Abstract
Background:
Transportation noise is increasingly acknowledged as a cardiovascular risk factor, but the evidence base for an association with stroke is sparse.
Objective:
We aimed to investigate the association between transportation noise and stroke incidence in a large Scandinavian population.
Methods:
We harmonized and pooled data from nine Scandinavian cohorts (seven Swedish, two Danish), totaling 135,951 participants. We identified residential address history and estimated road, railway, and aircraft noise for all addresses. Information on stroke incidence was acquired through linkage to national patient and mortality registries. We analyzed data using Cox proportional hazards models, including socioeconomic and lifestyle confounders, and air pollution.
Results:
During follow-up (), 11,056 stroke cases were identified. Road traffic noise () was associated with risk of stroke, with a hazard ratio (HR) of 1.06 [95% confidence interval (CI): 1.03, 1.08] per 10-dB higher 5-y mean time-weighted exposure in analyses adjusted for individual- and area-level socioeconomic covariates. The association was approximately linear and persisted after adjustment for air pollution [particulate matter (PM) with an aerodynamic diameter of () and ]. Stroke was associated with moderate levels of 5-y aircraft noise exposure (40–50 vs. ) (; 95% CI: 0.99, 1.27), but not with higher exposure (, ; 95% CI: 0.79, 1.11). Railway noise was not associated with stroke.
Discussion:
In this pooled study, road traffic noise was associated with a higher risk of stroke. This finding supports road traffic noise as an important cardiovascular risk factor that should be included when estimating the burden of disease due to traffic noise. https://doi.org/10.1289/EHP8949
Introduction
Stroke is a leading cause of morbidity and mortality worldwide, and identification of new, modifiable risk factors is a crucial step in prevention (Zhang et al. 2019). Transportation noise is increasingly acknowledged as a risk factor for cardiovascular disease (Münzel et al. 2018). Noise is thought to act through an indirect pathway, with cognitive perception of noise followed by cortical activation, with sympathetic activation and release of corticoids, as well as via disturbance of sleep (Babisch 2002). This may result in oxidative stress, endothelial dysfunction, and low-grade inflammation, all of which are involved in the etiology of cardiovascular disease (Münzel et al. 2018). In addition, transportation noise has been associated with known cardiovascular risk factors such as obesity (Christensen et al. 2015; Pyko et al. 2017) and diabetes (Zare Sakhvidi et al. 2018).
When examining the epidemiological evidence for the role of transportation noise in developing cardiovascular disease, a 2018 World Health Organization (WHO) review concluded that there was an association between road traffic noise and ischemic heart disease { [95% confidence interval (CI): 1.01, 1.15] }, whereas for all other cardiovascular diseases, the evidence was insufficient to draw a conclusion (van Kempen et al. 2018). For stroke, the WHO identified only five prospective studies: One found road traffic noise to be associated with higher risk of stroke incidence, whereas the four other studies, all on cerebrovascular mortality, observed no association (van Kempen et al. 2018). Since the WHO review, a few additional studies on incidence, or mortality, or both, have been published (Andersson et al. 2020; Cai et al. 2018; Halonen et al. 2015; Héritier et al. 2017; Pyko et al. 2019; Seidler et al. 2018). Studies on stroke incidence have reported mixed results, with three suggesting a positive association with road traffic noise (Andersson et al. 2020; Halonen et al. 2015; Seidler et al. 2018), whereas two studies observed no association (Cai et al. 2018; Pyko et al. 2019). For railway noise, one study reported a slightly higher stroke risk (Seidler et al. 2018), whereas another study reported no association (Pyko et al. 2019), and for aircraft noise, two studies reported no association (Pyko et al. 2019; Seidler et al. 2018). Two very large registry-based studies in London and Switzerland reported potential associations between stroke mortality and road noise, and (in Switzerland) aircraft noise (Halonen et al. 2015; Héritier et al. 2017). The evidence base for stroke is, therefore, still limited, with discrepant results for different transportation noise sources, as well as for morbidity vs. mortality.
Because of the European population is exposed to transportation noise exceeding the Environmental Noise Directive threshold of 55 dB (European Environment Agency 2020), assessing the risk of stroke associated with transportation noise is important for future guiding of public health risk assessments. Hence, further large, prospective studies, with well-validated exposure and outcome data, are necessary to determine whether, and by how much, transportation noise increases stroke risk.
We aimed to investigate in a large, pooled study of nine Scandinavian cohorts, the association between transportation noise and stroke incidence and to explore the exposure–response function. Six of the nine cohorts have previously reported on associations between road traffic noise and stroke incidence, but the length of follow-up has been extended 5–7 y for four of these cohorts, thereby increasing the number of incident stroke cases.
Methods
Study Population
The present study was based on the Nordic Studies on Occupational and Traffic Noise in Relation to Disease (NordSOUND) project (https://www.cancer.dk/nordsound/). We pooled data from nine Scandinavian cohorts (seven Swedish, two Danish) after coding according to a common codebook. Harmonization and data checks were performed after data pooling.
Four of the cohorts were based in Stockholm County (Table S1): the Swedish National Study of Aging and Care in Kungsholmen (SNAC-K) (Lagergren et al. 2004), Stockholm Screening Across the Lifespan Twin Study (SALT) (Magnusson et al. 2013), Stockholm 60 years old study (Sixty) (Wändell et al. 2007), and the Stockholm Diabetes Prevention Program (SDPP) (Eriksson et al. 2008). These cohorts used identical methodology for environmental exposure assessment and harmonized covariate information within the Cardiovascular Effects of Air pollution and Noise Study (CEANS) (Pyko et al. 2019). The remaining cohorts were the Swedish Primary Prevention Cohort (PPS) (Wilhelmsen et al. 1986) and the Multinational Monitoring of Trends and Determinants in Cardiovascular Diseases cohort (GOT-MONICA) cohort (Wilhelmsen et al. 1997), both from Gothenburg, Sweden; the Malmö Diet and Cancer study (MDC; Malmö, Sweden) (Berglund et al. 1993); the Diet, Cancer and Health cohort (DCH; Copenhagen and Aarhus, Denmark) (Tjønneland et al. 2007); and the Danish Nurses Cohort (DNC) (Hundrup et al. 2012). All cohorts had registry-based residential address histories for participants (with addresses registered annually for the Swedish cohorts and exact dates of changes in residence for the Danish cohorts) and transportation noise exposure estimates for each address. Follow-up for the NordSOUND project was delayed if needed to ensure that each participant had 5 y of transportation noise data prior to the start of follow-up (the NordSOUND baseline).
Data collection and analysis for all cohorts were conducted in accordance with local and ethical requirements and followed the Helsinki Declaration. All participants provided informed consent.
Exposure Assessment
Noise levels at each address were calculated as the equivalent continuous A-weighted sound pressure level () at the most-exposed façade for day (0700–1900 hours), evening (1900–2200 hours), and night (2200–0700 hours), expressed as . Road and railway noise were estimated annually for the Gothenburg cohorts (PPS and GOT-MONICA), every 5 y for the Danish (DCH and DNC) and Stockholm cohorts (SDPP, Sixty, SNAC-K, and SALT), and every 10 y for the Malmö cohort (MDC). For the Danish, Stockholm, and Malmö cohorts, linear interpolation was used to estimate address-specific noise levels for intervening years and to calculate annual mean exposures for each year, from 5 y before enrollment to the end of follow-up.
Road traffic noise.
All cohorts modeled road traffic noise using the Nordic prediction method for road traffic noise (Bendtsen 1999). See Table S2 for further details. Input variables for each residence included geocodes, screening by terrain and buildings, and information on annual average daily traffic, distribution of light/heavy traffic, travel speed, and road type for all major road links. Furthermore, all cohorts but the Stockholm cohorts included traffic information from minor roads (i.e., roads with vehicles/d), and the Danish and Gothenburg cohorts additionally included information on noise barriers. Ground absorption was considered in all estimations.
Railway noise.
Railway noise was estimated for all cohorts using either the Nordic prediction method for railway noise or Nord2000, the updated version of this method (Plovsing and Kragh 2006). Noise was calculated for all addresses located within a buffer around railway (all cohorts), tram (Stockholm and Gothenburg), and metro lines (Stockholm and Copenhagen). Input variables included geocodes, screening by terrain and buildings, average number of trains per period (day/evening/night), train types, and travel speed. Residences located from railway, tram, and metro lines were classified as unexposed to railway noise. Cohorts from Denmark and Gothenburg included information on noise barriers. Ground absorption was considered in all estimations.
