteins listed together with the cellular processes or pathways in which they are involved.
| Interaction partner | Cellular Process | References |
| RPB5 | Transcriptional machinery | Cheong et al., 1995 |
| TFIIB | Transcriptional machinery | Lin et al., 1997 |
| TBP | Transcriptional machinery | Qadri et al., 1995 |
| TFIIH | Transcriptional machinery | Qadri et al., 2011 |
| CBP | Coactivator | Cougot et al., 2007 |
| P300 | Coactivator | Cougot et al., 2007 |
| PCAF | Coactivator | Chan et al., 2013 |
| ATF/CREB | Transcription factor | Maguire et al., 1991 |
| ATF3 | Transcription factor | Barnabas and Andrisani, 2000 |
| ICERIIgamma | Transcription factor | Barnabas et al., 1997; Barnabas and Andrisani, 2000 |
| gadd153/Chop10 | Transcription factor | Barnabas et al., 1997 |
| c/EBPA | Transcription factor | Choi et al., 1999 |
| NF-IL-6 | Transcription factor | Barnabas et al., 1997 |
| ETS/ERG# | Transcription factor | Qin et al., 2013 |
| EGR/EGRF1 | Transcription factor | Yoo and Lee, 2004 |
| SMAD4 | Transcription factor | Shi et al., 2016 |
| Oct1 | Transcription factor | Antunovic et al., 1993 |
| RXR | Transcription factor | Kong et al., 2000 |
| P53 | Transcription factor. Induces destabilization of HBx. | Belloni et al., 2009; Xian et al., 2010; Iyer and Groopman, 2011 |
| PRMT1 | Relieves PRMT1 suppression from viral replication. | Benhenda et al., 2013 |
| Spindlin1 | Interaction with HBx relieves repression by Spindlin1. Knockdown induced an increase in HBV transcription and H3H4 trimethylation on the cccDNA. | Ducroux et al., 2014 |
| PP1 | HBx interferes with the inactivation of CREB/CREB1 by PP1. | Cougot et al., 2012 |
| JMJD5 | Interaction with HBx facilitates HBV replication through the hydroxylase activity of JMJD5. | Kouwaki et al., 2016 |
| DDB1 | Recruited resulting in SMC5/6 degradation. | Decorsiere et al., 2016 |
| SMC5/6 | Recruited to the ubiquitin machinery to be degraded to enhance transcription. | Decorsiere et al., 2016 |
| hepatocystin | May be an antiviral pathway, hepatocystin seems to accelerate HBx degradation. | Shin et al., 2013 |
| Clathrin heavy chain | Unknown | Shin et al., 2013 |
| HSPA5 | Unknown | Shin et al., 2013 |
| HSPA9 | Unknown | Shin et al., 2013 |
| CALD1 | Unknown | Shin et al., 2013 |
| HSPA8 | Unknown | Shin et al., 2013 |
| XRCC6 | Unknown | Shin et al., 2013 |
| PDIA4 | Unknown | Shin et al., 2013 |
| PRKCSH | Unknown | Shin et al., 2013 |
| HSPA6 | Unknown | Shin et al., 2013 |
| DDX17 | Unknown | Shin et al., 2013 |
| HSPA1L | Unknown | Shin et al., 2013 |
| HSPA1A | Unknown | Shin et al., 2013 |
| SIRT1 | SIRT1 interacts with HBx thereby enabling HBx-induced transcriptional activity cccDNA. | Srisuttee et al., 2012; Deng et al., 2017 |
| Set1A/SETD1A# | Recruited by HBx to cccDNA to increase transcription. | Alarcon et al., 2016 |
| LSD1# | Bound to viral promotors. | Alarcon et al., 2016 |
| CRTC1 | Interaction associated with increased transcription. | Tang et al., 2014 |
| CPAP/CENPJ | Promotes HBx-mediated cell proliferation and migration in a SUMO-dependent manner. | Yang et al., 2013 |
| CREB/CREB1 | Upregulated via HBx-CREB/CREB1 interaction. | Yang et al., 2013 |
| CRM1/XPO1 | Potential activation of CRM1/XPO1 and role in HBx-mediated carcinogenesis. | Forgues et al., 2001 |
| NFκB# | Relocalization via NES motif. | Forgues et al., 2001 |
| VISA/MAVs | Disruption of VISA/MAVs and downstream interacting proteins thereby impairing IFN signaling. | Wang X. et al., 2010 |
| MDA5 | Impairment of IFN signaling. | Wang X. et al., 2010 |
| GRP78 | Role in HCC via suppression of eIF2α phosphorylation, inhibited expression of ATF4/CHOP/Bcl-2, and reduced cleavage of PARP. | Li et al., 2017 |
| AKT1 | Cell proliferation, abrogation of apoptosis and tumorigenic transformation of cells. | Khattar et al., 2012 |
| Bcl-2 | Management of calcium levels to benefit viral replication. | Geng et al., 2012 |
| BCL2L1 | Management of calcium levels to benefit viral replication. | Geng et al., 2012 |
| HDAC1 | Repression insulin-like growth factor binding protein-3. HBx also induces HDAC1. | Pollicino et al., 2006; Yoo et al., 2008; Shon et al., 2009 |
| SP1# | HBx induces deacetylation of SP1. | Pollicino et al., 2006; Yoo et al., 2008; Shon et al., 2009 |
| HIF1a | HBx aids the MTA1/HDAC complex in stabilizing HIF1a. | Yoo et al., 2008 |
| USP-15 | USP-15 mediated deubiquitylation protects HBx from proteasomal degradation. | Su et al., 2017 |
| PARP1 | DNA damage and repair, carcinogenesis. | Na et al., 2016 |
| Cardiolipin (lipid) | Mitochondrial membrane permeabilization. | You et al., 2019 |
| Prdx1 | Peroxiredoxin interfaces with HBV-RNA to promote RNA decay, potentially HBx rescues this event. | Deng et al., 2018, 2019 |
| Parvulin 14/PIN4 | Interaction with HBx in nucleus, cytoplasm and mitochondria to enhance HBx stability, translocation to the nucleus and mitochondria to increase HBV replication. | Saeed et al., 2018 |
| Parvulin 17 | Interaction with HBx in nucleus, cytoplasm and mitochondria to enhance HBx stability, translocation to the nucleus and mitochondria to increase HBV replication. | Saeed et al., 2018 |
| 14-3-3ζ | Interaction found in HCC cells, involvement of AKT pathway. | Tang et al., 2018 |
| c-myc | Oncogenesis | Lee et al., 2016 |
| Orail protein | Calcium metabolism | Yao et al., 2018 |
| HMGB1 | Autophagy | Fu et al., 2018 |
| FXR/NR1H4 | Transactivation FXR/NR1H4, oncogenesis | Niu Y. et al., 2017 |
| PP2Ac/PP2CA | Cell cycle and apoptosis | Gong et al., 2016 |
| SMYD3 | Involved in AP1 activation | Hayashi et al., 2016 |
| P62 | Glucose metabolism | Liu B. et al., 2015 |
| TLR4 | Tumorigenesis | Wang et al., 2015 |
| BST-2@ | HBV restriction factor | Lv et al., 2015 |
| MBD2 | Involved in epigenetics of histones, potentially in HCC. | Liu X.Y. et al., 2015 |
| TRUSS/TRPC4AP | May be linked to pathological sequelae of HBV. | Jamal et al., 2015 |
| MKI67 | Cell proliferation | Zhang et al., 2015 |
| ENPEP | Cell proliferation | Zhang et al., 2015 |
| MIF | Cell proliferation | Zhang et al., 2015 |
| PYY | Cell proliferation | Zhang et al., 2015 |
| NOLC1 | Cell proliferation | Zhang et al., 2015 |
| CDC42 | Cell adhesion | Zhang et al., 2015 |
| IQGAP1 | Cell adhesion | Zhang et al., 2015 |
| LMO7 | Cell adhesion | Zhang et al., 2015 |
| ACTN4 | Cell adhesion | Zhang et al., 2015 |
| CTNNA2 | Cell adhesion | Zhang et al., 2015 |
| MYH2 | Cell adhesion | Zhang et al., 2015 |
| FILAMIN | Cell adhesion | Zhang et al., 2015 |
| ITGB1 | Cell adhesion | Zhang et al., 2015 |
| TLN1 | Cell adhesion | Zhang et al., 2015 |
| NRXN1 | Cell adhesion | Zhang et al., 2015 |
| CDH2 | Cell migration | Zhang et al., 2015 |
| NOTCH4 | Angiogenesis | Zhang et al., 2015 |
| CTNNB1 | Angiogenesis | Zhang et al., 2015 |
| ANXA2 | Angiogenesis | Zhang et al., 2015 |
| ATP5B | Angiogenesis/cell adhesion | Zhang et al., 2015 |
| PSMC4 | Protein degradation | Zhang et al., 2015 |
| PSMB3 | Protein degradation | Zhang et al., 2015 |
| VDAC1 | Anion transport | Zhang et al., 2015 |
| VDAC2 | Anion transport | Zhang et al., 2015 |
| SLC25A3 | Transport | Zhang et al., 2015 |
| S100A9 | Viral reproduction | Zhang et al., 2015 |
| SLC25A5 | Viral reproduction | Zhang et al., 2015 |
| SLC25A10 | Metabolic process | Zhang et al., 2015 |
| SLC20A1 | Signal transduction | Zhang et al., 2015 |
| SLC3A2 | Immune system process | Zhang et al., 2015 |
| RAP1B | Signal transduction | Zhang et al., 2015 |
| RAB10 | Signal transduction | Zhang et al., 2015 |
| RAB11B | Signal transduction | Zhang et al., 2015 |
| RAB5A | Signal transduction | Zhang et al., 2015 |
| FIS1 | Programmed cell death | Zhang et al., 2015 |
| KIF1B | Programmed cell death | Zhang et al., 2015 |
| DAP3 | Induction of apoptosis | Zhang et al., 2015 |
| VIM | Apoptosis | Zhang et al., 2015 |
| JUP | Cell migration | Zhang et al., 2015 |
| RPS7 | Viral reproduction | Zhang et al., 2015 |
| RPS10 | Viral reproduction | Zhang et al., 2015 |
| RPS16 | Viral reproduction | Zhang et al., 2015 |
| RPS20 | Viral reproduction | Zhang et al., 2015 |
| RPL30 | Viral reproduction | Zhang et al., 2015 |
| RPL38 | Viral reproduction | Zhang et al., 2015 |
| BANF1 | Viral reproduction | Zhang et al., 2015 |
| AP1B1 | Viral reproduction | Zhang et al., 2015 |
| BSG | Immune system process | Zhang et al., 2015 |
| ACTR1A | Cell cycle | Zhang et al., 2015 |
| SRSF1 | mRNA processing | Zhang et al., 2015 |
| DDB1 | Wnt receptor signaling pathway | Zhang et al., 2015 |
| ATP5C1 | Oxidative phosphorylation | Zhang et al., 2015 |
| PCMT1 | Protein methylation | Zhang et al., 2015 |
| PPIA | Viral reproduction | Zhang et al., 2015 |
| HIST2H2BE | Nucleosome assembly | Zhang et al., 2015 |
| PCBP1 | Metabolic process | Zhang et al., 2015 |
| GAPDH | Glycolysis | Zhang et al., 2015 |
| HSP90AB1 | Regulation of signaling pathway | Zhang et al., 2015 |
| COXIII@ | Mitochondrial function | Li et al., 2015; Zou et al., 2015 |
| ECSIT | Involved in IL-1β induction of NF-κB activation. | Chen et al., 2015 |
| Skp2 | Cell cycle deregulation and transformation. | Kalra and Kumar, 2006 |
| PSMA7/XAPC7 | Proteasome | Huang et al., 1996 |
| PSMC1 | Proteasome | Zhang et al., 2000 |
| PSMA1 | Proteasome | Hu et al., 1999 |
| PLSCR1 | Unknown | Yuan et al., 2015 |
| GRN | Unknown | Yuan et al., 2015 |
| SPRY1 | Unknown | Yuan et al., 2015 |
| NKD2 | Unknown | Yuan et al., 2015 |
| SYVN1 | Unknown | Yuan et al., 2015 |
| NOTCH3 | Unknown | Yuan et al., 2015 |
| LAMC3 | Unknown | Yuan et al., 2015 |
| SERTAD1 | Unknown | Yuan et al., 2015 |
| GAA | Unknown | Yuan et al., 2015 |
| USP37 | Cell cycle progression | Saxena and Kumar, 2014 |
| E4F1 | P53-dependent growth arrest | Dai Y. et al., 2014 |
| Pregnane X receptor | Potentially involved in carcinogenesis | Niu et al., 2013 |
| apoA-I | HBV secretion | Zhang et al., 2013 |
| hBubR1/BUB1 | Genomic stability | Chae et al., 2013 |
| c-FLIPL | Apoptosis | Kim and Seong, 2003 |
| c-FLIPS | Apoptosis | Kim and Seong, 2003 |
| AIF | Apoptosis | Liu et al., 2012 |
| AMID | Apoptosis | Liu et al., 2012 |
| AIB1 | NFκB signaling | Hong et al., 2012 |
| eEF1A1 | Actin bundling | Lin et al., 2012 |
| VCP | NFκB signaling | Jiao et al., 2011 |
| RPS3a | NFκB signaling | Lim et al., 2011 |
| Gli1 | Hedgehog signaling | Kim et al., 2011 |
| Phosphor-p65 | NFκB signaling | Shukla et al., 2011 |
| IPS-1 | RIGI signaling | Kumar et al., 2011 |
| C/EBPα | Insulin signaling | Kim K. et al., 2010 |
| PTTG1@ | Tumorigenesis | Molina-Jimenez et al., 2010 |
| Cul1@ | Tumorigenesis | Molina-Jimenez et al., 2010 |
| TNFR1@ | NFκB signaling | Kim J.Y. et al., 2010 |
| Cortactin | Cytoskeletal | Feng et al., 2010 |
| Yes1 | Cell growth and survival, apoptosis, cell-cell adhesion, cytoskeleton remodeling, and differentiation. | Feng et al., 2010 |
| CRK-D2 | Regulates cell adhesion, spreading and migration. | Feng et al., 2010 |
| c-Src | Signal transduction | Feng et al., 2010 |
| Y124 | Unknown | Feng et al., 2010 |
| RasGAP | GTPase, unknown | Feng et al., 2010 |
| Abl | Cell growth and survival, cytoskeleton remodeling in response to extracellular stimuli, cell motility and adhesion, receptor endocytosis, autophagy, DNA damage response and apoptosis. | Feng et al., 2010 |
| ITSN-D1/ITSN1 | Unknown | Feng et al., 2010 |
| Abl2 | Cell growth and survival, cytoskeleton remodeling in response to extracellular stimuli, cell motility and adhesion and receptor endocytosis. | Feng et al., 2010 |
| OSF/OSTF1 | Cell adhesion | Feng et al., 2010 |
| Tec | Cytoskeletal, adaptive immunity | Feng et al., 2010 |
| PIG2/GAMT | Carcinogenesis | Feng et al., 2010 |
| ARH6 | DNA damage | Feng et al., 2010 |
| EFS | Cell adhesion | Feng et al., 2010 |
| RHG4 | Unknown | Feng et al., 2010 |
| VINE-D1 | Cytoskeletal | Feng et al., 2010 |
| VINE-D3 | Cytoskeletal | Feng et al., 2010 |
| HSP72/ASPA1A | Chaperone | Wang et al., 2008 |
| C/EBPbeta | Phase II detoxifying pathways. | Cho et al., 2009 |
| DNMT3A | Epigenetic modifications | Zheng et al., 2009 |
| Bax | Apoptosis | Kim H.J. et al., 2008 |
| VBP1 | NFκB signaling | Kim S.Y. et al., 2008 |
| betaPIX | Rec1 signaling | Tan et al., 2008 |
| HBXIP | Centrosome and spindle formation. | Wen et al., 2008 |
| Pin1 | Carcinogenesis | Pang et al., 2007 |
| AR | Gene expression | Zheng et al., 2007 |
| PP2Calpha | Carcinogenesis | Kim et al., 2006 |
| cyclin E/A | Cell cycle regulation | Mukherji et al., 2007 |
| vinexin-beta | Cytoskeletal organization | Tan et al., 2006 |
| MIF | Apoptosis | Zhang et al., 2006 |
| Jab1/cops5 | AP1 signaling | Tanaka et al., 2006 |
| GNbeta5 | Unknown | Lwa and Chen, 2005 |
| p120E4F | Mitosis and cell cycle | Rui et al., 2006 |
| Hepsin | Apoptosis | Zhang et al., 2005 |
| Hsp60 | Apoptosis | Tanaka et al., 2004 |
| PPARgamma | Apoptosis | Choi et al., 2004 |
| ASC-2 | Carcinogenesis | Kong et al., 2003 |
| E2F1 | Carcinogenesis | Choi et al., 2002 |
| NF-AT1/NFATC2 | Calcium metabolism | Carretero et al., 2002 |
| Tbp1 | Transcription | Barak et al., 2001 |
| NF-IL6 | IL6 signaling | Ohno et al., 1999 |
| Jak1 | JAK/STAT signaling | Lee and Yun, 1998 |
| XAP-1/UVDDB/DDB1 | DNA damage repair, carcinogenesis. | Becker et al., 1998 |
| RPB5 | Transcription | Lin et al., 1997 |
| HVDAC3/HDAC3@ | HBx colocalized with HVDAC3/HDAC3 at the mitochondria. | Rahmani et al., 2000 |
| AP2α# | HBx modulates SPHK1 via AP2α. | Lu et al., 2015 |
| SetDB1# | HBx relieves SETDB1-mediated H3K9me3 induced silencing of cccDNA. | Riviere et al., 2015 |
| HP1/CBX1# | HBx relieves HP1/CBX1 induced silencing of cccDNA. | Riviere et al., 2015 |
| Id-1# | Id-1 destabilizes HBx by facilitating the interaction between ubiquitinated HBx and the proteasome. | Ling et al., 2008 |
| HDM2/MDM2# | Promotes NEDDylation of HBx thereby enhancing its stability. | Liu et al., 2017 |
| WDR5 | Facilitates recruitment of HBx to promotor regions. | Gao et al., 2020 |
| CBFβ | Blocks HBx function in promoting replication. | Xu et al., 2019 |
| inhibitors of differentiation 1 (Id1) | Interaction accelerates degradation of these proteins. | Xia et al., 2020 |
| inhibitors of differentiation (Id3) | Interaction accelerates degradation of these proteins. | Xia et al., 2020 |
| PRPF31 | Potential enhancement of cccDNA transcription through this interaction. | Kinoshita et al., 2017 |
# Unknown if this pertains a real protein-protein interaction; @ potential interaction, evidenced by co-localization.
Besides the transcriptional modulation of cccDNA, HBx has also been described to modulate gene expression of multiple proteins involved in signaling pathways such as the AKT serine/threonine kinase 1 (AKT1), Ras-Raf-mitogen-activated protein (MAP) kinase, MAPK8/pSMAD3L, (TβRI)/pSMAD3C, nuclear factor-kappa B (NF-kB) pathways and potential restriction factors such as STIM1, zinc finger E-box binding homeobox 2 (ZEB2), and proteasome activator subunit 4 (PSME4) (Benn et al., 1996; Klein and Schneider, 1997; Waris et al., 2001; Yoo et al., 2008; Zhang et al., 2012; Liu et al., 2014; Lu et al., 2015; Rawat and Bouchard, 2015; Wu et al., 2016; Yu et al., 2016; Cheng et al., 2018; Zheng et al., 2019; Minor et al., 2020; Table 2). Interestingly, HBx expression itself is also influenced by cellular proteins, for example, NRF1 has shown to bind the HBx promotor to activate it in contrast to ATF2, which showed the opposite effect (Choi et al., 1997; Tokusumi et al., 2004; Quasdorff and Protzer, 2010).
The HBc Interactome
HBc is mostly known as the building block of the HBV capsid (Summers et al., 1975) but in recent years it has been shown that its function is not limited to this and also plays a role in cccDNA stability, transcription and epigenetic regulation (Newbold et al., 1995; Bock et al., 2001; Zlotnick et al., 2015; Chong et al., 2017), evasion of antiviral mechanisms (Lucifora et al., 2014), reverse transcription (Tan et al., 2015), cellular trafficking (Schmitz et al., 2010; Yang et al., 2014), genomic replication (Lott et al., 2000), and viral egress (Bardens et al., 2011). The field is also discovering more and more that HBc expression is extensively regulated by core promotor regulation, core mRNA modulation and post-translational modifications which highlights its importance in the life cycle (Buckwold et al., 1997; Sohn et al., 2006; Kohno et al., 2014; Qian et al., 2015; He et al., 2016; Bartusch et al., 2017; Lubyova et al., 2017; Heger-Stevic et al., 2018; Makokha et al., 2019).
Initially, the impact on the capsid made HBc an appealing drug-target (Berke et al., 2017). However, given that there is also an interplay with cccDNA and HBx these molecules may have more far-reaching consequences. As more protein interactions between HBc and the host are elucidated, we also compiled the interactome of the core protein and linked it to the HBx and cccDNA interactomes (Figure 2).
A cccDNA and HBx Gene Association Network: Expanding the Potential cccDNA and HBx Interactome
Tables 1–3 summarize what is currently known in the literature (manual curation) about cccDNA, HBx protein, and HBc protein-DNA and protein-protein interactions, respectively. However, to utilize this information to predict and potentially identify new protein interactions, network pathway analysis was performed (Ingenuity Pathway Analysis, IPA, Qiagen). IPA enables gene network generation from the Ingenuity Knowledge Base, a data repository of biological interactions and functional annotations.
TABLE 3.
HBc interacting proteins listed together with the cellular processes or pathways in which they are involved.
| Protein interaction partner | Process | References |
| Filamin B | Interaction promotes replication. | Li et al., 2018 |
| Nucleophosmin | Promotion of capsid assembly. | Jeong et al., 2014 |
| APOBEC3B | Potential editing of DNA during reverse transcription. | Chen et al., 2018 |
| SRSF10 | Acts as a restriction factor that regulates HBV RNAs levels. | Chabrolles et al., 2020 |
| p70 ribosomal S6 kinase S6K1 | HBc modulates phosphorylation levels of S6K1. | Wang et al., 2021 |
| PRMT5 | Methylation of the cccDNA. | Zhang Y. et al., 2017 |
| Importin β | Capsid assembly. | Chen et al., 2016 |
| NIRF | Inhibition of infection. | Qian et al., 2015 |
| Hsp90 | Catalyzes the formation of the capsid by binding HBc dimers. | Shim et al., 2011 |
| hypermethylated in cancer 2 HIC2 | Unknown | Lin et al., 2006 |
| eukaryotic translation elongation factor 2 EEF2 | Unknown | Lin et al., 2006 |
| acetyl-coenzyme A synthetase 3 | Unknown | Lin et al., 2006 |
| DNA polymerase gamma POLG | Unknown | Lin et al., 2006 |
| putative translation initiation factor SUI | Unknown | Lin et al., 2006 |
| chemokine C-C motif receptor 5 | Unknown | Lin et al., 2006 |
| mitochondrial ribosomal protein L41 MRPL41 | Unknown | Lin et al., 2006 |
| kyot binding protein genes | Unknown | Lin et al., 2006 |
| RanBPM | Unknown | Lin et al., 2006 |
| HBeAg-binding protein 3 HBEBP3 | Unknown | Lin et al., 2006 |
| programmed cell death 2 PDCD2 | Unknown | Lin et al., 2006 |
| SP1 | Inhibition of anti-viral mechanism of Mitochondrial antiviral signaling protein MAVS. | Li et al., 2021 |
| coactivator cAMP response element CRE | aspecific interaction enhances the binding of the cAMP response element-binding protein CREB to CRE. | Xiang et al., 2015 |
| C12 protein | Unknown | Lu et al., 2005 |
| SRPK2 | Mediate HBV core protein phosphorylation, unknow role in viral infection. | Daub et al., 2002 |
| SRPK1 | Mediate HBV core protein phosphorylation, unknow role in viral infection. | Daub et al., 2002 |
| NXF1 | Involved in cellular trafficking of HBc | Yang et al., 2014 |
| TREX transcription/export complex | Involved in cellular trafficking of HBc | Yang et al., 2014 |
| BAF200C | Evasion of host anti-viral mechanisms. | Li et al., 2019 |
| BAF200 | Evasion of host anti-viral mechanisms. | Li et al., 2019 |
| Hsp70 | Promotes capsid formation. | Seo et al., 2018 |
| MxA | Immobilizes HBc in perinuclear compartiment, possible interference with capsid formation. | Li et al., 2012 |
| Hdj1 | Accelerated degradation of the viral core and HBx proteins | Shon et al., 2009 |
| hTid1 | Accelerated degradation of the viral core and HBx proteins | Shon et al., 2009 |
| Skeletal muscle and kidney enriched inositol phosphatase SKIP | Interaction induces HBV gene suppression. | Hung et al., 2009 |
| Atg12 | Modulation of authophagy. | Doring et al., 2018 |
| Np95/ICBP90-like RING finger protein NIRF | Potentially involved in maturation of the virus. | Qian et al., 2012 |
| PTPN3 | Supression of HBV gene expression. | Hsu et al., 2007 |
| APOBEC3G | APOBEC3G is potentially incorporated in the virion through this interaction. | Zhao et al., 2010 |
| PTPN3 | May be bound within the capsid, function unknown. | Genera et al., 2021 |
| PML | Link between DNA damage response and HBV replication. HBc co-localizes in PML-NBs. | Chung and Tsai, 2009 |
| HDAC1 | Link between DNA damage response and HBV replication. HBc co-localizes in PML-NBs. | Chung and Tsai, 2009 |
| GIPC1 | Unknown. | Razanskas and Sasnauskas, 2010 |
| Activation-induced cytidine deaminase AID | HBc is the link between AID and cccDNA. | Qiao et al., 2016 |
| Gamma-2 adaptin | Endosomal function and viral egress. | Rost et al., 2006 |
| Nedd4 | Virus production. | Rost et al., 2006 |
| ABP-276/278 | Affects viral replication via unknown mechanism. | Huang et al., 2000 |
| B23 | Unknown | Ludgate et al., 2011 |
| I2PP2A | Unknown | Ludgate et al., 2011 |
| APOBEC3B | APOBEC3B A3B displays dual inhibitory effects on HBV core-associated DNA synthesis. | Zhang et al., 2008 |
| Receptor of activated protein kinase C 1 RACK1 | Interference in normal TNF-a-regulated apoptosis. | Jia et al., 2015 |
| nucleophosmin B23 | Unknown | Lee et al., 2009 |
| CDK2 | Role in disassembly of the nucleocapsid. | Liu et al., 2021 |
| E2F1 | HBc reduced the DNA-binding ability of E2F1 to the binding site of the p53 promoter and respectively represses expression of p53. | Kwon and Rho, 2003 |
| SIRT7 | cccDNA expression modulation, HBc functions as a bridge between cccDNA and SIRT7. | Yu et al., 2021 |
| HBs | Interaction prevents nuclear translocation to HBc. | Zajakina et al., 2014 |
To generate gene association networks, the HBx, HBc, and HBV cccDNA interacting proteins were individually analyzed to create three separate network schemes. The database was filtered and core analysis performed to only query the following: (1) Species = Human, (2) Molecules per networks = 35, Networks per analysis = 10, (3) Node Types = All, (4) Data Source = All, (5) Confidence = Experimentally Observed, (6) Species = Human, (7) Tissues and Cell Types = Liver, Hepatocytes, Hepatoma Cell Lines not otherwise specified, HuH7 cell line, Hep3B cell line, HepG2 cell line and “Other” Hepatoma cell lines, and (8) Mutation = All.
If proteins selected as network “seeds” were not apparently connected or networks had less than 35 gene products, IPA added proteins from the IPA Knowledge data base to maximize the connectivity of the “seed” molecules within the filter limits. We also filtered out those proteins that were only interacting with either cccDNA, HBx, or HBc and had no extrapolated nodes. This kept the networks to a manageable size and reduced redundancy while deriving as much as possible biological context from the analysis. When adding molecules from the knowledge database, IPA uses a connectivity metric (edge-weighted spring layout) that prioritizes molecules that have the greatest overlap with the existing network. This means that the organization of the network in clusters is not based on proteins sharing similar pathways but is based on the number of described interactions in between those proteins. Upon completion of the IPA network generating algorithm, two networks were produced showing both “direct” and “indirect” relationships for either HBx, HBc, or HBV cccDNA interacting proteins. These were then merged and exported to Cytoscape 3.7.1 using an edge weighted spring layout to create the final network illustration showing the relationship between HBx, HBc, and HBV cccDNA interactingproteins (Figure 2).
In the network, proteins that interact with HBc are depicted in red, those interacting with cccDNA in pink and those interacting with HBx in green. We also highlighted those proteins that were described to interact with 2 or more of our founding (HBc, HBx, and cccDNA) nodes (Figure 2). Nineteen proteins are identified (P300, TBP, PIN4, CBP, SPIN1, CEBPB, SP1, CRTC1, RXRA, NR1H4, KDM1A, HSPA1A, APOBEC3G, APOBEC 3B, CREB1, PRMT5, HDAC1, E2F1, and SIRT1) as interacting proteins of HBx, HBc, and cccDNA. These are interesting because these components may be a driving force in cccDNA transcription and maintenance. Moreover, these may be interesting proteins for further functional research as they seem to play a connecting role in the viral life cycle (Figure 2). Most of these proteins, 12 out of 19, are regulators of transcription, for example, TBP and CRTC1 are both involved in transcription initiation; CREB1 and E2F1 are enhancers of transcription; P300, CBP, SPIN1, SP1, PRMT5, HDAC1, and SETD1B are all epigenetic modifiers that can influence the chromatin to a specific transcriptionally accessible, active state. Finally, PIN4 was described as a chromatin remodeler. Any of these proteins could be a potentially interesting target to influence transcriptional status of cccDNA. Notable is that all these transcription-related proteins have interactions with HBc, hereby confirming a role for HBc beyond capsid assembly. Also interesting is the occurrence of two APOBEC proteins as partners for HBx, HBc and cccDNA. APOBEC proteins play a role in anti-viral immunity (Stavrou and Ross, 2015) and is a means of the cell to counteract the effect of infection (Lucifora et al., 2014).
Through the IPA approach, the network was expanded from just those proteins with known interactions with HBx, HBc, or cccDNA to an additional 210 proteins (indicated in light blue) which may play a role in protein-protein or protein-cccDNA interactions. While the interactions itself are verified in literature, their involvement in the HBV pathology and viral replication cycle is not confirmed yet. Hence, these proteins provide an interesting starting point for further research. Analysis of the network shows that via these interacting proteins, HBV also taps into host pathways such as cell cycle, cell signaling, DNA repair, transcription regulation and apoptosis. This is not surprising as many of these processes have been described in relation to HBV already. However, this is the first time description of proteins which may be involved in these processes and how they relate to the cccDNA minichromosome, HBc or HBx. An additional interesting observation is that many heat shock proteins (HSP) (Hsp70, Hsp90, Hsp27, HSPD1, HSPA1A, HSPA1B, HSPA8, HSPA9, HSPA1L, HSP90AB1, HSPA5, and HSPA6) were observed as interacting proteins in this network. Literature has already described that viruses rely on host HSPs for viral protein folding and induce overexpression of HSPs in the infected cells (Bolhassani and Agi, 2019). Moreover, several HSPs were associated with some viral particles (Fust et al., 2005; Bolhassani and Agi, 2019). In HBV, downregulation of Hsp70 and Hsp90 by small interfering RNA significantly inhibited HBV production. Furthermore, also a significant reduction of HBV secretion could be observed in HepG2.2.15 cells treated with an Hsp90 inhibitor (Liu et al., 2009; Bolhassani and Agi, 2019). Further research will be required to confirm the additional protein partners identified in this network analysis.