Aircraft noise.
For the Danish cohorts (DCH and DNC), aircraft noise was estimated in 5-dB categories based on noise maps generated by local authorities for individual airports and airfields using the Danish Airport Noise Simulation Model (Plovsing and Svane 1990) and the Integrated Noise Model (Boeker et al. 2008). For the four Stockholm cohorts, aircraft noise was estimated in 1-dB categories based on noise maps generated by Swedavia using the Integrated Noise Model (Boeker et al. 2008). Aircraft noise maps were updated at varying time intervals. Because aircraft noise was modeled in 5-dB intervals in the Danish cohorts and because of variations in modeling over time and between airports/airfields, aircraft noise was operationalized as a categorical variable with three categories: , 40.1–50, . Aircraft noise was not estimated for participants in the Malmö (MDC) and Gothenburg (PPS and GOT-MONICA) cohorts because few residences were exposed.
Outcome
Information on stroke was based on linkage to the nationwide Danish and Swedish Patient and Mortality registries. The Danish and Swedish registers are very similar and known to have high validity and completeness with regard to cardiovascular diagnoses (Ludvigsson et al. 2011; Schmidt et al. 2015). Participants diagnosed with a stroke before their NordSOUND baseline were excluded. The main outcome was incident stroke [categorized according to the International Classification of Disease, Eighth Revision (ICD 8; WHO 1966), the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM; CDC 2013), or the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10; WHO 2016) as ICD-8 and ICD-9 codes 431–434 and 436 and ICD-10 codes I61–I64]. In subtype analyses, we defined ischemic stroke as ICD-8 codes 432–434, ICD-9 codes 433–434, or ICD-10 code I63; hemorrhagic stroke as ICD-8 code 431, ICD-9 codes 431–432, or ICD-10 codes I61–I62; and unspecified stroke as ICD-8 and ICD-9 code 436 and ICD-10 code I64. In subtype analyses, we combined unspecified strokes with ischemic strokes. Secondary analyses also addressed stroke-fatality, with a fatal stroke defined as an incident stroke resulting in death within .
Covariates
Covariates were selected a priori. This was done based on a review of existing literature (indicating association with both exposure and outcome) and the availability of homogeneous variables or data that could be harmonized across cohorts.
At enrollment into the original cohorts, all participants completed questionnaires concerning dietary and lifestyle characteristics, including smoking status (never, former, current), smoking intensity (in grams tobacco per day; not available for PPS), alcohol consumption (daily, weekly, seldom, never; not available for PPS), leisure-time physical activity, and body mass index (BMI, measured by trained staff at enrollment in all cohorts except DNC and SALT, where it was self-reported). Data on educational level (low, medium, high) and marital status (married/cohabiting, single) were obtained from national registries or questionnaires, and area-level income data (the percentage of residents in each national income quartile within small socioeconomically homogeneous areas with inhabitants) were obtained from national registries.
Annual address-specific mean concentrations of particulate matter (PM) with an aerodynamic diameter of () and nitrogen dioxide () were estimated for all addresses (5 y before baseline to the end of follow-up) using dispersion models with high spatial resolution (see Table S3 for details). Briefly, for all cohorts, the exposure was estimated as a sum of local, regional and long-range contributions, using input data on local sources (e.g., road traffic, residential heating, shipping, industry), meteorology, and monitoring station measurements.
Statistical Methods
We used Cox proportional hazards models, with age as the underlying timescale, to estimate stroke hazard ratios (HRs), using separate models for overall stroke, stroke subtypes (ischemic, hemorrhagic, and ischemic/unspecified) and stroke-fatality (information not available for MDC). We followed each cohort member from their NordSOUND baseline until a) stroke; b) death (obtained through linkage with Swedish and Danish nationwide registers); c) emigration or loss to follow-up [information on emigration and loss to follow-up (no residential address recorded) was obtained through linkage with Swedish and Danish nationwide registers]; or d) end of follow-up (31 December 2011–31 December 2017 for the different cohorts), whichever occurred first.
HRs were estimated for each 10-dB increase in road and railway noise, modeled as time-weighted means (energy-weighted) over 1- and 5-y periods preceding stroke onset, taking all addresses in these periods into account. All road and railway noise values were set to 40 dB because of the high risk of imprecision of low-level noise estimates. In addition, all models of railway noise as a continuous variable also included a categorical indicator variable for any exposure vs. none (i.e., if all residences were from a railway line). We also used separate models to estimate HRs for 5-y mean road and railway noise exposures categorized into 5-dB intervals, using as the reference for both exposures. Aircraft noise was included only as a categorical variable with three categories: , 40.1–50, . Participants in the three cohorts that lacked information on aircraft noise (PPS, GOT-MONICA, and MDC) were assigned to the category when estimating associations with road or railway noise adjusted for aircraft noise but were excluded when estimating associations with aircraft noise.
We analyzed the association between transportation noise and stroke in four models with increasing adjustment. Model 1 was adjusted for age (by design), cohort, sex, and calendar year (5-y categories). Model 2, which was selected as the primary model a priori, was additionally adjusted for educational status (low, medium, high), marital status (married/cohabiting, single), area-level income (quartiles), and other transportation noise sources. In Model 3, we further included lifestyle factors: smoking status (never, former, current), physical activity (low, medium, high), and BMI (in kilograms per meter squared). In Model 4, we added time-weighted exposure to (1- or 5-y mean) to Model 2. Because the present analysis was limited to cohort participants with complete data for all covariates in Models 1–3 (other than aircraft noise), Models 1–3 were based on the same observations. In contrast, Model 4 was performed as a complete case analysis limited to participants with exposure data (10,349 total cases). Therefore, we repeated Model 2 after excluding participants without data to further assess the influence of adjustment.
The assumption of linearity of continuous variables in Model 3 with all strokes as outcome [road traffic noise (5-y), railway noise (5-y), and BMI] was evaluated using smoothed splines with 4 degrees of freedom (df) (Figures S1 and S2). Deviation from linearity was observed for BMI, which was therefore included as a linear spline with a cut point at . The proportional hazards assumption was tested by a correlation test between scaled Schoenfeld residuals and the rank order of event time. Deviation from the assumption was detected for sex, educational level, smoking, physical activity, and BMI (; Table S4). Sex, educational level, smoking, and physical activity were, therefore, included as strata, whereas BMI was kept in the model as a linear variable to avoid loss of information from categorization. All models were stratified by cohort, thereby allowing different baseline hazards across cohorts.
We investigated cohort-specific associations between traffic noise and stroke by running the primary model (Model 2) for each cohort separately and by running leave-one-out analyses, omitting the cohorts one by one.
We investigated effect modification of the association between road traffic noise and stroke by sex (male/female), BMI ( or ), physical activity (low/medium/high), smoking status (never/former/current), educational level (low/medium/high), calendar year ( or ), and ( or ) by including interaction terms between the potential effect modifiers and the 5-y mean noise exposure, and we tested interaction by the Wald test. Last, we estimated associations between road traffic noise and stroke among persons and of age. We focused on 5-y mean road traffic noise in these analyses because almost all participants were exposed to this noise source, giving high statistical power to the analyses.
In sensitivity analyses, we additionally adjusted Model 3 for smoking intensity (in grams tobacco per day; continuous) and alcohol intake (daily, weekly, seldom, never) in cohorts with data available (excluding PPS), and, for comparison, repeated the model without adjustment among those with complete data for both variables (9,493 total cases). Prior to this analysis, we evaluated the assumption of linearity for smoking intensity using smoothed splines with 4 df (Figure S2). In addition, we repeated Model 2 with and without additional adjustment for in analyses limited to participants with complete exposure data (10,558 total cases).
Analyses were performed in SAS (version 9.4; SAS Institute) and R (version 3.2.3; R Development Core Team).
Results
Of the 149,894 persons included in the original cohorts, we excluded 1,720 with stroke before the NordSOUND baseline, 1,594 with missing noise exposure data for the 5 y preceding the baseline, and 10,629 with missing data for covariates included in Models 2 and 3, leaving 135,951 persons for the study. Of these, 11,056 were classified as incident stroke cases during a median follow-up of 19.5 y.