Interactions During the Late Phases of HBV Infection
In HBV infection, besides the budding of virions, there is also the shedding of an excess amount of subviral particles (Figure 1). These particles are non-infectious 22 nm spheres or filaments of variable length consisting solely of the HBsAg envelope protein, which may be expressed from either cccDNA or HBV DNA that is integrated into the human genome (Heermann et al., 1984; Figure 1). Budding of infectious virus and shedding of subviral particles happen via distinct pathways (Selzer and Zlotnick, 2015).
Although redundant in viral assembly, the M-protein and its interaction with calnexin has been shown to be involved in the secretion of subviral particles (Werr and Prange, 1998). In the cytoplasm, HBsAg interacts with cyclophilin A (CypA) and stimulates the extracellular secretion of CypA (Tian et al., 2010; Figure 1). Interestingly, it seems that the presence of CypA reciprocally stimulates HBsAg secretion, as inhibitors against CypA reduce the amount of secreted HBsAg (Phillips et al., 2015).
To construct new virions, the pgRNA is packaged together with the viral polymerase in the nucleocapsid, which is formed in the cytoplasm by assembly of 120 HBc dimers (Lambert et al., 2007). Although not well understood, the interaction between HBc dimers and cellular protein nucleophosmin (B23) was shown to promote this assembly (Jeong et al., 2014; Figure 1). This nucleocapsid is surrounded by a cellular lipid layer embedded with three viral S glycoproteins, which originate from the endoplasmic reticulum (Bruss, 2007). Virion assembly depends solely on the L-protein, whereas the S-protein is required but not sufficient, and the M-protein is redundant (Bruss, 2004). To aid in building this unusual composition, Hsp70, and mammalian BiP were described as interaction partners of the L-protein in vitro and in vivo (Loffler-Mary et al., 1997; Lambert and Prange, 2003; Wang Y.P. et al., 2010; Figure 1). In the assembly of the mature virion, the S-protein needs to interact with the nucleocapsid (Loffler-Mary et al., 2000).
Once the mature virion is formed, it is ready to bud on the surface of the cells. The whole orchestration of this process is not clear at all, let alone accurately described in terms of interacting proteins. HBV makes use of the ESCRT, a machinery essential for the sorting of cellular cargo proteins in multivesicular bodies (Bardens et al., 2011). In this process, aryl hydrocarbon receptor interacting protein (AIP1)/ALIX and vacuolar protein sorting 4 homolog B (VPS4B) were found to colocalize with HBV particles (Kian Chua et al., 2006; Watanabe et al., 2007; Figure 1). Also, expression of dominant negative mutants of ESCRT-III complex-forming charged multivesicular body protein (CHMP) proteins (CHMP3, 4B, and 4C), as well as vacuolar protein sorting 4 homolog A (VPS4A) or VPS4B mutants, and knockout of γ2-adaptin blocked HBV assembly and egress (Hartmann-Stuhler and Prange, 2001; Rost et al., 2006; Lambert et al., 2007; Figure 1). However, the manipulation of these proteins did not alter the secretion of subviral particles. Also involved in viral egress is Neural precursor cell Expressed, Developmentally Down-regulated 4 (NEDD) E3 ubiquitin protein ligase, which appears to control virus production by binding to the late assembly domain-like PPAY motif of HBV capsids (Rost et al., 2006; Garcia et al., 2013). It is also known that at some point, autophagy is involved in HBV production as the S-protein was shown to interact with the autophagy factor LC3 and manipulations to the pathway result in changes in HBV secretion (Li et al., 2011).
Concluding Remarks
The interactome we build of the cccDNA, HBc and HBx protein in this review emphasizes the vast amount of knowledge there is about the interactions between HBV proteins and in particular HBx, HBc and the cccDNA. To our knowledge, this is the first time the information has been brought together in a comprehensive overview. Bringing this information together, it shows that there are still clear gaps in knowledge. For example, the network shows that several proteins were only described in a single publication as an interacting protein of cccDNA, HBc, or HBx. Further characterization of this kind of interactions and potentially understanding the reason behind these interactions will greatly benefit the understanding of HBV-related processes. In addition, through analysis of the known interacting proteins, we predicted 210 proteins which potentially interact with either cccDNA, HBx, HBc, or with multiple key modalities of HBV.
Experimental verification of these proteins can lead to the discovery of novel mechanisms and expansion of known protein interaction networks.
Being able to position cccDNA, HBc and HBx in the greater whole of the cellular environment is paramount to better understand how HBV hijacks the cellular environment.
Author Contributions
EVD, JV, LV, and FP conceived, designed, and wrote the manuscript. BS performed the network pathway analysis, designed the gene association network, and contributed to scientific discussions about the generated network. All authors have read and edited the manuscript.
Conflict of Interest
EVD, FP, LV, and BS are employees of Janssen Research and Development and may be Johnson & Johnson stockholders. JV was employed at Janssen Research and Development at the time of the work and drafting of the manuscript and may be Johnson & Johnson stockholder.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
JV did most of the work under the first affiliation at Johnson & Johnson and moved then to Charles River laboratories (present address) during the writing and finalizing of the manuscript.
References
- Addison W. R., Walters K. A., Wong W. W., Wilson J. S., Madej D., Jewell L. D., et al. (2002). Half-life of the duck hepatitis B virus covalently closed circular DNA pool in vivo following inhibition of viral replication. J. Virol. 76 6356–6363. 10.1128/jvi.76.12.6356-6363.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alarcon V., Hernandez S., Rubio L., Alvarez F., Flores Y., Varas-Godoy M., et al. (2016). The enzymes LSD1 and Set1A cooperate with the viral protein HBx to establish an active hepatitis B viral chromatin state. Sci. Rep. 6:25901. 10.1038/srep25901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antunovic J., Lemieux N., Cromlish J. A. (1993). The 17 kDa HBx protein encoded by hepatitis B virus interacts with the activation domains of Oct-1, and functions as a coactivator in the activation and repression of a human U6 promoter. Cell Mol. Biol. Res. 39 463–482. [PubMed] [Google Scholar]
- Barak O., Aronheim A., Shaul Y. (2001). HBV X protein targets HIV Tat-binding protein 1. Virology 283 110–120. 10.1006/viro.2001.0883 [DOI] [PubMed] [Google Scholar]
- Bardens A., Doring T., Stieler J., Prange R. (2011). Alix regulates egress of hepatitis B virus naked capsid particles in an ESCRT-independent manner. Cell Microbiol. 13 602–619. 10.1111/j.1462-5822.2010.01557.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnabas S., Andrisani O. M. (2000). Different regions of hepatitis B virus X protein are required for enhancement of bZip-mediated transactivation versus transrepression. J. Virol. 74 83–90. 10.1128/jvi.74.1.83-90.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnabas S., Hai T., Andrisani O. M. (1997). The hepatitis B virus X protein enhances the DNA binding potential and transcription efficacy of bZip transcription factors. J. Biol. Chem. 272 20684–20690. 10.1074/jbc.272.33.20684 [DOI] [PubMed] [Google Scholar]
- Barrasa M. I., Guo J. T., Saputelli J., Mason W. S., Seeger C. (2001). Does a cdc2 kinase-like recognition motif on the core protein of hepadnaviruses regulate assembly and disintegration of capsids? J. Virol. 75 2024–2028. 10.1128/JVI.75.4.2024-2028.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartusch C., Doring T., Prange R. (2017). Rab33B Controls Hepatitis B Virus Assembly by Regulating Core Membrane Association and Nucleocapsid Processing. Viruses 9:9060157. 10.3390/v9060157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S. A., Lee T. H., Butel J. S., Slagle B. L. (1998). Hepatitis B virus X protein interferes with cellular DNA repair. J. Virol. 72 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belloni L., Allweiss L., Guerrieri F., Pediconi N., Volz T., Pollicino T., et al. (2012). IFN-alpha inhibits HBV transcription and replication in cell culture and in humanized mice by targeting the epigenetic regulation of the nuclear cccDNA minichromosome. J. Clin. Invest. 122 529–537. 10.1172/JCI58847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belloni L., Pollicino T., De Nicola F., Guerrieri F., Raffa G., Fanciulli M., et al. (2009). Nuclear HBx binds the HBV minichromosome and modifies the epigenetic regulation of cccDNA function. Proc. Natl. Acad. Sci. U S A 106 19975–19979. 10.1073/pnas.0908365106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benhenda S., Cougot D., Buendia M. A., Neuveut C. (2009). Hepatitis B virus X protein molecular functions and its role in virus life cycle and pathogenesis. Adv. Cancer Res. 103 75–109. 10.1016/S0065-230X(09)03004-8 [DOI] [PubMed] [Google Scholar]
- Benhenda S., Ducroux A., Riviere L., Sobhian B., Ward M. D., Dion S., et al. (2013). Methyltransferase PRMT1 is a binding partner of HBx and a negative regulator of hepatitis B virus transcription. J. Virol. 87 4360–4371. 10.1128/JVI.02574-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benn J., Su F., Doria M., Schneider R. J. (1996). Hepatitis B virus HBx protein induces transcription factor AP-1 by activation of extracellular signal-regulated and c-Jun N-terminal mitogen-activated protein kinases. J. Virol. 70 4978–4985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berke J. M., Dehertogh P., Vergauwen K., Van Damme E., Mostmans W., Vandyck K., et al. (2017). Capsid Assembly Modulators Have a Dual Mechanism of Action in Primary Human Hepatocytes Infected with Hepatitis B Virus. Antimicrob. Agents Chemother. 61:517. 10.1128/AAC.00560-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitton Alaluf M., Shlomai A. (2016). New therapies for chronic hepatitis B. Liver Int. 36 775–782. 10.1111/liv.13086 [DOI] [PubMed] [Google Scholar]
- Bock C. T., Schranz P., Schroder C. H., Zentgraf H. (1994). Hepatitis B virus genome is organized into nucleosomes in the nucleus of the infected cell. Virus Genes 8 215–229. [DOI] [PubMed] [Google Scholar]
- Bock C. T., Schwinn S., Locarnini S., Fyfe J., Manns M. P., Trautwein C., et al. (2001). Structural organization of the hepatitis B virus minichromosome. J. Mol. Biol. 307 183–196. 10.1006/jmbi.2000.4481 [DOI] [PubMed] [Google Scholar]
- Bolhassani A., Agi E. (2019). Heat shock proteins in infection. Clin. Chim. Acta 498 90–100. 10.1016/j.cca.2019.08.015 [DOI] [PubMed] [Google Scholar]
- Bouchard M. J., Wang L., Schneider R. J. (2006). Activation of focal adhesion kinase by hepatitis B virus HBx protein: multiple functions in viral replication. J. Virol. 80 4406–4414. 10.1128/JVI.80.9.4406-4414.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourne E. J., Dienstag J. L., Lopez V. A., Sander T. J., Longlet J. M., Hall J. G., et al. (2007). Quantitative analysis of HBV cccDNA from clinical specimens: correlation with clinical and virological response during antiviral therapy. J. Viral. Hepat. 14 55–63. 10.1111/j.1365-2893.2006.00775.x [DOI] [PubMed] [Google Scholar]
- Boyd A., Lacombe K., Lavocat F., Maylin S., Miailhes P., Lascoux-Combe C., et al. (2016). Decay of ccc-DNA marks persistence of intrahepatic viral DNA synthesis under tenofovir in HIV-HBV co-infected patients. J. Hepatol. 65 683–691. 10.1016/j.jhep.2016.05.014 [DOI] [PubMed] [Google Scholar]
- Bruss V. (2004). Envelopment of the hepatitis B virus nucleocapsid. Virus Res. 106 199–209. 10.1016/j.virusres.2004.08.016 [DOI] [PubMed] [Google Scholar]
- Bruss V. (2007). Hepatitis B virus morphogenesis. World J. Gastroenterol. 13 65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckwold V. E., Chen M., Ou J. H. (1997). Interaction of transcription factors RFX1 and MIBP1 with the gamma motif of the negative regulatory element of the hepatitis B virus core promoter. Virology 227 515–518. 10.1006/viro.1996.8360 [DOI] [PubMed] [Google Scholar]
- Cai D., Mills C., Yu W., Yan R., Aldrich C. E., Saputelli J. R., et al. (2012). Identification of disubstituted sulfonamide compounds as specific inhibitors of hepatitis B virus covalently closed circular DNA formation. Antimicrob. Agents Chemother. 56 4277–4288. 10.1128/AAC.00473-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Y. N., Zhou Q., Kong Y. Y., Li M., Viollet B., Xie Y. H., et al. (2003). LRH-1/hB1F and HNF1 synergistically up-regulate hepatitis B virus gene transcription and DNA replication. Cell Res. 13 451–458. 10.1038/sj.cr.7290187 [DOI] [PubMed] [Google Scholar]
- Carretero M., Gomez-Gonzalo M., Lara-Pezzi E., Benedicto I., Aramburu J., Martinez-Martinez S., et al. (2002). The hepatitis B virus X protein binds to and activates the NH(2)-terminal trans-activation domain of nuclear factor of activated T cells-1. Virology 299 288–300. [DOI] [PubMed] [Google Scholar]
- Chabrolles H., Auclair H., Vegna S., Lahlali T., Pons C., Michelet M., et al. (2020). Hepatitis B virus Core protein nuclear interactome identifies SRSF10 as a host RNA-binding protein restricting HBV RNA production. PLoS Pathog. 16:e1008593. 10.1371/journal.ppat.1008593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae S., Ji J. H., Kwon S. H., Lee H. S., Lim J. M., Kang D., et al. (2013). HBxAPalpha/Rsf-1-mediated HBx-hBubR1 interactions regulate the mitotic spindle checkpoint and chromosome instability. Carcinogenesis 34 1680–1688. 10.1093/carcin/bgt105 [DOI] [PubMed] [Google Scholar]
- Chan C., Wang Y., Chow P. K., Chung A. Y., Ooi L. L., Lee C. G. (2013). Altered binding site selection of p53 transcription cassettes by hepatitis B virus X protein. Mol. Cell Biol. 33 485–497. 10.1128/MCB.01189-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Wang J. C., Pierson E. E., Keifer D. Z., Delaleau M., Gallucci L., et al. (2016). Importin beta Can Bind Hepatitis B Virus Core Protein and Empty Core-Like Particles and Induce Structural Changes. PLoS Pathog. 12:e1005802. 10.1371/journal.ppat.1005802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W. N., Liu L. L., Jiao B. Y., Lin W. S., Lin X. J., Lin X. (2015). Hepatitis B virus X protein increases the IL-1beta-induced NF-kappaB activation via interaction with evolutionarily conserved signaling intermediate in Toll pathways (ECSIT). Virus Res. 195 236–245. 10.1016/j.virusres.2014.10.025 [DOI] [PubMed] [Google Scholar]