Table 1 presents baseline characteristics across cohorts. Most cohorts included middle-aged adults, the majority of whom had a secondary school degree or equivalent, were married/cohabiting, and practiced little leisure-time physical activity. There was a fairly even distribution of smoking status and area-level income. However, for most variables, there was some variation between cohorts.
Table 1.
Characteristics of the study population across included cohorts at the NordSOUND baseline.
| Variable | DCH | DNC | SDPP | Sixty | SNAC-K | SALT | MDC | PPS | GOT-MONICA | TOTAL |
|---|---|---|---|---|---|---|---|---|---|---|
| Enrollment area | Copenhagen, Aarhus | Denmark | Stockholm County | Stockholm County | Stockholm City | Stockholm County | Malmö | Gothenburg | Gothenburg | — |
| Total participants () | 54,339 | 26,456 | 7,561 | 3,915 | 2,472 | 6,316 | 27,255 | 5,294 | 2,343 | 135,951 |
| Original enrollmenta | 1993–1997 | 1993 or 1999 | 1992–1998 | 1997–1999 | 2001–2004 | 1998–2020 | 1991–1996 | 1970–1973 | 1985, 1990, or 1995 | — |
| End of follow-up | 2016 | 2014 | 2011 | 2016 | 2016 | 2017 | 2016 | 2011 | 2011 | — |
| Person-years | 987,291 | 455,741 | 116,694 | 63,976 | 24,296 | 91,331 | 484,520 | 132,861 | 37,945 | 2,391,655 |
| Stroke cases () | 5,048 | 1,381 | 157 | 344 | 384 | 587 | 2,045 | 1,012 | 98 | 11,056 |
| Ischemic strokes () | 2,207 | 596 | 124 | 260 | 270 | 444 | 1,757 | 579 | 71 | 6,308 |
| Hemorrhagic strokes () | 557 | 177 | 18 | 44 | 45 | 71 | 203 | 105 | 12 | 1,232 |
| Unspecified strokes () | 2,284 | 608 | 15 | 40 | 69 | 72 | 85 | 328 | 15 | 3,516 |
| Fatal cases ()b | 449 | 215 | 14 | 30 | 81 | 97 | — | 198 | 0 | 1,084 |
| Non-fatal cases ()b | 4,599 | 1,166 | 143 | 314 | 303 | 490 | — | 814 | 98 | 7,927 |
| Gender (%) | ||||||||||
| Men | 47.4 | 0 | 39.3 | 47.7 | 38.5 | 45.1 | 39.0 | 100 | 47.4 | 37.8 |
| Women | 52.6 | 100 | 60.7 | 52.3 | 61.5 | 54.9 | 61.0 | 0 | 52.6 | 62.2 |
| Age at inclusion | 56.3 (50.9–64.4) | 50.9 (45.0–71.7) | 48.0 (38.0–53.9) | 60.4 (60.3–60.8) | 72.4 (60.4–90.5) | 56.5 (44.5–79.6) | 57.9 (47.3–71.6) | 55.0 (49.8–60.0) | 50.1 (31.5–66.9) | 55.6 (45.7–70.3) |
| Educational level (%) | ||||||||||
| Low | 27.9 | 0 | 31.5 | 39.7 | 23.4 | 26.8 | 68.0 | 68.3 | 20.5 | 32.4 |
| Medium | 48.7 | 100 | 38.6 | 32.2 | 39.7 | 36.5 | 17.7 | 20.4 | 50.2 | 49.6 |
| High | 23.4 | 0 | 29.9 | 28.0 | 36.9 | 36.7 | 14.4 | 11.3 | 29.2 | 18.0 |
| Marital status (%) | ||||||||||
| Married/cohabiting | 76.8 | 71.4 | 83.5 | 74.2 | 48.8 | 67.7 | 65.4 | 85.8 | 69.0 | 72.9 |
| Single/divorced/widow(er) | 23.2 | 28.6 | 16.5 | 25.8 | 51.2 | 32.3 | 34.6 | 14.2 | 31.0 | 27.1 |
| Area-level income [quartile (%)] | ||||||||||
| 1 | 33.1 | 32.8 | 3.5 | 4.5 | 3.0 | 7.0 | 23.2 | 25.9 | 22.1 | 26.4 |
| 2 | 22.5 | 26.6 | 5.6 | 8.7 | 0.0 | 10.5 | 21.0 | 22.3 | 15.2 | 20.6 |
| 3 | 16.9 | 24.8 | 21.0 | 24.3 | 0.2 | 18.6 | 26.6 | 24.5 | 21.5 | 21.0 |
| 4 | 27.5 | 15.8 | 69.8 | 62.5 | 96.8 | 64.0 | 29.1 | 27.3 | 41.2 | 32.1 |
| Smoking Status (%) | ||||||||||
| Current | 36.3 | 35.3 | 26.4 | 21.1 | 15.2 | 20.3 | 28.2 | 40.0 | 27.9 | 32.3 |
| Former | 28.2 | 30.6 | 36.4 | 38.9 | 40.1 | 36.2 | 33.7 | 33.4 | 23.9 | 31.2 |
| Never | 35.6 | 34.1 | 37.2 | 40.1 | 44.7 | 43.6 | 38.1 | 26.7 | 48.2 | 36.4 |
| Physical activity (%) | ||||||||||
| Low | 51.7 | 6.9 | 65.8 | 69.1 | 74.5 | 54.6 | 50.3 | 25.3 | 17.5 | 42.9 |
| Medium | 19.5 | 66.5 | 26.6 | 23.4 | 18.7 | 36.3 | 21.1 | 59.1 | 62.2 | 32.5 |
| High | 28.8 | 26.7 | 7.7 | 7.5 | 6.8 | 9.1 | 28.6 | 15.6 | 19.7 | 24.6 |
| BMI | 25.5 (20.4–33.4) | 23.1 (19.2–30.2) | 25.1 (20.4–33.3) | 26.2 (21.0–34.3) | 25.4 (19.9–32.8) | 24.2 (19.6–30.5) | 25.3 (20.2–32.9) | 25.1 (20.7–30.5) | 24.5 (19.7–32.3) | 24.9 (20.0–32.6) |
| Smoking intensity (g tobacco/d)c | 15.1 (5.0–32.1) | 15.0 (3.0–25.5) | 15.0 (2.0–25.0) | 13.0 (2.0–25.0) | 10.0 (0.0–28.6) | 10.0 (2.0–25.0) | 14.0 (1.0–30.0) | — | 15.0 (4.0–25.0) | 15.0 (3.0–30.0) |
| Missing (%) | 0.7 | 1.9 | 0.0 | 0.0 | 1.9 | 0.0 | 0.0 | 100 | 0 | 5.5 |
| Alcohol intake (%) | ||||||||||
| Daily | 19.8 | 12.8 | 4.0 | 5.8 | 11.2 | 9.0 | 16.7 | — | 1.0 | 15.4 |
| Weekly | 59.1 | 60.0 | 65.1 | 39.9 | 48.1 | 63.1 | 34.4 | — | 35.3 | 53.5 |
| Seldom | 18.3 | 11.5 | 27.5 | 44.8 | 33.9 | 24.9 | 32.6 | — | 56.3 | 22.5 |
| Never | 2.9 | 15.7 | 3.4 | 9.5 | 6.8 | 3.0 | 16.4 | — | 7.3 | 8.6 |
| Missing | 0.1 | 2.5 | 0.3 | 0.1 | 0.0 | 0.0 | 1.6 | 100 | 0.8 | 4.8 |
Note: Values are expressed as medians and 5th–95th percentiles, unless otherwise stated. —, Not applicable; BMI, body mass index; DCH, Diet, Cancer and Health cohort; DNC, Danish Nurses Cohort; GOT-MONICA, Multinational Monitoring of Trends and Determinants in Cardiovascular Disease cohort (Gothenburg); MDC, Malmö Diet and Cancer Study; NordSOUND, Nordic Studies on Occupational and Traffic Noise in Relation to Disease; PPS, Primary Prevention Study cohort; SALT, Stockholm Screening Across the Lifespan Twin Study; SDPP, Stockholm Diabetes Prevention Program; Sixty, Stockholm 60 years old study; SNAC-K, Swedish National Study of Aging and Care in Kungsholmen.
Original enrollment period for each cohort.
Not available for the MDC; defined as incident stroke resulting in death within .
Among current smokers.
Table 2 presents baseline exposure to transportation noise and air pollution across cohorts. Median 5-y road traffic noise was 54.5 dB, with cohort-specific medians ranging from 40.3 to 57.5 dB. There was large variation across cohorts with regard to railway and aircraft noise. Baseline road traffic noise (all participants) and aircraft noise (among those with any exposure) showed a close-to-normal distribution, whereas railway noise (among those with any exposure) was skewed to the left (Figure S3). The correlation between 5-y road traffic noise and 1-y road traffic noise was 0.96, and correlations between 5-y road traffic and 5-y railway noise, , and were 0.12, 0.39, and 0.65, respectively (Table S5).
Table 2.
Baseline exposure to transportation noise () and air pollution across the included cohorts.
| Exposure | DCH | DNC | SDPP | Sixty | SNAC-K | SALT | MDC | PPS | GOT-MONICA | TOTAL |
|---|---|---|---|---|---|---|---|---|---|---|
| Road traffic noise [5-y (dB)] | 56.6 (45.0–69.3) | 53.6 (40.3–66.9) | 40.3 (40.0–54.3) | 46.6 (40.0–62.7) | 58.1 (46.2–68.2) | 47.4 (40.0–63.2) | 54.6 (42.4–67.5) | 57.5 (45.4–72.4) | 56.1 (40.0–69.2) | 54.5 (40.0–68.1) |
| Railway noise (% exposed)a | 25.9 | 19.1 | 14.5 | 31.8 | 51.6 | 34.3 | 28.1 | 15.3 | 19.4 | 24.9 |
| Railway noise [5-y (dB)]b | 52.3 (42.1–66.6) | 52.9 (41.8–65.9) | 50.4 (42.3–67.2) | 48.9 (40.9–63.6) | 49.0 (41.7–59.4) | 49.2 (40.7–64.2) | 46.8 (40.5–67.7) | 44.9 (40.4–58.8) | 44.5 (40.2–57.5) | 50.5 (41.0–66.0) |
| Aircraft noise {5-y [dB (%)]} | ||||||||||
| 98.6 | 98.8 | 74.7 | 83.5 | 15.3 | 83.3 | — | — | — | 95.0 | |
| 40.1–50 | 0.7 | 0.4 | 9.6 | 13.5 | 65.5 | 13.6 | — | — | — | 3.1 |
| 0.7 | 0.8 | 15.7 | 3.0 | 19.1 | 3.2 | — | — | — | 1.9 | |
| [5-y ()] | 19.2 (18.5–23.9) | 20.7 (15.4–26.1) | 7.6 (6.7–8.3) | 8.0 (6.8–9.5) | 8.3 (7.7–10.3) | 7.7 (6.4–9.2) | 11.0 (9.8–12.4) | — | 9.2 (7.1–11.6) | 18.7 (7.4–24.0) |
| Missing (%) | 0.0 | 9.0 | 0 | 0 | 0 | 0 | 0.0 | 100c | 0 | 5.6 |
| [5-y ()] | 27.5 (19.6–46.5) | 10.8 (5.6–28.1) | 8.6 (4.9–13.8) | 12.9 (5.3–26.0) | 20.3 (15.1–31.9) | 13.0 (5.5–25.3) | 24.2 (13.7–34.9) | 30.8 (23.1–43.5) | 28.0 (19.1–42.9) | 23.8 (7.0–40.2) |
| Missing (%) | 0.0 | 9.0 | 0 | 0 | 0 | 0 | 0.0 | 2.5 | 0 | 1.1 |
Note: Values are expressed as medians and 5th–95th percentiles unless otherwise stated. —, Not applicable; DCH, Diet, Cancer, and Health cohort; DNC, Danish Nurses Cohort; GOT-MONICA, Multinational Monitoring of Trends and Determinants in Cardiovascular Disease cohort (Gothenburg); , 24-h annual average noise level of road traffic noise; MDC, Malmö Diet and Cancer Study; , nitrogen dioxide; NordSOUND, Nordic Studies on Occupational and Traffic Noise in Relation to Disease; PPS, Primary Prevention Study cohort; SALT, Stockholm Screening Across the Lifespan Twin Study; SDPP, Stockholm Diabetes Prevention Program; Sixty, Stockholm 60 years old study; SNAC-K, Swedish National Study of Aging and Care in Kungsholmen.
Exposed to in the 5-y period preceding the NordSOUND baseline. Residences from a railway line were classified as unexposed.
Among persons exposed to railway noise .
PPS only had information on from baseline until follow-up.
Road traffic noise was associated with stroke, with an estimated (95% CI: 1.03, 1.08) per 10-dB increase in 5-y exposure based on the main model (Model 2, Table 3). The association followed a close-to-linear exposure–response relationship when modeled as a categorical variable (Figure 1A; Table S6) and using smoothed splines (Figure S1). Adjustment for lifestyle factors (Model 3) and (Model 4) resulted in only marginal changes in the association. Model 4 was calculated among persons with available. However, Model 2 rendered the same HR when run only in this subset of the study population (Table S7).
Table 3.
Association between traffic noise exposure and stroke incidence.
| Exposure | Cases () | Model 1 [HR (95% CI)]a | Model 2 [HR (95% CI)]b | Model 3 [HR (95% CI)]c | Model 4 [HR (95% CI)]d |
|---|---|---|---|---|---|
| Road traffic noise [years exposure, per 10 dB ()] | |||||
| 1 | 11,056 | 1.07 (1.04, 1.09) | 1.05 (1.03, 1.08) | 1.05 (1.02, 1.07) | 1.06 (1.03, 1.08) |
| 5 | 11,056 | 1.07 (1.04, 1.10) | 1.06 (1.03, 1.08) | 1.05 (1.02, 1.07) | 1.06 (1.03, 1.09) |
| Railway noise [years exposure, per 10 dB ()] | |||||
| 1 | 11,056 | 0.97 (0.92, 1.02) | 0.96 (0.91, 1.01) | 0.96 (0.92, 1.01) | 0.96 (0.91, 1.01) |
| 5 | 11,056 | 0.97 (0.92, 1.02) | 0.96 (0.91, 1.01) | 0.96 (0.91, 1.01) | 0.96 (0.91, 1.01) |
| Aircraft noise {dB [5-y exposure ()]}e | |||||
| 7,347 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |
| 40.1–50 | 396 | 1.11 (0.98, 1.26) | 1.12 (0.99, 1.27) | 1.14 (1.00, 1.30) | 1.12 (0.99, 1.28) |
| 158 | 0.91 (0.77, 1.08) | 0.94 (0.79, 1.11) | 0.98 (0.82, 1.17) | 0.93 (0.78, 1.11) | |
Note: BMI, body mass index; CI, confidence interval; GOT-MONICA, Multinational Monitoring of Trends and Determinants in Cardiovascular Diseases cohort (Gothenburg); HR, hazard ratio; , 24-h annual average noise level of road traffic noise; MDC, Malmö Diet and Cancer Study; , particulate matter with an aerodynamic diameter of (fine particulate matter); PPS, Primary Prevention Study cohort; Ref, reference.
Model 1: adjusted for age, cohort (strata), sex (strata), and calendar year (in 5-y periods); and in analyses of railway noise: railway noise (yes/no).
Model 2: Model 1 plus adjustment for educational level (strata; low, medium, high), marital status (married/cohabiting, single), area income (quartiles), and other noise sources (road and rail (continuous), railway noise (yes/no), aircraft noise (, 40–50, ; for the three cohorts without aircraft noise information, all cohort members were assigned to the group).
Model 3: Model 2 plus adjustment for smoking status (strata; never, former, current), physical activity (strata; low, medium, high), and BMI (, continuous).
Model 4: Model 2 plus adjustment for time-weighted exposure (1- or 5-y). exposure history available for 10,349 cases.
Among cohorts with estimation of aircraft noise exposure (thus excluding MDC, PPS, and GOT-MONICA), including 7,901 cases (7,735 in analyses including ; for aircraft noise analyses in Model 4, there were 7,182 cases exposed to , 396 cases exposed to 40.1–50 dB, and 157 cases exposed to ).
Figure 1.