- Chen Y., Hu J., Cai X., Huang Y., Zhou X., Tu Z., et al. (2018). APOBEC3B edits HBV DNA and inhibits HBV replication during reverse transcription. Antiviral. Res. 149 16–25. 10.1016/j.antiviral.2017.11.006 [DOI] [PubMed] [Google Scholar]
- Cheng S. T., Ren J. H., Cai X. F., Jiang H., Chen J. (2018). HBx-elevated SIRT2 promotes HBV replication and hepatocarcinogenesis. Biochem. Biophys. Res. Commun. 496 904–910. 10.1016/j.bbrc.2018.01.127 [DOI] [PubMed] [Google Scholar]
- Cheong J. H., Yi M., Lin Y., Murakami S. (1995). Human RPB5, a subunit shared by eukaryotic nuclear RNA polymerases, binds human hepatitis B virus X protein and may play a role in X transactivation. EMBO J. 14 143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho I. J., Ki S. H., Brooks C., III, Kim S. G. (2009). Role of hepatitis B virus X repression of C/EBPbeta activity in the down-regulation of glutathione S-transferase A2 gene: implications in other phase II detoxifying enzyme expression. Xenobiotica 39 182–192. 10.1080/00498250802549808 [DOI] [PubMed] [Google Scholar]
- Choi B. H., Park G. T., Rho H. M. (1999). Interaction of hepatitis B viral X protein and CCAAT/enhancer-binding protein alpha synergistically activates the hepatitis B viral enhancer II/pregenomic promoter. J. Biol. Chem. 274 2858–2865. 10.1074/jbc.274.5.2858 [DOI] [PubMed] [Google Scholar]
- Choi C. Y., Choi B. H., Park G. T., Rho H. M. (1997). Activating transcription factor 2 (ATF2) down-regulates hepatitis B virus X promoter activity by the competition for the activating protein 1 binding site and the formation of the ATF2-Jun heterodimer. J. Biol. Chem. 272 16934–16939. [DOI] [PubMed] [Google Scholar]
- Choi M., Lee H., Rho H. M. (2002). E2F1 activates the human p53 promoter and overcomes the repressive effect of hepatitis B viral X protein (Hbx) on the p53 promoter. IUBMB Life 53 309–317. 10.1080/15216540213466 [DOI] [PubMed] [Google Scholar]
- Choi Y. H., Kim H. I., Seong J. K., Yu D. Y., Cho H., Lee M. O., et al. (2004). Hepatitis B virus X protein modulates peroxisome proliferator-activated receptor gamma through protein-protein interaction. FEBS Lett. 557 73–80. [DOI] [PubMed] [Google Scholar]
- Chong C. K., Cheng C. Y. S., Tsoi S. Y. J., Huang F. Y., Liu F., Seto W. K., et al. (2017). Role of hepatitis B core protein in HBV transcription and recruitment of histone acetyltransferases to cccDNA minichromosome. Antiviral. Res. 144 1–7. 10.1016/j.antiviral.2017.05.003 [DOI] [PubMed] [Google Scholar]
- Chung Y. L., Tsai T. Y. (2009). Promyelocytic leukemia nuclear bodies link the DNA damage repair pathway with hepatitis B virus replication: implications for hepatitis B virus exacerbation during chemotherapy and radiotherapy. Mol. Cancer Res. 7 1672–1685. 10.1158/1541-7786.MCR-09-0112 [DOI] [PubMed] [Google Scholar]
- Cougot D., Allemand E., Riviere L., Benhenda S., Duroure K., Levillayer F., et al. (2012). Inhibition of PP1 phosphatase activity by HBx: a mechanism for the activation of hepatitis B virus transcription. Sci. Signal 5:ra1. 10.1126/scisignal.2001906 [DOI] [PubMed] [Google Scholar]
- Cougot D., Wu Y., Cairo S., Caramel J., Renard C. A., Levy L., et al. (2007). The hepatitis B virus X protein functionally interacts with CREB-binding protein/p300 in the regulation of CREB-mediated transcription. J. Biol. Chem. 282 4277–4287. 10.1074/jbc.M606774200 [DOI] [PubMed] [Google Scholar]
- Cui X., Mcallister R., Boregowda R., Sohn J. A., Cortes Ledesma F., Caldecott K. W., et al. (2015). Does Tyrosyl DNA Phosphodiesterase-2 Play a Role in Hepatitis B Virus Genome Repair? PLoS One 10:e0128401. 10.1371/journal.pone.0128401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai X., Zhang W., Zhang H., Sun S., Yu H., Guo Y., et al. (2014). Modulation of HBV replication by microRNA-15b through targeting hepatocyte nuclear factor 1alpha. Nucleic Acids Res. 42 6578–6590. 10.1093/nar/gku260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Y., Cros M. P., Pontoizeau C., Elena-Hermann B., Bonn G. K., Hainaut P. (2014). Downregulation of transcription factor E4F1 in hepatocarcinoma cells: HBV-dependent effects on autophagy, proliferation and metabolism. Carcinogenesis 35 635–650. 10.1093/carcin/bgt353 [DOI] [PubMed] [Google Scholar]
- Dandri M., Burda M. R., Will H., Petersen J. (2000). Increased hepatocyte turnover and inhibition of woodchuck hepatitis B virus replication by adefovir in vitro do not lead to reduction of the closed circular DNA. Hepatology 32 139–146. 10.1053/jhep.2000.8701 [DOI] [PubMed] [Google Scholar]
- Daub H., Blencke S., Habenberger P., Kurtenbach A., Dennenmoser J., Wissing J., et al. (2002). Identification of SRPK1 and SRPK2 as the major cellular protein kinases phosphorylating hepatitis B virus core protein. J. Virol. 76 8124–8137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis L. G., Weber D. J., Lemon S. M. (1989). Horizontal transmission of hepatitis B virus. Lancet 1 889–893. [DOI] [PubMed] [Google Scholar]
- Decorsiere A., Mueller H., Van Breugel P. C., Abdul F., Gerossier L., Beran R. K., et al. (2016). Hepatitis B virus X protein identifies the Smc5/6 complex as a host restriction factor. Nature 531 386–389. 10.1038/nature17170 [DOI] [PubMed] [Google Scholar]
- Deng J. J., Kong K. E., Gao W. W., Tang H. V., Chaudhary V., Cheng Y., et al. (2017). Interplay between SIRT1 and hepatitis B virus X protein in the activation of viral transcription. Biochim. Biophys. Acta 1860 491–501. 10.1016/j.bbagrm.2017.02.007 [DOI] [PubMed] [Google Scholar]
- Deng L., Gan X., Ito M., Chen M., Aly H. H., Matsui C., et al. (2018). Peroxiredoxin 1, a novel HBx-interacting protein, interacts with Exosc5 and negatively regulates HBV propagation through degradation of HBV RNA. J. Virol. 2018:2218. 10.1128/JVI.02203-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng L., Gan X., Ito M., Chen M., Aly H. H., Matsui C., et al. (2019). Peroxiredoxin 1, a Novel HBx-Interacting Protein, Interacts with Exosome Component 5 and Negatively Regulates Hepatitis B Virus (HBV) Propagation through Degradation of HBV RNA. J. Virol. 93:2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doring T., Zeyen L., Bartusch C., Prange R. (2018). Hepatitis B Virus Subverts the Autophagy Elongation Complex Atg5-12/16L1 and Does Not Require Atg8/LC3 Lipidation for Viral Maturation. J. Virol. 92:1517. 10.1128/JVI.01513-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducroux A., Benhenda S., Riviere L., Semmes O. J., Benkirane M., Neuveut C. (2014). The Tudor domain protein Spindlin1 is involved in intrinsic antiviral defense against incoming hepatitis B Virus and herpes simplex virus type 1. PLoS Pathog. 10:e1004343. 10.1371/journal.ppat.1004343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanning G. C., Zoulim F., Hou J., Bertoletti A. (2019). Therapeutic strategies for hepatitis B virus infection: towards a cure. Nat. Rev. Drug Discov. 18 827–844. 10.1038/s41573-019-0037-0 [DOI] [PubMed] [Google Scholar]
- Fay N., Pante N. (2015). Nuclear entry of DNA viruses. Front. Microbiol. 6:467. 10.3389/fmicb.2015.00467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng H., Tan T. L., Niu D., Chen W. N. (2010). HBV X protein interacts with cytoskeletal signaling proteins through SH3 binding. Front. Biosci. 2 143–150. [DOI] [PubMed] [Google Scholar]
- Forgues M., Marrogi A. J., Spillare E. A., Wu C. G., Yang Q., Yoshida M., et al. (2001). Interaction of the hepatitis B virus X protein with the Crm1-dependent nuclear export pathway. J. Biol. Chem. 276 22797–22803. 10.1074/jbc.M101259200 [DOI] [PubMed] [Google Scholar]
- Fu S., Wang J., Hu X., Zhou R. R., Fu Y., Tang D., et al. (2018). Crosstalk between hepatitis B virus X and high-mobility group box 1 facilitates autophagy in hepatocytes. Mol. Oncol. 12 322–338. 10.1002/1878-0261.12165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fust G., Beck Z., Banhegyi D., Kocsis J., Biro A., Prohaszka Z. (2005). Antibodies against heat shock proteins and cholesterol in HIV infection. Mol. Immunol. 42 79–85. 10.1016/j.molimm.2004.07.003 [DOI] [PubMed] [Google Scholar]
- Gallucci L., Kann M. (2017). Nuclear Import of Hepatitis B Virus Capsids and Genome. Viruses 9:9010021. 10.3390/v9010021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao W., Jia Z., Tian Y., Yang P., Sun H., Wang C., et al. (2020). HBx Protein Contributes to Liver Carcinogenesis by H3K4me3 Modification Through Stabilizing WD Repeat Domain 5 Protein. Hepatology 71 1678–1695. 10.1002/hep.30947 [DOI] [PubMed] [Google Scholar]
- Garcia M. L., Reynolds T. D., Mothes W., Robek M. D. (2013). Functional characterization of the putative hepatitis B virus core protein late domain using retrovirus chimeras. PLoS One 8:e72845. 10.1371/journal.pone.0072845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genera M., Quioc-Salomon B., Nourisson A., Colcombet-Cazenave B., Haouz A., Mechaly A., et al. (2021). Molecular basis of the interaction of the human tyrosine phosphatase PTPN3 with the hepatitis B virus core protein. Sci. Rep. 11:944. 10.1038/s41598-020-79580-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geng X., Huang C., Qin Y., Mccombs J. E., Yuan Q., Harry B. L., et al. (2012). Hepatitis B virus X protein targets Bcl-2 proteins to increase intracellular calcium, required for virus replication and cell death induction. Proc. Natl. Acad. Sci. U S A 109 18471–18476. 10.1073/pnas.1204668109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore D. T., Dick R., Appleby T., Birkus G., Willkom M., Delaney W. E., et al. (2017). Antiviral activity of GS-5801, a liver-targeted prodrug of a lysine demethylase 5 inhibitor, in a hepatitis B virus primary human hepatocyte infection model. J. Hepatol. 66 S690–S691. 10.1016/S0168-8278(17)31855-X [DOI] [Google Scholar]
- Gong S. J., Feng X. J., Song W. H., Chen J. M., Wang S. M., Xing D. J., et al. (2016). Upregulation of PP2Ac predicts poor prognosis and contributes to aggressiveness in hepatocellular carcinoma. Cancer Biol. Ther. 17 151–162. 10.1080/15384047.2015.1121345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gripon P., Cannie I., Urban S. (2005). Efficient inhibition of hepatitis B virus infection by acylated peptides derived from the large viral surface protein. J. Virol. 79 1613–1622. 10.1128/JVI.79.3.1613-1622.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H., Xu C., Zhou T., Block T. M., Guo J. T. (2012). Characterization of the host factors required for hepadnavirus covalently closed circular (ccc) DNA formation. PLoS One 7:e43270. 10.1371/journal.pone.0043270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L., Wang X., Ren L., Zeng M., Wang S., Weng Y., et al. (2014). HBx affects CUL4-DDB1 function in both positive and negative manners. Biochem. Biophys. Res. Commun. 450 1492–1497. 10.1016/j.bbrc.2014.07.019:10.1016/j.bbrc.2014.07.019 [DOI] [PubMed] [Google Scholar]
- Guo Y. H., Li Y. N., Zhao J. R., Zhang J., Yan Z. (2011). HBc binds to the CpG islands of HBV cccDNA and promotes an epigenetic permissive state. Epigenetics 6 720–726. [DOI] [PubMed] [Google Scholar]
- Hao R., He J., Liu X., Gao G., Liu D., Cui L., et al. (2015). Inhibition of hepatitis B virus gene expression and replication by hepatocyte nuclear factor 6. J. Virol. 89 4345–4355. 10.1128/JVI.03094-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Z., Zheng L., Kluwe L., Huang W. (2012). Ferritin light chain and squamous cell carcinoma antigen 1 are coreceptors for cellular attachment and entry of hepatitis B virus. Int. J. Nanomedicine 7 827–834. 10.2147/IJN.S27803:10.2147/IJN.S27803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann-Stuhler C., Prange R. (2001). Hepatitis B virus large envelope protein interacts with gamma2-adaptin, a clathrin adaptor-related protein. J. Virol. 75 5343–5351. 10.1128/JVI.75.11.5343-5351.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi M., Deng L., Chen M., Gan X., Shinozaki K., Shoji I., et al. (2016). Interaction of the hepatitis B virus X protein with the lysine methyltransferase SET and MYND domain-containing 3 induces activator protein 1 activation. Microbiol. Immunol. 60 17–25. 10.1111/1348-0421.12345 [DOI] [PubMed] [Google Scholar]
- He Q., Li W., Ren J., Huang Y., Huang Y., Hu Q., et al. (2016). ZEB2 inhibits HBV transcription and replication by targeting its core promoter. Oncotarget 7 16003–16011. 10.18632/oncotarget.7435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heermann K. H., Goldmann U., Schwartz W., Seyffarth T., Baumgarten H., Gerlich W. H. (1984). Large surface proteins of hepatitis B virus containing the pre-s sequence. J. Virol. 52 396–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heger-Stevic J., Zimmermann P., Lecoq L., Bottcher B., Nassal M. (2018). Hepatitis B virus core protein phosphorylation: Identification of the SRPK1 target sites and impact of their occupancy on RNA binding and capsid structure. PLoS Pathog. 14:e1007488. 10.1371/journal.ppat.1007488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henkler F., Hoare J., Waseem N., Goldin R. D., Mcgarvey M. J., Koshy R., et al. (2001). Intracellular localization of the hepatitis B virus HBx protein. J. Gen. Virol. 82 871–882. 10.1099/0022-1317-82-4-871 [DOI] [PubMed] [Google Scholar]
- Hodgson A. J., Hyser J. M., Keasler V. V., Cang Y., Slagle B. L. (2012). Hepatitis B virus regulatory HBx protein binding to DDB1 is required but is not sufficient for maximal HBV replication. Virology 426 73–82. 10.1016/j.virol.2012.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong A., Han D. D., Wright C. J., Burch T., Piper J., Osiowy C., et al. (2012). The interaction between hepatitis B virus X protein and AIB1 oncogene is required for the activation of NFkappaB signal transduction. Biochem. Biophys. Res. Commun. 423 6–12. 10.1016/j.bbrc.2012.05.021:10.1016/j.bbrc.2012.05.021 [DOI] [PubMed] [Google Scholar]
- Hsu E. C., Lin Y. C., Hung C. S., Huang C. J., Lee M. Y., Yang S. C., et al. (2007). Suppression of hepatitis B viral gene expression by protein-tyrosine phosphatase PTPN3. J. Biomed. Sci. 14 731–744. 10.1007/s11373-007-9187-x [DOI] [PubMed] [Google Scholar]
- Hu Z., Zhang Z., Doo E., Coux O., Goldberg A. L., Liang T. J. (1999). Hepatitis B virus X protein is both a substrate and a potential inhibitor of the proteasome complex. J. Virol. 73 7231–7240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C. J., Chen Y. H., Ting L. P. (2000). Hepatitis B virus core protein interacts with the C-terminal region of actin-binding protein. J. Biomed. Sci. 7 160–168. 10.1007/BF02256623 [DOI] [PubMed] [Google Scholar]
- Huang H. C., Chen C. C., Chang W. C., Tao M. H., Huang C. (2012). Entry of hepatitis B virus into immortalized human primary hepatocytes by clathrin-dependent endocytosis. J. Virol. 86 9443–9453. 10.1128/JVI.00873-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Kwong J., Sun E. C., Liang T. J. (1996). Proteasome complex as a potential cellular target of hepatitis B virus X protein. J. Virol. 70 5582–5591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q., Zhou B., Cai D., Zong Y., Wu Y., Liu S., et al. (2021). Rapid Turnover of Hepatitis B Virus Covalently Closed Circular DNA Indicated by Monitoring Emergence and Reversion of Signature-Mutation in Treated Chronic Hepatitis B Patients. Hepatology 73 41–52. 10.1002/hep.31240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh K. W., Siddiqui A. (2002). Characterization of the mitochondrial association of hepatitis B virus X protein, HBx. Mitochondrion 1 349–359. [DOI] [PubMed] [Google Scholar]
- Hung C. S., Lin Y. L., Wu C. I., Huang C. J., Ting L. P. (2009). Suppression of hepatitis B viral gene expression by phosphoinositide 5-phosphatase SKIP. Cell Microbiol. 11 37–50. 10.1111/j.1462-5822.2008.01235.x [DOI] [PubMed] [Google Scholar]
- Ishida H., Ueda K., Ohkawa K., Kanazawa Y., Hosui A., Nakanishi F., et al. (2000). Identification of multiple transcription factors, HLF, FTF, and E4BP4, controlling hepatitis B virus enhancer II. J. Virol. 74 1241–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto M., Saso W., Sugiyama R., Ishii K., Ohki M., Nagamori S., et al. (2019). Epidermal growth factor receptor is a host-entry cofactor triggering hepatitis B virus internalization. Proc. Natl. Acad. Sci. U S A 116 8487–8492. 10.1073/pnas.1811064116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer S., Groopman J. D. (2011). Interaction of mutant hepatitis B X protein with p53 tumor suppressor protein affects both transcription and cell survival. Mol. Carcinog. 50 972–980. 10.1002/mc.20767:10.1002/mc.20767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A., Swarnalatha M., Sultana S., Joshi P., Panda S. K., Kumar V. (2015). The G1 phase E3 ubiquitin ligase TRUSS that gets deregulated in human cancers is a novel substrate of the S-phase E3 ubiquitin ligase Skp2. Cell Cycle 14 2688–2700. 10.1080/15384101.2015.1056946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong H., Cho M. H., Park S. G., Jung G. (2014). Interaction between nucleophosmin and HBV core protein increases HBV capsid assembly. FEBS Lett. 588 851–858. 10.1016/j.febslet.2014.01.020 [DOI] [PubMed] [Google Scholar]
- Jia B., Guo M., Li G., Yu D., Zhang X., Lan K., et al. (2015). Hepatitis B virus core protein sensitizes hepatocytes to tumor necrosis factor-induced apoptosis by suppression of the phosphorylation of mitogen-activated protein kinase kinase 7. J. Virol. 89 2041–2051. 10.1128/JVI.03106-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao B. Y., Lin W. S., She F. F., Chen W. N., Lin X. (2011). Hepatitis B virus X protein enhances activation of nuclear factor kappaB through interaction with valosin-containing protein. Arch. Virol. 156 2015–2021. 10.1007/s00705-011-1099-4 [DOI] [PubMed] [Google Scholar]
- Kalra N., Kumar V. (2006). The X protein of hepatitis B virus binds to the F box protein Skp2 and inhibits the ubiquitination and proteasomal degradation of c-Myc. FEBS Lett. 580 431–436. 10.1016/j.febslet.2005.12.034 [DOI] [PubMed] [Google Scholar]
- Kann M., Sodeik B., Vlachou A., Gerlich W. H., Helenius A. (1999). Phosphorylation-dependent binding of hepatitis B virus core particles to the nuclear pore complex. J. Cell Biol. 145 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kau J. H., Ting L. P. (1998). Phosphorylation of the core protein of hepatitis B virus by a 46-kilodalton serine kinase. J. Virol. 72 3796–3803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattar E., Mukherji A., Kumar V. (2012). Akt augments the oncogenic potential of the HBx protein of hepatitis B virus by phosphorylation. FEBS J. 279 1220–1230. 10.1111/j.1742-4658.2012.08514.x [DOI] [PubMed] [Google Scholar]
- Kian Chua P., Lin M. H., Shih C. (2006). Potent inhibition of human Hepatitis B virus replication by a host factor Vps4. Virology 354 1–6. 10.1016/j.virol.2006.07.018 [DOI] [PubMed] [Google Scholar]
- Kim B. K., Lim S. O., Park Y. G. (2008). Requirement of the cyclic adenosisne monophosphate response element-binding protein for hepatitis B virus replication. Hepatology 48 361–373. 10.1002/hep.22359 [DOI] [PubMed] [Google Scholar]
- Kim H. J., Kim S. Y., Kim J., Lee H., Choi M., Kim J. K., et al. (2008). Hepatitis B virus X protein induces apoptosis by enhancing translocation of Bax to mitochondria. IUBMB Life 60 473–480. 10.1002/iub.68 [DOI] [PubMed] [Google Scholar]
- Kim H. Y., Cho H. K., Hong S. P., Cheong J. (2011). Hepatitis B virus X protein stimulates the Hedgehog-Gli activation through protein stabilization and nuclear localization of Gli1 in liver cancer cells. Cancer Lett. 309 176–184. 10.1016/j.canlet.2011.05.033 [DOI] [PubMed] [Google Scholar]
- Kim J. S., Rho B., Lee T. H., Lee J. M., Kim S. J., Park J. H. (2006). The interaction of hepatitis B virus X protein and protein phosphatase type 2 Calpha and its effect on IL-6. Biochem. Biophys. Res. Commun. 351 253–258. 10.1016/j.bbrc.2006.10.028 [DOI] [PubMed] [Google Scholar]
- Kim J. Y., Song E. H., Lee H. J., Oh Y. K., Choi K. H., Yu D. Y., et al. (2010). HBx-induced hepatic steatosis and apoptosis are regulated by TNFR1- and NF-kappaB-dependent pathways. J. Mol. Biol. 397 917–931. 10.1016/j.jmb.2010.02.016 [DOI] [PubMed] [Google Scholar]
- Kim K. H., Seong B. L. (2003). Pro-apoptotic function of HBV X protein is mediated by interaction with c-FLIP and enhancement of death-inducing signal. EMBO J. 22 2104–2116. 10.1093/emboj/cdg210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K., Kim K. H., Cheong J. (2010). Hepatitis B virus X protein impairs hepatic insulin signaling through degradation of IRS1 and induction of SOCS3. PLoS One 5:e8649. 10.1371/journal.pone.0008649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. Y., Kim J. C., Kim J. K., Kim H. J., Lee H. M., Choi M. S., et al. (2008). Hepatitis B virus X protein enhances NFkappaB activity through cooperating with VBP1. BMB Rep. 41 158–163. [DOI] [PubMed] [Google Scholar]
- Kim W. R. (2018). Emerging Therapies Toward a Functional Cure for Hepatitis B Virus Infection. Gastroenterol. Hepatol. 14 439–442. [PMC free article] [PubMed] [Google Scholar]
- Kinoshita W., Ogura N., Watashi K., Wakita T. (2017). Host factor PRPF31 is involved in cccDNA production in HBV-replicating cells. Biochem. Biophys. Res. Commun. 482 638–644. 10.1016/j.bbrc.2016.11.085 [DOI] [PubMed] [Google Scholar]
- Kitamura K., Que L., Shimadu M., Koura M., Ishihara Y., Wakae K., et al. (2018). Flap endonuclease 1 is involved in cccDNA formation in the hepatitis B virus. PLoS Pathog. 14:e1007124. 10.1371/journal.ppat.1007124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein N. P., Schneider R. J. (1997). Activation of Src family kinases by hepatitis B virus HBx protein and coupled signaling to Ras. Mol. Cell Biol. 17 6427–6436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C., Lee S., Windisch M. P., Ryu W. S. (2014). DDX3 DEAD-box RNA helicase is a host factor that restricts hepatitis B virus replication at the transcriptional level. J. Virol. 88 13689–13698. 10.1128/JVI.02035-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kock J., Rosler C., Zhang J. J., Blum H. E., Nassal M., Thoma C. (2010). Generation of covalently closed circular DNA of hepatitis B viruses via intracellular recycling is regulated in a virus specific manner. PLoS Pathog. 6:e1001082. 10.1371/journal.ppat.1001082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohno T., Tsuge M., Murakami E., Hiraga N., Abe H., Miki D., et al. (2014). Human microRNA hsa-miR-1231 suppresses hepatitis B virus replication by targeting core mRNA. J. Viral. Hepat. 21 e89–e97. 10.1111/jvh.12240 [DOI] [PubMed] [Google Scholar]
- Kong H. J., Hong S. H., Lee M. Y., Kim H. D., Lee J. W., Cheong J. (2000). Direct binding of hepatitis B virus X protein and retinoid X receptor contributes to phosphoenolpyruvate carboxykinase gene transactivation. FEBS Lett. 483 114–118. 10.1016/s0014-5793(00)02091-3 [DOI] [PubMed] [Google Scholar]
- Kong H. J., Park M. J., Hong S., Yu H. J., Lee Y. C., Choi Y. H., et al. (2003). Hepatitis B virus X protein regulates transactivation activity and protein stability of the cancer-amplified transcription coactivator ASC-2. Hepatology 38 1258–1266. 10.1053/jhep.2003.50451 [DOI] [PubMed] [Google Scholar]
- Koniger C., Wingert I., Marsmann M., Rosler C., Beck J., Nassal M. (2014). Involvement of the host DNA-repair enzyme TDP2 in formation of the covalently closed circular DNA persistence reservoir of hepatitis B viruses. Proc. Natl. Acad. Sci. U S A 111 E4244–E4253. 10.1073/pnas.1409986111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouwaki T., Okamoto T., Ito A., Sugiyama Y., Yamashita K., Suzuki T., et al. (2016). Hepatocyte Factor JMJD5 Regulates Hepatitis B Virus Replication through Interaction with HBx. J. Virol. 90 3530–3542. 10.1128/JVI.02776-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Jung S. Y., Hodgson A. J., Madden C. R., Qin J., Slagle B. L. (2011). Hepatitis B virus regulatory HBx protein binds to adaptor protein IPS-1 and inhibits the activation of beta interferon. J. Virol. 85 987–995. 10.1128/JVI.01825-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon J. A., Rho H. M. (2003). Transcriptional repression of the human p53 gene by hepatitis B viral core protein (HBc) in human liver cells. Biol. Chem. 384 203–212. 10.1515/BC.2003.022 [DOI] [PubMed] [Google Scholar]
- Lambert C., Prange R. (2003). Chaperone action in the posttranslational topological reorientation of the hepatitis B virus large envelope protein: Implications for translocational regulation. Proc. Natl. Acad. Sci. U S A 100 5199–5204. 10.1073/pnas.0930813100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert C., Doring T., Prange R. (2007). Hepatitis B virus maturation is sensitive to functional inhibition of ESCRT-III, Vps4, and gamma 2-adaptin. J. Virol. 81 9050–9060. 10.1128/JVI.00479-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus J. V., Block T., Brechot C., Kramvis A., Miller V., Ninburg M., et al. (2018). The hepatitis B epidemic and the urgent need for cure preparedness. Nat. Rev. Gastroenterol. Hepatol. 15 517–518. 10.1038/s41575-018-0041-6 [DOI] [PubMed] [Google Scholar]
- Lee H., Jeong H., Lee S. Y., Kim S. S., Jang K. L. (2019). Hepatitis B Virus X Protein Stimulates Virus Replication Via DNA Methylation of the C-1619 in Covalently Closed Circular DNA. Mol. Cells 42 67–78. 10.14348/molcells.2018.0255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. J., Shim H. Y., Hsieh A., Min J. Y., Jung G. (2009). Hepatitis B virus core interacts with the host cell nucleolar protein, nucleophosmin 1. J. Microbiol. 47 746–752. 10.1007/s12275-009-2720-z [DOI] [PubMed] [Google Scholar]
- Lee S., Kim W., Ko C., Ryu W. S. (2016). Hepatitis B virus X protein enhances Myc stability by inhibiting SCF(Skp2) ubiquitin E3 ligase-mediated Myc ubiquitination and contributes to oncogenesis. Oncogene 35 1857–1867. 10.1038/onc.2015.251 [DOI] [PubMed] [Google Scholar]
- Lee Y. H., Yun Y. (1998). HBx protein of hepatitis B virus activates Jak1-STAT signaling. J. Biol. Chem. 273 25510–25515. [DOI] [PubMed] [Google Scholar]
- Levrero M., Pollicino T., Petersen J., Belloni L., Raimondo G., Dandri M. (2009). Control of cccDNA function in hepatitis B virus infection. J. Hepatol. 51 581–592. 10.1016/j.jhep.2009.05.022 [DOI] [PubMed] [Google Scholar]
- Li B., Carey M., Workman J. L. (2007). The role of chromatin during transcription. Cell 128 707–719. 10.1016/j.cell.2007.01.015 [DOI] [PubMed] [Google Scholar]
- Li D., Ding J., Chen Z., Chen Y., Lin N., Chen F., et al. (2015). Accurately mapping the location of the binding site for the interaction between hepatitis B virus X protein and cytochrome c oxidase III. Int. J. Mol. Med. 35 319–324. 10.3892/ijmm.2014.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., He J., Fu Y., Hu X., Sun L. Q., Huang Y., et al. (2017). Hepatitis B virus X protein inhibits apoptosis by modulating endoplasmic reticulum stress response. Oncotarget 8 96027–96034. 10.18632/oncotarget.21630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Liu Y., Wang Z., Liu K., Wang Y., Liu J., et al. (2011). Subversion of cellular autophagy machinery by hepatitis B virus for viral envelopment. J. Virol. 85 6319–6333. 10.1128/JVI.02627-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li N., Zhang L., Chen L., Feng W., Xu Y., Chen F., et al. (2012). MxA inhibits hepatitis B virus replication by interaction with hepatitis B core antigen. Hepatology 56 803–811. 10.1002/hep.25608 [DOI] [PubMed] [Google Scholar]
- Li T., Ke Z., Liu W., Xiong Y., Zhu Y., Liu Y. (2019). Human Hepatitis B Virus Core Protein Inhibits IFNalpha-Induced IFITM1 Expression by Interacting with BAF200. Viruses 11:11050427. 10.3390/v11050427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., Yang X., Li W., Song J., Li Z., Zhu X., et al. (2021). ADAR1 Stimulation by IFN-alpha Downregulates the Expression of MAVS via RNA Editing to Regulate the Anti-HBV Response. Mol. Ther. 29 1335–1348. 10.1016/j.ymthe.2020.11.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Sun Y., Sun F., Hua R., Li C., Chen L., et al. (2018). Mechanisms and Effects on HBV Replication of the Interaction between HBV Core Protein and Cellular Filamin B. Virol. Sin. 33 162–172. 10.1007/s12250-018-0023-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang T. J., Block T. M., Mcmahon B. J., Ghany M. G., Urban S., Guo J. T., et al. (2015). Present and future therapies of hepatitis B: From discovery to cure. Hepatology 62 1893–1908. 10.1002/hep.28025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman P. M. (2016). Epigenetics and Genetics of Viral Latency. Cell Host Microbe 19 619–628. 10.1016/j.chom.2016.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim K. H., Kim K. H., Choi S. I., Park E. S., Park S. H., Ryu K., et al. (2011). RPS3a over-expressed in HBV-associated hepatocellular carcinoma enhances the HBx-induced NF-kappaB signaling via its novel chaperoning function. PLoS One 6:e22258. 10.1371/journal.pone.0022258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Gu C., Shen Z., Liu Y., Wang W., Tao S., et al. (2017). Hepatocyte nuclear factor 1alpha downregulates HBV gene expression and replication by activating the NF-kappaB signaling pathway. PLoS One 12:e0174017. 10.1371/journal.pone.0174017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S. M., Cheng J., Lu Y. Y., Zhang S. L., Yang Q., Chen T. Y., et al. (2006). Screening and identification of interacting proteins with hepatitis B virus core protein in leukocytes and cloning of new gene C1. World J. Gastroenterol. 12 1043–1048. 10.3748/wjg.v12.i7.1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin W. S., Jiao B. Y., Wu Y. L., Chen W. N., Lin X. (2012). Hepatitis B virus X protein blocks filamentous actin bundles by interaction with eukaryotic translation elongat ion factor 1 alpha 1. J. Med. Virol. 84 871–877. 10.1002/jmv.23283 [DOI] [PubMed] [Google Scholar]