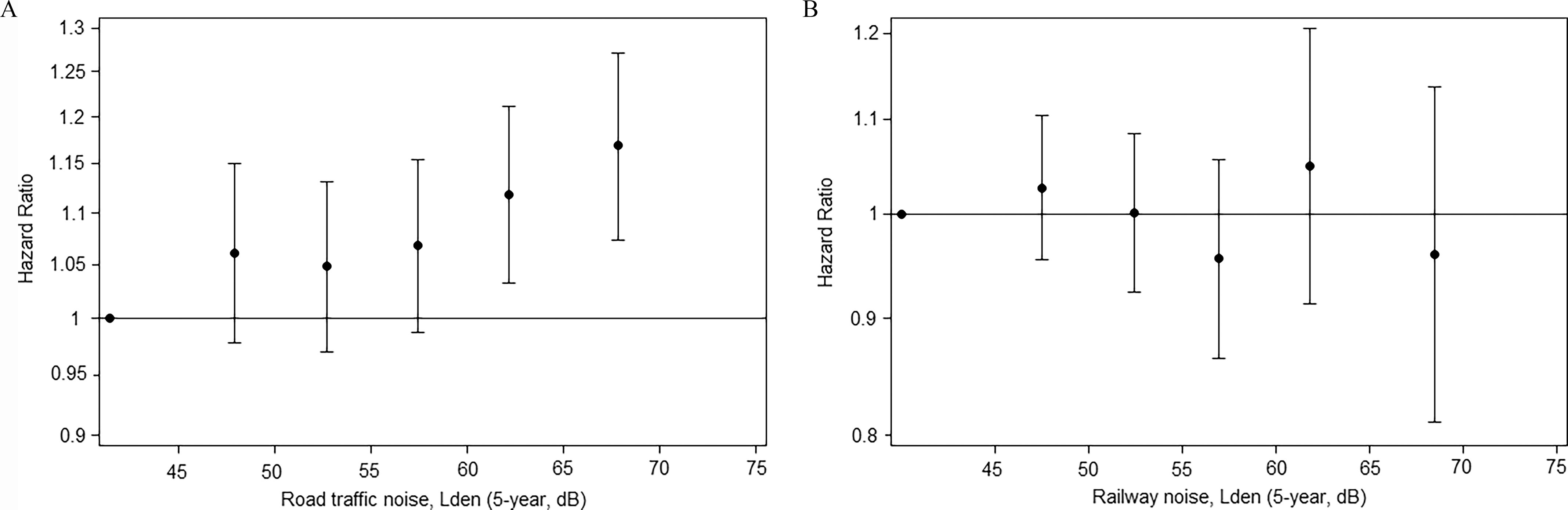
Exposure–outcome relationship between 5-y exposure to (A) road traffic noise and (B) railway noise and risk for stroke in models adjusted for age, sex, calendar year, educational level, marital status, area income, and other noise sources. The vertical whiskers show HRs with 95% CIs positioned at the median of each exposure category, compared with the reference category [see Table S6 for HRs (95% CIs), and numbers of cases]. Note: CI, confidence interval; HR, hazard ratio, , 24-h annual average noise level of road traffic noise.
Cohort-specific analyses indicated that road traffic noise was associated with a higher risk of stroke in DCH, DNC, SDPP, Sixty, and PPS, whereas no associations were found in SNAC-K, SALT, MDC, and GOT-MONICA (Table S8). One-by-one exclusion (leave-one-out analyses) of the three largest cohorts (DCH, MDC, and DNC) in analyses of 5-y road traffic noise and stroke resulted in HRs of 1.03 (95% CI: 1.00, 1.07), 1.06 (95% CI: 1.03, 1.09), and 1.05 (95% CI: 1.03, 1.08), respectively. Leave-one-out analyses for the remaining cohorts had little influence on the risk estimates (1.05–1.06 for all; Table S9).
Railway noise was not associated with stroke, regardless of the exposure time window or adjustment level (Table 3), and analyses did not support a monotonic exposure–outcome relationship (Figure 1B; Table S6). For aircraft noise, Model 2 HRs were 1.12 (95% CI: 0.99, 1.27) and 0.94 (95% CI: 0.79, 1.11) for those exposed to 40.1–50 dB and , respectively, compared with (Table 3).
We found no suggestion of effect modification of the association between road traffic noise and stroke by BMI, education, or calendar year, but stronger associations were suggested among persons exposed to vs. (), current smokers compared with former and never smokers (), and potentially those with low or medium physical activity compared with high physical activity () (Figure 2; Table S10). Model 2 HRs for a 10-dB increase in 5-y road traffic noise and stroke before and after 70 years of age were 1.08 (95% CI: 1.04, 1.12) and 1.04 (95% CI: 1.00, 1.07), respectively.
Figure 2.
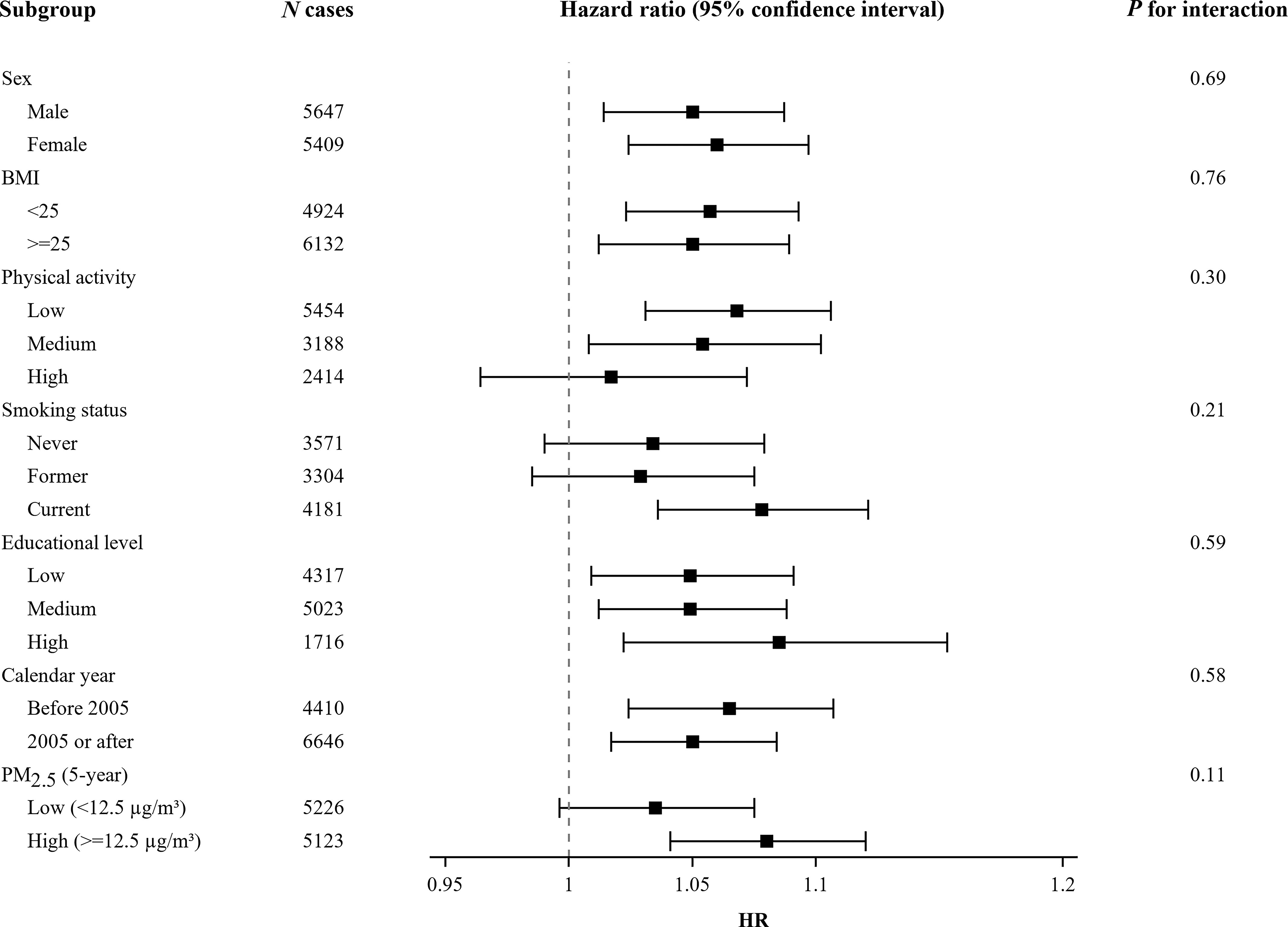
HRs (95% CI) for 10-dB increases in 5-y road traffic noise exposure and stroke incidence according to strata of potential effect modifiers based on separate models with interaction terms between road traffic noise and each potential modifier, adjusted for age, sex, calendar year, educational level, marital status, area income, and other noise sources (see Table S10 for numeric data) -Values are Wald terms. Note: BMI, body mass index; CI, confidence interval; HR, hazard ratio.