- Lin Y., Nomura T., Cheong J., Dorjsuren D., Iida K., Murakami S. (1997). Hepatitis B virus X protein is a transcriptional modulator that communicates with transcription factor IIB and the RNA polymerase II subunit 5. J. Biol. Chem. 272 7132–7139. [DOI] [PubMed] [Google Scholar]
- Ling M. T., Chiu Y. T., Lee T. K., Leung S. C., Fung M. K., Wang X., et al. (2008). Id-1 induces proteasome-dependent degradation of the HBX protein. J. Mol. Biol. 382 34–43. 10.1016/j.jmb.2007.06.020 [DOI] [PubMed] [Google Scholar]
- Liu B., Fang M., He Z., Cui D., Jia S., Lin X., et al. (2015). Hepatitis B virus stimulates G6PD expression through HBx-mediated Nrf2 activation. Cell Death Dis. 6:e1980. 10.1038/cddis.2015.322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Cai D., Zhang L., Tang W., Yan R., Guo H., et al. (2016). Identification of hydrolyzable tannins (punicalagin, punicalin and geraniin) as novel inhibitors of hepatitis B virus covalently closed circular DNA. Antiviral. Res. 134 97–107. 10.1016/j.antiviral.2016.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Lou G., Li C., Wang X., Cederbaum A. I., Gan L., et al. (2014). HBx inhibits CYP2E1 gene expression via downregulating HNF4alpha in human hepatoma cells. PLoS One 9:e107913. 10.1371/journal.pone.0107913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Xi J., Hu J. (2021). Regulation of Hepatitis B Virus Replication by Cyclin Docking Motifs in Core Protein. J. Virol. 95:21. 10.1128/JVI.00230-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Yuan Y., Guo H., Mitchelson K., Zhang K., Xie L., et al. (2012). Hepatitis B virus encoded X protein suppresses apoptosis by inhibition of the caspase-independent pathway. J. Proteome Res. 11 4803–4813. 10.1021/pr2012297 [DOI] [PubMed] [Google Scholar]
- Liu K., Qian L., Wang J., Li W., Deng X., Chen X., et al. (2009). Two-dimensional blue native/SDS-PAGE analysis reveals heat shock protein chaperone machinery involved in hepatitis B virus production in HepG2.2.15 cells. Mol. Cell Proteomics 8 495–505. 10.1074/mcp.M800250-MCP200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang J., Yang X., Jiao T., Zhao X., Li W., et al. (2017). HDM2 Promotes NEDDylation of Hepatitis B Virus HBx To Enhance Its Stability and Function. J. Virol. 91 340–317. 10.1128/JVI.00340-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X. Y., Tang S. H., Wu S. L., Luo Y. H., Cao M. R., Zhou H. K., et al. (2015). Epigenetic modulation of insulin-like growth factor-II overexpression by hepatitis B virus X protein in hepatocellular carcinoma. Am. J. Cancer Res. 5 956–978. [PMC free article] [PubMed] [Google Scholar]
- Loffler-Mary H., Dumortier J., Klentsch-Zimmer C., Prange R. (2000). Hepatitis B virus assembly is sensitive to changes in the cytosolic S loop of the envelope proteins. Virology 270 358–367. 10.1006/viro.2000.0268 [DOI] [PubMed] [Google Scholar]
- Loffler-Mary H., Werr M., Prange R. (1997). Sequence-specific repression of cotranslational translocation of the hepatitis B virus envelope proteins coincides with binding of heat shock protein Hsc70. Virology 235 144–152. 10.1006/viro.1997.8689 [DOI] [PubMed] [Google Scholar]
- Long Q., Yan R., Hu J., Cai D., Mitra B., Kim E. S., et al. (2017). The role of host DNA ligases in hepadnavirus covalently closed circular DNA formation. PLoS Pathog. 13:e1006784. 10.1371/journal.ppat.1006784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lott L., Beames B., Notvall L., Lanford R. E. (2000). Interaction between hepatitis B virus core protein and reverse transcriptase. J. Virol. 74 11479–11489. 10.1128/jvi.74.24.11479-11489.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y. Y., Cheng J., Yang Y. P., Liu Y., Wang L., Li K., et al. (2005). Cloning and characterization of a novel hepatitis B virus core binding protein C12. World J. Gastroenterol. 11 5666–5671. 10.3748/wjg.v11.i36.5666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Z. P., Xiao Z. L., Yang Z., Li J., Feng G. X., Chen F. Q., et al. (2015). Hepatitis B virus X protein promotes human hepatoma cell growth via upregulation of transcription factor AP2alpha and sphingosine kinase 1. Acta Pharmacol. Sin. 36 1228–1236. 10.1038/aps.2015.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luber B., Lauer U., Weiss L., Hohne M., Hofschneider P. H., Kekule A. S. (1993). The hepatitis B virus transactivator HBx causes elevation of diacylglycerol and activation of protein kinase C. Res. Virol. 144 311–321. [DOI] [PubMed] [Google Scholar]
- Lubyova B., Hodek J., Zabransky A., Prouzova H., Hubalek M., Hirsch I., et al. (2017). PRMT5: A novel regulator of Hepatitis B virus replication and an arginine methylase of HBV core. PLoS One 12:e0186982. 10.1371/journal.pone.0186982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucifora J., Esser K., Protzer U. (2013). Ezetimibe blocks hepatitis B virus infection after virus uptake into hepatocytes. Antiviral. Res. 97 195–197. 10.1016/j.antiviral.2012.12.008 [DOI] [PubMed] [Google Scholar]
- Lucifora J., Xia Y., Reisinger F., Zhang K., Stadler D., Cheng X., et al. (2014). Specific and nonhepatotoxic degradation of nuclear hepatitis B virus cccDNA. Science 343 1221–1228. 10.1126/science.1243462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludgate L., Adams C., Hu J. (2011). Phosphorylation state-dependent interactions of hepadnavirus core protein with host factors. PLoS One 6:e29566. 10.1371/journal.pone.0029566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X., Huang Y., Chen Y., Tu Z., Hu J., Tavis J. E., et al. (2016). Association of Hepatitis B Virus Covalently Closed Circular DNA and Human APOBEC3B in Hepatitis B Virus-Related Hepatocellular Carcinoma. PLoS One 11:e0157708. 10.1371/journal.pone.0157708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv M., Zhang B., Shi Y., Han Z., Zhang Y., Zhou Y., et al. (2015). Identification of BST-2/tetherin-induced hepatitis B virus restriction and hepatocyte-specific BST-2 inactivation. Sci. Rep. 5:11736. 10.1038/srep11736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lwa S. H., Chen W. N. (2005). Hepatitis B virus X protein interacts with beta5 subunit of heterotrimeric guanine nucleotide binding protein. Virol. J. 2:76. 10.1186/1743-422X-2-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lythgoe K. A., Lumley S. F., Pellis L., Mckeating J. A., Matthews P. C. (2021). Estimating hepatitis B virus cccDNA persistence in chronic infection. Virus Evol. 7:veaa063. 10.1093/ve/veaa063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macovei A., Petrareanu C., Lazar C., Florian P., Branza-Nichita N. (2013). Regulation of hepatitis B virus infection by Rab5, Rab7, and the endolysosomal compartment. J. Virol. 87 6415–6427. 10.1128/JVI.00393-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macovei A., Radulescu C., Lazar C., Petrescu S., Durantel D., Dwek R. A., et al. (2010). Hepatitis B virus requires intact caveolin-1 function for productive infection in HepaRG cells. J. Virol. 84 243–253. 10.1128/JVI.01207-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire H. F., Hoeffler J. P., Siddiqui A. (1991). HBV X protein alters the DNA binding specificity of CREB and ATF-2 by protein-protein interactions. Science 252 842–844. 10.1126/science.1827531 [DOI] [PubMed] [Google Scholar]
- Makokha G. N., Abe-Chayama H., Chowdhury S., Hayes C. N., Tsuge M., Yoshima T., et al. (2019). Regulation of the Hepatitis B virus replication and gene expression by the multi-functional protein TARDBP. Sci. Rep. 9:8462. 10.1038/s41598-019-44934-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minor M. M., Hollinger F. B., Mcnees A. L., Jung S. Y., Jain A., Hyser J. M., et al. (2020). Hepatitis B Virus HBx Protein Mediates the Degradation of Host Restriction Factors through the Cullin 4 DDB1 E3 Ubiquitin Ligase Complex. Cells 9:9040834. 10.3390/cells9040834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina-Jimenez F., Benedicto I., Murata M., Martin-Vilchez S., Seki T., Antonio Pintor-Toro J., et al. (2010). Expression of pituitary tumor-transforming gene 1 (PTTG1)/securin in hepatitis B virus (HBV)-associated liver diseases: evidence for an HBV X protein-mediated inhibition of PTTG1 ubiquitination and degradation. Hepatology 51 777–787. 10.1002/hep.23468 [DOI] [PubMed] [Google Scholar]
- Mueller H., Lopez A., Tropberger P., Wildum S., Schmaler J., Pedersen L., et al. (2019). PAPD5/7 Are Host Factors That Are Required for Hepatitis B Virus RNA Stabilization. Hepatology 69 1398–1411. 10.1002/hep.30329 [DOI] [PubMed] [Google Scholar]
- Mukherji A., Janbandhu V. C., Kumar V. (2007). HBx-dependent cell cycle deregulation involves interaction with cyclin E/A-cdk2 complex and destabilization of p27Kip1. Biochem. J. 401 247–256. 10.1042/BJ20061091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy C. M., Xu Y., Li F., Nio K., Reszka-Blanco N., Li X., et al. (2016). Hepatitis B Virus X Protein Promotes Degradation of SMC5/6 to Enhance HBV Replication. Cell Rep. 16 2846–2854. 10.1016/j.celrep.2016.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na T. Y., Ka N. L., Rhee H., Kyeong D., Kim M. H., Seong J. K., et al. (2016). Interaction of hepatitis B virus X protein with PARP1 results in inhibition of DNA repair in hepatocellular carcinoma. Oncogene 35 5435–5445. 10.1038/onc.2016.82 [DOI] [PubMed] [Google Scholar]
- Newbold J. E., Xin H., Tencza M., Sherman G., Dean J., Bowden S., et al. (1995). The covalently closed duplex form of the hepadnavirus genome exists in situ as a heterogeneous population of viral minichromosomes. J. Virol. 69 3350–3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen D. H., Gummuluru S., Hu J. (2007). Deamination-independent inhibition of hepatitis B virus reverse transcription by APOBEC3G. J. Virol. 81 4465–4472. 10.1128/JVI.02510-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen D. H., Ludgate L., Hu J. (2008). Hepatitis B virus-cell interactions and pathogenesis. J. Cell Physiol. 216 289–294. 10.1002/jcp.21416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu C., Livingston C. M., Li L., Beran R. K., Daffis S., Ramakrishnan D., et al. (2017). The Smc5/6 Complex Restricts HBV when Localized to ND10 without Inducing an Innate Immune Response and Is Counteracted by the HBV X Protein Shortly after Infection. PLoS One 12:e0169648. 10.1371/journal.pone.0169648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu Y., Wu Z., Shen Q., Song J., Luo Q., You H., et al. (2013). Hepatitis B virus X protein co-activates pregnane X receptor to induce the cytochrome P450 3A4 enzyme, a potential implication in hepatocarcinogenesis. Dig. Liver Dis. 45 1041–1048. 10.1016/j.dld.2013.06.004 [DOI] [PubMed] [Google Scholar]
- Niu Y., Xu M., Slagle B. L., Huang H., Li S., Guo G. L., et al. (2017). Farnesoid X receptor ablation sensitizes mice to hepatitis b virus X protein-induced hepatocarcinogenesis. Hepatology 65 893–906. 10.1002/hep.28924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkongolo S., Ni Y., Lempp F. A., Kaufman C., Lindner T., Esser-Nobis K., et al. (2014). Cyclosporin A inhibits hepatitis B and hepatitis D virus entry by cyclophilin-independent interference with the NTCP receptor. J. Hepatol. 60 723–731. 10.1016/j.jhep.2013.11.022 [DOI] [PubMed] [Google Scholar]
- Nkongolo S., Nussbaum L., Lempp F. A., Wodrich H., Urban S., Ni Y. (2019). The retinoic acid receptor (RAR) alpha-specific agonist Am80 (tamibarotene) and other RAR agonists potently inhibit hepatitis B virus transcription from cccDNA. Antiviral. Res. 168 146–155. 10.1016/j.antiviral.2019.04.009 [DOI] [PubMed] [Google Scholar]
- Ohno H., Kaneko S., Lin Y., Kobayashi K., Murakami S. (1999). Human hepatitis B virus X protein augments the DNA binding of nuclear factor for IL-6 through its basic-leucine zipper domain. J. Med. Virol. 58 11–18. [DOI] [PubMed] [Google Scholar]
- Ori A., Atzmony D., Haviv I., Shaul Y. (1994). An NF1 motif plays a central role in hepatitis B virus enhancer. Virology 204 600–608. 10.1006/viro.1994.1574 [DOI] [PubMed] [Google Scholar]
- Osseman Q., Gallucci L., Au S., Cazenave C., Berdance E., Blondot M. L., et al. (2018). The chaperone dynein LL1 mediates cytoplasmic transport of empty and mature hepatitis B virus capsids. J. Hepatol. 68 441–448. 10.1016/j.jhep.2017.10.032 [DOI] [PubMed] [Google Scholar]
- Pang R., Lee T. K., Poon R. T., Fan S. T., Wong K. B., Kwong Y. L., et al. (2007). Pin1 interacts with a specific serine-proline motif of hepatitis B virus X-protein to enhance hepatocarcinogenesis. Gastroenterology 132 1088–1103. 10.1053/j.gastro.2006.12.030 [DOI] [PubMed] [Google Scholar]
- Pante N., Kann M. (2002). Nuclear pore complex is able to transport macromolecules with diameters of about 39 nm. Mol. Biol. Cell 13 425–434. 10.1091/mbc.01-06-0308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei D. Q., Shih C. H. (1990). Transcriptional activation and repression by cellular DNA-binding protein C/EBP. J. Virol. 64 1517–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips S., Chokshi S., Chatterji U., Riva A., Bobardt M., Williams R., et al. (2015). Alisporivir inhibition of hepatocyte cyclophilins reduces HBV replication and hepatitis B surface antigen production. Gastroenterology 148 403–414e407. 10.1053/j.gastro.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollicino T., Belloni L., Raffa G., Pediconi N., Squadrito G., Raimondo G., et al. (2006). Hepatitis B virus replication is regulated by the acetylation status of hepatitis B virus cccDNA-bound H3 and H4 histones. Gastroenterology 130 823–837. 10.1053/j.gastro.2006.01.001 [DOI] [PubMed] [Google Scholar]
- Qadri I., Fatima K., Abde L. H. H. (2011). Hepatitis B virus X protein impedes the DNA repair via its association with transcription factor, TFIIH. BMC Microbiol. 11:48. 10.1186/1471-2180-11-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qadri I., Maguire H. F., Siddiqui A. (1995). Hepatitis B virus transactivator protein X interacts with the TATA-binding protein. Proc. Natl. Acad. Sci. U S A 92 1003–1007. 10.1073/pnas.92.4.1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi Y., Gao Z., Xu G., Peng B., Liu C., Yan H., et al. (2016). DNA Polymerase kappa Is a Key Cellular Factor for the Formation of Covalently Closed Circular DNA of Hepatitis B Virus. PLoS Pathog. 12:e1005893. 10.1371/journal.ppat.1005893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian G., Hu B., Zhou D., Xuan Y., Bai L., Duan C. (2015). NIRF, a Novel Ubiquitin Ligase, Inhibits Hepatitis B Virus Replication Through Effect on HBV Core Protein and H3 Histones. DNA Cell Biol. 34 327–332. 10.1089/dna.2014.2714 [DOI] [PubMed] [Google Scholar]
- Qian G., Jin F., Chang L., Yang Y., Peng H., Duan C. (2012). NIRF, a novel ubiquitin ligase, interacts with hepatitis B virus core protein and promotes its degradation. Biotechnol. Lett. 34 29–36. 10.1007/s10529-011-0751-0 [DOI] [PubMed] [Google Scholar]
- Qiao Y., Han X., Guan G., Wu N., Sun J., Pak V., et al. (2016). TGF-beta triggers HBV cccDNA degradation through AID-dependent deamination. FEBS Lett. 590 419–427. 10.1002/1873-3468.12058 [DOI] [PubMed] [Google Scholar]
- Qin D., Li K., Qu J., Wang S., Zou C., Sheng Y., et al. (2013). HBx and HBs regulate RhoC expression by upregulating transcription factor Ets-1. Arch. Virol. 158 1773–1781. 10.1007/s00705-013-1655-1 [DOI] [PubMed] [Google Scholar]
- Quarleri J. (2014). Core promoter: a critical region where the hepatitis B virus makes decisions. World J. Gastroenterol. 20 425–435. 10.3748/wjg.v20.i2.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quasdorff M., Protzer U. (2010). Control of hepatitis B virus at the level of transcription. J. Viral. Hepat. 17 527–536. 10.1111/j.1365-2893.2010.01315.x [DOI] [PubMed] [Google Scholar]
- Rahmani Z., Huh K. W., Lasher R., Siddiqui A. (2000). Hepatitis B virus X protein colocalizes to mitochondria with a human voltage-dependent anion channel, HVDAC3, and alters its transmembrane potential. J. Virol. 74 2840–2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawat S., Bouchard M. J. (2015). The hepatitis B virus (HBV) HBx protein activates AKT to simultaneously regulate HBV replication and hepatocyte survival. J. Virol. 89 999–1012. 10.1128/JVI.02440-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razanskas R., Sasnauskas K. (2010). Interaction of hepatitis B virus core protein with human GIPC1. Arch. Virol. 155 247–250. 10.1007/s00705-009-0561-z [DOI] [PubMed] [Google Scholar]
- Ren J. H., Hu J. L., Cheng S. T., Yu H. B., Wong V. K. W., Law B. Y. K., et al. (2018). SIRT3 restricts hepatitis B virus transcription and replication through epigenetic regulation of covalently closed circular DNA involving suppressor of variegation 3-9 homolog 1 and SET domain containing 1A histone methyltransferases. Hepatology 68, 1260–1276. 10.1002/hep.29912 [DOI] [PubMed] [Google Scholar]
- Ren J. H., Tao Y., Zhang Z. Z., Chen W. X., Cai X. F., Chen K., et al. (2014). Sirtuin 1 regulates hepatitis B virus transcription and replication by targeting transcription factor AP-1. J. Virol. 88 2442–2451. 10.1128/JVI.02861-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riviere L., Gerossier L., Ducroux A., Dion S., Deng Q., Michel M. L., et al. (2015). HBx relieves chromatin-mediated transcriptional repression of hepatitis B viral cccDNA involving SETDB1 histone methyltransferase. J. Hepatol. 63 1093–1102. 10.1016/j.jhep.2015.06.023 [DOI] [PubMed] [Google Scholar]
- Rost M., Mann S., Lambert C., Doring T., Thome N., Prange R. (2006). Gamma-adaptin, a novel ubiquitin-interacting adaptor, and Nedd4 ubiquitin ligase control hepatitis B virus maturation. J. Biol. Chem. 281 29297–29308. 10.1074/jbc.M603517200 [DOI] [PubMed] [Google Scholar]
- Rui E., Moura P. R., Goncalves K. A., Rooney R. J., Kobarg J. (2006). Interaction of the hepatitis B virus protein HBx with the human transcription regulatory protein p120E4F in vitro. Virus Res. 115 31–42. 10.1016/j.virusres.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Saeed U., Kim J., Piracha Z. Z., Kwon H., Jung J., Chwae Y. J., et al. (2018). Parvulin 14 and parvulin 17 bind to HBx and cccDNA and upregulate HBV replication from cccDNA to virion in a HBx-dependent manner. J. Virol. 2018:18. 10.1128/JVI.01840-18 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Salerno D., Chiodo L., Alfano V., Floriot O., Cottone G., Paturel A., et al. (2020). Hepatitis B protein HBx binds the DLEU2 lncRNA to sustain cccDNA and host cancer-related gene transcription. Gut 69 2016–2024. 10.1136/gutjnl-2019-319637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saracco G., Rizzetto M., Verme G. (1994). Interferon in chronic hepatitis B. Antiviral. Res. 24 137–143. 10.1016/0166-3542(94)90062-0 [DOI] [PubMed] [Google Scholar]
- Saxena N., Kumar V. (2014). The HBx oncoprotein of hepatitis B virus deregulates the cell cycle by promoting the intracellular accumulation and re-compartmentalization of the cellular deubiquitinase USP37. PLoS One 9:e111256. 10.1371/journal.pone.0111256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz A., Schwarz A., Foss M., Zhou L., Rabe B., Hoellenriegel J., et al. (2010). Nucleoporin 153 arrests the nuclear import of hepatitis B virus capsids in the nuclear basket. PLoS Pathog. 6:e1000741. 10.1371/journal.ppat.1000741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiner S., Nassal M. (2017). A Role for the Host DNA Damage Response in Hepatitis B Virus cccDNA Formation-and Beyond? Viruses 9:9050125. 10.3390/v9050125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulze A., Gripon P., Urban S. (2007). Hepatitis B virus infection initiates with a large surface protein-dependent binding to heparan sulfate proteoglycans. Hepatology 46 1759–1768. 10.1002/hep.21896 [DOI] [PubMed] [Google Scholar]
- Schulze A., Schieck A., Ni Y., Mier W., Urban S. (2010). Fine mapping of pre-S sequence requirements for hepatitis B virus large envelope protein-mediated receptor interaction. J. Virol. 84 1989–2000. 10.1128/JVI.01902-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweitzer A., Horn J., Mikolajczyk R. T., Krause G., Ott J. J. (2015). Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet 386 1546–1555. 10.1016/S0140-6736(15)61412-X [DOI] [PubMed] [Google Scholar]
- Sekiba K., Otsuka M., Ohno M., Yamagami M., Kishikawa T., Seimiya T., et al. (2019b). Pevonedistat, a Neuronal Precursor Cell-Expressed Developmentally Down-Regulated Protein 8-Activating Enzyme Inhibitor, Is a Potent Inhibitor of Hepatitis B Virus. Hepatology 69 1903–1915. 10.1002/hep.30491 [DOI] [PubMed] [Google Scholar]
- Sekiba K., Otsuka M., Ohno M., Yamagami M., Kishikawa T., Suzuki T., et al. (2019a). Inhibition of HBV Transcription From cccDNA With Nitazoxanide by Targeting the HBx-DDB1 Interaction. Cell Mol. Gastroenterol. Hepatol. 7 297–312. 10.1016/j.jcmgh.2018.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzer L., Zlotnick A. (2015). Assembly and Release of Hepatitis B Virus. Cold Spring Harb. Perspect. Med. 5:21394. 10.1101/cshperspect.a021394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo H. W., Seo J. P., Jung G. (2018). Heat shock protein 70 and heat shock protein 90 synergistically increase hepatitis B viral capsid assembly. Biochem. Biophys. Res. Commun. 503 2892–2898. 10.1016/j.bbrc.2018.08.065 [DOI] [PubMed] [Google Scholar]
- Sheraz M., Cheng J., Tang L., Chang J., Guo J. T. (2019). Cellular DNA Topoisomerases Are Required for the Synthesis of Hepatitis B Virus Covalently Closed Circular DNA. J. Virol. 93:2218. 10.1128/JVI.02230-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Zhang H., Han Z., Mi X., Zhang W., Lv M. (2016). HBx interacted with Smad4 to deprive activin a growth inhibition function in hepatocyte HL7702 on CRM1 manner. Tumour Biol. 37 3405–3415. 10.1007/s13277-015-4076-9 [DOI] [PubMed] [Google Scholar]
- Shim H. Y., Quan X., Yi Y. S., Jung G. (2011). Heat shock protein 90 facilitates formation of the HBV capsid via interacting with the HBV core protein dimers. Virology 410 161–169. 10.1016/j.virol.2010.11.005 [DOI] [PubMed] [Google Scholar]
- Shimura S., Watashi K., Fukano K., Peel M., Sluder A., Kawai F., et al. (2017). Cyclosporin derivatives inhibit hepatitis B virus entry without interfering with NTCP transporter activity. J. Hepatol. 66 685–692. 10.1016/j.jhep.2016.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin G. C., Ahn S. H., Choi H. S., Lim K. H., Choi D. Y., Kim K. P., et al. (2013). Hepatocystin/80K-H inhibits replication of hepatitis B virus through interaction with HBx protein in hepatoma cell. Biochim. Biophys. Acta 1832 1569–1581. 10.1016/j.bbadis.2013.04.026 [DOI] [PubMed] [Google Scholar]
- Shon J. K., Shon B. H., Park I. Y., Lee S. U., Fa L., Chang K. Y., et al. (2009). Hepatitis B virus-X protein recruits histone deacetylase 1 to repress insulin-like growth factor binding protein 3 transcription. Virus Res. 139 14–21. 10.1016/j.virusres.2008.09.006 [DOI] [PubMed] [Google Scholar]
- Shukla R., Yue J., Siouda M., Gheit T., Hantz O., Merle P., et al. (2011). Proinflammatory cytokine TNF-alpha increases the stability of hepatitis B virus X protein through NF-kappaB signaling. Carcinogenesis 32 978–985. 10.1093/carcin/bgr057 [DOI] [PubMed] [Google Scholar]
- Sohn S. Y., Kim S. B., Kim J., Ahn B. Y. (2006). Negative regulation of hepatitis B virus replication by cellular Hsp40/DnaJ proteins through destabilization of viral core and X proteins. J. Gen. Virol. 87 1883–1891. 10.1099/vir.0.81684-0 [DOI] [PubMed] [Google Scholar]
- Srisuttee R., Koh S. S., Kim S. J., Malilas W., Boonying W., Cho I. R., et al. (2012). Hepatitis B virus X (HBX) protein upregulates beta-catenin in a human hepatic cell line by sequestering SIRT1 deacetylase. Oncol. Rep. 28 276–282. 10.3892/or.2012.1798 [DOI] [PubMed] [Google Scholar]
- Stavrou S., Ross S. R. (2015). APOBEC3 Proteins in Viral Immunity. J. Immunol. 195 4565–4570. 10.4049/jimmunol.1501504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su Z. J., Cao J. S., Wu Y. F., Chen W. N., Lin X., Wu Y. L., et al. (2017). Deubiquitylation of hepatitis B virus X protein (HBx) by ubiquitin-specific peptidase 15 (USP15) increases HBx stability and its transactivation activity. Sci. Rep. 7:40246. 10.1038/srep40246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers J., O’connell A., Millman I. (1975). Genome of hepatitis B virus: restriction enzyme cleavage and structure of DNA extracted from Dane particles. Proc. Natl. Acad. Sci. U S A 72 4597–4601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers J., Smith P. M., Horwich A. L. (1990). Hepadnavirus envelope proteins regulate covalently closed circular DNA amplification. J. Virol. 64 2819–2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tacke F., Liedtke C., Bocklage S., Manns M. P., Trautwein C. (2005). CREB/PKA sensitive signalling pathways activate and maintain expression levels of the hepatitis B virus pre-S2/S promoter. Gut 54 1309–1317. 10.1136/gut.2005.065086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan T. L., Fang N., Neo T. L., Singh P., Zhang J., Zhou R., et al. (2008). Rac1 GTPase is activated by hepatitis B virus replication–involvement of HBX. Biochim. Biophys. Acta 1783 360–374. 10.1016/j.bbamcr.2007.10.024 [DOI] [PubMed] [Google Scholar]
- Tan T. L., Feng Z., Lu Y. W., Chan V., Chen W. N. (2006). Adhesion contact kinetics of HepG2 cells during Hepatitis B virus replication: Involvement of SH3-binding motif in HBX. Biochim. Biophys. Acta 1762 755–766. 10.1016/j.bbadis.2006.06.016 [DOI] [PubMed] [Google Scholar]
- Tan Z., Pionek K., Unchwaniwala N., Maguire M. L., Loeb D. D., Zlotnick A. (2015). The interface between hepatitis B virus capsid proteins affects self-assembly, pregenomic RNA packaging, and reverse transcription. J. Virol 89, 3275–3284. 10.1128/JVI.03545-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y., Kanai F., Ichimura T., Tateishi K., Asaoka Y., Guleng B., et al. (2006). The hepatitis B virus X protein enhances AP-1 activation through interaction with Jab1. Oncogene 25 633–642. 10.1038/sj.onc.1209093 [DOI] [PubMed] [Google Scholar]
- Tanaka Y., Kanai F., Kawakami T., Tateishi K., Ijichi H., Kawabe T., et al. (2004). Interaction of the hepatitis B virus X protein (HBx) with heat shock protein 60 enhances HBx-mediated apoptosis. Biochem. Biophys. Res. Commun. 318 461–469. 10.1016/j.bbrc.2004.04.046 [DOI] [PubMed] [Google Scholar]
- Tang H. M., Gao W. W., Chan C. P., Cheng Y., Chaudhary V., Deng J. J., et al. (2014). Requirement of CRTC1 coactivator for hepatitis B virus transcription. Nucleic Acids Res. 42 12455–12468. 10.1093/nar/gku925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y., Zhang Y., Wang C., Sun Z., Li L., Dong J., et al. (2018). 14-3-3zeta binds to hepatitis B virus protein X and maintains its protein stability in hepatocellular carcinoma cells. Cancer Med. 7 5543–5553. 10.1002/cam4.1512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian X., Zhao C., Zhu H., She W., Zhang J., Liu J., et al. (2010). Hepatitis B virus (HBV) surface antigen interacts with and promotes cyclophilin a secretion: possible link to pathogenesis of HBV infection. J. Virol. 84 3373–3381. 10.1128/JVI.02555-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian X., Zhao F., Sun W., Zhi X., Cheng Z., Zhou M., et al. (2014). CRTC2 enhances HBV transcription and replication by inducing PGC1alpha expression. Virol. J. 11:30. 10.1186/1743-422X-11-30:10.1186/1743-422X-11-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokusumi Y., Zhou S., Takada S. (2004). Nuclear respiratory factor 1 plays an essential role in transcriptional initiation from the hepatitis B virus x gene promoter. J. Virol. 78 10856–10864. 10.1128/JVI.78.20.10856-10864.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tropberger P., Mercier A., Robinson M., Zhong W., Ganem D. E., Holdorf M. (2015). Mapping of histone modifications in episomal HBV cccDNA uncovers an unusual chromatin organization amenable to epigenetic manipulation. Proc. Natl. Acad. Sci. U S A 112 E5715–E5724. 10.1073/pnas.1518090112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuttleman J. S., Pourcel C., Summers J. (1986). Formation of the pool of covalently closed circular viral DNA in hepadnavirus-infected cells. Cell 47 451–460. [DOI] [PubMed] [Google Scholar]
- Umetsu T., Inoue J., Kogure T., Kakazu E., Ninomiya M., Iwata T., et al. (2018). Inhibitory effect of silibinin on hepatitis B virus entry. Biochem. Biophys. Rep. 14 20–25. 10.1016/j.bbrep.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbossche J., Jessner W., Van Den Boer M., Biewenga J., Berke J. M., Talloen W., et al. (2019). Pharmacokinetics, Safety and Tolerability of JNJ-56136379, a Novel Hepatitis B Virus Capsid Assembly Modulator, in Healthy Subjects. Adv. Ther. 36 2450–2462. 10.1007/s12325-019-01017-1 [DOI] [PubMed] [Google Scholar]