In analyses concerning stroke-fatality, Model 2 HRs for nonfatal and fatal strokes with a 10-dB increase in 5-y road traffic noise were 1.07 (95% CI: 1.03, 1.10) and 1.03 (95% CI: 0.95, 1.12), respectively (Table 4). Corresponding HRs for subtypes of stroke were 1.03 (95% CI: 0.95, 1.11) for hemorrhagic strokes, 1.03 (95% CI: 0.99, 1.06) for ischemic strokes, and 1.06 (95% CI: 1.03, 1.09) for the combined group of ischemic and unspecified strokes. The Danish cohorts accounted for 82% of the unspecified strokes. Railway noise was not associated with any of the stroke subtypes.
Table 4.
Association between 5-y exposure to road traffic and railway noise (per 10 dB) and stroke subtypes and fatality.
| Road/Railway noise exposure and disease subgroups | Cases () | Model 2 [HR (95% CI)]a | Model 3 [HR (95% CI)]b | Model 4 [HR (95% CI)]c |
|---|---|---|---|---|
| Road traffic noise | ||||
| All strokes | 11,056 | 1.06 (1.03, 1.08) | 1.06 (1.02, 1.07) | 1.06 (1.03, 1.09) |
| Fatalityd | ||||
| Fatal strokes | 1,084 | 1.03 (0.95, 1.12) | 1.02 (0.94, 1.11) | 1.04 (0.95, 1.13) |
| Non-fatal strokes | 7,927 | 1.07 (1.03, 1.10) | 1.06 (1.02, 1.09) | 1.06 (1.03, 1.10) |
| Stroke subtypes | ||||
| Hemorrhagic stroke | 1,232 | 1.03 (0.95, 1.11) | 1.02 (0.95, 1.11) | 1.05 (0.97, 1.14) |
| Ischemic stroke | 6,308 | 1.03 (0.99, 1.06) | 1.02 (0.98, 1.05) | 1.05 (1.01, 1.09) |
| 9,824 | 1.06 (1.03, 1.09) | 1.05 (1.02, 1.08) | 1.06 (1.03, 1.09) | |
| Railway noise | ||||
| All strokes | 11,056 | 0.96 (0.91, 1.01) | 0.96 (0.92, 1.01) | 0.96 (0.91, 1.01) |
| Fatalityd | ||||
| Fatal strokes | 1,084 | 0.93 (0.79, 1.09) | 0.92 (0.78, 1.08) | 0.92 (0.78, 1.09) |
| Non-fatal strokes | 7,927 | 0.97 (0.91, 1.03) | 0.97 (0.91, 1.03) | 0.97 (0.91, 1.03) |
| Stroke subtypes | ||||
| Hemorrhagic stroke | 1,232 | 0.92 (0.79, 1.07) | 0.93 (0.80, 1.08) | 0.88 (0.75, 1.03) |
| Ischemic stroke | 6,308 | 0.95 (0.90, 1.01) | 0.96 (0.90, 1.02) | 0.95 (0.89, 1.01) |
| 9,824 | 0.96 (0.92, 1.02) | 0.96 (0.92, 1.01) | 0.97 (0.92, 1.02) | |
Note: BMI, body mass index; CI, confidence interval; HR, hazard ratio; , particulate matter with an aerodynamic diameter of (fine particulate matter).
Model 2: adjusted for age, cohort (strata), sex (strata), calendar year (in 5-y periods), educational level (strata, low, medium, high), marital status (married/cohabiting, single), area income (quartiles), and other noise sources (road and rail continuous), railway noise (yes/no), aircraft noise (, 40–50, ; for the three cohorts without aircraft noise information, all cohort members were assigned to the group).
Model 3: Model 2 plus adjustment for smoking status (strata, never, former, current), physical activity (strata, low, medium, high), and BMI (, continuous).
Model 4: Model 2 plus adjustment for time-weighted exposure (5-y running mean). exposure history available for 10,349 cases.
Data on fatality were not available for the 2,045 cases in the MDC-cohort; defined as incident stroke resulting in death within .
In sensitivity analyses adjusted for smoking intensity and alcohol consumption, estimates were similar to Model 2 estimates based on participants with available data (Table S7). In analyses adjusted for , the associations were still present, with (95% CI: 1.00, 1.07) for a 10-dB increase in 5-y road traffic noise exposure.
Discussion
In this pooled study of nine Scandinavian cohorts, 1- and 5-y residential exposures to road traffic noise were associated with an increased risk of incident stroke, with a monotonic exposure–outcome relationship. Associations were robust to adjustment for socioeconomic and lifestyle factors and adjustment for air pollution ( and ), and there were no clear differences according to gender, calendar year, or baseline educational level, physical activity, or BMI. We found suggestions of an interaction with smoking and . The association with road traffic noise seemed to be stronger for nonfatal strokes than fatal strokes. Railway noise was not associated with stroke, and although moderate exposure to aircraft noise was positively associated with stroke (relative to little or no exposure), there was no evidence of an increase in risk among those with higher exposure.
These findings add to the relatively limited and inconsistent evidence base on transportation noise and stroke. Similar to our results, two large registry-based studies of road traffic noise, one with residents around Frankfurt Airport, and one with London residents, reported an increased risk of incident stroke, with estimates of (95% CI: 1.00, 1.03) per 10 dB (Seidler et al. 2018) and RR 1.05 (95% CI: 1.02, 1.09) for vs. , respectively (Halonen et al. 2015). However, these studies had limited information on potential confounders, and Halonen et al. (2015) estimated noise levels at the postal-code level, which increases the likelihood of exposure misclassification (Vienneau et al. 2019). In general, findings from studies with more detailed questionnaire-based information on confounders have been inconsistent: A pooled analysis of three cohorts from Norway/UK () found no association between road traffic noise and stroke (Cai et al. 2018), but 85% of cases came from Norway (cohort with mean follow-up of 14.1 y), where road traffic noise was relatively low (). In addition, noise was estimated at the baseline address only, in contrast with our time-varying exposure estimates based on all residences during follow-up. Findings for road traffic noise and stroke have also previously been reported for six of the nine cohorts in the present study. A positive association was reported for the Swedish PPS cohort based on the same cases included the present analysis (Andersson et al. 2020) and for the Danish DCH cohort based on 1,881 cases (Sørensen et al. 2011), which in the present study was expanded to 5,048 DCH cases owing to 7 additional years of follow-up. A pooled analysis of the four Stockholm cohorts (SDPP, Sixty, SNAC-K, and SALT) indicated no association overall, but a positive association for the SDPP in cohort-specific analyses was suggested (Pyko et al. 2019). Follow-up time for the present analysis was extended 5–6 y for the Sixty, SNAC-K, and SALT cohorts, resulting in 1,472 cases for the four cohorts combined (vs. 902 in the previous analysis), and we estimated a positive association for the Sixty cohort, as well as for the SDPP, whereas HRs remained null for SNAC-K and SALT. Similar to the Norwegian cohort included in the analysis by Cai et al. (2018), the Stockholm cohorts were characterized by low levels of traffic noise (). Thus, with the exception of studies conducted in populations with low exposures, previous findings have generally supported an association between road traffic noise and the risk of stroke.
Particulate air pollution (i.e., ) increases the risk of cardiovascular disease (Brook et al. 2010), and mutual adjustment is important because and , correlates with road traffic noise. We found the association between road traffic noise and stroke to be robust to adjustment for and , which suggests that road traffic noise is a risk factor for stroke independent of traffic-related air pollution, consistent with most previous studies of road traffic noise and cardiovascular outcomes [as reviewed by Tétreault et al. (2013)] and noted more recently by Héritier et al. (2019) for a large Swiss cohort. Interestingly, our results suggested a possible interaction between and road traffic noise, with an (95% CI: 1.04, 1.12) per 10-dB increase in 5-y among those with higher 5-y exposures () compared with (95% CI: 1.00, 1.08) for those with lower (). This suggests the possibility of synergistic effects, consistent with different biological mechanisms for particles and noise (Münzel et al. 2017). The association between road traffic noise and stroke was also stronger among current smokers (; 95% CI: 1.04, 1.12) compared with former and never smokers [ (95% CI: 0.99, 1.08) for both subgroups, ]. Previous studies that investigated combined effects of noise and air pollution in relation to cardiovascular disease have reported inconsistent results, and further evidence on this potentially important interaction is needed (Héritier et al. 2019; Sørensen et al. 2014; Tétreault et al. 2013).
We found no association between railway noise and stroke incidence. This is in line with a nationwide Swiss study on stroke mortality (Héritier et al. 2017) and a Swedish cohort study on stroke incidence (Pyko et al. 2019), whereas a large German case–control study reported that railway noise was associated with stroke incidence (Seidler et al. 2018). Weak and inconsistent findings for railway noise and stroke may reflect lower perceived annoyance compared with road traffic noise (Miedema and Vos 1998), as well as substantial regional/national differences in the amount of railway traffic during the night and the amount of freight train traffic. We also found no convincing association between aircraft noise and stroke given that the association was positive only for the moderate-exposure group (40–50 dB vs. little or no exposure). A potential explanation is the installation of noise-reducing windows and other noise abatement procedures among persons living close to an airport, which may result in a leveling off in risk estimates at high exposures, although it seems unlikely that this could drive the estimates to unity. Findings from previous prospective studies on aircraft noise and stroke incidence/mortality have been inconsistent (Hansell et al. 2013; Héritier et al. 2017; Pyko et al. 2019; Seidler et al. 2018). However, our results should be interpreted with caution because we had only 396 and 158 cases with low and high exposure to aircraft noise, respectively, in our study population.
Our finding of an association primarily with nonfatal strokes suggests that road traffic noise may affect the risk of mild-to-moderate strokes but not strokes with a more severe course. This might occur if noise had a greater influence on the risk of ischemic stroke than hemorrhagic stroke, which often has a more severe course than ischemic stroke (Andersen et al. 2009). In accordance with this, previous studies have reported associations primarily between transportation noise and ischemic strokes, whereas associations have been weak or null for hemorrhagic strokes (Héritier et al. 2017; Sørensen et al. 2014). We estimated comparable RR estimates for hemorrhagic and ischemic stroke. However, in our study population, 32% of the strokes were unspecified, and, given that of all strokes are ischemic (Go et al. 2013), the majority of the unspecified strokes were probably ischemic. When ischemic and unspecified strokes were combined into one group, associations were stronger than for hemorrhagic strokes. Therefore, our results do not necessarily contradict previous findings that suggest that transportation noise is mainly a risk factor for ischemic stroke. We are not aware of previous studies of noise and incident fatal stroke, but previous studies on road traffic noise and stroke mortality have been inconsistent (Beelen et al. 2009; Halonen et al. 2015; Héritier et al. 2017).
The strengths of the present study include a large study population with pooling and harmonization of cohort data from nine Scandinavian cohorts; information on stroke incidence and fatality from well-validated, national registries on hospitalization and mortality (Ludvigsson et al. 2011; Schmidt et al. 2015); information on a number of potential socioeconomic and lifestyle confounders; and complete address histories for all cohort members from national registries. In addition, all cohorts had information on modeled long-term exposure to air pollution at the residential level, estimated using dispersion models. Last, the diverse study populations from several cohorts allows for a higher generalizability of our findings than from a single-center study.
Study limitations include the cohort-specific estimation of noise, which did not follow a standardized protocol. However, all cohorts estimated both railway and road traffic noise using the Nordic prediction methods with comparable high-quality input data on traffic and screening from buildings and terrain. We were not able to precisely model very low noise exposure, and hence all road and railway noise exposures were set to 40 dB. Furthermore, aircraft noise was missing for three cohorts, and the data available for the Danish cohorts were rather crude (5-dB intervals). Another limitation is that 46% of the cases belonged to the DCH cohort, which could thus, to some extent, drive the findings. However, cohort-specific analyses showed road traffic noise to be associated with risk of stroke in five of the nine cohorts, and one-by-one exclusions of the nine cohorts yielded HRs in the range of 1.03–1.06, suggesting that the association was not carried by one specific cohort. Last, the inclusion of five covariates as strata in Model 3 because of deviation from the proportional hazard assumption resulted in 414 strata of which some had few or no stroke cases. This may reduce the risk estimates and result in wider CIs. However, HRs and CI widths are quite consistent across models with increasing levels of adjustment, which suggests that stratification did not affect model performance.
In summary, in this pooled, multicenter Scandinavian study, we found residential road traffic noise to be associated with a higher risk of incident stroke. In contrast, railway noise was not associated with stroke, and for the few persons exposed to aircraft noise, stroke was associated with low exposure, but there was no association among those in the high-exposure group. These findings add to the evidence of road traffic noise as an important cardiovascular risk factor that should be taken into account in future assessments of the public health implications of traffic noise.
Supplementary Material
Acknowledgments
This work was supported by NordForsk (grant 83597). Funding for the included cohorts is shown in Table S1.
References
- Andersen KK, Olsen TS, Dehlendorff C, Kammersgaard LP. 2009. Hemorrhagic and ischemic strokes compared: stroke severity, mortality, and risk factors. Stroke 40(6):2068–2072, PMID: 19359645, 10.1161/STROKEAHA.108.540112. [DOI] [PubMed] [Google Scholar]
- Andersson EM, Ögren M, Molnár P, Segersson D, Rosengren A, Stockfelt L. 2020. Road traffic noise, air pollution and cardiovascular events in a Swedish cohort. Environ Res 185:109446, PMID: 32278155, 10.1016/j.envres.2020.109446. [DOI] [PubMed] [Google Scholar]
- Babisch W. 2002. The noise/stress concept, risk assessment and research needs. Noise Health 4(16):1–11, PMID: 12537836, https://www.noiseandhealth.org/text.asp?2002/4/16/1/31833. [PubMed] [Google Scholar]
- Beelen R, Hoek G, Houthuijs D, van den Brandt PA, Goldbohm RA, Fischer P, et al. . 2009. The joint association of air pollution and noise from road traffic with cardiovascular mortality in a cohort study. Occup Environ Med 66(4):243–250, PMID: 19017691, 10.1136/oem.2008.042358. [DOI] [PubMed] [Google Scholar]
- Bendtsen H. 1999. The Nordic prediction method for road traffic noise. Sci Total Environ 235(1–3):331–338, 10.1016/S0048-9697(99)00216-8. [DOI] [Google Scholar]
- Berglund G, Elmstähl S, Janzon L, Larsson SA. 1993. The Malmo Diet and Cancer Study. Design and feasibility. J Intern Med 233(1):45–51, PMID: 8429286, 10.1111/j.1365-2796.1993.tb00647.x. [DOI] [PubMed] [Google Scholar]
- Boeker ER, Dinges E, He B, Fleming G, Roof CJ, Gerbi PJ, et al. . 2008. Integrated Noise Model (INM), Version 7.0, Technical Manual. Report No. FAA-AEE-08-01. Washington, DC: Federal Aviation Administration, U.S. Department of Transportation. [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA III, Brook JR, Bhatnagar A, Diez-Roux AV, et al. . 2010. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121(21):2331–2378, PMID: 20458016, 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Cai Y, Hodgson S, Blangiardo M, Gulliver J, Morley D, Fecht D, et al. . 2018. Road traffic noise, air pollution and incident cardiovascular disease: a joint analysis of the HUNT, EPIC-Oxford and UK Biobank cohorts. Environ Int 114:191–201, PMID: 29518662, 10.1016/j.envint.2018.02.048. [DOI] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention). 2013. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). http://www.cdc.gov/nchs/icd/icd9cm.htm [accessed 22 September 2021].