- Voss T. C., Hager G. L. (2014). Dynamic regulation of transcriptional states by chromatin and transcription factors. Nat. Rev. Genet. 15 69–81. 10.1038/nrg3623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Jia J., Chen R., Ding S., Xu Q., Zhang T., et al. (2018). RFX1 participates in doxorubicin-induced hepatitis B virus reactivation. Cancer Med. 7 2021–2033. 10.1002/cam4.1468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L. Z., Qihui Z., Jing Y., Zhipeng F., Andrew Y., John G. (2019). PS-074-A first-in-class orally available HBV cccDNA destabilizer ccc_R08 achieved sustainable HBsAg and HBV DNA suppression in the HBV circle mouse model through elimination of cccDNA-like molecules in the mouse liver. J. Hepatol. 70:e48. 10.1016/S0618-8278(19)30086-6 [DOI] [Google Scholar]
- Wang X., Li Y., Mao A., Li C., Li Y., Tien P. (2010). Hepatitis B virus X protein suppresses virus-triggered IRF3 activation and IFN-beta induction by disrupting the VISA-associated complex. Cell Mol. Immunol. 7 341–348. 10.1038/cmi.2010.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Zhou Y., Sun L., Chen W., Li X., Wang Q., et al. (2008). Complex formation between heat shock protein 72 and hepatitis B virus X protein in hepatocellular carcinoma tissues. J. Proteome Res. 7 5133–5137. 10.1021/pr800435g [DOI] [PubMed] [Google Scholar]
- Wang Y. P., Liu F., He H. W., Han Y. X., Peng Z. G., Li B. W., et al. (2010). Heat stress cognate 70 host protein as a potential drug target against drug resistance in hepatitis B virus. Antimicrob. Agents Chemother. 54 2070–2077. 10.1128/AAC.01764-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Cai J., Zeng X., Chen Y., Yan W., Ouyang Y., et al. (2015). Downregulation of toll-like receptor 4 induces suppressive effects on hepatitis B virus-related hepatocellular carcinoma via ERK1/2 signaling. BMC Cancer 15:821. 10.1186/s12885-015-1866-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Han M., Liu S., Yuan X., Zhao J., Lu H., et al. (2021). S6K1 inhibits HBV replication through inhibiting AMPK-ULK1 pathway and disrupting acetylation modification of H3K27. Life Sci. 265:118848. 10.1016/j.lfs.2020.118848 [DOI] [PubMed] [Google Scholar]
- Waris G., Huh K. W., Siddiqui A. (2001). Mitochondrially associated hepatitis B virus X protein constitutively activates transcription factors STAT-3 and NF-kappa B via oxidative stress. Mol. Cell Biol. 21 7721–7730. 10.1128/MCB.21.22.7721-7730.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe T., Sorensen E. M., Naito A., Schott M., Kim S., Ahlquist P. (2007). Involvement of host cellular multivesicular body functions in hepatitis B virus budding. Proc. Natl. Acad. Sci. U S A 104 10205–10210. 10.1073/pnas.0704000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watashi K., Urban S., Li W., Wakita T. (2014). NTCP and beyond: opening the door to unveil hepatitis B virus entry. Int. J. Mol. Sci. 15 2892–2905. 10.3390/ijms15022892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei L., Ploss A. (2020). Core components of DNA lagging strand synthesis machinery are essential for hepatitis B virus cccDNA formation. Nat. Microbiol. 5 715–726. 10.1038/s41564-020-0678-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Y., Golubkov V. S., Strongin A. Y., Jiang W., Reed J. C. (2008). Interaction of hepatitis B viral oncoprotein with cellular target HBXIP dysregulates centrosome dynamics and mitotic spindle formation. J. Biol. Chem. 283 2793–2803. 10.1074/jbc.M708419200 [DOI] [PubMed] [Google Scholar]
- Werle-Lapostolle B., Bowden S., Locarnini S., Wursthorn K., Petersen J., Lau G., et al. (2004). Persistence of cccDNA during the natural history of chronic hepatitis B and decline during adefovir dipivoxil therapy. Gastroenterology 126 1750–1758. 10.1053/j.gastro.2004.03.018 [DOI] [PubMed] [Google Scholar]
- Werr M., Prange R. (1998). Role for calnexin and N-linked glycosylation in the assembly and secretion of hepatitis B virus middle envelope protein particles. J. Virol. 72 778–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2017). Global hepatitis report, 2017. Geneva: World Health Organization. [Google Scholar]
- Wu T. T., Coates L., Aldrich C. E., Summers J., Mason W. S. (1990). In hepatocytes infected with duck hepatitis B virus, the template for viral RNA synthesis is amplified by an intracellular pathway. Virology 175 255–261. [DOI] [PubMed] [Google Scholar]
- Wu Y. H., Ai X., Liu F. Y., Liang H. F., Zhang B. X., Chen X. P. (2016). c-Jun N-terminal kinase inhibitor favors transforming growth factor-beta to antagonize hepatitis B virus X protein-induced cell growth promotion in hepatocellular carcinoma. Mol. Med. Rep. 13 1345–1352. 10.3892/mmr.2015.4644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia L., Wang S., Zhang H., Yang Y., Wei J., Shi Y., et al. (2020). The HBx and HBc of hepatitis B virus can influence Id1 and Id3 by reducing their transcription and stability. Virus Res. 284:197973. 10.1016/j.virusres.2020.197973 [DOI] [PubMed] [Google Scholar]
- Xian L., Zhao J., Wang J., Fang Z., Peng B., Wang W., et al. (2010). p53 Promotes proteasome-dependent degradation of oncogenic protein HBx by transcription of MDM2. Mol. Biol. Rep. 37 2935–2940. 10.1007/s11033-009-9855-1 [DOI] [PubMed] [Google Scholar]
- Xiang A., Ren F., Lei X., Zhang J., Guo R., Lu Z., et al. (2015). The hepatitis B virus (HBV) core protein enhances the transcription activation of CRE via the CRE/CREB/CBP pathway. Antiviral. Res. 120 7–15. 10.1016/j.antiviral.2015.04.013 [DOI] [PubMed] [Google Scholar]
- Xu F., Song H., Xiao Q., Li N., Zhang H., Cheng G., et al. (2019). Type III interferon-induced CBFbeta inhibits HBV replication by hijacking HBx. Cell Mol. Immunol. 16 357–366. 10.1038/s41423-018-0006-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Wu Z., Tan S., Wang Z., Lin Q., Li X., et al. (2018). Tumor suppressor ZHX2 restricts hepatitis B virus replication via epigenetic and non-epigenetic manners. Antiviral. Res. 153 114–123. 10.1016/j.antiviral.2018.03.008 [DOI] [PubMed] [Google Scholar]
- Yan H., Peng B., He W., Zhong G., Qi Y., Ren B., et al. (2013). Molecular determinants of hepatitis B and D virus entry restriction in mouse sodium taurocholate cotransporting polypeptide. J. Virol. 87 7977–7991. 10.1128/JVI.03540-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H., Zhong G., Xu G., He W., Jing Z., Gao Z., et al. (2012). Sodium taurocholate cotransporting polypeptide is a functional receptor for human hepatitis B and D virus. Elife 1:e00049. 10.7554/eLife.00049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H., Zhong G., Xu G., He W., Jing Z., Gao Z., et al. (2014). Sodium taurocholate cotransporting polypeptide is a functional receptor for human hepatitis B and D virus. Elife 3:49. [DOI] [PubMed] [Google Scholar]
- Yang C. C., Huang E. Y., Li H. C., Su P. Y., Shih C. (2014). Nuclear export of human hepatitis B virus core protein and pregenomic RNA depends on the cellular NXF1-p15 machinery. PLoS One 9:e106683. 10.1371/journal.pone.0106683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S. T., Yen C. J., Lai C. H., Lin Y. J., Chang K. C., Lee J. C., et al. (2013). SUMOylated CPAP is required for IKK-mediated NF-kappaB activation and enhances HBx-induced NF-kappaB signaling in HCC. J. Hepatol. 58 1157–1164. 10.1016/j.jhep.2013.01.025 [DOI] [PubMed] [Google Scholar]
- Yao J. H., Liu Z. J., Yi J. H., Wang J., Liu Y. N. (2018). Hepatitis B Virus X Protein Upregulates Intracellular Calcium Signaling by Binding C-terminal of Orail Protein. Curr. Med. Sci. 38 26–34. 10.1007/s11596-018-1843-z [DOI] [PubMed] [Google Scholar]
- Yoo Y. G., Lee M. O. (2004). Hepatitis B virus X protein induces expression of Fas ligand gene through enhancing transcriptional activity of early growth response factor. J. Biol. Chem. 279 36242–36249. 10.1074/jbc.M401290200 [DOI] [PubMed] [Google Scholar]
- Yoo Y. G., Na T. Y., Seo H. W., Seong J. K., Park C. K., Shin Y. K., et al. (2008). Hepatitis B virus X protein induces the expression of MTA1 and HDAC1, which enhances hypoxia signaling in hepatocellular carcinoma cells. Oncogene 27 3405–3413. 10.1038/sj.onc.1211000 [DOI] [PubMed] [Google Scholar]
- You D. G., Cho Y. Y., Lee H. R., Lee J. H., Yu S. J., Yoon J. H., et al. (2019). Hepatitis B virus X protein induces size-selective membrane permeabilization through interaction with cardiolipin. Biochim. Biophys. Acta Biomembr. 1861 729–737. 10.1016/j.bbamem.2019.01.006 [DOI] [PubMed] [Google Scholar]
- Yu H. B., Cheng S. T., Ren F., Chen Y., Shi X. F., Wong V. K. W., et al. (2021). SIRT7 restricts HBV transcription and replication through catalyzing desuccinylation of histone H3 associated with cccDNA minichromosome. Clin. Sci. 135 1505–1522. 10.1042/CS20210392 [DOI] [PubMed] [Google Scholar]
- Yu X., Mertz J. E. (2003). Distinct modes of regulation of transcription of hepatitis B virus by the nuclear receptors HNF4alpha and COUP-TF1. J. Virol. 77 2489–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., He Z., Cao Y., Tang H., Huang F. (2016). TAGLN2, a novel regulator involved in Hepatitis B virus transcription and replication. Biochem. Biophys. Res. Commun. 477 1051–1058. 10.1016/j.bbrc.2016.07.034 [DOI] [PubMed] [Google Scholar]
- Yuan Y., Tian C., Gong Q., Shang L., Zhang Y., Jin C., et al. (2015). Interactome map reveals phospholipid scramblase 1 as a novel regulator of hepatitis B virus x protein. J. Proteome Res. 14 154–163. 10.1021/pr500943x [DOI] [PubMed] [Google Scholar]
- Zajakina A., Bruvere R., Kozlovska T. (2014). A Semliki Forest virus expression system as a model for investigating the nuclear import and export of hepatitis B virus nucleocapsid protein. Acta Virol. 58 173–179. 10.4149/av_2014_02_173 [DOI] [PubMed] [Google Scholar]
- Zhang J. L., Zhao W. G., Wu K. L., Wang K., Zhang X., Gu C. F., et al. (2005). Human hepatitis B virus X protein promotes cell proliferation and inhibits cell apoptosis through interacting with a serine protease Hepsin. Arch. Virol. 150 721–741. 10.1007/s00705-004-0446-0 [DOI] [PubMed] [Google Scholar]
- Zhang S., Lin R., Zhou Z., Wen S., Lin L., Chen S., et al. (2006). Macrophage migration inhibitory factor interacts with HBx and inhibits its apoptotic activity. Biochem. Biophys. Res. Commun. 342 671–679. 10.1016/j.bbrc.2006.01.180 [DOI] [PubMed] [Google Scholar]
- Zhang T., Xie N., He W., Liu R., Lei Y., Chen Y., et al. (2013). An integrated proteomics and bioinformatics analyses of hepatitis B virus X interacting proteins and identification of a novel interactor apoA-I. J. Proteomics 84 92–105. 10.1016/j.jprot.2013.03.028 [DOI] [PubMed] [Google Scholar]
- Zhang T., Zhang J., You X., Liu Q., Du Y., Gao Y., et al. (2012). Hepatitis B virus X protein modulates oncogene Yes-associated protein by CREB to promote growth of hepatoma cells. Hepatology 56 2051–2059. 10.1002/hep.25899 [DOI] [PubMed] [Google Scholar]
- Zhang W., Chen J., Wu M., Zhang X., Zhang M., Yue L., et al. (2017). PRMT5 restricts hepatitis B virus replication through epigenetic repression of covalently closed circular DNA transcription and interference with pregenomic RNA encapsidation. Hepatology 66 398–415. 10.1002/hep.29133 [DOI] [PubMed] [Google Scholar]
- Zhang W., Zhang X., Tian C., Wang T., Sarkis P. T., Fang Y., et al. (2008). Cytidine deaminase APOBEC3B interacts with heterogeneous nuclear ribonucleoprotein K and suppresses hepatitis B virus expression. Cell Microbiol. 10 112–121. 10.1111/j.1462-5822.2007.01020.x [DOI] [PubMed] [Google Scholar]
- Zhang Y. Y., Zhang B. H., Theele D., Litwin S., Toll E., Summers J. (2003). Single-cell analysis of covalently closed circular DNA copy numbers in a hepadnavirus-infected liver. Proc. Natl. Acad. Sci. U S A 100 12372–12377. 10.1073/pnas.2033898100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., He S., Guo J. J., Peng H., Fan J. H., Li Q. L. (2017). Retinoid X Receptor alpha-Dependent HBV Minichromosome Remodeling and Viral Replication. Ann. Hepatol. 16 501–509. 10.5604/01.3001.0010.0275 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Liu J., Liu H., He Y., Yi R., Niu Y., et al. (2015). Comparative study of the different activities of hepatitis B virus whole-X protein and HBx in hepatocarcinogenesis by proteomics and bioinformatics analysis. Arch Virol 160 1645–1656. 10.1007/s00705-015-2421-3 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Mao R., Yan R., Cai D., Zhang Y., Zhu H., et al. (2014). Transcription of hepatitis B virus covalently closed circular DNA is regulated by CpG methylation during chronic infection. PLoS One 9:e110442. 10.1371/journal.pone.0110442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Torii N., Furusaka A., Malayaman N., Hu Z., Liang T. J. (2000). Structural and functional characterization of interaction between hepatitis B virus X protein and the proteasome complex. J. Biol. Chem. 275 15157–15165. 10.1074/jbc.M910378199 [DOI] [PubMed] [Google Scholar]
- Zhao D., Wang X., Lou G., Peng G., Li J., Zhu H., et al. (2010). APOBEC3G directly binds Hepatitis B virus core protein in cell and cell free systems. Virus Res. 151 213–219. 10.1016/j.virusres.2010.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng D. L., Zhang L., Cheng N., Xu X., Deng Q., Teng X. M., et al. (2009). Epigenetic modification induced by hepatitis B virus X protein via interaction with de novo DNA methyltransferase DNMT3A. J. Hepatol. 50 377–387. 10.1016/j.jhep.2008.10.019 [DOI] [PubMed] [Google Scholar]
- Zheng Y., Chen W. L., Ma W. L., Chang C., Ou J. H. (2007). Enhancement of gene transactivation activity of androgen receptor by hepatitis B virus X protein. Virology 363 454–461. 10.1016/j.virol.2007.01.040:10.1016/j.virol.2007.01.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Ming P., Zhu C., Si Y., Xu S., Chen A., et al. (2019). Hepatitis B virus X protein-induced SH2 domain-containing 5(SH2D5) expression promotes hepatoma cell growth via an SH2D5-transketolase interaction. J. Biol. Chem. 2019:5739. 10.1074/jbc.RA118.005739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou D. X., Yen T. S. (1991). The ubiquitous transcription factor Oct-1 and the liver-specific factor HNF-1 are both required to activate transcription of a hepatitis B virus promoter. Mol. Cell Biol. 11 1353–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Tan T., Tian Y., Zheng B., Ou J. H., Huang E. J., et al. (2011). Kruppel-like factor 15 activates hepatitis B virus gene expression and replication. Hepatology 54 109–121. 10.1002/hep.24362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick A., Venkatakrishnan B., Tan Z., Lewellyn E., Turner W., Francis S. (2015). Core protein: A pleiotropic keystone in the HBV lifecycle. Antiviral. Res. 121 82–93. 10.1016/j.antiviral.2015.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L. Y., Zheng B. Y., Fang X. F., Li D., Huang Y. H., Chen Z. X., et al. (2015). HBx co-localizes with COXIII in HL-7702 cells to upregulate mitochondrial function and ROS generation. Oncol. Rep. 33 2461–2467. 10.3892/or.2015.3852 [DOI] [PubMed] [Google Scholar]