- Christensen JS, Raaschou-Nielsen O, Tjønneland A, Nordsborg RB, Jensen SS, Sørensen TI, et al. . 2015. Long-term exposure to residential traffic noise and changes in body weight and waist circumference: a cohort study. Environ Res 143(pt A):154–161, PMID: 26492400, 10.1016/j.envres.2015.10.007. [DOI] [PubMed] [Google Scholar]
- Eriksson A-K, Ekbom A, Granath F, Hilding A, Efendic S, Stenson C-G. 2008. Psychological distress and risk of pre-diabetes and type 2 diabetes in a prospective study of Swedish middle-aged men and women. Diabet Med 25(7):834–842, PMID: 18513304, 10.1111/j.1464-5491.2008.02463.x. [DOI] [PubMed] [Google Scholar]
- European Environment Agency. 2020. Environmental Noise in Europe—2020. Publications Office of the European Union. https://www.eea.europa.eu/publications/environmental-noise-in-europe/at_download/file [accessed 22 September 2021]. [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. . 2013. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation 127(1):e6–e245, PMID: 23239837, 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halonen JI, Hansell AL, Gulliver J, Morley D, Blangiardo M, Fecht D, et al. . 2015. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur Heart J 36(39):2653–2661, PMID: 26104392, 10.1093/eurheartj/ehv216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansell AL, Blangiardo M, Fortunato L, Floud S, de Hoogh K, Fecht D, et al. . 2013. Aircraft noise and cardiovascular disease near Heathrow Airport in London: small area study. BMJ 347:f5432, PMID: 24103537, 10.1136/bmj.f5432. [DOI] [PubMed] [Google Scholar]
- Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, de Hoogh K, et al. . 2019. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur Heart J 40(7):598–603, PMID: 30357335, 10.1093/eurheartj/ehy650. [DOI] [PubMed] [Google Scholar]
- Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, Thiesse L, et al. . 2017. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur J Epidemiol 32(4):307–315, PMID: 28280950, 10.1007/s10654-017-0234-2. [DOI] [PubMed] [Google Scholar]
- Hundrup YA, Simonsen MK, Jørgensen T, Obel EB. 2012. Cohort profile: the Danish Nurse Cohort. Int J Epidemiol 41(5):1241–1247, PMID: 21421694, 10.1093/ije/dyr042. [DOI] [PubMed] [Google Scholar]
- Lagergren M, Fratiglioni L, Hallberg IR, Berglund J, Elmståhl S, Hagberg B, et al. . 2004. A longitudinal study integrating population, care and social services data. The Swedish National study on Aging and Care (SNAC). Aging Clin Exp Res 16(2):158–168, PMID: 15195992, 10.1007/BF03324546. [DOI] [PubMed] [Google Scholar]
- Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim J-L, Reuterwall C, et al. . 2011. External review and validation of the Swedish National Inpatient Register. BMC Public Health 11:450. [Database], PMID: 21658213, 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson PKE, Almqvist C, Rahman I, Ganna A, Viktorin A, Walum H, et al. . 2013. The Swedish Twin Registry: establishment of a biobank and other recent developments. Twin Res Hum Genet 16(1):317–329, PMID: 23137839, 10.1017/thg.2012.104. [DOI] [PubMed] [Google Scholar]
- Miedema HM, Vos H. 1998. Exposure-response relationships for transportation noise. J Acoust Soc Am 104(6):3432–3445, PMID: 9857505, 10.1121/1.423927. [DOI] [PubMed] [Google Scholar]
- Münzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sørensen M. 2018. Environmental noise and the cardiovascular system. J Am Coll Cardiol 71(6):688–697, PMID: 29420965, 10.1016/j.jacc.2017.12.015. [DOI] [PubMed] [Google Scholar]
- Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. . 2017. Environmental stressors and cardio-metabolic disease: part II—mechanistic insights. Eur Heart J 38(8):557–564, PMID: 27460891, 10.1093/eurheartj/ehw294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plovsing B, Kragh J. 2006. Nord2000. Comprehensive Outdoor Sound Propagation Model. Part 1: Propagation in an Atmosphere without Significant Refraction. Revised report AV 1849/00. Hørsholm, Denmark: DELTA Acoustics & Vibration. [Google Scholar]
- Plovsing B, Svane C. 1990. DANSIM, Danish Airport Noise Simulation Model: basic principles, experience, and improvements. In: INTER-NOISE and NOISE-CON Congress and Conference Proceedings. InterNoise90, Gothenburg, Sweden. Reston, VA: Institute of Noise Control Engineering, 425–428. [Google Scholar]
- Pyko A, Andersson N, Eriksson C, de Faire U, Lind T, Mitkovskaya N, et al. . 2019. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: a cohort study. Occup Environ Med 76(4):201–207, PMID: 30804165, 10.1136/oemed-2018-105333. [DOI] [PubMed] [Google Scholar]
- Pyko A, Eriksson C, Lind T, Mitkovskaya N, Wallas A, Ögren M, et al. . 2017. Long-term exposure to transportation noise in relation to development of obesity—a cohort study. Environ Health Perspect 125(11):117005, PMID: 29161230, 10.1289/EHP1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. 2015. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490, PMID: 26604824, 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler AL, Hegewald J, Schubert M, Weihofen VM, Wagner M, Dröge P, et al. . 2018. The effect of aircraft, road, and railway traffic noise on stroke—results of a case–control study based on secondary data. Noise Health 20(95):152–161, PMID: 30136675, 10.4103/nah.NAH_7_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen M, Hvidberg M, Andersen ZJ, Nordsborg RB, Lillelund KG, Jakobsen J, et al. . 2011. Road traffic noise and stroke: a prospective cohort study. Eur Heart J 32(6):737–744, PMID: 21266374, 10.1093/eurheartj/ehq466. [DOI] [PubMed] [Google Scholar]
- Sørensen M, Lühdorf P, Ketzel M, Andersen ZJ, Tjønneland A, Overvad K, et al. . 2014. Combined effects of road traffic noise and ambient air pollution in relation to risk for stroke? Environ Res 133:49–55, PMID: 24906068, 10.1016/j.envres.2014.05.011. [DOI] [PubMed] [Google Scholar]
- Tétreault LF, Perron S, Smargiassi A. 2013. Cardiovascular health, traffic-related air pollution and noise: are associations mutually confounded? A systematic review. Int J Public Health 58(5):649–666, PMID: 23887610, 10.1007/s00038-013-0489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjønneland A, Olsen A, Boll K, Stripp C, Christensen J, Engholm G, et al. . 2007. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health 35(4):432–441, PMID: 17786808, 10.1080/14034940601047986. [DOI] [PubMed] [Google Scholar]
- van Kempen EV, Casas M, Pershagen G, Foraster M. 2018. WHO environmental noise guidelines for the European Region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health 15(2):379, PMID: 29470452, 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vienneau D, Héritier H, Foraster M, Eze IC, Schaffner E, Thiesse L, et al. . 2019. Façades, floors and maps—influence of exposure measurement error on the association between transportation noise and myocardial infarction. Environ Int 123:399–406, PMID: 30622064, 10.1016/j.envint.2018.12.015. [DOI] [PubMed] [Google Scholar]
- Wändell P-E, Wajngot A, de Faire U, Hellénius ML. 2007. Increased prevalence of diabetes among immigrants from non-European countries in 60-year-old men and women in Sweden. Diabetes Metab 33(1):30–36, PMID: 17258927, 10.1016/j.diabet.2006.07.001. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization). 1966. International Statistical Classification of Diseases and Related Health Problems, 8th Revision. Geneva, Switzerland: WHO. [Google Scholar]
- WHO. 2016. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. http://apps.who.int/classifications/icd10/browse/2016/en [accessed 22 September 2021].
- Wilhelmsen L, Berglund G, Elmfeldt D, Samuelsson O, Svardsudd K. 1986. The Multifactor Primary Prevention Trial in Göteborg, Sweden. Comparison with a previously untreated population sample. Drugs 31(suppl 1):47–51, PMID: 3720570, 10.2165/00003495-198600311-00009. [DOI] [PubMed] [Google Scholar]
- Wilhelmsen L, Johansson S, Rosengren A, Wallin I, Dotevall A, Lappas G. 1997. Risk factors for cardiovascular disease during the period 1985–1995 in Göteborg, Sweden. The GOT-MONICA Project. J Intern Med 242(3):199–211, PMID: 9350164, 10.1046/j.1365-2796.1997.00163.x. [DOI] [PubMed] [Google Scholar]
- Zare Sakhvidi MJ, Zare Sakhvidi F, Mehrparvar AH, Foraster M, Dadvand P. 2018. Association between noise exposure and diabetes: a systematic review and meta-analysis. Environ Res 166:647–657, PMID: 30006240, 10.1016/j.envres.2018.05.011. [DOI] [PubMed] [Google Scholar]
- Zhang S, Zhang W, Zhou G. 2019. Extended risk factors for stroke prevention. J Natl Med Assoc 111(4):447–456, PMID: 30878142, 10.1016/j.jnma.2019.02.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


